Abstract
Robot-assisted surgery (RAS) continues to grow globally. Despite this, in the UK and Ireland, it is estimated that over 70% of surgical trainees across all specialities have no access to robot-assisted surgical training (RAST). This study aimed to provide educational stakeholders guidance on a pre-procedural core robotic surgery curriculum (PPCRC) from the perspective of the end user; the surgical trainee. The study was conducted in four Phases: P1: a steering group was formed to review current literature and summarise the evidence, P2: Pan-Specialty Trainee Panel Virtual Classroom Discussion, P3: Accelerated Delphi Process and P4: Formulation of Recommendations. Forty-three surgeons in training representing all surgical specialties and training levels contributed to the three round Delphi process. Additions to the second- and third-round surveys were formulated based on the answers and comments from previous rounds. Consensus opinion was defined as ≥ 80% agreement. There was 100% response from all three rounds. The resulting formulated guidance showed good internal consistency, with a Cronbach alpha of > 0.8. There was 97.7% agreement that a standardised PPCRC would be advantageous to training and that, independent of speciality, there should be a common approach (95.5% agreement). Consensus was reached in multiple areas: 1. Experience and Exposure, 2. Access and context, 3. Curriculum Components, 4 Target Groups and Delivery, 5. Objective Metrics, Benchmarking and Assessment. Using the Delphi methodology, we achieved multispecialty consensus among trainees to develop and reach content validation for the requirements and components of a PPCRC. This guidance will benefit from further validation following implementation.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11701-022-01518-2.
Keywords: Robotic surgery, Robot-assisted surgery, Training, Curriculum, Delphi method
Introduction
The adoption of robotic-assisted surgery (RAS) across multiple surgical specialities continues to expand globally. Between 2018 and 2019, there was a 20% increase in hospital acquisition of the Da Vinci robot and with growth sustained throughout the COVID-19 pandemic [1–3]. With the development of robotic technology, the surgical robotics market is expected to grow to a value of £18 billion by 2025 [4]. This increased adoption of robotic technology has coincided with the emergence of several new robotic surgery systems entering clinical practice including CMR Surgical’s ‘Versius’ robot and Medtronic’s ‘Hugo’ robot. In the United Kingdom (UK) between 2000 and 2019 Lam et al. [5] demonstrated that around 25% of NHS trusts had a robotic platform and in the same time frame the number of cases performed robotically increased by 400%. Following this study there has been a landmark £20 m investment by NHS Scotland [6] and a further £18 m by NHS Wales into robotics platforms [7].
Despite this expansion and increasing adoption of RAS in clinical practice recognising the perceived benefits of improved dexterity, ergonomics and improved anatomical access [8], surgical trainee exposure to robotic-assisted surgical training (RAST) is limited. It is estimated that > 70% of current UK and Irish surgical trainees have had no access to any form of robotic surgery during their surgical training to date [9, 10]. This same cohort of trainees, however, do place significant value on RAST prior to completion of training as they feel it will be important for their future consultant practice and they would support its incorporation into the UK and Irish surgical training curriculae [11–13]. As with any new technology, appropriate training to safeguard patients and optimise outcomes is crucial but with the increasing adoption of robotic surgery, there is a clear requirement for safe and standardised RAST during surgical training.
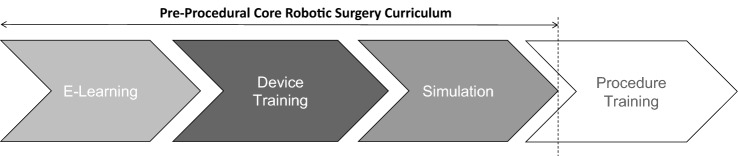
Training in robotic surgery can generally be divided into four sequential stages: e-learning, device training, simulation and finally procedure training (Fig. 1). In current surgical practice, RAST is significantly industry led and focused on procedure-based training for consultant and senior stage surgical trainees and fellows and design of RAST has been replete of trainee stakeholder input [11].
Fig. 1.
There was 95.3% agreement that following successful completion of core robotic surgery training, a trainee should be able to proceed to procedural training in their preferred specialty
Furthermore, basic skills training requires access to hardware and has historically been industry driven, while procedural focused training has been curtailed by the lack of expertise from UK and Ireland surgical trainers or replete of trainee surgeon consultation [9, 10, 13, 14]. However, with increasing adoption of robotic surgery and requirement for robotic proficient surgeons in the future there is a requirement to increase surgical trainee literacy, knowledge and skills in robotic surgery through structured and validated training at all stages of training, so that trainees are appropriately skilled and prepared for procedure-based training when that opportunity arises [15]. This form of a pre-procedural core robotic surgery training to proficiency level in basic robotic skills training can be pan-specialty relevant and appropriate for integration in parallel to current surgical training structures [16]. Current Specialty Training curricula in the UK and Ireland do not reference the role or requirement for RAST in surgical training [17]. The aim of this Delphi process was to explore surgical trainee consensus on the requirement for and components of, a pre-procedural core robotic surgery curriculum (PPCRC) for use in current surgical training in the UK and Ireland.
Methodology
This Delphi consensus consisted of four phases, where each phase informed the subsequent phase. The Delphi method is a well-established approach to answering a research question through the identification of a consensus view across subject experts—in this instance surgical trainees in elected speciality positions. It allows for reflection among participants, who are able to reconsider their opinion based on the anonymised opinions of their peers [18].
Available evidence was reviewed which informed pan-specialty trainee panel discussion to develop the Delphi consensus questionnaire. Finally, an accelerated Delphi process was delivered to formulate these guidance and recommendations. Descriptive statistics describing demographics were performed using Stata/SE16 (Stata Corp, UK).
Phase 1: Evidence acquisition
A steering group was formed consisting of trainee representatives, a robotic surgeon and robotic surgery trainer to review and summarise the current evidence base for RAST curriculae across all surgical specialities through review of peer-reviewed publications, association guidelines and industry published literature.
