Abstract
Obesity is global health problem with an estimated three billion people worldwide being classified as overweight or obese. In addition to being associated with a range of adverse health outcomes, obesity is linked to higher risks of atrial and ventricular arrhythmias, as well as sudden cardiac death. Obesity is a multifactorial disease that often co-exists with hypertension, diabetes, and sleep apnoea, which are also independent risk factors for cardiac arrhythmias. Nevertheless, compelling evidence suggests that increasing adiposity is an independent proarrhythmic risk factor and that weight loss can be a mitigating and preventative intervention to reduce arrhythmia incidence. This review briefly outlines the economic and social burden of obesity and summarises evidence for the direct and indirect effects of increasing adiposity on risk of atrial and ventricular arrhythmias. The paper also summarises the evidence for electrocardiographic changes indicative of obesity-related atrial and ventricular remodelling and how weight reduction and management of comorbidity might reduce arrhythmic burden.
Keywords: cardiology, electrophysiology, metabolic diseases
Introduction
Approximately 3 billion people, or half the world’s population, is either overweight or obese.1 The worldwide prevalence of obesity has tripled since 1975, and is thus an increasingly important global economic and health burden.2 Body mass index is the ratio of weight to height and forms the basis for most healthcare recommendations and guidelines because it is quick and easy to calculate, enabling tracking of changes in whole body adiposity over time. A healthy body mass index is considered 18.5-24.9, overweight is 25.0-29.9, and obesity is 30.0 or more. Subclassifications include grade 1 obesity, defined as 30.0-34.9, grade 2 as 35.0-39.9, and grade 3 as 40.0 or more. However, these definitions are flawed because body mass index is an imprecise measure of adiposity. UK obesity management guidelines3 suggest that waist girth, an indicator of abdominal visceral adiposity, might therefore be a useful adjunct to measure health risks in individuals who are overweight or obese. Other anthropometric indices can quantify adiposity, such as waist to hip ratio and waist to height ratio, although these indices do not yield substantially more information on adiposity than can be gained from waist girth. Abdominal diameter is a surrogate for waist girth but is more difficult to measure clinically.4 For these reasons, body mass index and waist girth are the mainstay metrics for quantifying weight and adiposity in guidelines.3 5 6 In this review, we summarise evidence for obesity as a risk factor for atrial and ventricular arrhythmias, and the extent to which these are conferred by increasing adiposity or mediated by cardiometabolic comorbidity. We also explore evidence for the effects of lifestyle and surgical weight management, and management of comorbidity related to obesity that might mitigate arrhythmic risks.
Epidemiology of obesity and related arrhythmias
Obesity affects more than 600 million adults worldwide.7 The increasing prevalence of obesity in low and middle income countries is attributed to urbanisation, easy accessibility to processed energy-dense food, and cultural shifts towards lifestyles of high income countries.8 Two thirds of the UK population is overweight or obese.9 In 2011, modelling suggested that by 2030 the number of obese adults would increase by 65 million in the US and by 11 million in the UK. As a consequence, the number of patients in the UK with diabetes would increase by up to 8 million, for heart disease and stroke by 7 million, and for cancer by 0.5 million, at the expense of 55 million quality adjusted life years, adding £2000 million (€2.3 billion; $2.2 billion) to healthcare costs each year.10 Another meta-analysis estimated that, compared with individuals of healthy weight, UK healthcare costs increase by as much as 12% for excess weight and 36% for obesity, secondary to greater demand for drug treatments, hospital admission, and ambulatory care.11 Indeed, prescription costs incurred by a patient who is morbidly obese over a three year period are 10 times greater than that of someone of a healthy weight.12 Given that ageing confers a higher risk of arrhythmias and the increase in ageing populations in high income countries,13 evidence linking increasing adiposity and atrial and ventricular arrhythmias presented in this review suggests that the obesity epidemic is likely to add to the burden of arrhythmias in the future.
Sources and selection criteria
We searched PubMed and Embase databases for clinical studies in the English language that were published between 1 January 1980 and 1 April 2022. Studies must have evaluated arrhythmic risks and electrocardiographic adaptations associated with obesity, or cardiovascular outcomes associated with weight reduction strategies in obesity. We used the following search terms: "obesity," "arrhythmia," "atrial arrhythmia," "atrial fibrillation OR AF," "ventricular arrhythmia," "QT OR QTc," "P wave," "electrocardiographic," "OSA OR sleep apnoea OR sleep apnea OR obstructive sleep apnoea," "diabetes," "hypertension," "weight loss OR weight reduction," "bariatric surgery." We prioritised peer reviewed randomised controlled trials and cohort studies and excluded case studies or series. In addition to primary sources, we searched reference lists as additional sources of information.
Obesity related atrial remodelling
Atrial dilatation and consequent electroanatomic architectural distortion causes conduction slowing and increases conduction heterogeneity, which are hallmarks of a proarrhythmic substrate.14 In multivariable analyses of 13 382 echocardiograms, which were adjusted for age and sex, patients who were obese had increased odds of left atrial enlargement (odds ratio 2.53 (95% confidence interval 2.30 to 2.75)), in addition to other parameters of diastolic dysfunction.15 A prospective study of 1212 adults who were followed up over 10 years showed that obesity and hypertension were independent predictors of left atrial volume after adjusting for age, sex, cardiovascular disease, and other risk factors.16 Furthermore, linear regression analyses showed that the effect of obesity was almost twice that of hypertension. The Framingham Heart Study (FHS), a prospective, community based observational study of 5282 participants, also showed that left atrial dilatation was a mediator of atrial arrhythmias associated with increasing body mass index.17
Atrial electroanatomic adaptations related to obesity manifest as changes in P wave indices on 12 lead electrocardiogram, including P wave duration and dispersion, which characterise right and left atrial electrical depolarisation.18 P wave indices have been associated with atrial remodelling in an echocardiographic study,19 as well as with increased risk of atrial fibrillation (AF) in the Atherosclerosis Risk in Communities study20 and in the FHS.21 22 Furthermore, investigation of 14 433 participants in the Atherosclerosis Risk in Communities study showed progressive abnormalities in the P wave indices with increasing weight after adjustment for cardiovascular risk factors.23 Correspondingly, reverse atrial remodelling denoted by regression of adverse P wave indices correlates with degree of weight loss in obesity.24
Obesity as a risk factor for atrial fibrillation
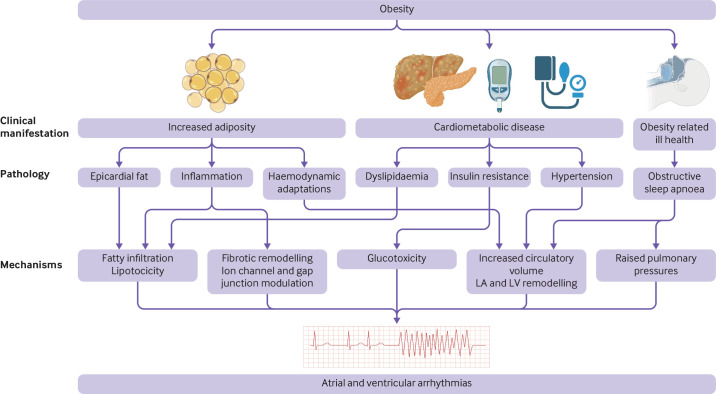
AF is the most common sustained arrhythmia.25 Strong clinical evidence from prospective and retrospective studies links obesity to a higher AF incidence.26 27 A meta-analysis of 51 studies including 626 603 participants showed that a 5 unit increase in body mass index conferred 29% higher odds of incident AF in cohort studies and 19% higher odds in case control studies.26 Odds of postoperative AF resulted in 10% greater per 5 unit increase in body mass index, as was the case after ablation AF, which reported a 13% greater risk, suggesting that AF recurrence after invasive treatment is greater in people with higher body mass.26 Additionally, a nationwide cohort study showed that although AF incidence was low among more than 270 000 young women (mean age 31 years, standard deviation 5 years), obesity still independently predicted AF in this age group.28 Furthermore, in a prospective, community cohort study that followed up 3000 patients for six years, body mass index independently predicted progression of paroxysmal to permanent AF (1.04 per kg/m2 (95% confidence interval 1.03 to 1.06)) after adjustment for age and sex.29 Thus, compelling evidence links obesity to higher risks of AF across a wide age range and in both sexes. Mendelian randomisation studies use genetic variation to investigate causal relations between modifiable risk factors and health outcomes in observational data; the results of which have supported a causal association between higher body mass index and AF risk.30 Mendelian randomisation studies also show that obesity often co-exists with hypertension,20 insulin resistance,31 and obstructive sleep apnoea,32 which each independently confer increased arrhythmic risk (figure 1). In the following sections we explore the extent to which increases in arrhythmic risk in obesity is explained by increases in adipose volume, particularly epicardial fat, or by obesity related comorbidity.
Figure 1.
