Abstract
Background
This paper describes the development of an eight-week Compassion Focused Therapy for Pain Management (CFT-PM) group. This group was specifically designed for ‘strivers’ a sub-group of people with persistent pain who tend to engage in over-activity and resist making reasonable adjustments to their activity levels to accommodate their persistent pain. ‘Strivers’ tend to cope by ignoring their pain and pushing on through, in the shorter term leading to ‘boom and bust’ activity-related exacerbations of their pain. They also risk the development of additional persistent fatigue and burnout in the longer term.
Method
117 people completed the CFT-PM group; The group was delivered in person (n = 84) but in online format from July 2020 (n = 33). 162 people started the CFT-PM group but 45 dropped-out (27.43%).
Results
There was a significant effect for time across all measures: significant improvement was found for depression, self-compassion, pain-related disability, pain-related anxiety and pain self-efficacy. Pain numeric rating scores were approaching significance. There was a significant main effect of diagnosis; post-hoc t-test analysis found significant improvement for all diagnoses on all measures with the exception of spinal. There was also a significant interaction between time and format: post-hoc t-test analysis found greater improvement for virtual format on self-compassion and pain-related anxiety.
Discussion
Findings suggests that CFT-PM may be a clinically effective group intervention with virtual format showing superior improvement. This approach might be less suitable for certain diagnoses; the spinal group may benefit more from traditional CBT-based PMPs. Limitations include the lack of random selection or allocation to treatment group. Future studies should adopt an experimental design to be able to draw firm conclusions regarding causation and efficacy. Despite these limitations, present findings suggest that CFT-PM may be an effective group intervention worthy of further investigation and clinical application.
Keywords: compassion, pain, strivers, self-compassion, self-kindness, pacing, self-criticism, self-care
Introduction
Psychological approaches to pain management have well-been established for over 50 years and the most recent Cochrane review 1 included 75 randomised control trials of cognitive behavioural therapy (CBT) for pain (n = 9401). Williams et al. (2020) 1 found small to moderate effects of CBT for chronic pain with the strongest effect for mood (mostly depression) then catastrophic thinking, disability and least of all for pain.
The ‘fear avoidance model’ 2 is the most widely used CBT model for working with persistent pain. It explains how catastrophic beliefs about the causes of pain or an inability to cope with pain, can lead to hypervigilance and avoidance of movement or activity. The unintended consequences of this are disuse, deconditioning, depression and ultimately lead to increased pain. CBT-based PMPs aim to reverse this vicious cycle. 2 Core components include psycho-education about the nature of persistent pain, understanding the links between stress and pain; behavioural stress reduction exercises, graded exposure to movement; gentle exercise to improve strength, flexibility; cognitive strategies to recognise and challenge unhelpful thought patterns.
The traditional CBT-based approach includes advice on pacing activities, setting baseline tolerance levels and gradually returning to previously enjoyed goal-directed behaviour. However, in clinical practice it is familiar to see people engaging in a ‘boom and bust’ approach to activity management, on a good pain day engaging in too much activity or trying to catch up on the things that pain has prevented them from doing on bad pain days. This can be understood as a common sense approach to ‘make hay whilst the sun shines’, but unfortunately evidence shows this short-term strategy leads to later flare-ups of pain with further deconditioning and depression. 3
‘Strivers’3,4 are a sub-group of people with persistent pain who tend to present with lower levels of pain-related disability, because they have not fallen into the vicious cycle of ‘fear avoidance’. 2 Rather, they tend to engage in the opposite behaviour of over-activity, resisting making reasonable adjustments to their activity levels to accommodate their persistent pain. ‘Strivers’ tend to cope by ignoring their pain and pushing on through despite their pain. Unfortunately this ‘striving’ behaviour leads to activity-related flare-ups or exacerbations of their pain in the shorter term. It also risks the development of additional persistent fatigue and burnout in the longer term. Striving tends to be associated with self-critical thoughts that are triggered by attempts to regulate over-activity. For example, ‘strivers’ might report ‘I am lazy’ or ‘I am stupid’ when they are trying to slow down and pace their activity or if having to rest during a flare-up.3–5
Compassion Focused Therapy (CFT)6–8 is an evolution-informed, biopsychosocial approach to understanding and alleviating human suffering. It draws upon both evolutionary psychology and Buddhist principles, employing a non-judgemental approach that acknowledges that humans have ‘tricky brains and tricky bodies’ which can have consequences in modern life.6–8
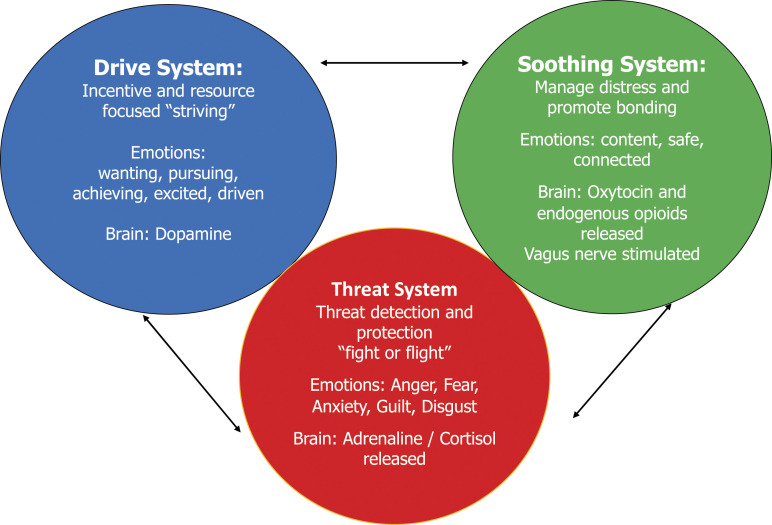
Gilbert (2009)6–8 proposes the CFT ‘3 systems approach’ to understanding the balance between the three human motivational states of threat, drive and soothing (see Figure 1).
Figure 1.
‘3 systems’ model of human motivational states (Gilbert, 2009)6–8.
Strategies to tackle the ‘Threat system’6–8 have already been well established in CBT for pain management. Indeed, stress management is a core component of most PMPs. 9
The ‘Drive’6–8 system can be seen as useful addition to understanding our normal reactions to pain; ‘Striving’ behaviour can been understood as having its evolutionary roots in the resource-seeking motivation of our ancestors who lived in times of feast and famine, when food was not always readily available so they gorged during times of plenty. Other key resources activating the drive system include finding shelter and a mate to reproduce with.6–8
The ‘Soothing system’6–8 comprises the mammalian attachment system. These neural pathways evolved to subserve the secure attachments and the evolution of a longer childhood in mammals. This soothing/affiliation system includes the parasympathetic branch of the autonomic nervous system (vagus nerve) and the oxytocin and endogenous opioid pathways. 10
Gilbert (2009)6–8 proposes in the CFT 3 systems model, that the absence of threat (safety) allows mammals to engage in resource-seeking behaviour. The soothing system then assesses whether resource needs are met and the proximity of supportive others (safeness).
