Abstract
Objective
School nurses are engaging worldwide to promote and protect children’s health. Many researchers who examined the effectiveness of the school nurse criticized the inadequate methodology employed in many of the studies. We therefore carried out an evaluation on the effectiveness of school nurses based on a rigorous methodological approach.
Methods
In this overview of reviews we performed an electronic databank search and global research results on the effectiveness of school nurses were sought. We identified 1,494 records through database search. Abstracts and full texts were screened and summarized using the dual control principle. We summarized the aspects of quality criteria as well as the significance of the effectiveness of the school nurse. In the first step, k = 16 systematic reviews were summarized and evaluated following the AMSTAR-2 guidelines. In a second step, j = 357 primary studies included in these k = 16 reviews were summarized and assessed following the GRADE guidelines.
Results
Research results on the effectiveness of school nurses show that school nurses play a key role in improving the health of children with asthma (j = 6) and diabetes (j = 2), results on combating obesity are less certain (j = 6). The quality of identified reviews is mostly very low with only six studies of medium quality, of which one identified as a meta-analysis. A total of j = 289 primary studies were identified. Approximately 25% (j = 74) of identified primary studies were either randomized controlled trials (RCT) or observational studies, of which roughly 20% (j = 16) had a low risk of bias. Studies with physiological variables such as blood glucose or asthma labeling led to higher quality results.
Conclusion
This paper represents an initial contribution and recommends further evaluation of the effectiveness of school nurses, particularly in the areas of mental health or children from low socioeconomic backgrounds. The general lack of quality standards in school nursing research should be integrated into the scientific discourse of school nursing researchers to provide robust evidence for policy planners and researchers.
1 Introduction
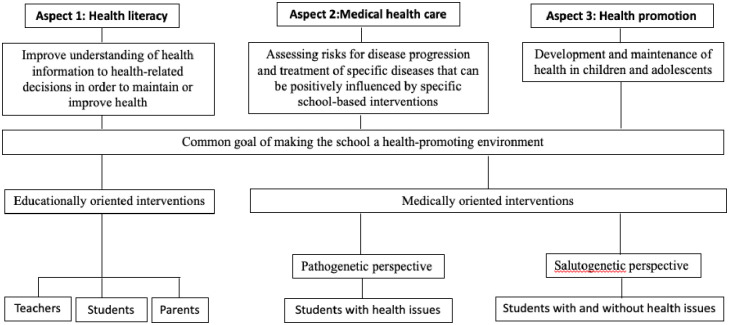
School nurses are medically trained professionals who work in both the school and healthcare sectors, with the aim of making the school a health-promoting environment for teachers and pupils [1–3]. School nurses play a pivotal role in improving the health and well-being of children and adolescents by providing health promotion, health counseling, referral to other sources of help, active treatment, education, family support, care coordination, and multiagency work [1,4–6]. School nurses have a wide range of roles and responsibilities that cover three core aspects of school health 1) health literacy, 2) medical care, and 3) health promotion [7–9]. These three areas of school nursing complement each other in terms of the common goal of making the school a health-promoting environment but differ in their approaches and strategies to achieve this goal. Health literacy has the aim of enabling students and teachers to find, understand, evaluate, and apply health information to health-related decisions in order to maintain or improve health and quality of life [10,11]. Health literacy holds the educational perspective with the goal of knowledge gain. In contrast, health promotion and medical health care share the aspect of medically oriented interventions but differ from one another in their perspective on health aspects. Medical health care at schools takes the pathogenetic perspective. Here, the focus is on assessing risks for disease progression and treatment of specific diseases that can be positively influenced by specific school-based interventions. Health promotion in schools, on the other hand, argues salutogenetically. Here, the focus is on the development and maintenance of health in children and adolescents. This can be achieved through resource-strengthening measures at schools, promoting healthy behaviors such as sports and nutrition and through preventive care services, e.g. care coordination by school nurses [11,12]. All three aspects of school health cannot be clearly distinguished from each other.
Most international research on school nurse interventions addressing the three aspects of school health originated in Anglo-Saxon countries [13–15] where the school nurse was first introduced and where most research has been conducted. Many of these studies evaluate school-nurse led interventions and refer to the number of days absent due to medical conditions [13,16], health risk factors such as obesity [17,18] and cigarette consumption [19,20], children with asthma symptoms [21,22], mental health conditions [23,24], the management of chronic diseases [3,25] or preventing various forms of child abuse [26–28]. Apart from more positive health outcomes for children, the support provided by the school nurse may lessen the burden on teachers confronted with such problems in the classroom [29–31].
The importance of the school nurse came particularly apparent when the COVID-19 pandemic hit and new health-related challenges for both pupils and teachers arose. Recent studies focused on an examination of the role of school nurses and their valuable input particularly on the question of the wisdom of closing schools or keeping them open [32]. Additionally studies also addressed how their work could help to minimize community-wide risk [33] through improved hygiene concepts [34] and effective immunization programs [35].
Besides the aforementioned health-related benefits, studies calculated financial savings in health care for society as a whole [36,37] by involving school nurses at primary and secondary schools. Wang and Vernon-Smiley [38] estimated that in one year alone, for every dollar invested in their program in the US, $2.20 is saved. Binder [36] investigated whether poor parental health awareness, poor integration in society as well as rising numbers of children with chronic health issues could ultimately cause higher follow-up costs than investing in prevention.
While there is a large body of research available about school nursing, it becomes apparent that despite the abundance of literature on the subject, scientifically sound conclusions regarding the effectiveness of school nurses are anything but clear-cut. Researchers [20,21] have repeatedly criticized the lack of methodological quality and the resulting lack of robust, meaningful research findings regarding the effectiveness of school nurses. The main points of criticism are the lack of evidence-based, quantitative data with randomized controlled trial designs and the predominantly descriptive study designs [39].
We see an urgent need to address this increasingly vocal criticism of school nurse research and to organize the miscellany of research findings. For this reason, we conducted an overview of reviews, the first of its kind in school nurse research. This paper is a response to the prevailing criticism of poor study quality, which is why reviews and primary studies are subject to strict methodological guidelines. By introducing methodological standards, our aim is to ensure clinical validity regarding school nurse effectiveness.
Our aim is to critically assess the current state of the relevant literature by applying rigorous and valid quality criteria. Well-established quality assessment tools such as AMSTAR-2 and GRADE guidelines were chosen and adapted to our purposes, as these tools are widely recognized among researchers and overcome the criticisms aimed at school nursing research. This paper will review studies which are in line with well-established methodological guidelines to arrive at sound conclusions on interventions and on meaningful results on health outcomes.
2 Materials and methods
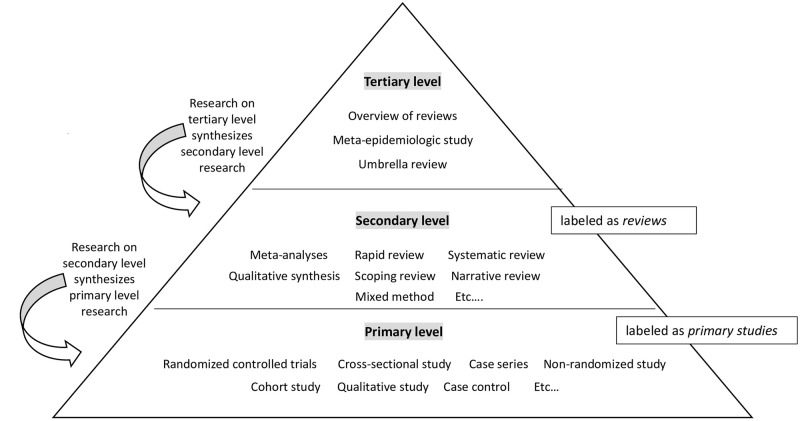
Studies are divided into three categories: primary, secondary and tertiary level. Primary level studies are e.g. randomized controlled trial designs or observational studies. For the sake of simplicity, studies on primary level are called primary studies in this paper. Secondary level studies are e.g. meta-analyses or systematic reviews, and are called reviews. Tertiary level studies are e.g. overview of reviews or umbrella reviews. The present paper is an overview of reviews. Overview of reviews encompass reviews, which in turn encompass primary studie (Fig 1).
Fig 1. Hierarchy of research levels.
Notes. On tertiary level (e.g., overview of reviews) we synthesize studies on secondary level. On secondary level (e.g., meta-analysis) synthesize studies on primary level.
The methodological approach of conducting an overview of reviews is based on the guidelines of Biondi-Zoccai [40], who describe the research process and tools to summarize evidence relevant for policymakers in evidence-based medicine. Due to the lack of guidelines for overview of reviews in the educational or psychological field, this paper applies (to our knowledge for the first time in school nurse research) clinically relevant standards, which is intended to create solid and meaningful results and is a prerequisite for optimal decision-making. The methodological research standards were based on Zawacki-Richter, Kerres [41], who describe the methodological procedure of systematic reviews in the educational research field. The overview of reviews differs from reviews in only a few respects (e.g. databases are searched exclusively for reviews) [40]. For this reason, this study also followed the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) [42], including the recommended Cochrane Checklist (Attachment 1). The quality of included reviews was assessed according to the validated scale Assessment of Multiple Systematic Reviews 2 (AMSTAR-2) [43]. The strict quality rating was adapted to allow the reader a comparison of our reviews. Biondi-Zoccai [40] recommended an analysis of primary studies that were summarized in each review, in order to be able to make authoritative statements regarding its informative value. To assess the body of evidence of primary studies the Grading of Recommendations Assessment, Development and Evaluation (GRADE) [44] was used. GRADE provides instructions for assessing the strength of evidence for each outcome in a review [44]. In our work, the GRADE assessment remains at descriptive level and risk of bias, imprecision, indirectness of evidence, publication bias and impact are described. Magnitude of effects, dose-response relations and the impact of residual confounding were removed, as these criteria are not relevant for studies from the educational and psychological field.
Our approach to this work is explained in a protocol that was created a priori and continuously updated during the research process and uploaded to the PROSPERO website on 08.02.2021 [45]. The protocol can be viewed on PROSPERO with the registration number CRD42021235152. All relevant data are within the manuscript and its Supporting Information files.
2.1 Inclusion and exclusion criteria
We outlined our inclusion and exclusion criteria in terms of the PICOS format. We included studies examining children aged 5 to 21 (IC1), with either the school nurse himself/herself being the intervention or a school nurse-led health program as the intervention (IC2). The criterion of the comparison group was not applicable for this work. Studies examining the effect of various health outcomes, school attendance, academic achievements, risky and difficult behavior in the school setting were included (IC3). Only research in English and German and reviews were searched (IC4) with no date restrictions. We excluded primary studies and studies with interventions that were not conducted by at least one school nurse or in the school setting. Studies without specific health outcomes for school children, as well as recommendations for school nurses, were also excluded (Table 1).
Table 1. Inclusion and exclusion criteria based on PICOS scheme.
| INCLUSION CRITERIA (IC) | ||
| IC1 | P opulation | |
| IC 1.1 | School children aged between 5 and 21
|
|
| IC 1.2 | Teachers in primary schools, middle schools and high schools (and other types of schools based on countries)
|
|
| IC 1.3 | School nurses who work in primary schools, middle schools or high schools
|
|
| IC2 | I ntervention | |
| IC 2.1 | Effectiveness of the school nurse
|
|
| IC 2.2 | Effectiveness of the interventions performed by the school nurses
|
|
| IC3 | O utcome | |
| IC 3.1 | Physical and psychological health outcomes for children and teachers | |
| IC 3.2 | Outcomes regarding health literacy of children and teachers | |
| IC4 | S tudy Design | |
| IC 4 | Study Design: Study designs on secondary level, e.g. meta-analysis, mixed method systematic review, narrative review, qualitative synthesis, scoping review, systematic review, rapid review | |
| IC5 | Publication | |
| IC 5.1 | peer-reviewed reviews (journal article) | |
| IC 5.2 | published in English or German language | |
| EXCLUSION CRITERIA (EC) | ||
| EC1 | Participants | |
| EC 1.1 | Parents | |
| EC 1.2 | Children younger than 5 years old or older than 21 years old | |
| EC 1.3 | All professions in the school context except for teachers and school nurses (e.g. social workers, school psychologists, doctors) | |
| EC2 | Interventions | |
| EC 2.1 | All regarding the role of school nurses Financial feasibility |
|
| EC 2.2 | All interventions that do not examine the effectiveness of the intervention performed by the school nurse | |
| EC 2.3 | „Best Practice" for school nurses | |
| EC 2.4 | Interventions that do not examine the effectiveness of the school nurse | |
| EC 2.5 | Framework for school nurses | |
| EC 2.6 | Challenges for school nurses | |
| EC 2.7 | Curriculum | |
| EC 3 | Outcome | |
| EC 3.1 | Outcomes that do not regard the physical or psychological health of children and teachers | |
| EC 3.2 | Outcomes that do not regard the impact on health literacy | |
| EC 3.3 | Pros and cons for school nurses | |
| EC 3.4 | Implications for school nurses | |
| EC 3.5 | How school nurses benefit | |
| EC 3.6 | How parents benefit | |
| EC 3.7 | How school psychologists benefit | |
| EC 3.8 | No health outcome | |
| EC 4 | Study design | |
| EC 4 | Study designs on primary level, e.g. case study, case series, case-control-study, cohort study, cross-sectional study, qualitative study, pre-clinical study, randomized controlled trial | |
2.2 Information sources
We conducted a search of peer-reviewed literature in Medline, Cochrane Library, Cinahl, Web of Science, Scopus, PubMed, Subject portal Pedagogy [Fachportal Pädagogik], Educational Resource Information Center (ERIC) and German National Bank Catalogue [Katalog der deutschen Nationalbank] from November 2020 to January 2021. Additionally, we searched Google Scholar, reference lists, and also contacted leading researchers in the field of school nursing for additional overviews, finishing the search process in February 2021.
2.3 Search strategy
Before starting the search process, we conducted a pilot study of the scope of school nurse-related literature. For this purpose, we used the Medline database as a trial database, analyzing the first 150 results using the search term "school nurs*". The results of this pilot study were presented to an expert panel of eight members, optimizing our methodology and focus (e.g. deciding to only include reviews). In addition, the PROSPERO database was searched to exclude possible content overlap with studies not yet published [45]. Following the suggestion of Zawacki-Richter, Kerres (41), a record log was initiated to develop a search string (Table 2). Our final search string (“School-nurs* (only in title)” AND (“Review* OR meta-analysis”) NOT (“Barrier* OR framework OR role* (only in title))) was searched in 9 databases and had to be adapted for the database ERIC (“school nurse” AND “review” OR “reviews” NOT “barrier” NOT “barriers” NOT “framework” NOT “frameworks” NOT “role” NOT “roles”) and for German databases (“Schulgesundheitsfachkraft” OR “Schulgesundheitspflege”, which translates into school nurse).
Table 2. Terms used in systematic database literature search.
| Category | PubMed, Medline, Web of Science, Cochrane, CINAHL, Scopus | ERIC* |
|---|---|---|
| A: School Nurse | school-nurs* (only in title) | “school nurse” |
| B: Method | review*OR meta-analysis | Review OR reviews |
| C: Excluded terms | Barrier* OR role*OR framework | NOT barrier NOT barriers NOT framework NOT frameworks NOT role NOT roles |
Notes. Categories were combined into a search string as follows: A and B NOT C.
*The database ERIC did not recognize the word “meta-analysis”. Therefor this search term was removed. ERIC does not have the option to use “*” to show all endings to a word. The hyphen between “school” and “nurse” showed no results. To avoid search results with only “school” or only “nurse” ERIC gives the option of enclosing a term in quotation marks. For this reason, our search string had to be adapted.
Additionally, reference lists were searched (FM), Google Scholar was searched using the terms "school nurse and review" (SH) and the National Association of School Nursing and leading researchers (n = 9) in school nursing research were contacted (SH and SS).
2.4 Screening and study selection
Citations identified from the systematic search were exported to EndNote (EndNote 20.1, Bld 12060), a reference management tool. Duplications were removed and two independent reviewers (SH and FM) screened all titles and abstracts using the inclusion and exclusion criteria, adding an explanation for the exclusion of the excluded references. Articles that were labelled as “excluded” by both researchers were removed, while articles that received conflicting votes (ineligible vs. potentially or probably eligible) were discussed and a consensus was reached. Interrater reliability was calculated using IBM SPSS 23 (IBM Corp., Armonk, NY). The agreement rate was measured by determining the percentage of the sum of all matching “included” and “excluded” references, where the total number of references assessed equalled 100%. The same two reviewers (SH and FM) screened the full texts of all the probably eligible articles using the same inclusion and exclusion criteria. If consensus was not possible during the screening of title and abstract or full text screening, a third or fourth reviewer (SP or DM), who had the casting vote, would have been asked to independently screen the article. However, this was never necessary as consensus was always reached.
2.5 Data extraction process of reviews
The selection of characteristics to be extracted from reviews was discussed with the research team, consisting of five members, and unanimous agreement was reached. Data items included author, year, country, time-period covered, type of review, number of primary studies included, subject-matter and summary of findings. One reviewer (SH) and an assistant researcher (SS) independently extracted data from each study and were generally in agreement.
2.6 Data extraction process of primary studies
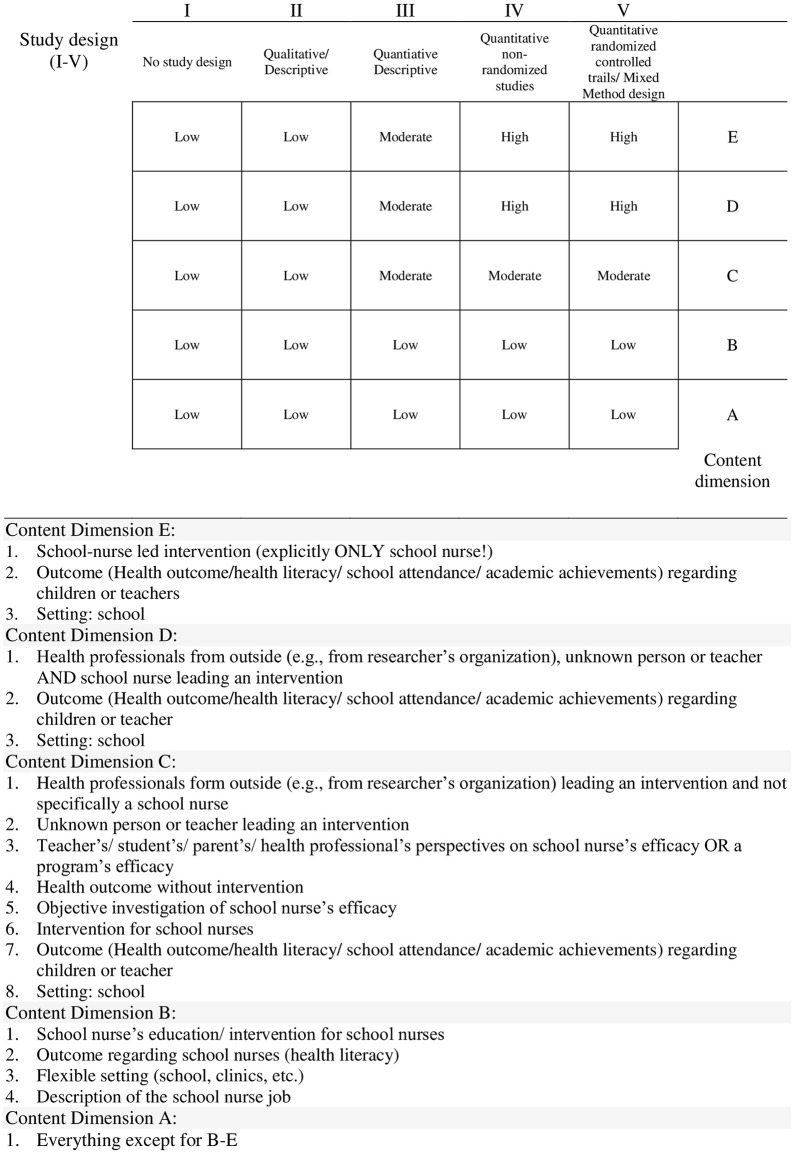
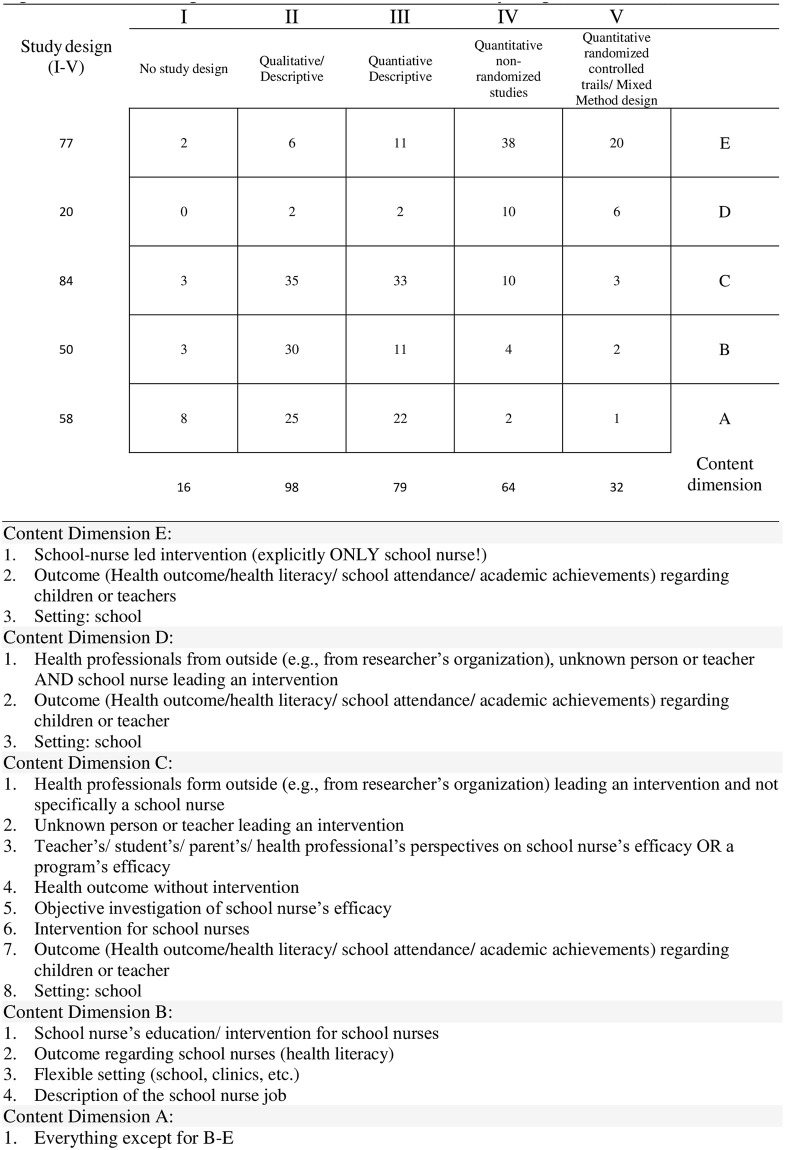
In order to extract data from primary studies, they first had to be identified in the respective reviews. Once identified, researchers exported references into EndNote, removed duplications, and searched full texts. The selection of characteristics to be extracted was discussed with the same research team, and unanimous agreement was reached. Data items included author, year, country, studied population, research design according to the Mixed Method Appraisal Tool (MMAT) [46], main topic, study subject-matter, intervention, data collection, outcome, and information value. The same reviewer (SH) and assistant researcher (SS) independently extracted data from each primary study. Due to the huge number of primary studies, references had to be divided up, so that no data extraction agreement could be measured. To counteract bias, the data extraction of the respective other was checked selectively. The description of primary studies is the basis for further data analysis and is discussed in the results. Due to the heterogeneity and the large and hence unmanageable amount of data, an additional criterion (information value) was added, which requires further explanation: This criterion represents a rating based on two dimensions: a) the study design used and b) the content covered. A matrix was developed to categorize each study. The first dimension represents the quality of the study design (I-V), based on the MMAT criteria. The second dimension classifies the relevance of the content (A-E), depending on the extent to which the primary study examines the effectiveness of school nurses (Fig 2).
