Key Points
Question
What is the effect of the world’s largest conditional cash transfer program, Bolsa Família (BFP), on maternal mortality?
Findings
This analysis nested within the 100 Million Brazilian Cohort, including more than 6 million women, found an association of BFP with reducing maternal mortality. A longer duration of receiving BFP was associated with a higher reduction in maternal mortality, and the poorest women benefited most from BFP.
Meaning
These findings suggest that programs such as BFP have a potential to reduce maternal mortality and health inequalities.
This cohort study uses national Brazilian linked data from health and social administrative databases to investigate the association between the Bolsa Família conditional cash transfer program and maternal mortality among women and girls of child-bearing age.
Abstract
Importance
Conditional cash transfers (CCTs) have been consistently associated with improvements to the determinants of maternal health, but there have been insufficient investigations regarding their effects on maternal mortality.
Objective
To evaluate the association between being a Bolsa Família program (BFP) beneficiary and maternal mortality and to examine how this association differs by duration of BFP receipt, maternal race, living in rural or urban areas, the Municipal Human Development Index (MHDI), and municipal primary health care coverage.
Design, Setting, and Participants
This cross-sectional analysis was nested within the 100 Million Brazilian Cohort. Girls and women aged 10 to 49 years (hereinafter referred to as women) who had at least 1 live birth were included, using data from Brazilian national health databases linked to the 100 Million Brazilian Cohort (January 1, 2004, to December 31, 2015). Propensity score kernel weighting was applied to control for sociodemographic and economic confounders in the association between BFP receipt and maternal mortality, overall and stratified by different subgroups (race, urban or rural area, and MHDI), and duration of BFP receipt. Data were analyzed from July 12, 2019, to December 31, 2022.
Main Outcome(s) and Measures
Maternal death.
Results
A total of 6 677 273 women aged 10 to 49 years were included in the analysis, 4056 of whom had died from pregnancy-related causes. The risk of maternal death was 18% lower in women who received BFP (weighted odds ratio [OR], 0.82 [95% CI, 0.71-0.93]). A longer duration receiving BFP was associated with an increased reduction in maternal mortality (OR for 1-4 years, 0.85 [95% CI, 0.75-0.97]; OR for 5-8 years, 0.70 [95% CI, 0.60-0.82]; OR for ≥9 years, 0.69 [95% CI, 0.53-0.88]). Receiving BFP was also associated with substantial increases in the number of prenatal appointments and interbirth intervals. The reduction was more pronounced in the most vulnerable groups.
Conclusions and Relevance
This cross-sectional analysis nested within the 100 Million Brazilian Cohort found an association between BFP receipt and maternal mortality. This association was of greater magnitude in women with longer exposure to BFP and in the most vulnerable groups. These findings reinforce evidence that programs such as BFP, which have already proven effective in poverty reduction, have great potential to improve maternal survival.
Introduction
Many women, especially those from low and middle-income countries, experience pregnancy-related complications, with increased risk of death.1 Maternal mortality remains a looming problem in contexts of inequality, as in the US, which maintains high rates (23.8 deaths per 100 000 live births in 2020), with those for non-Hispanic Black women almost 3 times higher (55.3 deaths per 100 000 live births) than for non-Hispanic White women (19.1 deaths per 100 000 live births).2 In Brazil, the maternal mortality rate remains high (57.0 deaths per 100 000 live births in 2019), with a modest improvement in the last decade.3
Given that most maternal and child deaths are poverty-related,4,5 conditional cash transfers (CCTs) have been proposed as a promising strategy to promote maternal and child survival.6 While some CCTs aim to alleviate poverty and increase human capital through transfers that are conditioned on school attendance and the use of maternal and child health services (child welfare, maternal and child vaccination, and prenatal attendance), other CCT transfers, such as India’s Janani Suraksha Yojana (JSY) and Nepal’s Safe Delivery Incentive Program, transfer cash only for use of specific services, such as health facility–based delivery.4 Despite these differences, studies have shown consistent associations between CCTs and reduction of poverty and improved access to health care services,4,5 which are considered strategic actions to decrease maternal mortality.4,5 However, most of these studies are generally performed with small samples. There is still little knowledge of whether CCT programs have led to improvements in maternal health outcomes, such as maternal mortality, and whether their effects are generalizable across different settings. A study of the Mexican CCT Oportunidades found an 11% reduction in maternal mortality,7 and another study of the Indian CCT JSY showed no significant association.8 A recent Brazilian study using ecological data from municipalities over a 11-year period9 demonstrated the association of CCTs with reductions in maternal mortality. The association increased with the increment in coverage levels and years of implementation.9
The mechanisms through which the program can affect maternal mortality were proposed and described in the research protocol10 and a previous study.9 Like other CCTs, BFP can affect maternal health both through receipt of the benefit and conditionalities. Income transfers can have a more immediate effect with the allocation of money for the purchase of food and other necessities and the use of health services. On the other hand, these health requirements impact the use of services during pregnancy and puerperium.4,5 In this study, drawing from a large, longitudinal populational-based cohort study using national Brazilian linked data from health and social administrative databases (the 100 Million Brazilian Cohort), we investigated the association between BFP and maternal mortality. We hypothesize that BFP is associated with decreased maternal mortality and that this association is more prominent with the increased duration of the benefit.
Methods
This cohort study was approved by the research ethics committee of the Federal University of Bahia, Salvador, Brazil. Data were stored on secure servers on the Center for Data and Knowledge Integration for Health (CIDACS) Big Data Integrated Platform.11 Since no personally identifiable information was included in the data set used for analysis, informed consent was waived. The study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
All of the methods and analyses were described in the previously published research protocol.10 We conducted a cross-sectional analysis nested within the 100 Million Brazilian Cohort, a retrospective dynamic cohort resulting from linkage of national administrative, social, and health data sets.12 The cohort baseline includes records from over 114 million individuals in the Unified Registry for Social programs (Cadastro Único), an administrative system with detailed information on the poor and extremely poor in Brazil (families with a monthly income ≤3 minimum wages [approximately US $750]) (eMethods in Supplement 1). Detailed information on the 100 Million Brazilian Cohort is available on its profile.13
Our study population consisted of girls and women aged 10 to 49 years (hereinafter referred to as women), registered on the cohort baseline, who had at least 1 live birth in their last pregnancy between January 1, 2004, and December 31, 2015. To reduce selection biases and to produce the best comparative group for women who had died from maternal causes, we only included the woman’s most recent delivery in the cohort and not all of the deliveries during her lifetime.
Linkage Process
We identified all of the women who had at least 1 live birth by connecting the live birth information system (Sistema de Informações sobre Nascidos Vivos [SINASC]) with the 100 Brazilian Million Cohort baseline. To identify maternal death records and causes of death in the cohort, we then linked the matched pairs of the first stage (SINASC and 100 Million Brazilian Cohort baseline) to records of pregnancy-related causes within the mortality information system (Sistema de Informações sobre Mortalidade). These linkages were conducted by similarity scores, using the CIDACS record linkage tool, an innovative algorithm developed to connect large-scale administrative data sets,14,15,16 based on their similarity across several identifiers. In our case, the linkage attributes were the woman’s name and age at the time of delivery, date of birth, and the municipality of residence at the time of delivery. Analysis of the linkage accuracy included manual verification of a randomly selected sample of records, assessing the receiver operating characteristics curve of sensitivity, and specificity indexes14 (eFigure 3 in Supplement 1). In this validation process, we obtained a mean sensitivity and specificity of over 92% (eFigure 3 and eTable 18 in Supplement 1).
