Abstract
Context
School-based nutrition interventions can support healthy eating in children.
Objective
To identify components of school-based nutrition interventions and synthesize the impact on consumption of fruits and vegetables (FV) and nutrition knowledge (NK) in children aged 4–12 y.
Data sources
Following Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines and PICOS inclusion criteria, relevant systematic reviews and/or meta-analyses, written in English, published between 2010 and August 2020, across 6 databases were identified.
Data extraction
Two reviewers independently performed data extraction and assessed the study quality.
Data analysis
The JBI Critical Appraisal Instrument for Systematic Reviews and Research Syntheses was used to assess review quality, and the Grading of Recommendations Assessment, Development, and Evaluation approach was used to rate strength of evidence.
Results
From 8 included reviews, 7 intervention components were identified: FV provision, gaming/computer-delivered, curriculum, experiential learning, reward/incentives, nudging, and caregiver involvement. FV provision had the greatest effect on F intake, gaming/computer-delivered on V intake, and curriculum on NK.
Conclusion
FV provision and gaming/computer-delivered components showed, overall, some positive effect on FV intake, as did the curriculum component on NK. More evidence evaluating single-component effectiveness that considers the setting and context of nutrition interventions is required to strengthen the evidence base.
Systematic Review Registration
PROSPERO, registration no.: CRD42020152394.
Keywords: dietary intake, healthy eating in children, intervention components, nutrition education programs, nutrition knowledge, primary schools
INTRODUCTION
The school environment, including policies, curricula, and staff, can have an important impact on child eating behavior.1 Schools can establish policies to promote healthy eating through the foods and beverages offered there.2 Additionally, they can be an effective setting for educating children about food and nutrition.3 Schools provide an optimal learning environment that reaches children from all socioeconomic backgrounds.4 Therefore, many school-based nutrition programs have been developed and evaluated in recent decades.5 Several school-based nutrition interventions that aimed to increase consumption of fruits and vegetables (FV) among children have been found to be effective.6,7 For example, 1 review reported that providing schools healthy foods in a familiar way to children, involving taste and preparation of these foods, resulted in children making healthier food choices.8 This is of great importance because research shows that unhealthy eating habits are related to childhood overweight, which, in turn, is significantly associated with adverse school outcomes.9,10 High intakes of energy-dense foods that are high in added fat and sugars can contribute to an energy imbalance with total energy intake exceeding needs, which, in turn, contributes to weight gain and, potentially, development of obesity.11
Diets high in FV have both a high-fiber content and lower energy density and therefore may support the prevention of overweight and obesity by inducing fullness and decreasing total energy intake.12 Some studies suggest FV consumption may be associated with better school performance, with children whose dietary habits are poor having lower school achievement than children with healthier dietary patterns.13,14 Results of several international studies have identified that average FV intakes of children are160–240 g FV/day, well below the recommended 400 g/day target set by the World Health Organization.15 This low FV intake in children may be explained by several barriers that prevent children from consuming FV, including those at the intrapersonal, interpersonal, community, and macro levels.16 Intrapersonal factors such as a low preference for FV or negative perceptions toward FV can prevent a child from trying and/or consuming FV. Interpersonal factors, such as low FV availability at home or lack of encouragement from caregivers to eat FV can also limit intakes. In addition, factors at the community level, such as low FV availability in stores or in the school environment can be a barrier to FV intake in children. On the macro level, production, availability, convenience, cost, and media advertising and promotion of unhealthy foods can also adversely influence consumption.16,17
One study identified that children with obesity are up to twice as likely to consider themselves poor-performing students, compared with children at a healthy weight.9 It has been reported that moving from not-overweight to overweight between kindergarten entry and end of third grade was significantly associated with lower test scores, teacher ratings of social-behavioral outcomes, and approaches to learning, but only among girls, whereas boys who became overweight had significantly more absences from school than did boys who remained at a normal weight.10
School-based nutrition interventions to date have adopted a variety of strategies to improve children’s healthy eating behavior.18,19 Given that intervention aims, methods, and activities often differ between programs, the Joint Research Centre, the European Commission’s in-house science service,20 conducted a review on how to promote FV consumption in schools and categorized various components of interventions as follows: (1) education components, targeting school children directly; (2) environmental components, targeting the school environment, including school staff but not students; and (3) parental and family components, which involve parents to reinforce the school intervention. Mak et al20 identified 66 successful intervention studies that reported an increase in FV consumption in children, whereby 16 studies implemented education components only and 50 studies included a multicomponent approach (ie, education, environment, and/or parental components). Similar findings have been reported by other studies, indicating that interventions implementing a multicomponent approach were more successful than single-component interventions.19–22 Although the successes of multicomponent programs are well documented, it is unclear which program components were successful. Evans et al19 highlighted the need to evaluate the effectiveness of individual components, given the diverse nature of multicomponent programs and that many will be difficult to replicate due to considerable funding, time, and resource requirements.3,19,23 In addition, single-component programs, such as those providing and distributing free or subsidized FV, have been rated as less complex and risky by teachers, compared with multicomponent programs.24 Having a better understanding of the effectiveness of individual components could contribute to development of more effective programs. Combining only effective components could enhance impact, with children encouraged to consume FV through multiple strategies (eg, class lessons, greater FV availability in schools) while saving time and resources related to ineffective components. Hence, knowing which individual components are most effective is important.
To gain more insight into the effectiveness of school-based nutrition programs, several systematic reviews have been conducted.19,22 However, every review has its own inclusion criteria, outcomes, and focus, with results mixed or interpreted differently based on the review aim. These reviews include results of multicomponent studies, without reporting the effect of the components individually. Therefore, it remains unclear what components of school-based program are most effective in improving healthy eating behavior in children. To address this knowledge gap, systematic reviews and meta-analyses of nutrition program components targeting FV intake in children aged 4–12 years are examined in this review, and an overview is provided of individual intervention components and their effectiveness. Here, the term components refers to the strategies, elements, techniques, activities, or mechanisms of a program designed to change behavior and achieve the program’s goal (eg, increase child FV intake).25
Given the volume of systematic reviews to date, an umbrella review, which synthesizes existing systematic reviews, was conducted to provide an overview of existing evidence to guide practitioners and policy makers in their decision-making.26,27
METHODOLOGY
This umbrella review was conducted according to the preregistered protocol deposited in June 2020 with PROSPERO (registration no: CRD42020152394; www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42020152394).
Search strategy
Database searches, keywords, and index terms were identified and reviewed in collaboration with an experienced academic librarian. The following 6 electronic databases were searched: Medline, Embase, PsycINFO, CINAHL, ERIC, and Scopus. Because systematic reviews or meta-analyses use a broader time frame, the search included reviews published from 2010 to August 2020. Searches were limited to those published in English, and terms were used that related to nutrition programs for primary schools and healthy eating in children (Table S2 in the Supporting Information online). PROSPERO and the JBI Database of Systematic Reviews and Implementation Reports were searched to identify any existing umbrella reviews on the same topic. No unpublished or grey literature was searched, because it seemed unlikely that conducted reviews in this area had not been published. EndNote X9 software was used to manage all references.
Study selection
All articles retrieved from the search were first screened on the bases of title and abstract by 2 reviewers independently. All potentially relevant full texts were assessed against the PICOS (Population, Intervention, Comparators, Outcome, and Study design) inclusion and exclusion criteria (Table 1) independently by 2 reviewers (A.V. and B.M.F.). Disagreements were resolved through discussion or with an additional independent evaluation of a third reviewer (T.B.). The study selection was managed using Covidence.28
Table 1.
PICOS criteria for the inclusion of studies
| Category | Inclusion | Exclusion |
|---|---|---|
| Participants | Primary school children aged 4-12 y | Children aged <4 or >12 y; children with special needs (eg, obesity only) |
| Intervention | School-based health promotion interventions, with the main aim of improving or promoting FV consumption and/or NK in primary school children | Interventions on mental or emotional health, eating disorders, community farming or gardening only, and cultural aspects |
| Comparator | With control group | Without control group |
| Outcomes | Quantitative results of child F, V, or FV intake (eg, grams or ES) and/or NK (eg, score or ES) | No quantitative results of child F, V, FV intake, or NK (eg, described only) |
| Study design | Systematic reviews and meta-analyses of quantitative studies. Only results from relevant intervention studies were extracted for inclusion. Reviews published in English language between 2010 and August 2020 | When results for children, school-based, or FV intake and NK were not reported separately (eg, only reporting means for the whole study sample including children and adults). Studies of multicomponent programs only if no separate results for the individual components were listed |
Abbreviations: F, fruit; FV, fruits and vegetables; NK, nutrition knowledge; V, vegetable.
Methodological quality rating
The methodological quality of the included reviews was assessed by 1 reviewer (A.V.) using the standard JBI Critical Appraisal Instrument for Systematic Reviews and Research Syntheses.27 A second reviewer (B.M.F.) reviewed the quality rating critically and any disagreements were resolved through discussion.