Fig 2. Matrix for categorization of content dimension and study design.
2.7 Assessment of study quality of reviews based on AMSTAR-2
The AMSTAR-2 checklist [43] was used to assess the quality of reviews. One reviewer (SH) assessed all reviews, and the assistant researcher (SS) duplicated the appraisal with 80% agreement. AMSTAR-2 is a critical appraisal tool for reviews, such as meta-analysis, that include primary studies covering healthcare interventions. Because school nurse research is mainly comprised of descriptive literature, reviews included in this study cannot meet the strict guidelines according to AMSTAR-2. Despite these strict guidelines, we decided to differentiate between the quality of reviews by slightly adjusting the AMSTAR-2 criteria.
The following clusters were assessed): A) Research question & selection process, B) assessment of included primary studies, C) interpretation of results, and D) report of potential source of conflict.
Each cluster (A-D) consists of criteria which in turn contains sub-categories. Depending on the percentage of sub-criteria met in a criterion, numbers 0–4 were assigned for each quartile, with “0” no sub-criterion and “4” over 75% of sub-criteria met. The numbers in each category were then added together. The maximum score, 48 points, represents the best possible quality of reviews. The classification into low, medium and high quality is determined by dividing the maximum score by 3, so that studies with more than 32 points are of high quality, studies with 16 to 31 points are of medium quality and studies with less than 16 points are of low quality.
As a result, reviews were graded according to the number of sub-criteria actually met, and not downgraded if one sub-criterion was missing, and reviews that would have been downgraded under normal circumstances because a requirement was not met would in our study only be downgraded if less than 75% of the required sub-categories had not been met (Table 3).
Table 3. Adapted rating of the quality of reviews, based on AMSTAR-2 [43].
| Categorisation of the subcategories that apply to the corresponding rating (0–4) | Categorisation of the total score to the quality rating (low, medium, high) | ||
|---|---|---|---|
| Percentage of sub-criteria met (%) | Category | Overall score | Category |
| 0% | 0 | <16 | Low |
| 1–24% | 1 | 16–32 | Moderate |
| 25–49% | 2 | >32 | High |
| 50–74% | 3 | ||
| 75–100% | 4 | ||
2.8 Assessment of body of evidence of primary studies based on GRADE
The body of evidence was only conducted for primary studies with randomized controlled trials (RCTs) or observational studies, i.e. non-randomized studies (Obs), based on the GRADE assessment tool [44]. Because information relevant to the assessment, such as the confidence interval, was often not included in primary studies, the body of evidence remained on a descriptive level. Relevant characteristics to evaluate the body of evidence such as the indirectness of evidence (population studied, type of intervention, measures and desired measures), publication bias, risk of bias, imprecision (number of participants, confidence interval) and impact are described for each health outcome.
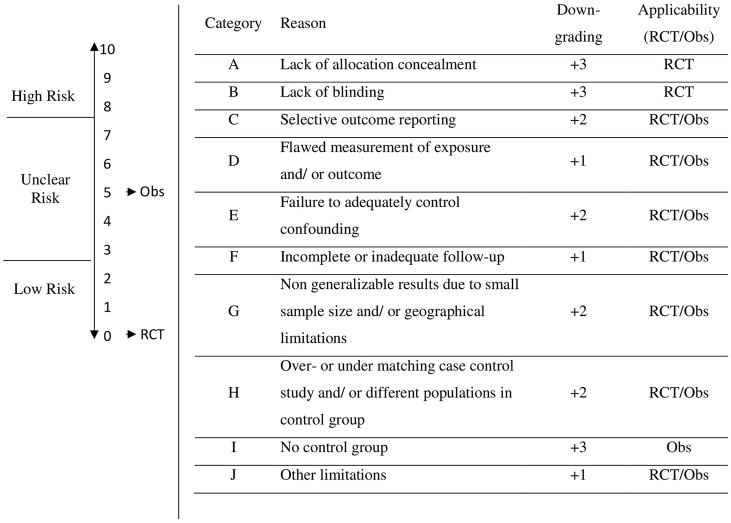
2.9 Assessment of risk of bias
Our assessment of the level of effectiveness and the resulting recommendations are less credible if the studies have significant limitations, such as the risk of bias (RoB) [44]. For this reason, we assessed the RoB for RCTs and Obs. All other study designs may not be applicable for RoB assessment. The GRADE handbook [47] for grading the quality of evidence was used as a guideline and limitations that influence the risk of bias were identified. The magnitude of an effect decreases when studies suffer from major limitations that are likely to lead to a biased assessment of the intervention. Lack of allocation concealment, lack of blinding, incomplete accounting of patients and outcome events, selective outcome reporting, failure to develop and apply appropriate eligibility criteria (inclusion of control population), flawed measurement of both exposure and outcome, failure to adequately control confounding and incomplete or inadequately short follow-up were considered when assessing the risk of bias for each RCT or Obs study.
Authors of this study developed a scale to determine the degree of risk of bias: low (0 to 2 points), unclear (3 to 7 points) and high risk (8 to 10 points). Starting point for RCTs is “Low Risk” with 0 points. Starting point for Obs. is at “Unclear Risk” with 5 points. For each limitation, the risk of bias increases by the corresponding grade (+1, +2, +3) on the scale (0 to 10), which results in the categorization of the RoB (Low, Unclear, High) (Fig 3).
Fig 3. Risk of bias assessment based on GRADE assessment.
Note. Starting point for RCTs is “Low Risk” with 0 points. Starting point for Obs is at “Unclear Risk” with 5 points. For each limitation, the corresponding downgrade (+1, +2, +3) is made on the scale (0 to 10), which results in the categorization of the risk of bias (Low, Unclear, High). Downgrading scores and categorization to low, unclear, and high risk were defined by authors.
2.10 Narrative synthesis of results
During the evaluation of the pilot study, we found that primary studies and reviews, on the school nursing subject-matter were qualitatively deficient, in the sense that hardly any meta-analyses were conducted, and most studies used descriptive designs rather than RCTs or Obs. In order to find out to what extent conclusive statements can be made regarding the effectiveness of school nurses, a comprehensive and transparent analysis of the studies was conducted, using well-validated and acknowledged clinical research methods, such as the AMSTAR-2 [43] and GRADE assessment tool [44].
The quality assessment of reviews was based on AMSTAR-2 criteria, whereby the scaling and subsequent grading of the quality of reviews was adapted by the research team (see 2.6). The body of evidence of primary studies was based on GRADE recommendations, and the evaluation did not go beyond a descriptive level (see 2.8). Characteristics to evaluate the body of evidence are study design, the measurement instrument and the characteristic being measured, publication bias, risk of bias, number of subjects, confidence interval, effect size, and comparability of population groups and interventions. These characteristics were classified for each health outcome.
3 Results
3.1 Study selection
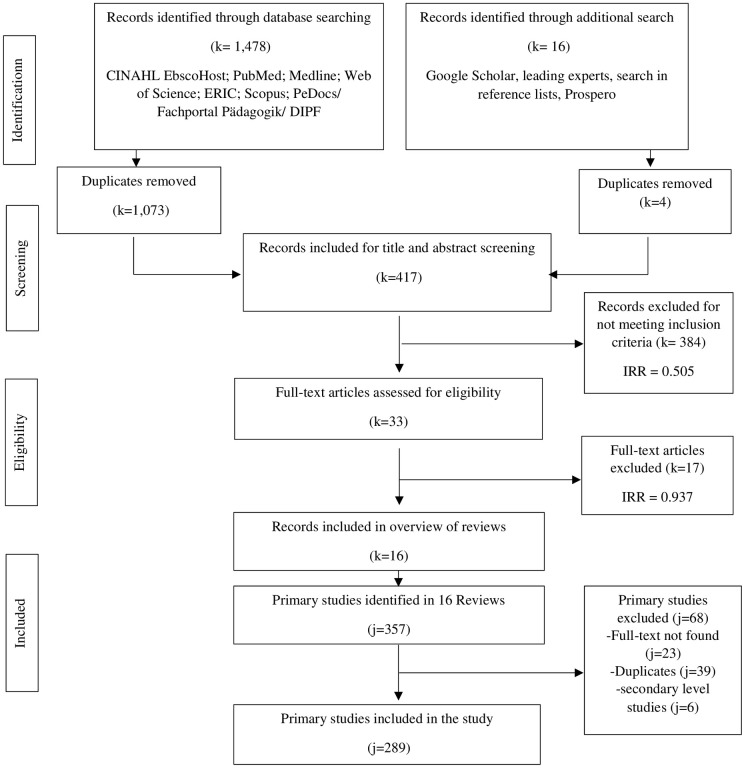
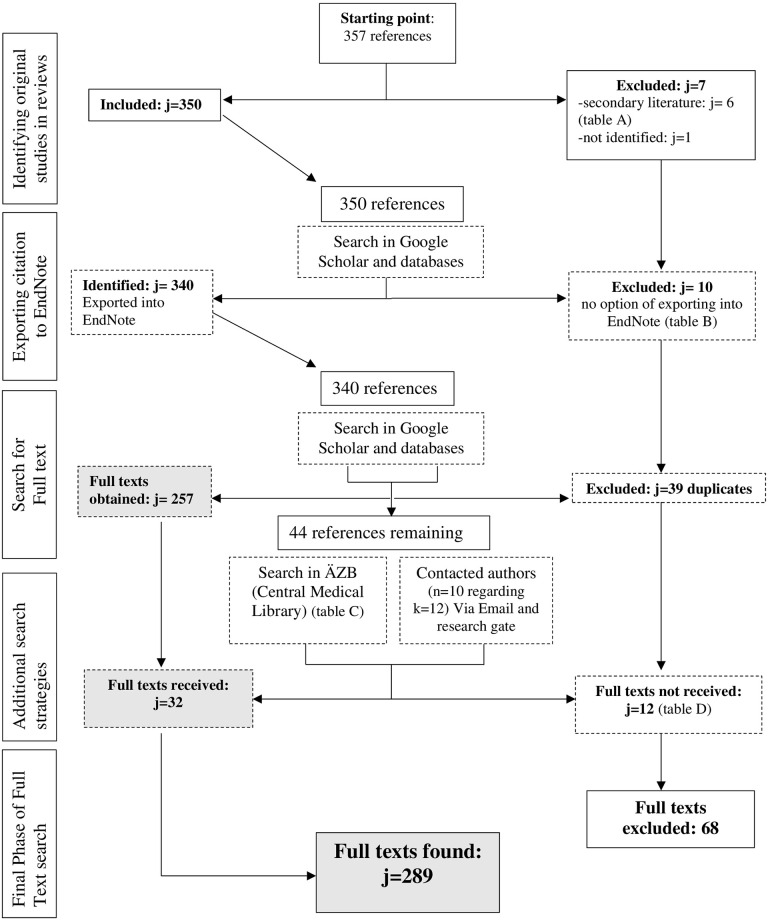
The study selection for this overview of reviews consisted of two parts: First, reviews were searched (Fig 4), later full texts of primary studies included in each review, were searched (Fig 5).
Fig 4. PRISMA flow chart [42] for reviews.
Notes: k = reviews; j = primary studies. A search f 9 databases identified 1,478 articles. The additional search yielded 16 more articles. After subtracting duplicates (k = l,077), abstract and title of 417 articles were screened. 33 articles met the inclusion criteria (k = 385 excluded). After full texts of the 33 articles were screened, 16 articles met the inclusion criteria (k = 17 excluded). Primary studies identified in 16 reviews were identified (j = 357). After subtracting duplicates (j = 39) and excluding reviews (j = 6), and a study that could not be found (j = l), 311 primary studies were identified, and full texts were searched for. Further 23 primary studies had to be excluded as full texts could not be found, which totaled in 289 included primary studies in this Overview of Reviews.
Fig 5. Flow chart of search process for full texts of primary studies.
3.1.1 Selection of reviews
In the first part of the study selection, 9 databases were searched identifying 1,478 studies, and an additional search yielded further 16 references. After removing duplications (1,077), two independent researchers screened titles and abstracts of the remaining 417 studies (interrater reliability = 0.505; agreement rate: 92%). Records that did not meet the inclusion criteria were excluded (384). The remaining 33 full texts were screened to assess eligibility (interrater reliability = 0.760; agreement rate: 88%). At the end of the first part of the study selection process, 16 records were included in the overview of reviews. The 17 excluded full texts can also be found in Table 4.
Table 4. List of excluded reviews after full text screening (k = 17).
| Reference | Reason for exclusion | PICOS criteria | |
|---|---|---|---|
| 1 | Aguado, V. C. (2017). La enfermera escolar: comunicación eficaz para la prevención y detención del acoso escolar = The school nurse: effective communication for prevention and arrest of bullying. Revista Española de Comunicación en Salud, 8(2), 247–253. | Interventions that do not examine the effectiveness of the school nurse | EC7 |
| 2 | Aronowitz, S. V., Kim, B., & Aronowitz, T. (2021). A mixed-studies review of the school-to-prison pipeline and a call to action for school nurses. The Journal of School Nursing, 37(1), 51–60. | Outcomes that do not relate to the physiological and psychological health of students and teachers | EC11 |
| 3 | Bradley, B. J. (1998). Establishing a research agenda for school nursing. Journal of School Health, 68(2), 53–61. | Outcomes that do not relate to the physiological and psychological health of students and teachers | EC11 |
| 4 | DeBell, D. (2006). School nurse practice: a decade of change. Community Practitioner, 79(10), 324. | Interventions that do not examine the effectiveness of the school nurse | EC7 |
| 5 | DeSocio, J., & Hootman, J. (2004). Children’s mental health and school success. The Journal of School Nursing, 20(4), 189–196. | No examination of school nurse-led interventions | EC5 |
| 6 | Dosa, N., & Ilardi, D. (2003). An opportunity for school nurses and pediatricians to collaborate. School nurse news, 20(5), 16–22. | Full text not found | other |
| 7 | Forward, C. (2012). Measuring the effectiveness of school nursing interventions: A review of outcome tools. British Journal of School Nursing, 7(10), 490–500. | Health outcomes for students or teachers wasn’t subject matter | EC11 |
| 8 | Johnson, T., Weed, L. D., & Touger-Decker, R. (2012). School-based interventions for overweight and obesity in minority school children. The Journal of School Nursing, 28(2), 116–123. | No examination of school nurse-led interventions | EC5 |
| 9 | Markkula, V., & Muhli, U. H. (2013). Diskursen om den svenska skolsköterskans hälsostödjande arbete i kvalitativ forskning: En kvalitativ metasyntes. Vård i norden, 33(2), 22–27. | Interventions that do not examine the effectiveness of the school nurse | EC7 |
| 10 | McCabe, E. M., McDonald, C., Connolly, C., & Lipman, T. H. (2019). A review of school nurses’ self-efficacy in asthma care. The Journal of School Nursing, 35(1), 15–26. | No health outcome for students or teachers of interest | EC11 |
| 11 | Quinn, B. L., Lee, S. E., Bhagat, J., Holman, D. W., Keeler, E. A., & Rogal, M. (2020). A retrospective review of school nurse approaches to assessing pain. Pain Management Nursing, 21(3), 233–237. | Not secondary level research | EC19 |
| 12 | Ravenna, J., & Cleaver, K. (2016). School nurses’ experiences of managing young people with mental health problems: A scoping review. The Journal of School Nursing, 32(1), 58–70. | No examination of school nurse-led interventions | EC5 |
| 13 | Shannon, R. A., Bergren, M. D., & Matthews, A. (2010). Frequent visitors: Somatization in school-age children and implications for school nurses. The Journal of School Nursing, 26(3), 169–182. | No examination of school nurse-led interventions | EC5 |
| 14 | Strunk, J. A. (2008). The effect of school-based health clinics on teenage pregnancy and parenting outcomes: An integrated literature review. The Journal of School Nursing, 24(1), 13–20. | No examination of school nurse-led interventions | EC5 |
| 15 | Taylor, C., & Bailey, V. (2017). Nurse prescribing: An essential requirement or an expensive luxury for school nurses?. British Journal of School Nursing, 12(7), 346–352. | Not secondary level research | EC19 |
| 16 | Vessey, J. A., & Founding Oversight Board Members of MASNRN. (2007). Development of the Massachusetts School Nurse Research Network (MASNRN): A practice-based research network to improve the quality of school nursing practice. The Journal of School Nursing, 23(2), 65–72. | Interventions that do not examine the effectiveness of the school nurse | EC7 |
| 17 | Weismuller, P. C., Grasska, M. A., Alexander, M., White, C. G., & Kramer, P. (2007). Elementary school nurse interventions: Attendance and health outcomes. The Journal of School Nursing, 23(2), 111–118. | Not secondary level research | EC19 |
3.1.2 Selection of primary studies
In the second part of the study selection process, 357 primary studies included in each review were identified. Some primary studies were used in more than one overview (S1 Table). Among 357 primary studies, there were 6 reviews (Table 5a), 1 missing literature and 10 not exportable literature (Table 5b) that had to be excluded, leaving 340 primary studies which were exported into EndNote (EndNote 20.1, Bld 12060; j = 340). A total of 39 duplications were removed. 44 references were ordered via the central medical library [Ärztliche Zentral Bibliothek] (Table 6). A further 12 primary studies had to be excluded, as full texts could not be found (Table 5c), which left 289 primary study full texts included for our data analysis of primary studies.
Table 5. 5a, 5b, 5c.
