The first cohort of IIPE projects from 2009 are beginning to realize some early successes. We bring you this article in the spirit of sharing what works and what doesn't. The lesson about the importance of context is critical in adopting and adapting innovations to your own learning environment.
—Carol Carraccio, MD, MA
Section Editor
New duty hours standards have increased the frequency of transitions in care or handoffs for resident physicians. Because miscommunications are a leading cause of adverse events in hospitals, optimizing the handoff process is essential for patient safety. The I-PASS Study aims to determine the effectiveness of implementing a “resident handoff bundle” to standardize inpatient transitions in care and decrease medical errors in 10 pediatric institutions. 1 The resident handoff bundle includes 3 major elements: team training by using focused TeamSTEPPS communication strategies, 2 implementation of a standardized template for the written or printed computerized handoff document, and introduction of several evidence-based verbal handoff processes, which are referred to by using a novel verbal mnemonic. This multisite collaborative education and research project was launched with the support of the Initiative for Innovation in Pediatric Education (IIPE) and the Pediatric Research in Inpatient Settings (PRIS) network. The title I-PASS is an acronym that not only denotes the title and purpose of our research study—IIPE-PRIS Accelerating Safe Sign-outs—but also serves as the verbal mnemonic for the standardized handoff itself. Individual elements of the I-PASS mnemonic will be defined in this article.
Mnemonics are memory aids. Effective mnemonics are catchy, symbolic, parsimonious, utilitarian, and may conjure up a visual image linked to a process or subject. In this report, we emphasize the importance of structured communication strategies to enhance patient safety, review literature pertinent to the handoff process, including the use of verbal mnemonics, and describe the creation of the I-PASS mnemonic, a core element of our resident handoff bundle.
Background
Communication errors are a contributing cause of approximately two-thirds of sentinel events, 3 over half of which involve handoff failures. 4 In health care, the magnitude of the patient safety epidemic first became widely recognized with the publication of To Err Is Human in 1999, which concluded that medical errors cause up to 98 000 preventable deaths annually in the United States. 5 Subsequently, calls for action emerged from the federal government and many private and professional organizations, including the recommendation that principles from High Reliability Organizations (HROs) be applied to the health care system.
HROs are organizations in high-risk, high-impact industries that consistently achieve high quality outcomes despite experiencing many unexpected events where the potential for error is very high. 6 These organizations employ team training and reliability science to improve their performance, the roots of which arose from the military and civilian aviation communities. Programs such as Crew Resource Management have led to major advances in team training and may result in dramatic improvements in fatalities, accident related costs, and human factor based mishaps.
A specific application of HRO principles is the use of explicit verbal mnemonics to standardize communication. One of the most commonly used communication tools, SBAR, an acronym for “situation, background, assessment, recommendation,” was developed by Doug Bonacum, vice president of Kaiser Permanente and former safety officer on a nuclear submarine. 7 During a patient safety workgroup meeting, Bonacum described expectations when handing off a situation to an officer on deck. These key concepts were translated into core elements of the SBAR mnemonic. Success of a pilot study investigating the use of SBAR as a communication tool led to rapid spread across hospitals nationwide and studies examining its effectiveness. 8 Implementation of SBAR in 1 hospital was associated with substantial drops in the rates of adverse events (from 90 to 40 per 1000 patient days) and adverse drug events (from 30 to 18 per 1000 patient days). 9
SBAR was developed to facilitate the efficient transmission of information. It is most effective when time is limited and a quick decision is needed, as this tool is suited to situations when a brief summary is sufficient and fewer than 5 key points need to be communicated. Further, this mnemonic should be used as a situational briefing tool, as intended, and is appropriate for use across hierarchical boundaries. 10 Although use of SBAR has been extended to handoffs of patient care at change of shift or patient location, there are limitations in its applicability, particularly in situations that include transmission of information about complex patients who require broader information and context.
