Abstract
A healthy diet is essential to prevent childhood obesity, however, adherence to a healthy diet is challenging. The aim of this study was to give a comprehensive overview of the literature investigaating associations between food and beverages and overweight/obesity in children and adolescents in order to identify dietary risk factors. A systematic search was performed in four databases and observational studies were included. Meta-analysis was performed using the random effect model. Sixty records met inclusion criteria and 14 different food or beverage categories were identified. A higher intake of sugar-sweetened beverages increased the odds of overweight/obesity by 1.20 (p < 0.05) (n = 26) and higher intake of fast food increased the odds of overweight/obesity by 1.17 (p < 0.05) (n = 24). Furthermore, higher intake of meat (OR 1.02, p < 0.05 (n:7)) and refined grains (OR 1.28, p < 0.05 (n:3)) was associated with an increased risk of overweight/obesity. In contrast, higher intake of whole grain (OR 0.86, p = 0.04 (n:5)) and more surprisingly sweet bakery (OR 0.59, p < 0.05 (n:3)) was associated with a decreased risk of overweight/obesity. In conclusion, a higher intake of sugar-sweetened beverages and a higher intake of fast food was identified as the primary dietary risk factors for overweight/obesity. Future research is needed to strengthen the generalizability of these results.
Keywords: nutrition, dietary risk factors, childhood obesity, adiposity, BMI-SDS, weight development
1. Introduction
Childhood obesity is reaching alarming proportions in many countries and due to the complex interplay between genetic, psychosocial, and environmental factors the progress in tackling childhood obesity is challenging [1]. Despite an obvious complexity, a healthy diet is still essential to prevent childhood obesity and the development of obesity-related diseases in adulthood [2]. A healthy diet is characterized as a balanced diet including an adequate intake of whole grains, milk and dairy, fish, fruits, and vegetables whereas a dietary pattern rich in meat, soda, fried food, instant noodles, burgers, and pizza is recognized as being unhealthy and obesogenic [2,3,4]. A recent systematic review also suggested that children and adolescents who adhere to dietary patterns composed of unhealthy foods such as the Western diet are more likely to develop obesity [5]; however, evidence supporting beneficial effects on weight development in children when following a healthy diet is scare [6]. Furthermore, most dietary intervention studies show no consistent effect on changes in body mass index in children [7] and adherence to dietary intervention principles seem to decrease over time [8] which highlights the importance of ensuring that dietary advices are converted into sustained dietary habits.
Therefore, the aim of the present study was to summarize the literature investigating association between food and beverages categories and overweight/obesity in children and adolescents. A comprehensive overview of the current literature within this area will help identify lack of knowledge, provide valuable insight on dietary risk factors, and potentially provide simple strategies to promote healthy weight development in children and adolescents.
2. Materials and Methods
2.1. Data Sources, Search Strategies, and Search Process
The study was designed according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses guidelines (PRISMA) and registered at PROSPERO (ID number: CRD42020173201) [9].
A systematic search was initiated in PubMed, EMBASE, SCOPUS, and Web of Science in March 2020 and in accordance with the PROSPERO protocol the initial search included both randomized controlled trials and longitudinal and cross-sectional studies. A systematic review and meta-analysis based on eligible randomized controlled trials was finalized in July 2021 and has already been published [10] why this paper focuses on evaluating eligible observational studies (i.e., longitudinal and cross-sectional studies). In August 2022, the systematic search was renewed to identify eligible observational studies published within the last two years.
In all four databases the search block for the population (#1) was combined with each search block for the exposure separately (#2 to #10). The search strategy from PubMed is shown in Table 1.
Table 1.
Search strategy used in the systematic literature review.
| Population | Exposure | |
|---|---|---|
| #1 “Body Mass Index”[Mesh] OR “Body Weight Maintenance”[Mesh] OR “Weight Loss”[Mesh] OR “Body Mass Index” OR “Weight Loss” OR “weight maintenance”; AND “child”[Mesh] OR “Adolescent”[Mesh] OR Child* OR adolescen*; AND “Pediatric Obesity”[Mesh] OR “Pediatric Obesity” OR “Childhood Obesity” Sort by: Most Recent | AND | #2 “Carbonated Beverages”[Mesh] OR “Sugar Sweetened Beverages”[Mesh] OR “Beverages”[Mesh] OR “Artificially Sweetened Beverages”[Mesh] OR Beverage* Sort by: Most Recent |
| #3 “Vegetables”[Mesh] OR “Fruit”[Mesh] OR “Salads”[Mesh] OR Vegetable* OR Fruit OR Salad* Sort by: Most Recent | ||
| #4 “Dairy Products”[Mesh] OR “Cheese”[Mesh] OR “Yogurt”[Mesh] OR Milk OR Dairy OR Cheese OR Yogurt Sort by: Most Recent | ||
| #5 “Fast Food”[Mesh] OR “Fast Food” Sort by: Most Recent | ||
| #6 “Seafood”[Mesh] OR “Meat”[Mesh] OR “Egg Proteins, Dietary”[Mesh] OR “Poultry”[Mesh] OR Seafood OR Meat OR Egg OR Poultry OR chicken OR fish Sort by: Most Recent | ||
| #7 “Candy”[Mesh] OR “Chocolate”[Mesh] OR “Snacks”[Mesh] OR Candy OR Chocolate OR Snacks OR Cake OR Sweets OR nuts Sort by: Most Recent | ||
| #8 “Whole Grains”[Mesh] OR “Dietary Fiber”[Mesh] OR Grain* OR “Dietary Fiber” Sort by: Most Recent | ||
| #9 potato* OR rice OR pasta Sort by: Most Recent |
The study selection process was conducted by the first reviewer (D.J.), and questionable records were sent to the second reviewer (J.B.) to assess eligibility. Any doubts or discrepancies were resolved by discussion with the third reviewer (L.B). All identified records were screened by title and abstract and full-text records were retrieved if the title and abstract met the predefined inclusion criteria. Second all full-texts were read carefully to evaluate the study eligibility.
www.covidence.org was used for review management.
2.2. Eligibility Criteria
Records were eligible for inclusion based on the following criteria stratified by participants/population, intervention/exposure and comparison, outcome measures and study design (PICOS) [11].
Participants/population: Records were included if investigating otherwise healthy children or adolescents (mean age between 5 and 18 years of age) with overweight and/or obesity or a mixed population of children or adolescents with normal weight and children or adolescents with overweight/obesity. Records were excluded if examining only non-overweight children or adolescents (ISO-Body Mass Index (BMI) < 25 kg/m2), athletes or adolescents who underwent bariatric surgery. Also records investigating children or adolescents with diagnosed non-alcoholic-fatty-liver disease, diabetes, or other comorbidities were excluded.
Intervention/exposure and comparison: Records were included if investigating higher consumption of a certain food or beverage (intervention/exposure) as compared with lower consumption of the same food or beverage (comparator) and if they investigated consumption of single food or beverage categories. Records were excluded if they investigated dietary patterns.
Outcome measures: Records were included if the primary outcome was overweight, overweight/obesity, and obesity categorized by an age-and-sex specific BMI comparable to international standards [12,13,14] and if they reported associations between overweight/obesity and food or beverage consumption as odds ratio (OR) and 95% confidence interval (95% CI). Records were excluded if they were not categorized by an age-and-sex-specific BMI; if they reported associations as correlation coefficients (β), mean (SD), or other; or if they did not adjust for any confounders.
Study design: Cross-sectional studies and longitudinal studies were included if they were written in English and published in peer-reviewed journals from 1 January 1990 until 31 August 2022.