Mechanisms underpinning obesity as a risk factor for atrial and ventricular arrhythmias. The higher risk of cardiac arrhythmias in obesity is conferred by increasing adiposity, concurrent cardiometabolic disease, and related ill health. These result in adverse electrophysiological remodelling of the atria and ventricles to create a proarrhythmic substrate. The evidence for some of these mechanisms and their potential for reversibility with weight reduction are discussed in the main text. LA=left atrium; LV=left ventricle
Epicardial adipose tissue as mediator of atrial fibrillation
Epicardial adipose tissue is the visceral fat depot of the heart and is in intimate contact with the underlying myocardium, covering up to 80% of the epicardial surface. This tissue shares the same embryological origin and circulation as the myocardium, facilitating paracrine cross-talk between these neighbouring tissues.33 The epicardial adipose tissue volume increases with increasing obesity,34 resulting in fatty myocardial infiltration and relative fat depot hypoxia, causing adipocytes to secrete pro-inflammatory and pro-fibrotic adipocytokines that adversely affect electrophysiological function35 (figure 1). Consequently, epicardial adipose tissue volume is positively correlated with P wave duration,36 37 amplitude,36 and dispersion,37 and PR interval prolongation.38 Meta-analysis of eight observational studies comprising 375 526 participants reported PR interval prolongation is associated with a 45% increased relative risk of AF (hazard ratio 1.45 (95% confidence interval 1.23 to 1.71)).39 Initial evidence that increased epicardial adipose tissue is associated with increased risk of AF was provided by a computed tomography study of 3217 participants in the FHS which showed an AF odds of 28% higher after body mass index and intrathoracic fat deposit adjustment (odds ratio per standard deviation of pericardial fat volume 1.28 (95% confidence interval 1.03 to 1.58)).40 Epicardial fat volumes are greater in patients with AF versus people in sinus rhythm and the volume is related to duration and burden of AF, independent of age, sex, left atrial enlargement, hypertension, diabetes, and body mass index.41 42 In a meta-analysis of 63 observational studies of 352 275 individuals, every standard deviation increment in epicardial adipose tissue volume was associated with 2.6-fold higher odds of AF, as well as 2.2-fold higher odds of persistent versus paroxysmal AF.27 Interestingly, AF risk for every standard deviation increment in anthropometric indices of adiposity was weaker than for epicardial adipose tissue volume (odds ratio of body mass index 1.22 (95% confidence interval 1.17 to 1.27); waist circumference 1.32 (1.25 to 1.41); waist to hip 1.11 (1.08 to 1.14), v epicardial adipose tissue 2.61 (1.89 to 3.60)), suggesting arrhythmic risk related to obesity is at least partly attributable to epicardial adipose tissue.
Mediators of atrial fibrillation risk in obesity
Obesity often co-exists with cardiometabolic diseases, such as hypertension, dyslipidaemia, and insulin resistance, broadly referred to as the metabolic syndrome.6 This clustering of cardiometabolic perturbations confers a higher risk of AF.43 Obstructive sleep apnoea is also common in obesity and has been linked to AF.32 44 45 The extent to which obesity related AF risk is mediated via concurrent hypertension, insulin resistance, and obstructive sleep apnoea will be discussed.
Hypertension
Obesity causes essential hypertension,46 which in turn increases risk of AF. In the Atherosclerosis Risk in Communities cohort study of 14 598 individuals, hypertension was the largest population attributable fraction to AF risk contributing to more than a fifth of incident AF (21.6% (95% confidence interval 16.8 to 26.7)).20 Hypertension augments obesity related haemodynamic adaptations, although echocardiographical observations suggest disparate mechanisms of myocardial remodelling between hypertension and obesity.47 In a prospective Norwegian population based cohort study with a 35 year follow-up,48 incident AF after adjustment for other cardiovascular risk factors increased for people with blood pressures at the upper limit of normal (hazard ratio 1.50 (95% confidence interval 1.10 to 2.03)) and in people in the hypertensive range (1.60 (1.15 to 2.21)). Other evidence suggesting that the higher risks of AF in obesity are mediated by hypertension was provided by the LEGACY cohort study of 355 people, in which weight loss reduced blood pressure and antihypertensive use in tandem with reduction of AF burden.49 These studies provide evidence that arrhythmic risks might be partly explained by hypertension when in people with obesity.
Diabetes
Multisystem lipotoxic effects of increasing adiposity results in insulin resistance and eventually diabetes, which increases AF risk.50 In the FHS, diabetes was an independent risk factor for AF (odds ratio of 1.4 for men and 1.6 for women).31 A population based case-control study comprising 3613 individuals showed that every percent increment in glycated haemoglobin (HbA1c) was associated with 14% higher adjusted odds of AF increasing by as much as 3% for every year of diabetic treatment.51 Similarly in the Atherosclerosis Risk in Communities study, a positive linear association between HbA1c and incident AF risk was noted in people with diabetes.52 Additionally, increased HbA1c independently predicts recurrent AF post-ablation,53 54 and among 106 patients with a new diagnosis of AF followed up over five years with ambulatory electrocardiogram monitoring, diabetes independently predicted progression from paroxysmal to persistent AF.55 A meta-analysis of 25 case-control studies comprising 2932 patients reported reduced heart rate variability in patients with type two diabetes, suggesting autonomic dysfunction.56 Diabetic autonomic neuropathy is characterised by parasympathetic denervation resulting in unchecked, increased sympathetic tone that contributes to AF pathogenesis.57 A meta-analysis of 8 037 756 individuals reported a higher risk of AF in patients with diabetes even after adjusting for obesity (relative risk 1.22 (95% confidence interval 1.09 to 1.38)).58 Diabetes is therefore an arrhythmic risk factor, both independently and in the context of obesity.
Obstructive sleep apnoea
Obstructive sleep apnoea was associated with AF, independent of body mass index, neck circumference, hypertension, and diabetes, in a prospective cohort study of 463 patients (odds ratio 2.19 (95% confidence interval 1.40 to 3.42)).32 An analysis of the Sleep Heart Health Study, a multicentre longitudinal study of 6441 participants that investigated the cardiovascular consequences of sleep-disordered breathing, showed an even greater association with AF after adjustment for age, sex, body mass index, and coronary disease (odds ratio 4.02 (95% confidence interval 1.03 to 15.74)).44 A dose dependent relation between obstructive sleep apnoea and AF burden was also reported in an Australian cohort of 6841 patients referred for polysomnography, in whom duration of apnoea and time in hypoxaemia were arrhythmic predictors independent of body mass index.45 Similarly, the Outcomes Registry for Better Informed Treatment of Atrial Fibrillation (ORBIT-AF) registry, which enrolled 10 132 participants with AF who were followed up for two years, found that patients with obstructive sleep apnoea had a greater burden of severe or disabling symptomatic AF than did those without (22% v 16%, P<0.001), although no differences in risk of AF progression were reported (hazard ratio 1.06 (95% confidence interval 0.89 to 1.28)).59
Despite these data, evidence for the link between obstructive sleep apnoea and AF is conflicting. For instance, the Olmsted Country retrospective cohort study of 3542 adults reported that obesity, but not obstructive sleep apnoea, was an independent risk factor for incident AF in adults older than 65 years.60 Similarly, the Outcomes of Sleep Disorders in Older Men Study of 2911 men showed that obstructive sleep apnoea severity was associated with risk of cardiovascular events but not with incident AF.61 Consistent with these findings, no differences were reported in freedom from arrhythmia after ablation among AF patients receiving standard care or weight and obstructive sleep apnoea management.62 Finally, a large retrospective study of 30 188 patients with sleep-disordered breathing (obstructive sleep apnoea or central sleep apnoea) showed that time to recurrent AF after cardioversion or ablation was not influenced by continuous positive airway pressure treatment (hazard ratio 1.01 (95% confidence interval 1.00 to 1.02)).63
The conflicting evidence for the effects of obstructive sleep apnoea on AF risk might be partly explained by the confounding effects of concurrent obesity. For instance, although obstructive sleep apnoea is twice as prevalent in patients who are obese compared with people of healthy weight;64 this association might be bidirectional and obstructive sleep apnoea can increase susceptibility to weight gain by inducing leptin resistance.65 Given these complexities, Mendelian randomisation studies can overcome some limitations of observational data to identify causal links between phenotypes. One Mendelian randomisation study showed that the genetic propensity for obstructive sleep apnoea also increased AF risk (odds ratio 1.21 (95% confidence interval 1.12 to 1.31)).66 However, this analysis was based on only five single nucleotide polymorphisms, of which two were also associated with body mass index or fat-free mass at the genome wide significance level, suggesting this link could be mediated by obesity. Indeed, another Mendelian randomisation study including almost sixfold single nucleotide polymorphisms showed that although obstructive sleep apnoea was associated with AF in univariable analysis (odds ratio 2.09 (95% confidence interval 1.10 to 3.98)), this finding became non-significant after adjustment for body mass index (0.68 (0.42 to 1.10)).30 In brief, available data suggest that proarrhythmic risks associated with obstructive sleep apnoea are partly mediated by obesity.
Abnormal ventricular repolarisation and ventricular arrhythmias
The QT interval is a measure of the duration of ventricular activation and repolarisation. Given that action potential duration shortens as heart rate increases, in clinical practice the interval is corrected for heart rate (corrected QT, or QTc). Generally, QTc intervals of 450 ms or more in men and of 470 ms or more in women are considered abnormal. QTc dispersion non-invasively quantifies dispersion of ventricular repolarisation, and is calculated as the difference between the longest and shortest QTc interval on a 12 lead electrocardiogram. This term refers to spatial heterogeneity of repolarisation, such that increased dispersion can result in re-entry thereby facilitating ventricular tachycardia or fibrillation. Although the clinical usefulness of QTc dispersion over QTc interval in predicting adverse arrhythmic and cardiovascular outcomes has been debated,67 both prolong with obesity and reverse with weight reduction.68–72 A comprehensive meta-analysis of the effects of the obesity on ventricular repolarisation showed that QTc was longer in individuals who were obese versus people who were not (mean difference 21.74 ms (95% confidence interval 18.76 to 32.32)).68 Similarly, pooled estimates for QTc dispersion were greater in obesity (15.17 ms (13.59 to 16.74)). Another meta-analysis of 22 studies showed that QTc shortened and QTc dispersion decreased after weight loss induced by lifestyle or surgery (QTc, mean difference −25.77 ms (95% confidence interval −18.86 to −28.21); QTc dispersion, −13.46 ms (−11.32 to −15.60)).69 71
Consistent with abnormal ventricular repolarisation associated with obesity, increasing body mass index has also been associated with higher risk of ventricular arrhythmias and sudden cardiac death73 (figure 1). However, this risk might not be attributable to only obesity given the variable definitions of sudden cardiac death that could also include fatal cardiovascular events resulting from comorbidity. Nevertheless, one meta-analysis of 14 prospective studies reported relative risks for sudden cardiac death of 1.16 (95% confidence interval 1.05 to 1.28) per 5 unit increment in body mass index, 1.82 (1.61 to 2.07) per 0.1 unit increase in waist to hip ratio, and 1.03 (0.93 to 1.15) per 10 cm increase in waist circumference.73 In the MADIT trial, individuals who were obese received a higher rate of appropriate shock treatment from implantable cardiac defibrillators than individuals who were not obese (39% v 24%, p=0.014).74 The higher burden of ventricular ectopy, particularly in the context of left ventricular hypertrophy,75 might partly explain the higher incidence of ventricular arrhythmias and sudden cardiac death in obesity, whereby critically timed extrasystoles can trigger re-entrant arrhythmias in a remodelled substrate.76 The risks of ventricular arrhythmias and sudden cardiac death in obesity are likely to be mediated by increasing adiposity as well as cardiometabolic comorbidity that independently cause electrophysiological remodelling.
