Abstract
Background:
Women with high body mass indices are at risk of lower breastfeeding rates but the drivers of successful breastfeeding in this population are unclear.
Research Aim:
We aimed to (a) explore the barriers and enablers to breastfeeding among women with high body mass indices and (b) map specific behaviors suitable for intervention across the antenatal to postpartum periods.
Methods:
This was a prospective, cross-sectional qualitative study. We conducted semi-structured interviews with women with high body mass indices who successfully breastfed for 6 months or more (n =20), partners (n = 22), and healthcare professionals (n =19) in Ireland during 2018. Interviews were audio recorded, and transcribed verbatim. Data were inductively coded using reflexive thematic analysis and deductively mapped within the Capability, Opportunity, Motivation–Behavior model.
Results:
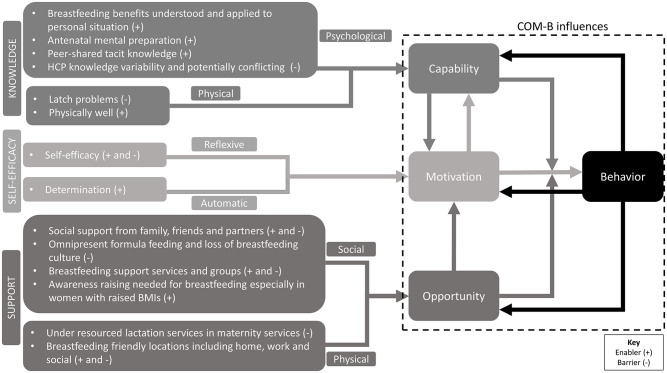
The three themes developed were knowledge, support, and self-efficacy. Knowledge supported a participant’s psychological and physical capability to engage in breastfeeding. Support was related to the social and physical opportunity to enable performance of breastfeeding behaviors. Self-efficacy influenced reflective and automatic motivation to perform breastfeeding behaviors. A multifactorial intervention design is needed to support successful breastfeeding.
Conclusion:
The barriers and enablers identified for participants with high body mass indices were similar to those for the broader population; however, the physicality and associated social bias of high body mass indices mean that additional support is warranted. Antenatal and postpartum breastfeeding services need a multifaceted, inclusive, and high-quality program to provide the necessary support to women with higher body mass indices.
Keywords: breastfeeding, breastfeeding barriers, breastfeeding experience, breastfeeding support, Capability, Opportunity, Motivation Behavior-Model, Ireland, positive deviance, qualitative methods
Key Messages.
Breastfeeding is 10%–20% lower in women with high body mass indices (≥ 25 kg/m2). Factors to support successful breastfeeding for this population are not well understood.
Personal knowledge and knowing how to manage physical breastfeeding challenges supported participants’ breastfeeding capability.
Participants reported that breastfeeding opportunity was supported by social influences, resources, and environments, while breastfeeding motivation was fostered by self-efficacy.
Understanding successful breastfeeding behaviors will help develop evidence-based interventions to increase breastfeeding rates in women with high body mass indices.
Background
In 2014, 38.9 million and 14.6 million pregnant women globally had a pregnancy with a body mass index (BMI) ≥ 25 and 30 respectively (Chen et al., 2018). The prevalence of obesity and overweight are increasing worldwide (NCD Risk Factor Collaboration, 2017) and are linked to lower breastfeeding rates (Ramji et al., 2018; Mangel et al., 2019). In Australia, women with obesity were reported to have 9% less breastfeeding initiation (Bish et al., 2021), and lower breastfeeding initiation rates have also been reported in the United States (Kair & Colaizy, 2016) and France (Boudet-Berquier et al., 2018). A lower likelihood of sustained breastfeeding among women with high BMIs also has been reported as prevalent globally (Boudet-Berquier et al., 2018; Chen et al., 2020; Joham et al., 2016). Successfully establishing and sustaining breastfeeding has numerous health benefits, including reduced childhood obesity (Sirkka et al., 2021) and increased postpartum weight loss (Dalrymple et al., 2021). Given that the number of women of childbearing age with high BMIs is rising, improving their breastfeeding rates would contribute towards reductions in obesity in later life. The measurable difference in breastfeeding outcomes among women with high BMIs supports potentially different behavioral factors influencing their infant feeding decisions and the need to understand these better to facilitate breastfeeding outcomes.
Most behavioral research undertaken to date has examined what barriers exist for breastfeeding in women with high BMIs. The barriers commonly reported include lack of support (Chang et al., 2020), lack of confidence, difficulty finding suitable breastfeeding clothes (Garner et al., 2017), formula feeding culture, and embarrassment of feeding in public (Chang et al., 2020). The mixed-methods review undertaken by Chang and colleagues (2020) explored issues relating to larger breasts, delayed onset of lactation, and psychosocial factors. Limited research exists on what is known to contribute to and to support successful extended breastfeeding in women with high BMIs. Researchers have focused on stakeholder groups in isolation with little data collected from partners and healthcare professionals involved in supporting this population.
Breastfeeding is a multifaceted and multilevel behavior, which means a complex intervention design is required to address it. The U.K. Medical Research Council’s guidance (Skivington et al., 2021) about developing and evaluating complex interventions recommended that the development phase involve identifying or developing theory about changes required. We have used two theoretical frameworks, the Capability, Opportunity, Motivation-Behavior (COM-B) Model and positive deviance, to ground our work.