2.3. Data Extraction and Coding Decisions
For the meta-analysis ORs and 95% CI for the highest consumption were directly extracted from the included records. Some records provided separate outcome measures for different levels of consumption (e.g., 0–1 cups/day, 1–2 cups/day and ≥2 cups/day). In these records, the lowest consumption was always coded as the reference value (OR = 1) and compared to the highest consumption reported. If necessary, the scale reported by the author was reversed. Some records reported outcome measures separately for overweight and obesity while others reported outcome measures for overweight/obesity combined. Whenever available, the outcome measures for the obesity category were extracted and otherwise the outcome measures for the overweight/obesity category were extracted. Data were extracted by the first reviewer (D.J.) and any doubts or questions concerning data extraction were resolved with the second reviewer (J.B.). Discrepancies were solved in discussion with the third reviewer (L.B.). Data extraction forms were created by the authors in Microsoft Excel and included author (year published), country, age (year), sex, study, dietary instrument, definition of high intake, sample size, adjustments, and study quality assessment.
2.4. Risk of Bias Assessment and Study Quality Assessment
The methodical quality of included records was assessed using an adapted version of The Newcastle-Ottawa Scale (NOS) for cross-sectional studies [15]. Representativeness of the sample, sample size, response rate, ascertainment of the exposure, adjustment for confounding factors with total energy intake evaluated as the most important factor, reliability of the outcome determination and appropriateness of statistical analysis was evaluated. A maximum of ten stars could be assigned to each study and more than six stars were considered high quality. Guidelines from The Grading of Recommendation Assessment, Development and Evaluation (GRADE) was used to evaluate study quality of evidence [16].
2.5. Statistical Analysis
Meta-analysis was carried out if three or more records investigated consumption of the same food or beverage. Whenever possible, age-divided meta-analysis was carried out investigating children, 5–11 years old and adolescents, 12–18 years old. Due to an assumption of heterogeneity between records e.g., in population, dietary instrument used, and the definition of “high intake”, a random effect-model was used. All meta-analyses were analyzed using a significance level of 0.05. Statistical heterogeneity was evaluated based on the Chi2 statistics and reported as a tau2 and I2 value below each forest plot [11]. If the heterogeneity was moderate to high (I2 > 50%), heterogeneity was investigated using subgroup analysis according to age (5–18 years, 5–11 years, 12–18 years) and funnel plots.
Stata software version 17.0 (StataCorp LLC, College Station, TX, USA) was used to perform meta-analyses.
3. Results
3.1. Description of Records
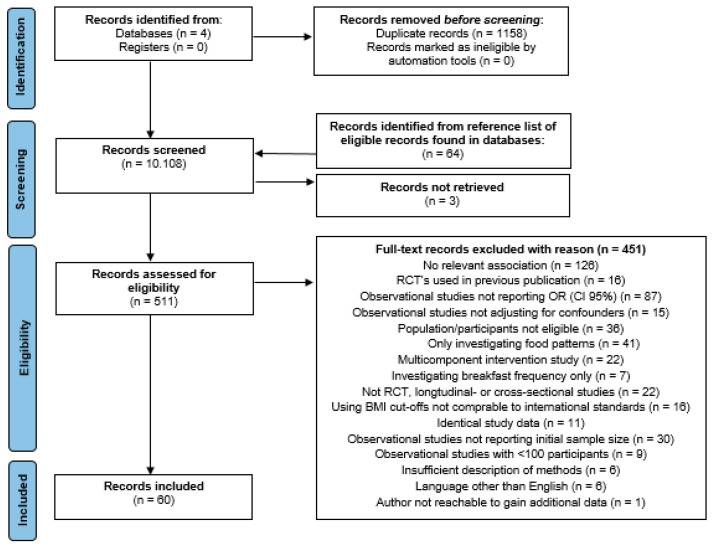
A total of 10,108 records were identified and 511 full-text records were screened for eligibility. In total, 451 full-text records were excluded due to various reasons of which 87 records were excluded because they did not report OR (95% CI) and 15 records were excluded because reported results were not adjusted for any confounders. Detailed flow-chart is available in Figure 1.
Figure 1.
Study selection process.
In total, 60 records including 242,061 participants were eligible for data synthesis. Based on the included records 14 different food or beverage categories could be identified. Most records included were cross-sectional studies and few were longitudinal studies. Food and beverage consumption were most often investigated using a self-administrated food-frequency questionnaire, but also one or two-day dietary records, interviews, and other types of questionnaires were used as dietary instrument. Dietary consumption was typically parent-reported for children and self-reported for adolescents (See Supplementary Table S1 for characteristics of included studies).
3.2. Synthesis of Results
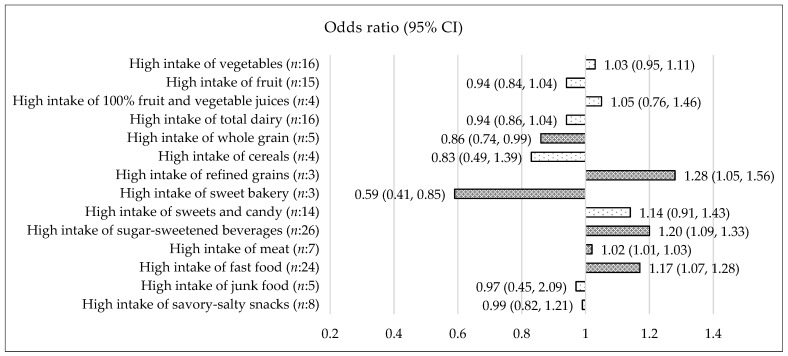
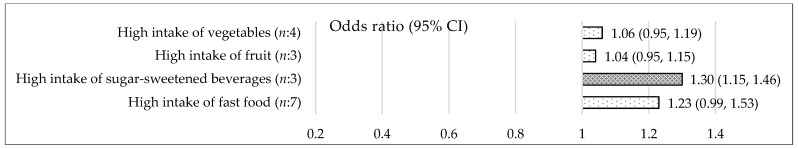
Vegetables: Based on 16 records (n:16) [17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32], the OR (95% CI) for higher intake of vegetables compared to lower intake of vegetables was 1.03 (0.95, 1.11) (p = 0.49) (I2 = 76.98%) in children and adolescents 5–18 years (Figure 2). In children 5–11 years, the OR (95% CI) was 1.04 (0.94, 1.16) (p = 0.43) (n:7) (Figure 3) and in adolescents 12–18 years, the OR (95% CI) was 1.06 (0.95, 1.19) (p = 0.28) (n:4) (Figure 4). The types of vegetables investigated were not specified.
Figure 2.
Association between a high intake of 14 different food and beverages categories and risk of overweight/obesity in children and adolescents 5–18 years. OR < 1 = decreased risk of overweight/obesity, OR > 1 = increased risk of overweight/obesity. Dark shades are significant (p ≤ 0.05). White shades are not significant. The forest-plots for each food or beverages category is available in Supplementary Figures S1–S15.
Figure 3.
Association between a high intake of eight different food and beverages categories and risk of overweight/obesity in children 5–11 years. OR < 1 = decreased risk of overweight/obesity, OR > 1 = increased risk of overweight/obesity. Dark shades are significant (p ≤ 0.05). White shades are not significant. The forest-plots for each food or beverages category is available in Supplementary Figures S16–S24.
Figure 4.
Association between a high intake of four different food and beverages categories and risk of overweight/obesity in adolescents 12–18 years. OR < 1 = decreased risk of overweight/obesity, OR > 1 = increased risk of overweight/obesity. Dark shades are significant (p ≤ 0.05). White shades are not significant. The forest-plots for each food or beverages category is available in Supplementary Figures S25–S28.
