Abstract
Sedentary lifestyles and evolving work environments have created challenges for global health and cause huge burdens on healthcare and fitness systems. Physical immobility and functional losses due to aging are two main reasons for noncommunicable disease mortality. Smart electronic textiles (e-textiles) have attracted considerable attention because of their potential uses in health monitoring, rehabilitation, and training assessment applications. Interactive textiles integrated with electronic devices and algorithms can be used to gather, process, and digitize data on human body motion in real time for purposes such as electrotherapy, improving blood circulation, and promoting wound healing. This review summarizes research advances on e-textiles designed for wearable healthcare and fitness systems. The significance of e-textiles, key applications, and future demand expectations are addressed in this review. Various health conditions and fitness problems and possible solutions involving the use of multifunctional interactive garments are discussed. A brief discussion of essential materials and basic procedures used to fabricate wearable e-textiles are included. Finally, the current challenges, possible solutions, opportunities, and future perspectives in the area of smart textiles are discussed.
Keywords: Wearable electronics, Smart textiles, e-textiles, Light therapy, Digital health
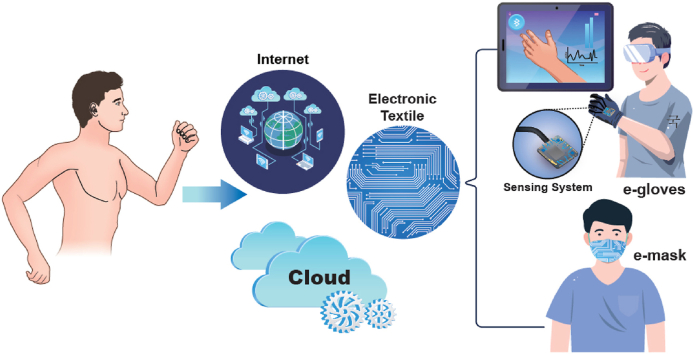
Graphical abstract
1. Introduction
1.1. General overview
A current trend is the development of high-mass-consumption printable electronic devices that are flexible, wearable, and integrated into fabrics in the form of smart apparel. E-textiles are being recognized for their usefulness in monitoring and diagnosis of daily activities and health conditions and for the treatment of many health conditions, with the help of digital electronics and computer algorithms [[1], [2], [3], [4], [5], [6], [7], [8]]. COVID-19 has led to a spike in the development of wearable systems with sensors for early detection of signs of SARS COV-2 [[9], [10], [11]]. For example, stretchable strain sensors printed on clothes can monitor the expansion of the chest and hence deviations in breathing patterns. Clothes with embedded actuators can be used as exoskeletons and rehabilitation devices for ailments such as stiff necks and joints. The engineering of flexible, stretchable devices and circuits is the key component of electronically functional wearable textiles capable of sensing, heating, illuminating, and transmitting data [12,13]. The integration of electronics and communication into shirts and trousers, blankets and bed sheets, bandages and head caps, etc., facilitates functions for making human lives easier [14].
The integration of electronics into conventional fabrics is called e-textiles, which also named as smart or intelligent garments [1,[15], [16], [17]]. Smart e-textiles can sense, react, and interact with a range of ambient stimuli conditions and respond to perform a task in a manual pre-programmed processing manner [18]. E-textiles require electrical components to function with external stimuli such as chemical, mechanical, thermal, electromagnetic field, radiant, moisture, pH etc [18,19]. The different characteristics of intelligent garments differs according to the integrated electronic components or technology platform. The integration of electronic components creates a new functionality in traditional clothes that enhances their functions and provide added value for advanced state-of-the-art applications. The working mechanism or electronic feedback process of e-textiles is based on eliciting or stimulation is received by the senses or any physical response/action from any object or environment in form of touch, heat, sound and light. Then smart e-textiles detect the stimulation and process the information in form quantitative data as a resulting function to deliver response or action [20,21]. Consequently, e-textiles can sense changes that take place due to human body movements, gather data from the wearer, and transmit the data to a computer or smartphone, which can give appropriate feedback. Because e-textiles integrate electronics into textiles, it is anticipated that e-textile technology will continue to advance to include the major product types and a wide range of application areas and markets.
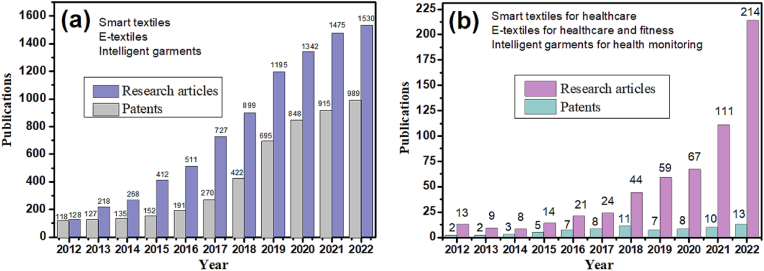
The immense growth of the e-textiles’ market and the number of scientific papers published in the last 10 years in this field have increased. Fig. 1 shows the number of papers published over the past 10 years in e-textiles or smart textiles. The data was taken from the Lens Scholarly Search (www.lens.org) using keywords, smart textiles or smart fabrics, e-textiles and intelligent garments. According to the Lens search data, the number of patents and research articles on smart e-textiles have increased exponentially since 2017 (Fig. 1(a)). Thus, over the past few years, smart e-textiles have gained huge attention from research investigators, as shown by the expanding of the application areas and the rise in the number of publications. Fig. 1(b) shows the total number of publications and patents on smart textiles, e-textiles and intelligent garments specifically designed for healthcare, fitness and health monitoring applications over the last 10 years. The data indicate only a limited research papers and patents on e-textiles have been published however number of publications on the applications to health and fitness are increasing with time. The e-textiles in medical and sports sectors will gain more considerable attention in coming years.
Fig. 1.
(a) Total research papers and patents yearly publications in past 10 years in area of e-textiles and smart textiles or intelligent garments. (b) Total research articles and patents published in the area of e-textiles, smart textiles and intelligent garments for healthcare and fitness applications. Data Source: Lens Scholarly Search, LENS.ORG.
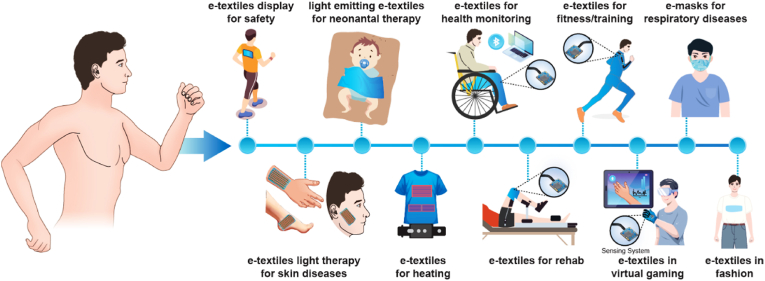
In the last decade, e-textiles have attracted significant attention because of successful applications in several fields, including medicine [1,5,22], sports [23,24], rehabilitation and personalized healthcare [18,25,26], safety [[27], [28], [29]], and virtual reality [30,31]. Fig. 2 shows a pathway of e-textiles’ applications in various fields for the prevention of respiratory illnesses, joint injury, skin diseases, neonatal jaundice, road safety, training, and fashion. Worldwide, the elderly population and the number of people with disabilities are increasing every day. Thus, wearable e-textile prototypes are becoming increasingly important for health monitoring and treatment [25,32]. For example, e-textiles integrated with interactive sensors can send a user's real-time monitoring data to a hospital, thereby minimizing the dependence on bulky and expensive monitoring tools and reducing hospital visit frequency. Fitness training is another large potential market for the use of e-textiles. In nearly every sport, athletes can benefit from e-textiles as an advanced, affordable, and compelling new wearable technology to assess and improve performance. Advances in wearable smart garments are not limited to healthcare and fitness but are also driving the technology into soft robotics, virtual reality, and the internet-of-smart-textiles with the rise of the Internet of Things (IoT) [33]. Within the next decade, in the age of IoT, it is likely that e-textile technology will transform human lives, along with artificial intelligence, human–machine interfaces, and cloud technology [5,34]. It is anticipated that the e-textile prototypes will grow rapidly into commercial products and increase their market size, especially in the healthcare and sports sectors [35,36]. According to a report published by IDTechEx, the market for e-textiles has been growing rapidly and is forecasted to grow to $5 billion by 2027 [37]. The market for wearable e-textiles is expected to be growing at a rate of more than $1.3 billion per year by 2031 [38].
Fig. 2.
Schematic illustration of a pathway of e-textile applications in different areas.
Wearable e-textiles are currently facing numerous challenges because they are still in an early phase of development [39,40]. As most electronic devices are delicate and fragile, they have limited washability and hence a short life. Reliability and washability are major hurdles currently facing the e-textile industry. In addition, primarily off-the-shelf sensors and electronics are currently used with wearables [41]. Another issue is poor adhesion of devices, which fall off easily under active conditions and are obstructive [42]. Despite great progress, there remain some limitations in applications to health monitoring-particularly because the benefits of e-textiles may come at the cost of user comfort. Seamless integration of functionalities with garments that can withstand high levels of deformation/deflection is needed. Deformation/deflection properties typically depend on adhesion, which has considerable operational limitations (<10% strain) due to poor embedding of sensors or gluing of components directly onto textiles [43,44]. Complicated wiring, external electric circuits, and reliance on external power sources are other limiting factors that need reliable solutions [45]. For now, research in the area of smart textiles is advancing as it has the potential to achieve goals such as conformability, low cost, low weight, and comfort in self-management [46,47]. The miniaturization of functional materials has led to advances in fabrication techniques, such as the direct printing of devices and electronics onto clothes [48,49]. This can bring the seamless integration of devices and electronics into clothing a step closer.
Several review articles have been published in area of smart or e-textiles developed for different applications [1,5,18,25,50,51]. Wang et al. discussed a textile-based strain sensors for human motion detection [52]. Most recently, Tat et al. published a perspective which describes the smart textiles as functional wearable systems for healthcare and sustainability [53]. Additional critical reviews have been reported on self-powered energy harvesting and sensing e-textiles from Professor Wang's research group [47,[54], [55], [56]]. In area of smart wearable bioelectronics, Wu et al. published two reviews on advanced electrospun nanofibers/yarns-based textiles for biomedical and spinal cord injury regeneration applications [57,58]. Most of the review article discussed the smart e-textiles applications for diagnosis, monitoring and textile devices for disease prevention and phototherapy. In last few years, a lot of research papers has been published on smart e-textiles or intelligent apparels combined with more advanced technologies interface as the gateway for real-time monitoring, collect and processing the information for self-health and fitness management. Thus, an additional comprehensive review on e-textiles for personalized healthcare and fitness assessments could be very helpful for people actively working in this filed.
1.2. The vision of this review
The primary focus of this review article is on smart e-textiles as a wearable technology specifically designed for health monitoring, diagnosis, and fitness assessment. This review article is very specific which provides a broad analysis to the researchers in area of e-textiles as a solution to medical and sports sectors. It is expected that in future, smart apparels will promote the digital health and IoT with huge market potential. This review paper is divided into several sections that cover recently published important research in the field of wearable e-textiles consisting of discrete devices and electronics. We briefly discuss historical developments, potential applications, and future market growth for smart apparel. In the next section, we highlight the necessary materials and fabrication methods for sensors and devices integrated into textiles for use in the medical and fitness sectors. This is followed by descriptions of different health concerns and fitness problems and their possible solutions using interactive smart textiles. We then summarize the current challenges associated with the materials and techniques used in the fabrication of e-textiles. Finally, we present conclusions regarding the prospects for smart e-textiles, emerging solutions, and products, along with future research directions.
2. Historical developments and current progress in e-textiles
Although innovations in textiles began with the advent of human civilization, which spans thousands of years, a revolution started in the 16th century with key inventions [59,60]. The focus was initially on enhancing the artistic and stylistic aspects of textiles but later shifted to improving the functionality of garments for various applications. The first example of an electronic textile dates back to 1883 with the debut of illuminated headbands in the ballet La Farandole Inn at the Conservatoire in Paris [61]. The performers wore electric headbands with lights on their heads, and the lights were illuminated when they touched buttons on their belts. At the end of the 20th century, developments in material chemistry and electronics widened the potential for integrating electronics into textiles. Another important development took place in the mid-1990s when a team of researchers at the Massachusetts Institute of Technology (MIT) led by Steve Mann began to develop a wearable computer, which consisted of traditional computer hardware attached to textiles and carried on the human body [62]. Textile technology has also been highly impacted by the development of nanometer-scale systems. In the last two decades, advances in nanotechnology and fabrication methods have had huge impacts and brought about tremendous changes in large-area flexible and stretchable electronics. Nanotechnology has contributed significantly to major advances in smart textiles with the incorporation of additive features to increase their commercial value [63]. At present, classical electronic components such as conducting yarns and wires, integrated circuits, sensors, light-emitting diodes (LEDs), and power sources embedded into garments are in high demand for wellness and fitness. In the past two decades, a considerable amount of research has resulted in vast numbers of patents and publications on the integration of electronic components and devices with textiles.
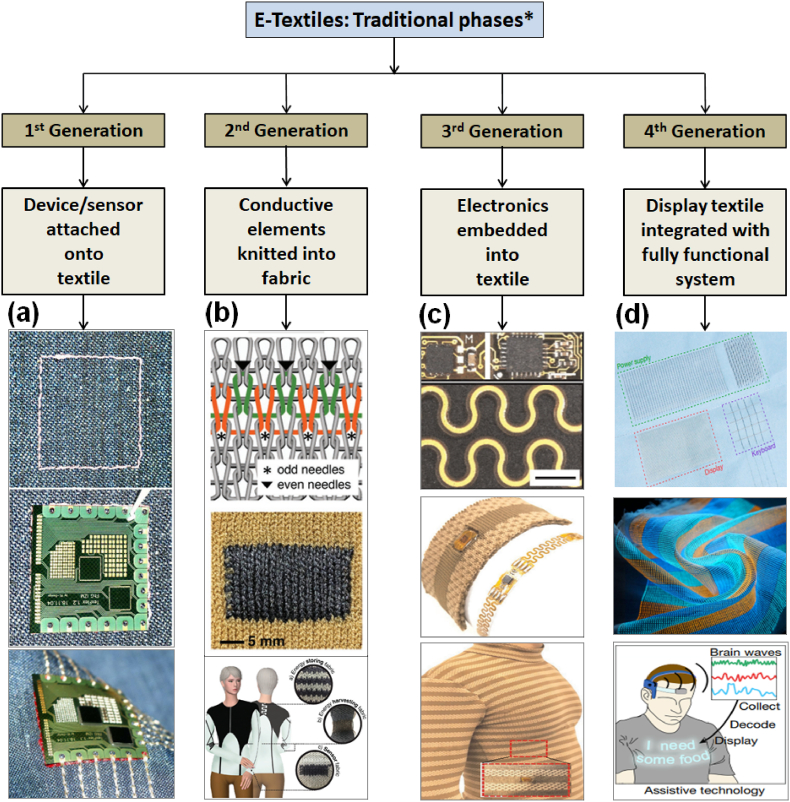
Since the beginning of the e-textile era, various ways to integrate electronics into textiles have been demonstrated. Wu et al. categorized developments in e-textiles into various phases referred to as the first to third generations of this technology [39].
First-generation e-textiles involve a hard component, such as an antenna or an electronic device, stitched or attached to the surface of a garment as shown in Fig. 3 (a). In first-generation types of e-textiles, a soft electronic module is embroidered on a piece of textile using conductive yarn [64]. In this way, an electrical and mechanical connection is made using the basic yarn embroidery process. This approach has been adopted and continues to be developed by some well-known sportswear brands [65]. However, as might be expected, first-generation e-textile products tend to be bulkier and more rigid than is practical for everyday use.
Fig. 3.
Summarize the development of the e-textiles from phase-one to the current fourth-generation phase. (a) Embroider mark (top); placing of the flexible circuitry device along with the marker, and then embroidered through the contact pads sequentially. Images are reproduced with permission [64], Copyright 2005, IEEE Publishing Group. (b) Interlocked knitted fabric using different stitch patterns (top) resulted in dense fabric (middle) and the concept illustration of a garment integrated with sensing device; insets show actual device prototypes. Images are reproduced with permission [66], Copyright 2019, Wiley-VCH Publishing Group. (c) Illustration of embedding flexible-stretchable electronic strips (top) microscopic image and woven electronic strip in a knit textile (middle) and showing its conformability to the wearer. Images are reproduced with permission [41], Copyright 2020, Springer Nature. (d) Real image of a fully integrated textile system comprising of display, keyboard and power supply (top), photograph of multicolor display textile (middle) and concept design displaying brain waves can be decoded into messages that is displaying on a shirt made from a fully functional display textile. Images are reproduced with permission [71] Copyright 2021, Springer Nature. ∗ Information deduced from published research papers/publicly available information.
In second-generation wearables, conductive yarns are knitted or woven into the textile structure to make it electronically functional. Conductive yarns are intertwined into various stitch patterns using industrial-scale knitting machines to fabricate fully functional wearable electronic textiles as depicted in Fig. 3(b) [66]. The process is very simple. This approach is most frequently used to develop electronically functional apparel without any noticeable flaws or discomfort for the wearer. Examples of second-generation smart textiles include wearable cloth sensors fabricated by knitting or weaving conductive yarns [39] and LEDs interwoven with electrically conductive yarns into the textile pattern [67]. Second-generation e-textiles are usually soft but are limited in terms of comfort and adaptability. Athos, a sportswear brand and important player in the market, has patented the world's first intelligent clothing to measure the strength of a wearer's muscles based on the principle of electromyography (EMG). Firm, CuteCircuit, has been producing electronic clothes of second and even next-generation electronic garments that can play music, display messages and tweets [68]. Some retail brands, such as Amazon and Flipkart, are selling second-generation sensing and display clothes.
Third-generation intelligent textiles have sensors and electronics embedded into garments integrating the technology and the fabrics together (Fig. 3(c)) [41]. Third-generation e-textiles are more suitable than the e-textiles of the first two generations for producing durable, comfortable, and reliable electronic systems with better functionality. Firms such as Samsung, Alphabet, Ralph Lauren, AdvanPro, Tamicare, and BeBop Sensors have developed third-generation products and are growing rapidly in this direction [69].
This review also describes a future generation or fourth generation intelligent e-textiles that may represent the future of e-textile products, although they are currently in fabrication at lab scale and exist only as concept designs and/or prototypes. The fourth generation is the state-of-art technology that will be able to fully integrate electronic functionality into textiles seamlessly. Fourth-generation products should conform to the essential e-textile requirements of softness, comfort, flexibility, washability, and durability. For example, a light-emitting device could be manufactured as a textile fiber that illuminates without an external power source [70,71]. Fig. 3(d) shows next generation fully integrated intelligent textile system comprising of display, keyboard and power supply as well photograph of display textile and concept design demonstrating brain waves can be decoded into messages that is exhibiting on a shirt [71]. The seamless light-emitting or interactive textile could transform the concept of wearable e-textile display directly onto human skin, leading to the modernization of fashion, visual retailing, and individual safety. Most of these wearable textiles will connect to a user's smartphone via a wireless communication system such as Bluetooth or Wi-Fi and transmit data to boost big data cloud computing [1,33,72]. Fundamentally, e-textile technology is in a transformation period in which the focus is shifting from embedding or embroidering approaches to more user-friendly e-textiles with the technology manufactured into the garment itself. Developing the fourth generation of e-textiles will place substantial demands on the innovation capability of the clothing industry-demands that also offer huge potential for growth in new business sectors. Wearable textile technology is moving forward, and in the next decade, it will increasingly be connected to the IoT, along with artificial intelligence, human–machine interfaces, and cloud technology.
3. Prospective application areas of smart e-textiles
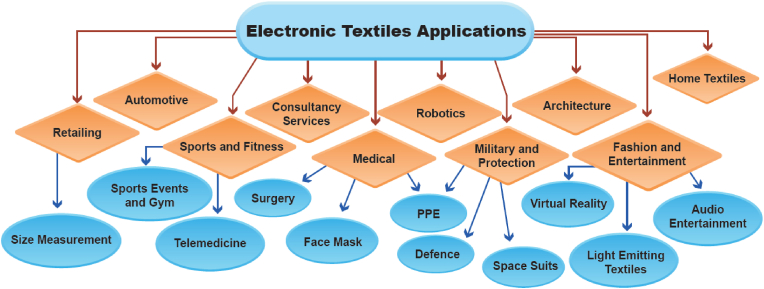
E-textiles with intelligent designs and enhanced capabilities offer potential solutions to several medical and fitness problems. Today, e-textiles have numerous applications in the clothing industry. E-textiles are indeed an asset because technologically advanced textiles are more adaptable and have the potential to be used not only in the medical and safety industries but in many other sectors. Fig. 4 illustrates various state-of-the-art application areas of e-textiles. There is currently a great emphasis on applications that are affordable and wearable. Current prototypes of e-textiles are being developed for sports and medical applications such as sports training and patient monitoring. In the future, the automotive, retailing, military, fashion, and entertainment industries will also be niche application areas [73,74]. The shift is toward the design and development of technically advanced high-performance garments that are not just attractive and interactive but also offer substantial added value in terms of functionality [75]. The incorporation of flexible and stretchable sensors offers excellent capabilities for monitoring human actions and physical activities. These e-textiles could be effectively employed to detect human motions, and the data collected could be analyzed to track movement accurately. Such e-textiles may be used for real-time body measurements in retailing and for self-protection. E-textiles can be used in numerous sectors, depending on their basic functionality. Some specific developments of e-textiles in the areas of health and fitness are described below, based on recently published reports and research articles.
Fig. 4.
Application areas of e-textiles.
3.1. Medical: E-textiles use for telehealth remote patient monitoring
Conventional textile products, such as diapers, braces, breathable prostheses/orthoses, spiral dressings, rubs, breathing masks, bedding, and covers, are used for numerous human hygiene and medical applications [76]. Recently, some e-textiles have been used in the manufacture of other health products, such as surgical masks [77], personal protective equipment (PPE) [78], light therapy systems [79], wound dressings [1,80], flexible sensors [81], and actuators [82]. A recent study by Yang et al. [45] looked at the use of e-textiles to support healthy aging, including monitoring health conditions, treating chronic diseases, rehabilitation, and improving health and social lifestyles. A breakthrough has been the ability to monitor a patient in a health care center or at home using e-textile technology [83]. However, a gap still exists in the care provider's ability to assess the current and historical physiological state of the patient. The use of sensors has enabled wearables to carry out virtual health assessments and collect real-time feedback on health and fitness [[84], [85], [86]].
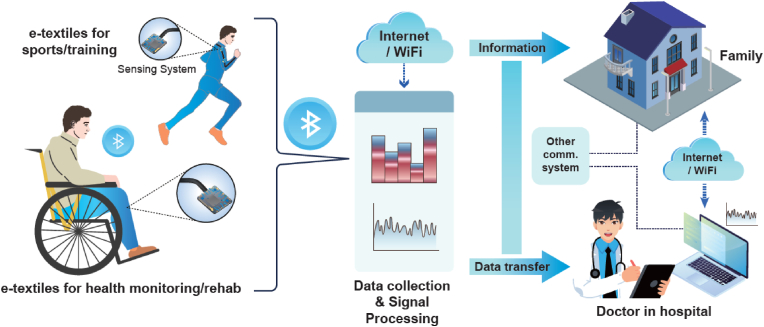
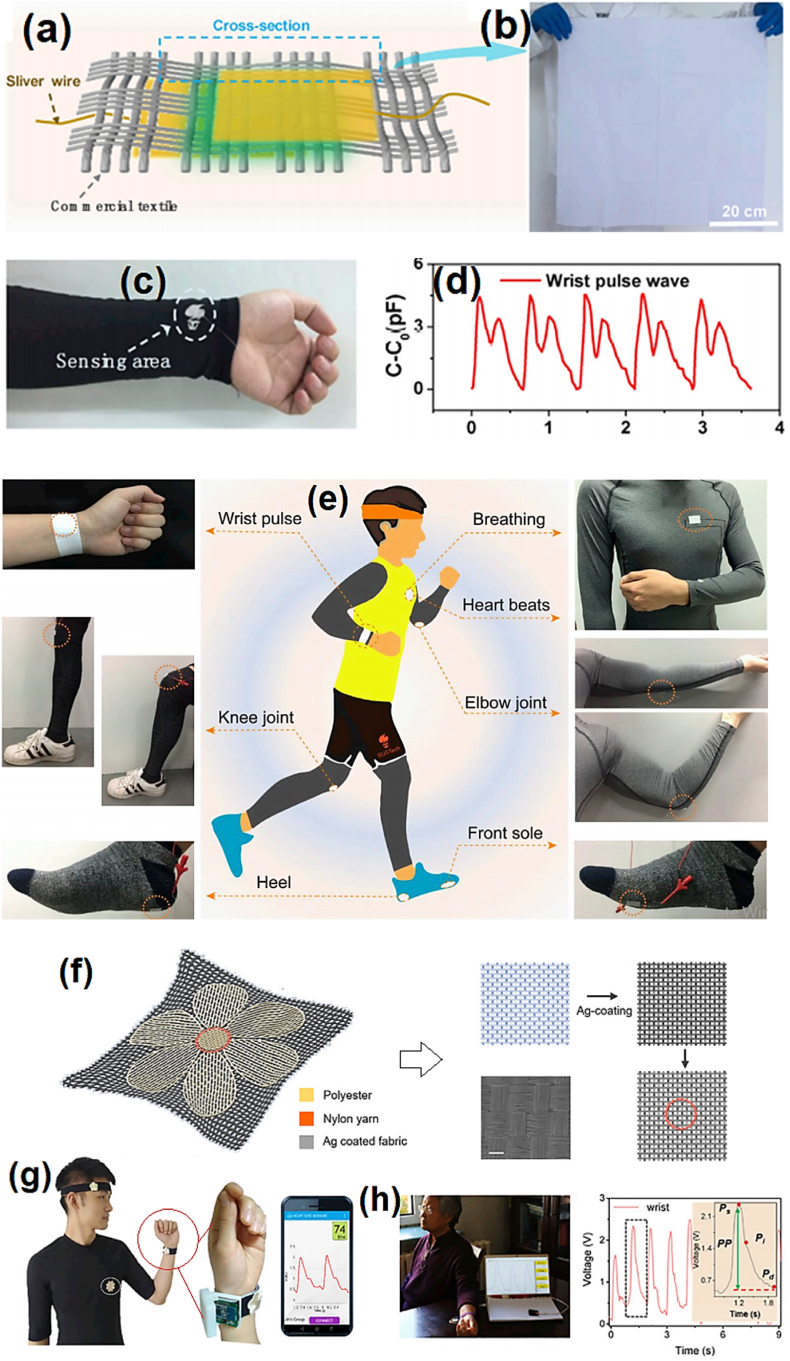
In the future, advanced e-textile-based sensing systems can be developed that can monitor chronic diseases and collect biometrics and other vital signs/disease signals wirelessly via Bluetooth and send them to a doctor/physician through the internet. Fig. 5 illustrates such a health and fitness monitoring system based on wearable sensors for rehabilitation or health monitoring to recovery via data analyses. E-textile technology could be used to detect patients’ movements and body positions. E-textile could be used to send emergency alerts: for example, it could distinguish whether a patient was sitting, lying down, or walking or whether there was a rapid change in position, such as would result from a fall [87]. E-textiles could also help achieve improvements in telemedicine, such as decreases in appointment times, faster diagnosis processes, and time savings for patients in getting concerns addressed. These improvements may provide patients and doctors more time to strategize effective treatment plans.
Fig. 5.
Illustration of a remote fitness and health monitoring system based on wearable sensors. The e-textile could access information from real-time body movements from personalized rehabilitation and other physical training/exercise and transmit that data to a smartphone via wireless communication signals (e.g., Bluetooth) and to a home system and clinic/hospital for analysis.
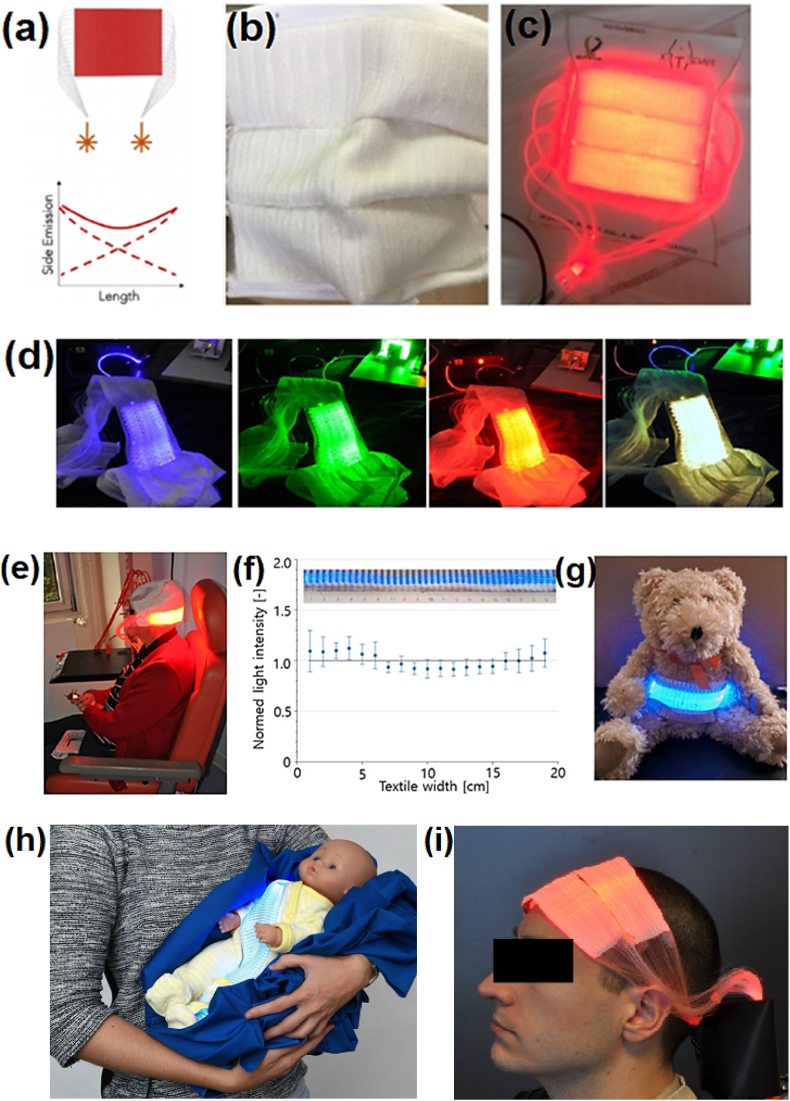
Wearable e-textiles could also provide smaller, more reliable, more lightweight, easier-to-use, and more cost-effective self-health management systems. Light-emitting device-based textiles are potentially useful for wearable therapy systems and as displays for self-protection. Finally, we hope that e-textiles will eventually become integral to home-based wearable health care systems that are integrated seamlessly into the wearer's everyday routine and offer more advanced functionality than the currently available stiff and wired harness devices.
