Abstract
TDP-43 is the primary or secondary pathological hallmark of neurodegenerative diseases, such as amyotrophic lateral sclerosis, half of frontotemporal dementia cases, and limbic age-related TDP-43 encephalopathy, which clinically resembles Alzheimer’s dementia. In such diseases, a biomarker that can detect TDP-43 proteinopathy in life would help to stratify patients according to their definite diagnosis of pathology, rather than in clinical subgroups of uncertain pathology. For therapies developed to target pathological proteins that cause the disease a biomarker to detect and track the underlying pathology would greatly enhance such undertakings. This article reviews the latest developments and outlooks of deriving TDP-43-specific biomarkers from the pathophysiological processes involved in the development of TDP-43 proteinopathy and studies using biosamples from clinical entities associated with TDP-43 pathology to investigate biomarker candidates.
Keywords: TDP-43, biomarker, neurodegeneration, amyotrophic lateral sclerosis, frontotemporal dementia, dementia, cerebrospinal fluid, biofluid
1. Introduction
Amyotrophic lateral sclerosis (ALS) and frontotemporal dementia (FTD) are diagnosed based on clinical criteria. Often, this leads to a delay between the onset of symptoms and diagnosis up to one year in ALS and 5 years in FTD, narrowing the window where potentially disease-modifying therapies would likely be most effective [1,2,3,4,5]. In order to intervene early and effectively in those diseases, biomarkers reflective of the underlying core pathobiology are needed [6,7]. These biomarkers will serve to identify the right cohorts for therapeutic targets and to determine the efficacy of therapies and clinical trials more accurately [8].
Ubiquitinated cytoplasmic aggregates of the nuclear 43 kDa transactive-response, DNA-binding protein, TDP-43, is the core pathobiology in almost all cases (97%) of ALS [9]. TDP-43 pathology is also found in 50% of frontotemporal lobar degeneration (FTLD) cases, most commonly associated with the clinical syndrome of behavioral variant frontotemporal dementia (bvFTD), while the rest is associated with tau protein pathology [10,11,12]. The interest in TDP-43 proteinopathies has further broadened since TDP-43 neuropathology has been found in 30% of Alzheimer’s disease (AD) cases [13,14]. Neuropathological evidence of TDP-43 pathology in AD has recently been defined as limbic-predominant age-related TDP-43 encephalopathy (LATE), which can present itself with or without coexisting hippocampal sclerosis pathology [15].
The clinical heterogeneity ranging from pure motor (ALS) to cognitively impaired (ALS-FTD) or dementia (FTD, LATE) phenotypes that are associated with TDP-43 proteinopathy is striking and likely associated with a distinct topographical distribution of TDP-43 pathology in the brain [16,17]. Pathological TDP-43 in ALS predominantly involves the spinal cord and the motor cortex but can be more widespread in the frontal and temporal lobe structures [18]. In FTD, TDP-43 is mostly found in the orbitofrontal cortex, but can exceed into the frontal and temporal cortices before involving the motor system, visual cortex, and cerebellum [19]. In contrast, TDP-43 pathology in LATE is mostly localized to the hippocampus and amygdala, suggesting that a selective cellular and regional vulnerability contributes to the disease [15]. There is, indeed, increasing evidence that TDP-43 functionality can be shaped depending on cell type [20,21]. Different types of TDP-43 pathology can be found in ALS/FTD clinical phenotypes; for example, type B pathology with large cytoplasmic inclusions and few dendritic neurites is mostly associated with ALS and bvFTD [22]. The clinical heterogeneity among FTD (bvFTD or primary progressive aphasia (PPA)) and the clinical similarity of LATE to AD makes it difficult to accurately predict the underlying pathology in life. At present, stratifying patients by core pathology and their assignment in treatment trials designed to interfere with TDP-43 pathobiology is not yet possible, except for rare well-defined genetic cases [23]. Hence, it is paramount to develop TDP-43 molecule-specific biomarkers.
Here, we will review the latest developments and outlooks of deriving TDP-43-specific biomarkers from: (1) pathophysiological processes involved in the development of TDP-43 proteinopathy, and (2) biofluid studies using biosamples from clinical entities associated with TDP-43 pathology. We identified the existing evidence through author knowledge and PubMed searches from the database’s inception to April 2022.
2. TDP-43 Pathobiology Informed Biomarker Development
2.1. Cellular Homeostasis and Aggregation Propensity
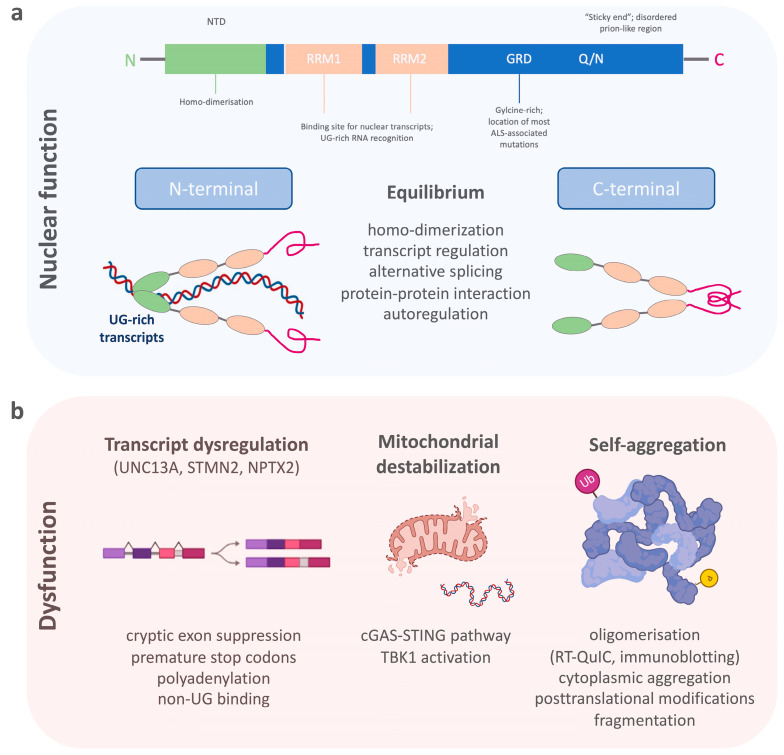
TDP-43 belongs to a family of heterogeneous nuclear ribonucleoproteins (hnRNP) [24]. Structurally, TDP-43 consists of a structured N-terminal domain (NTD) involved in physiological self-oligomerization, followed by two tandem RNA-recognition motifs (RRM), which bind to certain nuclear transcripts and therefore regulate important DNA/RNA metabolism functions (Figure 1a) [25,26,27,28,29]. The RRMs are flanked by N- and C-terminal regions. The C-terminal end of TDP-43 is a conserved, glycine-rich region important for the function of alternative splicing, protein–protein interactions and to promote the formation of phase-separated RNA granules [30,31,32,33,34]. The C-terminal domain of TDP-43 is also affected by most ALS-associated genetic variants [35,36], which, together with changes in RNA levels, can enhance the formation of dynamic liquid-like condensates [37,38]. In addition, an intrinsically disordered (IDR) prion-like region within the C-terminus harbors a tendency to self-assemble (“sticky ends”) and to form different oligomeric states [39,40]. There is, therefore, a critical equilibrium between TDP-43′s physiological function and its soluble form [25]. TDP-43 preferentially binds to long UG-rich sequences, including its own mRNA, via N-terminal homo-dimerization and its C-terminal conserved region [28,41,42,43]. Many of these regions have been found to be selectively modified by a variety of post-translational modifications, which include phosphorylation, acetylation, and SUMOylation [44]. Many of these events are now known to act as drivers of the pathology mostly by modifying the phase separation properties of this protein [45,46].
Figure 1.
The schematic shows (a) the structure of TDP-43 and its importance for the physiological functions within the cell nucleus, and (b) the dysfunctional state of TDP-43 with the dysregulation of its nuclear function, destabilization of mitochondria, and its aggregation propensity.
Pathological processes that disturb the selective binding mechanism of TDP-43 enhance homonymous binding and self-aggregation, disturb its autoregulation, and lead to increased concentrations of TDP-43-aggravating protein accumulation (Figure 1b) [47,48]. Its potential for dimerization and oligomerization and the transcellular transmission of such TDP-43 oligomers has been shown in in vitro experiments [49,50,51]. Such self-aggregation and seeding propensities of misfolded proteins have been exploited for diagnostic purposes in prion disease, and later, a-synuclein and ß-amyloid pathologies using real-time quaking-induced conversion (RT-QuIC) [52,53,54,55]. Therefore, RT-QuIC for inducing TDP-43′s intrinsic aggregation propensity into non-amyloid, fibrillar aggregates, seemed a plausible technique for the detection of pathological TDP-43 species in patient biosamples [56,57,58]. A major requisite for developing RT-QuIC was achieved by producing functionally intact recombinant full-length and C-terminal fragmented TDP-43 species, which after mechanical and heat activation were able to seed amorphous TDP-43 aggregates or fibrillary structures in a measurable time frame [59]. This technique was then employed for cerebrospinal fluid (CSF) samples from patients with genetically confirmed TDP-43 proteinopathy and normal controls using the recombinant C-terminal fragment. A positive RT-QuIC reaction was obtained from TDP-43 positive samples with a high sensitivity of 94% and specificity of 85%. However, the limitations of this study were the false positive results, possibly originating from the presence of low levels of TDP-43 aggregates in healthy subjects, or by the heterogeneous presence of contaminants in the CSF, which needs to be tested in future studies. Another technique that uses aggregate formations of TDP-43 as a readout for TDP-43 proteinopathy is immuno-infrared sensor technology [60]. Here, TDP-43 is captured from CSF using oligoclonal antibodies targeting the aminoacid epitopes 130–275 of TDP-43. Bound TDP-43 is then measured by an infrared beam to assess the absorbance maximum indicative of the presence of an alpha-helical or β-sheet structure. The comparison of CSF from patients with ALS and Parkinson’s disease (PD), as well as neurological controls, demonstrated an increase in the β-sheet structures in CSF samples of ALS compared to PD and control samples. This approach displayed a diagnostic accuracy to discriminate ALS from PD (or controls) with 89% (89%) sensitivity and 77% (83%) specificity, with the caveat that this study lacked direct evidence of antibody-bound TDP-43 by immunoblotting. In summary, the self-aggregation propensity of TDP-43 has become a valuable tool for developing in vivo diagnostics; whether these techniques have the potential to be standardized for routine measurements requires further research.
2.2. Post Mortem TDP-43 Proteinopathy
The pathology of TDP-43 in ALS and FTD is characterized by its mislocalization from the nucleus to the cytoplasm of neurons and glia cells, where it is found post-translationally modified by phosphorylation and ubiquitination, as well as N-terminally cleaved into smaller C-terminal fragments (CTF) [9]. Neuropathological studies in ALS and FTD have shown that the phosphorylated form of TDP-43 is distributed in a relatively stereotyped spectrum of anatomical patterns, which has led to the definition of neuropathological stages [18,19]. In addition, the subtypes of characteristic TDP-43 staining were classified as different types (A–E) of TDP-43 proteinopathy, often characteristic for certain clinical syndromes within the ALS-FTD spectrum [61,62]. Both the regional localization of TDP-43 and the type of TDP-43 pathology are associated with a variable degree of cellular degeneration reaching from moderate whole-brain atrophy in ALS [63] to more severe focal frontal/temporal tissue loss in FTD [64].
