Summary
Background
Knowledge regarding the modifiable risk factors of dementia is fundamental to guide public health policy. We aimed to estimate the population attributable fraction of modifiable risk factors of dementia among adults from a nationwide epidemiological study.
Methods
We used the public database of the Brazilian Longitudinal Study of Aging (ELSI-Brazil) to calculate the Population Attributable Fraction (PAF) for ten risk factors, including education level, hearing loss, hypertension, alcohol consumption, obesity, active smoking, depression, social isolation, physical inactivity, and diabetes. PAF was estimated for this sample after accounting for the communality of each risk factor.
Findings
The ten preventable risk factors for dementia accounted for 50·5% of the Population Attributable Fraction in Brazil. Hearing loss (14·2%), physical inactivity (11·2%), and hypertension (10·4%) accounted for the highest PAF among all the risk factors. Considerable variation in the relative contribution of the different risk factors was found in different regions.
Interpretation
This study might provide an opportunity to change the impact of dementia in Brazil. By targeting modifiable risk factors of dementia, the health of individuals in Brazil might be considerably improved.
Funding
This study did not receive any funding.
Keywords: Dementia, Modifiable risk factors, Prevention, Public health system, Health providers
Research in context.
Evidence before this study
A systematic review was conducted to retrieve risk factors for dementia in Medline with the following terms: "dementia", “risk factors”, "population attributable”, “Latin America”, “Brazil” from inception until December 7, 2021. Only two references were found and in only one of them the population attributable fraction (PAF) was calculated with Brazilian data. The study performed with the Brazilian data calculated PAF using the National Health Survey (PNAS) of seven modifiable risk factors and found that 32.3% of dementia cases could be related to these factors. The other study was performed in six Latin American countries and analysed nine risk factors for dementia, totalizing a PAF of 55.8% for these risk factors.
Added value of this study
We analysed the Brazilian Longitudinal Study of Aging (ELSI-Brazil) with accurate medical data to estimate the prevalence of ten risk factors for dementia in Brazil and to calculate the percentage of reduction of dementia cases if each risk factor were reduced. Our estimates were higher than that previously found in Brazil, potentially associated with a more accurate methodology and the inclusion of more risk factors.
Implications of all the available evidence
The PAF percentage in Brazil is higher than that estimated worldwide. It indicates the fundamental role of the potentially modifiable risk factors in reducing dementia in developing countries. Hearing loss, physical inactivity and hypertension exhibited the highest PAF percentages among all risk factors. Public health strategies that target these risk factors may have a massive impact on the incidence of dementia within the next decades.
Alt-text: Unlabelled box
Introduction
A large number of cases of dementia are expected within the next few years across the globe.1,2 High-income countries have demonstrated decreasing rates of dementia, probably associated with rigorous control of vascular risk factors in the last decades.3 However, the incidence has rapidly increased in low and middle-income countries (LMIC), which account for almost two-thirds of the global population suffering from dementia.1
Widespread uncontrolled vascular risk factors associated with low education levels synergistically make older people living in LMIC even more vulnerable to cognitive decline.3 Several modifiable risk factors of dementia have been established, some of them important in early-life (poor schooling), midlife (hearing loss, traumatic brain injury, hypertension, alcohol consumption, and obesity), and late-life (smoking, diabetes, depression, social isolation, physical inactivity, and air pollution). Mukadam et al. analyzed nine modifiable risk factors of dementia in LMIC and calculated the Population Attributable Fraction (PAF). For the six Latin American countries analyzed in the study (Brazil not included), the PAF estimated was 55·8%,4 which was higher than the PAF of high-income countries. Brazil is a large upper-middle-income country with a unified healthcare system. However, a significant share of the adult population is still exposed to several risk factors of dementia,5 besides having a low average education level.
Although the adult population of Brazil is large, little is known about the prevalence of risk factors of dementia in this population. A nationwide epidemiological task force was established under the name ELSI-Brazil (Brazilian Longitudinal Study of Aging)6 to conduct a longitudinal study with older adults from Brazil. The data were collected from a nationally representative sample of individuals who were 50 years or older, and ten established potentially reversible risk factors of dementia were included. We aimed to calculate the population attributable fraction of modifiable risk factors of dementia from Brazilian adults by conducting an epidemiological study.