3.2. Sport: E-textiles use for training data accumulation and rehabilitation
Edmison et al. stated in 2004 that advanced sensing structured e-textiles could be used for motion analyses [88]. Applications of e-textiles for sports and daily routine activities are extremely important to tracking performance. The growing attention and participation worldwide of people in active sports and outdoor leisure activities, such as walking, dancing, running, hiking, and swimming, has resulted in great demand for textile products in sports, games, and physical training. Fig. 5 (person running image) shows examples of e-textiles with printed sensors that can detect body movements during exercise or training and then transmit the collected data to a cell phone via Bluetooth or another wireless communication device. E-textiles for sports have the potential to substantially change the way athletes/trainers train and participate at all levels. In particular, applications of e-textiles include strain and bending sensors mounted on textiles and worn on body joints such as knees, arms, and necks. E-textiles can collect information about different knee positions and decipher physical actions, such as walking, running, jumping, and crouching [89]. Consequently, e-textiles can sense the body's position and muscle movements and offer feedback. Thus, we can access and then evaluate the performance of a person for further improvement. Commercial production of such systems has already begun, as two Canadian startups, OMsignal, smart clothing lab [90] and Myant [91] have introduced electronic sports garments that can monitor a wearer's heart rate, breathing, and movement and then send the collected data to a smartphone using Bluetooth Low Energy (BLE) for real-time analysis [92].
3.3. Elderly: E-textiles aim for physical activity tracking usage
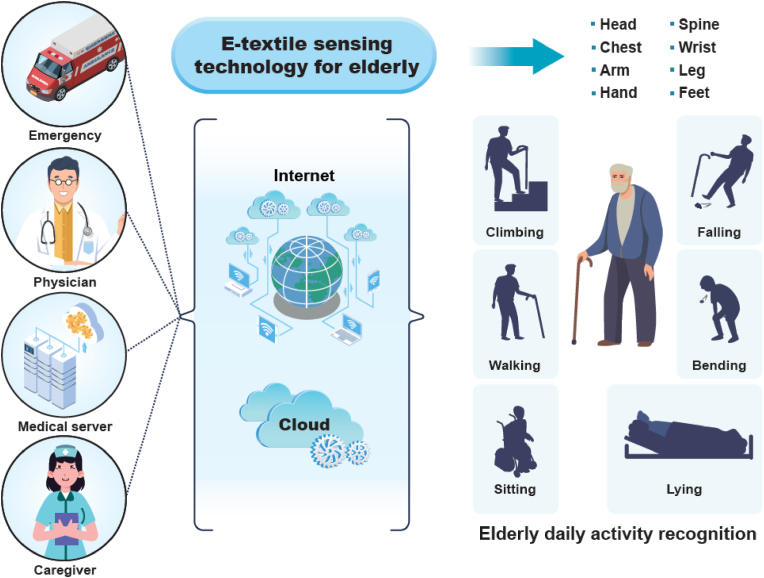
According to world population prospects (United Nations, 2019), health concerns are increasing in an aging society, and the elderly account will account for more than 16% of the world's population by 2050 [93]. Worldwide, the population of people aged 65 and above is growing faster than all other age groups. Thus, the health of elderly people is a major concern now and will continue to be so in the near future. In addition, the prevalence of modern unhealthy lifestyles and diets is expected to lead to ailments such as diabetes and high blood pressure (BP) in nearly half of the population [94]. In the telecare realm, obtaining information about the movement of the body is vital to ensuring the wellness of the elderly. As mentioned above, telehealth and telemedicine concepts, i.e., health and fitness-associated information being obtained from a distance by a health care provider (e.g., a fitness trainer, a doctor in a clinic/hospital, a physiotherapist, etc.) while users remain at home, can play a major role [95]. E-textiles could easily track all the movements of an elderly person using a sensing system for real-time monitoring. Thus, e-textiles can be used by emergency medical services (EMS) to give essential and urgent pre-hospital treatment and stabilizing medication for severe injuries and other illnesses, such as heart failure, asthma attacks, unconsciousness, etc., while transporting patients to hospitals. Fig. 6 shows an example of a future wearable e-textile sensing technology that can be highly beneficial for the care of the elderly to track movements and other parameters. The technology can be used for the detection of accurate positioning, tracking of physical activity, and monitoring of vital body signs. There is a vital need to develop a smart wearable for the elderly that can accurately sense body positions and remain connected in real time with modules for data processing and extraction. The data or information from the sensing system should be delivered to a controller lump/access and then to a cloud center, where it could be processed by data analysis algorithms.
Fig. 6.
Future application of an e-textile sensing system for the care of the elderly to monitor real-time movements (sitting, lying, climbing, walking, bending, and falling) and process data to track daily activity.
The impact of e-textiles is more evident in pandemics, such as the current coronavirus (COVID-19) pandemic, during which people face involuntary mass quarantines and must prevent human-to-human interaction to reduce virus transmission. These constraints can contribute to physically inactive lifestyles, which are associated with health problems such as obesity, lower back pain, poor blood circulation, osteoarthritis, and cardiovascular diseases [96]. As a consequence, a lack of physical inactivity may jeopardize the health of the elderly and people suffering from diabetes and chronic organ diseases. Wearable real-time sensing textiles can be used at home and in hospitals, care centers, and other training or fitness facilities to remotely monitor the elderly and other vulnerable people (e.g., COVID-19 patients) to ensure their safety throughout the day without the need for a risky visit to a hospital/clinic or care center. Recently, firm Sleeptite has launched a portable smart bed to monitor elderly's daily activities to improve the health and wellbeing through technologically advanced solutions [97]. In coming years, a portable e-textile sensing systems could become essential components of solutions for monitoring the health and safety of an aging population, an area likely to see growing market demand in the coming years. We believe that the significant advances made in miniaturization and development of smart materials will help to create a fifth generation of e-textiles that are integrated with cloud and wireless services and are suitable for the speedy adoption of cognitive technologies.
4. E-textiles market growth
The e-textile technology trend is gaining momentum, and the market will be a witness to an increasingly large number of new e-textile products soon. With the increasing demand in the already competitive market, there has also been a steady rise in new design, technology, and innovation. As a result, many technology companies and individual textile manufacturers around the world have started selling and working on an expanding array of new high-tech advanced electronic garments. We have summarized a few of commercially available wearable smart textiles/or e-textiles solutions for healthcare and fitness in Table 1.
Table 1.
Commercialized smart textiles/or e-textiles for healthcare and fitness applications.
| Company | Commercial smart/e-textile product |
Healthcare/fitness solution | Main Mechanism/technology |
Reference (Website) |
|---|---|---|---|---|
| Nextiles | Nextiles fabric | Mobility, physical therapy | Piezoresistive sensors | [98] |
| Sleeptite | Remi | Mobility, sleep monitoring | Flexible sensors | [97] |
| MesoMat | Sensing fibers | Physical mobility, real-time monitoring | Strain sensors | [99] |
| Toray Inc. | Hitoe | Respiratory monitoring, physical therapy | Strain sensors, conductive fabric | [100] |
| e-skin Meva | Xenoma | Mobility, Physical therapy, | Flexible sensors | [101] |
| Palarum | Smart socks | Mobility, physical therapy | Pressure sensors | [102] |
| Texisense | Texisock | Mobility, physical therapy | Pressure sensors | [103] |
| Carre Technologies Inc. | Hexoskin | Cardiovascular, Physical therapy, Mobility, breath monitoring | Strain and pressure sensors | [104] |
| Nanowear Inc. | SimpleSense | Cardiovascular, Physical therapy | Flexible sensors | [105] |
| DuPont | Intexar | Respiratory monitoring, Physical therapy | Electrodes | [106] |
| Clim8 | Heating gloves | Thermo-physiology | Joule Heaters | [107] |
| Loomia | LEL | Pressure monitoring, Seat heating | Electrodes, Heaters, Pressure sensors | [108] |
| Myant Inc. | Skiin | Mobility, thermotherapy, physical therapy | Strain sensors, Joule heaters | [91] |
| Souyarn | Heated garments, Sensing textiles | Mobility, sweat, respiration, and heart rate monitoring | Pressure sensors, Heaters | [109] |
| Smart Fabric Inks | Fabric heaters, | Thermotherapy | Heaters, Electrodes | [110] |
Moreover, wearable technologies are growing exponentially, and every day, new textile products are reaching the market, with functionalities such as heat regulation, luminousness, and touch sensitivity. James Hayward, a principal analyst at IDTechEx, has observed that many of the companies in the emerging smart textile trade create most of their revenue on a project-by-project basis, with consulting and R&D often being more profitable than focusing on specific products [83]. The total worth of the wearable electronics market is currently US$70 billion, but only approximately US$0.5 billion is derived from electronic fabric-based products [111]. The market revenue could increase further with the increasing miniaturization of electric components and circuits integrated/printed into textiles to create more robust e-textile products. Seamless integration of functionalities might help to avoid the possible bionic stigma and clinch market insight of wearable e-textiles. Further information is provided below on the remarkable records on profits being realized by e-textiles corporations, as well as examples of types of products available in each sector.
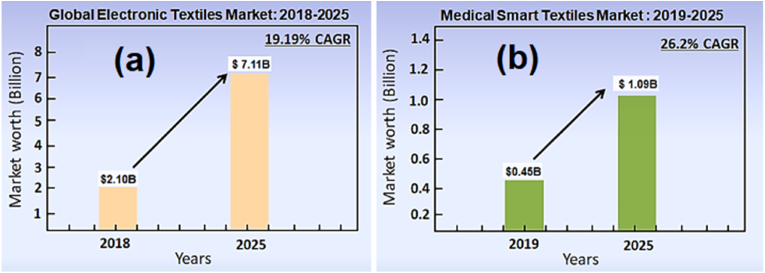
Hundreds of firms are actively working in the early-stage development and commercialization of smart e-textiles. According to a forecast from the IDTechEx report, in the next 10 years, the market for wearable e-textiles is expected to grow in value to US$2.0 billion (US$2000 million) per year by 2028 [112]. Information published in the Global Electronic Textiles Market Report suggests an even higher growth rate. According to this report, the global Electronic Textiles market size was US$2.1 billion in 2018, and it is expected to reach approximately US$7.1 billion by the end of 2025, with a compound annual growth rate (CAGR) of 19.19% between 2019 and 2025, as shown Fig. 7(a) [113]. This report shows the e-textiles market size in terms of value and dimensions by firms, regions, product types, and end-users, historical statistics for 2014–2018, and projections for 2019–2025. The scope of this report encompasses North America, South America, Europe, the Middle East, Africa, and the Asia-Pacific region. An analysis based on a market study report suggests that over the next few years, the medical smart textile market will exhibit a CAGR of approximately 26.2% in terms of returns. The global market size is projected to increase from $0.45 billion in 2019 to $1.09 billion by 2025, as shown in Fig. 7(b) [114].
Fig. 7.
(a) Global electronic textile market growth for years 2018–2015 and (b) medical smart textile market growth for years 2019–2025, based on quantitative data [113,114].
However, possessing a more progressive technology does not always result in a more effective product with a more complex design and competitive price, which are essential to adding value. The data presented above represent two different perspectives on common smart wearable product types. Their differences demonstrate how some important narratives can deviate from market realities. Advances in smart apparel with wearable sensors and light-emitting devices and several types of smart clothing exist as prototypes or are already on the market. The global e-textiles market can be described as following the example of integrated/printed electronic devices and their applications, as shown in reports on the progress of commercial e-textiles projects. The market encompasses e-textiles using first-generation electronic devices and those using modern third-generation electronic devices. In general, a driving force for the e-textiles industry is an emerging market in sensing coupled with internet connectivity. This combination makes it possible to communicate data on body movements and vital signs (e.g., heart rate), which are important for trade in healthcare, sports, and fitness. Electronic outfits (e.g., t-shirts/trousers) can capture heart rates to track physical activity, and thus such intelligent clothes are expected to stimulate demand from health- and fitness-conscious people. Recently, wearable devices have been in huge demand in the market, as demonstrated by the rate of growth of the wearable fitness market to US$34 billion in 2020, and this growth is likely to continue in the future [115,116]. Sensing wearables have also developed rapidly in the smart textile market, and this trend is expected to continue in the next few years. This trend is expected to influence a major portion of the global market globally, based on the data forecast in the IDTech report. Applications in the medical and sports sectors and others are expected to lead the global e-textiles market in the next decade and beyond. Apart from medicine and sports, another major sector for applications of e-textiles will be the military/defense sector, which would serve as a driving force for escalating growth opportunities for e-textile market revenue. There is also a considerable demand for self-regulating smart textile products in the architecture, automotive, consultancy services, fashion, and entertainment sectors. Therefore, these sectors will also account for notable proportions of the e-textile market. Sensors and light-emitting devices are currently the most commonly used components in smart electronic garments, which account for a large proportion of smart textiles. This is because sensing ability and electronics are the most vital characteristics of any type of smart e-textile product [117,118]. Despite e-textiles being extremely useful in the medical, sports, PPE, fashion, shelter, defense, and aerospace sectors, where they are already used for sensing and monitoring, they need to be more efficient and convenient if they are to be integrated with pliable electronics and power sources (e.g., batteries).
Face masks are currently one of the most used and demanded products in the world because of the COVID-19 pandemic [119]. Furthermore, because of the alarming spread of the SARS-CoV-2 virus around the world, face masks, respirators, and PPE garments are in high demand [120]. This has had an economic impact on the global market, and the growth of the respiratory fabric market has been among the top apparel industry trends in the last two years. The COVID-19 pandemic has drastically increased demand for face masks and encouraged the development of electric anti-viral face masks to meet the current high market demand [121]. The Wall Street Journal reported in July 2020 that N95 face mask manufacturers increased production substantially to meet COVID-19 demand. Some companies, such as 3 M, Honeywell, and Prestige Ameritech, are capitalizing on the fabrication of technical masks and PPE. With the increase in demand, electric face masks could become more desirable and fulfill current and future market needs to prevent the spread of respiratory infections. There are clear indications of growth in the market for electric respiratory apparel, with annual growth projected to increase over the next few years.
5. Textiles forming strategies: from fiber to fabric
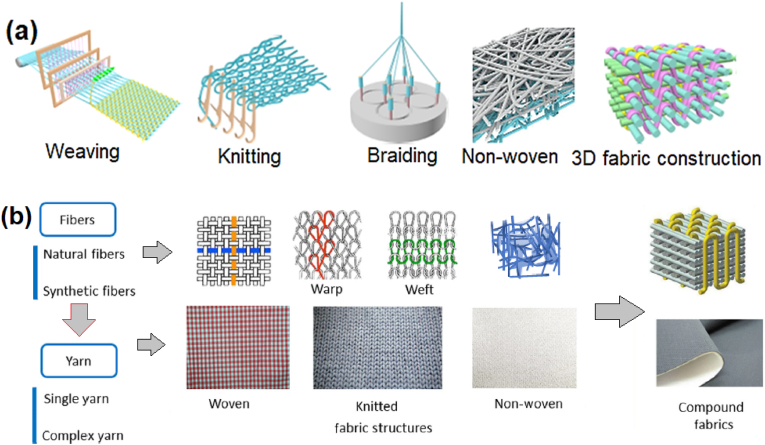
A textile is a hierarchical material, and it is important to understand basic formation process of textile fabric. Textile is 2D/3D composite structure constructed by fiber/yarn interlacing [15,122]. Fiber (natural/synthetic) is the most fundamental or raw material used to make fabric [123]. Yarns are made from fibers when they spun or twisted together [124,125]. Fabrics are made from yarns or threads when they interlaced or bonded together using different methods. Wu et al. described and compared some commonly explored textile forming strategies like weaving, knitting, braiding, non-woven and 3D textile structure [57]. The schematic designs of these textile forming strategies are shown in Fig. 8(a). Weaving is a highly recognized textile making technique. In this technique, a set of weft yarns is normally interwoven into other set of warp yarns that lie perpendicular to each other to create different weaving forms. In knitted process, various yarn loops connected to each other and to the nearest columns and rows. Braiding is a simple technique in which interlacing three or more yarns using a machine or manually using hands that they cross one another and are laid diagonally overlapping pattern to form a narrow strip or flat fabric. Nonwoven fabric is a web-like structure manufactured with fibers that are held together by using various techniques such as electrospinning, stitching, thermal, mechanical, and chemical bonding. Lastly, the 3D flat interlaced woven fabric structure made of three yarn sets (warp, weft and z-yarn) [126]. In this process, warp yarns are interlaced with weft yarns to the weave pattern in in-plane primary directions, while z-yarns are interlaced with warp yarns according to the weave pattern in out-of-plane at each layer.
Fig. 8.
Summarization of various fabric making strategies: (a) weaving, knitting, braiding, nonwoven and 3D formation. Images are reproduced with permission from Ref. [57], Copyright, 2022 Elsevier Ltd., [18], Copyright, 2022 Springer Nature Ltd. (b) Fabric production stages and hierarchy from fibers to multilayers compound fabric. Images are adopted with permission from Ref. [52], Copyright, 2019 Zhengzhou University.
In addition, Wang et al. also discussed the manufacturing methodologies from fiber to yarn and then to multilayers compound fabric as shown in Fig. 8 (b) [52]. These constructed fabrics can be further utilized for regular clothing and e-textiles applications.
Although fiber created yarns are basic building blocks of the textiles, but their physical properties are highly reliant on the types of elementary materials and fabrication strategies utilized. Various materials and yarns construction strategies are reported for different applications from advanced e-textiles to bio-textiles [[127], [128], [129], [130], [131], [132]]. Wu et al. have also discussed the merits and demerits of textile fabrications strategies [57]. For instance, in weaving, the fabric could be created with controllable size, shape and air absorbency but relatively nonextensile in the warp and weft directions and remain opposite in other preferable directions. In braiding, fabric showed high stiffness and excellent durability but showed low porosity than other strategies like knitting and weaving. In knitting, fabric could be designed with controllable size, structure and porosity and it is able to stretch in all desirable directions but showed poor Youn's modulus. Woven fabric is stronger and structurally sound better than non-woven fabric, but it showed defective selvage and broken ends/picks (warp/weft). 3D structured fabric could be constructed with controllable size and porosity with excellent mechanical characteristics, but its fabrication process is very complex.
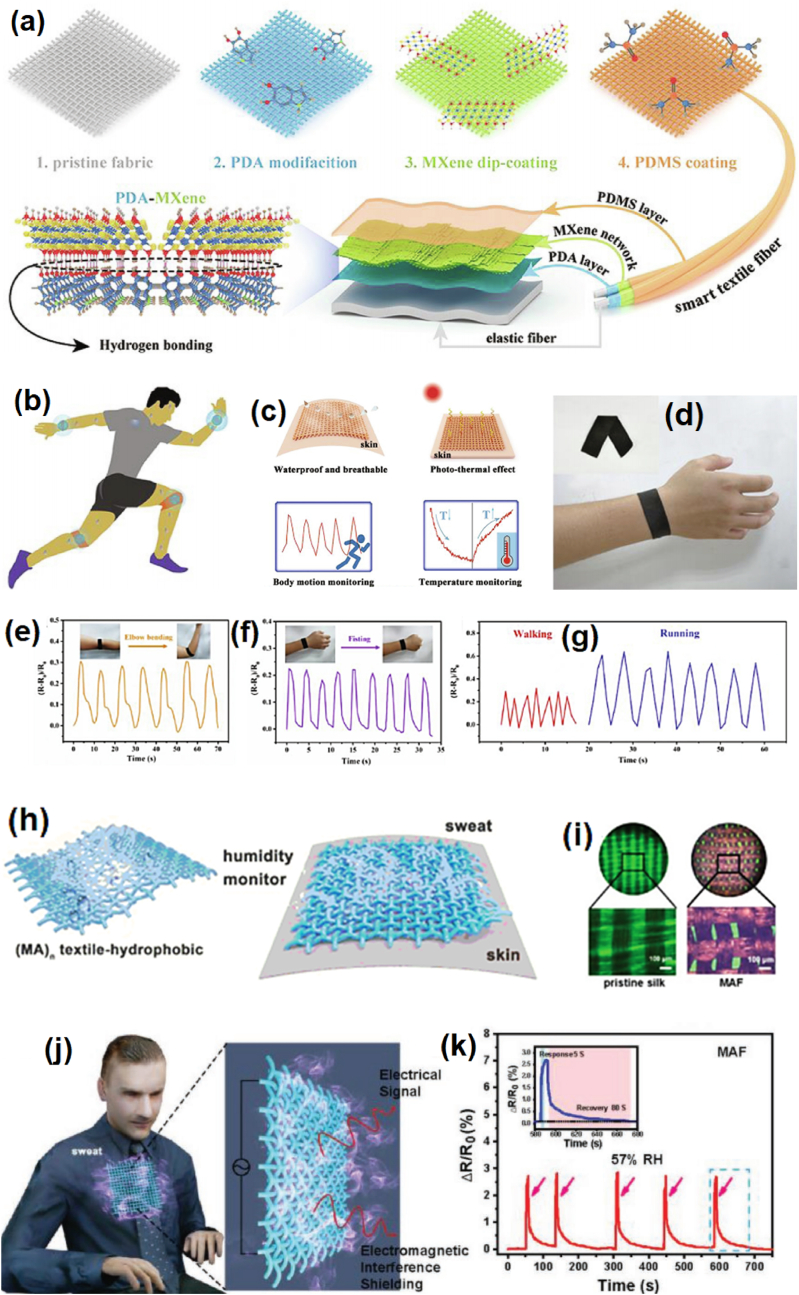
6. Materials and techniques required for fabrication of e-textiles
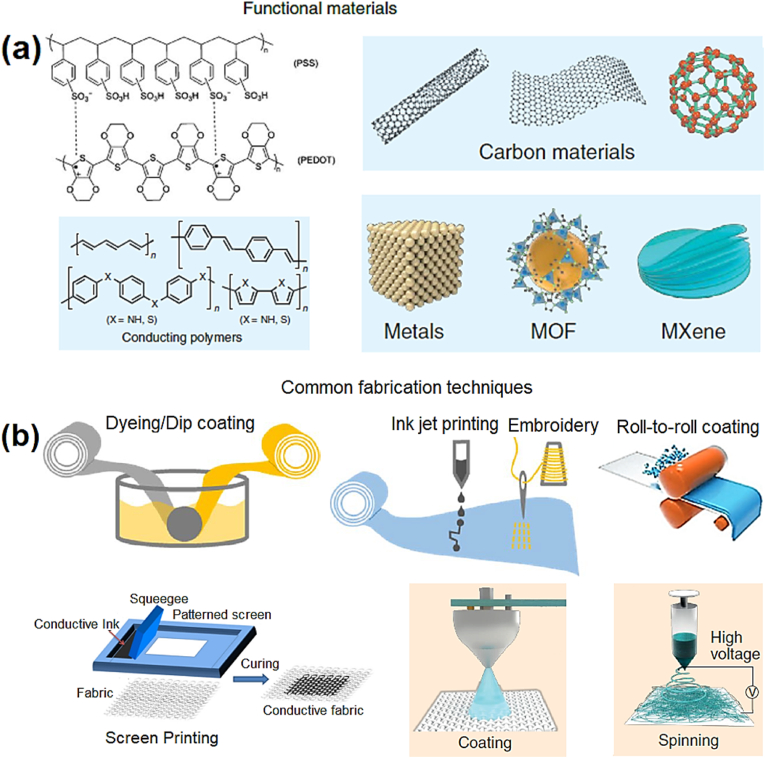
This section describes essentially functional materials and fabrication techniques for smart textiles/e-textiles and their application areas. Currently, a wide range of functional materials and techniques are being used in the development of electrically functional clothes for healthcare, fitness, and many other uses [1,20,123]. Smart textiles/e-textiles can be customized to measure strain, pressure, chemicals, humidity/sweat and temperature variations. Examples include dry conductors for monitoring, diagnosis, and treatment; dielectric elastomers for stretchable capacitive sensors; resistive and piezoelectric materials for sensors; electroactive polymers (EAPs) for actuators; carbon materials-based filament; dielectric adhesive-coated conductive yarns for conductors and heaters; and light-emitting active polymers for phototherapy, thermotherapy and electrotherapy [1,22,39,133]. Although, several materials and fabrication strategies and electronic device integration into textiles have been reported to produce e-textiles prototypes in academic research laboratories and mass scale production in industries. However, in this section we provide some most common materials and techniques being used in fabrication of e-textiles. Fig. 9(a) shows most common materials such as conductive polymers (Poly (3,4-ethylenedioxythiophene)-poly (styrenesulfonate) (PEDOT: PSS)), carbon materials, metals, metal-organic frameworks (MOF) and carbide/carbonitride (Ti3C2Tx) MXene, being used in development of e-textiles in recent years [1,18,127]. Fig. 9 (b) shows commonly explored methods such as dyeing, dip-coating, jet printing, embroidery (conductive fiber/thread), roll-to-roll coating, screen/stencil printing, spray-coating and spinning being used to produce conductive textiles and device/sensor integration into fabrics [15,18,134]. Moreover, metals can be integrated onto the textile fibers or co-mingled with their pristine form using thin metal nanoparticles and nanowires form. It has been observed from the literature sufrvey that for wearable applications, it is most common to combine metals or other conductive materials as a thin layer on the insulating surface of a pristine fabrics. Lastly, the electrically conductive fabrics can be transformed into proper wearable e-textile system integrated with computer/mobile and power source via connectors/wireless module to data accumulation for health and fitness assessment.
Fig. 9.
(a) Common conductive materials (conductive polymers, carbon materials, metals, MOF and MXene). Images are reproduced with permission from Ref. [18], Copyright, 2022 Springer Nature Ltd. (b) Fabrication techniques (dyeing, dip-coating, jet printing, embroidery, roll-to-roll coating, screen/stencil printing, spray-coating and spinning) using for the development of electrically functional textiles. Images adapted with permission from Ref. [15], Copyright, The Author(s) 2021.
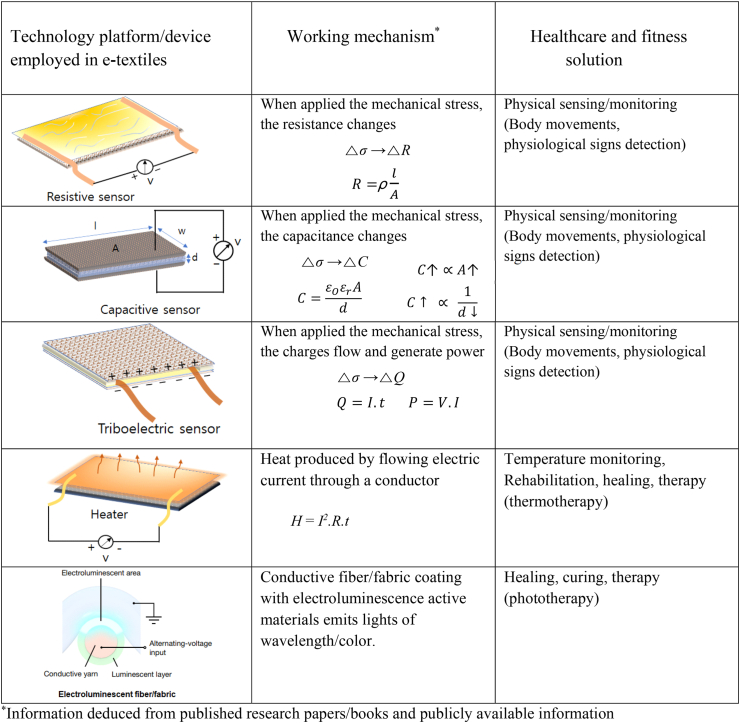
We have summarized the five main categories of electronic devices/technology have been employed so far for wearable e-textiles developments in Table 2. Basically, e-textiles comprises resistance, capacitance and triboelectric sensors for body movements and physiological detection. Wearable heaters integrated into fabric and light-emitting fibers/fabric used in rehabilitation and therapy treatments. Triboelectric, piezoresistive, capacitive and resistance-types strain and pressure sensors have used for physical sensing/monitoring to advance the e-textile technology [51,52,123,127,135]. Restive-type heaters [136,137] and light-emitting fibers and fabrics have utilized for therapeutic applications [79,138,139]. Herein, we describe only selected devices/technology platform used in smart e-textiles but there are many other materials and devices are being used in the development of the e-textiles for several applications.
Table 2.
Although we have cited most of the e-textile-related literature in this review, we provide more information about active materials and fabrication approaches. Several material preparation methods and manufacturing technologies that have been used in the last few years to develop wearable, comfortable, electronically functional garments for healthcare and fitness applications are summarized in Table 3.
Table 3.
