Abstract
Background: Evidence indicates that certain healthy lifestyle factors are associated with non-alcoholic fatty liver disease (NAFLD). However, little is known about the effect of combined healthy lifestyle factors. Objective: To assess the association of combined healthy lifestyle factors with the incidence of NAFLD. Methods: This cohort study was conducted in Changsha, Hunan Province, China. The healthy lifestyles factors studied were not being a current smoker, having a healthy diet, engaging in physical activity, having a normal body mass index (BMI) and engaging in non-sedentary behavior. NAFLD was diagnosed based on abdominal ultrasonography. Logistic regression models were conducted to investigate the associations being studied. Results: Of the 5411 participants, 1280 participants had NAFLD, with a prevalence of 23.7% at baseline. The incidence of NAFLD among participants without NAFLD at baseline was found to be 7.2% over a mean follow-up of 1.1 years. Compared with participants with 0–1 low-risk factors, the OR of NAFLD was 0.50 (95% CI: 0.29–0.82, p = 0.008) for those with at least 4 low-risk factors. Similar associations were observed in subgroup analyses and sensitivity analyses. Conclusion: This study suggests that a combined healthy lifestyle pattern may considerably decrease the risk of NAFLD in Chinese government employees.
Keywords: lifestyle factors, combined impact, non-alcoholic fatty liver disease (NAFLD), government employees, cohort
1. Introduction
Non-alcoholic fatty liver disease (NAFLD) is one of the most common chronic liver diseases in the world, affecting approximately 25% of the general population. NAFLD has expanded into a global public health issue and imposes a substantial economic burden on all societies [1]. Increasing evidence indicates that NAFLD may develop into end-stage liver disease [2] (e.g., decompensated cirrhosis, severe hepatitis, advanced liver cancer, etc.). In addition, it can contribute to an increased risk of multisystem disease, including cardiovascular events, metabolic disorders and kidney problems, by affecting extra-hepatic organs and regulatory pathways [3]. Previous research has observed that the prevalence of NAFLD parallels urbanization and industrialization trends, and lifestyle changes have been found to be associated with the NAFLD epidemic worldwide, especially in the Asia-Pacific region [4].
Having an unhealthy lifestyle, a common and crucial modifiable risk factor, has been proven to be independently related to many chronic noncommunicable diseases, such as type 2 diabetes [5], cancer [6] and cardiovascular disease [7]. In addition, a recent study suggested that maintaining a healthy lifestyle may contribute to a higher life expectancy [8]. Meanwhile, many studies have shown that smoking [9], physical inactivity [10], sedentary behavior [11,12], higher weight [13] and an unhealthy diet [14] were individually related to an increased risk of NAFLD. For example, replacing saturated fatty acids with plant-based polyunsaturated fatty acids in the diet reduces serum insulin, the total/high-density lipoprotein cholesterol ratio, low-density lipoprotein cholesterol, triglycerides and liver fat [15]. However, most of these studies only investigated the relationship between individual healthy lifestyle factors with NAFLD, thus ignoring the fact that many lifestyle factors often coexist. It is necessary, therefore, to evaluate the joint effects of these modifiable healthy lifestyle factors on the risk of NAFLD. Further, less is known about the possible benefit of combined healthy lifestyle factors with regards to the risk of NAFLD, particularly in developing countries such as China.
Given this, we combined five modifiable healthy lifestyle factors recommended in previous studies, namely, smoking, physical activity, BMI, sedentary behavior and diet, in order to further assess the relationship between combined healthy lifestyle factors and NAFLD. We set out to clarify the following aims in this study: to investigate the relationship between a combination of healthy lifestyle factors and the risk of NAFLD, and how this relationship differs across subgroups.
2. Methods
2.1. Research Design and Study Participants
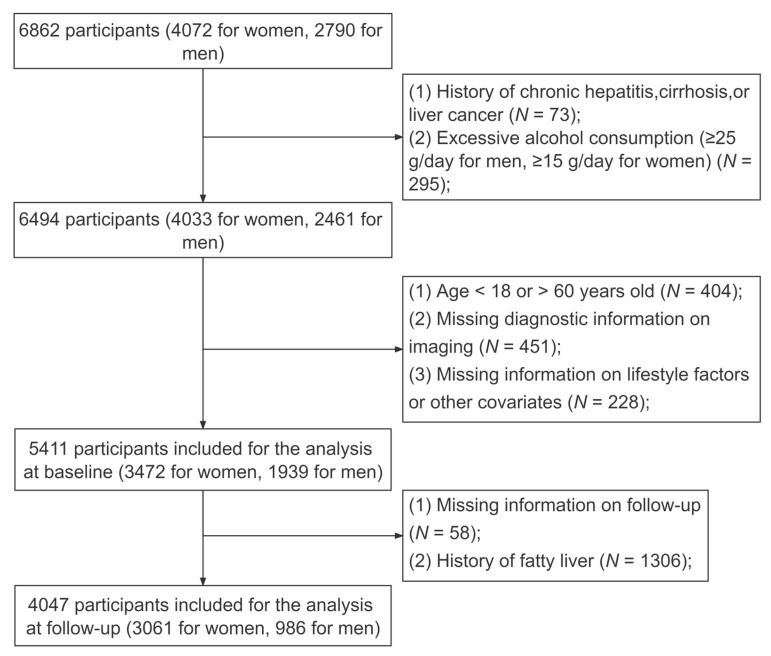
The research involved a prospective cohort study conducted in Changsha City, Hunan Province, which aimed to investigate chronic diseases in Chinese government employees. Government employees in China are those who carry out legal public duties in the national legislative branch, judicial branch, administrative organs, Communist Party of China Party organs, democratic parties, people’s organizations and public institutions. In our research, participants were mainly from government departments, universities and hospitals with a predominantly sedentary work style. The baseline survey consecutively enrolled a total of 6862 participants from 10 government organizations through stratified cluster sampling from January 2018 to April 2020. In addition, we conducted a 1-year follow-up survey for government employees who participated in the baseline survey [16]. All employees filled out an online questionnaire via a cellphone or tablet prior to the ultrasound examination. Detailed information and data collection procedures have been published in previous studies [17,18]. We excluded participants who had a previous history of chronic hepatitis, cirrhosis, liver cancer (N = 73) or excessive alcohol consumption (Males: ≥25 g per day; females: ≥15 g per day) (N = 295). In addition, participants with missing ultrasound diagnosis data (N = 451) and other related covariate data (N = 228), as well as those below 18 or above 60 years of age (N = 404) at baseline, were excluded. As a result, 5411 participants (3472 women, 1939 men) were included in the analyses at baseline. However, 58 employees refused to participate in the follow-up survey. After excluding those with a history of fatty liver (N = 1306) at baseline, 4047 employees (3061 women, 986 men) were included in the final analyses (Figure 1).