Exposure
Bolsa Família is a CCT program that aims to reduce poverty by providing a monthly benefit and to break the intergenerational poverty of its beneficiaries through health and education conditionalities.17 Women and their families can receive basic and/or variable benefits, with values according to their level of income, considering groups of extreme poverty and poverty. Families who receive BFP are required to fulfill educational (a minimum of 85% school attendance) and health (health care appointments and a vaccination schedule) conditionalities, with a variable benefit intended for pregnant and lactating women.18 Since BFP was implemented in 2004, women registered on Cadastro Único before 2004 were considered the first to benefit from social programs on January 1, 2004. We deemed those exposed to BFP as all women with records of live births who started receiving BFP before or during pregnancy and did not stop receiving the benefit until childbirth or before death. Women who had not received the benefit at any time or until delivery were considered not exposed. Women who stopped receiving the benefit at some point before childbirth were excluded from the analysis.
Outcome
Our main study outcome was maternal death, according to code XV, O00 to O99 from the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10). Conditions classified in other chapters of ICD-10 were also included (A34, F53, M83.0, B20-B24, D39.2, and E23.0), provided that these deaths occurred within 42 days following delivery.19 We were not able to include deaths that occurred before delivery, due to linkage with SINASC.
Statistical Analysis
All analyses were performed from July 12, 2019, to December 31, 2022, using Stata, version 15.0 (StataCorp LLC). Two-sided P < .05 indicated statistical significance. In line with the published research protocol10 and previous quasi-experimental studies using the Cadastro Único data set and the 100 Million Brazilian Cohort,20,21,22 the association between BFP and maternal mortality was estimated based on the propensity score–based method. First, we used logistic regression to estimate the conditional probability of receiving treatment (being a BFP beneficiary or not), given the set of observable characteristics using the propensity score (eFigures 1 and 2 and eTable 2 in Supplement 1).23 Since whether a family receives the benefit or not is determined by per capita income and a set of family socioeconomic characteristics, the following covariates were considered to estimate the propensity score: self-reported race (5 categories available in Cadastro Único, according to the Brazilian Institute of Geography and Statistics classification [definitions provided hereinafter]),19 level of education, age, parity (number of childbirths in the cohort), location of the household (urban or rural residency), Brazilian region, household density, type of water supply, waste disposal system (sewer system), and garbage disposal. Cadastro Único was created in 2001, and the registry has been improved and expanded over the years.8 With creation of BFP (2004), there was a greater incentive to attract families in situations of poverty and extreme poverty to Cadastro Único and, in 2006, BFP achieved full expansion.24 To solve any problems that may arise with this variation in the registry over time, we also incorporated the year of registration on Cadastro Único for propensity score estimation.
As a second step, we performed a kernel-matching approach, which uses weights based on the propensity score to select observations of nonbeneficiaries who are more similar to the set of beneficiaries.25 In this study, we estimate the standard error by the bootstrap method, which was based on a resampling estimate with substitution of the original sample.26,27 As a third step, we estimated the mean treatment effect on the treated, after applying the matching weights (eTable 3 in Supplement 1) estimated through the kernel process. As a fourth and final step, we adjusted weighted logistic regression models with 95% CIs between BFP receipt and maternal death. To control for risk factors of maternal mortality (eMethods in Supplement 1, section 3.5),25 we also adjusted multivariate models for other covariates not used to estimate the propensity score: prenatal care (none, 1-3, 4-6, or ≥7 appointments), type of delivery (vaginal or cesarean), gestational period (<22, 22-27, 28-31, 32-36, 37-41, and ≥42 weeks), and multiple pregnancy (yes or no). We compared the differences in the distribution of propensity score covariates between beneficiaries and nonbeneficiaries, using proportions to assess the covariate balance before and after kernel weighting.
Duration of Receipt
To evaluate exposure to BFP, according to benefit duration, we estimated the kernel-matching and weighted logistic regressions, comparing women exposed to different ranges of years between BFP receipt until delivery (1-4, 5-8, or ≥9 years) with those not exposed to the program. In addition, since the exposure time may differ according to the woman’s age, we calculated an indicator considering the years of BFP exposure, divided by the woman’s age on delivery, multiplied by 100, resulting in a proxy of the percentage of the lives of women exposed to BFP until delivery (mean [SD], 30.44% [16.06%]), classified as less than 30%, 30% to 69%, and 70% or greater.
Subgroup Analysis
To evaluate possible effect modifications of the association between BFP exposure and maternal mortality, we conducted an analysis stratified by subgroups of sociodemographic indicators, such as area of residence (rural and urban), Municipal Human Development Index (MHDI; high or very high, medium, low, and very low), and race (Black, Pardo [which translates from Portuguese as “brown” or “mixed” and is used to denote individuals with predominantly Black and also mixed ancestry, including European, African, and Indigenous backgrounds28,29], and White). Racial categories were based on Brazilian Institute of Geography and Statistics terminology, which reflects Brazilian concepts of race and gives mothers the option of categorizing themselves as Asian, Black, Pardo, Indigenous, or White. We estimated the propensity score for each subgroup of these sociodemographic indicators, with the same variables in the previous steps, and conducted kernel-weighted logistic analysis with models separately within each subgroup. We also investigated the association between BFP and maternal mortality by the mean municipal Family Health Program (FHP) coverage, as stratified in a previous study (≤30%, 30%-70%, or >70%),30 and conducted multivariate logistic regression adjusted for the same propensity score variables, exploring the association of receiving BFP with prenatal care (<4 or ≥4 appointments) and the interbirth interval (<24 or ≥24 months or 1 live birth in the cohort). The maternal mortality rate was measured by the number of maternal deaths over the number of women who had at least 1 live birth, to provide a closer approximation of risk in the cohort.31
Sensitivity Analysis
We performed the following analyses to assess the robustness of the results. First, to investigate possible biases in the kernel-weighting procedure, we estimated the association of BFP using the inverse probability of treatment weighting, estimating the weights for BFP beneficiaries (weight = 1) and nonbeneficiaries using Weight = Propensity Score/[1 − Propensity Score].32 We also performed an analysis using conventional, multivariate regression models adjusted for confounders (eTables 4 and 5 in Supplement 1). Second, to verify whether different definitions of BFP exposure would affect the results, we tested other classifications for nonexposure and exposure, considering the period of pregnancy covered by exposure (eTables 6 and 7 in Supplement 1). Third, to test whether the results considering different ranges of years between BFP receipt until delivery (1-4, 5-8, or ≥9 years) were consistent for each year, we also estimated kernel-matching and weighted logistic regressions for each year of the duration of BFP receipt in the study period (eTables 8-10 in Supplement 1). To assess the robustness of the variables used for matching, we also performed analyses by removing variables from propensity score housing conditions (eTables 15-18 in Supplement 1).