Weight loss strategies to mitigate obesity related risk of atrial fibrillation
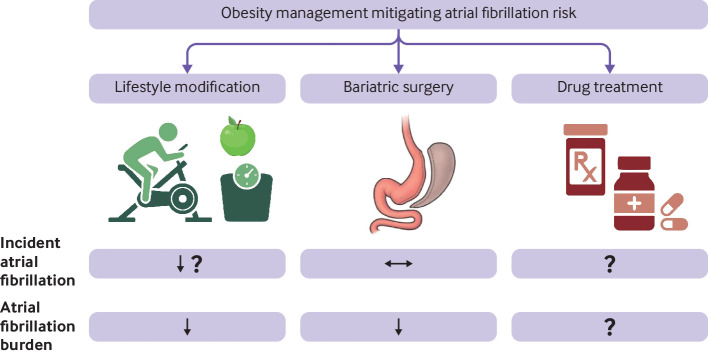
The anti-arrhythmic effects of weight loss treatments have gained much interest. Here, we review weight management strategies for reducing AF risk and burden and are summarised in figure 2.
Figure 2.
Management options for obesity and their effects on atrial fibrillation risks. Although lifestyle changes and bariatric surgery reduces atrial fibrillation burden in obese patients with pre-existing atrial fibrillation, the evidence for surgical weight reduction on mitigating the risk of incident atrial fibrillation is conflicting. Lifestyle changes are likely to reduce incident atrial fibrillation risk. The effects of pharmacological modulation of obesity on incident atrial fibrillation risk and atrial fibrillation burden is not well described
Non-surgical weight reduction interventions
Given that every 5 unit increment in body mass index confers about 30% greater risk of incident AF, 13% increase in recurrent AF post-ablation, and 10% increase in post-surgical AF,26 weight loss was hypothesised to potentially alleviate AF burden. This theory was tested in a single centre, partially blinded study, in which 150 ambulatory patients who were overweight or obese with symptomatic paroxysmal AF were randomly assigned to an active weight management programme or offered general lifestyle advice.77 Participants randomly assigned to active weight management experienced on average 14.3 kg weight reduction compared with 3.6 kg in the control group, as well as improvements in AF symptom burden scores (11.8 v 2.6 points) and symptom severity scores (8.4 v 1.7 points). This occurred in the context of reduced number of AF episodes, cumulative AF duration, interventricular septal thickness, and left atrial area in those randomised to active weight management, suggesting reverse remodelling of atrial tissue with weight loss.
The ARREST-AF cohort study offered 281 patients with a body mass index of 27 or more and hypertension, glucose intolerance or diabetes, hyperlipidaemia, obstructive sleep apnoea, smoking, or alcohol excess, undergoing catheter ablation for symptomatic AF either aggressive risk factor management or standard care.78 Risk factor management resulted in significantly greater blood pressure reductions (34.1 mm Hg (standard deviation 7.5) v 20.6 mm Hg (standard deviation 3.2), P=0.003), and better glycaemic control (HbA1c concentrations of <7% in 100% v 29%, P=0.001) and lipid profiles (46% v 17%, P=0.01) compared with the control group. AF-free survival was greater in the risk factor management arm, and furthermore, risk factor management independently predicted AF-free survival after multiple ablations. In the context of comprehensive blood pressure and glycaemic, lipid, and weight management, the extent to which weight loss contributed to the reduction in AF burden is not possible to ascertain.
In the LEGACY cohort study, 355 patients who were obese with AF receiving risk factor management were followed up over a mean of four years.49 The degree of weight loss related to freedom from AF and individuals maintaining more than 10% weight loss had a sixfold greater probability of arrhythmia-free survival compared with patients with 3-9% or less than 3% weight loss. Importantly, the number of anti-arrhythmic drugs or ablation procedures were similar between groups at baseline, and degree of weight loss corresponded with participation in weight management clinic suggesting a positive reinforcement effect. AF-free survival associated not only with weight loss but also subsequent weight maintenance, such that AF burden and symptom severity was less in those with less than 2% weight fluctuation compared with those with more than 5%.49
The implications for weight loss on AF in the LEGACY cohort was further characterised in the REVERSE-AF study comprising 355 individuals.79 Approximately 48 (40%) of 116 individuals with less than 3% weight loss progressed from paroxysmal to persistent AF and a quarter reversed from persistent to paroxysmal or no AF. Of the individuals who had 3-9% weight loss, a third (n=33/104) progressed from paroxysmal to persistent AF and almost half reversed from persistent to paroxysmal or no AF. Among individuals recording more than 10% weight loss, only 3% progressed to persistent AF, and almost 90% reversed from persistent to paroxysmal or no AF. Taken together, the degree of weight loss and its maintenance are likely important lifestyle changes assisting in alleviating arrhythmic burden. Importantly, these results show that early weight management intervention helps to mitigate and even reverse progression of AF to prevent irreversible atrial remodelling. The dose response effect of weight loss and improved fitness on AF burden was corroborated in a retrospective cohort study of 69 885 patients undergoing treadmill stress tests which showed that every one metabolic equivalent increment during exercise was associated with 7% lower risk of incident AF (hazard ratio, 0.93; 95% confidence interval 0.92-0.94; P<0.001), and that this effect was more pronounced in obese individuals and independent of baseline fitness.80 In short, there is compelling evidence supporting weight reduction to alleviate arrhythmic burden.
Orlistat, a lipase inhibitor, is the only guideline recommended drug for obesity management in the UK,81 however its effects on arrhythmia reduction are not well described. Recently, glucagon-like peptide-1 receptor agonists (GLP-1RA) have emerged as novel drugs in obesity, irrespective of diabetic status.82–89 The first to be approved by the Food and Drug Administration and European Medicine Agency was liraglutide, followed by semaglutide by the FDA in June 2021. Although GLP-1RAs appear to have bridged the weight reduction gap between lifestyle and surgical weight reduction strategies, which typically result in less than 10% and more than 20% weight loss respectively,90 their anti-arrhythmic effects when prescribed for weight reduction remain unproven. In the context of treating diabetes, a meta-analysis of 31 randomised trials comprising about 18 000 patients with diabetes on GLP-1RA versus 15 000 controls concluded that GLP-1RAs did not influence AF incidence.91
Bariatric surgery
Bariatric surgery is a cost effective intervention for moderately to severely obese people compared with non-surgical interventions.92 Despite compelling evidence suggesting weight loss reduces arrhythmic burden in those with pre-existing atrial arrhythmias,93 conflicting evidence exists for the effect of bariatric surgery on incident AF risk.94 95 One meta-analysis comprising 39 prospective and retrospective cohort studies showed that bariatric surgery reduced all-cause mortality (pooled hazard ratio 0.55 (95% confidence interval 0.49 to 0.62)), cardiovascular mortality (hazard ratio 0.59 (95% confidence interval 0.47 to 0.73)), and incidence of heart failure (0.50 (0.38 to 0.66)), myocardial infarction (0.58 (0.43 to 0.76)), and stroke (0.64 (0.53 to 0.77)).96 However, no statistical reduction was noted in incident AF (hazard ratio 0.82 (95% confidence interval 0.64 to 1.06)).96 Of the 39 studies included in this meta-analysis,96 only seven listed AF in their primary or secondary outcomes, of which only three studies assessed incident AF as a primary outcome measure after bariatric surgery. Consequently, the absence of any effect of bariatric surgery on incident AF risk might be partly explained by the relative paucity of studies investigating AF as their primary objective.
A reduction in AF after bariatric surgery has also been reported in the context of a reduction in obesity related comorbidities. For example, in a longitudinal study of 827 patients who were morbidly obese and who underwent laparoscopic adjustable gastric banding, incident AF was significantly greater in patients with obstructive sleep apnoea than in those without obstructive sleep apnoea (1.7% v 0.5%, P<0.001).97 By contrast, among the 5067 participants in the Look AHEAD (Action for HEAlth in Diabetes) cohort, weight loss from lifestyle modification in overweight and obese individuals with type 2 diabetes did not reduce incident AF risk.98 The absence of the preventive anti-arrhythmic effect might be due to the relatively modest body weight reductions achieved by lifestyle measures compared with bariatric surgery (about 10% v 20%) and is consistent with observations from studies supporting sustained weight reduction for greater arrhythmia-free survival and improvements in cardiovascular outcomes.49 77 99 Similarly, among a national primary and secondary healthcare database of more than 11 million patients in the UK, although rate of AF resolution among patients undergoing bariatric surgery was greater than among matched controls for age, sex, and body mass index, a downward but non-significant trend for AF incidence was reported (adjusted hazard ratio 0.72 (95% confidence interval 0.49 to 1.05)).95 In summary, although surgical and non-surgical weight reduction is an effective intervention for reducing AF recurrence, the evidence for bariatric surgery reducing incident arrhythmic risk is less consistent.71
Evidence for reduction in sudden cardiac death risk with weight loss
Although obesity has been associated with a higher risk of sudden cardiac death in large multicentre, prospective cohort studies,73 100–102 no studies to date have quantified any reduction in risk following weight loss. This lack of data is perhaps unsurprising given the practical challenges in anticipating terminal events and contribution of morbidity. However, given that obesity is also associated with a higher risk of ventricular tachycardia or fibrillation74 103 and weight loss with electrocardiogram changes suggestive of favourable changes in ventricular activation and repolarisation,68 69 104 105 it may be inferred the weight loss at least partly mitigates sudden cardiac death risk in obesity.