Figure 1.
Flowchart of the population included in our analyses.
2.2. Assessment of Healthy Lifestyle Factors
A structured online questionnaire evaluated a range of healthy lifestyle factors at baseline. For cigarette smoking, it asked all respondents the following question: Do you smoke, at least one cigarette per day for more than a half-year? (there were 3 response categories: never, former or current). Further, we collected information on current smokers regarding the amount of cigarettes they smoked per day and the age at which they started smoking. For alcohol consumption, the questionnaire asked all employees the following question: Do you consume alcohol, at least once per week for more than a half-year? (there were 3 response categories: never, former or current). Information about alcohol consumption included the frequency current drinkers drank per week, the volume of alcohol they consumed per drinking session and the types of alcohol they consumed. Regarding a healthy diet, the questionnaire asked: How frequently have you eaten the following foods in the last 12 months? (Eating is considered to have occurred once in one meal; select the corresponding frequency). The details are shown in Table S1 in Supplementary Materials. Information on sedentary behavior [19] involved the time participants spent sitting or reclining in activities (e.g., screen-time, reading, playing cards or mahjong, etc.) engaged in during their leisure time a day [20]. For physical activity, the questionnaire asked the following question: How frequently and for how long have you engaged in physical activities in the last 12 months? The usual types and durations of activities were also collected. The participants’ daily physical activity levels were calculated based on previous literature [21]. All participants’ heights, weights and waist circumferences were assessed by skilled researchers using industry-recognized tools. The following formula was used to determine BMI: BMI = weight/height2 (kg/m2).
2.3. Healthy Lifestyle Definition
Five healthy lifestyle factors were identified and combined in order to form our healthy lifestyle definitions, namely, smoking, diet quality, sedentary behavior, physical activity and BMI according to the American Heart Association (AHA) and previous studies [9,11,14,22].
For smoking, we defined non-smoker participants and those participants who had not smoked for more than half a year as belonging to the healthy group. For diet intake, according to the recommendations of Dietary Guidelines for Chinese Residents (2022) and the actual situation of this cohort, we considered 5 types of food items, namely, red meat, vegetables, fruits, soybean and products, and fish. A participant’s diet was defined as healthy if it included more than 4 of the healthy diet food items. Information on the construction of the healthy diet score is displayed in Supplementary Materials Table S2. Non-sedentary behavior was defined as ≤2 h per day of sitting during leisure time [23]. For physical activity, we assigned participants to the healthy group if they were higher than or equal to a sex-specific upper quarter with regards to their physical activity level. Finally, we used two methods to define a healthy weight [24]. The first involved assigning participants with a BMI of 18.5 to 23.9 kg/m2 to be in the healthy group. The other was assigning participants to the healthy group if their waist measurements were less than 80 cm for women and 85 cm for men [24]. The details are shown in Supplementary Materials Table S3.
2.4. Diagnosis of NAFLD
All employees in our study were examined by a qualified physician using abdominal ultrasonography, and the diagnostic standard was based on the Chinese Association of Liver Diseases recommendations [25]. Diagnosing NAFLD involved the following five criteria: (1) Diffuse enhancement of the near-field echogenicity in the hepatic region that is stronger than that in the kidney and spleen regions, with there being gradual attenuation of the far-field echogenicity; (2) Poor visualization of intrahepatic luminal structures; (3) Mild to moderate hepatomegaly, with rounded and blunted liver margins; (4) Reduced or even difficult to visualize blood flow signal in the liver on color Doppler ultrasound, but normal blood flow distribution; and (5) Poorly visualized or incomplete right lobe of the liver and diaphragm.
2.5. Assessment of Covariates
The following variables were considered as covariates: (1) categorical variables: gender (male or female), employment grade (primary, intermediate or senior/deputy senior), educational levels (high school or below, undergraduate or postgraduate or above), marriage status (divorced/widowed, single or married), annual household income (<100,000, 100,000–300,000 or >300,000 CNY), alcohol consumption (current or never/former), and a history of using statins (yes or no); and (2) continuous variables: age, total cholesterol (TC), triglycerides (TG), fasting plasma glucose (FPG), total bilirubin (TBIL), high-density lipoprotein cholesterol (HDL-C) and low-density lipoprotein cholesterol (LDL-C).
Covariate information was estimated through questionnaires, including sociodemographic factors and family medical history information. Blood samples, following a 12 h fast, were taken and transmitted immediately to the medical laboratory for biomarker analysis. FPG levels were measured by the glucose oxidase method, TBIL levels were measured by the diazobenzene sulfonate method and TC, TG, HDL-C and LDL-C levels were measured by the standard enzyme method. All determinations were carried out with a Chemistry System Autoanalyzer (Hitachi 7600-110; Tokyo, Japan) in the Medicine Laboratory Department of the Third Xiangya Hospital, which has been accredited by the Chinese Society of Laboratory Medicine.
2.6. Statistical Analyses
The basic characteristics of the qualitative variables of the participants were described using percentages, and means and standard deviations (SDs) were used to express the quantitative variables. Chi-square tests for qualitative variables and analysis of variance (ANOVA) for quantitative variables were used to compare differences in basic characteristics. Contingency coefficients were used to estimate the pairwise correlation of healthy lifestyle factors.
We performed the multivariable logistic regression method to assess the association between a combination of lifestyle factors and the risk of NAFLD. We employed three regression models, namely, a crude model (unadjusted model) and two adjusted models (model 1 and model 2). To assess the association between a combination of healthy lifestyle factors and NAFLD, model 1 did not correct for any covariates, and model 1 adjusted for age, gender, education level, marriage status and employment grade. Model 2, the full model, was employed by additionally adjusting for a history of using statins, as well as TC, TG, FPG, TBIL, HDL-C and LDL-C. Potential confounders that were analyzed were based on the previous literature and our work with the data [26,27].
