Abstract
Background
Physiotherapy-led airway clearance interventions are indicated for some people with chronic lung conditions. This study describes Australian clinical models for the provision of adult airway clearance services.
Methods
This cross-sectional national study recruited public and private health care providers (excluding cystic fibrosis-specific services) identified by a review of websites. Providers were invited to complete an electronic 61-item survey with questions about airway clearance service context, referral demographics, service provision and program metrics. Data were reported descriptively with differences between metropolitan and non-metropolitan services explored with chi-square tests.
Results
Between October-December 2019, the survey was disseminated to 131 providers with 91 responses received (69% response rate; 87 (96%) public (34 metropolitan; 53 non-metropolitan) and 4 (4%) private). Intent (chronic condition self-management) and types of intervention provided (education, breathing techniques, exercise prescription) were common across all services. Geographic location was associated with differences in airway clearance service models (greater use of regular clinics, telephone/telehealth consultations and dedicated cardiorespiratory physiotherapists in metropolitan locations versus clients incurring service and device provision costs in non-metropolitan regions).
Conclusions
While similarities in airway clearance interventions exist, differences in service models may disadvantage people living with chronic lung conditions, especially in non-metropolitan regions of Australia.
Keywords: Airway clearance, respiratory, physiotherapy, chronic lung conditions, service provision
Introduction
In 2017 chronic lung diseases affected an estimated 544.9 million people worldwide, with rates of premature mortality highest in regions with less resourced health systems.1 These conditions are often characterised by high symptom burden (cough, excess secretion production and retention, and breathlessness).2 Where excess secretions are a feature, airway clearance interventions including education, individually tailored breathing exercises and secretion clearance strategies are indicated and recommended during both stable disease states and periods of exacerbation.3,4
Health services worldwide have historically integrated physiotherapy-led airway clearance services (ACSs) into hospital-based ambulatory services; operated as an adjunct to existing broader services such as respiratory clinics5 or pulmonary rehabilitation (PR);6,7 or airway clearance has not been available as an outpatient service at all.8,9 During 2019, a review of publicly available websites identified 296 potential Australian ACSs (290 public health services, six private services) with 189 (176 public sites and 13 private providers) confirmed via direct contact as currently providing an ACS in an outpatient/ambulatory setting.6 Little is known about the availability or characteristics of ACSs in private and public settings in Australia or internationally. The aim of this study was to describe Australian clinical models for the provision of ACSs for adults with chronic lung conditions.
Methods
Design
This cross-sectional study collected data via an electronic survey disseminated to Australian ACS providers. Australian ACS was defined as any service provided by a publicly funded Australian health network (or associated department) or private practice that offered to provide airway clearance techniques in a non-acute setting to improve the health of people with chronic lung disease, either as a specific service or as a component of a service.
Ethical approval was provided by the Southern Adelaide Clinical Human Research Ethics Committee (Approval No. 10.19) and the University of South Australia HREC (Approval No. 201308). Governance approval for each public health site was sought in accordance with local research governance processes.
Survey development and pilot testing
In the absence of a pre-existing survey instrument appropriate for describing ACSs, a purpose-designed survey was developed informed by instruments used to evaluate national and international PR programs10–12 and national management of bronchiectasis/COPD.13 Items from these questionnaires were reviewed and grouped into four domains; health care context, referral demographics, service provision and program metrics. Where required, questionnaire items were modified or created to enable appropriateness for ACSs. The preliminary draft survey and dissemination process was piloted with three experienced Australian respiratory physiotherapy clinicians to assess suitability of questions (wording, instances of ambiguity or errors of logic) and response options, completion times and functionality of the dissemination platform (Survey Monkey). Pilot testing resulted in minor adjustments to survey questions and functionality.
As part of the “Demographic” questions, responders self-designated their service location (inner city, metropolitan, regional, rural or remote, Supplemental Appendix 1). In addition to the ‘Demographic’ section, the final survey instrument (61 questions) consisted of four domains; health care context, referral pathways, service provision and program metrics (Supplemental Appendix 1). Survey response options were a combination of single/multiple choice answers and free text.
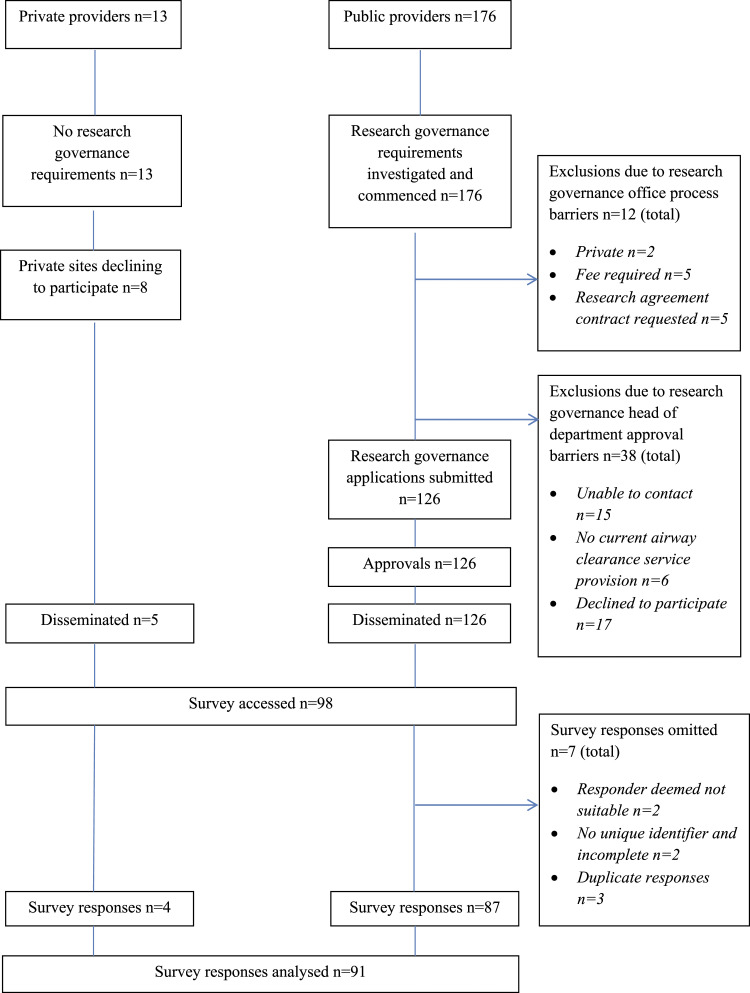
Sampling frame
The sample comprised 189 (176 public health services; 13 private providers) potential participants identified by a scoping study conducted by the same authors.6 Prior to survey dissemination, potentially eligible services were contacted to nominate a single survey respondent (physiotherapist or registered nurse). Services were eligible for inclusion if they currently provided an ACS to adults with chronic lung conditions (asthma, COPD and bronchiectasis) irrespective of setting (outpatient, community or home-based). Services providing airway clearance specifically to people with cystic fibrosis were excluded as specialised, centre-based health service models operate in Australia for this population.6,14,15 Services were excluded if site-specific research governance requirements such as fee schedules and research agreements were unable to be successfully negotiated. The final sample consisted of 131 participants (126 public health sites, 5 private providers) (Figure 1).