List of excluded studies.
| 5a. Reviews identified in Reviews (k = 6) | Review | |
| 1 | Barlow J., Brown S.S. & Fletcher J. (1997) Systematic Review of the School Entry Medical Examination. Health Services Research Unit, Oxford. | Wainwright et al. (2000) [39] |
| 2 | Wainwright, P.; Thomas, J.; Jones, M. (2000). Health Promotion and the Role of the School Nurse: a Systematic Review. Journal of Advanced Nursing, 5, 1083–1091. | Schmitt & Goerres (2012) [48] |
| 3 | DeBell, D. (2006). School Nurse Practice: a Decade of Change. Community Practitioner, 10, 324–327. | Schmitt & Goerres (2012) [48] |
| 4 | Edwards, D., Noyes, J., Lowes, L., Spencer, L. H., & Gregory, J. W. (2014). An ongoing struggle: a mixed-method systematic review of interventions, barriers and facilitators to achieving optimal self-care by children and young people with type 1 diabetes in educational settings. BMC pediatrics, 14(1), 1–27. | Stefanowicz & Stefanowicz (2018) [49] |
| 5 | Kelo M, Martikainen M, Eriksson E. Self-care of school-age children with diabetes: an integrative review. J Adv Nurs. 2011;67:2096–108. doi: 10.1111/j.1365-2648.2011.05682.x. | Stefanowicz & Stefanowicz (2018) [49] |
| 6 | Maughan, E. (2003). The impact of school nursing on school performance: A research synthesis. The Journal of School Nursing, 19(3), 163–171 | Schmitt & Goerres (2012) [48] |
| 5b. References that could not be exported to EndNote (k = 10) | Reviews that included reference | |
| 1 | Bergren M.D. & Mehl R. (1995a) Electronic Communication Part 111. Journal of School Nursing 11, 7±9. | Wainwright et al. (2000) [39] |
| 2 | British Paediatric Association. (1995) Health Needs of School Age Children. British Paediatric Association, London. | Wainwright et al. (2000) [39] |
| 3 | Cohen P. (1997) School nurses: in a class of their own. Healthlines 42, 14±16. | Wainwright et al. (2000) [39] |
| 4 | Department of Health (n.d.) Promoting effective health services for school aged children and young people: A good practice guide. The Stationery Office, London (Autor angeschrieben) | Turner & Mackay (2015) [50] |
| 5 | Health Visitors Association. (1991) Pro®ling school health. Health Visitors Association, London. | Wainwright et al. (2000) [39] |
| 6 | Health Visitors Association. (1992) Health assessments and the school nurse. Health Visitors Association, London. | Wainwright et al. (2000) [39] |
| 7 | Joyner, S. (2012). ‘What are school health nurses lived experiences of working with children and their families who are subject to a child protection plan? | Harding et al. (2019) [27] |
| 8 | Naish J. & Barr M. (1991) Rights of access. Health Visitor 64, 300±301. | Wainwright et al. (2000) [39] |
| 9 | NHS Wales (1988). Putting Patients First. HMSO, London. | Wainwright et al. (2000) [39] |
| 10 | Welsh Office (1997) Supporting Pupils with Medical Needs in Schools. Welsh Office Circular 34/97, Welsh Health circular 97/31, Welsh Office (Education Dept), Cardiff. | Wainwright et al. (2000) [39] |
| 5c. Primary studies excluded, as full texts not found | Reviews [reason for exclusion] | |
| 1 | Anyanwu, I. (2005). The Face of Diversity. Challenges in School Health. School Nurse News, 1, 27. | Schmitt & Goerres (2012) [48] [not found] |
| 2 | Baldwin, C. M. (1998). Changing health outcomes for African American children: Utilizing a self-care health promotion curriculum in urban elementary schools. Journal of Multicultural Nursing & Health, 4(20), 40–45. | Stock et al. (2002) [51] [not found] |
| 3 | Bergren M.D. & Mehl R. (1995b) Health software for school nurses. Journal of School Nursing 11, 6±7. | Wainwright et al. (2000) [39] [not digitalized, no copy available] |
| 4 | Bergren M.D. & Murphy E.A. (1997) The best of the web for school health. Journal of School Nursing 13, 36±37. | Wainwright et al. (2000) [39] [not digitalized, no copy available] |
| 5 | Bergren M.D. (1996) School nurse politics on the web. Journal of School Nursing 12, 39±40. | Wainwright et al. (2000) [39] [not digitalized, no copy available] |
| 6 | Diao, W., Patel, J., Snitzer, M., Pond, M., Rabinowitz, M. P., Ceron, G.,… & Levin, A. V. (2016). The effectiveness of a mobile clinic in improving follow-up eye care for at-risk children. Journal of Pediatric Ophthalmology & Strabismus, 53(6), 344–348. | Best et al. (2018) [3] [not found] |
| 7 | Fox, P. G., Cowell, J. M., Montgomery, A. C., & Willgerodt, M. A. (1997). Southeast Asian refugee women and depression: A nursing intervention. The International Journal of Psychiatric Nursing Re- search, 4, 423–432. | Stock et al. (2002) [51] [not found] |
| 8 | Fox, P. G., Rossetti, J., Burns, K. R., & Popovich, J. (2005). Southeast Asian refugee children: a school-based mental health intervention. The international journal of psychiatric nursing research, 11(1), 1227–1236. | Tanner (2020) [52] [not found] |
| 9 | Kaufman, J., & Blanchon, D. (1996). Managed care for children with special needs: A care coordination model. Journal of Care Management, 2, 46–59. | McClanahan & Weismuller (2014) [53] [not found] |
| 10 | Palmore S. & Millar K. (1996) Some common characteristics of pregnant teens who choose childbirth. Journal of School Nursing 12, 19±22. | Wainwright et al. (2000) [39] [not found] |
| 11 | Rote S. (1997b) Healthy futures. Nursing Standard 11, 17. | Wainwright et al. (2000) [39] [not found] |
| 12 | Smith, S. (2008). The School Nurse as Prevention Specialist. School Nurse News, 11, 28–32. | Schmitt & Goerres (2012) [48] [not found] |
Table 6. Primary studies ordered via the central medical library.
| Articles ordered via Central Medical Library [Ärztliche Zentral Bibliothek] | Reviews that included reference | |
|---|---|---|
| 1 | Adams C. (1990) Perceptions of the comprehensive-based school nurse. Health Visitor 63, 90±92 | Wainwright et al. (2000) [39] |
| 2 | Allensworth D.D. (1996) Guidelines for Adolescent Preventive Services: a Role for The School Nurse. Journal of School Health 66, 281±285. | Wainwright et al. (2000) [39] |
| 3 | Anyanwu, I. (2005). The Face of Diversity. Challenges in School Health. School Nurse News, 1, 27. | Schmitt & Goerres (2012) [48] |
| 4 | Bagnall P. (1995) School nurses’ response to the measles vaccination campaign. Nursing Times 91, 38±39. | Wainwright et al. (2000) [39] |
| 5 | Bagnall P. (1997) Children’s health: taking it seriously. British Journal of Community Health Nursing 2, 68. | Wainwright et al. (2000) [39] |
| 6 | Baldwin, C. M. (1998). Changing health out- comes for African American children: Utilizing a self-care health promotion curriculum in urban elementary schools. Journal of Multicultural Nursing & Health, 4(20), 40–45. | Stock et al. (2002) [51] |
| 7 | Barlow J., Brown S.S. & Fletcher J. (1997) Systematic Review of the School Entry Medical Examination. Health Services Research Unit, Oxford. | Wainwright et al. (2000) [39] |
| 8 | Barrett, J. C. (2000). A school-based care management services for children with special needs. Family and Community Health, 23, 36–42. | McClanahan & Weismuller (2014) [53] |
| 9 | Bhardwa, S. (2013). "Mental health in young people." Independent Nurse 6. | Turner & Mackay (2015) [50] |
| 10 | Bolton P. (1994) School entry screening by the school nurse. Health Visitor 67, 135±136. | Wainwright et al. (2000) [39] |
| 11 | Bonaiuto M.M. (1995) Students who depend on medical technology. Journal of School Nursing 11, 21±28. | Wainwright et al. (2000) [39] |
| 12 | Bradley, B. J. (1998). Establishing a research agenda for school nursing. Journal of School Health, 68(2), 53–61. | Wainwright et al. (2000) [39] |
| 13 | Bradley,B.J.(1997). TheSchoolNurse as Health Educator. Journal of School Health, 1, 3–8. | Schmitt & Goerres (2012) [48] |
| 14 | Brother N. (1998) School nursing and student assistance. A natural partnership. Journal of School Nursing 14, 32±35. | Wainwright et al. (2000) [39] |
| 15 | Costante C. (1996) Supporting student success: School nurses make a difference. Journal of School Nursing 12, 4±26. | Wainwright et al. (2000) [39] |
| 16 | Diao, W., Patel, J., Snitzer, M., Pond, M., Rabinowitz, M. P., Ceron, G.,… & Levin, A. V. (2016). The effectiveness of a mobile clinic in improving follow-up eye care for at-risk children. Journal of Pediatric Ophthalmology & Strabismus, 53(6), 344–348. | Best et al. (2018) [3] |
| 17 | Fagan R. (1995) Health of the Nation Targets: where school nurses ®nd constraints on achievement. Nursing Standard 9, 36±40. | Wainwright et al. (2000) [39] |
| 18 | Few C., Hicken I. & Butterworth T. (1996) Alliances in school sex education: teachers and school nurses’ views. Health Visitor 69, 220±223. | Wainwright et al. (2000) [39] |
| 19 | Fox, P. G., Cowell, J. M., Montgomery, A. C., & Willgerodt, M. A. (1997). Southeast Asian refugee women and depression: A nursing intervention. The International Journal of Psychiatric Nursing Re- search, 4, 423–432. | Stock et al. (2002) [51] |
| 20 | Fox, P. G., Rossetti, J., Burns, K. R., & Popovich, J. (2005). Southeast Asian refugee children: a school-based mental health intervention. The international journal of psychiatric nursing research, 11(1), 1227–1236. | Tanner et al. (2020)[52] |
| 21 | France J (2013) New texting service for teenagers has all-round benefits. Nursing Standard 28(5): 13 | Turner & Mackay (2016) [50] |
| 22 | Fryer, G. E., & Igoe, J. B. (1995). A relationship between avail- ability of school nurses and child well-being. Journal of School Nursing, 11(3), 12–18. | Wainwright et al. (2000) [39] |
| 23 | Gaffrey, E. A.; Dewey Bergren, M. (1998). School Health Services and Mana- ged Care. Journal of School Nurs- ing, 4, 5–20. | Schmitt & Goerres (2012) [48] |
| 24 | Henry. (1997) A nursing informatics approach for addressing national issues and priorities for school nursing services. Journal of School Nursing 13, 39±41. | Wainwright et al. (2000) [39] |
| 25 | Igoe J.B. (1994) School Nursing. Nursing Clinics of North America 29, 443±458. | Wainwright et al. (2000) [39] |
| 26 | Kaufman, J., & Blanchon, D. (1996). Managed care for children with special needs: A care coordination model. Journal of Care Management, 2, 46–59. | McClanahan & Weismuller (2014) [53] |
| 27 | Kimel L.S. (1996) Handwashing education can decrease illness absenteeism. Journal of School Nursing 12, 14±18. | Wainwright et al. (2000) [39] |
| 28 | Kornguth M.L. (1991) Preventing school absences due to illness. Journal of School Health 61, 272±274 | Wainwright et al. (2000) [39] |
| 29 | Lamb J.M., Albrecht S. & Sereika S. (1998) Consideration of factors prior to implementing a smoking cessation program. Journal of School Nursing 14, 14±19 | Wainwright et al. (2000) [39] |
| 30 | Land, M., & Barclay, L. (2008). Nurses’ contribution to child protection. Neonatal, paediatric and child health nursing, 11(1), 18–24. | Harding et al. (2019) [27] |
| 31 | Lunney M. (1996) The signi®cance of nursing classi®cation systems to school nursing. Journal of School Nursing 12, 35±37. | Wainwright et al. (2000) [39] |
| 32 | Lunney M., Cavendish R., Kraynyak Luise B. & Richardson K. (1997) Relevance of NANDA and health promotion diagnoses to School Nursing. Journal of School Nursing 13, 16±22. | Wainwright et al. (2000) [39] |
| 33 | Nutbeam D., Farley P. & Smith C. (1990) England and Wales. Perspectives in school health. Journal of School Health 60, 318±322. | Wainwright et al. (2000) [39] |
| 34 | Oda D.S. (1992) Is school nursing really the invisible practice? Journal of School Health 62, 112±113. | Wainwright et al. (2000) [39] |
| 35 | Palmore S. & Millar K. (1996) Some common characteristics of pregnant teens who choose childbirth. Journal of School Nursing 12, 19±22. | Wainwright et al. (2000) [39] |
| 36 | Reid J.A. (1991) Developing the role of the school nurse in public health. Health Education Journal 50, 118±122. | Wainwright et al. (2000) [39] |
| 37 | Resnicow K. & Allensworth D. (1996) Conducting a comprehensive school health program. Journal of School Health 66, 59±63. | Wainwright et al. (2000) [39] |
| 38 | Rote S. (1997b) Losing sight of the future. Nursing Times 93, 24, 58±59. | Wainwright et al. (2000) [39] |
| 39 | Schoenfeld D.J. (1996) Talking with school-age children about AIDS and death. Journal of School Nursing 12, 26±32. | Wainwright et al. (2000) [39] |
| 40 | Skelley JP, Luthin DR, Skelley JW, Kabagambe EK, Ashraf AP, Atchison J.A. Parental perspectives of diabetes management in Alabama public schools. South Med J. 2013;106:274–9. doi: 10.1097/smj.0b013e31828de4a4. | Stefanowicz & Stefanowicz (2018) [49] |
| 41 | Smith, S. (2008). The School Nurse as Prevention Specialist. School Nurse News, 11, 28–32. | Schmitt & Goerres (2012) [48] |
| 42 | Staudt, A.M., Alamgir, H., Long, D. L., Inscore, S. C.,&Wood, P. R. (2015). Developing and implementing a citywide asthma action plan: A community collaborative partnership. Southern Medical Journal, 108, 710–714. doi:10.14423/SMJ.0000000000000380 | Best et al. (2018) [3] |
| 43 | Urbinati, D.; Steele, P.; Harter, B. J. E.; Harrell, D. (1996). The Evolution of the School Nurse Practitioner: Past, Present and Future. Journal of School Nursing, 2, 6–9. | Schmitt & Goerres (2012) [48] |
| 44 | Whitmore K. (1988) School refusal. Health Visitor 61, 349±351. | Wainwright et al. (2000) [39] |
3.2 Study characteristics of reviews
All of the reviews included in our overview of reviews focus on school nurse-led interventions and their impact on children’s health outcomes. Each of the research papers focuses on different aspects of the content. Studies that summarized the scope of school nurses’ interventions and general health outcomes were examined by two research groups [3,51]. Two papers summarized evidence on vaccination rates for students [54,55]. Child maltreatment and prevention [27], asthma care [56], school performance [57,58], obesity prevention [31], diabetes [49], epileptic seizures [29] and mental health [50,59] were also scrutinized. While one study focused on children with complex needs [53], another paper concentrated on general health promotion [39]. One German study summarized evidence on the school nurse, with implications for the German school system [48]. The time periods covered by reviews were 1976 up to 2021. About 50% of reviews were conducted in the USA [3,31,51–53,55,56,58], while the other references were from the UK [27,39,50,57,59], Italy [54], Poland [49] and Germany [48] (Table 7).
Table 7. Characteristics of reviews (k = 16).
| First author [country] (year) | Time-period covered | Study design (Type of Overview) | Number of included references | Subject matter | Summary findings | Funding | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mental health | Somatic Illness | Health literacy | Prevention & Health Promotion | Interdisciplinary Aspects | Case management | Attendance and / academic achievement | ||||||
| Best, Oppewal [3] [USA] (2018) | 2011–2017 | (Integrative Literature Review) | 65 | X | X | X | “School nurse interventions […] benefited school-aged children with life-threatening diseases like asthma and diabetes and children with serious health conditions […]”. | No funding | ||||
| Guarinoni and Dignani [54] [Italy] (2021) | 1976–2016 | (Narrative Review) | 9 | X | “The present study shows that the school nurse plays a key role in increasing the rate of adhesion to immunization for school-aged children/ adolescents”. | Not mentioned | ||||||
| Harding, Davison-Fischer [27] [UK] (2019) | Until 2019 | (Integrative Literature Review) | 21 | X | “Huge variety of activities that school nurses undertake to protect children from maltreatment. Several challenges to this role are identified, including time management and building relationships with children”. | Not mentioned | ||||||
| Isik and Isik [56] [USA] (2019) | 2011–2018 | (Integrative Literature Review) | 12 | X | X | “School nurses can drive effective asthma care […] and prevent health care fragmentation, emergency room visits, hospitalization, school absenteeism, and can increase asthma knowledge and the quality of life for students and parents”. | Not mentioned | |||||
| Lineberry and Ickes [55] [USA] (2014) | 1937–2013 | (Systematic Review) | 30 | X | X | X | X | “While some studies of immunization compliance, attendance rates, body mass index screening, vision screening, and follow-up are promising, results are mixed and additional evidence is needed”. | No funding | |||
| Maughan [58] [USA] (2003) | 1965–2003 | (Research Synthesis) | 15 | X | X | “Nursing interventions targeted at specific populations, including parents, have had significant effects.” | Not mentioned | |||||
| McClanahan and Weismuller [53] [USA] (2014) | 1990–2013 | (Integrative Literature Review) | 25 | X | “Recommendations for improving care coordination were elucidated in the review. Analysis of the literature can help assure application of best practice methods for the coordination of care for students in the school setting”. | No funding | ||||||
| Schmitt and Görres [48] [Germany] (2012) | 1983–2009 | (Integrative Literature Review) | 34 | X | X | “The School Nurse has a wide range of activities, with coordination and mediation as a central area of responsibility”. | Not mentioned | |||||
| Schroeder, Travers [60] [USA] (2016) | unclear | (Systematic Review and Meta-Analysis) | 8 | X | “Findings […] suggest that school nurses can play a key role in implementing sustainable, effective school-based obesity interventions”. | National Institute of Nursing Research | ||||||
| Stefanowicz and Stefanowicz [49] [Poland] (2018) | unclear | (Literature Review) | 12 | X | “According to parents and children with type 1 diabetes mellitus, various forms of school nurse support […] are consistently effective and should have an impact on the condition, improvement of metabolic control, school activity and safety at school”. | No funding | ||||||
| Stock, Larter [51] [USA] (2002) | 1980–2001 | (Literature Review) | 26 | X | X | X | X | “15 articles documented positive outcomes related to school nurse services. A majority of the outcomes pertained to health education and prevention”. | Wash-ington State Office of Superinten-dent of Public Instruction | |||
| Tanner et al. [52] [USA] (2020) | 1998–2017 | (Integrative Review) | 15 | X | “School nurses play an active role in mental health interventions and should be involved in replicating and testing known mental health interventions to investigate their effectiveness for students with Psychogenic nonepileptic seizures (PNES)”. | Robert Wood Johnson Foundation: Future of Nursing Scholars Program | ||||||
| Tilley and Chambers [59] [UK] (2003) | 1990–2003 | (Systematic Review) | 0 | X | “The systematic review did not locate any current published evidence of existing screening tools being applied by school nurses to detect mental ill health among adolescents in schools. The effectiveness or ineffectiveness of such tools used by school nurses thus could not be evaluated”. | Welsh Office of Research and Development for Health and Social Care | ||||||
| Turner and Mackay [50] [UK] (2015) | unclear | (Literature Review) | 29 | X | “A variety of evaluation methods were used to identify outcomes, including qualitative and quantitative methods and standardised tools. However, the majority of papers described outcomes without reference to a systematic approach to evaluation”. | Not mentioned | ||||||
| Wainwright, Thomas [39] [UK] (2000) | 1980–2000 | (Brief of Literature) | 48 | X | X | X | X | “The results of the review were disappointing, in that little research of acceptable quality was found and little could be said about the effectiveness [of school nurses]. The result is therefore a more diffuse review that gives a summary of descriptive research and current views and opinions […]”. | Not mentioned | |||
| Yoder [57] [UK] (2020) | 2002–2018 | (Integrative Literature Review) | 16 | X | “[…] The presence of a school nurse is associated with reduced absenteeism and missed class time but not with academic achievement”. | No funding | ||||||
3.3 Quality assessment of reviews
Out of a total of sixteen references, six studies are of moderate quality (score: 16–32) [31,32,49,52,56,57], ten are of low quality [3,27,39,48,50,51,54,55,58,59] and no study is of high quality (Table 8).
Table 8. Methodological quality assessment of reviews based on AMSTAR-2 criteria (k = 16).
| Best et al. (2018) [3] | Guarinoni & Dignani (2021) [54] | Harding et al. (2019) [27] | Isik & Isik (2019) [56] | Lineberry & Ickes (2014) [55] | Maughan (2003) [58] | McClanahan & Weismuller (2014) [53] | Schmitt & Görres (2012) [48] | Schroeder et al. (2016) [31] | Stefanowicz & Stefanowicz (2018) [49] | Stock et al. (2002) [51] | Tanner et al. (2020)[52] | Tilley & Chambers (2003) [59] | Turner & Mackay (2015) [50] | Wainwright et al. (2000) [39] | Yoder (2020) [57] | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A. Research question & selection process | ||||||||||||||||
| 1. Report of inclusion criteria (PICO) | 3 | 0 | 2 | 1 | 2 | 3 | 2 | 1 | 3 | 4 | 3 | 3 | 2 | 0 | 3 | 4 |
| 2. Explanation for selected study designs | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 3. Comprehensive search strategy | 3 | 3 | 3 | 4 | 2 | 2 | 4 | 2 | 2 | 3 | 3 | 3 | 2 | 4 | 4 | 2 |
| 4. Two independent researchers | 4 | 4 | 3 | 3 | 0 | 0 | 4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 0 |
| 5. List of excluded studies | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 0 | 0 | 0 | 0 | 0 | 0 |
| B. Assessment of included primary studies | ||||||||||||||||
| 1. Description of studies in adequate detail | 0 | 3 | 3 | 2 | 3 | 3 | 0 | 1 | 4 | 3 | 2 | 3 | 0 | 2 | 1 | 3 |
| 2. Assessment of Risk of Bias (RoB) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 3. Report of funding | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 4. Performance of meta-analysis with appropriate methods | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| C. Interpretation of results | ||||||||||||||||
| 1. Consideration of RoB in results | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 2. Explanation of heterogeneity in results | 0 | 4 | 4 | 4 | 0 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 0 | 4 |
| D. Other | ||||||||||||||||
| 1. Report of potential source of conflict | 4 | 0 | 0 | 4 | 4 | 0 | 4 | 0 | 4 | 4 | 0 | 4 | 0 | 4 | 0 | 4 |
| Overall assessment | ||||||||||||||||
| 1. Overall score (max = 48) | 14 | 14 | 15 | 18 | 11 | 12 | 18 | 8 | 28 | 22 | 12 | 17 | 8 | 14 | 11 | 17 |
| 2. Assessment (high, moderate or low quality) | L | L | L | M | L | L | M | L | M | M | L | M | L | L | L | M |
Notes. Categorisation of quality rating (see table X): 0 = 0% of sub-criteria met, 1 = 1%–24% of sub-criteria met, 2 = 25%–49% of sub-criteria met, 3 = 50%–74% of sub-criteria met, 4 = 75%-100% of sub-criteria met; H = high study quality (overall score = 32 or more), M = moderate study quality (overall score = 16 to 32), L = low study quality (overall score = 16 or less).
3.4 Study characteristics of primary studies
Of the 289 primary studies included, there were 32 references (11%) that were identified as RCTs, 64 (22%) as Obs, a further 98 (34%) used a qualitative-descriptive design, 79 (27%) used a quantitative-descriptive design and 16 references (6%) could not be assigned to any study design. Studies were conducted in the USA (j = 210), UK (j = 59), Sweden (j = 8), Australia (j = 3), Finland (j = 3), Netherlands (j = 2), France (j = 2), Spain (j = 1) and Nigeria (j = 1).
A total of 77 references (27%) examined school nurse-led interventions, where a school nurse alone was involved, whereas 20 references (7%) examined interventions where a school nurse as well as other health professionals or teachers performed an intervention. Most studies (84; 29%) examined interventions conducted by other health professionals (not school nurses) or they described health outcomes without conducting an intervention. These studies focused on a program’s efficacy and school nurse’s efficacy from the perspective of teachers, parents or health professionals. A significant number of studies (50; 17%) focused on school nurses`training and described the school nursing job. The remaining studies (58; 20%) examined different aspects not relevant to the present study (S2 Table, Fig 6).