Further, to estimate the consistency of our findings, sensitivity analyses were performed. As waist circumference is often used as an indicator of central adiposity, we used WC instead of BMI to construct the combined lifestyle factors for comparison. Then, the second sensitivity analysis was carried out, which only included non-current drinkers. In addition, we stratified the analysis by gender, age, marriage status and socioeconomic status using logistic regression.
The primary statistical analyses were carried out in R version 4.1.1. Specifically, the “glmnet” package was used for the logistic regression, and all figures in the article were implemented using the “ggplot2” and “foreign” packages. A two-tailed p < 0.05 was used to determine the statistical significance.
3. Results
3.1. Basic Characteristics of Study Participants
Table 1 provides the basic characteristics of the participants, which are grouped by the combined healthy lifestyle factors. Of the 5411 participants (1939 men and 3472 women, with an average age of 38.19 years), 521 (9.6%), 1390 (25.7%), 2201 (40.7%) and 1299 (24.0%) had at least four and five, three, two, one and zero healthy lifestyle factors, respectively. A total of 1280 participants had NAFLD, with the disease having a prevalence of 23.7% at baseline. Its prevalence decreased as the number of combined healthy lifestyle factors increased, with participants with only 0–1 healthy lifestyle factors having the highest prevalence of NAFLD. The participants who had more healthy lifestyle factors than the other participants were females, with higher levels of education and income, and lower levels of triglycerides, total cholesterol, fasting rapid glucose, low-density lipoprotein cholesterol, platelet count, albumin and alanine aminotransferase, as well as a higher level of high-density lipoprotein cholesterol than other participants. All basic characteristics, except education level and family income, differed markedly between the healthy lifestyle factor groups (p-values < 0.05). There were 341 participants who were diagnosed with NAFLD over a period of 4761.5 person-years, and the median follow-up time was 1.1 years. In addition, the prevalence of metabolic syndrome was 47.5% in the NAFLD group, compared to 5.5% in the non-NAFLD group (N = 5134). Among the 5411 participants, 4897 (90.5%) were non-current smokers, 1405 (26.0%) chose non-sedentary behavior, 3224 (59.6%) had a normal BMI, 938 (17.3%) maintained a healthy diet and 1376 (25.4%) were active in physical activity. See Table S4 for details. Table S5 provides details about the combination of lifestyle factors and includes 32 combinations in total. The most frequent combinations were the not currently smoking and normal BMI group and the no current smoking group, corresponding to 26.1% and 16.8%, respectively.
Table 1.
Characteristics of the baseline study.
| Characteristics | Total | Healthy Lifestyle Score | p Value | |||
|---|---|---|---|---|---|---|
| 0–1 | 2 | 3 | 4–5 | |||
| N | 5411 | 1299 | 2201 | 1390 | 521 | |
| Age (years), mean ± SD | 38.19 ± 9.32 | 38.48 ± 9.66 | 37.03 ± 9.03 | 38.86 ± 9.21 | 40.60 ± 9.28 | <0.001 |
| Gender, n (%) | <0.001 | |||||
| Female | 3472 (64.2) | 500 (38.5) | 1527 (69.4) | 1034 (74.4) | 411 (78.9) | |
| Male | 1939 (35.8) | 799 (61.5) | 674 (30.6) | 356 (25.6) | 110 (21.1) | |
| Education level, n (%) | 0.057 | |||||
| High school or below | 252 (4.7) | 77 (5.9) | 89 (4.0) | 69 (5.0) | 17 (3.3) | |
| University | 2704 (50.0) | 648 (49.9) | 1129 (51.3) | 673 (48.4) | 254 (48.8) | |
| Postgraduate or above | 2455 (45.4) | 574 (44.2) | 983 (44.7) | 648 (46.6) | 250 (48.0) | |
| Marriage status, n (%) | <0.001 | |||||
| Divorced/widowed | 137 (2.5) | 26 (2.0) | 50 (2.3) | 46 (3.3) | 15 (2.9) | |
| Single | 854 (15.8) | 222 (17.1) | 405 (18.4) | 181 (13.0) | 46 (8.8) | |
| Married | 4420 (81.7) | 1051 (80.9) | 1746 (79.3) | 1163 (83.7) | 460 (88.3) | |
| Grades of employment | <0.001 | |||||
| Primary | 2174 (40.2) | 550 (42.3) | 953 (43.3) | 518 (37.3) | 153 (29.4) | |