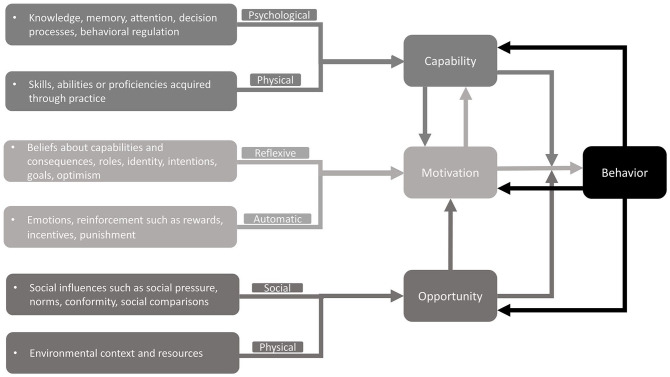
The COM-B Model of behavior has been widely used to map behaviors suitable for intervention design (Michie et al., 2011). It synthesizes 14 behavioral constructs and proposes that behavior is the result of the interaction between capability (psychological or physical), opportunity (social or physical), and motivation (reflective or automatic; Michie et al., 2011). The COM-B model is widely used to examine barriers and enablers at multiple levels, including those of the patient, the provider, and the system (McDonagh et al., 2018).
One of the most efficient ways to improve health outcomes within population subgroups is to identify individuals already practicing the desired health behavior, in this case extended breastfeeding, and to study how they have adopted these behaviors using an approach called positive deviance (Rose & McCullough, 2017). The health behaviors identified through this approach are likely to be both acceptable and sustainable because they are already being practiced by the desired population subgroup within existing resources (Bradley et al., 2009; Marsh et al., 2004, ). The positive deviance approach typically consists of four steps (Bradley et al. 2009). The first two are explored in this study, which are the identification of “positive deviants” who are individuals demonstrating the desired health behavior and conducting in-depth qualitative analyses to generate insights about the behaviors that will allow development of suitable interventions.
The final two positive deviance approach steps are testing the intervention in representative samples and working in partnership with key stakeholders to disseminate the new intervention. These steps will be conducted based on the findings of this study. For the purposes of this study, both the women and partners were considered “positive deviants.” This study aimed to (a) explore the barriers and enablers to breastfeeding in women with high body mass indices, and (b) map specific behaviors suitable for intervention across the antenatal to postpartum periods.
Method
Research Design
This was a prospective, cross-sectional qualitative study performed using a semi-structured interview guide. This design enabled us to explore both barriers and enablers to successful breastfeeding behaviors and to map those behaviors for intervention development. Ethical approval was granted by the National Maternity Hospital Ethics Committee (EC.19.2017).
Setting and Relevant Context
This study was conducted in Ireland, a high-income country with low breastfeeding rates. Breastfeeding upon discharge from maternity services is 58.5% (Health Service Executive, 2021), which normally occurs on Day 2 postpartum. At 6 months, about 25% of mothers are breastfeeding and less than 10% are exclusively breastfeeding (Purdy et al., 2017). Women are entitled to paid (26 weeks, with 2 weeks mandated to be prior to the baby’s due date) and unpaid maternity leave (up to 16 weeks) alongside job protection during that time. Ireland has a public health system that provides maternity services for free, or women can opt for private care for an additional cost. The services provided within the antenatal period include education classes about pregnancy, birth, and parenting. These classes are not mandatory to attend, and breastfeeding preparation is covered within many of these classes. Additional breastfeeding education can be accessed privately through International Board Certified Lactation Consultants (IBCLCs). The BMI of women becoming pregnant in Ireland aligns with other high-income countries and, on average, one in two women enter pregnancy with a high BMI as categorized using the World Health Organizations (WHO) classifications (Reynolds et al., 2019).
Sample
The target population consisted of women with high BMIs who had exclusively breastfed for more than 6 months, partners of women who had exclusively breastfed for more than 6 months, and HCP staff within the National Maternity Hospital. The inclusion criteria varied; for women, a BMI ≥ 25kg/m2 and exclusive breastfeeding for 6 months or more within the previous 2 years were required, for partners it was being the main support for a woman who had breastfed successfully for 6 months or more within the previous 2 years, and for HCPs being a registered HCP involved in providing breastfeeding support (obstetricians, midwives, dietitians, and IBCLCs) and being employed by the National Maternity Hospital. A sampling target of 20 participants for each stakeholder group was set for the interviews based on previous research experience, but we determined that a sufficient sample had occurred when our major categories showed depth and variation in their development. This sampling frame yielded high quality informational power, whereby the greater information the sample holds, the lower number of participants needed (Malterud et al., 2016). The final sample size was 61, with 20 breastfeeding participants, 22 partners, and 19 HCPs.
Data Collection
Data were collected between March and December 2018. Women were recruited through open advertisement on Irish social media sites including Facebook groups and pages, with leaflets circulated and posters placed in the National Maternity Hospital, Dublin. Partners were recruited through social media advertisements, posters in the National Maternity Hospital, and word of mouth. HCPs were recruited via posters and direct invitation. A participant information sheet and consent sheet were provided to all individuals who expressed an interest in taking part. The research team contacted all individuals expressing an interest in participating by phone and confirmed their eligibility prior to answering any questions, receiving provisional verbal consent, and organizing the research interview. Informed consent was provided prior to or at the start of each interview and participants were asked to sign the interview consent form. Only those with signed consent proceeded to interview.