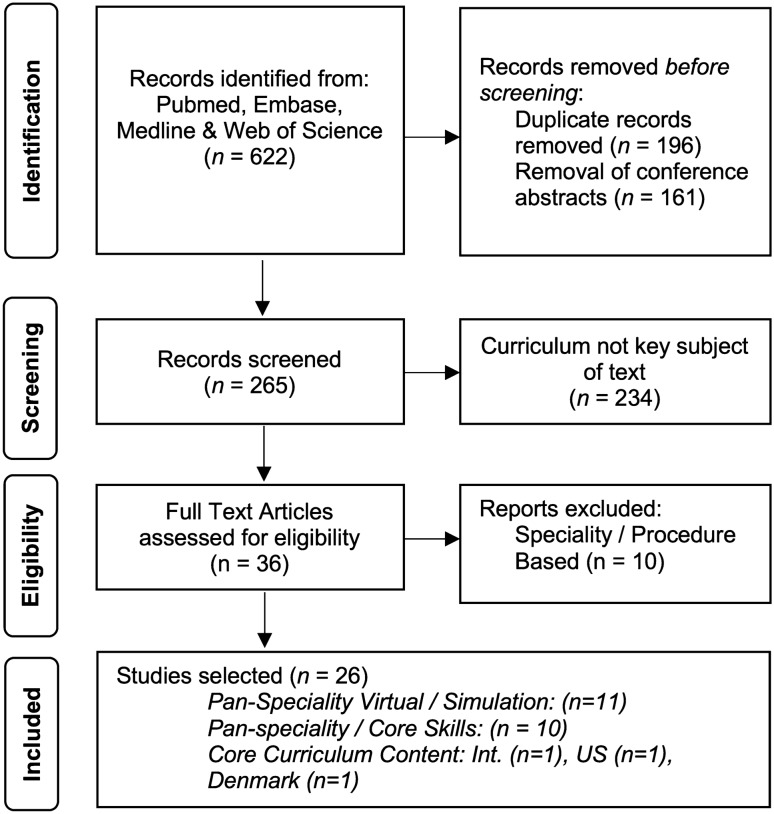
A systematic review of the current literature and was completed independently by three individuals (JB, CF and JC). The systematic review was not registered with PROSPERO as it does not meet the registration criteria but is reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement [19]. The authors reviewed current published literature on PubMed, EMBASE, and Web of Science databases for full-text English-language articles published between 1995 and 2020, using the keywords “Robotic” OR “Robot-assisted”, AND “Surgery” OR “Surgical” AND “Curriculum” OR “Programme”. Additional significant studies cited in the reference list of selected papers were evaluated. The reviewers independently selected papers for detailed review after evaluating the abstract and, if necessary, the full-text manuscript. Potential discrepancies were resolved by open discussion. The electronic search yielded a total of 622 potential articles. Figure 2 summarises the selection process.
Fig. 2.
PRISMA flow diagram summarising the study selection process. PRISMA Preferred Reporting Items for Systematic Reviews and Meta-analyses
Multiple prospective studies were identified, which made recommendations as to the contents of a generic robotics curriculum [20–44]. Overall, the quality of available studies was moderate to low reported as per the GRADE quality assessment framework [45]. Available evidence consists largely of expert opinion, consensus statements, and small qualitative studies. One opinion piece and was identified that focused specifically on a PPCRC in the UK and Ireland [43] and one international consensus piece with limited trainee involvement [46]. Twenty-six articles were selected by the core team and placed into five categories to inform discussion on Access and Context (n = 6), Experience and Exposure to Robotic Surgery (n = 8), Curriculum Components (n = 22), Objective Metrics (n = 13), Benchmarking and Assessment (n = 21). Eighteen papers were considered in more than one category.
Phase 2: Pan-specialty trainee panel virtual classroom discussion
43 Trainees in elected trainee representative roles covering all surgical specialties from the council of The Association of Surgeon of Training (ASiT) were invited and agreed to participate. This participating group represented all surgical specialties and all levels of surgical training from medical student to post-Certification of Completion Training (CCT) fellow. ASiT is the largest trainee organisation in the UK and Ireland representing over 4500 members from all 15 trainee speciality associations, grades and training regions and is a registered charity (1,196,477). This panel of surgical trainee stakeholders convened and discussed the themes identified in Phase 1 over two 1.5-h structured discussion sessions.
This was conducted through audio and visual recording of presentation, mini-poll and open discussion using the UCL Virtual Software Platform (University College London, London) [47]. Given the study was run during the COVID-19 pandemic participants were asked to rate the impact of the pandemic on their current training using a Likert scale of 0 (No Disruption) to 5 (Significant Disruption) as an indication of general disruption to current surgical training which could influence opinion on surgical training as a whole.
Phase 3: Internet survey and accelerated Delphi process
Following Phase 2, an accelerated Delphi methodology was used to quantify consensus in the participating group. This was performed electronically using Google Forms (Google, USA). The Delphi was generated fallowing a qualitative content-analysis [48] (performed by JB and CF) of Phase 2 recordings and distributed to all Phase 2 panel members. Delphi content was divided into 7 Sections as follows: (1) Demographics, (2) Access and Context (3) Experience and Exposure to Robotic Surgery, (4) Relevance to Individual, (5) Curriculum Components, (6) Target Groups and Delivery, (7) Objective Metrics, Benchmarking and Assessment (Supplementary Material 1). An accelerated three round electronic consensus exercise, over three consecutive days (planned a priori), using the Delphi methodology was then conducted [49]. Participants were asked to indicate their ‘agreement/disagreement’ with the proposed themes and criteria generated during Phase 2. Survey items with ≥ 80% consensus were removed from the subsequent round of the survey with the consensus threshold achieved disseminated to all participants. Repeated iterations of anonymous voting continued over three rounds, where an individual’s vote in the next round was informed by knowledge of the panel’s results in the previous round. For inclusion in the final recommendations, each survey item had to have reached group consensus (≥ 80% agreement) by the end of the three survey rounds (Supplementary Material 2—> 1). Items that did not achieve consensus were also discussed in Phase 4.
Phase 4: Generation of recommendations
The study steering group summarised and reported the recommendations within this manuscript based on the consensus results of the Delphi process. The authorship of this paper is comprised of ASiT, The Royal College of Surgeons of England Robotics and Digital Surgery (RADAR) committee and Health Education England and Industry representatives who support the recommendations. Those Phase 3 items which did not reach consensus and are not included in the recommendations but were felt to be important by the steering group have been taken forward in further qualitative work by Health Education England and RCS England.
Results
A 100% (43/43) response rate was received from participants in all three rounds. Following conclusion of the three rounds of the Delphi process 97 of 151 items achieved consensus (≥ 80% agreement or disagreement). There was 97.7% agreement that a standardised PPCRC would be advantageous to training and that independent of speciality, there should be a common approach (95.5% agreement). Tables 1, 2, 3, 4, 5 summarise the five themes identified when considering a PPCRC and detail those statement which reached 80–100% agreement using the Delphi process and the levels of agreement reached. A comprehensive list of all statements can be found in supplementary tables.
Table 1.
Statements achieving consensus in the ‘Experience and Exposure to Robotic Surgery’ theme (n = 7)
| Item | Statement | Agree (%) | Disagree (%) | Achieved consensus | Round achieved |
|---|---|---|---|---|---|
| Experience and Exposure to Robotic Surgery | |||||
| 1 | Robotic surgery can support an increase in delivery of minimally invasive surgery | 95.5 | 4.5 | Yes | 1 |
| 2 | Robotic surgery can enable microsurgical techniques in surgery | 97.7 | 2.3 | Yes | 1 |
| 3 | Robotic surgery can enable automated data collection on individual surgical performance | 93.0 | 7.0 | Yes | 1 |
| 5 | Robotic surgery will be relevant to your preferred speciality | 95.3 | 4.7 | Yes | 1 |
| 6 | You foresee robotic surgery as part of your future consultant practice | 81.4 | 18.6 | Yes | 2 |
| Integration of robotic surgery training could have a negative impact on your overall surgical training due to | |||||
| 7.1 | Consultants still on robotic learning curve resulting in less learning opportunities | 86.0 | 14.0 | Yes | 2 |
| 7.5 | Compete with more valuable learning opportunities in current training environment | 18.6 | 81.4 | Yes | 1 |
Numbers in bold represent > 80% consensus
Table 2.