Functional materials, fabrication procedures, and textile-based electronic devices and their applications in various sectors.
| Functional material(s) | Fabrication method | Type of e-textile device/technology | Application | Reference |
|---|---|---|---|---|
| Acrylamide cross-linking cotton fabric | Dip coating | Textile-based capacitive sensor | Real-time breath monitoring, talking, winking, and joint motions for rehab exercises | [26] |
| Silver (Ag)/silicone carbon paste | Printing | e-sleeve for functional electrical stimulation | Stroke rehabilitation/human body stimulation | [45] |
| MXene-coated cellulose yarns | Seamless knitting | Textile-based capacitive pressure sensor | Sensing body (finger) pressures and weights | [65] |
| Poly (3,4-ethylenedioxythiophene) polystyrene sulfonate (PEDOT: PSS) | Printing | ECG monitoring device | Chest and wrist monitoring | [146] |
| Single-wall carbon Nanotube | Coating | ECG-conductive cotton yarn | Body monitoring | [147] |
| Piezoresistive carbon | Stencil printing | Stretchable sensor | Human joint movement | [148] |
| Stainless steel yarn | Flat-knitting | Fabric strain sensors | Physiological monitoring | [149] |
| Carbon black | Dip coating process | Core-sheath fiber strain sensor | Triaxial trunk motion angles | [150] |
| Ag/AgCl-coated yarn | Knitting and sewing | Functional electrical stimulation fabric | Electrical stimulation of the body | [151] |
| Polymer optical fibers | Weaving | Luminous textile | Neonatal skin therapy | [152] |
| Cu-doped zinc sulfide (ZnS:Cu) | Roll-to-roll-compatible patterning | Light-emitting fiber | Electronic skin | [70] |
| Silver (Ag) ink | Knitting | EMG | Interossei muscles | [153] |
| Graphene | Dip coating | Electrooculography (EOG)- elastic headband | Forehead | [154] |
| Ag/AgCl-coated thread | Seamless knitting | Electroencephalography (EEG) | Forehead | [155] |
| rGO/single-wall carbon nanotube (SWCNT) | Dip coating | Fabric strain and pressure sensor | Body/joints movements | [156] |
| AgNW-coated P(VDF-TrFE) fiber sensor | Electrospinning/yarn dip-coating | Textile strain sensors | Heart rate monitoring | [157] |
| Carbon nanotube (CNT) | Spinning/chemical vapor deposition (CVD) | Strain sensor | Assessment of body movements | [158] |
| Polyurethane (PU) core/nylon cover fiber yarns decorated with AgNWs | Dip coating | Piezoresistive strain sensor | Health monitoring/artificial skin | [159] |
| Poly (ethylene terephthalate) (PET) yarns and PEDOT enclosed with PMMA | In situ polymerization | Textile strain sensor | Human motion monitoring | [160] |
| One-ply terylene yarns/stainless steel fiber | Stitching/knitting | High-pressure textile sensor array | Epidermal physiological signal monitoring | [161] |
| Eeonyx conductive thread | Sewing/embroidery | Conductive fabric sensor | Knee angle measurement | [162] |
| Silver/polyester fibers | Dyeing | E-textile strain-electric sensor | Physical kinesis monitoring | [163] |
| Ecoflex/carbon black | Machine sewing/embroidery | Battery-free textile temperature/strain sensor | Human physiological signals | [7] |
| Graphene flakes | Yarn dyeing/knitting | Wearable textile sensors | Wireless body temperature monitoring | [164] |
| Silicone/silk-coated wire/tencel yarn | Weaving/printing | Wearable electrotherapy | Pain relief | [165] |
| Graphene-based conductive pattern | Ink-jet printing | Wearable e-textiles | Health monitoring | [166] |
| Stainless steel/cotton fiber | Weave design/seam construction | E-textile jumpsuit | Motion capture | [167] |
| Carbon nanotube (CNT)/polyurethane (PU) | Dip coating process | Pressure-sensing textiles | Tactile touch/pressure perception | [168] |
| CNT ink/cotton composite fabric | Direct screen printing | Strain sensor | Electrical heating/color changing | [169] |
| PEDOT:PSS/zirconate titanate (PZT) | Dip coating | Pressure-based sensing socks | Sports and health monitoring (gait, sweat analysis, etc.) | [170] |
| Electroactive ferroelectric/copper | Embedding/entrenching | Capacitive pressure sensor-based smart sock | Human gait segmentation and analyses | [171] |
| Liquid metal paste | Printing | Stretchable biomechanical strain sensor | Measurement of elbow flexion angle | [172] |
| Silicone foil with silver particles | Weaving | Electroconductive textile device | Electrotherapy | [173] |
| Photodiode and LED-embedded textiles | Woven, knitting | Photoplethysmography (PPG) sensing textile | Heart rate monitoring | [174] |
| MXene | Electrospinning | Near-infrared (NIR) irradiation nanobelt fibers | Wound healing | [175] |
| MXene | Dip coating | Multifunctional nonwoven smart fabric | Joule heating for healthcare and thermotherapy | [176] |
| Polydopamine (PDA)/PEDOT:PSS | Self-assembly dip coating | Conductive silk microfiber patch | Analysis and wound treatment in diabetes cases | [177] |
| Silver fractal dendrites (Ag-FD) Conductive ink | Screen printing | Stretchable aesthetic e-textile | Human motion detection and body-temperature management | [178] |
| CNT films, PEDOT:PSS | Electrospray | Stretchable thermoelectric woven fabric | Sensing, energy harvesting, thermal management | [179] |
| Silkworm cocoons, water-soluble poly (vinyl alcohol) (PVA)-assisted Ag nanofibers | Electrospinning, Magnetron sputtering | Battery-free sensing fabric | Compression sensor for movement monitoring | [180] |
| PVDF/AgNWs nanofibrous membrane | Electrospinning | Self-powered pressure sensor textile | Motion sensing and pulse monitoring | [181] |
| Nylon, Polytetrafluoroethylene (PTFE) | Weaving | Breathable and washable sensing textile | Human activity and pulse monitoring | [182] |
| Cotton fabric, PEDOT:PSS | Dip coating | Three-dimensional (3D) thermoelectric spacer fabric | Self-powered pressure−temperature-sensing | [183] |
| Polyaniline (PANI) with nanodiamond (ND) | In situ polymerization | Strain-sensing fabric | Human motion detection | [184] |
| Silver flakes, PU | Screen/stencil printing | Large-scale e-textiles for health care and sports | EMG health monitoring | [185] |
| AgNWS | Screen printing | Supersensitive all-textile pressure sensors | Human motion detection and human–machine interaction | [186] |
| CNT/Ni on polyester/nylon textile | Electroless plating, dip coating | Large-area fully textile pressure sensor | Human motion and physiological signals monitoring | [187] |
| AgNPs/PU | Thermal bonding approach | Pillow-shaped hierarchical 3D pressure sensor | Physiological activities (sleep posture and breath status) | [188] |
| GO, l-ascorbic acid (l-AA) reduction (rGO) | Pad dyeing | Wool-knitted fabric strain sensor | Breathing, perspiration, movement | [189] |
| Polypyrrole (Ppy) | In situ polymerization | Knitted fabric wearable sensor | Strain sensing | [190] |
| Graphene/PDMS | CVD, spin coating | Woven fabric strain sensor | Fitness tracking and communication | [191] |
| MXene/PU/cellulose nanocrystal | Dip coating | Nonwoven fabric tunable wearable strain/pressure sensor | Motion detection, human physical signal detection | [192] |
| MXene | Dip coating, pad trying | Breathable, durable, and bark-shaped MXene/textiles | Pressure sensor and heat physiotherapy | [193] |
7. Current health problems and their potential e-textile solutions
7.1. Viral infection caused by coughs and sneezes
Transmittable illnesses such as flu, colds, SARS, and strep throat spread from human to human through close interaction or physical contact, such as touching or kissing somebody who is infected. Infection also spreads when infectious germs travel through the air when someone nearby sneezes or coughs. Cold and influenza are common viral infections caused by coughs and sneezes that disperse a large number of droplets into the environment, and they transmit respiratory viral infections by physical contact or through inhalation, leading to mild to severe illness. Respiratory droplets remain the most common source of contagion, with the limit of transmission typically being a distance of 1 m in the case of normal breathing, as shown in Fig. 10(a) [194]. Germs can easily be spread by coughing, sneezing, or talking and can cause the spread of serious respiratory diseases, such as influenza, respiratory syncytial virus (RSV), and the novel SARS-CoV-2 corona (COVID-19) virus. The COVID-19 pandemic has resulted in people facing mass quarantine to prevent human-to-human interaction to reduce transmission.
Fig. 10.
(a) Acute respiratory virus propagation by droplets. Reproduced with permission [194]. Copyright 2020, Society to Improve Diagnosis in Medicine. (b) Mechanisms of deposition of inhaled particles in the lung. Reproduced with permission [195]. Copyright 2020, ATS journals. (c) Possible mechanisms of cardiac and lung injury with COVID-19. Reproduced with permission [196]. Copyright 2020, Elsevier. (d) Model of COVID-19 virus entry into the brain and effectual antiviral drugs. Drugs that can cross the blood–brain barrier could be advantageous in treatment strategies. Reproduced with permission [197]. Copyright 2020, Elsevier.
Coronavirus particles enter the body generally through the nose and mouth and from there can enter the lungs, causing potentially serious illness, as shown in Fig. 10(b) [195]. The coronavirus can also invade the heart and the central nervous system (CNS), leading to neurological diseases. Fig. 10(c) shows the mechanisms of cardiac and lung ailments associated with COVID-19 that can have serious consequences, including death, for patients with lung infections and heart diseases [196]. The virus can enter the CNS through olfactory nerves upon nasal infection, resulting in inflammation and demyelination. The virus can also enter the brain via the blood–brain barrier and cerebrospinal fluid (CSF) through the blood–CSF artery in just a few days. The coronavirus can thereby damage the entire CNS. A few days is sufficient time for the virus to spread and harm the medullary neurons. The mechanism of the spread of SARS-CoV-2 once it has invaded the CNS is illustrated in Fig. 10(d). In a recent study, Vellingiri et al. observed that the symptoms that might point to lung disease are related to a failure of air flow into the lungs, which might be due to weakened inhalation, which is controlled by the nervous system [197]. The novel coronavirus's association with respiratory illness has put unprecedented strain on the global healthcare system. The COVID-19 epidemic remains a threat to populations around the world and may contribute to alarming types of respiratory diseases in the future. Fabric masks and surgical masks are designed to keep other people safe from the spread of viruses by the mask wearer. There have recently been considerable advancements in the design and production of masks that are highly effective in controlling virus transmission.
In the face of evidence that the coronavirus and other infectious disease-causing particles may spread by talking and breathing, as well as coughing and sneezing, the World Health Organization (WHO) recommends that people cover their faces with specially designed cloth or fabric masks in public places to help stop the spread of germs and viruses [198]. There are various types of face masks currently available on the market that protect the mouth and nose in various ways. The most common and affordable masks, such as cloth face masks, simple face masks, more specially designed masks (R95, R99, R100, P95, P99, P100), surgical face masks (N95, N99, N100), and electric face masks are all reported to be effective against various virus sizes [119,[199], [200], [201]]. Konda et al. described the filtration effectiveness of different types of fabrics as depending strongly on the aerosol particle size of aerosol, with the best results achieved for particles from 10 nm to 6 μm in size [202]. Not all fabrics meet the requirements for power-driven face masks, which use battery power and fan filters to enable air circulation. This could be the reason that such masks can be quite comfortable to use because they do not retain humidity around the mouth and nose.
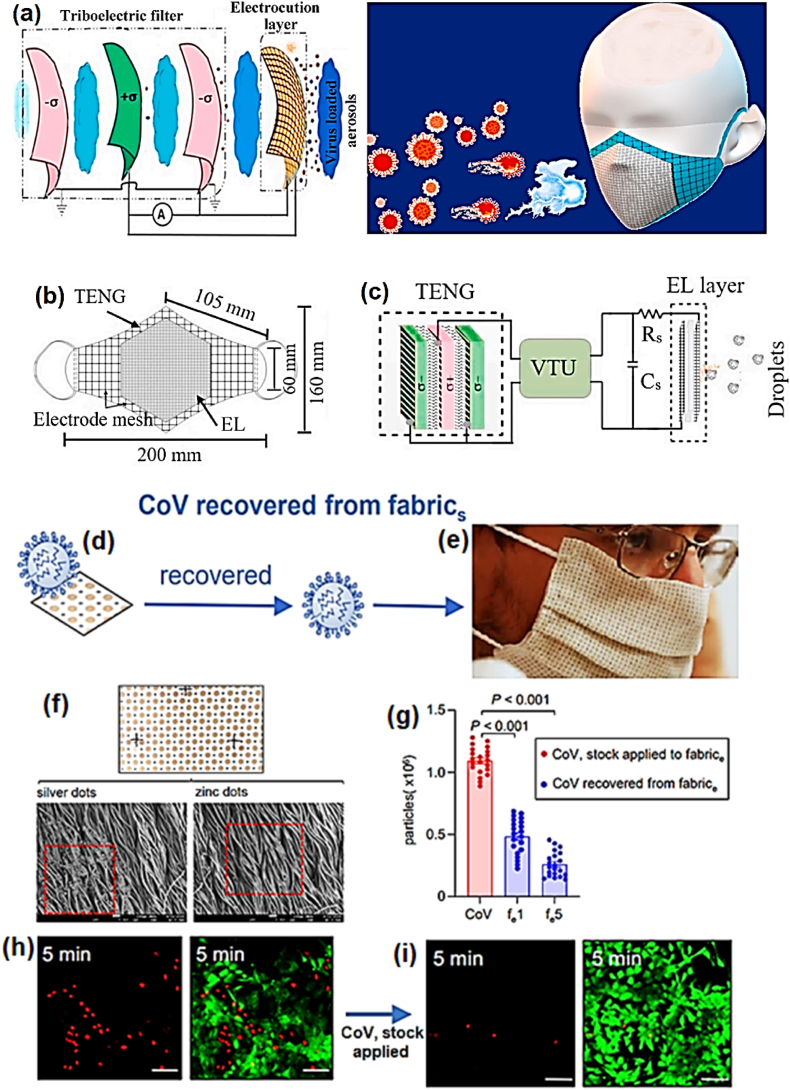
7.2. Use of e-masks to control respiratory disease transmission
The effectiveness of electronically functional fabric masks is under evaluation by various research groups worldwide to assess how useful they may be in preventing the spread of respiratory diseases. According to Leung et al. [203], surgical masks are less effective than electric masks in reducing the transmission of influenza and seasonal viruses that cause common colds. To overcome these complications and suppress sneak currents, the use of electronic fabric masks is highly desirable. For example, Ghatak et al. reported a newly designed self-powered e-mask for the prevention of COVID-19 [204]. Although simple fabric masks [202], as well as surgical masks [205], are considered to protect others from virus spread by the mask wearer, this newly designed mask is believed to be able to kill the COVID-19 virus within the range of the electrical field and protect the user from the deadly virus. Fig. 11(a) shows a schematic representation of a multilayered face mask in which the inner and middle layers consist of tribo-series materials (TSM), together with a self-charged triboelectric nano-generator. The proposed design and the working mechanism of the self-powered mask are shown in Fig. 11(b and c, respectively). The design is based on a triboelectric nanogenerator (TENG) device with an electrocution layer (EL) that may work for the deactivation and filtration of SARS-CoV-2. A latex rubber–polyurethane (PU) was used in the fabrication of this self-powered electric mask. The mask was able to induce power in the μW range based on its maximum triboelectric charge density. The study showed that because of the contact electrification of the triboelectric layers (TLs), the power generated in the mask helped to deactivate the virus transmission. The working mechanism of the mask is derived from the triboelectricity and proper use of the electric field to stimulate the EL. Other factors are also considered in obtaining effective filtration, such as the inhalation/exhalation rate and the distance between TLs. This work shows that technology could be very helpful in stopping the transmission of the novel coronavirus through the charge adsorption method. Electrocution by triboelectrification offers effective protection against the potentially fatal effects of SARS-CoV-2 or other similar viruses that may exist in the future. The outer layer of the mask functions as a smart layer, and the tribo-charges induced through contact electrification and triboelectrification between tribo-pairs help to decimate virus particles in aerosols. The triboelectric nano-generator would be self-charged, i.e., no external power is required to turn it on. The mask can work efficiently even when the user is resting or sleeping and retains additional charge when the inward and outward aerosol flow contains no virus particles. In addition, the integration of the outer layer provides extra protection for the wearer in case inward aerosols interact with the mask. Consequently, the electrically charged virus can be killed by electrocution when exposed to the smart layer. This gives double-layered protection from middle and inner TLs in a self-powered mask. The storage capacity of the self-powered mask lets the wearer act immediately to deactivate charged viruses comfortably. The results of this study motivate the development of textile-based e-masks that are capable of operating without external control or intervention to keep users safe from the spread of viruses. This e-mask has huge potential to be used for critical purposes by anyone, as it is inexpensive to manufacture, self-powered, and safe.
Fig. 11.
(a) Proposed schematic view of triboelectric self-powered mask with multiple layers. The first three layers (left side) function as a triboelectric filter, and the outer layer function as a conducting mesh. (b) Concept design. (c) Working mechanism of the proposed multilayered self-powered prototype mask. Reproduced with permission [204]. Copyright 2020, Elsevier. (d) Sketch of SARS-CoV recovered from fabric when pre-exposed to the electroceutical fabric for 5 min and the stock applied on fabric. (e) Digital photograph of fabricated mask used on a volunteer that can generate a weak electric field to destroy the virus. (f) Photomicrographs of electroceutical fabric and SEM images of Ag and Zn dots. (g) Calculation of viral particles from stock applied to fabric and recovered from fabric, when SARS-CoV contacts the electroceutical fabric. ST cells infected with viruses exposed to the electroceutical fabric for 5 min each and loss of cell viability. (h & i) Eradication of respiratory coronavirus (CoV) subjected to contact with the charged mask for 5 min, which indicates that the effectiveness of the cartridge improves from 85% to approximately 95%. Reproduced with permission [206], Copyright 2021, Springer Nature.
Ghatak et al. developed an electric facemask using electroceutical fabric to kill coronaviruses that come into contact with the mask [206]. This electroceutical fabric mask was first tested against a pig coronavirus and then on a human coronavirus that causes the common cold or fever. Although it was not tested against the SARS-CoV-2 virus, it could also be effective against this deadly virus. This work offers potential benefit to the scientific community by contributing to providing a solution to ending the COVID-19 pandemic. Fig. 11(d and e) shows illustrations of virus-pre-exposed fabric and the prototype face mask on a wearer. The mask is fabricated using stretchable electroceutical textiles referred to as electroceutical fabric (fe). A polyester fabric was used to produce the electroceutical fabric, printed with various spherical dots of silver (Ag) and zinc (Zn) particles, as shown in Fig. 11(f). Scanning electron microscopy (SEM) showed the deposition pattern of the Ag and Zn dots on the fabric. Fragments (∼105) of a pig respiratory coronavirus were put into direct contact with the fabric for 1–5 min, and approximately 104 virus particles were recovered. The mask consists of a designed pattern of Ag and Zn dots printed onto a piece of fabric made of polyester or cotton material. These Ag and Zn dots create a power source that generates a weak electric field when exposed to a conductive medium, such as sweat or gel. Electrons move from the Zn to the Ag in an oxidation–reduction (redox) reaction that produces a voltage of 0.5 V. Fig. 11(g) shows a size distribution plot demonstrating the presence of a cluster of the virus. The calculated yield of the viral dots was 44.29%, and recovery of 23.73% from the fabric was achieved when exposed to electroceutical fabric for 1–5 min. The loss of coronavirus infectivity when exposed to electroceutical fabric for testing cell viability is shown in Fig. 11(h and i). The contamination of cells with CoV was found to affect the apparent loss of cell viability. A cytopathic effect of CoV was entirely absent when the virus was exposed to the fabric. This work demonstrates the potential of electric fabrics for use in stopping the spread of viruses such as COVID-19. No external power source is required to induce the electric field; instead, the electroceutical fabric coated with Ag and Zn particles serves as the source of a weak electric field. The term “electroceutical” indicates a pattern of embedded microcell batteries that generates an electrical field and produces a low amount of power in the presence of moisture (humidity) or gel particles. Research has shown that viruses can be electrically charged and eliminated or destabilized [[207], [208], [209]]. According to these studies, coronaviruses can be destroyed or disabled when exposed to the low-level electric field produced [204,206]. The results suggest that it is feasible to recharge the masks post sterilization and regain filtration efficacy. This is an encouraging technological development that merits additional study, as it may be useful for everyday purposes, such as in PPE.
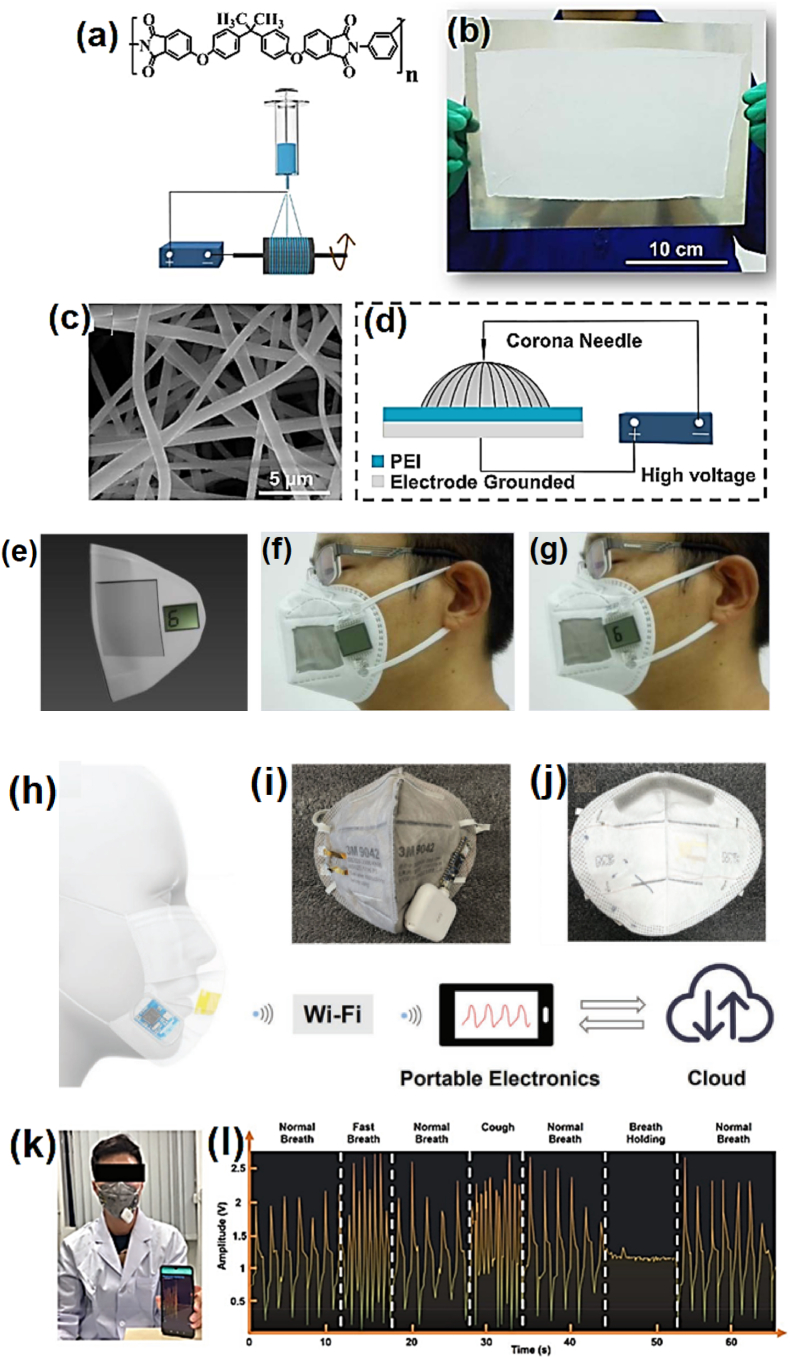
A recent study by Cheng et al. proposed a bi-functional electronic face mask fabricated using a nonwoven polyetherimide (PEI) fabric as an electret material using an electrospinning technique [210]. The mask was used to eliminate particulate matter (PM, also called particle pollution) and monitor a person's breath rate. The smart electric face mask has two functions: removing PM and generating electricity. The electric mask was designed to maintain residual charges steadily in the nonwoven PEI. The chemical formula of PEI and the electrospinning process used to produce the nonwoven PEI fabric are shown in Fig. 12(a). In this study, PEI was used because of its chemical stability and low cost as an electret material. Fig. 12(b) shows the developed uniform and large-area free-standing nonwoven PEI produced using an electrospinning technique. A PEI solution was used to form the robust and flexible nonwoven PEI at a high applied voltage of 25 kV. Fig. 12(c) shows an SEM image of the PEI fibers (1 μm diameter) deposited via layer-by-layer (LBL) assembly to produce the nonwoven PEI. Next, a corona charging method was used to insert charges into the nonwoven PEI, as schematically illustrated in Fig. 12(d). Furthermore, the nonwoven PEI was capable of working as an electrostatic field supplier when assembled in a sandwich-structured nanogenerator. The assembled nonwoven PEI was integrated with a commercially available mask to supply power to a low-consumption liquid crystal display (LCD), as shown in Fig. 12(e). At any state of motion of the nanogenerator, negative charges (σ0) in the nonwoven PEI generated resultant positive charges in the upper (σ1) and bottom (σ2) net electrodes, distributed as σ0 = −(σ1 + σ2) [211]. For example, exhalations might stimulate the nanogenerator to produce electricity to light up an LCD, as shown in Fig. 12(f and g). The PEI exhibited a maximum removal efficiency of approximately 99.6% of sub-micron particulate matter (0.3 μm size). This work demonstrated a novel approach to the development of wireless self-powered wearable electronics and electric smart air filters with low manufacturing cost and high efficiency.
Fig. 12.
(a) Chemical formula for PEI and schematically designed electrospinning technique for creating nonwoven fabric. (b) Digital image of nonwoven PEI fabric produced on a metal sheet. (c) SEM image of nonwoven PEI fibers. (d) Graphic representation of corona charging technique. (e) Smart electric mask. (f) Digital photograph of the mask. (g) Digital image of exhalation producing electricity that illuminates an LCD, which displays the number “6.” Reproduced with permission [210]. Copyright 2017, Elsevier. (h) Schematic representation of cordless self-powered face mask for breath monitoring. Digital images of the smart face mask (i) front and (j) back sides. (k) Digital photograph of demonstration of wireless real-time breath monitoring procedure for an actual application. (l) Screenshot illustrating the quantified constant and consecutive breathing activity during a sequence of normal breathing, rapid breathing, normal breathing, coughing, normal breathing, breath holding, and normal breathing. Reprinted with permission [212]. Copyright 2021, Wiley-VCH GmbH.
Recently, Zhong et al. designed a self-powered wireless smart face mask for real-time monitoring of breathing conditions in daily life [212]. The smart face mask was constructed by incorporating a pressure sensor and a wireless readout circuit into a regular fabric mask, as shown in Fig. 12(h). Breathing conditions are monitored using this smart face mask, and the data are transmitted wirelessly using a portable device such as a smartphone. The pressure sensor was integrated into a typical mask, and the circuits were connected to a battery power supply. Breath gestures were sensed by the electric mask and then transmitted to the cloud database via a portable device. The breathing data of an individual or a group of people can be transmitted to a cloud database to populate a health database for further analysis. Front- and back-side images of the prototype electric face mask images are shown in Fig. 12(i and j, respectively). The pressure sensor was manufactured using double gold bonding (Au–Au) of two Au/parylene/Teflon films that produced internal electric dipoles. These electric dipoles permit pressure sensing through the generation of a piezoelectric-like response [213]. The smart face mask exhibited excellent outcome stability and could be used for continuous monitoring and analysis of breathing patterns, such as normal breathing, rapid breathing, breath holding, and coughing. The smart mask was tested on a healthy 28-yr-old old male volunteer to assess its practicality and for data validation, as shown in Fig. 12(k). Fig. 12(l) shows the different breath conditions detected by the wireless smart facemask. Thus, we can conclude from this work that a suitable and convenient breath-monitoring e-mask can detect and store long-term breath data for use in the health care of an individual or a group of people.
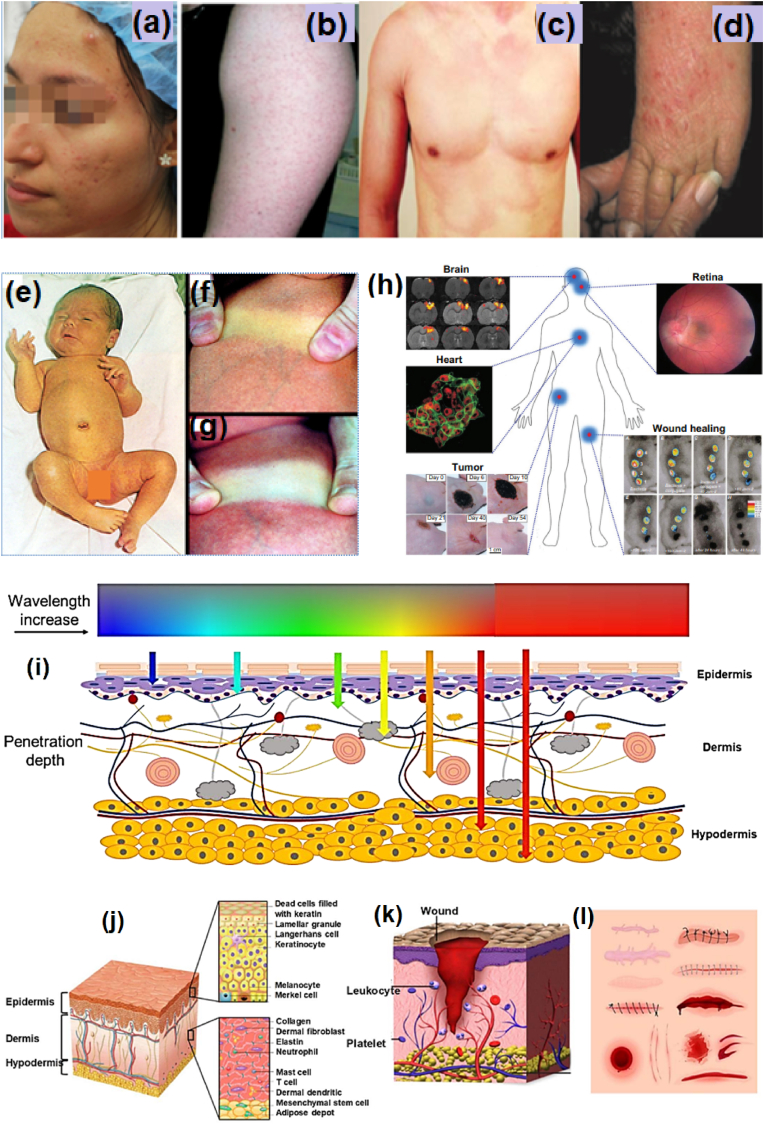
7.3. Health problems due to sedentary lifestyles
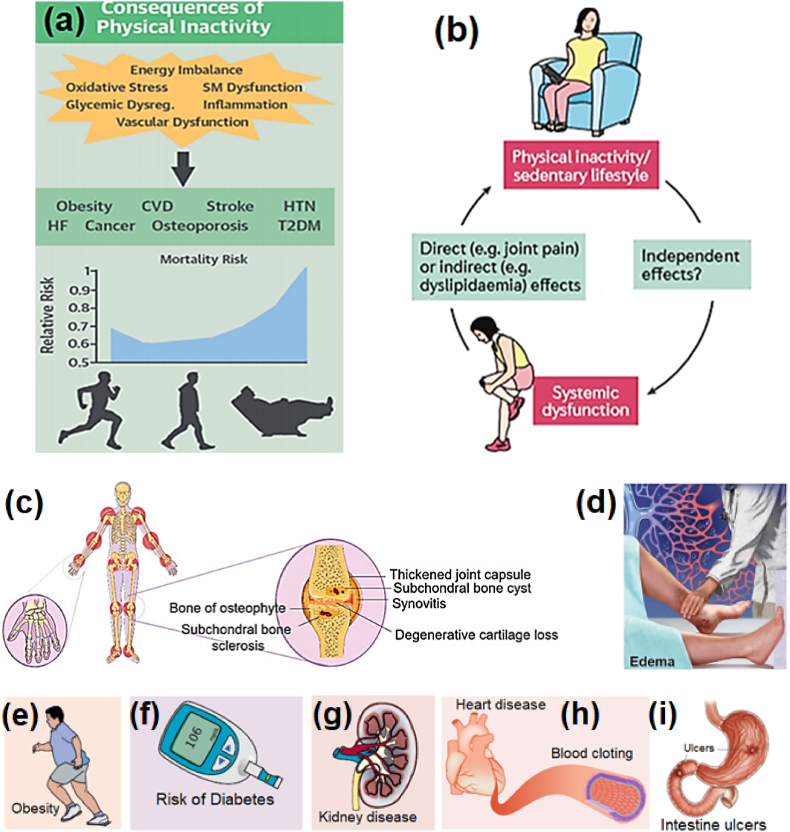
Any physical movements due to skeletal muscle actions of the body are recognized as parts of a physically active or sedentary routine. In 2018, WHO reports indicated that physical inactivity (lack of body movements) had been recognized as the fourth primary cause of 6% of deaths worldwide [214,215]. Some of the health problems associated with physical inactivity for people in any age group, from teenagers to the elderly, are shown in Fig. 13. Because of the lack of physical activity, the risk of noncommunicable diseases is increasing and causing increasing numbers of deaths worldwide. Physically inactive people are projected to be at a 20%–30% greater risk of casualties than people who are physically active [216]. Physical inactivity accompanied by pathophysiology is one of the major causes of the increased incidence of metabolic and heart diseases, osteoporosis, ulcers, and cancers. An active lifestyle significantly decreases the risk of contracting such ailments and reduces the risk of mortality, as shown in Fig. 13(a). Inactive lifestyles increase the risk of death from all causes; double the risks of cardiac diseases, obesity, diabetes, and edema; and increase the risk of cancer. Fig. 13(b) shows that physical idleness and sedentary behavior lead to systemic dysfunction and the aggravation of symptoms of pediatric rheumatic illnesses. Certain symptoms can have direct effects; for example, joint pain can affect physical functioning. Other systems can have indirect effects, such as inclining a patient to a more inactive routine [217]. As the aging population worldwide continues to increase, more patients are projected to suffer from marked physical disabilities by 2050 [93].
Fig. 13.