A qualified midwife with more than 10 years midwifery experience and a lived experience of extended breastfeeding of all her children for 6 months or more (JC) performed the interviews with participants and partners. A final year BSc Human Nutrition student (EOC) with no personal experience of breastfeeding, apart from their extended family, completed formal interview training and conducted the HCP interviews. Interviews were audio recorded using a digital device. Interviews with participants and partners were conducted by telephone by JC in a quiet room and lasted approximately 1 hr. HCP interviews were conducted by EOC via telephone or face-to-face in a private room. These interviews lasted approximately 30 min. No relationships existed between any interviewer and participants. The interviewers did not disclose any information about their professional or lived experience with breastfeeding during these interviews. The study objectives and recording of interviews were explained to participants before the interviews began. All question topics (breastfeeding experience and knowledge, attitudes, key supports) were covered in the semi-structured interview (Supplementary Materials Table 1). Background information about age, education level, and number of children was obtained at the start of the participant and partner interviews. Trustworthiness was established through pilot testing of the interview guides, maintaining interview field notes, member checking, triangulation, clarifying bias to ensure accuracy, and using multiple data coders (Lub, 2015).
Interviews were also used to identify any “emotional truths” conveyed during discussions of barriers and enablers encountered. Emotional truths are insights or observations within the positive deviance approach that could resonate affectively with a target audience and can influence decision-making. The HCP interviews were conducted to add the provider perspective and maternity service context to the COM-B analysis.
Participant confidentiality was maintained by allocating a study ID to each participant allowing for all names and participant details to be removed during data transcription. Audio recordings were stored on a secure computer with password protection and deleted once transcribed verbatim and checked for accuracy. Transcripts were stored on a secure, password protected computer. The interviews were transcribed verbatim by trained members of the wider research team, specifically by BSc Human Nutrition students (HW, EOC, AG, EOG, SC).
Data Analysis
Demographic data were analyzed and presented as numbers (%). HW and EOC performed the data analysis of the transcripts independently and neither researcher had any lived experience of breastfeeding other than extended family members or receiving lectures on breastfeeding. Reflexive thematic analysis was applied inductively (Braun & Clarke, 2006, 2019). Initially the transcripts were read and reread to familiarize researchers with the data and, after this, they generated codes relating to the first research aim. Initial themes were developed using these codes and subsequently refined so that they contained a pattern of shared meaning underpinned by a central concept (Table 1). Finally, the themes were named and defined and a consensus discussion involving an experienced researcher (SOR, academic HCP with more than 15 years’ experience, and a lived experience of extended breastfeeding several children) resolved any discrepancies. The transcripts were then coded deductively by a third researcher (EM, BSc Human Nutrition final year student, no personal experience of breastfeeding as per HW and EOC) using the COM-B domains as shown in Figure 1 (Michie et al., 2011) and a reflexive thematic analysis approach used for this secondary analysis. When the COM-B barrier and enabler analysis was complete, the behavioral enablers were mapped onto existing lactation services across the antenatal and postpartum time points to address the second aim.
Table 1.
Data Analysis Structure.
| Theme | Theme Definition | Category | Category Definition |
|---|---|---|---|
| Knowledge supports a woman’s capability to engage in BF behavior | How personalized knowledge of BF benefits, mental preparation, healthcare professional support, potential physical difficulties women may face, and the experience of others contributes towards extended BF | 1. Personalize BF benefits 2. Antenatal mental preparation needed 3. Peer-shared tacit knowledge 4. Healthcare professional knowledge inconsistent 5. Knowledge of potential latch problems 6. Physical health important |
1. Descriptions of how BF benefits are applied to personal circumstances 2. Descriptions of mental preparation supporting readiness to breastfeed 3. Descriptions of peer-sharing practical knowledge through a variety of routes 4. Descriptions of healthcare professional knowledge being variable and potentially conflicting 5. Descriptions of challenges with latching due to larger breast volume or tongue-tie 6. Descriptions of importance of overall physical health and staying healthy to engage in BF |
| Support provided by social, environmental and resources enable the performance of BF behaviors | How the opportunity to perform BF behaviors are influenced by social supports, the physical environment, and resources available | 1. Social support importance 2. Reduced support of BF due to omnipresent formula feeding and loss of BF culture 3. BF support services and groups variable 4. Awareness raising needed 5. BF friendly environments 6. Lack of lactation support in maternity services 7. BF aids |
1. Descriptions of social supports that supported or inhibited BF behaviors 2. Descriptions of formula feeding as the norm in Ireland and suppressing BF in cultures where BF is normal 3. Descriptions of different support groups and services impacting BF experience positively and negatively 4. Descriptions of different healthcare professionals needing greater education and awareness to support BF 5. Descriptions of environments such as workplaces, home and social settings that either supported or inhibited BF 6. Descriptions of lactation services being insufficient within maternity settings 7. Descriptions of BF aids such as pillows, co-sleeper cot, lanolin improving BF |
| Self-efficacy impacts motivation to perform BF behaviors | The importance of self-efficacy and determination in extended BF | 1. Self-efficacy is important 2. Determination drives the habit |
1. Descriptions of self-efficacy attributes supporting BF or body image negatively impacting self-efficacy 2. Descriptions of determination positively driving BF and cultural norms facilitating the determination |
Note. BF = breastfeeding.
Figure 1.
The Capability, Opportunity, Motivation-Behavior (COM-B) Model (Michie et al., 2011).
Results
Characteristics of the Sample
Participants and partners interviewed were aged 25–49, had a child who was breastfed for a minimum of 6 months and maximum of 30 months, and the majority had completed third level education (Table 2). Nineteen HCPs, including obstetricians, midwives, dietitians, and IBCLCs participated, whose practice experience ranged from 8 months to 30 years (Table 3). Three themes developed were knowledge, support, and self-efficacy following data analysis (Table 1), which are visually represented in Figure 2 where specific barriers and enablers are identified, and how these relate to the COM-B model.
Table 2.