Fig 6. Matrix for categorization of content dimension and study design (with results).
3.5 Selected primary studies to examine body of evidence
Relevant primary studies were selected according to two criteria: study design and content dimension (Fig 6). Studies with the study design RCT and Obs and content dimensions “D” and “E” were selected (total: 74 studies). There were eight references examining the outcome “school attendance” of which one study identified as an RCT [61]. From eleven studies investigating obesity prevention, six were RCTs [17,38,62–65]. Physical activity was investigated by three research groups of which one identified as RCT [66]. Researchers of eight studies investigated emotional health, of which two were RCTs [14,67]. Of 16 papers examining asthma care, six identified as RCTs [68–73]. One RCT examined smoking cessation [19] and one RCT investigated immunization rates as a health outcome [35]. Sexually transmitted virus prevention was covered by two RCTs [74,75] and evidence on teenage pregnancy, nutrition, and teasing and bullying, respectively, was investigated in one Obs [76–78]. Allergies [79], alcohol use prevention [80], hearing screening [81], cardiovascular health [82], psychosomatic headaches [83] and hygiene [34] were each assessed by one RCT. Two research groups investigating diabetes used RCTs [84,85]. Five research groups did not confine themselves to one specific outcome but addressed a range of different health outcomes in one primary study, of which one identified as RCT [86]. Assessing the RoB, 16 primary studies showed a low risk of bias, 33 showed a high risk and 25 showed an unclear risk of bias (Table 9).
Table 9. Body of Evidence according to GRADE assessment.
| Author | Design RCT/Obs | Indirectiveness of Evidence | Publication bias | RoB [Scale] Category |
Imprecision | Impact | |||
|---|---|---|---|---|---|---|---|---|---|
| Population | Intervention | Measures | N | CI* | |||||
| School Attendance | |||||||||
| Allen [13] | Obs | Children in elementary schools | Full-time school nurse | All day attendance, check out for medical reasons, health care insurance | No indication | High [8] E, F |
10,000 | / | The percentage of student checkouts for medical reasons in schools with a full-time nurse (M = 11.1%) was statistically significantly lower, t(20) = 2.27, a< .05, d = 2.77 than schools without a fulltime nurse (M = 15.7%). |
| Long et al. [61] | RCT | Children with more than 14 days absence in one year | Activity of the school nurse and record of her activity | Mean days of absence | No indication | Low [2] E |
302 | / | The control group’s mean decline was 5.10, resulting in a statistically significant mean difference of 1.98 between the intervention and control groups. In other words, pupils in the intervention group showed a decline in absences which averaged 2 days more than the reduction experienced by those in the control group, and this difference can be viewed as a non-chance occurrence. |
| Foster & Keele [87] | Obs | Children in kindergarten up to grade 5 | School nurses administer Over-the-Counter medications | Sent home rates | No indication | High [8] E, D |
Approx. 10,000 | / | There were no statistically significant differences found among sent home rates for the 2 school years after the policy change. The mean number of students sent home before the policy was implemented was 353, or 3.6%, whereas the mean number of students sent home in the first year after the policy was implemented was 342 students, or 3.4%, 2(23) = -.37, P = .72. The second year of implementation found 329 students, or 3.1%, were sent home. |
| Rodriguez, Rivera [88] | Obs | Children in pre-kindergarten to grade 8 | Trained full-time school nurse and part-time school nurses | Average Daily Attendance was measured through parent report + verification of school clerk, health measures | Unlikely, funded by Lucile Packard Foundation for Children’s Health and the Lucile Packard Children’s Hospital | High [8] H, F |
6,664 | √ | Decrease in the mean number of absences due to illness among students in demonstration schools, whereas the mean number of absences among students in control schools increased. This reduction in mean absences due to illness was statistically significant between demonstration and comparison groups (p < .05). students in demonstration schools were less likely than students in control schools to miss 1 or more days of school due to illness (OR = 0.876, 95% CI: 0.767–1.001, p < .05). |
| Telljohann, Dake [89] | Obs | Children with asthma in kindergarten to grade 6 | Full-time school nurse (5 days) vs. part-time school nurse (2 days) | Grade, race, sex, school lunch status, and number of days missed | No indication | High [9] D, I |
569 | / | Students with full-time school nurses missed significantly fewer school days (M = 510.6, SD = 59.2) than students with part-time school nurses (M = 513.0, SD = 511.6) (t = 522.68, DF = 5566, p < .05). |
| Van Cura [90] | Obs | Students with lower socioeconomic status | School-based health centers | Academic outcomes and loss of seat time (data on early dismissal) | No indication | Unclear [7] G, F |
764 | / | SBHCs significantly reduced the number of early dismissals from school (p = .013) in a comparison with students who received school nursing services alone. Students not enrolled in an SBHC lost 3 times as much seat time as students enrolled in an SBHC. |
| Weismuller, Grasska [116] | Obs | Children in kindergarten to grade 5 | Retrospective review of health records | Referrals to school nurse, interventions, outcome of school nurse intervention; Schools Administrative Student Information system (SASIS) to document reason for absence | No indication | High [10] G, J(1), I |
240 | / | The most common reason (65.8%) for referral was screening. After that, physical illness. No referrals to the school nurse for absenteeism and school nurse interventions were not targeted to attendance, despite 17% of students missing 11 or more school days. Documentation was sparse (primarily task related). Information about the outcome was insufficient to determine the effectiveness of nursing interventions. |
| Wiggs-Stayner, Purdy [91] | Obs | School-aged children and staff | Free Flu-Mist immunizations | Attendance rates | Unlikely, funded by the Parkview Hospital Community Health Improvement Program |
Unclear [7] H(2) |
277 + unknown control | / | The 2 schools receiving FluMist increased their attendance rates from 95.3% and 93.9% to 96.1% and 95.8%. Previously, the comparison schools each had a 94.6% attendance rate; one fell to 94.4% and the other rose very slightly to 94.7%. The differences in self- or parent reported influenza absences were not significant. However, the difference in days absent between individual vaccinated and nonvaccinated schools was statistically significant. |
| Overweight and Obesity Prevention | |||||||||
| Bonsergent, Agrinier [17,62] | 2x RCT | Children in high schools | Education, environment and screening by school nurse | Weight and height (waist circumference later excluded) | No indication | Low [2] D(3), F |
3,538 | √ | The 2-year change of outcomes was more favorable in the 12 month screening compared to the no-screening ones: a 0.11 lower increase in BMI (p<0.0303); a 0.04 greater decrease in BMI z-score (p<0.0173); and a 1.71% greater decrease in overweight/obesity prevalence (p_0.0386). Education and environment strategies were not more effective than no strategy intervention. |
| Hawthorne et al. [92] | Obs | Children in schools | Walking program 3 days a week/ 16 weeks | Body Mass Index (BMI), waist circumference, and cardio-respiratory (by using the Progressive Aerobic Cardiovascular Endurance Run test (PACER test) | Unlikely, funded by Kids Sports Stars for data analysis funding |
High [8] F, G |
1,074 | / | Cardio-respiratory fitness increased by 37.1% over baseline in the entire sample (p < .01). The increase in fitness was observed in both genders and across all grade levels. Furthermore, significant improvements in fitness were observed among healthy weight, overweight, and obese youth. However, obese youth had a smaller overall change in fitness compared to overweight or healthy weight participants. No significance changes in BMI or waist circumference (p > .05); |
| Johnston et al. [38,63] | RCT | Children aged 7–9 years | Curriculum with health information + health professional | Weight and height to measure Body Mass Index (BMI); Grades in math, science and reading to measure academic outcome |
No indication | Unclear [5] B, D, F |
835 | √ | After 2 years, children who were overweight/obese in the professional-facilitated intervention (PFI) condition significantly reduced their standardized BMI (zBMI) compared to children in the Self-help (SH) condition (Wald χ2 = 28.7, p < .001). End-of-year grades decreased for overweight/obese students in both conditions; however, students in the PFI exhibited a smaller decrease in grades compared to the SH condition (Wald χ2 = 80.3, p < .001). |
| Melin and Lenner [93] | Obs | Overweight children 7 years of age | Dietary advice | Weight, BMI, Changes in well-being and lifestyle were measured with the help of a structured interview | No indication | High [10] G, J(4), I |
20 | / | A good (91%) or fair (54%) adherence to dietary advice was found in children who decreased or maintained their z-score respectively. Mean BMI z-score reduced [)0.16 (p = 0.03)] during the intervention period. Generally, parents and school nurses were satisfied with the program, helping them to set limits and be more self-confident in their role as ‘health adviser’ respectively. |
| Note. Detailed risk of bias assessment (1) Use of existing health records; documentation varied widely among school sites and study information was limited to existing record contents; (2) No information on control group (size, population, etc.); (3) Lack of an “ideal” anthropometric outcome to evaluate the effectiveness of prevention strategies. BMI might be considered an inappropriate way to evaluate weight status in children and adolescents, as it naturally increases with age; (4) Fear for stigmatization, considering the intervention design with visits to the nurse during school hours | |||||||||
| Pbert, Druker [65] | RCT | Overweight or obese adolescents in grades 9 to 12 | School nurse-delivered cognitive behavioral counseling and an afterschool exercise program | BMI, 24-hour dietary recall interview, Physical activity (PA) with accelerometer, Survey to measure sedentary behaviour, TV, computer games, questionnaires to measure self-efficacy (11-item questionnaire) and perceived barriers |
Unlikely, funded by National Institutes of Health, National Heart, Lung and Blood Institute | Low [2] G |
126 | √ | Students in the intervention compared with control schools showed no significant differences in anthropometric variables including BMI, percent body fat, and waist circumference at follow-up. Students in intervention compared with control schools reported eating breakfast on significantly more days/weeks at follow-up, adjusted mean 4.65 vs. 3.84 days, respectively (adjusted mean difference 0.81 days; 95% CI 0.11–1.52). The mean number of days students reported being physically active in the past 7 days was similarly high in the intervention compared with control schools at follow-up, adjusted mean 4.54 days vs. 3.64 days, respectively (adjusted mean difference 0.89 days; 95% CI 0.25–1.53). |
| Pbert, Druker [64] | RCT | Overweight or obese adolescents in grades 9 to 12 | School nurse-delivered counseling intervention “Lookin’ Good Feelin’ Good”, utilizing cognitive-behavioral techniques |
BMI, 24-hour dietary recall interview, PA with accelerometer, Survey to measure sedentary behaviour, TV, computer games, questionnaires to measure self-efficacy and perceived barriers |
Unlikely, funded by National Institutes of Health, National Heart, Lung and Blood Institute | Unclear [4] E, G |
84 | √ | At 2 months, intervention participants ate breakfast on more days/week (difference = 1.01 days; 95% CI 0.11, 1.92), and had a lower intake of total sugar (difference = −45.79g; 95% CI −88.34, −3.24) and added sugar (difference = −51.35g; 95% CI −92.45, −10.26) compared to control participants. At 6 months, they were more likely to drink soda ≤ one time/day (OR 4.10: 95% CI 1.19, 16.93) and eat at fast food restaurants ≤ one time/week (OR 4.62: 95% CI 1.10, 23.76) compared to control participants. There were no significant differences in BMI, activity or caloric intake. |
| Sherman, Alexander [94] | Obs | Obese children in grades 4–6 | 9 lessons of a 9-week period which addressed self-esteem, food choices and nutrition, and PA and fitness | Weight skinfold measurements (desired outcome: amount of lean and fat tissue in the body), questionnaires to measure self-esteem and nutritional knowledge | No indication | High [10] G, I, F |
26 | / | Self-esteem increased significantly (p< .001) between the pre-test and post-test interval. Weight status and nutritional knowledge showed no improvement. |
| Speroni, Earley [95] | Obs | Children grade 2–5 | Kids Living Fit-Intervention ($100 fee to Participate) PA activity, dietary education | BMI, waist circumference, questionnaires to measure food, activity, and satisfaction | No indication | Unclear [7] H |
185 | / | All KLF intervention groups in the four schools experienced a decrease in BMI percentile from the baseline measure to remeasure recorded at Weeks 12 and 24. The two single largest decreases in BMI percentile occurred in the contrast groups in Schools 1 and 4, with an 8.5 and 7.9 (p< .1) percentile point decrease, respectively. By comparison, participants in the KLF group in School 1 had a 4.0 (p< .1) percentile point decrease in BMI. |
| Tucker and Lanningham-Foster [96] | Obs | Children in grade 4 and 5 | Refined health messaging (Let’s Go 5-2-1-0) program | BMI percentile, Healthy Habits Survey to measure nutrition, screen time, PA, and family eating patterns, a StepWatch Activity Monitor to measure PA levels |
No indication | High [10] G, D, I |
72 | / | School A: BMI percentile did not change significantly over time. The mean/median number of servings of fruits and vegetables per day significantly increased from baseline to end of year (p = .001), while the number of servings of 100% fruit juice per day significantly decreased (p = .003). There was also a trend in minutes of self-reported active play, which increased from baseline to end of year (p = .057). Objectively measured participant PA levels increased significantly (p < .005) from baseline (M = 12,139, SD = 401 steps) to end of year (M = 15,120, SD = 680). |
| Wong and Cheng [97] | Obs | Obese children in primary schools | Motivational interviewing (MI) counselling; + telephone consultation for parents (MI+) | Change in weight for- height percentage with reference to a territory-wide growth survey, changes in weight-related behaviours and anthropometric measures |
Unlikely, funded by the Hong Kong Institute of Education | Unclear [6] I |
185 | / | There was a significant decrease in the average calorie intake from food in the past seven days in the MI group (mean difference: 389 57; p < 0 01) and in the MI+ group (mean difference: 376 65; p < 0 01). It also showed a significant increase in the average calories consumed due to an increase in physical exercise in the past seven days in the MI group (mean difference: 2052 10; p < 0 01) and in the MI+ group (mean difference: 2590 64; p < 0 01). Control group had significant deterioration in their anthropometric measures. |
| Physical activity | |||||||||
| Robbins, Pfeiffer [98] | Obs | Middle school girls | Girls on the Move (3 motivational, individually tailored counseling sessions + after-school physical activity | Questionnaires on benefits/barriers of PA, self-efficacy, etc. to measure cognitive and affective variables related to PA, PA, cardiovascular, and body composition (BMI, waist circumference) | Unlikely, funded by National Heart, Lung, and Blood Institute and the National Institutes of Health |
High [8] J(5), G |
69 | / | Linear regressions controlling for baseline measures showed no statistically significant group differences, but directionality of differences was consistent with greater intervention group improvement for minutes of moderate to vigorous physical activity/ hour (t = 0.95, p = .35), cardiovascular fitness (t = 1.26, p = .22), body mass index (BMI; t = −1.47, p = .15), BMI z-score (t = −1.19, p = .24), BMI percentile (t = −0.59, p = .56), percent body fat (t = −0.86, p = .39), and waist circumference (t = −0.19, p = .85). |
| Williams and Warrington [99] | Obs | Children in grade 3–5 (8–10 years of age) in elementary school | Pedometer-based walking program, Get Fit Kids | Change in step counts from the children’s pedometers, participant satisfaction, and program costs | No indication | Unclear [7] D, J(6) |
231 | √ | There was a statistically significant difference in the step counts from Time 1 (M = 6,567.73, SD = 5,189.51) to Time 2 (M = 10,804.60, SD = 11,664.81), t = 3.374, p = 0.001 (two-tailed). The mean difference in the step counts was 4,236.87, with confidence levels ranging between 1,715.633 and 6,758.098. |
| Wright, Giger [66] | RCT | Children aged 8–12 years | Kids N Fitness (45 min PA), nutrition education, school-wide wellness activities | Child and Adolescent Trial for Cardiovascular Health School Physical Activity and Nutrition Student Questionnaire, anthropometric measures (Height, weight, body mass index, resting blood pressure, and waist circumference) | Unlikely, funded by the NIH/ NCMHD Loan Repayment Program and Robert Wood Johnson Foundation | Low [2] G |
251 | √ | Significant results for students in the intervention, included for boys decreases in TV viewing; and girls increases in daily physical activity, physical education class attendance, and decreases in body mass index z-scores from baseline to the 12-month follow-up. |
| Note. Detailed risk of bias assessment: (5) non-compliance with accelerometer wear; (6) Not a validated questionnaire; | |||||||||
| Emotional Health | |||||||||
| Attwood et al. [14] | 1 x RCT 1 x Obs |
Children with mean age of 10.6 years | Computerized cognitive therapy | Spence Children’s Anxiety Scale (SCAS), Strengths and Difficulties Questionnaire (SDQ) to measure desired outcome of anxiety and parental perception of child behavior | No indication | Unclear [7] B, J(7),F, G |
12 | / | A statistically significant post-intervention reduction in total child anxiety ratings on the SCAS-C for the cCBT (Z =) 1.79, p < .05), but not for the gaming condition (Z =) 1.59, p > .05). Analysis of subscale scores revealed a statistically significant post-intervention reduction on the social anxiety (Z =) 1.80, p < .05) and generalized anxiety (Z =) 1.73, p < .05) sub-scale scores for the cCBT group only. |
| Clausson and Berg [23] | Obs | Children aged 11–17 and their families | Calgary Family Assessment Model (CFAM), Calgary Family Intervention Model (CFIM), Illness Beliefs Model (IBM) | SDQ to measure desired outcome of emotional symptoms, conduct, hyperactivity, peer problems, and prosocial behavior | No indication | High [10] G(8), F, C, E |
4 | / | The families reported feeling relief and described positive affective, behavioral, and cognitive changes as a consequence of the interventions. The school nurses experienced the family sessions as time-saving and easy-to-use tools in their work. |
| DeSocio et al. [100] | Obs | Children aged 10–12 | Education program (brain, managing stress, resources, help) | 16-item pre-and posttest covering content delivered in the modules to measure the desired outcome of knowledge gain | Unlikely, funded by Northwest Health Foundation | High [8] H, F |
370 | / | Overall, student scores improved significantly from pre- to posttest (mean score increased by 1.5, P = .000). Greatest improvements in: (a) knowledge that mental illness is not the same as mental retardation; (b) knowledge that genetic factors, internal thoughts, and environmental events contribute to mental health; (c) recognition that when someone talks about suicide, it is a message to be taken seriously-the person is not just trying to get attention; (d) awareness that relationships, as well as events, can generate stress; I knowledge of chemical changes that occur in the body during stress; and (f) awareness that it is not possible to tell if someone has a mental illness just by looking at them. |
| Houck, Darnell [101] | Obs | Adolescents with depressive symptoms and related problems | 1: cognitive–behavioral intervention„ 2: A Peer Group Approach to Building Life Skills | Questionnaires to measure desired outcome of emotional distress, resources and coping skills and survey of risk to measure suicide risk factors | No indication | High [10] E, G, I |
12 | / | Assessment revealed that the students were at suicide risk. At the conclusion of the group intervention, there was a 55% decrease in suicidal ideation, a 27% decrease in perceived stress, and a 26% decrease in family distress. In addition, most of the students became engaged in formal treatment for the first time. |
| Lamb et al. [67] | RCT | Children 14–18 years in rural area | Screening of depressive symptoms, suicidal ideation, nurse-led coping skills group | The Jalowiec Coping Scale (JCS) to measure desired outcome of coping skills, The Reynolds Adolescent Depression Scale (RADS) to measure depressive symptoms | No indication | Unclear [3] G, J(9) |
40 | / | Intervention subjects showed marginally significant greater decrease than control subjects (p < .001), intervention subjects showed a marginally significant greater decrease than control subjects (p = .074). Analysis of the depression screening tool (RADS) score demonstrated that 86.9% of the intervention group showed decreased depressive symptomatology with mean improvement of 15 points, whereas 61.1% of controls showed mean improvement of 13.8 points on RADS. |
| Note. Detailed risk of bias assessment: (7) Absence of an appropriate comparison group limits the strength of any conclusions as it is unclear whether the reported improvements were due to cCBT or the passage of time; differences in both child-rated total anxiety and parent-rated SDQ scores between the cCBT and gaming groups at baseline; (8) Insufficient reporting of results, descriptive; (9) Unclear if control group didn’t realize they weren’t in the intervention group, as they didn’t receive any treatment, not even a placebo. It seems as if there was a lack of allocation concealment | |||||||||
| Muggeo, Stewart [102] | Obs | Children with anxiety symptoms aged 5–11 years | Child Anxiety Learning Modules (CALM), (cognitive behavioral strategy) | Screen for Child Anxiety-Related Emotional Disorders, Child and Parent Versions (SCARED) to measure desired outcome of anxiety; Woodcock–Johnson Tests—Achievement and Cognitive Batteries (WJ-III) to measure academic achievement and cognitive abilities | Possibly, funded by the Dep. Of Education’s Institute of Education Sciences | High [10] I, G, J(10) |
11 | √ | Results indicated significant reductions in anxiety based on child self-reported SCARED-C; t(9) = 3.36, p = .004, 95% CI [3.24, 16.56], Cohen’s d = 0.81. Significant reductions in somatic symptoms were reported at post-intervention by parents CSI-24; t(10) = 2.49, p = .016, 95% CI [41, 7.58], Cohen’s d = .78 9 and children CSI-24; t(9) = 2.21, p = .027, 95% CI [-.18, 15.98], Cohen’s d = .85. Global functioning scores, as measured by the CGAS, were significantly higher at post-intervention, with a small effect size, t(10) = -3.45, p = .003, 95% CI [-12.11, -2.61], Cohen’s d = .35 |
| Ramirez, Harland [103] | Obs | Trauma-exposed children | Listen, Protect, Connect (LPC) | Modified Child PTSD Symptom Scale, Center for Epidemiologic Studies Depression Scale (CES-D) to measure depression, Multidimensional Scale of Perceived Support (MSPSS) to measure perceived social support and Healthy Kids Resilience Measure of School Connectedness | Unlikely, funded by the University of Iowa Injury Prevention Research Center | High [10] G, E, I |
20 | √ | A significant decline in depressive symptoms was seen from baseline to each follow-up period, all levels below the clinical cut point for depression. PTSD symptoms decreased 3.7 points from baseline to the 8-week follow-up, although this change was not statistically significant (range 15.5–11.8; p = 0.09). Total social support increased from baseline to the 2-week follow-up (p = 0.08) and increased significantly from baseline to the 8-week follow-up (p < 0.01). Students felt more connected to their school at 2- (mean = 63.8, p = 0.06) and 4-weeks (mean = 68.9, p < 0.01) than at baseline (mean = 58.6), but this relationship diminished by 8-weeks. |
| Stallard et al. [104,105] | Obs | Children aged 9 and 10 | Evidence-based emotional health cognitive behaviour therapy programme, (FRIENDS) |
Spence Children’s Anxiety Scale and Culture-Free Self-Esteem Questionnaire Form B to measure desired outcome of levels of anxiety and self-esteem | No indication | High [10] G, I, E |
106 | / | Initial ANOVAs revealed a significant change for total anxiety (F = 5.84, df = 2,315, p = 0.003) and self-esteem (F = 2.98, df = 2,315, p = 0.052) across time. Post-hoc comparisons using Tukey’s test revealed no significant change in anxiety or self-esteem over the two pre-intervention assessments (T1—T2) but a significant change from T1 to post intervention (T3) for both anxiety (p = 0.002) and self-esteem (p = 0.040). There were no significant differences between the three and 12-month follow- up (T3–T4) suggesting that post FRIENDS gains were maintained. |