(a) Consequences of a sedentary lifestyle: mortality risk vs. relative risks. Reproduced with permission [216]. Copyright 2018, Elsevier. (b) Vicious cycle of physical inactivity and/or sedentary lifestyle and systemic dysfunction leads to systematic dysfunctions. Reproduced with permission [217]. Copyright 2017, Macmillan Publishers, Ltd. (c) Schematic illustration of osteoarthritis, which affects all of the joints in the human body. Reproduced with permission [218]. Copyright 2019, Taylor & Francis Group. (d) Edema: fluid accumulation or swelling. Reproduced with permission [220]. Copyright 2013, American Academy of Family Physicians. Other risks, such as (e) obesity, (f) diabetes, and (g) kidney disease. Reproduced with permission [221]. Copyright 2018, Elsevier. (h) Heart diseases and blood clotting. Reproduced with permission [222]. Copyright 2018, Springer Nature. (i) Intestinal ulcers. Reproduced with permission [223]. Copyright 2017, Elsevier.
Kou et al. described osteoarthritis as a progressive and degenerative ailment that affects the whole joint system [218]. Like most of the diseases associated with aging, osteoarthritis is a primary cause of chronic disability, affecting approximately 40% of those 60 or more years of age [219]. Fig. 13(c) shows damage from joint osteoarthritis that has affected the joint structure and articulation functionality. The human body's skeletal system includes the synovial membrane, articular cartilage, subchondral bone, joint sheath, and other parts of the body joints. Edema is the accumulation of fluid in the legs that results in swelling, particularly in the elderly and women during the last trimester of pregnancy, as described by Trayes et al. [220]. Edema (Fig. 13(d)) can result in blood clots that block arteries and cause heart attacks.
Edema can occur for many reasons other than heart failure and preeclampsia, such as enlarged and twisted veins, lymphatic drainage blockage, and kidney and liver diseases. However, many patients have lower-limb edema without any diagnosis of illness. Edema must be treated by elevation of the limbs and muscular isometrics to repair arterial drainage. Therapeutic healing is essential and requires diuretic drugs (water pills) to achieve significant results. Fig. 13(e–g) shows other risks, such as obesity, diabetes, lethargy, tiredness, kidney dysfunction, and others that can result from a sedentary lifestyle [221]. Health risks such as heart disease [222] and intestinal ulcers [223] can also result from a lack of physical activity in daily life, as shown in Fig. 13(h and i). There are greater risks of developing cancers, ulcers, and diabetes, especially in those who sit most of the time and do not engage in any physical activity or work. People who eat foods high in sugars and therefore experience increased blood sugar levels are also at increased risk. A sedentary lifestyle can lead to a lack of vitamin D and calcium in the body, weakening the bones and spine and leading to osteoporosis. Other consequences of an inactive lifestyle are lethargy and sleep disorders that affect brain functioning and memory. Knight et al. examined the harmful consequences of bed rest on the body and mind and showed that the risks of changes to the gastrointestinal, endocrine, and nervous systems are increased by lengthy bed rest and immobility [224]. Excessive sitting or lying on bed and not getting regular exercise can increase the risk of several serious health problems listed in Table 4. A sedentary lifestyle can also increase the risk of early death or disability. It would not be an exaggeration to say that the more physically inactive people are, the higher their health risks are.
Table 4.
Possible harms and health risks associated with a sedentary lifestyle and potential solutions using noninvasive e-textile sensor technology.
| Affected body part | Possible harms | Health risks | E-textile sensors solution | Reference |
|---|---|---|---|---|
| Head | Sitting for a long period can cause blood clots (thrombus) inside the brain's arteries, resulting in a stroke. | Increased feelings of depression and anxiety, as well as neurological disorders resulting from a thrombotic stroke causing brain cells to stop functioning and resulting in sudden death. | Sensors integrated into smart textiles can monitor and stimulate brain-related disorders and diseases and can be useful for sleep analysis. | [225,226] |
| Neck | Fluid accumulated in the feet throughout the day can move toward the neck and cause sleep apnea. | Neck muscle stress and pain resulting from disk diseases (such as cervical-region strain, osteoarthritis, cervical spondylosis, and spinal stenosis) and neck injuries (such as whiplash and herniated disks). | Wearable sensor clothing can monitor neck moments and help to reduce neck pain and repetitive strain syndrome by muscle stimulation. | [25,227] |
| Lungs | The risk of a pulmonary embolism (PE) or blood coagulating in a lung artery and blocking blood flow more than doubles if a human sits or lies most of the time. | Shortness of breath, chest congestion, pain (especially during respiration), coughing up blood, and unconsciousness. | An e-textile can monitor the expansion of the chest and hence any deviation in the breathing pattern. In addition, e-masks help to stop virus transmission. | [204,228] |
| Heart | People who live a sedentary lifestyle or do not exercise regularly are at higher risk of death due to diabetes or heart disease than those who are physically active. | Cardiovascular and coronary artery disease, among other risk factors, including obesity, high BP, and high cholesterol. | Electrocardiography (ECG) and e-textiles are based on sensors that can detect chest wall expansion due to breathing and heart beating. | [43,151] |
| Arm and Hand | Lack of physical activity or not getting sufficient exercise can lead to hypertension, high BP, and diabetes. | Stroke, heart failure, and prolonged high BP can damage the kidneys if the blood supply is affected. Chronic rheumatoid arthritis disease that affects the small joints of the hands can also develop. | Wearable e-textile can help in treating and managing arm disabilities. Smart gloves are also useful in the treatment/management of rheumatoid arthritis-related effects on small hand joints. | [229,230] |
| Stomach | Excessive lying or resting contributes to obesity, digestive problems, heartburn, liver dysfunction, kidney dysfunction, and swelling. Enzymes protect blood vessels, keep vessel walls intact, and consume fat to maintain metabolism. | Abdominal pain, obesity, ulcers, and some different types of cancers, such as colon, breast, and uterine cancers. Kidney and liver problems, high cholesterol. | Wearable sensors to detect chest and abdominal respiration help in monitoring and diagnosing stomach problems. E-textiles can help in stimulation. | [164,231] |
| Spinal cord | Sitting for long periods of time with weight on a single point on the spine can result in stiffness of backbone disks and muscle tightness due to constant pressure. Sudden movement can then cause injury. | Unconsciousness, loss of motor nerve functions, such as the ability to tiptoe or heel walk. Disks or vertebrae can squeeze nerves and nerve roots, causing permanent damage. Spine osteoarthritis and ankylosing spondylitis problems recur over time. | Electrically functional stimulated garments are very useful in achieving recovery from spinal cord injuries. | [232,233] |
| Legs | Sitting for a long time causes fluid to accumulate in the feet, ankles, and lower legs. This makes it difficult for the veins to pump blood back to the heart. Varicose veins may result from the accumulation of fluid. | High pressure causes inflammation in the lower limbs and feet. Congestion in the chest contributes to heart failure, a state in which the heart can no longer function well, causing fluid accumulation in the lungs and other parts of the body, such as blood veins. | Compression e-sleeves are useful, together with user input and assessment, in treating knee joint distress or pain. Compression e-sleeves are also useful for reducing knee pain and stimulating muscles in arthritis patients. | [165,234] |
| Feet | Lack of sensation in the legs or lower limbs can be due to poor blood circulation and can cause nerve impairment or stress on nerves if a person takes rests for long periods of time. | Swelling in the feet and ankles. Severe chronic heart and lung illnesses, together with chronic bronchitis and emphysema, raise arterial pressure in the heart and lungs. Heart attacks are very common in such cases. | Smart stockings containing resistive sensors sensitive to pressure for foot motion analysis are also useful in rehabilitation. | [235,236] |
The challenges facing elderly healthcare are becoming increasingly important because of the numerous health issues that are associated with age, as discussed in the previous section. Therefore, current and newly developing wearable intelligent health care techniques are of vital importance. As this review article is intended to provide a comprehensive overview for readers interested in e-textiles, it may contribute significantly to addressing these issues. Using stretch sensors embedded or printed into clothing is smart wearable technology to sense, stimulate and monitor body movements and provide real-time feedback, informing users of a need to adjust or change their posture. For illustration, for those suffering from spinal injuries, preventative procedures are often not sufficient; a more instantaneous and reliable solution might be required. A sensing system incorporated seamlessly into clothing can offer advantages over currently available rigid rehabilitation apparatuses, capturing in-depth body motion and posture data for a new generation of health monitoring and assessment solutions. The high level of sensitivity made possible by soft elastic sensors permit people to monitor body movements at a much more refined level, including movements as slight as chest expansions and the corresponding changes in breathing.
7.4. E-textiles for monitoring physiological signs of health risks associated with physical inactivity
To determine an individual's health status and reaction to external factors, it is necessary to examine and then treat health conditions by analyzing several physiological factors, which can be done with the help of appropriate smart e-textiles. Vital signs such as high temperature or fever, pulse rate, blood pressure, heart rate, and blood oxygen level have been examined using smart e-textiles [237]. Such vital signs can be monitored using a non-intrusive sensor system, typically referred to as a wearable sensing system, for prolonged health monitoring [238]. These devices can detect and collect information about a person's physical condition and movements in real time, painlessly, noninvasively, and without interrupting the person's daily activities [239]. Observation of the physical movements and everyday activities of patients is the main purpose of public healthcare services that provide supportive living environments. Wearable sensing technology plays a very important part in gathering health-related data that can be employed to assess a person's physical condition in real time [240]. As discussed earlier, monitoring can be established based on wearable sensors and actuators linked to home-based systems and can transmit data to health care providers in real time. Wireless sensing systems are being developed to connect sensors to intelligent doorways and healthcare purposes, letting clinicians and doctors monitor information on patients' health conditions remotely. We have summarized most of the functional materials and their uses in the development of e-textiles for various applications, and herein we also provide information on some recent developments in e-textile applications for monitoring, analyzing, and treating various health conditions.
Fan et al. developed a highly sensitive triboelectric all-textile sensor array (TATSA) for subtle epidermic pressure detection [161]. Intertwined electrically conductive and nylon yarns were utilized in a completely packed cardigan stitch shape for sensing use. A stretchy, durable, and noninvasive health monitoring smart e-textile sensing system was developed for the assessment of cardiovascular conditions and sleep apnea disorders. This research demonstrates great progress in the assessment of various prolonged illnesses. In this study, the TATSA was shown to have a high-pressure sensitivity response of 7.84 mV Pa−1, a quick response time of approximately 20 ms, a high cycling stability of more than 100 000 cycles, a high frequency with a bandwidth up to 20 Hz, and more than 40 washing cycles. As shown in Fig. 14(a), two TATSAs were sewn into the sleeve handcuff and chest space of a t-shirt to permit real-time monitoring of arterial pulse and respiration signals. Fig. 14(b) shows the TATSA sewed into a piece of fabric, and the inset shows an enlarged image of the TATSA. The TATSA was made by knitting commercial nylon yarn and the conductive yarn together into a knitted garden using a cardigan stitch. The sensors were sewn into various parts of the fabric to record arterial pulse signals and breathing signals simultaneously. The TATSA sewn into a piece of cloth, a photograph of the all-textile sensor array, and two sensors seamlessly stitched into a sweater are shown in Fig. 14(c). Both pulse and respiration monitoring using this TATSA were more attractive than traditional polysomnography as it can be seamlessly incorporated into clothing for better comfort. Fig. 14(d) shows a stitched white elastic chest strap attached to the human body and fixed over the chest for monitoring respiration. The breathing and heartbeat (pulse) signals detected can be wirelessly transmitted to a smartphone application for health data analysis. These two types of physiological signals (respiratory and pulse) are also recognized as basic indicators of medical conditions. This textile-based wearable sensing system can also be used to observe and detect a person's sleeping patterns and assess sleep conditions. Fig. 14(e) shows a healthy volunteer sleeping while wearing a smart t-shirt integrated with sensors to monitor respiratory and pulse signals that were recorded. The TATSA deformed with the enlargement and narrowing of the ribcage, causing changes in the electrical signals. Low-pass (0.8 Hz) and band-pass (0.8–20 Hz) filters were used to separate the breathing and pulse signals, as shown in Fig. 14(f). Then, the TATSA on the chest was used to monitor breathing and heartbeats signals accurately and continuously, along with necessary physiological data such as the respirational speed, pulse rate, and peak points of the pulse movements. This research presented a method for developing safe, effective, and user-friendly wearable smart e-textiles for monitoring human pulse and respiratory information.
Fig. 14.
(a) Sensors stitched into a t-shirt for monitoring of respiratory and pulse signals. (b) Schematic graphic design of sensor and fabric. Inset: an enlarged picture of the sensor. (c) Photograph of fabric sensors seamlessly sewn into a shirt. (d) Photograph of TATSA positioned on the chest for monitoring pressure signals associated with breathing. (e) Photograph of two TATSAs located on the wrist and abdomen for measurement of pulse and respiration, respectively, while a volunteer is sleeping. (f) Signals as heartbeat and respiratory waveforms. Reproduced with permission [161]. Copyright 2020, AAAS Publications. (g) Schematic design of the textile MEG. (h) Photograph of wearable textile-based pulse sensor as a smart wristband to measure cardiovascular parameters under water without encapsulation for telehealth use. (i) User interface on a smartphone application. (j) Digital photograph showing effects of the use of a wearable textile-based MEG and a magnetic wrist strap on skin rashes. (k) Schematic representation of two ways health data can be transmitted either directly to a doctor for instant medical diagnosis or into the cloud for big data analysis. Reproduced with permission [243]. Copyright 2021, Springer Nature.
Measurement of the heart's contraction rate as a pulse wave is vital for monitoring of cardiovascular syndrome [[241], [242]]. The continuous and precise measurement of heartbeat changes without the influence of sweat and fluidic conditions is critical for customized health care. An interactive textile magnetoelastic generator (MEG) has recently been designed to detect and convert the arterial pulse into electric signals in the context of severe body perspiration for the measurement of self-managed vascular issues [243]. Textile MEG was used to transform the heart's contraction rate into electrical signals with a very small detection limit (0.05 kPa), even in circumstances of severe sweating or underwater submersion without encapsulation. Fig. 14(g) illustrates the smart textile MEG manufactured by interweaving magnetic fibers with electrically conductive yarns. This textile MEG was used for sensing applications, demonstrated by the integration of the textile MEG into a wristband worn against the wrist artery during an underwater dive (Fig. 14(h)). The pulse waveforms generated by arterial pressure variations can be easily monitored by the smart e-textile-based wristband. For ease of use, a customized portable mobile application with a built-in database algorithm was developed and integrated into the smart textile-based wristband. This smartphone application-based wearable wireless cardiovascular monitoring system was used for continuous physiological bodily signs measurements, as illustrated in Fig. 14(i). With the support of the built-in algorithm and data structure, the wearable cardiovascular monitoring system can measure real-time pulse movements and can distinguish among distinctive parameters such as heart rate and present the health data using the phone application. The wearable conformability of the fabric MEG is an essential consideration for long-term pulmonary monitoring. An on-skin assessment was also performed to demonstrate its wearability, as shown in Fig. 14(j). This textile-based wearable MEG was not observed to have any negative impact on the skin when worn for almost a week. It also has some distinct advantages, such as personal health data being processable in two ways. One way is for data to be sent directly to doctors for urgent medical analysis via message, email, or Bluetooth-transmitted screenshot, as shown in Fig. 14(k). The other way is to upload the monitored health data into the cloud by creating a separate and personal health database designed for big data evaluation. Access to this health database can be provided to the doctor when required for health information records-based diagnosis through a legal downloading process. This textile MEG will help to couple e-textile technology with cloud computing to obtain information about an individual's health remotely and wirelessly.
A similar approach has been reported by Roger's research group, who developed wearable and wireless sensing devices for complete body pressure and temperature measurement [244]. The sensors used can be stitched onto clothes to monitor a person's well-being instantaneously, continuously, and noninvasively. Yang et al. developed a user-friendly electronic sleeve (e-sleeve) with an array of integrated printed electrodes for wearable healthcare, particularly for muscle stimulation applications [45]. A fabric electrode array with four functional layers was fabricated using screen printing for use as part of a functional electrical stimulation rehabilitation device. The electrode array of silver and conductive silicone on the e-sleeve was coupled with the control electronics via a 24-way ribbon cord. These e-textiles are very useful in rehabilitation exercises for stroke patients to enable targeted hand motions and repetitive movements. Furthermore, the surface conductors can be used to calculate the myoelectric abilities needed to control the electric properties of muscles through a recording procedure called EMG [245,246]. EMG is used for many applications, such as prosthetic tools, neuromuscular diagnostic assessments, physical therapy, rehabilitation, ergonomics, and studies of people in their working environments, to assess their health and fitness [247]. E-textiles permit monitoring and data acquisition that can directly benefit EMG in real-time and outside-the-laboratory settings to detect neuromuscular deformities in the body. There are many application areas of these electronic textiles, such as muscle condition monitoring, rehabilitation, prosthetics, etc. [153,246,248]. Wearable EMG devices combined with fabric conductors have also been utilized in applications such as trousers for muscle fatigue measurement [249], shorts for power expenditure measurement [246], ventilatory threshold testing [250], spectacles for the study of mastication [251], and a shirt for athletic training. ECG is an approach to biological signal acquisition in which changes in heartbeats are detected using e-textiles supported by conductive electrodes wrapped around the body. This is a noninvasive technique for generating signals and information from variations in heartbeats [252]. EEG is one of the few noninvasive approaches to monitoring brain activities in real time that can be conducted using inexpensive hardware [253]. Newly developed soft conductive fabrics that can function as soft wearable electrodes and can be produced by jet-printing techniques using Ag-ash/fluoropolymer-based nanocomposite hybrid inks can be used in EEG monitoring applications with conductive fabric electrodes attached to the body [254]. The fine measurement capability of textile-based electrodes indicates that e-textiles are feasible candidates for use in EEG, ECG, and EMG recording, which suggests promise for long-term physiological monitoring applications. The design and working principles of e-textiles can be expected to encourage the development of new approaches to manufacturing functional wearable devices for use in health care in the near future.
Fang et al. developed a machine-learning-supported wireless textile bio-monitoring sensing network for continuous and customized cardiovascular system monitoring in the age of the IoT and human–machine interfaces [255]. The sensing system exhibited a signal-to-noise ratio of 23.3 dB, a fast response time of approximately 40 ms, and a sensitivity of 0.21 μA kPa−1. They proposed a flexible, scalable, uniform, water-resistant, and machine-learning-assisted cord-free textile triboelectric pulse measurement sensor with body motion artifacts, as schematically shown in Fig. 15(a). The designed fabric triboelectric sensor for pulse measurement incorporates the triboelectric effects and electrostatic stimulation to transform biomechanical strain into electricity. This sensor was fabricated with flexibility and water-resistance features, as shown in Fig. 15(b). The surface fabric layer functions as both a shielding layer and a water-resistant layer. This self-power-driven textile triboelectric sensor is sufficiently sensitive to detect extremely low pulse sensations for reasonable electrical signals (Fig. 15(c)). The internal encapsulated coating of poly (dimethylsiloxane) (PDMS) is normally employed as a biocompatible and water-resistant layer in biomedical device fabrication [256]. The non-woven textile made of fluorinated ethylene propylene is a negative electron affinity material that is very lightweight and stable [257]. The other triboelectric layer is a single-walled CNTs electrically conductive system that serves as a lead-out conducting probe. A scalable fabrication of the CNTs/cotton film showed high flexibility, as shown in Fig. 15(d). The monodispersed CNTs were loaded on a hierarchically structured cotton fabric using a simple spray coating technique (Fig. 15(e)). The fabricated textile-based conformable triboelectric sensor-enabled cordless biomonitoring system is a substantial work and a step forward in applications for personalized ambulant cardiac or pulmonic health conditions in the age of IoT.
Fig. 15.
(a) Conceptual design of a self-powered textile triboelectric sensor for heart and blood vessel monitoring that transmits data to a mobile phone. (b) Structure of the triboelectric textile sensor. (c) Working mechanism of the triboelectric textile sensor's generation of electricity in response to a radial artery pulse. (d & e) Digital photographic images showing CNTs textile produced using spray coating technique. Reproduced with permission [255]. Copyright 2021, Wiley-VCH GmbH. NIT textile fabrication methodology scheme: (f) Schematic representation of NIT procedure and an NIT-type IC. (g) Real image of a fabricated wearable and flexible NIT on a textile, similar to a typical IC. (h) Demonstration of detected body motion data transfer from the NIT to a personal computer. (i) Wireless data sketch captured by the NIT sensing system. (j) Captured signals (currents) for different situations (nighttime and daytime) for detection of body movements and sweating. The fabric NIT also functions as an alarm in case of emergencies: (k) as a sound alarm for irregular pH value change, indicating light illumination; (l) as both light and sound alarms for unusual pH value change in the dark; (m) as both sound and light alarms for hitting or stretching on the body in dim light or complete darkness. Reproduced with permission [258]. Copyright 2021, Springer Nature.
Yang et al. reported the development of a non-printed integrated-circuit textile (NIT) designed via a weaving method for theranostic and biomedical applications [258]. The NIT device was made with entangled nodes or fibers and then knitted into a bendable textile integrated circuit (IC). The woven circuit textile functioned as a fully self-powered fabric IC for monitoring of biomedical and early caution applications. The NIT-type IC textile is capable of being used as a 24/7 personal artificial intelligence caretaker for regular health checks, diabetes checking, emergency calls, and even COVID-19 patient care. A textile-based wearable sweat sensing system was developed by integrating two types of sensors—one for strain and the other for light—for monitoring health conditions and body movements. As shown in Fig. 15(f), all the electronic components, comprising diodes, solar cells, transistors, sensors, and power batteries, were assembled along with polymer cross-nodes to make a cloth-like sensing system by textile weaving. This cloth-like sensing system was used for sensing, signal magnification, logic computing, data transfer, and continuous power supply. No external power supply source or signal cable was required. The NIT-type IC functional textile was sufficient for continuous 24/7 routine healthcare monitoring and converting data into alarm signals for emergencies. Fig. 15(g) shows a fully developed prototype NIT-type IC textile sensing system with a completely different structure than a traditional printed circuit board-based IC system. The conformable NIT contains an entirely interwoven structure as a self-regulating IC system. The NIT system has been tested and found to perform well as both a wireless physiological monitoring and early alarm system for emergencies indicated by sweating, diabetic conditions, and body movements in the dark. The NIT-type IC sensing textile has potential for use with future on-body artificial intelligence hardware. Fig. 15(h) shows a demonstration of a typical lab setup for testing the NIT sensing textile when attached to the arm. When the textile was touched or stretched randomly, it detected the movements and sent the corresponding signals wirelessly to a home computer nearby. Fig. 15(i) shows the signals recorded by the self-powered wireless NIT textile sensing system and sent to the computer. As shown in Fig. 15(j), the NIT could detect sweating and body movements. The textile sensing system is programmed to logically decode sweating and body movements into light-emitting signals with different intensities for daytime or nighttime. In addition, this textile-type sensor could continuously transform data for body motion, moisture (sweat), and ambient light into electronic signals. Fig. 15(k–m) illustrates practical uses for physiological monitoring. The smart textile can obtain three signals (i.e., sweat, body motion, and light), decode them, and transmit them wirelessly via optical signals to a nearby device/system. A virtual emergency test was conducted to validate the fabric NIT's ability to function as an alarm in case of emergencies. For instance, a sound alarm is emitted for a random pH value change indicating light illumination due to sweats and body movements due to hitting or stretching the body. This work strongly supports the future of e-textile technology and has shown its potential to be used for detection, signal magnification, logic processing, and wireless data transmission as a self-supported sensing cloth with no outside power or data cable connection.
Textile-based conductors and apparel-implanted wearable communication technologies are unique, body-worn, personalizable, and accessible on demand. Recent research articles have demonstrated a common, economically low-cost, and simple operational technique for manufacturing wearable sensor systems on synthesized or even commercial garments. Yang et al. described a typical approach to fabricating soft tactile devices in which the fabric or other similar porous substance is the sensing component, using ionic activation [259]. An ionic liquid (IL) is coated on a synthesized porous film structure or commercial fabric to activate the fabric network for tactile sensing. As a result, a capacitive-type tactile sensor was fabricated with silver nanowires (AgNWs) coated on both sides of the activated surface of the textile, as shown in Fig. 16(a). A wearable textile reacts to external pressure, whereas the coated IL produces electrical signals, as shown in Fig. 16(b). The spongy-type structure works as a flexible structure that helps to improve fast response, which is comparable to the role of a crosslinked elastomer in an ion-gel. Fig. 16(c and d) demonstrates that the sensing region is very sensitive to recognizing the radial vein and the corresponding pulse-wave detection in the form of a change in capacitance. A flexible sensor is a soft capacitor that provides precise information when the sensor deforms or changes its shape due to applied pressure. This is based on the change in capacitance, according to the parallel plate equation [260]:
where C is the sensor's capacitance value, A is the surface area of the sensor, t is the thickness of the dielectric layer, is the absolute permittivity, and is the relative permittivity of the insulator. Thus, the capacitance of the stretchable and bendable sensor is directly proportional to the area of the sensor and inversely proportional to the distance between the bottom and top electrodes or the width of the insulator layer, as follows:
Fig. 16.
(a) Configuration of the sensing fabric activated by IL and biocompatible elargol as conductive electrodes. (b) Digital photograph of a cotton fabric decorated with IL. (c & d) Textile sensing unit integrated into shirtsleeve to monitor radial blood vessel pulse signals at wrist. (e) Drawing of human wearing textile sensors and photographs of textile sensors for detecting physiological signals due to human motions. Reproduced with permission [259]. Copyright 2019, Elsevier. (f) Diagram of as-prepared smart e-textile sensor fabricated with two layers, one of Ag as the base electrode and one as a printed bloom-pattern textile as the superstructure, with production process steps and SEM image of Ag-coated textile surface. (g) Digital image of wearable wireless smart textile sensing device for continuous health monitoring with cardiovascular information displayed on a -smartphone screen simultaneously through wireless communication. (h) Textile-based wireless biomonitoring system worn by an elderly woman and the resultant pulse wave signals. Reproduced with permission [262]. Copyright 2019, Elsevier.
The sensitivity (S) is defined as δ(ΔC/Co)/δP, where Co is the initial capacitance value, ΔC is the relative change in capacitance (C–Co) due to an applied strain/force, and P is the applied pressure [259,261]. The textile-based soft and flexible capacitive-type sensor has a reported maximum sensitivity of 4.46 kPa-1, mechanical stability of 10 000 cycles when compressed or folded, and a fast response time of approximately 39 ms [3]. Thus, considering the benefit of these qualities of high sensitivity, textile-based sensors can be utilized to monitor sensations generated by different physical activities or from physiological signs. Fig. 16(e) illustrates various applications and photographs of the sensing device attached to body parts, such as the wrist, knee, elbow, heel, and chest, for measurements of physical movements such as breathing, artery pulse, and heartbeats. This technique proposes a broad and simple approach to fabricating a high-performing wearable smart e-textile for everyday functional applications, including information collection.
In another application, a wireless and wearable textile-based sensing system with a visual arts layout was fabricated for monitoring various physiological signals for personalized health care applications by Meng et al. [262]. This work is of the highest standard for digitized health systems. A unique self-powered wireless biomonitoring system (WBS) was produced for artery pulse signal recognition and data collection. The gathered data is wirelessly transmitted via an application user interface to a smartphone and saved for the patient's health record. A commercially purchased piece of polyester textile was painted with Ag for conductive layers and to work as triboelectric layers. Second, a nylon yarn was used as an insulator to stitch a round structure 5 mm in diameter on the silver-covered fabric as a support sheet. A printed flower-like smart fabric sensor was configured as shown in Fig. 16(f). The Ag layer was evenly dispersed over the textile exterior, which yielded excellent electric conduction throughout the fabric. The Ag coating process and its SEM image are shown on the right of Fig. 16(f). Fig. 16(g) shows the textile-based sensor device sewn into a t-shirt and into a wristband for wireless pulse signal monitoring application. The wearable sensing system performed continuous pulse movement detection and cardiovascular data collection in real time on a smartphone screen through wireless data transfer. Over more than 80 000 cycles, the sensitivity of the textile sensor did not exhibit any hysteresis over an exceedingly large pressure range of 0.1–9.8 kPa. To validate the practical usefulness and check the sensitivity of the wearable textile sensor for pulse wave detection, the sensor was tested on an elderly volunteer. Fig. 16(h) shows the WBS textile sensing system being tested on an elderly woman and the arterial pulse wave signs being recorded. At this point, the arterial wave pulse applied a tiny force to the sensor attached to the wrist and produced a periodic compulsion. Throughout this process, the arterial pulse movement was articulated in the form of electrical signal formation. As a result, this textile-based wireless sensing system symbolizes a step forward in the fabrication of a body part sensing device for self-managed healthcare in the time of the IoT.
Luo et al. prepared a wearable smart fabric device with several core-shell structures using a very simple dip-coating process [263]. A Ti3C2Tx MXene-based smart textile exhibited an outstanding photo-electro-thermal response and showed excellent temperature and strain sensing performance with a superior thermal coefficient of resistance. The MXene was coated with a polydopamine (PDA)-modified stretchy textile and then PDMS, abbreviated as a PM/PDMS textile. A bendable, breathable, superhydrophobic, smart PM/PDMS textile showed potential application in future-generation wearable electronics. Fig. 17(a) illustrates the manufacturing process and the configuration of smart fabrics. The PM/PDMS textile was placed on human body joints to monitor their movements, as shown in Fig. 17(b). The textile exhibited superior performance and promise for use in various applications, such as detection of body movements and temperature monitoring by photo-thermal heat conversion, as shown in Fig. 17(c). Fig. 17(d) shows the textile working as a smart strain sensor worn on the wrist by a volunteer. The relative resistance (ΔR/R0 = (R-R0)/R0) was used to calculate the sensing performance of the smart strain textile sensor, where R0 is the initial resistance and R is the transient resistance to an induced strain. This smart textile was used to monitor body temperature via the signal sensing s response. Fig. 17(e) shows the equivalent detecting signals in real time when the volunteer bent the elbow from 0° to 90° and the elbow movements were recorded. Fig. 17(f) shows the signals used to monitor the movements of injured hands. The wearable PM/PDMS textile sensor was found to be of significant use to patients during rehabilitation treatment for joint injuries. Furthermore, smart PM/PDMS textiles can be used for sports training by being integrated into sportswear to give real-time feedback. The resultant sensing signals can be recorded when the user performs exercises such as walking and running, as shown in Fig. 17(g). PM/PDMS textiles exhibit excellent performance in providing protection from rain and snow, are efficient at self-cleaning, and ensure user comfort when worn. However, it remains a challenge to extend the upper and lower limits of the cloth sensor and incorporate PM/PDMS textile sensors into fully smart electronic wearable systems.
Fig. 17.
(a) Schematic diagram of fabrication methodology and structure of PM/PDMS textile. (b) Sketch of PM/PDMS textile on body joints for motion detection. (c) The PM/PDMS textile exhibits excellent performance as a smart strain sensor for several potential applications. (d) Photograph of textile sensor worn on the wrist of a volunteer and illustration of bending textile. The textile sensor captures signals for monitoring (e) elbow bending, (f) fist clenching, (g) walking and running. Reproduced with permission [263]. Copyright 2020, Elsevier. (h) Sketch illustrating (MA)n-type hydrophobic fabric and its use for monitoring human sweating. (i) Optical images of pristine silk and (MA0.3)10F silk. (j) Schematic illustration of MAF silk monitoring of moisture due to sweating. (k) Relative resistance change for MAF silk. The inset shows the moisture response and recovery time. Reproduced with permission [264]. Copyright 2019, Wiley-VCH Verlag GmbH & Co.