Anti-arrhythmic effects of treatments for obesity related comorbidities
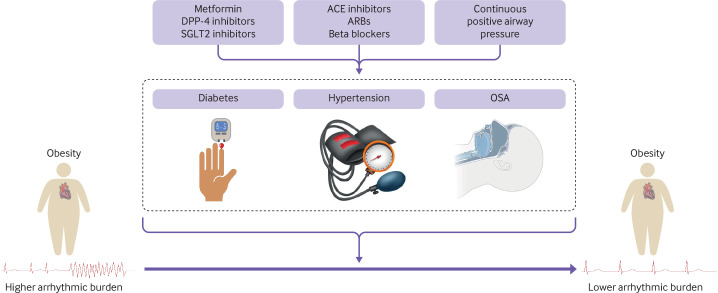
A detailed review of evidence based management for comorbidities related to obesity is beyond the scope of this review. Instead, we specifically outline the evidence for the treatment of hypertension, obstructive sleep apnoea, and diabetes in patients who are obese that might confer anti-arrhythmic benefits, in addition to weight reduction highlighted in the previous section (figure 3).
Figure 3.
Management of diabetes, hypertension, and obstructive sleep apnoea (OSA) have additional anti-arrhythmic effects. Arrhythmic risk in obesity is partly mediated by concurrent cardiometabolic disease and obesity related ill health, such as OSA. Their respective treatments might alleviate arrhythmic burden in the long term. DPP-4=dipeptidyl-peptidase-4 inhibitors; SGLT2=sodium-glucose cotransporter-2; ACE=angiotensin-converting enzyme; ARBs=angiotensin receptor blockers
Anti-hypertensive treatments
Obesity and chronic hypertension independently cause left ventricular hypertrophy, which has been associated with a higher risk of atrial and ventricular arrhythmias.106 In the double blind, placebo controlled, TRACE study comprising 790 patients randomly assigned to trandolapril treatment and 787 to placebo, the incidence of AF over a four year follow-up was greater in the trandolapril group compared with the placebo group (5.3% v 2.8%, P<0.05). Adjusted multivariable regression analysis suggested trandolapril treatment independently reduced the risk of new AF (risk ratio 0.45 (95% confidence interval 0.26 to 0.76)) in people with left ventricular dysfunction after a myocardial infarction.107 Similarly, angiotensin receptor blockers in combination with anti-arrhythmic treatment have been shown to reduce AF burden in patients with persistent AF, defined as an episode of AF lasting for more than seven days.108 Despite the short two month follow-up duration, the intention-to-treat analysis of 154 patients in a randomised trial showed that people prescribed irbesartan in addition to amiodarone had lower rate of recurrent AF (84.79% v 63.16%) as well as a greater probability of remaining AF-free (79.52% v 55.91%).108 First line agents for hypertension treatment can therefore confer additional anti-arrhythmic effects.
Continuous positive airway pressure
Continuous positive airway pressure (CPAP) is the mainstay treatment for obstructive sleep apnoea,109 although reports on the effects of this treatment on AF risk are conflicting. Observational studies have reported reductions in atrial and ventricular ectopy110 and arrhythmias111 with continuous positive airway pressure and maintenance of sinus rhythm after cardioversion and catheter ablation for AF.112 Two meta-analyses of 108 observational studies evaluating the effect of continuous positive airway pressure on AF risk reported similar results. One meta-analysis of 3743 people suggested that AF risk increased by almost 60% in people with obstructive sleep apnoea who were not treated with continuous positive airway pressure.113 The other meta-analysis of 4752 patients reported a 42% relative risk reduction of AF recurrence with continuous positive airway pressure among more than 1000 patients.114 Another meta-analysis of clinical and observational studies comprising 14 812 patients showed that continuous positive airway pressure reduced AF recurrence by over 60%.115 The benefits of this treatment in reducing AF recurrence might also be greater in younger patients (<60 years).116 Similarly, continuous positive airway pressure has been shown to be particularly efficacious at decreasing AF risk in younger men who are obese, supporting intervention early in the progression of obesity.117
Nevertheless, an open label randomised trial of 108 patients with paroxysmal AF and moderate to severe obstructive sleep apnoea, showed no difference in AF burden between groups treated with continuous positive airway pressure and the standard care group.118 Likewise, in a randomised trial of 37 patients receiving continuous positive airway pressure and 46 patients receiving standard care, no difference was reported in AF burden after pulmonary vein isolation between groups.119 Discrepancies between observational and randomised data might be due to selection of individuals with minimal symptoms in clinical trials. Patients with symptoms are more likely to be established on CPAP and physicians might be reluctant to recruit them to studies where the patients are randomly assigned to a control arm. Furthermore, incomplete CPAP adherence in patients who have minimal symptoms can confound results. Nevertheless, a Mendelian randomisation study of data from 55 114 patients with AF and 482 295 controls, published in 2022, showed that sleep disordered breathing was not associated with AF after adjusting for body mass index.30 Importantly, however, body mass index remained associated with AF after adjusting for obstructive sleep apnoea. This finding suggests that the link between obstructive sleep apnoea and AF might be mediated or confounded by concurrent obesity in patients with mild-to-moderate obstructive sleep apnoea30 and supports aggressive strategies for weight reduction to mitigate AF risk in these patients.
Oral hypoglycaemic agents
Metformin is the first line agent for type two diabetes, with sulphonylureas, thiazolidinediones, dipeptidyl-peptidase 4 inhibitors, GLP-1RAs, and sodium-glucose cotransporter-2 inhibitors (SGLT2i) considered second line or third-line options.120 Insulin is useful when other drugs do not result in normoglycaemia, or in patients with type one diabetes, in which insulin is a first-line treatment. The absence of arrhythmic endpoints in prespecified primary outcomes is a limitation of many trials. For this reason, the evidence for any anti-arrhythmic properties of drugs intended for other clinical indications is often limited to retrospective post-hoc analysis. Nevertheless, metformin has been associated with a decreased risk of AF121 and AF recurrence after catheter ablation.122 SGLT2i have been shown to confer beneficial cardiovascular effects, particularly in reducing major adverse cardiovascular events.123–127 Consistent with improvements in rates of myocardial infarction and heart failure events, meta-analyses of randomised controlled trials have shown reductions of atrial and ventricular arrhythmias with SGLT2i treatment128 129 that are greater than those observed with dipeptidyl-peptidase-4 inhibitors.130 One meta-analysis of 31 randomised studies (n=75 279) showed that SGLT2i reduced AF related events compared with placebo or no treatment (1.1% v 1.5%; risk ratio 0.75 (95% confidence interval 0.66 to 0.86)).129 Another analysis of 34 randomised trials consisting of more than 63 000 patients aged 53-67 years followed up between 24 weeks and 5.7 years, SLGT2i treatment was associated with lower incidence of atrial arrhythmias (odds ratio 0.81 (95% confidence interval 0.69 to 0.95)), but not of ventricular arrhythmias or cardiac arrest.128 Notably, not all studies in this meta-analysis reported arrhythmic events, and even in those that did, the overall incidence was 1% for atrial arrhythmias and less than 0.5% for ventricular arrhythmias and sudden cardiac death. Nevertheless, a post-hoc analysis of the Dapagliflozin and Prevention of Adverse Outcomes in Heart Failure trial (DAPA-HF) showed reduced a risk reduction of 21% in ventricular arrhythmias and cardiac arrest in the dapagliflozin arm (hazard ratio 0.79 (95% confidence interval 0.63 to 0.99), although ventricular arrhythmias may have been underreported as they did not constitute a prespecified outcome.131 Similarly, in another post hoc analysis, dapagliflozin was associated with a 19% relative risk reduction in incident atrial arrhythmias compared with placebo among more than 17 000 patients who are diabetic, independent of any arrhythmic history.132
Emerging treatments
The EMPA-ICD study (jRCTs031180120) is underway and will examine SGLT2i effects on ventricular arrhythmias in patients with diabetes and an implanted defibrillator, clarifying whether their indications will extend beyond current guidelines. Similarly, ERASE, a multicentre, phase 3 study (NCT04600921), will report on the effects of ertugliflozin on ventricular arrhythmias in patients with heart failure irrespective of diabetic status. For AF burden, EMPA-AF (NCT04583813) will also report on the effect of empagliflozin and DAPA-AF (NCT04792190) will investigate use of dapagliflozin.
Guidelines
Guidelines for arrhythmia management include reference to weight management as a modifiable risk factor. The 2020 European Society for Cardiology guidelines for the diagnosis and management of AF developed in collaboration with the European Association for Cardio-Thoracic Surgery state that "given the potential to reduce AF episodes by weight reduction, AF catheter ablation should be offered to obese patients in conjunction with lifestyle modifications for weight reduction."133 Furthermore, patients who are overweight or obese that require radiofrequency ablation for AF should aim for more than a 10% weight reduction and a target body mass index of less than 27 to optimise outcomes.133 The guidelines mention that "weight loss, strict control of risk factors, and avoidance of triggers for AF are important strategies to improve outcome of rhythm control."133 The 2019 American Heart Association, American College of Cardiology, and Heart Rhythm Society also recommend weight loss for patients with AF who are overweight and obese.134
Conclusion
Obesity is a complex multisystem disorder that causes compensatory cardiovascular adaptations, culminating in electromechanical dysfunction. Atrial and ventricular electrophysiological remodelling in obesity manifest as detectable electrocardiographical changes. In atrial tissue, these changes can be explained by increased fibrosis, reduced conduction velocity, and increased conduction heterogeneity. Increasing adiposity, especially epicardial fat, is detrimental to atrial and ventricular electrophysiology due to paracrine effects and fatty infiltration, promoting a proarrhythmic substrate. Furthermore, the haemodynamic, lipotoxic, and mechanical consequences of increasing body mass results in cardiometabolic and ventilatory perturbations, such as hypertension, diabetes, and obstructive sleep apnoea. AF risk that is related to obesity is likely to be also partly mediated by these phenotypes. Compelling evidence suggests that lifestyle and surgical weight loss reduces AF burden, but evidence for a reduction in incident AF risk by either intervention remains uncertain. Evidence shows that treating hypertension, diabetes, and obstructive sleep apnoea might have additional anti-arrhythmic effects. Most recently, novel drugs have been identified to induce weight loss to a degree that is similar to bariatric surgery, although effects on reducing arrhythmias is yet to be established.
