Abstract
Understanding the roots of Covid-19 vaccine hesitancy in at-risk groups, such as persons living with HIV (PLWH), is of utmost importance. We developed a modified Vaccine Hesitancy Scale (VHS) questionnaire using items from the National Advisory Committee on Immunization Acceptability Matrix. To examine factors associated with receiving COVID-19 vaccine and the link between vaccine attitudes and beliefs with vaccine behavior, PLWH were recruited via social media and community-based organizations (February-May 2022). Descriptive statistics were used to summarize results. Total VHS score was generated by adding Likert scale scores and linear regression models used to compare results between participants who received or did not receive COVID-19 vaccines. Logistic regression models were used to identify factors associated with vaccine uptake. A total of 246 PLWH indicated whether they received a COVID-19 vaccine. 89% received ≥ 1 dose. Mean total VHS(SD) for persons having received ≥ 1 COVID-19 vaccine was 17.8(6.2) vs. 35.4(9.4) for participants not having received any COVID-19 vaccine. Persons who received ≥ 1 dose were significantly older than those who had not received any (48.4 ± 13.8 vs. 34.0 ± 7.7 years, p < 0.0001). The majority of participants considered COVID-19 vaccination important for their health(81.3%) and the health of others(84.4%). Multivariate logistic regression revealed the odds of taking ≥ 1dose were increased 2.4-fold [95% CI 1.6, 3.5] with each increase in age of 10 years (p < 0.0001). Sex and ethnicity were not different between groups. In conclusion, PLWH accept COVID-19 vaccines for both altruistic and individual reasons. With evolving recommendations and increasing numbers of booster vaccines, we must re-examine the needs of PLWH regularly.
Supplementary Information
The online version contains supplementary material available at 10.1007/s10461-023-03991-8.
Keywords: HIV; intention to vaccinate; COVID-19 vaccine; vaccine confidence; vaccine hesitancy, survey
Introduction
Approximately 37 million people are living with HIV (PLWH) worldwide UNAIDS. 38 million people are living with HIV around the world. https://www.unaids.org/en/resources/infographics/people-living-with-hiv-around the world. Acccessed 6 June 2022[1], of whom ~ 67,000 reside in Canada Public Health Agency of Canada Estimates of HIV incidence, prevalence and Canada’s progress on meeting the 90-90-90 targets https://www.canada.ca/en/public-health/services/publications/diseases-conditions/summary-estimates-hiv-incidence-prevalence-canadas-progress-90-90-90.html#s2, Accesssed 6 June 2022[2]. Effective antiretroviral therapy (ART) dramatically reduced morbidity and mortality associated with HIV infection Palella FJ, Jr., Delaney KM, Moorman AC, Loveless MO, Fuhrer J, Satten GA, et al. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. HIV Outpatient Study Investigators. N Engl J Med. 1998;338(13):853-60. Hogg RS, Heath KV, Yip B, Craib KJ, O'Shaughnessy MV, Schechter MT, et al. Improved survival among HIV-infected individuals following initiation of antiretroviral therapy. JAMA. 1998;279(6):450-4. 2022[3,4]. and lowered the rate of opportunistic infections and associated deaths. People with advanced HIV, those with low CD4 T-cell counts and high HIV viral loads and those who are not on ART have increased risk of COVID-19-associated complications. Higher rates of chronic lung disease and behaviors that impact lung function (cigarette smoking, drug and alcohol use) among PLWH [1–3] are proposed to increase their COVID-19 risk. Also, the fact that HIV disproportionately affects persons of racial and ethnic minorities and lower sociodemographic status[4] can contribute to disparities in COVID-19 incidence and outcomes[5, 6].
Effective and safe vaccines against SARS-CoV-2 (COVID-19 vaccines) were developed and distributed with an unprecedented speed. Canada launched its COVID-19 vaccine roll-out in December 2020 for adults, with eligibility expanding to include all individuals 12 + years of age (without contraindications) by June 2021[7]. However, since the roll-out, PLWH were not prioritized for vaccination unless individuals met other priority population criteria.
The success of any vaccination program depends on high and persistent vaccine uptake, guided by confidence in the vaccine program and its effectiveness. Even before the COVID-19 global vaccination effort, vaccine hesitancy emerged as a public health challenge[8]. The prevalence of COVID-19 vaccine hesitancy globally was estimated at 8–15%[9–13] and approximately 20% in Canada in 2021[14]. The reasons are dynamic and have changed over time[14, 15]. Vaccine hesitancy is a multi-dimensional construct with various underlying factors[16].
Determinants of Vaccine Hesitancy and Confidence
Vaccine confidence describes beliefs about vaccination (knowledge), which relate to the attitude towards vaccination[17], while hesitancy refers to delay in acceptance or refusal of vaccination despite the availability of vaccination services[18]. Various models exist to describe the determinants of vaccine hesitancy and/or confidence. Examples include the Theory of Planned Behavior, the Health Belief Model, the “3 C model,” and the “Working Group Determination of Vaccine Hesitancy Matrix”[14, 15, 18, 19]. The Theory of Planned Behavior aims to provide a rationale for behaviors over which people can exert self-control[20, 21]. The key component to this model is behavioral intent, in that behavioral intentions are influenced by the attitude about the likelihood that the behavior will have the expected outcome and the weighing of the risks and benefits of that outcome. This model also stipulates that behavioral achievement depends on both motivation (intention) and ability (behavioral control) [20, 21]. Meanwhile, according to the Health Belief Model, the two components of health-related behavior are 1) the desire to avoid illness, or conversely get well if already ill; and 2) the belief that a specific health action will prevent, or cure, illness[22, 23]. Ultimately, an individual’s course of action often depends on the person’s perceptions of the benefits and barriers related to health behavior[22, 23]. In the “3 C model,” determinants include 1) confidence, which refers to the issues of trust in the safety and effectiveness of vaccines and the competence of health care providers, health care systems and policy makers; 2) convenience, which refers to the ease at which vaccines are accessed; and 3) complacency, which occurs when the need to vaccinate is low due to perceived low risk of vaccine preventable disease[18, 24]. In later years, additional determinants have been added to this model including calculation, which occurs when individuals seek out information and assess their findings to guide decision making, and collective, which describes when individuals make decisions based on their sense of social responsibility[18, 24]. Meanwhile, in the “Working Group Determination of Vaccine Hesitancy Matrix,” determinants include 1) contextual influences, 2) individual and group influences and 3) vaccine and vaccination-specific issues[25]. Each category contains specific items which gives details about their determinants and the specific scope[25]. These large theoretical constructs can be used to ground Vaccine Hesitancy Models. In a review of 15 studies by Troiano et al., COVID-19 vaccine acceptance or refusal was associated with ethnicity, working status, religious beliefs, politics, gender, age, education and income[16]. The most common reasons for COVID-19 vaccine refusal included: being against vaccines in general, concerns about safety/thinking that the vaccine was produced in a rush and was too dangerous, or considering the vaccine useless because of the harmless nature of COVID-19, general lack of trust, doubts about the efficiency of the vaccine, belief to be already immunized, and doubts about the vaccine provenience[26].