A study by Liu et al. [264] highlighted functional applications of electromagnetic interference (EMI) shielding and moisture (humidity) monitoring. They used a vacuum-assisted LBL assembly technique to make a superhydrophobic and electrically conductive silk fabric. The leaf-like nanostructure produced consisted of AgNWs as the extremely conductive skeleton-type structure of layers (the frame) and transition metal Ti3C2-based MXene nanosheets as the lamina. Fig. 17(h) illustrates a multifunctional silk textile (MAx)n that is responsive to moisture and effective in the detection of sweat from the human body. In the (MAx)n designation, M and A represent MXene and AgNWs, respectively, x represents the AgNWs concentration measure, and n represents the repetitive numbers. Fig. 17(i) shows the pristine silk and pore shape that support the (MA)10F (or MAF) silk with exceptional gas penetrability. The silk (MAx)n textile demonstrates a low sheet resistance (0.8 Ω sq−1), excellent EMI shielding efficacy of 54 dB in the X-band at a low thickness (120 μm), and extremely sensitive humidity reactions. The high sensitivity to moisture allows the MAF silk to detect nose and mouth breathing and monitor trace amounts of moisture for a very intense mouth breath or sniff. Thus, the MAF silk can be used for several purposes that require monitoring deviations in humidity due to the human body (i.e., sweating levels), provided that in situ factors signifying the human health of several people having special conditions (Fig. 17(j)). This MAF sensing textile works on the simple principle that when the humidity or wetness increases, the resistance change increases in a similar way. Fig. 17(k) shows a cyclic test of the MAF silk with steady and repeatable resistance changes, which demonstrates intriguingly sensitive consistency and endurance to humidity. The inset of Fig. 17(k) shows a very low response time of 5 s for humidity sensing and a recovery time of 80 s for the MAF silk textile sensor. This multifunctional fabric has potential for exceptional long-term stability in smart wearable textiles for humidity monitoring and EMI shielding with quantitative data collection for statistical health analysis.
7.5. Complications caused by skin disorders
The skin is one of the largest organs of the human body. It functions as an integumentary system that protects the interior of the human body and holds all component parts together. Various skin diseases affect millions of people worldwide, including children [265,266]. Based on WHO reports, skin diseases are common and spreading worldwide and require immediate medical care [267]. There are numerous skin conditions, such as acne [268], keratosis pilaris rubra (KPR) [269], urticaria [270], and eczema [271], that occur commonly in children and adults, as shown in Fig. 18(a–d). Common skin conditions include skin cancer, moles, acne, eczema, hives, keratosis pilaris, impetigo, warts, seborrheic dermatitis, varicella, rosacea, psoriasis, and vitiligo [266,272]. Any kind of skin disease can be temporary or permanent; some may be due to environmental causes, whereas others may be genetic. Some skin conditions are minor, whereas others are more serious and can be life-threatening. The number of cases of skin cancer has been increasing as the world's population increases. According to world rankings produced by WHO, the World Bank, and UNESCO, deaths due to skin diseases rank 53rd, with an estimated 111 178 total deaths per year, and deaths due to skin cancer rank 55th, with an estimated total of nearly 10 thousand per year [267]. Skin conditions put a huge burden on health care systems globally, and thus prevention of skin conditions should be prioritized.
Fig. 18.
(a) 24-yr-old female with Fitzpatrick skin acne. Image adapted with permission [268]. Copyright 2014, Authors and Scientific Research Publishing, Inc. (b) A patient with KPR. Image adapted with permission [269]. Copyright 2008, Elsevier. (c) Patients with giant hives (urticaria), Image adapted with permission [2270]. Copyright 2012, Bpac NZ. (d) Eczema on feet of 10-yr-old child. Image adapted with permission [271]. Copyright 2006, MJA Wiley & Sons. (e) Infant with jaundice. (f) Pressing the skin aids in recognition of the yellow color of jaundice. (g) No jaundice sign on the chest while pressing. Image reproduced with permission, update, 2013 [273]. (h) Applications of LED light for the brain, heart tumor, retina, and wound. Image adapted from Ref. [276]. Copyright 2012, Authors and Dove Medical Press, Ltd. (i) Schematic representation of varying depths of light penetration in tissue. Image adapted from Ref. [279] Copyright 2022, MDPI. (j) Skin structure. (k) Usual wound dressing. (l) Wound structure. Reproduced with permission [285]. Copyright 2022, Authors. (For interpretation of the references to color/colour in this figure legend, the reader is referred to the Web version of this article.)
A skin issue that arises in newborn babies is neonatal hyperbilirubinemia or neonatal jaundice, which causes yellowing of the skin and other tissues and may cause death if not treated in time. Around the world, especially in low-income countries in Africa and South Asia, newborns continue to die from complications of jaundice not treated with phototherapy. A newborn infant suffering from neonatal jaundice disease is shown in Fig. 18(e–g) [273]. Failure to prevent neonatal hyperbilirubinemia has unavoidable consequences, including newborn deaths, and many other children survive but grow up with related disorders [274]. Phototherapy is a therapeutic treatment involving exposure to light of different wavelengths to treat skin conditions such as newborn jaundice (icterus), actinic keratosis, psoriasis, and acne and accelerate tissue repair.
There are several ways to prevent skin diseases, but light therapy is the most ancient and is also simple and cost-effective. Light has been used as a therapeutic and diagnostic tool for centuries, with some of the initial applications being sunlight as therapy for skin diseases in ancient China, Egypt, and India [275]. Phototherapy, the controlled exposure to specific wavelengths of light to treat various skin diseases, has led to the development of the field of light-based therapies for the brain, heart, retina, and tissues of the human body. Light therapy stimulates the natural healing control of the cells of the body. Phototherapy has also been used to treat neonatal jaundice and various brain, retina, and skin diseases, including acne, eczema, cancer, neuropathy, seasonal affective disorder, other skin disorders, wounds, and tumors [276,277], as shown in Fig. 18(h). Lifeguard LED blue light phototherapy treats newborns with neonatal jaundice [278]. Wavelength selection is very important in light therapy because different light wavelengths have different penetration depths into human tissues [279]. Fig. 18(i) shows the light penetration effect on the human body with increasing wavelength from blue to red. The change in wavelength is correlated to different therapeutic effects on the human body [5,79]. The range of wavelengths involved does not damage skin tissue, unlike UV light [79]. LED therapies and their advantages are summarized in Table 5.
Table 5.
LED colors and corresponding wavelengths used for skin disease treatments.
| LED Color Therapy | Wavelength (nm) | Skin Diseases Treatment | Reference |
|---|---|---|---|
| Red | 663, 660 | Wound healing, acne, allergic rhinitis, incisions, venous ulcers, etc. | [280] |
| Blue | 415, 470 | Acne, wound, skin disorder, cancer, etc. | [281] |
| Blue | 400–500 | Most effective in treatment of neonatal jaundice in newborn infants | [282] |
| Red/Orange | 620 | Acne treatment, anti-inflammatory/wound healing | [280,283] |
| Green | 500 | Redness and rosacea etc. | [278] |
| Cyan | 490–520 | Acne, inflammation, contraction, redness, oily skin, rosacea, etc. | [277,284] |
7.6. Muscle pain and skin wounds health ailments
Another health issue is skin wounds due to cuts, grazes, infections, and underlying medical conditions such as diabetes that cause skin lesions [176,[285], [286], [287]]. Fig. 18(j-l, respectively) shows the skin structure, conventional wound dressing, and types of skin wounds [285]. There are different types of wound treatments, such as broken full skin flaps and grafts, skin expansion practices, and epidermic replacements. Skin injuries are among the major physical conditions affecting the everyday lives of millions of individuals around the world. Everyday injuries and muscle pain due to stretching of the body become prolonged health issues and may even lead to mortality if not cured in time. According to a 2021 report, chronic wounds affect the well-being of approximately 2.5% of people in the United States, and wound control has a large economic impact on the health care system [288]. The resulting burden is significant, affecting more than 40 million people worldwide and costing healthcare systems approximately US$ 1 billion annually [289]. The substantial loss of progenitor cells and, more significantly, the loss of skin tissue change the biological healing process and stop the formation of granulation tissue because of coagulation necrosis of damaged tissue. New and smart multifunctional wound dressings and bandages have been developed to meet this medical need. Some wounds cause damage to a depth greater than the threshold skin thickness for recovery by the natural self-healing process. In addition, some wounds that develop over a threshold diameter can cause death in patients whose skin's self-healing ability is chronically impaired. Chronic wounds are not easy to treat because they do not follow the typical injury healing process. A long-lasting inflammatory response causes collagen to be accumulated to a greater degree than in the usual healing process. Therefore, chronic wounds can cause serious cosmetic abnormalities arising from excessive damage and functional deficiencies. Currently, the best method for skin-related injury treatment is to provide a temporary solution using a noninvasive smart wound dressing or skin graft, which provides basic mechanical and biochemical cues to accelerate the healing process.
Some other health conditions, such as reduced blood flow, can cause unpleasant symptoms, such as stiffness, pain, muscle cramps, impassiveness, and coldness in the body. Improving blood circulation and relieving muscle pain can also be accomplished with wearable thermotherapy. Recent progress in the development of smart wearable textile-based thermotherapy solutions for monitoring wound healing and curing are discussed next.
7.7. Fibers-based e-textiles for light therapy treatments of skin ailments
Light emission is a very stimulating function that can be integrated with textiles for different applications. Light-emitting devices can be fabricated on fibers and planar textiles in the form of alternating-current electroluminescent devices [28], organic light-emitting devices [290], and light-emitting electrochemical cells [291]. Although various technologies can be useful for light therapy, electroluminescent fiber-based therapy is the main focus of this review. In recent years, fiber-based smart textiles have been developed and used for the treatment of various diseases. Wavelength selection is a major consideration in light therapy treatments (Table 5), as the change in the light wavelength modifies the light penetration into human skin tissues [281,292]. Electronic skin (e-skin) light phototherapy devices are capable of providing emission spectrums targeted for the treatment of a specific skin disease or disorder with variable intensity and lower heat output than conventional phototherapy devices. Thus, the current progress in research on the fabrication of wearable light-emitting devices for e-skin application will be very advantageous over conventional light therapy technology. A panel of multiple lights can be directly laminated over human skin to make it more effective and achieve deep penetration into skin tissues. This new bio-integrated, flexible, and bendable e-skin light source can deliver light to tissues with bright intensity, a fine wavelength band, and greater delivered irradiance. Textile-based phototherapy systems can make light-emitting therapy more efficacious than currently available conventional or LED phototherapy systems, resulting in more rapid decreases in serum bilirubin, shorter phototherapy sessions, and fewer exchange transfusions. The new bio-integrated e-textile light therapy may also be more economical because of the long lifetime of the light source and lower energy consumption. The fabric-enabled light pixels for displays and position-sensitive functions are a pathway for e-skin and e-textile applications [70]. The wearable prototypes can not only support skin treatment but also address the issues of stigma and social acceptance for those who suffer from skin-related ailments [173,174]. It seems that little progress has been made in this area of the development of e-textile light therapy systems. A few of the current prototype product developments are discussed in the following section. The light-delivery therapy system should be fabricated using biocompatible polymer materials (both synthetic and natural) to control the light penetration into tissue and maximize its efficiency. In contrast to conventional light remedy sources, which are easily peeled off from the skin immediately after use, a biocompatible therapy source could be employed for light supply for a long period of time and must not be separated as they remain slowly reabsorbed by the skin tissue. It must be soft, wearable, and bio-integrated with a multi-color panel that can be layered over the skin. It must be cost-effective and affordable and create new opportunities for e-skin, light-emitting devices, biomedical treatment, and tactile sensing areas.
A recent study by Mordon et al. reported the development of a light-emitting fabric (LEF) for use in photodynamic therapy (PDT) to treat skin lesions and prevent skin cancer [293]. This study introduced a new technique for the use of laser light to create a wearable and flexible LEF for in vitro cell treatment or in vivo PDT for large-scale skin damage. The technology is based on the use of optical fibers, which can transmit a ray of light from a light-reactive source into a medium by a series of total internal reflections [294]. The textile shown in Fig. 19(a) is a bundle of optical knitted fibers that is assembled and bonded in a bundle of metallic texture connected to a laser light source through beam expanders. Optical fibers are typically woven as conventional yarn according to various satin weave structures along the fabric's length to control light emission [152]. Fig. 19(b) shows an LEF device made using the knitting method and linked to a red laser light source (635 nm), along with a 3D illustration of irradiance dispersal across the LEF exterior (Fig. 19(c)). Fig. 19(d) shows the LEF, which can emit a range of different wavelengths from violet to infrared (400–1200 nm). This wearable LEF was used for PDT to prevent skin disorders, as shown in Fig. 19(e). The procedure involved a 30-min incubation with methyl aminolevulinate (MAL, a topical photosensitizing agent used in PDT) followed by 2.5 h of irradiation with a light-emitting textile-based device. Because of the short incubation time, the wearable LEF can serve as an almost painless, fully year-round substitute for traditional PDT, which involves the use of a rigid LED board for ∼3 h after MAL application for 10 min and irradiance of 75 mW/cm2. The various applications of this wearable LEF for neoadjuvant or photodynamic therapy demonstrate that it is highly suitable for large-area homogeneous illumination. Photosensitive fibers can emit light at wavelengths from 400 to 1200 nm, which permits the linkage of the LEF to different laser lights involving the beam spectrum of each photosensitizer applied for therapeutic applications. This is a new and unique technological development in the area of e-textiles for the use of LEF within voids (cavities), such as pleural and peritoneal voids.
Fig. 19.
(a) An illuminated LEF device coupled with a laser source applies light to both sides of woven optical fibers. (b) Photograph of fabric device before connection with the laser light source. (c) 3-D image of light dispersal across the LEF surface (d) Light-emitting fabrics emitting light of different colors (blue, green, red, and white) with different wavelengths from violet to infrared. (e) Photograph of photodynamic therapy to treat actinic keratosis using a POF-based light-emitting textile at 635 nm. Reproduced with permission [293]. Copyright 2020, Authors and LEY-VCH Verlag GmbH & Co. (f) Light intensity and a demonstration of a LED light pixel embedded into clothing from both sides. (g) Photograph of illuminated fabric wrapped around a teddy bear. (h) Photograph of illuminated fabric on baby's body to cure neonatal jaundice by blue light emission. Reproduced with permission [152]. Copyright 2017, Optica Publishing Group. (i) Photograph of photodynamic therapy treatment of actinic keratosis. Reproduced with permission [295]. Copyright 2014, Elsevier.
Other wearable fabric light therapies for neonatal jaundice treatment are anticipated. A study by Quandt et al. described the production of a uniform radiant fabric from polymer optical fibers to work as a soft, wearable, durable phototherapy device [152]. Polymer optical fibers (POFs) have been used for several healthcare and fitness applications, and the interweaving of POFs has been explored for the treatment of neonatal jaundice. The light-out coupling intensity of the LEDs across the textile is illustrated in Fig. 19(f). The inset of Fig. 19(f) shows the conforming brightened woven light pixel fixed in a piece of fabric on both sides for clear visual support. Fig. 19(g) shows a piece of light-emitting fabric wrapped around a teddy bear to demonstrate the flexibility of the developed weave. This is an example of lighting-LED-enabled fabric with great potential that can be used in the treatment of jaundice in neonatal infants. The textile exhibited a highly consistent light intensity with a minor deviation of approximately 4% over the whole fabric. In this study, a melt spinning method was used to combine the optical and automated characteristics of POFs. Fig. 19(h) shows the light-emitting e-textile being used to treat jaundice in a newborn infant's skin. The researchers previously developed a knitted light-emitting textile using a modified cloth interweaving loom and achieved results equivalent to clinical results for a conventional LED system for therapy [295]. Fig. 19(i) illustrates the lighted fabric wrapped around a patient's scalp for photodynamic therapy to cure an actinic keratosis skin condition. This work showed that soft, flexible knitted light-emitting wearable fabric achieves flexibility and comfort levels that are not achievable with conventional rigid light therapy systems.
Scientists from Empa, the Swiss Federal Laboratories for Materials Science and Technology in St. Gallen, Switzerland, manufactured a luminous textile that they interwove with light-conducting optical fibers to produce a very precise wavelength of therapeutic light [296]. This woven e-textile fabrication technique permits uninterrupted treatment at home or in hospitals in the presence of family members or caregivers. This is a portable and wearable device that can be very useful in the treatment of neonatal jaundice. This luminous fabric could be an asset to healthcare systems for newborn babies and lessen the economical and societal burdens of their care. Various skin diseases can be treated using wearable light therapy with different wavelengths, as summarized in Table 5. One approach involves embedding LEDs into clothing, and another involves the use of illuminated fiber. Laser therapy, an innovative approach to controlling discomfort and speeding up soft tissue healing, is considered the most effective therapy for curing various skin conditions [297]. However, the light produced by these methods can be weak (high wavelength) compared to light produced by a laser (lower wavelength) because of its indiscriminate and extremely strong light intensity. Recently, Texinov Medical Textiles has developed a knitted fabric that projects high-intensity laser light directly onto the body to cure skin diseases [298]. The device contains tightly packed woven optical fibers connected to an external laser light source for illumination and then wrapped around the body for treatment of skin-related conditions. The light initiates a reaction between a photosensitizer cream and oxygen in the air that makes the skin more sensitive to the phototherapy process. The softness and flexibility of the light-emitting textile help it to adhere firmly to the skin that needs to be covered to treat skin diseases and injuries.
7.8. Wearable e-textiles as therapeutic treatment in skin wound-healing and pain relief
Near-infrared LED phototherapy has been reported to relieve body pain, accelerate wound healing, and improve tissue restoration through various mechanisms [299,300]. Blue light stimulates the production of nitric oxide on the skin, relieves muscle soreness, and improves blood circulation, which results in pain relief. Infrared sensors could be used to prevent any hazardous exposure of the skin or eyes. This device is reported to be safe to use at home, as it does not release any harmful radiation. Many clinical studies are ongoing to measure the healing power of the technology. Protection and comfort are priorities for the manufacturers, who see significant market potential for wearable light-emitting e-textiles. Recent studies have shown that smart textiles are very useful in wound healing and bacterial ablation when applied to wound areas. However, information is limited regarding the safety and suitability of smart textiles, which are electrically excitable cells, for in vivo wound healing. Thus, this section highlights the use of smart fabrics in wound healing applications.
Zhao et al. developed a multifunctional smart textile by coating two-dimensional (2D) Ti3C2Tx MXene nanosheets onto nonwoven cellulose fiber fabric using a distinctive MXene-cellulose fiber structure [176]. The Mxene-decorated textile had an exceptional Joule heating impact, killing bacteria around a skin wound and thereby speeding wound healing. Fig. 20(a) shows the conductive MXene-decorated nonwoven fabric (M-fabric) and an infrared (IR) image under an applied voltage of 4 V prior to heat therapy application. The M-fabric was prepared by dip coating Ti3C2Tx nanosheets into an MXene dispersion. When the voltage is applied across the M-fabric, it generates heat, and the surface temperatures can be easily captured by a thermal imaging IR camera. In in vivo infectious wound healing experiments, the generated heat is transmitted to bacteria-contaminated skin for therapeutic bacterial ablation. An M-fabric was also integrated into a wearable neck-guarding pad and tested on a person's neck for thermotherapy purposes, as shown in Fig. 20(b). The heat produced spreads across the neck-protecting pad and radiates into the epidermis. This can even stimulate hypodermic tissue (the bottom layer of skin) to minimize cervical spondylosis toughness, boost blood flow, and alleviate muscle pain. Fig. 20(c) shows the M-fabric on a volunteer's neck in an application of thermotherapy: generating heat to relieve body pain. The wearable M-fabric is exceptionally durable, regardless of the position of the head. We conclude from the results of these studies that conductive textiles offer potential advantages in safe and convenient health care and therapeutic treatment.
Fig. 20.
(a) Digital photographs of MXene-fabric (40 mm × 10 mm) and corresponding IR thermal image at 4 V showing the heating characteristic. (b) Illustration of thermotherapeutic use of soft M-fabric integrated into neckpad on a person's neck. (c) Digital image of the use of an M-fabric-integrated neckpad with thermal IR images for different head postures. Reproduced with permission [176], Copyright 2020, American Chemical Society. (d) Illustration of a thread-based patch with a thermoresponsive hydrogel layer painted on a soft and wearable fabric-based electric heater. The inset shows a picture of knitted functional threads as a patch attached to a volunteer's hand. Reproduced with permission [301]. Copyright 2017, Wiley-VCH Verlag GmbH & Co. (e) Schematic illustration of PEDOT-PDA-mSF patch development. (f) Schematic illustration of mSF patch use for diabetic wound therapy. Reproduced with permission [177]. Copyright 2021, Wiley-VCH GmbH.
Very recently, Mostafalu et al. fabricated a self-operated wireless wound patch based on a basic electric heater principle, using fused fibers coated with a layer of cross-linked hydrogel containing a thermoresponsive drug [301]. The fibers were loaded with different drugs, including biological agents, and then combined using the fabric to construct a bandage-type wearable wound dressing. Fig. 20(d) illustrates the fabrication process and the wound dressing applied to a hand. The wearable wound dressing pad is coupled to a microcontroller unit to wirelessly transmit the information to a portable device nearby (such as a smartphone). A simple textile-based microheater is made with cotton yarns that are dip-coated with carbon ink so that they can be used as an electrically functional conductive substance. The estimated resistivity of the electrically conductive yarns (1.2 mm in diameter) was very high (5 Ω cm−1). The conductivity of the main yarn was sufficient to transmit electrical power and disseminate heat rapidly and consistently. A wireless smart textile device was designed using electrically functional threads for chronic wound therapy. This wearable textile patch could be very useful in the future in treating skin-related diseases.
Jia et al. reported a conductive silk microfiber (mSF) integrated with a bioelectronic smart electronic patch for the treatment of diabetic wounds (which typically are slow to heal) by decreasing infection and controlling oxidative damage [177]. Fig. 20(e) illustrates the fabrication process for the conductive mSF patch. A conductive and flexible mSF was extracted from unprocessed silk fiber using an extraction–protection procedure and deposition of PDA and PEDOT on the surface of the mSF. PDA was used to protect the structure of the mSF during the extraction process. Fig. 20(f) shows that the PEDOT–PDA–mSF patch was effective in diabetic wound healing. Furthermore, the PDA embedded in the mSF patch was effective in preventing cell/tissue affinity and cohesion, which improved cell attachment and replacement. All of these effects synergistically contributed to countering damage to the skin and ultimately led to effective results. New cell/tissue and blood vessels reformed on the surfaces of a wound during the healing process and led to diabetic wound shrinkage. Ion summary, electrically conductive mSF as a biocompatible element could be very useful for smart e-textile technologies for diabetic wound healing. This research explored a new application of silk used as a reflexive element to manufacture biocompatible wearable devices.
A research team from Empa in Switzerland has developed a high-tech wearable device to supply relevant data to medical staff about skin wound conditions [302]. Their biomimetic e-textile bandage with an integrated glow sensor provides continuous and real-time information about the state of the recovery process without the need for removal and replacement of dressings. This treatment reduces the workload of medical staff and hence lowers expenditures. The textile-based electronic bandage (e-bandage) with glow sensors alerts the medical staff when the skin wound has healed considerably. The use of these novel soft bandages allows even chronic wounds to be monitored at home by self-care management. Once a wound has cured, the body generates specific constituents in a complex cycle of biochemical practices that indicate substantial changes in several metabolic factors. For example, the volumes of oxygen and glucose in the body fluctuate depending on the stage of the healing process, and similarly, the skin wound's pH level changes [303]. Sensors in the textile shine with a distinct intensity if the pH level varies. The pH level in the skin wound can be confirmed without removing the dressing, and the healing process can continue without pause. Similar work has been done by Gokarneshan on contemporary wound dressings integrated into medical textiles using active compounds that stimulate wounds while protecting against infection [304]. In this study, an electrospun skin wound bandage was studied, and the electrospinning technique was established as an effective approach for the manufacture of nanoscale fibrous bases. All the literature discussed above supports the idea that wearable light therapy can be more efficient than a distant light source in treating skin-related diseases. In the future, illuminated e-textiles will find wider use in wearable light treatment. Thus, it is expected that the combination of sensing and lighting of e-textiles could increasingly be used in medical health applications in the coming years.
8. E-textiles in sports for training assessment and injury physiotherapy
Athletic activities such as running, jumping, and throwing are the basis of many sports, such as hockey, football, volleyball, basketball, and others. While performing these activities, athletes can get injured and need feedback to recover. Analysis of training and rehabilitation data plays a very crucial role in providing feedback and supporting communication between trainers and athletes to aid in injury recovery and fitness improvement. Inertial devices are used extensively in sports for training analyses and personalized rehabilitation [305,306]. Athletes and sports mentors are very eager to achieve improvements and are always looking for an edge, and motion-sensing technology incorporated into workout clothes can provide an exciting incentive [307]. The use of motion detection technology by sports professionals has until recently been limited to sports performance arenas. However, progress in low-power electronics and sensor technology has made it feasible to generate motion-tracking e-textiles for athletes to use in practice wherever they choose to train. These scientifically improved e-garments can be used in typical sporting and training environments to deliver a complete picture of body gestures and even provide real-time feedback. The data obtained can benefit athletes in learning to execute athletic behaviors that improve their performance consistently and repeatable. In this section, we cite some recent progress in the manufacturing of e-textiles, mostly prototypes, that may be very useful in rehabilitation to overcome joint-related injuries and improve fitness.
Knee injuries are very common, and almost 50% of them are associated with sports and training. Such injuries can be very expensive for athletes in terms of recovery time and economic impact [308]. Wearable technology could be very useful for monitoring an athlete's recovery progress and consistency in performing recovery procedures [309]. Recently, Watson et al. reported the development of a soft stretchable conductive fabric sensor called TracKnee to monitor knee movements [162]. TracKnee is a very useful wearable for tracking injured knee movement and obtaining data that can be used in the rehabilitation process. The main components of this wearable device are a non-washable electronic microcontroller that serves as a control patch, electrically conductive threads, a power supply, a Bluetooth chip, and several electronic components necessary for circuit completion.
Tian et al. reported on an e-textile that functions as a strain sensor for human motion detection in real time for data acquisition [178]. Fig. 21(a) illustrates the fabrication process for a new printed smart e-textile using water-based conductive ink composed of silver fractal dendrites (Ag-FD). The e-textile sensor was made using a screen-printing technique to print a water-based conductive Ag-FD ink directly on the textile surface. Next, the as-printed e-textile was spray-coated with an invisible water-resistance additive. This invisible waterproofing agent exhibits excellent elasticity, water repellence, ease of wear, abrasion resistance, and air permeability. The printed e-textile exhibits a very high conductivity (sheet resistance of 0.088 Ω sq−1), superior stretchability of more than 150%, and outstanding stability for 1000 cycles at 100% stretchability. This e-textile has been employed as a strain sensor to monitor real-time human motions in everyday life. As a proof of concept, this aesthetic smart clothing for practical use was tested on a human body for motion monitoring through induced relative resistance change (△R/R0). The functional sensor textile was used to detect the body motions of a person as he raised and lowered his hands, as shown in Fig. 21(b). In physical training or exercise, this e-textile can capture the motion patterns (e.g., barbell lifting) of a volunteer to monitor different walking states of humans (Fig. 21(c)). The data gathered during such exercises could be very useful for analyses of body movements to achieve improvements. The smart e-textile may offer new possibilities in terms of the manufacture of motion-sensing soft and wearable electronics and smart apparel for commercial applications in the near future.
Fig. 21.
(a) Schematic illustration of printed smart and wearable e-textile sensing clothes and fabrication procedure for custom-made design. (b) Calculated relative resistance changes from signals sensed by smart apparel as a volunteer moved his hands up and down. (c) Real-time monitoring of human movements with smart outfit during states of rest, slow walking, fast walking, and running. Reproduced with permission [178]. Copyright 2022, Wiley-VCH GmbH. (d) Schematic illustration of Ag-coated e-textile strain sensor attached to human body for real-time sensing and data collection on decisive muscle movements. (e–g) Images of fabric sensors on different parts (joints) of the body. Curve of resistance changes in real time during walking and knee movements. Reproduced with permission [163]. Copyright 2017, Wiley-VCH Verlag GmbH. (h) Structure of a pressure sensor matrix plan and its application in sport/training for detecting user postures. (i) Demonstration of gym training performance monitoring using sensor matrix for different exercise situations. Adapted with permission [311] Copyright 2016, Elsevier.
In continuing progress in e-textile technology, Li et al. presented a flexible and stretchable e-textile device to monitor and analyze the kinesis of the human body [163]. In this work, a silver-coated polyester textile was developed using an electronic dyeing process at a low temperature for in situ diminution of an Ag antecedent into nanocrystals. The e-textile exhibited good elasticity and adaptability and excellent response in capturing body movements. This type of e-textile could be used to observe many human activities and recognize similar movements, with potential applications for physiological monitoring, soft robotics, and human–machine interfaces. Fig. 21(d) presents the schematic design of the e-textile, which demonstrates good stretchability and is easily affixed to different human body parts for motion detection [310]. A multichannel recorder is used to detect body motion and manage the information collected. To validate the sensing data collected by the e-textile device, as shown in Fig. 21(e), a strip of the e-textile sensor was tested on the top of the heel and upper and lower knee of a volunteer to track movements during physical activities that involve different limb activities, such as walking, running, and other body movements. The sensors from the different joints produce different resistance responses, as shown in Fig. 21(f), which indicate the strain change of the equivalent position throughout the motion. As Fig. 21(g) shows, the movements of a joint, such as the knee of a volunteer, produce different resistance responses during different movements, such as relaxing, squatting, walking, jogging, jumping, and stretching. As a result, specific joints can be associated with separate or collective response changes that occur due to joint movements, and the data can be used to compare the knee position of an individual with the positions of other knees. The authors reported that this e-textile sensing device can be manufactured on a big scale and can measure fine resistance changes that occur during bends or twists. This e-textile sensing device offers encouragement for finding solutions necessary for healthcare system improvements, athletic training, and rehabilitation. Furthermore, the complex and combined sensing data assessment process would be very useful in accelerating the detection of different modes of activity by multipoint wearable smart sensors [18].
In a study by Cheng et al. on a fabric-based surface pressure matrix as an innovative, discreet data resource for mapping several activities, such as walking, running, and sitting [311], a simple pressure-responsive component was made by inserting a pressure-complex coating of carbon polymer foam between two conductors. As pressure was put on the sensor, the conductive layers were squeezed, and the density of the conductive material increased, which increased the resistance. This change in resistance is directly proportional to the applied pressure on the sensor and is converted to a voltage by a resistance–voltage converter. The voltage signals can then be digitized by connecting an analog-to-digital converter. The design is based on the idea that the vast majority of human activities are associated with certain kinds of surface contact that can be performed as exercises on a textile-based fitness mat. Fig. 21(h) illustrates a textile-based sensing matrix that enables the realization of surface force for shape propagation through significant spatiotemporal data analysis for a large dynamic range and its use in sports training. To demonstrate this e-textile mat application in sports training, Fig. 21(i) shows a spatial recognition fabric pattern used as a smart fitness center rug that is able to recognize various exercise positions and count repetitions. The researchers stated that these workouts involved synchronized movements of distinct human body limbs that are difficult to detect using a single body-worn textile sensor. This type of smart mat is highly useful for real-time recognition and feedback on fitness and athletic performance. Real-time responses such as those detected by this smart mat could be extremely beneficial in fitness center workouts because the image assessment is based on sensing matrix measurements that can be significantly improved with the help of corresponding recorded data analyses. The data can be streamed to other devices such as smartphones or nearby systems via real-time wireless communication for analyses and feedback. The data can be highly beneficial to athletes in training to evaluate and improve their performance.