Figure 1.
Sampling frame - research governance processes, approvals, survey dissemination and analysis.
Survey dissemination and data collection
The survey was disseminated (via Survey Monkey platform) to the nominated participant via email with an embedded survey link and unique site identifier code. The unique site identifier was used to calculate response rates and allowed reminder emails to be sent (at two weeks and 48 h before survey close). The survey was open to each participant for 1 month (Survey available between October 31 and December 26, 2019).
Data were exported from the electronic platform after survey closure, imported to spreadsheet (Microsoft Excel Workbook 2010) and securely stored.
Data analysis
Response rate was calculated (number of surveys submitted on platform as a percentage of the total number of surveys disseminated). Geographic location of responders versus non-responders was compared (chi square test). Survey response data were reviewed for completeness. Where respondents did not complete the administrative questions (consent and individual responder code), and/or did not enter data beyond the administrative questions, surveys were excluded from analysis. Descriptive statistics (frequencies, percentages calculated as proportion of all included survey responses, missing responses reported as an additional category), were used to summarise survey item responses. Provider type and self-reported service location categories of participants were grouped according to responses (private; public metropolitan (“inner city” and “metropolitan”); and public non-metropolitan (“regional”, “rural” and “remote”)). Non-responders were identified by their postcode and the Australian Standard Geographical Classification 201616 was used to allocate location categories (defined by the distance to travel by road to a location). Characteristics of public metropolitan and public non-metropolitan ACSs were compared for differences (chi-square test, significance level p < .05, SPSS Version 25). Free text responses within each domain were grouped into themes where appropriate.
Results
Survey dissemination and response
Figure 1 summarises the flow of respondents. The survey was disseminated to 131 recipients (public health sites n = 126; private services n = 5). A total of 91 unique surveys were available for analysis (response rate 69%). All Australian States and Territories were represented within the study. Data reflected private healthcare providers (n = 4/91, 4.4%, all in metropolitan areas), public metropolitan (n = 34/91, 37.4% including inner city, metropolitan locations including a single not for profit organisation) and non-metropolitan (n = 53/91, 58.2% including regional (n = 20), rural (n = 31) and remote (n = 2) locations) (Table 1). Given the small number of private providers, differences between geographic locations (metropolitan vs non-metropolitan) were explored only for public health providers. All non-responders were from public sites with 8/40 (20%) from metropolitan versus 32/40 (80%) from non-metropolitan locations, indicating a difference in likelihood of responding based on location (greater likelihood in metropolitan location, χ2 = 5.774, p < .016).
Table 1.
Survey responses regarding health care context of airway clearance services (ACSs), n (%).
| All data (n = 91) | Private (n = 4) | Public - metropolitan (n = 34) | Public - non-metropolitan (n = 53) | p value | |
|---|---|---|---|---|---|
| Organisation providing ACS, | |||||
| Public health service | 86 (95) | 0 (0) | 33 (97) | 53 (100) | |
| Private healthcare | 4 (4) | 4 (100) | 0 (0) | 0 (0) | |
| Not for profit organisation | 1 (1) | 0 (0) | 1 (3) | 0 (0) | |
| Location of the ACS | |||||
| Inner city | 6 (7) | 0 (0) | 6 (18) | 0 (0) | |
| Metropolitan | 32 (35) | 4 (100) | 28 (82) | 0 (0) | |
| Regional | 20 (22) | 0 (0) | 0 (0) | 20 (38) | |
| Rural | 31 (34) | 0 (0) | 0 (0) | 31 (58) | |
| Remote | 2 (2) | 0 (0) | 0 (0) | 2 (4) | |
| ACS venues | |||||
| Public hospital | 67 (74) | 0 (0) | 25 (74) | 42 (79) | |
| Private hospital | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
| Community clinic | 15 (16) | 0 (0) | 6 (18) | 9 (17) | |
| Primary care setting | 11 (12) | 0 (0) | 2 (6) | 9 (17) | |
| Clients home | 29 (32) | 2 (50) | 12 (35) | 15 (28) | |
| Outpatient setting | 22 (24) | 3 (75) | 7 (21) | 12 (23) | |
| Othera | 10 (11) | 2 (50) | 2 (6) | 6 (11) | |
| State or territory the ACS operates from | |||||
| Queensland | 16 (18) | 1 (25) | 6 (18) | 9 (17) | |
| New South Wales | 43 (47) | 1 (25) | 15 (44) | 27 (51) | |
| Victoria | 13 (14) | 1 (25) | 3 (9) | 9 (17) | |
| Australian Capital Territory | 1 (1) | 0 (0) | 1 (3) | 0 (0) | |
| South Australia | 8 (9) | 1 (25) | 4 (12) | 3 (6) | |
| Tasmania | 4 (4) | 0 (0) | 1 (3) | 3 (6) | |
| Western Australia | 5 (5) | 0 (0) | 4 (12) | 1 (2) | |
| Northern Territory | 1 (1) | 0 (0) | 0 (0) | 1 (2) | |
| Number of ACS sites (primary & outreach) | |||||
| 1 | 53 (58) | 2 (50) | 23 (68) | 28 (53) | |
| 2 | 18 (20) | 0 (0) | 7 (21) | 11 (21) | |
| 3 | 10 (11) | 2 (50) | 2 (6) | 6 (11) | |
| 4 | 4 (4) | 0 (0) | 1 (3) | 3 (6) | |
| 5 or more | 6 (7) | 0 (0) | 1 (3) | 5 (9) | |
| ACS delivery (primary site) | |||||
| 1:1 face to face | 90 (99) | 4 (100) | 34 (100) | 52 (98) | |
| Group based | 33 (36) | 1 (25) | 10 (29) | 22 (42) | |
| Phone consultation | 20 (22) | 1 (25) | 15 (44) | 4 (8) | .000 |
| Tele-health | 8 (9) | 1 (25) | 6 (18) | 1 (2) | .008 |
| Otherb | 3 (3) | 1 (25) | 1 (3) | 1 (2) | |
| ACS delivery (outreach site) | |||||
| N/A | 61 (67) | 4 (100) | 25 (74) | 32 (60) | |
| 1:1 face to face delivery | 30 (33) | 0 (0) | 9 (26) | 21 (40) | |
| Group based delivery | 9 (10) | 0 (0) | 2 (6) | 7 (13) | |
| Phone consultation | 5 (5) | 0 (0) | 4 (12) | 1 (2) | |
| Tele-health delivery | 3 (3) | 0 (0) | 1 (3) | 2 (4) | |
ACS: airway clearance service. For p values <.05 the values were in bold
a‘Inpatient hospital’, ‘hospital admission risk Program’
b‘Telehealth’.
