Abstract
Introduction
The aim of this study was to explore the chronological trends in clinical features and utilization of healthcare resources for hospitalized patients with urolithiasis in China.
Methods
Patients with urolithiasis were extracted from the Hospital Quality Monitoring System, a national database of hospitalized patients in China, based on the International Classification of Diseases, Tenth Revision, codes. Variables including demographic characteristics, comorbidities, treatment modalities for urolithiasis, length of hospital stay, and expenditures were collected and analyzed.
Results
Among 79.8 million hospitalized patients, 3.5 million were diagnosed with urolithiasis with an increasing trend (from 3.0% in 2013 to 4.0% in 2018). Most of these patients had upper urinary tract calculi (76.6% in 2013 and 81.7% in 2018). Middle-aged patients (46–65 years) constituted the largest proportion with a stable trend (from 46.9% in 2013 to 48.8% in 2018), while the proportion of older patients (>65 years) showed an increasing trend (from 23.7% in 2013 to 27.4% in 2018). The percentages of gout/hyperuricemia, hypertension, diabetes, and cardiovascular disease among the hospitalized patients with urolithiasis increased steadily, with the sharpest increases in patients from rural areas. Overall, 656,952 patients (18.9%) received surgical interventions for urolithiasis. The proportions of ureteroscopy and extracorporeal shockwave lithotripsy increased steadily during the 6-year study period, with simultaneous decreases in open surgery and percutaneous nephrolithotomy. The median length of hospital stay decreased from 10 days to 8 days. The cost of urolithiasis intervention accounted for 2.0% of the total hospitalization fee in 2013 and increased to 2.7% in 2018.
Conclusions
The analysis showed an increasing trend in the percentage of hospitalized patients with urolithiasis, accompanied by an increased percentage of the total hospitalization fee for urolithiasis intervention during the 6-year study period. Based on the increasing trends in the proportion of older patients (>65 years) and percentages of metabolic comorbidities among patients with urolithiasis, an increased burden of urolithiasis on the healthcare system in China is anticipated.
Keywords: Urinary tract calculi, Urolithiasis, Trends, Treatment, Intervention, Metabolic disease
Introduction
Urolithiasis is a common urological disease presenting with symptoms such as hydronephrosis, urinary tract infection, hematuria, and lumbago that can eventually induce development of chronic kidney disease and renal function decline [1]. The incidence and prevalence of urolithiasis have steadily increased in developed countries as well as developing countries during the past few decades [2]. The prevalence of kidney calculi verified by ultrasonography examination was 6.4% in the latest nationwide Chinese survey conducted in 2013–2014, with approximately one in every 17 Chinese adults affected [3]. Due to its high prevalence and recurrence rate, interventions for urolithiasis represent a significant burden on healthcare systems worldwide.
Epidemiological studies indicated that aging, dietary factors, and metabolic diseases such as diabetes, obesity, hypertension, and metabolic syndrome were associated with the incidence of urolithiasis. For example, the rising prevalence of urolithiasis in the USA has been linked to increasing rates of obesity, diabetes, and metabolic syndrome in the country [4, 5, 6]. Meanwhile, obesity was identified as a shared risk factor for the incidence of kidney calculi in both men and women in two prospective cohorts: the Shanghai Women's Health Study and the Shanghai Men's Health Study [7]. Recently, it was reported that new onset of hypertension, diabetes, and obesity was strongly associated with an increased risk of kidney calculi development in the prospective Qingdao Port Cardiovascular Health Study [8]. Lifestyle and dietary habits have greatly changed with the industrialization of China during the last several decades, and dramatically increased prevalence of noncommunicable diseases such as obesity, hypertension, diabetes, metabolic syndrome, and cardiovascular disease has been observed [9]. At the same time, China has become an aging society [10]. We hypothesize that these changes may bring about substantial changes to the problem of urolithiasis in China. It would be optimal to conduct another population-based nationwide survey on the incidence and prevalence of urolithiasis to test this hypothesis. However, based on the time and economic cost required for such a study, we chose to investigate the issue by analyzing data from the Hospital Quality Monitoring System (HQMS) over a 6-year period (2013–2018). We aimed to evaluate the chronological trends in the frequency and characteristics of hospitalized patients with urolithiasis and the changing patterns in surgical intervention modalities for treatment of calculi and associated expenditure.
Materials and Methods
Data Source
Hospital discharges between January 1, 2013, and December 31, 2018, were extracted from the HQMS, a national database containing standardized electronic inpatient discharge records for tertiary hospitals in China. Under the administration of the National Health Commission of the People's Republic of China, tertiary hospitals in China have mandatorily and automatically submitted daily electronic discharge records to the HQMS since January 1, 2013.
The front page of each discharge record includes the inpatient diagnoses, demographic characteristics, procedures, and expenditures per hospitalization. All diagnoses are encoded using the International Classification of Disease, Tenth Revision (ICD-10). All procedures are encoded using the International Classification of Diseases, Ninth Revision, Clinical Modification.