Questions for future research.
To what extent can any subclinical electrophysiological remodelling in arrhythmia-free morbidly obese (body mass index >40) patients be reversed with lifestyle or surgical weight reduction interventions?
To what extent do primary prevention weight reduction strategies reduce incidence of atrial and ventricular arrhythmias in morbidly obese (body mass index >40) patients?
How can obesity management be effectively delivered to groups who are at risk and in whom weight loss might be difficult to maintain, such as patients with mobility problems or learning difficulties?
What are the long term outcomes of bariatric surgery in children and young people with obesity?
Patient involvement.
No patients were asked for input in the creation of this article.
Footnotes
Twitter: @DrKiranPatel1, @DrFuSiongNg
Contributors: KHKP wrote, edited, and compiled the manuscript, and created the figures. RKR assisted with writing and editing the manuscript. AS, PS, and MA assisted with writing the manuscript. FSN reviewed the manuscript and provided critical appraisal. FSN is responsible for the overall content as guarantor and corresponding author.
Funding: This work was supported by British Heart Foundation Grant RG/16/3/32175 and RG/F/22/110078 (to FSN) and by the National Institute for Health Research Imperial Biomedical Research Council (NIHR Imperial BRC).
Competing interests: We have read and understood the BMJ policy on declaration of interests and declare the following interests: none.
Provenance and peer review: Commissioned; externally peer reviewed.
References
- 1. Maffetone PB, Rivera-Dominguez I, Laursen PB. Overfat and Underfat: new terms and definitions long overdue. Front Public Health 2016;4:279. 10.3389/fpubh.2016.00279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Organization WH . Obesity and overweight. Available: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweightfiles/25868/obesity-and-overweight.html
- 3. National Clinical Guideline C . National Institute for health and care excellence: guidelines. obesity: identification, assessment and management of overweight and obesity in children, young people and adults: partial update of CG43. London: National Institute for Health and Care Excellence (NICE) Copyright © National Clinical Guideline Centre, 2014. [PubMed] [Google Scholar]
- 4. Pouliot MC, Després JP, Lemieux S, et al. Waist circumference and abdominal sagittal diameter: best simple anthropometric indexes of abdominal visceral adipose tissue accumulation and related cardiovascular risk in men and women. Am J Cardiol 1994;73:460–8. 10.1016/0002-9149(94)90676-9 [DOI] [PubMed] [Google Scholar]
- 5. NICE . Surveillance report 2018 – obesity: identification, assessment and management (2014) NICE guideline CG189 and BMI: preventing ill health and premature death in black, Asian and other minority ethnic groups (2013) NICE guideline PH46. London: National Institute for Health and Care Excellence (NICE), 2018. [PubMed] [Google Scholar]
- 6. Alberti KGMM, Eckel RH, Grundy SM, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International diabetes Federation Task force on epidemiology and prevention; National heart, lung, and blood Institute; American heart association; world heart Federation; international atherosclerosis Society; and international association for the study of obesity. Circulation 2009;120:1640–5. 10.1161/CIRCULATIONAHA.109.192644 [DOI] [PubMed] [Google Scholar]
- 7. Chooi YC, Ding C, Magkos F. The epidemiology of obesity. Metabolism 2019;92:6–10. 10.1016/j.metabol.2018.09.005 [DOI] [PubMed] [Google Scholar]
- 8. Ford ND, Patel SA, Narayan KMV. Obesity in low- and middle-income countries: burden, drivers, and emerging challenges. Annu Rev Public Health 2017;38:145–64. 10.1146/annurev-publhealth-031816-044604 [DOI] [PubMed] [Google Scholar]
- 9. NCD Risk Factor Collaboration (NCD-RisC) . Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 2017;390:2627–42. 10.1016/S0140-6736(17)32129-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wang YC, McPherson K, Marsh T, et al. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet 2011;378:815–25. 10.1016/S0140-6736(11)60814-3 [DOI] [PubMed] [Google Scholar]
- 11. Kent S, Fusco F, Gray A, et al. Body mass index and healthcare costs: a systematic literature review of individual participant data studies. Obes Rev 2017;18:869–79. 10.1111/obr.12560 [DOI] [PubMed] [Google Scholar]
- 12. le Roux CW, Hartvig NV, Haase CL, et al. Obesity, cardiovascular risk and healthcare resource utilization in the UK. Eur J Prev Cardiol 2021;28:1235–41. 10.1177/2047487320925639 [DOI] [PubMed] [Google Scholar]
- 13. Ford ES, Mokdad AH. Epidemiology of obesity in the Western hemisphere. J Clin Endocrinol Metab 2008;93:s1–8. 10.1210/jc.2008-1356 [DOI] [PubMed] [Google Scholar]
- 14. Abed HS, Samuel CS, Lau DH, et al. Obesity results in progressive atrial structural and electrical remodeling: implications for atrial fibrillation. Heart Rhythm 2013;10:90–100. 10.1016/j.hrthm.2012.08.043 [DOI] [PubMed] [Google Scholar]
- 15. Movahed MR, Saito Y. Obesity is associated with left atrial enlargement, E/A reversal and left ventricular hypertrophy. Exp Clin Cardiol 2008;13:89–91. [PMC free article] [PubMed] [Google Scholar]
- 16. Stritzke J, Markus MRP, Duderstadt S, et al. The aging process of the heart: obesity is the main risk factor for left atrial enlargement during aging the MONICA/KORA (monitoring of trends and determinations in cardiovascular disease/cooperative research in the region of Augsburg) study. J Am Coll Cardiol 2009;54:1982–9. 10.1016/j.jacc.2009.07.034 [DOI] [PubMed] [Google Scholar]
- 17. Wang TJ, Parise H, Levy D, et al. Obesity and the risk of new-onset atrial fibrillation. JAMA 2004;292:2471–7. 10.1001/jama.292.20.2471 [DOI] [PubMed] [Google Scholar]
- 18. Chen LY, Soliman EZ. P wave Indices-Advancing our understanding of atrial Fibrillation-Related cardiovascular outcomes. Front Cardiovasc Med 2019;6:53. 10.3389/fcvm.2019.00053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Goyal SB, Spodick DH. Electromechanical dysfunction of the left atrium associated with interatrial block. Am Heart J 2001;142:823–7. 10.1067/mhj.2001.118110 [DOI] [PubMed] [Google Scholar]
- 20. Huxley RR, Lopez FL, Folsom AR, et al. Absolute and attributable risks of atrial fibrillation in relation to optimal and borderline risk factors: the Atherosclerosis risk in communities (ARIC) study. Circulation 2011;123:1501–8. 10.1161/CIRCULATIONAHA.110.009035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Magnani JW, Johnson VM, Sullivan LM, et al. P wave duration and risk of longitudinal atrial fibrillation in persons ≥ 60 years old (from the Framingham Heart Study). Am J Cardiol 2011;107:917–21. 10.1016/j.amjcard.2010.10.075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Maheshwari A, Norby FL, Soliman EZ, et al. Refining prediction of atrial fibrillation risk in the general population with analysis of P-Wave axis (from the Atherosclerosis risk in Communities study). Am J Cardiol 2017;120:1980–4. 10.1016/j.amjcard.2017.08.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Magnani JW, Lopez FL, Soliman EZ, et al. P wave indices, obesity, and the metabolic syndrome: the Atherosclerosis risk in Communities study. Obesity 2012;20:666–72. 10.1038/oby.2011.53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Falchi AG, Grecchi I, Muggia C, et al. Weight loss and P wave dispersion: a preliminary study. Obes Res Clin Pract 2014;8:e614–7. 10.1016/j.orcp.2014.08.005 [DOI] [PubMed] [Google Scholar]
- 25. Camm AJ, Naccarelli GV, Mittal S, et al. The increasing role of rhythm control in patients with atrial fibrillation: JACC state-of-the-art review. J Am Coll Cardiol 2022;79:1932–48. 10.1016/j.jacc.2022.03.337 [DOI] [PubMed] [Google Scholar]
- 26. Wong CX, Sullivan T, Sun MT, et al. Obesity and the Risk of Incident, Post-Operative, and Post-Ablation Atrial Fibrillation: A Meta-Analysis of 626,603 Individuals in 51 Studies. JACC Clin Electrophysiol 2015;1:139–52. 10.1016/j.jacep.2015.04.004 [DOI] [PubMed] [Google Scholar]
- 27. Wong CX, Sun MT, Odutayo A, et al. Associations of epicardial, abdominal, and overall adiposity with atrial fibrillation. Circ Arrhythm Electrophysiol 2016;9:e004378. 10.1161/CIRCEP.116.004378 [DOI] [PubMed] [Google Scholar]
- 28. Karasoy D, Bo Jensen T, Hansen ML, et al. Obesity is a risk factor for atrial fibrillation among fertile young women: a nationwide cohort study. Europace 2013;15:781–6. 10.1093/europace/eus422 [DOI] [PubMed] [Google Scholar]
