Abstract
Anxiety and obsessive-compulsive disorders are common childhood psychiatric disorders. Behavioral inhibition (BI) is a widely studied risk factor for anxiety. Less is known about overcontrol, a related behavioral phenotype characterized by concern for errors, perfectionism, and inflexibility and also associated with anxiety and obsessive-compulsive disorder. Both BI and overcontrol show associations with aberrant cognitive control and neural error responding (via the error-related negativity; ERN) yet it is unknown whether each imparts differential risk. Understanding whether overcontrol demonstrates independent associations from BI with cognitive functioning, neural error monitoring, and childhood anxiety and obsessive-compulsive presentations could aid in identifying a novel mechanistic treatment target. We assessed BI, overcontrol, cognitive functioning and psychopathology in a cross-sectional sample of 5-6 year old children (N=126). Children completed an electroencephalogram (EEG) to assess the ERN. Overcontrol was associated with worse cognitive shifting, worse inhibitory control and higher anxiety and obsessive-compulsive symptoms, beyond BI. BI was associated with worse cognitive shifting, better inhibitory control and higher anxiety symptoms, beyond overcontrol. When assessed simultaneously, only overcontrol demonstrated a significant relationship with a blunted ERN. Moreover, overcontrol mediated (cross-sectionally) the well-established relationship between ERN and anxiety and obsessive-compulsive symptoms. BI and overcontrol impart differential risk for child cognitive functioning and anxiety while overcontrol demonstrates additional risk for aberrant neural error monitoring, anxiety and obsessive-compulsive presentations. Overcontrol may also be a mechanistic pathway between the ERN and transdiagnostic anxiety and obsessive-compulsive symptoms. Overcontrol may be a target warranted for early-childhood intervention in anxiety and OCD.
Keywords: overcontrol, error-related negativity, behavioral inhibition, performance monitoring, pediatric anxiety, OCD
Anxiety is the most common psychopathology in childhood (Kessler, Chiu, Demler, & Walters, 2005) and although categorical diagnostic symptoms distinguish between pediatric anxiety disorders and obsessive-compulsive disorders (OCD; DSM-V; American Psychiatric Association, 2000), these presentations are commonly comorbid in early childhood, as approximately 50% of children with OCD meet criteria for an anxiety disorder (Peris et al., 2017). Comorbidity between these presentations is associated with greater psychiatric severity (Langley, Lewin, Bergman, Lee, & Piacentini, 2010), highlighting the need to understand early-emerging mechanisms that could provide novel, more focused, treatment targets for early intervention in these heterogeneous and difficult to treat childhood disorders (Allen, Benningfield, & Blackford, 2020).
The current paper investigates an understudied transdiagnostic phenotype of ‘overcontrol.’ Overcontrol is a constellation of characteristics including elevated monitoring of performance, extreme concern for errors, perfectionism and cognitive inflexibility (Asendorpf, Borkenau, Ostendorf, & Van Aken, 2001; Gilbert, Barch, & Luby, 2019; Lynch, 2018). Overcontrol is of interest as a putative unique and modifiable mechanistic treatment target that spans broadly across anxiety disorders, OCD, and other later-emerging psychiatric presentations, including anorexia and treatment-resistant depression (Gilbert, Hall, & Codd, 2020; Lynch, 2018). We compare independent and differential associations of overcontrol in relation to behavioral inhibition (BI), one of the most well known risk factors for childhood anxiety. To do this, we aim to validate overcontrol’s relationship, beyond the role of BI with cognitive control, neural error monitoring and pediatric anxiety and obsessive-compulsive symptoms in 5-6 year old children. We also test overcontrol as a possible mechanism explaining the well-established link between neural error monitoring (via the error-related negativity; (ERN)) and childhood anxiety and OCD (Carrasco et al., 2013; Meyer, 2017).
Behavioral Inhibition (BI) and Overcontrol
Behavioral inhibition (BI), a temperamental trait characterized by distress and withdrawal in response to novelty and unfamiliar people (Kagan, Reznick, Clarke, Snidman, & Garcia-Coll, 1984), is one of the most researched and best-known predictors for the development of social anxiety disorder (Clauss, Avery, & Blackford, 2015). BI is an identifiable risk factor in infants and toddlers (Fox, Henderson, Marshall, Nichols, & Ghera, 2005) and while 15% of young children are thought to exhibit BI, only ~40% of BI children end up exhibiting social anxiety disorder during childhood or adolescence (Gladstone, Parker, Mitchell, Wilhelm, & Malhi, 2005). Based on this, recent research has focused on identifying more nuanced pathways between BI and social anxiety (Fox et al., 2021). In particular, in the context of elevated BI in children, heightened neural error monitoring increases risk for social anxiety (Lahat et al., 2014) while BI children with better inhibitory control and worse cognitive set shifting have repeatedly demonstrated elevated social anxiety (Buzzell et al., 2021; Henderson, Pine, & Fox, 2015). As such, Fox and colleagues (2021) have suggested that heightened detection of errors, more reactive and automatic cognitive control (e.g., elevated reactive inhibitory control), and less planful cognitive control (e.g., worse cognitive shifting abilities) are all associated with higher risk of social anxiety in the context of BI.
A separate and later-emerging phenotype that is purportedly characterized by heightened error monitoring and aberrant cognitive control processing is overcontrol. Overcontrolled tendencies repeatedly cluster together (Asendorpf et al., 2001; Gilbert, Whalen, et al., 2020), the overcontrolled phenotype manifests around age 5 (Eisenberg, Spinrad, & Eggum, 2010; Gilbert et al., 2019; Gilbert, Whalen, et al., 2020) and is stable over the lifespan (Asendorpf et al., 2001; Specht, Luhmann, & Geiser, 2014). Overcontrolled children struggle with transition and change, prefer structure, often are perfectionists with high social comparisons and experience distress when making mistakes. Although originally examined in the personality and temperament literatures (Eisenberg et al., 2010; Robins, John, Caspi, Moffitt, & Stouthamer-Loeber, 1996), overcontrol has also been studied in relation to BI (Henderson et al., 2015). Specifically, the above-mentioned characteristics that have been shown to exacerbate risk in BI (Fox et al., 2021) also make up the characteristics of the overcontrolled phenotype. As such, similar to BI children, overcontrolled children show aberrant neural error monitoring (Gilbert et al., 2019; Gilbert, Perino, Myers, & Sylvester, 2020) and deficits in cognitive set shifting (Gilbert et al., 2019). Although some hypothesize that, similar to BI, overcontrol is characterized by better inhibitory control (Lynch et al., 2018), preliminary evidence indicates overcontrolled children show inhibitory control deficits (Gilbert et al., 2019). Given the overlap of BI and overcontrol and that high BI children who exhibit overcontrolled tendencies are at elevated risk, it is important to understand how overcontrol, the lesser studied and understood of these two risk factors, may be differentially associated with cognitive deficits, error processing, and psychiatric outcomes so as to better design targeted intervention.
BI, Overcontrol, and Risk for Psychopathology
BI is the best-known predictor of social anxiety disorder (Clauss & Blackford, 2012) and to a lesser degree, also demonstrates significant associations with other child anxiety presentations (Sandstrom, Uher, & Pavlova, 2020). Similar to BI, overcontrol is also associated with broad pediatric anxiety presentations (Gilbert, Perino, et al., 2020). However, overcontrol is implicated in other child and adolescent psychiatric presentations that are less associated with BI, including OCD (Gilbert, Barclay, Tillman, Barch, & Luby, 2018; Pinto, Greene, Storch, & Simpson, 2015) and later on in development, anorexia nervosa (Isaksson, Ghaderi, Wolf-Arehult, & Ramklint, 2021). Social anxiety, OCD, and anorexia are commonly comorbid (Kerr-Gaffney, Harrison, & Tchanturia, 2018; Levinson et al., 2019), share etiological overlap, and may represent variations on a common phenotype (Cederlöf et al., 2015). Moreover, comorbidity between these disorders is often associated with treatment resistance (Kerr-Gaffney et al., 2018). Of note, early-onset OCD exhibits between 6 – 11 years of age (Taylor, 2011), half of patients with social anxiety exhibit onset by age 13 (Stein, 2006) and the median onset for anorexia is during the teen years, ranging from 12 to 19 years (Swanson, Crow, Le Grange, Swendsen, & Merikangas, 2011; Udo & Grilo, 2018), possibly demonstrating a progression of overlapping psychiatric presentations that starts early in development and could be linked by shared overcontrolled tendencies. As such, in contrast to more specific BI and anxiety relationships, overcontrol may be an underlying dimension contributing risk for a broader range of psychiatric presentations. If so, overcontrol could be a separate and independent transdiagnostic target for early intervention that decreases risk across multiple psychiatric presentations across the lifespan.