For the present study, we enrolled patients with urolithiasis identified by ICD-10 codes. For patients with multiple admissions, only the first admission was included in the analysis. Patients were excluded if they lacked an identification number or were <18 years of age. Urban/rural residency was identified by the type of health insurance (basic or free medical insurance for urban residency; new rural cooperative medical care for rural residency). The Ethics Committee of Peking University First Hospital approved the study.
Patient Characteristics
The patient characteristics, including age, sex, residency, expected source of payment, type of admission, intensive care unit stay, diagnoses, length of hospital stay, and expenditure, were extracted from the front page of the medical records.
Definition
The ICD-10 codes for the discharge diagnoses were used to identify inpatients with a primary or secondary diagnosis of urinary tract calculi (relevant ICD-10 codes in online suppl. Table S1; see www.karger.com/doi/10.1159/000527967 for all online suppl. material) between January 1, 2013, and December 31, 2018. Upper urinary tract calculus was defined as a calculus located in the kidney and/or ureter. Lower urinary tract calculus was defined as a calculus located in the bladder and/or urethra. Diagnosis of various comorbidities, including gout and/or hyperuricemia, cardiovascular diseases, hypertension, diabetes, and obesity, was based on the ICD-10 codes extracted from the front page (online suppl. Tables S2–S6). Within the identified population, we searched for patients who underwent interventions for urinary tract calculi (relevant International Classification of Diseases, Ninth Revision, Clinical Modification codes in online suppl. Tables S7).
Statistical Analysis
Data from January 1, 2013, to December 31, 2018, were used to assess the temporal trends in patient proportions, background characteristics, and management. Frequencies and proportions were generated for categorical variables. The proportion of upper urinary tract calculi was calculated as the number of patients with upper urinary tract calculi divided by the total number of urolithiasis patients. Similar calculations were performed for the proportions of lower urinary tract calculi, urinary calculi unspecified, kidney calculi, ureteral calculi, and kidney and ureteral calculi. The percentages of comorbidities were calculated as the number of patients with each comorbidity divided by the total number of urolithiasis patients. The proportions of interventional procedures were calculated as the number of patients with each procedure divided by the total number of interventional procedures. The frequency of urolithiasis patients among the tertiary hospital inpatient population was calculated as the number of patients with urolithiasis divided by the number of tertiary hospital inpatients in each year. The frequency of urolithiasis patients among the inpatient population in various regions was calculated as the number of patients with urolithiasis divided by the number of tertiary hospital inpatients in relevant geographical regions (south, central, southwest, east, northwest, northeast, and north). The total frequency of urolithiasis patients among the whole inpatient population was calculated as the proportion of urolithiasis patients in tertiary hospitals multiplied by the proportion of inpatients in tertiary hospitals to the total number of inpatients in China, which was obtained from the China Statistical Yearbook. Continuous data were presented as the mean ± standard deviation or as the median (interquartile range) for highly skewed variables. Categorical variables were presented as the proportion. One-way ANOVA or the Kruskal-Wallis test was used to compare continuous variables and χ2 test was used to compare categorical variables. A two-sided value of p < 0.05 was considered statistically significant. All analyses were conducted using SAS software version 9.4 (SAS Institute, Cary, NC, USA).
Results
Demographic Data
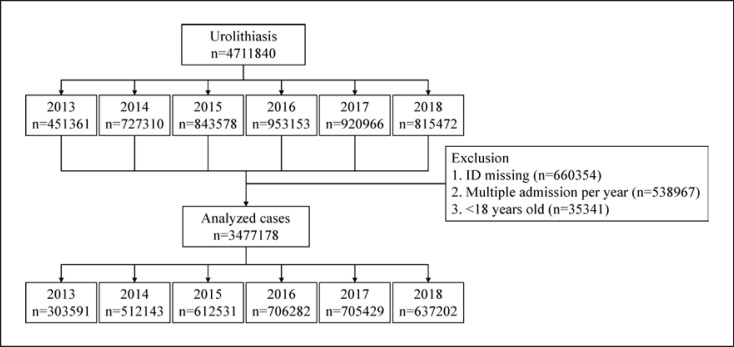
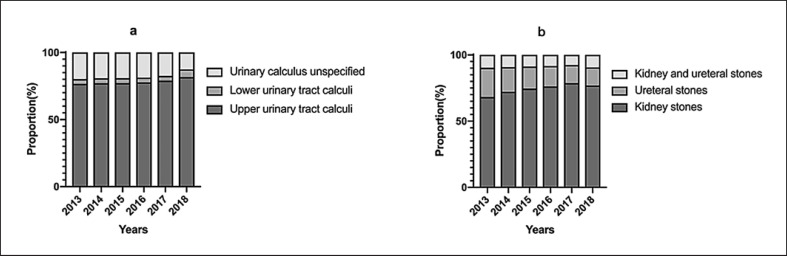
Between January 1, 2013, and December 31, 2018, 4.8 million patients were hospitalized with a diagnosis of urinary tract calculi. After deduplication and exclusion of patients who lacked an identification number or were <18 years of age, we identified 3,477,178 patients who were eligible for the analysis, representing 3.6% of the total admissions (Fig. 1). As shown in Table 1, the frequency of admission with a diagnosis of urolithiasis increased moderately but steadily during the study period in the tertiary hospitals, from the lowest rate of 3.0% in 2013 to the highest rate of 4.0% in 2018, while the proportion of patients with urolithiasis relative to the total number of inpatients in China remained relatively stable. The top three regions with the highest proportions of inpatients with urolithiasis were the south, central, and southwest. Patients with a diagnosis of upper urinary tract calculi constituted the majority of the urolithiasis cases over the 6-year study period, ranging from 76.6% in 2013 to 81.7% in 2018 (Fig. 2a). A subset analysis of patients with upper urinary tract calculi revealed that the proportion of kidney calculi increased steadily during the 6-year study period, accompanied by a decrease in the proportion of ureteric calculi only, while the proportion of both renal and ureteric calculi remained relatively stable (Fig. 2b).