Ultimately, a major breakthrough in neuropathology was achieved when the serial fractionation of post mortem brain tissue led to the extraction of insoluble proteins, which specifically recovered pathological TDP-43 from the affected brain regions [9]. A characteristic biochemical pattern of TDP-43 from the insoluble protein fraction includes a high molecular weight smear, which likely reflects phosphorylated and ubiquitinated TDP-43, phosphorylated full-length TDP-43 with a molecular mass size of 45–50 kDa and 60 kDa, and truncated forms at 24–26 kDa, identified as C-terminal fragments of TDP-43. C-terminal fragments and post-translational modifications of TDP-43 have been a prominent hypothesis proposed for TDP-43-associated neuronal toxicity and pathobiology [65,66]. Several studies therefore exploited the enrichment of pathological TDP-43 species from post mortem tissue in order to find a pathology-specific TDP-43 biomarker [9,10,67]. By mass spectrometry analysis, TDP-43 post-translational modifications or pathological peptide sequences were identified without the limitations of antibody-based methods. This approach enabled the identification of the pathological phosphorylation sites of TDP-43 predominantly located at its C-terminal glycine-rich domain [67,68]. These findings confirmed the disease-specificity of phosphorylated TDP-43 from previous studies using phosphorylation dependent TDP-43 antibodies [69]. Regarding phosphorylation, a recent important development has also occurred following the isolation of TDP-43 fibrils from post mortem brain samples and their analysis using mass-spec. This approach has allowed us to start investigating possible PTM differences between the different types of TDP-43 pathology in GRN vs. C9ORF72 cases [70]. Further, a proteomic approach using post mortem tissue from different subtypes of TDP-43 proteinopathies allowed the identification of subtype-specific insoluble proteomes [71], while a similar approach using ALS post mortem tissue enabled the characterization of peptide sequences that were representative of TDP-43 protein fragments [67]. This work showed that peptides with a non-enzymatic N-terminal truncation site are representative of an endogenously cleaved C-terminal fragment, while less common peptides with a C-terminal truncation site represented N-terminal TDP-43 fragments. This was then taken forward to develop methods by targeted mass spectrometry for the absolute quantification of such fragment peptides [72,73,74]. Heavy isotope-labelled peptides of the reference peptides were used to absolutely quantify endogenous TDP-43 peptide levels. Using this method, it was shown that in the motor cortex of ALS patients with TDP-43 proteinopathy, the C:N-terminal peptide ratio of TDP-43 was significantly increased compared to both normal and other neurodegenerative disease control groups, suggesting a measurement for the enrichment of pathological C-terminal TDP-43 fragments in ALS [72]. The pathological cleavage of TDP-43 was further confirmed by measuring the N-terminal truncation site-specific TDP-43 peptides. This included the identification of a novel N-terminal truncation of a C-terminal fragment. Of note, the cleavage of TDP-43 was found in ALS, but also in the motor cortices of AD, that were later confirmed with LATE neuropathological changes [72]. In another work, multiple peptides spanning TDP-43 on structural and pathological relevant sites, including the N-terminus, both RNA-binding domains (residues 101–262) and the domains of TDP 35 kDa, and TDP 25 kDa fragments (residues 90–414 and 220–414) were developed [73]. Together with an enrichment process of functional RNA-binding TDP-43 using aptamers prior to mass spectrometric analysis, the sensitivity of detection was increased, and this enabled the improved quantification of the cleavage patterns of TDP-43 [74]. In conclusion, shifting the detection of TDP-43 on a proteotypic peptide level enables to form the basis for the absolute quantification of N-terminal and C-terminal TDP-43 fragments in future proteomic studies of complex matrices, such as blood and CSF, as well as the development of novel antibodies recognizing the pathological forms of TDP-43.
2.3. TDP-43 Loss of Function Mechanisms
While cytoplasmic aggregation with a toxic gain of function is a proposed mechanism of TDP-43 pathobiology, a second mechanism of toxicity is the nuclear loss of TDP-43 leading to altered RNA/DNA metabolism [75,76]. It is also suggested that the nuclear loss of TDP-43 could be an early event in the development of the disease preceding cytoplasmic TDP-43 aggregate formation [77,78]. TDP-43 acts as a splicing repressor of non-conserved intronic sequences, which, when disturbed, results in the inclusion of normally cryptic exons into mature RNAs (Figure 1b) [36]. This can lead to premature stop codons, premature polyadenylation, or the degradation of certain transcripts [79]. In line with this loss of function mechanism, a major alteration of the RNA levels of stathmin 2 (STMN2) and unc-13 homolog A (UNC13A) has been recently described [80,81]. Truncated and non-functional STMN2 mRNA, caused by premature polyadenylation resulting in an eightfold reduction of normal STMN2 levels, was found in the TDP-43 proteinopathy positive postmortem brain regions of FTD patients [82]. STMN2 is important for the stabilization of long axons in neurons and the loss of STMN2 has been associated with toxicity in ALS [83,84]. A similar pathology has been described for UNC13A, where TDP-43 depletion in neuronal cell lines lead to reduction of UNC13A transcripts through nonsense-mediated decay [81]. The repression of cryptic exon inclusion in UNC13A was present in neuronal nuclei with TDP-43 proteinopathy in post mortem brains from patients with ALS and FTD and the reduction of UNC13A protein after TDP-43 depletion was shown [85]. UNC13A is a synaptic protein important for glutamatergic neuronal transmission [86,87,88]. Pathological UNC13A polymorphisms in the same intronic region affected by mis-splicing have been associated with an increased risk in developing ALS/FTD, as well as a shorter survival [89,90,91,92]. In neurons overexpressing TDP-43 and post mortem brains with TDP-43 proteinopathy, the loss of nuclear TDP-43 was specifically associated with the upregulation of the synaptic neuronal pentraxin 2 (NPTX2) mRNA [93]. TDP-43 regulates the levels of NPTX2 mRNA through binding at its GU-rich region [94]. This function was shown to be disrupted in FTLD brain tissue where NPTX2 was also found aberrantly accumulated in neurons [93]. From a biomarker point of view, it is important to note that NPTX2 has also been found decreased in CSF samples of symptomatic FTD mutation carriers [95]. While most patients had TDP-43-associated chromosome 9 open reading frame 72 (C9ORF72) gene and granulin (GRN) gene mutations, NPTX2 was also lower in microtubule-associated protein Tau (MAPT) gene mutation carriers. Therefore, the specificity of NPTX2 as a biomarker for TDP-43 pathology is unclear and requires further investigation.
A further example of using a transcriptome-driven approach to develop non-invasive prognostic biomarkers for disease has been demonstrated for ALS [96]. In this approach, gene expression was derived from laser captured spinal motor neurons with TDP-43 pathology, and the data was bioinformatically processed into the modules associated with disease progression and upstream genetics. Measuring TDP-43 proteinopathy-dependent transcript alterations could therefore be a promising biomarker for discerning TDP-43 proteinopathies from other pathologies in life. In addition to the quantification of full-length protein levels, peptidomics is a promising tool to characterize protein isoforms and truncation signals that may arise from transcript alterations by including the search for unspecifically cleaved peptides. Data from proteomic studies of CSF samples so far have not been successful to detect STMN2 in either ALS patients or non-neurodegenerative diseases [97,98]. Alternative detection methods, such as hypothesis-driven targeted proteomics may therefore be considered in the future to enhance the sensitivity to detect a protein of interest by absolute quantification even in more complex matrices such as CSF [99].
2.4. TDP-43 Proteinopathy Induced Mitochondrial Dysfunction and Inflammatory Response
It is known that TDP-43 specifically interacts with mitochondrial proteins and alters mitochondrial dynamics [100]. Pathological TDP-43 fragments have also been found in mitochondrial protein fractions. However, these changes might be decreasing once neurodegeneration is severe, as recently shown in atrophic FTLD brain regions [101]. Nonetheless, many alterations in axonal mitochondrial transport and respiration have also been demonstrated in genetic models of ALS [102,103]. Most interestingly, in a cellular model of ALS cytoplasmic mislocalization of TDP-43 itself triggers its localization to mitochondria and leads to the release of mitochondrial DNA (Figure 1b) [104,105]. This process destabilizes the mitochondria by mitochondrial membrane permeabilization which eventually activates an inflammatory response via the cGAS/STING pathway. Other than the activation of the inflammatory cGAS/STING pathway, this leads directly to the activation of the TANK-binding kinase 1 (TBK1). In support, the TBK1 loss-of-function mutations have been linked to the development of both ALS and FTD TDP-43 proteinopathies [106]. While cGAS/STING activates TBK1, which then triggers a type 1 interferon response, mutations lead to haploinsufficiency of TBK1, meaning decreased TBK1 activity. Another interesting observation is that even loss of function of TBK1 seems to have an opposing effect in an ALS animal model [107]. The fact that TBK1 is directly associated with TDP-43 proteinopathy through the cGAS/STING pathway and can clinically lead to both diseases, ALS and FTD, and is eventually differentially regulated in early and late-stage disease, makes it an interesting pathway to follow for biomarker derivation. Inflammatory response, as well as evidence for inflammatory components that shape specific clinical and neuropathological patterns in the ALS-FTD-spectrum syndromes underpin the role of non-cell autonomous in ALS-FTD TDP-43 proteinopathy [108]. Among different inflammatory markers, chitinases, including chitotriosidase (CHIT1), chitinase-3-like-1 (CHI3L1), and chitinase-3-like-2 (CHI3L2), have been found to be significantly elevated in CSF of ALS patients compared to other neurodegenerative diseases and CHIT1-positive immunostaining was found in ALS spinal cord tissue, but not in the cortical tissue of ALS, FTD, or AD [109,110,111]. CHIT1 has also been found higher in the CSF of FTD patients with TDP-43 pathology [112]. However, the elevation of CSF CHIT1 levels in FTD are restricted to the clinical phase [113]. In addition, CHI3L1 in FTD correlates with frontal cognitive dysfunction [114,115].
Taken together the differential expression patterns of the chitinases in the ALS-FTD spectrum suggests that other factors, such as the severity of the disease, progression, or neurodegeneration pattern may account for differences rather than simply reflecting a reliable signal for TDP-43 proteinopathy.
2.5. Molecular Aspects of TDP-43 Pathology
TDP-43 pathology has been identified in a wide range of neurodegenerative diseases, both in cases inherited in a Mendelian pattern or sporadic patients, providing an exciting link between the pathophysiology of apparently sporadic and familial diseases. Generally, ~97% of all ALS and ~45% of FTLD cases involve TDP-43 aggregation [17,116]. In ALS, most sporadic patients and most patients carrying genetic variants, such as C9ORF72-, TARDBP-, OPTN-, UBQLN2-, and TBK1-ALS, show TDP-43 pathology [117,118]. Interestingly, in superoxide dismutase 1 (SOD1)-ALS, neuronal inclusions show immunopositivity for ubiquitin, but usually negativity for TDP-43. Similarly, in ALS due to genetic variants in the FUS RNA binding protein (FUS), a gene that is also encoding an RNA-processing protein involved in transcriptional regulation, TDP-43 positive inclusions are absent [119,120]. In FTD, TDP-43 pathology has been identified in Tau-negative sporadic cases (50%) as well as patients with genetic variants in, e.g., C9ORF72, GRN, and valosin-containing protein (VCP), but not in MAPT-FTD [17,117,118].