To further explore the use of e-textile wearables for solutions in medical diagnostics, games, and human–machine interfaces, Lin et al. studied near-field-enabled textiles [7]. A conventional wireless smart e-textile was developed with power and information connectivity among several distinct points all over the body. Computer-supported stitching of conductive threads was integrated with wearable smart clothing with near-field-reactive designs that were fully fabric made and free from hard electronic modules. The researchers developed this e-textile system for real-time, continuous, multi-nodal detection of temperatures and movements for analyses of human gaits during training or doing exercise. Fig. 22(a) shows the fabric combined with a designed planar coil that functions as a transmitter between physically disconnected positions, made by stitching a conductive cord onto a piece of textile. Standard near-field communication (NFC) allows a gap of a few centimeters between a sensor and a mobile phone, as shown in Fig. 22(b). Near-field communication facilitates communication of information within a range of 1 m. The pattern was designed using design software and then uploaded to an embroidery/sewing machine. The conductive thread was sewn into a cotton–polyester shirt and trousers by a system controller. The connections were made using conductive epoxy and sealed by applying hot glue. In real-time monitoring, they demonstrated constant physiological monitoring by the wearable sensors without an external power supply throughout a workout by a volunteer wearing the near-field-enabled apparel. The application was demonstrated with a healthy volunteer wearing athletic pants and a shirt, both integrated with a near-field relay, as shown in Fig. 22(c and d). Fig. 22(e–g) shows actual images from the data compilation and a comparison of angular speed measurements during walking from sensors coupled with and without wires. The gait cycle time (Δt) determined from both measurement sets using a peak signal detection algorithm showed close agreement through the varying-pace stage, demonstrating that the strain sensor delivers consistent gait data for analysis. The developers emphasized that the data could be employed to calculate pace time differences for use in performance comparisons. In contrast to typical smart wearables or e-textiles in which sensors and electrical circuits are directly integrated into clothing [312,313], near-field-enabled apparel derives its utility from passive near-field signals, does not rely on functional electrical modules that are not suitable for cleaning and everyday wear, and interrelates wirelessly with nearby devices/systems without the need for external connectors that need to be plugged in or unplugged.
Fig. 22.
(a) Near-field-enabled connectivity with a gap of a few cm between the reader and a sensor integrated into a wearable textile. (b) Digital photograph of a smartphone wirelessly supplying power to a sensor node on a relay. Digital images of near-field-enabled (c) shirt and (d) trousers integrated with sensors. Demonstration of workout data measurement with battery-free sensors for comparison of wired (e) and wireless (f) monitoring systems for walking/running that provide strain measurements while connected to a smart mobile phone. (g) Data plotted during the gyroscope phase and strain sensor node. Reproduced with permission [7]. Copyright 2020, Nature Publications. Fabrication steps of knitted sensing wearable. (h) Woven temperature sensor fabricated using graphene-decorated yarns. (i) Wide woven pattern of graphene yarns used in making a temperature sensor. (j) Yarn trail illustration for knitted temperature sensors. (k) Smart t-shirt knitted with textile sensors for sensing the physical state of the human body and transmitting the data to a smartphone application via Bluetooth. Reproduced with permission [164]. Copyright 2019, ACS Publications.
It is essential to develop multifunctional wearable e-textiles that are well suited to applications in healthcare, fitness, training, virtual games, big data analysis, aerospace, fashion, military operations, etc. [314]. Such intelligent wearable clothes could directly interact with the human body and simultaneously sense, capture, and stream data on various physiological parameters, such as heart rate, BP, body temperature, and serum levels of various stress hormones, as well as joint movements and other bodily movements and responses [36,166]. In pursuit of this goal, a study on graphene-built soft, machine-washable, flexible, wearable garment sensors was conducted by Afroj et al. [164]. A graphene-layered knitted temperature textile sensor was manufactured to obtain an intertwined structure created using dual-coated yarns with a Lycra string core and nylon fiber cover, as shown in Fig. 22(h and i). Fig. 22(j) shows the yarn trail of the knitted temperature sensor. The pattern repeats from a few blue knitted sequences to another blue knitted track. Covers of Ag yarn-knitted shapes were similarly gathered on both sides of the woven textile courses of graphene yarns. Radio-frequency identification tag (RFID) technology was used because its “zero power” nature was considered to fulfill requirements such as low price and low-maintenance wireless sensors. Fig. 22(k) illustrates the concept of a smart garment integrated with a knitted sensor and an RFID tag that transmits temperature information to a phone application. The graphene-based e-textile sensing system exhibits superb temperature sensitivity and is washable, stretchable, and very soft. This process for fabricating smart apparel is a significant step forward in producing textile sensor yarns for future wearable electronics applications.
Choudhry et al. [315] reported on an accessible and innovative manufacturing procedure to fabricate wearable textile-based piezoresistive sensors using conductive embroidery threads. The sensors can be easily embedded in wearable fabrics for the measurement of subtle muscle movements and other vital signs, such as body temperature, pulse rate, respiration rate, and blood pressure. The design of the sensor is very simple. It consists of four layers. A sensor attached to the chest can measure breathing patterns indicated by the expansion of the chest during exhaling and inhaling. A sensor attached to the thigh detects muscle motion and can be used to calculate footsteps or detect changes in the hamstring muscle during contraction and extension. Fig. 23(a) illustrates a setup for breathing pattern monitoring and the corresponding resistance–time diagram. Similarly, Fig. 23(b) shows muscle activity monitoring and the corresponding change in resistance. Piezoresistive sensors were formed by embroidery of conductive threads into a textile. The sensors were affixed to the trousers to ensure close contact with the hamstring muscle to precisely measure the muscle's movement during running or slow walking. The trousers were tested on a healthy volunteer moving on a treadmill at a slow pace (1 km/h). The test results confirm that the fabricated sensors were effective in measuring very subtle pressure changes due to muscle movement.
Fig. 23.
Textile-based sensor consisting of four layers (shown in center), (a) breathing rate setup and resistance–time graph, and (b) muscle activity setup and corresponding changes in resistance. Reproduced with permission [315]. Copyright 2020, IEEE. (c) Schematic illustration of fabrication of smart garment with knitted sensing fibers. (d) SEM image of different weaved sensing fibers (glucose, Ag/AgCl) in the textile. (e) Photograph of volunteer wearing a smart textile sensor during running exercise, with data wirelessly transmitted to a smartphone. (f) Results for different sensing fibers knitted into electrochemical sensing fabric as a whole system reference. (g) Comparison of ex-situ data with the in-situ data collected from the sweat samples. Images are reproduced with permission [316]. Copyright 2018, Wiley-VCH Verlag GmbH & Co.
In another interesting study, Wang et al. created an electrochemical textile sensor with the potential for application to instantaneous fitness monitoring [316]. The textile sensor was manufactured by interweaving different types of detecting fibers as the basic structural components [316]. The various sensing fibers were formed by the deposition of active materials onto CNT fibers to form a coaxial shape. Many illustrative physiological indicators, such as glucose, Na+, K+, Ca2+, and pH, were examined to validate the success of the electrochemical textile sensor. Fig. 23(c) illustrates the fabrication of the sensing fiber and the resulting electrochemical textile sensor. Fig. 23(d) shows an SEM image of a fabric glucose sensor made by knitting Ag/AgCl and glucose-sensing fibers into the textile. It has been observed that a textile contains thousands of fibers; hence, several different sorts of sensing fibers can be integrated together. As an application demonstration, five different types of sensing fibers were created to develop an electrochemical textile sensor to detect humid metabolites. As shown in Fig. 23(e), a healthy volunteer wore the sensor garment while running on a treadmill. After approximately 10 min, the sweat generated as a result of the running soaked the fabric sensor, and a real-time study revealed that the signals associated with moisture could be captured continuously. Fig. 23(f) shows the sensing results for different sensing fibers in a knitted electrochemical sensing fabric. The data can be wirelessly received with a custom-developed smartphone application. The results were confirmed by comparison with data from on-body sensors collected from sweat tests conducted subsequently with a volunteer running similarly for approximately 35 min (Fig. 23(g)). The authors stated that this is the first report on any type of electrochemical fabric sensor that can effectively and precisely detect several different types of physiological signals at the same time. This study demonstrates a crucial step forward in the manufacture of smart e-textiles for real purposes. This work initiated a new trend in the development of smart wearable e-textile sensors that could be commercialized for various applications within a few years.
In another exciting study, Wu et al. fabricated an all-textile pressure sensor for monitoring human motion in real time [180]. An all-fabric capacitive-type sensor was produced using typical apparel with intelligent functionalities, including a cordless sensing system. The article explains that the whole-fabric pressure sensor was more appropriate for smart wearable technology than conventional pressure sensors and demonstrated considerable potential for applications as e-skin and in human activity detection. The researchers tested the feasibility of perceptible detection by intelligent fabrics, which were found to exhibit high sensitivity (0.283 KPa−1) and good stability over more than 20 000 cycles). An array of textile sensors was designed to detect and record pressure information spatially. Unlike resistance-type multichannel compression sensors, the capacitance sensor array developed in this study was designed in a sandwich style that combined a planar electric fabric circuit with a coplanar insulator film. Fig. 24(a) illustrates a 4 × 4 pixel sensing array, including a mask-assisted striped conductive silk fabric used for the top and bottom electrodes and a 3D permeated spacer fabric used as the middle non-conducting (insulator) material layer. Fig. 24(b) shows digital photographs of the sensor arrays, electrode arrays, and spacer fabric insulator layer. The water-soluble PVA template-supported silver nanofibers (AgNFs) with very high conductivity and mechanical bendability were coated on the textile surface to act as sensor conductors. AgNFs were coated on the textile's surface using electrospinning followed by magnetron sputtering, consistent with conventional textile technology. Because of the high mechanical flexibility and sensitivity and huge sensing range of the fully textile capacitive-type pressure sensor, it can be easily integrated into garments to monitor body motions such as coughing, arm gestures, finger bending, etc. Furthermore, using an inductor-capacitor wireless electric circuit, capacitance signals data could be transferred to a portable device or to cloud servers through wireless communication (Bluetooth) using a phone application for real-time monitoring, as demonstrated in Fig. 24(c). Fig. 24(d) shows digital photographs and changes in capacitance signals captured using a fabric sensor fastened to an elbow joint bending at an angle of 30°. Once the elbow is bent, the capacitance of the all-fabric pressure sensor increases because the sensor's area changes during bending and more pressure is applied to the sensor, which reduces the distance between two conductive fabrics (C = εA/d). Stitching the fabric sensor onto the sleeve of a sports garment changes the capacitance, and the resulting bending angle can be determined precisely, as shown in Fig. 24(e). The inset in Fig. 24(e) illustrates the capacitance signal detection and communication processing. The study results show that the proposed fully textile sensor is better suited for use in smart textile technology than typical pressure sensors. This work showed broad possible uses in the field of smart textiles for e-skin and real-time motion detection.
Fig. 24.
(a) Illustration of fabrication of fully-textile pressure sensor. (b) Digital images of the textile sensor, including electrode and spacer fabric dielectric layer. (c) Representation of whole smart motion monitoring textile sensing system for detecting bodily movements and transmitting data wirelessly to a smartphone application. Digital photographs and plotted data for variation in capacitance while the user wore the sensing textile on her elbow and bent the elbow at angles of (d) 30° and (e) 60°. Inset of image (e) shows the schematic circuit design for the motion data detection and transfer. Images reproduced with permission [180], Copyright 2019, American Chemical Society. (f) Schematic illustration of fabricated supercapacitor-integrated strain sensor plus a circuit diagram of the whole system, with digital photographs. (g) Conceptual illustration of the integration of whole sensing system sewn into a nylon glove and a t-shirt for detection of bodily movements. Images reproduced with permission [317], Copyright 2019, American Chemical Society. (h) Schematic design of the fabrication process of the mechanical sensor (strain and pressure) using laser-induced technique for the volleyball game and other sports smart electronic wearable garments. Images are reproduced with permission [318], Copyrights 2022, American Chemical Society.
In another study, Park et al. reported a high-performance stretchable supercapacitor for powering a unified strain sensor as a single textile sensing system to monitor numerous physiological signals [317]. This work is a model of a perfect wireless textile-based sensor system for self-powered personalized training and fitness applications. The supercapacitor-based sensor was produced with nanocomposite electrodes using multiwall carbon nanotubes and molybdenum trioxide (MW-CNT/MoO3). In addition, a nonaqueous gel electrolyte, along with the fabric course direction, exhibited excellent and very stable electrochemical performance in static and dynamic bending. This study established the possibility of using manufactured soft and stretchable all-in-one textile sensor systems for real-time health measurement during daily routines. The single sensor system constructed with liquid metallic interconnections was embroidered into clothes to monitor signals from the wrists, elbow joints, fingers, and knees. To evaluate the practical applicability of a single wearable sensor system, a supercapacitor and strain sensor were packed and coupled with liquid-metal Galinstan (GaInSn) interconnections for electric connections. Fig. 24(f) shows a graphic layout and digital images of the integrated structure, along with an electrical circuit diagram. The wearable textile strain sensor can be powered by the stored energy in the supercapacitor. The stretchy textile sensor is embroidered into wearable clothes and can be removed so that the clothes can be washed. The sensing system can then be resewn into the fabric. The wearable textile strain sensor was employed to monitor the wrist pulse and the motion of joints. This strain sensor offers the advantage of being self-driven because of the power saved in the supercapacitor. The integrated all-in-one textile sensing system was stitched into a nylon glove and a t-shirt to measure different biosignals over a long period of time without any interruption to the user, as shown in Fig. 24(g). This research work demonstrates the feasibility of employing the manufactured strain sensor in a compact textile sensing system for real-time monitoring in various sports.
Very recent, Raza et al. reported a textile-based mechanical (strain and pressure) sensor fabricated via laser-induced graphene technology for the detection of various movements for sports monitoring application [318]. The wearable fabric sensor is based on the resistance change between two layers of conductive graphene when the strain/pressure applied during player's body movements. The schematically designed structure of the fabrication process and application of the wearable sensor in volleyball game is shown in Fig. 24(h). This recently constructed graphene-based sportswear sensor system acts four different functions in volleyball game, involving volleyball reception recognition, finger touch foul recognition through preventing or stopping the ball from an opponent player, spike force detection and monitoring the position of a player. This wearable sports outfit integrated with mechanical sensor would be very useful sportswear to assist players and couch during training to prepare their strategies in the games.
9. Current challenges facing smart wearable e-textiles
E-textiles have shown their potential for protection against transmissible diseases, assistance in assessing health conditions, and managing fitness. However, e-textiles have many manufacturing limitations that must be addressed to ensure their reliability and user confidence. Currently, off-the-shelf sensors/devices and electronics are typically used in wearable e-textiles. For example, the use of inertial devices together with advanced electronic and an appropriate algorithm has been a popular solution [319]. Another alternative involves placing a sensing device on a garment directly by embroidery, sewing, or knitting and using a cable connection and power supply [320]. These methods are limited because of issues such as poor adhesion of devices, which results in them falling off easily with physical activity, and the devices being obstructive [321]. These solutions have nonetheless undoubtedly advanced the use of wearable technology in several areas, despite their obvious limitations in relation to health monitoring-particularly because their benefits come at the cost of user comfort. As a result, the adoption of these technologies for day-to-day health monitoring has been negatively affected and, in fact, has already approached the point of diminishing returns. It is critical to find solutions for such end-use issues so that e-textiles can be used to promote and encourage physical activity. Current e-textiles are typically inadequate in terms of consistency and stability during use (e.g., twisting, stretching, washing, etc.) [25,44]. Various research challenges remain, such as meeting market standards, washability, seamless fabrication, low cost, and being self-driven. The seamless integration of sensors and electronics into clothing can achieve a significant step forward for both the fundamental integration of technology and its use. The seamless integration of sensors and electronics into clothes is challenging because of technological bottlenecks such as poor conformability to the body, poor adhesion of off-the-shelf sensors to clothes that results in undesirable noise signals, and reliability issues associated with the integration of electronics into textiles. At the same time, the benefit of overcoming these challenges will be huge. In the next section, we briefly describe the current challenges and technical limitations facing the development of e-textiles.
9.1. Smart wearable e-textiles need to meet the market standard protocol for everyday use
A lack of standardization is contributing to e-textiles being manufactured with flaws that adversely affect their success in the marketplace. Fundamentally, there is a scale to each innovative product that must be matched before promoting e-textile products to end-users [322]. A gap must be overcome for e-textiles to achieve commercial viability. For example, textile technology should employ smart materials and integration without any functional limitations, and technical components (i.e., electronics) should be completely integrated in such a way that they are washable and durable. All e-textiles proposed for commercialization must meet American Society for Testing and Materials (ASTM) textile standards. ASTM provides standards for the physical, mechanical, and compound or chemical properties of fabrics, as well as the natural and artificial fibers used to produce them. E-textiles conforming to these standards are normally manufactured by knitting, weaving, or spinning of fibers, yarn, and sewing threads. These textile standards help to ensure that cloths used for e-textile applications conform to expectations for suitable end-use. This helps designers and manufacturers gain insight into user feedback and contribute to better design, innovation, marketing, and other services. It is, therefore, necessary that all e-textile products meet market standards to ensure their validation and suitability for user applications.
9.2. Seamless integration
The technology shift from rigid to soft materials brought about revolutionary changes in all manufacturing sectors, including textiles, but the miniaturization of electronics and nanotechnology made wearable systems more achievable. This allows materials layers and electronics to be simply integrated into textiles via either printing or weaving techniques. As stated previously, seamless integration could be more efficient than sewing or embroidering. Conventional e-textiles with distance wiring, separate electronics, and power source are technical limiting factors that affect sensor accuracy and data privacy [[44], [323]]. In addition, the e-textile must be lower weight for portable sensing, stimulating, and phototherapy wearable devices than existing bulky and off-the-shelf devices. The textile-based wearable devices require excellent mechanical properties against various deformations such as twisting, stretching, and binding to be assimilated into clothes for daily use [324]. These concerns must be addressed with a new approach by developing a method to produce a complete sensing system on fabric by the printing circuit and sensors with direct coupling on the fabric itself. The new technological development would be innovation and solution for the current problems in e-textile. The e-textile sector is likely one of the largest end-users in the future, and unified, seamless integration could be a gigantic transformation to meet market viability.
9.3. Consistent power source
Providing a well-organized and stable power supply for the e-textile wearable is a big obstacle for manufacturers, and this is an obstacle to market growth for e-textiles. Conventional batteries could be used, as they are reliable and easily accessible power sources and have low power consumption, but they are bulky. There is a need to find a solution to circuits and power sources prepared like organic electronics, as they are lightweight, flexible, robust, comparatively inexpensive to manufacture, and highly compatible with garments. The connectors need to be soft and easy to integrate, but most of them are clumsy, rigid, and hard. Another problem is wiring for both power and data transfer, which needs to be flexible and must be sewn or glued into seams; even a self-powered approach could be highly beneficial. There are no bus standards, textile cables, or washable interconnects that can be used straight out of the box. There is a need to combine wires, textile yarns, and elastic weaving methods with custom, specific connectors. Furthermore, the current approaches use device attachments to fabrics and separate power supplies, which limit their applicability in sports and self-health management, etc., where flexibility or conformability to the body is critical to acquiring precise data. In particular, an e-textile system with a consistent power source could be capable of working as a complete wearable system to attain the goal of self-management.
9.4. Washability and durability
It is a challenge to develop cables, connectors, and circuits that can survive washing machines, tumble dryers, and high-humidity environments. The washing test is generally used as a reliability protocol for all types of garments and therefore for e-textiles [322,325]. Stability against distortion, twisting or bending, and therefore ensuring a long lifetime and sustainable performance, is one of the other key challenges facing wearable e-textiles that use clothing or fabric as a platform for integrating electronics [33,326]. These are two main issues related to the problem of making electronic garments ready for the market on a large scale. A standard washing procedure such as a standardized laboratory washing practice should be applied compared with conventional household machine washing and drying. Basic research is essential to improve the durability of e-textiles. Maturation can also be increased by direct printing of devices/sensors on fabric to meet the market demand.
9.5. High manufacturing cost
Manufacturing cost is another parameter that limits the applicability of wearable e-textiles as smart clothes are more costly than typical textiles [59]. The R&D budget that drives the manufacture of clothes integrated with state-of-the-art electronic components increases the cost, making them inaccessible to some vendors. For example, LEDs are currently more expensive than conventional lighting technologies; thus, a lower-middle-class family cannot afford light therapy for medical diseases. Low-cost integration of electronics into garments could help to control the price, and consequently, the e-textiles would be affordable.
9.6. Green development and biodegradability
Green development and biodegradability are the two most important factors in the production of fibers/fabrics. Eco-friendly and recyclable development of e-textiles is one of the future trends and challenges for better ecological impact. The green development and biodegradability of any textiles rely on the types of fiber materials and their synthesis methods [327]. For example, synthetic textile fibers like PET, nylon, polyester are inherently unsustainable which resist biological degradation, thus creating environmental and waste management challenges [327,328]. Pure natural fibers, like cotton, spider silk and silkworm silk, both perform well for consumer textiles and normally meet certain standardized biodegradability criteria [[329], [330], [331], [332], [333]]. Naturally biocompatible/biodegradable materials like silkworm and cotton fibers are eco-friendly and biodegradable therefore considered as outstanding facilitating textile materials for e-textiles production [334,335]. Although synthetic polymer fibers are showing great potential to be used for smart e-textiles fabrication due to high flexibility, tensile strength and toughness however they show low rates of biodegradation. Moreover, the synthesis process used for producing synthetic fibers are often too complex, which contain harmful ingredients. Thus, e-textiles need innovative solutions which meet the requirements of green production and biodegradability.
9.7. Meet the rising demand from medical and sports sectors
Demand from the medical and sports areas is a strong emerging driver for the e-textiles market on a large scale. As discussed earlier, IDTechEx estimates that the smart textile market will be worth more than US$1.3 billion by the end of 2031 [38], with fitness and healthcare being the two largest sectors. Athletes and the elderly are the major end-users of e-textiles for monitoring, and huge future market demand for fully functional technical textiles is projected [336]. Continual efforts are underway to enhance their performance, and an immense part of these efforts involves collecting and storing data for analysis and feedback. E-textiles are utilized as shielding tools in dangerous sports to help lessen risks without detracting from the adventure of the sports. Smart textiles are playing increasingly significant roles in sports by merging utilitarian functions with sportswear that facilitates performance improvements [337]. The demand for smart textiles has also grown as a result of various health and fitness issues arising from population aging. Numerous research efforts are underway to develop intelligent garments suitable for commercial applications. Advances in nanotechnology have also revealed new possibilities for e-textile applications to healthcare and fitness, including wearables that relieve chronic spinal pain, shirts with soft elastic sensors for detecting breathing rates in patients with prolonged lung disease, abdominal bands that monitor uterine contractions and fetal heart rates in pregnant women, pressure-monitoring stockings for diabetic patients that apply electrical stimuli to patients suffering from severe heart problems. Smart apparel has been proposed for use in bedside monitoring in hospitals, with shirts that track pulse rate, blood pressure, oxygen intake, and other vital signs. Many professionals in the field believe that signal recognition could also be used with clothing for other healthcare applications, such as in the treatment of paraplegics and patients with loss of muscle density due to aging. Such clothing might also be useful in monitoring stroke victims, people with severe heart problems, and people who suffer from falls in their home or at a care center—although currently, there are better-known and far less expensive technologies that serve these purposes. Electronic clothes could also be used universally throughout the day and worn on any portion of the body to monitor physical activity, stimulate muscle movements, or facilitate personalized rehabilitation.
10. Conclusion and future outlooks
Electronic textiles have attracted significant attention in recent years for applications including rehabilitation, health monitoring, fitness, and fashion, as discussed in this review. Health and fitness are higher priorities for applications of e-textiles than other areas because of their potential benefits in remote health monitoring, self-management, and digital health for the well-being of individuals and society. The wearable healthcare market is gaining momentum because of worldwide population aging trends, unexpected pandemics such as COVID-19, chronic diseases, and the digitalization of the healthcare system. The literature cited in this review shows that clothes with embedded sensors or actuators can be used as exoskeletons or in rehabilitation devices with great potential to benefit end-users facing synovial and sacroiliac joint ailments. Furthermore, because of COVID-19, there has been huge progress in the development of wearable systems with sensors for the detection of early signs of SARS Cov-2 infection. Despite the many challenges faced, e-textiles or intelligent garments are capable of integrating new sensing devices and a variety of electronic functionalities using various fabrication methods, such as weaving, spinning, embroidery, knitting, screen printing, and stitching. In the future, electronic apparel will increasingly be self-powered to facilitate the use of portable wearable sensing systems for self-health management and remote patient care. The seamless integration of devices and electronics into clothing offers great promise for fundamental change in the integration and use of wearable technologies. Several e-textile-related research projects are underway and may take a few years to achieve appreciable progress. Despite the number of scientific challenges facing e-textile technology, it is expected that in the next five to ten years, there will be many innovative e-textile solutions in healthcare and fitness involving unobtrusive monitoring and stimulation. To overcome operational limitations, the seamless integration of electronic functionalities and wearable garments could be made more adaptable, in terms of deformation, affordability, and user-friendliness, than current embroidery-based integration. The relevant literature and information on electronic garments will be significantly useful in future technological developments in e-textiles. At the same time, the use of more traditional flexible, stretchable, and pressure-sensitive sensors and light-emitting displays will continue to increase the range of applications of smart textiles to the home textile, fashion, aerospace, and defense sectors.
Additionally, smart e-textiles can also support progress in the development of more advanced applications in big data and cloud computing for intelligent health monitoring and fitness rehabilitation training via data analyses. Advances in wearable smart clothes are not confined to healthcare and fitness monitoring but lead toward new emerging technological developments in virtual reality and the Internet of Things (IoT). Textile technology is advancing and is likely to interact with IoT artificial intelligence, human–machine interfaces, and cloud technology within the next decade. Virtual reality is also expected to transform our lives in the IoT age, considering that the broader future application areas of smart textiles are intelligent and computing apparel. The Internet of Textiles is an extension of the IoT. This review is devoted to all of these current and future endeavors. A focus on new findings and investments in health and fitness is paramount and could also attract other interested audiences. This review has established a baseline for those interested in contributing to solving the fundamental challenges and obstacles that currently exist in wearable textile technology.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (No. 2019R1A6A1A03033215 ).
Biographies
Jagan Singh Meena specializes in wearable electronics for various applications. He is currently a Senior Research Fellow at the Research Center for Advanced Materials Technology, Core Research Institute, Sungkyunkwan University, South Korea, and working in the area of smart wearable electronics. He earned his M. Tech from IIT Kharagpur, India and Ph.D., on the design and development of soft electrical devices on flexible substrates, from National Chiao Tung University, Taiwan. He completed his postdoctoral research training at the University of Windsor, Canada. He has published many research articles in top-rated high-impact scientific journals/letters and presented his research in international meetings.

Jong-Woong Kim received his B·S., M.S., and Ph.D. degrees from the School of Advanced Materials Science and Engineering of Sungkyunkwan University, Suwon, Republic of Korea, in 2001, 2004, and 2008, respectively. From 2009 to 2017, he worked as a principal researcher at the Korea Electronics and Technology Institute. From 2017 to 2022, he worked in Jeonbuk National University as an Associate Professor in the School of Advanced Materials Engineering. Recently, he has joined Sungkyunkwan University, South Korea as an Associate Professor in the School of Mechanical Engineering and the Department of Smart Fab Technology. He is currently developing flexible, stretchable, self-healing, and transparent materials and electrodes that can be used in various advanced electronic devices. He has been granted various patents for his work and has published a number of national and international research articles in top-rated peer-reviewed journals.

Su Bin Choi is pursuing her Ph.D. in the Department of Smart Fab Technology, Sungkyunkwan University, South Korea, under the guidance of Prof. Jong-Woong Kim. She received her M.S. degree in the fabrication of soft and self-healable wearable electronics from the Jeonbuk National University, South korea. Her research areas are flexible, stretchable, and self-healing electrodes and devices that can be used in various smart functional systems.

Seung-Boo Jung received his B.S. in Metallurgical Engineering from Sungkyunkwan University, Suwon, Republic of Korea, in 1987, and his M.S. and Ph.D. in Metal and Materials Engineering from Osaka University, Osaka, Japan, in 1990 and 1993, respectively. He is a professor in the School of Advanced Materials Science and Engineering of Sungkyunkwan University. He is a past director of the Micro Electronic Packaging Consortium, Sungkyunkwan University and a past president of the Korean Microelectronics and Packaging Society. He has published more than 500 international papers in the areas of joining, microelectronic materials, and electronic packaging.
Contributor Information
Seung-Boo Jung, Email: sbjung@skku.edu.
Jong-Woong Kim, Email: wyjd@skku.edu.
Data availability
Data will be made available on request.