Statement achieving consensus in the ‘Access and Context’ theme (n = 12)
| Item | Statement | Agree (%) | Disagree (%) | Achieved consensus | Round achieved |
|---|---|---|---|---|---|
| Access and context | |||||
| 8 | Where robotic surgery training is not available in all hospitals, a deanery/regional-based structure should be established for delivering training in robotic surgery to increase access | 95.3 | 4.7 | Yes | 1 |
| 9 | Where robotic surgery training is available in hospitals, a deanery/regional-based structure should be established for delivering training in robotic surgery and further increase access | 83.7 | 16.3 | Yes | 1 |
| 10 | Monthly access to a regional hub for core robotic surgery training is reasonable | 86.0 | 14.0 | Yes | 2 |
| 11 | Regional hubs should be supervised by robotic surgery trainers if they were an option | 93.0 | 7.0 | Yes | 1 |
| 12 | Individual robotic surgery trainers should be accredited | 93.0 | 7.0 | Yes | 1 |
| 13 | Training centres and training hospitals should be assessed and accredited via a recognised education entity, like a royal college or society | 90.7 | 9.3 | Yes | 1 |
| Deanery/regional base approach to robotic surgery training should comprise | |||||
| 14.1 | Device training in regional hub | 86.0 | 14.0 | Yes | 1 |
| During which times should trainees attend regional hubs if they were available through | |||||
| 15.1 | Time-tables as part of working day | 88.4 | 11.6 | Yes | 2 |
| 15.2 | Approved educational leave | 81.4 | 18.6 | Yes | 3 |
| 15.3 | Zero days | 4.7 | 95.3 | Yes | 1 |
| 15.4 | Free time | 4.7 | 95.3 | Yes | 1 |
| A reasonable distance to travel to a regional hub is | |||||
| 17.1 | < 20 km | 27.9 | 72.1 | – | – |
| 17.2 | < 50 km | 83.7 | 16.3 | Yes | 3 |
| 17.3 | < 100 km | 2.3 | – | – | – |
Numbers in bold represent > 80% consensus
Table 3.
Statement achieving consensus in the ‘Curriculum Components’ theme (n = 41)
| Item | Statement | Agree (%) | Disagree (%) | Achieved Consensus | Round achieved |
|---|---|---|---|---|---|
| Curriculum components | |||||
| Components of a core robotic surgery curriculum should include | |||||
| 18.1 | Virtual simulation training and e-learning | 90.7 | 9.3 | Yes | 1 |
| 18.2 | Baseline evaluation | 83.7 | 16.3 | Yes | 2 |
| 18.3 | Device training | 88.4 | 11.6 | Yes | 1 |
| 18.4 | Dry lab training | 86.0 | 14.0 | Yes | 1 |
| 18.8 | History of robotics | 18.6 | 81.4 | Yes | 1 |
| 18.9 | Live operating | 16.3 | 83.7 | Yes | 1 |
| 19 | Division of robotic surgery training into different progressive phases to include: e-learning, device training, basic skills and procedural training is an effective approach | 95.3 | 4.7 | Yes | 1 |
| 20 | A core robotic surgery curriculum should include: e-learning, device training and basic skills | 97.7 | 2.3 | Yes | 1 |
| 21 | Following successful completion of core robotic surgery training, a trainee should be able to proceed to procedural training in their preferred specialty | 95.3 | 4.7 | Yes | 1 |
| 22 | All training should include objective metrics to assess progression to a defined level | 97.7 | 2.3 | Yes | 1 |
| 23 | Core robotic surgery training should be linked to proficiency-based progression, with 'bench marking' of pass/fail levels? | 86.0 | 14.0 | Yes | 2 |
| 24 | Trainees benefit from validated objective scoring systems to provide consistent feedback | 93.0 | 7.0 | Yes | 1 |
| 25 | Benchmarking of an acceptable standard of performance for trainees should be defined within the curriculum | 88.4 | 11.6 | Yes | 1 |
| 26 | Trainees should pass core robotic training before commencing advanced procedural training | 95.3 | 4.7 | Yes | 1 |
| 27 | All training should include baseline evaluation for assessment of training needs | 93.0 | 7.0 | Yes | |
| 28 | Baseline evaluation could enable different entrance levels to the core training, that takes into account the individuals current exposure to robotic surgery training | 86.0 | 14.0 | Yes | 1 |
| 29 | For novice trainees, online e-learning and completion of a baseline evaluation should be a pre-requisite proceeding to 'practical' core robotic training in the form of device training and basic skills | 81.4 | 18.6 | Yes | 1 |
| Baseline evaluation should include | |||||
| 30.1 | VR Simulation modules | 83.7 | 16.3 | Yes | 1 |
| E-learning should include | |||||
| 31.1 | Description of hardware in various systems | 90.7 | 9.3 | Yes | 1 |
| 31.2 | Info on patient selection and preparation | 86.0 | 14.0 | Yes | 1 |
| 31.3 | Info on trouble shooting | 90.7 | 9.3 | Yes | 1 |
| 31.4 | How to dock | 93.0 | 7.0 | Yes | 1 |
| 31.8 | History and development of robotic surgery | 18.6 | 81.4 | Yes | 1 |
| Technical core robotic skills training should include | |||||
| 32.1 | Two-handed movements | 97.7 | 2.3 | Yes | 1 |
| 32.2 | Camera direction | 97.7 | 2.3 | Yes | 1 |
| 32.3 | Basic movements | 95.3 | 4.7 | Yes | 1 |
| 32.4 | Tissue dissection | 81.4 | 18.6 | Yes | 1 |
| 32.5 | Knot tying | 83.7 | 16.3 | Yes | 1 |
| 33 | Formal device training should be mandatory in a core robotic surgery curriculum | 90.7 | 9.3 | Yes | 1 |
| 34 | Training on each type of robotic surgery device is required before operating on a patient | 93.0 | 7.0 | Yes | 1 |
| 35 | Non-technical skills training should be a component of a core robotic surgery curriculum | 88.4 | 11.6 | Yes | 1 |
| Non-technical skills should include | |||||
| 36.1 | Situation awareness training | 90.7 | 9.3 | Yes | 1 |
| 36.2 | Operative team training | 86.0 | 14.0 | Yes | 2 |
| 36.3 | Communication | 88.4 | 11.6 | Yes | 2 |
| 36.4 | Emergency scenarios | 83.7 | 16.3 | Yes | 1 |
| 37 | Operative team training should be a component of a core robotic surgery curriculum | 90.7 | 9.3 | Yes | 1 |
| Operative team training should include | |||||
| 38.1 | Docking | 92.9 | 7.1 | Yes | 1 |
| 38.2 | Emergency scenarios | 90.5 | 9.5 | Yes | 1 |
| 38.3 | Bedside assistance | 85.7 | 14.3 | Yes | 1 |
| 39 | Non-technical skills training and team training should be evaluated with a scoring system? | 83.7 | 16.3 | Yes | 3 |
| 40 | Non-technical skills and team training can be sufficiently assessed with NOTSS | 88.4 | 11.6 | Yes | 1 |
Numbers in bold represent > 80% consensus
Table 4.