Results
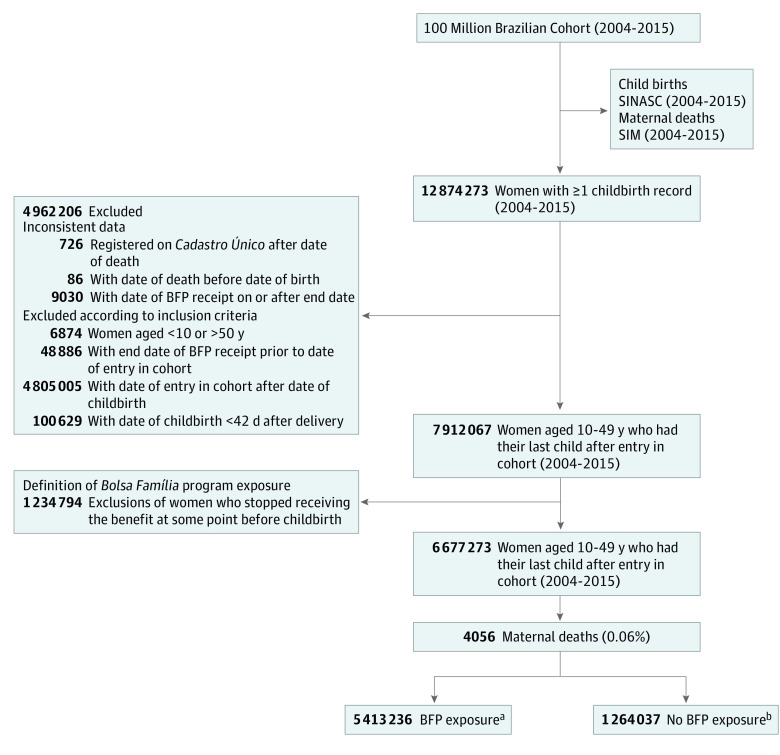
Following definition of BFP exposure, we included 6 677 273 women aged 10 to 49 years who had at least 1 live birth, and 4056 of these had died of pregnancy-related causes. A total of 5 413 236 (81.07%) were BFP beneficiaries and 1 264 037 (18.93%) were nonbeneficiaries (Figure 1). The characteristics of the population excluded from the analysis on account of the BFP exposure definition (women who stopped receiving the benefit at some point before childbirth) are described in eTable 1 in Supplement 1.
Figure 1. Flowchart of Study Population Definition.
SIM indicates mortality information system (Sistema de Informações sobre Mortalidade); SINASC, live birth information system (Sistema de Informações sobre Nascidos Vivos).
aIncludes women who started receiving Bolsa Família program (BFP) benefit before or during pregnancy and did not stop receiving the benefit until childbirth, or before death.
bIncludes women who did not receive the benefit at any time or until childbirth.
At baseline, BFP beneficiaries were more likely to be younger, Black or Pardo, have a lower level of education, reside in rural areas, and have worse housing conditions (Table 1). Compared with baseline characteristics, the 2 groups became more similar after kernel weighting (Table 1). Lower maternal mortality rates were observed among BFP beneficiaries after kernel-weighting balancing (60.63 [95% CI, 58.46-62.89] vs 71.59 [95% CI, 62.87-81.53] deaths per 100 000 women who had live births). In the model adjusted for the number of prenatal appointments, type of delivery, gestational period, and multiple pregnancies, BFP receipt was associated with an 18% decreased maternal mortality (weighted odds ratio [OR], 0.82 [95% CI, 0.71-0.93]) in the kernel-weighting regression (Table 2).
Table 1. Description of BFP Nonbeneficiaries and Beneficiaries Before and After Kernel Weighting, 2004 to 2015 (N = 6 677 273).
| Variable | Before kernel weighting, % | After kernel weighting, % | ||||
|---|---|---|---|---|---|---|
| Non-BFP (n = 1 264 037) | BFP (n = 5 413 236) | Diff (BFP-Non-BFP | Non-BFP (n = 1 017 154) | BFP (n = 4 731 624) | Diff (BFP-Non-BFP) | |
| Race | ||||||
| Asian | 0.47 | 0.35 | −0.12 | 0.31 | 0.34 | 0.03 |
| Black | 7.36 | 8.78 | 1.42 | 8.56 | 8.74 | 0.18 |
| Indigenous | 0.29 | 1.03 | 0.74 | 0.70 | 0.80 | 0.10 |
| Pardo | 55.69 | 63.69 | 8.00 | 64.04 | 63.57 | −0.47 |
| White | 36.19 | 26.15 | −10.04 | 26.39 | 26.49 | 0.10 |
| Missing dataa | 9.35 | 5.76 | NA | NA | NA | NA |
| Educational attainment | ||||||
| High school or college (≥8 y) | 69.64 | 58.88 | −10.76 | 57.82 | 58.78 | 0.96 |
| Elementary or middle school (4-7 y) | 24.21 | 32.86 | 8.65 | 33.68 | 33.02 | −0.66 |
| Elementary school or illiterate (<3 y) | 6.15 | 8.26 | 2.11 | 8.50 | 8.20 | −0.30 |
| Missing dataa | 1.98 | 2.26 | NA | NA | NA | AN |
| Age group, y | ||||||
| 10-19 | 14.09 | 23.24 | 9.15 | 23.47 | 23.66 | 0.19 |
| 20-34 | 75.89 | 69.32 | −6.57 | 69.45 | 68.88 | −0.57 |
| ≥35 | 10.02 | 7.44 | −2.58 | 7.08 | 7.46 | 0.38 |
| Missing dataa | 0 | 0 | NA | NA | NA | NA |
| No. of children in cohort | ||||||
| 1 | 39.74 | 44.35 | 4.61 | 45.46 | 44.21 | −1.25 |
| 2-3 | 57.80 | 49.66 | −8.14 | 48.90 | 49.87 | 0.97 |
| >3 | 2.46 | 5.99 | 3.53 | 5.64 | 5.92 | 0.28 |
| Missing dataa | 0 | 0 | NA | NA | NA | NA |
| Household density | ||||||
| ≤2 Persons per room | 79.30 | 53.22 | −26.08 | 53.21 | 53.33 | 0.12 |
| >2 Persons per room | 20.70 | 46.78 | 26.08 | 46.79 | 46.67 | −0.12 |
| Missing dataa | 11.63 | 5.10 | NA | NA | NA | NA |
| Water supply | ||||||
| Public network | 77.51 | 65.42 | −12.09 | 65.64 | 65.98 | 0.34 |
| Well, natural source, or other | 22.49 | 34.58 | 12.09 | 34.36 | 34.01 | −0.35 |
| Missing dataa | 7.53 | 2.79 | NA | NA | NA | NA |
| Waste disposal system | ||||||
| Public network | 77.51 | 38.72 | −38.79 | 38.28 | 38.81 | 0.53 |
| Septic tank, ditch, or other | 22.49 | 61.28 | 38.79 | 61.72 | 61.19 | −0.53 |