Underlying Reasons for Vaccine Confidence and Hesitancy in PLWH
Attitudes towards vaccination result from a complex interaction between different social, cultural and personal factors. Factors facilitating willingness to be vaccinated amongst high-risk populations included personal susceptibility[27]. For Black, indigenous and people of colour (BIPOC) communities, vaccine hesitancy is partially rooted in systemic racism, marginalization and neglect[11]. Stigma, defined as a societal process leading to devaluation or discrediting based on particular attributes, is recognized as a barrier to protective health behaviors across a range of health conditions, including vaccine hesistancy[28]. Medical mistrust is defined as active distrust in health care systems and medical providers with the belief that they are acting against one’s best interest[29]. Nearly all PLWH (97%) in a study from the USA held at least one COVID-19 vaccine or treatment hesitancy belief[30]. Recognizing that PLWH face additional barriers to health care including stigma, discrimination and isolation, Rodriguez et al. found that “lack of confidence” and “risks” explained 46% and 12% of the variance between individuals accepting or refusing the vaccine[31]. At the current time, reasons for COVID-19 vaccine hesitancy and confidence in PLWH in Canada are only starting to be examined, and interventions to increase COVID-19 vaccine uptake in this population have not yet been implemented. Identification of facilitators underlying vaccine confidence among PLWH may reduce health disparities which could be exacerbated by COVID-19 and will guide intervention strategies, such as educational interventions targeted toward specific sub-populations. Given the unique characteristics of PLWH, whose reasons for vaccine refusal may differ from those in the general population, we aimed to address this gap of knowledge in the Canadian context.
Study Objective
We aimed to identify factors associated with COVID-19 vaccine uptake versus vaccine refusal in PLWH in Canada and determine factors related to confidence in COVID-19 vaccines in order better tailor vaccine recommendations to PLWH.
Methods
Study Design and Participants
We carried out a national online survey of PLWH across Canada. In an attempt to ensure a representative sample[32], we aimed to recruit a minimum number of participants who identified with various group membership: men who have sex with men (MSM), people who inject drugs, women, persons of African, Caribbean or Black communities, persons of indigenous communities and persons ≥ 65 years of age.
Strategies for Recruitment
Participants were recruited between February to May 2022 via social media and through community-based organizations serving PLWH. Approximately fifteen clinics or community-based organizations serving PLWH agreed to distribute the survey. Some clinics also put up poster advertisements and provided social media cards in their offices/clinics. As we wanted to hear from as many PLWH as possible, we did not use recruitment quotas for different sub-populations of PLWH. However, in an attempt to ensure a diverse sample of PLWH in Canada, we aimed to recruit a minimum number of participants (at least 20 per group) who identified with particular group membership.
The public survey link was disseminated on community organizations websites and was directly sent to their members via e-mail, e-posters or other social media. Participants were invited to share their thoughts on COVID-19 vaccination by completing an online survey to help us understand factors that contribute to COVID-19 vaccine uptake or refusal among PLWH. It was indicated that this anonymous survey would take about 15 min to complete, and that all adults living with HIV in Canada could take the survey. Furthermore participants were offered the chance to enter a draw to win one of twenty $50 gift cards.
Study Procedures
After providing consent to participate, screened participants completed the questionnaire online, using a secure, web-enabled survey application (REDCap), hosted on the University of British Columbia network. Data was saved on the CIHR Canadian HIV Trials Network servers at the St Paul’s Hospital in Vancouver, British Columbia. All data were encrypted.
Questionnaire
Our study was founded on The Theory of Planned Behavior, which aims to provide a rationale for behaviors over which people can exert self-control[20, 21]. A key component of this model is behavioral intent, in that behavioral intentions are influenced by the attitude about the likelihood that the behavior will have the expected outcome and the weighing of the risks and benefits of that outcome [20, 21]. The questionnaire evaluated factors associated with COVID-19 vaccine beliefs and acceptance among PLWH. Vaccine hesitancy is generally associated with a lower compliance with immunization[33]. The study questionnaire was based on instruments developed in several previous studies[25, 34], including those involving PLWH [31, 35, 36]. We used items validated in another study of PLWH since an HIV diagnosis could modify a person’s perception of disease susceptibility and severity. For example, some PLWH may perceive themselves to be at greater risk of COVID-19 acquisition due to having an immunocompromised status. This perception, in turn, could influence their attitudes towards vaccination. In addition, since many PLWH have traditionally encountered stigma due to their HIV status[37], past experiences may impact their perception of stigma related to COVID-19 acquisition, which could also influence their attitudes towards vaccination. Similarly, many sub-populations of PLWH, including individuals born outside of Canada, may have high levels of mistrust in messages from government and health care providers with regards to messaging related to vaccination[38]. The items in the questionnaire contain those included in the validated Acceptability Matrix which focuses on factors demonstrated to have the highest impact on vaccine uptake. These included: (a) perception of vaccine safety and efficacy, (b) perception of disease susceptibility and severity, (c) process of vaccination and (d) knowledge, attitudes and trust [39]. Furthermore, the questionnaire contains a modified Vaccine Hesitancy Scale (VHS) for PLWH toward the COVID-19 vaccine which has acceptable reliability, internal consistency and construct validity[31]. Ten questions/items from the VHS were included using a five-point Likert scale ranging from 1 (strongly agree) to 5 (strongly disagree). The full list of questions can be found in Supplemental Table 1. Participants also answered a series of additional demographic questions. After collection, variables were checked for fraudulent participants or data.
Primary Endpoint
The primary endpoint was vaccine uptake of at least one dose of COVID-19 vaccine (yes/no).
Sample Size
We aimed to enroll 250 participants in the study with the expectation that about 200 would have accepted the COVID-19 vaccine and 50 participants would have refused (4:1 ratio), which reflects the level of vaccine uptake in the general Canadian population as of 2021 (80%)[40]. In our protocol, we assumed a standard deviation of 4. We determined that we would have at least 80% power to detect a 2-point difference assuming a standard deviation of 4 and a ratio of 4:1 of those accepting, compared to those refusing, vaccine. In an attempt to capture a diverse sample of PLWH in Canada, we recorded how each participant identifies with particular group membership(s). We decided not to set quotas for specific subpopulations in an effort to allow everyone who wanted to participate the opportunity to do so.
Data Analyses
Descriptive statistics were used to describe the characteristics of the study participants. For items on the 5-point Likert scale, the scores for each participant were added together (reversing for direction, as necessary). The scores of the ten items were added together to generate a total VHS score[31, 41] for participants who provided a valid response on the ten questions/items. A linear regression model was constructed to compare the VHS total score between participants who took the COVID-19 vaccine and those who refused. The model was adjusted for age and sex as confounding variables. Logistic regression models were used to identify factors associated with COVID-19 vaccine uptake and refusals, Univariate analysis was performed on potential factors. Furthermore, multivariable logistic regression model were created. Age, sex and statistical significant factors from univariate analysis were included in the multivariable logistic regression model. Two-sided p-value of less than 0.05 were considered to indicate statistical significance. Analyses were conducted using SAS version 9.4.