Data extraction
From each individual review the following data were extracted: author/year, objectives, number of included studies, participants (characteristics and total number), intervention component(s) (eg, fruits [F], vegetables [V], or FV provision; school lessons about nutrition; caregivers’ involvement), measure instruments, results or outcomes (ie, effect on children’s FV intake and nutrition knowledge [NK]), and recommendations for practice and research, based on the standardized data extraction format in Covidence.28
Intervention components were categorized on the basis of the reviews’ program descriptions and, if unclear, program-component content of primary studies was retrieved. In cases where multiple components were combined within 1 program or intervention (eg, an intervention with lessons about nutrition and FV provision in school) without evaluating the components separately, the study was excluded. When data from the included systematic reviews or meta-analyses were unclear or missing (eg, number of participants), the primary studies were retrieved and data extracted for the present umbrella review. In cases where additional outcomes were reported, such as health-related measures (eg, body mass index, sugar intake), population groups (eg, infants, adults), intervention context (eg, home based, after-school based), only the subset of relevant studies (ie, those discussing FV intake and NK in primary school–aged children) was extracted for synthesis. Primary studies that were included in multiple reviews were cross-checked for accuracy and reported only once to avoid duplication of results (see Table S3 in the Supporting Information online for included reviews and primary studies).
Data summary
Findings were categorized by nutrition-program components. The quality of evidence for each component against FV intake and NK was assessed using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) approach, by 2 reviewers independently (A.V. and B.M.F.).29,30 The GRADE approach is a framework for systematically presenting summaries of evidence; it informs the strength of recommendations for practice.29,31,32 GRADE identifies the following 5 categories: (1) risk of bias (considering limitations in study design or execution and randomization); (2) imprecision (sample size, number of included studies); (3) inconsistency (heterogeneity level measured by I2: low heterogeneity, I2 < 40%; moderate, I2 = 40%–60%; and high, I2 > 60%); (4) indirectness of evidence (applicability of studies to the PICOS of interest); and (5) publication bias (considered if all relevant studies are included). These 5 categories address nearly all issues that influence recommendations based on the evidence.30 The GRADE approach was chosen because it has been used in previous umbrella reviews in this field.29,30,33
The evidence of impact of individual components on each relevant outcome is presented by using a color-coded “traffic-light indicator” based on average results of the primary studies for each specific outcome. Green indicates an effective or beneficial intervention; amber indicates no intervention effect, no significant results, or no clear effect, due to insufficient data reported; and red indicates an adverse effect of the intervention compared with the control group. Effect sizes (ESs) were reported and other measures (eg, FV changes in grams) were only listed when ESs were unreported. ESs with r = 0.10 are defined as small effect (the effect explains 1% of the total variance); r = 0.30 indicates medium effect (the effect accounts for 9% of the total variance), and r = 0.50 defines large effect (the effect accounts for 25% of the variance.34
RESULTS
Study inclusion
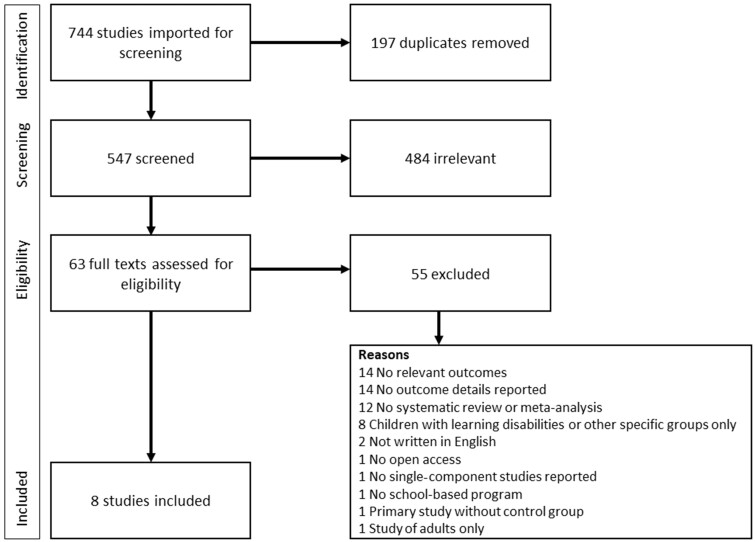
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) framework was used for presenting the study selection (Figure 1).35 The searches in the databases resulted in 744 records for screening. After removing 197 duplicates, 547 articles were screened on the bases of title and abstract, and 63 potentially relevant articles were identified for full-text screening. Of those 63 full texts, 55 articles were excluded (eg, no FV intake or NK reported as outcome). This resulted in a total of 8 reviews that met the inclusion criteria and were included in the present umbrella review.1,19,22,36–40
Figure 1.
PRISMA flowchart of study selection and inclusion process
Methodological quality
All included reviews met 5 out of the total 11 quality appraisal criteria (questions [Qs] Q1, Q2, Q3, Q4, and Q8) listed in the JBI Critical Appraisal Instrument for Systematic Reviews and Research Syntheses27 (Table 2).1,19,22,36–40 Criteria Q5 and Q11 were met by all reviews, except 1 for each criterion (1 study did not report any details on critical appraisal [Q5]37 and 1 study did not list any recommendations for future research [Q11]40). The remaining 4 criteria (Q6, Q7, Q9, and Q10) were not met or were rated as unclear due to insufficient reported information. Two reviews did not conduct critical appraisal (Q6) by 2 or more reviewers,37,38 were reported as “no”, and 1 review36 was rated unclear that reported the critical appraisal was conducted by 3 of the review’s authors but did not report if this was done independently. Two reviews did not implement methods to minimize errors in data extraction (Q7),37,40 and although authors of 1 review did mention they used standardized forms, they did not report if this was done in duplicate or independently.36 Four reviews did not assess the likelihood of publication bias (Q9)1,36,38,40 and, for 1 review,39 it was unclear if the authors assessed publication bias. Two reviews did not report recommendations for policy and/or practice (Q10) and, therefore, did not meet the quality criteria.1,38
Table 2.
Critical appraisal of included reviews27
| Included reviews | Questiona |
No. of criteria met | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | ||
| Delgado-Noguera et al (2011)36 | Y | Y | Y | Y | Y | U | U | Y | N | Y | Y | 8 |
| Dudley et al (2015)1 | Y | Y | Y | Y | Y | Y | Y | Y | N | N | Y | 9 |
| Evans et al (2012)19 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 11 |
| Langellotto et al (2012)37 | Y | Y | Y | Y | N | N | N | Y | Y | Y | Y | 8 |
| Metcalfe et al (2020)38 | Y | Y | Y | Y | Y | N | Y | Y | N | N | Y | 8 |
| Micha et al (2018)22 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 11 |
| Morgan et a. (2020)39 | Y | Y | Y | Y | Y | Y | Y | Y | U | Y | Y | 10 |
| Silveira et al (2011)40 | Y | Y | Y | Y | Y | Y | N | Y | N | Y | N | 8 |
Question (Q)1: Is the review question clearly and explicitly stated? Q2: Were the inclusion criteria appropriate for the review question? Q3: Was the search strategy appropriate? Q4: Were the sources and resources used to search for studies adequate? Q5: Were the criteria for appraising studies appropriate? Q6: Was critical appraisal conducted by ≥2 reviewers independently? Q7: Were there methods to minimize errors in data extraction? Q8: Were the methods used to combine studies appropriate? Q9: Was the likelihood of publication bias assessed? Q10: Were recommendations for policy and/or practice supported by the reported data? Q11: Were the specific directives for new research appropriate? Based on Chai et al.33
Abbreviations: ES, effect size; N, no; U, unclear; Y, yes.
According to the GRADE assessment of strength of evidence for recommendations, the primary studies included in the reviews were generally rated as being of “low quality”, described as “Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect”.30 Almost all outcomes were downgraded by 1 level due to presence of heterogeneity. The second most common reason for downgrading quality level was the low quality of the primary study, according to the reviews. Risk of bias was also indicated in more than half of the reviews, and a few were downgraded on the basis of having a nonrandomized study design. See Table S3 in the Supporting Information online for more details on the GRADE results for each component and identified outcomes.
Program components
The following 7 nutrition program components were identified on the basis of descriptions provided in systematic reviews: (1) FV provision; (2) gaming/computer-delivered; (3) curriculum; (4) experiential learning; (5) reward/incentives; (6) nudging; and (7) caregiver involvement.