| Missing dataa | 8.88 | 3.51 | NA | NA | NA | NA |
| Garbage disposal | ||||||
| Public collection system | 51.21 | 68.78 | 17.57 | 69.35 | 69.77 | 0.42 |
| Burned, buried, or other | 49.79 | 31.22 | −18.57 | 30.64 | 30.22 | −0.42 |
| Missing dataa | 7.53 | 2.79 | NA | NA | NA | NA |
| Geographical region | ||||||
| South | 14.19 | 8.55 | −5.64 | 8.43 | 8.71 | 0.28 |
| North | 9.78 | 13.21 | 3.43 | 12.99 | 12.74 | −0.25 |
| Northeast | 30.69 | 42.87 | 12.18 | 42.80 | 42.86 | 0.06 |
| Southeast | 35.10 | 29.29 | −5.81 | 29.66 | 29.68 | 0.02 |
| Center-West | 10.24 | 6.08 | −4.16 | 6.12 | 6.01 | −0.11 |
| Missing dataa | 0 | 0 | NA | NA | NA | NA |
| Location of household | ||||||
| Urban | 81.56 | 71.74 | −9.82 | 72.15 | 72.40 | 0.25 |
| Rural | 18.44 | 28.26 | 9.82 b | 27.85 | 27.60 | −0.25b |
| Missing dataa | 5.56 | 2.06 | NA | NA | NA | NA |
| Year | ||||||
| 2004 | 7.85 | 10.26 | 2.41 | 10.39 | 10.55 | 0.16 |
| 2005 | 7.12 | 7.92 | 0.80 b | 7.53 | 7.85 | 0.32b |
| 2006 | 26.84 | 45.62 | 18.78 | 46.44 | 46.69 | 0.25 |
| 2007 | 11.18 | 13.71 | 2.53 | 14.64 | 14.44 | −0.2 |
| 2008 | 5.37 | 5.53 | 0.16 | 6.06 | 5.84 | −0.22 |
| 2009 | 4.33 | 4.85 | 0.52 | 5.22 | 5.09 | −0.13 |
| 2010 | 6.12 | 4.36 | −1.76 | 3.59 | 3.50 | −0.09 |
| 2011 | 5.18 | 2.51 | −2.67 | 1.56 | 1.58 | 0.02 |
| 2012 | 10.41 | 2.79 | −7.62 | 2.61 | 2.54 | −0.07 |
| 2013 | 7.44 | 1.61 | −5.83 | 1.17 | 1.16 | −0.01 |
| 2014 | 6.09 | 0.72 | −5.37 | 0.67 | 0.65 | −0.02 |
| 2015 | 2.07 | 0.12 | −1.95 | 0.12 | 0.11 | −0.01 |
| Missing dataa | 0 | 0 | NA | NA | NA | NA |
Abbreviations: BFP, Bolsa Família program; NA, not applicable.
Percentage was not included when calculating the categories.
P < .005. For all others in these columns, P < .001.
Table 2. Kernel-Weighted Regression for Associations Between BFP Receipt and Maternal Deatha.
| Kernel-weighted rate, % (95% CI) | OR (95% CI) | |||
|---|---|---|---|---|
| Non-BFPb | BFPb | Nonadjusted | Adjustedc | |
| Rate or OR | 71.59 (62.87-81.53) | 60.63 (58.46-62.89) | 0.84 (0.73-0.96) | 0.82 (0.71-0.93) |
| No. of women | 1 017 154 | 4 731 624 | 5 748 917 | 5 542 230 |
Abbreviations: BFP, Bolsa Família program; OR, odds ratio.
Data are from the 100 Million Brazilian Cohort, 2004 to 2015.
Non-BFP and BFP correspond to kernel-weighted maternal rates per 100 000 parturients of the live birth information system (Sistema de Informações sobre Nascidos Vivos) to nonbeneficiaries and beneficiaries, respectively.
Adjusted by prenatal care, gestational age, type of delivery, and multiple pregnancy.
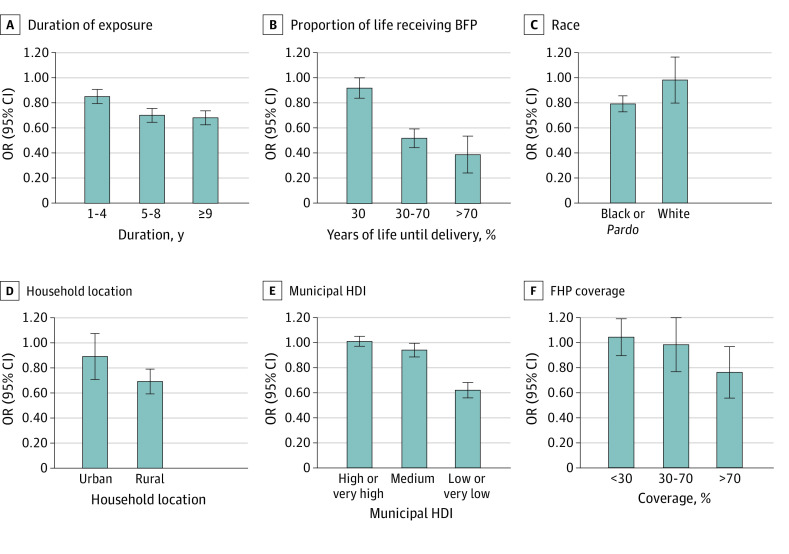
Increased duration of BFP exposure was associated with a reduction in maternal mortality (weighted OR for 1-4 years, 0.85 [95% CI, 0.75-0.97]; weighted OR for 5-8 years, 0.70 [95% CI, 0.60-0.82]; and weighted OR for ≥9 years, 0.69 [95% CI, 0.53-0.88]). The higher the percentage of the woman’s lifetime exposed to BFP on delivery, the greater the chances were of reducing maternal death (weighted OR for <30%, 0.92 [95% CI, 0.77-1.09]; weighted OR for 30%-70%, 0.52 [95% CI, 0.40-0.69]; and weighted OR for >70%, 0.39 [95% CI, 0.18-0.82]). A higher protective effect of BFP was observed among Black or Pardo women (weighted OR, 0.79 [95% CI, 0.69-0.93]), women living in rural areas (weighted OR, 0.69 [95% CI, 0.53-0.92]), and women who lived in less developed municipalities (weighted OR for low or very low MHDI, 0.62 [95% CI, 0.47-0.84]), although the 95% CIs overlapped (Figure 2 and eTables 8-10 and 11-13 in Supplement 1). Receiving BFP was associated with the reduction of maternal mortality among women living in municipalities with high FHP coverage (weighted OR for ≥70%, 0.76 [95% CI, 0.57-0.97]; weighted OR for 30%-70%, 0.98 [95% CI, 0.78-1.22]; weighted OR for <30%, 1.04 [95% CI, 0.78-1.39]) (Figure 2 and eTable 14 in Supplement 1).
Figure 2. Receipt of Bolsa Família program (BFP) Benefit, Sociodemographic Vulnerability Markers, and Duration of BFP Receipt.
