Abstract
This systematic review examined the audiological and nonaudiological factors that influence hearing help-seeking and hearing aid uptake in adults with hearing loss based on the literature published during the last decade. Peer-reviewed articles published between January 2011 and February 2022 were identified through systematic searches in electronic databases CINAHL, PsycINFO, and MEDLINE. The review was conducted and reported according to the PRISMA protocol. Forty-two articles met the inclusion criteria. Seventy (42 audiological and 28 nonaudiological) hearing help-seeking factors and 159 (93 audiological and 66 nonaudiological) hearing aid uptake factors were investigated with many factors reported only once (10/70 and 62/159, respectively). Hearing aid uptake had some strong predictors (e.g., hearing sensitivity) with others showing conflicting results (e.g., self-reported health). Hearing help-seeking had clear nonpredictive factors (e.g., education) and conflicting factors (e.g., self-reported health). New factors included cognitive anxiety associated with increased help-seeking and hearing aid uptake and urban residency and access to financial support with hearing aid uptake. Most studies were rated as having a low level of evidence (67%) and fair quality (86%). Effective promotion of hearing help-seeking requires more research evidence. Investigating factors with conflicting results and limited evidence is important to clarify what factors support help-seeking and hearing aid uptake in adults with hearing loss. These findings can inform future research and hearing health promotion and rehabilitation practices.
Keywords: hearing loss, hearing aid, help-seeking, uptake, adoption, systematic review
Introduction
Unaddressed hearing loss can have severe negative consequences with pervasive effects across the life course (Huddle et al., 2017; Nordvik et al., 2018; Olusanya et al., 2014). If addressed in a timely and appropriate manner, the adverse consequences of hearing loss can largely be avoided or mitigated (World Health Organization, 2021). Hearing aids are most commonly used to rehabilitate hearing loss and can improve listening abilities as well as health-related quality of life (Ferguson et al., 2017). However, a significant proportion of people with hearing loss does not seek help for their hearing problems and does not acquire hearing aids (Orji et al., 2020). Research has shown that people wait 9 years on average to seek help for their hearing loss (Simpson et al., 2019). In a national study in the United States, 32% of adults with hearing difficulty reported never having seen a physician about their hearing problems and 28% never had a hearing test (Mahboubi et al., 2018). Studies from other countries, especially in low- and middle-income countries, have similarly reported low levels of hearing help-seeking. In Malaysia, only 29% of adults who had self-perceived hearing loss sought professional help (Mukari & Wan Hashim, 2018). A study done by Schönborn et al. (2020) in South Africa reported that only 14% of people who failed an app-based digits-in-noise hearing test followed up with an audiologist. Worldwide, the hearing aid uptake numbers have been low with fewer than 11% of people with disabling hearing loss acquiring hearing aids (Bisgaard et al., 2021). Moreover, longitudinal population-based studies revealed that the 5- and 10-year incidence rates of hearing aid adoption by people who exhibited hearing loss at baseline were approximately 8.5% and 36%, respectively (Fischer et al., 2011; Gopinath et al., 2011).
In the last decade, there have been significant efforts to improve access to hearing healthcare services (Blazer et al., 2016). They include mobile health applications for promotion, screening, diagnosis, treatment, and support for hearing loss (Frisby et al., 2021), tele-audiology services such as home-based otoscopy, online hearing screenings, and remote hearing aid fittings (D’Onofrio & Zeng, 2022), as well as computational audiology (Wasmann et al., 2021). Computational audiology can be used to expand telehealth by incorporating clinical expertise into algorithms that can be employed on devices used by patients in underserved areas (Wasmann et al., 2021). Furthermore, a technological revolution in hearing aids has led to more affordable and accessible options such as direct-to-consumer hearing devices (Manchaiah et al., 2017). Despite these efforts, hearing help-seeking and hearing aid uptake remain low. This may be explained by a wide range of audiological and nonaudiological factors influencing hearing help-seeking and hearing aid uptake.
Various reviews have investigated the factors affecting hearing help-seeking and hearing aid uptake (Jenstad & Moon, 2011; Knudsen et al., 2010; Meyer & Hickson, 2012; Ng & Loke, 2015). A comprehensive review by Knudsen et al. (2010) investigated factors influencing hearing help-seeking, hearing aid uptake, use, and satisfaction. The authors identified 31 factors (personal, demographic, and external factors) relating to the outcomes. Motivation by others to seek help for hearing loss showed a positive association with help-seeking as opposed to being self-motivated. Hearing aid uptake was positively affected by attitudes toward hearing aids. Greater acceptance of hearing loss and poorer hearing sensitivity had a positive effect on both help-seeking and hearing aid uptake. Furthermore, age and gender did not show any relationship with any of the outcomes but that self-reported hearing disability positively influenced all four outcomes. The most recent review by Meyer and Hickson (2012) that explored the factors influencing both hearing help-seeking and hearing aid uptake concluded that people are more likely to seek help for their hearing problems and/or adopt hearing aids if they have moderate to severe hearing loss and self-reported hearing-related activity limitations or participation restrictions, are older, perceive their hearing as poor, consider there to be more benefits than barriers to amplification and perceive their significant others as supportive of hearing rehabilitation. Meyer and Hickson (2012) also mentioned that the influence of some factors requires further investigation, for example, ethnicity, education, and employment, due to a limited number of studies and/or conflicting results within the literature. Since previous reviews, there has been an increasing number of investigations to better understand factors affecting help-seeking and hearing aid uptake (e.g., Humes & Dubno, 2021; Pronk et al., 2017; Sawyer et al., 2020; Singh & Launer, 2018). This systematic review, therefore, aims to review and summarize the evidence concerning the audiological and nonaudiological factors that influence hearing help-seeking and hearing aid uptake in adults with hearing loss based on the research evidence published during the last decade.
Method
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 guidelines were followed in performing and reporting of this review (Page et al., 2021). The review protocol was registered on the International Prospective Register of Systematic Reviews (PROSPERO) (CRD42022312208).
Search Strategy
The primary reviewer (MK) searched for relevant articles in electronic databases including CINAHL, PsycINFO, and MEDLINE. The search was conducted using key terms: (hearing OR “hearing loss” OR “hearing impair*” OR “hearing diff*” OR “hearing disability” OR “hearing problem” OR “hard of hearing”) AND (“hearing aid” OR “hearing device” OR amplification OR “audiological rehabilitation*” OR “aural rehab*” OR “auditory rehab*” AND “help seeking” OR help OR advice OR uptake OR adopt* OR acqui* OR purchase OR refusal OR reject* OR adherent OR nonadherent OR candidate OR applicant). Limiters included language (only studies published in English were considered) and publication period (only studies published after January 1, 2011, were considered). A final search was done on June 1, 2022, but no additional studies were found during this search.
Eligibility Criteria
The Population Intervention Comparison Outcome Study Design Timeline framework was used to select the inclusion and exclusion criteria for the review:
Population: Studies including adults (18 years and older) with hearing loss (either self-reported hearing difficulties or confirmed hearing loss based on a hearing screening or assessment) were included. Studies including adults without hearing loss or children (younger than 18 years) were excluded.
Intervention/Exposure: The intervention for hearing help-seeking referred to an action toward seeking help for hearing loss (i.e., making an appointment to consult with a hearing healthcare professional). With regard to hearing aid uptake, the intervention was obtaining conventional air-conduction hearing aids.
Comparison: The review included studies in all settings and contexts.
Outcome: Studies focusing on hearing help-seeking (e.g., consulting professionals, performing online hearing screening) and hearing aid uptake were included. When studies focused on multiple outcomes (e.g., hearing help-seeking, hearing aid uptake, hearing aid use, and satisfaction/benefit), we only extracted and reported on the outcomes relevant to this review (i.e., hearing help-seeking and hearing aid uptake). Studies focusing on hearing aid use and hearing aid benefit/satisfaction alone were excluded as were studies dealing with amplification devices other than conventional hearing aids (e.g., cochlear implants, middle-ear implants, bone-anchored hearing aids, and assistive listening devices).
Study Design: Quantitative studies with any design were included. Qualitative studies were excluded from this review to be in line with the previous reviews by Knudsen et al. (2010) and Meyer and Hickson (2012) for comparative data. Knudsen et al. (2010) also excluded qualitative studies, and Meyer and Hickson (2012) mostly focused on quantitative studies (20 out of the 22 included studies were quantitative).
Timeline: Studies published between January 1, 2011, and February 2, 2022, were included.
Other: Studies published in peer-reviewed scientific journals were eligible for inclusion. Nonpeer-reviewed publications, discussion papers, dissertations/theses, and conference papers were excluded. Only studies published in English were included in the review.
Selection Procedure
The study selection was carried out by two researchers (MK and BM) independently. Articles were exported from the databases into Rayyan (https://www.rayyan.ai/). The Rayyan software was used for screening studies and to record decisions. Firstly, duplicate articles were removed. Thereafter, studies were screened based on their titles and abstracts with regard to the inclusion criteria, while the researchers were blinded to each other's decisions. The full-text article was retrieved and reviewed if a decision could not be made based on the abstract. Subsequently, the reference lists of the identified publications were checked for additional studies to be included in the review. There were disagreements in 20% of the articles. Disagreements were resolved by discussion and involving other research team members (VM and DWS). The full-text PDF versions of the articles that met the inclusion criteria were inspected closely to extract the relevant data.
Data Extraction
Microsoft Excel was used for data extraction and management. A specific form was used to summarize the information obtained from the articles. It included the following elements: Publication (e.g., reference, authors, title, country of study, and date of publication), study design (e.g., aim, study design, data collection method, and data analysis method), population (e.g., sampling method, sample size, age of participants, and gender of participants), factor(s) examined (audiological and nonaudiological factors), and outcomes (e.g., key findings, associations, and the direction of effect). The primary reviewer (MK) extracted all the data, and the second reviewer (BM) cross-checked 20% of the data using a random number generator to ensure completeness and accuracy. There were disagreements in 14% of the articles, mostly relating to the study designs and sampling methods. These were resolved by discussion and involving other research team members (VM and DWS).
Risk of Bias (Quality) Assessment and Determination of Level of Evidence
The National Institute of Health (NIH) quality assessment tools were used to assess the quality of the studies included in the review (National Institute of Health, 2021). The NIH tools are specific to certain study designs and were designed to assist reviewers in focusing on concepts that are important in determining a study's internal validity (National Institute of Health, 2021). Reviewers could respond with “yes,” “no,” or “cannot determine/not reported/not applicable” to each item on the tool. In the end, every “yes” represented 1 point. The reviewers added up the points to determine the total score and decide whether the study should be rated as good, fair, or poor quality. To prevent bias, the NIH tool does not provide specific parameters to rate the quality as good, fair, or poor since each study should be assessed on its own. However, we used parameters as specified in another systematic review as a guide on how to rate the quality, where a score of 0–4 was rated as poor, 5–10 as fair, and 11–14 as good (Bagias et al., 2021). The level of evidence was determined according to the Oxford Centre for Evidence-Based Medicine Levels of Evidence based on each study's design (OCEBM Levels of Evidence Working Group, 2011). We used the OCEBM hierarchy of evidence (level 1 being the highest level of evidence) as it was created for researchers to easily identify the likely best evidence. The primary reviewer (MK) conducted the quality assessment and the determination of the level of evidence. The second reviewer (BM) cross-checked 20% using a random number generator to ensure reliability. There were disagreements in 5% of the articles, mostly relating to the participation rate. These were resolved by discussion and involving other research team members (VM and DWS).
Data Synthesis
Due to the high heterogeneity of included studies, the synthesis without meta-analysis (SWiM) reporting guidelines as described by Campbell et al. (2020) was used to identify, characterize, and summarize available research evidence on audiological and nonaudiological factors influencing hearing help-seeking and hearing aid uptake. Vote counting based on the direction of effect was selected as the synthesis method (Campbell et al., 2020). The synthesis was conducted by the primary reviewer (MK) and was approved by the rest of the research team (BM, VM, and DWS).