| Note. Detailed risk of bias assessment: (10) Participation in study was on voluntary bases for students who were motivated. This could have an impact on the results when only motivated students are considered in study | |||||||||
| Asthma care | |||||||||
| Bruzzese et al. [106] | Obs | Children in Kindergarten up to grade 5 | School nurses coordinating between families, primary care providers (PCPs), and school personnel | Paediatric Asthma Caregiver’s Quality of Life Questionnaire (PACQLQ) to measure desired outcome of impact on children’s quality of life; school absence | No indication | Unclear [7] H |
591 | / | Relative to controls, 12-months post-test intervention students had a reduction in activity limitations due to asthma (35% vs _9%, p, .05) and days with symptoms (26% vs 39%, p. .06). The intervention had no impact on the use of urgent health care services, school attendance, or caregiver’s quality of life. There were also no improvements at 24-months postintervention. |
| Christian-sen et al. [21] | Obs | Children in grade 4 (age 9–12 years) | Asthma education by school nurses | Asthma knowledge test and symptoms questionnaire to measure desired outcome of severity of asthma symptoms | No indication | Unclear [7] G |
42 | / | Mean scores for the asthma quiz improved from 9.9 (SEM = 0.44) to 13.7 (SEM = 0.30). Peak flowmeter scores improved from 3.9 (SEM = 0.33) to 6.4 (SEM = 0.29), and inhaler technique scores improved from 2.3 (SEM = 0.26) to 4.3 (SEM = 0.26). All changes in this group were highly significant (p -< 0.00001). After 180 days, the symptom scores validated for functional asthma severity were significantly lower in the educated group (2.87 + 0.447) compared with the control group (4.36 + 0.573, p = 0.0188). Asthma-related school absences, emergency department visits, and hospitalizations showed no differences between the education and control groups |
| Engelke et al. [25] | Obs | Children in grade 1–12 | Case management | PedsQL 3.0 SF22 to measure desired outcome of quality of life, grades to measure academic achievements, individualized goals evaluated by school nurses | Unlikely, funded by a grant from the Kate B. Reynolds Charitable Trust. |
High [8] E, D(11) |
143 | / | The proportion of children reporting symptom and treatment problems was significantly lower at the end of the program compared to baseline (p < .01). The largest improvement in asthma symptom and treatment problems was among students who met the goal of reducing emergency department (ED) visits/hospitalizations, symptom gain: n = 42, M = 16.0, SD = 17.0; treatment problem gain: M = 13.3, SD = 15.3) compared to those who did not met the goal [symptom gain: n = 19, M = 6.2, SD = 10.2, t(54). 2.20, p = .03, η2 = 08; treatment problem gain: M = 1.7, SD = 9.6, t(54). 2.86, p = .01, η2 = .13]. |
| Fransisco et al. [107] | Obs | Children with asthma aged 5–14 years | School nurse training, 4 key messages from EPR-3, nurses supplied with assessment tools | self-reported Inhaled corticosteroid (ICS) use and adherence, CHSA-C to measure desired outcome of impairments and inspiratory flow rate, Forced expiratory volume (FEV) and EPR-3 to assess asthma control | No indication | High [9] E, J(12), D |
178 | √ | At enrolment, 69.7% of students had “not well-controlled” or “Very poorly controlled” asthma. Postintervention, FEV significantly improved (82.9% to 92.1% predicted), and self-reported impairment and tobacco smoke exposure significantly declined (P < .001). For Teaming Up for Asthma Control (TUAC) students enrolled in Medicaid, there was an average 12-month health care cost difference (−$1,431) compared with controls. |
| Note. Detailed risk of bias assessment: (11) Not all students received grades and could be compared on academic outcome; (12) Control group was not described appropriately | |||||||||
| Halterman et al. [68] | RCT | Children with asthma aged 3–10 years | Preventive asthma medications by school nurses | Symptom-free days | No indication | Unclear [5] B, G |
530 | √ | Children receiving preventive medications through school had significantly more symptom-free days compared to children in the control group (adjusted difference = 0.92 days per 2 weeks) and also had fewer night-time symptoms, less rescue medication use, and fewer days with limited activity (all P < .01). |
| Harrington et al. [69] | RCT | Children with asthma in kindergarten up until grade 8 | Nurse-administered inhaled corticosteroids (ICS) | Morning doses of ICS, Questionnaires to measure desired outcome of asthma-related morbidity, quality of life, and health-care utilization | Unlikely, funded by EJF Philanthropies | Unclear [4] G, D, F |
46 | √ | Intervention patients reported significantly less functional limitation (42.9% vs. 73.9%, p = 0.04), adjustment to family life (23.8% vs. 56.5%, p = 0.03), and sleep loss (1.7 vs. 4.1 nights in last 2weeks, p = 0.035) than control patients at the end of the 60-days study period. There were no differences in unscheduled health-care utilization by group. |
| Janevic et al. [108] | Obs | Children with asthma mean age 7 in underserved communities | Medical–social care coordination program | Childhood Asthma Control Test to measure daytime and night-time symptoms | Possibly, Funded by Merck Childhood Asthma Network, Inc. (MCAN) | High [8] C, F |
805 | √ | At follow-up, intervention participants had 2.2 fewer symptom days per month (SD = 0.3; P < .01) and 1.9 fewer symptom nights per month (SD = 0.35; P < .01) than did the comparison group. The relative risk in the past year associated with the intervention was 0.63 (95% confidence interval [CI] = 0.45, 0.89) for an emergency department visit and 0.69 (95% CI = 0.47, 1.01) for hospitalization. |
| Levy et al. [70] | RCT | Medically underserved inner-city children aged 6–10 years | School-based asthma case management (open airways curriculum) | Student records to measure absences, hospital utilization; knowledge tests to measure student’s knowledge and skills | No indication | Unclear [3] E, F |
243 | / | Case management (CM) students had fewer school absences than their counterparts in Usual care (UC) schools (mean 4.38 vs 8.18 days, respectively) and experienced significantly fewer emergency department visits (p < .0001) and fewer hospital days (p < .05) than UC students. No such differences existed before program initiation. Replication and follow-up in year 2 showed continued significant improvements. |
| Liptzin et al. [109] | Obs | School aged children in inner-city schools | School centered asthma program “Step-Up Asthma Program” | Inhaler technique, Open Airways for School (OAS) scare and Kickin`Asthma (KA) score to measure desired outcome of asthma knowledge, Asthma control was measured with a questionnaire. | Possibly, authors received support by different organizations | High [9] I, D |
252 | / | Inhaler technique, OAS scores, and modified KA scores improved significantly from baseline to the 1-year follow-up. Students who participated in the Step-Up Asthma Program experienced decreased asthma exacerbations. Emergency department and urgent care visits, use of systemic corticosteroids, and missed school days all decreased significantly from baseline. Hospital admissions decreased significantly from baseline to the 1-year follow-up (P = .002), but baseline to 2-year follow-up was not significant (P = .2). |
| Mickel, Shanovich [110] | Obs | Children with asthma; 7–11 years of age in a Midwest metropolitan school district | Iggy and the Inhalers—an asthma education program | Children’s knowledge and family awareness of asthma management was measured with the help of test questions | Unlikely, funded by a Wisconsin State Asthma Coalition | High [10] F, I, D, G |
147 | √ | Asthma knowledge increased significantly (p < .001) between pre-test and post-test, and this increase was retained at 1-month follow-up. This program evaluation suggests that our program had a significant, sustained impact on students’ asthma knowledge |
| Moricca, Grasska [111] | Obs | Children with asthma aged 7–12 years | Screening for asthma risk status, case management | CST-ELA and CST-Math scores to measure desired outcome of academic achievements, postintervention absenteeism | No indication | Unclear [7] G |
142 | √ | Grade did emerge as a statistically significant predictor of students’ CST-Math scores with fifth to sixth grade students outperforming second to fourth grade students (p < .001). While year, gender, and the interaction of group and year failed to serve as statistically significant predictors of postintervention absenteeism (p > .05 for each), younger children (grades 2–4) missed approximately 2 more days per year than older children (Grades 5–6) 7.1 days (SE = 0.85). versus 5.1 days (SE. 0.42), p. .019. |
| Noyes, Bajorska [71] | RCT | Children with asthma aged 3–10 year | 1 dose of preventive asthma medication | Mean number of symptom free days and parent questionnaire to measure desired outcome of health serves utilization | No indication | Low [1] F |
525 | √ | The health benefit of the intervention was equal to ∼158 SFD gained per each 30-day period (P, .05) per 100 children. The programmatic expenses summed to an extra $4822 per 100 children per month. The net saving due to the intervention (reduction in medical costs and parental productivity, and improvement in school attendance) was $3240, resulting in the incremental cost-savings difference of $1583 and CE of $10 per 1 extra SFD gained. |
| Persaud, Barnett [72] | RCT | Children with asthma aged 8–12 years (mean 10,2) | School nurse-delivered asthma self-management and skills, personal peak flow meter | Devilbiss surveyor 1 Spirometer to measure Pulmonary function, 5 questionnaires (parent’s and child’s asthma knowledge, control, feeling, attitude) | Unlikely, funded in part by Health Services and Resources Administration, U.S. Public Health Service. | Unclear [3] G, F |
36 | / | Both treatment and control subjects demonstrated improvement in asthma knowledge and child health locus of control: 2.2 +/- 2.3 for the intervention and .8 +/-3.5 for the control group. The groups did not differ significantly in the magnitude of this effect. The intervention group experienced a small positive change in asthma attitude (1.4 +/- 8.7), while the control group showed a small negative change of -1.4 +/-8.1. The functional impact score was unchanged for both groups. |
| Splett, Erickson [73] | RCT | School-aged children with asthma | Enhanced asthma management, as defined in The Healthy Learners Asthma Initiative (HLAI) procedures | Daily visit log, student medication, and health records, clinic process improvements, attendance data, | Unlikely, funded by Member Organizations of the Healthy Learners Board, Controlling Asthma in American Cities | Unclear [5] H, E(13), D(14) |
1,561 | / | Control schools had significantly more total visits (p = .02) and episodic visits (p = .003) than intervention schools. No significant differences were found in attendance between control and intervention schools overall or for students with or without asthma for each of the 2 study years. From 1999–2000 to 2000–2001, attendance for students without asthma increased by 0.6% or nearly half of a day. This reached statistical significance for control (p = .04) and intervention schools (p = .02). There was no significant change for students with asthma, and a significant interaction was found between asthma status and time (p = .01). |
| Taras, Wright [112] | Obs | Children with asthma | Case management protocol | Asthma severity, medication, peak flow, case management provided, days absent | No indication | High [10] D, G, I |
1,094 | / | Students with moderate/severe asthma were more likely to receive a larger number of school nurse case management activities than students with mild asthma for all three years. Students with mild and moderate/ severe asthma who received at least one nurse case management activity in Year 1 were more likely to have an asthma medication available at school and to use a peak flow meter in Year 2. Change in absentee rate from Year 1 to Year 2, and Year 2 to Year 3, showed no significant association with nurse case management the previous year. |
| Note. Detailed risk of bias assessment: (13) Practice changes in the intervention group could not be controlled, risk of confounding factors; (14) Attendance rate might not be an appropriate tool to measure the effectiveness of an asthma initiative | |||||||||
| Trivedi, Patel [113] | Obs | Children with asthma (mean age 10,5) | Daily inhaled corticosteroid at school, supervised by their school nurse | Number of emergency department visits, hospital admissions, school absences, rescue medication use | No indication | High [10] G, I |
84 | / | Asthma-related ED visits over a 1-year period decreased 37.5%, from a pre-intervention mean of 0.8 visits to a post-intervention mean of 0.3 visits (p < 0.001). Asthma-related hospital admissions decreased from a pre-intervention mean of 0.3 admissions to post-intervention mean of 0 admissions (p < 0.001). Asthma rescue medication refills decreased by 46.3% from the pre- to post-intervention period (p = < .001). There were also non-significant declines in school absences and oral steroid use for children enrolled. |
| Smoking cessation | |||||||||
| Cameron et al. [19] | RCT | Children in grade 6 to 8 | Teacher workshop, School nurse (SN) workshop, teacher self-preparation, sn-self-preparation | Breath sample and self-reports to measure desired outcome of smoking habits | Unlikely, funded by the National Heart, Lung, and Blood Institute (NHLBI) | Low [114] |
3,972 | / | The overall smoking rate was 18.6% (95% confidence interval [CI] = 16.8%, 20.4%). Fewer than half (46.3%; 95% CI = 44.1%, 48.5%) of the students had never smoked by the end of grade 8. All 4 treatment conditions produced smoking rates that were less than the control group rate but were not significant. After adjustment for extrabinomial variation with the Pearson goodness-of-fit statistic, this model showed a significant interaction between condition and senior smoking rate (F4,84 = 3.88, P = .006). |
| Lamb et al. [67] | Obs | Pregnant African American teens aged 15–20 years | Eight group sessions “Teen fresh start” | Questionnaire and self-report to measure desired outcome of smoking behavior | Unlikely, funded by the American Nurse Foundation | High [10] G, F, D, I |
9 | / | While the number of subjects was too small to demonstrate significance, the team was encouraged to learn that five girls quit smoking and two cut down on their smoking. Descriptive analysis of results. |
| Thomson [115] | Obs | School-aged children | School-based smoking cessation programme | Questionnaire to measure | No indication | High [9] H, E |
4,505–4,999 | / | The target schools showed a reduction in smoking prevalence of 8% compared to a reduction of only 5.7% in the comparison schools. School E showed the highest percentage with a reduction of 14.1%. In this school smoking prevalence was 25.3 in 2006–2007 and only 11.2 in 2008–2009.The Department of Health (DoH) requires that stop smoking services collect and submit information on the number of smokers who remain abstinent for 4 weeks following their quit date. Although much good work in terms of health promotion was reported during the 2005–2006 pilot project, there were no 4-week quitters. During the Local Area Agreement (LAA), the quit rate rose from 0 to 24%. |
| Immunization | |||||||||
| Ferson et al. [35] | RCT | Children in Kindergarten and primary schools | Letters and leaflets + telephone calls | Immunization rate | Unlikely, funded by the Prince Henry Hospital Centenary Research Fund | Low [1] J(15) |
239 | / | Excluding children lost to follow up and those fully immunized at the start of the study, 20 (37%) of 54 were immunized following the passive intervention, and 35 (71%) out of 49 following the active intervention (P = 0.001). Receipt of the letter and leaflet was associated with an increased uptake of booster vaccination (P = 0.036). These proportions are significantly different (Yates corrected) χ2 = 10.9, P = 0.001). |
| Note. Detailed risk of bias assessment: (15) Excluding children lost to follow up | |||||||||
| Luthy et al. [116] | Obs | Children in grade 6 and 7 | Educational and incentive program | Tetanus, diphtheria, and acellular pertussis (Tdap) booster compliance rates | Unlikely, funded by Association of Pediatric nurse Practitioners and Wyeth Pharmaceutical Company | High [10] G, I |
958 | / | The compliance rate expanded from 4% to 57% during a 4-week intervention program. Notably, the Tetanus, diphtheria, and acellular pertussis (Tdap) immunization compliance rate in the previous year (2008) was 54%. Researchers concluded that the intervention did not improve compliance rates significantly. |
| Toole and Perry [117] | Obs | High risk-students in inner-city schools | Immunization audits + immunization at school at no cost | Immunization rate | No indication | High [8] I |
2,222 | / | Immunization compliance rates have gone from an average of 64% to an average of 97%. An audit of 2,222 kindergarten records performed 5 years after the intervention indicated that less than 1% had no immunization records on file, only 2% needed immunizations, and less than 3% were out of compliance. |
| Vernon, Conner [118] | Obs | School-aged children | A: inviting immunization-deficient children; B: permission slips; C: health education program | Immunization rate | No indication | Unclear [7] E |
5,636 | / | Using an average of 38 hours of school nurse time, Method A succeeded significantly better than Method B in immunizing more immunization-deficient children and raising immunization levels, while giving fewer unnecessary immunizations. Method C did not produce significant improvement of immunization levels. |
| Sexually transmitted Virus Prevention | |||||||||
| Borawski et al. [74] | RCT | Children in 9th and 10th grade high schools | Be Proud! Be Responsible (BPBR) curriculum taught by school nurses and teachers | Questionnaires to measure desired outcomes of knowledge, efficacy, participants’ beliefs, perceived peer beliefs, and behavioral intentions | No indication | Unclear [5] E, J(16), G |
1,357 | / | Both groups reported significant improvements in Human immunodeficiency virus (HIV)/ Sexually transmitted infections (STI)/condom knowledge immediately following the intervention, compared to controls. Yet, those taught by school nurses reported significant and sustained changes (up to 12months after intervention) in attitudes, beliefs, and efficacy, whereas those taught by health education teachers reported far fewer changes, with sustained improvement in condom knowledge only. |
| Grandahl et al. [75] | RCT | Teenagers 16 years of age | Specific Human papillomavirus (HPV) education guided by Health belief Model (HBM) | Questionnaire based on HBM to measure desired outcome of health behavior, beliefs, knowledge awareness | No indication | Low [1] D(17) |
741 | √ | The intervention had a significant effect on HBM total score (p = 0.003), (i.e., the students perceived more benefits of vaccination, perceived themselves to be at increased risk for an HPV infection or HPV-related disease, considered HPV-related disease a severe threat and perceived fewer barriers against HPV vaccination), with a 2.559 points higher score for the intervention compared to the control group. |
| Note. Detailed risk of bias assessment: (16) Only 25% of the classes could be randomly assigned to school nurses, reducing the sample size and power to detect smaller intervention effects; sample size of teacher-led classrooms was not large enough; (17) It is questionable if questionnaires on beliefs and intentions are the method of choice to measure health behavior | |||||||||
| Teenage pregnancy | |||||||||
| Chen et al. [76] | Obs | Pregnant students | Monthly visits to the school nurse (nutrition, infant care, father of baby, finance, family support, future plans, education… | Birth weight and parental care was measured by conducting month prenatal care began and frequency of visits | No indication | High [8] D, E |
578 | / | The program effects on birth weight have two pathways. To test the direct effect, a two-tailed, paired t test was applied to compare the difference of birth weight between cases and controls (M = 27.6g, SD = 864.7g) and the result was not statistically significant (t (287) = 0.543; P>0.05). However, the finding showed a higher mean birth weight (27.8g) for cases than for controls. |
| Allergies | |||||||||
| Spina, McIntyre [79] | RCT | Children (mean age 15 years) diagnosed with a life-threatening allergy + auto-injectable epinephrine | Education (for intervention and control), showing school nurse their epinephrine | Periodic checks and expiry checks | No indication | Unclear [4] G, E(18) |
77 | / | No significant differences were found between the intervention and control groups in the proportion of students who had epinephrine available during the initial check (x2 = 1.63, df = 1, p = .2) or the final check at the end of the study (x2 = 1.73, df = 1, p = .189). In the intervention group, all participants who had unexpired epinephrine during the first check continued to have current epinephrine, while one person with expired epinephrine on the first check had acquired current epinephrine during the final check (p < .01). For the control group, of the 21 participants who reported having unexpired epinephrine during the first check, 5 participants had expired epinephrine during the final check. |
| Nutrition | |||||||||
| O’Donnell et al. [77] | Obs | Children in Kindergarten to grade 6 | Educating teachers and offering mini grant materials | Knowledge test on nutrition for students to measure desired outcome of effectiveness of mini grant materials | No indication | High [10] D, E, F, I, G |
1,106 | / | In summary, most of the classroom teachers used the nutrition resource materials, and it would appear that the availability of these nutrition resource materials caused an increase in time spent on nutrition education. |
| Alcohol use prevention | |||||||||
| Werch, Carlson [80] | RCT | Children in grade 6–8 (mean age 12,2 years) in inner-city school | STARS program (Start Taking Alcohol Risks Seriously) | Alcohol use, Alcohol consumption patterns, negative consequences experienced during drinking | Unlikely, funded in part by National Institute on Alcohol Abuse and Alcoholism | Low [2] G |
138 | / | A significant difference was found on heavy alcohol use with intervention subjects showing a reduction and control subjects an increase in heavy drinking (t = -2.33, I20dJ; p = .02). No differences were found between groups on other alcohol use measures. |
| Note. Detailed risk of bias assessment: (18) The educational intervention available to both the control and the intervention group to ensure the safety of students. The education may have had an impact on increasing the likelihood that students would carry epinephrine. | |||||||||
| Hearing screening | |||||||||
| Sekhar et al. [119] | Obs | Children in Kindergarten, 1st-3rd grade; adolescents in grade 7 and 11 | High-frequency screen and PA-screen | PA-screen to measure low-frequency, conductive hearing losses; high-frequency screen for adolescent hearing loss | Unlikely, funded by Academic Pediatric Association and Child Health Bureau | High [10] G(19), D(20), F, J(21) |
282 | / | Five participants (2%) were referred on the Pennsylvania school screen, and 85 (30%) were referred on the high-frequency screen. Of the 48 who returned for gold standard testing with audiology, hearing loss was diagnosed in 9/48 (19%). Sensitivity of the Pennsylvania and high frequency screens were 13% (95% confidence interval [CI] 0–53%) and 100% (95% CI 66–100%) respectively. |
| Cardiovascular Health | |||||||||
| Harrell et al. [82] | RCT | Elementary school children aged 7–12 years | Classroom-based and risk-based interventions (nutrition, physical activity and smoking) | Questionnaires to measure desired outcome of knowledge, attitude and physical activity; Health outcome was measured with BMI, cholesterol level, blood pressure, aerobic power and skinfolds | Unlikely, funded by the National Institute for Nursing Research | Unclear [3] F, E |
2,109 | √ | Total knowledge in the classroom-based intervention schools was significantly greater than that in the control schools (7.86; 95% CI = 3.32, 12.40). The physical activity score improved significantly only in the risk-based schools (3.87; 95% CI = 1.35, 6.39). There were statistically significant differences among the 3 groups in regard to changes in cholesterol (P< .01), but only the classroom-based approach reduced mean cholesterol significantly more than in the control group. Adjusted differences among the groups were nonsignificant for systolic blood pressure but were significant for diastolic blood pressure (P = .03). Both the classroom-based and risk-based groups exhibited a significantly smaller increase in diastolic blood pressure than the control group. |
| Psychosomatic headaches | |||||||||
| Larsson and Carlsson [83] | RCT | Children aged 10–15 | Nurse-administered relaxation training | Headache diary to measure headache free days | No indication | Low [2] G |