The discovery of key proteins might lead to the identification of candidate ALS-FTD genes, a prominent example being the identification of missense variants in TARDBP. Mutations in the gene encoding TDP-43 have, however, only being associated in less than 5% of ALS patients [35]. This is in line with the hypothesis that TDP-43 pathology may arise through multiple different mechanisms, emphasizing that ALS as a multistep disease, with fewer steps required in familial ALS [26,121]. On the other hand, the identification of mutated genes has a relevant impact on the development of novel disease biomarkers. For example, a loss of function mutation in cyclophilin A has been found in ALS and knocking out cyclophilin A in a mouse model led to the development of TDP-43 proteinopathy [122]. Cyclophilin A has also been found differentially expressed in ALS peripheral blood monocytes and plasma-derived extracellular vesicles [123,124]. These biomarkers could also be directly linked to the genetic defect, e.g., poly-GP in C9ORF72 expansion carriers or SOD1 protein concentrations in CSF of SOD1-ALS [125,126,127].
As alterations in RNA metabolism have emerged as one critical driver of ALS/FTD pathogenesis, the role of microRNA, small non-coding RNAs and key determinants of mRNA stability, has recently been studied [128,129]. Besides their important regulatory role in a variety of biological processes, miRNAs can also be released into the circulation by altered tissues as “fingerprints”, reflecting an activation of specific pathogenic pathways. Furthermore, they are easily detected in body fluids such as blood, CSF, or saliva, where they display remarkable stability. Interestingly, specific miRNA profiles have been identified in familial ALS, but also in pre-symptomatic mutation carriers [130]. At the level of a functional connection, it is known that the C-terminus of TDP-43 forms a complex with nuclear Drosha and cytoplasmic Dicer, which regulate miRNAs [131]. MiRNAs are gene expression modulators and influence cytoplasmic mRNA translation, indirectly giving evidence for a role of TDP-43 on cytoplasmic translation. Interestingly, TDP-43 has a direct effect on specific pri-miRNA processing and leads to differential expression of selected miRNAs [132,133], but the importance of these changes on disease onset and progression still remains to be largely evaluated.
In the future, however, additional types of non-coding RNAs could also be explored as ALS biomarkers. These include circRNAs that originate from back-splicing events during precursor mRNA processing and may act as miRNA sponges or to sequester RBP proteins, thus affecting protein and gene expression. Their usefulness as a biomarker mostly resides in the fact that circRNAs are very resistant to RNA exonucleases and are thus highly stable in cells. For example, a recent promising study of circRNAs in blood leukocytes of sporadic ALS patients has allowed us to identify four circRNAs whose expression may be differentially affected in patients compared to controls [134].
Finally, long noncoding RNAs (lncRNAs) could also represent another possible type of RNA that could be easily detected in blood and CSF of patients. As the name suggests, lncRNAs are long RNAs that are not normally translated but can affect gene expression by affecting epigenetic and transcriptional profiles of their target genes. To this date, lncRNAs have not received a very high level of attention in ALS, but differential expression of several lncRNAs has been reported to occur in peripheral blood monocytes of ALS patients [135]. It should also be noted that TDP-43 has been described to also affect the processing of several of these molecules, such as NEAT1 and MALAT, and to affect the severity of the disease in animal models [136,137].
3. Biofluid Studies of Clinical Entities Associated with TDP43 Pathology
The lack of studies aiming to develop TDP-43 disease-specific in vivo biofluid biomarkers by searching for common changes in TDP-43 pathology relevant patient groups is striking [138]. Especially in FTD, the clinical spectrum does not correlate with the distinct pathologies, except when the underlying pathology of FTD is predicted by the presence of an autosomal dominant mutation, which is found in only 20%–30% of the patients [139]. Here, therefore, we have wished to review biofluid studies that aim to identify biomarkers in patient groups that are clinically indicative, genetically, or autopsy-defined as TDP-43 proteinopathies using either applied unbiased proteomics or a data-driven approach.
3.1. Unbiased Shot-Gun Proteomics
A recent proteomic study compared CSF samples from FTD patients with TDP-43 or Tau proteinopathy, confirmed by autopsy or genetic testing to a group of patients with subjective memory complaint [138]. For the discovery experiments, only a small number of samples (n = 8 for Tau and n = 12 for TDP-43) were investigated. In total, ten biomarkers were observed to be differentially expressed between FTD-TDP and FTD-Tau, which were later validated. Specifically, Ubiquitin-like protein 3 was upregulated in FTD-TDP versus FTD-Tau, while α-Galactosidase A, Heat shock protein 8 and Kallikrein 7 were all downregulated in FTD-TDP compared to FTD-Tau. As a result, ten biomarkers were differentially regulated between the control group and FTD-TDP patients. However, only one candidate, catalase activity, was also found downregulated in FTD patients compared to the control group in the validation experiments, while other candidates failed. A second study investigated CSF samples from asymptomatic (n = 14), symptomatic (n = 14), ALS mutation carriers (SOD1, C9ORF72 and TARDBP), and sporadic ALS patients (n = 12) [97]. In these patient groups, changes were likely to reflect fast progressive neurodegeneration rather than TDP-43 pathology. However, a more specific ALS pathology was also discussed with regards to the observed upregulation of Ubiquitin C-terminal hydrolase-L1 (UCHL1) in patient’s CSF, which had been shown to be differentially expressed in ALS cases before [140,141,142,143]. Of particular interest, there was also the observation that several proteins involved in the splicing function were differentially regulated in ALS samples, which could indicate a dysfunction of TDP-43 [97].
3.2. Hypothesis Driven Investigation of Biomarkers
Specific biomarkers have been investigated across clinical cohorts of ALS-FTD spectrum disorders in comparison to other neurodegenerative diseases, such as AD and PD. Here we review biomarker studies in light of their potential to differentiate ALS, FTD-TDP, and eventually LATE, from FTD-Tau and AD patient cohorts (Table 1).
Table 1.
Hypothesis driven investigation of biomarkers in ALS-FTD spectrum diseases.
| Biomarker | ALS | FTD | AD | Sample | Ref. | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Clinical Subtypes | Pathology Subtypes | Genetic Subtypes | |||||||||||||
| all | C9ORF72 | all | bvFTD | PPA | FTD-ALS | -TDP | -Tau | C9ORF72 | GRN | MAPT | |||||
| SD | PNFA | ||||||||||||||
| Neurofilaments + | ↑ (vs. controls, FTD-ALS, FTD, AD) |
↑ (vs. asymptomatic C9-carriers, C9-FTD) |
↑ (vs. controls, AD) |
↑ (vs. controls) |
↑ (vs. controls) |
↑ (vs. controls) |
↑ (vs. controls, bvFTD, PPA) – (vs. FTD) |
Not sufficiently studied (n = 2) |
Not sufficiently studied (n = 2) |
↑ (vs. asympomatic C9-carriers, sporadic FTD) |
↑ (vs. asympomatic GRN-carriers, sporadic FTD, C9-FTD, MAPT-FTD) |
↑ (vs. asympomatic MAPT-carriers) |
↑ (vs. controls) |
CSF Serum |
[144,145,146,147,148,149,150] |
| CHIT1 | ↑ (vs. controls, FTD, AD) |
↑ (vs. controls, asymptomatic carriers, genetic FTD) * |
↑ (vs. controls, not vs. ALS, AD) |
– (vs. PPA, FTD-ALS) |
– (vs. bvFTD, FTD-ALS) |
– (vs. bvFTD, PPA) |
Not sufficiently studied | Not sufficiently studied | ↑ (vs. controls, asymptomatic carriers) * |
Not studied | Not studied | ↑ (vs. controls, not vs. FTD) |
CSF | [109,112,113] | |
| YKL-40 | ↑ (vs. controls, not vs. ALS) |
↑ (vs. controls, asymptomatic carriers, not vs. genetic FTD) * |
↑ (vs. controls, slighty vs. ALS, not vs. AD) |
– (vs. PPA, FTD-ALS) |
– (vs. bvFTD, FTD-ALS) |
↑ (vs. bvFTD, not PPA) |
Not sufficiently studied | Not sufficiently studied | ↑ (vs. controls, asymptomatic carriers, not vs. genetic ALS) * |
Not studied | Not studied | ↑ (vs. controls, not vs. FTD) |
CSF | [112,113] | |
| GFAP | – (vs. controls) |
– (vs. controls, asymptomatic carriers) * |
↑ (vs. controls, ALS, not vs. AD) |
– (vs. PPA, FTD-ALS) |
– (vs. bvFTD, FTD-ALS) |
– (vs. bvFTD, not PPA) |
Not sufficiently studied | Not sufficiently studied | ↑ (vs. controls, asymptomatic carriers, genetic ALS) * |
Not studied | Not studied | ↑ (vs. controls, not vs. FTD) |
CSF | [112,113] | |
| TREM2 | ↑ (vs. controls) |
Not studied | – (vs. controls) |
– (vs. controls, PPA) |
– (vs. controls, bvFTD) |
– (vs. controls, bvFTD) |
Not studied | Not studied | Not studied | – (vs. controls, C9-FTD, MAPT-FTD) |
↑ (vs. controls, C9-FTD, MAPT-FTD) |
– (vs. controls, C9-FTD, MAPT-FTD) |
↑ (vs. controls) |
CSF | [96,151,152] |
| Progranulin | – (vs. controls, GRN-negative FTD, AD) |
Not studied | ↓ (vs. controls) |
↓ (bvFTD and SD vs. controls, PNFA) |
↓ (SD and bvFTD vs. controls, PNFA) |
– (vs. controls) |
Not studied | Not studied | Not studied | – (vs. controls) |
↓ (vs. controls) – (vs. asymptomatic carriers) |
Not studied | ↓ (vs. controls) |
Plasma CSF |
[153,154,155,156] |
| Neurogranin | ↓ (vs. AD) |
Not studied | ↓ (vs. AD, controls) |
↓ (vs. AD) – (vs. SD, PNFA) |
↓ (vs. AD) – (vs. bvFTD, PNFA) |
↓ (vs. AD) – (vs. bvFTD, SD) |
Not studied | Not studied | Not studied | Not studied | Not studied | Not studied | ↑ (vs. controls, ALS, FTD) |
CSF | [157,158] |
| SNAP-25 | Not studied | Not studied | – (vs. controls) |
Not studied | Not studied | Not studied | Not studied | Not studied | Not studied | Not studied | Not studied | Not studied | ↑ (vs. controls) |
CSF | [159,160] |
| Transthyretin | ↑/↓ (vs. controls) |
Not studied | ↑ (vs. controls) |
Not studied | Not studied | Not studied | Not studied | Not studied | Not studied | Not studied | Not studied | Not studied | ↑/↓ (vs. controls) |
CSF | [161,162,163] |
| Clusterin | ↓ (vs. controls) |
Not studied | ↑ (vs. controls) |
Not studied | Not studied | Not studied | Not studied | Not studied | Not studied | Not studied | Not studied | Not studied | ↑ (vs. controls) |
Serum plasma |
[164,165,166] |
| p/t ratio | Not studied | Not studied | ↓ (vs. controls) |
↓ (vs. controls) |
↓ (vs. controls) |
↓ (vs. controls) |
↓ (vs. controls, FTD without ALS, AD) |
Not sufficiently studied | Not sufficiently studied | Not studied | Not studied | Not studied | ↓ (vs. controls, FTD) |
CSF | [150,167,168] |
| TDP-43 | ↑ (vs. controls, FTD) |
↑ (vs. controls, FTD, C9-FTD) |
↓ (vs. ALS, C9-ALS) ↑ (vs. controls) |
↓ (vs. controls) |
– (vs. controls, FTD) |
– (vs. controls, FTD) |
↓ (vs. FTD, controls) |
↓ (vs. FTD-Tau) |
Not sufficiently studied | ↓ (vs. GRN-FTD) |
↑ (vs. C9-FTD) |
↑ (vs. FTD-TDP) |
↓ (vs. FTD-TDP, FTD, AD-TDP) ↑ (vs. controls) |
CSF serum |
[169,170,171,172,173,174,175] |
↑/↓ arrows indicate increased or decreased biomarker levels. Arrows do not always reflect statistical significance. + includes neurofilament light and phosphorylated heavy chain levels, * genetic ALS/FTD with the majority being C9ORF72-carriers. AD—Alzheimer’s disease, ALS—Amyotrophic lateral sclerosis, FTD—Frontotemporal dementia, bvFTD—Behavioral variant frontotemporal dementia, GRN—Granulin, PNFA—Progressive non-fluent aphasia, PPA—Primary progressive aphasia, SD—Semantic dementia.