Methods
Study design and sampling
The ELSI-Brazil is an ongoing population-based cohort to study the social and biological determinants of aging. The baseline evaluation was performed in 2015–16 and included individuals who were 50 years or older. All participants signed the informed consent form before enrollment. The study was conducted by the Oswaldo Cruz Foundation (FIOCRUZ), Minas Gerais, Brazil, and was approved by the Ethics Committee of the FIOCRUZ.
The ELSI-Brazil followed a methodology similar to that of other longitudinal aging studies from other parts of the world (i.e., the Health and Retirement family of studies). A complex sampling design was used based on the size of municipalities to include small, medium, and large cities of urban and rural areas. The estimated sample size was 10,000 individuals, at a significance level of 95% and an effective sample design of 1.5. This method allowed an estimated prevalence of 1% with a sample error of 0.25%.
Sample weights were derived to account for differential probability of selection and differential non-response. The research procedure included (1) an interview about general household characteristics and socioeconomic conditions; (2) individual consultation to determine the physical and mental health condition and other relevant aspects; (3) blood pressure measurements, anthropometric measures, and physical functioning assessment; (4) blood collection. Further details regarding the procedure are provided elsewhere.6
Variables collected
Ten of the twelve previously potentially modifiable risk factors of dementia described by Livingston et al.3 were analyzed in this study, which included education level, hearing loss, hypertension, alcohol consumption, obesity, active smoking, depression, social isolation, physical inactivity, and diabetes. Clinical and demographic data were recorded in a clinical interview based on self-reported values. Only body mass index was measured objectively. Skin color was reported according to the self-description of the subjects and comprised Indigenous, Asian, White, Black, and Brown (or Pardo) individuals. Brown or Pardo individuals constitute an ethnic category that represents a wide range of skin colors within the black-white spectrum.7 The variables we used to define these risk factors are presented in Panel 1, and their corresponding questions within the dataset are presented in Supplementary Table 1. For this study, individuals with a previous diagnosis of Alzheimer's disease were excluded. Traumatic brain injury and air pollution, both risk factors of dementia, were not included in the ELSI-Brazil cohort.
Panel 1.
Description and definition of ten risk factors for dementia collected within the ELSI-Brazil cohort and their corresponding codes in the original dataset (See the supplementary material for full codes description).
|
Less education (E22) Self-reported less or equal than 4 years of education (similar to primary education in Brazil). Hearing loss (N16) Self-reported hearing impairment. Hypertension (N28) Self-reported known diagnosis of hypertension given by a physician. Heavy drinking (L25 and L26) Self-reported drinking above 168g of alcohol per week. Obesity (MF22 and MF13) Body mass index measured by the ELSI-Brazil team above 29. Smoking (L30) Self-reported current smoking. Depression (N59) Self-reported previous medical history of major depression. Physical inactivity (L5) Self-reported less than 3 days a week of walking or any physical exercise Social isolation (S2, S5, S8) Self-reported social contact frequency less than once per month with relatives, friends, or outdoor group activities. Diabetes (N35) Self-reported known diagnosis of diabetes given by a physician. |
Statistical analysis
We replicated the methods described by Livingston et al.3 to calculate the Population Attributable Fraction for each of the ten risk factors recorded. Unweighted and weighted PAF estimates were calculated (accounting for communality of each risk factor for this sample), followed by the overall national weighted PAF for all ten risk factors. Calculating PAF required the relative risk of dementia-associated risk factors and the prevalence of the same risk factor for the studied population. The prevalence of each risk factor was calculated based on complex survey analysis, and a 95% confidence interval was also generated. The meta-analytic relative risk for each risk factor was estimated in the previous studies.8 Communality was also estimated to avoid misinterpretation of our results by performing Principal Component Analysis, considering the sampling weights and the tetrachoric correlation. The formula we used to calculate the weighted PAF are described in Supplementary Panel 1. Further information on the technique used can be found in the study by Mukadami et al.2. All analyses were performed using the built-in functions and the packages survey and psych of the R software (V4.1.0).
Role of the funding source
This study did not have a funding source.