Ethics
This study was conducted according to the Tri-Council Policy Statement Version 2 (TCPS2) and the principles in the Declaration of Helsinki. Ethical approval was received from the University of British Columbia Providence Health Care Research Ethics Board (H21-03432).
Results
Baseline Characteristics and COVID‑19 Vaccine Uptake
A total of 259 individuals participated in the online survey and 246 indicated whether they were vaccinated. The data collection flow chart can be found in Supplement methods (Supplemental Fig. 1). Characteristics of participants and COVID-19 vaccine uptake for each level of a categorical variable can be seen in Table 1 and Supplemental Table 2. The mean age (± standard deviation) was 47 ± 14 years and 73% were male. 80% had completed at least some high school. 65% were born in Canada, 53.7% declared themselves as being white and 44.4% as belonging to the BIPOC community. 52% were diagnosed with HIV for more than 15 years. In the overall sample, 84.5% 84.% This should read 84.5% reported receiving at least one dose of COVID-19 vaccine.
Table 1.
COVID-19 Vaccine uptake by participant characteristics
| All responders n = 259 |
Vaccinated n = 219, 84.5% |
Unvaccinated n = 27, 10.4% |
PNTA* n = 3, 1.1% |
Missing n = 10, 4% |
|
|---|---|---|---|---|---|
| Age, mean (SD), year | 46.8 (14.0) | 48.4(13.8) | 34.0 (7.7) | 37.0 (7.2) | 47.1(15.6) |
| Age ≥ 40 years old | 175 | 162 (92.6) | 5 (2.9) | 1 (0.6) | 7 (4.0) |
| Sex | |||||
| Female | 69 | 57 (82.6) | 9 (13.0) | 1 (1.4) | 2 (2.9) |
| Male | 189 | 162 (85.7) | 18 (9.5) | 2 (1.1) | 7 (3.7) |
| Highest education level | |||||
| Less than HS** | 5 | 4 (80.0) | 1 (20.0) | 0 (0.0) | 0 (0.0) |
| Some/completed HS | 55 | 36 (65.5) | 14 (25.5) | 1 (1.8) | 4 (7.3) |
| Some/completed university | 150 | 137 (91.3) | 6 (4.0) | 2 (1.3) | 5 (3.3) |
| Some/completed graduate education | 47 | 41 (87.2) | 6 (12.8) | 0 (0.0) | 0 (0.0) |
| Total household income | |||||
| $29,999 under | 83 | 71 (85.5) | 7 (8.4) | 1 (1.2) | 4 (4.8) |
| $30,000–59,999 | 77 | 64 (83.1) | 10 (13.0) | 1 (1.3) | 2 (2.6) |
| $60,000 to 89,999 | 36 | 29 (80.6) | 6 (16.7) | 1 (2.8) | 0 (0.0) |
| $90,000 and up | 47 | 41 (87.2) | 3 (6.4) | 0 (0.0) | 3 (6.4) |
| Current employment status | |||||
| Employed | 139 | 120 (86.3) | 16 (11.5) | 1 (0.7) | 2 (1.4) |
| Unemployed | 113 | 95 (84.1) | 10 (8.8) | 1 (0.9) | 7 (6.2) |
| Born in Canada | 165 | 132 (80.0) | 25 (15.2) | 2 (1.2) | 6 (3.6) |
| Inject drugs user | 17 | 14 (82.4) | 2 (11.8) | 1 (5.9) | 0 (0.0) |
| Non-prescription illicit drug user | 31 | 29 (93.5) | 0 (0.0) | 1 (3.2) | 1 (3.2) |
| Gender | |||||
| Woman | 66 | 53 (80.3) | 10 (15.2) | 1 (1.5) | 2 (3.0) |
| Man | 163 | 139 (85.3) | 17 (10.4) | 2 (1.2) | 5 (3.1) |
| Transgender | 2 | 2 (100.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Two-spirit | 9 | 7 (77.8) | 0 (0.0) | 0 (0.0) | 2 (22.2) |
| Queer | 12 | 12 (100.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Non-binary | 4 | 4 (100.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Agender | 0 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Other | 1 | 1 (100.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| MSM*** | 164 | 141 (86.0) | 17 (10.4) | 1 (0.6) | 5 (3.0) |
| Ethnicity | |||||
| White | 139 | 115 (82.7) | 20 (14.4) | 1 (0.7) | 3 (2.2) |
| BIPOC | 115 | 100 (87.0) | 7 (6.1) | 2 (1.7) | 6 (5.2) |
| Ethnicity subgroup | |||||
| African, Caribbean or Black community | 30 | 26 (86.7) | 1 (3.3) | 0 (0.0) | 3 (10.0) |
| Person from the Indigenous community | 12 | 11 (91.7) | 1 (8.3) | 0 (0.0) | 0 (0.0) |
| Migrant | 13 | 13 (100.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Received HIV diagnosis | |||||
| ≤ 4 years ago | 38 | 27 (71.1) | 10 (26.3) | 0 (0.0) | 1 (2.6) |
| 5–9 years ago | 37 | 23 (62.2) | 12 (32.4) | 1 (2.7) | 1 (2.7) |
| 10–14 years ago | 41 | 37 (90.2) | 3 (7.3) | 0 (0.0) | 1 (2.4) |
| ≥ 15 years ago | 134 | 126 (94.0) | 2 (1.5) | 2 (1.5) | 4 (3.0) |
| On AVR**** medication | 253 | 215 (85.0) | 27 (10.7) | 3 (1.2) | 8 (3.2) |
| Comorbidity | |||||
| Hepatitis C | 14 | 8 (57.1) | 5 (35.7) | 1 (7.1) | 0 (0.0) |
| Diabetes | 38 | 29 (76.3) | 7 (18.4) | 1 (2.6) | 1 (2.6) |
| Kidney failure | 14 | 5 (35.7) | 8 (57.1) | 1 (7.1) | 0 (0.0) |
| Chronic liver disease | 15 | 9 (60.0) | 6 (40.0) | 0 (0.0) | 0 (0.0) |
| Chronic lung disease | 17 | 12 (70.6) | 5 (29.4) | 0 (0.0) | 0 (0.0) |
| Severe asthma | 20 | 17 (85.0) | 3 (15.0) | 0 (0.0) | 0 (0.0) |
| Smoking | |||||
| Yes | 57 | 46 (80.7) | 8 (14.0) | 2 (3.5) | 1 (1.8) |
| Not currently/in the past | 96 | 84 (87.5) | 9 (9.4) | 1 (1.0) | 2 (2.1) |
| Never | 97 | 86 (88.7) | 9 (9.3) | 0 (0.0) | 2 (2.1) |
| Vaping | |||||
| Yes | 32 | 24 (75.0) | 7 (21.9) | 0 (0.0) | 1 (3.1) |
| Not currently/in the past | 36 | 27 (75.0) | 7 (19.4) | 2 (5.6) | 0 (0.0) |
| Never | 182 | 165 (90.7) | 12 (6.6) | 1 (0.5) | 4 (2.2) |
| Smoking cannabis | |||||
| Yes | 65 | 57 (87.7) | 5 (7.7) | 0 (0.0) | 3 (4.6) |
| Not currently/in the past | 80 | 68 (85.0) | 10 (12.5) | 2 (2.5) | 0 (0.0) |
| Never | 101 | 86 (85.1) | 12 (11.9) | 1 (1.0) | 2 (2.0) |
| Consumption of cannabis or cannabinoid-based products (form other than smoking) | |||||
| Yes | 58 | 49 (84.5) | 6 (10.3) | 1 (1.7) | 2 (3.4) |
| Not currently/in the past | 62 | 53 (85.5) | 8 (12.9) | 1 (1.6) | 0 (0.0) |
| Never | 128 | 111 (86.7) | 13 (10.2) | 1 (0.8) | 3 (2.3) |
Legend: Data presented as n(%),* PREFER NOT TO ANSWER, **HS = high school, ***MSM = men having sex with men, percent represented as MSM/males, ****AVR = antiviral therapy
Table 2.