3.2.1. Neurofilaments
A promising biomarker in neurodegenerative diseases is the light and phosphorylated heavy chain of neurofilaments (NfL and pNfH). Neurofilaments (Nf) are abundant cytoskeletal proteins of myelinated central and peripheral neurons [176]. Increased neurofilaments levels reflect axonal damage and are therefore unspecific. However, Nfs can aid to discriminate certain neurodegenerative disorders. In ALS, for example, NfL and pNFH are strongly elevated in CSF and serums with diagnostic sensitivities and specificities >80% [144,177,178]. Furthermore, Nfs were observed to be highly expressed in most FTD-spectrum diseases (including bvFTD, FTD-ALS, PPA, corticobasal syndrome (CBS), and progressive supranuclear palsy) with the highest values in FTD-ALS [146,147,148,149,167]. An autoptic or genetically secured FTD with TDP-43 pathology (FTD-TDP) showed higher Nf values when compared to FTD with Tau pathology (FTD-Tau) [150,179,180]. However, definite cut-off values to discriminate FTD-TDP from FTD-Tau have not been established and studies are restricted by the small numbers of pathology-confirmed cases. Further work will therefore be necessary to exactly evaluate the usefulness of Nf levels as a diagnostic disease biomarker in FTD pathology subtypes.
3.2.2. Glial Markers: CHIT1, YKL-40, GFAP and TREM2
It is now widely accepted that neuroinflammation contributes to neurodegeneration in ALS and FTD, although it is unresolved whether the immune response causes, aggravates, or counteracts neurodegeneration [181]. Specifically, activated microglia and astrocytes produce several inflammatory proteins that have been explored in terms of biomarker value in neurodegenerative diseases. Among the first targets to be explored, Chitotriosidase 1 (CHIT1) was shown to be significantly increased in CSF of sporadic ALS patients [109,114]. While it is also increased in genetic ALS cases, CHIT1 is normal in genetic FTD cases and in asymptomatic gene carriers when compared to controls [113]. Another study showed higher CHIT1 levels in prion disease subtypes, FTD, and AD, but also higher values in FTD-TDP compared to FTD-Tau, but with the highest values in the ALS-FTD group [112]. Because CHIT1 is predominantly elevated in ALS, its levels are more likely to reflect the degree of motor neuron degeneration rather than reflecting the type of proteinopathy [109,113,114]. This conclusion has been supported by a comparison between FTD-TDP and a small group of “definite” FTD-Tau cases (definite PSP, CBD, and MAPT carriers) which revealed no differences. Similarly, levels of chitinase-3-like protein 1 (YKL-40) and glial fibrillary acidic protein (GFAP) were higher in prion disease subtypes, FTD, and AD compared to the controls [112]. In this study, it was also shown that the values of YKL-40 did not differ between FTD-TDP and FTD-Tau, but were increased when associated with ALS-FTD, while GFAP showed similar values among the clinical syndromes and proteinopathies. However, like p-Tau there is growing evidence that GFAP could be a biomarker for AD and serum GFAP levels could differentiate AD from bvFTD [182,183]. Another promising connection is represented by triggering receptor expressed on myeloid cells 2 (TREM2), which is a surface receptor expressed on brain microglia and whose genetic variants have been identified as risk factors for AD [184,185]. Since its description, this link has led to an extensive study of TREM2 biology and its potential role as an immune-related biomarker in neurodegenerative diseases. In CSF of AD cohorts, soluble TREM2 levels were reported to increase over the course of the disease, reaching a peak during the early-phase stages [151], possibly reflecting an initial immune response to the deposition of pathological aggregates. Furthermore, TREM2 levels have been shown to correlate with p- and t-Tau, but not with β-Amyloid 1–42 levels, suggesting that TREM2 in CSF might be a useful marker of glial activation in response to neuronal damage independent of amyloid pathology [186,187,188]. Moreover, in sporadic ALS CSF samples, the soluble TREM2 levels were higher compared to the controls [96]. Moreover, the mean levels of TREM2 were higher in the early disease phase compared to the later phases, where higher levels were associated with a slower disease progression, indicating a possible neuroprotective effect of TREM2 on microglia. Finally, in a study investigating 64 individuals with FTD, soluble TREM2 levels did not differ between FTD overall or in a particular clinical subtype of FTD; however levels were significantly higher in GRN mutation carriers as well as FTD individuals with AD-like CSF profiles (t-Tau/ Aβ 1–42 ratio > 1.0) [152].
3.2.3. Progranulin
Variants in GRN are among the most frequent genetic causes of FTD, most leading to progranulin haploinsufficiency. Progranulin is a ubiquitous protein involved in several biological pathways, including growth factor-like activities, neuroinflammation, and neuronal survival [153]. Levels of progranulin can be measured in patient plasma and were shown to be decreased in both GRN mutation carriers and pre-symptomatic GRN carriers compared to controls without significant differences between the three major FTD phenotypes represented by FTD, PPA, and CBS [154]. In addition, GRN-negative FTD patients also displayed decreased levels of progranulin in CSF without correlation to CSF tau levels [189]. However, these conclusions need to be further investigated because another study analyzed progranulin concentrations in CSF of the different FTD subtypes and found levels to be significantly lower in semantic dementia and bvFTD compared to progressive non-fluent aphasia (PNFA) and controls, indicating that CSF-progranulin might represent a promising biomarker for TDP-mediated FTD instead of tau-mediated FTD [155]. In ALS, causal genetic variants in GRN, segregating with the disease, have not been observed so far, but GRN seems to act as a genetic modifier of the degree of motor neuron degeneration [190]. Importantly, levels of progranulin measured in plasma and CSF of newly diagnosed ALS patients did not differ from healthy controls, GRN-negative FTD patients, or AD [191]. Progranulin can also be found elevated in the blood of AD patients compared to controls [156].
3.2.4. Synaptic Proteins
Neurogranin is a neuron-specific dendritic protein regulating synaptic plasticity and learning. Considering the central role of synaptic pathology in AD pathogenesis, neurogranin is particularly interesting as a biomarker in AD. Large studies showed that neurogranin levels in CSF specifically increased in AD compared to several other neurodegenerative diseases, including PD, FTD, ALS, and vascular dementia [157,158], confirming the potential of CSF neurogranin in separating AD dementia from non-AD dementia. On a neuropathological level, CSF neurogranin was associated with Amyloid-ß plaque pathology but not with neurofibrillary tangle of tau protein, α-synuclein, or TDP-43 loads [157]. Another synaptic protein and potentially important marker for functional synapses is synaptosomal-associated protein 25 (SNAP-25). Regarding this factor, increased levels of SNAP-25 could be detected in CSF of AD and Creutzfeldt–Jakob disease (CJD) patients but not in FTD, ALS or controls [159,160,192]. Finally, as mentioned in our previous section, NPTX2, which is involved in synaptic plasticity, was found lower in the CSF of the symptomatic phase of FTD patients regardless of the underlying genetic mutation (C9ORF72, GRN and MAPT) and, therefore, is of yet unclear significance as TDP-43 specific biomarker [95].
3.2.5. Transthyretin
Another biomarker candidate is transthyretin, which is required for the transport of thyroxine and retinol but also binds with β-amyloid, and thus, is considered to prevent formation of senile plaques. Proteomic studies have demonstrated an increase in transthyretin concentration in CSF from both AD and FTD patients [99,161,162]. In addition, two studies have reported reduced levels of transthyretin in AD CSF [163,193]. These findings seem to represent an apparent contradiction but they can possibly be explained by the fact that transthyretin is modified post-translationally [194], making reliable measurement difficult [99]. Following up on this possibility, transthyretin levels were decreased in ALS CSF of one study [195], but increased in a second one [196].
3.2.6. Clusterin
Clusterin is a potent chaperone that can inhibit protein aggregation, and therefore, might protect against neurotoxicity. Importantly, it has been shown that clusterin protects against TDP-43 aggregation and mislocalization [197]. In initial studies, plasma clusterin concentrations were significantly increased only in AD and not in vascular dementia, Parkinson’s disease-related dementia, dementia with Lewy bodies (DLB), or FTD [164]. One study measured clusterin in neuronal exosomes from serum and found it to be elevated in FTD, progressive supranuclear palsy (PSP) and CBS compared to α-synuclein proteinopathies [165]. In ALS, plasma levels of clusterin seem to be decreased; however, the sample sizes were small [166].
3.2.7. Tau
Tau, the major microtubule associated protein of a mature neuron, is regulated by its phosphorylation state. In AD and other tauopathies, brain tau is hyperphosphorylated (p-tau) and becomes aggregated, resulting in neurofibrillary tau pathology. The CSF biomarkers for AD, particularly (p-) tau and amyloid b-42, mostly appeared to be of limited value for the diagnosis of FTD and its pathological subtypes [198,199]. However, a reduced CSF phospho-tau-181 to total tau ratio (p/t-tau ratio) has been demonstrated to be useful to discriminate FTLD-TDP from FTLD-Tau (p < 0.01 and p = 0.005) [167,200]. Intriguingly, the presence of ALS has been shown to relevantly influence the effect on this ratio [167,168].