Demographic data
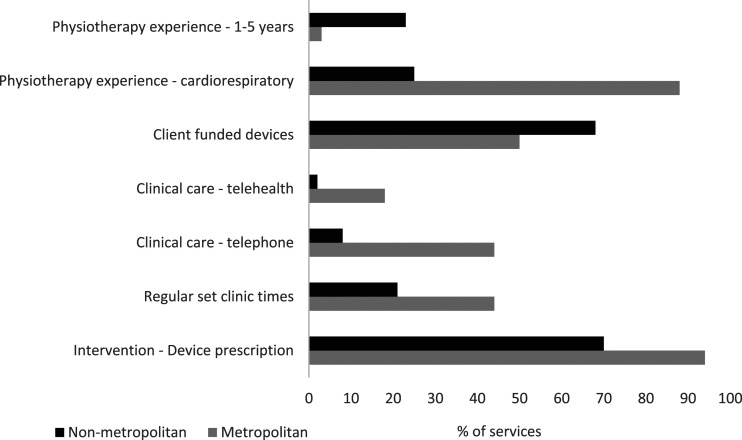
Ninety-nine percent of survey respondents identified as being physiotherapists (n = 1 registered nurse) with almost half (43/91, 47%) having worked in the field of respiratory physiotherapy for more than 6 years and in their profession for over 15 years. A greater proportion (n = 12/53, 23%) of non-metropolitan respondents had only 1–5 years of profession specific employment compared to metropolitan respondents (n = 1/34 (3%), χ2 = 6.3, p = .012, Figure 2).
Figure 2.
Significant differences between metropolitan and non-metropolitan provision of airway clearance services in Australia (chi square tests, p < .05).
Health care context
Most public sites provided ACSs from a public hospital, with service provision from primary care, community clinics, client’s homes and outpatient settings comparable between metropolitan and non-metropolitan locations (Table 1). Few ACSs were provided in community clinics (15/91, 16%) or primary care settings (11/91, 12%). Just over half of the ACSs were provided at a single site (Overall 58%; metropolitan 68%; non-metropolitan 53%), with approximately half (47%) of non-metropolitan ACSs providing a service across two or more sites (Table 1). A quarter of ACSs offered an outreach service to other locations.
In both airway clearance specific and outreach sites, individual, face-to-face consultations were the most common method of ACS delivery available, followed by group-based, phone and telehealth approaches. In metropolitan locations ACSs were delivered by telephone (n = 15/34 (44%) versus n = 4/53 (8%), χ2 = 16.2, p < .001) and telehealth (n = 6/34 (18%) versus n = 1/53 (2%), χ2 = 7.0, p = .008) more frequently than in non-metropolitan locations (Figure 2).
Eligibility and referral processes
Most ACSs (>70%) accepted and received referrals from private and public physicians, GPs, nursing staff and allied health with fewer (<40%) accepting and receiving referrals from respiratory scientists or home oxygen teams (Table 1 – supplementary data). The most common source of referrals differed by geographic location (χ2 = 27.3, p < .001); 76% (n = 26/34) of metropolitan sites indicated referral from public physicians versus 40% (n = 21/53) of non-metropolitan sites from GPs. Both metropolitan (32%) and non-metropolitan (42%) sites accepted referrals directly from clients (Table 1 – Supplementary Data).
Referrals were made on a needs basis, with only small numbers of sites also accepting blanket (standard referral for all people with a particular diagnosis) referrals. Metropolitan sites indicated that blanket referrals were only received for people with a diagnosis of bronchiectasis.
Referral numbers of greater than 120 clients in 2018 were more common in metropolitan versus non-metropolitan locations (n = 12/34 (35%) versus n = 5/53 (9%), χ2 = 25.3, p < .001). Overall, bronchiectasis was considered the most eligible condition for airway clearance (86/91, 95%) with the most common condition referred to ACSs differing between metropolitan (bronchiectasis n = 18/34, 53%) and non-metropolitan locations (COPD n = 36/53 (68%), χ2 = 6.3, p = .043, Table 2).
Table 2.