Neural Error Monitoring (ERN) Associations with BI and Overcontrol
In addition to overlap in cognitive control functioning and psychiatric outcomes, BI and overcontrol are also both associated with aberrant neural error monitoring, as assessed using the error-related negativity (ERN). The ERN is an electroencephalogram (EEG) recorded event related potential (ERP) that occurs as a negative deflection after a behavioral error (Gehring, Liu, Orr, & Carp, 2012). Within the context of BI, the ERN has consistently been implicated as a moderating factor that increases risk for social anxiety disorder (Henderson et al., 2015). However, heightened neural error monitoring is implicated in additional psychiatric disorders outside of social anxiety. The ERN is particularly elevated in OCD (Riesel, 2019) and in adults, meta-analytic evidence indicates that both anxiety and obsessive-compulsive traits are unique dimensions that account for heightened ERN and internalizing associations (Pasion & Barbosa, 2020). Indeed, the ERN has been speculated to be an endophenotype of OCD (Riesel, 2019). Importantly, children have also repeatedly demonstrated the well-established relationship between ERN alterations and broad anxiety and OCD (Meyer, 2017).
Notably, preliminary evidence indicates that a blunted ERN is characteristic of overcontrolled 5-6 year olds (Gilbert et al., 2019). A blunted ERN associated with overcontrol in the preschool period may appear counterintuitive given that adolescents and adults with anxiety and OCD demonstrates a larger ERN (Pasion & Barbosa, 2020; Riesel, 2019). However, differential ERN-anxiety associations are evident at different stages of childhood development (Moser, 2017). Specifically, a blunted ERN is associated with higher fearful behaviors in 6 year olds (Torpey et al., 2013), higher anxiety symptoms in 5-7 year olds (Lo et al., 2016), and higher age 3 fear predicts an age 6 blunted ERN (Meyer et al., 2018). Yet, by age 9, this relationship is opposite (and mirrors adult literature) such that a larger ERN is associated with anxiety (Ip et al., 2019). As such, at ages 5-6, blunted ERN-anxiety relationships are expected.
Taken together, the ERN has repeatedly been linked with anxiety and OCD in both children and adults (Meyer, 2017; Pasion & Barbosa, 2020) and is thought to be a transdiagnostic endophenotype (Riesel, 2019), yet the mechanistic process that leads this neural marker to be associated with psychiatric presentations is unknown. The ERN has been hypothesized to index error detection in order to recruit cognitive control (Yeung & Summerfield, 2012) or a compensatory neural process resulting from increased stimulus processing of the error (Moser, 2017). As such, in the context of increased processing of the error and recruitment of cognitive control, elevated perfectionism and checking tendencies characteristic of overcontrol may be a pathway by which the ERN is associated with increased anxiety and OCD symptoms. As such, overcontrol may not only demonstrate associations with the ERN, but overcontrol may in fact be a mechanistic phenotype that associates the ERN with anxiety and OCD.
The Current Study
The aim of the current study was two-fold. First, we sought to examine whether overcontrol demonstrates independent and differential relationships (compared with BI) with cognitive control, neural error monitoring (ERN) and transdiagnostic anxiety and OCD symptoms in a cross-sectional sample of 5-6-year-old children. The 5-6 year age range is of importance as although BI has been readily identifiable since toddlerhood, overcontrol is thought to be crystallizing and clearly manifests by age 5 (Eisenberg et al., 2010; Fox et al., 2005; Gilbert et al., 2019). Moreover, age 5-6 years is a pivotal time for children who are transitioning to school, which might exacerbate psychiatric presentations, yet this age range is also prior to most onsets of OCD and social anxiety (Stein, 2006; Taylor, 2011). As such, this age range provides the earliest time to identify maladaptive associations with overcontrol prior to onset of full psychiatric disorder, potentially providing a window of opportunity for early intervention. Second, we examined whether overcontrol may act as a mechanistic pathway linking previously demonstrated associations of the ERN with anxiety and OCD (Meyer, 2017; Moser, 2017; Riesel, 2019). For our first aim, we examined independent associations of BI and overcontrol with aspects of cognitive control (e.g., inhibitory control, shifting abilities, working memory), the ERN, and parent-reported and clinician administered psychiatric diagnostic information. We hypothesized that BI and overcontrol would each demonstrate independent associations with poor cognitive set-shifting abilities, the ERN, and anxiety symptoms. We hypothesized only BI would demonstrate associations with better inhibitory control. Additionally, we hypothesized that only overcontrol would demonstrate associations with OCD symptoms. For our second aim, we examined whether the known relationship between neural error monitoring and transdiagnostic anxiety and OCD symptoms (Meyer, 2017; Riesel, Goldhahn, & Kathmann, 2016) was mediated by overcontrol after accounting for BI.
Methods
Participants.
Children aged 5.0-6.99 years were recruited from the St. Louis region. Children were 48% (n=59) female, 6.7% (n=9) Hispanic/Latinx ethnicity; 76% (n=97) Caucasian, 10% (n=13) Black, 12% (n=15) mixed race and 1% (n=1) Native American and 1% (n=1) Asian race, and came from relatively high socioeconomic backgrounds. See Table 1 for demographic and clinical information about the sample and associations with BI and overcontrol. Recruitment materials sought healthy and overcontrolled children through posted flyers, online posting boards, informational talks about child anxiety at local schools and childhood anxiety clinics. We oversampled for overcontrolled children by recruiting children with “perfectionistic, shy, and self-critical tendencies.” Exclusion criteria included Autism Spectrum Disorders, chronic medical, neurological disorders, speech, language or cognitive delays or learning disabilities, and current psychotropic medication use.
Table 1.
Sociodemographic and psychiatric disorder associations with behavioral inhibition and overcontrol (n=123)
| Entire Sample | Behavioral Inhibition Questionnaire (BIQ) |
Overcontrol in Youth Checklist (OCYC) |
|||
|---|---|---|---|---|---|
| Mean(SD) | r | r | |||
| Sociodemographic Information | |||||
| Age | 5.95(.62) | .16 | .09 | ||
| Income to needs ratio | 2.91(1.24) | −.02 | .02 | ||
| Gender (% female (n)) | 48%(59) | .05 | .09 | ||
| n | Yes Mean(SD) |
No Mean(SD) |
Yes Mean(SD) |
No Mean(SD) |
|
| KSADS-EC Child Diagnoses | |||||
| Overcontrol-related Anxiety Disorder | 30 | 120.37(35.80)** | 86.25(32.17) | 10.97(4.56)** | 5.11(4.45) |
| Separation Anxiety Disorder | 6 | 129.67(22.16)* | 92.61(35.72) | 11.00(3.03)* | 6.24(5.09) |
| Social Anxiety Disorder | 10 | 149.40(27.06)** | 89.63(32.66) | 10.20(5.07)* | 6.15(5.00) |
| GAD | 24 | 117.92(35.95)** | 88.83(33.88) | 11.26(4.89)** | 5.39(4.51) |
| Specific Phobia | 2 | 98.50(89.80) | 94.31(35.39) | 8.00(11.31) | 6.45(5.03) |
| OCD | 2 | 103.00(11.31) | 94.23(36.27) | 11.00(4.24) | 6.40(5.10) |
| ADHD | 4 | 93.50(51.07) | 94.41(35.71) | 8.75(6.80) | 6.40(5.06) |
| MDD | 5 | 144.00(21.63)* | 92.32(35.05) | 13.40(1.51)* | 6.18(4.99) |
| ODD | 3 | 99.33(58.05) | 94.25(35.68) | 8.33(6.81) | 6.42(5.08) |
| CD | 1 | 119.00(⊗) | 94.18(36.09) | 6.00(⊗) | 4.00(5.12) |
Note: ^Female gender=0; PAS = Preschool anxiety scale; CYBOCS= Child Yale Brown Obsessive Compulsive Symptoms; Overcontrol-related Anxiety Disorder = Anxiety disorders purportedly related to overcontrol, including OCD; Separation Anxiety Disorder, Social Anxiety Disorder and GAD; OCD= Obsessive Compulsive Disorder; GAD= Generalized Anxiety Disorder; MDD= Current Major Depressive Disorder; ADHD= Attention Deficit Hyperactivity Disorder; ODD= Oppositional Defiant Disorder; CD= Conduct Disorder; ⊗= unable to calculate due to only one participant meeting criteria.
p<.01
p<.001
Of the 163 participants who were phone screened, 155 were eligible, 126 of which completed the in-person session (n=29 were no longer interested and/or didn’t schedule a session). This session consisted of questionnaires and clinical interviews assessing child psychiatric symptoms for the caregiver, cognitive assessments and an electroencephalogram (EEG) for the child, and a parent-child interaction task as part of the larger study on early overcontrolled tendencies. A subset of children (n=86) completed the EEG assessment (this EEG portion was added to the study after initial start) and the cognitive control measure (n=63). Caregivers were primarily biological mothers (92%), followed by biological fathers (7%), and other relations (1%). All materials were approved by the Washington University School of Medicine IRB and conform to Declaration of Helskini standards. All legal guardians provided written consent and children provided verbal assent.