Fruit: Based on 15 records [17,18,19,20,23,25,27,28,29,30,31,33,34,35,36], the OR (95% CI) for higher intake of fruit compared to lower intake of fruit was 0.94 (0.84, 1.04) (p = 0.22) (I2 = 72.44%) in children and adolescents 5–18 years (Figure 2). In children 5–11 years, the OR (95% CI) was 0.73 (0.48, 1.11) (p = 0.14) (n:6) (Figure 3) and in adolescents 12–18 years, the OR (95% CI) was 1.04 (0.95, 1.15) (p = 0.39) (n:3) (Figure 4). Types of fruits investigated were not specified.
100% fruit and vegetables juices: Based on four records [29,37,38,39], the OR (95% CI) for higher intake of 100% fruit and vegetable juices versus lower intake of 100% fruit and vegetable juices was 1.05 (0.76, 1.46) (p = 0.77) (I2 = 78.61%) in children and adolescents 5–18 years (Figure 2). 100% fruit and vegetable juices were defined as 100% orange juices, 100% fruit juices/drinks, and fruit/vegetable juice.
Total dairy: Based on 16 records [17,22,25,27,28,39,40,41,42,43,44,45,46,47,48,49], the OR (95% CI) for higher intake of total dairy compared to lower intake of total dairy was 0.94 (0.86, 1.04) (p = 0.26) (I2 = 88.50%) in children and adolescents 5–18 years (Figure 2). Excluding the two outcome measure from the meta-analysis, investigating cheese specifically [22,27] did not change the results (data not shown). In children 5–11 years, the OR (95% CI) for a higher intake of total dairy compared to a lower intake of total dairy was 0.92 (0.84, 1.01) (p = 0.08) (n:8) (Figure 3). When excluding cheese, the OR (95% CI) for a higher intake of milk and dairy compared to a lower intake of milk and dairy was 0.90 (0.80, 1.00) (p = 0.06) (n:7) (see Supplementary Figure S20). Total dairy was defined to include white milk, flavored/chocolate milk, dairy and cheese with varying fat content.
Whole grain: Based on five records [17,22,28,50,51], the OR (95% CI) for higher intake of whole grain compared to lower intake of whole grain was 0.86 (0.74, 0.99) (p = 0.04) in children and adolescents 5–18 years (Figure 2). In children 5–11 years, the OR (95% CI) was 0.89 (0.71, 1.11) (p = 0.30) (n:3) (Figure 3). Whole grain was defined as whole grain, grains, bread/grains, and dietary fiber.
Cereals: Based on four records [26,27,40,42], the OR (95% CI) for higher intake of cereals versus lower intake of cereals was 0.83 (0.49, 1.39) (p = 0.47) (I2 = 74.49%) in children and adolescents 5–18 years (Figure 2). Cereals were defined as ready to eat cereal, bread and cereal, porridge, and instant noodles.
Refined grains: Based on three records [24,35,40], the OR (95% CI) for higher intake of refined grains versus lower intake of refined grains was 1.28 (1.05, 1.56) (p < 0.05) in children and adolescents 5–18 years (Figure 2). Refined grains were defined as buns, bread foods, or bread and cereals combined.
Sweet bakery: Based on three records [23,26,27], the OR (95% CI) for higher intake of sweet bakery versus lower intake of sweet bakery was 0.59 (0.41, 0.85) (p < 0.05) (I2 = 53.34%) in children and adolescents 5–18 years (Figure 2). Sweet bakery was defined as pastries, cakes, doughnuts, and pies.
Sweets and candy: Based on 14 records [19,22,23,25,26,27,35,38,40,49,52,53,54,55], the OR (95% CI) for higher intake of sweets and candy compared to lower intake of sweets and candy was 1.14 (0.91, 1.43) (p = 0.24) (I2 = 91.95%) in children and adolescents 5–18 years (Figure 2). In children 5–11 years, the OR (95% CI) was 1.50 (0.91, 2.48) (p = 0.11) (n:6) (Figure 3). Sweets and candy was defined as candy, chocolate, ice cream, sugar, and sweets.
Sugar sweetened beverages: Based on 26 records [17,19,21,22,23,25,29,33,39,40,41,42,43,45,52,53,56,57,58,59,60,61,62,63,64,65], the OR (95% CI) for higher intake of sugar-sweetened beverages versus lower intake of sugar-sweetened beverages was 1.20 (1.09, 1.33) (p < 0.05) (I2 = 79.34%) in children and adolescents 5–18 years (Figure 2). In children 5–11 years, the OR (95% CI) was 1.23 (1.10, 1.38) (p < 0.05) (n:12) (Figure 3) and in adolescents 12–18 years of age, the OR (95% CI) was 1.30 (1.15, 1.46) (p < 0.05) (n:3) (Figure 4). Sugar-sweetened beverages were defined as beverages with sugar e.g., soft drinks, sugary beverages, sweetened beverages, and soda. Records investigating 100% fruit/vegetables juices and records including diet drinks were excluded.
Meat: Based on seven records [19,22,27,28,32,40,42], the OR (95% CI) for higher intake of meat compared to lower intake of meat was 1.02 (1.01, 1.03) (p < 0.05) in children and adolescents 5–18 years. However, this result was driven primarily by the result from Chen et al. [32] due to a large sample size (Figure 2). When excluding Chen et al. from the meta-analysis, no association between meat intake and overweight/obesity was found (p = 0.57) (data not shown). Meat was defined as mixed meats, red meat, meat products, meat and equivalent, meta/fish/eggs, and sausage.
Fast food: Based on 24 records [18,19,20,23,25,27,29,30,31,35,40,42,52,54,55,59,66,67,68,69,70,71,72,73], the OR (95% CI) for higher intake of fast food versus lower intake of fast food was 1.17 (1.07, 1.28) (p < 0.05) (I2 = 56.44) in children and adolescents 5–18 years (Figure 2). In children 5–11 years, the OR (95% CI) was 1.27 (1.10,1.46) (p < 0.05) (n:8) (Figure 3) and in adolescents 12–18 years, the OR (95% CI) was 1.23 (0.99, 1.53) (p = 0.06) (n:7) (Figure 4). Fast food was defined as pizza, French fries, burgers, fried potatoes, fast or fatty foods, and fried food.
Junk food: Based on five records [20,24,28,60,74], the OR (95% CI) for higher intake of junk food versus lower intake of junk food was 0.97 (0.45, 2.09) (p = 0.94) (I2 = 86.06%) in children and adolescents 5–18 years (Figure 2). Junk food was defined as high-fat and/or high-sugar foods e.g., sugar-sweetened beverages, pastries, candies, French fries, chips, cakes, and fatty/processed meat.
Savory-salty snacks: Based on eight records [22,23,25,27,29,30,52,53], the OR (95% CI) for higher intake of savory-salty snacks compared to lower intake of savory-salty snacks was 0.99 (0.82, 1.21) (p = 0.96) (I2 = 78.54) in children and adolescents 5–18 years (Figure 2). In children 5–11 years, the OR (95% CI) was 1.01 (0.47, 2.18) (p = 0.97) (n:4) (Figure 3). Savory-salty snacks were defined as chips/fried potatoes, crisps, popcorn, peanuts, and corn chips.
3.3. Risk of Bias Assessment and Study Quality Assessment
Risk of bias assessment using NOS showed that most records were considered high quality (see Supplementary Table S1). However, only few records presented a power calculation and reported a total response rate. Most records did not compare characteristics between respondents and non-respondents, and furthermore, most included records did not adjust for total energy intake, which was evaluated as the most important confounding factor. Due to the study design of included studies, study quality of evidence was evaluated as low to very low for all outcomes [75].