Survey responses regarding eligibility and referral processes for airway clearance services (ACSs), n (%).
| All data (N = 91) | Private (N = 4) | Public – Metropolitan (N = 34) | Public – Non metropolitan (N = 53) | p value | |
|---|---|---|---|---|---|
| Inclusion criteria for ACSsa | 55 (60) | 3 (75) | 25 (74) | 29 (55) | |
| Exclusion criteria for ACSsb | 42 (46) | 3 (75) | 19 (56) | 20 (38) | |
| Conditions eligible for ACSs | |||||
| Bronchiectasis | 86 (95) | 4 (100) | 33 (97) | 49 (92) | |
| COPD | 85 (93) | 4 (100) | 32 (94) | 49 (92) | |
| Interstitial lung disease | 79 (87) | 4 (100) | 31 (91) | 44 (83) | |
| Lung cancer | 73 (80) | 4 (100) | 29 (85) | 40 (75) | |
| Asthma | 72 (79) | 4 (100) | 29 (85) | 39 (74) | |
| Otherc | 17 (19) | 2 (50) | 11 (32) | 4 (8) | |
| Missing | 4 (4) | 0 (0) | 1 (3) | 3 (6) | |
| 2018 ACS referralsd | |||||
| <30 | 37 (40) | 0 (0) | 7 (21) | 30 (57) | |
| 31–60 | 17 (19) | 0 (0) | 5 (15) | 12 (23) | |
| 61–90 | 6 (7) | 1 (25) | 2 (6) | 3 (6) | |
| 91–120 | 9 (10) | 2 (50) | 7 (21) | 0 (0) | |
| 121+ | 18 (20) | 1 (25) | 12 (35) | 5 (9) | <.0001 |
| Missing | 4 (4) | 0 (0) | 1 (3) | 3 (6) | |
| Conditions frequently referred | |||||
| COPD | 51 (56) | 0 (0) | 15 (44) | 36 (68) | .043 |
| Bronchiectasis | 36 (40) | 4 (100) | 18 (53) | 14 (26) | |
| Missing | 4 (4) | 0 (0) | 1 (3) | 3 (6) | |
| ACS referral mode | |||||
| Paper form | 65 (71) | 2 (50) | 25 (74) | 38 (72) | |
| Fax | 58 (64) | 3 (75) | 24 (71) | 31 (58) | |
| 54 (59) | 3 (75) | 26 (76) | 25 (47) | ||
| Electronic database | 30 (33) | 1 (25) | 14 (41) | 15 (28) | |
| Phone | 29 (32) | 4 (100) | 10 (29) | 15 (28) | |
| Othere | 11 (12) | 1 (25) | 6 (18) | 4 (8) | |
| Missing | 4 (4) | 0 (0) | 1 (3) | 3 (6) | |
| Triage ACS referrals (urgency) | |||||
| Yes | 63 (69) | 1 (25) | 27 (74) | 37 (70) | |
| No | 24 (26) | 3 (75) | 8 (24) | 13 (25) | |
| Missing | 4 (4) | 0 (0) | 0 (0) | 3 (6) | |
| Describe categories of urgencyf | 55 (60) | 1 (25) | 22 (65) | 32 (60) | |
ACS: airway clearance service; COPD: Chronic obstructive pulmonary disease for p values <0.05 the values were in bold
a’diagnosed lung condition’, ‘catchment area’, ‘>18 years of age’, ‘association with PR program’.
b‘NDIS’, ‘DVA’, ‘cognitive impairment’, ‘absence of confirmed lung diagnosis’, ‘co-morbid conditions’.
c’neurological conditions’, ‘breathing dysfunction’, ‘cystic fibrosis’, ‘pulmonary hypertension’, ‘awaiting lung transplant’.
dresponse categories based on clinical experience of local ACS provision’.
eonline referral system’, ‘verbal referral’, ‘face to face’.
f’categories of urgency (30 day, 90 day, 1 year)’, ‘acuity’, ‘health care utilisation’.
Triage criteria were used by more than two thirds of ACSs to prioritise referrals. Common triaging tools were the use of a categorical system which considered the acuity/stability of the person referred and taking in to account the frequency of exacerbations and hospitalisations (Table 2).
Service provision
Across all locations, ACSs were primarily provided by physiotherapists (Table 2 - Supplementary data). Nineteen percent of non-metropolitan services reported airway clearance was delivered by a respiratory nurse, compared to six percent of metropolitan respondents (not significantly different by location, chi square χ2 = 2.9, p = .087). Service location indicated differences in whether airway clearance was provided by a “cardiorespiratory” physiotherapist (88% in metropolitan, 25% in non-metropolitan locations) or a “generalist” physiotherapist (9% versus 66%, χ2 = 33.8, p < .001, Figure 2) (Table 2 – Supplementary data).
Clients were more likely to pay for airway clearance sessions in non-metropolitan locations (χ2 = 8.4, p = .015, Figure 2) and to pay for the cost of a device if prescribed (clients funded devices in 36/53, 68% of non-metropolitan vs 17/34, 50% of metropolitan locations, χ2 = 6.2, p = .045). There was a significant difference between the amount of administrative support available for ACSs in metropolitan (n = 20/34, 59%) and non-metropolitan locations (n = 17/53 (32%), χ2 = 6.4, p = .040) (Table 3).
Table 3.
Service provision characteristics of airway clearance services (ACSs), n (%).
