Abstract
Objectives
To systematically review current research applications of radiomics in patients with cholangiocarcinoma and to assess the quality of CT and MRI radiomics studies.
Methods
A systematic search was conducted on PubMed/Medline, Web of Science, and Scopus databases to identify original studies assessing radiomics of cholangiocarcinoma on CT and/or MRI. Three readers with different experience levels independently assessed quality of the studies using the radiomics quality score (RQS). Subgroup analyses were performed according to journal type, year of publication, quartile and impact factor (from the Journal Citation Report database), type of cholangiocarcinoma, imaging modality, and number of patients.
Results
A total of 38 original studies including 6242 patients (median 134 patients) were selected. The median RQS was 9 (corresponding to 25.0% of the total RQS; IQR 1–13) for reader 1, 8 (22.2%, IQR 3–12) for reader 2, and 10 (27.8%; IQR 5–14) for reader 3. The inter-reader agreement was good with an ICC of 0.75 (95% CI 0.62–0.85) for the total RQS. All studies were retrospective and none of them had phantom assessment, imaging at multiple time points, nor performed cost-effectiveness analysis. The RQS was significantly higher in studies published in journals with impact factor > 4 (median 11 vs. 4, p = 0.048 for reader 1) and including more than 100 patients (median 11.5 vs. 0.5, p < 0.001 for reader 1).
Conclusions
Quality of radiomics studies on cholangiocarcinoma is insufficient based on the radiomics quality score. Future research should consider prospective studies with a standardized methodology, validation in multi-institutional external cohorts, and open science data.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13244-023-01365-1.
Keywords: Systematic review, Cholangiocarcinoma, Liver, Quality improvement
Key points
The quality of current radiomics studies on cholangiocarcinoma is insufficient, with a median radiomics quality score of 8–10, corresponding to 22–28% of the ideal quality score.
None of the current studies conducted phantom assessment, imaging at multiple time points, prospective registration in a trial database, nor cost-effectiveness analysis.
The inter-reader agreement of the radiomics quality score is good (ICC of 0.75; 95% CI 0.62–0.85) among readers with different levels of experience.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13244-023-01365-1.
Introduction
Radiomics is a rapidly expanding area of active research with promising results based on the extraction and analysis of a large number of quantitative features from biomedical images [1]. Recent radiomics studies aimed to construct predictive models that can be combined with qualitative radiological features, clinical characteristics, and laboratory markers to develop decision support tools and improve patients’ care [1]. Several research studies proposed models based on computed tomography (CT) and magnetic resonance imaging (MRI) exams, with high performances for preoperative lesion characterization, prediction of treatment response, and assessment of prognosis after surgical resection [2]. Despite the promising results in research setting, there is still very limited translation in clinical practice due to the limitations of current radiomics research. These include heterogeneity of imaging acquisition protocols, segmentation, type of extracted features, and lack of validation in multicenter setting [3, 4]. Quality of radiomics studies represents a significant landmark for improvement of radiomics research and future clinical applications.
The radiomics quality score (RQS) has been proposed by Lambin et al. [5] for assessing the quality of radiomics studies based on 16 items related to the main steps of radiomics workflow. In the setting of liver imaging, recent systematic reviews have applied the RQS for assessment of quality of radiomics studies on hepatocellular carcinoma [6–9] and hepatic metastases [10] reporting an overall RQS of 8–14 (corresponding to 23–39% of the total score) and 10 (28%), respectively. Cholangiocarcinoma is the most common malignancy originating from the bile ducts and the second most common primary intrahepatic carcinoma [11]. Cholangiocarcinoma can occur in various location with heterogeneous imaging appearance on CT or MRI, and it is characterized by high biological aggressiveness and poor prognosis [11]. Recently, a growing number of radiomics applications have been proposed in patients with cholangiocarcinoma imaged with either CT or MRI, including differential diagnosis with other hepatic malignancies, prediction of lymph node metastasis, and prediction of recurrence after curative resection. However, to date the quality of radiomics studies in cholangiocarcinoma has not been comprehensively investigated. Assessment of quality in radiomics research studies is a necessary and fundamental step for the improvement of radiomics research and future implementation in clinical practice.
This systematic review aims to provide an overview of the current research applications of radiomics in patients with cholangiocarcinoma and to assess the quality of CT and MRI radiomics studies.
Materials and methods
This study was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines [12]. The review protocol was registered on the International Prospective Register of Systematic Reviews (CRD42022295218).
Literature search strategy
A systematic search was conducted to identify studies on PubMed/Medline, Web of Science, and Scopus databases using the following terms: “texture,” “radiomics,” “machine learning,” “artificial intelligence,” “cholangiocarcinoma” and “biliary cancer.” Detailed search strings are reported in the Additional file 1. The literature search was performed for articles published between 01/01/2010 and 30/11/2021.
Eligibility criteria
After removal of duplicate studies, three Authors (R.Ca., F.V., and L.U., radiologists, each with five years of experience in radiomics studies) independently evaluated the titles and abstracts of all studies to exclude ineligible papers according to the following criteria: (1) non-English studies; (2) animal studies; (3) abstracts of conference papers; (4) reviews, systematic reviews, and case reports. The full texts of the relevant articles were read to determine their inclusion. The following eligibility criteria were applied during full-text manuscript review for the inclusion of original papers: (1) radiomics studies based on the evaluation of quantitative features obtained from tumor segmentations of cholangiocarcinoma; (2) features extracted from CT or MRI exams. Studies assessing only semantic features, other lesions than cholangiocarcinoma, or features on other diagnostic exams (i.e., ultrasound or PET/CT due to their limited applications in cholangiocarcinoma) were excluded. Any disagreement between reviewers was resolved with consensus discussion.
Data extraction
The following data were collected from the included studies: authors, journal with its type, journal ranking according to quartile and impact factor, year of publication of the study and country based on the Institutions in which the CT/MRI of the study population exams were acquired. The journals were classified into imaging, clinical, and computer science according to the main journal category of Web of Science. The journal quartile, according to the main journal scientific sector, and impact factor were retrieved from the Journal Citation Report database, and the quartile and impact factor of the year of publication were registered. For articles published in 2021–2022, the 2020 reports were considered as this is the last available at the time of data analysis. The full manuscripts were assessed to collect the following data: type of the study (retrospective or prospective), number of involved Institutions, total number of included patients (divided into training and validation cohorts), type of cholangiocarcinoma (i.e., intrahepatic, perihilar, or extrahepatic), imaging modality (CT and/or MRI), sequences and/or phases in which the segmentation was performed, software used for segmentation and imaging analysis, and number of extracted radiomics features.
The studies were grouped according to the main purpose of investigation: diagnostic (including radiomics analysis for the differential diagnosis among hepatic lesions, prediction of tumor histopathological differentiation and markers, or lymph node involvement), prognostic (prediction of early recurrence and survival), and treatment response (response to locoregional or systemic treatments) studies.
Radiomics quality score assessment
Three different readers from distinct Institutions and with different levels of experience (Reader 1, R1, A.P., a radiologist with 4 years of experience in radiomics research and with experience on the RQS assessment, Reader 2, R2, M.E.K., a radiologist with 10 years of experience in radiological research and 4 years of experience in radiomics research, and Reader 3, R3, E.P., a radiologist with 9 years of experience in radiological research), not involved in manuscript screening, independently evaluated all the studies using the RQS [5]. Before the manuscript assessment, a training session was held to discuss the main items of the RQS and examples on manuscripts not included in this systematic review. Both full-text manuscripts and Supplementary Materials were screened. The RQS consists of 16 items divided by three main checkpoints: the first checkpoint includes item 1, the second includes items from 2 to 4, and the third is composed by items from 5 to 16 [5]. The detailed description of the RQS is available in the Additional file 2: Table S1. The total RQS (ranging from − 8 to + 36) and the percentage of the total score (0–100%) were recorded from all three readers [5].