Kernel-weighted logistic regression was used for associations between BFP receipt and maternal death by time of exposure and BFP participation by years of life until delivery (ie, years of receipt divided by years of life until delivery). Stratified analysis by sociodemographic vulnerability markers included race, location of household, Municipal Human Development Index (HDI), and Family Health Program (FHP) coverage. All the analytical steps (propensity score estimation, kernel-matching and weighted logistic regressions) were conducted separately for each category of this subgroup. Pardo translates from Portuguese as “brown” or “mixed” and is used to denote individuals with predominantly Black and also mixed ancestry, including European, African, and Indigenous backgrounds. OR indicates odds ratio.
The BFP beneficiaries were more likely to attend 4 or more prenatal appointments (adjusted OR, 1.43 [95% CI, 1.42-1.44]). They also had a longer interbirth interval than nonbeneficiaries (adjusted OR, 1.39 [95% CI, 1.39-1.40]) (Table 3).
Table 3. Logistic Regression for Associations Between BFP Participation, Prenatal Care Appointments, and Interpregnancy Intervalsa.
| Variable | Non-BFP | BFP | Adjusted OR (95% CI)b |
|---|---|---|---|
| Prenatal care appointments | |||
| <4 | 14 087 (1.25) | 435 718 (8.12) | 1 [Reference] |
| ≥4 | 1 112 322 (98.75) | 4 930 276 (91.88) | 1.43 (1.42-1.44) |
| No. of women | 1 126 409 | 5 365 994 | 6 619 173 |
| Interpregnancy interval, mo | |||
| <24 | 509 786 (40.33) | 1 769 593 (32.98) | 1 [Reference] |
| ≥24 | 754 251 (59.67) | 3 596 401 (67.02) | 1.39 (1.39-1.40) |
| No. of women | 1 264 037 | 5 365 994 | 6 677 293 |
Abbreviations: BFP, Bolsa Família program; OR, odds ratio.
Data are from the 100 Million Brazilian Cohort, 2004 to 2015.
Multivariate logistic regression adjusted by propensity score variables.
Sensitivity Analysis
We obtained similar point estimates for the association between receiving BFP and decreased maternal mortality in all of the sensitivity analyses performed. Details are found in eTables 4 to 10 and 15 to 17 in Supplement 1.
Discussion
Our findings in this cohort study suggest that BFP is associated with a reduction in maternal mortality among the poorest Brazilian women. This association remained robust after adjustment for health care, multiple pregnancies, and type of delivery, achieving an 18% decrease in the chance of maternal mortality among BFP beneficiaries. Increased exposure to BFP increased the magnitude of the association. Receipt of BFP was also associated with prenatal appointments and increased interbirth interval. There was also an association among the most vulnerable groups, such as Black or Pardo women and municipalities with the lowest MHDI.
Several studies have shown that CCT programs have had a positive association with the social determinants of maternal health, such as nutritional status, immunization coverage, the promotion of healthy behaviors, and use of health care services.4,8,33,34,35,36 However, few studies have evaluated the effect of CCTs on maternal mortality, with controversial results. A study conducted in Mexico7 reported an 11% decrease in maternal mortality, associated with higher Oportunidades CCT coverage levels. An investigation in India8 showed an increase in the percentage of births delivered at health facilities to be associated with being a beneficiary of the Indian CCT (JSY), but no effect on maternal mortality was found. The short period of the analysis following implementation of JSY (only 2 years) could be a limitation, since more time between the implementation and health service support may be required to affect maternal death among beneficiaries. An ecological study9 found a 17% decrease in maternal death in municipalities with higher BFP coverage over the last 11 years in Brazil.
The CCT BFP might affect maternal mortality through different mechanisms. First, the income transferred to women can have a more immediate effect, with the allocation of money for purchase of food, the use of health services, and mobility, particularly if it is coupled with shifts in intrahousehold power or autonomy favoring women.37,38,39,40,41,42 Second, by fulfilling conditionalities, BFP can increase access and the use of health services by reducing barriers and increasing the monitoring and treatment of comorbidities, facilitating referrals to high-risk prenatal care, and ensuring adequate assistance while giving birth. Receipt of BFP increased the interbirth interval and use of prenatal care, lending additional support to our hypothesis that BFP is associated with maternal mortality through the effect of relevant determinants of maternal mortality. In our study, an association of BFP with maternal mortality was found in municipalities with the highest level of FHP coverage. Conditional cash transfers are designed to have both short- and long-term effects on their beneficiaries’ lives.43 The findings of the present study suggest that the association between BFP and maternal mortality increased in magnitude, according to extended duration of the benefits. Studies have shown that longer exposure to a CCT program is associated with higher levels of engagement in utilizing health services44 and increased levels of education.43,45
Another important finding of our study is the association of BFP and maternal mortality among the most vulnerable (Black women, Pardo women, and women who live in rural areas and less developed municipalities), suggesting a potential contribution of BFP to reducing social inequalities.46 A high focalization of CCTs contributes to a significant downturn in susceptibilities among the most vulnerable beneficiaries. For example, Black women are disproportionately affected by poverty and maternal morbidities and mortality.47,48 Many of these morbidities, such as hypertension and gestational diabetes, can be controlled with adequate access to health care through conditionalities and receipt of the benefit, reducing access barriers and unmet needs.49 In addition, the most vulnerable women are more dependent on publicly provided and funded services,49,50 and the FHP was also prioritized within the more impoverished areas. The role of the FHP in the reduction of social inequalities has been well documented in the literature.49,51,52,53 Despite differences in the 2 public policies (social and health policies), it seems plausible that the mechanisms underlying the effects are synergic.
Limitations
This study has some limitations. Although the 100 Million Brazilian Cohort is a powerful source of sociodemographic information, it contains data on the poorest half of the population; therefore, the results are not necessarily representative of all Brazilian women. Furthermore, residual confounding is possible, since data on other maternal mortality–related factors, including access to health care at the time of delivery, distance to services, the skills and preparedness of health care professionals, and preexisting comorbidities, were not available in the routinely collected data sets. We have attempted to minimize this by using different analytical approaches and performing subgroup and sensitivity analyses to strengthen the evidence produced and to minimize uncontrolled confounding. Limitations also arise from the linkage process (missed or false matches). However, we obtained a mean sensitivity and specificity of more than 92% in the linkage validation process, and these errors are probably nondifferential (eFigure 3 and eTable 18 in Supplement 1).