Compassion has been defined as ‘a sensitivity to the suffering of self and others and a deep commitment to prevent or alleviate it’.6–8 Self-Compassion has been proposed to be part of the soothing-affiliative system of affect regulation and has been linked to physiological processes that can exacerbate or soothe pain, for example, heart rate variability and oxytocin-endorphin pathways.10,38
Purdie and Morley 11 emphasised the role of self-compassion as a buffer in pain management, associated with more adaptive coping rather than fear-avoidance. Costa and Pinto Gouveia 12 found that experiential avoidance and self-compassion were the main factors in predicting psychological distress. Vowles et al. (2014) 13 proposed that self-compassion is a key psychological mediator in acceptance-based approaches to chronic pain and this was supported by Carvalho et al. (2018) 14 who found that self-compassion was associated with greater levels of pain acceptance and lower levels of depression, stress and anxiety.
Compassion-based interventions for people with a range of long term physical conditions have been shown to lead to a reduction in depression and anxiety, greater acceptance of the long term nature of the condition, improved emotional regulation and reduced social isolation. 15 Gooding et al. 16 report that a CFT for pain group helped people to reduce feelings of isolation, improved ability to self-reassure, learn new ways of coping and develop a growing acceptance of the limitations associated with their pain.
Lanzaro et al. (2021) 17 conducted a recent systematic review examining whether compassion-based interventions lead to improvement in pain-related outcomes. They identified 16 studies and found promising benefits in terms of reduction in pain intensity and pain interference, greater pain acceptance and pain self-efficacy, reduction in pain catastrophizing, pain anxiety and pain disability. However, they advise caution in the interpretation of these findings, given that the studies identified were judged to be of poor quality experimental design, lacking control conditions or blinding. Further there was wide variation in the types of compassion-based interventions included, pain diagnoses, pain outcomes measures administered and timepoints for data collection.
Whilst Lanzaro et al. (2021) 17 found insufficient current evidence for the effectiveness of compassion-based treatment on pain outcomes, they have highlighted the importance of self-compassion in pain management. Further, they have proposed that understanding the relationship between self-compassion and persistent pain may lead to the development of more specific evidence-based compassion focused interventions for pain management. 16
The present authors propose that applying a CFT ‘3 systems’6–8 model to pain management may address some of the gaps in the existing models. We propose that for ‘strivers’ persistent pain can lead to a reduction in activity that evokes a sense of shame when people compare themselves to others and how they used to be before the onset of their pain. This shame then leads to self-critical thoughts and self-blame which can trigger an urge to ‘strive’ to engage in a burst of activity to regain previous status. In the short term, this burst of activity is associated with a sense of pleasure and pride which serves to reinforce this striving behaviour. Unfortunately in the longer term, it leads to exacerbation of pain, further shame and increases risk of burnout and fatigue. Thus, the drive motivational state is triggered by an internal threat, social comparison to others and pre-pain self. We propose that this underpins the ‘boom and bust’ coping strategy of ‘strivers’.
A Compassion-based approach to addressing this problem would initially be skills-based to develop the soothing system and strategies to regulate ‘striving’ urges, (Compassionate Mind Training (Gilbert 2009)6–8 Later therapeutic techniques would then involve deriving multiple selves formulations to understand historical drivers for this striving behaviour (Compassion Focused Therapy, Gilbert 2009).6–8 This differs from existing approaches to pain management in that it encourages the development of safeness, building a wise compassionate self to directly counter stressful and striving urges. Fear-avoidant CBT approaches appear to focus on the threat-related aspects of this model and acceptance-based approaches can be understood to focus on the drive-related aspects. The CFT 3 systems model of pain management therefore proposes a novel therapeutic approach to hold both threat and drive systems in mind simultaneously, whilst developing the skills and understanding to respond compassionately, preventing any further engagement in unhelpful behaviours with the unintended consequences of further suffering.
Aims of this service evaluation
To investigate whether completing this innovative CFT-PM group leads to a significant reduction in pain-related outcomes: depression, pain-related anxiety and pain-related disability. It also aims to investigate whether there is an increase in self-compassion, self-kindness and pain self-efficacy.
Methods
The CFT-PM group was developed in 2015 as a collaboration between two pain services in the North East and North West of England. Both services were multidisciplinary pain services. At the time of writing, only one author was still working in pain management and thus data is only presented from the North West of England.
The authors completed introductory and advanced training in Compassion Focused therapy (CFT6–8) delivered by the Compassionate Mind Foundation. This ‘3 systems’ and ‘multiple selves’ work was then combined with evidence-based pain management approaches, to propose a Compassion Focused Therapy model of Pain Management.3–5 For example, ‘threat’ (see Figure 1) is a well-established area in pain management and behavioural stress reduction is a core component of most pain management programmes. However, understanding ‘drive’ is the new addition to pain management as it offers a novel perspective to understand the impact of ‘striving’ on pain-related activity, particularly activity-related flare-ups. This was introduced as a key innovation for the CFT-PM group (see Table 1 above for an outline of the content for the 8 weekly sessions).
Table 1.
Treatment outline of compassion focused therapy for pain management group.
| Week | Session content (Each weekly session = 3 hours) |
|---|---|
| 1 | Information session: Evolution of our tricky brains – why we need self-compassion, biopsychosocial understanding of pain, 3 systems approach and the evolution of compassion as a new approach to pain management |
| 2 | Stress and pain: Understanding how autonomic arousal exacerbates pain, behavioural stress reduction with breathing and relaxation, calming body and mind |
| 3 | Striving and pain: Understanding how dopamine drive triggers flare-ups of pain, using mindfulness to observe our reactions to events, notice those unhelpful urges |
| 4 | Compassionate imagery: Understanding how soothing can balance stress and striving, creating a safe place, compassionate companion and compassionate self |
| 5 | Multiple selves ‘threat’ - understanding our anxious and angry selves, recognising how those side of our tricky bodies and minds link to past coping |
| 6 | Multiple selves ‘drive’ - understanding our critical self and building our compassionate self, again link to past coping, when did I learn to criticise myself? |
| 7 | Working with our inner critic: Applying compassionate selves to pain-related suffering: Hanging out in the green zone to reduce risk of flare-ups and burnout |
| 8 | Maintaining change: The longer term benefits of adopting self-compassion and the pain journey, flare-up management and maintaining progress |
| ** | Quarterly booster drop-in sessions: A follow-up opportunity to consolidate CFT-PM skills, problem solve and further practice (every 3 months) |
aQuarterly booster drop-in sessions (offered in March, June, September and December).
Referral pathways and collection of outcome measures
In this multidisciplinary (MDT) pain service in the North West of England, all people referred to the service complete opt-in questionnaires, prior to being seen for first assessment with a medical consultant. They can then be referred onto the pain rehabilitation team for further assessment with the physiotherapists and psychologists. This secondary referral process involves watching an online video about pain self-management and completion of further opt-in questionnaires. People are then triaged based upon the level of distress identified in their scores, those with highest level of distress are offered an assessment with a psychologist.