Statement achieving consensus in the ‘Target Groups and Delivery’ theme (n = 22)
| Item | Statement | Agree (%) | Disagree (%) | Achieved consensus | Round achieved |
|---|---|---|---|---|---|
| Target groups and delivery | |||||
| 41 | A standardised core robotic training curriculum will be advantageous to training | 97.7 | 2.3 | Yes | 1 |
| 42 | Independent of specialty, there should be a common approach for core robotic surgery training | 95.3 | 4.7 | Yes | 1 |
| 43 | A core robotic surgery training programme should bring you to point of procedural training | 88.4 | 11.6 | Yes | 1 |
| A core robotic curriculum should be available to the following | |||||
| 44.1 | Core surgical trainees (or equivalent) | 88.4 | 11.6 | Yes | 1 |
| 44.2 | Registrars (or equivalent) | 97.7 | 2.3 | Yes | 1 |
| 44.3 | Fellows (or equivalent) | 83.7 | 16.3 | Yes | 1 |
| 44.4 | Robot naïve surgeons | 83.7 | 16.3 | Yes | 1 |
| 44.5 | Laparoscopic surgeons | 81.4 | 18.6 | Yes | 1 |
| 44.9 | Foundation year doctors | 16.3 | 83.7 | Yes | 1 |
| A core robotic curriculum should consider the experience of the following | |||||
| 45.1 | Core surgical trainees (or equivalent) | 90.7 | 9.3 | Yes | 1 |
| 45.2 | Registrars (or equivalent) | 95.3 | 4.7 | Yes | 1 |
| 45.3 | Fellows (or equivalent) | 81.4 | 18.6 | Yes | 1 |
| 45.4 | Robot naïve surgeons | 91.4 | 8.6 | Yes | 1 |
| 45.5 | Laparoscopic surgeons | 86.0 | 14.0 | Yes | 1 |
| 45.6 | Open Surgeons | 83.7 | 16.3 | Yes | 1 |
| 45.8 | Extended surgical team | 18.6 | 81.4 | Yes | 1 |
| 45.9 | Foundation year doctors | 14.0 | 86.0 | Yes | 1 |
| 45.10 | Medical student | 7.0 | 93.0 | Yes | 1 |
| 46 | Does robotic surgery only have a role in senior years of training? (Answer—NO) | 90.7 | 9.3 | Yes | 2 |
| 47 | Robotic surgery training should only be delivered post-CCT (Answer—DISAGREE) | 93.0 | 7.0 | Yes | 1 |
| 48 | Training in robotic surgery is beneficial in earlier years of surgical training (Answer—AGREE) | 90.7 | 9.3 | Yes | 1 |
| Training in robotic surgery is beneficial in early years of training due to | |||||
| 50.1 | Familiarity with basic principles in robotics | 83.7 | 16.3 | Yes | 1 |
Numbers in bold represent > 80% consensus
Table 5.
Statement achieving consensus in the ‘Objective Metrics, Benchmarking and Assessment’ theme (n = 15)
| Item | Statement | Agree (%) | Disagree (%) | Achieved consensus | Round achieved |
|---|---|---|---|---|---|
| Objective metrics, benchmarking and assessment | |||||
| 51 | Cases performed robotically should be accepted for indicative numbers for index cases in surgical training | 83.7 | 16.3 | Yes | 1 |
| 52 | Should standard logbook programmes facilitate an option for recording robotic approach to standard surgical procedures | 88.1 | 11.9 | Yes | 1 |
| 53 | Surgical curricula should reference the role of robotic surgery and guide on its place in training | 90.7 | 9.3 | Yes | 1 |
| 54 | Current curricula approved Procedure-Based Assessments (PBAs) should be adjusted (where appropriate) to be suitable to assess robotic approach to index cases | 90.7 | 9.3 | Yes | 1 |
| 55 | Specialty-relevant index procedure PBAs should be completed in simulation prior to live-operating? | 81.4 | 18.6 | Yes | 2 |
| 56 | Completion of core robotic surgery skills training should be considered as an approved surgical training course for certification | 83.7 | 16.3 | Yes | 1 |
| 57 | Trainees should receive a 'sign-off' following completion of core robotic surgery skills | 95.3 | 4.7 | Yes | 1 |
| Final assessment for ‘sign-off’ should include | |||||
| 58.1 | VR simulation modules | 97.7 | 2.3 | Yes | 2 |
| 59 | Core robotic surgery skills training should be formally built into surgical curriculum? | 86.0 | 14.0 | Yes | 2 |
| 60 | Robotic surgery training could have any negative impact on your overall surgical training | 83.7 | 16.3 | Yes | 3 |
| Technical core robotic skills training assessments should include | |||||
| 61.1 | ISCP OBAs | 81.0 | 19.0 | Yes | 1 |
| 61.5 | GEARS | 7.0 | 93.0 | Yes | 1 |
| 62 | Videos should be analysed with a validated standardised objective scoring system | 90.7 | 9.3 | Yes | 1 |
| Scoring systems for video analysis should include | |||||
| 63.5 | ABS operative performance rating | 2.3 | 97.7 | Yes | 1 |
| 63.6 | At least two 'experts' should analyse and review video performance | 81.4 | 18.6 | Yes | 1 |
Numbers in bold represent > 80% consensus
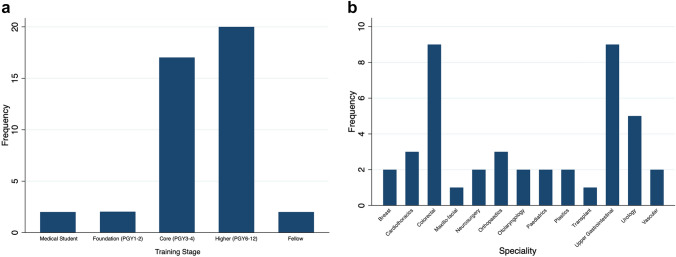
Participant demographics
Forty-three elected surgical trainee representatives participated representing all surgical subspecialties (Fig. 1). 25 (58%) were female and 18 (42%) were male. The majority of participants were higher surgical trainees (39.5%) with all training grades represented (Fig. 3). Three participants (7%) were less than full-time trainees and six (14%) were Academic Trainees. All training regions (Deaneries) were represented with a maximum of five (11.6%) trainees from any given deanery. The mean Likert score of current impact of COVID-19 on training was 3.3 (SD ± 1.5) representing a subjective trainee reported snapshot opinion of the impact of the COVID-19 pandemic on training. 97% of respondents reported that the COVID-19 pandemic had a significant disruption to their training (75% reported severe disruption).
Fig. 3.
Training stage and preferred surgical speciality (n = 43)
Experience and exposure to robotic surgery
There was strong consensus that robotic surgery can support an increase in the delivery of minimally invasive surgery, enable microsurgical techniques, automated data collection and is relevant to future consultant practice across the majority of specialities (Table 1). It was perceived that robotic surgery may have a negative impact on overall surgical training due to current consultant colleague learning curves and through competing with more valuable learning opportunities in the current UK and Ireland training environment. There was no consensus on consultant learning curves effecting training or on the possible negative effect of less complex cases selected for robotic procedures that would have offered ideal open or laparoscopic training opportunities (46.5%).
Access and context
There was clear support for a regional-based training infrastructure, where robotic surgery is not available in all hospitals within said region with access facilitated through timetabling as part of the working day or on approved educational leave. They should not be limited to zero/rest days and trainees personal time Both trainers and training centres should be accredited (Table 2).