Participants’ Characteristics of Participants and Their Partners (n = 42).
| Characteristic | Participants n=20 (47.6%) n (%) | Partners n=22 (52.4%) n (%) |
|---|---|---|
| Age | ||
| 18-24 | 0 (0) | 0 (0) |
| 25-29 | 5 (25) | 2 (9) |
| 30-34 | 4 (20) | 5 (23) |
| 35-39 | 4 (20) | 12 (55) |
| 40-44 | 6 (30) | 2 (9) |
| 45-49 | 1 (5) | 1 (5) |
| Level of education | ||
| None | 0 (0.0) | 1 (5) |
| Secondary education, vocational certificate | 3 (15) | 4 (18) |
| Undergraduate | 6 (30) | 9 (41) |
| Postgraduate | 11 (55) | 8 (36) |
| Number of Children | ||
| 1 | 7 (35) | 12 (55) |
| 2 | 9 (45) | 7 (32) |
| 3 | 2 (10) | 2 (9) |
| 4 | 1 (5) | 1 (5) |
| 5 | 1 (5) | 0 (0) |
| Breastfeeding duration (months) | ||
| 6-12 | 7 (35) | 7 (33) |
| 13-18 | 6 (30) | 4 (19) |
| 19-24 | 2 (10) | 5 (24) |
| 25-29 | 0 (0) | 2 (9) |
| >30 | 5 (25) | 3 (14) |
Table 3.
Characteristics of Healthcare Provider Participants (n =19).
| Type of Healthcare Provider | Female Participants n (%) | Experience (years) |
|---|---|---|
| Obstetricians (n=5) | 4 (80) | 4 – 19 |
| Midwives (n=10) | 10 (100) | <1 – 30 |
| Dietitians (n=1) | 1 (100) | 25 |
| Lactation consultants (n=2) | 2 (100) | 18 – 43 |
| Pharmacists (n=1) | 1 (100) | 10 |
Figure 2.
Themes Alongside Barriers and Enablers Mapped Onto the Capability, Opportunity, Motivation-Behavior (COM-B) Model.
Themes
Knowledge
From the psychological capability perspective, both participants and partners described personalized breastfeeding benefits. Participants spoke frequently about breastfeeding being best for their baby as a strong motivator “Because I knew that was the best for my baby. That was the best choice for baby, yeah. That’s why I never gave up” (Participant 8). Partners also described breastfeeding’s financial benefits that it would “save you a ton of money” and had family benefits “I think that. . .it’s very good for the child’s immune system and it’s very natural and in our kids were they were rarely sick. . .. I think it’s very good for the bonding process as well” (Partner 7).
Antenatal mental preparation and acknowledging breastfeeding as being difficult at times was an important enabler for all. Participants described how knowledge of what was normal for breastfeeding would have helped them feel more prepared for breastfeeding:
I wish I’d informed myself a lot more. I thought I was, but I wasn’t quite prepared because I didn’t have that background information, like from my mum or. . .you know, even just that kind of information that filters in of what’s normal and what isn’t. (Participant 6)
For partners, mental preparation to support their partner’s breastfeeding journey was described as “the baby isn’t going to come out and feed perfectly. . .. If you know that beforehand then maybe it might be easier just to stick with it” (Partner 1). Peer-shared tacit knowledge through the lived experiences of others provided participants with important emotional reassurance. In particular, social breastfeeding groups were mentioned as useful resources for this knowledge “So I didn’t get to go [to antenatal classes]. I would’ve went on to like. . .like Facebook pages. . .breastfeeding pages to kind of—because you get an idea of what to expect” (Participant 13).
Partners identified that inconsistent healthcare professional knowledge and information made them feel “like I don’t know who to believe.” This inconsistency was further identified as a barrier by HCPs:
One of us will say “you have to feed like every 3 hours,” another one will “oh you can go up to 6 hours.” It just depends on the midwife. I think we all really need to be preaching from the same book; I think that’s a massive issue. (HCP9)
The importance of consistent pre-discharge information and continued consistent advice from public health nurses and family practitioners in the community was also raised.
Latch describes how the baby fastens to the breast during breastfeeding. Some participants noted that latching was not easy and required considerable effort to address. The physicality associated with having a high BMI, notably breast size, was a barrier acknowledged by participants and a contributor to latching problems “The size of my breasts probably were hindering things a little bit” (Participant 20). Conversely, partners noted that mothers being physically well was important for breastfeeding. One stated:
I think for both of us, because she needs to be physically well to be able to feed and manage that kind of energy drain that does come along with it. . .so she needs to be physically well for that and mostly she needs to be able to. . .you know, deal with the baby and the neediness kind of part of it as well. (Partner 13)
Support
The importance of social support was well described by both HCPs and participants. They described having a supportive partner and family members with a lived experience of breastfeeding, for example, a mother or sister, as critical supports: “that’s why you need your mammy and your sisters and anyone around you that has done it. You know, experienced people that’d be able to help” (Participant 12). Unsupportive attitudes of older generations, and body image, specifically stigma associated with body image, were highlighted as barriers by participants. Partners spoke of feeling “a little bit useless” (Partner 20) but acknowledged their role in supporting their breastfeeding partner.
Participants described reduced support for breastfeeding due to omnipresent formula feeding and loss of breastfeeding culture. Participants found “everyone’s very encouraging of quitting. . .” (Participant 12) and hospitals were quick to offer formula as a solution to any feeding issue: “I think if you’re not, if you’re not supported, or if people, like, in the hospital—the one negative I’d say about the hospital is they are, well for me, I found they were quick to offer a bottle (Participant 4).
HCPs identified cultural differences in language with overseas-born women asserting that they would breastfeed, whereas Irish women would say “I’d like to breastfeed” (HCP 8).