- 29. Tsang TSM, Barnes ME, Miyasaka Y, et al. Obesity as a risk factor for the progression of paroxysmal to permanent atrial fibrillation: a longitudinal cohort study of 21 years. Eur Heart J 2008;29:2227–33. 10.1093/eurheartj/ehn324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ardissino M, Reddy RK, Slob EAW, et al. Sleep disordered breathing, obesity and atrial fibrillation: a Mendelian randomisation study. Genes 2022;13:104. 10.3390/genes13010104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Benjamin EJ, Levy D, Vaziri SM, et al. Independent risk factors for atrial fibrillation in a population-based cohort. The Framingham Heart Study. JAMA 1994;271:840–4. [PubMed] [Google Scholar]
- 32. Gami AS, Pressman G, Caples SM, et al. Association of atrial fibrillation and obstructive sleep apnea. Circulation 2004;110:364–7. 10.1161/01.CIR.0000136587.68725.8E [DOI] [PubMed] [Google Scholar]
- 33. Sacks HS, Fain JN. Human epicardial adipose tissue: a review. Am Heart J 2007;153:907–17. 10.1016/j.ahj.2007.03.019 [DOI] [PubMed] [Google Scholar]
- 34. Rabkin SW. The relationship between epicardial fat and indices of obesity and the metabolic syndrome: a systematic review and meta-analysis. Metab Syndr Relat Disord 2014;12:31–42. 10.1089/met.2013.0107 [DOI] [PubMed] [Google Scholar]
- 35. Patel KHK, Hwang T, Se Liebers C, et al. Epicardial adipose tissue as a mediator of cardiac arrhythmias. Am J Physiol Heart Circ Physiol 2022;322:H129–44. 10.1152/ajpheart.00565.2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Friedman DJ, Wang N, Meigs JB, et al. Pericardial fat is associated with atrial conduction: the Framingham Heart Study. J Am Heart Assoc 2014;3:e000477. 10.1161/JAHA.113.000477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Çiçek Y, Doğan S, Durakoğlugil ME, et al. The relationship between epicardial adipose tissue and P wave and QT dispersions. Turk Kardiyol Dern Ars 2015;43:621–9. 10.5543/tkda.2015.47598 [DOI] [PubMed] [Google Scholar]
- 38. Chi P-C, Chang S-C, Yun C-H, et al. The associations between various ectopic visceral adiposity and body surface electrocardiographic alterations: potential differences between local and remote systemic effects. PLoS One 2016;11:e0158300. 10.1371/journal.pone.0158300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Kwok CS, Rashid M, Beynon R, et al. Prolonged PR interval, first-degree heart block and adverse cardiovascular outcomes: a systematic review and meta-analysis. Heart 2016;102:672–80. 10.1136/heartjnl-2015-308956 [DOI] [PubMed] [Google Scholar]
- 40. Thanassoulis G, Massaro JM, O'Donnell CJ, et al. Pericardial fat is associated with prevalent atrial fibrillation: the Framingham Heart Study. Circ Arrhythm Electrophysiol 2010;3:345–50. 10.1161/CIRCEP.109.912055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Al Chekakie MO, Welles CC, Metoyer R, et al. Pericardial fat is independently associated with human atrial fibrillation. J Am Coll Cardiol 2010;56:784–8. 10.1016/j.jacc.2010.03.071 [DOI] [PubMed] [Google Scholar]
- 42. Wong CX, Abed HS, Molaee P, et al. Pericardial fat is associated with atrial fibrillation severity and ablation outcome. J Am Coll Cardiol 2011;57:1745–51. 10.1016/j.jacc.2010.11.045 [DOI] [PubMed] [Google Scholar]
- 43. Watanabe H, Tanabe N, Watanabe T, et al. Metabolic syndrome and risk of development of atrial fibrillation: the Niigata preventive medicine study. Circulation 2008;117:1255–60. 10.1161/CIRCULATIONAHA.107.744466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Mehra R, Benjamin EJ, Shahar E, et al. Association of nocturnal arrhythmias with sleep-disordered breathing: the sleep heart health study. Am J Respir Crit Care Med 2006;173:910–6. 10.1164/rccm.200509-1442OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Cadby G, McArdle N, Briffa T, et al. Severity of OSA is an independent predictor of incident atrial fibrillation hospitalization in a large sleep-clinic cohort. Chest 2015;148:945–52. 10.1378/chest.15-0229 [DOI] [PubMed] [Google Scholar]
- 46. Hall JE. Pathophysiology of obesity hypertension. Curr Hypertens Rep 2000;2:139–47. 10.1007/s11906-000-0073-4 [DOI] [PubMed] [Google Scholar]
- 47. Messerli FH, Sundgaard-Riise K, Reisin ED, et al. Dimorphic cardiac adaptation to obesity and arterial hypertension. Ann Intern Med 1983;99:757–61. 10.7326/0003-4819-99-6-757 [DOI] [PubMed] [Google Scholar]
- 48. Grundvold I, Skretteberg PT, Liestøl K, et al. Upper normal blood pressures predict incident atrial fibrillation in healthy middle-aged men: a 35-year follow-up study. Hypertension 2012;59:198–204. 10.1161/HYPERTENSIONAHA.111.179713 [DOI] [PubMed] [Google Scholar]
- 49. Pathak RK, Middeldorp ME, Meredith M, et al. Long-Term effect of goal-directed weight management in an atrial fibrillation cohort: a long-term follow-up study (legacy). J Am Coll Cardiol 2015;65:2159–69. 10.1016/j.jacc.2015.03.002 [DOI] [PubMed] [Google Scholar]
- 50. Papazoglou AS, Kartas A, Moysidis DV, et al. Glycemic control and atrial fibrillation: an intricate relationship, yet under investigation. Cardiovasc Diabetol 2022;21:39. 10.1186/s12933-022-01473-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Dublin S, Glazer NL, Smith NL, et al. Diabetes mellitus, glycemic control, and risk of atrial fibrillation. J Gen Intern Med 2010;25:853–8. 10.1007/s11606-010-1340-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Huxley RR, Alonso A, Lopez FL, et al. Type 2 diabetes, glucose homeostasis and incident atrial fibrillation: the Atherosclerosis risk in Communities study. Heart 2012;98:133–8. 10.1136/heartjnl-2011-300503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Donnellan E, Aagaard P, Kanj M, et al. Association Between Pre-Ablation Glycemic Control and Outcomes Among Patients With Diabetes Undergoing Atrial Fibrillation Ablation. JACC Clin Electrophysiol 2019;5:897–903. 10.1016/j.jacep.2019.05.018 [DOI] [PubMed] [Google Scholar]
- 54. Lu Z-H, Liu N, Bai R, et al. HbA1c levels as predictors of ablation outcome in type 2 diabetes mellitus and paroxysmal atrial fibrillation. Herz 2015;40 Suppl 2:130–6. 10.1007/s00059-014-4154-6 [DOI] [PubMed] [Google Scholar]
- 55. Pappone C, Radinovic A, Manguso F, et al. Atrial fibrillation progression and management: a 5-year prospective follow-up study. Heart Rhythm 2008;5:1501–7. 10.1016/j.hrthm.2008.08.011 [DOI] [PubMed] [Google Scholar]
- 56. Benichou T, Pereira B, Mermillod M, et al. Heart rate variability in type 2 diabetes mellitus: a systematic review and meta-analysis. PLoS One 2018;13:e0195166. 10.1371/journal.pone.0195166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Wang A, Green JB, Halperin JL, et al. Atrial fibrillation and diabetes mellitus: JACC review topic of the week. J Am Coll Cardiol 2019;74:1107–15. 10.1016/j.jacc.2019.07.020 [DOI] [PubMed] [Google Scholar]
- 58. Xiong Z, Liu T, Tse G, et al. A machine learning aided systematic review and meta-analysis of the relative risk of atrial fibrillation in patients with diabetes mellitus. Front Physiol 2018;9:835. 10.3389/fphys.2018.00835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Holmqvist F, Guan N, Zhu Z, et al. Impact of obstructive sleep apnea and continuous positive airway pressure therapy on outcomes in patients with atrial fibrillation-Results from the outcomes Registry for better informed treatment of atrial fibrillation (ORBIT-AF). Am Heart J 2015;169:647–54. 10.1016/j.ahj.2014.12.024 [DOI] [PubMed] [Google Scholar]
- 60. Gami AS, Hodge DO, Herges RM, et al. Obstructive sleep apnea, obesity, and the risk of incident atrial fibrillation. J Am Coll Cardiol 2007;49:565–71. 10.1016/j.jacc.2006.08.060 [DOI] [PubMed] [Google Scholar]
- 61. Mehra R, Stone KL, Varosy PD, et al. Nocturnal arrhythmias across a spectrum of obstructive and central sleep-disordered breathing in older men: outcomes of sleep disorders in older men (MROS sleep) study. Arch Intern Med 2009;169:1147–55. 10.1001/archinternmed.2009.138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Yaeger A, Keenan BT, Cash NR, et al. Impact of a nurse-led limited risk factor modification program on arrhythmia outcomes in patients with atrial fibrillation undergoing catheter ablation. J Cardiovasc Electrophysiol 2020;31:423–31. 10.1111/jce.14336 [DOI] [PubMed] [Google Scholar]
- 63. Srivali N, Chahal AC, Mansukhani MP, et al. The effect of positive airway pressure treatment of obstructive and central sleep apnea on the recurrence of atrial Fibrillation/Flutter Postintervention. J Clin Sleep Med 2019;15:1459–68. 10.5664/jcsm.7976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Romero-Corral A, Caples SM, Lopez-Jimenez F, et al. Interactions between obesity and obstructive sleep apnea: implications for treatment. Chest 2010;137:711–9. 10.1378/chest.09-0360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Phillips BG, Kato M, Narkiewicz K, et al. Increases in leptin levels, sympathetic drive, and weight gain in obstructive sleep apnea. Am J Physiol Heart Circ Physiol 2000;279:H234–7. 10.1152/ajpheart.2000.279.1.H234 [DOI] [PubMed] [Google Scholar]