Curriculum components
Components of a PPCRC should include a baseline evaluation of skill, e-learning, with device training and basic skills training delivered in various simulation settings, including VR simulation and dry lab training. Division of the curriculum into these phases was deemed an effective approach (Table 3). Following successful completion of core robotics surgery training a trainee should be able to progress onto procedural training in their preferred speciality (Fig. 1). Trainees recognised the importance of non-technical skills and device training within the robotic operating environment. Both live operating and the history of robotics was deemed an unnecessary component of a PPCRC. Emergency scenarios and how to deal with them (72.1%) and suturing (67.4%) failed to achieved consensus but were deemed important by the steering committee in Phase 4. The use of ISCP procedure-based assessments achieved consensus in the first round (81%) supporting that any new curriculum should align with current reporting practices.
Target groups and delivery
A standardised PPCRC would be advantageous to all trainees at or above the level of core surgical training (or equivalent) in the UK and Ireland and exposure should not be limited to only the senior years of the training programme (Table 4).
Objective metrics, benchmarking and assessment
Participants supported that robotic cases should be deemed acceptable for index cases in higher surgical training programmes in the UK and Ireland (Table 5) and logbooks and workplace-based assessments should be updated to reflect this. Completion of core robotics skills training should be included in curriculae and required for completion of training and video assessments should be analysed with a validated, standardised scoring system.
Recommendations
Based on the above findings, the authors make the following recommendations on the requirement and components of PPCRC:
A PPCRC integrating into surgical training in an inclusive and deliverable way would focus on the first three steps of training, not inclusive of procedural training and ensure all trainees receive standardised and validated training in the basics of robotic surgery
A universal PPCRC should focus on three main areas of training: e-learning, device training and simulation (virtual and dry lab).
A formal PPCRC should commence at the level of core surgical trainee or SHO or equivalent level of experience but exposure prior to this stage of trainings to be encouraged.
Assessment standards and ability to progress to procedural-based training should be clearly defined, standardised and validated. It should be collaborative to avoid duplication.
Training requirements in understanding the hardware technology as well as operative technique is required for all individual robotic surgery systems should be included in a PPCRS prior to live operating.
A PPCRC will benefit from a structured, proficiency-based curriculum that incorporates technical and non-technical skills training while interacting with the multi-disciplinary team.
A PPCRC should be aligned to ISCP and crowdsourced feedback should be considered.
Certain components of a PPCRC can be delivered at an individual level; however, robust collaborative local and national level training solutions are required.
Royal Colleges, educational authorities, industry and trainee and trainer stakeholders should all be consulted on the components of a PPCRC.
Discussion
Using the Delphi methodology, we have achieved multispecialty consensus among trainees to develop and reach content validation for the requirements and components of a PPCRC in the UK and Ireland. There was 100% response from all three rounds and 97.7% agreement that a standardised PPCRC would be advantageous to training and that, independent of speciality, there should be a common approach (95.5% agreement).
Global adoption of robotic assisted surgery (RAS) in clinical practice is rapidly growing with clear evidence of this trend in the UK and Ireland [50, 51]. However, the current UK and Ireland Training Speciality curriculae contain no reference or training outcomes specific to RAST and trainee surgeons broadly remain robotic naïve until completion of certificate of training (CCT), where they are then expected to rapidly adopt procedure-based curricula that is significantly industry-driven and ad hoc delivered without universal access [31, 46, 52–56]. This is in direct contrast to training surgeons in the US [57].
The authors and Delphi participants believe that a PPCRC, integrated in parallel to current surgical training structures would improve surgical trainee literacy and skills in robotic surgery and could be delivered universally regardless of geographical location, surgical specialty and stage of training. This in turn would increase training opportunities in robotic surgery training for all surgical trainees and better prepare the future surgical workforce. As the adoption of robotic surgery is exponentially increasing, it is important that there is a mechanism in place to ensure the future consultant workforce have the foundational training required to be able to adapt to both robotics and digital surgery in real-time.
Consensus was reached in multiple areas: 1. Experience and Exposure, 2. Access and context, 3. Curriculum Components, 4 Target Groups and Delivery, 5. Objective Metrics, Benchmarking and Assessment. Trainees should have access to multiple industry e-learning curricula for common clinically integrated systems until a bespoke design of universal e-learning is achieved. Robotic technical skills training should be broken down into a PPCRC and procedural training (Fig. 1). By separating these two aspects we negate some of the limitations to access due to bottle necks in training related to lack of expertise in new technologies. This also fits with a proficiency-based progression approach as procedural training builds on the foundation knowledge and skills from a PPCRC [16]. Acquisition of robotic surgical skills by junior surgical trainees is often hindered by time pressure, financial imperatives and access to both robotic kit and patients undergoing robotic surgery. Robotic simulation training offers an attractive solution, because it allows trainees to learn in a safe, controlled, and standardised environment [58, 59]. Future procedural training will also likely incorporate VR simulation, so this approach also gives exposure to future novel training modalities [60].
Surgical training environments include classroom instruction, e-learning and practical training, in both the operating room and simulation. Surgical training focuses not just on technical and procedural instruction, but also training in non-technical skills, including crisis (emergency) management, decision making, leadership and communication, that benefits the team performance. In robotic surgery it is crucial to successfully complete device training and basic skills training prior to commencing advanced procedural training on patients. By utilising objective scores there are also opportunities for credentialing in robotic surgery that will help further guarantee patient safety through agreed processes of quality control. There is debate around whether this should be achievable (in part of in full) prior to CCT [61, 62].
A proficiency-based progression approach to training with objective metrics and benchmarks will give safety assurances to training. The curricula should be standardised and will require agreement from societies and education of trainers to achieve widespread adoption while delivering consistent content and assessments [16].
Kinematic data or automated performance metrics (APMs) (instrument and endoscopic camera motion tracking and events data, such as energy usage) can be recorded during robotic surgery and can collect large amounts of data, related to the surgeon’s performance. Machine learning, which is a form of artificial intelligence, relies on computer algorithms and large volumes of data to “learn” and recognize broad patterns that are often imperceptible to human reviewers. Machine learning (ML) algorithms have been used to process these large volumes of automatically collected data from robotic surgery and have been shown to correlate with patient outcomes [63]. Objective automated scores of surgical performance have huge potential to assess surgeons, predict patient outcomes and in the near future, give opportunities to personalize surgeon training. However, as the role of AI in healthcare continues to expand there is increasing awareness of the potential pitfalls of AI and the need for guidance to avoid them [64].
Crowdsourced feedback appears to be a cost effective and efficient way to assess surgical performance in procedural training, with results comparable to expert feedback, when assessing technical skills. However, inter-rater reliability is poor and further work is needed to increase consistency in evaluations, to explore sources of discrepant assessments between surgeons and crowds, and to identify optimal populations and novel applications for this technology [65].
It is recognised that robotic training curriculums often focus on technical skills training and lack training in the area of non-technical skills (NTS). For trainees to attain the requisite knowledge and skills to provide safe and effective surgical care, robotic surgical training will benefit from a structured, proficiency-based curriculum that incorporates technical and non-technical skills training. A growing awareness of the importance of cognitive and NTS will encourage further development of NTS training and inclusion in curricula [66].