Statistical analysis
Categorical variables were reported as numbers, proportions, and percentages, while continuous variables were reported as medians and interquartile ranges (IQR), after testing for normal distribution by applying the Shapiro–Wilk normality test. Adherence rate to the reporting quality of the RQS was calculated for the most experience reader (R1), considering the proportion of articles obtaining at least one point in each specific item. Differences in total RQS according to publication and study characteristics were evaluated by using the Kruskal–Wallis or the Mann–Whitney U test, as appropriate. The correlation between total RQS, journal impact factor, and number of included patients was calculated by using the Spearman’s rank correlation coefficient (Spearman’s ρ).
The intraclass correlation coefficient (ICC) with 95% confidence intervals (CI), based on an absolute-agreement with 2-way mixed-effects model, was used to assess the inter-reader agreement in the total and percentage RQS among the three readers. Agreement was categorized as poor (ICC < 0.50), moderate (ICC = 0.50–0.75), good (ICC = 0.75–0.90), or excellent (ICC > 0.90) [13].
A p value < 0.05 was considered to be statistically significant. Statistical analyses were conducted by using the SPSS Software (v26.0. IBM, Armonk, NY, USA).
Results
Literature search
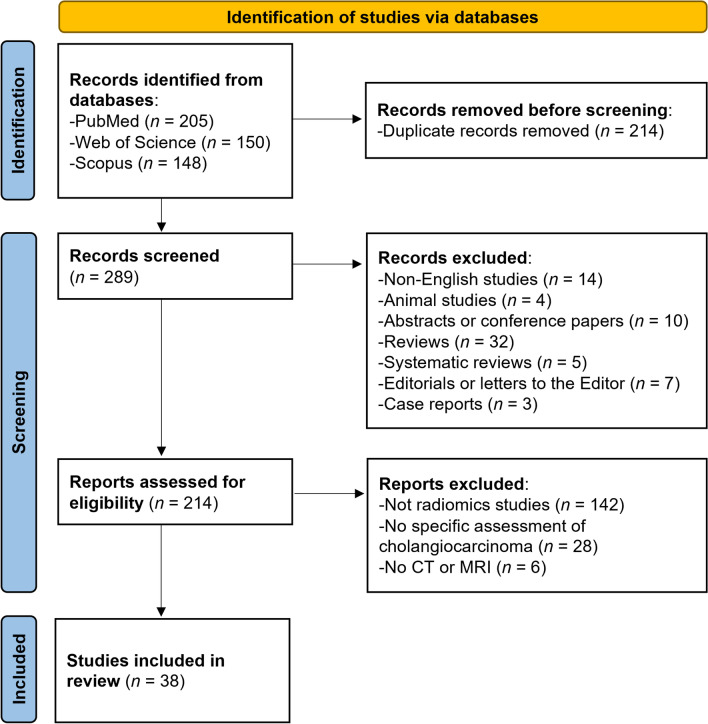
The systematic search initially identified 503 articles (Fig. 1). After removing 214 duplicated manuscripts, 289 were screened by their title and abstracts, and 214 studies underwent full-text screening to assess their eligibility. Finally, 38 original articles on radiomics of cholangiocarcinoma were included for RQS assessment [14–51].
Fig. 1.
Flow diagram of the study selection process
Characteristics of the included studies
The characteristics of included publications are summarized in Table 1. Among the included original articles, 18/38 (47.4%) were published in an imaging journal, 15/38 (39.5%) in a clinical journal, and the remaining (5/38, 13.1%) in a computer science journal. Twenty-one (55.3%) articles were published in 2021, 9/38 (23.7%) in 2020, 5/38 (13.2%) in 2019, and 3/38 (7.8%) in 2018 or earlier years. The 17/38 (44.7%) of included articles were published in first quartile journals, with an overall median impact factor of 4.43 (IQR, 3.50–5.31). The study population most frequently originated from China (27/38, 71.1%), followed by the USA (3/38, 7.8%). Thirty (79.0%) studies were performed at one Institution, 7/38 (18.4%) were performed in two Institutions, and only one (2.6%) involved six different Centers. All the included studies were conducted retrospectively.
Table 1.
General characteristics of the included studies
| Articles | Journal | Journal type | Publication year | Quartile* | Impact factor* | Country | Centers |
|---|---|---|---|---|---|---|---|
| Chu [14] | Eur Radiol | Imaging | 2021 | Q1 | 5,315 | China | Two |
| Duda [15] | Studies in Logic, Grammar and Rhetoric | Computer science | 2013 | Q2 | NA | France | Two |
| Hamn [16] | Eur Radiol | Imaging | 2019 | Q1 | 4,101 | US | Single |
| Huang [17] | Eur J Cancer | Clinical | 2021 | Q1 | 9,162 | China | Single |
| Ji [18] | Eur Radiol | Imaging | 2019 | Q1 | 4,101 | China | Single |
| Ji [19] | Radiology | Imaging | 2019 | Q1 | 7,931 | China | Single |
| King [20] | Cancer Imaging | Imaging | 2020 | Q2 | 3,909 | US | Single |
| Liang [21] | Front Oncol | Clinical | 2018 | Q2 | 4,137 | China | Single |
| Liu [22] | Eur Radiol | Imaging | 2021 | Q1 | 5,315 | Canada | Single |
| Mosconi [23] | Eur Radiol | Imaging | 2020 | Q1 | 5,315 | Italy | Two |
| Nakai [24] | Jpn J Radiol | Imaging | 2021 | Q3 | 2,374 | Japan | Single |
| Park [25] | Eur Radiol | Imaging | 2021 | Q1 | 5,315 | Korea | Six |
| Park [26] | Korean J Radiol | Imaging | 2021 | Q2 | 3,500 | Korea | Single |
| Ponnoprat [27] | Med Biol Eng Comput | Computer science | 2020 | Q3 | 2,602 | Thailand | Single |
| Qin [28] | Liver Int | Clinical | 2020 | Q2 | 5,828 | China | Two |
| Sadot [29] | PLoS One | Clinical | 2015 | Q1 | 3,057 | US | Single |
| Silva [30] | Abdom Radiol | Imaging | 2021 | Q2 | 3,039 | Italy | Single |
| Tang [31] | BMC Cancer | Clinical | 2021 | Q2 | 4,430 | China | Single |
| Tang [32] | World J Surg Oncol | Clinical | 2021 | Q2 | 2,754 | China | Single |
| Wang [33] | Comput Biol Med | Computer science | 2021 | Q1 | 4,598 | China | Single |
| Wang [34] | Front Oncol | Clinical | 2021 | Q2 | 6,244 | China | Two |
| Xu [35] | Technol Cancer Res Treat | Computer science | 2021 | Q3 | 3,399 | China | Single |
| Xu [36] | Phys Med Biol | Imaging | 2021 | Q2 | 3,609 | China | Single |
| Xu [37] | Theranostics | Clinical | 2019 | Q1 | 8,579 | China | Single |
| Xue [38] | Front Oncol | Clinical | 2021 | Q2 | 6,244 | China | Two |
| Xue [39] | Abdom Radiol | Imaging | 2021 | Q2 | 3,039 | China | Two |
| Yang [40] | Cancer Lett | Clinical | 2020 | Q1 | 8,679 | China | Single |
| Yao [41] | JMIR Med Inform | Computer science | 2020 | Q3 | 2,955 | China | Single |
| Zhang [42] | ESMO Open | Clinical | 2020 | Q1 | 6,540 | China | Single |
| Zhang [43] | Ann Transl Med | Clinical | 2020 | Q3 | 3,932 | China | Single |
| Zhang [44] | Ann Transl Med | Clinical | 2020 | Q3 | 3,932 | China | Single |
| Zhang [45] | Eur Radiol | Imaging | 2021 | Q1 | 5,315 | China | Single |
| Zhao [46] | Eur J Radiol | Imaging | 2021 | Q2 | 5,315 | China | Single |
| Zhao [47] | J Magn Reson Imaging | Imaging | 2021 | Q1 | 4,813 | China | Single |
| Zhao [48] | Cancer Imaging | Imaging | 2019 | Q3 | 2,193 | China | Single |
| Zhou [49] | Eur Radiol | Imaging | 2021 | Q1 | 5,315 | China | Single |
| Zhu [50] | Sci Rep | Clinical | 2021 | Q1 | 4,380 | China | Single |
| Zhu [51] | Sci Rep | Clinical | 2021 | Q2 | 4,380 | China | Single |
Journal quartile and impact factor are based on the year of publication. For articles published in 2021–2022 the 2020 data were considered
NA not available
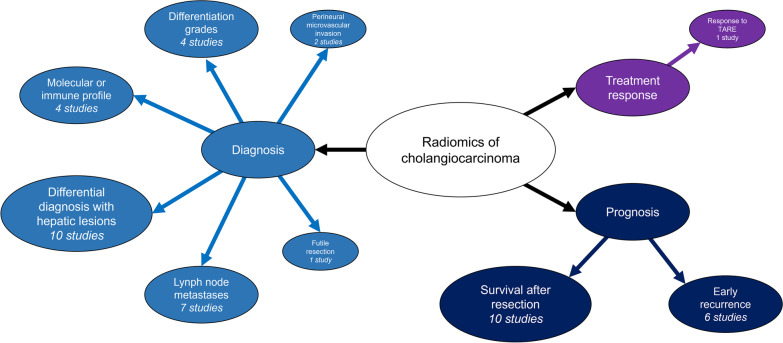
Study purpose and methodology are detailed in Table 2. The most common study aims (Fig. 2) included differential diagnosis against other hepatic lesions (10/38, 26.3%), prediction of survival after surgical resection (10/38, 26.3%), and prediction of lymph node metastases (7/38, 18.4%). Only one article explored the potential of radiomics for the prediction of therapeutic response to radioembolization in intrahepatic cholangiocarcinoma [23]. The total number of patients was 6242 (median = 134 per study; IQR, 98–198). Intrahepatic, perihilar, and extrahepatic cholangiocarcinoma were assessed in 29/38 (76.3%), 4/38 (10.5%), and 5/38 (13.2%) papers, respectively. CT was the most commonly used imaging technique (20/38, 52.6%), while MRI was adopted in 16/38 (42.1%) studies. Only two (5.3%) used both techniques. Lesion segmentations for radiomics features extraction were more commonly performed in the hepatic arterial phase (27/38, 71.1%) and/or portal venous phase (25/38, 65.8%), almost always by manually drawing the region of interest (35/38, 92.1%). Segmentation of the peritumoral or adjacent hepatic parenchyma was performed in only 5/38 (13.1%) studies.