References
- 1.Chen G., Xiao X., Zhao X., Tat T., Bick M., Chen J. Chem. Rev. 2022;122:3259–3291. doi: 10.1021/acs.chemrev.1c00502. [DOI] [PubMed] [Google Scholar]
- 2.Wang G., Hou C., Wang H. Wiley-VCH Verlag GmbH & Co.; Germany: 2020. Flexible and Wearable Electronics for Smart Clothing. [Google Scholar]
- 3.Zhang Y., Zhang T., Huang Z., Yang J. Adv. Sci. 2022;9 doi: 10.1002/advs.202105084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jayathilaka W.A.D.M., Qi K., Qin Y., Chinnappan A., Serrano-García W., Baskar C., Wang H., He J., Cui S., Thomas S.W., Ramakrishna S. Adv. Mater. 2019;31 doi: 10.1002/adma.201805921. [DOI] [PubMed] [Google Scholar]
- 5.Zaman S., Tao X., Cochrane C., Koncar V. Electronics. 2022;11:99. [Google Scholar]
- 6.Sayem A.S.M., Teay S.H., Shahariar H., Fink P.L., Albarbar A. Sensors. 2020;20:587. doi: 10.3390/s20030587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lin R., Kim H.-J., Achavananthadith S., Kurt S.A., Tan S.C.C., Yao H., Tee B.C.K., Lee J.K.W., Ho J.S. Nat. Commun. 2020;11:444. doi: 10.1038/s41467-020-14311-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yang W., Gong W., Hou C., Su Y., Guo Yi, Zhang W., Li Y., Zhang Q., Wang H. Nat. Commun. 2019;10:5541. doi: 10.1038/s41467-019-13569-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ates H.C., Yetisen A.K., Güder F., Dincer C. Nat. Electron. 2021;4:13–14. [Google Scholar]
- 10.Mirjalali S., Peng S., Fang Z., Wang C.-H., Wu S. Adv. Mater. Technol. 2022;7 doi: 10.1002/admt.202100545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bassam N.A., Hussain S.A., Qaraghuli A.A., Khan J., Sumesh E.P., Lavanya V. Inform. Med. Unlocked. 2021;24 doi: 10.1016/j.imu.2021.100588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Xu C., Yang Y., Gao W. Matter. 2020;2:1414–1445. doi: 10.1016/j.matt.2020.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mulatier S., Nasreldin M., Delattre R., Ramuz M., Djenizian T. Adv. Mater. Technol. 2018;3 [Google Scholar]
- 14.Ismar E., Bahadir S.K., Kalaoglu F., Koncar V. Glob. Chall. 2020;4 doi: 10.1002/gch2.201900092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lund A., Wu Y., Fenech-Salerno B., Torrisi F., Carmichael T.B., Müller C. MRS Bull. 2021;46:491–500. doi: 10.1557/s43577-021-00117-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dulal M., Afroj S., Ahn J., Cho Y., Carr C., Kim I.-D., Karim N. ACS Nano. 2022;16:19755–19788. doi: 10.1021/acsnano.2c07723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ornaghi Júnior H.L., Neves R.M., Monticeli F.M., Agnol L.D. Textiles. 2022;2:582–605. [Google Scholar]
- 18.Libanori A., Chen G., Zhao X., Zhou Y., Chen J. Nat. Electron. 2022;5:142–156. [Google Scholar]
- 19.Ruckdashel R.R., Khadse N., Park J.H. Sensors. 2022;22:6055. doi: 10.3390/s22166055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Çelikel D.C. In: Advanced Functional Materials. Tasaltin N., Nnamchi P.S., Saud S., editors. Intech Open London; 2020. Smart E-textile materials. [Google Scholar]
- 21.Shuvo I.I., Shah A., Dagdeviren C. Adv. Intell. Syst. 2022;4 [Google Scholar]
- 22.Yao S., Yang J., Roblete F.R., Hu X., Zhu Y. ACS Appl. Mater. Interfaces. 2019;11:31028–31037. doi: 10.1021/acsami.9b07520. [DOI] [PubMed] [Google Scholar]
- 23.Zhang S., Xu J., Sun Y. Cellulose. 2021;28:4439–4453. [Google Scholar]
- 24.Mao Y., Shen M., Liu B., Xing L., Chen S., Xue X. Sensors. 2019;19:3310. doi: 10.3390/s19153310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yang K., Isaia B., Laura, Brown J.E., Beeby S. Sensors. 2019;19:4463. doi: 10.3390/s19204463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen L., Lu M., Yang H., Avila J.R.S., Shi B., Ren L., Wei G., Liu X., Yin W. ACS Nano. 2020;14:8191–8201. doi: 10.1021/acsnano.0c01643. [DOI] [PubMed] [Google Scholar]
- 27.van Langenhove L. In: Woodhead Publishing Series in Textiles, Smart Textiles For Protection. Chapman R.A., editor. Woodhead Publishing; 2013. pp. 3–33. [Google Scholar]
- 28.Wu Y., Mechael S.S., Lerma C., Carmichael R.S., Carmichael T.B. Matter. 2020;2:882–895. [Google Scholar]
- 29.Wu Y., Mechael S.S., Carmichael T.B. Acc. Chem. Res. 2021;54:4051–4064. doi: 10.1021/acs.accounts.1c00433. [DOI] [PubMed] [Google Scholar]
- 30.Liu S., Ma K., Yang B., Li H., Tao X. Adv. Funct. Mater. 2021;31 [Google Scholar]
- 31.Zhang Z., He T., Zhu M., Sun Z., Shi Q., Zhu J., Dong B., Yuce M.R., Lee C. npj Flex. Electron. 2020;4:29. [Google Scholar]
- 32.Esfahani M.I.M. In: Micro and Nano Technologies, Nanosensors and Nanodevices for Smart Multifunctional Textiles. Ehrmann A., Nguyen T.A., Tri P.N., editors. 2021. Chapter 6 - smart textiles in healthcare: a summary of history, types, applications, challenges, and future trends; pp. 93–107. [Google Scholar]
- 33.Fernández-Caramés T.M., Fraga-Lamas P. Electronics. 2018;7:405. [Google Scholar]
- 34.Andrew T.L. Matter. 2020;2:794–795. [Google Scholar]
- 35.Jansen K.M.B. EuroSimE); 2019. International Conference on Thermal, Mechanical and Multi-Physics Simulation and Experiments in Microelectronics and Microsystems; pp. 1–4. [Google Scholar]
- 36.Karim N., Afroj S., Tan S., He P., Fernando A., Carr C., Novoselov K.S. ACS Nano. 2017;11:12266–12275. doi: 10.1021/acsnano.7b05921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.E-textiles 2017–2027: Technologies, Markets, Players. IDTechEx; Cambridge, UK: 2017. https://www.idtechex.com/en/research-report/e-textiles-2017-2027-technologies-markets-players/522 Accessed: [Google Scholar]
- 38.Hayward J. 2021. E-Textiles and Smart Clothing 2021-2031: Technologies, Markets and Players IDTechEx.https://www.idtechex.com/en/research-report/e-textiles-and-smart-clothing-2021-2031-technologies-markets-and-players/828 Accessed: [Google Scholar]
- 39.Wu J.X., Li L. Intech Open; London, UK: 2019. Smart and Functional Soft Materials; p. 11. [Google Scholar]
- 40.Bae H., Jang B.C., Park H., Jung S.-H., Lee H.M., Park J.-Y., Jeon S.-B., Son G., Tcho I.-W., Yu K., Im S.G., Choi S.-Y., Choi Y.-K. Nano Lett. 2017;17:6443–6452. doi: 10.1021/acs.nanolett.7b03435. [DOI] [PubMed] [Google Scholar]
- 41.Wicaksono I., Tucker C.I., Sun T., Guerrero C.A., Liu C., Woo W.M., Pence E.J., Dagdeviren C. npj Flexible Electronics. 2020;5:5292. doi: 10.1038/s41528-020-0068-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Simegnaw A.A., Malengier B., Rotich G., Tadesse M.G., Langenhove L.V. Materials. 2021;14:5113. doi: 10.3390/ma14175113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ankhili A., Tao X., Cochrane C., Coulon D., Koncar V. Materials. 2018;11:256. doi: 10.3390/ma11020256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Thekkekara L.V., Gu M. Sci. Rep. 2019;9 doi: 10.1038/s41598-019-48320-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yang K., Meadmore K., Freeman C., Grabham N., Hughes A.M., Wei Y., Torah R., Glanc-Gostkiewicz M., Beeby S., Tudor J. Sensors. 2018;18:2410. doi: 10.3390/s18082410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kan C.-W., Lam Y.-L. Appl. Sci. 2021;11:3914. [Google Scholar]
- 47.Dong K., Peng X., Cheng R., Ning C., Jiang Y., Zhang Y., Wang Z.L. Adv. Mater. 2022;34 doi: 10.1002/adma.202109355. [DOI] [PubMed] [Google Scholar]
- 48.Shahariar H., Kim I., Soewardiman H., Jur J.S. ACS Appl. Mater. Interfaces. 2019;11:6208–6216. doi: 10.1021/acsami.8b18231. [DOI] [PubMed] [Google Scholar]
- 49.Zhang Y., Wang H., Lu H., Li S., Zhang Y. iScience. 2021;24 doi: 10.1016/j.isci.2021.102716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kubicek J., Fiedorova K., Vilimek D., Cerny M., Penhaker M., Janura M., Rosicky J. IEEE Rev. Biomed. Eng. 2022;15:36–60. doi: 10.1109/RBME.2020.3043623. [DOI] [PubMed] [Google Scholar]
- 51.Cho S., Chang T., Yu T., Lee C.H. Biosensors. 2022;12:222. doi: 10.3390/bios12040222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wang J., Lu C., Zhang K. Energy Environ. Mater. 2020;3:80–100. [Google Scholar]
- 53.Tat T., Chen G., Zhao X., Zhou Y., Xu J., Chen J. ACS Nano. 2022;16:13301–13313. doi: 10.1021/acsnano.2c06287. [DOI] [PubMed] [Google Scholar]
- 54.Dong K., Wang Z.L. J. Semiconduct. 2022;42 [Google Scholar]
- 55.Dong K., Peng X., Cheng R., Wang Z.L. Nanoenergy Adv. 2022;2:133–164. [Google Scholar]
- 56.Dong K., Hu Y., Yang J., Kim S.-W., Hu W., Wang Z.L. MRS Bull. 2021;46:512–521. [Google Scholar]
- 57.Wu S., Dong T., Li Y., Li Y., Sun M., Qi Y., Liu J., Kuss M.K., Chen S., Duan B. Appl. Mater. Today. 2022;27 doi: 10.1016/j.apmt.2022.101473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Dong T., Li Z., Ni S., Zhou F., Alimi O.A., Chen S., Duan B., Kuss M., Wu S. Mater. Today Chem. 2022;24 [Google Scholar]
- 59.Hughes-Riley T., Dias T., Cork C. Fibers. 2018;6:34. [Google Scholar]
- 60.Lewis P. Textil. Hist. 1986;17:129–147. [Google Scholar]
- 61.Guler S.D., Gannon M., Sicchio K. Springer Science+Business Media; New York: 2016. Crafting Wearables: Blending Technology with Fashion, Apress. [Google Scholar]
- 62.Post E.R., Orth M., Russo P.R., Gershenfeld N. IBM Syst. J. 2000;39:840–860. [Google Scholar]
- 63.Hassan B.S., Islam G., Haque A. Adv. Res. Text. Eng. 2019;4:1038. [Google Scholar]
- 64.Linz T., Kallmayer C., Aschenbrenner R., Reichl H. IEEE; Osaka, Japan: 2005. Proc. Ninth IEEE Int. Symp. Wearable Comp. [Google Scholar]
- 65.Lancos L., Thronickle W., Ristol S. 2018. Smart Fabric-White Paper. Atos. [Google Scholar]
- 66.Uzun S., Seyedin S., Stoltzfus A.L., Levitt A.S., Alhabeb M., Anayee M., Strobel C.J., Razal J.M., Dion G., Gogotsi Y. Adv. Funct. Mater. 2019;29 [Google Scholar]
- 67.Quinn B. Laurence King Publishing; London: 2013. Textile Visionaries: Innovation and Sustainability in Textile Design. [Google Scholar]
- 68.CuteCircuit, https://cutecircuit.com/.
- 69.Smart Textiles and Wearables - Markets, Applications and Technologies, Innovation in Textiles, UK. 2016. https://www.innovationintextiles.com/new-report-smart-textiles-and-wearables-markets-applications-and-technologies/ September. Accessed in December 2022: [Google Scholar]
- 70.Alonso E.T., Rodrigues D.P., Khetani M., Shin D.-W., De Sanctis A., Joulie H., de Schrijver I., Baldycheva A., Alves H., Neves A.I.S., Russo S., Craciun M.F. npj Flexible Electron. 2018;2:25. [Google Scholar]
- 71.Shi X., Zuo Y., Zhai P., Shen J., Yang Y., Gao Z., Liao M., Wu J., Wang J., Xu X., Tong Q., Zhang B., Wang B., Sun X., Zhang L., Pei Q., Jin D., chen P., Peng H. Nature. 2021;591:240–245. doi: 10.1038/s41586-021-03295-8. [DOI] [PubMed] [Google Scholar]
- 72.Tao X., Huang T.-H., Shen C.-L., Ko Y.-C., Goe G.-T., Koncar V. Adv. Mater. Tech. 2018;3 [Google Scholar]
- 73.Smart textiles and wearables-markets, applications and technologies. Innovation in Textiles (Report), September 2016 UK. https://www.innovationintextiles.com/new-report-smart-textiles-and-wearables-markets-applications-and-technologies/ Accessed: [Google Scholar]
- 74.Viswanathan S. Inter. J. Eng. Sci. Computing. 2019;9 [Google Scholar]
- 75.David Global. 2020. Smart Wearables for Sports and Fitness Market 2020 by Manufacturers, Type and Application, Forecast to 2025, May.https://www.marketsandresearch.biz/ Accessed: [Google Scholar]
- 76.Shirvan A.R., Nouri A. The Textile Institute Book Series; 2020. Medical Textiles, Advances in Functional and Protective Textiles; pp. 291–333. July. [Google Scholar]
- 77.Lian Y., Yu H., Wang M., Yang X., Li Z., Yang F., Wang Y., Tai H., Liao Y., Wu J., Wang X., Jianga Y., Tao G. J. Mater. Chem. C. 2020;8:8399–8409. [Google Scholar]
- 78.Basodan R., Park B., Chung H.-J. Flex. Print. Electron. 2021;6 [Google Scholar]
- 79.Cinquino M., Prontera C.T., Pugliese M., Giannuzzi R., Taurino D., Gigli G., Maiorano V. Micromachines. 2021;12:652. doi: 10.3390/mi12060652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Yang L., Ma Z., Tian Y., Meng B., Peng Z. Micromachines. 2021;12:666. doi: 10.3390/mi12060666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Liman M.L.R., Islam M.T., Hossain M.M. Adv. Electron. Mater. 2022;8 [Google Scholar]
- 82.Wu Y., Yang Y., Li C., Li Y., Chen W. Front. Bioeng. Biotechnol. 2020;8:212. doi: 10.3389/fbioe.2020.00212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Lin C.-C., Yang C.-Y., Zhou Z., Wu S. Int. J. Distributed Sens. Netw. 2018;14:8. [Google Scholar]
- 84.Imani S., Bandodkar A.J., Vinu Mohan A.M., Kumar R., Yu S., Wang Joseph, Mercier P.P. Nat. Commun. 2016;7 doi: 10.1038/ncomms11650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kakria P., Tripathi N.K., Kitipawang P. Inter. J. Telemed. Appl. 2015 doi: 10.1155/2015/373474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Patel S., Park H., Bonato P., Chan L., Rodgers M. J. NeuroEng. Rehabil. 2012;9:21. doi: 10.1186/1743-0003-9-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Angelov G.V., Nikolakov D.P., Ruskova I.N., Gieva E.E., Spasova M.L. Enhanced Living Environments. 2019;11369:226–262. [Google Scholar]
- 88.Edmison J., Jones M., Lockhart T., Martin T. Stud. Health Technol. Inf. 2004;108:292–301. [PMC free article] [PubMed] [Google Scholar]
- 89.Poomsalood S., Muthumayandi K., Hambly K. Biomed. Hum. Kinet. 2019;11:1. [Google Scholar]
- 90.OMsignal: smart clothing lab, https://smartclothinglab.com/.
- 91.Myant Inc, https://myant.ca/.
- 92.Brown D. 2020. The Arrival of 2020 Brings Smart Clothing to the Forefront of Healthcare.https://www.youareunltd.com/2020/01/03/smart-clothing-at-the-forefront-of-a-new-frontier-in-healthcare/ January. Accessed: [Google Scholar]
- 93.United Nations, Department of Economic and Social Affairs, Population Division . ST/ESA/SER.A/430; 2019. World Population Ageing 2019, Highlights. [Google Scholar]
- 94.Martinez-Ferran W.M., de la Guía-Galipienso F., Sanchis-Gomar F., Pareja-Galeano H. Nutrients. 2020;12:1549. doi: 10.3390/nu12061549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Haleem A., Javaid M., Singh R.P., Suman R. Sens. Int. 2021;2 doi: 10.1016/j.sintl.2021.100117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ricci F., Izzicupo P., Moscucci F., Sciomer S., Maffei S., Baldassarre A.D., Mattioli A.V., Gallina S. Front. Public Health. 2020;8:199. doi: 10.3389/fpubh.2020.00199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Sleeptite, www.sleeptite.com.au/.
- 98.Nextiles, https://www.nextiles.tech/.
- 99.MesoMat, https://mesomat.com/.
- 100.Toray Inc, https://www.hitoe.toray/en/.
- 101.E-skin Meva, https://xenoma.com/en/.
- 102.Palarum, https://palarum.org/.
- 103.Texisense, https://www.texisense.com/.
- 104.Carre Technologies Inc. (Hexoskin), https://www.hexoskin.com/.
- 105.Nanowear Inc., https://www.nanowearinc.com/.
- 106.DuPont, https://electronics-imaging.dupont.com/intexar.
- 107.Clim8, https://myclim8.com/.
- 108.Loomia, https://www.loomia.com/.
- 109.Souyarn, https://www.soliyarn.com/.
- 110.Smart Fabric Inks, http://www.fabinks.com/.
- 111.Hayward J., Coles C., Tsao N., Backer M.D. IDTechEx Research; 2020. Wearable Technology Forecasts: 2020-2030.https://www.idtechex.com/en/research-report/wearable-technology-forecasts-2020-2030/747 Accessed: [Google Scholar]
- 112.Hayward J. 2020. Updating the E-Textiles Mantra: an Analyst's Commentary, IDTechEx Research.https://www.idtechex.com/en/research-article/updating-the-e-textiles-mantra-an-analysts-commentary/20938 Accessed: [Google Scholar]
- 113.Global E-Textiles Market 2021-2025, Market Research Report. Infiniti Research Ltd.); TechNavio: 2021. https://www.giiresearch.com/report/infi601396-global-e-textile-market.html Accessed: [Google Scholar]
- 114.August 26. Future Markets, Inc.; 2021. https://www.giiresearch.com/report/fmi1022570-global-market-electronic-textiles-e-textiles-smart.html The Global Market for Electronic Textiles (E-Textiles) and Smart Clothing, Market Research Report Accessed: [Google Scholar]
- 115.Hatamie A., Angizi S., Kumar S., Pandey C.M., Simchi A., Willander M., Malhotra B.D. J. Electrochem. Soc. 2020;167 [Google Scholar]
- 116.Vooris R., Blaszka M., Purrington S. Int. J. Sociol. Leisure. 2019;2:421–437. [Google Scholar]
- 117.Lio X., Song W., Zhang X., Huang H., Wang Y., Zheng Y. J. Mater. Chem. C. 2018;6:12841–12848. [Google Scholar]
- 118.Shi J., Liu S., Zhang L., Yang B., Shu L., Yang Y., Ren M., Wang Y., Chen J., Chen W., Chai Y., Tao X. Adv. Mater. 2019;32 doi: 10.1002/adma.201901958. [DOI] [PubMed] [Google Scholar]
- 119.MacIntyre R., Chughtai A.A. Int. J. Nurs. Stud. 2020;108 doi: 10.1016/j.ijnurstu.2020.103629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Desai A.N., Mehrotra P. JAMA. 2020;323:1517–1518. doi: 10.1001/jama.2020.2331. [DOI] [PubMed] [Google Scholar]
- 121.Pullangott G., Kannan U., Gayathri S., Kiranb D.V., Maliyekkal S.M. RSC Adv. 2021;11:6544–6576. doi: 10.1039/d0ra10009a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Uddin F. Textile Manufacturing Processes. 2019. Introductory chapter: textile manufacturing processes. London, UK IntechOpen. [Google Scholar]
- 123.Agcayazi T., Chatterjee K., Bozkurt A., Ghosh T.K. Adv. Mater. Technol. 2018;3 [Google Scholar]
- 124.Fangueiro R., Soutinho F. Woodhead Publishing Series in Textiles. Woodhead Publishing; 2011. Textile structures; pp. 62–91. [Google Scholar]
- 125.Murthy H.V.S. first ed. WPI Publishing; 2015. Introduction to Textile Fibres. [Google Scholar]
- 126.Faridal Hasan K.M., Horvath P.G., Alpar T. J. Mater. Sci. 2021;56:14381–14415. [Google Scholar]
- 127.Meena J.S., Choi S.B., Jung S.-B., Kim J.-W. Appl. Mater. Today. 2022;29 [Google Scholar]
- 128.Chen Q., Akram W., Cao Y., Ge C., Lin T., Fang J. 2022. Carbon Neutralization; pp. 1–27. [Google Scholar]
- 129.Yin Z., Lu H., Gan L., Zhang Y. Adv. Mater. Technol. 2022 [Google Scholar]
- 130.Wu S., Qi Y., Shi W., Kuss M., chen S., Duan B. Acta Biomater. 2022;139:91–104. doi: 10.1016/j.actbio.2020.11.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Wu S., Liu J., Cai J., Zhang J., Duan B., Chen S. Biofabrication. 2021;13 doi: 10.1088/1758-5090/ac2209. [DOI] [PubMed] [Google Scholar]
- 132.Liu J., Li T., Zhang H., Zhao W., Qu L., Chen S., Wu S. Mater. Today Bio. 2022;14 doi: 10.1016/j.mtbio.2022.100243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Seyedin S., Zhang P., Naebe M., Qin S., Chen J., Wanga X., Razal J.M. Mater. Horiz. 2019;6:219–249. [Google Scholar]
- 134.Ojstršek A., Plohl O., Gorgieva s., Kurecic M., Jancic U., Hribernik S., Fakin D. Sensors. 2021;21:3508. doi: 10.3390/s21103508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Meena J.S., Choi S.B., Khanh T.D., Shin H.S., Choi J.S., Joo J., Kim J.-W. Appl. Surf. Sci. 2023;613 [Google Scholar]
- 136.Faruk M.O., Ahamed A., Jalil M.A., Islam M.T., Shamim A.M., Adak B., Hossain M.M., Mukhopadhyay S. Appl. Mater. Today. 2021;23 [Google Scholar]
- 137.Jalil M.A., Ahamed A., Hossain M.M., Adak B., Islam M.T., Moniruzzaman M., Parvez M.S., Shkir M., Mukhopadhyay S. ACS Omega. 2022;7:12716–12723. doi: 10.1021/acsomega.1c07148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.George A., Shrivastav P.S. Arch. Dermatol. Res. 2022;314:929–936. doi: 10.1007/s00403-021-02301-3. [DOI] [PubMed] [Google Scholar]
- 139.Tylcz J.-B., Vicentini C., Mordon S. Woodhead Publishing Series in Textiles, Smart Textiles and Their Applications. Woodhead Publishing; 2016. vladan koncar; pp. 71–87. [Google Scholar]
- 140.Meng K., Xiao X., Wei W., Chen G., Nashalian A., Shen S., Xiao X., Chen J. Adv. Mater. 2022;34 doi: 10.1002/adma.202109357. [DOI] [PubMed] [Google Scholar]
- 141.Pang Y., Tian H., Tao L., Li Y., Wang X., Deng N., Yang Y., Ren T.-L. ACS Appl. Mater. Interfaces. 2016;8:26458–26462. doi: 10.1021/acsami.6b08172. [DOI] [PubMed] [Google Scholar]
- 142.Liu X., Jin X., Li L., Wang J., Yang Y., Cao Y., Wang W. J. Mater. Chem. 2020;8:12526–12537. [Google Scholar]
- 143.Mi H., Zhong L., Tang X., Xu P., Liu X., Luo T., Jiang X. ACS Appl. Mater. Interfaces. 2021;13:11260–11267. doi: 10.1021/acsami.0c19743. [DOI] [PubMed] [Google Scholar]
- 144.Tian Z., Zhang H., Xiu F., Zhang M., Zou J., Ban C., Nie Y., Jiang W., Hu B., Liu J. Nanoscale Adv. 2021;3:2475–2480. doi: 10.1039/d1na00063b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Yambem S.D., Brooks-Richards T.L., Forrestal D.P., Kielar M., Sah P., Pandey A.K., Woodruff M.A. Sci. Rep. 2019;9:9875. doi: 10.1038/s41598-019-45867-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Takamatsu S., Lonjaret T., Crisp D., Badier J.-M., Malliaras G.G., Ismailova E. Sci. Rep. 2015;5 doi: 10.1038/srep15003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Zhao Y., Cao Y., Liu J., Zhan Z., Li X., Li W.J. Micromachines. 2018;9:132. doi: 10.3390/mi9030132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Liu M., Arumugam S., Li Y., Yong S., White N., Yang K., Beeby S. IEEE; Glasgow, UK: 2019. IEEE International Conference on Flexible and Printable Sensors and Systems (FLEPS) July (2019. [Google Scholar]
- 149.Pacelli M., Loriga G., Taccini N., Paradiso R. September; Boston, USA: 2006. Proceedings of the 3rd IEEE-EMBS International Summer School and Symposium on Medical Devices and Biosensors MIT. [Google Scholar]
- 150.Rezaei A., Cuthbert T.J., Gholami M., Menon C. Sensors. 2019;19:4288. doi: 10.3390/s19194288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Presti D.L., Romano C., Massaroni C., D'Abbraccio J., Massari L., Caponero M.A., Oddo C.M., Formica D., Schena E. Sensors. 2019;19:358. doi: 10.3390/s19163581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Quandt B.M., Pfister M.S., Lubben J.F., Spano F., Rosi R.M., Bona G.-L., Boesel L.F. Biomed. Opt Express. 2017;8:4316–4330. doi: 10.1364/BOE.8.004316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Guo J., Yu S., Li Y., Huang T.-H., Wang J., Lynn B., Fidock J., Shen C.-L., Edwards D., Su H.A. April; Italy: 2018. Proceedings of the IEEE International Conference on Soft Robotics (RoboSoft), Livorno. [Google Scholar]
- 154.Golparvar A.J., Yapici M.K. IEEE Sensor. J. 2018;18:8971–8978. [Google Scholar]
- 155.Fleury A., Alizadeh M., Stefan G., Chau T. vols. 13–15. LSC); Sydney, NSW, Australia: 2017. p. 3538. (Proceedings of the 2017 IEEE Life Sciences Conference). December. [Google Scholar]
- 156.Kim S.J., Song W., Yi Y., Min B.K., Mondal S., An K.-S., Choi C.-G. ACS Appl. Mater. Interfaces. 2018;10:3921–3928. doi: 10.1021/acsami.7b15386. [DOI] [PubMed] [Google Scholar]
- 157.Chen S., Lou Z., Chen D., Jiang K., Shen G. Adv. Mater. Technol. 2016;1 [Google Scholar]
- 158.Zhao H., Zhang Y., Bradford P.D., Zhou Q., Jia Q., Yuan F.-G., Zhu Y. Nanotechnology. 2010;21 doi: 10.1088/0957-4484/21/30/305502. [DOI] [PubMed] [Google Scholar]
- 159.Ge J., Sun L., Zhang F., Zhang Y., Shi L., Zhao H., Zhu H., Jiang H., Yu S.A. Adv. Mater. 2016;28:722–728. doi: 10.1002/adma.201504239. [DOI] [PubMed] [Google Scholar]
- 160.Eom J., Jaisutti R., Lee H., Lee W., Heo J., Lee J., Park S.K., Kim Y. ACS Appl. Mater. Interfaces. 2017;9:10190–10197. doi: 10.1021/acsami.7b01771. [DOI] [PubMed] [Google Scholar]
- 161.Fan W., He Q., Meng K., Tan X., Zhou Z., Zhang G., Yang J., Wang Z.L. Sci. Adv. 2020;6:2840. doi: 10.1126/sciadv.aay2840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Watson A., Sun M., Pendyal S., Zhou G. Smart Health. 2020;15 [Google Scholar]
- 163.Li Y., Li Y., Su M., Li W., Li Y., Li H., Qian X., Zhang X., Li F., Song Y. Adv. Electron. Mater. 2017;3 [Google Scholar]
- 164.Afroj S., Karim N., Wang Z., Tan S., He P., Holwill M., Ghazaryan D., Fernando A., Novoselov K.S. ACS Nano. 2019;13:3847–3857. doi: 10.1021/acsnano.9b00319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Liu M., Ward T., Young D., Matos H., Wei Y., Adams J., Yang K. Sens. Actuators A Phys. 2020;303 [Google Scholar]
- 166.Karim N., Afroj S., Malandraki A., Butterworth S., Beach C., Rigout M., Novoselov K. J. Mater. Chem. C. 2017;5:11640–11648. [Google Scholar]
- 167.Martin T., Jones M., Chong J., Quirk M., Baumann K., Passauer L. 2009. Conference IEEE Xplore. October. [Google Scholar]
- 168.Deng J., Zhuang W., Bao L., Wu X., Gao J., Wang B., Sun X., Peng H. Carbon. 2019;149:63–70. [Google Scholar]
- 169.Sadi M.S., Yang M., Luo L., Cheng D., Cai G., Wang X. Cellulose. 2019;26:6179–6188. [Google Scholar]
- 170.Zhu M., Shi Q., He T., Yi Z., Ma Y., Yang B., Chen T., Lee C. ACS Nano. 2019;13:1940–1952. doi: 10.1021/acsnano.8b08329. [DOI] [PubMed] [Google Scholar]
- 171.Aqueveque P., Germany E., Osorio R., Pastene F. Sensors. 2020;20:656. doi: 10.3390/s20030656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Votzke C., Daalkhaijav U., Mengue Y., Johnston M.L. BioCAS); Cleveland, OH, USA: 2018. IEEE Biomedical Circuits and Systems Conference; pp. 1–4. October. 2018. [Google Scholar]
- 173.Zięba J., Frydrysiak M., Tokarska M. Fibres text. East. Eure. 2011;19:70–74. [Google Scholar]
- 174.Satharasinghe A., Hughes-Riley T., Dias T. 2019. AUTEX2019–19th World Textile Conference on Textiles, Ghent, Belgium June. [Google Scholar]
- 175.Jin L., Guo X., Gao D., Wu C., Hu B., Tan G., Du N., Cai X., Yang Z., Zhang X. NPG Asia Mater. 2021;13:24. [Google Scholar]
- 176.Zhao X., Wang L.-Y., Tang C.-Y., Zha X.-J., Liu Y., Su B.-H., Ke K., Bao R.-Y., Yang M.-B., Yang W. ACS Nano. 2020;14:8793–8805. doi: 10.1021/acsnano.0c03391. [DOI] [PubMed] [Google Scholar]
- 177.Jia Z., Gong J., Zeng Y., Ran J., Liu J., Wang K., Xie C., Lu X., Wang J. Adv. Funct. Mater. 2021;31 [Google Scholar]
- 178.Tian B., Fang Y., Liang J., Zheng K., Guo P., Zhang X., Wu Y., Liu Q., Huang Z., Cao C., Wu W. Small. 2022;18 doi: 10.1002/smll.202107298. [DOI] [PubMed] [Google Scholar]