Limitations
It is important to acknowledge that the data presented in this manuscript is a consensus opinion and not based on previously published evidence. While surgical trainees are significant stakeholders in surgical training and as end users in surgical training are in a unique position to identify solutions and obstacles to practical introduction of robotic surgery training opportunities there are other significant stakeholders that were not involved in this consensus. All participants also understand the current training crisis that we are experiencing in our healthcare systems with 97% of participants reporting a significant disruption to their training. However, there is still an appetite and desire to continue to evolve and ensure that we do continue to grow and develop new and innovative surgical techniques including robotic surgery for the betterment of patient care.
Conclusion
Robotic surgery practice is increasing, therefore, access to standardised and validated training should also increase. It is crucial that surgical trainees are prepared for this practice trend using a defined curriculum with a clear start and end point and appropriate assessment and benchmarking. Using the Delphi methodology, we achieved multispecialty consensus among trainees to develop and reach content validation for the requirements and components of a PPCRC in the UK and Ireland. This guidance will benefit from further validation following implementation.
Supplementary Information
Below is the link to the electronic supplementary material.
Author contributions
All authors contributed to the study conception and design. Material preparation, data collection, running of the Delphi exercise and analysis were performed by the Steering Group: JB, CF, MK and JC. The first draft of the manuscript was written by JB and CF. JB, CF, CES, MK, WB, DH, CM, SB and JWC critically revised the manuscript and agreed on recommendations based on the consensus statements. All authors read and approved the final manuscript.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Data availability
All data is available on request to the corresponding author.
Declarations
Conflict of interest
ASiT has an educational and sponsorship relationship with CMR Surgical. DH has received funding from Intuitive Foundation. Simon Bach receives research funding from Intuitive Surgical Inc, USA. CF is in receipt of a European Society of Coloproctology Robotic Surgery Fellowship, supported by Intuitive Surgical Inc. JWC is an associate medical director at CMR Surgical Ltd, UK.
Consent to participate
Informed verbal consent was obtained from all individual participants who took part in the Delphi.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Joshua Richard Burke, Email: joshburke@doctors.org.uk.
Christina A. Fleming, Email: christina.fleming49@gmail.com
Martin King, Email: martin.king@rcsed.net.
Charlotte El-Sayed, Email: c.el-sayed@nhs.net.
William S. Bolton, Email: W.S.Bolton@leeds.ac.uk
Chris Munsch, Email: chris.munsch@hee.nhs.uk.
Deena Harji, Email: deena_harji@hotmail.com.
Simon P. Bach, Email: S.P.Bach@bham.ac.uk
Justin W. Collins, Email: justin.collins@ucl.ac.uk
References
- 1.Khalid S, Goldenberg M, Grantcharov T, Taati B, Rudzicz F. Evaluation of deep learning models for identifying surgical actions and measuring performance. JAMA Netw Open. 2020;3(3):e201664–e201664. doi: 10.1001/jamanetworkopen.2020.1664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Annual Report 2019 - Intuitive Surgical. Availanble from: https://isrg.gcs-web.com/static-files/31b5c428-1d95-4c01-9c85-a7293bac5e05. Accessed 24 Jan 2023
- 3.Intuitive Announces First Quarter Earnings | Intuitive Surgical. Available from: https://isrg.intuitive.com/news-releases/news-release-details/intuitive-announces-first-quarter-earnings-2
- 4.Global Healthcare Companion Robots Market estimated at. Available from: https://www.globenewswire.com/en/news-release/2022/04/04/2415884/0/en/Global-Healthcare-Companion-Robots-Market-estimated-at-about-3-Billion-2020-is-growing-at-a-CAGR-close-to-20-through-2020-2025.html
- 5.Lam K, Clarke J, Purkayastha S, Kinross JM. Uptake and accessibility of surgical robotics in England. Int J Med Robot. 2021;17(1):1–7. doi: 10.1002/rcs.2174. [DOI] [PubMed] [Google Scholar]
- 6.Surgical robots for NHS Scotland - gov.scot. Available from: https://www.gov.scot/news/surgical-robots-for-nhs-scotland/
- 7.CMR’s surgical robotics help NHS Wales launch world first programme | Business Weekly | Technology News | Business news | Cambridge and the East of England. Available from: https://www.businessweekly.co.uk/news/biomedtech/cmr’s-surgical-robotics-help-nhs-wales-launch-world-first-programme
- 8.Wee IJY, Kuo LJ, Ngu JCY. A systematic review of the true benefit of robotic surgery: Ergonomics. Int J Med Robot Comput Assist Surg MRCAS. 2020 doi: 10.1002/rcs.2113. [DOI] [PubMed] [Google Scholar]
- 9.Fleming CA, Ali O, Clements JM, Hirniak J, King M, Mohan HM, et al. Pan-specialty access to robotic surgery in surgical training. Br J Surg. 2021;108(7):e245–e246. doi: 10.1093/bjs/znab107. [DOI] [PubMed] [Google Scholar]
- 10.Fleming CA, Ali O, Clements JM, Hirniak J, King M, Mohan HM, et al. Surgical trainee experience and opinion of robotic surgery in surgical training and vision for the future: a snapshot study of pan-specialty surgical trainees. J Robot Surg. 2021 doi: 10.1007/s11701-021-01344-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moit H, Dwyer A, De Sutter M, Heinzel S, Crawford D. A Standardized robotic training curriculum in a general surgery program. JSLS. 2019 doi: 10.4293/JSLS.2019.00045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bhakhri K, Harrison-Phipps K, Harling L, Routledge T. Should robotic surgery simulation be introduced in the core surgical training curriculum? Front Surg. 2021;8:42. doi: 10.3389/fsurg.2021.595203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.FOS: TEST Commission. Future of Surgery: Technology Enhanced Surgical Training: Report of the FOS: TEST Commission, August 2022. [Internet]. 2022. 10.1308/FOS2.2022. Available from: https://futureofsurgery.rcseng.ac.uk/training. Accessed 24 Jan 2023 [DOI]
- 14.Harji D, Houston F, Burke J, Griffiths B, Tilney H, Miskovic D, et al. The current status of robotic colorectal surgery training programmes. J Robot Surg. 2022 doi: 10.1007/s11701-022-01421-w. [DOI] [PubMed] [Google Scholar]
- 15.Satava RM, Stefanidis D, Levy JS, Smith R, Martin JR, Monfared S, et al. Proving the effectiveness of the fundamentals of robotic surgery (FRS) skills curriculum: a single-blinded, multispecialty, multi-institutional randomized control trial. Ann Surg. 2020;272(2):384–392. doi: 10.1097/SLA.0000000000003220. [DOI] [PubMed] [Google Scholar]