3.4. Subgroup Analysis and Publication Bias
Most meta-analysis reported a moderate to high heterogeneity which was investigated using subgroups analysis according to age groups (5–11 years, 12–18 years, 5–18 years) and funnel plots. Only the subgroup analysis investigating sweets and candy showed a significant difference between age groups, which could explain the high heterogeneity reported. Investigating heterogeneity by funnel plots showed that the results concerning fast food consumption, sweets and candy consumption, and fruit consumption could be affected by publication bias. Furthermore, the moderate to high heterogeneity could be due to the different definitions of e.g., cereals, sugar-sweetened beverages and dairy, and the variation in high consumption vs. low consumption between records (see Supplementary Figures S29–S39).
4. Discussion
This systematic review and meta-analysis identified higher intake of sugar-sweetened beverages and higher intake of fast food to be the main dietary risk factors for overweight/obesity in children and adolescents 5–18 years of age. In addition, higher intake of meat and a higher intake of refined grains were also associated with an increased risk of overweight/obesity; however, these results were based on only a few records. Only higher intake of whole grain and more surprisingly higher intake of sweet bakery were associated with a decreased risk of overweight/obesity in children and adolescents 5–18 years of age.
Findings from the present study suggest that reducing the intake of sugar-sweetened beverages as well as fast food should be of highest priority to promote healthy weight development among children and adolescents. Based on the present result, a higher intake of sugar-sweetened beverages compared to a lower intake of sugar-sweetened beverages was associated with an increased risk of overweight/obesity in 5–18-year-olds (i.e., 12–18-year-olds and 5–11-year-olds). These results are essentially in line with three previous systematic reviews and meta-analysis [76,77,78]. A way to attenuate the deleterious effects of sugar-sweetened beverages could be to replace these with non-caloric beverages or flavored milk, which seems to have beneficial effects reducing body fat [10]. Currently there is no universal consensus on the definition of sugar-sweetened beverages [79] and in the present meta-analysis, sugar-sweetened beverages include a variety of beverages with sugar. Furthermore, the definition of high intake varies between studies, which altogether might explain the high heterogeneity reported. Nevertheless, these findings and a substantial body of evidence demonstrating a higher intake of sugar-sweetened beverages to increase the risk of overweight/obesity and a higher risk of developing type 2 diabetes, cardiovascular disease, and some cancers [76,77,78,79] show that reducing the intake of sugar-sweetened beverages should be a cornerstone in weight management in children and adolescents.
Based on this systematic review, a higher intake of fast food defined as pizza, French fries, burgers, fried potatoes, fast/fatty foods, and fried food was identified as a dietary risk factor for overweight/obesity in children and adolescents. In children and adolescents, the association between fast food consumption and overweight/obesity is often investigated in relation to fast food access or visits at fast food restaurants [80,81]. In a recent systematic review and meta-analysis, fast food restaurant access was positively associated with fast food consumption. However, only about half of the cohort studies and one-third of the cross-sectional studies reported a positive association between access to fast food restaurants and measures of overweight/obesity and when using BMI-related continuous measures most studies reported no association between access to fast food restaurants and overweight/obesity [81]. Likewise, another systematic review and meta-analysis reported no association between fast food consumption and childhood obesity [76]. The present meta-analysis investigating children and adolescents 5–18 years of age presented with a moderate heterogeneity and investigating the heterogeneity by funnel plots showed that these results could be affected by publication bias. Furthermore, the definition of fast food includes a variety of high-fat foods and several of included studies are not adjusting for total energy intake which altogether could explain the heterogeneity reported. Thus, the evidence supporting a direct association between fast food consumption and overweight/obesity in children and adolescents is scare, and still more high quality evidence is needed.
The results of this systematic review and meta-analysis indicate that a higher intake of meat is associated with an increased risk of overweight/obesity in children and adolescents. However, this result is driven primarily by one study [32] and therefore it must be interpreted with outmost caution. Evidence supporting this association is scare and a recent systematic review and meta-analysis investigating the association between consumption of red meat and overweight/obesity across all ages found no association [82]. In adults, the evidence demonstrating a positive association between meat intake and overweight/obesity is more robust [83,84], but different types of meat (e.g., pork, veal, lamb, red meat) is typically investigated together which could affect the estimate of association.
In the present systematic review and meta-analysis, a higher intake of refined grains was found to be associated with an increased risk of overweight/obesity and in contrast a higher intake of whole grain was associated with a decreased risk of overweight/obesity. These results are essentially in line with the previous studies in adults [84,85] and also in accordance with the current dietary guidelines recommending children, adolescents, and adults to choose whole grain when eating bread foods and cereals [3,4,86]. However, the meta-analysis investigating refined grains was based on only three records and the meta-analysis investigating whole grain was based on only five records why these results must be interpreted with caution. Thus, the evidence supporting these associations in children and adolescents need to be substantiated with more high quality evidence.
To some surprise, a higher intake of sweet bakery defined as pastries, cakes, doughnuts, and pies was found to be associated with a decreased risk of overweight/obesity in children and adolescents. One theory explaining this association could be that sweet bakery is more satiating than sugar from liquids and candy and therefore could be compensating for other calories. However, the most plausible explanation is that the reliability of this result is questionable due to study limitations, e.g., this result is based on only three records, only one of the included studies is adjusting for total energy intake and the meta-analysis presented with a high heterogeneity. Moreover, evidence supporting this association is scare, therefore the result must be interpreted with outmost caution [87]. Hence, added sugar in food should still be minimized and future research investigating children and adolescents needs to investigate the impact of sugar consumption on overweight/obesity and metabolic health in the absence of a positive energy balance.
Based on this systematic review and meta-analysis, higher intake of total dairy was not associated with overweight/obesity in children and adolescents. However, higher intake of milk and dairy (cheese excluded) was non-significantly associated with a decreased risk of overweight/obesity in children 5–11 years (p = 0.06). This tendency is in line with results from a recent systematic review and meta-analysis of randomized controlled trials, demonstrating a beneficial effect of higher-dairy diets (600–1000 mL) compared to lower-dairy diets (0–500 mL) by increasing lean body mass and reducing body fat in children and adolescents [10]. Evidence suggests that high intake of dairy is associated with a reduced risk of overweight/obesity in children and adolescents [88,89] and a recent meta-analysis of randomized controlled trials also concluded that children and adolescents consuming milk and milk products were more likely to achieve a lean body phenotype [90]. The present meta-analysis investigating dairy presented with a high heterogeneity possibly due to the different types of dairy investigated. Future research investigating dairy should therefore aim at differentiating between different milk- and cheese-products and also investigate smaller children and older children separately.
Weight management programs do almost always encourage children, adolescents, and their families to eat plenty of fruit and vegetables. However, in the present systematic review and meta-analysis, a higher intake of fruit or vegetables was neither positive nor negatively associated with overweight/obesity in children and adolescents. Fruit and vegetables are often investigated in combination and evidence suggests that diets including fruit and vegetables among other “healthy” foods, are associated with lower likelihood of overweight/obesity in children and adolescents [5,91]. However, for some children and adolescents the consumption of fruit and/or vegetables might be add-on calories which could explain the lack of association. Thus, future research investigating the effect of fruit and vegetables should differentiate between different fruits and vegetables and be conducted in a isocaloric randomized controlled setting.
Results from the present systematic review and meta-analysis must be interpreted in the light of several limitations. First, the study design of the included records limits inference of causality. Second, a small number of records were included in some meta-analysis. Third, only few of the included records adjusted for total energy intake, which is highly relevant and important when investigating associations between diet and weight development. Fourth, different instruments were used to evaluate dietary consumption. Fifth, several of the included records did not provide adequate description of the food or beverages investigated e.g., types of fruit and vegetables and the definition of low versus high consumption varied between records.