Fig. 1.
Flowchart of patients' enrollment.
Table 1.
General data of hospitalized patients with urolithiasis
| 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | |
|---|---|---|---|---|---|---|
| Number | 303,591 | 512,143 | 612,531 | 706,282 | 705,429 | 637,202 |
| Frequencya (%) | 3.0 | 3.3 | 3.5 | 3.6 | 3.8 | 4.0 |
| Frequencyb (%) | 0.2 | 0.3 | 0.3 | 0.3 | 0.3 | 0.3 |
| Age (years) | 54.1±15.2 | 54.6±15.1 | 55.0±15.1 | 55.3±15.0 | 55.6±15.0 | 55.9±14.9 |
| Age group (%)* | ||||||
| 18–45 | 29.4 | 27.8 | 26.7 | 25.8 | 24.8 | 23.8 |
| 46–65 | 46.9 | 47.5 | 47.9 | 48.2 | 48.4 | 48.8 |
| >65 | 23.7 | 24.6 | 25.4 | 26.1 | 26.8 | 27.4 |
| Males (%) Region (%) | 63.8 | 63.6 | 63.8 | 63.8 | 63.9 | 63.7 |
| South | 4.0 | 4.3 | 4.7 | 4.7 | 4.7 | 4.7 |
| Central | 3.2 | 3.3 | 3.7 | 4.1 | 4.1 | 4.5 |
| Southwest | 3.9 | 4.4 | 4.6 | 4.6 | 4.5 | 4.0 |
| East | 1.5 | 1.6 | 1.7 | 1.7 | 2.0 | 2.1 |
| Northwest | 1.5 | 1.6 | 1.7 | 1.7 | 2.0 | 2.1 |
| Northeast | 1.6 | 1.7 | 1.7 | 1.8 | 1.8 | 1.9 |
| North | 1.0 | 1.1 | 1.3 | 1.3 | 1.4 | 1.5 |
The proportion of urolithiasis patients to the inpatient in tertiary hospitals.
The proportion of urolithiasis patients to the total number of inpatients.
p < 0.001.
Fig. 2.
Proportion of hospitalized patients with urolithiasis stratified by calculi location from 2013 to 2018.
Overall, 2.2 million hospitalized men had urolithiasis, constituting the majority (64%) of the cases diagnosed with urolithiasis. The temporal trend in the male-to-female ratio among hospitalized patients with urolithiasis was relatively constant during the study period (Table 1).
The mean age of the patients with urolithiasis remained constant at 55 years during the study period. Middle-aged patients (46–65 years) constituted the largest proportion of hospitalized patients with urinary tract calculi, and this proportion remained largely unchanged during the study period. Age trend analyses revealed an increasing trend in the proportion of older patients (>65 years) with urolithiasis, from 23.7% in 2013 to 27.4% in 2018. Conversely, there was a decreasing trend in the proportion of younger hospitalized patients with urolithiasis (Table 1). Table 2 shows the chronological changes in the sex- and age-related percentages of upper urinary tract calculi during the 6-year study period. In men, the peak age shifted from the 41- to 60-year-old group to the 51- to 70-year-old group. In women, the peak age remained stable in the 51- to 60-year-old group, while the secondary peak age shifted from the 41- to 50-year-old group to the 61- to 70-year-old group.
Table 2.