Results
Search and Study Selection
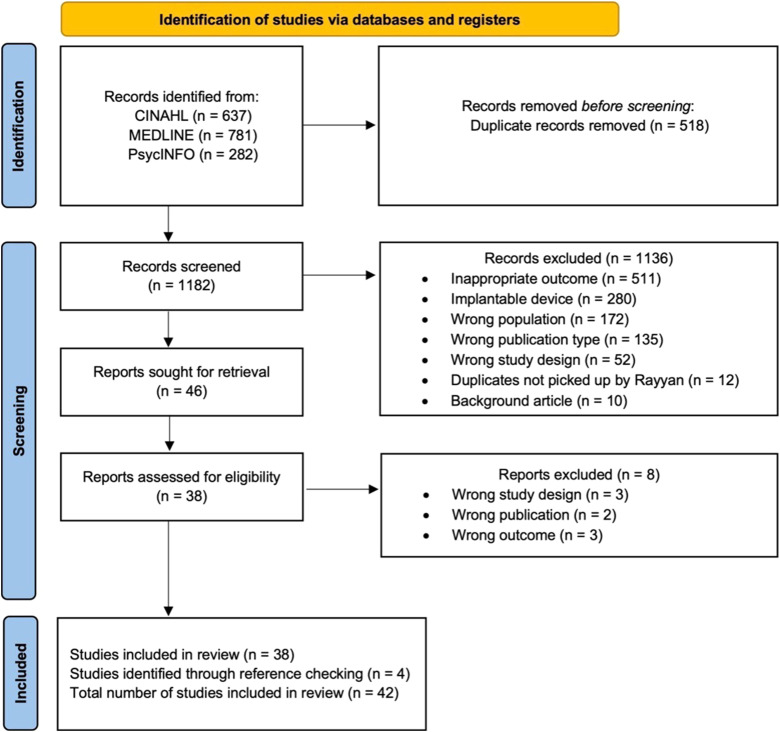
The search identified 637 records on CINAHL, 781 on MEDLINE, and 282 on PsycINFO. After removing 518 duplicates, 1182 records were screened based on their titles and abstracts. Full texts of 46 articles were assessed for eligibility. Of these, eight were excluded (three had an inappropriate study design, two had the wrong publication type, and three were focused on an inappropriate outcome, e.g., hearing aid use). Four additional studies were identified through reference checking. Therefore, a total of 42 studies were included in the review (see Figure 1).
Figure 1.
PRISMA Flow Diagram of the Selection Process.
Study Characteristics
Table 1 summarizes the key characteristics of the included studies (n = 42). Sixteen studies were conducted in the Americas (38%), nine in Australia (21%), eight in Europe (19%), five in Asia (12%), and four in the United Kingdom (10%). Most studies were cross-sectional or cohort studies except for one true experimental study (Adorni et al., 2021) and one cluster randomized controlled trial in which groups of individuals were randomized (Pronk et al., 2019). Thirty studies (71%) were prospective and 12 were retrospective (29%). Convenience (26% of the studies) and purposive (14% of the studies) sampling were the most used sampling methods. Both these are nonprobability sampling techniques. A convenience sample is drawn from a population that is easily accessible to the researcher, whereas a purposive sample is intentionally selected based on the characteristics of the participants that are relevant to the study (Etikan et al., 2016). The sample size ranged from 32 to 60,964 participants. Participants’ ages ranged from 20 to 77 years. Of the 38 studies that reported the mean age of participants, the average was 68 years. Thirty studies investigated factors influencing hearing aid uptake, four studies investigated factors influencing hearing help-seeking, and eight studies investigated factors influencing both. All factors investigated for their potential influence on hearing help-seeking and hearing aid uptake are presented in Tables 2–5, but only the factors showing at least one positive or negative association are described in the text.
Table 1.
Key Characteristics of Included Articles (n = 42).
| Authors | Year | Country | Study design | Sampling method | N | Age (Mean ± SD unless otherwise reported) | Hearing help-seeking | Hearing aid uptake | Level of evidence | Quality rating |
|---|---|---|---|---|---|---|---|---|---|---|
| Cho et al. | 2022 | Korea | Cross-sectional survey (P) | NR | 1464 | 70.4 ± 12.2 | ✓ | 4 | Fair | |
| Weycker et al. | 2021 | USA | Cohort (P) | NR | 579 | 56.0 | ✓ | 3 | Fair | |
| Adorni et al. | 2021 | Italy | True-experimental (P) | Snowball | 209 | 33.9 ± 13.0 | ✓ | 2 | Fair | |
| Humes & Dubno | 2021 | USA | Cross-sectional survey (P) | Community sample: convenience Clinic samples: NR | 764 | Community: 68.6 ± 6.1 Clinic- No HA: 74.5 ± 7.0 Clinic- HA: 75.7 ± 6.7 | ✓ | ✓ | 4 | Fair |
| Van Leeuwen et al. | 2021 | Netherlands | Cohort (P) | Convenience | 218 | Across two cohorts: 48.9 ± 10.0 to 49.7 ± 11.1 | ✓ | 3 | Fair | |
| Tran et al. | 2021 | USA | Cross-sectional survey (P) | Convenience | 1376 | 54.7 ± 17.4 | ✓ | 4 | Fair | |
| Maidment & Wege | 2021 | England | Cross-sectional (R) | N/A | 17172 | Median: 77.0 | ✓ | 4 | Fair | |
| Nixon et al. | 2021 | Australia | Cohort (P) | NR | 85 | 70.2 ± 5.2 | ✓ | 4 | Fair | |
| Humes | 2021 | USA | Cohort (P) | Convenience | 139 | Adherents 74.7 ± 7.7 years Nonadherents 72.7 ± 7.0 | ✓ | 3 | Fair | |
| Chua Wei De | 2021 | Singapore | Cross-sectional (R) | N/A | 109 | Median: 76.0 | ✓ | 3 | Fair | |
| Angara et al. | 2021 | USA | Cross-sectional survey (R) | N/A | 5230 | Range: 20.0–70.0+ | ✓ | 4 | Fair | |
| Sawyer et al. | 2020 | England | Cross-sectional (R) | N/A | 2845 | 72.1 ± 9.1 | ✓ | ✓ | 4 | Poor |
| Pronk et al. | 2019 | Netherlands | Cluster randomized controlled trial (P) | NR | 267 | 66.9 | ✓ | 2 | Fair | |
| Simpson et al. | 2019 | USA | Cohort (P) | Snowball | 857 | Adopted: 69.1 ± 8.6 Not adopted: 70.2 ± 10.6 | ✓ | 3 | Fair | |
| Mukari & Hashim | 2018 | Malaysia | Cohort (P) | Stratified cluster random | 301 | 68.4 ± 6.0 | ✓ | 3 | Fair | |
| He et al. | 2018 | China | Cross-sectional (R) | Probability proportional | 1503 | 74.5 ± 6.6 | ✓ | 4 | Fair | |
| Singh & Launer | 2018 | Canada | Cohort (R) | N/A | 24842 | 75.4 ± 13.5 | ✓ | 4 | Fair | |
| Chan et al. | 2017 | USA | Cross-sectional survey (P) | NR | 336 | Urban: 66.3 Rural: 66.7 | ✓ | 4 | Fair | |
| Sciacca et al. | 2017 | Australia | Cross-sectional (P) | Audiologists: Convenience Patients: Purposive | 62 | 71.6 ± 9.1 | ✓ | 4 | Fair | |
| Pronk et al. | 2017 | Netherlands | Cross-sectional (P) | Convenience | 377 | 72.6 ± 8.0 | ✓ | 4 | Fair | |
| Singh & Launer | 2016 | UK | Cohort (R) | N/A | 60964 | Alone: 70.4 ± 12.4 With other: 74.5 ± 11.6 | ✓ | 4 | Fair | |
| Ridgway et al. | 2016 | Australia | Cohort (P) | NR | 216 | 69.6 ± 10.5 | ✓ | 3 | Fair | |
| Saunders et al. | 2016 | USA | Cohort (P) | NR | 167 | 69.3 ± 7.5 | ✓ | 3 | Fair | |
| Otavio et al. | 2016 | Brazil | Cross-sectional (P) | NR | 32 | 71.4 ± 12.1 | ✓ | 4 | Fair | |
| Ridgway et al. | 2015 | Australia | Cohort (P) | NR | 253 | 69.9 ± 10.5 | ✓ | 3 | Fair | |
| Moschis et al. | 2015 | USA | Cross-sectional survey (P) | Purposive | 477 | 58.8 ± 7.1 | ✓ | 4 | Poor | |
| Benova et al. | 2015 | England | Cross-sectional survey (R) | N/A | 8780 | Between 50.0–64.0: 46.4% Between 65.0–74.0: 29.7% 75.0+: 23.9% | ✓ | 4 | Fair | |
| Cobelli et al. | 2014 | Italy | Cross-sectional survey (P) | Purposive | 243 | 69.5 ± 8.3 | ✓ | 4 | Fair | |
| Meyer et al. | 2014 | Australia | Cross-sectional (R) | N/A | 307 | 73.0 ± 7.2 | ✓ | ✓ | 4 | Fair |
| Ham et al. | 2014 | Australia | Cross-sectional survey (P) | NR | 251 | 72.0 ± 7.0 | ✓ | ✓ | 4 | Poor |
| Kelly-Campbell & Parry | 2014 | USA | Cross-sectional (P) | Purposive | 35 | Adopters: 64.2 ± 5.1 Nonadopters: 62.0 ± 2.8 | ✓ | 4 | Good | |
| Saunders et al. | 2013 | USA | Cross-sectional survey (P) | Convenience | 223 | Male: 61.1 ± 14.1 Female: 57.7 ± 14.0 | ✓ | ✓ | 4 | Fair |
| Öberg et al. | 2012 | Sweden | Cross-sectional survey (R) | N/A | 346 | 77.0 | ✓ | ✓ | 4 | Fair |
| Robertson et al. | 2012 | USA | Cross-sectional (R) | N/A | 144 | Across three groups: 65.7 ± 2.9 to 67.6 ± 5.5 | ✓ | 4 | Fair | |
| Meyer et al. | 2011 | Australia | Cohort (P) | Stratified cluster random | 193 | 67.6 ± 12.3 | ✓ | 3 | Fair | |
| Fischer et al. | 2011 | USA | Cohort (P) | NR | 718 | 70.5 | ✓ | 3 | Fair | |
| Meister et al. | 2014 | Germany | Cross-sectional survey (P) | Convenience | 204 | 65.2 ± 9.9 | ✓ | ✓ | 4 | Fair |
| Gopinath et al. | 2011 | Australia | Cohort study (P) | Purposive | 1371 | Nonowner: 67.1 ± 7.3 Owner: 73.5 ± 7.0 User: 73.6 ± 6.9 | ✓ | 3 | Fair | |
| Kelly et al. | 2011 | USA | Cross-sectional (P) | Nonconsulters: Convenience Consulters: Purposive | 93 | Nonconsulters: 72.8 ± 4.3 Consulters: 70.6 ± 4.7 Consulters 2: 73.1 ± 6.2 | ✓ | ✓ | 4 | Poor |
| Laplante-Lévesque et al. | 2012 | Australia | Cross-sectional (P) | Convenience | 153 | Median: 70.0 | ✓ | 4 | Fair | |
| Chang et al. | 2016 | Taiwan | Cross-sectional survey (P) | Convenience | 599 | 72.1 ± 5.8 | ✓ | 4 | Fair | |
| Tahden et al. | 2018 | Germany | Cross-sectional (R) | N/A | 211 | HA nonuser: 70.6 ± 5.1 HA user: 72.1 ± 6.1 | ✓ | 4 | Fair |
Note. P = Prospective; R = Retrospective; NR = Not Reported; N/A = Not Applicable; HA = Hearing aid.
Table 2.