5. Conclusions
Based on the present systematic review and meta-analysis, a higher intake of sugar-sweetened beverages and a higher intake of fast food was identified as dietary risk factors for overweight/obesity in children and adolescents. Furthermore, a higher intake of meat and a higher intake of refined grains were also associated with an increased risk of overweight/obesity, whereas higher consumption of whole grain and a higher intake of sweet bakery were associated with a decreased risk. Due to a small number of records included in some of the meta-analysis, heterogeneity between records and lack of causality, these results must be interpreted with caution. Nevertheless, this systematic review and meta-analysis underlines that reducing the intake of sugar-sweetened beverages and fast food should be a priority to promote healthy weight development in children and adolescents and furthermore, that future research is needed to investigate associations between consumption of food and beverages and childhood obesity.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/nu15030764/s1. Table S1: Characteristics of included studies and ROB assessment of each study. Figures S1–S15: Individual forest plots (results) for each food and beverage category investigating children and adolescents 5–18 years of age. Figures S16–S24: Individual forest plots (results) for each food and beverage category investigating children and adolescents 5–11 years of age. Figures S25–S28: Individual forest plots (results) for each food and beverage category investigating children and adolescents 12–18 years of age. Figures S29–S39: Subgroup analysis and funnel plots investigating heterogeneity. References [92,93] are cited in the supplementary materials
Author Contributions
D.D.J., L.B. and J.M.B. designed the research and developed the protocol; D.D.J. and J.M.B. conducted the research; L.B. resolved conflicts over screening and study selection. D.D.J. performed the statistical analysis and wrote the initial manuscript. L.B. and J.M.B. critically revised the manuscript. D.D.J. had the primary responsibility for the final content. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data described in the manuscript, code book and analytic code will be made available upon reasonable request to the corresponding author.
Conflicts of Interest
The second author (L.B.) is affiliated with Arla Foods Amba, however, she was only involved in the study selection and data extraction process if there were any doubts or discrepancies between the first and third author.
Funding Statement
This research was funded by Steno Diabetes Center Aarhus (SDCA) which is partially funded by an unrestricted donation from the Novo Nordisk Foundation, Sygeforsiking “danmark” and Arla Foods Amba (unrestricted grant).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.World Health Organization . Report of the Commision on Ending Childhood Obesity. World Health Organization; Geneva, Switzerland: 2017. Implementation Plan: Executive Summary. [Google Scholar]
- 2.Kim J., Lim H. Nutritional Management in Childhood Obesity. J. Obes. Metab. Syndr. 2019;28:225–235. doi: 10.7570/jomes.2019.28.4.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fischer G.C., Garnett T. Plates, Pyramids, Planet. Developments in National Healthy and Sustainable Dietary Guidelines: A State of Play Assessment. FAO; Rome, Italy: 2016. [Google Scholar]
- 4.World Health Organization Regional Office for Europe . Food-Based Dietary Guidelines in the WHO European Region. World Health Organization Regional Office for Europe; Copenhagen, Denmark: 2003. [Google Scholar]
- 5.Liberali R., Kupek E., De Assis M.A.A. Dietary Patterns and Childhood Obesity Risk: A Systematic Review. Child. Obes. 2020;16:70–85. doi: 10.1089/chi.2019.0059. [DOI] [PubMed] [Google Scholar]
- 6.Lassale C., Fitó M., Morales-Suárez-Varela M., Moya A., Gómez S.F., Schröder H. Mediterranean diet and adiposity in children and adolescents: A systematic review. Obes. Rev. 2022;23((Suppl. 1)):e13381. doi: 10.1111/obr.13381. [DOI] [PubMed] [Google Scholar]
- 7.Pereira A.R., Oliveira A. Dietary Interventions to Prevent Childhood Obesity: A Literature Review. Nutrients. 2021;13:3447. doi: 10.3390/nu13103447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smith K.L., Kerr D.A., Howie E.K., Straker L.M. Do Overweight Adolescents Adhere to Dietary Intervention Messages? Twelve-Month Detailed Dietary Outcomes from Curtin University’s Activity, Food and Attitudes Program. Nutrients. 2015;7:4363–4382. doi: 10.3390/nu7064363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jakobsen D.D., Brader L., Bruun J.M. Effects of foods, beverages and macronutrients on BMI z-score and body composition in children and adolescents: A systematic review and meta-analysis of randomized controlled trials. Eur. J. Nutr. 2022 doi: 10.1007/s00394-022-02966-0. [DOI] [PubMed] [Google Scholar]
- 11.The Cochrane Collaboration . Cochrane Handbook for Systematic Reviews of Interventions. John Wiley & Sons, Ltd.; Hoboken, NJ, USA: 2019. pp. 257–259. [Google Scholar]
- 12.World Health Organization Obesity and Overweight. [(accessed on 16 July 2021)]; Available online: http://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight.
- 13.World Health Organization Growth Reference 5–19 Years—Comparison with IOTF and CDC. [(accessed on 16 July 2021)];2007 Available online: https://www.who.int/growthref/who2007_bmi_for_age/en/
- 14.Center for Disease Control and Prevention, Basics about Childhood Obesity. [(accessed on 16 July 2021)];2018 Available online: https://www.cdc.gov/obesity/childhood/defining.html.
- 15.Modesti P.A., Reboldi G., Cappuccio F.P., Agyemang C., Remuzzi G., Rapi S., Perruolo E., Parati G., ESH Working Group on CV Risk in Low Resource Settings Panethnic Differences in Blood Pressure in Europe: A Systematic Review and Meta-Analysis. PLoS ONE. 2016;11:e0147601. doi: 10.1371/journal.pone.0147601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Guyatt G.H., Oxman A.D., Kunz R., Vist G.E., Falck-Ytter Y., Schünemann H.J. What is “quality of evidence” and why is it important to clinicians? BMJ. 2008;336:995–998. doi: 10.1136/bmj.39490.551019.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liu J.H., Jones S.J., Sun H., Probst J.C., Merchant A.T., Cavicchia P. Diet, physical activity, and sedentary behaviors as risk factors for childhood obesity: An urban and rural comparison. Child. Obes. 2012;8:440–448. doi: 10.1089/chi.2011.0090. [DOI] [PubMed] [Google Scholar]
- 18.Pengpid S., Peltzer K. Overweight, Obesity and Associated Factors among 13–15 Years Old Students in the Association of Southeast Asian Nations Member Countries, 2007–2014. Southeast Asian J. Trop. Med. Public Health. 2016;47:250–262. [PubMed] [Google Scholar]