3.2.8. TDP-43
As already described, TDP-43 is the pathological protein found aggregated in neurons and glial cells of patients with ALS, FTD, and LATE. While the pathological form of TDP-43 can be detected in human post mortem brains, the detection in patient biofluids, such as CSF and serums using antibody-based assays, have been difficult [201], mainly because most antibodies bind both the pathological and physiological form of TDP-43. While most studies report elevated levels of TDP-43 in sporadic ALS independently of the genotype, an autopsy-controlled study of FTLD-TDP CSF samples reported lower levels of TDP-43 [169,170,202]. In addition, TDP-43 in the serum was also found decreased in FTD patients with the C9ORF72 mutation or FTD-MND phenotype (both subtypes are strongly associated with TDP-43 type B brain pathology) but not in FTD patients with GRN mutation [171] that are associated with Type A pathology [203]. Thus far, the detection of phosphorylated TDP-43 has failed in CSF [172,202]. In serum, however, higher phosphorylated TDP-43 levels were found in FTD C9ORF72 and GRN mutation carriers, while the same group reported lower levels of normal TDP-43 [173]. High-sensitivity assays improved the detection rate of TDP-43 in biofluids without improving the specificity to the pathological forms [204,205]. TDP-43 levels in serum were reported to be lower in AD patients compared to FTD and FTD patients with autopsy-confirmed TDP-43 pathology [174,175]. The detection of the pathological aggregated form of TDP-43 using RT-QuIC in CSF is in development and its clinical application must be further tested [59].
In summary, none of the biomarkers described above yet have the ability to differentiate between clinical phenotypes of TDP-43 pathology across the ALS/FTLD spectrum diseases. Most studies show potential biomarkers of fast progressive ALS. Only a few studies have investigated biomarkers in different FTD clinical subtypes, of which some, such as bvFTD, are more likely to have underlying TDP-43 proteinopathy. However, most studies do not compare biomarkers across all clinical cohorts of ALS, FTD, and AD sufficiently. Rather worryingly, some studies have also included clinical entities that often harbour TDP-43 pathology but without a definite proof of its pathology. In addition, definite FTD-TDP patient cohorts are usually mixed cohorts of autopsy-confirmed or genetically proven FTD-TDP and limited to small numbers. Furthermore, at the moment there have been no studies that separate confirmed LATE-NC from typical AD biosamples. This should be considered of high priority because an important development of biomarkers for AD would be to allow them to discriminate AD from definite FTD-TDP or LATE. Indeed, an initial step towards developing such a biosample cohort could be to already separate samples that lack typical AD profiles, such as TREM2, Tau, p-Tau, and Amyloid-ß changes.
4. Conclusions
Thus far, the development of TDP-43 as a biomarker to detect TDP-43 proteinopathies has not been successful for several reasons. In general, low concentrations in CSF and serum, as well as the detection of pathology unspecific forms are limiting such developments. Therefore, to advance TDP-43-specific biomarker development it will be necessary to further develop techniques that are aimed at detecting the pathological forms of TDP-43. As proteomic studies have yet failed to detect such forms in vivo in CSF [72,73,74], it might be necessary in the future to investigate biomarkers or techniques that are linked to its pathology, as we have described in the first part of this review. Importantly, the role of TDP-43 in regulating certain transcripts could lead to measuring changes in a range of target proteins that could lead to a differential proteome in the central nervous system and to some extent in CSF [97]. Parallel to these approaches, a still rather understudied approach could be looking at extracellular vesicles or leukocyte-derived microvesicles, which could be a potential alternative source to identify TDP-43-specific biomarkers [124,201,206]. However, while matrix effects for proteomic studies are usually lower in these species, their enrichment is often challenging. In addition, to test any pathology-derived biomarker, biosamples are needed that are well defined by TDP-43 pathology. The focus must therefore be on larger autopsy-confirmed biosample cohorts (matched biofluid tissue cohorts) or genetically confirmed TDP-43 cases. Like the amyloid-tau-neurodegeneration (ATN) classification system in AD, already established biomarkers of neurodegeneration, such as Nfs, should be routinely integrated in the search for pathology-specific biomarkers. In addition, using as a reference a combination of existing biomarkers which already have been tested in clinical cohorts could enhance the specificity of discovering novel biomarkers. The development of TDP-43-specific biomarkers is important as it may inform about TDP-43 pathology among clinical subtypes of FTD or AD cases, and could therefore enable the stratification of patients by TDP-43 pathology and eventually result in more precise treatment strategies and better interpretations of clinical trial results.
5. Patents
E.F. has a patent filed for a method for diagnosing a condition characterized by TDP-43 proteinopathy (PCT/GB2021/050821; https://patentscope.wipo.int/search/en/detail.jsf?docId=WO2021198698, accessed on 8. February 2023).
Author Contributions
Conceptualization, I.C. and E.F.; writing—original draft preparation, I.C., A.W. and E.F.; writing—review and editing, P.L., C.S., M.P., E.B. and E.F.; visualization, A.W., I.C.; supervision, E.F. All authors have read and agreed to the published version of the manuscript.
Data Availability Statement
The data presented in this study are openly available in [Pubmed].
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Bott N.T., Radke A., Stephens M.L., Kramer J.H. Frontotemporal dementia: Diagnosis, deficits and management. Neurodegener Dis. Manag. 2014;4:439–454. doi: 10.2217/nmt.14.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cellura E., Spataro R., Taiello A.C., La Bella V. Factors affecting the diagnostic delay in amyotrophic lateral sclerosis. Clin. Neurol. Neurosurg. 2012;114:550–554. doi: 10.1016/j.clineuro.2011.11.026. [DOI] [PubMed] [Google Scholar]
- 3.Cipriani G., Danti S., Nuti A., Di Fiorino M., Cammisuli D.M. Is that schizophrenia or frontotemporal dementia? Supporting clinicians in making the right diagnosis. Acta Neurol. Belg. 2020;120:799–804. doi: 10.1007/s13760-020-01352-z. [DOI] [PubMed] [Google Scholar]
- 4.Draper B., Cations M., White F., Trollor J., Loy C., Brodaty H., Sachdev P., Gonski P., Demirkol A., Cumming R.G., et al. Time to diagnosis in young-onset dementia and its determinants: The INSPIRED study. Int J. Geriatr. Psychiatry. 2016;31:1217–1224. doi: 10.1002/gps.4430. [DOI] [PubMed] [Google Scholar]
- 5.Richards D., Morren J.A., Pioro E.P. Time to diagnosis and factors affecting diagnostic delay in amyotrophic lateral sclerosis. J. Neurol. Sci. 2020;417:117054. doi: 10.1016/j.jns.2020.117054. [DOI] [PubMed] [Google Scholar]
- 6.Benatar M., Wuu J., McHutchison C., Postuma R.B., Boeve B.F., Petersen R., Ross C.A., Rosen H., Arias J.J., Fradette S., et al. Preventing amyotrophic lateral sclerosis: Insights from pre-symptomatic neurodegenerative diseases. Brain. 2022;145:27–44. doi: 10.1093/brain/awab404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kiernan M.C., Vucic S., Talbot K., McDermott C.J., Hardiman O., Shefner J.M., Al-Chalabi A., Huynh W., Cudkowicz M., Talman P., et al. Improving clinical trial outcomes in amyotrophic lateral sclerosis. Nat. Rev. Neurol. 2021;17:104–118. doi: 10.1038/s41582-020-00434-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Turner M.R., Kiernan M.C., Leigh P.N., Talbot K. Biomarkers in amyotrophic lateral sclerosis. Lancet Neurol. 2009;8:94–109. doi: 10.1016/S1474-4422(08)70293-X. [DOI] [PubMed] [Google Scholar]
- 9.Neumann M., Sampathu D.M., Kwong L.K., Truax A.C., Micsenyi M.C., Chou T.T., Bruce J., Schuck T., Grossman M., Clark C.M., et al. Ubiquitinated TDP-43 in frontotemporal lobar degeneration and amyotrophic lateral sclerosis. Science. 2006;314:130–133. doi: 10.1126/science.1134108. [DOI] [PubMed] [Google Scholar]
- 10.Arai T., Hasegawa M., Akiyama H., Ikeda K., Nonaka T., Mori H., Mann D., Tsuchiya K., Yoshida M., Hashizume Y., et al. TDP-43 is a component of ubiquitin-positive tau-negative inclusions in frontotemporal lobar degeneration and amyotrophic lateral sclerosis. Biochem. Biophys. Res. Commun. 2006;351:602–611. doi: 10.1016/j.bbrc.2006.10.093. [DOI] [PubMed] [Google Scholar]
- 11.Mackenzie I.R., Neumann M. Molecular neuropathology of frontotemporal dementia: Insights into disease mechanisms from postmortem studies. J. Neurochem. 2016;138((Suppl. 1)):54–70. doi: 10.1111/jnc.13588. [DOI] [PubMed] [Google Scholar]
- 12.Mackenzie I.R., Neumann M., Bigio E.H., Cairns N.J., Alafuzoff I., Kril J., Kovacs G.G., Ghetti B., Halliday G., Holm I.E., et al. Nomenclature for neuropathologic subtypes of frontotemporal lobar degeneration: Consensus recommendations. Acta Neuropathol. 2009;117:15–18. doi: 10.1007/s00401-008-0460-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Amador-Ortiz C., Lin W.L., Ahmed Z., Personett D., Davies P., Duara R., Graff-Radford N.R., Hutton M.L., Dickson D.W. TDP-43 immunoreactivity in hippocampal sclerosis and Alzheimer’s disease. Ann. Neurol. 2007;61:435–445. doi: 10.1002/ana.21154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Josephs K.A., Whitwell J.L., Knopman D.S., Hu W.T., Stroh D.A., Baker M., Rademakers R., Boeve B.F., Parisi J.E., Smith G.E., et al. Abnormal TDP-43 immunoreactivity in AD modifies clinicopathologic and radiologic phenotype. Neurology. 2008;70:1850–1857. doi: 10.1212/01.wnl.0000304041.09418.b1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nelson P.T., Dickson D.W., Trojanowski J.Q., Jack C.R., Boyle P.A., Arfanakis K., Rademakers R., Alafuzoff I., Attems J., Brayne C., et al. Limbic-predominant age-related TDP-43 encephalopathy (LATE): Consensus working group report. Brain. 2019 doi: 10.1093/brain/awz099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kawakami I., Arai T., Hasegawa M. The basis of clinicopathological heterogeneity in TDP-43 proteinopathy. Acta Neuropathol. 2019;138:751–770. doi: 10.1007/s00401-019-02077-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tan R.H., Ke Y.D., Ittner L.M., Halliday G.M. ALS/FTLD: Experimental models and reality. Acta Neuropathol. 2017;133:177–196. doi: 10.1007/s00401-016-1666-6. [DOI] [PubMed] [Google Scholar]