| All data (N = 91) | Private (N = 4) | Public –Metropolitan (N = 34) | Public - Non-metropolitan (N = 53) | p Value | |
|---|---|---|---|---|---|
| Average wait time for ACSs | |||||
| <1 week | 22 (24) | 3 (75) | 6 (18) | 13 (25) | |
| 1–3 weeks | 37 (41) | 1 (25) | 14 (41) | 22 (42) | |
| 3–6 weeks | 12 (13) | 0 (0) | 6 (18) | 6 (11) | |
| 6 weeks-3 months | 8 (9) | 0 (0) | 5 (15) | 3 (6) | |
| 3 months + | 1 (1) | 0 (0) | 1 (3) | 0 (0) | |
| N/A | 5 (5) | 0 (0) | 1 (3) | 4 (8) | |
| Missing | 6 (7) | 0 (0) | 1 (3) | 5 (9) | |
| Type of appointments for ACSs | |||||
| Ad hoc appointments | 68 (75) | 1 (25) | 27 (79) | 40 (75) | .020 |
| Regular set clinic times | 30 (33) | 4 (100) | 15 (44) | 11 (21) | |
| Missing | 6 (7) | 0 (0) | 1 (3) | 5 (9) | |
| Airway clearance device funding | |||||
| Client funded | 57 (63) | 4 (100) | 17 (50) | 36 (68) | .045 |
| Program funded | 28 (31) | 0 (0) | 16 (47) | 12 (23) | |
| Other | 19 (21) | 2 (50) | 6 (18) | 11 (21) | |
| Missing | 6 (7) | 0 (0) | 1 (3) | 5 (9) | |
| Average number of 1:1 ACS sessions received | |||||
| 1 visit | 13 (14) | 0 (0) | 6 (18) | 7 (13) | |
| 2–3 visits | 52 (57) | 3 (75) | 20 (59) | 29 (55) | |
| 4–5 visits | 16 (18) | 0 (0) | 6 (18) | 10 (19) | |
| 6–7 visits | 2 (2) | 0 (0) | 1 (3) | 1 (2) | |
| 8+ visits | 2 (2) | 1 (25) | 0 (0) | 1 (2) | |
| Missing | 6 (7) | 0 (0) | 1 (3) | 5 (9) | |
| Format of ACSs | |||||
| Breathing techniques | 85 (93) | 4 (100) | 33 (97) | 48 (91) | |
| Education | 85 (93) | 4 (100) | 33 (97) | 48 (91) | |
| Exercise prescription | 77 (85) | 4 (100) | 30 (88) | 43 (81) | |
| Device prescription | 73 (80) | 4 (100) | 32 (94) | 37 (70) | .006 |
| Manual techniques | 41 (45) | 3 (75) | 15 (44) | 23 (43) | |
| Missing | 6 (7) | 0 (0) | 1 (3) | 5 (9) | |
| Hours of administrative support for ACSs weekly | |||||
| 0 h | 48 (53) | 2 (0) | 13 (38) | 33 (62) | |
| 1–5 h | 20 (22) | 0 (0) | 9 (26) | 11 (21) | |
| 6–15 h | 2 (2) | 0 (0) | 1 (3) | 1 (2) | |
| 16–25 h | 2 (2) | 0 (0) | 2 (6) | 0 (0) | |
| 26–38 h | 13 (14) | 2 (50) | 8 (24) | 3 (6) | |
| Missing | 6 (7) | 0 (0) | 1 (3) | 5 (9) | |
ACS: airway clearance service. For p values <0.05 the values were in bold
Eighty-five respondents estimated the number of clinical hours that were spent on providing airway clearance intervention at their site each week in 2018 (median = 4 h, interquartile range = 9 h, range = 0–500 h). Fifty (59%) sites reported 5 h or less each week, 11 (13%) sites 6–10 h, 7 (8%) sites 11–20 h, 3 (4%) sites 21–30 h, 1 (1%) site 31–40 h and 7 (8%) sites reported more than 41 h per week.
Seventy-five percent of all respondents reported a wait time for ACSs, with 1–3 weeks the most common range selected. Appointments to ACSs were largely ad hoc in nature with more metropolitan sites (n = 15/34, 44%) having regular set clinic times than non-metropolitan sites (n = 11/53 (21%), χ2 = 5.4, p = .020, Figure 2). Most ACSs across all locations allocated 60 min for an initial assessment and 30 min for a review with more metropolitan sites having 45 and 60 min review appointments than non-metropolitan sites. Clients typically received 2–3 airway clearance sessions in total (52/91, 57%) and routine follow up at regular intervals was not provided (74/91, 81%).
Nearly all sites provided interventions of breathing techniques, education and exercise prescription, with fewer performing manual techniques. Airway clearance devices were prescribed in metropolitan settings (n = 32/34,94%) more often than in non-metropolitan settings (n = 37/53 (70%), χ2 = 7.5, p = .006). Free text comments indicated that devices were occasionally subsidised for health care card holders and those with private health funds. Metropolitan sites had access to a wider range of airway clearance devices than non-metropolitan sites. The three most accessible devices were Bottle PEP, Flutter® and Acapella Choice® (Green).
In the event of a client being medically unstable, access to additional staff was greater in metropolitan than non-metropolitan areas: respiratory physicians (85% of respondents versus 40%, χ2 = 17.7, p < .001), respiratory nurses (74% versus 45%, χ2 = 6.7, p = .010) and medical emergency teams (62% versus 25%, χ2 = 12.1, p = .001).
Program metrics
Chronic condition self-management (81/91, 89%), management of acute exacerbations (60/91, 66%) and hospital avoidance (50/91, 55%) were the key service focus areas reported (Table 3 - Supplementary data). Most services regularly used outcome measures (85/91, 93%), with a large proportion measuring outcomes before and after intervention (64/91, 70%). Functional capacity outcomes such as the 6 Minute Walk Test (65/91, 71%) and measures of health status such as the COPD Assessment Tool (34/91, 37%) and the St George’s Respiratory Questionnaire (30/91, 33%) were most common (Table 4). Around two thirds of ACSs (59/91, 65%) reported they did not record health care utilisation data. Methods for providing feedback to ACSs were widely available (79/91, 87%) with the most common being written (62/91, 68%) and verbal (49/91, 54%). Greater than two thirds of all ACSs (62/91, 68%) routinely correspond with referrers with over 50% of public providers and 75% of private providers communicating with the GP on a regular basis.
Table 4.