Audiological Factors Influencing Hearing Help-Seeking.
| Category and factors | No. of studies | Positive association | Negative association | No association |
|---|---|---|---|---|
| Hearing sensitivity | ||||
| Worst ear PTA (1, 2, 4 kHz) | 1 | 1 | - | - |
| Better ear PTA (0.5, 1, 2 kHz) | 1 | - | - | 1 |
| Better ear PTA (0.5, 1, 2, 4 kHz) | 2 | 1 | - | 1 |
| Hearing screening | ||||
| Hearing screening (1 and 3 kHz) | 1 | 1 | - | - |
| Reason for hearing screening | 1 | - | - | 1 |
| Self-reported hearing difficulties and beliefs | ||||
| Perceived hearing loss | 1 | - | - | 1 |
| Self-reported hearing disability | 1 | 1 | - | - |
| Tinnitus | 1 | - | - | 1 |
| Otorrhea | 1 | - | - | 1 |
| Hearing Beliefs Questionnaire: | ||||
| Susceptibility | 1 | 1 | - | - |
| Severity | 1 | - | - | 1 |
| Benefits | 1 | - | - | 1 |
| Barriers | 1 | - | 1 | - |
| Self-efficacy | 1 | - | - | 1 |
| Cues to action | 1 | 1 | - | - |
| Communication difficulties | ||||
| Self-assessment of communication | 1 | 1 | - | - |
| Communication Profile for the Hearing Impaired: | ||||
| Performance—social* | 1 | - | 1 | - |
| Performance—work | 1 | - | 1 | - |
| Performance—home | 1 | - | 1 | - |
| Performance—problem awareness | 1 | - | 1 | - |
| Environment—communication need | 1 | - | - | 1 |
| Environment—physical characteristics | 1 | - | - | 1 |
| Environment—attitudes of others | 1 | - | - | 1 |
| Environment—behaviors of others | 1 | - | - | 1 |
| Strategies—maladaptive behaviors | 1 | - | - | 1 |
| Strategies—verbal strategies | 1 | - | - | 1 |
| Strategies—nonverbal strategies | 1 | - | - | 1 |
| Personal adjustment—self-acceptance | 1 | - | - | 1 |
| Personal adjustment—acceptance of loss | 1 | - | - | 1 |
| Personal adjustment—anger | 1 | - | - | 1 |
| Personal adjustment—displacement of responsibility | 1 | - | - | 1 |
| Personal adjustment—exaggeration of responsibility | 1 | - | - | 1 |
| Personal adjustment—discouragement | 1 | - | - | 1 |
| Personal adjustment—stress | 1 | - | - | 1 |
| Personal adjustment—withdrawal | 1 | - | - | 1 |
| Personal adjustment—denial | 1 | - | 1 | - |
| Expectations and perceived benefits from hearing aids | ||||
| Attitude toward hearing aids: Benefits scale | 2 | 2 | - | - |
| Attitude to hearing aids | 1 | - | - | 1 |
| Attitude toward hearing aids: Negative support scale | 1 | - | - | 1 |
| Basic handling scale | 1 | - | - | 1 |
| Considered hearing aids before* | 1 | 1 | - | - |
| Other | ||||
| Noise exposure | 1 | - | - | 1 |
Note: PTA = Pure Tone Average.
*Significant factors that have not been reported in previous reviews relevant to the specific outcome.
Table 5.
Nonaudiological Factors Influencing Hearing Device Uptake.
| Category and factors | No. of studies | Positive association | Negative association | No association |
|---|---|---|---|---|
| Demographics | ||||
| Age | 25 | 8 | 1 | 16 |
| Duration in old-age roles | 1 | - | - | 1 |
| Number of transitions experienced | 1 | - | - | 1 |
| Male sex (vs. female) | 20 | 3 | 1 | 16 |
| White race (vs. other) | 4 | 2 | - | 2 |
| Education | 12 | 4 | - | 8 |
| Country of birth | 1 | - | - | 1 |
| Urban area of residence (vs. rural)* | 2 | 2 | - | - |
| Living situation | 3 | - | - | 3 |
| Marital status | 5 | 1 | - | 4 |
| Household size | 1 | - | - | 1 |
| Job | 2 | - | - | 2 |
| Job control | 1 | - | - | 1 |
| Psychological job demand* | 1 | 1 | - | - |
| Need for recovery after work | 1 | - | - | 1 |
| Retired | 1 | - | - | 1 |
| Socioeconomic status | ||||
| Socioeconomic status | 5 | 3 | - | 2 |
| Household income* | 2 | 1 | - | 1 |
| Income | 2 | - | - | 2 |
| Poverty income ratio | 1 | - | - | 1 |
| Pension* | 1 | 1 | - | - |
| Hearing healthcare funding and health insurance | ||||
| Eligibility for subsidized hearing services | 1 | - | - | 1 |
| Applied for subsidized hearing services* | 1 | 1 | - | - |
| Government assistance* | 1 | 1 | - | - |
| Senior Mobility Fund* | 1 | 1 | - | - |
| Health insurance* | 2 | 1 | - | 1 |
| Health | ||||
| Self-reported health | 4 | 2 | 2 | - |
| Chronic health conditions | 1 | - | - | 1 |
| Self-reported diabetes* | 1 | - | 1 | - |
| Self-reported hypertension* | 1 | - | 1 | - |
| Self-reported dementia | 1 | - | - | 1 |
| Self-reported history of stroke* | 1 | - | 1 | - |
| Number of diseases | 1 | - | - | 1 |
| Cognition and mental health | ||||
| Cognition | 3 | - | - | 3 |
| Cognitive reasoning: similarities* | 1 | 1 | - | - |
| Cognitive anxiety* | 2 | 2 | - | - |
| Mental health | 2 | - | - | 2 |
| Distress | 1 | - | - | 1 |
| Attention | 1 | - | - | 1 |
| Psychomotor function | 1 | - | - | 1 |
| Executive function | 1 | - | - | 1 |
| Visual learning | 1 | - | - | 1 |
| Working memory | 1 | - | - | 1 |
| Loneliness scale | 1 | - | - | 1 |
| Social network | 1 | - | - | 1 |
| Anxiety | 1 | - | - | 1 |
| Depression | 1 | - | - | 1 |
| Memory | 1 | - | - | 1 |
| Affect and personality | 1 | - | - | 1 |
| Emotional response | 1 | - | - | 1 |
| Motivation, support, subjective norms and trust | ||||
| Autonomous motivation* | 2 | 2 | - | - |
| Autonomous support | 1 | - | - | 1 |
| Controlled motivation | 1 | - | - | 1 |
| Subjective norm | 2 | 2 | - | - |
| Trust | 1 | - | - | 1 |
| Attitude X trust | 1 | - | - | 1 |
| Subjective norm X trust* | 1 | 1 | - | - |
| Attitudes toward behavior and control | ||||
| Behavioral control* | 1 | 1 | - | - |
| Attitude toward behavior* | 1 | 1 | - | - |
| Locus of control | 1 | - | - | 1 |
| Readiness for change | ||||
| Precontemplation | 3 | 1 | - | 2 |
| Contemplation | 3 | 2 | - | 1 |
| Action | 3 | 1 | - | 2 |
| Committed action | 1 | - | - | 1 |
| Other | ||||
| Self-efficacy | 1 | - | - | 1 |
| Technology commitment | 2 | 1 | - | 1 |
*Significant factors that have not been reported in previous reviews relevant to the specific outcome.
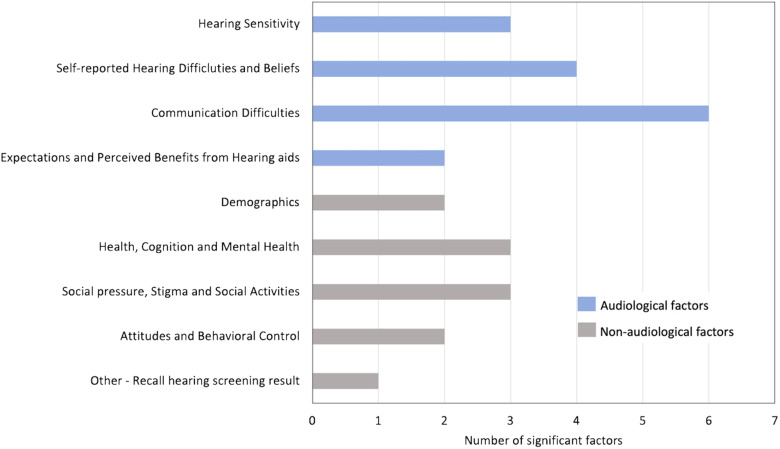
Hearing Help-Seeking
Forty-two audiological factors (see Table 2) and 28 nonaudiological factors (see Table 3) influencing hearing help-seeking were investigated in the 12 studies that focused on this topic. The number of significant factors (i.e., factors that either showed a positive or negative association) per category is shown in Figure 2, and these are discussed below. Significant factors that have not been reported in previous reviews are marked by an asterisk in Tables 2 and 3. Nonsignificant factors (i.e., factors that showed no association) are also shown in Tables 2 and 3. For more detail, see Supplementary Tables 1 and 2. Additionally, evidence from previous reviews, as reported by Knudsen et al. (2010) and Meyer and Hickson (2012), is compared to evidence from the present systematic review in Table 6.
Table 3.
Nonaudiological Factors Influencing Hearing Help-Seeking.
| Category and factors | No. of studies | Positive association | Negative association | No association |
|---|---|---|---|---|
| Demographics | ||||
| Age | 5 | 2 | - | 3 |
| Age participant felt | 1 | - | - | 1 |
| Male sex (vs. female) | 6 | 3 | - | 3 |
| Ethnicity | 2 | - | - | 2 |
| Marital status | 1 | - | - | 1 |
| Education | 3 | - | - | 3 |
| Area of residence | 2 | - | - | 2 |
| Living situation | 1 | - | - | 1 |
| Retired | 1 | - | - | 1 |
| Socioeconomic status | ||||
| Socioeconomic position | 1 | - | - | 1 |
| Wealth | 1 | - | - | 1 |
| Perceived income | 1 | - | - | 1 |
| Pension | 1 | - | - | 1 |
| Health, Cognition, and Mental Health | ||||
| Self-reported health* | 3 | 1 | 1 | 1 |
| Number of diseases | 1 | - | - | 1 |
| Cognitive performance* | 2 | 1 | - | 1 |
| Cognitive anxiety* | 1 | 1 | - | - |
| Mental health | 2 | - | - | 2 |
| Social pressure, Stigma and Social Activities | ||||
| Social pressure | 2 | 2 | - | - |
| Stigma | 1 | 1 | - | - |
| Number of social activities* | 1 | - | 1 | - |
| Number of leisure activities | 1 | - | - | 1 |
| Attitudes and Behavioral Control | ||||
| Attitude to ageing | 1 | - | - | 1 |
| Attitude toward behavior* | 1 | 1 | - | - |
| Behavioral control* | 1 | 1 | - | - |
| Other | ||||
| Source of recruitment | 1 | - | - | 1 |
| Technology | 1 | - | - | 1 |
| Recall hearing screening result* | 1 | 1 | - | - |
*Significant factors that have not been reported in previous reviews relevant to the specific outcome.
Figure 2.
Number of Significant Factors Identified Within Studies That Influence Hearing Help-Seeking for Each Category of Audiological or Nonaudiological Factors.
Table 6.
Combined Evidence from Previous Reviews, Including Knudsen et al. (2010) and Meyer and Hickson (2012), and the Current Systematic Review (2011–2022) on Factors Influencing Hearing Help-Seeking.
| Audiological factors | ||||||
|---|---|---|---|---|---|---|
| Factor | Previous reviews (<2012) | Current systematic review (2011–2022) | Combined | |||
| No. of studies | Results | No. of studies | Results | No. of studies | Results | |
| Attitudes toward hearing aids | 1 | 0 | 1 | 0 | 2 | 0, 0 |
| Attitudes toward own hearing loss | 1 | - (coping style) | No data | 1 | - | |
| Self-reported hearing problems (and/or activity limitation, participation restriction) | 5 | +, +, +, +, + | 2 | + (self-reported hearing disability), 0 (self-perceived HL) | 7 | +, +, +, +, +, +, 0 |
| Hearing sensitivity | 5 | +, +, +, +, 0 | 5 | +, +, +, 0, 0 | 10 | +, +, +, + , +, +, +, 0, 0, 0 |
| Age of hearing loss onset | 1 | + (before 65 years) | No data | 1 | + | |
| Acknowledge hearing loss | 1 | + | 1 | + (Self-assessment of communication) | 2 | +, + |
| Hearing screening | 1 | + | 1 | + | 2 | +, + |
| Nonaudiological factors | ||||||
| Age | 4 | +, 0, 0, 0 | 5 | +, +, 0, 0, 0 | 9 | +, +, +, 0, 0, 0, 0, 0, 0 |
| Male sex (vs. female) | 4 | 0, 0, 0, 0 | 6 | +, +, +, 0, 0, 0 | 10 | +, +, +, 0, 0, 0, 0, 0, 0, 0 |
| Education | 1 | + | 3 | 0, 0, 0 | 4 | +, 0, 0, 0 |
| Motivation | 2 | + (others) + (client, health professional, and family) | 2 | +, + (both social pressure) | 4 | +, +, +, + |
| General practitioner | 1 | - | No data | 1 | - | |
| Personality* | 1 | + (lower neuroticism, lower openness, pragmatic and routine orientated, higher internal locus of control) | No data | 1 | + | |
Note: Four studies from the Meyer and Hickson (2012) review were excluded from the table, including Carson (2005) and Wallhagen (2010) because they are qualitative studies as well as Kochkin (2007) and Kochkin (2009) because they are not peer-reviewed papers. “+” indicates a positive association between the factor and the outcome, “–” a negative association, and “0” no association. *Factors including multiple outcomes.