Results
The ELSI-Brazil study included 9412 individuals between 50 and 105 years. We excluded 157 individuals from the study who were previously diagnosed with dementia. A total of 9255 (56.6% females) individuals were included in this analysis, with an average of 63·4 (SD 10·1) years of age and 5·4 (SD 4·3) years of education. There were 2413 (26·9%) individuals who could not write or read a note, which was a proxy for illiteracy. Brown individuals (“Pardo” in Portuguese) comprised the largest proportion of individuals included (4,213, 45·5%), followed by white (3,529, 38·1%), Black (878, 9·5%), Indigenous (217, 2·3%), and Asian (90, 1%) individuals. Region-wise demographic characteristics are presented in Table 1.
Table 1.
Regional prevalence of demographic characteristics in the ELSI-Brazil cohort.
| North (n = 743) | Northeast (n = 2,549) | Southeast (n = 3,922) | South (n = 1,278) | Midwest (n = 920) | P-value | |
|---|---|---|---|---|---|---|
| Sex (M) | 370 (49.8%) | 1,122 (44.0%) | 1,660 (42.3%) | 535 (41.9%) | 411 (44.7%) | 0.003 |
| Age (years) | 62.9 (±10.1) | 64.1 (±10.5) | 63.5 (±10.1) | 63.2 (±9.6) | 63.5 (±10.0) | 0.42 |
| Education (years) | 4.9 (±4.3) | 4.3 (±4.3) | 5.9 (±4.2) | 5.9 (±4.0) | 5.2 (±4.2) | < 0.0001 |
| Illiterate | 221 (31.1%) | 1,051 (43.5%) | 755 (19.8%) | 173 (14.0%) | 253 (28.2%) | < 0.0001 |
| Family income | 3.8 (±2.5) | 3.8 (±2.6) | 5.1 (±3.5) | 5.1 (±3.3) | 4.9 (±3.4) | < 0.0001 |
| Race | < 0.0001 | |||||
| White | 113 (15.2%) | 554 (21.7%) | 1,702 (43.4%) | 918 (71.8%) | 303 (32.9%) | |
| Black | 51 (6.9%) | 321 (12.6%) | 384 (9.8%) | 44 (3.4%) | 87 (9.5%) | |
| Brown | 482 (64.9%) | 1,548 (60.7%) | 1,492 (38.0%) | 274 (21.4%) | 487 (52.9%) | |
| Asian | 7 (0.9%) | 27 (1.1%) | 39 (1.0%) | 7 (0.5%) | 10 (1.1%) | |
| Indigenous | 87 (11.7%) | 31 (1.2%) | 79 (2.0%) | 6 (0.5%) | 17 (1.8%) | |
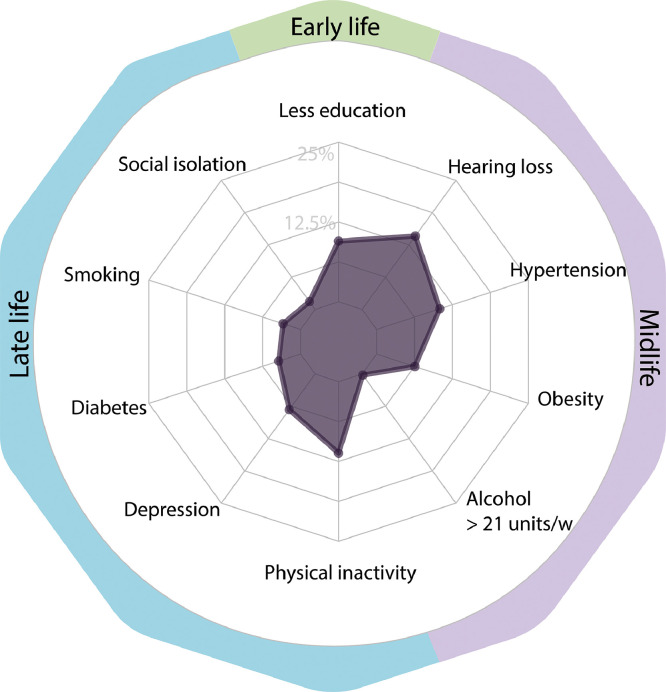
The total weighted Population Attributable Fraction for the ten risk factors of dementia analyzed in Brazil was 50·5%. The highest PAF corrected for communality was hearing loss (14·2%), followed by physical inactivity (11·2%), hypertension (10·4%), and low education level (9·5%) (Figure 1). Importantly, the use of hearing aid was very limited across the nation (165, 1·7%). Table 2 presents all modifiable risk factors of dementia and their respective weighted PAF.