Odds Ratios of receiving at least one dose of COVID-19 vaccine (unadjusted analysis)
| Factor | Odds ratio | 95% Confidence interval | p-value |
|---|---|---|---|
| Sex (Male vs. Female) | 1.42 | [0.60, 3.34] | 0.42 |
| Age /per 10-year | 2.55 | [ 1.71, 3.82] | < 0.0001 |
| Person ≥ 65 years of age (Yes vs. No) | 1.82 | [ 0.32, 10.39] | 0.50 |
| Education - at least with completed university (Yes vs. No) | 2.33 | [1.02, 5.32] | 0.04 |
| Person who injects drugs (Yes vs. No) | 0.85 | [0.18, 3.98] | 0.84 |
| Person who uses non-prescription illicit drugs (Yes vs. No) | 8.52 | [0.48, 150.59] | 0.14 |
| Persons of African, Caribbean or Black communities (Yes vs. No) | 2.42 | [0.43, 13.57] | 0.32 |
| Person from the Indigenous community (Yes vs. No) | 0.98 | [0.16, 6.00] | 0.98 |
| MSM (Yes vs. No) * – Male participants only | 0.56 | [0.10, 3.29] | 0.52 |
Legend of table: *MSM = men who have sex with men
Vaccine Hesitancy Scale and Confidence in COVID-19 Vaccine
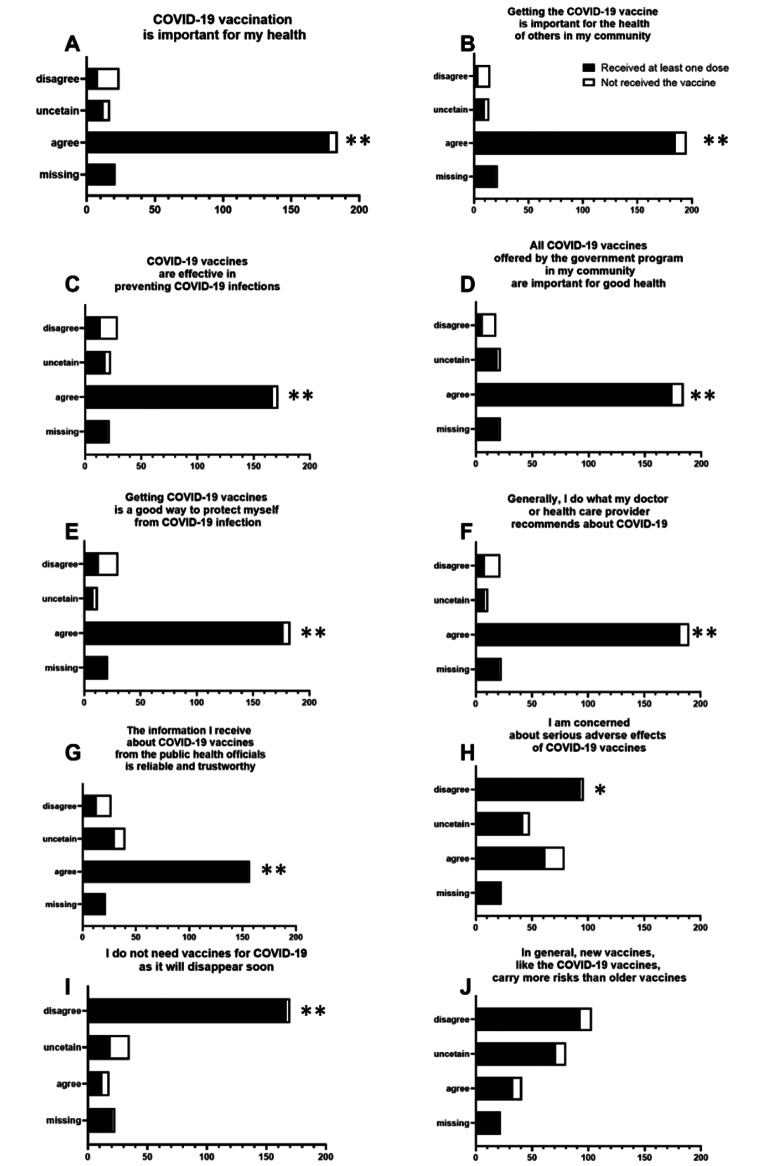
The responses in VHS were grouped into three categories, “agree”, “uncertain” and “disagree” (Fig. 1). A total of 219 participants received at least one dose and 27 did not. The mean total VHS (SD) for persons having received at least one COVID-19 vaccine was 17.8 (6.2) compared to 35.4 (9.4) for participants not having received any COVID-19 vaccine (Supplemental Table 3 A). Participants accepted COVID-19 vaccines for both altruistic (i.e., protection of community) and individual reasons (i.e., protection of self). 89% of participants who received the vaccine considered COVID-19 vaccination to be important for their health, while 93% considered vaccination important for the health of others in the community. 87% trusted all COVID-19 vaccines offered by the government program and 92% trusted their health care provider recommendations. 90% believed that receiving COVID-19 vaccines offers good protection against COVID-19 infection, while 31% of participants who received the vaccine were concerned about serious adverse effects. Participants were divided on the risks that newly developed vaccines (e.g. COVID-19 vaccines) carry compared to older vaccines (18% agree, 36% uncertain and 46% disagree) regardless of their vaccination status. Individuals who felt that the pandemic would linger on longer were more likely to accept the vaccine (84.3% of vaccinated participants) than those who did not feel the pandemic would last that long (24% of unvaccinated).
Fig. 1.
Vaccine Hesitancy Scale (VHS) results based on COVID-19 vaccine uptake status. A-J Overall patterns of vaccine hesitancy across the two groups based on the vaccine uptake presented by question. Five-point Likert scale ranging from 1 (strongly agree) to 5 (strongly disagree) are grouped into three categories, “agree”, “uncertain” and “disagree”. In the presence of a missing response, the total score was not calculated and set as missing. P values refer to the statistically different answers between vaccinated and not vaccinated individuals (**p < 0.0001, *p = 0.001)
Univariate logistic regression analyses revealed that the odds of taking at least one vaccine dose were increased 2.55 fold [95% CI 1.71, 3.82] with each increase in age of 10 years (p < 0.0001). No effect was observed for sex, belonging to the BIPOC or MSM community or use of injectable or non-prescription illicit drugs. We ran models including all significant variables from the univariate analysis (including and excluding VHS score). In both analyses, age, either as a continuous variable or dichomotomous variable (over 40 versus under 40), was identified as a risk factor. Multivariate logistic regression analyses revealed an odds of taking at least one vaccine dose were increased 2.4 fold [95% CI 1.6, 3.5] with each increase in age of 10 years (p<0.0001). The impact of age (over 40 versus under 40 years) was diminished but still significant when VHS was considered. Of note, we preferred the model without VHS because VHS is assumed to be on the causal pathway – older patients are less vaccine hesitant and hesitancy drives vaccination status.