Development of the I-PASS Mnemonic
Given the limitations of SBAR, alternative mnemonics have been developed, implemented, and tested for use in handoffs of care. A recent systematic review of published handoff mnemonics identified 46 articles describing 24 different handoff mnemonics. 11 Most have not been rigorously studied, however, and descriptions of their derivation are lacking. A notable exception includes an article describing the use of the SIGNOUT mnemonic, which was shown to increase the consistency and confidence with which residents perform verbal sign-outs, as compared with an implicit, informally structured process. 12
Drawing from the apparent evidence-based success of the SIGNOUT mnemonic, we included the SIGNOUT mnemonic in a pilot resident handoff bundle intervention study at the Children's Hospital Boston that preceded the ongoing multicenter I-PASS study. Resident input was a key factor in this selection. Efforts were made to reinforce use of the mnemonic during the postintervention study period, including regular faculty and chief resident observations and feedback regarding the verbal handoff process. However, we found that a majority of verbal handoffs did not adhere to the structure of the SIGNOUT mnemonic.
As part of the process for curriculum development for the I-PASS study, we reflected on the successes and challenges of SIGNOUT, and considered use of the mnemonic, IPASSTHEBATON from TeamSTEPPS. 13 Feedback from chief residents who had been involved in the pilot curriculum, however, expressed the need for a mnemonic that was shorter, easier to remember, and had discrete elements without overlap. They felt strongly that elements of the mnemonic needed to be fully integrated into computerized handoff tools.
Modeling the process used to design the original SBAR mnemonic, we (Drs Starmer, Spector, Landrigan, and Sectish) conducted a brainstorming session and identified the essential elements of a verbal handoff. We focused on elements that pilot study faculty observers noted were most commonly absent from resident handoffs (illness severity assessment, contingency planning, and read-back by the receiving resident) and incorporated best practices for verbal handoffs from our review of existing literature.
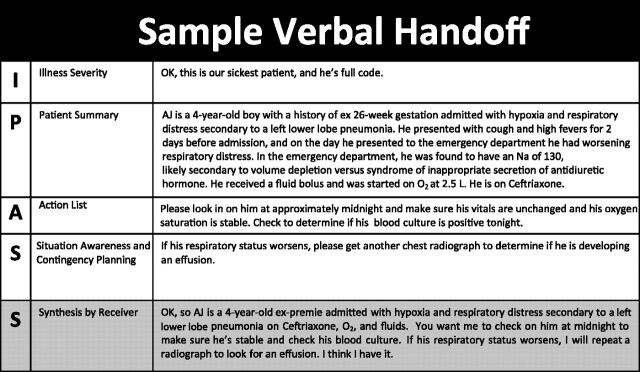
The results of this session led to the development of a novel mnemonic, I-PASS (Fig 1), which serves as the cornerstone for the resident handoff bundle that is currently being implemented and tested in the I-PASS study.
FIGURE 1.
Elements of the I-PASS mnemonic.
The I-PASS mnemonic provides a framework for the patient handoff process as follows:
I: Illness severity
P: Patient summary
A: Action list
S: Situation awareness and contingency planning
S: Synthesis by receiver
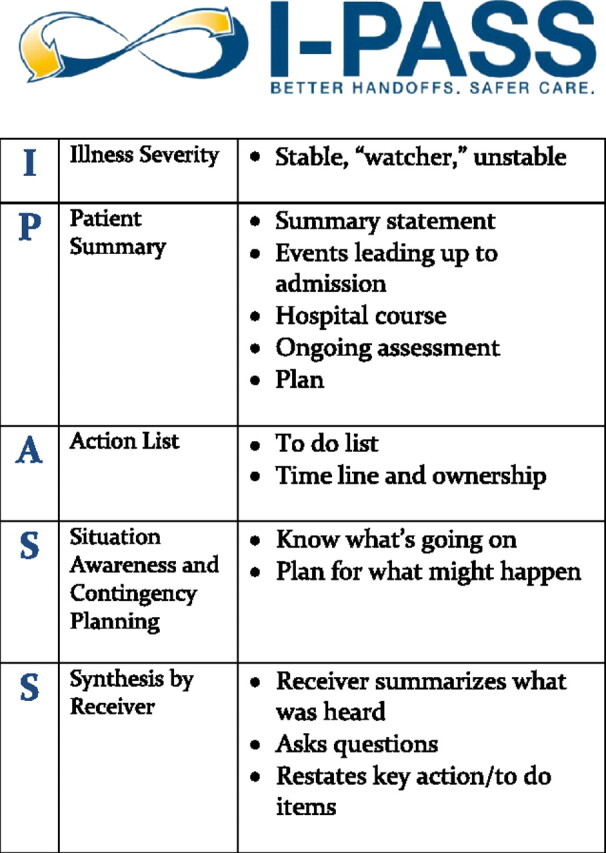
An example of a verbal I-PASS handoff communication is provided in Fig 2.