| Intermediate | 2117 (39.1) | 456 (35.1) | 852 (38.7) | 590 (42.4) | 219 (42.0) | |
| Senior/deputy senior | 1120 (20.7) | 293 (22.6) | 396 (18.0) | 282 (20.3) | 149 (28.6) | |
| Annual household income (CNY), n (%) | 0.127 | |||||
| <100,000 | 1850 (34.2) | 470 (36.2) | 755 (34.3) | 457 (32.9) | 168 (32.2) | |
| 100,000–300,000 | 3040 (56.2) | 703 (54.1) | 1253 (56.9) | 795 (57.2) | 289 (55.5) | |
| >300,000 | 521 (9.6) | 126 (9.7) | 193 (8.8) | 138 (9.9) | 64 (12.3) | |
| Alcohol | <0.001 | |||||
| Current | 303 (5.6) | 146 (11.2) | 96 (4.4) | 54 (3.9) | 7 (1.3) | |
| Never/former | 5108 (94.4) | 1153 (88.8) | 2105 (95.6) | 1336 (96.1) | 514 (98.7) | |
| History of using statins, n (%) | 39 (0.7) | 17 (1.3) | 11 (0.5) | 7 (0.5) | 4 (0.8) | 0.033 |
| TC (mmol/L), mean ± SD | 4.77 ± 0.91 | 4.92 ± 0.96 | 4.73 ± 0.90 | 4.74 ± 0.88 | 4.68 ± 0.90 | <0.001 |
| TG (mmol/L), mean ± SD | 1.35 ± 1.19 | 1.82 ± 1.62 | 1.26 ± 1.03 | 1.14 ± 0.90 | 1.08 ± 0.81 | <0.001 |
| FPG (mmol/L), mean ± SD | 5.32 ± 0.88 | 5.49 ± 1.09 | 5.26 ± 0.81 | 5.28 ± 0.83 | 5.22 ± 0.54 | <0.001 |
| TBIL (μmol/L), mean ± SD | 13.34 ± 4.91 | 12.90 ± 4.42 | 13.31 ± 4.82 | 13.65 ± 5.26 | 13.72 ± 5.38 | <0.001 |
| HDL-C (mmol/L), mean ± SD | 1.44 ± 0.33 | 1.30 ± 0.31 | 1.46 ± 0.33 | 1.51 ± 0.32 | 1.53 ± 0.32 | <0.001 |
| LDL-C (mmol/L), mean ± SD | 2.72 ± 0.76 | 2.79 ± 0.81 | 2.69 ± 0.75 | 2.72 ± 0.73 | 2.66 ± 0.73 | 0.001 |
| PLT (109/L), mean ± SD | 224.95 ± 51.39 | 227.11 ± 50.78 | 225.93 ± 51.74 | 222.37 ± 50.34 | 222.32 ± 53.88 | 0.047 |
| ALB (g/L), mean ± SD | 45.44 ± 3.03 | 45.84 ± 3.17 | 45.36 ± 3.06 | 45.36 ± 2.88 | 45.00 ± 2.88 | <0.001 |
| ALT (U/L), mean ± SD | 21.68 ± 18.85 | 28.99 ± 27.76 | 20.11 ± 15.19 | 18.67 ± 13.36 | 18.18 ± 11.82 | <0.001 |
| Ultrasound-based NAFLD, n (%) | 1280 (23.7) | 618 (47.6) | 414 (18.8) | 189 (13.6) | 59 (11.3) | <0.001 |
SD, standard deviation; CNY, Chinese yuan; TC, total cholesterol; TG, triglyceride; FPG, fasting plasma glucose; TBIL, total bilirubin; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; PLT, platelet count; ALB, albumin; ALT, alanine aminotransferase; NAFLD, non-alcoholic fatty liver disease.
3.2. Associations between Combined Lifestyle Factors and NAFLD
The associations between single lifestyle factors and the risk of NAFLD are displayed in Table S6. The univariate logistic analysis found that, among the five individual risk factors, BMI, leisure-time sedentary behavior and physical activity were most associated with NAFLD, with these having corresponding ORs of 0.12 (95% CI: 0.10–0.14, p < 0.001), 0.78 (95% CI: 0.66–0.91, p = 0.002) and 0.84 (95% CI: 0.71–1.00, p = 0.045), respectively.
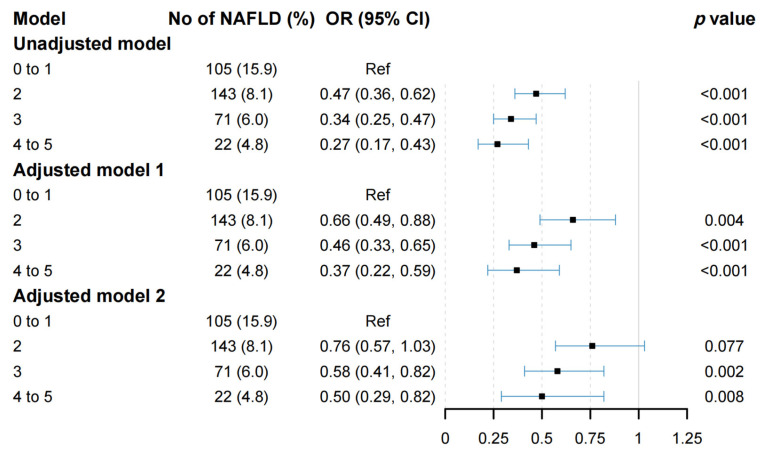
A multivariable logistic regression model was carried out to examine the relationship between the combined healthy lifestyle factors and the risk of NAFLD. As indicated in Figure 2, compared to the group living unfavorable lifestyles (0 to 1 healthy lifestyle factors), the risk of developing NAFLD was reduced by 53% (OR = 0.47, 95% CI: 0.36–0.62, p < 0.001), 66% (OR = 0.34, 95% CI: 0.25–0.47, p < 0.001) and 73% (OR = 0.27, 95% CI: 0.17–0.43, p < 0.001) in the groups with two, three and at least four healthy lifestyle factors, respectively. Model 1 showed the same trends after adjusting for age, gender, education level, marital status and employment grade, with the corresponding ORs of 0.66 (95% CI: 0.49–0.88, p = 0.004), 0.46 (95% CI: 0.33–0.65, p < 0.001) and 0.37 (95% CI: 0.22–0.59, p < 0.001) obtained, respectively. Based on model 1, additional adjustment for a history of using statins, as well as TC, TG, FPG, TBIL, HDL-C and LDL-C, did not substantially change the associations found (OR for two healthy lifestyle factors: 0.76, 95% CI: 0.57–1.03, p = 0.077; OR for three healthy lifestyle factors: 0.58, 95% CI: 0.41–0.82, p = 0.002; OR for at least four healthy lifestyle factors: 0.50, 95% CI: 0.29–0.82, p = 0.008).
Figure 2.
Logistic regression of healthy lifestyle scores and NAFLD. NAFLD, non-alcoholic fatty liver disease; OR, odds ratio; CI, confidence interval.