26 | / | Nine pupils (69%) who were treated with relaxation training had achieved a clinical improvement level (of at least 50%), whereas only one subject (8%) in the no-treatment control condition had attained such an improvement level, a difference that was highly significant, x2(1) = 10.40, p < .001. Although a small improvement was noticed in the no-treatment control group at the 6-month follow-up, the difference between the two treatment conditions was still significant, x2 = 3.94, p < .05. Pearson product-moment correlation analysis revealed a nonsignificant association between children’s age and their headache (pre—post) improvement (r = .07). |
| Diabetes | |||||||||
| Izquierdo et al. [84] | RCT | Children with diabetes aged 5–14 years | Usual care + a videoconference between school nurse, child, and diabetes team every month. | Hemoglobin A1c to measure the long-term glycaemic control and Pediatric Quality of Life (PedsQL) to measure quality of life | No indication | Low [2] G |
41 | / | There was a significant difference in slopes between the telemedicine and usual care groups during the first 6 months (P < .02). A1c values increased from baseline to 6 months for students in the usual care group (not statistically significant) but decreased in the telemedicine cohort (P < .02), and the improvement was maintained over the next several months. No significant differences in slopes, or within-group slopes were observed after the 6-month point. |
| Note. Detailed risk of bias assessment: (19) Statistically, the small number of adolescents presenting for gold standard testing resulted in wider confidence intervals around the estimates of sensitivity and specificity; (20) Time lapse between two screenings too big; (21) Expectation bias | |||||||||
| Nguyen, Mason [85] | RCT | Children with high levels of HbA1c | Insulin glargine, insulin aspart, OneTouch Ultra glucometer, access to the GlucoMON system | Blood glucose records during school hours; Hemoglobin A1c (HbA1c) level and BMI (to measure weight gain) | Unlikely, funded by investigator-initiated grant Rubina Heptulla from Sanofi-Aventis | Unclear [4] G, F, J(22) |
36 | √ | The HbA1c level remained unchanged in the control group but was decreased significantly in the intervention group. For the intervention group, the rate of hypoglycemia (BG<59 mg/dL) was 0.86 +/-0.55 episode/patient-week. No data of hypoglycemia in control group. There was no difference in BMI between the 2 groups either before or after the 3-month study period. There was no correlation between the change in BMI and the change in HbA1c level in the intervention group (r = 0.24). |
| Teasing and Bullying | |||||||||
| Vessey and O’Neill [78] | Obs | Children with diabetes aged 5–14 years | Identification of at-risk students, web-based program to build resiliency, biweekly support/discussion group | Child-Adolescent Teasing Scale (CATS) measuring 4 components of teasing, Pediatric Symptom Checklist (PSC) measuring parent’s perception of psychological functioning, Piers-Harris Children’s Self-concept Scale (PHCSCS) measuring self-concept | Unlikely, funded by Deborah Munroe Noonan Memorial Research Fund | High [10] I, E |
65 | / | Statistically significant, positive differences were noted in students’ total scores on the CATS (t = 3.432, p = .001) and PHCSCS (t = 2.546, p = .007). These results imply that the participants, after completing the study intervention, perceived that they experienced fewer bothersome peer interactions and that they felt better about themselves, as reflected in their view of their self-concepts. Scores on the PSC, reflective of parental assessments of their children’s global psychosocial functioning, did not differ significantly following the intervention |
| Hygiene | |||||||||
| Kimel [120] | Obs | Children in Kindergarten and 1st grade | Handwashing program | Absentee rates | No indication | High [8] E, F |
199 | / | After the intervention, absenteeism was significantly higher among non-participants. Percentages of students absent because of flu-like illness in on-participating classes were approximately double those of participating classes. Chi-square values were significant at the p = 0.05 level: x2 (1, N = 199) = 22.225, p = .001 |
| Morton and Schultz [121] | RCT | Children in Kindergarten to 3rd grade | A 45-minute ‘‘Germ Unit” and use of alcohol gel | Communicable illnesses, vacations, respiratory-, gastrointestinal illnesses and days absent | Unlikely, funded by Maine Administrative School District | Low [1] D |
253 | / | Using McNemar’s test for dichotomous variables with paired subjects, significantly fewer children became ill while using the alcohol gel as an adjunct to regular handwashing than when using regular handwashing only (chi square 5 7.787; p 5 .0053). The odds of being absent due to infectious illness were reduced by 43% with the adjunct use of the alcohol gel. Fewer children were absent in total during phase two. |
| Note. Detailed risk of bias assessment: (22) No Blood glucose records were available for the control group, because these subjects did not bring their BG logbooks to their visits as required | |||||||||
| Studies with mixed outcomes | |||||||||
| A. Challenging behavior | |||||||||
| Buckland et al. [122] | Obs | Children aged 4–15 (mean 8) | School nurse-led interventions (group work, class work, partnership work) | SDQ (parent and teacher perspective) to measure desired outcome of hyperactivity, peer problems, conduct, emotional symptoms and prosocial behavior | No indication | High [10] G, F, E, C, I |
6 | √ | Changes in Total difficulty score (TDS) of 3 or more were assumed to be clinically meaningful. Based on this, all six children were reported to have improved (clinically meaningful) according to either their parents or their teacher. However, in three cases, the teacher believed that children had deteriorated marginally (by two points in each case). The mean improvement in parents TDS ratings was 5.6 and in teacher rating 1.3. |
| Krug et al. [86] | RCT | Children in areas with high rates of crime (Kindergarten to grade 5) | PeaceBuilders | Number of school nurse visits to measure desired outcome of level of violence | No indication | High [10] E, D, F, G, A, B |
3,899 | / | When the data were aggregated across the intervention schools, the weekly rate of visits for all reasons per 1,000 student days decreased by 12.6% (P < .001). The patterns for injury-related visits were the same as the patterns for visits for all reasons. Rates of confirmed fighting-related injuries did not change significantly in the intervention schools but increased 56.0% (P = .01) in the control schools. |
| B. Chronic Illnesses (asthma, diabetes, severe allergies, seizures, and sickle-cell anemia) | |||||||||
| Engelke et al. [123] | Obs | Children aged 5–19 | Care Coordination (teaching, direct care, school personnel, families, referrals) | PedsQL 3.0 SF22 (asthma treatment), PedsQL 3.0 (diabetes symptoms) and PedsQL 4.0 SF15 (physical health, emotional, social functioning) | Unlikely, funded by the Kate B. Reynolds Health Care Trust | High [9] J(23), C(24), F |
114 | / | For children with asthma, there was a significant improvement in total quality of life (p < .001, Eta squared = .47), treatment scale (p < .001, Eta squared = .49) and the symptom scale (p = .001, Eta squared = .18). For children with diabetes, there was a significant improvement in the treatment barrier subscale (p = .01, Eta squared = .19). |
| C. Physical activity and mental health | |||||||||
| Hoying and Melnyk [124] | Obs | Children aged 11–13 | Creating Opportunities for Personal Empowerment (COPE), Healthy Lifestyles Thinking, Emotion, Exercise, and Nutrition (TEEN), physical activity and mental health | Healthy lifestyle belief scale, OMRONTM pedometer to measure PA, The Beck Youth Inventory (BYI-II) to measure depressive symptoms, anxiety, anger, disruptive behavior and self-concept | Possibly, Bernadette Melnyk’s company, COPE2THRIVE, disseminating the COPE program; funded by Sigma Theta Tau | High [10] F, G, I, E |
31 | / | Preadolescents who received COPE reported significant decreases in anxiety. Although there was not a statistically significant improvement in healthy lifestyle beliefs, there was a small to medium positive effect. Students demonstrated significant increases in PA. The subgroup of anxious, depressed, or low self-concept preadolescents who received the COPE intervention demonstrated significant increases in self-concept and significant decreases in anxiety and depression scores. Four out of six students who scored positive for suicidal ideation at T0 no longer scored positively for suicidal ideation at T1. |
| Note. Detailed risk of bias assessment: (23) Difficulty retrieving data from the PDA, it was not possible to determine the number of times a nurse provided a specific intervention; (24) Grades were not available for all children, all goals were not appropriate for all children | |||||||||
| D. Resilience and mixed health outcomes | |||||||||
| Olowokere and Okanlawon [125] | Obs | Vulnerable children in secondary schools | Experimental group (E)1: resilience training, E2: peer support group (basic life skill support and sharing of feelings + coping techniques) E3: E1+E2 | Adapted anxiety, depression, and self-esteem questionnaires to measure psychosocial outcomes; knowledge scores | No indication | High [8] F, G(24) |
109 | / | No significant difference in the anxiety scores of the children in the intervention group compared with the control group (M = 5.37, t 0.870, p = .386). Significant reduction in the depression score in the intervention group compared with the control group postintervention (M = -4.94, t = -2.26, p = .03). For self-esteem, the independent t-test showed a significant increase in self-esteem scores in the intervention group (M = 3.27, t = -.2.26, p = .03). A significant increase in social connection was also observed in the intervention group compared with the control group (M = 2.86, t = 3.16, p = .002). |
| Note. Detailed risk of bias assessment: (24) Study with lager power >.80 needs to be conducted to be able to generalize effectiveness of the intervention | |||||||||
*CI (Confidence interval) was described “√” and can be looked at in detail in respective study; “/” is not available.
3.6 Results based on health outcomes
3.6.1 Findings on somatic health
Among the multitude of studies there are some significant results that are worth mentioning. One RCT study [61] with a low RoB showed that when a school nurse was available the number of days a student was absent was significantly reduced (on average two days per year) compared to the control group where there was no school nurse. Other studies examining school attendance were less reliable due to significant limitations (e.g. RoB).
Asthma. The majority of school nurse research examines asthma-related interventions, some providing meaningful results. The outcome variables studied vary greatly, which complicates the comparability of the results. Often research groups investigate more than one outcome such as the quality of life [69,106], school absenteeism [70,73,106,112,113], asthma knowledge [21,70,72,109,110], severity of asthma symptoms [21,108,112], quality of life [25], academic achievements [25,111], individualized goals [25], impairments and inspiratory flow rate [107], asthma control [72,107–109], symptom-free days [68,71], medication [69,112,113], health-care utilization [69–71,113], pulmonary function [72] and clinic process improvements [73]. While the heterogeneity in asthma research is striking (e.g. various health outcomes, populations, and types of interventions), a fair number of studies are of high quality with only a few limitations. One study with good reliability (low RoB) showed that preventive asthma medication for 530 students resulted in a significant reduction in symptoms compared to the control group. In addition, there were fewer night-time symptoms and rescue medication use and more peace of mind for the children [68]. Another study showed that nurse-administered inhaled corticosteroids (ICS) resulted in significantly fewer functional limitations, better adjustment to family life and improved sleep compared to the control group [69]. Results investigating asthma case management on medically underserved inner-city children show that there was less school absenteeism among children in the intervention group compared to the control group. They also experienced significantly fewer emergency department visits and fewer hospital days. A replication and follow-up in year 2 also showed continued significant improvements [70].
Obesity. In assessing the effectiveness of school nurse-led obesity prevention studies, j = 4 references with low risk of bias were of significance. All studies had in common that the BMI score was one of the main outcome measures, but the type of interventions to reduce the BMI score differed. One intervention consisted of educational programs on nutrition, an improved environment with healthy foods and more physical activity and screening procedures [17,62], but results showed no clear advantage for children in the intervention group. Although slight reductions in BMI were found, education and environmental strategies had no effect on BMI compared to the control group. Another intervention consisted of integrated health education for teachers and nutrition counselling for parents [63]. Risk of bias was unclear for this study due to lack of blinding and failure to adequately control confounding, so that results may be less reliable. However, results showed that overweight children achieved a significant reduction in weight after two years compared to the control group. School grades deteriorated in both groups, but the deterioration was less dramatic in the experimental group. In a third intervention conducted in 2013 [64] and replicated three years later [64,65], computerized cognitive behavioral counselling and an after-school physical activity program were implemented. In addition to BMI scores, diet, physical activity, sedentary behavior, self-efficacy, and perceived barriers were measured. Results showed no significant changes in BMI, body fat and waist circumference compared with control schools. A different way of looking at obesity prevention is to increase physical activity. One study investigated the impact of a Kids N Fitness intervention, with 45-minute physical activity sessions, nutrition education and wellness activities [66]. Children were asked to complete a questionnaire about their diet and anthropometric measures were collected. The study had a low risk of bias and the results showed that the intervention (delivered by school nurses) had a significant impact on BMI, sedentary behavior in boys and increased physical activity behavior in girls.
Diabetes. In assessing the effectiveness of school nurse-led diabetes management interventions, two references with low [84] and unclear [85] risk of bias were significant. One study used the hemoglobin A1c (HbA1c) value to measure long-term glycemic control. Results showed that monthly videoconferences between school nurse, child, and diabetes team showed significant improvements in the first 6 months. However, no further significant improvements were observed after the 6-month mark [84]. In the second study, blood glucose levels, HbA1c and BMI were measured and compared between experimental and control groups. Results showed that the HbA1c level remained unchanged in the control group but was significantly lower in the intervention group [85]. Neither group showed a significant change in BMI. Other investigated health outcomes such as teasing and bullying [78], resilience [125] and hyperactivity and peer problems [126] were not reliable due to limitations.
Sexually transmitted illnesses. Research groups that have set out to study sexually transmitted illness (STI) prevention interventions are consistent in that the interventions consist of educational programs for students. The outcomes measured by questionnaires relate to knowledge, beliefs, and behavioural intentions [74,75]. Despite the lack of adequate follow-up, both studies showed significant improvements in knowledge, attitudes and beliefs compared to the control group.
Vaccination. All studies on vaccination used immunisation rates as an outcome measure. Study interventions ranged from information brochures [35] to educational programmes [116] to free vaccination programmes [117,118] and results showed improved immunization rates across all studies.
Smoking. A reliable study on smoking cessation showed that properly educating teachers and school nurses had a significant impact on lowering smoking among school children [19]. Other studies examining smoking habits relied on self-reported questionnaires which however tends to lead to distortion [115,127].
3.6.2 Findings on mental health
There are several studies that examine the impact of school nurse-led interventions on mental health. Only two studies were considered adequate for assessing the effectiveness of school nurse-led programs, since the others showed limitations that could affect the validity of the results.
Anxiety. One study examined the impact of a computerized cognitive therapy (cCBT) intervention on anxiety [14], the other the impact of screening and coping skill interventions on depressive symptoms [67]. Anxiety was measured with the Anxiety Scale (SCAS) and the Strengths and Difficulties Questionnaire (SDQ) and results showed a significant reduction in the total child anxiety rate after the cCBT intervention [14].
Depression. Depression and coping skills were measured using the Reynolds Adolescent Depression Scale (RADS) and the Jalowiec Coping Scale (JCS) but the risk of bias was unclear, as the study sample consisted of only 40 participants [67]. Nevertheless, the results of the RADS showed that almost 87% of the students in the intervention group experienced a reduction in depressive symptoms, compared to a 60% reduction in the students of the control group [67].
4 Discussion
With 16 reviews and 289 primary studies, the present study indicates a saturated field of research in the field of school nursing. However, in the quality analysis conducted, the opposite is observed, as the number of high quality and meaningful studies must be considered low. First, it is striking that there is no consistently established classification system of school nursing terms, which is why research is based on individual views of the effectiveness of school nurses. This results in a wide collection of literature that makes a judgment about the effectiveness of the school nurse very difficult. The present paper presents a standardized classification of school nursing work fields according to their approaches and strategies in their goals to make the school a health promoting environment. In addition, results of this paper will be discussed against the background of qualitative limitations, followed by an outlook for research in the field of school nursing.
4.1 Barriers in assessing the effectiveness of the school nurse
School nursing research faces many hurdles that need to be identified and discussed. The coverage ratio of school nurses in schools has a major impact on the effectiveness of school nurses in schools and has so far been inadequately represented in impact analyses. The background to this assumption is a study by Paterson and Zderad [128] who indicate that the supply key could highly impact successful care taking. Their results show that the key to successful patient care is the relationship between the nurse and the patient [128]. This humanistic theory can be applied to the school setting, which increases the importance of the school nurse’s supply key in schools. This assumption is supported by researchers who showed that smaller nurse-to student ratio lead to better student outcomes [129]. The recommended nurse-to-student ratio is 1:750 according to the Centers for Disease Control and Prevention (CDC) but hardly ever realized in most schools across America [55]. The effect of the coverage key on a school nurse intervention has so far been an understudied aspect and may be a relevant variable in evaluating the effectiveness of school nurse interventions.
A further hurdle in school nurse research is the ethical aspect of school nurse interventions. It is hardly ethical that children with high care needs are assigned to the control group and do not receive any intervention. On the other hand, the lack of a control group leads to a severe loss of study quality [44,101].
Furthermore, it is difficult to attribute the effectiveness of school nurse to a single intervention. Instead, a variety of factors may play a role that could influence the effectiveness of the school nurse intervention. Excluding confounding variables is nearly impossible in the school setting and in the research field of interpersonal interactions but a strict quality criterion according to the GRADE guidelines. The crux of the matter is whether school nurse research can find a way to satisfy both the holistic nature of school nurse work and meet the scientific criteria. Results show that this is possible in certain niches of school nurse activities. For example, school-nurse led immunization projects [35] and hygiene projects [121] show great success. This is especially important in a time of global pandemic, where high immunization rates are crucial for the overall health of society. In light of these findings preventative measures (aspect 3) through immunization and hygiene interventions by school nurses may be a future area of focus for school nurse efficacy analyses.
In contrast, studies focusing on the increasing trend of obesity, do not yet show sufficiently clear evidence in favor of appointing school nurses. This may be because measuring BMI is not a satisfactory way of assessing the body weight of children and adolescents, which naturally increases with age [17], but also that underlying variables such as depression or family difficulties (low socio-economic status) allied with poor nutritional understanding may be the underlying causes of obesity. This raises the interesting question of whether the increasing trend towards overweight can be reversed by education [65] (aspect 1) and physical activity programs [124] (aspect 3), or whether overweight children have other underlying problems, such as mental issues (aspect 2), which sometimes go unrecognized for a long time. For example, if children are already overweight, they are often bullied by their peers, which in turn puts the child under a lot of emotional stress, potentially causing mental health problems. Escaping this cycle and intervening early through preventive measures is a major challenge.
There are few well-designed studies examining mental health in school children. The reason for this needs to be explored in school nurse research. One reason might be that mental illnesses are very complex and take a variety of forms. Depending on the type and severity of the illness, effective treatment, which has to be tailored to the individual’s needs, often takes many years. On the other hand, the effectiveness of preventive measures can only be measured in long-term studies and research resources are often insufficient [130]. Furthermore, it is noticeable that in some studies the control group does not receive a pure placebo and screening procedures are often applied, which could indeed amount to an intervention effect [14,67]. This could possibly explain the lack of any significant difference between the control and experimental group [67]. Another difficulty in measuring mental health interventions is ensuring allocation concealment and blinding. Unlike medical trials, where a group may be given a placebo drug, in school nurse research it is obvious when a group is not receiving an intervention [67]. Attempts have been made to minimize this bias by randomly assigning whole schools to an experimental or control group [65], although this runs the risk of studying geographically or socio-economically disparate groups. Another difficulty in assessing the effectiveness of school nurses in dealing with mental health may be the different levels of qualification for the otherwise medical-oriented school nurse work. How and whether the school nurse has received specialized training differs in each research project, making comparisons downright impossible.
Research groups focusing on the implementation of asthma-care-related interventions for school children face other challenges. Here, the high degree of heterogeneity in these studies is striking and the research pool has so far been inconsistent regarding the measurement tools, interventions or populations studied. However, asthma research has a major advantage in efficacy analyses, namely the close proximity to medicine, where interventions are somewhat more controlled through the administration of medication by the school nurse, for example nurse-administered inhaled corticosteroids (ICS) [69]. Likewise, diabetes studies show promising results in that Hemoglobin A1c can be controlled by school nurses and the values to be measured (e.g. blood glucose level) are largely free of possible bias. Researchers are taking advantage of this fact and study results show that school nurses are of great benefit in improving diabetes management in children [84,85].