Figure 1.
The Population Attributable Fraction for potentially modifiable risk factors of dementia in Brazil.
Table 2.
Risk factors prevalence and their calculated weighted PAF.
| RR for dementia | Overall prevalence calculated | CI 95% | Communality | PAF | Weighted PAF | |
|---|---|---|---|---|---|---|
| Less education | 1.6 (1.3–2) | 51.1% | 47.7–55 | 59.3% | 23.5% | 9.5% |
| Hearing loss | 1.9 (1.4–2.7) | 29.4% | 28–31 | 32.0% | 20.9% | 14.2% |
| Hypertension | 1.6 (1.2–2.2) | 52.0% | 50.1–54 | 56.4% | 23.8% | 10.4% |
| Alcohol (>21 units/week) | 1.2 (1.1–1.3) | 4.3% | 3.5–5 | 73.5% | 0.9% | 0.2% |
| Obesity | 1.6 (1.3–1.9) | 29.2% | 27.9–31 | 57.6% | 14.9% | 6.3% |
| Smoking | 1.6 (1.2–2.2) | 17.1% | 15.6–19 | 68.6% | 9.3% | 2.9% |
| Depression | 1.9 (1.6–2.3) | 18.1% | 16.5–20 | 51.1% | 14.1% | 6.9% |
| Low social contact | 1.6 (1.3–1.9) | 5.1% | 4.4–6 | 49.1% | 3.0% | 1.5% |
| Physical inactivity | 1.4 (1.2–1.7) | 47.2% | 44–50 | 29.0% | 15.9% | 11.3% |
| Diabetes | 1.5 (1.3–1.8) | 15.7% | 14.5–17 | 50.2% | 7.2% | 3.6% |
| Overall Weighted PAF | 50.5% | |||||
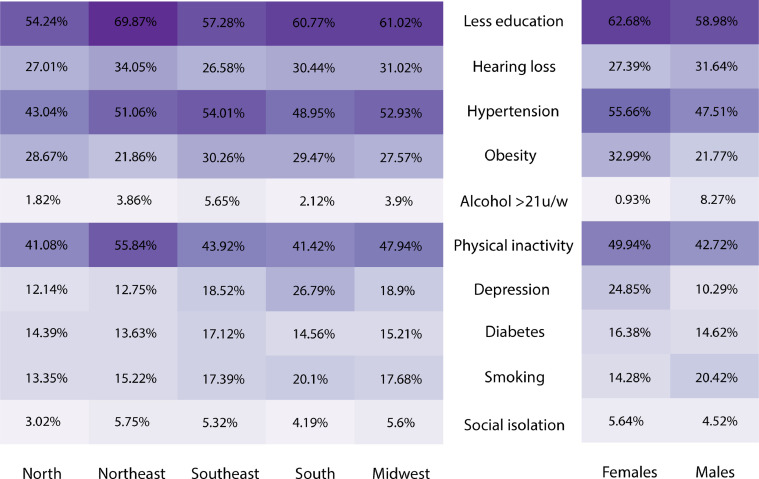
Regionally, the prevalence of modifiable risk factors exhibited a distinct profile. The prevalence of individuals with a low education level was the highest in the northeast (69·9%), while the highest rate of depression was observed in the south (26·8%). Individuals in the northeast also had the highest rates of hearing loss (34%), physical inactivity (55·8%), and social isolation (5·7%). Individuals from the southeast had the highest rates of hypertension (54%), obesity (30·3%), excessive alcohol consumption (5·7%), and diabetes (17·1%). Individuals from the midwest presented the highest rate of smoking (17·7%) (Figure 2).
Figure 2.
The prevalence of modifiable risk factors of dementia in each region of Brazil and genders.
Gender-associated differences in risk factors of dementia were also investigated. Diabetes and social isolation were statistically similar between males and females (p = 0·09 and p = 0·05, respectively). Females exhibited a higher frequency of low education level, hypertension, obesity, physical inactivity, and depression than males (p < 0·01 for all parameters; Figure 2). However, male individuals presented higher rates of hearing loss, smoking, and alcohol consumption than females (p < 0·01).