Measures.
Overcontrol.
Child overcontrol was assessed with the Overcontrol in Youth Checklist (OCYC; Gilbert et al., 2019). The OCYC is a validated 18-item yes/no parent-report assessing general child tendencies of perfectionism, social concern, inflexibility and frustration with change as part of the overcontrolled phenotype (e.g., “My child gets upset or has trouble when plans change at short notice” and “My child thinks there is only ‘one right way’ to do things”). The total score was used (α=.90)
Behavioral Inhibition.
The Behavioral Inhibition Questionnaire (BIQ; Bishop, Spence, & Mcdonald, 2003) is a 30-item parent-report assessing inhibited behaviors in response to adults, peers, preschool/separation, performance, new situations and physical challenges rated from 1 (hardly ever) to 6 (almost always). The BIQ demonstrates validity and reliability in preschoolers and complementary information to observed BI (Kim et al., 2011) and has been used in this age-range (e.g., Premo et al., 2021; Vreeke & Muris, 2012). The total score showed excellent internal consistency (α=.96).
Cognitive functioning.
The Behavior Rating Inventory for Executive Function-Preschool Version (BRIEF-P; Gioia, Espy, & Isquith, 2003)) was completed by parents. The BRIEF-P assesses behavioral manifestations of executive function in children <6 years. Due to an algorithm error, all children were administered the BRIEF-P; 6 year olds should have been administered the BRIEF (Gioia, Isquith, Guy, & Kenworthy, 2000). As such, analyses reported include the subset (n=60) with proper administration. Age-normed T-scores were used, with higher scores indicating greater impairment. Subscales include Inhibition (inhibitory control), Shifting, Emotional Control, Working Memory and Plan/organize; for the current study, theoretical subscales of interest in relation to BI and overcontrol include Inhibition (to assess inhibitory control) and Shifting (to assess cognitive shifting).
Anxiety and obsessive-compulsive symptoms.
Caregivers reported on child anxiety and OCD symptoms using two measures. First, the Preschool Anxiety Scale (PAS) is a 28-item parent-report measure of anxiety symptoms in 3-6 year old children (Spence, Rapee, McDonald, & Ingram, 2001). The PAS includes symptoms of generalized anxiety, social anxiety, obsessive-compulsive symptoms, physical injury fears and separation anxiety. The total score was used (α=.89). Second, the Child Yale-Brown Obsessive Compulsive Scale (CY-BOCS; Scahill et al., 1997) was used to assess child obsessive compulsive symptoms. The CY-BOCS is a clinician-rated semi-structured interview comprised of a symptom checklist and severity scale. In the current study, we calculated a sum of the total number of past and present obsessions and compulsions endorsed by the parent about their child.
Psychiatric Diagnoses.
Psychiatric diagnoses were obtained using the Kiddie Schedule for Affective Disorders, Early Childhood Version (KSADS-EC; Gaffrey & Luby, 2012). The KSADS-EC is a semi-structured interview administered to the caregiver that assessed current and past child anxiety disorders (separation anxiety disorder, generalized anxiety disorder, social anxiety disorder), obsessive-compulsive disorder, major depressive disorder and externalizing disorders (oppositional defiant disorder, conduct disorder, attention deficit hyperactivity disorder). We created an overcontrolled anxiety disorder variable that included (yes/no) whether a child met criteria for overcontrol-related presentations: separation anxiety disorder, social anxiety disorder, generalized anxiety disorder and OCD. Approximately 20% of tapes were coded for reliability, which was good across diagnoses (97.5% agreement).
Income-to-Needs Ratio.
Socioeconomic status was computed by dividing total family income by the federal poverty level, based on family size to obtain the income-to-needs ratio.
Tasks.
Children played a developmentally appropriate go/no-go task called the Space-Alien game (Meyer, Carlton, Chong, & Wissemann, 2019). Children were instructed to zap the aliens (go-trials; 75% of trials) and save the astronauts (no-go trials; 25% of trials). To zap aliens children pressed a button as quickly as possible. Errors were measured when children zapped (i.e., pressed the button) astronauts. Alien/astronaut stimuli appeared on the screen for 500ms, followed by a blank screen (with an intertrial interval (ITI) of 1000-2000ms). After receiving instructions and completing 5 practice trials, children completed 3 blocks of 100 trials each. After each block children received feedback according to their performance (i.e., “Try to respond more quickly” if their accuracy was 95% or higher). The task was presented on a 20-inch monitor using Presentation (Neurobehavioral Systems, In., Albany, California, USA) and a Logitech Gamepad F310 game controller. Prior to the task, children were shown three boxes of toys with increasingly attractive toys. Children were told for each alien they zapped, they accrued points and the more points they won, the better prize they could pick. Behavioral measures included reaction time (RT) and accuracy (errors).
Psychophysiological Recording, Processing and Analysis.
A BrainVision ActiCHamp 32-channel electrode system (Brain Products, Germany) was used to record electroencephalogram (EEG) subset of the International 10/20 system sites and a ground electrode at FPz. Additional electrooculogram (EOG) electrodes included two electrodes placed laterally to the eyes (horizontal EOG) and two electrodes placed above and below the left eye to detect blinks and eye movements (vertical EOG). Continuously recorded EEG was digitized at 500Hz with 24 bits of resolution and referenced to Cz, and were re-referenced to the average of TP9 and TP10 (adjacent to mastoids) during offline processing using BrainVision Analyzer software (Brain Products Germany). Additional offline processing included band-pass filtering from .1-30Hz, eye blink and movement correction using Gratton et al (Gratton, Coles, & Donchin, 1983) and artifact rejection using a semi-automated procedure allowing maximum voltage steps of 50 μV, maximum absolute voltage difference of 175 μV within 400ms and a minimum allowed activity of .5 μV within 100ms.
Response-locked ERP’s were averaged independently for correct and error trials. Baseline correction window was −500 to −300 ms before a response and the mean amplitude was measured between −50ms to 100ms of the response at electrode site Cz as has been done previously using this task (Meyer et al., 2019). To be included in analyses, children had to have at least 6 errors (n=1 excluded for this reason). Based on past literature (Meyer, Lerner, De Los Reyes, Laird, & Hajcak, 2017), we used linear regression to create residualized scores for error and correct responses, which allowed us to examine associations with errors, partialing out the effect of correct responses. These residualized scores reflected variation in the response to errors not accounted for by correct responses (ERNresid) and variation in correct responses not accounted for by error responses (CRNresid). In line with previous research (Meyer et al., 2017) and given errors were associated with the CRNresid (r=−.40,p<.001) and the ERNresid (r=.27, p=.01) and RT to correct trials was associated with the ERNresid (r=.30, p=.006), we included both behavioral indicators as covariates in ERN analyses. To measure internal consistency of the ERN and CRN, the correlation between odd and even trials for was examined, and corrected using the Spearman-Brown prophecy formula (Nunnally, Bernstein, & Berge, 1967).
Statistical Analyses.