Chronological trend of upper urinary tract calculi stratified by sex and age over the 6-year period
| 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | |
|---|---|---|---|---|---|---|
| Men (%) | ||||||
| 18–30 | 6.8 | 6.3 | 6.0 | 5.8 | 5.5 | 5.2 |
| 31–40 | 13.2 | 12.2 | 11.6 | 11.1 | 10.7 | 10.7 |
| 41–50 | 23.4 | 22.2 | 21.6 | 21.0 | 20.4 | 19.9 |
| 51–60 | 23.1 | 23.7 | 24.1 | 24.3 | 24.4 | 24.7 |
| 61–70 | 18.8 | 20.3 | 21.2 | 22.1 | 22.7 | 23.2 |
| 71–80 | 11.2 | 11.7 | 11.7 | 11.8 | 12.0 | 12.0 |
| >80 | 3.5 | 3.6 | 4.0 | 4.0 | 4.3 | 4.3 |
| Women (%) | ||||||
| 18–30 | 7.5 | 7.0 | 6.8 | 6.5 | 6.1 | 5.7 |
| 31–40 | 10.9 | 10.3 | 9.8 | 9.5 | 9.5 | 9.5 |
| 41–50 | 22.6 | 21.9 | 20.7 | 19.9 | 19.3 | 19.0 |
| 51–60 | 25.2 | 25.4 | 25.5 | 25.5 | 25.7 | 25.6 |
| 61–70 | 19.3 | 20.5 | 21.4 | 22.3 | 22.6 | 23.2 |
| 71–80 | 11.2 | 11.3 | 11.7 | 11.9 | 12.1 | 12.3 |
| >80 | 3.3 | 3.6 | 4.1 | 4.3 | 4.7 | 4.7 |
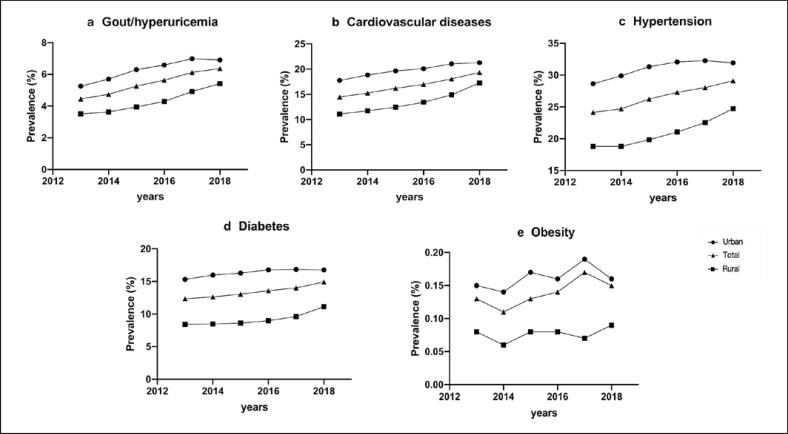
Figure 3 shows the temporal trends in the percentages of comorbidities in the patients with urolithiasis during the 6-year study period. The percentages of gout/hyperuricemia and cardiovascular disease increased markedly among patients with urolithiasis (42% increase from 4.5% in 2013 to 6.4% in 2018 and 33.7% increase from 14.5% in 2013 to 19.4% in 2018, respectively). The percentages of diabetes and hypertension also increased but to lesser degrees (21% increase from 12.3% to 14.9% and 20.7% increase from 24.1% to 29.1%, respectively). The proportion of obesity remained relatively stable at approximately 0.1–0.2% during the study period. Further analysis showed that the percentages of these comorbidities increased in both urban and rural patients with urolithiasis during the 6-year study period, with sharper increases observed in rural patients.
Fig. 3.
Prevalence of comorbidities in hospitalized patients with urinary tract calculi from 2013 to 2018.
Procedural Data
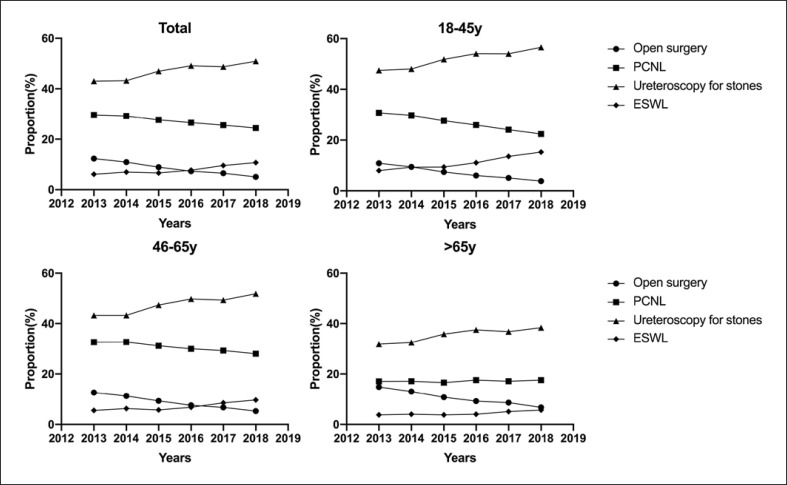
656,952 patients (18.9%) received surgical interventions for urolithiasis. We conducted subgroup analyses of the inpatients who received interventions for urolithiasis. As shown in online suppl. Table S8, these patients showed similar chronological trends in the age proportions and comorbidity prevalence to the whole population. Figure 4 shows the temporal trends in the choices of interventional treatments for upper urinary tract calculi during the 6-year study period. Overall, there were significant declines in the proportions of open surgery (58.9% reduction) and percutaneous nephrolithotomy (17.5% reduction). Performance of extracorporeal shockwave lithotripsy (ESWL) increased from 6.1% in 2013 to 10.7% in 2018 and surpassed the performance of open surgery from 2016. The proportion of ureteroscopic lithotripsy increased steadily (18.4% increase) during the study period. The temporal trends in the choices of interventional treatments were similar to those in the total population when stratified by age (Fig. 4) and comorbidities (online suppl. Fig. S1). Analyses showed that adoption of ESWL increased for treatment of both ureteric calculi and kidney calculi (online suppl. Table S9). A major increase in ureteroscopic lithotripsy adoption was observed for treatment of kidney calculi, while the proportion of ureteroscopic lithotripsy for treatment of ureteric calculi remained stable during the study period (online suppl. Table S9). We further analyzed the relationships of interventions with age and comorbidities (online suppl. Table S10). Patients who received open surgery were relatively older and had higher percentages of hypertension and cardiovascular disease comorbidities, while patients who received ESWL were the youngest and had low frequencies of all comorbidities except for gout.