3.3. Analyses of Subgroups and Sensitivity
Figure 3 displays the outcomes of the subgroup analyses. Compared with one or below factors, a significantly monotonical association between healthy lifestyles (≥3 factors) and NAFLD was observed among the subgroups, with an OR of 0.62 (95% CI: 0.40–0.95, p = 0.031) obtained for males, 0.40 (95% CI: 0.24–0.67, p < 0.001) for females, 0.60 (95% CI: 0.38–0.93, p = 0.024) for participants aged 18 to 40 and 0.52 (95% CI: 0.32–0.86, p = 0.011) for participants aged 41 to 60. A significantly inverse association between healthy lifestyles (≥3 factors) and NAFLD was also maintained in the high socioeconomic status and married subgroups, with the adjusted OR values and 95% confidence intervals being 0.49 (95% CI: 0.31–0.76, p = 0.002) and 0.55 (95% CI: 0.39–0.80, p = 0.001), respectively. When the healthy lifestyles were constructed using waist circumference rather than BMI, the inverse relationship between the healthy lifestyle factors and the risk of NAFLD was not substantially altered. In the final model, compared to the group having unfavorable lifestyles (0 to 1 healthy lifestyle factor), the risk of NAFLD was reduced by 52% (OR= 0.48; 95% CI: 0.35–0.65, p < 0.001), 52% (OR = 0.48, 95% CI: 0.34–0.68, p < 0.001) and 48% (OR = 0.52, 95% CI: 0.32–0.82, p = 0.005) in the groups with two, three and at least four healthy lifestyle factors, respectively (Table S7). We also noticed a significantly monotonical relationship between the increased healthy lifestyle factors and decreased risk of NAFLD among non-current drinkers, with an adjusted OR of 0.72 (95% CI: 0.53–0.99, p = 0.044) obtained for two healthy lifestyle factors, 0.54 (95% CI: 0.38–0.79, p = 0.001) for three healthy lifestyle factors and 0.51 (95% CI: 0.30–0.84, p = 0.010) for at least four healthy lifestyle factors, respectively (Table S8). Furthermore, Table S9 shows the weak correlations (r < 0.15) found between elements of the combined healthy lifestyle factors.
Figure 3.
Stratification analyses of the association between healthy lifestyle scores and NAFLD. OR, odds ratio; CI, confidence interval.
4. Discussion
In the present prospective follow-up study, we discovered a strong association between participants having a combined healthy lifestyle, which included their not currently smoking, having a healthy diet, engaging in regular physical activity, having a normal BMI and engaging in non-sedentary behavior, and a significantly lower risk of NAFLD. Participants who had two or more healthy lifestyle factors exhibited a reduction in their relative risk of NAFLD, ranging from 24% to 73%, compared to those having unhealthy lifestyles (0 to 1 healthy lifestyle factor).
Previous observational studies have demonstrated that individual lifestyle factors are of critical importance in the progression of NAFLD [9,10,11,12,28,29]. To the best of our knowledge, however, only a relatively small number of studies have looked into the relationship between combinations of lifestyle factors and NAFLD. A community-based cross-sectional study found that middle-aged and older Chinese persons with better healthy lifestyle scores—including nonsmoking, moderate BMI, periodic exercise and healthy food intake—had reduced prevalence of NAFLD, recording a corresponding OR value of 0.35 (95% CI: 0.25–0.51) [26]. A 22.83-year follow-up study in the National Health and Nutrition Examination Survey (NHANES) III showed that adopting a healthy lifestyle, which was defined as eating well, exercising regularly, quitting smoking and abstaining from alcohol, resulted in a 36% lower all-cause mortality among NAFLD patients, in comparison to the unfavorable lifestyle group [30]. Another study from NHANES found a significant association between five favorable lifestyle items, namely, dietary patterns, BMI, physical activity, smoking and sleep status, and NAFLD and fibrosis in a representative sample of US adults [31]. Further proof that lifestyle changes can greatly reduce the severity of steatosis and liver impairment has been revealed by clinical trials in NAFLD populations in China, Europe and the USA [32,33,34,35]. Similar to the previous studies, the present study demonstrates that adopting a healthy lifestyle may lower NAFLD incidence among the general public, a measure which has great potential in the primary prevention of NAFLD.
For both males and females, adopting a healthy lifestyle may greatly lower the risk of NAFLD. Gender roles and social norms lead to different lifestyle risk factors for men and women, such as unhealthy lifestyles like smoking, alcohol consumption and other risk-taking behaviors, which are widely regarded as desirable male norms in most parts of the world [36]. Evidence from prior epidemiological research also strongly suggests that males and females differ in terms of their risk factors for NAFLD. Among general adult populations, males have been found to be more likely to have NAFLD than females, mostly because they were more likely to be obese, have diabetes and metabolic syndrome, and engage in poor lifestyle behaviors, such as smoking, eating poorly and not exercising [37,38,39,40]. When further considering specific age groups, the incidence of hepatic steatosis has been found to be similar in postmenopausal women compared to men [41]. Similar to this previous research, our findings from the current study support the notion that women have a lower relative risk of developing NAFLD than men.
In this study, we found that obesity was the major contributor to the risk of NAFLD, which is consistent with the findings of earlier studies [42,43,44]. Waist circumference measurement may be a more reliable method of examining visceral obesity’s relationship with the likelihood of developing NAFLD, given its significance as a key risk factor for metabolic syndrome complications [45,46]. Interestingly, we found that, when we constructed the healthy lifestyle using WC rather than BMI, the most favorable lifestyle group had a lowered NAFLD risk of 48% compared to the unfavorable group (the original reduction was 50%). In addition, weight reduction has been found to be extremely beneficial in reducing liver steatosis and fibrosis, even in those who already had NAFLD [14,47,48]. Maintaining physical activity, watching one’s diet and reducing sedentary behavior are all essential for weight loss and maintenance. We found that physical exercise and sedentary behavior were both independently associated with the likelihood of developing NAFLD, which is also supported by data from earlier studies [11].
The study we conducted has a number of strengths. NAFLD, the outcome variable of interest, was diagnosed by specialists via abdominal ultrasonography. The prospective cohort study’s large sample size allowed for the detection of evidence of the relationship between a healthy lifestyle and a lower risk of NAFLD. Further, using a combined healthy lifestyle enabled us to comprehensively characterize an individual’s profile. Despite these advantages, there are several limitations to our research. First, the study had a median follow-up of 1.1 years, which might have been associated with reverse causation; this needs to be explained by further long-time cohort studies. In addition, our study population was not typical of the entire population since it excluded workers from rural areas, the jobless and people with unstable employment. As a result, the generalizability of our findings may be constrained. Third, the questions in the lifestyle factors questionnaire utilized in this investigation were modified and used in numerous other studies, rather than being directly validated. Nonetheless, such misclassification may have led to weakened associations. Additionally, recollection bias was not able to be totally eliminated from our study, and lifestyle characteristics that were only examined once at baseline might not have accurately reflected long-term exposure. Accordingly, these factors might have affected the risk estimates. More studies are required to evaluate the benefits of adopting healthy lifestyles over time with regards to lowering the risk of NAFLD. There may still have been residual confounding factors from additional unmeasured or unidentified factors, even when all the models were corrected for recognized potential biases.