Table 2.
Main purposes and methodology of the included studies
| Articles | Purpose | CCA type | Patients (training; validation) | Imaging modality | Sequences for analysis | Segmentation method | Software | Number of features |
|---|---|---|---|---|---|---|---|---|
| Chu [14] | Prediction of futile resection | Intrahepatic | 203 (142; 61) | CT | PVP | Manual | ITK-SNAP; A.K. software v2.0.0 | 1044 |
| Duda [15] | Differential diagnosis between HCC and iCCA | Intrahepatic | 76 | CT | PRE-HAP-PVP | Manual | In-house | 61 |
| Hamn [16] | Differential diagnosis among hepatic lesions | Intrahepatic | 494 (434; 60) | MRI | HAP-PVP-DP | Manual | Python v3.5 | NA |
| Huang [17] | Prediction of stage, perineural, and microvascular invasion | Extrahepatic | 101 | MRI | T1-T2-DWI-ADC | Manual | MadZa v4.6 | 1208 |
| Ji [18] | Prediction of lymph node metastasis and survival | Intrahepatic | 155 (103; 52) | CT | HAP | Manual | 3D Slicer v4.9.0 | 105 |
| Ji [19] | Prediction of lymph node metastasis and survival | Extrahepatic | 247 (177; 70) | CT | PVP | Manual | ITK-SNAP v3.6; Python | 93 |
| King [20] | Prediction of tumor grade and survival | Intrahepatic | 73 | CT/MRI | PRE-HAP-PVP | Manual | Osirix v5.5.2; MATLAB vR2016b | 14 |
| Liang [21] | Prediction of early recurrence | Intrahepatic | 209 (139; 70) | MRI | HAP | Manual | ITK-SNAP v3.6; MATLAB R2015a | 467 |
| Liu [22] | Differential diagnosis between HCC, iCCA, and cHCC-CCA | Intrahepatic | 85 | CT/MRI | PRE-HAP-PVP-DP-HBP-DWI-T2-In-Phase | Manual | MintLesion + Pyradiomics v2.1.2 | 1419 |
| Mosconi [23] | Prediction of response to radioembolization | Intrahepatic | 55 | CT | HAP-PVP-DP | Manual | LIFEx | 8 |
| Nakai [24] | Differential diagnosis between HCC and iCCA | Intrahepatic | 617 (493; 62 + 62) | CT | PRE-HAP-DP | Manual | RectLabel v3.02.7; Python v3.6.4; PyTorch v1.5.0 | NA |
| Park [25] | Prediction of survival after surgical resection | Intrahepatic | 354 (233; 112) | CT | HAP-PVP | Manual | In-house (AsanFEx); MATLAB R2015a | 661 |
| Park [26] | Prediction of survival after surgical resection | Intrahepatic | 89 | CT | HAP | Automatic; semi-automatic | Syngo.via Frontier, RADIOMCIS prototype | 19 |
| Ponnoprat [27] | Differential diagnosis between HCC and iCCA | Intrahepatic | 257 | CT | PRE-HAP-PVP-DP | Automatic | NA | NA |
| Qin [28] | Prediction of early recurrence | Perihilar | 274 (167; 70 + 37) | CT | HAP-PVP-DP | Manual | RadiAnt DICOM Viewer v4.6.5; MATLAB v9.2.0; Mazda v4.6 | 18,120 |
| Sadot [29] | Correlation with molecular profile | Intrahepatic | 25 | CT | HAP-PVP | Semi-automatic | MATLAB | 5 |
| Silva [30] | Prediction of survival after surgical resection | Intrahepatic | 78 | CT | PVP | Manual | 3D Slicer v4.10.2 | 108 |
| Tang [31] | Prediction of lymph node metastasis and differentiation | Extrahepatic | 100 | MRI | T1-T2-DWI-ADC | Manual | Madza v4.6 | 1200 |
| Tang [32] | Prediction of survival after surgical resection | Intrahepatic | 101 | CT | PVP | Manual | LIFEx v3.74 | 42 |
| Wang [33] | Differential diagnosis between HCC, iCCA, and cHCC-CCA | Intrahepatic | 196 | MRI | HAP-PVP-DP | Manual | ITK-SNAP v3.6; Pyradiomics | 1316 |
| Wang [34] | Prediction of lymph node metastasis | Perihilar | 179 | CT | HAP | Manual | ITK-SNAP | 1067 |
| Xu [35] | Differential diagnosis between iCCA and lymphoma | Intrahepatic | 129 | CT | DP | Manual |
LIFEx v3.74, Python v3.6.4 |
45 |
| Xu [36] | Prediction of early and late recurrence | Intrahepatic | 209 (159; 50) | MRI | T2 | Manual | ITK-SNAP; MATLAB | 2268 |
| Xu [37] | Prediction of lymph node metastasis | Intrahepatic | 148 (106; 42) | MRI | HAP | Manual |
ITK-SNAP; MATLAB V2017b |
491 |
| Xue [38] | Diagnosis of iCCA in patients with intrahepatic lithiasis | Intrahepatic | 131 (96; 35) | CT | HAP | Manual | LIFEx | 52 |
| Xue [39] | Differential diagnosis between iCCC and inflammatory masses | Intrahepatic | 145 (110; 35) | CT | HAP-PVP | Manual | LIFEx | 52 |
| Yang [40] | Prediction of lymph node metastasis and differentiation | Extrahepatic | 100 (80; 20) | MRI | T1-T2-DWI | Manual | MaZda v4.6 | 300 |
| Yao [41] | Prediction of lymph node metastasis and differentiation | Extrahepatic | 110 (88; 22) | MRI | T1-T2-DWI-ADC | Manual | MaZda v4.6 | 300 |
| Zhang [42] | Prediction of PD-1/PD-L1 and survival | Intrahepatic | 98 | MRI | HAP-PVP | Manual |
ITK-SNAP; AK software |
NA |
| Zhang [43] | Prediction of survival after surgical resection | Intrahepatic | 136 | MRI | DP-DWI | Manual | AK software | 384 |
| Zhang [44] | Differential diagnosis between iCCA and cHCC-CCA | Intrahepatic | 186 (132; 57) | CT | HAP-PVP | Manual |
ITK-SNAP v3.6; AK software |
396 |
| Zhang [45] | Prediction of immunophenotyping and survival | Intrahepatic | 78 | MRI | PRE-HAP-PVP-DWI-T2 | Manual | ITK-SNAP v3.6; Pyradiomics | 1037 |
| Zhao [46] | Prediction of survival after surgical resection | Perihilar | 184 (110; 74) | MRI | HAP-PVP | Manual |
ITK-SNAP v3.6; AK software v3.2.2 |
396 |
| Zhao [47] | Prediction of early recurrence | Perihilar | 184 (128; 56) | MRI | HAP-PVP | Manual |
ITK-SNAP v3.6; AK software v3.2.3 |
402 |