Breastfeeding support services and group experiences were variable, but participants identified them as important:
The lactation consultant—definitely a moment for me that just really. . . just gave me the fire in some ways. . . as soon as she kind of said to me you’re doing okay and she was—that moment was a fantastic moment to be honest. (Participant 4)
Partners reinforced these benefits “like breastfeeding Facebook groups and that and she’s found them great you know there’s a lot of people there going through the same kind of stuff and there’s a lot of good information” (Partner 7). HCPs highlighted the need for “more awareness maybe that they [women with high BMIs] might be a particularly high-risk group that should be given extra support” (HCP 13).
Participants described negative or positive breastfeeding environments and how it was the people within the setting that determined its positivity or negativity, rather than the physical environment. The workplace was commonly identified as a non-supportive environment, with one participant stating:
I work in a very. . .male dominated environment and, eh, it was kind of seen to “Oh breastfeeding oh” and it was kind of like “Yeah sure, you’re breastfeeding twins—like who does that?!” kind of, and I had a very, very negative experience in terms of the workplace. (Participant 15)
Participants reported hospital services as lacking, inaccessible, or under-resourced and seeking private IBCLC support. While critical, it came at a financial and emotional cost “[I] had to go looking for it [breastfeeding help] at all times, I had to beg in the hospital to get them to send up a lactation consultant” (Participant 15). HCPs felt that providing sufficient lactation support would reduce the practice of infant formula top-ups and improve breastfeeding outcomes:
I think that the postnatal wards are understaffed and that the midwives can’t give the women the attention that they need especially with their first-time babies and a lot of babies end up needing top ups and. . .like, I really think with proper support that that shouldn’t be necessary (HCP1).
Participants, partners, and HCPs described aids being a facilitator particularly in the earlier part of breastfeeding. Participants mentioned “The lanolin, I swear by it. You have to have that, yeah, [in the] early days” (Participant 2); while partners referred to “the chair and the pillow kind of helped a lot just for getting the right position and comfort and they were probably the two main things” (Partner 5). HCPs spoke specifically of breastfeeding pillows being useful for positioning: “I do find pillows are really, really necessary for larger women to give them support and make sure that the baby is up and nice and high and everything. . .” (HCP9).
Self-Efficacy
The critical nature of self-efficacy was expressed by all groups. Participants stated:
I think when you set your mind to breastfeed and you really want to do it, [it] doesn’t matter. You know if you are overweight, if you are depressed, or you know like—I think it’s personal. For example, I had postnatal depression, you know, I am overweight and I still breastfeeding. (Participant 8)
HCPs described the Irish culture as a barrier to self-efficacy and the need to be proactive and build this key attribute:
I think that if we were more proactive in some areas that it might be helpful for woman, especially in relation to woman with a high BMI. I think what we come across a lot of times is that there are body image self-efficacy issues, that woman have [a] huge amount of misconceptions about their own ability to breastfeed. (HCP16)
Partners reiterated how a lack of support made it easy for women to give up on breastfeeding and how it was a woman’s own determination that seemed to enable her to continue:
I suppose she felt nearly that she was failing, in a way, because she couldn’t do it, but she was—she was just so determined, but I suppose if the supports were more, well I know, I think more women would continue, if you know what I mean. Because I think it would’ve been very easy for [woman’s name] to give up, but she was—she was just so determined in herself to do it. (Partner 21)
HCPs spoke of the women who sought their support as demonstrating greater self-efficacy, whereas less prepared women appeared to give up quicker.
Intervention Mapping
The COM-B model barrier and enabler analysis findings were subsequently mapped onto a multifactorial breastfeeding intervention (Table 4) divided across the antenatal to postpartum periods to support successful breastfeeding in women with high BMIs.
Table 4.
Multifactorial Intervention Design for Supporting Breastfeeding in Women With High Body Mass Indices.
| Themes | Intervention Component | Timing | ||
|---|---|---|---|---|
| Antenatal (Hospital) | Immediate postpartum (Hospital) | Medium term postpartum (Community/peer-to- peer support) | ||
| Knowledge | Education | Education/training for hospital staff to increase BF knowledge, focus on being aware that women with high BMIs require extra support and possibly BF aids. Interactive class/classes covering benefits of BF, BF technique, common issues. Materials including representative images of BF women with high BMIs. Standardized materials developed with ensure fidelity of education delivery. | Consultation with IBCLC/specialist midwife | Lactation support offered by phone or drop-in clinic |
| Resources | Provide local links to resources such as websites, BF groups within handout, places to breastfeed outside the home, and suggestions for suitable BF clothes. | Reinforce local links to support services and provide information on BF aids. | Access to IBCLC/BF counsellors/public health nurses with lactation training Support networks including La Leche League, Cuidu, etc. |
|
| Support | Build social support | Support person attending antenatal class/classes | Drop-in lactation clinic and support network referral | |
| Workforce planning | Additional time allocation for engaging support person | Increased lactation support services | Additional lactation support services | |
| Self – Efficacy | Problem solving | Common issues presented with solutions in words of participants | Consultation with IBCLC/specialist midwife | Support networks developed |
Note. BF = breastfeeding; BMI = Body Mass Index.