Discussion
There is limited data related to factors associated with COVID-19 vaccine confidence in PLWH living in Canada. Our study was based on the The Theory of Planned Behavior, which aims to provide a rationale for behaviors over which people can exert self-control[20, 21]. The key component to this model is behavioral intent, in that behavioral intentions are influenced by the attitude about the likelihood that the behavior will have the expected outcome and the weighing of the risks and benefits of that outcome. Our study was done later in the pandemic, after a lot of assurance from the literature on the safety of the vaccine and evidence of their effectiveness in preventing hospitalization and death. We found that older PLWH were more likely to accept COVID-19 vaccines. In addition, PLWH accept COVID-19 vaccines for both altruistic and individual reasons.
To our knowledge, the only other study conducted on vaccine uptake in PLWH living in Canada was that performed by Kaida et al., where the intention to receive COVID-19 vaccination was examined in HIV-positive and HIV-negative women and gender-diverse individuals in British Columbia (from August 2020 to March 2021)[42]. Their results indicated that HIV status itself was not associated with COVID-19 vaccine intention in adjusted analyses. In the HIV group, as in our study, older PLWH were more likely to report an intention to vaccinate [42]. Additionally, positive attitudes towards the COVID-19 vaccine were more strongly influenced by direct and indirect social norms toward vaccination[42] – something that we did not examine in our survey. Using an online survey, in an analysis restricted to women and gender-diverse individuals (n = 5588), they found only 65% of PLWH reported intention to receive a COVID-19 vaccine if recommended to them, compared to people who did not have HIV (80%)[40]. Of note, HIV itself was not associated with COVID-19 vaccine intention in adjusted analyses. Among PLWH, positive attitudes towards the COVID-19 vaccine were more strongly influenced by direct and indirect social norms toward vaccination. Similar to our study, PLWH with a higher odds of reporting intention to vaccinate were older[40].
Among other published studies in PLWH performed outside of Canada, Govere-Hwenje et al. also found that older age was associated with willingness to accept vaccination[35]. Telephone interviews were conducted with a randomly selected subset of participants enrolled in an observational cohort study evaluating decentralized ART delivery in South Africa (n = 213). Close to half of all individuals were unsure or were unwilling to be vaccinated[35]. Higher medical mistrust related to COVID-19 and the use of social media for COVID-19 information were associated with a lower willingness to accept vaccination[35]. Age and educational level were examined in an online survey conducted by Zheng et al. on 1295 MSM living with HIV (median age 29 years) residing in mainland China. Uptake of COVID-19 vaccine was only 9%[43]. In contrast to our study, age was not correlated with COVID-19 vaccine hesitancy[43]. However, in line with our study, education level was not associatetd with COVID-19 vaccine hesitancy [43]. Interestingly, Zheng et al. reported that concern about disclosure of HIV status was one of the two top reasons not to initiate COVID-19 vaccination in the study[43].
Factors facilitating willingness to be vaccinated amongst high-risk populations include perceptions of personal susceptibility[15]. Older persons likely perceive themselves to be at greater risk of worse outcomes from COVID-19 infection than younger individuals. In PLWH, greater hesitancy was observed among those who did not perceive their health status to have a major influence on their risk of illness associated with COVID-19[31]. In another survey conducted among 267 PLWH in France, Vallée et al. found that 30% of respondents endorsed hesitancy toward COVID-19 vaccination[36]. They also identified concerns about self-health, the requirement of mandatory COVID-19 vaccination, and personal chronic disease status as independently associated with vaccine acceptance[36]. Participants presenting with general vaccine refusal endorsed concerns about the vaccine and included those who believed they had already developed immunity to COVID-19[36].
Although we did not observe an effect of educational level on COVID-19 vaccine uptake, persons who have obtained higher levels of education may be more comfortable critically evaluating health information and deciding which sources of information are reliable. Similarly, the role of health literacy is known to affect vaccine uptake, although it has not been examined in the context of COVID-19 vaccine uptake in PLWH. Context plays an important role when considering vaccine confidence. With this in mind, not all studies have found that age or education is associated with vaccine hesitancy status. In a study involving 438 PLWH living in India who participated in telephone interviews, over one-third of participants were deemed “vaccine hesitant”, indicating that they were either unlikely to get vaccinated or that they wanted to wait[44]. While neither age nor education was associated with vaccine hesitancy in this study, vaccine hesitancy was associated with a lack of confidence in vaccine safety, concerns about side effects and efficacy, and lack of confidence in common sources of vaccine-related information such as doctors, news media, government[44].
In our study, PLWH were motivated to accept the COVID-19 vaccine for both personal and altruistic reasons. Altruism has previously been demonstrated as a reason for behavior in PLWH including the willingness to participate in research studies even when some personal risk is involved, such as HIV therapeutic vaccine trials[45]. Fostering altruism and responsibly promoting the societal benefits of vaccination may facilitate vaccine uptake amongst PLWH.
Most studies on vaccine confidence conducted in PLWH have been cross-sectional surveys. In contrast, Iliyasu et al. conducted a mixed methods cross-section study administering questionnaires to adults in Nigeria. This was complemented with 20 in-depth interviews of approximately half of respondents willing to receive the COVID-19 vaccine [46]. Some findings were similar to ours - acceptability of the COVID-19 vaccine was influenced by risk perception and concern about vaccine safety. Unlike our study, sociodemographic variables (sex, ethnicity) were not associated with COVID-19 vaccine acceptance. Themes revealed doubts about the existence of COVID-19, mistrust of authorities, and popular credence to rumors and conspiracy theories[46]. In conclusion, COVID-19 vaccine acceptance was sub-optimal and influenced by respondents’ age, income, co-morbidities, risk perception, and concerns about vaccine safety, efficacy, and rumours.
Possible reasons for discrepancy across studies include timing of study completion considering that vaccine confidence is an evolving phenomenon. In studies published earlier during the vaccine roll-out, those believing that the COVID-19 vaccine would not be effective in preventing COVID-19 infection may have reported greater hesitancy. However, as the pandemic progressed, evidence regarding the vaccine’s safety and efficacy emerged, which may have increased vaccine confidence in persons who completed surveys later during the pandemic. Furthermore, social norms may affect individuals’ responses when survey questions are answered anonymously via an online survey compared to when questions are asked by research staff. Enforcing social norms encourages behaviors perceived as “normal” or the proper thing to do[47, 48]. Although social norms play a role in vaccine uptake[49, 50], their influence in modifying vaccine hesitancy in PLWH towards COVID-19 vaccination has not been explored.