Audiological Factors
Hearing Sensitivity
Hearing sensitivity measured using pure tone audiometry was found to be positively associated with hearing help-seeking in two studies, while two studies did not show any association. Pronk et al. (2017) reported that females (and not males) were more likely to enter a hearing aid evaluation period if they had greater hearing loss severity (determined by the worst ear pure tone average [PTA] at 1, 2, and 4 kHz). Meyer et al. (2014) reported that people were more likely to seek help if they had greater hearing loss severity (determined by better ear PTA at 0.5, 1, 2, and 4 kHz) relative to people who did not seek help. Additionally, Sawyer et al. (2020) reported that people were more likely to seek help if they had greater hearing loss according to a hearing screening test at 1 and 3 kHz.
Self-Reported Hearing Difficulties and Beliefs
Greater self-reported hearing disability was found to be a significant predictor of entering a hearing aid evaluation period in one study (Pronk et al., 2017). A study by Saunders et al. (2013) assessed hearing beliefs within the constructs of the health belief model (HBM). They found that people were more likely to seek help for their hearing loss if they had higher perceived susceptibility to hearing loss, lower perceived barriers to hearing rehabilitation, and higher cues to action. Cues to action referred to the participant's experience of cues (intrinsic or extrinsic) prompting him/her to take action (e.g., the participant knew where to get a hearing test).
Communication Difficulties
Perceived communication difficulties were found to be positively associated with hearing help-seeking in two studies. Meyer et al. (2014) reported that older adults were more likely to seek help if they acknowledged their communication difficulties due to their hearing loss. Humes and Dubno (2021) found that people were less likely to seek help if they had better communication performance (in social settings, at work, and at home), less awareness of communication problems, and greater denial using the Communication Profile for the Hearing Impaired (CPHI).
Expectations and Perceived Benefits from Hearing Aids
Two studies reported that the expected benefits of hearing aids were positively associated with hearing help-seeking. Pronk et al. (2017) found that people were more likely to enter a hearing aid evaluation period if they had more expected benefits of hearing aids. Similarly, Meyer et al. (2014) found that older adults were more likely to seek help for their hearing loss if they perceived there to be many benefits of hearing aids. People were also more likely to seek help for their hearing loss if they had considered hearing aids before in one study (Meyer et al., 2011).
Nonaudiological Factors
Demographics
Although three studies did not find any associations, Sawyer et al. (2020) and Saunders et al. (2013) reported increasing help-seeking with increasing age. Three studies (Öberg et al., 2012; Saunders et al., 2013; Sawyer et al., 2020) reported that males were more likely to seek help for their hearing loss than females, although three studies reported no association between sex and help-seeking.
Health, Cognition, and Mental Health
Two studies revealed mixed findings of self-reported health and its association with hearing help-seeking. On one hand, Sawyer et al. (2020) found that people in later categories of help-seeking (e.g., “told a health professional about hearing loss”) had poorer self-reported health. On the other hand, Meyer et al. (2014) found that people were more likely to seek help if they had better self-reported health. Similarly, two studies reported mixed findings on cognitive performance and its association with hearing help-seeking. Sawyer et al. (2020) reported that people were more likely to seek help if they had better cognitive performance, although Öberg et al. (2012) did not show any association. A study by Kelly et al. (2011) concluded that people actively seeking consultation for their hearing loss have higher cognitive anxiety than those who are not seeking help or those who already received assistance. Cognitive anxiety can be defined as a transient state where a person struggles to interpret situations meaningfully and judge their implications (Viney & Westbrook, 1976).
Social Pressure, Stigma, and Social Activities
Social pressure as exerted by significant others, for example, was found to be positively associated with hearing help-seeking in two studies. Pronk et al. (2017) reported that people were more likely to enter a hearing aid evaluation period if they experienced greater social pressure. Meister et al. (2014) used a survey based on the Theory of Planned Behavior (TPB). They also reported the construct of “subjective norm” (i.e., social pressure) to be positively associated with hearing help-seeking, specifically in the initial stages. Females were more likely to seek help if they experienced hearing aid stigma in one study (Pronk et al., 2017). According to one study, people were more likely to tell a health professional about their hearing loss if they participated in fewer social activities (Sawyer et al., 2020).
Attitudes and Behavioral Control
One study reported that those who sought help for their hearing problems were positively affected by the TPB constructs “attitude toward behavior” and “behavioral control” (Meister et al., 2014). Attitude toward behavior refers to whether a person is in favor of doing the behavior and behavioral control relates to whether a person feels in control of the action (Meister et al., 2014).
Other
A study by Meyer et al. (2011) found that people were more likely to seek help if they could accurately recall their hearing screening results.
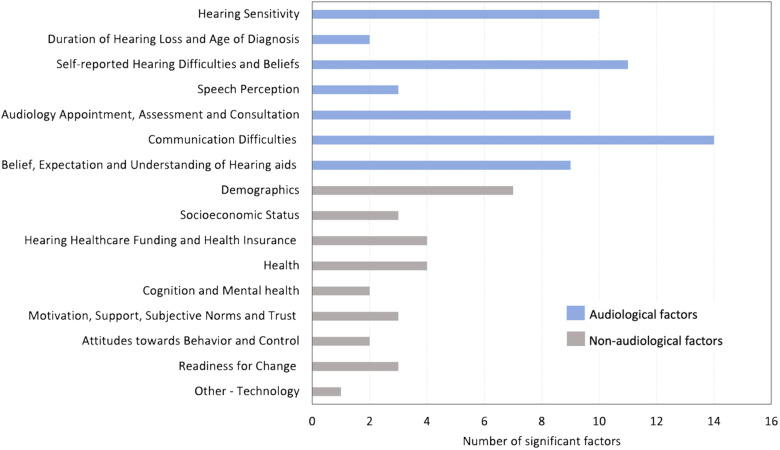
Hearing Aid Uptake
Ninety-three audiological factors (Table 4) and 66 nonaudiological factors (Table 5) influencing hearing aid uptake were investigated in 38 studies that investigated this topic. The number of significant factors (i.e., factors that either showed a positive or negative association) per category can be seen in Figure 3, and these are discussed below. Significant factors that have not been reported in previous reviews are marked by an asterisk in Tables 4 and 5. Nonsignificant factors (i.e., factors that showed no association) are also included in Tables 4 and 5. For more detail, see Supplementary Tables 3 and 4. Additionally, evidence from previous reviews, as reported by Knudsen et al. (2010) and Meyer and Hickson (2012), is compared to evidence from the present systematic review in Table 7.
Table 4.
Audiological Factors Influencing Hearing Device Uptake.
| Category and factors | No. of studies | Positive association | Negative association | No association |
|---|---|---|---|---|
| Hearing sensitivity | ||||
| Hearing screening (1 and 3 kHz) | 1 | 1 | - | - |
| Worst ear PTA (1, 2, 4 kHz) | 1 | 1 | - | - |
| Better ear PTA (0.5, 1, 2, 4 kHz) | 11 | 9 | - | 2 |
| Better ear PTA (0.5, 1, 2 kHz) | 1 | - | - | 1 |
| PTA (0.5, 1, 2, 4 kHz above 25 dB HL) | 2 | 2 | - | - |
| Mean binaural PTA (0.5, 1, 2 kHz) | 1 | 1 | - | - |
| Mean binaural PTA (0.5, 1, 2, 4 kHz) | 1 | 1 | - | - |
| High-frequency PTA (3, 4, 6, 8 kHz and 2, 3, 4, 6, 8 kHz) | 2 | 2 | - | - |
| Low-frequency PTA (0.25, 0.5, 1 kHz) | 1 | - | - | 1 |
| Degree of hearing loss (e.g., severe to profound) | 1 | 1 | - | - |
| Erber's area (includes hearing thresholds poorer than 35 dB in the frequency range below 1000 Hz)* | 1 | 1 | - | - |
| Bilateral hearing loss* | 1 | 1 | - | - |
| Duration of hearing loss and age of diagnosis | ||||
| Age of hearing loss onset | 2 | 2 | - | - |
| Hearing loss duration | 5 | 3 | - | 2 |
| Self-reported hearing difficulties and beliefs | ||||
| Self-reported hearing difficulties | 9 | 7 | - | 2 |
| Self-reported hearing disability (e.g., HHI) | 11 | 6 | - | 5 |
| Difficulty when someone whispers* | 1 | 1 | - | - |
| Hearing disability perceived by others | 1 | - | - | 1 |
| Hearing difficulties perceived by others* | 1 | 1 | - | - |
| Disturbance to daily life | 1 | - | - | 1 |
| Uses closed captions* | 1 | 1 | - | - |
| Tinnitus | 3 | - | - | 3 |
| Vertigo | 1 | - | - | 1 |
| Hearing beliefs questionnaire: | ||||
| Susceptibility | 2 | 1 | - | 1 |
| Severity | 2 | 1 | - | 1 |
| Benefits | 2 | 2 | - | - |
| Barriers | 2 | - | 1 | 1 |
| Self-efficacy | 2 | 1 | - | 1 |
| Cues to action | 2 | 2 | - | - |
| Speech perception | ||||
| Signal-to-noise ratio loss* | 2 | 2 | - | - |
| Speech recognition threshold* | 2 | 1 | - | 1 |
| Word recognition score | 1 | - | - | 1 |
| Word recognition in quiet | 1 | - | - | 1 |
| Low-context sentence recognition in babble* | 1 | - | 1 | - |
| High-context sentences in babble | 1 | - | - | 1 |
| Connected Speech Test | 1 | - | - | 1 |
| Acceptable Noise Level | 1 | - | - | 1 |
| Audiology appointment, assessment and consultation | ||||
| Self-referred for hearing test* | 1 | 1 | - | - |
| First hearing aid consultation institution* | 1 | 1 | - | - |
| Hearing aid recommendation | 1 | - | - | 1 |
| Recent hearing test* | 2 | 2 | - | - |
| Participant's recommendation of dispenser services | 1 | - | - | 1 |
| Consulted audiologist* | 1 | 1 | - | - |
| Consulted ear, nose and throat doctor | 1 | - | - | 1 |
| Consulted hearing aid dispenser* | 1 | 1 | - | - |
| Referral source | 1 | - | - | 1 |
| Later time of the day (vs. earlier)* | 1 | - | 1 | - |
| Day of the week | 1 | - | - | 1 |
| Attending appointment with other | 1 | 1 | - | - |
| Language | 1 | - | - | 1 |
| Health literacy | 1 | - | - | 1 |
| Medical language* | 1 | 1 | - | - |
| Flesch–Kincaid reading grade level of audiologist talk* | 1 | - | 1 | - |
| Audiologists’ number of sentences | 1 | - | - | 1 |
| Communication difficulties | ||||
| Communication partner assignment | 1 | - | - | 1 |
| Perceived communication program effectiveness | 1 | - | - | 1 |
| Perceived suitability of the individual program* | 1 | - | 1 | - |
| Communication self-efficacy* | 1 | - | 1 | - |
| Perceived likely adherence | 1 | - | - | 1 |
| Perceived suitability of group program | 1 | - | - | 1 |
| Other people's recommendation of the communication programs | 1 | - | - | 1 |
| Communication Profile for the Hearing Impaired: | ||||
| Performance—social | 2 | - | 2 | - |
| Performance—work | 2 | - | 2 | - |
| Performance—home | 2 | - | 2 | - |
| Performance—problem awareness | 2 | 2 | - | - |
| Environment—communication need | 2 | - | - | 2 |
| Environment—physical characteristics | 2 | - | - | 2 |
| Environment—attitudes of others | 2 | - | - | 2 |
| Environment—behaviors of others | 2 | - | - | 2 |
| Strategies—maladaptive behaviors | 3 | - | - | 3 |
| Strategies—verbal strategies | 3 | 1 | - | 2 |
| Strategies—nonverbal strategies | 3 | 2 | - | 1 |
| Personal adjustment—self-acceptance | 3 | 1 | - | 2 |
| Personal adjustment—acceptance of loss | 3 | 1 | - | 2 |
| Personal adjustment—anger | 2 | - | - | 2 |
| Personal adjustment—displacement of responsibility | 2 | 1 | - | 1 |
| Personal adjustment—exaggeration of responsibility | 2 | 1 | - | 1 |
| Personal adjustment—discouragement | 2 | - | - | 2 |
| Personal adjustment—stress | 3 | - | - | 3 |
| Personal adjustment—withdrawal | 3 | - | 1 | 2 |
| Personal adjustment—denial | 2 | - | 1 | 1 |
| Belief, expectation, and understanding of hearing aids | ||||
| HearSupport received* | 1 | 1 | - | - |
| Understanding HA function* | 1 | 1 | - | - |
| Hearing aid handling* | 2 | 1 | - | 1 |
| Desire for hearing aids | 2 | - | - | 2 |
| Concerns about hearing aid cost and practices | 1 | - | - | 1 |
| Attitude toward hearing aids: Benefits scale | 1 | 1 | - | - |
| Attitude toward hearing aids | 2 | 2 | - | - |
| Attitude toward hearing aids: Negative support scale | 1 | - | 1 | - |
| Expected Consequences of Hearing Aid Ownership: | ||||
| Positive effects | 1 | 1 | - | - |
| Negative effects | 1 | - | - | 1 |
| Service and cost | 1 | 1 | - | - |
| Personal image | 1 | 1 | - | - |
Note: PTA = Pure Tone Average; HHI = Hearing Handicap Inventory.