| Zhao [48] | Prediction of early recurrence | Intrahepatic | 47 | MRI | HAP-PVP-DP-T2 | Manual |
ITK-SNAP v2.2.0; AK software |
396 |
| Zhou [49] | Prediction of microvascular invasion | Intrahepatic | 126 (88; 38) | MRI | HAP-PVP-DP | Manual | ITK-SNAP v3.6: Pyradiomics v2.12 | 2364 |
| Zhu [50] | Prediction of IDH mutation | Intrahepatic | 138 | CT | PRE-HAP-PVP-DP | Manual | Pyradiomics | 72 |
| Zhu [51] | Prediction of early recurrence | Intrahepatic | 125 (92; 33) | CT | PRE-HAP-PVP-DP | Manual | Pyradiomics | 87 |
ADC apparent diffusion coefficient; CCA cholangiocarcinoma; cHCC-CCA combined hepatocellular-cholangiocarcinoma; CT computed tomography; DP delayed phase; DWI diffusion weighted imaging; HAP hepatic arterial phase; HBP hepatobiliary phase; HCC hepatocellular carcinoma; iCCA intrahepatic cholangiocarcinoma; MRI magnetic resonance imaging; NA not available; PRE pre-contrast phase; PVP portal-venous phase
Fig. 2.
Overview of radiomics research purposes. Notably each study could include multiple purposes
Radiomics quality score
Results of the total RQS by the three independent readers are summarized in Table 3. Details on the items’ score by each reader are provided in the Additional file 2: Tables S2, S3, and S4. The median RQS was 9 (corresponding to the 25.0% of the total RQS; IQR 1–13) for R1, 8 (22.2%, IQR 3–12) for R2, and 10 (27.8%; IQR 5–14) for R3. The inter-reader agreement for was good with an ICC of 0.75 (95% CI 0.62–0.85) for the total RQS and 0.77 (95% CI 0.65–0.86) for the RQS percentage scores.
Table 3.
Total radiomics quality score (RQS) with percentage of the total score of the included studies assessed by three independent readers
| Reader 1 | Reader 2 | Rader 3 | ||||
|---|---|---|---|---|---|---|
| Articles | Total | Percentage | Total | Percentage | Total | Percentage |
| Chu [14] | 11 | 30.6% | 11 | 30.6% | 14 | 38.9% |
| Duda [15] | 1 | 2.8% | −1 | 0% | −6 | 0% |
| Hamn [16] | 3 | 8.3% | 8 | 22.2% | 7 | 19.4% |
| Huang [17] | 8 | 22.2% | 4 | 11.1% | 5 | 13.9% |
| Ji [18] | 16 | 44.4% | 13 | 36.1% | 15 | 41.7% |
| Ji [19] | 14 | 38.9% | 15 | 41.7% | 14 | 38.9% |
| King [20] | −4 | 0% | −5 | 0% | 2 | 5.6% |
| Liang [21] | 12 | 33.3% | 14 | 38.9% | 6 | 16.7% |
| Liu [22] | 1 | 2.8% | 5 | 13.9% | −2 | 0% |
| Mosconi [23] | 0 | 0% | 5 | 13.9% | −2 | 0% |
| Nakai [24] | 4 | 11.1% | 6 | 16.7% | 14 | 38.9% |
| Park [25] | 18 | 50.0% | 18 | 50.0% | 17 | 47.2% |
| Park [26] | −2 | 0% | 3 | 8.3% | −4 | 0% |
| Ponnoprat [27] | 9 | 25.0% | 2 | 5.6% | 11 | 30.6% |
| Qin [28] | 15 | 41.7% | 11 | 30.6% | 15 | 41.7% |
| Sadot [29] | −5 | 0% | −4 | 0% | −1 | 0% |
| Silva [30] | −1 | 0% | 5 | 13.9% | −3 | 0% |
| Tang [31] | 8 | 22.2% | 7 | 19.4% | 13 | 36.1% |
| Tang [32] | 13 | 36.1% | 8 | 22.2% | 15 | 41.7% |
| Wang [33] | −1 | 0% | −1 | 0% | 2 | 5.6% |
| Wang [34] | 12 | 33.3% | 14 | 38.9% | 13 | 36.1% |
| Xu [35] | 9 | 25.0% | 10 | 27.8% | 12 | 33.3% |
| Xu [36] | 10 | 27.8% | 9 | 25.0% | 7 | 19.4% |
| Xu [37] | 16 | 44.4% | 13 | 36.1% | 13 | 36.1% |
| Xue [38] | 13 | 36.1% | 15 | 41.7% | 13 | 36.1% |
| Xue [39] | 11 | 30.6% | 16 | 44.4% | 14 | 38.9% |
| Yang [40] | 8 | 22.2% | 7 | 19.4% | 9 | 25.0% |
| Yao [41] | 9 | 25.0% | 9 | 25.0% | 11 | 30.6% |
| Zhang [42] | 8 | 22.2% | 2 | 5.6% | 5 | 13.9% |
| Zhang [43] | 2 | 5.6% | 6 | 16.7% | 4 | 11.1% |
| Zhang [44] | 15 | 41.7% | 12 | 33.3% | 14 | 38.9% |
| Zhang [45] | 3 | 8.3% | −1 | 0% | 9 | 25.0% |
| Zhao [46] | 15 | 41.7% | 12 | 33.3% | 6 | 16.7% |
| Zhao [47] | 15 | 41.7% | 13 | 36.1% | 15 | 41.7% |
| Zhao [48] | −2 | 0% | −2 | 0% | 6 | 16.7% |
| Zhou [49] | 9 | 25.0% | 11 | 30.6% | 12 | 33.3% |
| Zhu [50] | −5 | 0% | 3 | 8.3% | 11 | 30.6% |
| Zhu [51] | 13 | 36.1% | 12 | 33.3% | 9 | 25.0% |
|
Median (IQR) |
9 (1–13) |
25.0 (2.8–36.1) |
8 (3–12) |
22.1 (8.3–33.3) |
10 (5–14) |
27.8 (13.9–38.9) |
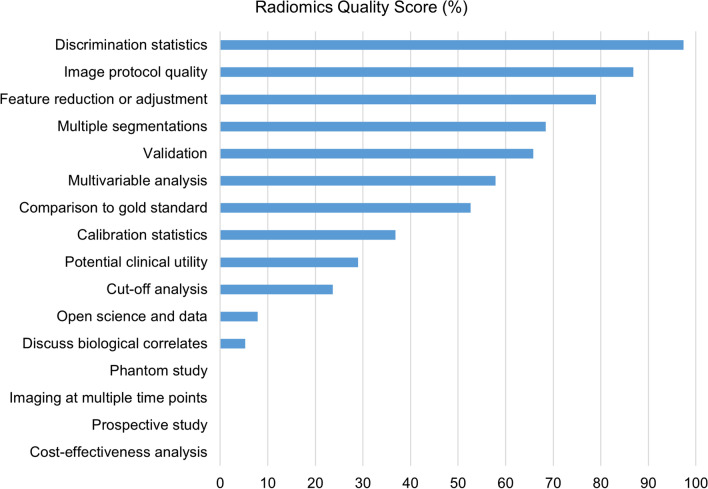
Adherence rate of each item (according to R1) is illustrated in Fig. 3. For the first checkpoint (item 1), 33/38 (88.6%) studies provided a well-documented image protocol. In the second checkpoint (items from 2 to 4), 26/38 (68.4%) studies had multiple segmentations, but none performed phantom assessment or imaging at multiple time points. In the third checkpoint (items from 5 to 16), feature reduction and adjustment for multiple tests was employed in 30/38 (78.9%) cases, with non-radiomics features included in 22/38 (57.9%) multivariate analyses. Only two (5.3%) articles discussed biological correlates related to the radiomics models. Cutoff analyses, discrimination statistics, and calibration statistics were available in 9/38 (23.7%), 37/38 (97.4%), and 14/38 (36.8%) investigations, respectively. Regarding the validation of the radiomics models, in most studies (23/38, 60.5%) it was based on an internal cohort, but validation was lacking in 13/38 (34.2%) investigations. Comparison with the gold standard and discussion of potential clinical utility were addressed in 20/38 (52.6%) and 11/38 (28.9%) studies, respectively. None of the assessed article was prospectively registered in a trial database or provided cost-effectiveness analysis, and only three (7.9%) made their code or data publicity available.