FV provision
Programs using the FV-provision component focused on FV availability and accessibility in the school environment. The retrieved systematic reviews included the following descriptions: free or subsidized school FV distribution, fruit-distribution scheme, food provision such as the availability of FV at lunchtime or in tuck shops (ie, a small retailer close to the school) or free FV distribution19; interventions providing healthful foods or beverages in classroom, also described as “direct provision” and “indirect provision”, meaning the availability of healthful foods in cafeterias, tuck shops, or vending machines,22 school food service (educational practices), or school nutrition policy (food or meal delivery).40
Gaming/computer-delivered
Programs using the gaming/computer-delivered component refer to programs including internet-administered activities that provide children with information on healthy eating in an entertaining way. One example is “Squire’s Quest!”, which is a 10-session game delivered over 5 weeks that includes 25 minutes per session on information about healthy eating. Squire’s Quest! includes activities to increase FV preferences through multiple exposures and associating fun with FV intake, increase asking for FV at home, and increase skills in preparing FV through making virtual recipes.41
The retrieved systematic reviews included the following descriptions: a psychoeducational multimedia game, internet-based feedback from questionnaires,19 educational games or use of internet,40 board games or computer-based interventions or interventions using a computer-based approach,36 web-based approaches such as internet-based resources or feedback mechanisms that could be accessed by students at home or at school.1
Curriculum
Curriculum-based programs include activities or strategies whereby teachers provide children with information on the importance of healthy eating through cognitive learning activities and materials that have similar design to other core curriculum subjects, such as group discussions or storytelling. For example, Taste Lessons, which includes a national school-based nutrition program for primary school children aged 4–12 years, consists of 10–12 lessons on 5 themes related to health (taste, nutrition and health, cooking, food production, and consumer skills) delivered over 2 school years and includes activities such as taste activities/experiments or assignments.42 Other curriculum-based programs included lessons on identifying the food groups, the nutritional qualities of FV, and discussing the importance of healthy eating,43 or included in-class visits from a nutritionist who discussed topics such as macro- and micronutrients, digestion, nutritional needs, and obesity.44
The retrieved systematic reviews included the following descriptions: school lessons as part of the school curriculum19; curriculum initiatives or an evaluations/curriculum approach, such as specialty-nutrition education programs beyond existing health curricula delivered by teachers or specialists; and cross-curricular approaches including nutrition-education programs delivered across ≥2 traditional primary school subjects (eg, science or math),1 traditional nutrition education programs without a gardening component (eg, nutrition lessons designed to support other subjects [eg, science and math], and targeted healthy eating behaviors.37
Experiential learning
Children who participate in a program based on an experiential learning component join activities focused on developing skills related to FV consumption (eg, preparing a healthy snack). Experiential learning has been described in the literature as practice-based education whereby children learn by doing and explore the knowledge content.45 An example would be a program in which students maintained a garden through weeding, watering, and harvesting, and participated in other garden activities such as a salsa-making workshop, class cookbook, and food experiences with harvested FV from the garden.46
The retrieved systematic reviews included the following descriptions: experiential learning (cooking, environment, and community garden),1 garden-based educational activities, hands-on gardening activities in a garden where a variety of FV were grown (eg, drying herbs, developing a cookbook inspired by the garden, planting a variety of vegetable seeds, maintaining the garden, or preparing a salad from garden-grown vegetables).37
Reward/incentives
Programs using the reward/incentives component refer to a setting where children receive small rewards (eg, stickers, pencils, erasers) paired with praise encouragement for eating FV47 and rewarding children, through stickers and praise encouragement, for tasting an initially disliked food.48
The retrieved systematic reviews included the following descriptions: contingent reinforcement approaches, such as rewards or incentives given to students in response to desired behavior; animation abstraction; and contingent reinforcement for FV intake or contingent reinforcement for vegetable tasting.1
Nudging
Children who participate in a program including a nudging component are encouraged in a gentle way to choose the healthier food option in the school setting (eg, through the school canteen). Nudging is defined as “any aspect of the choice architecture that alters people’s behavior predictably without forbidding any options or significantly changing their economic incentives”.49 The retrieved systematic reviews included the following descriptions: Metcalfe et al38 included primary studies comparing schools with salad bars and schools without salad bars50; using attractive bowls or baskets, signage, and images promoting FV; changing FV placement51; and verbal prompts promoting healthy items.38
Caregiver involvement
Programs that include the caregiver-involvement component engage caregivers in the activities or strategies to support healthy eating by children. The retrieved systematic reviews included the following descriptions: Morgan et al39 reported that caregiver participation in interventions to improve children’s dietary intake can be active or inactive: (1) active caregiver intervention components include asking caregivers to physically attend at the event, or participate in other intervention activities; whereas (2) inactive caregiver intervention components are those in which caregiver participation is limited to receiving information, such as a newsletter.39
Characteristics of included reviews
The 8 included reviews were published between 2011 and 2020 (Table 3).1,19,22,36–40 and included 2 systematic reviews,38,40 5 systematic reviews with meta-analysis,1,19,22,36,39 and 1 meta-analysis.37 FV consumption was assessed in all included reviews, and NK was only assessed in 2 reviews.1,37
Table 3.
Characteristics of included systematic reviews and meta-analyses
Delgado-Noguera et al. (2011)36 (3/19)
| Reference (relevant/total primary studies) | Outcomes assessed | Components assessed (no. of primary studies) | Standardized mean differences or ESsa and main results and findingsb | Conclusionsb |
|---|---|---|---|---|
| FV intake |
|
|
|
|
| Dudley et al. (2015)1 (16/49) |
|
|
|
|
| Evans et al. (2012)19 (8/27) | FV intake |
|
|
|
| Langellotto et al. (2012)37 (3/20) |
|
|
|
|
| Metcalfe et al. (2020)38 (4/29) | FV intake | Nudging (4 RCTs) |
|
Nudging: mixed results with neutral/positive effects. Two studies showed positive effect on F and/or V intake. |
| Micha et al. (2018)22 (6/91) | FV intake | FV provision (4 RCTs, 2 NRCTs) |
|
FV provision: positive effect on F intake, negative effect on V intake (based on 2 studies), and neutral/positive effect on FV intake |
| Morgan et al. (2020)39 (1/23) | FV intake | Caregiver involvement (1 RCT) |
|
Caregiver involvement: positive effect on FV intake, but only based on 1 study |
| Silveira et al. (2011)40 (5/24) | FV intake |
|
|
|
ESs with r = 0.10 are defined as small effect—the effect explains 1% of the total variance; r = 0.30 as medium effect—the effect accounts for 9% of the total variance; and r = 0.50 is defined as large effect—the effect accounts for 25% of the variance.34
Based on only relevant primary studies (eg, primary studies on adults, or after-school programs only are not included).
Abbreviations: CCT, cluster-controlled trial; ES, effect size; F, fruit; FV, fruit and vegetables; MD, mean difference; NK, nutrition knowledge; NR, not reported; NRCT, nonrandomized controlled trial; NS, nonsignificant; QET, quasi-experimental trial; RCT, randomized controlled trial; SMD, standard mean difference; V, vegetable.
The FV provision component was assessed in 4 reviews,19,22,36,40 including 10 randomized controlled trials (RCTs) and 5 nonrandomized controlled trials (NRCTs; primary studies). The gaming/computer-delivered component was listed in 4 reviews,1,19,36,40 based on 8 RCTs (no NRCTs), whereas the curriculum component was reported in 3 reviews,1,19,37 4 RCTs, and 8 NRCTs. The experiential learning component was reported in 2 reviews1,37 and 3 NRCTs (no RCTs). One review,1 including 1 RCT and 1 NRCT, reported the reward/incentives component, and 1 review38 addressed the nudging component (with 4 RCTs). The last component, caregiver involvement, was assessed in 1 review,39 including 1 RCT (no NRCTs).
The included 8 reviews reported, in total, 33 primary studies (12% of the total 282 primary studies) that were relevant for this umbrella review, published between 1973 and 2017. Some primary studies were listed in multiple reviews. Of the relevant primary studies, 9 (27%) were included in ≥2 reviews of the umbrella review (Table S3 in the Supporting Information online).
Review findings
All reviews reported at least some positive impacts of the assessed intervention components on children’s FV intake and/or NK. Besides those positive effects, 2 reviews showed slightly negative effects (eg, 1 primary study resulted in negative effect on F intake effect).22,37 The results of each individual component are discussed in the following sections (see Table S4 in the Supporting Information online for more details).
FV provision
In total, 8 primary studies reported the FV-provision component.52–59 Regarding FV-provision single-component programs, the most positive effect was found on F intake and mixed results were found on V intake by children. Five primary studies showed positive effect on F intake,52–56 with an ES ranging from 0.09 to 0.58, and a total sample size of 10 166 participants. V intake was measured in 3 studies, with 2 studies reporting a negative effect,53,55 with an ES ranging from –0.03 to –0.10; the third study found a positive effect, with an increase of 20.7 g/day.57 FV intake was measured in 5 primary studies, which reported mixed results, with 2 studies reporting positive effects,53,58 and 3 studies reporting no effect.54,55,57 The strength of recommendations for practice, based on the GRADE approach, ranged from very low (V intake) to moderate (F and FV intake), with presence of heterogeneity as the main reason for downgrading by a level.
Gaming/computer-delivered
Four primary studies evaluated the gaming/computer-delivered component.41,60–62 In contrast with FV provision programs, gaming/computer-based programs resulted in positive effect on V consumption, based on all 3 primary studies,41,60,61 with an ES ranging from 0.02 to 0.33 and a total sample of 2211 participants. Mixed results were found for the effect gaming/computer intervention on F intake: 1 study found positive effect of the intervention on F intake, with an ES of 0.5241 and another study indicated negative effect, with an ES of –0.10.60 A positive effect was found on FV intake in 2 studies, with an ES ranging from 0.15 to 0.91,41,62 and 1 study reported no effect.60 Two studies that used a gaming/computer component approach assessed NK, with 1 study that found a positive effect (ES, 0.77)62 and 1 study found no significant results (P < 0.005) but reported insufficient data to measure the ES.61 The quality of evidence for this component, based on the GRADE approach, ranged from very low (FV intake and NK) to moderate (F intake), with heterogeneity identified as the main reason for downgrading the strength of evidence by a level.