Program metrics of airway clearance services (ACSs), n (%).
| All data (N = 91) | Private (N = 4) | Public -Metropolitan (N = 34) | Public - Non-Metropolitan (N = 53) | |
|---|---|---|---|---|
| Focus of ACSs | ||||
| Chronic condition self-management | 81 (89) | 4 (100) | 32 (94) | 45 (85) |
| Management of acute exacerbation | 60 (66) | 2 (50) | 23 (68) | 35 (66) |
| Hospital avoidance | 50 (55) | 2 (50) | 20 (59) | 28 (53) |
| Reducing length of stay of clients | 36 (40) | 1 (25) | 12 (35) | 23 (43) |
| Blank | 6 (7) | 0 (0) | 1 (3) | 5 (9) |
| Measures of health care utilisation recorded | ||||
| No measures recorded | 59 (65) | 3 (75) | 21 (62) | 35 (66) |
| Number of hospital admissions | 25 (27) | 1 (25) | 12 (35) | 12 (23) |
| Number of hospital presentations | 21 (23) | 0 (0) | 10 (29) | 11 (21) |
| Duration of hospital admission (i.e. LOS) | 13 (14) | 1 (25) | 7 (21) | 5 (9) |
| Number of GP visits | 3 (3)3 (3) | 0 (0)0 (0) | 2 (6)2 (6) | 1 (2) |
| Number of resp physician appointments | 6 (7) | 0 (0) | 1 (3) | 5 (9) |
| Blank | ||||
| Measures of functional capacity used in ACSs | ||||
| Six minute walk test | 65 (71) | 3 (75) | 22 (65) | 40 (75) |
| No measures of functional capacity used | 20 (22) | 1 (25) | 11 (32) | 8 (15) |
| Othera | 18 (20) | 3 (75) | 8 (24) | 7 (13) |
| 4 meter gait speed | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Blank | 6 (7) | 0 (0) | 1 (3) | 5 (9) |
| Measures of health status used in ACSs | ||||
| COPD assessment tool (CAT) | 34 (37) | 1 (25) | 16 (47) | 17 (32) |
| St Georges respiratory questionnaire (SGRQ) | 30 (33) | 0 (0) | 10 (29) | 20 (38) |
| No measures of health status used | 28 (31) | 3 (75) | 11 (32) | 14 (26) |
| Otherb | 17 (19) | 0 (0) | 7 (21) | 10 (19) |
| Chronic respiratory questionnaire (CRQ) | 13 (14) | 0 (0) | 7 (21) | 6 (11) |
| 36-Item short form health survey (SF-36) | 6 (7) | 0 (0) | 2 (6) | 4 (8) |
| The quality of life questionnaire – bronchiectasis (QOL-B) | 3 (3) | 0 (0) | 1 (3) | 2 (4) |
| 12-Item short form health survey (SF-12) | 2 (2) | 0 (0) | 0 (0) | 2 (4) |
| Blank | 6 (7) | 0 (0) | 1 (3) | 5 (9) |
ACS: airway clearance service; LOS: length of stay; resp: respiratory
a‘step tests’, ‘timed up and go’, ‘10 metre walk test’, ‘spirometry’
b‘Hospital Anxiety and Depression Scale’, ‘Leicester cough questionnaire’, ‘Depression Anxiety Stress Scale’, ‘BODE index’
More than half of the metropolitan (21/34, 62%) and non-metropolitan (29/53, 55%) services stated the airway clearance needs of their region were not being met. Eighteen (20% of total respondents) metropolitan sites and 28 (31% of total respondents) non-metropolitan sites provided free text responses to support this response. The most frequent reasons in metropolitan locations were having limited resources (including devices) and inability to follow patients up as often as required. In non-metropolitan locations the main limiting factors were only being able to operate an ad-hoc service and having limited staffing (Table 4: Supplementary data).
Discussion
This Australia-wide survey, with overall response rate of 69% (and 53 of the 91 responses [58%] from non-metropolitan areas), comprehensively described ACSs for adults with chronic lung conditions prior to the COVID-19 global pandemic. A typical ACS in Australia operated from a public hospital setting, was ad hoc in nature, and provided airway clearance intervention for chronic condition self-management. In general, clients waited between one and 3 weeks for an appointment, were seen two to three times, and in most cases, there was no cost to the person for the service. It is unclear whether these service characteristics are unique to Australia, given country specific differences in health care systems and funding arrangements. We were unable to identify other published descriptive reports of ACS delivery models (outside of specialised CF care services) for direct comparison. However, differences identified in this study between urban and rural ACSs are likely to be relevant to populations outside Australia. Our findings align with internationally recognised disparities in access to health care amongst people with chronic respiratory disease based on their place of residence, amongst other (often concurrent) social determinants of health.17–21 Australia has a high rate of urbanisation with 72% of the population living in major cities/metropolitan areas22 served by city-based clustering of hospitals and health professionals.23 This is comparable with median urbanisation levels across countries of Europe and Northern America (74% in 2018) and well above those in China (59%) and India (34%).24
The key areas of unmet need described by survey respondents were not having a dedicated service for airway clearance; lack of funding for sufficient staffing and resources; inadequate access to airway clearance devices and being unable to follow clients up at regular intervals to manage their condition longer term. In non-metropolitan regions, absence of experienced clinicians and the large distances clients had to travel to access services further compounded the issue of unmet need and aligned with geographical challenges to rural and remote health.22 Survey respondents in metropolitan regions had considerable clinical experience which was indicative of a specialised workforce. The lack of such experience in non-metropolitan regions may be consistent with a high workforce turnover, exacerbating issues with staff recruitment and retention in rural Australia.25
Current national and international guidelines suggest that personalised airway clearance techniques should be prescribed, reviewed and the outcomes measured regularly by a respiratory physiotherapist for people with bronchiectasis26–29and COPD30,31 who experience chronic sputum production and/or retention. Our findings indicate that while ACS provision is available it may not always meet current clinical recommendations. Potential ACS providers and funders could be encouraged to broaden the scope and reach of the clinical workforce. Expanding modes of service delivery, retaining and learning from the COVID-19 related escalation in telehealth delivery,23 and prioritising funding models that incorporate the provision of devices and a base from which to deliver the care are indicated.