*Significant factors that have not been reported in previous reviews relevant to the specific outcome.
Figure 3.
Number of Significant Factors Identified Within Studies That Influence Hearing Aid Uptake for Each Category of Audiological or Nonaudiological Factors.
Table 7.
Combined Evidence from Previous Reviews, Including Knudsen et al. (2010) and Meyer and Hickson (2012), and the Current Systematic Review (2011–2022) on Factors Influencing Hearing Aid Uptake.
| Audiological factors | ||||||
|---|---|---|---|---|---|---|
| Factor | Previous reviews (<2012) | Current systematic review (2011–2012) | Combined | |||
| No. of studies | Results | No. of studies | Results | No. of studies | Results | |
| Attitudes toward hearing aids | 1 | + | 2 | +, + | 3 | +, +, + |
| Attitudes toward own hearing loss* | 3 | + Acceptance of hearing loss + Distress + Problem awareness - Denial of problems - Self-acceptance - Maladaptive behavior | No data | 3 | + Acceptance of hearing loss + Distress + Problem awareness - Denial of problems - Self-acceptance - Maladaptive behavior | |
| Expectations* | 2 | 0, + (impact on quality of life and would not be negatively perceived by others) | 1 | + Positive effects 0 Negative effects +Service and cost + Personal image | 3 | 0, + (impact on quality of life and would not be negatively perceived by others), + Positive effects + Service and cost + Personal image 0 Negative effects |
| Self-reported hearing problems (and/or activity limitation, participation restriction) | 5 | +, +, + , +, + | 25 | +, +, +, +, +, +, +, 0, 0 (self-reported hearing difficulties) +, +, +, +, +, +, +, +, +, +, +, 0, 0, 0, 0, 0 (self-reported hearing disability) | 30 | +, +, +, +, +, +, +, +, +, +, +, +, +, +, +, +, +, +, +, +, +, +, +, 0, 0, 0, 0, 0, 0, 0 |
| Hearing sensitivity | 5 | +, +, +, +, - | 22 | +, +, +, +, +, +, +, +, +, +, +, +, +, +, +, +, +, +, 0, 0, 0, 0 | 27 | +, +, +, +, +, +, +, +, +, +, +, +, +, +, +, +, +, +, +, +, +, +, -, 0, 0, 0, 0 |
| Age of hearing loss onset | 1 | 0 | 2 | +, + | 3 | +, +, 0 |
| Duration of hearing loss | 1 | 0 | 5 | +, +, +, 0, 0 | 6 | +, +, +, 0, 0, 0 |
| Speech reading | 1 | 0 | No data | 1 | 0 | |
| Hearing screening | 1 | + | 1 | + | 2 | +, + |
| Willingness to use HAs | 1 | + | No data | 1 | + | |
| Nonaudiological factors | ||||||
| Age | 4 | +, +, 0, 0 | 25 | +, +, +, +, +, +, +, +, -, 0, 0, 0, 0, 0, 0, 0, 0, 0, 0, 0, 0, 0, 0, 0, 0, | 29 | +, +, +, +, +, +, +, +, +, +, -, 0, 0, 0, 0, 0, 0, 0, 0, 0, 0, 0, 0, 0, 0, 0, 0, 0, 0 |
| Male sex (vs. female) | 4 | 0, 0, 0, 0 | 20 | +, +, +, -, 0, 0, 0, 0, 0, 0, 0, 0, 0, 0, 0, 0, 0, 0, 0, 0 | 24 | +, +, +, -, 0, 0, 0, 0, 0, 0, 0, 0, 0, 0, 0, 0, 0, 0, 0, 0, 0, 0, 0, 0 |
| Socioeconomic status | 4 | +, 0, 0, 0 | 5 | +, +, +, 0, 0 | 9 | +, +, +, +, 0, 0, 0, 0, 0 |
| Living arrangement | 4 | +, 0, 0, 0 | 3 | 0, 0, 0 | 7 | +, 0, 0, 0, 0, 0, 0 |
| Education | 5 | +, − (higher education), 0, 0, 0 | 12 | +, +, +, +, 0, 0, 0, 0, 0, 0, 0, 0 | 17 | +, +, +, +, +, -, 0, 0, 0, 0, 0, 0, 0, 0, 0, 0, 0 |
| Social interaction | 1 | 0 | No data | 1 | 0 | |
| Cost concerns | 1 | - | No data | 1 | - | |
| Marital status | 2 | 0, 0 | 5 | +, 0, 0, 0, 0 | 7 | +, 0, 0, 0, 0, 0, 0 |
| Health | 1 | 0 | 4 | +, +, −, − | 5 | +, +, -, -, 0 |
| General health attitude | 1 | 0 | No data | 1 | 0 | |
| Technology | 1 | - (internet and email) | 2 | +, 0 | 3 | +, -, 0 |
| Personality* | 1 | + responsibility for communication problems + locus of control and ego strength in females | 1 | 0 | 2 | + responsibility for communication problems + locus of control and ego strength in females, 0 |
| White race (vs. other) | 1 | + | 4 | +, +, 0, 0 | 5 | +, +, +, 0, 0 |
Note: Four studies from the Meyer and Hickson (2012) review were excluded from the table, including Carson (2005) and Wallhagen (2010) because they are qualitative studies as well as Kochkin (2007) and Kochkin (2009) because they are not peer-reviewed papers. “+” indicates a positive association between the factor and the outcome, “–” a negative association, and “0” no association. *Factors including multiple outcomes.
Audiological Factors
Hearing Sensitivity
Twenty studies found a positive association between greater hearing loss (i.e., poor hearing sensitivity measured using pure tone audiometry) and hearing aid uptake, while four studies showed no association. These studies used various measures to define hearing sensitivity (e.g., better ear PTA at 0.5, 1, 2, and 4 kHz) (see Table 5). A study by Robertson et al. (2012) reported that participants were more likely to purchase hearing aids if their audiograms fell within Erber's area (hearing thresholds poorer than 35 dB HL in the frequency range below 1000 Hz). One study found that people were more likely to adopt hearing aids if they had bilateral, as opposed to unilateral hearing loss (Angara et al., 2021).
Duration of Hearing Loss and Age of Diagnosis
Two studies reported positive associations between the age of hearing loss onset and hearing aid uptake. Chan et al. (2017) reported that the age of hearing loss onset was correlated with time to hearing aid acquisition, with older people acquiring hearing aids more quickly than younger people, and Moschis et al. (2015) concluded that the older the person at the time of diagnosis, the more likely they were to purchase a hearing aid. Three studies reported that people were more likely to take up hearing aids if they had a longer hearing loss duration (Cho et al., 2022; Moschis et al., 2015; Saunders et al., 2016), although two studies reported no association.
Self-Reported Hearing Difficulties and Health Beliefs
Seven studies reported a positive association between poor self-reported hearing difficulties and hearing aid uptake (e.g., Angara et al., 2021; Fischer et al., 2011), while two studies showed no association. A study by Gopinath et al. (2011) also reported that people were more likely to adopt hearing aids if they reported having difficulty hearing when someone whispered. One study reported that people were more likely to adopt hearing aids if they used closed captions or if their hearing difficulties were perceived by others (Weycker et al., 2021). Six studies reported a positive association between self-reported hearing disability and hearing aid uptake, although five studies reported no association. Five studies used various versions of the Hearing Handicap Inventory (Fischer et al., 2011; Gopinath et al., 2011; Saunders et al., 2016; Simpson et al., 2019; Weycker et al., 2021) and one study used the Amsterdam Inventory for Auditory Disability and Handicap (van Leeuwen et al., 2021). Two studies investigated hearing beliefs within the constructs of the HBM (Saunders et al., 2016, 2013). Saunders et al. (2013) found that people were more likely to adopt hearing aids if they had higher perceived susceptibility to hearing loss, higher perceived benefits of hearing and rehabilitation, lower perceived barriers to hearing rehabilitation, and higher cues to action. Saunders et al. (2016) found that people were more likely to adopt hearing aids if they had higher perceived severity of hearing loss, higher perceived benefits of hearing and rehabilitation, higher perceived self-efficacy regarding hearing rehabilitation, and higher cues to action.
Speech Perception
Two studies found that people were more likely to adopt hearing aids if they had a higher signal-to-noise ratio loss, which represented the dB increase in signal-to-noise ratio required by the participant to understand speech in noise compared to people with normal hearing, measured using the Quick Speech in Noise (QuickSIN) test (Kelly-Campbell & Parry, 2014; Robertson et al., 2012). Two studies reported mixed findings on speech recognition thresholds (SRTs) and their association with hearing aid uptake. Robertson et al. (2012) found that people who purchased hearing aids had higher SRTs than those who did not purchase hearing aids, although van Leeuwen et al. (2021) reported no association. The SRTs were measured for each ear using monitored live voice and the Central Institute for the Deaf W-1 spondaic word list (Hirsh et al., 1952). A study by Simpson et al. (2019) reported that people were more likely to adopt hearing aids if they had the poorest low-context sentences-in-babble scores.
Audiology Appointment, Assessment, and Consultation
Two studies reported on the association between a recent hearing test and hearing aid uptake. Angara et al. (2021) and He et al. (2018) found that people were more likely to adopt hearing aids if they had received a hearing assessment. A study by Saunders et al. (2016) reported that people were more likely to obtain hearing aids if they self-referred for a hearing test. One study reported that people were more likely to adopt hearing aids if they had their first hearing aid consultation at a hearing aid center instead of a hospital (Cho et al., 2022). A study by Moschis et al. (2015) concluded that people were more likely to take up hearing aids if they had a consultation with either an audiologist or a hearing aid dispenser. One study found that people were less likely to take up hearing aids if their appointment was scheduled at 12 pm and 4 pm compared to earlier in the day (Singh & Launer, 2018). A study by Singh and Launer (2016) reported that people were more likely to adopt hearing aids if they attended an audiology appointment with a significant other. Two studies reported on the relationship between the healthcare professional's language and hearing aid uptake. On one hand, Adorni et al. (2021) concluded that people were more likely to obtain hearing aids if the family doctor used medical language. On the other hand, a study by Sciacca et al. (2017) found that patients were less likely to obtain hearing aids if the audiologists’ language was at higher reading grade level measured using the Flesch–Kincaid readability formula.
Communication Difficulties
A study by Laplante-Lévesque et al. (2012) investigated the predictors of the uptake of hearing aids and communication programs. They found that people were more likely to complete communication programs and less likely to adopt hearing aids if they perceived greater suitability for the individual communication program. In addition, people were less likely to adopt hearing aids if they reported greater communication self-efficacy (Laplante-Lévesque et al., 2012). Two studies used the CPHI to investigate the relationship between communication profile and hearing aid uptake. Humes (2021) and Humes and Dubno (2021) found that people were more likely to obtain hearing aids if they had poorer communication performance (in social settings, at work, and at home), more awareness of communication problems, and better use of nonverbal communication strategies as assessed using the CPHI. Humes and Dubno (2021) also reported that people who decided to obtain hearing aids were more accepting of their hearing loss but allocated more responsibility for difficulties to their communication partners, whereas Humes (2021) found that people who decided to obtain hearing aids had better use of verbal communication strategies, lower self-acceptance of hearing loss, less exaggeration of responsibility, less withdrawal, and less denial of communication difficulties.
Belief, Expectation, and Understanding of Hearing Aids
According to one study, people who received a support program (HearSupport) were more likely to take up hearing aids (Pronk et al., 2019). A study by He et al. (2018) reported that people were more likely to adopt hearing aids if they understood hearing aid function. Two studies reported on hearing aid handling and its relationship with hearing aid uptake. Meyer et al. (2014) found that successful hearing aid owners perceived that they could better manage the basic functions of their hearing aids, although Pronk et al. (2019) reported no association. Two studies reported that people were more likely to adopt hearing aids if they had a positive attitude toward hearing aids (Cobelli et al., 2014; Meyer et al., 2014). A study by Meyer et al. (2014) concluded that people were more likely to take up hearing aids if they perceived more benefits of hearing aids and experienced more support for hearing aids from significant others. One study reported that people who did not take up hearing aids had lower expectations for hearing aids according to the Expected Consequences of Hearing Aid Ownership (ECHO) scale (Humes, 2021). This assessed the positive effects of hearing aids, service, and cost, as well as personal image (Humes, 2021).