Fig. 4.
Proportion of interventional procedures for upper urinary tract calculi in hospitalized patients from 2013 to 2018.
During the study period, there was an ongoing trend toward shorter hospital stays for patients who received interventions for urolithiasis (Table 3). The percentage of expenditure for urolithiasis treatments relative to the total annual expenditure for hospitalization increased from 2.0% in 2013 to 2.7% in 2018. The expenditure for urolithiasis treatment increased from 15,800 yuan to 18,500 yuan per hospitalization as well.
Table 3.
Information of interventional procedures for urolithiasis
| 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | |
|---|---|---|---|---|---|---|
| Interventional frequency (%) | 23.6 | 22.5 | 21.5 | 20.9 | 18.5 | 17.6 |
| Cost percentage of urolithiasis intervention (%) | 2.0 | 2.2 | 2.4 | 2.5 | 2.6 | 2.7 |
| Expenditure per urolithiasis hospitalization (1,000 RMB), median (Q1, Q3) | 15.8 (11.3, 21.8) | 16.4 (11.4, 22.8) | 17.3 (12.1, 24.0) | 17.8 (12.1, 24.7) | 17.6 (12.1, 24.2) | 18.5 (12.6, 25.1) |
| Length of stay (days), median (Q1, Q3) | 10 (7, 15) | 10 (7, 14) | 10 (7, 14) | 9 (6, 13) | 9 (6, 13) | 8 (5, 12) |
Discussion
Using data from a large national inpatient database from 2013 to 2018, we determined the temporal trends in the frequency and characteristics of hospitalized patients with urolithiasis, as well as the interventional procedure choices and expenditures in China for the first time. We observed a trend toward increased frequency of urolithiasis among hospitalized patients during the study period. The percentages of metabolic comorbidities among patients with urolithiasis increased during the 6-year study period, together with the proportion of older patients (>65 years). In addition, less invasive procedures were adopted more frequently as time progressed, accompanied by shortening of the hospital stay and increased expenditure.
Clearly, our results cannot be used to estimate the true incidence or prevalence of urolithiasis in China because not all patients with urolithiasis would be symptomatic and require further evaluation and/or treatment in hospitals. In fact, as shown in the present study, only approximately 20% of hospitalized patients with urolithiasis were admitted for interventions per se, while the others were admitted for treatment of other diseases and had urolithiasis as a comorbidity. However, the unique point of the present study is its provision of chronological trends in the annual changes in percentages of urolithiasis cases in a relatively defined and representative cohort, which would not be found in cross-sectional epidemiological surveys. We found that the percentage of patients with urolithiasis among hospitalized patients increased annually in the present study.
Of particular interest is the finding that the percentages of comorbidities, including diabetes, hypertension, gout, obesity, and cardiovascular disease, among patients with urolithiasis, increased annually during the study period. Epidemiological studies suggested that these noncommunicable chronic diseases were associated with the incidence of urolithiasis. It is important to note that the prevalence of these noncommunicable chronic diseases has greatly increased during the past few decades in the Chinese population, which may be attributed to the marked changes in lifestyle, including dietary habits, and the accelerating progress of population aging in China. The prevalence of diabetes was only 2.5% in the 1990s but increased to 9.7% in 2007–2008 and 11.6% in 2010 [11, 12, 13]. Similar trends have been observed for hypertension, obesity, and metabolic syndrome, among others [9, 14, 15, 16]. The surging prevalence of these diseases may have substantial effects on their related comorbidities as a consequence. For example, chronic kidney disease related to diabetes has become more common than chronic kidney disease related to glomerulonephritis in both the general population and hospitalized patients in China since 2011, a finding that is preceded by decades of increasing diabetes prevalence [17]. Therefore, it is conceivable that the prevalence of urolithiasis will also continue to increase in China in the coming years if the increasing trends in these metabolic diseases persist. Since the development of urinary tract calculi is potentially preventable by appropriate control of metabolic risk factors, we need to consider how to improve the management of urinary calculi by educating people to change their lifestyles appropriately to reduce the risks of both metabolic disease and calculi disease.