- 18.Brettschneider J., Del Tredici K., Toledo J.B., Robinson J.L., Irwin D.J., Grossman M., Suh E., Van Deerlin V.M., Wood E.M., Baek Y., et al. Stages of pTDP-43 pathology in amyotrophic lateral sclerosis. Ann. Neurol. 2013;74:20–38. doi: 10.1002/ana.23937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brettschneider J., Del Tredici K., Irwin D.J., Grossman M., Robinson J.L., Toledo J.B., Fang L., Van Deerlin V.M., Ludolph A.C., Lee V.M., et al. Sequential distribution of pTDP-43 pathology in behavioral variant frontotemporal dementia (bvFTD) Acta Neuropathol. 2014;127:423–439. doi: 10.1007/s00401-013-1238-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schweingruber C., Hedlund E. The Cell Autonomous and Non-Cell Autonomous Aspects of Neuronal Vulnerability and Resilience in Amyotrophic Lateral Sclerosis. Biology. 2022;11 doi: 10.3390/biology11081191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Susnjar U., Skrabar N., Brown A.L., Abbassi Y., Phatnani H., Consortium N.A., Cortese A., Cereda C., Bugiardini E., Cardani R., et al. Cell environment shapes TDP-43 function with implications in neuronal and muscle disease. Commun. Biol. 2022;5:314. doi: 10.1038/s42003-022-03253-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mackenzie I.R., Neumann M., Baborie A., Sampathu D.M., Du Plessis D., Jaros E., Perry R.H., Trojanowski J.Q., Mann D.M., Lee V.M. A harmonized classification system for FTLD-TDP pathology. Acta Neuropathol. 2011;122:111–113. doi: 10.1007/s00401-011-0845-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hayes L.R., Kalab P. Emerging Therapies and Novel Targets for TDP-43 Proteinopathy in ALS/FTD. Neurotherapeutics. 2022;19:1061–1084. doi: 10.1007/s13311-022-01260-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Krecic A.M., Swanson M.S. hnRNP complexes: Composition, structure, and function. Curr. Opin. Cell Biol. 1999;11:363–371. doi: 10.1016/S0955-0674(99)80051-9. [DOI] [PubMed] [Google Scholar]
- 25.Buratti E., Dork T., Zuccato E., Pagani F., Romano M., Baralle F.E. Nuclear factor TDP-43 and SR proteins promote in vitro and in vivo CFTR exon 9 skipping. EMBO J. 2001;20:1774–1784. doi: 10.1093/emboj/20.7.1774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Al-Chalabi A., Calvo A., Chio A., Colville S., Ellis C.M., Hardiman O., Heverin M., Howard R.S., Huisman M.H.B., Keren N., et al. Analysis of amyotrophic lateral sclerosis as a multistep process: A population-based modelling study. Lancet Neurol. 2014;13:1108–1113. doi: 10.1016/S1474-4422(14)70219-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lukavsky P.J., Daujotyte D., Tollervey J.R., Ule J., Stuani C., Buratti E., Baralle F.E., Damberger F.F., Allain F.H. Molecular basis of UG-rich RNA recognition by the human splicing factor TDP-43. Nat. Struct Mol. Biol. 2013;20:1443–1449. doi: 10.1038/nsmb.2698. [DOI] [PubMed] [Google Scholar]
- 28.Afroz T., Hock E.M., Ernst P., Foglieni C., Jambeau M., Gilhespy L.A.B., Laferriere F., Maniecka Z., Pluckthun A., Mittl P., et al. Functional and dynamic polymerization of the ALS-linked protein TDP-43 antagonizes its pathologic aggregation. Nat. Commun. 2017;8:45. doi: 10.1038/s41467-017-00062-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang A., Conicella A.E., Schmidt H.B., Martin E.W., Rhoads S.N., Reeb A.N., Nourse A., Ramirez Montero D., Ryan V.H., Rohatgi R., et al. A single N-terminal phosphomimic disrupts TDP-43 polymerization, phase separation, and RNA splicing. EMBO J. 2018;37:7452. doi: 10.15252/embj.201797452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.D’Ambrogio A., Buratti E., Stuani C., Guarnaccia C., Romano M., Ayala Y.M., Baralle F.E. Functional mapping of the interaction between TDP-43 and hnRNP A2 in vivo. Nucleic Acids Res. 2009;37:4116–4126. doi: 10.1093/nar/gkp342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Buratti E., Brindisi A., Giombi M., Tisminetzky S., Ayala Y.M., Baralle F.E. TDP-43 binds heterogeneous nuclear ribonucleoprotein A/B through its C-terminal tail: An important region for the inhibition of cystic fibrosis transmembrane conductance regulator exon 9 splicing. J. Biol. Chem. 2005;280:37572–37584. doi: 10.1074/jbc.M505557200. [DOI] [PubMed] [Google Scholar]
- 32.Ayala Y.M., Pantano S., D’Ambrogio A., Buratti E., Brindisi A., Marchetti C., Romano M., Baralle F.E. Human, Drosophila, and C.elegans TDP43: Nucleic acid binding properties and splicing regulatory function. J. Mol. Biol. 2005;348:575–588. doi: 10.1016/j.jmb.2005.02.038. [DOI] [PubMed] [Google Scholar]
- 33.Cartegni L., Maconi M., Morandi E., Cobianchi F., Riva S., Biamonti G. hnRNP A1 selectively interacts through its Gly-rich domain with different RNA-binding proteins. J. Mol. Biol. 1996;259:337–348. doi: 10.1006/jmbi.1996.0324. [DOI] [PubMed] [Google Scholar]
- 34.Tziortzouda P., Van Den Bosch L., Hirth F. Triad of TDP43 control in neurodegeneration: Autoregulation, localization and aggregation. Nat. Rev. Neurosci. 2021;22:197–208. doi: 10.1038/s41583-021-00431-1. [DOI] [PubMed] [Google Scholar]
- 35.Sreedharan J., Blair I.P., Tripathi V.B., Hu X., Vance C., Rogelj B., Ackerley S., Durnall J.C., Williams K.L., Buratti E., et al. TDP-43 mutations in familial and sporadic amyotrophic lateral sclerosis. Science. 2008;319:1668–1672. doi: 10.1126/science.1154584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fratta P., Sivakumar P., Humphrey J., Lo K., Ricketts T., Oliveira H., Brito-Armas J.M., Kalmar B., Ule A., Yu Y., et al. Mice with endogenous TDP-43 mutations exhibit gain of splicing function and characteristics of amyotrophic lateral sclerosis. EMBO J. 2018;37:8684. doi: 10.15252/embj.201798684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bolognesi B., Faure A.J., Seuma M., Schmiedel J.M., Tartaglia G.G., Lehner B. The mutational landscape of a prion-like domain. Nat. Commun. 2019;10:4162. doi: 10.1038/s41467-019-12101-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mann J.R., Donnelly C.J. RNA modulates physiological and neuropathological protein phase transitions. Neuron. 2021;109:2663–2681. doi: 10.1016/j.neuron.2021.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mompean M., Laurents D.V. Intrinsically Disordered Domains, Amyloids and Protein Liquid Phases: Evolving Concepts and Open Questions. Protein Pept Lett. 2017;24:281–293. doi: 10.2174/0929866524666170206122106. [DOI] [PubMed] [Google Scholar]
- 40.Lim L., Wei Y., Lu Y., Song J. ALS-Causing Mutations Significantly Perturb the Self-Assembly and Interaction with Nucleic Acid of the Intrinsically Disordered Prion-Like Domain of TDP-43. PLoS Biol. 2016;14:e1002338. doi: 10.1371/journal.pbio.1002338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Polymenidou M., Lagier-Tourenne C., Hutt K.R., Huelga S.C., Moran J., Liang T.Y., Ling S.C., Sun E., Wancewicz E., Mazur C., et al. Long pre-mRNA depletion and RNA missplicing contribute to neuronal vulnerability from loss of TDP-43. Nat. Neurosci. 2011;14:459–468. doi: 10.1038/nn.2779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shiina Y., Arima K., Tabunoki H., Satoh J. TDP-43 dimerizes in human cells in culture. Cell Mol. Neurobiol. 2010;30:641–652. doi: 10.1007/s10571-009-9489-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hallegger M., Chakrabarti A.M., Lee F.C.Y., Lee B.L., Amalietti A.G., Odeh H.M., Copley K.E., Rubien J.D., Portz B., Kuret K., et al. TDP-43 condensation properties specify its RNA-binding and regulatory repertoire. Cell. 2021;184:4680–4696. doi: 10.1016/j.cell.2021.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Buratti E. TDP-43 post-translational modifications in health and disease. Expert Opin. Ther. Targets. 2018;22:279–293. doi: 10.1080/14728222.2018.1439923. [DOI] [PubMed] [Google Scholar]
- 45.Portz B., Lee B.L., Shorter J. FUS and TDP-43 Phases in Health and Disease. Trends Biochem. Sci. 2021;46:550–563. doi: 10.1016/j.tibs.2020.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sternburg E.L., Gruijs da Silva L.A., Dormann D. Post-translational modifications on RNA-binding proteins: Accelerators, brakes, or passengers in neurodegeneration? Trends Biochem. Sci. 2022;47:6–22. doi: 10.1016/j.tibs.2021.07.004. [DOI] [PubMed] [Google Scholar]
- 47.Igaz L.M., Kwong L.K., Lee E.B., Chen-Plotkin A., Swanson E., Unger T., Malunda J., Xu Y., Winton M.J., Trojanowski J.Q., et al. Dysregulation of the ALS-associated gene TDP-43 leads to neuronal death and degeneration in mice. J. Clin. Invest. 2011;121:726–738. doi: 10.1172/JCI44867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ayala Y.M., De Conti L., Avendano-Vazquez S.E., Dhir A., Romano M., D’Ambrogio A., Tollervey J., Ule J., Baralle M., Buratti E., et al. TDP-43 regulates its mRNA levels through a negative feedback loop. EMBO J. 2011;30:277–288. doi: 10.1038/emboj.2010.310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Iguchi Y., Eid L., Parent M., Soucy G., Bareil C., Riku Y., Kawai K., Takagi S., Yoshida M., Katsuno M., et al. Exosome secretion is a key pathway for clearance of pathological TDP-43. Brain. 2016;139:3187–3201. doi: 10.1093/brain/aww237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Feiler M.S., Strobel B., Freischmidt A., Helferich A.M., Kappel J., Brewer B.M., Li D., Thal D.R., Walther P., Ludolph A.C., et al. TDP-43 is intercellularly transmitted across axon terminals. J. Cell Biol. 2015;211:897–911. doi: 10.1083/jcb.201504057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Smethurst P., Newcombe J., Troakes C., Simone R., Chen Y.R., Patani R., Sidle K. In vitro prion-like behaviour of TDP-43 in ALS. Neurobiol. Dis. 2016;96:236–247. doi: 10.1016/j.nbd.2016.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Franceschini A., Baiardi S., Hughson A.G., McKenzie N., Moda F., Rossi M., Capellari S., Green A., Giaccone G., Caughey B., et al. High diagnostic value of second generation CSF RT-QuIC across the wide spectrum of CJD prions. Sci. Rep. 2017;7:10655. doi: 10.1038/s41598-017-10922-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Orru C.D., Groveman B.R., Hughson A.G., Zanusso G., Coulthart M.B., Caughey B. Rapid and sensitive RT-QuIC detection of human Creutzfeldt-Jakob disease using cerebrospinal fluid. mBio. 2015;6 doi: 10.1128/mBio.02451-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Fairfoul G., McGuire L.I., Pal S., Ironside J.W., Neumann J., Christie S., Joachim C., Esiri M., Evetts S.G., Rolinski M., et al. Alpha-synuclein RT-QuIC in the CSF of patients with alpha-synucleinopathies. Ann. Clin. Transl. Neurol. 2016;3:812–818. doi: 10.1002/acn3.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Salvadores N., Shahnawaz M., Scarpini E., Tagliavini F., Soto C. Detection of misfolded Abeta oligomers for sensitive biochemical diagnosis of Alzheimer’s disease. Cell Rep. 2014;7:261–268. doi: 10.1016/j.celrep.2014.02.031. [DOI] [PubMed] [Google Scholar]