Disparity in some responses gathered in our evaluation compared to surveys from other countries may be explained by the impact of different levels of HIV-related stigma. Furthermore, mistrust of government likely differs based on the country and type of government in which the study was conducted. Stigma may have been a barrier to HIV management during the pandemic, by forcing individuals to disclose their HIV status to travel to the clinic during times of COVID-19-related travel restrictions. In a study of over 303 South African participants living with HIV, scales assessing medical mistrust, conspiracy beliefs, anticipated and internalized stigma and stereotypes specific to COVID-19 were applied. Greater than 50% of individuals agreed or strongly agreed, with at least one item suggestive of stigma, and more than 40% with an item assessing mistrust. Higher scores were associated with the female gender and a history of HIV-related stigma[28]. In another study conducted in Black Americans living with HIV, 101 individuals completed telephone interviews on negative impacts of COVID-19: general COVID-19 mistrust, COVID-19 vaccine and treatment hesitancy, and trust in COVID-19 information sources[30]. Greater COVID-19 mistrust was associated with greater vaccine and treatment hesitancy. Participants with more negative COVID-19 impacts reported lower ART adherence as well[30]. Therefore, stigma and medical mistrust may exacerbate pre-existing HIV stigma and medical mistrust on health protective behaviors in PLWH and especially ethnic minorities or persons of colour[30].
There are limitations to our study. PLWH are a very heterogeneous group, with different representation, volunteer and social desirability biases. We had difficulty recruiting participants in the prairie provinces and the Maritimes, in addition to some sub-populations that face social inequities, such as Indigenous persons. Therefore, the findings of the survey may not reflect all PLWH in Canada. Similarly, many more respondents lived in urban than in rural settings. Furthermore, adding focus groups whereby participants can exchange ideas and opinions amongst themselves may have highlighted other aspects of vaccine confidence which were not captured via the web-based e-questionnaire and provided richer data.
In the general public, educational interventions have been successful in increasing vaccine uptake for various infectious diseases[51, 52]. Understanding factors influencing COVID-19 vaccine uptake is critical to optimizing vaccine acceptance and preventing outbreaks. This is especially true for those experiencing social and health inequities. Persons with chronic disease, including PLWH, tend to have close relationships with their health care providers and this opportunity can be used for vaccination education. The provision of special services to offer dedicated and flexible vaccination, coupled with education about vaccination, has been shown to positively impact influenza vaccine uptake in PLWH. Provision of vaccination clinics and vaccine education by staff they trust at the clinics where PLWH are followed may help to increase vaccine uptake amongst PLWH and minimize stigma.
Conclusion
PLWH accept COVID-19 vaccines for altruistic and individual reasons. Interventions to promote vaccine uptake amongst PLWH should be culturally and context-appropriate tailored. Older PLWH were more likely to receive at least one dose of a COVID-19 vaccine. Additional work is required to examine sustainability of behaviour change beyond public health and other mandates. With evolving recommendations and increasing numbers of booster vaccines, we must re-examine the needs of PLWH on an regular basis. We must also consider how to transfer these findings to promote uptake of influenza and other vaccinations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Acknowledgements
The authors thank the CIHR Canadian HIV Trials Network staff who were involved in the planning and preparation of this study, including Elisa Lau from data management. The authors also thank the CIHR Canadian HIV Trials Network Scientific Review Committee and the Community Advisory Board, for their expedited review and helpful comments. In addition, the authors acknowledge all the individuals who assisted with survey dissemination, including Dr Angela Kaida, Dr Mona Loufty, Dr Melanie Murray, Dr Neora Pick, staff from Women’s Health in Women’s Hands, Oak Tree Clinic and community members. They also thank all of the participants who completed the survey.
List of Abbreviations
- ART
antiretroviral therapy
- BIPOC
Black, indigenous and people of colour
- MSM
men who have sex with men
- PLWH
persons living with HIV
- VHS
Vaccine Hesitancy Scale
Authors’ Contributions
Co-principal investigators of the study are CTC, CLC and AHA. CTC and SM conceived the study, led the proposal and protocol development. CTC wrote the first draft of the manuscript. JS is the biostatistician who provided methodological expertise and performed sample size calculations. HQ performed the statistical analyses while JS oversaw data analysis. All other authors contributed to protocol development, study design and development of the proposal. All authors critically reviewed and approved the final manuscript.
Funding
This project was supported by funding from CIHR Canadian HIV Trials Network (grant number: N/A).
Data Availability
All relevant data are within the paper and its supporting files.
Declarations
Conflict of Interest
The authors declare that they have no conflict of interests.
Author Information
CTC is supported by a Fonds de recherche du Québec-Santé (FRQS) Junior 2 career award. ANB holds a Canada Research Chair (Tier 2) in Sexually Transmitted Infection Prevention. WZ is supported by the Michael Smith Health Research BC Scholar Program.
Ethics
This study was carried out according to the Tri-Council Policy Statement Version 2 (TCPS2) and the principles in the Declaration of Helsinki. Ethical approval was received from the University of British Columbia—Providence Health Care Research Ethics Board (H21-03432).
Clinical Trial Number
N/A.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
6/27/2023
Last 2 pages are available as extra blank pages and it has been removed.
Contributor Information
Cecilia T. Costiniuk, Email: cecilia.costiniuk@mcgill.ca
Joel Singer, Email: jsinger@hivnet.ubc.ca.
Judy Needham, Email: jneedham@cheos.ubc.ca.
Yanbo Yang, Email: yanbo.yang@mail.mcgill.ca.
Hong Qian, Email: hqian@cheos.ubc.ca.
Catharine Chambers, Email: catharine.chambers@mail.utoronto.ca.
Ann N. Burchell, Email: ann.burchell@unityhealth.to
Hasina Samji, Email: hasina.samji@bccdc.ca.
Ines Colmegna, Email: ines.colmegna.med@ssss.gouv.qc.ca.
Sugandhi del Canto, Email: sdcanto@catie.ca.
Guy-Henri Godin, Email: guy-henri.godin@sympatico.ca.
Muluba Habanyama, Email: mulubahabanyama@gmail.com.
Christian Hui, Email: achui108@gmail.com.
Abigail Kroch, Email: akroch@ohtn.on.ca.
Enrico Mandarino, Email: emandarino@rogers.com.
Shari Margolese, Email: shari.margolese@gmail.com.
Carrie Martin, Email: carriem@caan.ca.
Maureen Owino, Email: achiengowino@gmail.com.
Tima Mohammadi, Email: tmohammadi@cheos.ubc.ca.
Wei Zhang, Email: wzhang@cheos.ubc.ca.
Sandra Pelaez, Email: sandra.pelaez@umontreal.ca.
Colin Kovacs, Email: ckovacs@mlmedical.com.
Erika Benko, Email: ebenko@mlmedical.com.
Branka Vulesevic, Email: bvulesevic@ohri.ca.