Another finding of the present study is that the proportion of older patients with urinary tract calculi increased during the 6-year study period. Older patients (>65 years) comprised 23.7% of all inpatients with urolithiasis in 2013 but increased to 27.4% in 2018. This appears to contrast with the observation of an increasing prevalence of urolithiasis in younger populations [18, 19], which was attributed to global warming, dietary habit alterations, and increased metabolic risk factors, such as obesity, among younger populations in recent years [3, 20]. One possible reason is that China is rapidly becoming an aging society [21]. Given that the present study only involved inpatients and older people were more likely to be admitted for evaluation and treatment of various comorbidities, this may have increased the chance for urolithiasis detection on routine examinations after admission. We also observed that the peak age for urolithiasis moved toward older age groups for both men and women in the present study, consistent with the finding that aging per se was a risk factor for urinary calculi. We consider that these findings at least partly reflect an ongoing change in the demographic burden of urinary tract calculi in China that requires more attention. As mentioned earlier, China is experiencing accelerated population aging, and this change may exert more influence on the Chinese healthcare system in the near future [10].
We noted that the regional distribution of urolithiasis did not change much during the 6-year study period. The south, central, and southwest regions had higher proportions of urolithiasis inpatients than the east, northwest, northeast, and north regions, in accordance with the observations from previous studies. This may be related to the elevated temperatures and many hours of sunshine as well as some dietary habits in these regions [22, 23].
The present analysis showed an increase in the proportion of kidney calculi during the 6-year study period, while the proportion of ureteric calculi declined. Interestingly, analysis for the trends in delivery of care for urolithiasis showed a trend toward decreased adoption of procedures specific to kidney calculi such as open surgery and percutaneous nephrolithotomy during the 6-year study period, which differed from the trends found in developed countries [24, 25]. Meanwhile, the proportions of ureteroscopic and ESWL procedures increased during the study period. These findings reflect the increasing availability of both equipment and experienced specialists for less invasive procedures such as ureteroscopy and ESWL in China in recent years. On the one hand, adoption of minimally invasive procedures can make the treatment more effective with fewer complications and faster recovery and shorten hospital stays as shown in the present analysis. On the other hand, this adoption can increase the total costs, which may partly explain the differences in procedures adopted among different countries, considering the different medical care systems and reimbursement policies involved. From this point of view, there is a need for Chinese urologists to optimize the procedure options for urolithiasis, trying to balance economic pressure, patient recovery, and hospital stay.
The strength of the present study is that we evaluated all admissions with diagnosis codes for urinary tract calculi as either a primary or secondary diagnosis in the inpatient database. This helped to create a comprehensive evaluation of the temporal trends in the percentages and characteristics of patients with urolithiasis in the present analysis, which was not fully reported in previous cross-sectional studies. However, the present study has a number of limitations that should be considered when interpreting the results. First, the nature of the dataset means that the true prevalence of urolithiasis cannot be extrapolated from the percentage of urolithiasis cases among hospitalized patients in the present study. Furthermore, a causality analysis between metabolic diseases and urolithiasis incidence could not be conducted. Second, only data for patients admitted to tertiary hospitals are included in the HQMS. Data for patients with urolithiasis treated solely in secondary or community hospitals are not captured and included in the HQMS, which may confer bias on the analysis. Third, the findings regarding the use of ESWL in the present study may underestimate the total use of this procedure in China because the procedure may be performed in outpatient departments in some hospitals. Fourth, the study cannot provide any detailed information on calculi composition analysis, calculus burden or size, and morbidity of treatments.
In summary, the present study examined temporal trends (2013–2018) in demographic and clinical features among hospitalized patients with urinary tract calculi in China. The findings of increased percentages of metabolic comorbidities as well as the increased proportion of older patients during the study period signify an anticipated increase in the burden of urolithiasis in China in the near future. Not only improvements in surgical intervention procedures but also efforts to prevent the continuous increase in metabolic diseases should be integrated to improve the management of urinary calculi.
Statement of Ethics
The Ethics Committee of Peking University First Hospital reviewed and approved the study (2020-018). Acquisition of informed consent was exempted.