First, we examined demographic differences to include as covariates, correlations among all variables and independent samples t-tests examining diagnostic differences on BI and overcontrol. To test independent associations of BI and overcontrol with cognitive control, we completed two hierarchical linear regressions predicting BI or overcontrol as outcomes in order to include all cognitive control facets in one model. In the first model predicting BI, Step 1 included demographic covariates and overcontrol and Step 2 included all subscales of the BRIEF (inhibition, set-shifting, emotional control, working memory and plan/organize). In the second model predicting overcontrol, Step 1 included demographic covariates and BI and Step 2 included all BRIEF subscales. To test independent and incremental associations of BI and overcontrol with the ERN, we completed two hierarchical linear regressions predicting the ERNresid and CRNresid, entering demographic and behavioral responding covariates in Step 1, BI in Step 2 and overcontrol in Step 3 of each model. To test the independent and incremental associations of BI and overcontrol on psychiatric symptoms of anxiety and OCD, we completed two hierarchical linear regressions with demographic covariates in step 1, the addition of BI in step 2, and the addition of overcontrol in step 3. To calculate effect sizes for regressions, we entered all variables in one model (including covariates and BI and overcontrol) and then all variables except the variable of interest (e.g., OCYC) in a second model to utilize R2 to convert to Cohen’s f2 (.02, .15, and .35 indicate small, medium and large effect sizes, respectively (Selya, Rose, Dierker, Hedeker, & Mermelstein, 2012).
Lastly, we tested two statistical mediations using overcontrol as a plausible mediator between cross-sectional 1) ERNresid and anxiety symptoms and 2) ERNresid and OCD symptoms, controlling for demographic covariates and BI. We used the SPSS v.26 (IBM Corporation, Amonk, NY, USA) PROCESS macro, v3.4 (Hayes, 2013) to estimate the indirect effects using bootstrap estimates and 95% confidence intervals. Secondary analyses included using overcontrol-related anxiety disorder status (yes/no) as an outcome in the mediational model and testing specificity of the mediation model in two ways: 1) reversing the model so the ERNresid was the mediator and overcontrol the predictor and 2) reversing the role of BI and overcontrol in the model by testing BI as the mediator (controlling for overcontrol).
Results
Demographic and preliminary clinical associations with BI and overcontrol.
BI and overcontrol were not associated with child age, gender, race or income-to-needs (p’s > .05; Table 1). However previous work indicates associations of overcontrol, BI and the ERN with age and gender (Gilbert et al., 2019; Ip et al., 2019) and thus to be conservative these two demographic indicators were included as covariates in all analyses. BI and overcontrol were correlated with each other (r=.52, p<.001) and as shown in Supplemental Table 1, BI and overcontrol were both associated with most cognitive control factors and psychiatric symptoms. See Table 1 for diagnostic differences in BI and overcontrol.
BI and Overcontrol Associations with Cognitive Control
Above age, gender and BI, worse cognitive shifting (f2=.27) and worse inhibitory control (f2=.16) were associated with higher overcontrol (Step 2: F(2,57)=25.44, R=.80, ΔR2=.34, p<.001) (see Table 2). Above age, gender and overcontrol, better inhibitory control (f2=.01)and worse cognitive shifting (f2=.39) were associated with higher BI (Step 2: F(2,57)=16.31, R=.76, ΔR2=.24, p<.001). Because cognitive inflexibility and rigidity is an aspect of the overcontrolled phenotype (i.e., one of the features of the larger constellation of characteristics), there is overlap in some of the questions from the OCYC and the BRIEF-P Shift subscale; there is also slight overlap in questions from the BIQ and BRIEF-P Inhibit subscale. As such, in secondary analyses, we removed 6 items from the OCYC that overlapped with questions from the BRIEF-P shift subscale and 2 items from the BIQ that overlapped with questions from the BRIEF-P inhibit subscale and re-ran above regressions. Findings were identical and are reported in Supplemental table 1.
Table 2.
Associations of cognitive control with overcontrol and behavioral inhibition (n=63).
| Overcontrol (OCYC) | Behavioral inhibition (BIQ) | |||||
|---|---|---|---|---|---|---|
| R2 | B(SE) | β | R2 | B(SE) | β | |
| Step 1 | .30*** | .28*** | ||||
| Age | −1.66(2.00) | −.01 | 28.88(13.40)* | .23 | ||
| Gender | −.20(1.15) | −.02 | 7.51(7.90) | .10 | ||
| BIQ/OCYC | .08(.02)*** | .56 | 3.69(.76)*** | .51 | ||
| Step 2 | .62*** | .48*** | ||||
| BIQ/OCYC | .02(.02) | .17 | .88(.99) | .12 | ||
| BRIEF Inhibitory Control | .25(.06)*** | .54 | −.91(.39)* | −.24 | ||
| BRIEF Shift | .15(.05)** | .30 | 2.33(.43)*** | .72 | ||
Note: BRIEF= Behavior Rating Inventory of Executive Functioning – Preschool Version; higher scores indicate more impairment; BIQ = Behavioral Inhibition Questionnaire; OCYC= Overcontrol in Youth Checklist; In models predicting behavioral inhibition, overcontrol used as covariate and in models predicting overcontrol, behavioral inhibition used as a covariate; this variable shown again in Step 2 to demonstrate continued predictive validity.
p<.05
p<.01
p<.001
BI and Overcontrol Associations with Anxiety and OCD Symptoms
After accounting for covariates (Step 1), BI predicted higher anxiety symptoms (Step 2: F(1,118)=75.75, R=.64, ΔR2=.38, p<.001) and both BI (f2=.28)and overcontrol (f2=.46) independently predicted higher anxiety symptoms when overcontrol was entered into the model (Step 3: F(1,117)=61.61, R=.78, ΔR2=.21, p<.001). Above covariates (Step 1), BI significantly predicted OCD symptoms when entered by itself (Step 2: F(1,119)=16.26, R=.13, ΔR2=.12, p<.001). However, when overcontrol was entered in Step 3, only overcontrol (f2=.21) was a significant predictor of OCD symptoms (Step 3: F (1,118)=22.61, R=.52, ΔR2=.14, p<.001), and BI (f2=.01) was no longer significant (See Table 3).
Table 3.
Independent associations of behavioral inhibition and overcontrol with anxiety and obsessive-comulsive symptoms (n=123)
| PAS Total |
CYBOCS |
|||
|---|---|---|---|---|
| R2 | B(SE) | R2 | B(SE) | |
| Step 1 | .03 | .01 | ||
| Age | 3.29(1.94)* | .32(.30) | ||
| Gender | −.01(2.42) | .22(.38) | ||
| Step 2 | .41** | .13** | ||
| BIQ | .23(.03)** | .02(.005)** | ||
| Step 3 | .61** | .27** | ||
| BIQ | .13(.03)** | .007(.005) | ||
| OCYC | 1.39(.18)** | .18(.04)** | ||
Note: PAS= Preschool anxiety scale; CYBOCS= Child Yale Brown Obsessive Compulsive Scale; BI= Behavioral Inhibition Questionnaire; OCYC= Overcontrol in Youth Checklist. BIQ shown in step 3 for continued predictive ability when OCYC entered in this step.
p<.01
p<.001
BI and Overcontrol Associations with Neural Error Monitoring
Children made an average 28.12(13.68) errors and RT was faster on error (M(SD)=498.31(88.22)) versus correct (M(SD)=561.52(78.87)) trials (F(1,85)=139.69, p<.001). The ERP response was more negative after errors than correct responses F(1,85)=134.47, p<.001. The ERN (r=.76, p<.001) and the CRN (r=.92; p<.001) demonstrated good split-half reliability that was better than previous split-half reliability using a different Go/No-Go task in young children (ERN: r=.67; CRN: r=.79; Szenczy, Levinson, Hajcak, Bernard, & Nelson, 2021). Behavioral indicators from the Space Alien go/no-go task, including number of errors and reaction time (RT) to go trials were associated with the ERNresid (errors: r=.27, p=.01; RT: r=.30, p=.06) and so were used as covariates in regressions, however, demonstrated no association with overcontrol (errors: r=−.01, p=.90; RT: r=−.03, p=.76) or BI (errors: r=−.06, p=.61; RT: r=−.05, p=.64). There were no demographic, overcontrol or BI differences between those with and without EEG data (age: t(121)=−1.52, p=.13; gender: χ2(1,123)=1.10, p=.29; race: χ2(4,123)=3.31, p=.51; OCYC Total: t(121)=−.14, p=.89; BI: t(121)=−.42, p=.68).