- 19.Zhang T., Cai L., Ma L., Jing J., Chen Y., Ma J. The prevalence of obesity and influence of early life and behavioral factors on obesity in Chinese children in Guangzhou. BMC Public Health. 2016;16:954. doi: 10.1186/s12889-016-3599-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Maitland T., Malcolm S., Handfield S. Nutritional Knowledge and Practices, Lifestyle Characteristics and Anthropometric Status of Turks and Caicos Islands Elementary School Children. West Indian Med. J. 2015;64:29–36. doi: 10.7727/wimj.2015.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang J., Zhang Y., Jiang Y., Sun W., Zhu Q., Ip P., Zhang D., Liu S., Chen C., Chen J., et al. Effect of Sleep Duration, Diet, and Physical Activity on Obesity and Overweight Elementary School Students in Shanghai. J. Sch. Health. 2018;88:112. doi: 10.1111/josh.12583. [DOI] [PubMed] [Google Scholar]
- 22.Nicklas T.A., Yang S.-J., Baranowski T., Zakeri I., Berenson G. Eating patterns and obesity in children: The Bogalusa Heart Study. Am. J. Prev. Med. 2003;25:9–16. doi: 10.1016/S0749-3797(03)00098-9. [DOI] [PubMed] [Google Scholar]
- 23.Wijnhoven T.M., van Raaij J.M., Yngve A., Sjöberg A., Kunešová M., Duleva V., Petrauskiene A., I Rito A., Breda J. WHO European Childhood Obesity Surveillance Initiative: Health-risk behaviours on nutrition and physical activity in 6–9-year-old schoolchildren. Public Health Nutr. 2015;18:3108–3124. doi: 10.1017/S1368980015001937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hanley A.J., Harris S.B., Gittelsohn J., Wolever T.M., Saksvig B., Zinman B. Overweight among children and adolescents in a Native Canadian community: Prevalence and associated factors. Am. J. Clin. Nutr. 2000;71:693–700. doi: 10.1093/ajcn/71.3.693. [DOI] [PubMed] [Google Scholar]
- 25.Hatami M., Taib M.N.M., Jamaluddin R., Abu Saad H., Djazayery A., Chamari M., Nazari M. Dietary factors as the major determinants of overweight and obesity among Iranian adolescents. A cross-sectional study. Appetite. 2014;82:194–201. doi: 10.1016/j.appet.2014.07.026. [DOI] [PubMed] [Google Scholar]
- 26.Abreu S., Santos R., Moreira C., Santos P.C., Mota J., Moreira P. Food consumption, physical activity and socio-economic status related to BMI, waist circumference and waist-to-height ratio in adolescents. Public Health Nutr. 2014;17:1834–1849. doi: 10.1017/S1368980013001948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Huus K., Brekke H.K., Ludvigsson J., Ludvigsson J. Relationship of food frequencies as reported by parents to overweight and obesity at 5 years. Acta Paediatr. 2009;98:139–143. doi: 10.1111/j.1651-2227.2008.01043.x. [DOI] [PubMed] [Google Scholar]
- 28.Matthews V.L., Wien M., Sabaté J. The risk of child and adolescent overweight is related to types of food consumed. Nutr. J. 2011;10:71. doi: 10.1186/1475-2891-10-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sanigorski A.M., Bell A.C., A Swinburn B. Association of key foods and beverages with obesity in Australian schoolchildren. Public Health Nutr. 2007;10:152–157. doi: 10.1017/S1368980007246634. [DOI] [PubMed] [Google Scholar]
- 30.Bel-Serrat S., Heinen M.M., Mehegan J., O’Brien S., Eldin N., Murrin C.M., Kelleher C.C. Predictors of weight status in school-aged children: A prospective cohort study. Eur. J. Clin. Nutr. 2019;73:1299–1306. doi: 10.1038/s41430-018-0359-8. [DOI] [PubMed] [Google Scholar]
- 31.Cutler G.J., Flood A., Hannan P.J., Slavin J.L., Neumark-Sztainer D. Association between major patterns of dietary intake and weight status in adolescents. Br. J. Nutr. 2012;108:349–356. doi: 10.1017/S0007114511005435. [DOI] [PubMed] [Google Scholar]
- 32.Chen J., Luo S., Liang X., Luo Y., Li R. The relationship between socioeconomic status and childhood overweight/obesity is linked through paternal obesity and dietary intake: A cross-sectional study in Chongqing, China. Environ. Health Prev. Med. 2021;26:56. doi: 10.1186/s12199-021-00973-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Flores G. and H. Lin, Factors predicting severe childhood obesity in kindergarteners. Int. J. Obes. 2013;37:31–39. doi: 10.1038/ijo.2012.168. [DOI] [PubMed] [Google Scholar]
- 34.Ahmed J., Laghari A., Naseer M., Mehraj V. Prevalence of and factors associated with obesity among Pakistani schoolchildren: A school-based, cross-sectional study. East. Mediterr. Health J. 2013;19:242–247. doi: 10.26719/2013.19.3.242. [DOI] [PubMed] [Google Scholar]
- 35.Santiago S., Zazpe I., Martí A., Cuervo M., Martínez J.A. Gender differences in lifestyle determinants of overweight prevalence in a sample of Southern European children. Obes. Res. Clin. Pract. 2013;7:e391–e400. doi: 10.1016/j.orcp.2012.07.001. [DOI] [PubMed] [Google Scholar]
- 36.Duan R., Kou C., Jie J., Bai W., Lan X., Li Y., Yu X., Zhu B., Yuan H. Prevalence and correlates of overweight and obesity among adolescents in northeastern China: A cross-sectional study. BMJ Open. 2020;10:e036820. doi: 10.1136/bmjopen-2020-036820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sakaki J.R., Melough M.M., Li J., Tamimi R.M., Chavarro J.E., Chen M.-H., Chun O.K. Associations between 100% Orange Juice Consumption and Dietary, Lifestyle and Anthropometric Characteristics in a Cross-Sectional Study of U.S. Children and Adolescents. Nutrients. 2019;11:2687. doi: 10.3390/nu11112687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.O’Neil C.E., Fulgoni V.L., 3rd, Nicklas T.A. Association of candy consumption with body weight measures, other health risk factors for cardiovascular disease, and diet quality in US children and adolescents: NHANES 1999–2004. Food Nutr. Res. 2011;55 doi: 10.3402/fnr.v55i0.5794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hwang S., Park S., Jin G.-R., Jung J., Park H., Lee S., Shin S., Lee B.-H. Trends in Beverage Consumption and Related Demographic Factors and Obesity among Korean Children and Adolescents. Nutrients. 2020;12:2651. doi: 10.3390/nu12092651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nasreddine L., Naja F., Akl C., Chamieh M.C., Karam S., Sibai A.-M., Hwalla N. Dietary, Lifestyle and Socio-Economic Correlates of Overweight, Obesity and Central Adiposity in Lebanese Children and Adolescents. Nutrients. 2014;6:1038–1062. doi: 10.3390/nu6031038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hirschler V., Buzzano K., Erviti A., Ismael N., Silva S., Dalamón R. Overweight and lifestyle behaviors of low socioeconomic elementary school children in Buenos Aires. BMC Pediatr. 2009;9:17. doi: 10.1186/1471-2431-9-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shin S.M. Association of Meat Intake with Overweight and Obesity among School-aged Children and Adolescents. J. Obes. Metab. Syndr. 2017;26:217–226. doi: 10.7570/jomes.2017.26.3.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Martinez-Ospina A., Sudfeld C.R., González S.A., Sarmiento O.L. School Food Environment, Food Consumption, and Indicators of Adiposity Among Students 7–14 Years in Bogotá, Colombia. J. Sch. Health. 2019;89:200–209. doi: 10.1111/josh.12729. [DOI] [PubMed] [Google Scholar]
- 44.Govindan M., Gurm R., Mohan S., Kline-Rogers E., Corriveau N., Goldberg C., DuRussel-Weston J., Eagle K.A., Jackson E.A. Gender Differences in Physiologic Markers and Health Behaviors Associated With Childhood Obesity. Pediatrics. 2013;132:468–474. doi: 10.1542/peds.2012-2994. [DOI] [PubMed] [Google Scholar]