FIGURE 2.
Example of a verbal handoff by using the I-PASS mnemonic.
As we began implementing the I-PASS mnemonic, we received widespread interest in it from other providers in our study institutions, including physicians from other specialties and nurses. We believe that it can readily be adapted for use beyond pediatrics. Specifically, the patient summary element is easily adapted to include specific information elements that are key for each provider type.
Conclusions
The novel mnemonic, I-PASS, was developed from best handoff practices cited in the literature, resident feedback from a pilot study, and observations made by faculty of the handoff process. Structured communication, especially at the time of transitions in care, is essential to promote patient safety. The multisite I-PASS study will test the effectiveness of the resident handoff bundle, including the I-PASS mnemonic, on medical errors in 10 pediatric institutions. Lessons learned may apply to other settings where the opportunities to improve the handoff process remain a challenge.
Acknowledgments
This project was supported with a grant from the US Department of Health and Human Services, Office of the Assistant Secretary for Planning and Evaluation, grant 1R18AE000023-01. Additionally Drs Landrigan and Srivastava are supported in part by the Child Health Corporation of America for their work on the PRIS Research Network Executive Council. Dr Starmer is supported in part by an institutional K12 award from Oregon Health and Science University and the Agency for Health Care Research and Quality, grant 1K12HS019456-01. Developed with input from the IIPE and the PRIS Network.
IIPE is the Initiative for Innovation in Pediatric Education and is the entity that recognizes innovative educational proposals for pediatric residency training programs. More can be found on the Web site, www.innovatepedsgme.org.
PRIS is a collaborative hospitalist research network sponsored by the American Academy of Pediatrics, the Academic Pediatric Association, the Society of Hospital Medicine, and the Child Health Corporation of America. Details are available at http://www.prisnetwork.org.
Members of the I-PASS Study Group include coinvestigators from the following institutions as follows: Children's Hospital Boston (primary site): April D. Allen, MPA, MA, Angela Feraco, MD, Christopher P. Landrigan, MD, MPH, Theodore C. Sectish, MD; Brigham and Women's Hospital (data coordinating center): Carol Keohane, RN, Stuart Lipsitz, PhD, Jeffrey Rothschild, MD, MPH; Cincinnati Children's Hospital Medical Center: Javier Gonzalez del Rey, MD, Med, Jennifer O'Toole, MD, Lauren Solan, MD; Doernbecher Children's Hospital/Oregon Health and Science University: Megan Aylor, MD, Gregory Blaschke, MD, MPH, Cynthia L. Ferrell, MD, MSEd, Benjamin D. Hoffman, MD, Amy J. Starmer, MD, MPH, Windy Stevenson, MD, Tamara Wagner, MD; Hospital for Sick Children/University of Toronto: Zia Bismilla, MD, Maitreya Coffey, MD, Sanjay Mahant, MD, MSc, Anne Matlow, MD; Lucile Packard Children's Hospital/Stanford University: Lauren Destino, MD, Jennifer Everhart, MD, Madelyn Kahana, MD, Shilpa J. Patel, MD; National Capital Consortium: Jennifer Hepps, MD, Joseph O. Lopreiato, MD, MPH, Clifton E. Yu, MD; Primary Children's Medical Center/Intermountain Health Care: James F. Bale, Jr., MD, Rajendu Srivastava, MD, MPH, Adam Stevenson, MD; St. Louis Children's Hospital/Washington University: Kathleen Berchelmann, MD, F. Sessions Cole, MD, Christine Hrach, MD, Kyle S. Schulz, MD, Michael Turmelle, MD, Andrew White, MD; St. Christopher's Hospital for Children: Sharon Calaman, MD, Bronwyn D. Carlson, MD, Matthew B. McDonald III, MD, Robert S. McGregor, MD, Vahideh Nilforoshan, MD, Nancy D. Spector, MD; and University of California, San Francisco, Benioff Children's Hospital: Glenn Rosenbluth, MD, Daniel C. West, MD. Dorene Balmer, PhD, RD and Alan Schwartz, PhD, serve the I-PASS Study Group as part of the IIPE Research Support Team. Karen M. Wilson, MD, MPH, serves the I-PASS Study Group as part of the PRIS advisory board.