Conclusions
The results of our cohort study show that a CCT program can substantially reduce maternal mortality in a large middle-income country such as Brazil. We have provided new evidence that continual exposure to BFP is associated with a reduction in maternal mortality, suggesting a long-term effect of CCTs. In the context of the COVID-19 pandemic and political instability affecting health care provision in Brazil, a country with considerable mortality among pregnant and postpartum women,54,55,56,57 we should consider intensifying efforts to maintain and implement appropriate social policies, in conjunction with improved quality of prenatal and obstetric care in the post–COVID-19 recovery period.
eMethods. Study Population, Propensity Score and Kernel Weighting, Sensitivity and Subgroup Analyses, and Data Linkage and Quality Assessment
eTable 1. Description of Women Excluded From the Main Analysis Following Definition of Bolsa Família Program (BFP) Exposure
eTable 2. Logistic Models to Estimate the Propensity Scores for Bolsa Família Participation
eTable 3. ATT of Maternal Mortality for BFP Receipt Between 2004 and 2015 Using Kernel Matching
eFigure 1. Propensity Scores Common Support Area
eFigure 2. Cumulative Distribution Balancing Plot
eTable 4. Baseline Characteristics of Bolsa Família Program (BFP) Nonbeneficiaries (non-BFP) and Beneficiaries From Cadastro Único Registration Between 2004 and 2015
eTable 5. Kernel-Weighted Regression and Other Strategies for Associations Between BFP Receipt and Maternal Death in 100 Million Brazilian Cohort, 2004-2015
eTable 6. Kernel-Weighted Regression for Associations Between BFP Receipt and Maternal Death in 100 Million Brazilian Cohort, 2004-2015
eTable 7. Kernel-Weighted Regression for Associations Between Duration of BFP Receipt and Maternal Death per Year in 100 Million Brazilian Cohort, 2004-2015
eTable 8. Kernel-Weighted Regression for Associations Between Length of Exposure to Receiving BFP and Maternal Death per Year in 100 Million Brazilian Cohort, 2004-2015
eTable 9. Kernel-Weighted Regression for Associations Between Length of Exposure to Receiving BFP/Age and Maternal Death per Year in 100 Million Brazilian Cohort, 2004-2015
eTable 10. Kernel-Weighted Regression for Associations Between Length of Exposure to Receiving BFP and Maternal Death per Year in 100 Million Brazilian Cohort, 2004-2015
eTable 11. Regression Results: Coefficients on Unadjusted Kernel-Weighted Logistic Regressions Within Subgroups of Municipal Human Development Index (MHDI)
eTable 12. Regression Results: Coefficients on Unadjusted Kernel-Weighted Logistic Regressions Within Subgroups of Maternal Race
eTable 13. Regression Results: Coefficients on Unadjusted Kernel-Weighted Logistic Regressions Within Subgroups of Area of Residence (Rural and Urban)
eTable 14. Regression Results: Coefficients on Unadjusted Kernel-Weighted Logistic Regressions Within Subgroups of Municipal Quintiles of Family Health Program Coverage
eTable 15. Logistic Models to Estimate the Propensity Scores for Bolsa Família Participation
eTable 16. Average Treatment Effect on the Treated (ATT) Estimated Using Kernel-Matching (Excluding Type of Water Supply, Waste Disposal System [Sewer System], and Location of Household of the PS)
eTable 17. Kernel-Weighted Regression for Associations Between BFP Receipt and Maternal Death (Excluding Type of Water Supply, Waste Disposal System [Sewer System], and Location of Household of the PS) in 100 Million Brazilian Cohort, 2004-2015
eTable 18. Accuracy Analysis of the Linkage Between Cadastro Único and the Mortality Information System in a Sample of 10 000 Record Pairs
eFigure 3. ROC Curve of the Linkage Between Mortality and Cadastro Único Between 2001 and 2015
eReferences
Data Sharing Statement
References
- 1.World Health Organization . Maternal Mortality: Levels and Trends 2000 to 2017. World Health Organization; 2019. [Google Scholar]
- 2.Hoyert DL. Maternal Mortality Rates in the United States, 2020: A Report. National Center for Health Statistics; 2022. doi: 10.15620/cdc:113967 [DOI] [PubMed] [Google Scholar]
- 3.Leal MDC, Szwarcwald CL, Almeida PVB, et al. Reproductive, maternal, neonatal and child health in the 30 years since the creation of the Unified Health System (SUS). Cien Saude Colet. 2018;23(6):1915-1928. doi: 10.1590/1413-81232018236.03942018 [DOI] [PubMed] [Google Scholar]
- 4.Glassman A, Duran D, Fleisher L, et al. Impact of conditional cash transfers on maternal and newborn health. J Health Popul Nutr. 2013;31(4)(suppl 2):48-66. [PubMed] [Google Scholar]
- 5.Kusuma D, Cohen J, McConnell M, Berman P. Can cash transfers improve determinants of maternal mortality? Evidence from the household and community programs in Indonesia. Soc Sci Med. 2016;163:10-20. doi: 10.1016/j.socscimed.2016.06.020 [DOI] [PubMed] [Google Scholar]
- 6.Fiszbein A, Schady NR. Conditional Cash Transfers: Reducing Present and Future Poverty. World Bank Publications; 2009. doi: 10.1596/978-0-8213-7352-1 [DOI] [Google Scholar]
- 7.Araujo MC, Suárez P. Oportunidades Human Development Program: evolution and challenges. Inter-American Development Bank. Accessed November 2013. Accessed November 25, 2020. https://publications.iadb.org/es/publicacion/15404/programa-de-desarrollo-humano-oportunidades-evolucion-y-desafios
- 8.Lim SS, Dandona L, Hoisington JA, James SL, Hogan MC, Gakidou E. India’s Janani Suraksha Yojana, a conditional cash transfer programme to increase births in health facilities: an impact evaluation. Lancet. 2010;375(9730):2009-2023. doi: 10.1016/S0140-6736(10)60744-1 [DOI] [PubMed] [Google Scholar]
- 9.Rasella D, Alves FJO, Rebouças P, et al. Long-term impact of a conditional cash transfer programme on maternal mortality: a nationwide analysis of Brazilian longitudinal data. BMC Med. 2021;19(1):127. doi: 10.1186/s12916-021-01994-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Falcão IR, Ribeiro-Silva RC, Alves FJO, et al. Evaluating the effect of Bolsa Familia, Brazil’s conditional cash transfer programme, on maternal and child health: a study protocol. PLoS One. 2022;17(5):e0268500. doi: 10.1371/journal.pone.0268500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Centro de Integração de Dados e Conhecimentos para Saúde . Accessed January 19, 2023. https://cidacs.bahia.fiocruz.br/sobre/quem-somos/