Identification and assessment of ‘Strivers’
The physiotherapists and psychologists in the pain rehabilitation team use their clinical judgement to identify ‘strivers’3,4 those people with chronic pain who tend to push themselves to keep going, despite their pain. ‘Strivers’ tend to use distraction-based coping, ignoring their pain, remaining active and pushing on through, clearly describing a ‘boom and bust’ approach to activity with evidence of activity-related flare-ups. They are more likely to still be working and often in care-giving roles, for example, to date occupation of CFT-PM attendees has included nurses, support workers, teachers, social workers, psychologists, psychiatrists and other medical doctors.
Psychological assessment and formulation might identify high levels of shame and self-critical thoughts regarding the impact of their pain on their functioning (‘I am a failure’), a tendency to blame themselves for any inability to complete a task (‘I am lazy’). They might be highly skilled at caring for others but often report poor self-care and an inability to prioritise their own needs. Striver outcome measures are likely to show lower levels of pain-related disability but still high pain-related distress, including high depression and pain-related anxiety. Any self-compassion measure collected at the assessment phase is likely to show very low self-compassion and very low self-kindness. Table 7 in the appendices shows mean pre-treatment outcome measures for people currently offered virtual CFT-PM and those offered a place on the more traditional virtual PMP.
In this service evaluation, people presenting for psychological assessment with this ‘striver’ formulation were given information about the CFT-PM group and asked if they wished to consider attending for this novel group treatment. The difference between CFT-PM and the more traditional MDT PMP approach was explained and emphasised that the CFT-PM group would be a psychology only intervention. If people then chose to attend for the CFT-PM group, then they consented to attend for a minimum of 6 of the 8 weekly sessions. They were aware that they would be asked to leave the group if they missed more than two sessions. A small number of people also chose to continue with medical interventions or individual physiotherapy support alongside their CFT-PM group.
Treatment
The CFT-PM was delivered in group format and comprised eight weekly sessions, each session is delivered once per week for 3 hours with a 30-min midpoint break. Thus, total group therapy contact time was 20 hours. The content for each consecutive weekly session is described briefly in Table 1 above. A written manual was also provided at the start of the CFT-PM group, with detailed content as a reminder for each weekly session. People were also invited to attend quarterly drop-in booster sessions, with each booster session comprising 2 hours of problems solving to consolidate skills and opportunity for further practice.
The CFT-PM groups were delivered in person, in an outpatient hospital setting, from April 2015-March 2020. Due to the social distancing restrictions of the COVID pandemic, from July 2020 all groups were delivered in online format, using Microsoft Teams videoconference software. The intensity of treatment remained once per week for 3 hours sessions. Some of the of the content was adapted for virtual format, for example, including a pre-recorded video demonstration of diaphragmatic breathing exercises to supplement on screen demonstration.
Design
This service evaluation was a repeated measures design. Data comprised routine outcome measures completed by an anonymised opportunity sample of 117 consecutive people who had successfully completed the CFT-PM group during the time period April 2015 – August 2021. Full set of data was available for 117 people.
Data collection
Demographic data was collected during the multidisciplinary team assessment phase, prior to commencing the CFT-PM group. This data included age, gender, diagnosis, employment status and ethnicity. The outcome measures are detailed in Table 2 and comprise 6 self-report pain-related measures covering the areas of self-compassion, depression, pain-related anxiety, pain-related disability, pain self-efficacy and pain intensity. Pre-treatment outcome measures were completed on the first day of the CFT-PM group. All post-treatment outcome measures were completed on the final day. Anonymised patient satisfaction surveys were also completed on the final day of the CFT-PM group.
Table 2.
Self-report outcome measures administered: 18 .
| Measure | Items | Clinical significance |
|---|---|---|
| Self-compassion scale 19 (SCS) | 12-item valid and reliable short form measure of self-compassion, with a possible range of scores from 0–30 | Higher scores indicate greater levels of self-compassion. Components include self-kindness, self-judgement, common humanity, isolation, mindfulness and over-identification |
| Excellent internal consistency published, Cronbach’s alpha ≥ 0.86 19 | ||
| Centre for epidemiological studies of depression scale 20 (CES-D) | 20-item valid and reliable measure of depression with a possible range of scores of 0–60 | Higher scores indicate more depressive symptomatology |
| Excellent internal consistency published, Cronbach’s alpha ≥ 0.9 20 | ||
| Pain anxiety symptom scale short form 20 21 (PASS) | 20-item valid and reliable measure of fear of pain with scores from 0–100 | Higher scores indicate greater anxiety |
| Excellent internal consistency published, Cronbach’s alpha ≥ 0.9 21 | ||
| Roland Morris disability questionnaire 22 (RMDQ): | 24-item valid and reliable check-list of lower back pain–related disability with scores from 0–24 | Higher scores indicate higher disability |
| Excellent internal consistency published, Cronbach’s alpha ≥ 0.91 22 | ||
| Pain self-efficacy questionnaire 23 (PSEQ) | 10-item valid and reliable measure of confidence of people with any type of chronic pain to engage in activity despite their pain. Possible scores range from 0–60 | Higher scores indicate greater self-efficacy beliefs, lower scores reflect a focus on the pain and seeking pain relief before increasing activity |
| Excellent internal published consistency, Cronbach’s alpha ≥ 0.92 23 | ||
| Pain numeric rating scale24,25 (NRS) | Single item measure of current pain with range of scores from 0–10 with 0 being ‘no pain’ and 10 being ‘worst pain imaginable’: This is the standard pain measure used in this hospital trust | Higher scores indicate greater level of pain |
Data from 2015–2020 was collected in paper format and groups were delivered in person in an outpatient hospital setting. From 2020–21 the data was collected electronically via Microsoft Forms and the CFT-PM group was delivered in virtual format, via Microsoft Teams. Total contact time remained 20 h for the virtual format.
Participants
Demographic data was available for 117 people. Mean age was 45.86 (range 21–77, see Table 3). 94% reported being female (n = 110) and 6% male (n = 7). Fibromyalgia was the most common diagnosis (n = 51), spinal (n = 28: low back, neck and thoracic), neuropathic (n = 18: chemotherapy induced, Multiple Sclerosis, Complex Regional Pain Syndrome, migraine) pelvic (n = 16: vulvadynia, pudendal neuralgia, endometriosis) and active inflammatory conditions were the least common diagnosis (rheumatological n = 4).
Table 3.
Age range.
| Age range (n = 117) | N | % of total |
|---|---|---|
| 18–29 | 10 | 8.54 |
| 30–39 | 27 | 23.07 |
| 40–49 | 34 | 29.06 |
| 50–59 | 35 | 29.91 |
| 60–79 | 12 | 10.26 |
89 people were currently in employment (76.3%) and this included many working in caring professions: nurses, health care assistants, social workers, teachers, psychologists, psychiatrists and other medical doctors. 28 people were not working (23.7%) and this included retired people and unpaid family carers. White British n = 58 comprised the largest ethnic group (49.6%), White Other n = 15 (14.7%), British Pakistani n = 5 (4.3%), Black British n = 3 (2.6%) British Indian n = 2 (1.7%) and Chinese n = 1 (1%). Ethnicity data was missing for 33 people (28.2%).