4.2 Effectiveness of school nurse interventions
In the presents paper the authors have examined the effectiveness of the school nurse. Based on a classification of school nurse strategies and approaches, the effectiveness of the school nurse was evaluated from two of the three aspects (see Fig 7), namely from the standpoint of medical health care interventions (aspect 2) analyzing the effectiveness of the school nurse for children suffering from asthma, diabetes, obesity, anxiety, depression, and students smoking, and also from the standpoint of health promotion (aspect 3) analyzing the effectiveness of the school nurse in combating sexually transmitted diseases (STD) and increasing vaccination rates. The evaluation of school-based interventions included a quality assessment. Present findings are largely consistent with findings by other researchers across the globe who have previously criticized the lack of methodological quality and therefore the lack of robust, meaningful results in this field [3,39]. The main point of criticism is the paucity of reliable, evidence-based, quantitative data using randomized controlled trial designs [39,40,47]. The present paper acknowledges this criticism and therefore presents a more nuanced discussion. Results of the present work show that there are indeed meaningful studies that are evidence-based with randomized controlled trial designs that cover a variety of health outcomes [17,19,35,38,61–67,71,72,75,79,80,82–85,121,131]. However, school nurse research lacks reliability because for most of the respective health outcomes no comparative studies were identified through our research findings. Contrary to the opinion of other researchers [3,39], the present paper allows conclusions about the effectiveness of the school nurse for students with asthma and diabetes. There are compelling studies that confirm the effectiveness of the school nurse in asthma care [70,71]. In the area of diabetes, the effectiveness of the school nurse can also be proven [84,85]. Results of the present work conclude that measurement methods based on physiological parameters, such as blood glucose in diabetes prevention or peak flowmeter scores in asthma care, yield more meaningful results. A possible key point could be the proximity to medical research.
Fig 7. Classification of the school nurse’s working fields according to their approaches and perspectives.
Notes. Three core aspects of school health 1) health literacy, 2) medical health care, and 3) health promotion complement each other in terms of the common goal of making the school a health-promoting environment but differ in their approaches and strategies to achieve this goal.
This Overview of Reviews shows that there are some well- and many not so well-researched health outcomes in school nurse research. The general debate on quality assessment strategies and research approaches in school nurse research need to be addressed continuously. Despite scientific challenges results of the present paper speak for the implementation of school nurses, especially in countries where school nurses have not been established, such as Germany. Here, large-scale, long-term studies to evaluate the effectiveness of the school nurse in her various functions seem promising [29,132].
4.3 Methodological limitations of overviews of reviews
Overview of reviews is a suitable tool for summarizing evidence in a particular field. However, there are some methodological limitations that need to be mentioned. Although the most recent study in this overview of reviews was published in 2021 [54], it cannot be guaranteed that the compiled evidence is complete and up-to-date [133]. Furthermore, the strength of a review is only as good as the primary studies it is drawn from [40]. If relevant primary studies are missing from a review, because they were not available or could not be identified by the review team, these findings will also be missing from this paper. It is striking that school nurse research lacks adequate quality evaluations, for both primary studies and reviews. Reviews included in this paper could not meet the strict guidelines of the AMSTAR-2 criteria, which is why the quality rating had to be adjusted downwards in order to still allow a determination about the quality of the reviews. This change in quality rating is not validated and risks biasing the results. For future research in educational and psychological research, there is a need for quality assessment tools that includes quality requirements that can be realistically met by researchers in educational or psychological contexts.
Studies with study designs other than RCTs or Obs were excluded from this study due to high methodological demands. It is worth considering whether studies with other study designs (e.g., qualitative study designs) provide relevant results that could not meet the strict qualitative guidelines of this study but nevertheless contribute meaningful information to school nurse research on the effectiveness of school nurses.
Another problem in the methodology of overview of reviews is the scope of the included primary studies which deviates from the subject-matter of the overview of reviews, sometimes dramatically. Ballard and Montgomery refer to this problem as "scope mismatch" [133]. In this overview of reviews, all primary studies included in each review were listed and tabulated. It is debatable whether the decision to include all primary studies adds value to the results.
4.4 Additional strengths and limitations of this overview of reviews
This is the first overview of reviews on the effectiveness of school nurses and undertakes a detailed analysis of studies for both primary studies and reviews. It shows that there is a clear need for a rigorous examination of the evidence on school nurses and a critical appraisal of the quality of research. All reviews dealing with the effectiveness of school nurses were included in this paper, but additional recent primary studies were not included. This paper is based on a comprehensive search, rigorous selection and data extraction and contains an assessment of the risk of bias of the included studies. Risk of bias in this study was limited to RCTs and Obs. This paper conducted a detailed analysis of current research on the effectiveness of school nurses and provides a sound basis for future research.
However, there are several limitations to this overview of reviews. The quality of reviews included was disappointing, as the database of primary studies does not allow for meta-analyses. A large number of the primary studies failed to provide convincing evidence on the effectiveness of school nurses. A precise assessment of the body of evidence for each health outcome was not possible due to lack of data (e.g. confidence interval). It should also be noted that the majority of the studies do not specify the ratio between school nurses and children. The supply key could be a possible confounding variable that cannot be controlled due to the absence of more information on this point. Furthermore, it should be mentioned that in multifaceted interventions it is not possible to determine which components are responsible for the observed effects. This is a fundamental problem of school nurse research. Additionally, the lack of a classification system of school nursing terms also effects this paper. Future research projects should choose their approach based on the classification system presented so that study designs can be developed based on the classification system. The final limitation is that the wealth of literature provides a sense of the effectiveness and relevance of the school nurse concept, while yet not being sufficient for policy decision purposes.
However, it is worth mentioning that in this overview of reviews the circle of evidence is closed by linking all sources of evidence together—even literature of lower quality or with less important interventions are included in the scientific discourse [134].
5 Conclusions
It is clear that school nurses play a key role in improving the health of children with asthma and diabetes. Research results on the effectiveness of school nurses in the context of combating obesity is less certain and calls for more conclusive research. The analysis of the overviews shows that the quality of the included primary studies is poor (few RCT and Obs). The evaluation of the primary studies shows that variables such as blood glucose or asthma labeling led to higher quality results. This gain in knowledge is invaluable for policy planners and scientists.
5.1 Conclusions for policy planners
The concept of the school nurse is known worldwide, although it is implemented differently in each country, even in each school. Differences relate to school nurse training, staffing ratios, qualifications and responsibilities. The heterogeneous deployment of the school nurse and differences in the implementation of the studies (e.g. school nurse as part of regular care vs. school nurse as part of a research project) complicate the comparability of study results. Nevertheless, our study shows the effectiveness of the school nurse for children with asthma and diabetes. In order to elevate the school nurse to a permanent component of standard medical care, evidence-based results in different areas of children’s mental and physical health are needed. This paper represents an initial contribution and recommends further evaluation of the effectiveness of the school nurse in light of existing studies.
Areas that have been insufficiently studied or cannot demonstrate evidence of such effectiveness are those dealing with mental health or problems associated with children from low socioeconomic backgrounds. The reasons for this lacuna need to be identified in future studies. One reason for the insufficient number of studies could be that studies on mental health are lengthy and costly, and they also do not meet the strict qualitative standards of research (RCTs or Obs). For ethical reasons, a control group often cannot be justified, and the practicablity of a control group in mental health studies is in most cases not implementable (e.g. lack of allocation concealment, lack of blinding).
Research groups studying school nurse effectiveness with respect to mental health or social inequity should consider setting other qualitative standards, such as including qualitative study designs in evaluating school nurse effectiveness. Policy planners should be aware of the practicablity and implementability of studies in these areas so as not to overlook the potential effectiveness of school nurses.
5.2 Conclusions for scientists
Randomized clinical trials certainly have their place, but voices from the social research community (e.g., APA) are growing louder, arguing that researchers would get better results if they used other methods as well (Clay, 2010). Over the past two decades, a movement towards alternative guidelines for the design and evaluation of complex interventions has emerged from the Medical Research Council (MRC). These guidelines are intended to help researchers choose appropriate methods, make the design of evaluations understandable, and weigh the findings from intervention studies in light of methodological and practical limitations. The authors of this paper argue that school nurse research should also engage with the MRC guidelines with a view to standardizing school nurse research as well as to establishing universal standards of school nurse research. Thus, in addition to RCTs and Obs, studies with other study designs can be integrated into the scientific discourse and provide an evidence-based contribution to the field of school nurse research.
Supporting information
(DOCX)
(DOCX)
(DOCX)
(ENL)
(ENL)
Data Availability
All relevant data are within the paper and its Supporting information files.
Funding Statement
SP and DM 01EL2025A (SP) 01EL2025B (DM) Bundesministerium für Bildung und Forschung (BMBF) https://www.bmbf.de NO - The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Godson R. Getting it right for children, young people and families. Community Practitioner. 2012;85(4):13–4. [PubMed] [Google Scholar]
- 2.Schroeder K, Malone SK, McCabe E, Lipman T. Addressing the social determinants of health: A call to action for school nurses. The Journal of School Nursing. 2018;34(3):182–91. doi: 10.1177/1059840517750733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Best NC, Oppewal S, Travers D. Exploring School Nurse Interventions and Health and Education Outcomes: An Integrative Review. J Sch Nurs. 2018;34(1):14–27. doi: 10.1177/1059840517745359 . [DOI] [PubMed] [Google Scholar]
- 4.Green R, Reffel J. Comparison of administrators’ and school nurses’ perception of the school nurse role. The Journal of School Nursing. 2009;25(1):62–71. doi: 10.1177/1059840508324248 [DOI] [PubMed] [Google Scholar]
- 5.Stockman TR. Different expectations can lead to confusion about the school nurse’s role. British Journal of School Nursing. 2009;4(10):478–82. [Google Scholar]
- 6.Hilli Y, Pedersen G. School nurses’ engagement and care ethics in promoting adolescent health. Nursing ethics. 2021;28(6):967–79. doi: 10.1177/0969733020985145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Whitehead D. The health-promoting school: what role for nursing? Journal of clinical nursing. 2006;15(3):264–71. doi: 10.1111/j.1365-2702.2006.01294.x [DOI] [PubMed] [Google Scholar]
- 8.Crabtree E, Davis T. Marketing the role of the school nurse. British Journal of School Nursing. 2009;4(8):395–8. [Google Scholar]
- 9.Hoekstra BA, Young VL, Eley CV, Hawking MK, McNulty CA. School Nurses’ perspectives on the role of the school nurse in health education and health promotion in England: a qualitative study. BMC nursing. 2016;15(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ernstmann N, Bauer U., Berens E. M., Bitzer E. M., Bollweg T. M., Danner M., et al. DNVF Memorandum Gesundheitskompetenz (Teil 1)–Hintergrund, Relevanz, Gegenstand und Fragestellungen in der Versorgungsforschung. Das Gesundheitswesen. 2020:82(07), e77–e93. [DOI] [PubMed] [Google Scholar]
- 11.Kostenius C. School Nurses’ Experiences With Health Dialogues: A Swedish Case. The Journal of School Nursing. 2021:10598405211022597. doi: 10.1177/10598405211022597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wachtlin M. Gesundheitsförderung ist (nicht) gleich Prävention. Pflegezeitschrift. 2021;74(7), 54–56.34025045 [Google Scholar]
- 13.Allen G. The impact of elementary school nurses on student attendance. J Sch Nurs. 2003;19(4):225–31. Epub 2003/07/29. doi: 10.1177/10598405030190040801 . [DOI] [PubMed] [Google Scholar]
- 14.Attwood M, Meadows S, Stallard P, Richardson T. Universal and targeted computerised cognitive behavioural therapy (Think, Feel, Do) for emotional health in schools: results from two exploratory studies. Child Adolesc Ment Health. 2012;17(3):173–8. Epub 2012/09/01. doi: 10.1111/j.1475-3588.2011.00627.x . [DOI] [PubMed] [Google Scholar]
- 15.Bartfay WJ, Bartfay E. Promoting health in schools through a board game. Western journal of nursing research. 1994;16(4):438–46. doi: 10.1177/019394599401600408 [DOI] [PubMed] [Google Scholar]
- 16.Gormley JM. School nurse advocacy for student health, safety, and school attendance: Impact of an educational activity. The Journal of School Nursing. 2019;35(6):401–11. doi: 10.1177/1059840518814294 [DOI] [PubMed] [Google Scholar]
- 17.Bonsergent E, Agrinier N, Thilly N, Tessier S, Legrand K, Lecomte E, et al. Overweight and obesity prevention for adolescents: a cluster randomized controlled trial in a school setting. Am J Prev Med. 2013a;44(1):30–9. Epub 2012/12/21. doi: 10.1016/j.amepre.2012.09.055 . [DOI] [PubMed] [Google Scholar]
- 18.Gothilander J, Johansson H. School nurses’ experiences and challenges of working with childhood obesity in Northern Sweden: A qualitative descriptive study. Nordic Journal of Nursing Research. 2021:20571585211044698. [Google Scholar]
- 19.Cameron R, Brown KS, Best JA, Pelkman CL, Madill CL, Manske SR, et al. Effectiveness of a social influences smoking prevention program as a function of provider type, training method, and school risk. American Journal of Public Health. 1999;89(12):1827–31. doi: 10.2105/ajph.89.12.1827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Deitche AL, Burda AM. Management of Toxicological Emergencies in the School Setting: An Overview for School Nurses Part 2. NASN school nurse. 2022:1942602X221100213. [DOI] [PubMed]
- 21.Christiansen SC, Martin SB, Schleicher NC, Koziol JA, Mathews KP, Zuraw BL. Evaluation of a school-based asthma education program for inner-city children. Journal of Allergy and Clinical Immunology. 1997;100(5):613–7. doi: 10.1016/s0091-6749(97)70164-7 [DOI] [PubMed] [Google Scholar]
- 22.Al Kindi Z, McCabe C, Mc Cann M. School nurses’ available education to manage children with asthma at schools: A scoping review. Journal of Pediatric Nursing. 2021;60:46–57. doi: 10.1016/j.pedn.2021.01.027 [DOI] [PubMed] [Google Scholar]
- 23.Clausson E, Berg A. Family intervention sessions: one useful way to improve schoolchildren’s mental health. Journal of family nursing. 2008;14(3):289–313. doi: 10.1177/1074840708322758 [DOI] [PubMed] [Google Scholar]
- 24.Lee RL, West S, Tang AC, Cheng HY, Chong CY, Chien WT, et al. A qualitative exploration of the experiences of school nurses during COVID-19 pandemic as the frontline primary health care professionals. Nursing Outlook. 2021;69(3):399–408. doi: 10.1016/j.outlook.2020.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Engelke MK, Swanson M, Guttu M. Process and outcomes of school nurse case management for students with asthma. The Journal of School Nursing. 2014;30(3):196–205. doi: 10.1177/1059840513507084 [DOI] [PubMed] [Google Scholar]
- 26.Jordan KS, MacKay P, Woods SJ. Child maltreatment: Optimizing recognition and reporting by school nurses. NASN school nurse. 2017;32(3):192–9. doi: 10.1177/1942602X16675932 [DOI] [PubMed] [Google Scholar]
- 27.Harding L, Davison-Fischer J, Bekaert S, Appleton JV. The role of the school nurse in protecting children and young people from maltreatment: An integrative review of the literature. International journal of nursing studies. 2019;92:60–72. doi: 10.1016/j.ijnurstu.2018.12.017 [DOI] [PubMed] [Google Scholar]
- 28.Reynolds AJ, Robertson DL. School–based early intervention and later child maltreatment in the Chicago longitudinal study. Child development. 2003;74(1):3–26. doi: 10.1111/1467-8624.00518 [DOI] [PubMed] [Google Scholar]
- 29.Tannen A, Adam Y, Ebert J, Ewers M. Schulgesundheitspflege an allgemeinbildenden Schulen–SPLASH, Teil 2: Implementationsbegleitung und Wirkungsanalyse. 2018.
- 30.Bergren M, Murphy E. The best of the web for school health. The Journal of school nursing: the official publication of the National Association of School Nurses. 1997;13(5):36–7. doi: 10.1177/105984059701300506 [DOI] [PubMed] [Google Scholar]
- 31.Schroeder K, Travers J, Smaldone A. Are School Nurses an Overlooked Resource in Reducing Childhood Obesity? A Systematic Review and Meta-Analysis. Journal of School Health. 2016;86(5):309–21. doi: 10.1111/josh.12386 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McDonald CC. Reopening schools in the time of pandemic: look to the school nurses. SAGE Publications Sage CA: Los Angeles, CA; 2020. [DOI] [PubMed] [Google Scholar]
- 33.Lee M-H, Perl DP, Nair G, Li W, Maric D, Murray H, et al. Microvascular injury in the brains of patients with Covid-19. New England Journal of Medicine. 2021;384(5):481–3. doi: 10.1056/NEJMc2033369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Morton JL, Schultz AA. Healthy hands: use of alcohol gel as an adjunct to handwashing in elementary school children. The Journal of School Nursing. 2004;20(3):161–7. doi: 10.1177/10598405040200030601 [DOI] [PubMed] [Google Scholar]
- 35.Ferson M, Fitzsimmons G, Christie D, Woollett H. School health nurse interventions to increaseimmunisation uptake in school entrants. Public Health. 1995;109(1):25–9. doi: 10.1016/s0033-3506(95)80072-7 [DOI] [PubMed] [Google Scholar]
- 36.Binder D. Herausgeberinnen und Herausgeber: Prof. Dr. Catharina Maulbecker-Armstrong FB Gesundheit, Technische Hochschule Mittelhessen Dieter Schulenberg, ehemaliger Geschäftsführer HAGE eV.