- 12.Barreto ML, Ichihara MY, Almeida BA, et al. The Centre for Data and Knowledge Integration for Health (CIDACS): linking health and social data in Brazil. Int J Popul Data Sci. 2019;4(2):1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barreto ML, Ichihara MY, Pescarini JM, et al. Cohort profile: the 100 Million Brazilian Cohort. Int J Epidemiol. 2022;51(2):e27-e38. doi: 10.1093/ije/dyab213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Almeida D, Gorender D, Ichihara MY, et al. Examining the quality of record linkage process using nationwide Brazilian administrative databases to build a large birth cohort. BMC Med Inform Decis Mak. 2020;20(1):173-173. doi: 10.1186/s12911-020-01192-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barbosa GCG, Ali MS, Araujo B, et al. CIDACS-RL: a novel indexing search and scoring-based record linkage system for huge datasets with high accuracy and scalability. BMC Med Inform Decis Mak. 2020;20(1):289. doi: 10.1186/s12911-020-01285-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pita R, Pinto C, Sena S, et al. On the accuracy and scalability of probabilistic data linkage over the Brazilian 114 Million Cohort. IEEE J Biomed Health Inform. 2018;22(2):346-353. doi: 10.1109/JBHI.2018.2796941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.da República P, Civil C. Subchefia para Assuntos Jurídicos. Decree 5209: Bolsa Família Program. Official Diary of the Union. September 17, 2004. November 20, 2020. http://www.mds.gov.br/webarquivos/legislacao/bolsa_familia/decreto/decreto_no_5209_de_17.09.2004-1.pdf
- 18.Família B. Transferência de Renda e Apoio à Família No Acesso à Saúde, à Educação e à Assistência Social. 2020. Accessed November 20, 2020. https://www.mds.gov.br/webarquivos/publicacao/bolsa_familia/Cartilhas/Cartilha_PBF_2015.pdf
- 19.World Health Organization . International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10). 2nd ed. World Health Organization; 2004. [Google Scholar]
- 20.Ramos D, da Silva NB, Ichihara MY, et al. Conditional cash transfer program and child mortality: a cross-sectional analysis nested within the 100 Million Brazilian Cohort. PLoS Med. 2021;18(9):e1003509. doi: 10.1371/journal.pmed.1003509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jesus GS, Pescarini JM, Silva AF, et al. The effect of primary health care on tuberculosis in a nationwide cohort of 7·3 million Brazilian people: a quasi-experimental study. Lancet Glob Health. 2022;10(3):e390-e397. doi: 10.1016/S2214-109X(21)00550-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pescarini JM, Campbell D, Amorim LD, et al. Impact of Brazil’s Bolsa Família Programme on cardiovascular and all-cause mortality: a natural experiment study using the 100 Million Brazilian Cohort. Int J Epidemiol. 2022;51(6):1847-1861. doi: 10.1093/ije/dyac188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rosenbaum PR, Rubin DB. Reducing bias in observational studies using subclassification on the propensity score. J Am Stat Assoc. 1984;79(387):516-524. doi: 10.1080/01621459.1984.10478078 [DOI] [Google Scholar]
- 24.Soares S, Ribas RP, Soares FV. Focalização e cobertura do Programa Bolsa-Família: qual o significado dos 11 milhões de famílias? 2009. Accessed December 28, 2022. https://repositorio.ipea.gov.br/bitstream/11058/1398/1/TD_1396.pdf
- 25.Ho DE, Imai K, King G, Stuart EA. Matching as nonparametric preprocessing for reducing model dependence in parametric causal inference. Polit Anal. 2007;15(3):199-236. doi: 10.1093/pan/mpl013 [DOI] [Google Scholar]
- 26.Abadie A, Imbens GW. Bias-corrected matching estimators for average treatment effects. J Bus Econ Stat. 2011;29(1):1-11. doi: 10.1198/jbes.2009.07333 [DOI] [Google Scholar]
- 27.Imbens GW. Nonparametric estimation of average treatment effects under exogeneity: a review. Rev Econ Stat. 2004;86(1):4-29. doi: 10.1162/003465304323023651 [DOI] [Google Scholar]
- 28.Travassos C, Williams DR. The concept and measurement of race and their relationship to public health: a review focused on Brazil and the United States. Cad Saude Publica. 2004;20(3):660-678. doi: 10.1590/S0102-311X2004000300003 [DOI] [PubMed] [Google Scholar]
- 29.Loveman M, Muniz JO, Bailey SR. Brazil in black and white? race categories, the census, and the study of inequality. Ethnic and Racial Studies. 2012;35(8):1466-1483. doi: 10.1080/01419870.2011.607503 [DOI] [Google Scholar]
- 30.Rasella D, Aquino R, Santos CA, Paes-Sousa R, Barreto ML. Effect of a conditional cash transfer programme on childhood mortality: a nationwide analysis of Brazilian municipalities. Lancet. 2013;382(9886):57-64. doi: 10.1016/S0140-6736(13)60715-1 [DOI] [PubMed] [Google Scholar]
- 31.Sustainable Development Goals . Indicator 3.1.1. Maternal mortality ratio. Updated January 17, 2022. Accessed May 26, 2021. https://sdgdata.gov.uk/3-1-1/
- 32.Austin PC. The use of propensity score methods with survival or time-to-event outcomes: reporting measures of effect similar to those used in randomized experiments. Stat Med. 2014;33(7):1242-1258. doi: 10.1002/sim.5984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lanre-Abass BA. Poverty and maternal mortality in Nigeria: towards a more viable ethics of modern medical practice. Int J Equity Health. 2008;7:11-11. doi: 10.1186/1475-9276-7-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Edmond KM, Foshanji AI, Naziri M, et al. Conditional cash transfers to improve use of health facilities by mothers and newborns in conflict affected countries: a prospective population based intervention study from Afghanistan. BMC Pregnancy Childbirth. 2019;19(1):193. doi: 10.1186/s12884-019-2327-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.de Brauw A, Peterman A. Can conditional cash transfers improve maternal health care? evidence from El Salvador’s Comunidades Solidarias Rurales program. Health Econ. 2020;29(6):700-715. doi: 10.1002/hec.4012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhou H, Wu Y, Liu C, et al. Conditional cash transfers, uptake of maternal and child health services, and health outcomes in western rural China. BMC Public Health. 2020;20(1):870. doi: 10.1186/s12889-020-08996-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.de Brauw A, Gilligan DO, Hoddinott J, Roy S. The impact of Bolsa Família on women’s decision-making power. World Dev. 2014;59:487-504. doi: 10.1016/j.worlddev.2013.02.003 [DOI] [Google Scholar]
- 38.Duarte GB, Sampaio B, Sampaio Y. Bolsa Família Program: impact of transfers on food expenditures in rural families. Article in Portuguese. Rev Econ Sociol Rural. 2009;47:903-918. doi: 10.1590/S0103-20032009000400005 [DOI] [Google Scholar]
- 39.Ferrario MN. The impacts on family consumption of the Bolsa Família subsidy programme. CEPAL Rev. 2014;2014(112):147-163. doi: 10.18356/5579e867-en [DOI] [Google Scholar]
- 40.Martins APB, Monteiro CA. Impact of the Bolsa Família program on food availability of low-income Brazilian families: a quasi experimental study. BMC Public Health. 2016;16(1):827-827. doi: 10.1186/s12889-016-3486-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sperandio N, Rodrigues CT, do Carmo Castro Franceschini S, Priore SE. Impact of the Bolsa Família Program on energy, macronutrient, and micronutrient intakes: Study of the Northeast and Southeast. Rev Nutr. 2016;29:833-844. doi: 10.1590/1678-98652016000600008 [DOI] [Google Scholar]
- 42.Coelho PL, Melo ASSA. The impact of the “Bolsa Família” Program on household diet quality, Pernambuco State, Brazil. Article in Portuguese. Cien Saude Colet. 2017;22:393-402. doi: 10.1590/1413-81232017222.13622015 [DOI] [Google Scholar]