Mean number of CFT-PM group treatment sessions completed was 7.79 or 18.98 hours (range 6–8 sessions or 15–20 hours). During the assessment phase, everybody offered a place on the CFT-PM had committed to attending a minimum of 6 sessions, or they would not be able to continue. 164 people started the CFT-PM group but 45 dropped-out (27.43%). Main reasons given were return to work, carer responsibilities, non-pain-related illness and flare-up of pain. Mean number of sessions completed by drop-outs = 3.88 (mean attendance of drop-outs = 11.64 h). Table 8 includes demographics and pre-treatment outcome measures for treatment completers and drop-outs.
Format
84 people attended the CFT-PM group in person (71.79%) and 33 completed in virtual format (28.21%).
Ethics
The authors applied the Health Research Authority (HRA) Decision tool to this project. The HRA tool indicated that this was a service evaluation and as such did not require application for formal ethical approval. This service evaluation was subsequently registered with the Clinical Audit Department, Manchester University NHS Foundation Trust as SE-58: Effectiveness of Compassion Focused Therapy for Pain Management Groups.
This outcome data was collected as part of routine clinical practice and as such, the authors did not seek consent to use this data for research purposes. The authors have subsequently discussed the use of this data with the follow-up patients attending for quarterly Compassion booster drop-in sessions and they advised that they were keen for the work to be shared with other pain services so that other patients may benefit from this approach. The authors have taken great care to ensure that this was secondary analysis of anonymised data, ensuring that no patient identifiable details were included in this service evaluation.
Statistical analyses
All anonymised demographic and outcome measure data was entered into Microsoft excel and subjected to statistical analysis using SPSS software. Repeated measures MANOVA was used to examine treatment effects upon the 6 outcome measures over time. Mixed MANOVA was used to examine the impact of the independent variables of diagnosis and treatment format upon the 6 outcome measures. Key population variance assumptions were checked using Box M plot and significance set at p < .001. Missing data was excluded from the analyses. Treatment completion was investigated using independent t-tests, with significance set at p < .001 to correct for multiple comparisons. (Table 4)
Table 4.
Mean Pre/Post-treatment outcomes and percentage improvement.
| Measure | Mean pre-treatment score | Mean post-treatment score | Mean change (%) |
|---|---|---|---|
| Self-compassion (SCS) | 11.68 | 15.44 | 3.76 (32.19) |
| Depression (CES-D) | 30.75 | 22.77 | 7.98 (25.95) |
| Pain anxiety (PASS) | 50.46 | 43.41 | 7.05 (13.97) |
| Pain disability (RMDQ): | 14.06 | 12.33 | 1.73 (12.30) |
| Pain self-efficacy (PSEQ) | 25.65 | 33.14 | 7.49 (29.2) |
| Pain numeric rating scale | 4.98 | 4.58 | 0.4 (8) |
Results
Statistical analyses
General change from pre- to post-treatment
A repeated measures MANOVA was completed to explore whether the CFT-PM group outcome measures significantly differed over time from pre-treatment to post-treatment. Across all outcome measures, there was a significant main effect of time (pre- to post-treatment), F (7,88) = 16.73, p < .001, with a large effect (η2 = 0.571). For the specific outcome measures, there was a significant main effect of time for depression scores F (1,94) = 67.15, p < .001, with a large effect (η2 = 0.417), self-compassion F (1,94) = 64.69, p < .001, with a large effect (η2 = 0.408), pain-related disability F (1,94) = 32.79, p < .001, with a large effect (η2 = 0.259), pain anxiety F (1,94) = 22.33, p < .001, with a large effect (η2 = 0.192), and pain self-efficacy F (1,94) = 75.21, p < .001, with a large effect (η2 = 0.444). The pain numeric rating scores were approaching significance F (1,94) = 3.79, p = .054, with a small effect (η2 = 0.039).
Planned contrasts were completed using six paired samples t-tests to explore these significant main effects of time for the outcome measures. A Bonferroni correction was applied to account for the multiple comparisons (0.05/6) and a corrected p-value was applied (p = .01). Participants depression scores significantly reduced from pre- to post-treatment t (116) = 9.14, p < .001, d = 0.85. Participants self-compassion scores significantly increased from pre- to post-treatment, t (115) = −8.96, p < .001, d=0.83. Pain-related disability scores significantly reduced from pre- to post-treatment t (116) = 4.89, p < .001, d = 0.45. Pain anxiety scores additionally significantly reduced from pre- to post-treatment t (115) = 5.03, p < .001, d = 0.47. Finally, pain self-efficacy scores significantly increased from pre- to post-treatment t (99) = −8.05, p < .001, d = 0.81. In summary, all outcome measures changed in the expected direction from pre- to post-treatment with self-compassion, self-kindness and pain self-efficacy significantly improving, and depression, pain-related disability, and pain-related anxiety all significantly decreasing.
Differences from pre- to post-treatment by diagnosis
To explore whether there were differences in outcomes based on pain diagnosis, a mixed MANOVA was utilised with the within-subject factor of time and the between-subjects factor of diagnosis. No significant time by diagnosis interaction was found (F (21,261) = 1.96, p = .353. However, there was a significant main effect of diagnosis, F (21, 261) = 2.94, p < .001, with a large effect (η2 = 0.191).
Planned contrasts were completed using 6 paired samples t-tests to explore main effects of diagnosis for the outcome measures. A Bonferroni correction was applied to account for the multiple comparisons (0.05/6) and a corrected p-value was applied (p = .01). Scores for all diagnostic groups improved significantly from pre- to post-treatment across (see Table 6 in appendices) with the exception of Spinal: no significant effect was found for pain-related anxiety (t = 0.85, df = 26, p = .404), or pain self-efficacy (t = .89, df = 21, p = .72) and pelvic: no significant effect was found for pain-related disability (t = 1.38, df = 15, p = .190).
Differences from pre- to post-treatment by format
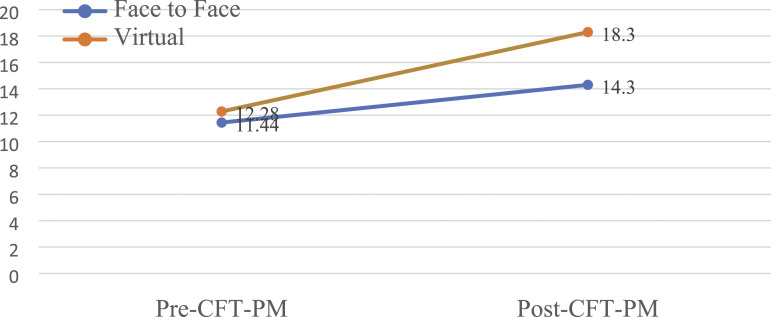
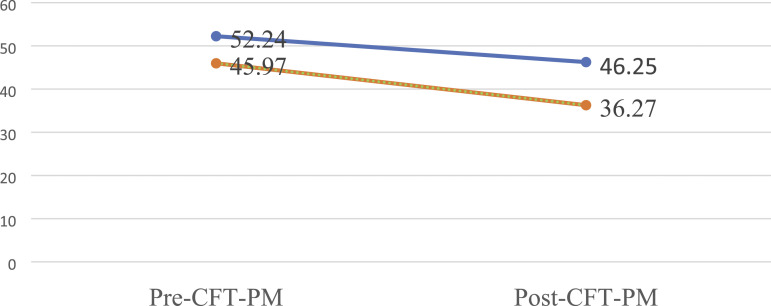
A mixed MANOVA was completed to explore the differences across time (pre and post) for the groups based on format. There was a significant interaction between time and format F (7, 87)= 3.23, p = .004, with a large effect (η2 = 0.206). There was additionally a significant main effect of format, F (7, 87)= 3.74, p = .001, with a large effect (η2 = 0.231). From carrying out post-hoc contrasts, both formats significantly increased on self-compassion and pain self-efficacy and significantly reduced on depression, pain-related disability and pain-related anxiety. When comparing in person with online formats, groups only significantly differed on the post-group self-compassion scores and post-group pain anxiety (online group significantly higher self-compassion and lower pain anxiety). (Figures 2 and 3)
Figure 2.