- 66. Chen W, Cai X, Yan H, et al. Causal effect of obstructive sleep apnea on atrial fibrillation: a Mendelian randomization study. J Am Heart Assoc 2021;10:e022560. 10.1161/JAHA.121.022560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Malik M, Batchvarov VN. Measurement, interpretation and clinical potential of QT dispersion. J Am Coll Cardiol 2000;36:1749–66. 10.1016/S0735-1097(00)00962-1 [DOI] [PubMed] [Google Scholar]
- 68. Omran J, Firwana B, Koerber S, et al. Effect of obesity and weight loss on ventricular repolarization: a systematic review and meta-analysis. Obes Rev 2016;17:520–30. 10.1111/obr.12390 [DOI] [PubMed] [Google Scholar]
- 69. Omran J, Bostick BP, Chan AK, et al. Obesity and ventricular repolarization: a comprehensive review. Prog Cardiovasc Dis 2018;61:124–35. 10.1016/j.pcad.2018.04.004 [DOI] [PubMed] [Google Scholar]
- 70. Yılmaz M, Altın C, Tekin A, et al. Assessment of atrial fibrillation and ventricular arrhythmia risk after bariatric surgery by P Wave/QT interval dispersion. Obes Surg 2018;28:932–8. 10.1007/s11695-017-2923-z [DOI] [PubMed] [Google Scholar]
- 71. Sanches EE, Topal B, de Jongh FW, et al. Effects of bariatric surgery on heart rhythm disorders: a systematic review and meta-analysis. Obes Surg 2021;31:2278–90. 10.1007/s11695-021-05314-z [DOI] [PubMed] [Google Scholar]
- 72. Mshui ME, Saikawa T, Ito K, et al. QT interval and QT dispersion before and after diet therapy in patients with simple obesity. Proc Soc Exp Biol Med 1999;220:133–8. 10.1046/j.1525-1373.1999.d01-20.x [DOI] [PubMed] [Google Scholar]
- 73. Aune D, Schlesinger S, Norat T, et al. Body mass index, abdominal fatness, and the risk of sudden cardiac death: a systematic review and dose-response meta-analysis of prospective studies. Eur J Epidemiol 2018;33:711–22. 10.1007/s10654-017-0353-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Pietrasik G, Goldenberg I, McNitt S, et al. Obesity as a risk factor for sustained ventricular tachyarrhythmias in MADIT II patients. J Cardiovasc Electrophysiol 2007;18:181–4. 10.1111/j.1540-8167.2006.00680.x [DOI] [PubMed] [Google Scholar]
- 75. Bikkina M, Larson MG, Levy D. Asymptomatic ventricular arrhythmias and mortality risk in subjects with left ventricular hypertrophy. J Am Coll Cardiol 1993;22:1111–6. 10.1016/0735-1097(93)90424-y [DOI] [PubMed] [Google Scholar]
- 76. Opthof T, Janse MJ, Meijborg VMF, et al. Dispersion in ventricular repolarization in the human, canine and porcine heart. Prog Biophys Mol Biol 2016;120:222–35. 10.1016/j.pbiomolbio.2016.01.007 [DOI] [PubMed] [Google Scholar]
- 77. Abed HS, Wittert GA, Leong DP, et al. Effect of weight reduction and cardiometabolic risk factor management on symptom burden and severity in patients with atrial fibrillation: a randomized clinical trial. JAMA 2013;310:2050–60. 10.1001/jama.2013.280521 [DOI] [PubMed] [Google Scholar]
- 78. Pathak RK, Middeldorp ME, Lau DH, et al. Aggressive risk factor reduction study for atrial fibrillation and implications for the outcome of ablation: the ARREST-AF cohort study. J Am Coll Cardiol 2014;64:2222–31. 10.1016/j.jacc.2014.09.028 [DOI] [PubMed] [Google Scholar]
- 79. Middeldorp ME, Pathak RK, Meredith M, et al. Prevention and regressive effect of weight-loss and risk factor modification on atrial fibrillation: the REVERSE-AF study. Europace 2018;20:1929–35. 10.1093/europace/euy117 [DOI] [PubMed] [Google Scholar]
- 80. Qureshi WT, Alirhayim Z, Blaha MJ, et al. Cardiorespiratory fitness and risk of incident atrial fibrillation: results from the Henry Ford exercise testing (fit) project. Circulation 2015;131:1827–34. 10.1161/CIRCULATIONAHA.114.014833 [DOI] [PubMed] [Google Scholar]
- 81. UK NCGC . Obesity: identification, assessment and management of overweight and obesity in children, young people and adults, 2014. [PubMed] [Google Scholar]
- 82. Halawi H, Khemani D, Eckert D, et al. Effects of liraglutide on weight, satiation, and gastric functions in obesity: a randomised, placebo-controlled pilot trial. Lancet Gastroenterol Hepatol 2017;2:890–9. 10.1016/S2468-1253(17)30285-6 [DOI] [PubMed] [Google Scholar]
- 83. Rubino D, Abrahamsson N, Davies M, et al. Effect of continued Weekly subcutaneous Semaglutide vs placebo on weight loss maintenance in adults with overweight or obesity: the step 4 randomized clinical trial. JAMA 2021;325:1414–25. 10.1001/jama.2021.3224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Blackman A, Foster GD, Zammit G, et al. Effect of liraglutide 3.0 mg in individuals with obesity and moderate or severe obstructive sleep apnea: the SCALE Sleep Apnea randomized clinical trial. Int J Obes 2016;40:1310–9. 10.1038/ijo.2016.52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Wadden TA, Bailey TS, Billings LK, et al. Effect of subcutaneous Semaglutide vs placebo as an adjunct to intensive behavioral therapy on body weight in adults with overweight or obesity: the step 3 randomized clinical trial. JAMA 2021;325:1403–13. 10.1001/jama.2021.1831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Rubino DM, Greenway FL, Khalid U, et al. Effect of Weekly subcutaneous Semaglutide vs daily liraglutide on body weight in adults with overweight or obesity without diabetes: the step 8 randomized clinical trial. JAMA 2022;327:138–50. 10.1001/jama.2021.23619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Wadden TA, Tronieri JS, Sugimoto D, et al. Liraglutide 3.0 Mg and intensive behavioral therapy (IBT) for obesity in primary care: the scale IBT randomized controlled trial. Obesity 2020;28:529–36. 10.1002/oby.22726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Wilding JPH, Batterham RL, Calanna S, et al. Once-Weekly Semaglutide in adults with overweight or obesity. N Engl J Med 2021;384:989–1002. 10.1056/NEJMoa2032183 [DOI] [PubMed] [Google Scholar]
- 89. Davies M, Færch L, Jeppesen OK, et al. Semaglutide 2·4 mg once a week in adults with overweight or obesity, and type 2 diabetes (step 2): a randomised, double-blind, double-dummy, placebo-controlled, phase 3 trial. Lancet 2021;397:971–84. 10.1016/S0140-6736(21)00213-0 [DOI] [PubMed] [Google Scholar]
- 90. Acosta A, Abu Dayyeh BK, Port JD, et al. Recent advances in clinical practice challenges and opportunities in the management of obesity. Gut 2014;63:687–95. 10.1136/gutjnl-2013-306235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Monami M, Nreu B, Scatena A, et al. Glucagon-like peptide-1 receptor agonists and atrial fibrillation: a systematic review and meta-analysis of randomised controlled trials. J Endocrinol Invest 2017;40:1251–8. 10.1007/s40618-017-0698-7 [DOI] [PubMed] [Google Scholar]
- 92. Picot J, Jones J, Colquitt JL, et al. The clinical effectiveness and cost-effectiveness of bariatric (weight loss) surgery for obesity: a systematic review and economic evaluation. Health Technol Assess 2009;13:1–190. 215-357, iii-iv. 10.3310/hta13410 [DOI] [PubMed] [Google Scholar]
- 93. Donnellan E, Wazni O, Kanj M, et al. Outcomes of atrial fibrillation ablation in morbidly obese patients following bariatric surgery compared with a nonobese cohort. Circ Arrhythm Electrophysiol 2019;12:e007598. 10.1161/CIRCEP.119.007598 [DOI] [PubMed] [Google Scholar]
- 94. Mohanty S, Mohanty P, Natale V, et al. Impact of weight loss on ablation outcome in obese patients with longstanding persistent atrial fibrillation. J Cardiovasc Electrophysiol 2018;29:246–53. 10.1111/jce.13394 [DOI] [PubMed] [Google Scholar]
- 95. Moussa O, Ardissino M, Eichhorn C, et al. Atrial fibrillation and obesity: long-term incidence and outcomes after bariatric surgery. Eur J Prev Cardiol 2021;28:e22–4. 10.1177/2047487320904515 [DOI] [PubMed] [Google Scholar]
- 96. van Veldhuisen SL, Gorter TM, van Woerden G, et al. Bariatric surgery and cardiovascular disease: a systematic review and meta-analysis. Eur Heart J 2022;43:1955–69. 10.1093/eurheartj/ehac071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Dalmar A, Singh M, Heis Z, et al. Risk of atrial fibrillation and stroke after bariatric surgery in patients with morbid obesity with or without obstructive sleep apnea. Stroke 2021;52:2266–74. 10.1161/STROKEAHA.120.031920 [DOI] [PubMed] [Google Scholar]
- 98. Alonso A, Bahnson JL, Gaussoin SA, et al. Effect of an intensive lifestyle intervention on atrial fibrillation risk in individuals with type 2 diabetes: the look ahead randomized trial. Am Heart J 2015;170:770–7. 10.1016/j.ahj.2015.07.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Sjöström L, Lindroos A-K, Peltonen M, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med 2004;351:2683–93. 10.1056/NEJMoa035622 [DOI] [PubMed] [Google Scholar]