Nonaudiological Factors
Demographics
Although 16 studies reported no association, eight studies reported that people were more likely to adopt hearing aids if they were older (Angara et al., 2021; Gopinath et al., 2011; Maidment & Wege, 2021; Saunders et al., 2016, 2013; Sawyer et al., 2020; Singh & Launer, 2016, 2018). Conversely, Chang et al. (2016) reported that people were more likely to accept a hearing aid if they were younger in an older cohort (65–90 years of age). Although 16 studies found no association, Angara et al. (2021), Chang et al. (2016), and Öberg et al. (2012) found a positive association between sex (being male) and hearing aid uptake, whereas Simpson et al. (2019) found that females were more likely to adopt hearing aids. Two studies by Angara et al. (2021) and Simpson et al. (2019) reported that people were more likely to take up hearing aids if they were white people, whereas two studies reported no association. Although eight studies showed no association, four studies (Angara et al., 2021; Cho et al., 2022; Fischer et al., 2011; Weycker et al., 2021) found that people were more likely to take up hearing aids if they had a higher education. Two studies by Chan et al. (2017) and He et al. (2018) reported that people were more likely to adopt hearing aids and to adopt them more quickly if they were urban residents compared to rural residents. Whereas four studies reported no association, one study concluded that people were more likely to obtain hearing aids if they were married compared to single (van Leeuwen et al., 2021). One study by van Leeuwen et al. (2021) found that males were more likely to take up hearing aids if they perceived higher psychological job demand (i.e., the psychological requirements for an employee's tasks).
Socioeconomic Status
Four studies reported that people were more likely to take up hearing aids if they had higher socioeconomic status or household income (Cho et al., 2022; Laplante-Lévesque et al., 2012; Simpson et al., 2019; Tahden et al., 2018), although three studies did not report any association. A study by Meyer et al. (2014) reported that older adults were more likely to obtain hearing aids if they received a pension.
Hearing Healthcare Funding and Health Insurance
According to four different studies, people were more likely to adopt hearing aids if they applied for subsidized hearing services (Laplante-Lévesque et al., 2012), received government assistance (Cho et al., 2022), senior mobility fund (Chua Wei De, 2021) or had health insurance (Tran et al., 2021). A study by Angara et al. (2021), however, reported no association between health insurance and hearing aid uptake.
Health
As with hearing help-seeking, mixed findings were reported regarding self-reported health and its association with hearing aid uptake in four studies. Öberg et al. (2012) and Tahden et al. (2018) found that people were more likely to own a hearing aid if they had better self-reported health. In contrast, Nixon et al. (2021) and Sawyer et al. (2020) found that people were more likely to take up hearing aids if they had poorer self-reported health. Two studies reported on comorbidities and their relationship with hearing aid uptake. People were less likely to adopt hearing aids if they had self-reported diabetes (Maidment & Wege, 2021), hypertension (Maidment & Wege, 2021), or a history of stroke (Gopinath et al., 2011).
Cognition and Mental Health
A study by Meyer et al. (2014) reported that people were more likely to obtain hearing aids if they had better cognitive reasoning skills. Two studies by Kelly-Campbell and Parry (2014) and Kelly et al. (2011) reported that people were more likely to take up hearing aids if they experienced higher cognitive anxiety.
Motivation, Support, Subjective Norms, and Trust
According to two studies by Ridgway et al. (2015, 2016), people were more likely to take up hearing aids if they had autonomous motivation. Two studies reported a positive relationship between the “subjective norm” construct of the TPB (i.e., social pressure) and hearing aid uptake (Cobelli et al., 2014; Meister et al., 2014). Cobelli et al. (2014), however, reported a significant interaction between subjective norm and trust, indicating that when trust in the health professional was high, the subjective norm was not significantly related to hearing aid uptake. When there was a lower level of trust in the health professional, the subjective norm was strongly related to hearing aid uptake.
Attitude Toward Behavior and Control
In one study, hearing aid uptake was positively affected by the “attitude toward behavior” and “behavioral control” constructs of the TPB (Meister et al., 2014).
Readiness for Change
Three studies used the University of Rhode Island change assessment to investigate readiness for change. Saunders et al. (2016) found that those who took up hearing aids had lower pre-contemplation scores (problem denial), higher contemplation scores (problem awareness and evaluation of the pros and cons of change), and higher action scores (devoting time and energy to behavior change). Pronk et al. (2019) and Laplante-Lévesque et al. (2012), however, did not report any association between hearing aid uptake and pre-contemplation or action scores. Similar to Saunders et al. (2016), Laplante-Lévesque et al. (2012) also found that people who took up hearing aids had higher contemplation scores (i.e., they acknowledged their hearing loss and compared the pros and cons of intervention uptake), although Pronk et al. (2019) did not report any association.
Other: Technology Commitment
Two studies reported on the influence of technology commitment on hearing aid uptake. Tahden et al. (2018) reported that people were more likely to own hearing aids if they had a technology commitment, although Ham et al. (2014) reported no association. Technology commitment included technology competence, acceptance, control, and usage habits of media devices.
Level of Evidence
The level of evidence according to the OCEBM for each study is indicated in Table 1. Twenty-eight cross-sectional studies (67%) were classified as level four evidence, 12 cohort studies (29%) as level three evidence, and two studies (one true experimental study and one cluster randomized control trial) (5%) as level 2 evidence.
Quality Assessment
The NIH quality assessment tool was used to assess the quality of each study included in the review. Quality ratings are shown in Table 1. Thirty-six studies (86%) were rated fair quality, two (5%) good quality, and four (10%) poor quality. The quality assessment showed a few poor areas. Firstly, only 7% of the studies gave a sample size justification, power description, or variance and effect estimates. Secondly, most studies were cross-sectional, and therefore, 74% of the studies did not measure the exposure(s) (i.e., audiological or nonaudiological factors) before the outcomes (hearing help-seeking and/or hearing aid uptake) but instead measured it at the same time. For the same reason, most studies (86%) did not measure the exposure(s) more than once. Thirdly, 79% of the studies used self-report measures to determine the outcomes (hearing help-seeking and/or hearing aid uptake). Lastly, none of the studies reported blinding.
Discussion
This systematic review examined audiological and nonaudiological factors influencing hearing help-seeking and hearing aid uptake in adults with hearing loss based on literature published between January 2011 and February 2022. Identified studies investigated 70 (42 audiological and 28 nonaudiological) hearing help-seeking factors and 159 (93 audiological and 66 nonaudiological) hearing aid uptake factors with many reported only once (10/70 and 62/159, respectively). Some of the keys identified audiological and nonaudiological factors will be discussed below.
Audiological Factors
As opposed to hearing help-seeking, audiological factors influencing hearing aid uptake have been widely studied (see Tables 6 and 7). However, some new factors emerged in the present review, including the health professional's language usage. Adorni et al. (2021) found that medical language compared to everyday language was more effective in persuading people to obtain hearing aids. Authors suggest that everyday language might come across as inappropriate and unprofessional, leading to mistrust in the health professional. Sciacca et al. (2017) found that patients were less likely to obtain hearing aids if the audiologists’ language was at a higher Flesch–Kincaid reading grade level. They concluded that reduced understanding might limit the patient's involvement in decision-making and cause them to be less willing to take up hearing aids. Therefore, hearing healthcare professionals should consider the accessible use of medical language, which still keeps the dialogue clear and understandable. Two studies also found that understanding hearing aid function affected hearing aid uptake positively. Additionally, a cluster randomized controlled trial by Pronk et al. (2019) showed that receiving a program (HearSupport) that includes information on hearing aid handling positively affected hearing aid uptake. This emphasizes the importance of counseling regarding hearing aid function and handling even before the patient has made the decision to take up hearing aids.
Like the present review, Meyer and Hickson (2012) and Knudsen et al. (2010) found that evidence on hearing sensitivity in relation to help-seeking is less clear compared to hearing aid uptake. In total (including studies from the current review and previous reviews), 10 studies have investigated the influence of hearing sensitivity on hearing help-seeking (Table 6), whereas 27 studies investigated the influence of hearing sensitivity on hearing aid uptake (Table 7). In the present review, three studies found positive associations between poorer hearing sensitivity and hearing help-seeking, while two studies did not find any associations. The severity of hearing loss was one of the strongest predictors of hearing aid uptake, as also reported by Meyer and Hickson (2012), whether it was measured by PTA (20/24 studies showed positive associations), speech perception testing (4/10 studies showed positive associations) or self-report (7/9 studies showed positive associations). In line with earlier reviews by Knudsen et al. (2010) and Meyer and Hickson (2012), self-reported hearing disability was also a strong predictor of hearing aid uptake (Table 7). Six studies found a positive association between greater self-reported disability using standardized tools and hearing aid uptake, whereas five did not find any association. As recommended by Humes and Dubno (2021), measuring self-reported hearing disability in addition to pure tone audiometry during the initial assessment can provide valuable information regarding hearing aid candidacy.
For help-seeking previous reviews identified factors such as self-reported hearing disability, hearing beliefs, and communication profile as important (Knudsen et al., 2010; Meyer & Hickson, 2012). In the present review, greater self-reported hearing disability was reported to be a significant predictor of entering a hearing aid evaluation period by Pronk et al. (2017). Using the Health Belief Questionnaire, Saunders et al. (2013) found that help-seekers had higher perceived susceptibility to hearing loss, lower barriers to hearing rehabilitation, and higher cues to action compared to nonhelp seekers. Humes and Dubno (2021) used the CPHI and concluded that older adults with self-awareness of hearing loss were more likely to seek help. Consistent with Meyer and Hickson (2012), two studies found positive associations between the perceived benefits of hearing aids and help-seeking. People who considered hearing aids before seeking help were also more likely to seek help for their hearing problems (Meyer et al., 2011). Similarly, Meyer et al. (2014) concluded that participants who perceived more benefits of hearing aids and experienced their significant others being more supportive of hearing aids were more likely to take up hearing aids. People with positive attitudes toward hearing aids were found to be more likely to adopt hearing aids in two studies, as also reported by Knudsen et al. (2010).
Nonaudiological Factors
Several new nonaudiological predictors not previously reported in systematic reviews were identified, including cognitive anxiety for both hearing help-seeking and hearing aid uptake (Kelly et al., 2011; Kelly-Campbell & Parry, 2014). People with hearing loss are at increased risk of cognitive anxiety because they cannot anticipate communication breakdowns due to missing conversations, and seeking treatment may help decrease this anxiety (Kelly et al., 2011). Being aware of the signs of cognitive anxiety, as described by Kelly et al. (2011), can potentially assist hearing healthcare professionals in determining readiness for intervention.
Two studies also demonstrated for the first time that urban residents were more likely to purchase hearing aids and to purchase them more quickly than rural residents (Chan et al., 2017; He et al., 2018). Rural residents typically have less access to hearing healthcare services, less education, and lower socioeconomic statuses than urban residents, which also influences hearing aid uptake (Chan et al., 2017). This highlights the importance of more accessible hearing healthcare services in rural areas.
Having access to financial support (whether receiving an income or funding from a third party) clearly affected hearing aid uptake in the present review. Three studies showed positive associations between higher socioeconomic status and hearing aid uptake. A higher household income, receiving a pension, applications for subsidized hearing services, government funding, and having health insurance were all linked to hearing aid uptake in six studies.
Comorbidities considered as risk factors for hearing loss, such as diabetes, hypertension, and history of stroke, were all negatively associated with hearing aid uptake (Kuo et al., 2016; Nawaz et al., 2021; Samocha-Bonet et al., 2021). This may be because people with chronic illnesses may have a more limited capacity to manage their hearing loss due to time, money, and other potential constraints. Thus, hearing healthcare professionals should focus on high-risk populations by, for example, performing hearing screenings to ensure that they receive the appropriate treatment.
Key nonaudiological factors reported in previous reviews were also confirmed by the current review. As shown in an earlier review (Knudsen et al., 2010), age and sex were the most studied factors in the present review (see Tables 6 and 7). Knudsen et al. (2010) concluded that age and sex show no relationship with hearing help-seeking or hearing aid uptake. In the present review, older age, which is linked to increasing hearing loss prevalence and severity (World Health Organization, 2021), was associated with hearing help-seeking, although three of the five studies did not report a significant association. Older age generally resulted in hearing aid uptake but not in all studies. In an older adult cohort (65–90 years of age), hearing aid uptake was greater for those closer to 65 years of age (Chang et al., 2016). Thus, it is important to consider the age range of participants in a study that aims to investigate the effect of age on other variables.