Mean pre- to post-treatment scores by format – Self-Compassion Scale (SCS, p < .001).
Figure 3.
Mean pre- to post-treatment scores by format – Pain Anxiety (PASS, p < .009).
Comparison of baseline scores for treatment completers versus non-completers
Independent t-tests were completed to explore whether there were differences in outcomes based on treatment completion. The between-subjects variable was whether or not people had completed the full CFT-PM group; the independent variables were age and score on pre-treatment outcome measures. Table 6 in the appendices shows mean scores and analyses. Figure 6 shows difference in mean pre-treatment Self-Kindness score and Mean Pain VAS score for treatment completers and for drop-outs. Drop-outs appear to have higher pre-treatment age, higher pain scores, higher depression, higher pain-related disability, higher anxiety and lower self-compassion, lower pain self-efficacy and lower self-kindness. However, the only pre-treatment difference to achieve statistical significance was for Self-Kindness score, with mean drop-out scores being 11.2% lower than for treatment completers (F = 7.533, t = 1.639, df = 171, p < .007).
Patient satisfaction survey ratings for CFT-PM
Anonymised patient satisfaction surveys were administered on the final day of the CFT-PM group. This comprised a series of 5 ratings and opportunities to add further qualitative feedback. 80% people rated the CFT-PM as extremely valuable (33%) or very valuable (47%). 67% people reported finding the online format very easy (27%) or easy (40%). 73% reported finding the theory to be helpful (a great deal 33%, a lot 40% and 20% moderate amount). 93% people reported finding the compassion-based exercises to be helpful (40% a great deal, 40% a lot and 13% a moderate amount). 100% reported that they would recommend the CFT-PM to friends or family if they needed it.
Discussion
This paper describes the development and clinical outcomes for a novel Compassion Focused Therapy for Pain Management group. Comparison of pre- and post-treatment outcome measures suggests that for this small uncontrolled sample, it was a clinically effective intervention, with improvement in mean scores found across all areas measured. It should be noted that this was a service evaluation rather than formal experimental design; thus, the observed improvements could have happened by chance or by the passage of time alone. The routine outcome measures collected suggest that mean self-compassion scores increased by 32% moving from the clinical to non-clinical range. 19 Mean depression scores reduced by 26% from moderate to mild levels 20 mean pain-related anxiety scores improved by 14% from severe to moderate range. 21 Mean pain-related disability scores improved by 12% remaining in the moderate range 22 mean pain self-efficacy scores improved by 29%. 23 A small reduction was also found for mean pain ratings (8%) although this is likely to be of questionable clinical significance. Broadly, these findings fit with those of the Lanzaro et al. (2021) 17 systematic review of self-compassion pain management and also Austin et al. (2020) 15 systematic review of compassion-based interventions for long term conditions.
When outcomes were examined by diagnosis, some groups appeared to derive greater benefit than others. For example, those with neuropathic diagnoses showed the greatest reduction on pain-related anxiety (mean reduction was 11.54 points), whereas those with spinal diagnoses showed the least benefit (mean reduction was only 2.4 points). It is noteworthy that the CFT-PM group was offered to people who might not usually have been included in our traditional pain management programme, for example, those with progressive neurological disorders (multiple sclerosis) or those with ongoing medical interventions (injection therapy). Analysis by diagnosis supports their inclusion in this pain psychology intervention and the authors recommend that this clinical approach should be continued. However, group outcomes for the spinal diagnoses were less encouraging, suggesting that they should continue to be offered our standard multidisciplinary pain management programme, which includes regular physiotherapist-led exercise sessions as a core component. The authors speculate that the spinal group might have struggled to challenge any threat-related catastrophic thoughts about the cause of their pain, without the opportunity to engage in regular physiotherapy sessions. This speculation was based upon the observation that at the end of the CFT-PM group, some people with spinal pain continued to report fear-avoidant beliefs about the cause of their pain and the safety of movement.2,26 However, this speculation this was not investigated in any systematic manner and thus, would require further exploration before any firm conclusions could be drawn.
It is noteworthy that the pelvic group appeared to show a smaller reduction in pain-related disability. However, their pre-treatment scores were lower than other groups and thus, relative improvement was smaller. Those with pelvic diagnoses did make clinically significant improvement on other measures and thus, the authors recommend their continued inclusion in the CFT-PM groups. Indeed, the service has recently trialled a CFT-PM group solely for people with pelvic pain and the initial findings suggests that they derive even greater benefit from this pelvic-specific group.
A change in format was imposed in 2020 due to the unexpected social distancing requirements of the COVID19 pandemic. This enabled the comparison of scores for those completing the group in person (n = 84) versus those who had completed the group online (n = 33). The analyses are reassuring in that significant improvement was still found across all measures when the group was conducted online. Indeed, two measures showed superior effectiveness for the virtual format, with online groups demonstrating greater improvement in self-compassion and pain-related anxiety. The authors were surprised at this finding and speculate that it may relate to the striving nature of the people offered a place on this group. They tended to be over-active and describing evidence of activity-related flare-ups. Thus, attending the group virtually from home, without the requirement to travel to the group venue, might have contributed to a beneficial reduction in their overall activity levels.
It should be noted that there were also significant contextual factors occurring during the COVID19 pandemic that may well have impacted upon outcomes, either as mediators or moderators of treatment effects. Whilst there is evidence that virtual formats can be effective therapeutic formats for the delivery of pain management programmes1,18 and psychological therapy27,28 further research would be required to understand the relative contribution of format and contextual factors to CFT-PM outcomes during the pandemic.
Unfortunately the current evaluation was not able to investigate the relationship between self-compassion and pain acceptance, due to insufficient data collection. The routine outcome measures for the CFT-PM did initially include the Chronic Pain Acceptance Questionnaire (CPAQ),13,29,33 but this was excluded from electronic data collection during the COVID pandemic due to authors’ fears that patients may not have been willing to complete an additional self-report measure. This additional measure has now been reinstated for future groups with the hope that it may help with further elucidating any changes associated with improving self-compassion.