Discussion
In this study, we calculated the PAF for ten modifiable risk factors of dementia in a large sample that represented the Brazilian population. We found a total weighted PAF of 50·5%, indicating that nearly half of the dementia cases in Brazil are potentially preventable. A previous study also estimated the PAF for the Brazilian population, though with fewer risk factors and using another type of sampling and found a lower PAF of 32·3%.9 Our results were similar to those of a study by Mukadam et al., who found that PAF from six Latin American countries was 55·8%.4
Population Attributable Fraction estimates are vulnerable to the accuracy of epidemiological data, especially risk factors. The cohort from which we estimated the prevalence of these ten risk factors, ELSI-Brazil, was established according to the international epidemiological guidelines.6 Furthermore, the complex sampling strategy was previously validated to present national representativeness. This was a major advantage in this cohort compared to the National Health Surveys, where a different methodology was applied. Thus, the estimates in this study accurately reflected the prevalence of risk factors in the country.
Only ten risk factors were enough to demonstrate a higher PAF in Brazil than the PAF calculated for high-income countries.3 Approximately half of the cases of dementia are potentially preventable in Brazil, compared to 39·7% of the cases estimated for HIC and 41·2% of the cases estimated for LMIC.4 Interestingly, Spanish-speaking Latin America presented a similar overall PAF (55·8%), which was estimated by the 10/66 Dementia Research Group. Furthermore, Latin America and Brazil showed a similar PAF for the majority of the presented risk factors, except for a higher weighted PAF for hearing loss (14·2% vs. 7·7%) and physical inactivity (11·2% vs. 4·5%), and lower for smoking rate (2·9% and 5·7%). Rigorously managing the risk factors might decrease over 300,000 new cases of dementia by 2050 in Brazil.9 Understanding regional differences for each modifiable risk factor could guide public health policies.10 We performed a detailed analysis of each risk factor to provide information to policymakers worldwide.
Hearing loss had the most robust effect as a potentially modifiable risk factor for dementia in this study. Almost one-third of the studied population had some type of hearing loss, which was more than that estimated for Latin America or the rest of the world.2 Self-reported hearing loss is potentially underestimated, as almost one-third of the individuals with confirmed hearing loss reported normal hearing.11 Theoretically, hearing loss might contribute to cognitive decline due to social and environmental isolation, direct effects on brain structure integrity, and a constant load on cortical resources that otherwise could have buffered other neuropathologies.12 Hearing loss may be easily underdiagnosed in primary care settings13 and raising awareness is the first step to decrease its burden. The World Report on Hearing estimated that 80% of the individuals with hearing loss are from LMIC and comprise 340 million individuals.14 Screening programs for identifying hearing loss in adults are cost-effective and might mitigate its impact on age-related diseases. Thus, auditory alterations might be critical for primary care interventions.15
The PAF for a low education level in our study was 9·5%. Low educational level is associated with cognitive decline throughout the lifespan.5 Here, it was defined as less than four years of schooling, and it is a major preventable risk factor of dementia but challenging to improve in LMIC.16 Illiteracy is not specifically high in Brazil, but unequal distribution of literacy rates exists among states, especially among females (Figure 2). The ELSI-Brazil population sample included individuals born from 1915 to 1965, which was a period of political transitioning in Brazil that impacted education policies. More recent estimates show that 6·6% of Brazilians are illiterate.17 The relative impact of education on dementia in the following generations will probably be lower than that in the one studied here.
Cardiovascular risk factors such as hypertension, diabetes, smoking, sedentary lifestyle, and obesity are associated with cognition.18 The PAFs for hypertension, diabetes, physical inactivity, obesity, and smoking were 10·4%, 6·3%, 11·2%, 6·3%, and 2·9%, respectively, accounting for more than a quarter of the overall PAF. Controlling hypertension and diabetes in adults and older adults can decrease the incidence of cognitive decline.19 However, operational diagnosis and management of these risk factors are still insufficient in primary care but account for the most impactful lifestyle changes.20 Brazilian adult subjects exhibited a worse clinical profile compared to their English peers, though the frequency of disability was similar for both samples.21 The ELSI-Brazil cohort included individuals who were 50 years or older. Thus, we were able to measure midlife obesity. Physical activity can have a direct and indirect impact in preventing dementia, with increasing evidence supporting the positive effect of aerobic exercises.22 Additionally, a low PAF of smoking in Brazil reflects strong and successful nationwide anti-tobacco policies.23 Strategies targeted toward gender-associated risk factors might also benefit the population, as females showed more hypertension, obesity, and physical inactivity, while males presented higher rates of substance use. Overall, making behavioral changes and improving lifestyle habits can enhance the quality of life at old age.24
Mental health is a major determinant of wellness in older adults. Depression is associated with increased mortality, substantial healthcare, and social costs.25 Depression presented a weighted PAF of 6·9%, and its prevalence was higher in this study compared to others in the Brazilian population. In this study, women reported significantly higher instances of depression than men (24% vs. 10%). However, the prevalence of depression in Brazil was lower than that estimated in Latin America 29·9%).2 The prevalence of depression varies largely among Brazilian studies (3·9% to 17%)26,27 mostly due to different methods of evaluating depression. The relationship between depression and dementia is complex, as severe depression might be a risk factor or a consequence of dementia,28 where depressive states are suggested as prodromal stages of Alzheimer's disease. Finally, we found a low PAF for alcohol consumption and social contact of 0·2% and 1·5%, respectively.