Fig. 3.
Adherence rate to the reporting quality of each item included in the radiomics quality score according to the most experienced reader (R1)
Subgroup analyses
Results of the subgroup analyses are reported in Table 4. No statistical differences were found according to the type of journal, year of publication, journal quartile, type of included cholangiocarcinoma, and imaging modalities. None of the RQS items (according to R1) was significantly higher in first quartile journals (p ≥ 0.101). Journals with impact factors > 4 published studies with significantly higher RQS according to the R1 (p = 0.048) and R2 (p = 0.035). The RQS was significantly higher in studies including more than 100 patients (p < 0.001 for all the readers).
Table 4.
Subgroup analyses of total radiomics quality score assessed by the three independent readers
| Reader 1 | Reader 2 | Reader 3 | |||||
|---|---|---|---|---|---|---|---|
| Group | N | RQS total | p value | RQS total | p value | RQS total | p value |
| Journal type | 0.542 | 0.302 | 0.562 | ||||
| Imaging | 18 | 6.5 (0–14) | 8.5 (4.5–13) | 8 (1–14) | |||
| Clinical | 15 | 12 (8–13) | 8 (4–13) | 11 (5–13) | |||
| Computer science | 5 | 9 (1–9) | 2 (−1 to 9.5) | 11 (−2 to 11.5) | |||
| Publication year | 0.772 | 0.322 | 0.352 | ||||
| 2021 | 21 | 9 (2–13) | 9 (4.5–12.5) | 12 (5.5–14) | |||
| 2013–2020 | 17 | 8 (0.5–14.5) | 7 (0.5–12.5) | 7 (3–13.5) | |||
| Journal quartile | 0.787 | 0.510 | 0.814 | ||||
| Q1 | 17 | 8 (0.5–14.5) | 7 (2.5–13) | 9 (3.5–14) | |||
| Q2 | 14 | 11.5 (0.5–13) | 10 (4.5–14) | 8 (0.7–13.2) | |||
| Q3 | 7 | 9 (2–9) | 6 (2–10) | 11 (6–14) | |||
| Impact factor | 0.048 | 0.035 | 0.224 | ||||
| ≤ 4 | 15 | 4 (−2 to 10) | 6 (−1 to 9) | 7 (−1 to 14) | |||
| > 4 | 23 | 11 (3–15) | 11 (5–13) | 11 (6–14) | |||
| Cholangiocarcinoma | 0.074 | 0.124 | 0.152 | ||||
| Intrahepatic | 29 | 8 (−0.5 to 12.5) | 6 (2–12) | 9 (2–13.5) | |||
| Perihilar/extrahepatic | 9 | 12 (8–15) | 11 (7–13.5) | 13 (7.5–14.5) | |||
| Imaging modality | 0.361 | 0.206 | 0.067 | ||||
| CT | 20 | 11 (0.2–13.7) | 10.5 (3.5–13.7) | 13 (1.5–14) | |||
| MRI/MRI and CT | 18 | 8 (1.7–10.5) | 7 (1.2–11.2) | 6.5 (4.7–11.2) | |||
| Number of patients | < 0.001 | < 0.001 | < 0.001 | ||||
| ≤ 100 | 12 | 0.5 (−2 to 6.7) | 2.5 (−1.7 to 5) | 0.5 (−2.7 to 8.2) | |||
| > 100 | 26 | 11.5 (8.7–15) | 11 (7.5–13.2) | 12.5 (7–14) | |||
Continuous variables are expressed as medians and interquartile range (25th to 75th percentile) in parenthesis. Continuous variables were compared using the Kruskal–Wallis or the Mann–Whitney U test. Statistically significant values (p < 0.05) are highlighted in bold
CT, Computed Tomography; MRI, Magnetic Resonance Imaging
For all the three readers, there was a statistically significant high correlation between the total RQS and number of included patients (p < 0.001 for all the readers) (Table 5). No significant correlation was observed between the total RQS and other characteristics.
Table 5.
Correlation between total radiomics quality score assessed by three independent readers, journal impact factor, number of included patients, and number or radiomics features
| Reader 1 | Reader 2 | Reader 3 | |
|---|---|---|---|
|
Journal impact factor p value |
0.315 0.057 |
0.288 0.083 |
0.089 0.602 |
|
Number of patients p value |
0.593 < 0.001 |
0.587 < 0.001 |
0.596 < 0.001 |
|
Number of features p value |
0.265 0.130 |
0.160 0.368 |
0.200 0.256 |
Numbers represent the Spearman’s rank correlation coefficient (ρ), unless otherwise specified. Statistically significant values (p < 0.05) are highlighted in bold
Discussion
Inadequate quality of radiomics studies is emerging as a major issue of current literature, contributing to the slow transition from research to clinical application in this field [52]. This systematic review of 38 radiomics studies on cholangiocarcinoma demonstrates a suboptimal quality of the current publications assessed through the RQS, with an overall total score of 8–10, corresponding to about one quarter of the ideal quality for this type of study. This is in line with other systematic reviews based on the RQS assessing radiomics of hepatic lesions, reporting a median RQS of 8–14 corresponding to 23–39% of the total score [6–10]. Importantly, in this review none of the included studies had phantom assessment, imaging at multiple time points, prospective registration in a trial database, nor performed cost-effectiveness analysis. These items account for 10 points (28%) of the total RQS [5].
Radiomics has been applied as a diagnostic tool for the differential diagnosis between cholangiocarcinoma and other hepatic tumors, for preoperative identification of histopathological and molecular markers associated with poor prognosis, and for predicting postoperative survival, while there is still a very limited experience on therapeutic response and advanced lesions that were not suitable for surgical resection [23]. To date, all studies on radiomics of cholangiocarcinoma are retrospective, mostly based on a single-center dataset with lack of validation cohorts in 34% of them. This is a relevant issue, determining a loss of 5 points in the total RQS, as external validation is a key item prior to clinical implementation of classification models. Only the study by Park et al. [25] validated a radiomics model for the prediction of postoperative outcome in patients with intrahepatic cholangiocarcinoma in an external test dataset from five different institutions (obtaining the maximum score of + 5 points in item 12 of the RQS). This means that even though most studies focused on radiomics of cholangiocarcinoma have a great potential, their results are still confined to the academic centers where the model originated. Further investigations should focus on the validation of existing models in a multicentric context rather than proposing alternative models based on a single-center experiences. Prospective validation of the radiomics models is also needed to evaluate their potential in clinical practice focusing on relevant patients’ outcomes such us evaluation of overall survival after treatment. In this setting, open science data providing the code and radiomics data is of utmost importance to facilitate the widespread application of radiomics and the reproducibility of the proposed models. Nevertheless, less than 10% of studies included in this systematic review made their code or data publicity available.