Discussion
Our findings build upon previous qualitative explorations and demonstrate considerable overlap in perceptions of women, partners, and HCPs on barriers and facilitators to successful breastfeeding. All stakeholders emphasized the potential for increased provision of health services and education as a way of changing the knowledge, self-efficacy, and social support given to women with high BMIs for successful breastfeeding. Stakeholders emphasized the need to normalize breastfeeding as optimal infant feeding and ensure all maternity service systems support this as routine care. This was key in, their eyes, to maximizing the effectiveness of any improved services. The interaction between themes mirrored the COM-B model’s hypothesized relationships between components (behavior can change capability, motivation, and opportunity as can motivation be influenced by opportunity and capability). We saw aspects of psychological capability (HCP knowledge inconsistent) and physical capability (latch problems) influencing breastfeeding participants’ reflexive motivation (self-efficacy). Equally, engaging in the behavior of learning to breastfeed altered the participant’s psychological and physical capability, consolidated her reflexive and automatic motivations, and increased the positive social opportunities to engage further in that behavior. These additional interactions highlight the complexity of breastfeeding as a behavior and the need for multilevel and multifactorial intervention to create meaningful change.
Systematic reviews have highlighted that the barriers and enablers to breastfeeding for women with high BMIs were similar to other women, but that the extent of the experience may be more problematic for women with higher BMIs because of their weight status (Chang et al., 2020; Lyons, Currie & Smith, 2019; Lyons, Currie & Peters, 2019). The physicality of breastfeeding and the stigma and social bias associated with high BMIs were pronounced findings in our results, which aligns with previous work (Incollingo Rodriguez et al., 2020; Lyons, Currie & Smith, 2019). Our findings also demonstrated that, when participants with high BMIs were provided with the right support, in a way that is acceptable to them, they breastfeed for extended periods. However, it is important to highlight that it remains to be seen if providing a tailored intervention using the findings of this study and testing it via a randomized clinical trial will deliver increased extended breastfeeding rates in this population. Antenatal and postnatal education needs to be inclusive of this growing population and should provide resources that help address social bias and stigma (Incollingo Rodriguez et al., 2020). A Cochrane review on interventions for supporting breastfeeding in women with overweight or obesity (Fair et al., 2019) highlights social support and provision of education and breastfeeding aids, for example breast pumps, as important. Our positive deviance approach showed that there is commonality with other breastfeeding intervention designs that should be exploited to ensure any intervention developed fits within routine antenatal services but are adaptable to the needs of at-risk populations.
To improve breastfeeding, we need to focus on targeting theoretically sound and evidence-based factors using best-practice complex intervention design. The evidence supports the capability of women to engage in breastfeeding being positively underpinned by knowledge, women in particular recognizing the health benefits for optimal child nutrition and health outcomes (Lyons, Currie & Peters, 2019). The importance of partners in supporting women to engage in breastfeeding is also acknowledged in previous work. Mothers who felt they had positive support from their partners via active involvement or verbal encouragement were more confident and able to breastfeed than those whose partners were ambivalent, or those who had negative partner support (Bhario & Elliott, 2018). Encouragement from partners also resulted in increased breastfeeding duration and exclusivity, as did assisting with breastfeeding difficulties and helping with household duties (Davidson & Ollerton, 2020; Ogbo et al., 2020). Previous researchers have highlighted that partners’ understand the benefits of breastfeeding and have empathy for their breastfeeding partner, but at times report feeling left out of the infant-feeding process (Crippa et al., 2021). Our findings confirm partners’ important role in supporting their breastfeeding partner’s capability by having access to knowledge in an inclusive manner that subsequently enables them to feel prepared to help with successful breastfeeding. The inclusion of a support partner in future antenatal breastfeeding interventions is essential to the building of social support and increasing a woman’s motivation to engage in the behavior. Another important ingredient in antenatal breastfeeding interventions is resourcing HCP services so that specific and tailored support can be provided (Balogun et al., 2016; Lyons, Currie & Peters, 2019). The failure to build additional resources into an intervention will result in diminished effects, a lack of sustainability in the intervention over time, and potentially a widening of the gap in breastfeeding rates between women with higher and lower BMIs.
Limitations
The study sampling frame is a potential limitation—namely, the partners were not matched to the participants interviewed and they were not required to state if their own partner had a high BMI. This limited our ability to associate how the relationship between the partner and breastfeeding participant’s experience interact. Participant response bias and researcher bias are two additional limitations. We did not formally record the participant ethnicity, which limits our ability to explore the influence of specific ethnic factors on breastfeeding. Another limitation was the interviews occurring at a single time point. Longitudinal data would have the potential to provide greater understanding of behavioral changes that may occur over time. A final limitation was that the participants and partners may or may not have experienced lactation support services provided by the participating HCPs or the maternity service that the HCPs were employed by. While indicative of their lived experience, their views may or may not represent the experience that the participant or her partner would experience if they were to attend that maternity hospital.
Conclusions
The positive deviance approach enabled the broader understanding of successful breastfeeding for women with high BMIs from a variety of stakeholder perspectives. Future research needs to test a complex breastfeeding intervention for this population using a randomized clinical trial design, after the behavior change techniques required to deliver the intervention with fidelity have been mapped.
Supplemental Material
Supplemental material, sj-docx-1-jhl-10.1177_08903344221102839 for Exploring Successful Breastfeeding Behaviors Among Women Who Have High Body Mass Indices by Sharleen L. O’Reilly, Marie C. Conway, Eileen C. O’Brien, Eva Molloy, Hannah Walker, Eimear O’Carroll and Fionnuala M. McAuliffe in Journal of Human Lactation
Acknowledgments
We are grateful for the time and knowledge supplied by participants. We would like to thank Joanne Courtney for the conduct of the interviews with women and partners. We would also like to thank Anna Gouldson, David Byrne, Sophie Callanan, and Ellen O’Grady for transcribing the interviews.