5. Conclusions
In conclusion, our findings provide robust evidence that adopting a healthy lifestyle pattern—including quitting smoking, maintaining a normal BMI, eating a balanced diet, cutting back on sedentary behavior and engaging in physical activity—can lower the risk of NAFLD. From a public health viewpoint, lifestyle modifications have great potential in the primary prevention of NAFLD. Further evidence of the effectiveness of comprehensive lifestyle modification in the prevention of NAFLD is expected to come from the continuing follow-up of this prospective cohort study.
Acknowledgments
The Department of Health Management Centers in the Third Xiangya Hospital of Central South University lent full support to the research. We express our sincere appreciation to the government employees who participated in this study.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/nu15030604/s1, Table S1: Food frequency questionnaire; Table S2: Diet score extended information; Table S3: Criteria of Healthy Lifestyle Score in the present study; Table S4: The prevalence of the individual risk factors; Table S5: Details about combination of lifestyle factors; Table S6: Association between single risk factors and risk of NAFLD; Table S7: The lifestyle that included waist circumference rather than BMI and risk of NAFLD; Table S8: Association of healthy lifestyle scores and risk of NAFLD among non-current drinkers; Table S9: Contingency coefficient between individual lifestyle factors.
Author Contributions
M.S. and S.X. conceptualized the study. Z.L. and C.Z. performed statistical analysis and drafted the manuscript. Z.L., C.Z., J.H., F.O., D.Q., L.L., Y.L., X.L., Y.D. and D.L. participated in the field investigation and study implementation. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and was approved by the Ethical Committee of Xiangya School of Public Health, Central South University (No. XYGW-2016-10).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data used in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare that there are no conflict of interest.
Funding Statement
The work was funded by the Ministry of Science and Technology of China (grant number 2016YFC0900802). Huxiang Youth Talent Program (2022RC1014). Ministry of Industry and Information Technology of China (TC210804V).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Younossi Z.M., Koenig A.B., Abdelatif D., Fazel Y., Henry L., Wymer M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64:73–84. doi: 10.1002/hep.28431. [DOI] [PubMed] [Google Scholar]
- 2.Powell E.E., Wong V.W., Rinella M. Non-alcoholic fatty liver disease. Lancet. 2021;397:2212–2224. doi: 10.1016/S0140-6736(20)32511-3. [DOI] [PubMed] [Google Scholar]
- 3.Byrne C.D., Targher G. NAFLD: A multisystem disease. J. Hepatol. 2015;62:S47–S64. doi: 10.1016/j.jhep.2014.12.012. [DOI] [PubMed] [Google Scholar]
- 4.Sarin S.K., Kumar M., Eslam M., George J., Al Mahtab M., Akbar S.M.F., Jia J., Tian Q., Aggarwal R., Muljono D.H., et al. Liver diseases in the Asia-Pacific region: A Lancet Gastroenterology & Hepatology Commission. Lancet Gastroenterol. Hepatol. 2020;5:167–228. doi: 10.1016/S2468-1253(19)30342-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Han X., Wei Y., Hu H., Wang J., Li Z., Wang F., Long T., Yuan J., Yao P., Wei S., et al. Genetic Risk, a Healthy Lifestyle, and Type 2 Diabetes: The Dongfeng-Tongji Cohort Study. J. Clin. Endocrinol. Metab. 2020;105:1242–1250. doi: 10.1210/clinem/dgz325. [DOI] [PubMed] [Google Scholar]
- 6.Zhu M., Wang T., Huang Y., Zhao X., Ding Y., Zhu M., Ji M., Wang C., Dai J., Yin R., et al. Genetic Risk for Overall Cancer and the Benefit of Adherence to a Healthy Lifestyle. Cancer Res. 2021;81:4618–4627. doi: 10.1158/0008-5472.CAN-21-0836. [DOI] [PubMed] [Google Scholar]
- 7.Zhang Y.B., Chen C., Pan X.F., Guo J., Li Y., Franco O.H., Liu G., Pan A. Associations of healthy lifestyle and socioeconomic status with mortality and incident cardiovascular disease: Two prospective cohort studies. BMJ. 2021;373:n604. doi: 10.1136/bmj.n604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sun Q., Yu D., Fan J., Yu C., Guo Y., Pei P., Yang L., Chen Y., Du H., Yang X., et al. Healthy lifestyle and life expectancy at age 30 years in the Chinese population: An observational study. Lancet Public Health. 2022;7:E994–E1004. doi: 10.1016/S2468-2667(22)00110-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Akhavan Rezayat A., Dadgar Moghadam M., Ghasemi Nour M., Shirazinia M., Ghodsi H., Rouhbakhsh Zahmatkesh M.R., Tavakolizadeh Noghabi M., Hoseini B., Akhavan Rezayat K. Association between smoking and non-alcoholic fatty liver disease: A systematic review and meta-analysis. SAGE Open Med. 2018;6:2050312117745223. doi: 10.1177/2050312117745223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Qiu S., Cai X., Sun Z., Li L., Zugel M., Steinacker J.M., Schumann U. Association between physical activity and risk of nonalcoholic fatty liver disease: A meta-analysis. Therap. Adv. Gastroenterol. 2017;10:701–713. doi: 10.1177/1756283X17725977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ryu S., Chang Y., Jung H.S., Yun K.E., Kwon M.J., Choi Y., Kim C.W., Cho J., Suh B.S., Cho Y.K., et al. Relationship of sitting time and physical activity with non-alcoholic fatty liver disease. J. Hepatol. 2015;63:1229–1237. doi: 10.1016/j.jhep.2015.07.010. [DOI] [PubMed] [Google Scholar]