At the time of this survey few ACSs in Australia used telehealth consultations despite the role of these strategies in detecting acute exacerbations and reducing hospital admission rates in people with severe COPD.32 The distance between clients and non-metropolitan sites providing airway clearance intervention was reported as a limitation to accessibility of service provision. The delivery of conventional healthcare, including airway clearance therapy, has since been impacted by COVID-19 health directives, with alternate modes such as telemedicine used to reduce the risk of viral transmission.33,34 In the United Kingdom outpatient virtual airway clearance physiotherapy is feasible35 and deemed an appropriate (by clinicians)36 and preferred (by patients)37 mode of service delivery. While short-term effectiveness of home-based PR has been demonstrated,38 effectiveness outcomes of remotely delivered ACSs remain unknown. Exploring changes to ACS provision instigated and subsequently retained by the surveyed providers as a result of the COVID-19 pandemic in Australia is indicated.
Few ACSs operated from community or primary care settings, despite evidence that implementation of chronic care model principles such as health promotion and health education are positively related to the comprehensive management of chronic conditions in primary care.39 Given the amount of time required for airway clearance assessments and reviews, as well as the need for access to a multidisciplinary team, services should consider that suitable locations to provide detailed and holistic care to people with chronic lung conditions may be away from the traditional hospital outpatient setting.
Using the sampling frame from a systematic scoping review of Australian ACSs ensured that invitations to participate reached existing and potential service providers.6 The process of obtaining site specific governance approval, and in particular liaising directly with potential participants, was one of the strengths of this study that contributed to the response rate and quality of responses received. The most comparable surveys have response rates of 85%13 and 72%,40 however, survey response rates of 70% or higher are considered good and well above the average medical practitioner response rate of less than 30%.41 Local governance processes at a small number of public health networks prevented some sites from participating and this limitation may have affected the representation of public ACSs. Geographic location was related to the likelihood of participating in the survey, with information about non-metropolitan ACSs still lacking.
In conclusion, components of ACSs explored in this survey (client conditions and prioritisation; intervention aims, strategies, devices and outcome measures) were similar across all regions in Australia, but there were differences in the way services were provided that may disadvantage those in non-metropolitan areas. This survey identified that non-metropolitan-based ACSs in Australia had limited access to experienced clinicians, inadequate administrative support, a lack of dedicated airway clearance clinics offering lower rates of device prescription at higher costs to clients. Services could be developed further with dedicated funding, resources and staff and these aspects should be a focus for ongoing service improvement to meet the airway clearance needs of adults with chronic lung conditions in the future.
Supplemental Material
Supplemental material for Australian airway clearance services for adults with chronic lung conditions: A national survey by Laura Cooper, Kylie Johnston and Marie Williams in Chronic Respiratory Disease
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: LC is supported by an Australian Government Research Training Program (RTP) Fee Scholarship (fee waiver). The funding body played no role in the design of the study; collection, analysis, and interpretation of data, nor in writing the manuscript.
Supplemental material: Supplemental material for this article is available online.
ORCID iD
Laura Cooper https://orcid.org/0000-0002-4199-9493
References
- 1.Soriano PJK, Paulson KR, Gupta V, et al. Prevalence and attributable health burden of chronic respiratory diseases, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet Respir Med 2020; 8: 585–596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pauwels RA, Rabe KF. Burden and clinical features of chronic obstructive pulmonary disease (COPD). Lancet 2004; 364: 613–620. [DOI] [PubMed] [Google Scholar]
- 3.Osadnik CR, McDonald CF, Jones AP, et al. Airway clearance techniques for chronic obstructive pulmonary disease. Cochrane Database Syst. Rev 2012; 3(3): Cd008328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee AL, Burge AT, Holland AE. Airway clearance techniques for bronchiectasis. Cochrane Database Syst. Rev 2015; 2015: Cd008351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McDonald VM, Harrington J, Clark VL, et al. Multidisciplinary care in chronic airway diseases: the newcastle model. ERJ Open Res 2022; 8(3): 0215–2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cooper L, Johnston K, Williams M. Airway clearance services (ACSs) in Australia for adults with chronic lung conditions: scoping review of publicly available web-based information. BMC Health Serv. Res 2019; 19: 808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schoovaerts K, Lorent N, Goeminne P, et al. National survey on the management of adult bronchiectasis in Belgium. COPD 2019; 16: 72–74. [DOI] [PubMed] [Google Scholar]
- 8.Dhar R, Singh S, Talwar D, et al. Bronchiectasis in India: results from the European multicentre bronchiectasis audit and research collaboration (EMBARC) and respiratory research network of india registry. Lancet Glob Health 2019; 7: e1269–e1279. [DOI] [PubMed] [Google Scholar]
- 9.Rees M, Liu B, Pascoe A, et al. Improving care for people with bronchiectasis: opportunities and challenges highlighted from service evaluation. Intern Med J 2022. Online ahead of print. DOI: 10.1111/imj.15730 [DOI] [PubMed] [Google Scholar]
- 10.Bowen JM, Campbell K, Sutherland S, et al. Pulmonary rehabilitation in Ontario: a cross-sectional survey. Ontario Health Technol. Assess. Ser 2015; 15: 1–67. [PMC free article] [PubMed] [Google Scholar]
- 11.Lung Foundation of Australia . Lung foundation Australia 2015 pulmonary rehabilitation survey, 2015, www.lungfoundation.com.au/resources (accessed 18 February 2018).
- 12.Steiner M, Holzhauer-Barrie J, Lowe D, et al. Pulmonary rehabilitation: time to breathe better. National chronic obstructive pulmonary disease (COPD) audit programme: resources and organisation of pulmonary rehabilitation services in england and wales 2015. UK London, 2015. [Google Scholar]
- 13.Lee A, Button B, Denehy L. Current Australian and New Zealand physiotherapy practice in the management of patients with bronchiectasis and chronic obstructive pulmonary disease. New Zealand Journal of Physiotherapy 2008; 36: 49–58. [Google Scholar]
- 14.Bell S, Robinson P. Cystic fibrosis standards of care, Australia, 2008, www.thoracic.org.au/journal-publishing/command/download_file/id/20/filename/CF_standardsofcare_Australia_2008.pdf (accessed 10 July 2018).
- 15.Agency for Clinical Innovation Respiratory Network . Cystic fibrosis, 2016, www.aci.health.nsw.gov.au/__data/assets/pdf_file/0003/338124/ACI16125_Cystic_Fibrosis_MoC_F_web.pdf (accessed 10 July 2018).