Footnotes
Author contribution(s): Sharleen O’Reilly: Conceptualization; Data curation; Formal analysis; Methodology; Supervision; Writing – original draft; Writing – review; editing
Marie Conway: Formal analysis; Writing – review; editing
Eileen O’Brien: Data curation; Methodology; Writing – review; editing
Eva Molloy: Investigation; Writing – review; editing
Hannah Walker: Investigation; Writing – review; editing
Eimear O’Carroll: Investigation; Writing – review; editing
Fionnuala McAuliffe: Conceptualization; Resources; Writing – review; editing
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Ethical Statement: Ethical approval was granted by the National Maternity Hospital Ethics Committee (EC.19.2017) on November 9, 2017.
ORCID iDs: Sharleen L. O’Reilly  https://orcid.org/0000-0003-3547-6634
https://orcid.org/0000-0003-3547-6634
Fionnuala M. McAuliffe  https://orcid.org/0000-0002-3477-6494
https://orcid.org/0000-0002-3477-6494
Supplementary Material: Supplementary Material may be found in the “Supplemental material” tab in the online version of this article.
References
- Balogun O. O., O’Sullivan E. J., McFadden A., Ota E., Gavine A., Garner C. D., Renfrew M. J., Macgillivray S. (2016). Interventions for promoting the initiation of breastfeeding. Cochrane Database of Systematic Reviews. 10.1002/14651858.CD001688.pub3 [DOI] [PMC free article] [PubMed]
- Bhairo R. L., Elliott H. (2018). Encouraging breastfeeding: The role of fathers. Journal of Health Visiting, 6(6), 290–301. 10.12968/johv.2018.6.6.290 [DOI] [Google Scholar]
- Bish M. R., Faulks F., Amir L. H., Huxley R. R., McIntyre H. D., James R., Mnatzaganian G. (2021). Relationship between obesity and lower rates of breast feeding initiation in regional Victoria, Australia: An 8-year retrospective panel study. BMJ Open, 11(2), Article e044884. 10.1136/bmjopen-2020-044884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boudet-Berquier J., Salanave B., Desenclos J. C., Castetbon K. (2018). Association between maternal prepregnancy obesity and breastfeeding duration: Data from a nationwide prospective birth cohort. Maternal and Child Nutrition, 14, Article e12507. 10.1111/mcn.12507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley E. H., Curry L. A., Ramanadhan S., Rowe L., Nembhard I. M., Krumholz H. M. (2009). Research in action: Using positive deviance to improve quality of health care. Implementation Science, 4, Article 25. 10.1186/1748-5908-4-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun V., Clarke V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101. 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- Braun V., Clarke V. (2019). Reflecting on reflexive thematic analysis. Qualitative Research in Sport, Exercise and Health, 11(4), 589–597. 10.1080/2159676X.2019.1628806 [DOI] [Google Scholar]
- Chang Y., Glaria A. A., Davie P., Beake S., Bick D. (2020). Breastfeeding experiences and support for women who are overweight or obese: A mixed-methods systematic review. Maternal and Child Nutrition, 16, Article e12865. 10.1111/mcn.12865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen C., Xu X., Yan Y. (2018). Estimated global overweight and obesity burden in pregnant women based on panel data model. PLoS One, 13(8), Article e0202183. 10.1371/journal.pone.0202183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen C. N., Yu H. C., Chou A. K. (2020). Association between maternal pre-pregnancy Body Mass Index and breastfeeding duration in Taiwan: A population-based cohort study. Nutrients, 12(8), Article 2361. 10.3390/nu12082361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crippa B. L., Consales A., Morniroli D., Lunetto F., Bettinelli M. E., Sannino P., Rampini S., Zanotta L., Marchisio P., Plevani L., Giannì M. L., Mosca F., Colombo L. (2021). From dyad to triad: A survey on fathers’ knowledge and attitudes toward breastfeeding. European Journal of Pediatrics, 180(9), 2861–2869. 10.1007/s00431-021-04034-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalrymple K. V., Uwhubetine O., Flynn A. C., Pasupathy D., Briley A. L., Relph S. A., Seed P. T., O’Keeffe M., Poston L. (2021). Modifiable determinants of postpartum weight loss in women with obesity: A secondary analysis of the UPBEAT Trial. Nutrients, 13(6), Article 1979. 10.3390/nu13061979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson E. L., Ollerton R. L. (2020). Partner behaviours improving breastfeeding outcomes: An integrative review. Women and Birth, 33(1), e15–e23. 10.1016/j.wombi.2019.05.010 [DOI] [PubMed] [Google Scholar]
- Fair F., Ford G., Soltani H. (2019). Interventions for supporting the initiation and continuation of breastfeeding among women who are overweight or obese. Cochrane Database of Systematic Reviews. 10.1002/14651858.CD012099.pub2 [DOI] [PMC free article] [PubMed]
- Garner C. D., McKenzie S. A., Devine C. M., Thornburg L. L., Rasmussen K. M. (2017). Obese women experience multiple challenges with breastfeeding that are either unique or exacerbated by their obesity: Discoveries from a longitudinal, qualitative study. Maternal and Child Nutrition, 13, Article e12344. 10.1111/mcn.12344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Service Executive. (2021). Irish Maternity Indicator System: National Report 2020. https://www.hse.ie/eng/about/who/acute-hospitals-division/woman-infants/national-reports-on-womens-health/irish-maternity-indicator-system-national-report-2020.pdf