Curriculum
The curriculum component was assessed by 11 primary studies.43,44,63–71 Mixed effects were found from curriculum-based interventions. Two studies found a positive effect on F intake,64,65 but 2 other studies resulted in nonsignificant results43 or the authors did not report sufficient data to measure the ES.63 Regarding V intake, 3 out of the 5 studies found a positive effect, with an ES ranging from 0.28 to 2.10,43,64,65 and 2 studies resulted in nonsignificant results67 or insufficient reported information to assess the ES.66 Considering FV intake, only 1 study showed positive effect (ES, 2.70)43; 3 studies resulted in nonsignificant results64,68 or did not report ES.44 NK was measured in 6 studies, but only 1 reported a significant ES, indicating a positive effect (ES, 0.59).64 The other 5 studies resulted in nonsignificant results69 or did not report ES, due to lack of information.43,66,70,71 The overall grade of recommendations, based on the GRADE approach, for all outcomes was assessed as very low, due to indicated heterogeneity, nonrandomized study designs, low quality indicated in original review, and limitation in publication as reasons for downgrading the strength of recommendations for practice by a level.
Experiential learning
Three primary studies reported the experiential learning component.46,72 Similar mixed results were found for interventions using an experiential learning component. One study found a positive effect on F intake,46 whereas 2 studies found a positive effect on V intake (ES, 0.12–3.75).46,72 Mixed results were found for NK, with 1 study reporting a positive effect (ES for grades K–3, 1.98 and grades 4–6, 1.94)73 and 1 study reported a negative effect (ES for experiential group, 0.201; ES for control group, 0.274).72 Similar to the curriculum component, the quality of evidence (by GRADE) for all outcomes was assessed as very low due to indicated heterogeneity, nonrandomized study designs, low quality indicated in the original review, and limitation in publication as reasons for downgrading the strength of evidence by a level.
Reward/incentives
The reward/incentives component was evaluated in 2 primary studies.47,48 One primary study resulted in a positive effect on both F and V intake (% eaten) as a result of a reward/incentives interventions (ES for F intake: ages 5–7 years, 2.21 and 7–11 years, 2.36; ES for V intake: ages 5–7 years, 2.01 and 7–11 years, 1.51).47 One study reported insufficient data on V intake to measure the ES.48 According to the GRADE assessment, the quality of evidence ranged from low (FV intake) to very low (F and V intake) with indicated heterogeneity, low quality indicated in the original review, and limitations in publication as the main reasons for downgrading the strength of recommendations for practice by a level.
Nudging
Four primary studies reported the nudging component.50,51,74,75 Mixed results were found for the nudging component intervention, including 1 study that showed a positive effect on F and V intake (via visual observation; F intake pre- and postintervention: 0.73 servings and 0.83 servings, respectively; V intake pre- and postintervention: 0.57 servings and 0.86 servings, respectively).74 Similar positive results for F intake (percentage who ate F, via visual observation) were found in another study (intervention: 87%; control: 65%).75 Two studies did not identify any significant results.50,51 The quality of evidence, based on the GRADE approach, for all outcomes was assessed as very low due to heterogeneity, nonrandomized study designs, low quality indicated in original review, and limitations in publication; and these were reasons for downgrading the strength of evidence by a level.
Caregiver involvement
Only 1 primary study reported the caregiver involvement component, and it showed a positive effect on FV intake (M = Measurement time point, intervention M1 (baseline): Mean: 1.89 (SD: 2.66), control M1: Mean: 1.80 (SD: 2.72); intervention M2: Mean: 2.19 (SD: 2.50), control M2: Mean: 1.68 (SD: 2.41); intervention M3: Mean: 2.30 (SD: 2.82), control M3: Mean: 1.93 (SD: 2.73); intervention M4: Mean: 2.31 (SD: 2.86), control M4: Mean: 2.27 (SD: 2.64)).76 The quality of evidence was assessed as very low due to indicated heterogeneity, nonrandomized study designs, low quality indicated in the original review, and limitations in publications; and these were reasons for downgrading the strength of evidence by a level.
Summary of evidence
Table 4 provides a summary of the evidence for each individual component and included outcomes, with the traffic-light visual indicator showing the effectiveness of the components on the listed outcomes, based on average results. Only results highlighted in green (positive effect) and amber (neutral/no effect) are listed, meaning no component showed a less-effective (negative) effect. The strength of recommendations, based on the GRADE approach, is identified with asterisks, ranging from 1, meaning very low quality, to 4, indicating high quality of evidence. According to these results, FV provision, gaming/computer-delivered, and curriculum component programs are most frequently listed in the literature and score highest on level-of-evidence strength. The remaining components also demonstrated positive effects but were low in evidence strength and were based on a few studies.
Table 4.
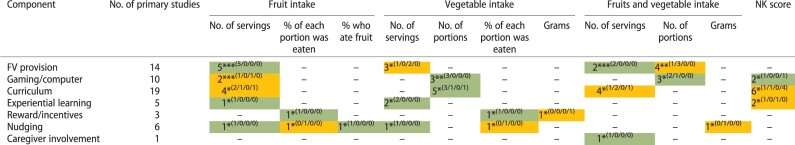
|
The asterisks indicate study quality based on GRADE results:
= high quality;
= moderate quality;
= low quality;
= very low quality. The numbers in parentheses indicate the following respectively: positive/neutral/negative/insufficient data.
Traffic-light indicator for effectiveness of interventions based on indicated single component: green indicates an effective or beneficial intervention component; amber indicates no intervention component effect, no difference compared with control group, or unclear effect due to insufficient information.
Abbreviations: FV, fruit and vegetables; NK, nutrition knowledge; “–” indicates outcomes that are not reported for that component.
DISCUSSION
The purpose of this umbrella review was to identify nutrition initiative components and to synthesize the effect of each individual component on FV intake and/or NK in primary school children. Seven components were identified as described in Table 4: (1) FV provision, (2) gaming/computer-delivered, (3) curriculum, (4) experiential learning, (5) reward/incentives, (6) nudging, and (7) caregiver involvement. These components have been grouped together in the discussion, given that the issues identified relate to all components.
This umbrella review includes results from 8 systematic reviews, which included a total of 282 primary studies, but only 33 studies (12%) were relevant for our review. This might suggest that relatively few studies report the effectiveness of single components on FV intake and NK in children, albeit it should be noted that studies on individual components may potentially have been excluded as part of the review criteria and, therefore, not included in this umbrella review (eg, 1 review included only RCTs40). Another reason for this lack of evidence may be that the current literature reports multicomponent programs as most effective, with the effectiveness of individual components not separated out from the total program; therefore, interventions use this approach.19 Regarding program effectiveness on NK, 2 of the 8 reviews reported child NK as an outcome.1,37 Hence, it may be assumed by program developers that enhancing child FV intake is more important than only including an NK component for children, when, in fact, this issue is understudied. One explanation for this lack of literature on NK may be that FV intake is more commonly associated with health promotion than NK.77 NK is shaped by lifelong personal experiences and beliefs and plays an important role in changing eating behavior.78 However, it must be acknowledged that the body of literature does not clearly indicate a direct relationship between NK and FV intake in children. This may be because poor eating habits can be due to factors other than NK, such as a deficient understanding of consequences, poor skills (eg, cooking), low motivational levels, lack of confidence, and an unsupportive environment.78 Additionally, the sensory property of food (eg, sweetness, bitterness) may override a child’s food preferences beyond their NK.79
NK is included in this review because multiple programs aim to increase NK, and it is suggested that NK contributes to healthy eating behaviors.80–83 Furthermore, NK is included in most models related to FV intake in children as an important personal-level factor.84,85 In addition, previous research suggests NK leads to higher FV intake when it is delivered with food skills interventions and critical decision-making, which relate to the term food literacy.80 Food literacy refers to “the capacity of an individual to obtain, process and understand basic information about food and nutrition as well as the competence to use that information in order to make appropriate health decisions”.86 Several studies have reported that higher food literacy is associated with healthier eating patterns and better health and well-being.87–91 It is suggested, therefore, that NK could be a valuable outcome for school-based nutrition programs. However, given that there is heterogeneity with the results from studies that focus on NK, and other factors affect children’s food intake, interventions that focus solely on NK may be not sufficient to increase FV consumption.
Additionally, effective nutrition initiatives are described as a complex undertaking that calls for a systematic and comprehensive assessment of the determinants of the desired outcome to inform the intervention.92 Most of the primary studies used a multicomponent approach without reporting single-component effectiveness and, therefore, did not provide data to inform the research question of this review. This was not expected, given the large volume of literature on the subject. However, this is still a valuable review outcome and it highlights the need for more research in the field of nutrition initiatives.