Public health policies might benefit from epidemiological studies like this one. Identifying adults at risk of developing dementia is pivotal for long-term public health planning, but studies on this issue are absent in Latin America.29,30 Latin American countries have one of the highest prevalence rates of dementia worldwide because of their unique characteristics, such as low literacy and multiethnic background.31 Preventable risk factors comprise a large part of the risk factors of dementia in Latin America. Thus, a coordinated plan to address these factors among nations can benefit the population.32 Compared to other Latin American countries, Brazil has a highly heterogeneous culture because of miscegenation between different ethnic groups. Additionally, older adults with dementia in Brazil represent two-thirds of the individuals diagnosed with dementia worldwide who live in a middle-income country with low education level.1 Further studies might benefit from conducting comparative efficiency research to determine the cost-effectiveness of primary care interventions targeting the abovementioned risk factors.
This study has some limitations. Some individuals included in the cohort might have underdiagnosed dementia,33 which could impact the estimation of PAF. Although including these individuals can overestimate the results, their proportion in the population is probably very small; moreover, our results were consistent with those of previous studies. Genetic data was unavailable for the analysis, though it is known that genetic factors substantially influence some of the abovementioned risk factors. The relationship between genetic and non-genetic risk factors of dementia was assumed while designing the methods but should be further investigated. The original ELSI-Brazil cohort was based on epidemiological sampling, and the majority of data were self-reported. PAF might be underestimated in regions with poor primary healthcare coverage due to a higher rate of underdiagnosis of risk factors (such as hypertension and diabetes). Self-reported cases might underestimate the PAFs across the nation, especially for diabetes and alcohol abuse. Additionally, hearing loss was determined from the cohort through a single question. Finally, due to the original content of the ELSI-Brazil study questionnaire, we could not calculate the PAF for air pollution and traumatic brain injury. Future epidemiological studies evaluating the risk factors of dementia should include these two factors, besides genetic factors and multidimensional communication to get adequate successful responses from the population.34
Conclusion
We found a high Population Attributable Fraction for ten preventable risk factors of dementia in Brazil. The results of this study might provide an opportunity to change the impact of dementia in Brazil. The proportion of new cases of dementia that can be prevented by acting upon the ten risk factors studied in Brazil can substantially affect public health. Policymakers and public health services might be able to develop a nationwide strategy focusing on the improvement of lifestyle.
Contributors
WVB designed, analyzed, and wrote the manuscript; VBL performed statistical analyses and wrote the manuscript; MZS wrote the manuscript and revised its final version; MLFG coordinated the study and revised its final version; RMC designed, performed statistical interpretation, wrote the manuscript, and revised its final version
Data sharing statement
For this study, we accessed a public database (ELSI-Brazil), which is available on the project website. The R script used to perform the analysis will be available upon request to the corresponding author.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of interests
The authors declare no conflict of interest.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.lana.2022.100256.