- 16.Collins JW, Levy J, Stefanidis D, Gallagher A, Coleman M, Cecil T, et al. Utilising the Delphi process to develop a proficiency-based progression train-the-trainer course for robotic surgery training. Eur Urol. 2019;75(5):775–785. doi: 10.1016/j.eururo.2018.12.044. [DOI] [PubMed] [Google Scholar]
- 17.Lund J. The new General Surgical Curriculum and ISCP. Surgery (United Kingdom) Elsevier Ltd; 2020. p. 601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dalkey N, Helmer O. An experimental application of the DELPHI method to the use of experts. Manag Sci. 1963;9(3):458–467. [Google Scholar]
- 19.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;29:372. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Melnyk R, Saba P, Holler T, Cameron K, Mithal P, Rappold P, et al. Design and Implementation of an Emergency Undocking Curriculum for Robotic Surgery. Simul Healthc J Soc Simul Healthc. 2022;17(2):78–87. doi: 10.1097/SIH.0000000000000596. [DOI] [PubMed] [Google Scholar]
- 21.Battaglia E, Mueller B, Hogg D, Rege R, Scott D, Fey AM (2021) Evaluation of pre-training with the da Vinci skills simulator on motor skill acquisition in a surgical robotics curriculum. 10.1142/S2424905X21500069
- 22.Gleason A, Servais E, Quadri S, Manganiello M, Cheah YL, Simon CJ, et al. Developing basic robotic skills using virtual reality simulation and automated assessment tools: a multidisciplinary robotic virtual reality-based curriculum using the Da Vinci Skills Simulator and tracking progress with the Intuitive Learning platform. J Robot Surg. 2022 doi: 10.1007/s11701-021-01363-9. [DOI] [PubMed] [Google Scholar]
- 23.Madion MP, Kastenmeier A, Goldblatt MI, Higgins RM. Robotic surgery training curricula: prevalence, perceptions, and educational experiences in general surgery residency programs. Surg Endosc. 2022 doi: 10.1007/s00464-021-08930-z. [DOI] [PubMed] [Google Scholar]
- 24.Hertz P, Houlind K, Jepsen J, Bundgaard L, Jensen P, Friis M, et al. Identifying curriculum content for a cross-specialty robotic-assisted surgery training program: a Delphi study. Surg Endosc. 2022;36(7):4786–4794. doi: 10.1007/s00464-021-08821-3. [DOI] [PubMed] [Google Scholar]
- 25.Green CA, Chern H, Rogers SJ, Reilly LM, O’Sullivan P. Transforming surgical education through a resident robotic curriculum. Ann Surg. 2021 doi: 10.1097/AS9.0000000000000076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Collins JM, Walsh DS, Hudson J, Henderson S, Thompson J, Zychowicz M. Implementation of a standardized robotic assistant surgical training curriculum. J Robot Surg. 2021 doi: 10.1007/s11701-021-01291-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bric J, Connolly M, Kastenmeier A, Goldblatt M, Gould JC. Proficiency training on a virtual reality robotic surgical skills curriculum. Surg Endosc. 2014;28(12):3343–3348. doi: 10.1007/s00464-014-3624-5. [DOI] [PubMed] [Google Scholar]
- 28.Mariani A, Pellegrini E, De Momi E. Skill-oriented and performance-driven adaptive curricula for training in robot-assisted surgery using simulators: a feasibility study. IEEE Trans Biomed Eng. 2021;68(2):685–694. doi: 10.1109/TBME.2020.3011867. [DOI] [PubMed] [Google Scholar]
- 29.Satava RM, Stefanidis D, Levy JS, Smith R, Martin JR, Monfared S, et al. Proving the effectiveness of the fundamentals of robotic surgery (FRS) skills curriculum: a single-blinded, multispecialty, multi-institutional randomized control trial. Ann Surg. 2020;272(2):384–392. doi: 10.1097/SLA.0000000000003220. [DOI] [PubMed] [Google Scholar]
- 30.Gerull W, Zihni A, Awad M. Operative performance outcomes of a simulator-based robotic surgical skills curriculum. Surg Endosc. 2020;34(10):4543–4548. doi: 10.1007/s00464-019-07243-6. [DOI] [PubMed] [Google Scholar]
- 31.Chen R, Rodrigues Armijo P, Krause C, Siu KC, Oleynikov D. A comprehensive review of robotic surgery curriculum and training for residents, fellows, and postgraduate surgical education. Surg Endosc. 2020;34(1):361–367. doi: 10.1007/s00464-019-06775-1. [DOI] [PubMed] [Google Scholar]
- 32.Tom CM, Maciel JD, Korn A, Ozao-Choy JJ, Hari DM, Neville AL, et al. A survey of robotic surgery training curricula in general surgery residency programs: How close are we to a standardized curriculum? Am J Surg. 2019;217(2):256–260. doi: 10.1016/j.amjsurg.2018.11.006. [DOI] [PubMed] [Google Scholar]
- 33.Raad WN, Ayub A, Huang CY, Guntman L, Rehmani SS, Bhora FY. Robotic thoracic surgery training for residency programs: a position paper for an educational curriculum. Innov Phila Pa. 2018;13(6):417–422. doi: 10.1097/IMI.0000000000000573. [DOI] [PubMed] [Google Scholar]
- 34.Mariani A, Pellegrini E, Enayati N, Kazanzides P, Vidotto M, De Momi E. Design and evaluation of a performance-based adaptive curriculum for robotic surgical training: a pilot study. Annu Int Conf IEEE Eng Med Biol Soc IEEE Eng Med Biol Soc Annu Int Conf. 2018;26(2018):2162–2165. doi: 10.1109/EMBC.2018.8512728. [DOI] [PubMed] [Google Scholar]
- 35.Ko YH, Choi JY, Song PH. Concurrent validation of a robotic simulator curriculum focused on “core” exercises: Does it help overcome baseline skill levels? Int J Urol. 2018;25(8):760–761. doi: 10.1111/iju.13704. [DOI] [PubMed] [Google Scholar]
- 36.Ballas DA, Cesta M, Gothard D, Ahmed R. Emergency undocking curriculum in robotic surgery. Cureus. 2019 doi: 10.7759/cureus.4321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hogg ME, Tam V, Zenati M, Novak S, Miller J, Zureikat AH, et al. Mastery-based virtual reality robotic simulation curriculum: the first step toward operative robotic proficiency. J Surg Educ. 2017;74(3):477–485. doi: 10.1016/j.jsurg.2016.10.015. [DOI] [PubMed] [Google Scholar]
- 38.Gomez PP, Willis RE, Van Sickle KR. Development of a virtual reality robotic surgical curriculum using the da Vinci Si surgical system. Surg Endosc. 2015;29(8):2171–2179. doi: 10.1007/s00464-014-3914-y. [DOI] [PubMed] [Google Scholar]
- 39.Ahmed K, Khan R, Mottrie A, Lovegrove C, Abaza R, Ahlawat R, et al. Development of a standardised training curriculum for robotic surgery: a consensus statement from an international multidisciplinary group of experts. BJU Int. 2015;116(1):93–101. doi: 10.1111/bju.12974. [DOI] [PubMed] [Google Scholar]
- 40.Raza SJ, Froghi S, Chowriappa A, Ahmed K, Field E, Stegemann AP, et al. Construct validation of the key components of Fundamental Skills of Robotic Surgery (FSRS) curriculum—a multi-institution prospective study. J Surg Educ. 2014;71(3):316–324. doi: 10.1016/j.jsurg.2013.10.006. [DOI] [PubMed] [Google Scholar]