The CFT-PM was associated with small reductions in pain but greater improvement in pain-related distress and pain-related disability. Thus, this approach appears to have minimal impact on soothing pain itself, rather focuses on soothing the impact of pain upon mood and function. This is an important theoretical distinction but given the major limitations of this service evaluation, it would be worthy of further rigorous investigation.
Thus, understanding the relationship between the ‘3 systems’ in the CFT model of pain management does appears to have led to the development of a more specific evidence-based compassion focused intervention for pain management. The current authors suggest that this fits well with the proposal from Lanzaro et al. regarding the benefits of understanding the relationship between self-compassion and pain management. 17
Unfortunately the current service evaluation is not able to elucidate whether the CFT ‘3 systems model’ can successfully conceptualise both ‘fear-avoidance’ 2 and acceptance 29 within same theoretical model. Patient feedback in the anonymous satisfaction survey appeared to support the beneficial role of self-compassion as regulating threat-related avoidance, self-critical social comparison and drive-related acceptance of allowing the compassionate mind to make reasonable adjustments, without judgement or self-blame. The authors are planning to explore this further with a qualitative study, asking people who have successfully completed CFT-PM to describe the benefits and the possible mechanism of change.
Many patients reported the benefits of attending a group rather than individual therapy. Whilst this has not been explored in a systematic manner, CFT is a prosocial therapy and it may be that this emphasises the safeness aspect for the group to work well, compared to individual therapy. Perhaps, this could be explored further in future studies, whether group bonding and secure attachments impact upon the effectiveness in terms of reducing pain, pain-related disability and pain-related distress? Wilson et al. (2016) 30 conducted a systematic review of the impact of group processes upon the outcomes for those attending group pain management programmes. They have proposed that there are both moderators, (e.g. group frequency and duration, the mix of participants’ age and gender, cultural and social group) and mediators, (e.g. catastrophizing, pain-related knowledge and self-efficacy) and the inclusion of group tasks, outputs or ‘products’ that might facilitate the group effect. Whilst they did not specifically address group bonding and secure attachments, further research might establish whether they are moderators or mediators for group outcomes.
This service evaluation had significant limitations; it did not include a control group to allow for treatment comparison and there was no random selection or random allocation to treatment group to allow for causal inference to be drawn. The authors recommend that future evaluation should adopt an experimental design. Within this hospital-based MDT pain service in the North West of England, people do complete outcome measures at various timepoints on the referral pathway including on opt-in to the pain service prior to medical consultation and again on referral to the physiotherapists and psychologists in the pain self-management team. Thus, this service evaluation may have benefitted from comparison with scores collected at earlier timepoints in the service, with people acting as their own wait list control, to determine whether time alone might have led to the significant change in the outcome measures.
There is also the theoretical limitation in that there is no objective measure for the striver criterion. Thus, people were invited to engage in this CFT-PM based solely upon the authors’ clinical judgement as to whether they were engaging in over-activity and high levels of self-criticism. The authors include data in the appendices (Table 9) that distinguishes those attending traditional pain management programmes from this CFT-PM group: This summary table suggests that ‘Strivers’ present with lower pain-related disability, lower pain-related anxiety and higher pain self-efficacy. Future studies would benefit from a more formal investigation of these pre-treatment differences.
Those willing and able to complete the CFT-PM in virtual format were a self-selecting group. The authors attempted to be as inclusive as possible, for example, ensuring those with visual impairment could access the group via telephone. However, there is the possibility that people with digital poverty were excluded from this virtual group, whether due to lack of access to wi-fi signal or to digital apparatus, or a lack of training in using this format. Many people used smartphones to access the virtual CFT-PM group meetings and the authors prepared information on downloading and using MS Teams application software. None the less, this remains a potential significant barrier to access for some people with persistent pain. The authors will continue to monitor for those people who are not willing or able to benefit from this approach, either due to digital poverty or anxiety about using online format. It may be that the pain service could support people by lending digital equipment or offering training and support in using online services.
Conclusions and recommendations
This service evaluation provides preliminary evidence that Compassion Focused Therapy may be a clinically effective group intervention for pain management. Significant improvement was found for self-compassion, depression, pain-related anxiety, pain-related disability and pain self-efficacy. However, this approach might not be appropriate for all diagnostic groups, strivers with a spinal diagnosis should always be offered multidisciplinary pain rehabilitation. Strivers with neuropathic pain and pelvic pain should continue to be offered this compassion-based approach. The virtual format was found to be superior to meeting in person for improving self-compassion and pain-related anxiety, with at least equivalent improvement for all other outcome measures. This was an unexpected but reassuring finding, when services are being delivered online during a global pandemic. It may well be that this is an enduring change in service delivery for those people who are well-equipped to engage in this innovative and convenient virtual treatment.
Acknowledgements
The authors would like to thank Professor Paul Gilbert and the Compassionate Mind Foundation (CMF), particularly Mary Welford who kindly presented on Compassion Focused Therapy at the Pain Management Programme SIG conference in Manchester in 2015. We would like to thank our pain psychology colleagues Doug Crix, Chris Penlington, Rebecca Chasey and the CMF Physical Health SIG who have so generously shared their ideas and experiences. Finally, we would like to extend our heartfelt gratitude to Professor Steven Morley, who inspired this journey into Compassion and pain management. We would like to offer our heartfelt gratitude to the service users who so generously participated in this service evaluation, offering their time and honest appraisal of our service to benefit future service users.
Appendix.
Table 5.
Post-hoc t-tests on diagnosis.
| Diagnosis | Pre-group | Post-group | T | df | P |
|---|---|---|---|---|---|
| Depression | |||||
| Spinal | 32.75 | 26.75 | 3.09 | 27 | .005 |
| Neuro | 27.81 | 19.64 | 5.12 | 21 | <.001 |
| Pelvic | 24.50 | 18.19 | 2.86 | 15 | .012 |
| Fibromyalgia | 32.88 | 23.37 | 6.88 | 50 | <.001 |
| Self-compassion | |||||
| Spinal | 11.17 | 12.89 | −2.63 | 26 | .014 |
| Neuro | 12.45 | 17.77 | −5.65 | 21 | <.001 |
| Pelvic | 13.16 | 17.47 | −4.66 | 15 | <.001 |
| Fibromyalgia | 11.15 | 15.14 | −5.68 | 50 | <.001 |
| Pain-related disability | |||||
| Spinal | 13.61 | 11.71 | 3.13 | 27 | .004 |
| Neuro | 13.27 | 11.14 | 2.21 | 21 | .038 |
| Pelvic | 11.75 | 10.13 | 1.38 | 15 | .190 |
| Fibromyalgia | 15.37 | 13.88 | 2.50 | 50 | .005 |
| Pain-related anxiety | |||||
| Spinal | 48.11 | 45.67 | 0.85 | 26 | .404 |
| Neuro | 52.86 | 41.32 | 3.22 | 21 | .004 |
| Pelvic | 49.44 | 40.25 | 2.71 | 15 | .016 |
| Fibromyalgia | 50.98 | 44.12 | 3.38 | 50 | .001 |
| Pain self-efficacy | |||||
| Spinal | 28.82 | 33.14 | −1.89 | 21 | .072 |
| Neuro | 24.05 | 32.10 | −3.48 | 19 | .003 |
| Pelvic | 23.36 | 31.57 | −3.20 | 13 | .007 |
| Fibromyalgia | 25.14 | 34.20 | −7.11 | 43 | <.001 |
Table 6.