- 12.Wei H., Qu H., Wang H., Deng H. Associations between sitting time and non-alcoholic fatty liver diseases in Chinese male workers: A cross-sectional study. BMJ Open. 2016;6:e011939. doi: 10.1136/bmjopen-2016-011939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zelber-Sagi S., Lotan R., Shlomai A., Webb M., Harrari G., Buch A., Nitzan Kaluski D., Halpern Z., Oren R. Predictors for incidence and remission of NAFLD in the general population during a seven-year prospective follow-up. J. Hepatol. 2012;56:1145–1151. doi: 10.1016/j.jhep.2011.12.011. [DOI] [PubMed] [Google Scholar]
- 14.Romero-Gomez M., Zelber-Sagi S., Trenell M. Treatment of NAFLD with diet, physical activity and exercise. J. Hepatol. 2017;67:829–846. doi: 10.1016/j.jhep.2017.05.016. [DOI] [PubMed] [Google Scholar]
- 15.Bjermo H., Iggman D., Kullberg J., Dahlman I., Johansson L., Persson L., Berglund J., Pulkki K., Basu S., Uusitupa M., et al. Effects of n-6 PUFAs compared with SFAs on liver fat, lipoproteins, and inflammation in abdominal obesity: A randomized controlled trial. Am. J. Clin. Nutr. 2012;95:1003–1012. doi: 10.3945/ajcn.111.030114. [DOI] [PubMed] [Google Scholar]
- 16.Qiu D., Li R., Li Y., He J., Ouyang F., Luo D., Xiao S. Job Dissatisfaction Mediated the Associations Between Work Stress and Mental Health Problems. Front. Psychiatry. 2021;12:711263. doi: 10.3389/fpsyt.2021.711263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li L., Ouyang F., He J., Qiu D., Luo D., Xiao S. Associations of Socioeconomic Status and Healthy Lifestyle with Incidence of Dyslipidemia: A Prospective Chinese Governmental Employee Cohort Study. Front. Public Health. 2022;10:878126. doi: 10.3389/fpubh.2022.878126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Qiu D., He J., Li Y., Li R., Ouyang F., Li L., Luo D., Xiao S. Stressful Life Events and Chronic Fatigue Among Chinese Government Employees: A Population-Based Cohort Study. Front. Public Health. 2022;10:890604. doi: 10.3389/fpubh.2022.890604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tremblay M.S., Aubert S., Barnes J.D., Saunders T.J., Carson V., Latimer-Cheung A.E., Chastin S.F.M., Altenburg T.M., Chinapaw M.J.M., Participants S.T.C.P. Sedentary Behavior Research Network (SBRN)—Terminology Consensus Project process and outcome. Int. J. Behav. Nutr. Phys. Act. 2017;14:75. doi: 10.1186/s12966-017-0525-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Healy G.N., Clark B.K., Winkler E.A., Gardiner P.A., Brown W.J., Matthews C.E. Measurement of adults’ sedentary time in population-based studies. Am. J. Prev. Med. 2011;41:216–227. doi: 10.1016/j.amepre.2011.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ainsworth B.E., Haskell W.L., Herrmann S.D., Meckes N., Bassett D.R., Jr., Tudor-Locke C., Greer J.L., Vezina J., Whitt-Glover M.C., Leon A.S. 2011 Compendium of Physical Activities: A second update of codes and MET values. Med. Sci. Sports Exerc. 2011;43:1575–1581. doi: 10.1249/MSS.0b013e31821ece12. [DOI] [PubMed] [Google Scholar]
- 22.Harrison S.A., Day C.P. Benefits of lifestyle modification in NAFLD. Gut. 2007;56:1760–1769. doi: 10.1136/gut.2006.112094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yuan F., Gong W., Ding C., Li H., Feng G., Ma Y., Fan J., Song C., Liu A. Association of Physical Activity and Sitting Time with Overweight/Obesity in Chinese Occupational Populations. Obes. Facts. 2021;14:141–147. doi: 10.1159/000512834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen C., Lu F.C., Department of Disease Control Ministry of Health, PR China The guidelines for prevention and control of overweight and obesity in Chinese adults. Biomed. Environ. Sci. 2004;17:1–36. [PubMed] [Google Scholar]
- 25.Zeng M.D., Fan J.G., Lu L.G., Li Y.M., Chen C.W., Wang B.Y., Mao Y.M., Chinese National Consensus Workshop on Nonalcoholic Fatty Liver Disease Guidelines for the diagnosis and treatment of nonalcoholic fatty liver diseases. J. Dig. Dis. 2008;9:108–112. doi: 10.1111/j.1751-2980.2008.00331.x. [DOI] [PubMed] [Google Scholar]
- 26.Deng Y.Y., Zhong Q.W., Zhong H.L., Xiong F., Ke Y.B., Chen Y.M. Higher Healthy Lifestyle Score is associated with lower presence of non-alcoholic fatty liver disease in middle-aged and older Chinese adults: A community-based cross-sectional study. Public Health Nutr. 2021;24:5081–5089. doi: 10.1017/S1368980021000902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Van Kleef L.A., Hofman A., Voortman T., de Knegt R.J. Objectively Measured Physical Activity Is Inversely Associated with Nonalcoholic Fatty Liver Disease: The Rotterdam Study. Am. J. Gastroenterol. 2022;117:311–318. doi: 10.14309/ajg.0000000000001584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Du S., Wang C., Jiang W., Li C., Li Y., Feng R., Sun C. The impact of body weight gain on nonalcoholic fatty liver disease and metabolic syndrome during earlier and later adulthood. Diabetes Res. Clin. Pract. 2016;116:183–191. doi: 10.1016/j.diabres.2016.04.047. [DOI] [PubMed] [Google Scholar]
- 29.Fernandes F.M.C., Martins E.S., Pedrosa D., Evangelista M. Relationship between climatic factors and air quality with tuberculosis in the Federal District, Brazil, 2003–2012. Braz. J. Infect. Dis. 2017;21:369–375. doi: 10.1016/j.bjid.2017.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yu C., Gao J., Ge X., Wang X., Ding Y., Tian T., Xu X., Guo W., Wang Q., Ge Z., et al. Healthy Lifestyle Is Associated with Reduced Mortality in Patients with Non-Alcoholic Fatty Liver Disease. Nutrients. 2022;14:3785. doi: 10.3390/nu14183785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhu Y., Yang H., Liang S., Zhang H., Mo Y., Rao S., Zhang Y., Zhang Z., Wang W., Yang W. Higher Adherence to Healthy Lifestyle Score Is Associated with Lower Odds of Non-Alcoholic Fatty Liver Disease. Nutrients. 2022;14:4462. doi: 10.3390/nu14214462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhang H.J., He J., Pan L.L., Ma Z.M., Han C.K., Chen C.S., Chen Z., Han H.W., Chen S., Sun Q., et al. Effects of Moderate and Vigorous Exercise on Nonalcoholic Fatty Liver Disease: A Randomized Clinical Trial. JAMA Intern. Med. 2016;176:1074–1082. doi: 10.1001/jamainternmed.2016.3202. [DOI] [PubMed] [Google Scholar]