Despite the need of well-conducted radiomics workflow has been emphasized over the last years, the quality of published radiomics papers on cholangiocarcinoma according to the RQS has not increased when comparing 2021 versus 2013–2020. High-impact journals have provided guidance highlighting the need for robust data and accurate methodology for radiomics research [1, 53, 54]. However, the analysis of current cholangiocarcinoma studies demonstrates no significant difference in the RQS based on the journal type or quartile, even though a tendency of higher RQS was observed in journals with impact factor greater than 4 in two out of three readers. In prior studies, no difference according to journal metrics were found by Spadarella et al. [55] in RQS of nasopharyngeal cancer studies, while Ponsiglione et al. [56] and Chang et al. [57] observed significantly higher RQS in journals with higher impact factor or quartile for cardiac imaging studies, respectively. Therefore, the explosion of research on radiomics, machine learning, and data-based science led to an increased number of published radiomics papers not followed by a significant increase in quality of those studies. This may be related to the overall tendency to perform and publish explorative radiomics studies based on the novelty of the topic rather than to improve the strict methodology and workflow of radiomics analysis [52, 58]. Standardization of the acquisition protocols in liver imaging is a fundamental effort in order to minimize the variability of radiomics features across centers and scanners [59]. Furthermore, the International Biomarker Standardization Initiative (IBSI) is working toward standardization of extraction of quantitative features extracted from medical images and it already provided reference values for radiomics features on CT [60].
The RQS provides a detailed description of each item’s score [5]. However, its application can be affected by the reader’s experience and interpretation of each item according to the data available in the papers. All the studies included in this review were evaluated by three independent readers with different levels of research experience and RQS assessment, which resulted in a good inter-observer agreement. Few studies evaluated the reproducibility of the RQS with discordant results (reported ICC between 0.57 and 0.99) and, to our knowledge, none of these studies evaluated the inter-observed agreement in readers from different Institutions [55, 61–63]. It should be noted that the RQS is based on expert opinion and currently not endorsed by scientific societies and it is limited by strong dependence on the methodological quality of the ideal radiomics workflow with low relevance to the potential clinical impact. Some of the items, such as phantom assessment and imaging at multiple time points, remain difficult to be investigated when considering real-word data based on retrospective observational studies. Nevertheless, the application of this score could be encouraged for the quality assessment of the papers submitted to peer-review journals in order to facilitate manuscript decisions and improve the overall quality of radiomics studies.
Some limitations pertain to this study. First, a meta-analysis was not performed due to the heterogeneity of the included studies, with a relatively small number of papers assessing the radiomics models for a specific aim, which makes challenging to pool data for a strong meta-analysis. Secondly, cholangiocarcinomas are rarer tumors compared to hepatocellular carcinoma and hepatic metastasis, and the applications of the radiomics in this field is relatively new. This is demonstrated by the fact that 55% of the included studies were published in 2021. Finally, papers with radiomics applied to cholangiocarcinoma on ultrasound and PET/CT were not included due to the limited clinical applicability in patients with cholangiocarcinoma and highly exploratory nature of radiomics analyses with these imaging modalities.
In conclusion, radiomics studies on cholangiocarcinoma demonstrated an insufficient quality with a low total radiomics quality score. Further prospective studies are needed with a standardized methodology, validation in multi-imitational external cohorts, and open science data in order to translate the promising research results in the field of radiomics into useful applications to improved patients’ management in many clinical scenarios.
Supplementary Information
Additional file 1. Detailed search strategy.
Additional file 2. Table S1: Detailed checklist of the radiomics quality score with corresponding checkpoints and items as reported by Lambin et al [5]. Table S2: Radiomics quality score of the included studies assessed by the Reader 1. Table S3: Radiomics quality score of the included studies assessed by the Reader 2. Table S4: Radiomics quality score of the included studies assessed by the Reader 3.
Acknowledgements
The European Society of Medical Imaging Informatics (EuSoMII) supports the Radiomics Auditing Group Initiative with the aim to evaluate and improve the quality of radiomics studies.
Abbreviations
- CI
Confidence interval
- CT
Computed tomography
- IBSI
International Biomarker Standardization Initiative
- ICC
Intraclass correlation coefficient
- IQR
Interquartile range
- MRI
Magnetic resonance imaging
- RQS
Radiomics quality score
Author contributions
RC (Roberto Cannella) and RC (Renato Cuocolo) contributed to study concept and design. RC (Roberto Cannella), FV, and LU performed literature search, manuscript selection, and data extraction. MEK, AP, and EP provided the radiomics quality score assessment. RC (Roberto Cannella) performed the data analysis and wrote the first manuscript draft. RC (Renato Cuocolo) and DPDS contributed to the results interpretation and provided important intellectual content. All authors reviewed and edited the manuscript. All authors read and approved the final manuscript.
Funding
None.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate:
Not applicable.
Consent for publication
Not applicable.
Competing interests
Roberto Cannella: support for attending meeting from Bracco and Bayer; co-funding by the European Union-FESR or FSE, PON Research and Innovation 2014–2020—DM 1062/2021; is a member of the Insights into Imaging Editorial Board. He has not taken part in the review or selection process of this article. Federica Vernuccio: received support from GE Healthcare to attend a meeting and served as speaker for Guerbet. Andrea Ponsiglione: is a member of the Insights into Imaging Editorial Board. He has not taken part in the review or selection process of this article. Daniel Pinto dos Santos: is a member of the Insights into Imaging Editorial Board, serves as Junior Deputy Editor of European Radiology and received consulting fees from cook medical. He has not taken part in the review or selection process of this article. Renato Cuocolo: serves as an editorial board member of European Radiology and European Radiology Experimental. He has not taken part in the review or selection process of this article.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gillies RJ, Kinahan PE, Hricak H. Radiomics: images are more than pictures, they are data. Radiology. 2016;278:563–577. doi: 10.1148/radiol.2015151169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lubner MG, Smith AD, Sandrasegaran K, Sahani DV, Pickhardt PJ. CT texture analysis: definitions, applications, biologic correlates, and challenges. Radiographics. 2017;37:1483–1503. doi: 10.1148/rg.2017170056. [DOI] [PubMed] [Google Scholar]
- 3.Ursprung S, Beer L, Bruining A, et al. Radiomics of computed tomography and magnetic resonance imaging in renal cell carcinoma-a systematic review and meta-analysis. Eur Radiol. 2020;30:3558–3566. doi: 10.1007/s00330-020-06666-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Borhani AA, Catania R, Velichko YS, Hectors S, Taouli B, Lewis S. Radiomics of hepatocellular carcinoma: promising roles in patient selection, prediction, and assessment of treatment response. Abdom Radiol (NY) 2021;46:3674–3685. doi: 10.1007/s00261-021-03085-w. [DOI] [PubMed] [Google Scholar]