- 100. Plourde B, Sarrazin J-F, Nault I, et al. Sudden cardiac death and obesity. Expert Rev Cardiovasc Ther 2014;12:1099–110. 10.1586/14779072.2014.952283 [DOI] [PubMed] [Google Scholar]
- 101. Adabag S, Huxley RR, Lopez FL, et al. Obesity related risk of sudden cardiac death in the Atherosclerosis risk in Communities study. Heart 2015;101:215–21. 10.1136/heartjnl-2014-306238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Hookana E, Junttila MJ, Puurunen V-P, et al. Causes of nonischemic sudden cardiac death in the current era. Heart Rhythm 2011;8:1570–5. 10.1016/j.hrthm.2011.06.031 [DOI] [PubMed] [Google Scholar]
- 103. Sabbag A, Goldenberg I, Moss AJ, et al. Predictors and Risk of Ventricular Tachyarrhythmias or Death in Black and White Cardiac Patients: A MADIT-CRT Trial Substudy. JACC Clin Electrophysiol 2016;2:448–55. 10.1016/j.jacep.2016.03.003 [DOI] [PubMed] [Google Scholar]
- 104. Chen H, Wang X, Xiong C, et al. The negative effects of obesity on heart, especially the electrophysiology of the heart. Artif Cells Nanomed Biotechnol 2020;48:1055–62. 10.1080/21691401.2020.1770269 [DOI] [PubMed] [Google Scholar]
- 105. Fraley MA, Birchem JA, Senkottaiyan N, et al. Obesity and the electrocardiogram. Obes Rev 2005;6:275–81. 10.1111/j.1467-789X.2005.00199.x [DOI] [PubMed] [Google Scholar]
- 106. Chatterjee S, Bavishi C, Sardar P, et al. Meta-analysis of left ventricular hypertrophy and sustained arrhythmias. Am J Cardiol 2014;114:1049–52. 10.1016/j.amjcard.2014.07.015 [DOI] [PubMed] [Google Scholar]
- 107. Pedersen OD, Bagger H, Kober L, et al. Trandolapril reduces the incidence of atrial fibrillation after acute myocardial infarction in patients with left ventricular dysfunction. Circulation 1999;100:376–80. 10.1161/01.CIR.100.4.376 [DOI] [PubMed] [Google Scholar]
- 108. Madrid AH, Bueno MG, Rebollo JMG, et al. Use of irbesartan to maintain sinus rhythm in patients with long-lasting persistent atrial fibrillation: a prospective and randomized study. Circulation 2002;106:331–6. 10.1161/01.cir.0000022665.18619.83 [DOI] [PubMed] [Google Scholar]
- 109. Lurie A. Obstructive sleep apnea in adults: epidemiology, clinical presentation, and treatment options. In: Obstructive sleep apnea in adults. 46. Karger Publishers, 2011: 1–42. [DOI] [PubMed] [Google Scholar]
- 110. Abumuamar AM, Newman D, Dorian P, et al. Cardiac effects of CPAP treatment in patients with obstructive sleep apnea and atrial fibrillation. J Interv Card Electrophysiol 2019;54:289–97. 10.1007/s10840-018-0482-4 [DOI] [PubMed] [Google Scholar]
- 111. Patel N, Donahue C, Shenoy A, et al. Obstructive sleep apnea and arrhythmia: a systemic review. Int J Cardiol 2017;228:967–70. 10.1016/j.ijcard.2016.11.137 [DOI] [PubMed] [Google Scholar]
- 112. Linz D, McEvoy RD, Cowie MR, et al. Associations of obstructive sleep apnea with atrial fibrillation and continuous positive airway pressure treatment: a review. JAMA Cardiol 2018;3:532–40. 10.1001/jamacardio.2018.0095 [DOI] [PubMed] [Google Scholar]
- 113. Li L, Wang Z-wu, Li J, et al. Efficacy of catheter ablation of atrial fibrillation in patients with obstructive sleep apnoea with and without continuous positive airway pressure treatment: a meta-analysis of observational studies. Europace 2014;16:1309–14. 10.1093/europace/euu066 [DOI] [PubMed] [Google Scholar]
- 114. Shukla A, Aizer A, Holmes D, et al. Effect of Obstructive Sleep Apnea Treatment on Atrial Fibrillation Recurrence: A Meta-Analysis. JACC Clin Electrophysiol 2015;1:41–51. 10.1016/j.jacep.2015.02.014 [DOI] [PubMed] [Google Scholar]
- 115. Li X, Zhou X, Xu X, et al. Effects of continuous positive airway pressure treatment in obstructive sleep apnea patients with atrial fibrillation: a meta-analysis. Medicine 2021;100:e25438. 10.1097/MD.0000000000025438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Yang Y, Ning Y, Wen W, et al. CPAP is associated with decreased risk of AF recurrence in patients with OSA, especially those younger and slimmer: a meta-analysis. J Interv Card Electrophysiol 2020;58:369–79. 10.1007/s10840-020-00738-6 [DOI] [PubMed] [Google Scholar]
- 117. Qureshi WT, Nasir UB, Alqalyoobi S, et al. Meta-Analysis of continuous positive airway pressure as a therapy of atrial fibrillation in obstructive sleep apnea. Am J Cardiol 2015;116:1767–73. 10.1016/j.amjcard.2015.08.046 [DOI] [PubMed] [Google Scholar]
- 118. Traaen GM, Aakerøy L, Hunt T-E, et al. Effect of continuous positive airway pressure on arrhythmia in atrial fibrillation and sleep apnea: a randomized controlled trial. Am J Respir Crit Care Med 2021;204:573–82. 10.1164/rccm.202011-4133OC [DOI] [PubMed] [Google Scholar]
- 119. Hunt T-E, Traaen GM, Aakerøy L, et al. Effect of continuous positive airway pressure therapy on recurrence of atrial fibrillation after pulmonary vein isolation in patients with obstructive sleep apnea: a randomized controlled trial. Heart Rhythm 2022;19:1433–41. 10.1016/j.hrthm.2022.06.016 [DOI] [PubMed] [Google Scholar]
- 120. Moran GM, Bakhai C, Song SH, et al. Type 2 diabetes: summary of updated NICE guidance. BMJ 2022;377:o775. 10.1136/bmj.o775 [DOI] [PubMed] [Google Scholar]
- 121. Chang S-H, Wu L-S, Chiou M-J, et al. Association of metformin with lower atrial fibrillation risk among patients with type 2 diabetes mellitus: a population-based dynamic cohort and in vitro studies. Cardiovasc Diabetol 2014;13:123. 10.1186/s12933-014-0123-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Deshmukh A, Ghannam M, Liang J, et al. Effect of metformin on outcomes of catheter ablation for atrial fibrillation. J Cardiovasc Electrophysiol 2021;32:1232–9. 10.1111/jce.14954 [DOI] [PubMed] [Google Scholar]
- 123. Neal B, Perkovic V, Mahaffey KW, et al. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med 2017;377:644–57. 10.1056/NEJMoa1611925 [DOI] [PubMed] [Google Scholar]
- 124. Wiviott SD, Raz I, Bonaca MP, et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med 2019;380:347–57. 10.1056/NEJMoa1812389 [DOI] [PubMed] [Google Scholar]
- 125. Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med 2015;373:2117–28. 10.1056/NEJMoa1504720 [DOI] [PubMed] [Google Scholar]
- 126. Packer M, Anker SD, Butler J, et al. Cardiovascular and renal outcomes with Empagliflozin in heart failure. N Engl J Med 2020;383:1413–24. 10.1056/NEJMoa2022190 [DOI] [PubMed] [Google Scholar]
- 127. McMurray JJV, Solomon SD, Inzucchi SE, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med 2019;381:1995–2008. 10.1056/NEJMoa1911303 [DOI] [PubMed] [Google Scholar]
- 128. Fernandes GC, Fernandes A, Cardoso R, et al. Association of SGLT2 inhibitors with arrhythmias and sudden cardiac death in patients with type 2 diabetes or heart failure: a meta-analysis of 34 randomized controlled trials. Heart Rhythm 2021;18:1098–105. 10.1016/j.hrthm.2021.03.028 [DOI] [PubMed] [Google Scholar]
- 129. Pandey AK, Okaj I, Kaur H, et al. Sodium-Glucose co-transporter inhibitors and atrial fibrillation: a systematic review and meta-analysis of randomized controlled trials. J Am Heart Assoc 2021;10:e022222. 10.1161/JAHA.121.022222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Ling AW-C, Chan C-C, Chen S-W, et al. The risk of new-onset atrial fibrillation in patients with type 2 diabetes mellitus treated with sodium glucose cotransporter 2 inhibitors versus dipeptidyl peptidase-4 inhibitors. Cardiovasc Diabetol 2020;19:188. 10.1186/s12933-020-01162-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Curtain JP, Docherty KF, Jhund PS, et al. Effect of dapagliflozin on ventricular arrhythmias, resuscitated cardiac arrest, or sudden death in DAPA-HF. Eur Heart J 2021;42:3727–38. 10.1093/eurheartj/ehab560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Zelniker TA, Bonaca MP, Furtado RHM, et al. Effect of dapagliflozin on atrial fibrillation in patients with type 2 diabetes mellitus: insights from the DECLARE-TIMI 58 trial. Circulation 2020;141:1227–34. 10.1161/CIRCULATIONAHA.119.044183 [DOI] [PubMed] [Google Scholar]
- 133. Hindricks G, Potpara T, Dagres N, et al. 2020 ESC guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European association for Cardio-Thoracic surgery (EACTS): the task force for the diagnosis and management of atrial fibrillation of the European Society of cardiology (ESC) developed with the special contribution of the European heart rhythm association (EHRA) of the ESC. Eur Heart J 2021;42:373–498. 10.1093/eurheartj/ehaa612 [DOI] [PubMed] [Google Scholar]
- 134. January CT, Wann LS, Calkins H, et al. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American heart association Task force on clinical practice guidelines and the heart rhythm society in collaboration with the Society of thoracic surgeons. Circulation 2019;140:e125–51. 10.1161/CIR.0000000000000665 [DOI] [PubMed] [Google Scholar]