Post-hoc t-tests comparing pre- to post-group scores for each format.
| Pre-group | Post-group | T | Df | P | |
|---|---|---|---|---|---|
| Depression | |||||
| F2F | 31.51 | 23.51 | 7.92 | 83 | <.001 |
| Online | 28.82 | 20.88 | 4.54 | 32 | <.001 |
| Self-compassion | |||||
| F2F | 11.44 | 14.30 | −7.07 | 82 | <.001 |
| Online | 12.28 | 18.30 | −6.20 | 32 | <.001 |
| Pain-related disability | |||||
| F2F | 14.06 | 12.36 | 4.36 | 83 | <.001 |
| Online | 14.06 | 12.27 | 2.31 | 32 | .027 |
| Pain-related anxiety | |||||
| F2F | 52.24 | 46.25 | 3.79 | 82 | <.001 |
| Online | 45.97 | 36.27 | 3.35 | 32 | .002 |
| Pain self-efficacy | |||||
| F2F | 25.75 | 33.63 | −7.52 | 66 | <.001 |
| Online | 24.94 | 32.27 | −3.68 | 32 | <.001 |
Table 7.
Post-hoc tests comparing formats on the pre- and post-scores.
| Pre-depression | Post-depression | |||
|---|---|---|---|---|
| F2F | Online | F2F | Online | |
| M | 31.51 | 28.82 | 23.51 | 20.88 |
| T | 1.20 | 1.15 | ||
| Df | 115 | 115 | ||
| P | 0.234 | 0.251 | ||
Table 8.
Mean pre-treatment outcomes for completers versus drop-outs.
| Measure | Completers mean pre-treatment score | Drop-outs mean pre-treatment score | Independent t-test |
|---|---|---|---|
| Age | 45.72 (20–77) | 48.46 (23–70) | F = 0.867, t = −1.394, df = 170, p = .353 ns |
| Self-compassion (SCS) | 11.63 | 10.85 | F = 0.480, t = 1.187, df = 171, p = .489 ns |
| Depression (CES-D) | 30.68 | 32.10 | F = 0.370, t = −0.777, df = 171, p = .544 ns |
| Pain anxiety (PASS) | 50.52 | 49.92 | F = 0.753, t=0.188, df = 171, p = .387 ns |
| Pain disability (RMDQ): | 14.14 | 15.15 | F = 0.238, t = −1.139, df = 171, p = .627 ns |
| Pain self-efficacy (PSEQ) | 25.78 | 24.46 | F = 0.358, t = 0.769, df = 171, p = .550 ns |
| Pain numeric rating scale | 4.97 | 5.88 | F = 0.000, t=−2.776, df = 171, p = .991 ns |
| Self-kindness (SK) | 4.45 | 3.95 | F = 7.533, t = 1.639, df = 171, p < .007 |
Table 9.
Comparison of virtual CFT-PM (20 hours) to virtual PMP (30 hours).
| Depression (CES-d) | Pain-related disability (RMDQ) | Pain-related anxiety (PASS) | Pain self-efficacy (PSEQ) | Pain (numeric rating scale) | |
|---|---|---|---|---|---|
| Mean pre-vPMP | 34.33 | 19.02 | 57.31 | 18.72 | 6.47 |
| Mean pre-vCFT-PM | 30.75 | 14.06 | 50.46 | 25.65 | 4.98 |
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: All authors participated in planning and progress meetings, co-wrote the interview schedule, information sheets and consent forms and were involved in drafting the manuscript and were involved in data analysis. AE and DY recruited and interviewed service users, EB led on writing of the published version of the manuscript, ZM additionally conceived and supervised the study.
Ethical approval: Completion of the National Health Service Health Research Authority decision-making questionnaire indicated that ethical approval was not required. The NHS Trust Research Office peer reviewed the proposal and confirmed that no further local approvals would be needed for this service evaluation.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Informed consent was received from all interviewees, who confirmed that they understood that the interview was entirely voluntary and their decision about participating would not affect their care in any way.
Guarantor: ZM
ORCID iD
Zoey Malpus https://orcid.org/0000-0001-6319-5931
References
- 1.Williams D, Booth G, Cohen H, et al. Rapid design and implementation of a virtual pain management programme due to COVID-19: a quality improvement initiative. Br J Pain 2022; 16(2): 191–202. Epub 2021 Sep 3. PMID: 35425594; PMCID: PMC8998524. DOI: 10.1177/20494637211039252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vlayen JWS, Linton SJ. Fear-avoidance model of chronic musculoskeletal pain: 12 years on. Pain 2012; 153(6): p1144–p1147. DOI: 10.1016/j.pain.2011.12.009. [DOI] [PubMed] [Google Scholar]
- 3.Armitage, Malpus Z. Compassion focused therapy for strivers in pain. Pain Rehabil J Pain Physiother Assoc 2019; 47: p6–p11. [Google Scholar]
- 4.Armitage L, Malpus Z. Compassion-focused pain management: preliminary findings across multiple sites, and future directions. Br J Pain 2017; 11(2): p5–p6. DOI: 10.1177/2049463717696602. [DOI] [Google Scholar]
- 5.Parry SL, Malpus Z. Reconnecting the mind and body: a pilot study of developing compassion for persistent pain. Patient Experience J 2017; 4(1): 145–153. DOI: 10.35680/2372-0247.1175. [DOI] [Google Scholar]
- 6.Gilbert P. The Compassionate Mind: How to Use Compassion to Develop Happiness, Self-Acceptance and Well-Being 2009. London, UK: Constable and Robinson Ltd. [Google Scholar]
- 7.Gilbert P. Compassion, Research and Applications 2017. Oxon UK: Routledge Ltd. [Google Scholar]
- 8.Gilbert P. Setting the scene: psychotherapy at a crossroads and a compassionate way forwards p3-23. In: Gilbert P, Simos G. (eds) Compassion Focused Therapy Clinical Practice and Applications. London and New York: Routledge, 2022. [Google Scholar]
- 9.British Pain Society . Guidelines for Pain Management Programmes for Adults an Evidence-Based Review Prepared on Behalf of the British Pain Society 2019. London, UK: Churchill House. [Google Scholar]
- 10.Petrocchi N, Di Bello M, Cheli S, et al. How physiological underpinnings of prosociality inform clinical practice. In: Gilbert P, Simos G. (eds) Compassion Focused Therapy Clinical Practice and Applications. New York, NY: Routledge London and, 2022, p345–p359. [Google Scholar]
- 11.Purdie F, Morley S. Compassion and chronic pain. Pain 2016; 157(12): p2625–p2627. DOI: 10.1097/j.pain.0000000000000638. [DOI] [PubMed] [Google Scholar]
- 12.Costa J, Pinto Gouveia J. Experiential avoidance and self-compassion in chronic pain. J Appl Soc Psychol 2013; 43(8): p1578–p1591. [Google Scholar]
- 13.Vowles KE, McCracken LM, McLeod C, et al. The chronic pain acceptance questionnaire: confirmatory factor analysis and identification of patient subgroups. Pain 2008; 140: 284–291. [DOI] [PubMed] [Google Scholar]