The few relevant studies on single-component effectiveness were low in overall study quality, especially for 4 components (experiential learning, reward/incentives, nudging, and caregiver involvement). For these, the level of evidence strength was downgraded on the basis of heterogeneity, nonrandomized study designs, low methodological quality of the original review, and/or publication bias (Table S3 in the Supporting Information online).27 It must be acknowledged as a limitation that 1 of the methodological quality criteria of the present review could have potentially biased findings toward positive effects (Q10 in Table 2).27 Reviews that have an inconclusive finding will not enable making evidence-based recommendations; rather, they focus on gaps in the research and hence potentially have limited implications or recommendations for policy and/or practice. However, because the 2 reviews that did not meet this criterion met most of the other criteria (9 vs 8 of the total 11 criteria), it potentially had a limited impact on the findings of the present review.
The description of the 7 effective components may be abstract to some extent and lack specific descriptions. This is due to the program descriptions in the retrieved studies being brief or lacking specific information.93 Michie et al25 developed a method to deconstruct behavior change interventions into the so-called behavior change techniques (BCTs) (n = 93). BCTs are the “active ingredients” of programs that aim to reach behavior change (eg, increasing FV consumption) and are more detailed and actionable than the individual components identified in the present review. BCTs can be used to identify previously unknown factors related to developing more effective programs, because they specify intervention content by using standardized labels and clear definitions that are understandable by all users.25 Identifying the use of specific BCTs could strengthen more-detailed reporting of program components, with the Coventry, Aberdeen, and London-Refined (CALO-RE) taxonomy as an appropriate framework applicable to programs on healthy eating, which includes 40 BCTs.94 BCTs could not be used for program evaluation in this review, due to the lack of detail presented and the summarizing function of an umbrella review. However, future studies measuring program effectiveness may benefit from clear reporting of BCTs used within the programs to improve the quality of research reporting and better inform program development and evaluations.
Another key issue is the variety of outcome measures used to assess effectiveness of nutrition programs. In this review, we reported several different types of outcome measures, such as F intake based on visual observational,75 or a weighed instrument,50,51 or a 24-hour recall.44,59,60,64,67 Although questionnaires were used most often, the content of questionnaires was not often shared, therefore making it difficult to compare with other questionnaires and making interpreting the results challenging and complex, because the quality of these used instruments is often unknown. In addition, the validity of measures was not included in the inclusion criteria of the present review to prevent exclusion of relevant literature. Some results, therefore, should be interpreted with caution because variation in the validity of the outcome measures exists. One might argue, for instance, that the visual observation methods are less valid than a questionnaire of known validity in terms of the relative accuracy of what the questionnaire aims to measure. To check for the sensitivity of the conclusions, data excluding the studies that used the visual observation method74,75 were reanalyzed, but this did not change the conclusions. Therefore, the full scope of the included reviews is reported.
Similarly, inconsistency in reported measurement-units use was observed. Some reviews reported FV intake in portions, whereas other reviews used number of servings as unit. It is often not reported what 1 portion or serving is in terms of grams or other household measure, making it difficult to compare results. Three reviews addressed the unit content, namely 80 g serving/day for FV intake,19,22,39 which is in line with the World Health Organization guidelines.77 Three other reviews reported both portions and servings, based on primary studies, and did not report unit content.1,38,40 Furthermore, Langellotto et al37 reported 1 serving of V included 75 g and 1 serving of F consisted of 150 g, based on previous research.95 One review described the daily recommended intake of 400 g/day or 5 servings of FV in the introduction, but included both servings and portions throughout the article, without clarifying the difference.36 It is recommended that future reviews consistently report the units used and provide a description or definition of used units, with servings from 80 g/day being a preferred unit when reporting FV intakes.77 This is in line with literature on the lack of clarity about serving sizes, which suggests standardizing the terminology for measuring food portions to avoid confusion.96
Another issue relates to children as the target group for nutrition programs. Research indicates that children from age 6 years can understand which foods are good for their health.97 However, health messaging for children and adolescents can be problematic,98 and strategies that focus on taste, aesthetics, and play, which are important drivers of children’s food choices, are promising.99,100 An example includes the earlier mentioned Squire’s Quest! game that aims to increase children’s preferences for FV by creating a fun experience.41
FV promotion in previous research is mostly combined, without reporting results for F and V separately. However, positive health outcomes are more related to increased V consumption rather than F consumption, because of the greater discrepancy with current intake relative to recommendations, compared with F. Moreover, children are generally closer to meeting F consumption guidelines. For example, in Australia, 45% of children aged 9–10 years met F intake, whereas only 9% met V intake.101 Also, the total FV consumed is often inflated by the increased amount of F, compared with V. This may be explained by the fact that children generally like F more than V, due to the sweetness of F and the bitterness of V.79 Considering the important health benefits of V but the low intake, it is recommended to report F and V intakes separately. Also, programs that specifically aim to increase V intake and not F intake, per se, are highly recommended.
In addition, 1 review1 included 9 primary studies with no ES for at least 1 outcome (F, V, or FV intake or NK)43,44,48,61,63,66,67 reported as “insufficient data reported for calculation.”1 Even if these studies addressed significant results, without the ES, their results could not be included. Because of this lack of data, we reported in this review several noneffective results in the summary of evidence, whereas the effects may be more positive or negative than identified in the present study. Therefore, it is highly recommended that future intervention studies report intervention ESs.
As previously reported, multicomponent programs are identified as most successful.3,19,102 This could be explained by the fact that children are encouraged to eat FV through multiple approaches, for example, through lessons in class, but also through the environment where FV are available. The present review provides insight into which individual components are effective. This knowledge may help strategically combine components to reach optimal impact and could help reduce costs by cutting components with small or no effects.
When assessing the effectiveness of multicomponent programs, it is not possible to determine the degree to which the individual components contribute to the increase of FV intake by children.1 Evaluation studies could assess the effectiveness of components separately by using a quasi-experimental design with 3 arms: 1 group of children receives a single-component program, a second group receives a 2-component program, and a control group.103 Nevertheless, it must be acknowledged that components might not be effective in isolation but only in combination with other components. However, a possible reinforcing effect could not be included in the present review in regard to individual components only.
Similarly, the finding that some programs do not result in the desirable outcome may be due to the existence of several barriers that prevent children from eating FV, but a given program may only be targeting 1 barrier. For example, a program may aim to increase FV intake, but FV availability remains low. In this case, the program may not increase FV intake, because of a lack of availability. The finding that FV provision has been identified as effective in the present study is not surprising, therefore, because children are probably more likely to eat FV when it is available, regardless of other determinants related to FV intake. On the other hand, children with better attitudes about or preferences for eating FV are still, to some extent dependent on the availability of FV, because they basically cannot consume any FV if none are available. FV provision, therefore, is more likely to result in increases in FV intake, compared with other determinants.
Furthermore, previous research proposed that determinants of FV intake include cultural, physical, and social-environment factors.104 Klepp et al104 expected that environmental factors such as FV availability influence children’s FV intake more directly due to children’s limited food-choice autonomy. The program context is not included in the present review, although this may be different for each study and is expected to influence the results (eg, involvement of caregivers may be possible in some schools but not in others, due to barriers such as travel time for caregivers). Research considering the context may be beneficial in enhancing suitability of programs to specific groups and may contribute to achievement of desirable outcomes.
Results of the this umbrella review indicate promising impacts on 3 components: FV provision, gaming/computer-delivered, and curriculum. Evidence for the 4 remaining components (experiential learning, reward/incentives, nudging, and caregiver involvement) is weak, mainly due to a lack of studies and/or low levels of quality, especially for the caregiver involvement component, for which only 1 study was identified.76 Integrating the home environment in nutrition programs has several challenges, such as nonresponse risk and socially desirable answers. However, caregivers’ health promotion behavior (eg, FV provision) contributes to FV intake and NK in children, suggesting involvement of the home environment may increase success of certain programs.105,106 This field of research, therefore, should be explored more. Some successes have already been reported, based on well-controlled evaluation studies, that have contributed to successful programs now implemented routinely in some schools.42
Recommendations for practice and future research
Based on the current results, it is recommended that nutrition-program developers or implementers include FV provision, gaming/computer-delivered, and/or curriculum components. These components have the most promising impacts on FV intake and NK in children to date. However, it is highly recommended that the setting and context of nutrition interventions be explored in future programs. The multilevel-implementation quality framework may be useful for particular studies in which contextual factors are categorized at 3 levels: (1) macro level (eg, community capacity to prioritize healthy eating and allocate a budget for implementation of health promotion programs), (2) school level (eg, school food policies such as FV policy whereby children can eat only FV during the morning breaks), and (3) individual level (eg, a positive attitude toward the program enhances implementation quality), because 1 approach can be a success in a certain setting but less or not successful in a different setting.107,108
Research on single-component programs is needed, especially studies using high-quality and valid instruments and quantitative methods (eg, reported ESs) to measure outcomes. RCTs measuring both short- and long-term effects are needed, along with studies on caregiver involvement, given the evidence for this component was based on only 1 primary study.76
CONCLUSION
School-based nutrition programs contribute to FV consumption and NK in primary school–aged children. Of the 7 components categorized, FV provision, gaming/computer-delivered, and curriculum components had an overall positive impact on FV intake. Although the remaining 4 components (experiential learning, reward/incentives, nudging, and caregiver involvement) had some positive effects, these were less abundant in the literature and were generally of lower quality. Results indicate there are many opportunities for the education sector to contribute to children’s health in addition to their development. Additional standardized, high-quality studies targeting specific settings and contexts, using valid instruments to measure change in FV in single-component nutrition programs, or that assess intervention components separately, are needed to further evaluate the relative effectiveness of individual components used to support healthy eating behavior in children and, thereby, the future adult population.