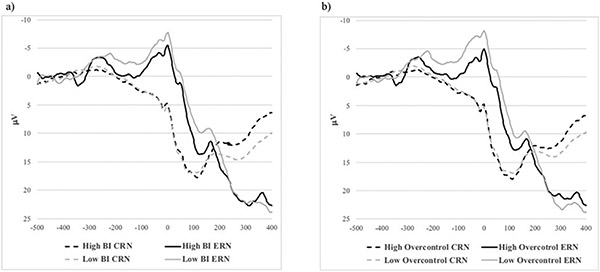
Both reaction time and errors were significant in Step 1 (F (4,75)=6.16, R=.50, ΔR2=.25, p<.001) in predicting the ERNresid. When BI was added, it was a significant predictor of a more blunted ERNresid (Step 2: F (1,74)=4.00, R=.54, ΔR2=.04, p=.049, f2=−.06). However, when overcontrol was entered in Step 3, only overcontrol significantly predicted a blunted ERNresid (F (1,73)=6.45, R=.59, ΔR2=.06, p=.01, f2=.08; see Supplemental Table 2) and BI was no longer a significant predictor. More errors predicted a more negative CRNresid (Step 1: F (4,75)=4.74, R=.45, ΔR2=.02, p=.002), but neither BI (f2=.02) nor overcontrol (f2=.001) were significant predictors of CRNresid (p’s>.22). See Figure 1 for graphical depiction.
Fig 1.
For graphical depiction, median split on (a) behavioral inhibition (BI) and (b) overcontrol of EEG error and correct responding at electrode Cz, showing blunted error response to errors in high behavioral inhibition and even more so in overcontrol in the −50 to 100ms time window
Overcontrol as Mediator of the Relationship Between ERN and Anxiety and Obsessive-compulsive presentations
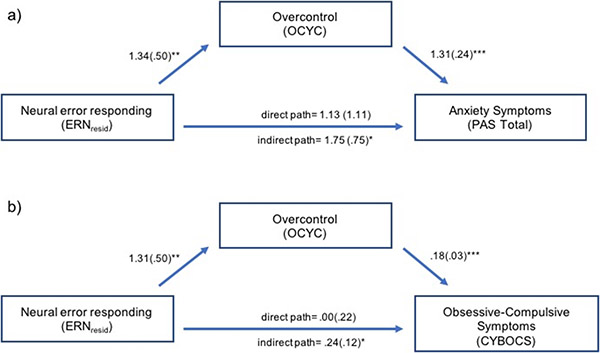
We then examined whether overcontrol was a plausible mediator of the relationships between the ERNresid and anxiety symptoms and the ERNresid and OCD symptoms, controlling for child age, gender and BI (see Figure 2). Above covariates, the ERNresid predicted overcontrol, which in turn was associated with higher anxiety symptoms and the indirect effect (mediation) was significant (Indirect effect: β(SE)=1.75(.75), 95% CI= .34 - 3.27). Similarly, above covariates, the ERNresid predicted overcontrol, which in turn was associated with increased sum obsessions and compulsions and the indirect effect (mediation) was significant (Indirect effect: β(SE)=.24(.12), 95% CI= .04 - .50). Testing this relationship with clinician administered KSADS-EC overcontrol-related anxiety disorder status (yes/no), we found above covariates, the same pattern of results emerged: the ERNresid was associated with overcontrol which again was associated with a higher likelihood of having a clinically diagnosed anxiety disorder (indirect effect: β(SE)=.28(4.43), 95% CI= .04 - .79). Finally, to test directionality of the plausible mediational relationship, we completed two tests of specificity. First, we tested whether the ERNresid mediated the relationship between overcontrol and 1) anxiety and 2) OCD symptoms. Above covariates, overcontrol predicted a blunted ERNresid, (anxiety and OCD: β(SE)=.06(.02), p=.01), although the ERNresid did not predict anxiety (coeff=1.13(1.11), p=.31) or OCD (β(SE)=.00(.22), p=.98) symptoms and the indirect effects were within the 95% CI and thus not significant (PAS anxiety: β(SE)=.07(.06), 95% CI: −.02 - .21; CYBOCS obsessions and compulsions: β(SE)=.00(.01), 95% CI: −.02 - .02). Second, we tested whether BI mediated the relationship between the ERNresid and 1) anxiety and 2) OCD symptoms. Above covariates, the ERNresid did not predict BI (anxiety: β(SE)=1.24(3.90), p=.75; OCD: β(SE)=1.36(3.85), p=.72), BI did predict anxiety (β(SE)=.14(.03), p<.001), but not OCD (β(SE)=.01(.01), p=.23), and the indirect effects were within the 95% CI and thus not significant (PAS anxiety: β(SE)=.18(.65), 95% CI: −.99 - 1.62; CYBOCS obsessions and compulsions: β(SE)=.01(.04), 95% CI: −.06 - .14).
Fig 2.
Overcontrol mediates the relationship between the ERNresid and Anxiety (a) and OCD (b) Symptoms (n=82), controlling for age, gender, and behavioral inhibition
Note: ERNresid= Residualized ERN regressing out the CRN. PAS= Preschool Anxiety Scale Total Score; CYBOCS= Child Yale Brown Obsessive Compulsive Symptoms Sum Score. *95% Confidence Intervals; **p<.01; ***p<.001
Discussion
We tested the independent roles of BI and overcontrol in relation to cognitive control functioning, neural error responding and anxiety and obsessive-compulsive symptoms in 5-6 year old children. BI and overcontrol were both independently associated with worse cognitive shifting and broad anxiety symptoms. Conversely, BI was associated with better inhibitory control while overcontrol was associated with worse inhibitory control and obsessive-compulsive symptoms. Moreover, when included in the same model, only overcontrol predicted neural error responding (ERNresid). Further, the well-established association between the ERN and broad childhood anxiety/OCD symptoms was (cross-sectionally) mediated by overcontrol. Although BI is an important and specific risk factor for childhood anxiety, overcontrol may be an under-explored risk factor evident across both anxiety and obsessive-compulsive presentations. Moreover, overcontrol appears to be a mechanism that associates neural error processing with transdiagnostic anxiety and obsessive-compulsive psychiatric illness.
Replicating past work, BI was associated with worse cognitive shifting and better inhibitory control, both of which act as pathways linking BI to social anxiety (Buzzell et al., 2021). Also replicating previous work, overcontrol was also associated with worse cognitive shifting and worse inhibitory control (Gilbert et al., 2019). Given both BI and overcontrol demonstrated independent associations with poor cognitive shifting abilities, the importance of teaching cognitive flexibility in young anxious and obsessive-compulsive children should be emphasized. Interestingly, although overcontrol in adults has purportedly been characterized by elevated inhibitory control capabilities (Lynch et al., 2018), the current study replicated previous findings in young children (Gilbert et al., 2019) that demonstrated the opposite: worse inhibitory control. This is in contrast to BI, which was associated with better inhibitory control. Further research is warranted on these opposing relationships with inhibitory control, but given better inhibitory control increases risk for social anxiety (Buzzell et al., 2021) while meta-analytic evidence indicates OCD is characterized by heightened error sensitivity and poor inhibitory control (Norman et al., 2018), we speculate that differences in inhibitory control might differentiate BI and overcontrol as independent risk factors. Specifically, although BI and overcontrol are correlated and are commonly co-occur, elevations in one or the other might confer slightly differential risk for social anxiety versus OCD, respectively (i.e., higher levels of BI confers higher risk for social anxiety while higher overcontrol may be more strongly linked with OCD presentations).
BI and overcontrol also demonstrated associations with broad child anxiety symptoms and diagnoses, however, only overcontrol demonstrated independent associations with OCD symptoms. Although BI is consistently one of the best predictors of social anxiety (Clauss & Blackford, 2012), and to a lesser extent broad child anxiety (Sandstrom et al., 2020), overcontrol may impart risk for multiple psychiatric presentations, including social anxiety, broad child anxiety (Gilbert et al., 2019; Gilbert, Perino, et al., 2020) and OCD (Gilbert et al., 2018). Although findings demonstrate a specific relationship between overcontrol and OCD and there is some conceptual overlap between overcontrol and OCD, we do not believe that overcontrol is a restatement of OCD behaviors in young children or a prodrome of the disorder. Overcontrolled tendencies are evident outside of OCD, including in broad childhood anxiety presentations (including social, generalized and separation anxiety; Gilbert, Perino, et al., 2020) and anorexia (Isaksson et al., 2021). As such, we hypothesize that overcontrol is a risk factor of obsessive-compulsive presentations, anorexia, and other anxiety presentations. Of note, social anxiety and OCD often precede and predict risk for anorexia (Anderluh, Tchanturia, Rabe-Hesketh, & Treasure, 2003; Kerr-Gaffney et al., 2018) and so although not feasible to study in the current sample, future studies may elucidate whether overcontrol imparts risk for this developmental progression from anxiety to anorexia.