- Incollingo Rodriguez A. C., Smieszek S. M., Nippert K. E., Tomiyama A. J. (2020). Pregnant and postpartum women’s experiences of weight stigma in healthcare. BMC Pregnancy and Childbirth, 20, Article 499. 10.1186/s12884-020-03202-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joham A. E., Nanayakkara N., Ranasinha S., Zoungas S., Boyle J., Harrison C. L., Forder P., Loxton D., Vanky E., Teede H. J. (2016). Obesity, polycystic ovary syndrome and breastfeeding: An observational study. Acta Obstetricia et Gynecologica Scandinavica, 95(4), 458–466. 10.1111/aogs.12850 [DOI] [PubMed] [Google Scholar]
- Kair L. R., Colaizy T. T. (2016). Obese mothers have lower odds of experiencing pro-breastfeeding hospital practices than mothers of normal weight: CDC Pregnancy Risk Assessment Monitoring System (PRAMS), 2004–2008. Maternal and Child Health Journal, 20(3), 593–601. 10.1007/s10995-015-1858-z [DOI] [PubMed] [Google Scholar]
- Lyons S., Currie S., Peters S., Lavender T., Smith D. M. (2019). The perceptions and experiences of women with a body mass index ≥ 30 kg m2 who breastfeed: A meta-synthesis. Maternal and Child Nutrition, 15, Article e12813. 10.1111/mcn.12813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyons S., Currie S., Smith D. M. (2019). Learning from women with a body mass index (BMI) ≥ 30 kg/m2 who have breastfed and/or are breastfeeding: a qualitative interview study. Maternal and Child Health Journal, 23(5), 648–656. 10.1007/s10995-018-2679-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lub V. (2015). Validity in qualitative evaluation: linking purposes, paradigms, and perspectives. International Journal of Qualitative Methods, 14(5), Article 1609406915621406. 10.1177/1609406915621406 [DOI] [Google Scholar]
- Malterud K., Siersma V.D., Guassora A.D. (2016). Sample size in qualitative interview studies guided by information power. Qualitative Health Research, 26, 1753–1760. https://doi.org/10.1177%2F1049732315617444 [DOI] [PubMed] [Google Scholar]
- Mangel L., Mimouni F. B., Mandel D., Mordechaev N., Marom R. (2019). Breastfeeding difficulties, breastfeeding duration, maternal Body Mass Index, and breast anatomy: Are they related? Breastfeeding Medicine, 14(5), 342–346. 10.1089/bfm.2018.0262 [DOI] [PubMed] [Google Scholar]
- Marsh D. R., Schroeder D. G., Dearden K. A., Sternin J., Sternin M. (2004). The power of positive deviance. British Medical Journal, 329(7475), 1177–1179. 10.1136/bmj.329.7475.1177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonagh L. K., Saunders J. M., Cassell J., Curtis T., Bastaki H., Hartney T., Rait G. (2018). Application of the COM-B model to barriers and facilitators to chlamydia testing in general practice for young people and primary care practitioners: A systematic review. Implementation Science, 13, Article 130. 10.1186/s13012-018-0821-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michie S., van Stralen M. M., West R. (2011). The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implementation Science, 6, Article 42. 10.1186/1748-5908-6-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCD Risk Factor Collaboration. (2017). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet, 390(10113), 2627–2642. 10.1016/S0140-6736(17)32129-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogbo F., Akombi B., Ahmed K., Rwabilimbo A., Ogbo A., Uwaibi N., Ezeh O., Agho K. (2020). Breastfeeding in the community—How can partners/fathers help? A systematic review. International Journal of Environmental Research and Public Health, 17(2), Article 413. 10.3390/ijerph17020413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Purdy J., McAvoy H., Cotter N. (2017). Breastfeeding on the island of Ireland. Institute of Public Health in Ireland. https://www.hse.ie/eng/about/who/healthwellbeing/our-priority-programmes/child-health-and-wellbeing/breastfeeding-healthy-childhood-programme/research-and-reports-breastfeeding/breastfeeding-on-the-island-of-ireland-report.pdf [Google Scholar]
- Ramji N., Challa S., Murphy P. A., Quinlan J., Crane J. (2018). A comparison of breastfeeding rates by obesity class. Journal of Maternal-Fetal and Neonatal Medicine, 31(22), 3021–3026. 10.1080/14767058.2017.1362552 [DOI] [PubMed] [Google Scholar]
- Reynolds C. M. E., Egan B., McMahon L., O’Malley E. G., Sheehan S. R., Turner M. J. (2019). Maternal obesity trends in a large Irish university hospital. European Journal of Obstetrics and Gynecology and Reproductive Biology, 238, 95–99. 10.1016/j.ejogrb.2019.05.003 [DOI] [PubMed] [Google Scholar]
- Rose A. J., McCullough M. B. (2017). A practical guide to using the positive deviance method in health services research. Health Services Research, 52(3), 1207–1222. 10.1111/1475-6773.12524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skivington K., Matthews L., Simpson S. A., Craig P., Baird J., Blazeby J. M., Boyd K. A., Craig N., French D. P., McIntosh E., Petticrew M., Rycroft-Malone J., White M., Moore L. (2021). A new framework for developing and evaluating complex interventions: Update of Medical Research Council guidance. British Medical Journal, 374, Article n2061. 10.1136/bmj.n2061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sirkka O., Hof M. H., Vrijkotte T., Abrahamse-Berkeveld M., Halberstadt J., Seidell J. C., Olthof M. R. (2021). Feeding patterns and BMI trajectories during infancy: A multi-ethnic, prospective birth cohort. BMC Pediatrics, 21(1), Article 34. 10.1186/s12887-020-02456-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-jhl-10.1177_08903344221102839 for Exploring Successful Breastfeeding Behaviors Among Women Who Have High Body Mass Indices by Sharleen L. O’Reilly, Marie C. Conway, Eileen C. O’Brien, Eva Molloy, Hannah Walker, Eimear O’Carroll and Fionnuala M. McAuliffe in Journal of Human Lactation