- 16.Australian Government Department of Health. Australian Standard Geographical Classification - Remoteness Area (ASGC-RA 2006). http://www.doctorconnect.gov.au/internet/otd/publishing.nsf/content/ra-intro (accessed 24 March 2019).
- 17.Gaffney AW, Hawks L, White AC, et al. Health care disparities across the urban-rural divide: a national study of individuals with COPD. J Rural Health 2022; 38: 207–216. [DOI] [PubMed] [Google Scholar]
- 18.Moscovice IS, Case MM, Wu Z. Disparities in geographic access to hospital outpatient pulmonary rehabilitation programs in the United States. Chest 2019; 156: 308–315. [DOI] [PubMed] [Google Scholar]
- 19.Rochester CL, Vogiatzis I, Holland AE, et al. An official American thoracic society policy statement: enhancing implementation, use and delivery of pulmonary rehabilitation. Am J Respir Crit Care Med 2015; 192: 1373–1386. [DOI] [PubMed] [Google Scholar]
- 20.Schraufnagel DE, Blasi F, Kraft M, et al. An official American thoracic socity/European respiratory society policy statement: disparities in respiratory health. Am J Respir Crit Care Med 2013; 188: 865–871. [DOI] [PubMed] [Google Scholar]
- 21.Singh SJ, Halpin DMG, Salvi S, et al. Exercise and pulmonary rehabilitation for people with chronic lung disease in LMICs: challenges and opportunities. Lancet Respir Med 2019; 7: 1002–1004. [DOI] [PubMed] [Google Scholar]
- 22.Australian Institute of Health and Welfare . Rural and remote health, www.aihw.gov.au/reports/rural-remote-australians/rural-and-remote-health (2022 (accessed 6 November 2022).
- 23.Caffery LA, Muurlink OT, Taylor-Robinson AW. Survival of rural telehealth services post-pandemic in Australia: a call to retain the gains in the ‘new normal. Aust J Rural Health 2022; 30: 544–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.United Nations, Department of Economic, Affairs Social, Division Population . World urbanization prospects: the 2018 revision, 2019, https://population.un.org/wup/publications/Files/WUP2018-Report.pdf (accessed 11 November 2022).
- 25.Chisholm M, Russell D, Humphreys J. Measuring rural allied health workforce turnover and retention: what are the patterns. Determinants and Costs? 2011; 19: 81–88. [DOI] [PubMed] [Google Scholar]
- 26.Franks LJ, Walsh JR, Hall K, et al. Measuring airway clearance outcomes in bronchiectasis: a review. Eur Respir Rev 2020; 29: 190161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Visser SK, Bye P, Morgan L. Management of bronchiectasis in adults. Med. J. Aust 2018; 209: 177–183. [DOI] [PubMed] [Google Scholar]
- 28.Polverino E, Goeminne PC, McDonnell MJ, et al. European respiratory society guidelines for the management of adult bronchiectasis. Eur. Respir. J 2017; 50: 1700629. [DOI] [PubMed] [Google Scholar]
- 29.Chang AB, Bell SC, Torzillo PJ, et al. Chronic suppurative lung disease and bronchiectasis in children and adults in Australia and New Zealand thoracic society of Australia and New Zealand guidelines. Med. J. Aust 2015; 202: 21–23. [DOI] [PubMed] [Google Scholar]
- 30.Yang IA, Brown JL, George J, et al. The COPD-X plan: Australian and New Zealand guidelines for the management of chronic obstructive pulmonary disease 2020. Version 2.61. www.copdx.org.au (2020, accessed 3 May 2021).
- 31.Strickland SL, Rubin BK, Drescher GS, et al. AARC clinical practice guideline: effectiveness of nonpharmacologic airway clearance therapies in hospitalized patients. Respir Care 2013; 58: 2187–2193. [DOI] [PubMed] [Google Scholar]
- 32.Holland A. Telehealth reduces hospital admission rates in patients with COPD. J Physiother 2013; 59: 129. [DOI] [PubMed] [Google Scholar]
- 33.Grabowski DC, Joynt Maddox KE. Postacute care preparedness for COVID-19: thinking ahead. Jama 2020; 323: 2007–2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Li J, Xia W, Zhan C, et al. A telerehabilitation programme in post-discharge COVID-19 patients (TERECO): a randomised controlled trial. Thorax 2021; 0: 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Parkin S, Long A, Forys I, et al. A retrospective service evaluation of a virtual respiratory physiotherapy outpatient clinical service. Thorax 2021; 76: A103–A104. [Google Scholar]
- 36.Wu F, Burt J, Chowdhury T, et al. Specialty COPD care during COVID-19: patient and clinician perspectives on remote delivery. BMJ Open Respir. Res 2021; 8: 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McCallion P, Davison J, DeSoyza A, et al. Delivering bronchiectasis physiotherapy clinics remotely: patient perceptions and future preferences. Thorax 2021; 76: A155–A156. [Google Scholar]
- 38.Stafinski T, Nagase FI, Avdagovska M, et al. Effectiveness of home-based pulmonary rehabilitation programs for patients with chronic obstructive pulmonary disease (COPD): systematic review. BMC Health Serv. Res 2022; 22: 557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schmittdiel JA, Shortell SM, Rundall TG, et al. Effect of primary health care orientation on chronic care management. Ann Fam Med 2006; 4: 117–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Van der Lee L, Hill AM, Patman S. A survey of clinicians regarding respiratory physiotherapy intervention for intubated and mechanically ventilated patients with community-acquired pneumonia. What is current practice in Australian ICUs? J Eval Clin Pract 2017; 23: 812–820. [DOI] [PubMed] [Google Scholar]
- 41.Bonevski B, Magin P, Horton G, et al. Response rates in GP surveys – trialling two recruitment strategies. Aust Fam Physician 2011; 40: 427–430. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material for Australian airway clearance services for adults with chronic lung conditions: A national survey by Laura Cooper, Kylie Johnston and Marie Williams in Chronic Respiratory Disease