Taken together, we speculate that overcontrol develops in early childhood and may be an underlying dimensional mechanism that contributes risk for and characterizes a subset of children who develop social anxiety and/or OCD, which over the course of development may lead to a higher risk of developing anorexia. Overcontrol may be especially prominent in youth who exhibit comorbidity between these psychiatric presentations. Indeed, these psychiatric disorders share genetic basis (Yilmaz et al., 2019) and comorbidity of these disorders is associated with greater treatment resistance (Kerr-Gaffney et al., 2018; Simic et al., 2017). In turn, overcontrol could purportedly be an early emerging shared mechanism that contributes to treatment-resistance (Lynch, 2018) if not targeted early in development. Future work would benefit from examining the longitudinal developmental course of overcontrol in relation to onset of social anxiety, OCD and anorexia, as well as comorbidities between these disorders, examining not only the temporal course of the emergence of these disorders but also shared and distinct mechanisms that confer risk for each presentation and whether overcontrol moderates treatment response.
Although BI demonstrated associations with a blunted ERNresid, this relationship was no longer significant when overcontrol was added to the model, and only overcontrol continued to be associated with a blunted ERNresid. First, these findings demonstrate that overcontrol shares a stronger, more direct relationship with the ERN than BI. Overcontrol has previously demonstrated direct associations with aberrant neural error processing (the ERN or fMRI response) (Gilbert et al., 2019; Gilbert, Perino, et al., 2020) and so aberrant responding to errors may represent a core and early-emerging feature of the overcontrolled phenotype. Second, these findings replicated in an independent sample that a blunted ERN is evident in overcontrolled children in this age range (Gilbert et al., 2019). It will be important for future work to follow this ERN-overcontrol association across development to test whether the ‘developmental flip’ from blunted to heightened ERN-anxiety relationship is due to the development of overcontrol and related compensatory cognitive control (Moser, 2017).
Taking this one step further, overcontrol was a plausible mechanism between the well-established relationship of the ERN with anxiety and obsessive-compulsive presentations. The ERN can be reliably assessed in children as young as 3 years (Torpey et al., 2013) while overcontrol purportedly manifests around age 5-6 years. As such, although the current study was cross-sectional, the results were consistent with the possibility that the relationship between the ERN and anxiety and obsessive-compulsive presentations may act through the development of the overcontrolled phenotype. Specifically, in response to early-emerging aberrant error responding (the ERN), perfectionism and checking tendencies central to overcontrol may exacerbate a focus on errors and hence increase psychiatric symptoms. Indeed, the ERN has been speculated to be a transdiagnostic endophenotype (Riesel et al., 2019) and overcontrol may be the mechanistic behavioral process associating this neural marker with anxiety and obsessive-compulsive presentations. However, longitudinal designs are needed to test this hypothesis.
Limitations of the current study should be noted. First, all analyses use cross-sectional data, and therefore there is no temporal precedence in understanding BI and overcontrol relationships or meditational relationships. For mediation, the ordering of constructs was theoretically based (the ERN manifests prior to the overcontrolled phenotype), statistically mediation is not dependent on temporal precedence (Hayes, 2013), and switching the order of variables resulted in a non-significant mediation. However, longitudinal research is imperative to understand the interactive effects of BI, the ERN, and overcontrol on the emergence of psychiatric disorders. Second, the sample size was small and although a community sample, was oversampled for overcontrolled tendencies, limiting generalizability and requiring replication in larger samples. Larger samples assessed repeatedly across development will also allow testing of ongoing developmental processes as well as potential biological sex differences. Although overcontrol has not demonstrated sex differences previously or in the current findings (Gilbert et al., 2019), sex differences are evident in ERN relationships (Ip et al., 2019) and in psychiatric disorders of overcontrol (Smink, van Hoeken, Oldehinkel, & Hoek, 2014; Taylor, 2011). Third, the gold-standard of assessing behavioral inhibition uses observational paradigms, and although the parent-report of BI has been shown to complement observational BI (Kim et al., 2011), future work should examine early observed BI and longitudinal associations with overcontrol. Similarly, the cognitive control measure was parent-based rather than behavioral. Although we looked at a behavioral measure from the go/no-go task (i.e., errors) in preliminary analyses, no associations with overcontrol or BI were found. Future studies should focus on utilizing different measures of cognitive control and accounting for method variance found between various indicators (i.e., possibly combining multiple methods of cognitive functioning by using structural equation modeling to create latent factors).
Clinically, overcontrol may be an under-explored yet highly pertinent risk factor in early childhood. Given overcontrol manifests across multiple psychiatric illnesses that emerge during childhood and adolescence (anxiety, OCD and anorexia), increasing identification and recognition of the overcontrolled phenotype early in development may be important in understanding a transdiagnostic mechanistic risk process independent of BI that is a prime intervention target. Recent psychosocial treatments in adults have effectively targeted overcontrol (Lynch et al., 2013; Lynch et al., 2020) across psychiatric illness, demonstrating that mechanistically targeting overcontrol early in development could lessen the severity and course of comorbid and treatment-resistant psychiatric presentations across the lifespan.
Supplementary Material
Acknowledgments:
We thank the children and caregivers who participated in this research.
Funding:
This work was supported by the National Institute of Mental Health (K23MH115074) to KG.
Footnotes
Conflicts:
The authors have no conflicts of interest to declare.
Ethics Approval:
This study was conducted in line with principles of the Declaration of Helsinki. Institutional Review Board approval was granted at Washington University in St. Louis.
Availability of Data and Material
The data and analytic syntax algorithms that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- Allen KB, Benningfield M, & Blackford JU (2020). Childhood Anxiety—If we know so much, why are we doing so little? JAMA Psychiatry, 77(9), 8870888. doi: 10.1001/jamapsychiatry.2020.0585 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2000). Diagnostic and Statistical Manual of Mental Disorders text revision (4th ed.). Washington DC: American Psychiatric Association. [Google Scholar]
- Anderluh MB, Tchanturia K, Rabe-Hesketh S, & Treasure J (2003). Childhood obsessive-compulsive personality traits in adult women with eating disorders: defining a broader eating disorder phenotype. Am J Psychiatry, 160(2), 242–247. doi: 10.1176/appi.ajp.160.2.242 [DOI] [PubMed] [Google Scholar]
- Asendorpf JB, Borkenau P, Ostendorf F, & Van Aken MAG (2001). Carving personality description at its joints: Confirmation of three replicable personality prototypes for both children and adults. European Journal of Personality, 15(3), 169–198. doi: 10.1002/per.408.abs. [DOI] [Google Scholar]
- Bishop G, Spence SH, & Mcdonald C (2003). Can parents and teachers provide a reliable and valid report of behavioral inhibition. Child Development, 74(6), 1899–1917. [DOI] [PubMed] [Google Scholar]
- Buzzell GA, Morales S, Bowers ME, Troller-Renfree SA-O, Chronis-Tuscano A, Pine DS, … Fox NA (2021). Inhibitory control and set shifting describe different pathways from behavioral inhibition to socially anxious behavior. Developmental Science, 24(1). doi: 10.1111/desc.13040 [DOI] [PubMed] [Google Scholar]
- Carrasco M, Harbin SM, Nienhuis JK, Fitzgerald KD, Gehring WJ, & Hanna GL (2013). Increased error-related brain activity in youth with obsessive-compulsive disorder and unaffected siblings. Depression and Anxiety, 30(1), 39–46. doi: 10.1002/da.22035 [DOI] [PubMed] [Google Scholar]