- 5.Lambin P, Leijenaar RTH, Deist TM, et al. Radiomics: the bridge between medical imaging and personalized medicine. Nat Rev Clin Oncol. 2017;14:749–762. doi: 10.1038/nrclinonc.2017.141. [DOI] [PubMed] [Google Scholar]
- 6.Wakabayashi T, Ouhmich F, Gonzalez-Cabrera C, et al. Radiomics in hepatocellular carcinoma: a quantitative review. Hepatol Int. 2019;13:546–559. doi: 10.1007/s12072-019-09973-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Harding-Theobald E, Louissaint J, Maraj B, et al. Systematic review: radiomics for the diagnosis and prognosis of hepatocellular carcinoma. Aliment Pharmacol Ther. 2021;54:890–901. doi: 10.1111/apt.16563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang Q, Li C, Zhang J, et al. Radiomics models for predicting microvascular invasion in hepatocellular carcinoma: a systematic review and radiomics quality score assessment. Cancers (Basel) 2021;13:5864. doi: 10.3390/cancers13225864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhong X, Long H, Su L, et al. Radiomics models for preoperative prediction of microvascular invasion in hepatocellular carcinoma: a systematic review and meta-analysis. Abdom Radiol (NY) 2022;47:2071–2088. doi: 10.1007/s00261-022-03496-3. [DOI] [PubMed] [Google Scholar]
- 10.Fiz F, Viganò L, Gennaro N, et al. Radiomics of liver metastases: a systematic review. Cancers (Basel) 2020;12:2881. doi: 10.3390/cancers12102881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Joo I, Lee JM, Yoon JH. Imaging diagnosis of intrahepatic and perihilar cholangiocarcinoma: recent advances and challenges. Radiology. 2018;288:7–13. doi: 10.1148/radiol.2018171187. [DOI] [PubMed] [Google Scholar]
- 12.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Benchoufi M, Matzner-Lober E, Molinari N, Jannot AS, Soyer P. Interobserver agreement issues in radiology. Diagn Interv Imaging. 2020;101:639–641. doi: 10.1016/j.diii.2020.09.001. [DOI] [PubMed] [Google Scholar]
- 14.Chu H, Liu Z, Liang W, et al. Radiomics using CT images for preoperative prediction of futile resection in intrahepatic cholangiocarcinoma. Eur Radiol. 2021;31:2368–2376. doi: 10.1007/s00330-020-07250-5. [DOI] [PubMed] [Google Scholar]
- 15.Duda D, Krętowski M, Bézy-Wendling J. Computer-aided diagnosis of liver tumors based on multi-image texture analysis of contrast-enhanced CT. Selection of the most appropriate texture features. Stud Log Gramm Rhetor. 2013;35:49–70. doi: 10.2478/slgr-2013-0039. [DOI] [Google Scholar]
- 16.Hamm CA, Wang CJ, Savic LJ, et al. Deep learning for liver tumor diagnosis part I: development of a convolutional neural network classifier for multi-phasic MRI. Eur Radiol. 2019;29:3338–3347. doi: 10.1007/s00330-019-06205-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Huang X, Shu J, Yan Y, et al. Feasibility of magnetic resonance imaging-based radiomics features for preoperative prediction of extrahepatic cholangiocarcinoma stage. Eur J Cancer. 2021;155:227–235. doi: 10.1016/j.ejca.2021.06.053. [DOI] [PubMed] [Google Scholar]
- 18.Ji GW, Zhu FP, Zhang YD, et al. A radiomics approach to predict lymph node metastasis and clinical outcome of intrahepatic cholangiocarcinoma. Eur Radiol. 2019;29:3725–3735. doi: 10.1007/s00330-019-06142-7. [DOI] [PubMed] [Google Scholar]
- 19.Ji GW, Zhang YD, Zhang H, et al. Biliary tract cancer at CT: a radiomics-based model to predict lymph node metastasis and survival outcomes. Radiology. 2019;290:90–98. doi: 10.1148/radiol.2018181408. [DOI] [PubMed] [Google Scholar]
- 20.King MJ, Hectors S, Lee KM, et al. Outcomes assessment in intrahepatic cholangiocarcinoma using qualitative and quantitative imaging features. Cancer Imaging. 2020;20:43. doi: 10.1186/s40644-020-00323-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liang W, Xu L, Yang P, et al. Novel nomogram for preoperative prediction of early recurrence in intrahepatic cholangiocarcinoma. Front Oncol. 2018;8:360. doi: 10.3389/fonc.2018.00360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu X, Khalvati F, Namdar K, et al. Can machine learning radiomics provide pre-operative differentiation of combined hepatocellular cholangiocarcinoma from hepatocellular carcinoma and cholangiocarcinoma to inform optimal treatment planning? Eur Radiol. 2021;31:244–255. doi: 10.1007/s00330-020-07119-7. [DOI] [PubMed] [Google Scholar]
- 23.Mosconi C, Cucchetti A, Bruno A, et al. Radiomics of cholangiocarcinoma on pretreatment CT can identify patients who would best respond to radioembolisation. Eur Radiol. 2020;30:4534–4544. doi: 10.1007/s00330-020-06795-9. [DOI] [PubMed] [Google Scholar]
- 24.Nakai H, Fujimoto K, Yamashita R, et al. Convolutional neural network for classifying primary liver cancer based on triple-phase CT and tumor marker information: a pilot study. Jpn J Radiol. 2021;39:690–702. doi: 10.1007/s11604-021-01106-8. [DOI] [PubMed] [Google Scholar]
- 25.Park HJ, Park B, Park SY, et al. Preoperative prediction of postsurgical outcomes in mass-forming intrahepatic cholangiocarcinoma based on clinical, radiologic, and radiomics features. Eur Radiol. 2021;31:8638–8648. doi: 10.1007/s00330-021-07926-6. [DOI] [PubMed] [Google Scholar]
- 26.Park S, Lee JM, Park J, et al. Volumetric CT texture analysis of intrahepatic mass-forming cholangiocarcinoma for the prediction of postoperative outcomes: fully automatic tumor segmentation versus semi-automatic segmentation. Korean J Radiol. 2021;22:1797–1808. doi: 10.3348/kjr.2021.0055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ponnoprat D, Inkeaw P, Chaijaruwanich J, et al. Classification of hepatocellular carcinoma and intrahepatic cholangiocarcinoma based on multi-phase CT scans. Med Biol Eng Comput. 2020;58:2497–2515. doi: 10.1007/s11517-020-02229-2. [DOI] [PubMed] [Google Scholar]
- 28.Qin H, Hu X, Zhang J, et al. Machine-learning radiomics to predict early recurrence in perihilar cholangiocarcinoma after curative resection. Liver Int. 2021;41:837–850. doi: 10.1111/liv.14763. [DOI] [PubMed] [Google Scholar]
- 29.Sadot E, Simpson AL, Do RK, et al. Cholangiocarcinoma: correlation between molecular profiling and imaging phenotypes. PLoS One. 2015;10:e0132953. doi: 10.1371/journal.pone.0132953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Silva M, Maddalo M, Leoni E, et al. Integrated prognostication of intrahepatic cholangiocarcinoma by contrast-enhanced computed tomography: the adjunct yield of radiomics. Abdom Radiol (NY) 2021;46:4689–4700. doi: 10.1007/s00261-021-03183-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tang Y, Yang CM, Su S, Wang WJ, Fan LP, Shu J. Machine learning-based Radiomics analysis for differentiation degree and lymphatic node metastasis of extrahepatic cholangiocarcinoma. BMC Cancer. 2021;21:1268. doi: 10.1186/s12885-021-08947-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tang Y, Zhang T, Zhou X, et al. The preoperative prognostic value of the radiomics nomogram based on CT combined with machine learning in patients with intrahepatic cholangiocarcinoma. World J Surg Oncol. 2021;19:45. doi: 10.1186/s12957-021-02162-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang X, Wang S, Yin X, Zheng Y. MRI-based radiomics distinguish different pathological types of hepatocellular carcinoma. Comput Biol Med. 2022;141:105058. doi: 10.1016/j.compbiomed.2021.105058. [DOI] [PubMed] [Google Scholar]
- 34.Wang Y, Shao J, Wang P, et al. Deep learning radiomics to predict regional lymph node staging for hilar cholangiocarcinoma. Front Oncol. 2021;11:721460. doi: 10.3389/fonc.2021.721460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Xu H, Zou X, Zhao Y, et al. Differentiation of intrahepatic cholangiocarcinoma and hepatic lymphoma based on radiomics and machine learning in contrast-enhanced computer tomography. Technol Cancer Res Treat. 2021;20:15330338211039125. doi: 10.1177/15330338211039125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Xu L, Wan Y, Luo C, et al. Integrating intratumoral and peritumoral features to predict tumor recurrence in intrahepatic cholangiocarcinoma. Phys Med Biol. 2021 doi: 10.1088/1361-6560/ac01f3. [DOI] [PubMed] [Google Scholar]