Curtis L. Cooper, Email: ccooper@toh.ca
Aslam H. Anis, Email: aslam.anis@ubc.ca
References
- 1.Tesoriero JM, Gieryic SM, Carrascal A, Lavigne HE. Smoking among HIV positive New Yorkers: prevalence, frequency, and opportunities for cessation. AIDS Behav. 2010;14(4):824–35. doi: 10.1007/s10461-008-9449-2. [DOI] [PubMed] [Google Scholar]
- 2.Lucas GM, Gebo KA, Chaisson RE, Moore RD. Longitudinal assessment of the effects of drug and alcohol abuse on HIV-1 treatment outcomes in an urban clinic. AIDS. 2002;16(5):767–74. doi: 10.1097/00002030-200203290-00012. [DOI] [PubMed] [Google Scholar]
- 3.Byanova K, Kunisaki KM, Vasquez J, Huang L. Chronic obstructive pulmonary disease in HIV. Expert Rev Respir Med. 2021;15(1):71–87. doi: 10.1080/17476348.2021.1848556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sullivan PS, Satcher Johnson A, Pembleton ES, Stephenson R, Justice AC, Althoff KN, et al. Epidemiology of HIV in the USA: epidemic burden, inequities, contexts, and responses. Lancet. 2021;397(10279):1095–106. doi: 10.1016/S0140-6736(21)00395-0. [DOI] [PubMed] [Google Scholar]
- 5.Brown LB, Spinelli MA, Gandhi M. The interplay between HIV and COVID-19: summary of the data and responses to date. Curr Opin HIV AIDS. 2021;16(1):63–73. doi: 10.1097/COH.0000000000000659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Collins LF. Persons with Human Immunodeficiency Virus and the Coronavirus Disease 2019 pandemic: a viral synergy of Biology and sociology. Clin Infect Dis. 2021;73(7):e2106–e8. doi: 10.1093/cid/ciaa1715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Public Health Agency of Canada Canada’s COVID-19. immunization plan: Saving lives and livelihoods 2020 https://www.canada.ca/content/dam/phac-aspc/document/servicces/diseases/2019-novel-coronavirus-infection/canadas-response/canadas-covid-19-vaccines-been-tested-people-hiv Accessed 1 April 2022
- 8.World Health Organization. Ten Threats to Global Health https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 Accessed 3 August 2022
- 9.Anderson RM, Vegvari C, Truscott J, Collyer BS. Challenges in creating herd immunity to SARS-CoV-2 infection by mass vaccination. Lancet. 2020;396(10263):1614–6. doi: 10.1016/S0140-6736(20)32318-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Giambi C, Fabiani M, D’Ancona F, Ferrara L, Fiacchini D, Gallo T, et al. Parental vaccine hesitancy in Italy - results from a national survey. Vaccine. 2018;36(6):779–87. doi: 10.1016/j.vaccine.2017.12.074. [DOI] [PubMed] [Google Scholar]
- 11.Quinn SC, Andrasik MP. Addressing vaccine hesitancy in BIPOC Communities - toward trustworthiness, Partnership, and reciprocity. N Engl J Med. 2021;385(2):97–100. doi: 10.1056/NEJMp2103104. [DOI] [PubMed] [Google Scholar]
- 12.Tankwanchi AS, Bowman B, Garrison M, Larson H, Wiysonge CS. Vaccine hesitancy in migrant communities: a rapid review of latest evidence. Curr Opin Immunol. 2021;71:62–8. doi: 10.1016/j.coi.2021.05.009. [DOI] [PubMed] [Google Scholar]
- 13.Tankwanchi AS, Jaca A, Larson HJ, Wiysonge CS, Vermund SH. Taking stock of vaccine hesitancy among migrants: a scoping review protocol. BMJ Open. 2020;10(5):e035225. doi: 10.1136/bmjopen-2019-035225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Troiano G, Nardi A. Vaccine hesitancy in the era of COVID-19. Public Health. 2021;194:245–51. doi: 10.1016/j.puhe.2021.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Williams SE. What are the factors that contribute to parental vaccine-hesitancy and what can we do about it? Hum Vaccin Immunother. 2014;10(9):2584–96. doi: 10.4161/hv.28596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cunningham RM, Minard CG, Guffey D, Swaim LS, Opel DJ, Boom JA. Prevalence of vaccine hesitancy among expectant mothers in Houston, Texas. Acad Pediatr. 2018;18(2):154–60. doi: 10.1016/j.acap.2017.08.003. [DOI] [PubMed] [Google Scholar]
- 17.Betsch C, Schmid P, Heinemeier D, Korn L, Holtmann C, Bohm R. Beyond confidence: development of a measure assessing the 5 C psychological antecedents of vaccination. PLoS ONE. 2018;13(12):e0208601. doi: 10.1371/journal.pone.0208601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.MacDonald NE, Hesitancy SWGoV. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161–4. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 19.Dube E, Gagnon D, Nickels E, Jeram S, Schuster M. Mapping vaccine hesitancy–country-specific characteristics of a global phenomenon. Vaccine. 2014;32(49):6649–54. doi: 10.1016/j.vaccine.2014.09.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bosnjak M, Ajzen I, Schmidt P. The theory of Planned Behavior: selected recent advances and applications. Eur J Psychol. 2020;16(3):352–6. doi: 10.5964/ejop.v16i3.3107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wolff K. COVID-19 vaccination intentions: the theory of Planned Behavior, optimistic Bias, and anticipated regret. Front Psychol. 2021;12:648289. doi: 10.3389/fpsyg.2021.648289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pang Q, Meng H, Fang M, Xing J, Yao J. Social distancing, health concerns, and digitally empowered consumption behavior under COVID-19: a study on Livestream Shopping Technology. Front Public Health. 2021;9:748048. doi: 10.3389/fpubh.2021.748048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yao J, Pang Q, Zhang B, Wang L, Huang Y. Public Health and Online MICE Technology during the COVID-19 pandemic: the role of Health Beliefs and Technology Innovation. Front Public Health. 2021;9:756987. doi: 10.3389/fpubh.2021.756987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.World Health Organizagion Report on the SAGE Working Group in Vaccine Hesitancy. 2014 https://www.who.int/immunization/sage/meetings/2014/october/1_Report_WORKING_GROUP_vaccine_hesitancy_final.pdf Accesseed July 4 2021
- 25.Larson HJ, Jarrett C, Eckersberger E, Smith DM, Paterson P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007–2012. Vaccine. 2014;32(19):2150–9. doi: 10.1016/j.vaccine.2014.01.081. [DOI] [PubMed] [Google Scholar]
- 26.Earnshaw VA, Chaudoir SR. From conceptualizing to measuring HIV stigma: a review of HIV stigma mechanism measures. AIDS Behav. 2009;13(6):1160–77. doi: 10.1007/s10461-009-9593-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Williams L, Gallant AJ, Rasmussen S, Brown Nicholls LA, Cogan N, Deakin K, et al. Towards intervention development to increase the uptake of COVID-19 vaccination among those at high risk: outlining evidence-based and theoretically informed future intervention content. Br J Health Psychol. 2020;25(4):1039–54. doi: 10.1111/bjhp.12468. [DOI] [PubMed] [Google Scholar]