- 43.Molina Millan T, Barham TCJ, Macours K, Maluccio JA, Stampini M. Long-term impacts of conditional cash transfers in Latin America: review of the evidence. World Bank Res Obs. 2019;34(1):119-159. doi: 10.1093/wbro/lky005 [DOI] [Google Scholar]
- 44.Sosa-Rubí SG, Walker D, Serván E, Bautista-Arredondo S. Learning effect of a conditional cash transfer programme on poor rural women’s selection of delivery care in Mexico. Health Policy Plan. 2011;26(6):496-507. doi: 10.1093/heapol/czq085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Molina Millán T, Macours K, Maluccio JA, Tejerina L. Experimental long-term effects of early-childhood and school-age exposure to a conditional cash transfer program. J Dev Econ. 2020;143:102385. doi: 10.1016/j.jdeveco.2019.102385 [DOI] [Google Scholar]
- 46.Veras Soares F, Soares S, Medeiros M, Osorio R. Cash Transfer Programmes in Brazil: Impacts on Inequality and Poverty. International Policy Centre for Inclusive Growth; 2006. [Google Scholar]
- 47.Martins AL. Maternal mortality among black women in Brazil. Article in Portuguese. Cad Saude Publica. 2006;22(11):2473-2479. doi: 10.1590/S0102-311X2006001100022 [DOI] [PubMed] [Google Scholar]
- 48.Tucker MJ, Berg CJ, Callaghan WM, Hsia J. The Black-White disparity in pregnancy-related mortality from 5 conditions: differences in prevalence and case-fatality rates. Am J Public Health. 2007;97(2):247-251. doi: 10.2105/AJPH.2005.072975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hone T, Rasella D, Barreto ML, Majeed A, Millett C. Association between expansion of primary healthcare and racial inequalities in mortality amenable to primary care in Brazil: a national longitudinal analysis. PLoS Med. 2017;14(5):e1002306. doi: 10.1371/journal.pmed.1002306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Paixão M, Carvano LM. Relatório Anual das Desigualdades Raciais no Brasil; 2007-2008. 2008. Accessed August 10, 2020. https://sites.utexas.edu/marcelo-paixao/files/2019/02/RADR_2007-2008.pdf
- 51.Andrade MV, Noronha KV, Queiroz Barbosa AC, et al. Family health strategy and equity in prenatal care: a population based cross-sectional study in Minas Gerais, Brazil. Int J Equity Health. 2017;16(1):24. doi: 10.1186/s12939-016-0503-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Carneiro Alves de Oliveira BL, Castro Cardoso LF, de Oliveira Dominice R, et al. The influence of the Family Health Strategy on the use of health services by hypertensive adults in Brazil. Rev Bras Epidemiol. 2020;23(3):1-14. [DOI] [PubMed] [Google Scholar]
- 53.Guimarães RM. Does the inverse theory hypothesis apply to primary health care? evidence from 5 564 Brazilian municipalities. Article in Portuguese. Rev Panam Salud Publica. 2018;42:e128.doi: 10.26633/RPSP.2018.128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Amorim MMR, Soligo Takemoto ML, Fonseca EBD. Maternal deaths with coronavirus disease 2019: a different outcome from low- to middle-resource countries? Am J Obstet Gynecol. 2020;223(2):298-299. doi: 10.1016/j.ajog.2020.04.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Takemoto MLS, Menezes MO, Andreucci CB, et al. The tragedy of COVID-19 in Brazil: 124 maternal deaths and counting. Int J Gynaecol Obstet. 2020;151(1):154-156. doi: 10.1002/ijgo.13300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Nakamura-Pereira M, Amorim MMR, Pacagnella RC, et al. COVID-19 and maternal death in Brazil: an invisible tragedy. Rev Bras Ginecol Obstet. 2020;42(8):445-447. doi: 10.1055/s-0040-1715138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Souza ASR, Amorim MMR. Maternal mortality by COVID-19 in Brazil. Rev Bras Saúde Mater Infant. 2021;21:253-256. doi: 10.1590/1806-9304202100s100014 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods. Study Population, Propensity Score and Kernel Weighting, Sensitivity and Subgroup Analyses, and Data Linkage and Quality Assessment
eTable 1. Description of Women Excluded From the Main Analysis Following Definition of Bolsa Família Program (BFP) Exposure
eTable 2. Logistic Models to Estimate the Propensity Scores for Bolsa Família Participation
eTable 3. ATT of Maternal Mortality for BFP Receipt Between 2004 and 2015 Using Kernel Matching
eFigure 1. Propensity Scores Common Support Area
eFigure 2. Cumulative Distribution Balancing Plot
eTable 4. Baseline Characteristics of Bolsa Família Program (BFP) Nonbeneficiaries (non-BFP) and Beneficiaries From Cadastro Único Registration Between 2004 and 2015
eTable 5. Kernel-Weighted Regression and Other Strategies for Associations Between BFP Receipt and Maternal Death in 100 Million Brazilian Cohort, 2004-2015
eTable 6. Kernel-Weighted Regression for Associations Between BFP Receipt and Maternal Death in 100 Million Brazilian Cohort, 2004-2015
eTable 7. Kernel-Weighted Regression for Associations Between Duration of BFP Receipt and Maternal Death per Year in 100 Million Brazilian Cohort, 2004-2015
eTable 8. Kernel-Weighted Regression for Associations Between Length of Exposure to Receiving BFP and Maternal Death per Year in 100 Million Brazilian Cohort, 2004-2015
eTable 9. Kernel-Weighted Regression for Associations Between Length of Exposure to Receiving BFP/Age and Maternal Death per Year in 100 Million Brazilian Cohort, 2004-2015
eTable 10. Kernel-Weighted Regression for Associations Between Length of Exposure to Receiving BFP and Maternal Death per Year in 100 Million Brazilian Cohort, 2004-2015
eTable 11. Regression Results: Coefficients on Unadjusted Kernel-Weighted Logistic Regressions Within Subgroups of Municipal Human Development Index (MHDI)
eTable 12. Regression Results: Coefficients on Unadjusted Kernel-Weighted Logistic Regressions Within Subgroups of Maternal Race
eTable 13. Regression Results: Coefficients on Unadjusted Kernel-Weighted Logistic Regressions Within Subgroups of Area of Residence (Rural and Urban)
eTable 14. Regression Results: Coefficients on Unadjusted Kernel-Weighted Logistic Regressions Within Subgroups of Municipal Quintiles of Family Health Program Coverage
eTable 15. Logistic Models to Estimate the Propensity Scores for Bolsa Família Participation
eTable 16. Average Treatment Effect on the Treated (ATT) Estimated Using Kernel-Matching (Excluding Type of Water Supply, Waste Disposal System [Sewer System], and Location of Household of the PS)
eTable 17. Kernel-Weighted Regression for Associations Between BFP Receipt and Maternal Death (Excluding Type of Water Supply, Waste Disposal System [Sewer System], and Location of Household of the PS) in 100 Million Brazilian Cohort, 2004-2015
eTable 18. Accuracy Analysis of the Linkage Between Cadastro Único and the Mortality Information System in a Sample of 10 000 Record Pairs
eFigure 3. ROC Curve of the Linkage Between Mortality and Cadastro Único Between 2001 and 2015
eReferences
Data Sharing Statement