- 56.Porta S., Xu Y., Restrepo C.R., Kwong L.K., Zhang B., Brown H.J., Lee E.B., Trojanowski J.Q., Lee V.M. Patient-derived frontotemporal lobar degeneration brain extracts induce formation and spreading of TDP-43 pathology in vivo. Nat. Commun. 2018;9:4220. doi: 10.1038/s41467-018-06548-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Furukawa Y., Kaneko K., Watanabe S., Yamanaka K., Nukina N. A seeding reaction recapitulates intracellular formation of Sarkosyl-insoluble transactivation response element (TAR) DNA-binding protein-43 inclusions. J. Biol. Chem. 2011;286:18664–18672. doi: 10.1074/jbc.M111.231209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Johnson B.S., Snead D., Lee J.J., McCaffery J.M., Shorter J., Gitler A.D. TDP-43 is intrinsically aggregation-prone, and amyotrophic lateral sclerosis-linked mutations accelerate aggregation and increase toxicity. J. Biol. Chem. 2009;284:20329–20339. doi: 10.1074/jbc.M109.010264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Scialo C., Tran T.H., Salzano G., Novi G., Caponnetto C., Chio A., Calvo A., Canosa A., Moda F., Caroppo P., et al. TDP-43 real-time quaking induced conversion reaction optimization and detection of seeding activity in CSF of amyotrophic lateral sclerosis and frontotemporal dementia patients. Brain Commun. 2020;2:fcaa142. doi: 10.1093/braincomms/fcaa142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Beyer L., Gunther R., Koch J.C., Klebe S., Hagenacker T., Lingor P., Biesalski A.S., Hermann A., Nabers A., Gold R., et al. TDP-43 as structure-based biomarker in amyotrophic lateral sclerosis. Ann. Clin. Transl. Neurol. 2021;8:271–277. doi: 10.1002/acn3.51256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mackenzie I.R., Neumann M. Reappraisal of TDP-43 pathology in FTLD-U subtypes. Acta Neuropathol. 2017;134:79–96. doi: 10.1007/s00401-017-1716-8. [DOI] [PubMed] [Google Scholar]
- 62.Lee E.B., Porta S., Michael Baer G., Xu Y., Suh E., Kwong L.K., Elman L., Grossman M., Lee V.M., Irwin D.J., et al. Expansion of the classification of FTLD-TDP: Distinct pathology associated with rapidly progressive frontotemporal degeneration. Acta Neuropathol. 2017;134:65–78. doi: 10.1007/s00401-017-1679-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Chen Z., Ma L. Grey matter volume changes over the whole brain in amyotrophic lateral sclerosis: A voxel-wise meta-analysis of voxel based morphometry studies. Amyotroph Lateral Scler. 2010;11:549–554. doi: 10.3109/17482968.2010.516265. [DOI] [PubMed] [Google Scholar]
- 64.Broe M., Hodges J.R., Schofield E., Shepherd C.E., Kril J.J., Halliday G.M. Staging disease severity in pathologically confirmed cases of frontotemporal dementia. Neurology. 2003;60:1005–1011. doi: 10.1212/01.WNL.0000052685.09194.39. [DOI] [PubMed] [Google Scholar]
- 65.Chiang C.H., Grauffel C., Wu L.S., Kuo P.H., Doudeva L.G., Lim C., Shen C.K., Yuan H.S. Structural analysis of disease-related TDP-43 D169G mutation: Linking enhanced stability and caspase cleavage efficiency to protein accumulation. Sci. Rep. 2016;6:21581. doi: 10.1038/srep21581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hergesheimer R.C., Chami A.A., de Assis D.R., Vourc’h P., Andres C.R., Corcia P., Lanznaster D., Blasco H. The debated toxic role of aggregated TDP-43 in amyotrophic lateral sclerosis: A resolution in sight? Brain. 2019;142:1176–1194. doi: 10.1093/brain/awz078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kametani F., Obi T., Shishido T., Akatsu H., Murayama S., Saito Y., Yoshida M., Hasegawa M. Mass spectrometric analysis of accumulated TDP-43 in amyotrophic lateral sclerosis brains. Sci. Rep. 2016;6:23281. doi: 10.1038/srep23281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kametani F., Nonaka T., Suzuki T., Arai T., Dohmae N., Akiyama H., Hasegawa M. Identification of casein kinase-1 phosphorylation sites on TDP-43. Biochem. Biophys. Res. Commun. 2009;382:405–409. doi: 10.1016/j.bbrc.2009.03.038. [DOI] [PubMed] [Google Scholar]
- 69.Hasegawa M., Arai T., Nonaka T., Kametani F., Yoshida M., Hashizume Y., Beach T.G., Buratti E., Baralle F., Morita M., et al. Phosphorylated TDP-43 in frontotemporal lobar degeneration and amyotrophic lateral sclerosis. Ann. Neurol. 2008;64:60–70. doi: 10.1002/ana.21425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Cracco L., Doud E.H., Hallinan G.I., Garringer H.J., Jacobsen M.H., Richardson R.M., Buratti E., Vidal R., Ghetti B., Newell K.L. Distinguishing post-translational modifications in dominantly inherited frontotemporal dementias: FTLD-TDP Type A (GRN) vs Type B (C9orf72) Neuropathol. Appl. Neurobiol. 2022;48:e12836. doi: 10.1111/nan.12836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Laferriere F., Maniecka Z., Perez-Berlanga M., Hruska-Plochan M., Gilhespy L., Hock E.M., Wagner U., Afroz T., Boersema P.J., Barmettler G., et al. TDP-43 extracted from frontotemporal lobar degeneration subject brains displays distinct aggregate assemblies and neurotoxic effects reflecting disease progression rates. Nat. Neurosci. 2019;22:65–77. doi: 10.1038/s41593-018-0294-y. [DOI] [PubMed] [Google Scholar]
- 72.Feneberg E., Charles P.D., Finelli M.J., Scott C., Kessler B.M., Fischer R., Ansorge O., Gray E., Talbot K., Turner M.R. Detection and quantification of novel C-terminal TDP-43 fragments in ALS-TDP. Brain Pathol. 2021;31:e12923. doi: 10.1111/bpa.12923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Pobran T.D., Forgrave L.M., Zheng Y.Z., Lim J.G.K., Mackenzie I.R.A., DeMarco M.L. Detection and characterization of TDP-43 in human cells and tissues by multiple reaction monitoring mass spectrometry. Clin. Mass Spectrom. 2019;14 Pt B:66–73. doi: 10.1016/j.clinms.2019.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Pobran T.D., Yang D., Mackenzie I.R.A., DeMarco M.L. Aptamer-based enrichment of TDP-43 from human cells and tissues with quantification by HPLC-MS/MS. J. Neurosci. Methods. 2021;363:109344. doi: 10.1016/j.jneumeth.2021.109344. [DOI] [PubMed] [Google Scholar]
- 75.Donde A., Sun M., Ling J.P., Braunstein K.E., Pang B., Wen X., Cheng X., Chen L., Wong P.C. Splicing repression is a major function of TDP-43 in motor neurons. Acta Neuropathol. 2019;138:813–826. doi: 10.1007/s00401-019-02042-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Highley J.R., Kirby J., Jansweijer J.A., Webb P.S., Hewamadduma C.A., Heath P.R., Higginbottom A., Raman R., Ferraiuolo L., Cooper-Knock J., et al. Loss of nuclear TDP-43 in amyotrophic lateral sclerosis (ALS) causes altered expression of splicing machinery and widespread dysregulation of RNA splicing in motor neurones. Neuropathol. Appl. Neurobiol. 2014;40:670–685. doi: 10.1111/nan.12148. [DOI] [PubMed] [Google Scholar]
- 77.Scaber J., Talbot K. What is the role of TDP-43 in C9orf72-related amyotrophic lateral sclerosis and frontemporal dementia? Brain. 2016;139:3057–3059. doi: 10.1093/brain/aww264. [DOI] [PubMed] [Google Scholar]
- 78.Vatsavayai S.C., Yoon S.J., Gardner R.C., Gendron T.F., Vargas J.N., Trujillo A., Pribadi M., Phillips J.J., Gaus S.E., Hixson J.D., et al. Timing and significance of pathological features in C9orf72 expansion-associated frontotemporal dementia. Brain. 2016;139:3202–3216. doi: 10.1093/brain/aww250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ling J.P., Pletnikova O., Troncoso J.C., Wong P.C. TDP-43 repression of nonconserved cryptic exons is compromised in ALS-FTD. Science. 2015;349:650–655. doi: 10.1126/science.aab0983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Melamed Z., Lopez-Erauskin J., Baughn M.W., Zhang O., Drenner K., Sun Y., Freyermuth F., McMahon M.A., Beccari M.S., Artates J.W., et al. Premature polyadenylation-mediated loss of stathmin-2 is a hallmark of TDP-43-dependent neurodegeneration. Nat. Neurosci. 2019;22:180–190. doi: 10.1038/s41593-018-0293-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Brown A.L., Wilkins O.G., Keuss M.J., Hill S.E., Zanovello M., Lee W.C., Bampton A., Lee F.C.Y., Masino L., Qi Y.A., et al. TDP-43 loss and ALS-risk SNPs drive mis-splicing and depletion of UNC13A. Nature. 2022;603:131–137. doi: 10.1038/s41586-022-04436-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Prudencio M., Humphrey J., Pickles S., Brown A.L., Hill S.E., Kachergus J.M., Shi J., Heckman M.G., Spiegel M.R., Cook C., et al. Truncated stathmin-2 is a marker of TDP-43 pathology in frontotemporal dementia. J. Clin. Invest. 2020;130:6080–6092. doi: 10.1172/JCI139741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Theunissen F., Anderton R.S., Mastaglia F.L., Flynn L.L., Winter S.J., James I., Bedlack R., Hodgetts S., Fletcher S., Wilton S.D., et al. Novel STMN2 Variant Linked to Amyotrophic Lateral Sclerosis Risk and Clinical Phenotype. Front. Aging Neurosci. 2021;13:658226. doi: 10.3389/fnagi.2021.658226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Klim J.R., Williams L.A., Limone F., Guerra San Juan I., Davis-Dusenbery B.N., Mordes D.A., Burberry A., Steinbaugh M.J., Gamage K.K., Kirchner R., et al. ALS-implicated protein TDP-43 sustains levels of STMN2, a mediator of motor neuron growth and repair. Nat. Neurosci. 2019;22:167–179. doi: 10.1038/s41593-018-0300-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Ma X.R., Prudencio M., Koike Y., Vatsavayai S.C., Kim G., Harbinski F., Briner A., Rodriguez C.M., Guo C., Akiyama T., et al. TDP-43 represses cryptic exon inclusion in the FTD-ALS gene UNC13A. Nature. 2022;603:124–130. doi: 10.1038/s41586-022-04424-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Augustin I., Rosenmund C., Sudhof T.C., Brose N. Munc13-1 is essential for fusion competence of glutamatergic synaptic vesicles. Nature. 1999;400:457–461. doi: 10.1038/22768. [DOI] [PubMed] [Google Scholar]