Supplementary Material
Acknowledgements
The authors thank Debbie Booth (librarian, University of Newcastle) for assisting with the development of the search strategy, and Matthijs Bekkers for assisting with the title and abstract screening. This study contributes to the thesis work for DADD PhD candidate A.V. at the University of Newcastle (Australia) and Wageningen University and Research (the Netherlands).
Author contributions. A.V., T.B., and C.E.C. conceptualized the umbrella review. A.V. conducted the literature search, wrote the manuscript, and edited the manuscript after revisions were made. A.V. and B.M.F. conducted the abstract, title and full-text screening and assessed the quality and extracted the information of the included studies. T.B. was the third reviewer in case of disagreement. B.M.F., T.B., A.H-N., E.V., and C.E.C. provided critical revision of the manuscript and approved the final version of the manuscript.
Funding. This research was financially supported by the Dutch Ministry of Agriculture, Nature and Food Quality, the Dutch Ministry of Health, Welfare and Sport. C.E.C. is supported by an Australian National Health and Medical Research Council Senior Research Fellowship and a University of Newcastle, Faculty of Health and Medicine Gladys M. Brawn Senior Research Fellowship.
Declaration of interest. The authors have no relevant interests to declare.
Contributor Information
Angeliek Verdonschot, are with the School of Health Sciences, College of Health, Medicine and Wellbeing, University of Newcastle, Newcastle, New South Wales, Australia; are with the Priority Research Centre for Physical Activity and Nutrition (PRCPAN), University of Newcastle, Callaghan, New South Wales, Australia; are with the Consumption and Healthy Lifestyles, Wageningen University and Research, Wageningen, The Netherlands.
Berit M Follong, are with the School of Health Sciences, College of Health, Medicine and Wellbeing, University of Newcastle, Newcastle, New South Wales, Australia; are with the Priority Research Centre for Physical Activity and Nutrition (PRCPAN), University of Newcastle, Callaghan, New South Wales, Australia.
Clare E Collins, are with the School of Health Sciences, College of Health, Medicine and Wellbeing, University of Newcastle, Newcastle, New South Wales, Australia; are with the Priority Research Centre for Physical Activity and Nutrition (PRCPAN), University of Newcastle, Callaghan, New South Wales, Australia.
Emely de Vet, are with the Consumption and Healthy Lifestyles, Wageningen University and Research, Wageningen, The Netherlands.
Annemien Haveman-Nies, are with the Consumption and Healthy Lifestyles, Wageningen University and Research, Wageningen, The Netherlands.
Tamara Bucher, are with the Priority Research Centre for Physical Activity and Nutrition (PRCPAN), University of Newcastle, Callaghan, New South Wales, Australia; with the School of Environmental and Life Sciences, College of Engineering, Science and Environment, University of Newcastle, Ourimbah, New South Wales, Australia.
Supporting Information
The following Supporting Information is available through the online version of this article at the publisher’s website.
Table S1 PRISMA 2020 checklist
Table S2 Search terms used for the systematic review
Table S3 Primary studies included in systematic reviews
Table S4 Summary of findings
References
- 1. Dudley DA, Cotton WG, Peralta LR.. Teaching approaches and strategies that promote healthy eating in primary school children: a systematic review and meta-analysis. Int J Behav Nutr Phys Act. 2015;12:1–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wechsler H, Devereaux RS, Davis M, et al. Using the school environment to promote physical activity and healthy eating. Prevent Med. 2000;31:S121–S137. [Google Scholar]
- 3. Van Cauwenberghe E, Maes L, Spittaels H, et al. Effectiveness of school-based interventions in Europe to promote healthy nutrition in children and adolescents: systematic review of published and ‘grey’ literature. Br J Nutr. 2010;103:781–797. [DOI] [PubMed] [Google Scholar]
- 4. Grosso G, Mistretta A, Turconi G, et al. Nutrition knowledge and other determinants of food intake and lifestyle habits in children and young adolescents living in a rural area of Sicily, South Italy. Public Health Nutr. 2013;16:1827–1836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. van Nassau F, Singh AS, van Mechelen W, et al. Implementation evaluation of school-based obesity prevention programmes in youth; how, what and why? Public Health Nutr. 2015;18:1531–1534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Methner S, Maschkowski G, Hartmann M.. The European School Fruit Scheme: impact on children’s fruit and vegetable consumption in North Rhine-Westphalia, Germany. Public Health Nutr. 2017;20:542–548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Keihner A, Rosen N, Wakimoto P, et al. Impact of California Children’s Power Play! Campaign on fruit and vegetable intake and physical activity among fourth-and fifth-grade students. Am J Health Promot. 2017;31:189–191. [DOI] [PubMed] [Google Scholar]
- 8. Contento I, Balch GI, Bronner YL, et al. The effectiveness of nutrition education and implications for nutrition education policy, programs, and research: a review of research. J Nutr Educ (USA) .1995;27:277–418. [Google Scholar]
- 9. Falkner NH, Neumark‐Sztainer D, Story M, et al. Social, educational, and psychological correlates of weight status in adolescents. Obes Res. 2001;9:32–42. [DOI] [PubMed] [Google Scholar]
- 10. Datar A, Sturm R.. Childhood overweight and elementary school outcomes. Int J Obes. 2006;30:1449–1460. [DOI] [PubMed] [Google Scholar]
- 11. World Health Organization. Obesity and overweight. 2021. Available at: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. Accessed October 12, 2021.
- 12. Kayode OO. Diet and obesity. In: Takada A, Himmerich H, eds. Psychology and Pathophysiological Outcomes of Eating. Adeleke University, Ede, Nigeria: IntechOpen; 2021:237. [Google Scholar]
- 13. Grantham-McGregor S. A review of studies of the effect of severe malnutrition on mental development. J Nutr. 1995;125:2233S–2238S. [DOI] [PubMed] [Google Scholar]
- 14. Florence MD, Asbridge M, Veugelers PJ.. Diet quality and academic performance. J Sch Health. 2008;78:209–215. [DOI] [PubMed] [Google Scholar]
- 15. World Health Organization. Healthy diet. 2020. Available at: https://apps.who.int/iris/bitstream/handle/10665/325828/EMROPUB_2019_en_23536.pdf. Accessed October 12, 2021.
- 16. Fitzgerald N, Spaccarotella K.. Barriers to a healthy lifestyle: from individuals to public policy—an ecological perspective. J Extens 2009;47:1–8. [Google Scholar]
- 17. Sawyer AD, van Lenthe F, Kamphuis CB, et al. ; PEN Consortium. Dynamics of the complex food environment underlying dietary intake in low-income groups: a systems map of associations extracted from a systematic umbrella literature review. Int J Behav Nutr Phys Act. 2021;18:96–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Contento IR, Manning AD, Shannon B.. Research perspective on school-based nutrition education. J Nutr Educ. 1992;24:247–260. [Google Scholar]
- 19. Evans CE, Christian MS, Cleghorn CL, et al. Systematic review and meta-analysis of school-based interventions to improve daily fruit and vegetable intake in children aged 5 to 12 y. Am J Clin Nutr. 2012;96:889–901. [DOI] [PubMed] [Google Scholar]
- 20. Mak T, Bonsmann S, Genannt S, et al. How to Promote Fruit and Vegetable Consumption in Schools: A Toolkit. Luxembourg: Publications Office of the European Union; 2016.
- 21. Singhal J, Herd C, Adab P, et al. Effectiveness of school‐based interventions to prevent obesity among children aged 4 to 12 years old in middle‐income countries: a systematic review and meta‐analysis. Obes Rev. 2021;22:e13105. [DOI] [PubMed] [Google Scholar]
- 22. Micha R, Karageorgou D, Bakogianni I, et al. Effectiveness of school food environment policies on children’s dietary behaviors: a systematic review and meta-analysis. PLoS One. 2018;13:e0194555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Grol R, Wensing M. Effective implementation of change in healthcare: A systematic approach. In: Grol R, Wensing M, Davis D, eds. Improving Patient Care: The Implementation of Change in Healthcare. 2nd edition. Oxford: John Wiley & Sons; 2013:40–63. [Google Scholar]
- 24. Reinaerts EB, De Nooijer J, De Vries NK.. Fruit and vegetable distribution program versus a multicomponent program to increase fruit and vegetable consumption: which should be recommended for implementation? J Sch Health. 2007;77:679–686. [DOI] [PubMed] [Google Scholar]
- 25. Michie S, Wood CE, Johnston M, et al. Behaviour change techniques: the development and evaluation of a taxonomic method for reporting and describing behaviour change interventions (a suite of five studies involving consensus methods, randomised controlled trials and analysis of qualitative data). Health Technol Assess. 2015;19:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hartling L, Chisholm A, Thomson D, et al. A descriptive analysis of overviews of reviews published between 2000 and 2011. PloS One. 2012;7:e49667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Aromataris E, Fernandez R, Godfrey C, et al. Chapter 10: Umbrella Reviews. In: Aromataris E, Munn Z, eds. JBI Manual for Evidence Synthesis. JBI; 2020. Available at: https://synthesismanual.jbi.global. 10.46658/JBIMES-20-11. [DOI]
- 28. Covidence systematic review software. Veritas Health Innovation. www.covidence.org. Accessed June 1, 2020.