- Cederlöf M, Thornton LM, Baker J, Lichtenstein P, Larsson H, Rück C, … Mataix-Cols D (2015). Etiological overlap between obsessive-compulsive disorder and anorexia nervosa: A longitudinal cohort, multigenerational family and twin study. World Psychiatry, 14(3), 333–338. doi: 10.1002/wps.20251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clauss JA, Avery SN, & Blackford JU (2015). The nature of individual differences in inhibited temperament and risk for psychiatric disease: A review and meta-analysis. Progress in neurobiology, 127, 23–45. doi: 10.1016/j.pneurobio.2015.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clauss JA, & Blackford JU (2012). Behavioral inhibition and risk for developing social anxiety disorder: A meta-analytic study. Journal of American Academy of Child and Adolescent Psychiatry, 51(10), 1066–1075. doi: 10.1016/j.jaac [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg N, Spinrad TL, & Eggum ND (2010). Emotion-related self-regulation and its relation to children's maladjustment. Annual Review of Clinical Psychology, 6, 495–525. doi: 10.1146/annurev.clinpsy.121208.131208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox NA, Buzzell GA, Morales S, Valadez EA, Wilson M, & Henderson HA (2021). Understanding the Emergence of Social Anxiety in Children With Behavioral Inhibition. Biological Psychiatry, 89(7), 681–689. doi: 10.1016/j.biopsych.2020.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox NA, Henderson HA, Marshall PJ, Nichols KE, & Ghera MM (2005). Behavioral inhibition: Linking biology and behavior within a developmental framework. Annu Rev Psychol, 56, 235–262. doi: 10.1146/annurev.psych.55.090902.141532 [DOI] [PubMed] [Google Scholar]
- Gaffrey MS, & Luby JL (2012). Kiddie-Schedule for Affective Disorders and Schizophrenia - Early Childhood Version (K-SADS-EC). St. Louis, MO: Washington University School of Medicine. [Google Scholar]
- Gehring WJ, Liu Y, Orr JM, & Carp J (2012). The error-related negativity (ERN/Ne). In Luck SJ & Kappenman ES (Eds.), The Oxford Handbook of Event-Related Potential Components (pp. 231–291). New York: Oxford University Press. [Google Scholar]
- Gilbert KE, Barch DM, & Luby J (2019). The Overcontrol in Youth Checklist: Validation of a behavioral measure of overcontrol in preschool aged children Child Psychiatry and Human Development, 51(1), 27–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert KE, Barclay ME, Tillman R, Barch DM, & Luby JL (2018). Associations of observed performance monitoring during preschool with obsessive-compulsive disorder and anterior cingulate cortex volume over 12 years. JAMA Psychiatry, 75(9), 940–948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert KE, Hall K, & Codd RT (2020). Radically Open Dialectical Behavior Therapy: Social Signaling, Transdiagnostic Utility and Current Evidence. Psychology research and behavior management, 13, 19–28. doi: 10.2147/PRBM.S201848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert KE, Perino MT, Myers MJ, & Sylvester CM (2020). Overcontrol and neural response to errors in pediatric anxiety disorders. Journal of Anxiety Disorders, 72(102224). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert KE, Whalen D, Jackson JJ, Tillman R, Barch DM, & Luby J (2020). Thin slice derived personality types predict longitudinal symptom trajectories. Personality Disorders: Theory Research and Treatment, 12(3), 275–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gioia GA, Espy KA, & Isquith PK (2003). Behavior Rating Inventory of Executive Function-Preschool Version. Lutz, FL: Psychological Assessment Resources. [Google Scholar]
- Gioia GA, Isquith PK, Guy SC, & Kenworthy L (2000). Behavior rating inventory of executive function (BRIEF): a professional manual. Lutz, Florida: Psychological Assessment Resources. [Google Scholar]
- Gladstone GL, Parker GB, Mitchell PB, Wilhelm KA, & Malhi GS (2005). Relationship between self-reported childhood behavioral inhibition and lifetime anxiety disorders in a clinical sample. Depression and Anxiety, 22(3), 103–113. doi: 10.1002/da.20082 [DOI] [PubMed] [Google Scholar]
- Gratton G, Coles MG, & Donchin E (1983). A new method for off-line removal of ocular artifact. Electroencephalography and Clinical Neurophysiology, 55(4), 468–484. doi: 10.1016/0013-4694(83)90135-9 [DOI] [PubMed] [Google Scholar]
- Hayes AF (2013). Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. Ney York, NY: Guilford Press. [Google Scholar]
- Henderson HA, Pine DS, & Fox NA (2015). Behavioral inhibition and developmental risk: a dual-processing perspective. Neuropsychopharmacology, 40(1), 207–224. doi: 10.1038/npp.2014.189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ip KI, Liu Y, Moser J, Mannella K, Hruschak J, Bilek E, … Fitzgerald K (2019). Moderation of the relationship between the error-related negativity and anxiety by age and gender in young children: A preliminary investigation. Developmental Cognitive Neuroscience, 39, 100702. doi: 10.1016/j.dcn.2019.100702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isaksson M, Ghaderi A, Wolf-Arehult M, & Ramklint M (2021). Overcontrolled, undercontrolled, and resilient personality styles among patients with eating disorders. Journal of Eating Disorders, 9(1), 47. doi: 10.1186/s40337-021-00400-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kagan J, Reznick J, Clarke C, Snidman N, & Garcia-Coll C (1984). Behavioral inhibition to the unfamiliar. Child Development, 55, 2212–2225. [Google Scholar]
- Kerr-Gaffney J, Harrison A, & Tchanturia K (2018). Social anxiety in the eating disorders: A systematic review and meta-analysis. Psychological Medicine, 48(15), 2477–2491. doi: 10.1017/S0033291718000752 [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, & Walters EE (2005). Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 617–627. doi: 10.1001/archpsyc.62.6.617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J, Klein DN, Olino TM, Dyson MW, Dougherty LR, & Durbin CE (2011). Psychometric properties of the Bbehavioral inhibition questionnaire in preschool children. Journal of Personality Assessment, 93(6), 545–555. doi: 10.1080/00223891.2011.608756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahat A, Lamm C, Chronis-Tuscano A, Pine DS, Henderson HA, & Fox NA (2014). Early behavioral inhibition and increased error monitoring predict later social phobia symptoms in childhood. Journal of American Academy of Child and Adolescent Psychiatry, 53(4), 447–455. doi: 10.1016/j.jaac.2013.12.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langley AK, Lewin AB, Bergman RL, Lee JC, & Piacentini J (2010). Correlates of comorbid anxiety and externalizing disorders in childhood obsessive compulsive disorder. European Child & Adolescent Psychiatry, 19(8), 637–645. doi: 10.1007/s00787-010-0101-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levinson CA, Zerwas SC, Brosof LC, Thornton LM, Strober M, Pivarunas B, … Bulik CM (2019). Associations between dimensions of anorexia nervosa and obsessive–compulsive disorder: An examination of personality and psychological factors in patients with anorexia nervosa. European Eating Disorders Review, 27(2), 161–172. doi: 10.1002/erv.2635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo SL, Schroder HS, Fisher ME, Durbin CE, Fitzgerald KD, Danovitch JH, & Moser JS (2016). Associations between disorder-specific symptoms of anxiety and error-monitoring brain activity in young children. Journal of Abnormal Child Psychology, 45(7), 1439–1448. doi: 10.1007/s10802-016-0247-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch TR (2018). Radically Open dialectical behavior therapy: Theory and practice for treating disorders of overcontrol. Oakland, CA: Context Press. [Google Scholar]
- Lynch TR, Gray KL, Hempel RJ, Titley M, Chen EY, & O'Mahen HA (2013). Radically open-dialectical behavior therapy for adult anorexia nervosa: feasibility and outcomes from an inpatient program. BMC Psychiatry, 13(1), 1–17. doi: 10.1186/1471-244X-13-293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch TR, Hempel RJ, Whalley B, Byford S, Chamba R, Clarke P, … Russell IT (2020). Refractory depression – mechanisms and efficacy of radically open dialectical behaviour therapy (RefraMED): findings of a randomised trial on benefits and harms. The British Journal of Psychiatry, 216(4), 204–212. doi: 10.1192/bjp.2019.53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch TR, Hempel RJ, Whalley B, Byford S, Chambra R, Clarke P, … Russell IT (2018). Radically open dialectical behaviour therapy for refractory depression: the RefraMED RCT. Efficacy Mechanism Evaluation, 5(7). [PubMed] [Google Scholar]