Footnotes
The opinions and conclusions expressed herein are solely those of the authors and should not be constructed as representing the opinions or policy of any agency of the Federal Government.
References
- 1. Sectish TC , Starmer AJ , Landrigan CP , Spector ND ; I-PASS Study Group. Establishing a multisite education and research project requires leadership, expertise, collaboration, and an important aim. Pediatrics. 2010;126(4):619–622 [DOI] [PubMed] [Google Scholar]
- 2. US Department of Health and Human Services, Agency for Healthcare Research and Quality. TeamSTEPPS home page. Available at: http://teamstepps.ahrq.gov/. Accessed September 29, 2011
- 3. The Joint Commission. Sentinel event statistics data: root causes by event type. Available at: www.jointcommission.org/Sentinel_Event_Statistics/. Accessed September 27, 2011
- 4. The Joint Commission. Improving hand-off communications: meeting national patient safety goal 2E. Joint Commission Perspectives on Patient Safety. 2006;6(8):9–15 [Google Scholar]
- 5. Institute of Medicine. To Err Is Human: Building a Safer Health System. Washington, DC: National Academy Press; 1999. [Google Scholar]
- 6. McKeon LM , Oswaks JD , Cunningham PD . Safeguarding patients: complexity science, high reliability organizations, and implications for team training in healthcare. Clin Nurse Spec. 2006;20(6):298–304, quiz 305–306 [DOI] [PubMed] [Google Scholar]
- 7. Denham CR . SBAR for patients. J Patient Saf. 2008;4(1):38–48 [Google Scholar]
- 8. McFerran S , Nunes J , Pucci D , Zuniga A . Perinatal Patient Safety Project: a multicenter approach to improve performance reliability at Kaiser Permanente. J Perinat Neonatal Nurs. 2005;19(1):37–45 [DOI] [PubMed] [Google Scholar]
- 9. Haig KM , Sutton S , Whittington J . SBAR: a shared mental model for improving communication between clinicians. Jt Comm J Qual Patient Saf. 2006;32(3):167–175 [DOI] [PubMed] [Google Scholar]
- 10. Monroe M . SBAR: A structured human factors communication technique. Health Beat. Des Plaines, IL: American Society of Safety Engineers. Available at: www.asse.org/practicespecialties/healthcare/docs/HealthBeat_Newsletter_Spring2006forWeb.pdf. Accessed September 27, 2011 [Google Scholar]
- 11. Riesenberg LA , Leitzsch J , Little BW . Systematic review of handoff mnemonics literature. Am J Med Qual. 2009;24(3):196–204 [DOI] [PubMed] [Google Scholar]
- 12. Horwitz LI , Moin T , Green ML . Development and implementation of an oral sign-out skills curriculum. J Gen Intern Med. 2007;22(10):1470–1474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. US Department of Health and Human Services, Agency for Healthcare Research and Quality. Pocket guide: TeamSTEPPS. Available at: www.ahrq.gov/teamsteppstools/instructor/essentials/pocketguide.htm#passbaton. Accessed September 28, 2011