Appendix. Supplementary materials
References
- 1.Alzheimer's disease international . Alzheimer's Disease International; 2018. World Alzheimer Report 2018 - The State of the Art of Dementia Research: New Frontiers.https://apo.org.au/sites/default/files/resource-files/2018-09/apo-nid260056.pdf [Internet][cited 2021 Jul 21]. Available from: [Google Scholar]
- 2.Mukadam N., Sommerlad A., Huntley J., Livingston G. Population attributable fractions for risk factors for dementia in low-income and middle-income countries: an analysis using cross-sectional survey data. Lancet Glob Health. 2019;7(5):e596–e603. doi: 10.1016/S2214-109X(19)30074-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Livingston G., Huntley J., Sommerlad A., et al. Dementia prevention, intervention, and care: 2020 report of the Lancet commission. Lancet. 2020;396(10248):413–446. doi: 10.1016/S0140-6736(20)30367-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mukadam N., Sommerlad A., Huntley J., Livingston G. Potential for dementia prevention in Latin America and Africa based on population-attributable fraction estimates - authors’ reply. Lancet Glob Health. 2019;7(10):e1325. doi: 10.1016/S2214-109X(19)30331-6. [DOI] [PubMed] [Google Scholar]
- 5.Nitrini R., Barbosa M.T., Brucki S.M.D., Yassuda M.S., Caramelli P. Current trends and challenges on dementia management and research in Latin America [Internet] J Glob Health. 2020;10 doi: 10.7189/jogh.10.010362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lima-Costa M.F., de Andrade F.B., de Souza P.R.B., et al. The brazilian longitudinal study of aging (ELSI-Brazil): objectives and design. Am J Epidemiol. 2018;187(7):1345–1353. doi: 10.1093/aje/kwx387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Telles EE. Princeton University Press; 2014. Race in Another America: The Significance of Skin Color in Brazil; p. 336. [Google Scholar]
- 8.Barnes D.E., Yaffe K. The projected effect of risk factor reduction on Alzheimer's disease prevalence. Lancet Neurol. 2011;10(9):819–828. doi: 10.1016/S1474-4422(11)70072-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Oliveira D., Jun Otuyama L., Mabunda D., et al. Reducing the number of people with dementia through primary prevention in Mozambique, Brazil, and Portugal: an analysis of population-based data. J Alzheimers Dis. 2019;70(s1):S283–S291. doi: 10.3233/JAD-180636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ferretti C., Sarti F.M., Nitrini R., Ferreira F.F., Brucki SMD. An assessment of direct and indirect costs of dementia in Brazil. PLoS One. 2018;13(3) doi: 10.1371/journal.pone.0193209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim S.Y., Kim H.J., Kim M.S., Park B., Kim J.H., Choi HG. Discrepancy between self-assessed hearing status and measured audiometric evaluation. PLoS One. 2017;12(8) doi: 10.1371/journal.pone.0182718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Powell D.S., Oh E.S., Lin F.R., Deal JA. Hearing impairment and cognition in an aging world. J Assoc Res Otolaryngol. 2021;22(4):387–403. doi: 10.1007/s10162-021-00799-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zazove P., Plegue M.A., McKee M.M., et al. Effective hearing loss screening in primary care: the early auditory referral-primary care study. Ann Fam Med. 2020;18(6):520–527. doi: 10.1370/afm.2590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Health Organization . World Health Organization; 2021. World Report on Hearing.https://www.who.int/publications/i/item/world-report-on-hearing [Internet][cited 2021 Sep 20]. Available from: [Google Scholar]
- 15.The Lancet Neurology Pointing the way to primary prevention of dementia. Lancet Neurol. 2017;16(9):677. doi: 10.1016/S1474-4422(17)30256-9. [DOI] [PubMed] [Google Scholar]
- 16.O'Donovan G., Hamer M., Sarmiento O.L., Hessel P. Education in early life markedly reduces the probability of cognitive impairment in later life in Colombia. Sci Rep. 2020;10(1):17685. doi: 10.1038/s41598-020-74822-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Instituto Brasileiro de Geografia e Estatística (IBGE) - Censo Agropecuário; 2017. [Internet] [cited 2021 Nov 28]. Available from: https://censos.ibge.gov.br/en/2184-news-agency/news/21266-illiteracy-decreases-in-2017-but-remains-above-2015-target.html.