- 28.Jarolimova J, Yan J, Govere S, Ngobese N, Shazi ZM, Khumalo AR, et al. Medical Mistrust and Stigma Associated with COVID-19 among people living with HIV in South Africa. AIDS Behav. 2021;25(12):3967–77. doi: 10.1007/s10461-021-03307-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jaiswal J, Halkitis PN. Towards a more inclusive and dynamic understanding of Medical Mistrust informed by Science. Behav Med. 2019;45(2):79–85. doi: 10.1080/08964289.2019.1619511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bogart LM, Ojikutu BO, Tyagi K, Klein DJ, Mutchler MG, Dong L, et al. COVID-19 Related Medical Mistrust, Health Impacts, and potential vaccine hesitancy among Black Americans Living with HIV. J Acquir Immune Defic Syndr. 2021;86(2):200–7. doi: 10.1097/QAI.0000000000002570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rodriguez VJ, Alcaide ML, Salazar AS, Montgomerie EK, Maddalon MJ, Jones DL. Psychometric Properties of a vaccine hesitancy scale adapted for COVID-19 vaccination among people with HIV. AIDS Behav. 2022;26(1):96–101. doi: 10.1007/s10461-021-03350-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Public Health Agency of Canada. – Estimates of HIV incidence https://www.canada.ca/en/public-health/services/publications/diseases-conditions/summary-estimates-hiv-incidence-prevalence-canadas-progress-90-90-90. html#s2, 2021
- 33.Karlsson LC, Lewandowsky S, Antfolk J, Salo P, Lindfelt M, Oksanen T, et al. The association between vaccination confidence, vaccination behavior, and willingness to recommend vaccines among finnish healthcare workers. PLoS ONE. 2019;14(10):e0224330. doi: 10.1371/journal.pone.0224330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Larson HJ, de Figueiredo A, Xiahong Z, Schulz WS, Verger P, Johnston IG, et al. The state of Vaccine confidence 2016: global insights through a 67-Country survey. EBioMedicine. 2016;12:295–301. doi: 10.1016/j.ebiom.2016.08.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Govere-Hwenje S, Jarolimova J, Yan J, Khumalo A, Zondi G, Ngcobo M et al. Willingness to accept COVID-19 vaccination among people living with HIV in a high HIV prevalence community.Res Sq. 2022. [DOI] [PMC free article] [PubMed]
- 36.Vallee A, Fourn E, Majerholc C, Touche P, Zucman D. COVID-19 Vaccine Hesitancy among French People Living with HIV.Vaccines (Basel). 2021;9(4). [DOI] [PMC free article] [PubMed]
- 37.Nyblade L, Stockton MA, Giger K, Bond V, Ekstrand ML, Lean RM, et al. Stigma in health facilities: why it matters and how we can change it. BMC Med. 2019;17(1):25. doi: 10.1186/s12916-019-1256-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.McFadden SM, Demeke J, Dada D, Wilton L, Wang M, Vlahov D, et al. Confidence and hesitancy during the early roll-out of COVID-19 Vaccines among Black, Hispanic, and undocumented immigrant Communities: a review. J Urban Health. 2022;99(1):3–14. doi: 10.1007/s11524-021-00588-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ismail SJ, Hardy K, Tunis MC, Young K, Sicard N, Quach C. A framework for the systematic consideration of ethics, equity, feasibility, and acceptability in vaccine program recommendations. Vaccine. 2020;38(36):5861–76. doi: 10.1016/j.vaccine.2020.05.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Statistics Canada https://www.150.statcan.gc.ca/n1/daily-quotidien/220315/dq220315b-eng.htm Accessed 20 May 2021
- 41.Shapiro GK, Tatar O, Dube E, Amsel R, Knauper B, Naz A, et al. The vaccine hesitancy scale: psychometric properties and validation. Vaccine. 2018;36(5):660–7. doi: 10.1016/j.vaccine.2017.12.043. [DOI] [PubMed] [Google Scholar]
- 42.Kaida A, Brotto LA, Murray MCM, Cote HCF, Albert AY, Nicholson V, et al. Intention to receive a COVID-19 vaccine by HIV Status among a Population-Based sample of women and gender diverse individuals in British Columbia, Canada. AIDS Behav. 2022;26(7):2242–55. doi: 10.1007/s10461-022-03577-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zheng W, Sun Y, Li H, Zhao H, Zhan Y, Gao Y, et al. COVID-19 vaccine uptake and hesitancy among HIV-infected men who have sex with men in mainland China: a cross-sectional survey. Hum Vaccin Immunother. 2021;17(12):4971–81. doi: 10.1080/21645515.2021.1996152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ekstrand ML, Heylen E, Gandhi M, Steward WT, Pereira M, Srinivasan K. COVID-19 vaccine hesitancy among PLWH in South India: implications for Vaccination Campaigns. J Acquir Immune Defic Syndr. 2021;88(5):421–5. doi: 10.1097/QAI.0000000000002803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Balfour L, Corace K, Tasca GA, Tremblay C, Routy JP, Angel JB. Altruism motivates participation in a therapeutic HIV vaccine trial (CTN 173) AIDS Care. 2010;22(11):1403–9. doi: 10.1080/09540121003693522. [DOI] [PubMed] [Google Scholar]
- 46.Iliyasu Z, Umar AA, Abdullahi HM, Kwaku AA, Amole TG, Tsiga-Ahmed FI, et al. "They have produced a vaccine, but we doubt if COVID-19 exists”: correlates of COVID-19 vaccine acceptability among adults in Kano, Nigeria. Hum Vaccin Immunother. 2021;17(11):4057–64. doi: 10.1080/21645515.2021.1974796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Agranov M, Elliott M, Ortoleva P. The importance of social norms against Strategic Effects: the case of Covid-19 vaccine uptake. Econ Lett. 2021;206:109979. doi: 10.1016/j.econlet.2021.109979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Schmelz K, Bowles S. Overcoming COVID-19 vaccination resistance when alternative policies affect the dynamics of conformism, social norms, and crowding out. Proc Natl Acad Sci U S A. 2021;118:25. doi: 10.1073/pnas.2104912118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Brunson EK. How parents make decisions about their children’s vaccinations. Vaccine. 2013;31(46):5466–70. doi: 10.1016/j.vaccine.2013.08.104. [DOI] [PubMed] [Google Scholar]
- 50.Brunson EK. The impact of social networks on parents’ vaccination decisions. Pediatrics. 2013;131(5):e1397–404. doi: 10.1542/peds.2012-2452. [DOI] [PubMed] [Google Scholar]
- 51.Carolan K, Verran J, Crossley M, Redfern J, Whitton N, Amos M. Impact of educational interventions on adolescent attitudes and knowledge regarding vaccination: a pilot study. PLoS ONE. 2018;13(1):e0190984. doi: 10.1371/journal.pone.0190984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Piedimonte S, Leung A, Zakhari A, Giordano C, Tellier PP, Lau S. Impact of an HPV Education and Vaccination Campaign among Canadian University students. J Obstet Gynaecol Can. 2018;40(4):440–6. doi: 10.1016/j.jogc.2017.07.028. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All relevant data are within the paper and its supporting files.