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
This study was supported by grants from the National Natural Science Foundation of China (91846101, 82003529), Beijing Nova Programme Interdisciplinary Cooperation Project (Z191100001119008), National Key R&D Program of the Ministry of Science and Technology of China (2019YFC2005000), Peking University (BMU2018MX020, PKU2017LCX05), CAMS Innovation Fund for Medical Sciences (2019-I2M-5-046), PKU-Baidu Fund (2019BD017), and the China-World Health Organization Biennial Collaborative Projects 2018–2019 (2019/892000-0). The authors thank the Bureau of Medical Administration and Medical Service Supervision, National Health Commission of the People's Republic of China, and the World Health Organization for the support of this study.
Author Contributions
Research area and study design: Yu Wang, Haibo Wang, Luxia Zhang, and Ming-Hui Zhao; data acquisition: Chao Yang, Jinwei Wang, and Shi Ying; data analysis/interpretation: Qin Wang, Chao Yang, Yu Wang, and Jinwei Wang; statistical analysis: Qin Wang. Each author contributed important intellectual content during manuscript drafting or revision and accepts accountability for the overall work by ensuring that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved. Yu Wang takes responsibility that this study has been reported honestly, accurately, and transparently, that no important aspects of the study have been omitted, and that any discrepancies from the study as planned have been explained.
Data Availability Statement
The data that support the findings of this study are available from the Bureau of Medical Administration and Medical Service Supervision, National Health Commission of China, but restrictions apply to the availability of these data, which were used under license for the current study and so are not publicly available. Data are, however, available from the authors upon reasonable request and with permission of the Bureau of Medical Administration and Medical Service Supervision, National Health Commission of China.
Supplementary Material
Supplementary data
Supplementary data
Acknowledgment
We thank Alison Sherwin, PhD, from Liwen Bianji, Edanz Group China (www.liwenbianji.cn/ac), for editing the English text of a draft of this manuscript.
Funding Statement
This study was supported by grants from the National Natural Science Foundation of China (91846101, 82003529), Beijing Nova Programme Interdisciplinary Cooperation Project (Z191100001119008), National Key R&D Program of the Ministry of Science and Technology of China (2019YFC2005000), Peking University (BMU2018MX020, PKU2017LCX05), CAMS Innovation Fund for Medical Sciences (2019-I2M-5-046), PKU-Baidu Fund (2019BD017), and the China-World Health Organization Biennial Collaborative Projects 2018–2019 (2019/892000-0). The authors thank the Bureau of Medical Administration and Medical Service Supervision, National Health Commission of the People's Republic of China, and the World Health Organization for the support of this study.
References
- 1.Alexander RT, Hemmelgarn BR, Wiebe N, Bello A, Morgan C, Samuel S, et al. Kidney stones and kidney function loss: a cohort study. BMJ. 2012;345((aug29 2)):e5287. doi: 10.1136/bmj.e5287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Raheem OA, Khandwala YS, Sur RL, Ghani KR, Denstedt JD. Burden of urolithiasis: trends in prevalence, treatments, and costs. Eur Urol Focus. 2017;3((1)):18–26. doi: 10.1016/j.euf.2017.04.001. [DOI] [PubMed] [Google Scholar]
- 3.Zeng G, Mai Z, Xia S, Wang Z, Zhang K, Wang L, et al. Prevalence of kidney stones in China: an ultrasonography based cross-sectional study. BJU Int. 2017;120((1)):109–116. doi: 10.1111/bju.13828. [DOI] [PubMed] [Google Scholar]
- 4.Scales CD, Jr, Curtis LH, Norris RD, Springhart WP, Sur RL, Schulman KA, et al. Changing gender prevalence of stone disease. J Urol. 2007;177((3)):979–982. doi: 10.1016/j.juro.2006.10.069. [DOI] [PubMed] [Google Scholar]
- 5.Nowfar S, Palazzi-Churas K, Chang DC, Sur RL. The relationship of obesity and gender prevalence changes in United States inpatient nephrolithiasis. Urology. 2011;78((5)):1029–1033. doi: 10.1016/j.urology.2011.04.011. [DOI] [PubMed] [Google Scholar]
- 6.Geraghty R, Abdi A, Somani B, Cook P, Roderick P. Does chronic hyperglycaemia increase the risk of kidney stone disease? results from a systematic review and meta-analysis. BMJ Open. 2020;10((1)):e032094. doi: 10.1136/bmjopen-2019-032094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shu X, Cai H, Xiang YB, Li H, Lipworth L, Miller NL, et al. Nephrolithiasis among middle aged and elderly urban Chinese: a report from prospective cohort studies in Shanghai. J Endourology. 2017;31((12)):1327–1334. doi: 10.1089/end.2017.0467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ping H, Lu N, Wang M, Lu J, Liu Y, Qiao L, et al. New-onset metabolic risk factors and the incidence of kidney stones: a prospective cohort study. BJU Int. 2019;124((6)):1028–1033. doi: 10.1111/bju.14805. [DOI] [PubMed] [Google Scholar]