- 33.Promrat K., Kleiner D.E., Niemeier H.M., Jackvony E., Kearns M., Wands J.R., Fava J.L., Wing R.R. Randomized controlled trial testing the effects of weight loss on nonalcoholic steatohepatitis. Hepatology. 2010;51:121–129. doi: 10.1002/hep.23276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wong V.W., Wong G.L., Chan R.S., Shu S.S., Cheung B.H., Li L.S., Chim A.M., Chan C.K., Leung J.K., Chu W.C., et al. Beneficial effects of lifestyle intervention in non-obese patients with non-alcoholic fatty liver disease. J. Hepatol. 2018;69:1349–1356. doi: 10.1016/j.jhep.2018.08.011. [DOI] [PubMed] [Google Scholar]
- 35.Bischoff M., Zimny S., Feiner S., Sauter J., Sydor S., Denk G., Nagel J.M., Bischoff G., Rust C., Hohenester S. Multidisciplinary lifestyle intervention is associated with improvements in liver damage and in surrogate scores of NAFLD and liver fibrosis in morbidly obese patients. Eur. J. Nutr. 2022;61:2725–2735. doi: 10.1007/s00394-022-02846-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.World Health Statistics 2019: Monitoring Health for the SDGs, Sustainable Development Goals. World Health Organization; Geneva, Switzerland: 2019. [Google Scholar]
- 37.Lonardo A., Nascimbeni F., Ballestri S., Fairweather D., Win S., Than T.A., Abdelmalek M.F., Suzuki A. Sex Differences in Nonalcoholic Fatty Liver Disease: State of the Art and Identification of Research Gaps. Hepatology. 2019;70:1457–1469. doi: 10.1002/hep.30626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lonardo A., Suzuki A. Sexual Dimorphism of NAFLD in Adults. Focus on Clinical Aspects and Implications for Practice and Translational Research. J. Clin. Med. 2020;9:1278. doi: 10.3390/jcm9051278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shima T., Seki K., Umemura A., Ogawa R., Horimoto R., Oya H., Sendo R., Mizuno M., Okanoue T. Influence of lifestyle-related diseases and age on the development and progression of non-alcoholic fatty liver disease. Hepatol. Res. 2015;45:548–559. doi: 10.1111/hepr.12384. [DOI] [PubMed] [Google Scholar]
- 40.Yatsuji S., Hashimoto E., Tobari M., Tokushige K., Shiratori K. Influence of age and gender in Japanese patients with non-alcoholic steatohepatitis. Hepatol. Res. 2007;37:1034–1043. doi: 10.1111/j.1872-034X.2007.00156.x. [DOI] [PubMed] [Google Scholar]
- 41.Long M.T., Pedley A., Massaro J.M., Hoffmann U., Ma J., Loomba R., Chung R.T., Benjamin E.J. A simple clinical model predicts incident hepatic steatosis in a community-based cohort: The Framingham Heart Study. Liver Int. 2018;38:1495–1503. doi: 10.1111/liv.13709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Li L., Liu D.W., Yan H.Y., Wang Z.Y., Zhao S.H., Wang B. Obesity is an independent risk factor for non-alcoholic fatty liver disease: Evidence from a meta-analysis of 21 cohort studies. Obes. Rev. 2016;17:510–519. doi: 10.1111/obr.12407. [DOI] [PubMed] [Google Scholar]
- 43.Fan J.G., Kim S.U., Wong V.W. New trends on obesity and NAFLD in Asia. J. Hepatol. 2017;67:862–873. doi: 10.1016/j.jhep.2017.06.003. [DOI] [PubMed] [Google Scholar]
- 44.Lu F.B., Hu E.D., Xu L.M., Chen L., Wu J.L., Li H., Chen D.Z., Chen Y.P. The relationship between obesity and the severity of non-alcoholic fatty liver disease: Systematic review and meta-analysis. Expert Rev. Gastroenterol. Hepatol. 2018;12:491–502. doi: 10.1080/17474124.2018.1460202. [DOI] [PubMed] [Google Scholar]
- 45.Camhi S.M., Bray G.A., Bouchard C., Greenway F.L., Johnson W.D., Newton R.L., Ravussin E., Ryan D.H., Smith S.R., Katzmarzyk P.T. The relationship of waist circumference and BMI to visceral, subcutaneous, and total body fat: Sex and race differences. Obesity. 2011;19:402–408. doi: 10.1038/oby.2010.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mongraw-Chaffin M., Golden S.H., Allison M.A., Ding J., Ouyang P., Schreiner P.J., Szklo M., Woodward M., Young J.H., Anderson C.A. The Sex and Race Specific Relationship between Anthropometry and Body Fat Composition Determined from Computed Tomography: Evidence from the Multi-Ethnic Study of Atherosclerosis. PLoS ONE. 2015;10:e0139559. doi: 10.1371/journal.pone.0139559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Vilar-Gomez E., Martinez-Perez Y., Calzadilla-Bertot L., Torres-Gonzalez A., Gra-Oramas B., Gonzalez-Fabian L., Friedman S.L., Diago M., Romero-Gomez M. Weight Loss through Lifestyle Modification Significantly Reduces Features of Nonalcoholic Steatohepatitis. Gastroenterology. 2015;149:367–378.e5. doi: 10.1053/j.gastro.2015.04.005. quiz e314–365. [DOI] [PubMed] [Google Scholar]
- 48.Koutoukidis D.A., Koshiaris C., Henry J.A., Noreik M., Morris E., Manoharan I., Tudor K., Bodenham E., Dunnigan A., Jebb S.A., et al. The effect of the magnitude of weight loss on non-alcoholic fatty liver disease: A systematic review and meta-analysis. Metabolism. 2021;115:154455. doi: 10.1016/j.metabol.2020.154455. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data used in this study are available on request from the corresponding author.