- 37.Xu L, Yang P, Liang W, et al. A radiomics approach based on support vector machine using MR images for preoperative lymph node status evaluation in intrahepatic cholangiocarcinoma. Theranostics. 2019;9:5374–5385. doi: 10.7150/thno.34149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Xue B, Wu S, Zheng M, et al. Development and validation of a Radiomic-based model for prediction of intrahepatic Cholangiocarcinoma in patients with intrahepatic Lithiasis complicated by imagologically diagnosed mass. Front Oncol. 2021;10:598253. doi: 10.3389/fonc.2020.598253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Xue B, Wu S, Zhang M, et al. A radiomic-based model of different contrast-enhanced CT phase for differentiate intrahepatic cholangiocarcinoma from inflammatory mass with hepatolithiasis. Abdom Radiol (NY) 2021;46:3835–3844. doi: 10.1007/s00261-021-03027-6. [DOI] [PubMed] [Google Scholar]
- 40.Yang C, Huang M, Li S, et al. Radiomics model of magnetic resonance imaging for predicting pathological grading and lymph node metastases of extrahepatic cholangiocarcinoma. Cancer Lett. 2020;470:1–7. doi: 10.1016/j.canlet.2019.11.036. [DOI] [PubMed] [Google Scholar]
- 41.Yao X, Huang X, Yang C, et al. A novel approach to assessing differentiation degree and lymph node metastasis of extrahepatic cholangiocarcinoma: prediction using a radiomics-based particle swarm optimization and support vector machine model. JMIR Med Inform. 2020;8:e23578. doi: 10.2196/23578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zhang J, Wu Z, Zhang X, et al. Machine learning: an approach to preoperatively predict PD-1/PD-L1 expression and outcome in intrahepatic cholangiocarcinoma using MRI biomarkers. ESMO Open. 2020;5:e000910. doi: 10.1136/esmoopen-2020-000910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhang J, Wang X, Zhang L, et al. Radiomics predict postoperative survival of patients with primary liver cancer with different pathological types. Ann Transl Med. 2020;8:820. doi: 10.21037/atm-19-4668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhang J, Huang Z, Cao L, et al. Differentiation combined hepatocellular and cholangiocarcinoma from intrahepatic cholangiocarcinoma based on radiomics machine learning. Ann Transl Med. 2020;8:119. doi: 10.21037/atm.2020.01.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhang J, Wu Z, Zhao J, et al. Intrahepatic cholangiocarcinoma: MRI texture signature as predictive biomarkers of immunophenotyping and survival. Eur Radiol. 2021;31:3661–3672. doi: 10.1007/s00330-020-07524-y. [DOI] [PubMed] [Google Scholar]
- 46.Zhao J, Zhang W, Fan CL, et al. Development and validation of preoperative magnetic resonance imaging-based survival predictive nomograms for patients with perihilar cholangiocarcinoma after radical resection: a pilot study. Eur J Radiol. 2021;138:109631. doi: 10.1016/j.ejrad.2021.109631. [DOI] [PubMed] [Google Scholar]
- 47.Zhao J, Zhang W, Zhu YY, et al. Development and validation of noninvasive MRI-based signature for preoperative prediction of early recurrence in perihilar cholangiocarcinoma. J Magn Reson Imaging. 2022;55:787–802. doi: 10.1002/jmri.27846. [DOI] [PubMed] [Google Scholar]
- 48.Zhao L, Ma X, Liang M, et al. Prediction for early recurrence of intrahepatic mass-forming cholangiocarcinoma: quantitative magnetic resonance imaging combined with prognostic immunohistochemical markers. Cancer Imaging. 2019;19:49. doi: 10.1186/s40644-019-0234-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhou Y, Zhou G, Zhang J, Xu C, Wang X, Xu P. Radiomics signature on dynamic contrast-enhanced MR images: a potential imaging biomarker for prediction of microvascular invasion in mass-forming intrahepatic cholangiocarcinoma. Eur Radiol. 2021;31:6846–6855. doi: 10.1007/s00330-021-07793-1. [DOI] [PubMed] [Google Scholar]
- 50.Zhu Y, Mao Y, Chen J, et al. Value of contrast-enhanced CT texture analysis in predicting IDH mutation status of intrahepatic cholangiocarcinoma. Sci Rep. 2021;11:6933. doi: 10.1038/s41598-021-86497-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhu Y, Mao Y, Chen J, et al. Radiomics-based model for predicting early recurrence of intrahepatic mass-forming cholangiocarcinoma after curative tumor resection. Sci Rep. 2021;11:18347. doi: 10.1038/s41598-021-97796-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Pinto Dos Santos D, Dietzel M, Baessler B. A decade of radiomics research: Are images really data or just patterns in the noise? Eur Radiol. 2021;31:1–4. doi: 10.1007/s00330-020-07108-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.van Timmeren JE, Cester D, Tanadini-Lang S, Alkadhi H, Baessler B. Radiomics in medical imaging-“how-to” guide and critical reflection. Insights Imaging. 2020;11:91. doi: 10.1186/s13244-020-00887-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Shur JD, Doran SJ, Kumar S, et al. Radiomics in oncology: a practical guide. Radiographics. 2021;41:1717–1732. doi: 10.1148/rg.2021210037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Spadarella G, Calareso G, Garanzini E, Ugga L, Cuocolo A, Cuocolo R. MRI based radiomics in nasopharyngeal cancer: systematic review and perspectives using radiomic quality score (RQS) assessment. Eur J Radiol. 2021;140:109744. doi: 10.1016/j.ejrad.2021.109744. [DOI] [PubMed] [Google Scholar]
- 56.Ponsiglione A, Stanzione A, Cuocolo R, et al. Cardiac CT and MRI radiomics: systematic review of the literature and radiomics quality score assessment. Eur Radiol. 2022;32:2629–2638. doi: 10.1007/s00330-021-08375-x. [DOI] [PubMed] [Google Scholar]
- 57.Chang S, Han K, Suh YJ, Choi BW. Quality of science and reporting for radiomics in cardiac magnetic resonance imaging studies: a systematic review. Eur Radiol. 2022 doi: 10.1007/s00330-022-08587-9. [DOI] [PubMed] [Google Scholar]
- 58.Pinto Dos Santos D. Radiomics in endometrial cancer and beyond-a perspective from the editors of the EJR. Eur J Radiol. 2022;150:110266. doi: 10.1016/j.ejrad.2022.110266. [DOI] [PubMed] [Google Scholar]
- 59.Carbonell G, Kennedy P, Bane O, et al. Precision of MRI radiomics features in the liver and hepatocellular carcinoma. Eur Radiol. 2022;32:2030–2040. doi: 10.1007/s00330-021-08282-1. [DOI] [PubMed] [Google Scholar]
- 60.Zwanenburg A, Vallières M, Abdalah MA, et al. The image biomarker standardization initiative: standardized quantitative radiomics for high-throughput image-based phenotyping. Radiology. 2020;295:328–338. doi: 10.1148/radiol.2020191145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Stanzione A, Gambardella M, Cuocolo R, Ponsiglione A, Romeo V, Imbriaco M. Prostate MRI radiomics: a systematic review and radiomic quality score assessment. Eur J Radiol. 2020;129:109095. doi: 10.1016/j.ejrad.2020.109095. [DOI] [PubMed] [Google Scholar]
- 62.Abdurixiti M, Nijiati M, Shen R, Ya Q, Abuduxiku N, Nijiati M. Current progress and quality of radiomic studies for predicting EGFR mutation in patients with non-small cell lung cancer using PET/CT images: a systematic review. Br J Radiol. 2021;94:20201272. doi: 10.1259/bjr.20201272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ugga L, Perillo T, Cuocolo R, et al. Meningioma MRI radiomics and machine learning: systematic review, quality score assessment, and meta-analysis. Neuroradiology. 2021;63:1293–1304. doi: 10.1007/s00234-021-02668-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Detailed search strategy.
Additional file 2. Table S1: Detailed checklist of the radiomics quality score with corresponding checkpoints and items as reported by Lambin et al [5]. Table S2: Radiomics quality score of the included studies assessed by the Reader 1. Table S3: Radiomics quality score of the included studies assessed by the Reader 2. Table S4: Radiomics quality score of the included studies assessed by the Reader 3.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.