- Meyer A (2017). A biomarker of anxiety in children and adolescents: A review focusing on the error-related negativity (ERN) and anxiety across development. Developmental Cognitive Neuroscience, 27, 58–68. doi: 10.1016/j.dcn.2017.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer A, Carlton C, Chong LJ, & Wissemann K (2019). The presence of a controlling parent is related to an increase in the error-related negativity in 5–7 year-old children. Journal of Abnormal Child Psychology, 47, 935–945. [DOI] [PubMed] [Google Scholar]
- Meyer A, Hajcak G, Torpey-Newman D, Kujawa A, Olino TM, Dyson M, & Klein DN (2018). Early temperamental fearfulness and the developmental trajectory of error-related brain activity. Dev Psychobiol, 60(2), 224–231. doi: 10.1002/dev.21605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer A, Lerner MD, De Los Reyes A, Laird RD, & Hajcak G (2017). Considering ERP difference scores as individual difference measures: Issues with subtraction and alternative approaches. Psychophysiology, 54(1), 114–122. doi: 10.1111/psyp.12664 [DOI] [PubMed] [Google Scholar]
- Moser JS (2017). The nature of the relationship between anxiety and the error-related negativity across development. Current Behavioral Neuroscience Reports, 4(4), 309–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norman LJ, Taylor ST, Liu Y, Radua J, Chye Y, De Wit SJ, … Fitzgerald KD (2018). Error Processing and Inhibitory Control in Obsessive-Compulsive Disorder: A Meta-analysis Using Statistical Parametric Maps. Biological Psychiatry, 85, 713–725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nunnally JC, Bernstein IH, & Berge JMF (1967). Psychometric Theory (Vol. 2). New York: McGraw-Hill. [Google Scholar]
- Pasion R, & Barbosa F (2020). ERN as a transdiagnostic marker of the internalizing-externalizing spectrum: A dissociable meta-analytic effect. Neurosci Biobehav Rev, 103, 133–149. [DOI] [PubMed] [Google Scholar]
- Peris TS, Rozenman M, Bergman RL, Chang S, O'Neill J, & Piacentini J (2017). Developmental and clinical predictors of comorbidity for youth with obsessive compulsive disorder. Journal of Psychiatric Research, 93, 72–78. doi: 10.1016/j.jpsychires.2017.05.002 [DOI] [PubMed] [Google Scholar]
- Pinto A, Greene AL, Storch EA, & Simpson HB (2015). Prevalence of childhood obsessive-compulsive personality traits in adults with obsessive compulsive disorder versus obsessive compulsive personality disorder. J Obsessive Compuls Relat Disord, 4, 25–29. doi: 10.1016/j.jocrd.2014.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Premo JE, Mannella KA, Duval ER, Liu Y, Morrison CL, Moser JS, … Fitzgerald KD (2021). Startle to neutral, not negative stimuli: A neurophysiological correlate of behavioral inhibition in young children. Developmental Psychobiology, 63(5), 1322–1329. doi: 10.1002/dev.22120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riesel A (2019). The erring brain: Error-related negativity as an endophenotype for OCD—A review and meta-analysis. Psychophysiology, 56(4), e13348. doi: 10.1111/psyp.13348 [DOI] [PubMed] [Google Scholar]
- Riesel A, Goldhahn S, & Kathmann N (2016). Hyperactive performance monitoring as a transdiagnostic marker: Results from health anxiety in comparison to obsessive-compulsive disorder. Neuropsychologia, 96, 1–8. doi: 10.1016/j.neuropsychologia.2016.12.029 [DOI] [PubMed] [Google Scholar]
- Riesel A, Klawohn J, Grützmann R, Kaufmann C, Heinzel S, Bey K, … Kathmann N (2019). Error-related brain activity as a transdiagnostic endophenotype for obsessive-compulsive disorder, anxiety and substance use disorder. Psychological Medicine, 49(7), 1207–1217. doi: 10.1017/S0033291719000199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robins RW, John OP, Caspi A, Moffitt TE, & Stouthamer-Loeber M (1996). Resilient, overcontrolled, and undercontrolled boys: Three replicable personality types. Journal of Personality and Social Psychology, 70(1), 157–171. doi: 10.1037/0022-3514.70.1.157 [DOI] [PubMed] [Google Scholar]
- Sandstrom A, Uher R, & Pavlova B (2020). Prospective Association between Childhood Behavioral Inhibition and Anxiety: a Meta-Analysis. Research on Child and Adolescent Psychopathology, 48(1), 57–66. doi: 10.1007/s10802-019-00588-5 [DOI] [PubMed] [Google Scholar]
- Scahill L, Riddle MA, McSwiggin-Hardin M, Ort SI, King RA, Goodman WK, … Leckman JF (1997). Children's Yale-Brown Obsessive Compulsive Scale: Reliability and Validity. Journal of the American Academy of Child & Adolescent Psychiatry, 36(6), 844–852. doi: 10.1097/00004583-199706000-00023 [DOI] [PubMed] [Google Scholar]
- Selya AS, Rose JS, Dierker LC, Hedeker D, & Mermelstein RJ (2012). A Practical Guide to Calculating Cohen’s f(2), a Measure of Local Effect Size, from PROC MIXED. Frontiers in Psychology, 3, 111–111. doi: 10.3389/fpsyg.2012.00111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simic M, Anderson LK, Berner LA, Peck SK, Hunt K, Kaye WH, & Eisler I (2017). When family therapy isn't enough: New treatment directions for highly anxious and dysregulated adolescents with anorexia nervosa. In Innovations in family therapy for eating disorders: Novel treatment developments, patient insights, and the role of carers. (pp. 113–131). New York, NY, US: Routledge/Taylor & Francis Group. [Google Scholar]
- Smink FRE, van Hoeken D, Oldehinkel AJ, & Hoek HW (2014). Prevalence and severity of DSM-5 eating disorders in a community cohort of adolescents. International Journal of Eating Disorders, 47(6), 610–619. doi: 10.1002/eat.22316 [DOI] [PubMed] [Google Scholar]
- Specht J, Luhmann M, & Geiser C (2014). On the consistency of personality types across adulthood: latent profile analyses in two large-scale panel studies. J Pers Soc Psychol, 107(3), 540–556. doi: 10.1037/a0036863 [DOI] [PubMed] [Google Scholar]
- Spence SH, Rapee RM, McDonald CG, & Ingram M (2001). The structure of anxiety symptoms among preschoolers. Behavior Research and Therapy, 39(11), 1293–1316. [DOI] [PubMed] [Google Scholar]
- Stein MB (2006). An epidemiologic perspective on social anxiety disorder. Journal of Clinical Psychiatry, 67, 3–8. [PubMed] [Google Scholar]
- Swanson SA, Crow SJ, Le Grange D, Swendsen J, & Merikangas KR (2011). Prevalence and Correlates of Eating Disorders in Adolescents: Results From the National Comorbidity Survey Replication Adolescent Supplement. Archives of General Psychiatry, 68(7), 714–723. doi: 10.1001/archgenpsychiatry.2011.22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szenczy AK, Levinson AR, Hajcak G, Bernard K, & Nelson BD (2021). Reliability of reward- and error-related brain activity in early childhood. Developmental Psychobiology, 63, e22175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S (2011). Early versus late onset obsessive–compulsive disorder: Evidence for distinct subtypes. Clinical Psychology Review, 31(7), 1083–1100. doi: 10.1016/j.cpr.2011.06.007 [DOI] [PubMed] [Google Scholar]
- Torpey DC, Hajcak G, Kim J, Kujawa AJ, Dyson MW, Olino TM, & Klein DN (2013). Error-related brain activity in young children: associations with parental anxiety and child temperamental negative emotionality. J Child Psychol Psychiatry, 54(8), 854–862. doi: 10.1111/jcpp.12041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Udo T, & Grilo CM (2018). Prevalence and Correlates of DSM-5-Defined Eating Disorders in a Nationally Representative Sample of U.S. Adults. Biological Psychiatry, 84(5), 345–354. doi: 10.1016/j.biopsych.2018.03.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vreeke LJ, & Muris P (2012). Relations Between Behavioral Inhibition, Big Five Personality Factors, and Anxiety Disorder Symptoms in Non-Clinical and Clinically Anxious Children. Child Psychiatry & Human Development, 43(6), 884–894. doi: 10.1007/s10578-012-0302-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeung N, & Summerfield C (2012). Metacognition in human decision-making: confidence and error monitoring. Philosophical transactions of the Royal Society of London. Series B, Biological sciences, 367(1594), 1310–1321. doi: 10.1098/rstb.2011.0416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yilmaz Z, Halvorsen M, Bryois J, Yu D, Eating disorders working group of the psychiatric genomics consortium, T. S. O.-C. d. w. g. o. t. P. G. C., Thornton LM, … Crowley JJ (2019). Examination of the shared genetic basis of anorexia nervosa and obsessive compulsive-disorder. Molecular Psychiatry, 35(9), 2036–2046. doi: 10.1038/s41380-018-0115-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.