- 41.Smith R, Patel V, Satava R. Fundamentals of robotic surgery: a course of basic robotic surgery skills based upon a 14-society consensus template of outcomes measures and curriculum development. Int J Med Robot Comput Assist Surg MRCAS. 2014;10(3):379–384. doi: 10.1002/rcs.1559. [DOI] [PubMed] [Google Scholar]
- 42.Stegemann AP, Ahmed K, Syed JR, Rehman S, Ghani K, Autorino R, et al. Fundamental skills of robotic surgery: a multi-institutional randomized controlled trial for validation of a simulation-based curriculum. Urology. 2013;81(4):767–774. doi: 10.1016/j.urology.2012.12.033. [DOI] [PubMed] [Google Scholar]
- 43.Bhakhri K, Harrison-Phipps K, Harling L, Routledge T. Should robotic surgery simulation be introduced in the core surgical training curriculum? Front Surg. 2021;10(8):42. doi: 10.3389/fsurg.2021.595203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Green CA, Chern H, O’Sullivan PS. Current robotic curricula for surgery residents: a need for additional cognitive and psychomotor focus. Am J Surg. 2018;215(2):277–281. doi: 10.1016/j.amjsurg.2017.09.040. [DOI] [PubMed] [Google Scholar]
- 45.Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–926. doi: 10.1136/bmj.39489.470347.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Smith R, Patel V, Satava R. Fundamentals of robotic surgery: a course of basic robotic surgery skills based upon a 14-society consensus template of outcomes measures and curriculum development. Int J Med Robot Comput Assist Surg MRCAS. 2014;10(3):379–384. doi: 10.1002/rcs.1559. [DOI] [PubMed] [Google Scholar]
- 47.Nathan A, Fricker M, Georgi M, Patel S, Hang MK, Asif A, et al. Virtual interactive surgical skills classroom: a parallel-group, non-inferiority, adjudicator-blinded, randomised controlled trial (VIRTUAL) J Surg Educ. 2022;79(3):791–801. doi: 10.1016/j.jsurg.2021.11.004. [DOI] [PubMed] [Google Scholar]
- 48.Bengtsson M. How to plan and perform a qualitative study using content analysis. NursingPlus Open. 2016;1(2):8–14. [Google Scholar]
- 49.de Villiers MR, de Villiers PJT, Kent AP. The Delphi technique in health sciences education research. Med Teach. 2005;27(7):639–643. doi: 10.1080/13611260500069947. [DOI] [PubMed] [Google Scholar]
- 50.NBOCA Dataset 2021/2022—National bowel cancer audit. Available from: https://www.nboca.org.uk/resources/nboca-dataset-2019-2020/
- 51.Data & Audit Project | The British Association of Urological Surgeons Limited. Available from: https://www.baus.org.uk/professionals/baus_business/data_audit.aspx
- 52.Gomez Ruiz M, Tou S, Matzel KE. Setting a benchmark in surgical training—robotic training under the European School of Coloproctology, ESCP. Colorectal Dis Off J Assoc Coloproctology G B Irel. 2019;21(4):489–490. doi: 10.1111/codi.14592. [DOI] [PubMed] [Google Scholar]
- 53.Petz W, Spinoglio G, Choi GS, Parvaiz A, Santiago C, Marecik S, et al. Structured training and competence assessment in colorectal robotic surgery. Results of a consensus experts round table. Int J Med Robot Comput Assist Surg MRCAS. 2016;12(4):634–641. doi: 10.1002/rcs.1731. [DOI] [PubMed] [Google Scholar]
- 54.Miskovic D, Ahmed J, Bissett-Amess R, Gómez Ruiz M, Luca F, Jayne D, et al. European consensus on the standardization of robotic total mesorectal excision for rectal cancer. Colorectal Dis Off J Assoc Coloproctology G B Irel. 2019;21(3):270–276. doi: 10.1111/codi.14502. [DOI] [PubMed] [Google Scholar]
- 55.Szold A, Bergamaschi R, Broeders I, Dankelman J, Forgione A, Langø T, et al. European Association of Endoscopic Surgeons (EAES) consensus statement on the use of robotics in general surgery. Surg Endosc. 2015;29(2):253–288. doi: 10.1007/s00464-014-3916-9. [DOI] [PubMed] [Google Scholar]
- 56.Herron DM, Marohn M, Advincula A, Aggarwal S, Palese M, Broderick T, et al. A consensus document on robotic surgery. Surg Endosc. 2008;22(2):313–325. doi: 10.1007/s00464-007-9727-5. [DOI] [PubMed] [Google Scholar]
- 57.Gall TMH, Malhotra G, Elliott JA, Conneely JB, Fong Y, Jiao LR (2022) The Atlantic divide: contrasting surgical robotics training in the USA, UK and Ireland. J Robot Surg. 10.1007/s11701-022-01399-5 [DOI] [PMC free article] [PubMed]
- 58.Martin JR, Stefanidis D, Dorin RP, Goh AC, Satava RM, Levy JS. Demonstrating the effectiveness of the fundamentals of robotic surgery (FRS) curriculum on the RobotiX Mentor Virtual Reality Simulation Platform. J Robot Surg. 2021;15(2):187–193. doi: 10.1007/s11701-020-01085-4. [DOI] [PubMed] [Google Scholar]
- 59.Brook NR, Dell’Oglio P, Barod R, Collins J, Mottrie A. Comprehensive training in robotic surgery. Curr Opin Urol. 2019;29(1):1–9. doi: 10.1097/MOU.0000000000000566. [DOI] [PubMed] [Google Scholar]
- 60.Ebbing J, Wiklund PN, Akre O, Carlsson S, Olsson MJ, Höijer J, et al. Development and validation of non-guided bladder-neck and neurovascular-bundle dissection modules of the RobotiX-Mentor® full-procedure robotic-assisted radical prostatectomy virtual reality simulation. Int J Med Robot Comput Assist Surg MRCAS. 2021 doi: 10.1002/rcs.2195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Stefanidis D, Huffman EM, Collins JW, Martino MA, Satava RM, Levy JS. Expert consensus recommendations for robotic surgery credentialing. Ann Surg. 2022;276(1):88–93. doi: 10.1097/SLA.0000000000004531. [DOI] [PubMed] [Google Scholar]
- 62.Association of Surgeons in Training Response to GMC framework and supplementary information regarding credentialing in postgraduate medical practice On behalf of ASiT Executive and Council Association of Otolaryngologists British Association of Oral and Maxillofacial Surgeons Fellows in Training British Association of Surgical Oncology Trainees. 2019
- 63.Hung AJ, Chen J, Gill IS. Automated performance metrics and machine learning algorithms to measure surgeon performance and anticipate clinical outcomes in robotic surgery. JAMA Surg. 2018;153(8):770–771. doi: 10.1001/jamasurg.2018.1512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Collins JW, Marcus HJ, Ghazi A, Sridhar A, Hashimoto D, Hager G, et al. Ethical implications of AI in robotic surgical training: a Delphi consensus statement. Eur Urol Focus. 2022 doi: 10.1016/j.euf.2021.04.006. [DOI] [PubMed] [Google Scholar]
- 65.Dai JC, Lendvay TS, Sorensen MD. Crowdsourcing in surgical skills acquisition: a developing technology in surgical education. J Grad Med Educ. 2017;9(6):697. doi: 10.4300/JGME-D-17-00322.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Collins JW, Dell’Oglio P, Hung AJ, Brook NR. The importance of technical and non-technical skills in robotic surgery training. Eur Urol Focus. 2018;4(5):674–676. doi: 10.1016/j.euf.2018.08.018. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data availability
All data is available on request to the corresponding author.
All data is available on request to the corresponding author.