Generally, males (who are more likely to have hearing loss; Hoffman et al., 2017) were also more likely to seek help for their hearing problems, although some studies (3/6) showed no association. The majority of studies (16/20) did not report different associations across sex but in three studies males were more likely to adopt hearing aids while in one study females were more likely. As in previous reviews (Knudsen et al., 2010; Meyer & Hickson, 2012), the present review demonstrates a positive association between social pressure and hearing help-seeking (Table 6). Hearing aid uptake was also positively affected by social pressure in two studies. Although autonomous motivation, suggesting that hearing aid uptake is largely/partly a self-determined behavior, was also positively associated with hearing aid uptake in two studies.
Based on previous studies, stigma is generally considered as a barrier to help-seeking (Meyer & Hickson, 2012). Pronk et al. (2017) however reported greater hearing aid stigma to be a positive predictor for entering a hearing aid evaluation period, but only for females. The limited and inconsistent evidence on the effect of stigma requires further investigation.
Contradictory or limited results were reported for factors concerning health, cognition, and mental health. A fair-quality study reported a positive association between better self-reported health and hearing help-seeking (Meyer et al., 2014), but a second fair-quality study did not find any association (Öberg et al., 2012), while a third poor-quality study found a negative association (Sawyer et al., 2020). Considering study quality, it is more likely that better self-reported health is associated with increased hearing help-seeking. Self-reported health and hearing aid uptake was negatively associated in two studies (both fair quality), while two other studies (one fair quality and one poor quality) found positive associations. Cognitive performance and hearing help-seeking showed no association in a fair-quality study (Öberg et al., 2012) compared to a positive association in a recent poor-quality study (Sawyer et al., 2020). More evidence on the influence of general health, cognition, and other aspects of mental health is required.
Conclusions
A range of hearing help-seeking and hearing aid uptake factors have been investigated with several reported only once (10/70 and 62/159) for help-seeking and hearing aid uptake. Most reviewed research has focused on hearing aid uptake (70%) as opposed to hearing help-seeking (30%), which reflects the need to better understand help-seeking as the first step to acquiring hearing aids as also mentioned by Meyer and Hickson (2012). Expanding our understanding of hearing help-seeking is especially important with the rapidly changing landscape in hearing aid service delivery models, including over-the-counter (OTC) hearing aids. The present review identified several predictors that have not been identified in systematic reviews before, including cognitive anxiety for both help-seeking and hearing aid uptake and urban residency for hearing aid uptake. Age and sex were not predictive of hearing help-seeking or hearing aid uptake in most studies. However, a few reports indicated that older people and males were more likely to seek help or to take up hearing aids. Social factors like social pressure appears important for hearing help-seeking. The perceived potential benefit of amplification was linked to hearing help-seeking and positive attitudes to hearing aids and an understanding of their function were predictive of hearing aid uptake. Access to financial support was a strong predictor of hearing aid uptake but not of hearing help-seeking. The severity of hearing loss and greater self-reported hearing disability were two of the most important predictors of hearing aid uptake.
More research is required where evidence is limited, for example, the influence of stigma on help-seeking. Additionally, further investigations are required where mixed findings were reported, for instance, the relationship between self-reported health and help-seeking/hearing aid uptake. Other factors to investigate are hearing aid cost and counseling style since they have been observed to affect hearing aid uptake in clinical practice but with limited evidence. A limitation of the synthesis methods used in this study (i.e., direction of effect and vote-counting) was that they did not provide information on the magnitude of the effects. Overall, studies of higher quality and stronger evidence (e.g., randomized controlled trials) are required for both hearing help-seeking and hearing aid uptake. A systematic review and synthesis of qualitative studies to obtain further insights into the factors influencing hearing help-seeking and hearing aid uptake may be helpful. A better understanding of factors influencing hearing help-seeking and hearing aid uptake can inform public health and clinical initiatives to promote hearing help-seeking and hearing aid uptake. This review highlights the need for further investigations to explore specific factors with limited or conflicting results.
Supplemental Material
Supplemental material, sj-docx-1-tia-10.1177_23312165231157255 for Factors Influencing Hearing Help-Seeking and Hearing Aid Uptake in Adults: A Systematic Review of the Past Decade by Megan Knoetze, Vinaya Manchaiah, Bopane Mothemela and De Wet Swanepoel in Trends in Hearing
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Megan Knoetze https://orcid.org/0000-0002-7187-9281
Vinaya Manchaiah https://orcid.org/0000-0002-1254-8407
Bopane Mothemela https://orcid.org/0000-0003-2937-6549
Supplemental Material: Supplemental material for this article is available online.
References
- Adorni R., Manzi C., Crapolicchio E., Steca P. (2021). The role of the family doctor’s language in modulating people’s attitudes towards hearing loss and hearing aids. Health & Social Care in the Community, 30(5), e1775–e1784. 10.1111/hsc.13606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angara P., Tsang D. C., Hoffer M. E., Snapp H. A. (2021). Self-perceived hearing status creates an unrealized barrier to hearing healthcare utilization. The Laryngoscope, 131(1), E289–E295. 10.1002/lary.28604 [DOI] [PubMed] [Google Scholar]
- Bagias C., Sukumar N., Weldeselassie Y., Oyebode O., Saravanan P. (2021). Cord blood adipocytokines and body composition in early childhood: A systematic review and meta-analysis. International Journal of Environmental Research and Public Health, 18(4), 1897. 10.3390/ijerph18041897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bisgaard N., Zimmer S., Laureyns M., Groth J. (2021). A model for estimating hearing aid coverage world-wide using historical data on hearing aid sales. International Journal of Audiology, 61(10), 841–849. 10.1080/14992027.2021.1962551 [DOI] [PubMed] [Google Scholar]
- Blazer D. G., Domnitz S., Liverman C. T., Medicine N. (2016). Hearing health care for adults: Priorities for improving access and affordability. 10.17226/23446 [DOI]
- Campbell M., McKenzie J. E., Sowden A., Katikireddi S. V., Brennan S. E., Ellis S., Ellis S., Hartmann-Boyce J., Ryan R., Shepperd S., Thomas J., Welch V., Thomson H. (2020). Synthesis without meta-analysis (SWiM) in systematic reviews: Reporting guideline. BMJ, 368, l6890. 10.1136/bmj.l6890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carson A. J. (2005). “What brings you here today?” The role of self-assessment in help-seeking for age-related hearing loss. Journal of Aging Studies, 19(2), 185–200. 10.1016/j.jaging.2004.07.001 [DOI] [Google Scholar]
- Chan S., Hixon B., Adkins M., Shinn J. B., Bush M. L. (2017). Rurality and determinants of hearing healthcare in adult hearing aid recipients. The Laryngoscope, 127(10), 2362–2367. 10.1002/lary.26490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang N.-C., Dai C.-Y., Lin W.-Y., Chien C.-Y., Hsieh M.-H., Ho K.-Y. (2016). Perception of hearing impairment and the willingness to use hearing aids in an elderly population in southern Taiwan: A community-based study. International Journal of Audiology, 55(9), 491–498. 10.1080/14992027.2016.1182651 [DOI] [PubMed] [Google Scholar]
- Cho Y. S., Kim G.-Y., Choi J. H., Baek S. S., Seol H. Y., Lim J., Lim J., Park J. G., Moon I. J. (2022). Factors influencing hearing aid adoption in patients with hearing loss in Korea. Journal of Korean Medical Science, 37(2), e11. 10.3346/jkms.2022.37.e11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chua Wei De K. (2021). The impact of senior mobility funding on hearing aid acquisition and compliance to hearing aid use in a Singapore hospital. Journal of Audiology & Otology, 25(1), 8–13. 10.7874/jao.2020.00213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cobelli N., Gill L., Cassia F., Ugolini M. (2014). Factors that influence intent to adopt a hearing aid among older people in Italy. Health & Social Care in the Community, 22(6), 612–622. 10.1111/hsc.12127 [DOI] [PubMed] [Google Scholar]
- D’Onofrio K. L., Zeng F.-G. (2022). Tele-audiology: Current state and future directions. Frontiers in Digital Health, 3, 788103. https://doi.org/10.3389/fdgth.2021.788103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Etikan I., Musa S. A., Alkassim R. S. (2016). Comparison of convenience sampling and purposive sampling. American Journal of Theoretical and Applied Statistics, 5(1), 1–4. 10.11648/j.ajtas.20160501.11 [DOI] [Google Scholar]
- Ferguson M. A., Kitterick P. T., Chong L. Y., Edmondson-Jones M., Barker F., Hoare D. J. (2017). Hearing aids for mild to moderate hearing loss in adults. Cochrane Database of Systematic Reviews, 2017(9), CD012023. 10.1002/14651858.CD012023.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fischer M. E., Cruickshanks K. J., Wiley T. L., Klein B. E. K., Klein R., Tweed T. S. (2011). Determinants of hearing aid acquisition in older adults. American Journal of Public Health, 101(8), 1449–1455. 10.2105/AJPH.2010.300078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frisby C., Eikelboom R., Mahomed-Asmail F., Kuper H., Swanepoel D. W. (2021). MHealth applications for hearing loss: A scoping review. Telemedicine and E-Health, 28(8), 1090–1099. 10.1089/tmj.2021.0460 [DOI] [PubMed] [Google Scholar]
- Gopinath B., Schneider J., Hartley D., Teber E., McMahon C. M., Leeder S. R., Mitchell P. (2011). Incidence and predictors of hearing aid use and ownership among older adults with hearing loss. Annals of Epidemiology, 21(7), 497–506. 10.1016/j.annepidem.2011.03.005 [DOI] [PubMed] [Google Scholar]
- Ham H. S., Bunn P., Meyer C., Khan A., Hickson L. (2014). Exploring the relationship between technology use, hearing help-seeking, and hearing aid outcomes in older adults. International Journal of Audiology, 53(Suppl 1), S38–S42. https://doi.org/10.3109/14992027.2013.847287 [DOI] [PubMed] [Google Scholar]
- He P., Wen X., Hu X., Gong R., Luo Y., Guo C., Chen G., Zheng X. (2018). Hearing aid acquisition in Chinese older adults with hearing loss. American Journal of Public Health, 108(2), 241–247. 10.2105/AJPH.2017.304165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirsh I. J., Davis H., Silverman S. R., Reynolds E. G., Eldert E., Benson R. W. (1952). Development of materials for speech audiometry. Journal of Speech and Hearing Disorders, 17(3), 321–337. https://doi.org/10.1044/jshd.1703.321 [DOI] [PubMed] [Google Scholar]
- Hoffman H. J., Dobie R. A., Losonczy K. G., Themann C. L., Flamme G. A. (2017). Declining prevalence of hearing loss in US adults aged 20 to 69 years. JAMA Otolaryngology–Head & Neck Surgery, 143(3), 274–285. 10.1001/jamaoto.2016.3527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huddle M. G., Goman A. M., Kernizan F. C., Foley D. M., Price C., Frick K. D., Lin F. R. (2017). The economic impact of adult hearing loss: A systematic review. JAMA Otolaryngology–Head & Neck Surgery, 143(10), 1040–1048. 10.1001/jamaoto.2017.1243 [DOI] [PubMed] [Google Scholar]
- Humes L. E. (2021). Differences between older adults who do and do not try hearing aids and between those who keep and return the devices. Trends in Hearing, 25, 23312165211014330. 10.1177/23312165211014329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humes L. E., Dubno J. R. (2021). A comparison of the perceived hearing difficulties of community and clinical samples of older adults. Journal of Speech, Language, and Hearing Research, 64(9), 3653–3667. 10.1044/2021_JSLHR-20-00728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenstad L., Moon J. (2011). Systematic review of barriers and facilitators to hearing aid uptake in older adults. Audiology Research, 1(1), e25–e25. 10.4081/audiores.2011.e25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly R. J., Neimeyer R. A., Wark D. J. (2011). Cognitive anxiety and the decision to seek services for hearing problems. Journal of Constructivist Psychology, 24(2), 168–179. 10.1080/10720531003799691 [DOI] [Google Scholar]