- 14.Carvalho SA, Gillanders D, Palmeira L, et al. Mindfulness, self-compassion and depressive symptoms in chronic pain: the role of acceptance. J Clin Psychol 2018; 74(2): p2094–p2106. DOI: 10.1002/jclp.22689. [DOI] [PubMed] [Google Scholar]
- 15.Austin J, Drossaert CC, Schroevers M, et al. Compassion-based interventions for people with long- term physical conditions: a mixed methods systematic review. Psychol Health 2020; 36(1): 16–42. DOI: 10.1080/08870446.2019.1699090. [DOI] [PubMed] [Google Scholar]
- 16.Gooding H, Stedman J, Crix D. All these things don't take the pain away but they do help you to accept it': making the case for compassion-focused therapy in the management of persistent pain. Br J Pain 2020; 14(1): p31–p41. DOI: 10.1177/2049463719857099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lanzaro C, Carvaalho SA, Lapa T, et al. A systematic review of self-compassion in chronic pain; from correlation to efficacy. Spanish J Psychol 2021: 1–19. DOI: 10.11017/SJP.2021.22. [DOI] [PubMed] [Google Scholar]
- 18.Booth G, Williams D, Patel H, et al. What is the content of virtually delivered pain management programmes for people with persistent musculoskeletal pain? A systematic review. Br J Pain 2022; 16(1): 84–95. Epub 2021 Jun 13. PMID: 35111317; PMCID: PMC8801687. DOI: 10.1177/20494637211023074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Raes F, Pommier E, eff KD, et al. Construction and factorial validation of a short form of the self-compassion scale. Clin Psychol and Psychotherapy 2011; 18: 250–255. DOI: 10.1002/cpp/702. [DOI] [PubMed] [Google Scholar]
- 20.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas 1977; 1: 385–401. DOI: 10.1177/014662167700100306. [DOI] [Google Scholar]
- 21.McCracken LM, Dhingra L. A short version of the pain anxiety symptoms scale (PASS-20): preliminary development and validity. Pain Res Manage 2002; 7(1): 45–50. [DOI] [PubMed] [Google Scholar]
- 22.Roland MO, Morris RW. A study of the natural history of back pain. Part 1: development of a reliable and sensitive measure of disability in low back pain. Spine 1983; 8: 141–144. DOI: 10.1097/00007632-198303000-00004. [DOI] [PubMed] [Google Scholar]
- 23.Nicholas MK. The pain self-efficacy questionnaire: taking pain in to account. Eur J Pain 2007; 11(2): 153–163. DOI: 10.1016/j.e.pain2005.12.008. [DOI] [PubMed] [Google Scholar]
- 24.British Pain Society and Faculty of Pain Medicine of the Royal College of Anaesthetists . Outcome Measures 2019. London, UK: Churchill House. [Google Scholar]
- 25.Jensen MP, Karoly P. “Self-report scales and procedures for assessing pain in adults”. In: Turk DC, Melzack R. (eds) Handbook of pain assessment. 3rd edition. New York, NY: Guilford Press, 2011, 19–44. [Google Scholar]
- 26.Rainville J, Smeets RJ, Bendix T, et al. Fear-avoidance beliefs and pain avoidance in low back pain--translating research into clinical practice. Spine J 2011; 11(9): 895–903. Epub 2011 Sep 9. PMID: 21907633. DOI: 10.1016/j.spinee.2011.08.006. [DOI] [PubMed] [Google Scholar]
- 27.Andersson G, Titov N, Dear BF, et al. Internet-delivered psychological treatments: from innovation to implementation. World Psychiatry 2019; 18(1): 20–28. PMID: 30600624; PMCID: PMC6313242. DOI: 10.1002/wps.20610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fairburn CG, Patel V. The impact of digital technology on psychological treatments and their dissemination. Behav Res Ther 2017; 88: 19–25. PMID: 28110672; PMCID: PMC5214969. DOI: 10.1016/j.brat.2016.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vowles K, E, Sowden G, Ashworth J. A comprehensive examination of the model underlying acceptance and commitment therapy for chronic pain. Behav Ther 2014; 45(3): p390–p401. DOI: 10.10.1016/j.beth.2013.12.2009. [DOI] [PubMed] [Google Scholar]
- 30.Wilson D, Mackintosh S, Nicholas MK, et al. Harnessing group composition-related effects in pain management programs: a review and recommendations. Pain Manag 2016; 6(2): 161–173. Epub 2016 Mar 23. PMID: 27008418. DOI: 10.2217/pmt.15.66. [DOI] [PubMed] [Google Scholar]
- 31.Faculty of Pain Medicine of the Royal College of Anaesthetists . Core Standards for Pain Services UK. Second Edition. London, UK: Churchill House, 2021. [Google Scholar]
- 32.Kilic A, Hudson J, McCracken L, et al. A systematic review of the effectiveness of self-compassion- related interventions for individuals with chronic physical health conditions. Behav Ther 2021; 52: p607–p625. DOI: 10.1016/j.beth.2020.08.001. [DOI] [PubMed] [Google Scholar]
- 33.McCraken LM, Vowles KE, Eccleston C. Acceptance of chronic pain: component analysis and a revised assessment method. Pain 2004; 107: 159–166. [DOI] [PubMed] [Google Scholar]
- 34.McCracken LM, Vowles KE, Eccleston C. Acceptance-based treatment for persons with complex, long standing chronic pain: a preliminary analysis of treatment outcome in comparison to a waiting phase. Behav Res Ther 2005; 43: 1335–1346. [DOI] [PubMed] [Google Scholar]
- 35.NICE guideline Chronic pain (primary and secondary) in over 16s: assessment of all chronic pain and management of chronic primary pain (NG193) 2021. [PubMed] [Google Scholar]
- 36.Penlington C. Exploring a compassion-focused intervention for persistent pain in a group setting. Br J Pain 2019; 13(1): p59–p66. DOI: 10.1177/2049463718772148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Raja SN, Carr DB, Cohen M, et al. The revised international association for the study of pain definition of pain: concepts, challenges, and compromises. Pain 2020; 161(9): 1976–1982. DOI: 10.1097/j.pain.0000000000001939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rockliff H, Karl A, Mcewan K, et al. Effects of intranasal oxytocin on ‘compassion focused imagery. Emotion 2011; 11(6): p1388–p1396. DOI: 10.1037/a0023861. [DOI] [PubMed] [Google Scholar]
- 39.Williams AC de C, Fisher E, Hearn L, et al. Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database Syst Rev 2020; 8. DOI: 10.1002/14651858.CD007407.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]