- 179.Sun T., Zhou B., Zheng Q., Wang L., Jiang W., Snyder G.J. Nat. Commun. 2020;11:572. doi: 10.1038/s41467-020-14399-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Wu R., Ma L., Patil A., Hou C., Zhu S., Fan X., Lin H., Yu W., Guo W., Liu X.Y. ACS Appl. Mater. Interfaces. 2019;11:33336–33346. doi: 10.1021/acsami.9b10928. [DOI] [PubMed] [Google Scholar]
- 181.Lou M., Abdalla I., Zhu M., Yu J., Li Z., Ding B. ACS Appl. Mater. Interfaces. 2020;12:1597–1605. doi: 10.1021/acsami.9b19238. [DOI] [PubMed] [Google Scholar]
- 182.Lou M., Abdalla I., Zhu M., Wei X., Yu J., Li Z., Ding B. ACS Appl. Mater. Interfaces. 2020;12:19965–19973. doi: 10.1021/acsami.0c03670. [DOI] [PubMed] [Google Scholar]
- 183.Li M., Chen J., Zhong W., Luo M., Wang W., Qing X., Lu Y., Liu Q., Liu K., Wang Y., Wang D. ACS Sens. 2020;5:2545–2554. doi: 10.1021/acssensors.0c00870. [DOI] [PubMed] [Google Scholar]
- 184.Rehman A., Houshyar S., Reineck P., Padhye R., Wang X., Houshyar S. ACS Appl. Polym. Mater. 2020;2:4848–4855. [Google Scholar]
- 185.Jin H., Matsuhisa N., Lee S., Abbas M., Yokota T., Someya T. Adv. Mater. 2017;29 doi: 10.1002/adma.201605848. [DOI] [PubMed] [Google Scholar]
- 186.Zhou Z., Li Y., Cheng J., Chen S., Hu R., Yan X., Liao X., Xu C., Yu J., Li L. J. Mater. Chem. C. 2018;6:13120–13127. [Google Scholar]
- 187.Liu M., Pu X., Jiang C., Liu T., Huang X., Chen L., Du C., Sun J., Hu W., Wang Z.L. Adv. Mater. 2017;29 doi: 10.1002/adma.201703700. [DOI] [PubMed] [Google Scholar]
- 188.Tian M., Lu Y., Qu L., Zhu S., Zhang X., Chen S. Ind. Eng. Chem. Res. 2019;58:5737–5742. [Google Scholar]
- 189.Xu L., Liu Z., Zhai H., Chen X., Sun R., Lyu S., Fan Y., Yi Y., Chen Z., Jin L., Zhang J., Li Y., Ye T.T. ACS Appl. Mater. Interfaces. 2020;12:13265–13274. doi: 10.1021/acsami.9b20964. [DOI] [PubMed] [Google Scholar]
- 190.Hao D., Xu B., Cai Z. J. Mater. Sci. Mater. Electron. 2018;29:9218–9226. [Google Scholar]
- 191.Liu X., Tang C., Du X., Xiong S., Xi S., Liu Y., Shen X., Zheng Q., Wang Z., Wu Y., Horner A., Kim J.K. Mater. Horiz. 2017;4:477–486. [Google Scholar]
- 192.Li Q., Yin R., Zhang D., Liu H., Chen X., Zheng Y., Guo Z., Liu C., Shen C. J. Mater. Chem. 2020;8:21131–21141. [Google Scholar]
- 193.Zheng X., Wang P., Zhang X., Hu Q., Wang Z., Nie W., Zou L., Li C., Han X. Composites Part A. 2022;152 [Google Scholar]
- 194.Lippi G., Henry G.B.M., Bovo C., Sanchis-Gomar F. Diagnosis (Berl.) 2020;7:85–90. doi: 10.1515/dx-2020-0041. [DOI] [PubMed] [Google Scholar]
- 195.Dhand R., Li J. Am. J. Respir. Crit. Care Med. 2020;202:651–659. doi: 10.1164/rccm.202004-1263PP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Tan W., Aboulhosn J. Int. J. Cardiol. 2020;309:70–77. doi: 10.1016/j.ijcard.2020.03.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Vellingiri B., Jayaramayya K., Iyer M., Narayanasamy A., Govindasamy V., Giridharan B., Ganesan S., Venugopal A., Venkatesan D., Ganesan H., Rajagopalan K., Rahman P.K.S.M., Cho S.-G., Kumar N.S., Subramaniam M.D. Sci. Total Environ. 2020;725 doi: 10.1016/j.scitotenv.2020.138277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.World Health Organization Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations. 2020. https://www.who.int/newsroom/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations Accessed:
- 199.Esposito S., Principi N., Leung C.C., Migliori G.B. Eur. Respir. J. 2020;55 doi: 10.1183/13993003.01260-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Rothe C., Schunk M., Sothmann P., Bretzel G., Froeschl G., Wallrauch C., Zimmer T., Thiel V., Janke C., Engl N. J. Med. 2020;382:970–971. doi: 10.1056/NEJMc2001468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Long Y., Hu T., Liu L., Chen R., Guo Q., Yang L., Cheng Y., Huang J., Du L. J. Evid. Base Med. 2020;13:93–101. doi: 10.1111/jebm.12381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Konda A., Prakash A., Moss G.A., Grant G.D., Guha S. ACS Nano. 2020;14:6339–6347. doi: 10.1021/acsnano.0c03252. [DOI] [PubMed] [Google Scholar]
- 203.Leung N.H.L., Chu D.K.W., Shiu E.Y.C., Chan K.-H., McDevitt J.J., Hau B.J.P., Yen H.-L., Li Y., Ip D.K.M., Malik Peiris J.S., Seto W.-H., Leung G.M., Milton D.K., Cowling B.J. Nat. Med. 2020;26:676–680. doi: 10.1038/s41591-020-0843-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Ghatak B., Banerjee S., Ali S.B., Bandhyopadhyay R., Das N., Tudu B., Mandal D., Tudu B. Nano Energy. 2021;70 doi: 10.1016/j.nanoen.2020.105387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Breul S., Landuyt K.L.V., Reichl F.X., Högg C., Hoet P., Godderis L., Meerbeek B.V., Cokic S.M. Eup. J. Oral Sceinces. 2020;128:233–240. doi: 10.1111/eos.12697. [DOI] [PubMed] [Google Scholar]
- 206.Ghatak S., Khona D.K., Sen A., Huang K., Jagdale G., Singh K., Gopalakrishnan V., Cornetta K.G., Roy S., Khanna S., Baker L.A., Sen C.K. Sci. Rep. 2021;11 doi: 10.1038/s41598-021-00910-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Li W. Preprints. 2020;1 [Google Scholar]
- 208.Ahmad M.A., Mustafa F., Ali L.M., Rizvi T.A. Sci. Rep. 2014;4:6831. doi: 10.1038/srep06831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Hernando-Pérez M., Cartagena-Rivera A.X., Lošdorfer Božič A., Carrillo P.J.P., San Martín C., Mateu M.G., Raman A., Podgornikand R., de Pablo P.J. Nanoscale. 2015;7:17289–17298. doi: 10.1039/c5nr04274g. [DOI] [PubMed] [Google Scholar]
- 210.Cheng Y., Wang C., Zhong J., Lin S., Xiao Y., Zhong Q., Jiang H., Wu N., Li W., Chen S., Wang B., Zhang Y., Zhou J. Nano Energy. 2017;34:562–569. [Google Scholar]
- 211.Zhong Q., Zhong J., Hu B., Hu Q., Zhou J., Wang Z.L. Energy Environ. Sci. 2013;6:1779–1784. [Google Scholar]
- 212.Zhong J., Li Z., Takakuwa M., Inoue D., Hashizume D., Jiang Z., Shi Y., Ou L., Nayeem M.O.G., Umezu S., Fukuda K., Someya T. Adv. Mater. 2022;34 doi: 10.1002/adma.202107758. [DOI] [PubMed] [Google Scholar]
- 213.Chu Y., Zhong J., Liu H., Ma Y., Liu N., Song Y., Liang J., Shao Z., Sun Y., Dong Y., Wang X., Lin L. Adv. Funct. Mater. 2018;28 [Google Scholar]
- 214.WHO . World Health Organization; 2018. Global Action Plan on Physical Activity 2018–2030.https://apps.who.int/iris/handle/10665/272722 Accessed: [Google Scholar]
- 215.Guthold R., Stevens G.A., Riley L.M., Bull F.C. Lancet Global Health. 2018;6:1077–1086. doi: 10.1016/S2214-109X(18)30357-7. [DOI] [PubMed] [Google Scholar]
- 216.Fletcher G.F., Landolfo C., Niebauer J., Ozemek C., Arena R R., Lavie C.J. J. Am. Coll. Cardiol. 2018;72:1622–1639. doi: 10.1016/j.jacc.2018.08.2141. [DOI] [PubMed] [Google Scholar]
- 217.Gualano B., Bonfa E., Pereira R.M.R., Silva C.A. Nat. Rev. Rheumatol. 2017;13:368–379. doi: 10.1038/nrrheum.2017.75. [DOI] [PubMed] [Google Scholar]
- 218.Kou L., Xiao S., Sun R., Bao S., Yao Q., Chen R. Drug Deliv. 2019;26:870–885. doi: 10.1080/10717544.2019.1660434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Ravalli S., Pulici C., Binetti S., Aglieco A., Vecchio M., Musumeci G. J. Funct. Morphol. Kinesiol. 2019;4:30. doi: 10.3390/jfmk4020030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Trayes K.P., Studdiford J.S., Pickle S., Tully A.S. Am. Fam. Physician. 2013;88:103–110. [PubMed] [Google Scholar]
- 221.Bjornstad P P., Donaghue K.C., Maahs D.M. Lancet Diabetes Endocrinol. 2018;6:809–820. doi: 10.1016/S2213-8587(18)30035-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Fiuza-Luces C., Santos-Lozano A., Joyner M., Carrera-Bastos P., Picazo O., Zugaza J.L., Izquierdo M., Ruilope L.M., Lucia A. Nat. Rev. Cardiol. 2018;15:731–743. doi: 10.1038/s41569-018-0065-1. [DOI] [PubMed] [Google Scholar]
- 223.Ulcer Disease Peptic. Clin. Gastroenterol. Hepatol. 2018;16:A31. A31. [Google Scholar]
- 224.J. Knight, Nursing Times. 2018;115:50–53. [Google Scholar]
- 225.Murphy M.A., Bergquist F., Hagström B., Hernández N., Johansson D., Ohlsson F., Sandsjö L., Wipenmyr J., Malmgren K. BMC Biomed. Eng. 2019;1:3. doi: 10.1186/s42490-019-0002-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Johansson D., Malmgren K., Alt Murphy M. J. Neurol. 2018;265:1740–1752. doi: 10.1007/s00415-018-8786-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Presti D.L., Carnevale A., D'Abbraccio J., Massari L., Massaroni C., Sabbadini R., Zaltieri M., Tocco J.D., Bravi M., Miccinilli S., Sterzi S., Longo U.G., Denaro V., Caponero M.A., Formica D., Oddo C.M., Schena E. Sensors. 2020;20:536. [Google Scholar]
- 228.Massaroni C., Tocco C.J.D., Presti D.L., Longo U.G., Miccinilli S., Sterzi S., Formica D., Saccomandi P., Schena D.-E. IEEE Sensor. J. 2019;19:7718–7725. [Google Scholar]
- 229.Goncu-Berk G., Topcuoglu N. Sapienza University of Rome; 2017. 12th EAD Conference; pp. 12–14. April. [Google Scholar]
- 230.Moineau B., Marquez-Chin C., Alizadeh-Meghrazi M., Popovic M.R. J. Rehabil. Assist. Technol. Eng. 2019;6:1–15. doi: 10.1177/2055668319854340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.da Costa T.D., Vara M.D.F.F., Cristino C.S., Zanella T.Z., Neto G.N.N., Nohama P. Wearable Devices. Intech Open; London, U. K: 2019. Breathing monitoring and pattern recognition with wearable sensors. [Google Scholar]
- 232.Bennett R., McDonnell C., Tyler D., Wood J. Proceedings. 2019;32:17. [Google Scholar]
- 233.Wang Q., Chen W., Timmermans A., Karachristos C., Martens J.-B., Markopoulos P. Proc. Of the 37th Annual Int. Conf. of the IEEE Engin. Med. Biol. Soc. (EMBC), IEEE; 2015. pp. 5736–5739. [DOI] [PubMed] [Google Scholar]
- 234.Ozlem K., Atalay O., Atalay A., Ince G. Springer; Berlin: 2019. International Conference on Neuro Rehabilitation (ICNR 2018), Cham, Switzerland, Converging Clinical and Engineering Research on Neurorehabilitation III; pp. 395–399. [Google Scholar]
- 235.Drăgulinescu A., Drăgulinescu A.-M., Zincă G., Bucur D., Neagu V. Feieș D.-M. Sensors. 2020;20:4316. doi: 10.3390/s20154316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Oks A., Katashev A., Bernans E., Abolins V. Rezekne; Latvia: 2017. Proceedings of the International Scientific and Practical Conference on Environment Technology Resources; pp. 238–241. [Google Scholar]
- 237.Elliott M., Coventry A. Br. J. Nurs. 2012;21:621–625. doi: 10.12968/bjon.2012.21.10.621. [DOI] [PubMed] [Google Scholar]
- 238.Deen M.J. Personal Ubiquitous Comput. 2015;19:573–599. [Google Scholar]
- 239.Rodrigues M.J., Postolache O., Cercas F. Sensors. 2020;20:2186. doi: 10.3390/s20082186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Majumder S., Mondal T., Deen M. Sensors. 2017;17:130. doi: 10.3390/s17010130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Baek S., Lee Y., Baek J., Kwon J., Kim S., Lee S., Strunk K.-P., Stehlin S., Melzer C., Park S.-M., Ko H., Jung S. ACS Nano. 2022;16:368–377. doi: 10.1021/acsnano.1c06695. [DOI] [PubMed] [Google Scholar]
- 242.Chen G., Au C., Chen J. Trends Biotechnol. 2021;39:1078–1092. doi: 10.1016/j.tibtech.2020.12.011. [DOI] [PubMed] [Google Scholar]
- 243.Zhao X., Zhou Y., Xu J., Chen G., Fang Y., Tat T., Xiao X., Song Y., Li S., Chen J. Nat. Commun. 2021;12:6755. doi: 10.1038/s41467-021-27066-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Han S., Kim J., Won S.M., Ma Y., Kang D., Xie Z., Lee K.-T., Chung H.U., Banks A., Min S., Heo S.Y., Davies C.R., Lee J.W., Lee C.-H., Kim B.H., Li K., Zhou Y., Wei C., Feng X., Huang Y., Rogers J.A. Sci. Transl. Med. 2018;10:4950. doi: 10.1126/scitranslmed.aan4950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Garcia M.C., Vieira T.M.M. Rev. Andal. Med. Deport. 2011;4:17–28. [Google Scholar]
- 246.Acar G., Ozturk O., Golparvar A.J., Elboshra T.A., Böhringer K., Yapici M.K. Electronics. 2019;8:479. [Google Scholar]
- 247.Turker H., Soze H. Electrodiagnosis in New Frontiers of Clinical Research. InTech; London, UK: 2013. Surface electromyography in sports and exercise. [Google Scholar]
- 248.Niijima A., Isezaki T., Aoki R., Watanabe T., Yamada T. Proceedings of the 2017 ACM international symposium on wearable computers-ISWC17. Maui, Hawaii. 2017:11–15. September. [Google Scholar]
- 249.Shafti A., Manero R.B.R., Borg A.M., Althoefer K., Howard M.J. IEEE Eng. Med. Biol. Mag. 2017;25:1472–1480. doi: 10.1109/TNSRE.2016.2633506. [DOI] [PubMed] [Google Scholar]
- 250.Tikkanen O., Hu M., Vilavuo T., Tolvanen P., Cheng S., Finni T. Physiol. Meas. 2012;33:603–614. doi: 10.1088/0967-3334/33/4/603. [DOI] [PubMed] [Google Scholar]
- 251.Zhang R., Bernhart S., Amft O. BSN); San Francisco, CA, USA: 2016. Proceedings of the IEEE 13th International Conference on Wearable and Implantable Body Sensor Networks; pp. 14–17. [Google Scholar]
- 252.Sornmo P., Laguna L. Bioelectrical Signal Processing in Cardiac and Neurological Applications. Elsevier Academic Press; Burlington, NJ, USA: 2005. The electrocardiogram-a brief background. [Google Scholar]
- 253.Löfhede J., Seoane F., Thordstein M.J.S. Sensors. 2012;12:16907–16919. doi: 10.3390/s121216907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.La T.G., Qiu S., Scott D.K., Bakhtiari R., Kuziek J.W., Mathewson K.E., Rieger J., Chung H.J. Adv. Healthc. Mater. 2018;7 doi: 10.1002/adhm.201801033. [DOI] [PubMed] [Google Scholar]
- 255.Fang Y., Zou Y., Xu J., Chen G., Zhou Y., Deng W., Zhao X., Roustaei M., Hsiai T.K., Chen J. Adv. Mater. 2021;33 doi: 10.1002/adma.202104178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Zhou Z., Chen K., Li X., Zhang S., Wu Y., Zhou Y., Meng K., Sun C., He Q., Fan W., Fan E., Lin Z., Tan X., Deng W., Yang J., Chen J. Nat. Electron. 2020;3:571. [Google Scholar]
- 257.Zou H., Zhang Y., Guo L., Wang P., He X., Dai G., Zheng H., Chen C., Wang A.C., Xu C., Wang Z.L. Nat. Commun. 2019;10:1427. doi: 10.1038/s41467-019-09461-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Yang Y., Wei1 X., Zhang N., Zheng J., Chen X., Wen Q., Luo X., Lee C.-Y., Liu X., Zhang X., Chen J., Tao C., Zhang W., Fan X. Nat. Commun. 2021;12:4876. doi: 10.1038/s41467-021-25075-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Yang J., Liu Q., Deng Z., Gong M., Lei F., Zhang J., Zhang X., Wang Q., Liu Y., Wu Z., Guo C.F. Mater. Today Phys. 2019;8:78–85. [Google Scholar]
- 260.Wan Y., Wang Y., Guo C.F. Mater. Today Phys. 2017;1:61–73. [Google Scholar]
- 261.Wan Y., Qiu Z., Hong Y., Wang Y., Zhang J., Liu Q., Wu Z., Guo C.F. Adv. Electron. Mater. 2018;4 [Google Scholar]
- 262.Meng K., Zhao S., Zhou Y., Wu Y., Zhang S., He Q., Wang X., Zhou Z., Fan W., Tan X., Yang J., Chen J. Matter. 2020;2:896–907. [Google Scholar]
- 263.Luo J., Gao S., Luo H., Wang L., Huang X., Guo Z., Lai X., Lin L., Lic R.K.Y., Gao J. Chem. Eng. J. 2021;406 [Google Scholar]
- 264.Liu L.-X., Chen W., Zhang H.-B., Wang Q.-W., Guan F., Yu Z.-Z. Adv. Funct. Mater. 2019;29 [Google Scholar]
- 265.Maymone M.B.C., Watchmaker J.D., Dubiel M., Wirya Stephen A., Shen L.Y., Vashi N.A. J. Pediatr. Health Care. 2019;33:727–737. doi: 10.1016/j.pedhc.2019.04.019. [DOI] [PubMed] [Google Scholar]
- 266.Hay R.J., Johns N.E., Williams H.C., Bolliger I.W., Dellavalle R.P., Margolis D.J., Marks R., Naldi L., Weinstock M.A., Wulf S.K., Michaud C., J L Murray C., Naghavi M. J. Invest. Dermatol. 2014;134:1527–1534. doi: 10.1038/jid.2013.446. [DOI] [PubMed] [Google Scholar]
- 267.World Health Organization (WHO) Scientific and Cultural Organization (UNESCO); 2016. The United Nations Educational. [Google Scholar]
- 268.Hellman J., Ramirez C.A. J. Cosmet. Dermatol. Sci. Applications. 2014;4:179–184. [Google Scholar]
- 269.Barolet D. Semin. Cutan. Med. Surg. 2008;27:227–238. doi: 10.1016/j.sder.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 270.Bpac N.Z., Best Pract. J. 2012;43:6–13. [Google Scholar]
- 271.Katelaris C.H., Peake J.E. Med. J. Aust. 2006;185:517–522. doi: 10.5694/j.1326-5377.2006.tb00670.x. [DOI] [PubMed] [Google Scholar]
- 272.English J.S.C., Dawe R.S., Ferguson J. Br. Med. Bull. 2003;68:129–142. doi: 10.1093/bmb/ldg026. [DOI] [PubMed] [Google Scholar]
- 273.UpToDate. 2013. Clinical manifestations of unconjugated hyperbilirubinemia in term and late preterm infants. 2014. Retrieved August 22, 2014. [Google Scholar]
- 274.Bhutani V.K., Zipursky A., Blencowe H., Khanna R., Sgr M., Ebbesen F., Bell J., Mori R., Slusher T.M., Fahmy N., Paul V.K., Du L., Okolo A.A., de Almeida M.F., O Olusanya B., Kumar P., Cousens S., Lawn J.E. Pediatr. Res. 2013;74:86–100. doi: 10.1038/pr.2013.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Azeemi S.T.Y., Raza S.M. E. Complement Alternat Med. 2005;2:481–488. doi: 10.1093/ecam/neh137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Koo M., Park S.Y., Lee K.J. Nanobiosensors Dis. Diagnosis. 2012;1:1–15. [Google Scholar]
- 277.Russell B.A., Kellett N., Reilly L.R. J. Cosmet. Laser Ther. 2005;7:196–200. doi: 10.1080/14764170500370059. [DOI] [PubMed] [Google Scholar]
- 278.Maisels M.J., McDonagh A.F. N. Engl. J. Med. 2008;358:920–928. doi: 10.1056/NEJMct0708376. [DOI] [PubMed] [Google Scholar]
- 279.Gong Z., Xiang Z., OuYang X., Zhang J., Lau N., Zhou J., Chan C.C. Materials. 2019;12:3311. doi: 10.3390/ma12203311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Yeh N.G., Wu C.-H., Cheng T.C. Renew. Sustain. Energy Rev. 2010;14:2161–2166. [Google Scholar]
- 281.Sorbellini E., Rucco1 M., Rinaldi F. Laser Med. Sci. 2018;33:1431–1439. doi: 10.1007/s10103-018-2584-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Vaishnodevi S., Nair Sajith S. Int. J. Sci. Res. 2015;4:458–461. [Google Scholar]
- 283.Stahl F., Ashworth S.H., Jandt K.D., Mills R.W. Biomaterials. 2000;21:1379–1385. doi: 10.1016/s0142-9612(00)00029-6. [DOI] [PubMed] [Google Scholar]
- 284.Kwon H.H., Lee J.B., Yoon J.Y., Park S.Y., Ryu H.H., Park B.M., Kim Y.J., Suh D.H. Br. J. Dermatol. 2013;168:1088–1094. doi: 10.1111/bjd.12186. [DOI] [PubMed] [Google Scholar]
- 285.Tsegay F., Elsherif M., But H. Polymers. 2022;14:1012. doi: 10.3390/polym14051012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Bhar B., Chouhan D., Pai N., Mandal B.B. ACS Appl. Bio Mater. 2021;4:7738–7763. doi: 10.1021/acsabm.1c00880. [DOI] [PubMed] [Google Scholar]
- 287.Moradian S., Klapper A.M. Int. Wound J. 2016;13:283–286. doi: 10.1111/iwj.12426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Sen C.K. Adv. Wound Care. 2021;10:281–292. doi: 10.1089/wound.2021.0026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Sen C.K. Adv. Wound Care. 2019;8:39–48. doi: 10.1089/wound.2019.0946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Yin D., Chen Z.-Y., Jiang N.-R., Liu Y.-F., Bi Y.-G., Zhang X.-L., Han W., Feng J., Sun H.-B. Org. Electron. 2020;76 [Google Scholar]
- 291.Zhang Z., Guo K., Li Y., Li X., Guan G., Li H., Luo Y., Zhao F., Zhang Q., Wei B., Pei Q., Peng H. Nat. Photonics. 2015;9:233–238. [Google Scholar]
- 292.Cios A., Ciepielak M., Szyma Ł., Lewicka A., Cierniak S., Stankiewicz W., Mendrycka M., Lewicki S. Int. J. Mol. Sci. 2021;22:2437. doi: 10.3390/ijms22052437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Mordon S., Thécua E., Ziane L., Lecomte F., Deleporte P., Baert G., Vignion-Dewalle A.-S. Transl. Biophotonics. 2020;2 [Google Scholar]
- 294.Fidanboylu K., Efendioğlu H.S. Fiber optics sensors and their applications. Symp. A Q. J. Mod. Foreign Lit. 2009:1–6. [Google Scholar]
- 295.Mordon S., Cochrane C., Tylcz J.B., Betrouni N., Mortier L., Koncar V. Photodiagnosis Photodyn. Ther. 2015;12:1–8. doi: 10.1016/j.pdpdt.2014.11.002. [DOI] [PubMed] [Google Scholar]
- 296.Waltz E. IEEE Spectrum; 2017. Light up Pajamas to Treat Babies with Jaundice.https://spectrum.ieee.org/the-human-os/biomedical/devices/lightup-pajamas-to-treat-babies-with-jaundice Accessed: [Google Scholar]
- 297.Samaneh R., Ali Y., Mostafa J., Mahmud N.A., Zohre R. Biosci. Biotech. Res. Asia. 2015;12:217–223. [Google Scholar]
- 298.Texinov Technical textiles, France. 2022. https://www.texinov.com/ May Accessed.
- 299.Ibe O., Morency E., Sosa P., Burkow-Heikkinen L. Healthy Aging Res. 2015;4:24. [Google Scholar]
- 300.Chia Y.-Y., Liu C.-C., Feng G.-M., Tseng C.-C.A., Hung K.-C., Chen C.-C., Tan P.-H. Pain Res. Manag. 2017;2017 doi: 10.1155/2017/4792489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Mostafalu P., Kiaee G., Giatsidis G., Khalilpour A., Nabavinia M., Dokmeci M.R., Sonkusale S., Orgill D.P., Tamayol A., Khademhosseini A. Adv. Funct. Mater. 2017;27 [Google Scholar]
- 302.Panzarasa G., Osypova A., Toncelli C., Buhmann M.T., Rottmar M., Ren Q., Maniura-Weber K., Rossi R., Boesel L.F. Sensors Actuat. B-Chem. 2017;249:156–160. [Google Scholar]
- 303.Dong R., Guo B. Nano Today. 2021;41 [Google Scholar]
- 304.Gokarneshan N. Res. Rev. Health Care Open Acc. J. 2018;2:103–106. [Google Scholar]
- 305.Ganchev I., Garcia N.M., Dobre C., Mavromoustakis C.X., Goleva R. Enhanced living environments. Springer Open, LNCS. 2019;11369:226–262. [Google Scholar]
- 306.Mendes J.J., Jr., Vieira M.E., Pires M.B., Stevan S.L., Jr. Sensors. 2016;16:10. doi: 10.3390/s16101569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Miller B., LaPenta D. 11 December. University of Delaware; 2017. https://www.udel.edu/udaily/2017/december/figure-skating-biomechanics-olympics/ (Sharpening that Competitive Edge). Accessed at. [Google Scholar]
- 308.Losina E., Paltiel A.D., Weinstein A.M., Yelin E., Hunter D.J., Chen S.P. Arthritis Care Res. 2015;67:203–215. doi: 10.1002/acr.22412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.Gholami M., Ejupi A., Rezaei A., Ferrone A., Menon C. 7th IEEE International Conference on Biomedical Robotics and Biomechatronics. 2018:589. [Google Scholar]
- 310.Yamada T., Hayamizu Y., Yamamoto Y., Yomogida Y., Izadi-Najafabadi A., Futaba D.N., Hata K. Nat. Nanotechnol. 2011;6:296–301. doi: 10.1038/nnano.2011.36. [DOI] [PubMed] [Google Scholar]
- 311.Cheng J., Sundholm M., Zhou B., Hirsch M., Lukowicz P. Pervasive Mob. Comput. 2016;30:97–112. [Google Scholar]
- 312.Niu S., Matsuhisa N., Beker L., Li J., Wang S., Wang J., Jiang Y., Yan X., Yun Y., Burnett W., Poon A.S.Y., Tok J.B.-H., Chen X., Bao Z. Nat. Electron. 2019;2:361–368. [Google Scholar]
- 313.Kim S.J., Kim H., Ahn J., Hwang D.K., Ju H., Park M.-C., Yang H., Kim S.H., Jang H.W., Lim J.A. Adv. Mater. 2019;31 doi: 10.1002/adma.201900564. [DOI] [PubMed] [Google Scholar]
- 314.Son D., Lee J., Qiao S., Ghaffari R., Kim J., Lee J.E., Song C., Kim S.J., Lee D.J., Jun S.W., Yang S., Park M., Shin J., Do K., Lee M., Kang K., Hwang C.S., Lu N., Hyeon T., Kim D.H. Nat. Nanotechnol. 2014;9:397–404. doi: 10.1038/nnano.2014.38. [DOI] [PubMed] [Google Scholar]
- 315.Choudhry N.A., Rasheed A., Ahmad S., Arnold L., Wang L. IEEE Sensor. J. 2020;20:10485–10494. [Google Scholar]
- 316.Wang L., Wang L., Zhang Y., Pan J., Li S., Sun X., Zhang B., Peng H. Adv. Funct. Mater. 2018;28 [Google Scholar]
- 317.Park H., Kim J.W., Hong S.Y., Lee G., Lee H., Song C., Keum K., Jeong Y.R., Jin S.W., Kim D.S., Ha J.S. ACS Nano. 2019;13:10469–10480. doi: 10.1021/acsnano.9b04340. [DOI] [PubMed] [Google Scholar]
- 318.Raza T., Tufail M.K., Ali A., Boakye A., Qi X., Ma Y., Ali A., Qu L., Tian M. ACS Appl. Mater. Interfaces. 2022;14:54170–54181. doi: 10.1021/acsami.2c14847. [DOI] [PubMed] [Google Scholar]
- 319.Chen P., Kuang Y., Li J. J. Sens. 2016;49 [Google Scholar]
- 320.Patiño A.G., Khoshnam M., Menon C. Sensors. 2020;20:905. doi: 10.3390/s20030905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321.Dias D., Paulo Silva Cunha J. Sensors. 2018;18:2414. doi: 10.3390/s18082414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 322.Zaman S.U., Tao X., Cochrane C., Koncar V. IOP Conf. Ser. Mater. Sci. Eng. 2019;459 [Google Scholar]
- 323.Matsuhisa N., Kaltenbrunner M., Yokota T., Jinno H., Kuribara K., Sekitani T., Someya T. Nat. Commun. 2015;6:7461. doi: 10.1038/ncomms8461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324.Heo J.S., Hossain M.F., Kim I. Sensors. 2020;20:3927. doi: 10.3390/s20143927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 325.Tao X., Koncar V., Huang T.-H., Shen C.-L., Ko Y.-C., Jou G.-T. Sensors. 2017;17:673. doi: 10.3390/s17040673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 326.Rotzler S., Schneider-Ramelow M. Textiles. 2021;1:37. [Google Scholar]
- 327.Egan J., Salmon S. SN Appl. Sci. 2022;4:22. [Google Scholar]
- 328.Samir A., Ashour F.H., Hakim A.A.A. npj Mater. Degrad. 2022;6:68. [Google Scholar]
- 329.He X., Fan C., Xu T., Zhang X. Nano Lett. 2021;21:8880–8887. doi: 10.1021/acs.nanolett.1c03426. [DOI] [PubMed] [Google Scholar]
- 330.Wang Y., Ren J., Lv Z., Cao L., Lin S., Pei Y., Zhang Q., Shao Z., Ling S. Chem. Eng. J. 2022;435 [Google Scholar]
- 331.Li J., Li S., Huang J., Khan A.Q., An B., Zhou X., Liu Z., Zhu M. Adv. Sci. 2022;9 doi: 10.1002/advs.202103965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 332.Wang C., Xia K., Zhang Y., Kalpan d. l. Acc. Chem. Res. 2019;52:2916–2927. doi: 10.1021/acs.accounts.9b00333. [DOI] [PubMed] [Google Scholar]
- 333.Ye C., Ren J., Wang Y., Zhang W., Qian C., Han J., Zhang C., Jin K., Buehler M.J., Kalpan D.K., Ling S. Matter. 2019;1:1411–1425. [Google Scholar]
- 334.Wu R., Ma L., Hou C., Meng Z., Guo W., Yu W., Yu R., Hu F., Liu X.Y. Small. 2019;15 doi: 10.1002/smll.201901558. [DOI] [PubMed] [Google Scholar]
- 335.O-Charoen N., Kampeerapappun P., Charoenlarp K., Petchwattana N., Jansri E. Recycling. 2022;7:78. [Google Scholar]
- 336.Mauriello M.L., Gubbels M., Froehlich J.E. Canada; Toronto: 2014. CHI 2014. May. [Google Scholar]
- 337.Sugathan M., Hendry D. Int. J. Technol. Diffusion (IJTD) 2017;8:3. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.