- 18.Teixeira M.M., Passos V.M.A., Barreto S.M., et al. Association between diabetes and cognitive function at baseline in the Brazilian longitudinal study of adult health (ELSA- Brasil) Sci Rep. 2020;10(1):1–10. doi: 10.1038/s41598-020-58332-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hughes D., Judge C., Murphy R., et al. Association of blood pressure lowering with incident dementia or cognitive impairment: a systematic review and meta-analysis. JAMA. 2020;323(19):1934–1944. doi: 10.1001/jama.2020.4249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee J.K., McCutcheon L.R.M., Fazel M.T., Cooley J.H., Slack MK. Assessment of interprofessional collaborative practices and outcomes in adults with diabetes and hypertension in primary care: a systematic review and meta-analysis. JAMA Netw Open. 2021;4(2) doi: 10.1001/jamanetworkopen.2020.36725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tavares Milhem Ygnatios N., de Oliveira C., Vaz de Melo Mambrini J., Bof de Andrade F., Lima-Costa M.F., Lustosa Torres J. Differences in disability and nutritional status among older Brazilian and English adults: the Brazilian longitudinal study of aging (ELSI-Brazil) and English longitudinal study of aging (ELSA) cohorts. Am J Clin Nutr. 2021;114(2):422–428. doi: 10.1093/ajcn/nqab060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hörder H., Johansson L., Guo X., et al. Midlife cardiovascular fitness and dementia. Neurology. 2018;90(15):e1298–e1305. doi: 10.1212/WNL.0000000000005290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Portes L.H., Machado C.V., Turci S.R.B. Tobacco control policies in Brazil: a 30-year assessment. Cien Saude Colet. 2018;23(6):1837–1848. doi: 10.1590/1413-81232018236.05202018. [DOI] [PubMed] [Google Scholar]
- 24.Chen M.L., Hu J., McCoy T.P., Letvak S., Ivanov L. Effect of a lifestyle-based intervention on health-related quality of life in older adults with hypertension. J Aging Res. 2018;2018 doi: 10.1155/2018/6059560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bock J.O., Luppa M., Brettschneider C., et al. Impact of depression on health care utilization and costs among multimorbid patients–from the MultiCare cohort study. PLoS One. 2014;9(3):e91973. doi: 10.1371/journal.pone.0091973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Silva M.T., Galvao T.F., Martins S.S., Pereira MG. Prevalence of depression morbidity among Brazilian adults: a systematic review and meta-analysis. Braz J Psychiatry. 2014;36(3):262–270. doi: 10.1590/1516-4446-2013-1294. [DOI] [PubMed] [Google Scholar]
- 27.de Ferreira-Filho S.F., Borelli W.V., Sguario R.M., et al. Prevalence of dementia and cognitive impairment with no dementia in a primary care setting in southern Brazil. Arq Neuropsiquiatr. 2021;79(7):565–570. doi: 10.1590/0004-282X-ANP-2020-0410. [DOI] [PubMed] [Google Scholar]
- 28.Bennett S., Thomas AJ. Depression and dementia: cause, consequence or coincidence? Maturitas. 2014;79(2):184–190. doi: 10.1016/j.maturitas.2014.05.009. [DOI] [PubMed] [Google Scholar]
- 29.Nitrini R., Caramelli P., Herrera E., et al. Incidence of dementia in a community-dwelling Brazilian population. Alzheimer Dis Assoc Disord. 2004;18(4):241–246. [PubMed] [Google Scholar]
- 30.Prince M., Acosta D., Ferri C.P., et al. Dementia incidence and mortality in middle-income countries, and associations with indicators of cognitive reserve: a 10/66 dementia research group population-based cohort study. Lancet. 2012;380(9836):50–58. doi: 10.1016/S0140-6736(12)60399-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Parra M.A., Baez S., Allegri R., et al. Dementia in Latin America: assessing the present and envisioning the future. Neurology. 2018;90(5):222–231. doi: 10.1212/WNL.0000000000004897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Parra M.A., Baez S., Sedeño L., et al. Dementia in Latin America: paving the way toward a regional action plan. Alzheimers Dement. 2021;17(2):295–313. doi: 10.1002/alz.12202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nakamura A.E., Opaleye D., Tani G., Ferri CP. Dementia underdiagnosis in Brazil. Lancet. 2015;385(9966):418–419. doi: 10.1016/S0140-6736(15)60153-2. [DOI] [PubMed] [Google Scholar]
- 34.Macinko J., Seixas B.V., de Mambrini J.V.M., Lima-Costa MF. Which older Brazilians will accept a COVID-19 vaccine? Cross-sectional evidence from the Brazilian longitudinal study of aging (ELSI-Brazil) BMJ Open. 2021;11(11) doi: 10.1136/bmjopen-2021-049928. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.