- 9.Xi B, Liang Y, He T, Reilly KH, Hu Y, Wang Q, et al. Secular trends in the prevalence of general and abdominal obesity among Chinese adults, 1993-2009. Obes Rev. 2012;13((3)):287–296. doi: 10.1111/j.1467-789X.2011.00944.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fang EF, Scheibye-Knudsen M, Jahn HJ, Li J, Ling L, Guo H, et al. A research agenda for aging in China in the 21st century. Ageing Res Rev. 2015;24((Pt B)):197–205. doi: 10.1016/j.arr.2015.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pan XR, Yang WY, Li GW, Liu J, National Diabetes Prevention and Control Cooperative Group Prevalence of diabetes and its risk factors in China, 1994. Diabetes Care. 1997;20((11)):1664–1669. doi: 10.2337/diacare.20.11.1664. [DOI] [PubMed] [Google Scholar]
- 12.Yang W, Lu J, Weng J, Jia W, Ji L, Xiao J, et al. Prevalence of diabetes among men and women in China. N Engl J Med. 2010;362((12)):1090–1101. doi: 10.1056/NEJMoa0908292. [DOI] [PubMed] [Google Scholar]
- 13.Xu Y, Wang L, He J, Bi Y, Li M, Wang T. Prevalence and control of diabetes in Chinese adults. JAMA. 2013;310((9)):948–959. doi: 10.1001/jama.2013.168118. [DOI] [PubMed] [Google Scholar]
- 14.Lan Y, Mai Z, Zhou S, Liu Y, Li S, Zhao Z, et al. Prevalence of metabolic syndrome in China: an up-dated cross-sectional study. PLoS One. 2018;13((4)):e0196012. doi: 10.1371/journal.pone.0196012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang Z, Chen Z, Zhang L, Wang X, Hao G, Zhang Z, et al. Status of hypertension in China: results from the China hypertension survey, 2012-2015. Circulation. 2018;137((22)):2344–2356. doi: 10.1161/CIRCULATIONAHA.117.032380. [DOI] [PubMed] [Google Scholar]
- 16.Chen Y, Peng Q, Yang Y, Zheng S, Wang Y, Lu W. The prevalence and increasing trends of overweight, general obesity, and abdominal obesity among Chinese adults: a repeated cross-sectional study. BMC Public Health. 2019;19((1)):1293. doi: 10.1186/s12889-019-7633-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang L, Long J, Jiang W, Shi Y, He X, Zhou Z, et al. Trends in chronic kidney disease in China. N Engl J Med. 2016;375((9)):905–906. doi: 10.1056/NEJMc1602469. [DOI] [PubMed] [Google Scholar]
- 18.Frassetto L, Kohlstadt I. Treatment and prevention of kidney stones: an update. Am Fam Physician. 2011;84((11)):1234–1242. [PubMed] [Google Scholar]
- 19.Tseng TY, Preminger GM. Kidney stones. BMJ Clin Evid. 2011:2011. [PMC free article] [PubMed] [Google Scholar]
- 20.Zeng Q, He Y. Age-specific prevalence of kidney stones in Chinese urban inhabitants. Urolithiasis. 2013;41((1)):91–93. doi: 10.1007/s00240-012-0520-0. [DOI] [PubMed] [Google Scholar]
- 21.Liu Y, Chen Y, Liao B, Luo D, Wang K, Li H, et al. Epidemiology of urolithiasis in asia. Asian J Urol. 2018;5((4)):205–214. doi: 10.1016/j.ajur.2018.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Deyi Luo HL, Wang K. Epidemiology of stone disease in China. In: JamsheerTalati JDMA, Tiselius H-G̈, Ye Z, editors. Urolithiasis. Springer; 2012. pp. p. 53–59. [Google Scholar]
- 23.Yang Y, Deng Y, Wang Y. Major geogenic factors controlling geographical clustering of urolithiasis in China. Sci The Total Environ. 2016;571:1164–1171. doi: 10.1016/j.scitotenv.2016.07.117. [DOI] [PubMed] [Google Scholar]
- 24.Ghani KR, Sammon JD, Karakiewicz PI, Sun M, Bhojani N, Sukumar S, et al. Trends in surgery for upper urinary tract calculi in the USA using the Nationwide Inpatient Sample: 1999-2009. BJU Int. 2013;112((2)):224–230. doi: 10.1111/bju.12059. [DOI] [PubMed] [Google Scholar]
- 25.Heers H, Turney BW. Trends in urological stone disease: a 5-year update of hospital episode statistics. BJU Int. 2016;118((5)):785–789. doi: 10.1111/bju.13520. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary data
Supplementary data
Data Availability Statement
The data that support the findings of this study are available from the Bureau of Medical Administration and Medical Service Supervision, National Health Commission of China, but restrictions apply to the availability of these data, which were used under license for the current study and so are not publicly available. Data are, however, available from the authors upon reasonable request and with permission of the Bureau of Medical Administration and Medical Service Supervision, National Health Commission of China.