- 37.Wang LY, Vernon-Smiley M, Gapinski MA, Desisto M, Maughan E, Sheetz A. Cost-benefit study of school nursing services. JAMA pediatrics. 2014;168(7):642–8. doi: 10.1001/jamapediatrics.2013.5441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Johnston CA, Moreno JP, Gallagher MR, Wang J, Papaioannou MA, Tyler C, et al. Achieving long-term weight maintenance in Mexican-American adolescents with a school-based intervention. Journal of Adolescent Health. 2013b;53(3):335–41. doi: 10.1016/j.jadohealth.2013.04.001 [DOI] [PubMed] [Google Scholar]
- 39.Wainwright P, Thomas J, Jones M. Health promotion and the role of the school nurse: a systematic review. Journal of Advanced Nursing. 2000;32(5):1083–91. doi: 10.1046/j.1365-2648.2000.01579.x [DOI] [PubMed] [Google Scholar]
- 40.Biondi-Zoccai G. Umbrella reviews. Evidence synthesis with overviews of reviews and meta-epidemiologic studies Cham, Switzerland: Springer International. 2016. [Google Scholar]
- 41.Zawacki-Richter O, Kerres M, Bedenlier S, Bond M, Buntins K. Systematic reviews in educational research: Methodology, perspectives and application: Springer Nature; 2020. [Google Scholar]
- 42.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic reviews. 2015;4(1):1–9. doi: 10.1186/2046-4053-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. bmj. 2017;358. doi: 10.1136/bmj.j4008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhang Y, Akl EA, Schünemann HJ. Using systematic reviews in guideline development: the GRADE approach. Research synthesis methods. 2019;10(3):312–29. [DOI] [PubMed] [Google Scholar]
- 45.Booth A, Clarke M, Dooley G, Ghersi D, Moher D, Petticrew M, et al. The nuts and bolts of PROSPERO: an international prospective register of systematic reviews. Systematic reviews. 2012;1(1):1–9. doi: 10.1186/2046-4053-1-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hong QN, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, et al. The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Education for Information. 2018;34(4):285–91. [Google Scholar]
- 47.Schünemann H, Brożek J, Guyatt G, Oxman A. Handbook for grading the quality of evidence and the strength of recommendations using the GRADE approach. Updated October. 2013;2013. [Google Scholar]
- 48.Schmitt S, Görres S. [School nursing in Germany?—A review about tasks and roles of School Nurses]. Pflege. 2012;25(2):107–17. Epub 2012/04/05. doi: 10.1024/1012-5302/a000186 . [DOI] [PubMed] [Google Scholar]
- 49.Stefanowicz A, Stefanowicz J. The role of a school nurse in the care of a child with diabetes mellitus type 1-the perspectives of patients and their parents: Literature review. Slovenian Journal of Public Health. 2018;57(3):166. doi: 10.2478/sjph-2018-0021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Turner G, Mackay S. The impact of school nurse interventions: Behaviour change and mental health. British Journal of School Nursing. 2015;10(10):494–506. doi: 10.12968/bjsn.2015.10.10.494 Language: English. Entry Date: 20151230. Revision Date: 20151231. Publication Type: Article. [DOI] [Google Scholar]
- 51.Stock JL, Larter N, Kieckehefer GM, Thronson G, Maire J. Measuring outcomes of school nursing services. J Sch Nurs. 2002;18(6):353–9. doi: 10.1177/10598405020180060801 . [DOI] [PubMed] [Google Scholar]
- 52.Tanner A, Miller WR, Gaudecker Jv, Buelow JM. An integrative review of school-based mental health interventions and implications for psychogenic nonepileptic seizures. The Journal of School Nursing. 2020;36(1):33–48. doi: 10.1177/1059840519854796 [DOI] [PubMed] [Google Scholar]
- 53.McClanahan R, Weismuller PC. School nurses and care coordination for children with complex needs: an integrative review. J Sch Nurs. 2014;31(1):34–43. doi: 10.1177/1059840514550484 . [DOI] [PubMed] [Google Scholar]
- 54.Guarinoni M, Dignani L. Effectiveness of the school nurse role in increasing the vaccination coverage rate: a narrative review. Ann Ig. 2021;33(1):55–66. doi: 10.7416/ai.2021.2408 [DOI] [PubMed] [Google Scholar]
- 55.Lineberry MJ, Ickes MJ. The role and impact of nurses in American elementary schools: A systematic review of the research. The Journal of School Nursing. 2014;31(1):22–33. doi: 10.1177/1059840514540940 [DOI] [PubMed] [Google Scholar]
- 56.Isik E, Isik IS. Asthma care coordination in schools by school nurses: An integrative literature review. Public Health Nurs. 2019;36(4):498–506. doi: 10.1111/phn.12610 . [DOI] [PubMed] [Google Scholar]
- 57.Yoder CM. School Nurses and Student Academic Outcomes: An Integrative Review. J Sch Nurs. 2020;36(1):49–60. doi: 10.1177/1059840518824397 . [DOI] [PubMed] [Google Scholar]
- 58.Maughan E. The impact of school nursing on school performance: a research synthesis. J Sch Nurs. 2003;19(3):163–71. doi: 10.1177/10598405030190030701 . [DOI] [PubMed] [Google Scholar]
- 59.Tilley S, Chambers M. Research in brief. A systematic review on the effectiveness of school nurse implemented mental health screening available for adolescents in schools. Journal of Psychiatric & Mental Health Nursing (Wiley-Blackwell). 2003;10(5):625–6. Language: English. Entry Date: 20050425. Revision Date: 20150711. Publication Type: Journal Article. [DOI] [PubMed] [Google Scholar]
- 60.Schroeder K, Travers J, Smaldone A. Are school nurses an overlooked resource in reducing childhood obesity? A systematic review and meta-analysis. Journal of school health. 2016;86(5):309–21. doi: 10.1111/josh.12386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Long G, Whitman C, Johansson M, Williams C, Tuthill R. Evaluation of a school health program directed to children with history of high absence. American journal of public health. 1975;65(4):388–93. doi: 10.2105/ajph.65.4.388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bonsergent E, Thilly N, Legrand K, Agrinier N, Tessier S, Lecomte E, et al. Process evaluation of a school-based overweight and obesity screening strategy in adolescents. Glob Health Promot. 2013b;20(2 Suppl):76–82. Epub 2013/05/25. doi: 10.1177/1757975913483330 . [DOI] [PubMed] [Google Scholar]
- 63.Johnston CA, Moreno JP, El-Mubasher A, Gallagher M, Tyler C, Woehler D. Impact of a school-based pediatric obesity prevention program facilitated by health professionals. Journal of School Health. 2013a;83(3):171–81. doi: 10.1111/josh.12013 [DOI] [PubMed] [Google Scholar]
- 64.Pbert L, Druker S, Gapinski MA, Gellar L, Magner R, Reed G, et al. A school nurse-delivered intervention for overweight and obese adolescents. Journal of School Health. 2013;83(3):182–93. doi: 10.1111/josh.12014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Pbert L, Druker S, Barton B, Schneider KL, Olendzki B, Gapinski MA, et al. A school-based program for overweight and obese adolescents: a randomized controlled trial. Journal of School Health. 2016;86(10):699–708. doi: 10.1111/josh.12428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wright K, Giger JN, Norris K, Suro Z. Impact of a nurse-directed, coordinated school health program to enhance physical activity behaviors and reduce body mass index among minority children: A parallel-group, randomized control trial. International Journal of Nursing Studies. 2013;50(6):727–37. doi: 10.1016/j.ijnurstu.2012.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lamb J, Albrecht S, Sereika S. Consideration of factors prior to implementing a smoking cessation program. The Journal of school nursing: the official publication of the National Association of School Nurses. 1998b;14(1):14–9. [PubMed] [Google Scholar]
- 68.Halterman JS, Szilagyi PG, Fisher SG, Fagnano M, Tremblay P, Conn KM, et al. Randomized controlled trial to improve care for urban children with asthma: results of the School-Based Asthma Therapy trial. Archives of pediatrics & adolescent medicine. 2011;165(3):262–8. doi: 10.1001/archpediatrics.2011.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Harrington CB, Langhans E, Shelef DQ, Savitz M, Whitmore C, Teach SJ. A pilot randomized trial of school-based administration of inhaled corticosteroids for at-risk children with asthma. J Asthma. 2018;55(2):145–51. Epub 2017/06/09. doi: 10.1080/02770903.2017.1323915 . [DOI] [PubMed] [Google Scholar]
- 70.Levy M, Heffner B, Stewart T, Beeman G. The efficacy of asthma case management in an urban school district in reducing school absences and hospitalizations for asthma. J Sch Health. 2006;76(6):320–4. Epub 2006/08/22. doi: 10.1111/j.1746-1561.2006.00120.x . [DOI] [PubMed] [Google Scholar]
- 71.Noyes K, Bajorska A, Fisher S, Sauer J, Fagnano M, Halterman JS. Cost-effectiveness of the School-Based Asthma Therapy (SBAT) program. Pediatrics. 2013;131(3):e709–17. Epub 2013/02/13. doi: 10.1542/peds.2012-1883 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Persaud DI, Barnett SE, Weller SC, Baldwin CD, Niebuhr V, McCormick DP. An asthma self-management program for children, including instruction in peak flow monitoring by school nurses. Journal of Asthma. 1996;33(1):37–43. doi: 10.3109/02770909609077761 [DOI] [PubMed] [Google Scholar]
- 73.Splett PL, Erickson CD, Belseth SB, Jensen C. Evaluation and sustainability of the healthy learners asthma initiative. J Sch Health. 2006;76(6):276–82. Epub 2006/08/22. doi: 10.1111/j.1746-1561.2006.00112.x . [DOI] [PubMed] [Google Scholar]
- 74.Borawski EA, Tufts KA, Trapl ES, Hayman LL, Yoder LD, Lovegreen LD. Effectiveness of health education teachers and school nurses teaching sexually transmitted infections/human immunodeficiency virus prevention knowledge and skills in high school. Journal of School Health. 2015;85(3):189–96. doi: 10.1111/josh.12234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Grandahl M, Rosenblad A, Stenhammar C, Tydén T, Westerling R, Larsson M, et al. School-based intervention for the prevention of HPV among adolescents: a cluster randomised controlled study. BMJ open. 2016;6(1). doi: 10.1136/bmjopen-2015-009875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Chen SPC, Fitzgerald MC, DeStefano LM, Chen EH. Effects of a school nurse prenatal counseling program. Public Health Nurs. 1991;8(4):212–8. doi: 10.1111/j.1525-1446.1991.tb00659.x [DOI] [PubMed] [Google Scholar]
- 77.O’Donnell NL, Alles WF. School Nurse Demonstrates that Mini-Grant Funding Can Improve Elementary Nutrition Education. Journal of School Health. 1983;53(5):316–9. doi: 10.1111/j.1746-1561.1983.tb05351.x [DOI] [PubMed] [Google Scholar]
- 78.Vessey JA, O’Neill KM. Helping students with disabilities better address teasing and bullying situations: A MASNRN study. The Journal of School Nursing. 2011;27(2):139–48. doi: 10.1177/1059840510386490 [DOI] [PubMed] [Google Scholar]
- 79.Spina JL, McIntyre CL, Pulcini JA. An intervention to increase high school students’ compliance with carrying auto-injectable epinephrine: a MASNRN study. The Journal of School Nursing. 2012;28(3):230–7. doi: 10.1177/1059840511431459 [DOI] [PubMed] [Google Scholar]
- 80.Werch CE, Carlson JM, Pappas DM, DiClemente CC. Brief nurse consultations for preventing alcohol use among urban school youth. Journal of School Health. 1996;66(9):335–8. doi: 10.1111/j.1746-1561.1996.tb03414.x [DOI] [PubMed] [Google Scholar]
- 81.Sekhar DL, Kraschnewski JL, Stuckey HL, Witt PD, Francis EB, Moore GA, et al. Opportunities and challenges in screening for childhood sexual abuse. Child abuse & neglect. 2018;85:156–63. doi: 10.1016/j.chiabu.2017.07.019 [DOI] [PubMed] [Google Scholar]
- 82.Harrell JS, McMurray RG, Gansky SA, Bangdiwala SI, Bradley CB. A public health vs a risk-based intervention to improve cardiovascular health in elementary school children: the Cardiovascular Health in Children Study. American journal of public health. 1999;89(10):1529–35. doi: 10.2105/ajph.89.10.1529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Larsson B, Carlsson J. A school-based, nurse-administered relaxation training for children with chronic tension-type headache. Journal of Pediatric Psychology. 1996;21(5):603–14. doi: 10.1093/jpepsy/21.5.603 [DOI] [PubMed] [Google Scholar]
- 84.Izquierdo R, Morin PC, Bratt K, Moreau Z, Meyer S, Ploutz-Snyder R, et al. School-centered telemedicine for children with type 1 diabetes mellitus. J Pediatr. 2009;155(3):374–9. Epub 2009/05/26. doi: 10.1016/j.jpeds.2009.03.014 . [DOI] [PubMed] [Google Scholar]
- 85.Nguyen TM, Mason KJ, Sanders CG, Yazdani P, Heptulla RA. Targeting blood glucose management in school improves glycemic control in children with poorly controlled type 1 diabetes mellitus. The Journal of pediatrics. 2008;153(4):575–8. doi: 10.1016/j.jpeds.2008.04.066 [DOI] [PubMed] [Google Scholar]
- 86.Krug EG, Brener ND, Dahlberg LL, Ryan GW, Powell KE. The impact of an elementary school-based violence prevention program on visits to the school nurse. American journal of preventive medicine. 1997;13(6):459–63. [PubMed] [Google Scholar]
- 87.Foster LS, Keele R. Implementing an over-the-counter medication administration policy in an elementary school. The Journal of school nursing. 2006;22(2):108–13. [PubMed] [Google Scholar]
- 88.Rodriguez E, Rivera DA, Perlroth D, Becker E, Wang NE, Landau M. School nurses’ role in asthma management, school absenteeism, and cost savings: a demonstration project. J Sch Health. 2013;83(12):842–50. Epub 2013/11/23. doi: 10.1111/josh.12102 . [DOI] [PubMed] [Google Scholar]
- 89.Telljohann SK, Dake JA, Price JH. Effect of full-time versus part-time school nurses on attendance of elementary students with asthma. J Sch Nurs. 2004;20(6):331–4. Epub 2004/11/25. doi: 10.1177/10598405040200060701 . [DOI] [PubMed] [Google Scholar]
- 90.Van Cura M. The relationship between school-based health centers, rates of early dismissal from school, and loss of seat time. J Sch Health. 2010;80(8):371–7. Epub 2010/07/14. doi: 10.1111/j.1746-1561.2010.00516.x . [DOI] [PubMed] [Google Scholar]
- 91.Wiggs-Stayner KS, Purdy TR, Go GN, McLaughlin NC, Tryzynka PS, Sines JR, et al. The impact of mass school immunization on school attendance. J Sch Nurs. 2006;22(4):219–22. Epub 2006/07/22. doi: 10.1177/10598405050220040601 . [DOI] [PubMed] [Google Scholar]
- 92.Hawthorne A, Shaibi G, Gance-Cleveland B, McFall S. Grand Canyon Trekkers: school-based lunchtime walking program. The Journal of School Nursing. 2011;27(1):43–50. doi: 10.1177/1059840510391669 [DOI] [PubMed] [Google Scholar]
- 93.Melin A, Lenner RA. Prevention of further weight gain in overweight school children, a pilot study. Scandinavian journal of caring sciences. 2009;23(3):498–505. doi: 10.1111/j.1471-6712.2008.00651.x [DOI] [PubMed] [Google Scholar]
- 94.Sherman JB, Alexander MA, Gomez D, Marole P. Intervention program for obese school children. Journal of community health nursing. 1992;9(3):183–90. doi: 10.1207/s15327655jchn0903_6 [DOI] [PubMed] [Google Scholar]
- 95.Speroni KG, Earley C, Atherton M. Evaluating the effectiveness of the Kids Living Fit™ program: A comparative study. The Journal of school nursing. 2007;23(6):329–36. [DOI] [PubMed] [Google Scholar]
- 96.Tucker S, Lanningham-Foster LM. Nurse-led school-based child obesity prevention. The Journal of School Nursing. 2015;31(6):450–66. doi: 10.1177/1059840515574002 [DOI] [PubMed] [Google Scholar]
- 97.Wong EM, Cheng MM. Effects of motivational interviewing to promote weight loss in obese children. Journal of Clinical Nursing. 2013;22(17–18):2519–30. doi: 10.1111/jocn.12098 [DOI] [PubMed] [Google Scholar]
- 98.Robbins LB, Pfeiffer KA, Maier KS, Lo Y-J, Wesolek SM. Pilot intervention to increase physical activity among sedentary urban middle school girls: a two-group pretest–posttest quasi-experimental design. The Journal of School Nursing. 2012;28(4):302–15. doi: 10.1177/1059840512438777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Williams AD, Warrington V. Get Fit Kids: a feasibility study of a pedometer-based walking program. Bariatric Nursing and Surgical Patient Care. 2011;6(3):139–43. [Google Scholar]
- 100.DeSocio J, Stember L, Schrinsky J. Teaching children about mental health and illness: A school nurse health education program. The Journal of school nursing. 2006;22(2):81–6. [PubMed] [Google Scholar]
- 101.Houck GM, Darnell S, Lussman S. A support group intervention for at-risk female high school students. The Journal of School Nursing. 2002;18(4):212–8. doi: 10.1177/10598405020180041201 [DOI] [PubMed] [Google Scholar]
- 102.Muggeo MA, Stewart CE, Drake KL, Ginsburg GS. A school nurse-delivered intervention for anxious children: An open trial. School Mental Health. 2017;9(2):157–71. [Google Scholar]
- 103.Ramirez M, Harland K, Frederick M, Shepherd R, Wong M, Cavanaugh JE. Listen protect connect for traumatized schoolchildren: a pilot study of psychological first aid. BMC psychology. 2013;1(1):26. doi: 10.1186/2050-7283-1-26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Stallard P, Simpson N, Anderson S, Hibbert S, Osborn C. The FRIENDS emotional health programme: Initial findings from a school-based project. Child and Adolescent Mental Health. 2007;12(1):32–7. doi: 10.1111/j.1475-3588.2006.00421.x [DOI] [PubMed] [Google Scholar]
- 105.Stallard P, Simpson N, Anderson S, Goddard M. The FRIENDS emotional health programme. European child & adolescent psychiatry. 2008;17(5):283–9. [DOI] [PubMed] [Google Scholar]
- 106.Bruzzese JM, Evans D, Wiesemann S, Pinkett-Heller M, Levison MJ, Du Y, et al. Using school staff to establish a preventive network of care to improve elementary school students’ control of asthma. J Sch Health. 2006;76(6):307–12. Epub 2006/08/22. doi: 10.1111/j.1746-1561.2006.00118.x . [DOI] [PubMed] [Google Scholar]
- 107.Francisco B, Rood T, Nevel R, Foreman P, Homan S. Peer reviewed: Teaming up for asthma control: EPR-3 compliant school program in Missouri is effective and cost-efficient. Preventing chronic disease. 2017;14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Janevic MR, Stoll S, Wilkin M, Song PX, Baptist A, Lara M, et al. Pediatric asthma care coordination in underserved communities: a quasiexperimental study. American journal of public health. 2016;106(11):2012–8. doi: 10.2105/AJPH.2016.303373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Liptzin DR, Gleason MC, Cicutto LC, Cleveland CL, White MK, Faino AV, et al. Developing, implementing, and evaluating a school-centered asthma program: step-up asthma program. The Journal of Allergy and Clinical Immunology: In Practice. 2016;4(5):972–9.e1. doi: 10.1016/j.jaip.2016.04.016 [DOI] [PubMed] [Google Scholar]
- 110.Mickel CF, Shanovich KK, Evans MD, Jackson DJ. Evaluation of a school-based asthma education protocol: iggy and the inhalers. The Journal of School Nursing. 2016;33(3):189–97. [DOI] [PubMed] [Google Scholar]
- 111.Moricca ML, Grasska MA, BM M, Morphew T, Weismuller PC, Galant SP. School asthma screening and case management: attendance and learning outcomes. J Sch Nurs. 2013;29(2):104–12. Epub 2012/07/17. doi: 10.1177/1059840512452668 . [DOI] [PubMed] [Google Scholar]
- 112.Taras H, Wright S, Brennan J, Campana J, Lofgren R. Impact of school nurse case management on students with asthma. J Sch Health. 2004;74(6):213–9. Epub 2004/10/08. doi: 10.1111/j.1746-1561.2004.tb07935.x . [DOI] [PubMed] [Google Scholar]
- 113.Trivedi M, Patel J, Lessard D, Kremer T, Byatt N, Phipatanakul W, et al. School nurse asthma program reduces healthcare utilization in children with persistent asthma. J Asthma. 2017;55(10):1131–7. Epub 2017/12/06. doi: 10.1080/02770903.2017.1396473 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Stone E. J. (1985). School health research funded by the National Heart, Lung, and Blood Institute. Journal of School Health, 55(5), 168–174. [DOI] [PubMed] [Google Scholar]
- 115.Thomson H. A successful approach to reduce youth smoking in Leicestershire. British Journal of School Nursing. 2012;7(9):441–7. [Google Scholar]
- 116.Luthy KE, Thorpe A, Dymock LC, Connely S. Evaluation of an intervention program to increase immunization compliance among school children. The Journal of School Nursing. 2011;27(4):252–7. doi: 10.1177/1059840510393963 [DOI] [PubMed] [Google Scholar]
- 117.Toole K, Perry CS. Increasing immunization compliance. The Journal of School Nursing. 2004;20(4):203–8. doi: 10.1177/10598405040200040401 [DOI] [PubMed] [Google Scholar]
- 118.Vernon TM, Conner JS, Shaw BS, Lampe JM, Doster ME. An evaluation of three techniques improving immunization levels in elementary schools. American journal of public health. 1976;66(5):457–60. doi: 10.2105/ajph.66.5.457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Sekhar DL, Zalewski TR, Ghossaini SN, King TS, Rhoades JA, Czarnecki B, et al. Pilot study of a high-frequency school-based hearing screen to detect adolescent hearing loss. Journal of medical screening. 2014;21(1):18–23. doi: 10.1177/0969141314524565 [DOI] [PubMed] [Google Scholar]
- 120.Kimel L. Handwashing education can decrease illness absenteeism. The Journal of school nursing: the official publication of the National Association of School Nurses. 1996;12(2):14–6, 8. doi: 10.1177/105984059601200204 [DOI] [PubMed] [Google Scholar]
- 121.Morton JL, Schultz AA. Healthy Hands: Use of alcohol gel as an adjunct to handwashing in elementary school children. J Sch Nurs. 2004;20(3):161–7. Epub 2004/05/19. doi: 10.1177/10598405040200030601 . [DOI] [PubMed] [Google Scholar]
- 122.Buckland L, Rose J, Greaves C. Making a difference to families: tackling challenging behaviour. Community Practitioner. 2005;78(2):50–5. . Language: English. Entry Date: 20050610. Revision Date: 20150820. Publication Type: Journal Article. [Google Scholar]
- 123.Engelke KM, Guttu M, Warren MB, Swanson M. School nurse case management for children with chronic illness: health, academic, and quality of life outcomes. J Sch Nurs. 2008;24(4):205–14. Epub 2008/09/02. doi: 10.1177/1059840508319929 . [DOI] [PubMed] [Google Scholar]
- 124.Hoying J, Melnyk BM. COPE: a pilot study with urban-dwelling minority sixth-grade youth to improve physical activity and mental health outcomes. The Journal of School Nursing. 2016;32(5):347–56. doi: 10.1177/1059840516635713 [DOI] [PubMed] [Google Scholar]
- 125.Olowokere A, Okanlawon F. The effects of a school-based psychosocial intervention on resilience and health outcomes among vulnerable children. The Journal of School Nursing. 2014;30(3):206–15. doi: 10.1177/1059840513501557 [DOI] [PubMed] [Google Scholar]
- 126.Buckland L, Rose J, Greaves C. New roles for school nurses: Preventing exclusion. Community Practitioner. 2005a;78(1):16. [Google Scholar]
- 127.LAMB JM, Puskar KR, SEREIKA SM, CORCORAN M. School-based intervention to promote coping in rural teens. MCN: The American Journal of Maternal/Child Nursing. 1998a;23(4):187–94. doi: 10.1097/00005721-199807000-00005 [DOI] [PubMed] [Google Scholar]
- 128.DE PATERSON RSLV. PALLIATIVE CARE TO THE CANCER PATIENT: REFLECTIONS ACCORDING TO PATERSON AND ZDERAD ‘S VIEW. Rev Latino-am Enfermagem. 2007;15(2):350–4. [DOI] [PubMed] [Google Scholar]
- 129.Guttu M, Engelke MK, Swanson M. Does the school nurse-to-student ratio make a difference? Journal of School Health. 2004;74(1):6–9. doi: 10.1111/j.1746-1561.2004.tb06593.x [DOI] [PubMed] [Google Scholar]
- 130.Williams NJ, Beidas RS. Annual research review: the state of implementation science in child psychology and psychiatry: a review and suggestions to advance the field. Journal of Child Psychology and Psychiatry. 2019;60(4):430–50. doi: 10.1111/jcpp.12960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Bonsergent E, Agrinier N, Thilly N, Tessier S, Legrand K, Lecomte E, et al. Overweight and obesity prevention for adolescents: a cluster randomized controlled trial in a school setting. Am J Prev Med. 2013;44(1):30–9. Epub 2012/12/21. doi: 10.1016/j.amepre.2012.09.055 . [DOI] [PubMed] [Google Scholar]
- 132.Tannen A, Adam Y, Ebert J, Ewers M. Schulgesundheitspflege an allgemeinbildenden Schulen–SPLASH, Teil 1: Analyse der Ausgangslage. 2018.
- 133.Ballard M, Montgomery P. Risk of bias in overviews of reviews: a scoping review of methodological guidance and four-item checklist. Res Synth Methods. 2017;8(1):92–108. Epub 2017/01/12. doi: 10.1002/jrsm.1229 . [DOI] [PubMed] [Google Scholar]
- 134.Petticrew M. Time to rethink the systematic review catechism? Moving from ‘what works’ to ‘what happens’. Systematic reviews. 2015;4(1):1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
(DOCX)
(ENL)
(ENL)
Data Availability Statement
All relevant data are within the paper and its Supporting information files.