- Kelly-Campbell R. J., Parry D. C. (2014). Relationship between cognitive anxiety level and client variables at initial consultation for adults with hearing impairment. Journal of Communication Disorders, 47, 47–56. 10.1016/j.jcomdis.2014.01.005 [DOI] [PubMed] [Google Scholar]
- Knudsen L. V., Oberg M., Nielsen C., Naylor G., Kramer S. E. (2010). Factors influencing help seeking, hearing aid uptake, hearing aid use and satisfaction with hearing aids: A review of the literature. Trends in Amplification, 14(3), 127–154. 10.1177/1084713810385712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kochkin S. (2007). MarkeTrak VII: Obstacles to adult non-user adoption of hearing aids. The Hearing Journal, 60, 24–51. 10.1097/01.HJ.0000285745.08599.7f [DOI] [Google Scholar]
- Kochkin S. (2009). MarkeTrak VIII: 25-year trends in the hearing health market. The Hearing Review, 16(11), 12–31. https://hearingreview.com/practice-building/marketing/marketrak-viii-25-year-trends-in-the-hearing-health-market [Google Scholar]
- Kuo C.-L., Shiao A.-S., Wang S.-J., Chang W.-P., Lin Y.-Y. (2016). Risk of sudden sensorineural hearing loss in stroke patients: A 5-year nationwide investigation of 44,460 patients. Medicine, 95(36), e4841–e4841. 10.1097/MD.0000000000004841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laplante-Lévesque A., Hickson L., Worrall L. (2012). What makes adults with hearing impairment take up hearing aids or communication programs and achieve successful outcomes? Ear and Hearing, 33(1), 79–93. 10.1097/AUD.0b013e31822c26dc [DOI] [PubMed] [Google Scholar]
- Mahboubi H., Lin H. W., Bhattacharyya N. (2018). Prevalence, characteristics, and treatment patterns of hearing difficulty in the United States. JAMA Otolaryngology–Head & Neck Surgery, 144(1), 65–70. 10.1001/jamaoto.2017.2223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maidment D. W., Wege T. E. (2021). The association between non-communicable disease and hearing aid adoption in older adults with hearing loss. International Journal of Audiology, 61(3), 220–227. 10.1080/14992027.2021.1910740 [DOI] [PubMed] [Google Scholar]
- Manchaiah V., Taylor B., Dockens A. L., Tran N. R., Lane K., Castle M., Grover V. (2017). Applications of direct-to-consumer hearing devices for adults with hearing loss: A review. Clinical Interventions in Aging, 12, 859–871. 10.2147/CIA.S135390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meister H., Grugel L., Meis M. (2014). Intention to use hearing aids: A survey based on the theory of planned behavior. Patient Preference and Adherence, 8, 1265–1275. 10.2147/PPA.S65008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer C., Hickson L. (2012). What factors influence help-seeking for hearing impairment and hearing aid adoption in older adults? International Journal of Audiology, 51(2), 66–74. 10.3109/14992027.2011.611178 [DOI] [PubMed] [Google Scholar]
- Meyer C., Hickson L., Khan A., Hartley D., Dillon H., Seymour J. (2011). Investigation of the actions taken by adults who failed a telephone-based hearing screen. Ear and Hearing, 32(6), 720–731. 10.1097/AUD.0b013e318220d973 [DOI] [PubMed] [Google Scholar]
- Meyer C., Hickson L., Lovelock K., Lampert M., Khan A. (2014). An investigation of factors that influence help-seeking for hearing impairment in older adults. International Journal of Audiology, 53(Suppl 1), S3–S17. 10.3109/14992027.2013.839888 [DOI] [PubMed] [Google Scholar]
- Moschis G. P., Lee E., Mathur A., Rigdon E. E., Fatt C. K. (2015). A study of delayed purchases of enabling products in the United States: The case of hearings aids. International Journal of Consumer Studies, 39(4), 380–386. 10.1111/ijcs.12204 [DOI] [Google Scholar]
- Mukari S. Z. M. S., Wan Hashim W. F. (2018). Self-perceived hearing loss, hearing-help seeking and hearing aid adoption among older adults in Malaysia. Annals of Otology, Rhinology and Laryngology, 127(11), 798–805. 10.1177/0003489418795982 [DOI] [PubMed] [Google Scholar]
- National Institute of Health (2021). Study Quality Assessment tools. Retrieved May 16, 2022, from https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools
- Nawaz M. U., Vinayak S., Rivera E., Elahi K., Tahir H., Ahuja V., Jogezai S., Maher W., Naz S. (2021). Association between hypertension and hearing loss. Cureus, 13(9), e18025–e18025. 10.7759/cureus.18025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng J. H.-Y., Loke A. Y. (2015). Determinants of hearing-aid adoption and use among the elderly: A systematic review. International Journal of Audiology, 54(5), 291–300. 10.3109/14992027.2014.966922 [DOI] [PubMed] [Google Scholar]
- Nixon G., Sarant J., Tomlin D., Dowell R. (2021). Hearing aid uptake, benefit, and use: The impact of hearing, cognition, and personal factors. Journal of Speech, Language, and Hearing Research, 64(2), 651–663. 10.1044/2020_JSLHR-20-00014 [DOI] [PubMed] [Google Scholar]
- Nordvik Ø, Laugen Heggdal P. O., Brännström J., Vassbotn F., Aarstad A. K., Aarstad H. J. (2018). Generic quality of life in persons with hearing loss: A systematic literature review. BMC Ear, Nose and Throat Disorders, 18(1), 1. 10.1186/s12901-018-0051-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Öberg M., Marcusson J., Nägga K., Wressle E. (2012). Hearing difficulties, uptake, and outcomes of hearing aids in people 85 years of age. International Journal of Audiology, 51(2), 108–115. 10.3109/14992027.2011.622301 [DOI] [PubMed] [Google Scholar]
- OCEBM Levels of Evidence Working Group (n.d.). The Oxford 2011 levels of evidence. https://www.cebm.ox.ac.uk/resources/levels-of-evidence/ocebm-levels-of-evidence
- Olusanya B. O., Neumann K. J., Saunders J. E. (2014). The global burden of disabling hearing impairment: A call to action. Bulletin of the World Health Organization, 92(5), 367–373. 10.2471/BLT.13.128728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orji A., Kamenov K., Dirac M., Davis A., Chadha S., Vos T. (2020). Global and regional needs, unmet needs and access to hearing aids. International Journal of Audiology, 59(3), 166–172. 10.1080/14992027.2020.1721577 [DOI] [PubMed] [Google Scholar]
- Page M. J. McKenzie J. E. Bossuyt P. M. Boutron I. Hoffmann T. C. Mulrow C. D. Shamseer L. Tetzlaff J. M. Akl E. A. Brennan S. E. Chou R. Glanville J. Grimshaw J. M. Hróbjartsson A. Lalu M. M. Li T. Loder E. W. Mayo-Wilson E. McDonald S., … Moher D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ, 372, n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pronk M., Deeg D. J. H., Versfeld N. J., Heymans M. W., Naylor G., Kramer S. E. (2017). Predictors of entering a hearing aid evaluation period: A prospective study in older hearing-help seekers. Trends in Hearing, 21, 2331216517744915. 10.1177/2331216517744915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pronk M., Meijerink J. F. J., Kramer S. E., Heymans M. W., Besser J. (2019). Predictors of purchasing a hearing aid after an evaluation period: A prospective study in Dutch older hearing aid candidates. American Journal of Audiology, 28(3S), 802–805. 10.1044/2019_AJA-HEAL18-18-0163 [DOI] [PubMed] [Google Scholar]
- Ridgway J., Hickson L., Lind C. (2015). Autonomous motivation is associated with hearing aid adoption. International Journal of Audiology, 54(7), 476–484. 10.3109/14992027.2015.1007213 [DOI] [PubMed] [Google Scholar]
- Ridgway J., Hickson L., Lind C. (2016). Decision-making and outcomes of hearing help-seekers: A self-determination theory perspective. International Journal of Audiology, 55(Suppl 3), S13–S22. 10.3109/14992027.2015.1120893 [DOI] [PubMed] [Google Scholar]
- Robertson M. A., Kelly-Campbell R. J., Wark D. J. (2012). Use of audiometric variables to differentiate groups of adults based on hearing aid ownership and use. Contemporary Issues in Communication Science & Disorders, 39, 114–120. https://search.ebscohost.com/login.aspx?direct=true&db=cin20&AN=104432789&site=ehost-live&scope=site [Google Scholar]
- Samocha-Bonet D., Wu B., Ryugo D. K. (2021). Diabetes mellitus and hearing loss: A review. Ageing Research Reviews, 71, 101423. 10.1016/j.arr.2021.101423 [DOI] [PubMed] [Google Scholar]
- Saunders G. H., Frederick M. T., Silverman S., Papesh M. (2013). Application of the health belief model: Development of the hearing beliefs questionnaire (HBQ) and its associations with hearing health behaviors. International Journal of Audiology, 52(8), 558–567. 10.3109/14992027.2013.791030 [DOI] [PubMed] [Google Scholar]
- Saunders G. H., Frederick M. T., Silverman S. C., Nielsen C., Laplante-Lévesque A. (2016). Health behavior theories as predictors of hearing-aid uptake and outcomes. International Journal of Audiology, 55(Suppl 3), S59–S68. 10.3109/14992027.2016.1144240 [DOI] [PubMed] [Google Scholar]
- Sawyer C. S., Armitage C. J., Munro K. J., Singh G., Dawes P. D. (2020). Biopsychosocial classification of hearing health seeking in adults aged over 50 years in England. Ear and Hearing, 41(5), 1215–1225. 10.1097/AUD.0000000000000839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schönborn D., Asmail F. M., De Sousa K. C., Laplante-Lévesque A., Moore D. R., Smits C., Swanepoel D. W. (2020). Characteristics and help-seeking behavior of people failing a smart device self-test for hearing. American Journal of Audiology, 29(3), 365–374. 10.1044/2020_AJA-19-00098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sciacca A., Meyer C., Ekberg K., Barr C., Hickson L. (2017). Exploring audiologists’ language and hearing aid uptake in initial rehabilitation appointments. American Journal of Audiology, 26(2), 110–118. 10.1044/2017_AJA-16-0061 [DOI] [PubMed] [Google Scholar]
- Simpson A. N., Matthews L. J., Cassarly C., Dubno J. R. (2019). Time from hearing aid candidacy to hearing aid adoption: A longitudinal cohort study. Ear and Hearing, 40(3), 468–476. 10.1097/AUD.0000000000000641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh G., Launer S. (2016). Social context and hearing aid adoption. Trends in Hearing, 20, 2331216516673833. 10.1177/2331216516673833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh G., Launer S. (2018). Time of day and hearing aid adoption. Trends in Hearing, 22, 2331216518769789. 10.1177/2331216518769789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tahden M. A. S., Gieseler A., Meis M., Wagener K. C., Colonius H. (2018). What keeps older adults with hearing impairment from adopting hearing aids? Trends in Hearing, 22, 2331216518809737. 10.1177/2331216518809737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tran E. D., Vaisbuch Y., Qian Z. J., Fitzgerald M. B., Megwalu U. C. (2021). Health literacy and hearing healthcare use. The Laryngoscope, 131(5), E1688–E1694. 10.1002/lary.29313 [DOI] [PubMed] [Google Scholar]
- van Leeuwen L. M., Goderie T. P. M., van Wier M. F., Lissenberg-Witte B. I., Lemke U., Kramer S. E. (2021). Uptake of hearing aids and hearing assistive technology in a working population: Longitudinal analyses of the Netherlands longitudinal study on hearing. Ear and Hearing, 42(4), 793–802. 10.1097/AUD.0000000000000983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viney L. L., Westbrook M. T. (1976). Cognitive anxiety: A method of content analysis for verbal samples. Journal of Personality Assessment, 40(2), 140–150. 10.1207/s15327752jpa4002_5 [DOI] [PubMed] [Google Scholar]
- Wallhagen M. I. (2010). The stigma of hearing loss. The Gerontologist, 50(1), 66–75. 10.1093/geront/gnp107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wasmann J.-W. A., Lanting C. P., Huinck W. J., Mylanus E. A. M., van der Laak J. W. M., Govaerts P. J., Swanepoel D. W., Moore D. R., Barbour D. L. (2021). Computational audiology: New approaches to advance hearing health care in the digital age. Ear and Hearing, 42(6), 1499–1507. https://doi.org/10.1097/AUD.0000000000001041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weycker J. M., Dillard L. K., Pinto A., Fischer M. E., Cruickshanks K. J., Tweed T. S. (2021). Factors affecting hearing aid adoption by adults with high-frequency hearing loss: The beaver dam offspring study. American Journal of Audiology, 30(4), 1067–1075. 10.1044/2021_AJA-21-00050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2021). World report on hearing. https://www.who.int/publications/i/item/world-report-on-hearing
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-tia-10.1177_23312165231157255 for Factors Influencing Hearing Help-Seeking and Hearing Aid Uptake in Adults: A Systematic Review of the Past Decade by Megan Knoetze, Vinaya Manchaiah, Bopane Mothemela and De Wet Swanepoel in Trends in Hearing