- 29. Guyatt GH, Oxman AD, Vist GE, et al. ; GRADE Working Group. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Balshem H, Helfand M, Schünemann HJ, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. 2011;64:401–406. [DOI] [PubMed] [Google Scholar]
- 31. Guyatt GH, Oxman AD, Kunz R, et al. ; GRADE Working Group. What is “quality of evidence” and why is it important to clinicians? BMJ. 2008;336:995–998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Langer G, Meerpohl JJ, Perleth M, et al. GRADE guidelines: 1. Introduction–GRADE evidence profiles and summary of findings tables. Z Evid Fortbild Qual Gesundhwes. 2012;106:357–368. [DOI] [PubMed] [Google Scholar]
- 33. Chai LK, Collins C, May C, et al. Effectiveness of family-based weight management interventions for children with overweight and obesity: an umbrella review. JBI Database System Rev Implement Rep. 2019;17:1341–1427. [DOI] [PubMed] [Google Scholar]
- 34. Cohen J. The earth is round (p<. 05). Am Psychol 1994;49:997. [Google Scholar]
- 35. Moher D, Liberati A, Tetzlaff J, et al. ; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Delgado-Noguera M, Tort S, Martínez-Zapata MJ, et al. Primary school interventions to promote fruit and vegetable consumption: a systematic review and meta-analysis. Prev Med. 2011;53:3–9. [DOI] [PubMed] [Google Scholar]
- 37. Langellotto GA, Gupta A.. Gardening increases vegetable consumption in school-aged children: a meta-analytical synthesis. Hortte. 2012;22:430–445. [Google Scholar]
- 38. Metcalfe JJ, Ellison B, Hamdi N, et al. A systematic review of school meal nudge interventions to improve youth food behaviors. Int J Behav Nutr Phys Act. 2020;17:1–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Morgan EH, Schoonees A, Sriram U, et al. Caregiver involvement in interventions for improving children's dietary intake and physical activity behaviors. Cochrane Database Syst Rev. 2020;1:CD012547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Silveira JA, Taddei JA, Guerra PH, et al. Effectiveness of school-based nutrition education interventions to prevent and reduce excessive weight gain in children and adolescents: a systematic review. J Pediatr (Rio J). 2011;87:382–392. [DOI] [PubMed] [Google Scholar]
- 41. Baranowski T, Baranowski J, Cullen KW, et al. Squire’s Quest!: dietary outcome evaluation of a multimedia game. Am J Prev Med. 2003;24:52–61. [DOI] [PubMed] [Google Scholar]
- 42. Battjes-Fries MC, van Dongen EJ, Renes RJ, et al. Unravelling the effect of the Dutch school-based nutrition programme Taste Lessons: the role of dose, appreciation and interpersonal communication. BMC Public Health. 2016;16:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Govula C, Kattelman K, Ren C.. Culturally appropriate nutrition lessons increased fruit and vegetable consumption in American Indian children. Topics Clin Nutr. 2007;22:239–245. [Google Scholar]
- 44. Panunzio MF, Antoniciello A, Pisano A, et al. Nutrition education intervention by teachers may promote fruit and vegetable consumption in Italian students. Nutr Res. 2007;27:524–528. [Google Scholar]
- 45. Schreiber J, Moerchen VA, Rapport MJ, et al. Experiential learning with children: an essential component of professional physical therapy education. Pediatr Phys Ther. 2015;27:356–367. [DOI] [PubMed] [Google Scholar]
- 46. McAleese JD, Rankin LL.. Garden-based nutrition education affects fruit and vegetable consumption in sixth-grade adolescents. J Am Diet Assoc. 2007;107:662–665. [DOI] [PubMed] [Google Scholar]
- 47. Horne PJ, Tapper K, Lowe C, et al. Increasing children's fruit and vegetable consumption: a peer-modelling and rewards-based intervention. Eur J Clin Nutr. 2004;58:1649–1660. [DOI] [PubMed] [Google Scholar]
- 48. Cooke LJ, Chambers LC, Añez EV, et al. Eating for pleasure or profit: the effect of incentives on children’s enjoyment of vegetables. Psychol Sci. 2011;22:190–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Thaler RH, Sunstein CR.. Nudge: improving decisions about health. Wealth Happiness. 2008;6:14–38. [Google Scholar]
- 50. Adams MA, Pelletier RL, Zive MM, et al. Salad bars and fruit and vegetable consumption in elementary schools: a plate waste study. J Am Dietetic Assoc. 2005;105:1789–1792. [DOI] [PubMed] [Google Scholar]
- 51. Cohen JF, Richardson SA, Cluggish SA, et al. Effects of choice architecture and chef-enhanced meals on the selection and consumption of healthier school foods: a randomized clinical trial. JAMA Pediatr. 2015;169:431–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Moore L, Tapper K.. The impact of school fruit tuck shops and school food policies on children’s fruit consumption: a cluster randomised trial of schools in deprived areas. J Epidemiol Commun Health. 2008;62:926–931. [DOI] [PubMed] [Google Scholar]
- 53. Bere E, Hilsen M, Klepp K-I.. Effect of the nationwide free school fruit scheme in Norway. Br J Nutr. 2010;104:589–594. [DOI] [PubMed] [Google Scholar]
- 54. Fogarty A, Antoniak M, Venn A, et al. Does participation in a population-based dietary intervention scheme have a lasting impact on fruit intake in young children? Int J Epidemiol. 2007;36:1080–1085. [DOI] [PubMed] [Google Scholar]
- 55. Eriksen K, Haraldsdóttir J, Pederson R, et al. Effect of a fruit and vegetable subscription in Danish schools. Public Health Nutr. 2003;6:57–63. [DOI] [PubMed] [Google Scholar]
- 56. Ashfield-Watt PA, Stewart EA, Scheffer JA.. A pilot study of the effect of providing daily free fruit to primary-school children in Auckland, New Zealand. Public Health Nutr. 2009;12:693–701. [DOI] [PubMed] [Google Scholar]
- 57. Tak NI, Te Velde SJ, Brug J.. Ethnic differences in 1-year follow-up effect of the Dutch Schoolgruiten Project–promoting fruit and vegetable consumption among primary-school children. Public Health Nutr. 2007;10:1497–1507. [DOI] [PubMed] [Google Scholar]
- 58. He M, Beynon C, Bouck MS, et al. Impact evaluation of the Northern Fruit and Vegetable Pilot Programme–a cluster-randomised controlled trial. Public Health Nutr. 2009;12:2199–2208. [DOI] [PubMed] [Google Scholar]
- 59. Bere E, Veierød MB, Klepp K-I.. The Norwegian School Fruit Programme: evaluating paid vs. no-cost subscriptions. Preventive Medicine. 2005;41:463–470. [DOI] [PubMed] [Google Scholar]
- 60. Mangunkusumo RT, Brug J, de Koning HJ, et al. School-based internet-tailored fruit and vegetable education combined with brief counselling increases children's awareness of intake levels. Public Health Nutr. 2007;10:273–279. [DOI] [PubMed] [Google Scholar]
- 61. Amaro S, Viggiano A, Di Costanzo A, et al. Kaledo, a new educational board-game, gives nutritional rudiments and encourages healthy eating in children: a pilot cluster randomized trial. Eur J Pediatr. 2006;165:630–635. [DOI] [PubMed] [Google Scholar]
- 62. Raby Powers A, Struempler BJ, Guarino A, et al. Effects of a nutrition education program on the dietary behavior and nutrition knowledge of second‐grade and third‐grade students. J School Health. 2005;75:129–133. [PubMed] [Google Scholar]
- 63. Perry CL, Mullis RM, Maile MC.. Modifying the eating behavior of young children. J Sch Health. 1985;55:399–402. [DOI] [PubMed] [Google Scholar]
- 64. Domel SB, Baranowski T, Davis H, et al. Development and evaluation of a school intervention to increase fruit and vegetable consumption among 4th and 5th grade students. Journal of Nutrition Education. 1993;25:345–349. [Google Scholar]
- 65. Auld GW, Romaniello C, Heimendinger J, et al. Outcomes from a school‐based nutrition education program alternating special resource teachers and classroom teachers. J Sch Health. 1999;69:403–408. [DOI] [PubMed] [Google Scholar]
- 66. Bell CG, Lamb MW.. Nutrition education and dietary behavior of fifth graders. J Nutr Educ. 1973;5:196–199. [Google Scholar]
- 67. Smolak L, Levine MP, Schermer F.. A controlled evaluation of an elementary school primary prevention program for eating problems. J Psychosom Res. 1998;44:339–353. [DOI] [PubMed] [Google Scholar]
- 68. Spiegel SA, Foulk D.. Reducing overweight through a multidisciplinary school‐based intervention. Obesity (Silver Spring). 2006;14:88–96. [DOI] [PubMed] [Google Scholar]
- 69. Friel S, Kelleher C, Campbell P, et al. Evaluation of the Nutrition Education at Primary school (NEAPS) programme. Public Health Nutr. 1999;2:549–555. [DOI] [PubMed] [Google Scholar]