- 45.Beck A.L., Tschann J., Butte N.F., Penilla C., Greenspan L.C. Association of beverage consumption with obesity in Mexican American children. Public Health Nutr. 2014;17:338–344. doi: 10.1017/S1368980012005514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Colapinto C.K., Rossiter M., Khan M.K.A., Kirk S.F.L., Veugelers P.J. Obesity, lifestyle and socio-economic determinants of vitamin D intake: A population-based study of Canadian children. Can. J. Public Health. 2014;105:e418–e424. doi: 10.17269/cjph.105.4608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Marcos-Pasero H., Aguilar-Aguilar E., de la Iglesia R., Espinosa-Salinas I., Gómez-Patiño M., Colmenarejo G., de Molina A.R., Reglero G., Loria-Kohen V. Association of calcium and dairy product consumption with childhood obesity and the presence of a Brain Derived Neurotropic Factor-Antisense (BDNF-AS) polymorphism. Clin. Nutr. 2019;38:2616–2622. doi: 10.1016/j.clnu.2018.11.005. [DOI] [PubMed] [Google Scholar]
- 48.White M.J., Armstrong S.C., Kay M.C., Perrin E.M., Skinner A. Associations between milk fat content and obesity, 1999 to 2016. Pediatr. Obes. 2020;15:e12612. doi: 10.1111/ijpo.12612. [DOI] [PubMed] [Google Scholar]
- 49.Nguyen T., Sokal-Gutierrez K., Lahiff M., Fernald L., Ivey S.L. Early childhood factors associated with obesity at age 8 in Vietnamese children: The Young Lives Cohort Study. BMC Public Health. 2021;21:301. doi: 10.1186/s12889-021-10292-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Choumenkovitch S.F., McKeown N.M., Tovar A., Hyatt R.R., I Kraak V., Hastings A.V., Herzog J.B., Economos C.D. Whole grain consumption is inversely associated with BMI Z-score in rural school-aged children. Public Health Nutr. 2013;16:212–218. doi: 10.1017/S1368980012003527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Notara V., Legkou M., Kanellopoulou A., Antonogeorgos G., Rojas-Gil A.P., Kornilaki E.N., Konstantinou E., Lagiou A., Panagiotakos D.B. Lack of association between dietary fibres intake and childhood obesity: An epidemiological study among preadolescents in Greece. Int. J. Food Sci. Nutr. 2020;71:635–643. doi: 10.1080/09637486.2020.1712681. [DOI] [PubMed] [Google Scholar]
- 52.Payab M., Kelishadi R., Qorbani M., Motlagh M.E., Ranjbar S.H., Ardalan G., Zahedi H., Chinian M., Asayesh H., Larjani B., et al. Association of junk food consumption with high blood pressure and obesity in Iranian children and adolescents: The CASPIAN-IV Study. J. Pediatr. 2015;91:196–205. doi: 10.1016/j.jped.2014.07.006. [DOI] [PubMed] [Google Scholar]
- 53.Walsh C., Seguin-Fowler R., Ammerman A., Hanson K., Jilcott S.B.P., Kolodinsky J., Sitaker M., Ennett S. Snacking, sugar-sweetened beverage consumption and child obesity in low-income households. Nutr. Food Sci. 2020;51:151–163. doi: 10.1108/NFS-02-2020-0048. [DOI] [Google Scholar]
- 54.Kollias A., Skliros E., Stergiou G.S., Leotsakos N., Saridi M., Garifallos D. Obesity and associated cardiovascular risk factors among schoolchildren in Greece: A cross-sectional study and review of the literature. J. Pediatr. Endocrinol. Metab. 2011;24:929–938. doi: 10.1515/JPEM.2011.309. [DOI] [PubMed] [Google Scholar]
- 55.Kostopoulou E., Tsekoura E., Fouzas S., Gkentzi D., Jelastopulu E., Varvarigou A. Association of lifestyle factors with a high prevalence of overweight and obesity in Greek children aged 10–16 years. Acta Paediatr. 2021;110:3356–3364. doi: 10.1111/apa.15960. [DOI] [PubMed] [Google Scholar]
- 56.Muckelbauer R., Gortmaker S.L., Libuda L., Kersting M., Clausen K., Adelberger B., Müller-Nordhorn J. Changes in water and sugar-containing beverage consumption and body weight outcomes in children. Br. J. Nutr. 2016;115:2057–2066. doi: 10.1017/S0007114516001136. [DOI] [PubMed] [Google Scholar]
- 57.Xu X., Pan C.L., Liu G.L., Chen H.M. Socioeconomic and lifestyle behavioral factors associated with overweight and obesity among rural to urban migrant children in central China. Int. J. Clin. Exp. Med. 2016;9:21635–21644. [Google Scholar]
- 58.Vinciguerra F., Tumminia A., Roppolo F., Romeo L.C., La Spina N., Baratta R., Parrino C., Sciacca L., Vigneri R., Frittitta L. Impact of unhealthy childhood and unfavorable parents’ characteristics on adiposity in schoolchildren. Diabetes/Metabolism Res. Rev. 2019;35:e3199. doi: 10.1002/dmrr.3199. [DOI] [PubMed] [Google Scholar]
- 59.Shan X.-Y., Xi B., Cheng H., Hou D.-Q., Wang Y., Mi J. Prevalence and behavioral risk factors of overweight and obesity among children aged 2–18 in Beijing, China. Int. J. Pediatr. Obes. 2010;5:383–389. doi: 10.3109/17477160903572001. [DOI] [PubMed] [Google Scholar]
- 60.Karki A., Shrestha A., Subedi N. Prevalence and associated factors of childhood overweight/obesity among primary school children in urban Nepal. BMC Public Health. 2019;19:1055. doi: 10.1186/s12889-019-7406-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Valente H., Teixeira V., Padrão P., Bessa M., Cordeiro T., Moreira A., Mitchell V., Lopes C., Mota J., Moreira P. Sugar-sweetened beverage intake and overweight in children from a Mediterranean country. Public Health Nutr. 2011;14:127–132. doi: 10.1017/S1368980010002533. [DOI] [PubMed] [Google Scholar]
- 62.Katzmarzyk P.T., Broyles S.T., Champagne C.M., Chaput J.-P., Fogelholm M., Hu G., Kuriyan R., Kurpad A., Lambert E.V., Maia J., et al. Relationship between Soft Drink Consumption and Obesity in 9–11 Years Old Children in a Multi-National Study. Nutrients. 2016;8:770. doi: 10.3390/nu8120770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Heo M., Wylie-Rosett J. Being obese versus trying to lose weight: Relationship with physical inactivity and soda drinking among high school students. J. Sch. Health. 2020;90:301–305. doi: 10.1111/josh.12879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Guerrero R.T.L., Barber L.R., Aflague T.F., Paulino Y.C., Hattori-Uchima M.P., Acosta M., Wilkens L.R., Novotny R. Prevalence and Predictors of Overweight and Obesity among Young Children in the Children’s Healthy Living Study on Guam. Nutrients. 2020;12:2527. doi: 10.3390/nu12092527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Haboush-Deloye A., Berlin H., Marquez E., Moonie S. Obesity in Early Childhood: Examining the Relationship among Demographic, Behavioral, Nutritional, and Socioeconomic Factors. Child. Obes. 2021;17:349–356. doi: 10.1089/chi.2020.0263. [DOI] [PubMed] [Google Scholar]
- 66.Mekonnen T., Tariku A., Abebe S.M. Overweight/obesity among school aged children in Bahir Dar City: Cross sectional study. Ital. J. Pediatr. 2018;44:17. doi: 10.1186/s13052-018-0452-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Xue H., Wu Y., Wang X., Wang Y. Time Trends in Fast Food Consumption and Its Association with Obesity among Children in China. PLoS ONE. 2016;11:e0151141. doi: 10.1371/journal.pone.0151141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Siddarth D. Risk Factors for Obesity in Children and Adults. J. Investig. Med. 2013;61:1039–1042. doi: 10.2310/JIM.0b013e31829c39d0. [DOI] [PubMed] [Google Scholar]
- 69.Pirinçci E., Durmuş B., Gündoğdu C., Açik Y. Prevalence and risk factors of overweight and obesity among urban school children in Elazig city, Eastern Turkey, 2007. Ann. Hum. Biol. 2010;37:44–56. doi: 10.3109/03014460903218984. [DOI] [PubMed] [Google Scholar]
- 70.Mihrshahi S., Drayton B.A., Bauman A.E., Hardy L.L. Associations between childhood overweight, obesity, abdominal obesity and obesogenic behaviors and practices in Australian homes. BMC Public Health. 2017;18:44. doi: 10.1186/s12889-017-4595-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lee E.Y., Kang B., Yang Y., Yang H.K., Kim H.-S., Lim S.-Y., Lee J.-H., Lee S.-S., Suh B.-K., Yoon K.-H. Study Time after School and Habitual Eating Are Associated with Risk for Obesity among Overweight Korean Children: A Prospective Study. Obes. Facts. 2018;11:46–55. doi: 10.1159/000486132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Joseph N. Fast Food Consumption Pattern and Its Association with Overweight Among High School Boys in Mangalore City of Southern India. J. Clin. Diagn. Res. 2015;9:LC13–LC17. doi: 10.7860/JCDR/2015/13103.5969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Zhao Y., Wang L., Xue H., Wang H., Wang Y. Fast food consumption and its associations with obesity and hypertension among children: Results from the baseline data of the Childhood Obesity Study in China Mega-cities. BMC Public Health. 2017;17:933. doi: 10.1186/s12889-017-4952-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hadi H., Nurwanti E., Gittelsohn J., Arundhana A.I., Astiti D., West J.K.P., Dibley M.J. Improved Understanding of Interactions between Risk Factors for Child Obesity May Lead to Better Designed Prevention Policies and Programs in Indonesia. Nutrients. 2020;12:175. doi: 10.3390/nu12010175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Guyatt G., Oxman A.D., Akl E.A., Kunz R., Vist G., Brozek J., Norris S., Glasziou P., deBeer H., Rind D., et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J. Clin. Epidemiol. 2011;64:383–394. doi: 10.1016/j.jclinepi.2010.04.026. [DOI] [PubMed] [Google Scholar]
- 76.Poorolajal J., Sahraei F., Mohamdadi Y., Doosti-Irani A., Moradi L. Behavioral factors influencing childhood obesity: A systematic review and meta-analysis. Obes. Res. Clin. Pract. 2020;14:109–118. doi: 10.1016/j.orcp.2020.03.002. [DOI] [PubMed] [Google Scholar]
- 77.Farhangi M.A., Tofigh A.M., Jahangiri L., Nikniaz Z., Nikniaz L. Sugar-sweetened beverages intake and the risk of obesity in children: An updated systematic review and dose–response meta-analysis. Pediatr. Obes. 2022;17:e12914. doi: 10.1111/ijpo.12914. [DOI] [PubMed] [Google Scholar]
- 78.Bleich S.N., Vercammen K.A. The negative impact of sugar-sweetened beverages on children’s health: An update of the literature. BMC Obes. 2018;5:6. doi: 10.1186/s40608-017-0178-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Malik V.S., Hu F.B. The role of sugar-sweetened beverages in the global epidemics of obesity and chronic diseases. Nat. Rev. Endocrinol. 2022;18:205–218. doi: 10.1038/s41574-021-00627-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Makri R., Katsoulis M., Fotiou A., Kanavou E., Stavrou M., Richardson C., Kanellopoulou A., Orfanos P., Benetou V., Kokkevi A. Prevalence of Overweight and Obesity and Associated Diet-Related Behaviours and Habits in a Representative Sample of Adolescents in Greece. Children. 2022;9:119. doi: 10.3390/children9010119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Jia P., Luo M., Li Y., Zheng J.S., Xiao Q., Luo J. Fast-food restaurant, unhealthy eating, and childhood obesity: A systematic review and meta-analysis. Obes. Rev. 2021;22((Suppl. 1)):e12944. doi: 10.1111/obr.12944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Daneshzad E., Askari M., Moradi M., Ghorabi S., Rouzitalab T., Heshmati J., Azadbakht L. Red meat, overweight and obesity: A systematic review and meta-analysis of observational studies. Clin. Nutr. ESPEN. 2021;45:66–74. doi: 10.1016/j.clnesp.2021.07.028. [DOI] [PubMed] [Google Scholar]
- 83.Rouhani M.H., Salehi-Abargouei A., Surkan P.J., Azadbakht L. Is there a relationship between red or processed meat intake and obesity? A systematic review and meta-analysis of observational studies. Obes. Rev. 2014;15:740–748. doi: 10.1111/obr.12172. [DOI] [PubMed] [Google Scholar]
- 84.Schlesinger S., Neuenschwander M., Schwedhelm C., Hoffmann G., Bechthold A., Boeing H., Schwingshackl L. Food Groups and Risk of Overweight, Obesity, and Weight Gain: A Systematic Review and Dose-Response Meta-Analysis of Prospective Studies. Adv. Nutr. Int. Rev. J. 2019;10:205–218. doi: 10.1093/advances/nmy092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Serra-Majem L., Bautista-Castaño I. Relationship between bread and obesity. Br. J. Nutr. 2015;113((Suppl. 2)):S29–S35. doi: 10.1017/S0007114514003249. [DOI] [PubMed] [Google Scholar]
- 86.Herforth A., Arimond M., Álvarez-Sánchez C., Coates J., Christianson K., Muehlhoff E. A Global Review of Food-Based Dietary Guidelines. Adv. Nutr. Int. Rev. J. 2019;10:590–605. doi: 10.1093/advances/nmy130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ruperez A.I., Mesana M.I., Moreno L.A. Dietary sugars, metabolic effects and child health. Curr. Opin. Clin. Nutr. Metab. Care. 2019;22:206–216. doi: 10.1097/MCO.0000000000000553. [DOI] [PubMed] [Google Scholar]
- 88.Thorning T.K., Raben A., Tholstrup T., Soedamah-Muthu S.S., Givens I., Astrup A. Milk and dairy products: Good or bad for human health? An assessment of the totality of scientific evidence. Food Nutr. Res. 2016;60:32527. doi: 10.3402/fnr.v60.32527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Lu L., Xun P., Wan Y., He K., Cai W. Long-term association between dairy consumption and risk of childhood obesity: A systematic review and meta-analysis of prospective cohort studies. Eur. J. Clin. Nutr. 2016;70:414–423. doi: 10.1038/ejcn.2015.226. [DOI] [PubMed] [Google Scholar]
- 90.Kang K., Sotunde O.F., A Weiler H. Effects of Milk and Milk-Product Consumption on Growth among Children and Adolescents Aged 6–18 Years: A Meta-Analysis of Randomized Controlled Trials. Adv. Nutr. Int. Rev. J. 2019;10:250–261. doi: 10.1093/advances/nmy081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.D’Innocenzo S., Biagi C., Lanari M. Obesity and the Mediterranean Diet: A Review of Evidence of the Role and Sustainability of the Mediterranean Diet. Nutrients. 2019;11:1306. doi: 10.3390/nu11061306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Denova-Gutiérrez E., Jiménez-Aguilar A., Halley-Castillo E., Huitrón-Bravo G., Talavera J.O., Pineda-Pérez D., Díaz-Montiel J.C., Salmerón J. Association between sweetened beverage consumption and body mass index, proportion of body fat and body fat distribution in Mexican adolescents. Ann. Nutr. Metab. 2008;53:245–251. doi: 10.1159/000189127. [DOI] [PubMed] [Google Scholar]
- 93.Gibson S., Neate D. Sugar intake, soft drink consumption and body weight among British children: Further analysis of National Diet and Nutrition Survey data with adjustment for under-reporting and physical activity. Int. J. Food Sci. Nutr. 2007;58:445–460. doi: 10.1080/09637480701288363. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data described in the manuscript, code book and analytic code will be made available upon reasonable request to the corresponding author.