- 70. Head MK. A nutrition education program at three grade levels. J Nutr Educ. 1974;6:56–59. [Google Scholar]
- 71. Shannon B, Chen AN.. A three-year school-based nutrition education study. J Nutr Educ. 1988;20:114–124. [Google Scholar]
- 72. Parmer SM, Salisbury-Glennon J, Shannon D, et al. School gardens: an experiential learning approach for a nutrition education program to increase fruit and vegetable knowledge, preference, and consumption among second-grade students. J Nutr Educ Behav. 2009;41:212–217. [DOI] [PubMed] [Google Scholar]
- 73. Liquori T, Koch PD, Contento IR, et al. The Cookshop Program: outcome evaluation of a nutrition education program linking lunchroom food experiences with classroom cooking experiences. J Nutr Educ. 1998;30:302–313. [Google Scholar]
- 74. Greene KN, Gabrielyan G, Just DR, et al. Fruit-promoting smarter lunchrooms interventions: results from a cluster RCT. Am J Prev Med. 2017;52:451–458. [DOI] [PubMed] [Google Scholar]
- 75. Schwartz MB. The influence of a verbal prompt on school lunch fruit consumption: a pilot study. Int J Behav Nutr Phys Act. 2007;4:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Crespo NC, Elder JP, Ayala GX, et al. Results of a multi-level intervention to prevent and control childhood obesity among Latino children: the Aventuras Para Niños Study. Ann Behav Med. 2012;43:84–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. World Health Organization. Diet, Nutrition, and the Prevention of Chronic Diseases: Report of a Joint WHO/FAO Expert Consultation. Vol. 916.World Health Organization; 2003. [Google Scholar]
- 78. Worsley A. Nutrition knowledge and food consumption: can nutrition knowledge change food behaviour? Asia Pac J Clin Nutr. 2002;11:S579–S585. [DOI] [PubMed] [Google Scholar]
- 79. Cox DN, Baird DL, Rebuli MA, et al. Sensory characteristics of vegetables consumed by Australian children. Public Health Nutr. 2022;25:1205–1216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Pendergast D, Garvis S, Kanasa H.. Insight from the public on home economics and formal food literacy. Family Consumer Sci Res J. 2011;39:415–430. [Google Scholar]
- 81. Haß J, Hartmann M.. What determines the fruit and vegetables intake of primary school children?-An analysis of personal and social determinants. Appetite. 2018;120:82–91. [DOI] [PubMed] [Google Scholar]
- 82. Reynolds KD, Bishop DB, Chou C-P, Xie B, et al. Contrasting mediating variables in two 5-a-day nutrition intervention programs. Prev Med. 2004;39:882–893. [DOI] [PubMed] [Google Scholar]
- 83. Triches RM, Giugliani ERJ.. Obesity, eating habits and nutritional knowledge among school children. Rev Saude Publica. 2005;39:541–547. [DOI] [PubMed] [Google Scholar]
- 84. Krølner R, Rasmussen M, Brug J, et al. Determinants of fruit and vegetable consumption among children and adolescents: a review of the literature. Part II: qualitative studies. Int J Behav Nutr Phys Act. 2011;8:112– 138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Rasmussen M, Krølner R, Klepp K-I, et al. Determinants of fruit and vegetable consumption among children and adolescents: a review of the literature. Part I: quantitative studies. Int J Behav Nutr Phys Act. 2006;3:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Kolasa KM, Peery A, Harris NG, et al. Food literacy partners program: a strategy to increase community food literacy. Topics Clin Nutr. 2001;16:1–10. [Google Scholar]
- 87. Colatruglio S, Slater J.. Food literacy: bridging the gap between food, nutrition and well-being. In: Deer F, Falkenberg T, Mcmillan B, Sims L, eds. Sustainable Well-Being: Concepts, Issues, and Educational Practices. Winnipeg: Education for Sustainable Well-Being (ESWB) Press; 2014;37–55. [Google Scholar]
- 88. Palumbo R. Sustainability of well-being through literacy. The effects of food literacy on sustainability of well-being. Agric Agric Sci Procedia. 2016;8:99–106. [Google Scholar]
- 89. Pendergast D, Dewhurst Y.. Home economics and food literacy: an international investigation. Int J Home Econ. 2012;5:245–263. [Google Scholar]
- 90. Nowak AJ, Kolouch G, Schneyer L, et al. Building food literacy and positive relationships with healthy food in children through school gardens. Child Obes. 2012;8:392–395. [DOI] [PubMed] [Google Scholar]
- 91. Krause C, Sommerhalder K, Beer-Borst S, et al. Just a subtle difference? Findings from a systematic review on definitions of nutrition literacy and food literacy. Health Promot Int 2018;33:378–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Baranowski T, Cerin E, Baranowski J.. Steps in the design, development and formative evaluation of obesity prevention-related behavior change trials. Int J Behav Nutr Phys Act. 2009;6:6–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Martin J, Chater A, Lorencatto F.. Effective behaviour change techniques in the prevention and management of childhood obesity. Int J Obes (Lond). 2013;37:1287–1294. [DOI] [PubMed] [Google Scholar]
- 94. Michie S, Ashford S, Sniehotta FF, et al. A refined taxonomy of behaviour change techniques to help people change their physical activity and healthy eating behaviours: the CALO-RE taxonomy. Psychol Health. 2011;26:1479–1498. [DOI] [PubMed] [Google Scholar]
- 95. Morgan PJ, Warren JM, Lubans DR, et al. The impact of nutrition education with and without a school garden on knowledge, vegetable intake and preferences and quality of school life among primary-school students. Public Health Nutr. 2010;13:1931–1940. [DOI] [PubMed] [Google Scholar]
- 96. Bucher T, Rollo ME, Smith SP, et al. Position paper on the need for portion-size education and a standardised unit of measurement. Health Promot J Austr. 2017;28:260–263. [DOI] [PubMed] [Google Scholar]
- 97. Strachan J, Pavie-Latour V.. Food for thought: shouldn't we actually target food advertising more towards kids and not less? Int J Market Res. 2008;50:13–27. [Google Scholar]
- 98. Chassiakos YLR, Radesky J, Christakis D, et al. ; Council on Communications and Media. Children and adolescents and digital media. Pediatrics. 2016;138:e20162593. [DOI] [PubMed] [Google Scholar]
- 99. Von Normann K. The impact of lifestyles and food knowledge on the food patterns of German children. Int J Consumer Stud. 2009;33:382–391. [Google Scholar]
- 100.Elliott C. Healthy food looks serious: How children interpret packaged food products. Can J Commun. 2009;34:359–380. [Google Scholar]
- 101. Whitrow M, Moran L, Davies M, et al. Core food intakes of Australian children aged 9–10 years: nutrients, daily servings and diet quality in a community cross‐sectional sample. J Hum Nutr Diet. 2016;29:449–457. [DOI] [PubMed] [Google Scholar]
- 102. Murimi MW, Moyeda-Carabaza AF, Nguyen B, et al. Factors that contribute to effective nutrition education interventions in children: a systematic review. Nutr Rev. 2018;76:553–580. [DOI] [PubMed] [Google Scholar]
- 103. Verdonschot A, De Vet E, Van Rossum J, et al. Education or provision? A comparison of two school-based fruit and vegetable nutrition education programs in the Netherlands. Nutrients. 2020;12:3280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Klepp K-I, Pérez-Rodrigo C, De Bourdeaudhuij I, et al. Promoting fruit and vegetable consumption among European schoolchildren: rationale, conceptualization and design of the pro children project. Ann Nutr Metab. 2005;49:212–220. [DOI] [PubMed] [Google Scholar]
- 105. Verdonschot A, de Vet E, van Seeters N, et al. Caregivers’ role in the effectiveness of two Dutch school-based nutrition education programmes for children aged 7–12 years old. Nutrients. 2021;13:140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Bellows LL, Johnson SL, Davies PL, et al. The Colorado LEAP study: rationale and design of a study to assess the short term longitudinal effectiveness of a preschool nutrition and physical activity program. BMC Public Health. 2013;13:1146–1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Brint S. Chapter 1. Schools as social institutions. In: Brint S, ed. Schools and Societies. 3rd edition.Redwood City: Stanford University Press; 2017:1–31. [Google Scholar]
- 108. Domitrovich CE, Bradshaw CP, Poduska JM, et al. Maximizing the implementation quality of evidence-based preventive interventions in schools: a conceptual framework. Adv Sch Ment Health Promot. 2008;1:6–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.