- 87.Deng L., Kaeser P.S., Xu W., Sudhof T.C. RIM proteins activate vesicle priming by reversing autoinhibitory homodimerization of Munc13. Neuron. 2011;69:317–331. doi: 10.1016/j.neuron.2011.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Lipstein N., Verhoeven-Duif N.M., Michelassi F.E., Calloway N., van Hasselt P.M., Pienkowska K., van Haaften G., van Haelst M.M., van Empelen R., Cuppen I., et al. Synaptic UNC13A protein variant causes increased neurotransmission and dyskinetic movement disorder. J. Clin. Invest. 2017;127:1005–1018. doi: 10.1172/JCI90259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Tan H.H.G., Westeneng H.J., van der Burgh H.K., van Es M.A., Bakker L.A., van Veenhuijzen K., van Eijk K.R., van Eijk R.P.A., Veldink J.H., van den Berg L.H. The Distinct Traits of the UNC13A Polymorphism in Amyotrophic Lateral Sclerosis. Ann. Neurol. 2020;88:796–806. doi: 10.1002/ana.25841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Diekstra F.P., Van Deerlin V.M., van Swieten J.C., Al-Chalabi A., Ludolph A.C., Weishaupt J.H., Hardiman O., Landers J.E., Brown R.H., Jr., van Es M.A., et al. C9orf72 and UNC13A are shared risk loci for amyotrophic lateral sclerosis and frontotemporal dementia: A genome-wide meta-analysis. Ann. Neurol. 2014;76:120–133. doi: 10.1002/ana.24198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Diekstra F.P., van Vught P.W., van Rheenen W., Koppers M., Pasterkamp R.J., van Es M.A., Schelhaas H.J., de Visser M., Robberecht W., Van Damme P., et al. UNC13A is a modifier of survival in amyotrophic lateral sclerosis. Neurobiol. Aging. 2012;33:630-e3. doi: 10.1016/j.neurobiolaging.2011.10.029. [DOI] [PubMed] [Google Scholar]
- 92.van Es M.A., Veldink J.H., Saris C.G., Blauw H.M., van Vught P.W., Birve A., Lemmens R., Schelhaas H.J., Groen E.J., Huisman M.H., et al. Genome-wide association study identifies 19p13.3 (UNC13A) and 9p21.2 as susceptibility loci for sporadic amyotrophic lateral sclerosis. Nat. Genet. 2009;41:1083–1087. doi: 10.1038/ng.442. [DOI] [PubMed] [Google Scholar]
- 93.Hruska-Plochan M., Betz K.M., Ronchi S., Wiersma V.I., Maniecka Z., Hock E.M., Laferriere F., Sahadevan S., Hoop V., Delvendahl I., et al. Human neural networks with sparse TDP-43 pathology reveal NPTX2 misregulation in ALS/FTLD. bioRxiv. 2021;9:12. doi: 10.1101/2021.12.08.471089. [DOI] [Google Scholar]
- 94.Tollervey J.R., Curk T., Rogelj B., Briese M., Cereda M., Kayikci M., Konig J., Hortobagyi T., Nishimura A.L., Zupunski V., et al. Characterizing the RNA targets and position-dependent splicing regulation by TDP-43. Nat. Neurosci. 2011;14:452–458. doi: 10.1038/nn.2778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.van der Ende E.L., Xiao M., Xu D., Poos J.M., Panman J.L., Jiskoot L.C., Meeter L.H., Dopper E.G., Papma J.M., Heller C., et al. Neuronal pentraxin 2: A synapse-derived CSF biomarker in genetic frontotemporal dementia. J. Neurol. Neurosurg. Psychiatry. 2020;91:612–621. doi: 10.1136/jnnp-2019-322493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Cooper-Knock J., Green C., Altschuler G., Wei W., Bury J.J., Heath P.R., Wyles M., Gelsthorpe C., Highley J.R., Lorente-Pons A., et al. A data-driven approach links microglia to pathology and prognosis in amyotrophic lateral sclerosis. Acta Neuropathol. Commun. 2017;5:23. doi: 10.1186/s40478-017-0424-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Oeckl P., Weydt P., Thal D.R., Weishaupt J.H., Ludolph A.C., Otto M. Proteomics in cerebrospinal fluid and spinal cord suggests UCHL1, MAP2 and GPNMB as biomarkers and underpins importance of transcriptional pathways in amyotrophic lateral sclerosis. Acta Neuropathol. 2020;139:119–134. doi: 10.1007/s00401-019-02093-x. [DOI] [PubMed] [Google Scholar]
- 98.Bian Y., Zheng R., Bayer F.P., Wong C., Chang Y.C., Meng C., Zolg D.P., Reinecke M., Zecha J., Wiechmann S., et al. Robust, reproducible and quantitative analysis of thousands of proteomes by micro-flow LC-MS/MS. Nat. Commun. 2020;11:157. doi: 10.1038/s41467-019-13973-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Heywood W.E., Galimberti D., Bliss E., Sirka E., Paterson R.W., Magdalinou N.K., Carecchio M., Reid E., Heslegrave A., Fenoglio C., et al. Identification of novel CSF biomarkers for neurodegeneration and their validation by a high-throughput multiplexed targeted proteomic assay. Mol. Neurodegener. 2015;10:64. doi: 10.1186/s13024-015-0059-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Davis S.A., Itaman S., Khalid-Janney C.M., Sherard J.A., Dowell J.A., Cairns N.J., Gitcho M.A. TDP-43 interacts with mitochondrial proteins critical for mitophagy and mitochondrial dynamics. Neurosci. Lett. 2018;678:8–15. doi: 10.1016/j.neulet.2018.04.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Umoh M.E., Dammer E.B., Dai J., Duong D.M., Lah J.J., Levey A.I., Gearing M., Glass J.D., Seyfried N.T. A proteomic network approach across the ALS-FTD disease spectrum resolves clinical phenotypes and genetic vulnerability in human brain. EMBO Mol. Med. 2018;10:48–62. doi: 10.15252/emmm.201708202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Mehta A.R., Gregory J.M., Dando O., Carter R.N., Burr K., Nanda J., Story D., McDade K., Smith C., Morton N.M., et al. Mitochondrial bioenergetic deficits in C9orf72 amyotrophic lateral sclerosis motor neurons cause dysfunctional axonal homeostasis. Acta Neuropathol. 2021;141:257–279. doi: 10.1007/s00401-020-02252-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Paron F., Barattucci S., Cappelli S., Romano M., Berlingieri C., Stuani C., Laurents D., Mompean M., Buratti E. Unraveling the toxic effects mediated by the neurodegenerative disease-associated S375G mutation of TDP-43 and its S375E phosphomimetic variant. J. Biol. Chem. 2022;298:102252. doi: 10.1016/j.jbc.2022.102252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Yu C.H., Davidson S., Harapas C.R., Hilton J.B., Mlodzianoski M.J., Laohamonthonkul P., Louis C., Low R.R.J., Moecking J., De Nardo D., et al. TDP-43 Triggers Mitochondrial DNA Release via mPTP to Activate cGAS/STING in ALS. Cell. 2020;183:636–649.e618. doi: 10.1016/j.cell.2020.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Lucini C.B., Braun R.J. Mitochondrion-Dependent Cell Death in TDP-43 Proteinopathies. Biomedicines. 2021;9:376. doi: 10.3390/biomedicines9040376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Freischmidt A., Wieland T., Richter B., Ruf W., Schaeffer V., Muller K., Marroquin N., Nordin F., Hubers A., Weydt P., et al. Haploinsufficiency of TBK1 causes familial ALS and fronto-temporal dementia. Nat. Neurosci. 2015;18:631–636. doi: 10.1038/nn.4000. [DOI] [PubMed] [Google Scholar]
- 107.Brenner D., Sieverding K., Bruno C., Luningschror P., Buck E., Mungwa S., Fischer L., Brockmann S.J., Ulmer J., Bliederhauser C., et al. Heterozygous Tbk1 loss has opposing effects in early and late stages of ALS in mice. J. Exp. Med. 2019;216:267–278. doi: 10.1084/jem.20180729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Bevan-Jones W.R., Cope T.E., Jones P.S., Kaalund S.S., Passamonti L., Allinson K., Green O., Hong Y.T., Fryer T.D., Arnold R., et al. Neuroinflammation and protein aggregation co-localize across the frontotemporal dementia spectrum. Brain. 2020;143:1010–1026. doi: 10.1093/brain/awaa033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Steinacker P., Verde F., Fang L., Feneberg E., Oeckl P., Roeber S., Anderl-Straub S., Danek A., Diehl-Schmid J., Fassbender K., et al. Chitotriosidase (CHIT1) is increased in microglia and macrophages in spinal cord of amyotrophic lateral sclerosis and cerebrospinal fluid levels correlate with disease severity and progression. J. Neurol. Neurosurg. Psychiatry. 2018;89:239–247. doi: 10.1136/jnnp-2017-317138. [DOI] [PubMed] [Google Scholar]
- 110.Thompson A.G., Gray E., Thezenas M.L., Charles P.D., Evetts S., Hu M.T., Talbot K., Fischer R., Kessler B.M., Turner M.R. Cerebrospinal fluid macrophage biomarkers in amyotrophic lateral sclerosis. Ann. Neurol. 2018;83:258–268. doi: 10.1002/ana.25143. [DOI] [PubMed] [Google Scholar]
- 111.Gille B., De Schaepdryver M., Dedeene L., Goossens J., Claeys K.G., Van Den Bosch L., Tournoy J., Van Damme P., Poesen K. Inflammatory markers in cerebrospinal fluid: Independent prognostic biomarkers in amyotrophic lateral sclerosis? J. Neurol. Neurosurg. Psychiatry. 2019;90:1338–1346. doi: 10.1136/jnnp-2018-319586. [DOI] [PubMed] [Google Scholar]
- 112.Abu-Rumeileh S., Steinacker P., Polischi B., Mammana A., Bartoletti-Stella A., Oeckl P., Baiardi S., Zenesini C., Huss A., Cortelli P., et al. CSF biomarkers of neuroinflammation in distinct forms and subtypes of neurodegenerative dementia. Alzheimers Res. Ther. 2019;12:2. doi: 10.1186/s13195-019-0562-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Oeckl P., Weydt P., Steinacker P., Anderl-Straub S., Nordin F., Volk A.E., Diehl-Schmid J., Andersen P.M., Kornhuber J., Danek A., et al. Different neuroinflammatory profile in amyotrophic lateral sclerosis and frontotemporal dementia is linked to the clinical phase. J. Neurol. Neurosurg. Psychiatry. 2019;90:4–10. doi: 10.1136/jnnp-2018-318868. [DOI] [PubMed] [Google Scholar]
- 114.Thompson A.G., Gray E., Bampton A., Raciborska D., Talbot K., Turner M.R. CSF chitinase proteins in amyotrophic lateral sclerosis. J. Neurol. Neurosurg. Psychiatry. 2019;90:1215–1220. doi: 10.1136/jnnp-2019-320442. [DOI] [PubMed] [Google Scholar]
- 115.Illan-Gala I., Alcolea D., Montal V., Dols-Icardo O., Munoz L., de Luna N., Turon-Sans J., Cortes-Vicente E., Sanchez-Saudinos M.B., Subirana A., et al. CSF sAPPbeta, YKL-40, and NfL along the ALS-FTD spectrum. Neurology. 2018;91:e1619–e1628. doi: 10.1212/WNL.0000000000006383. [DOI] [PubMed] [Google Scholar]
- 116.Ling S.C., Polymenidou M., Cleveland D.W. Converging mechanisms in ALS and FTD: Disrupted RNA and protein homeostasis. Neuron. 2013;79:416–438. doi: 10.1016/j.neuron.2013.07.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.de Boer E.M.J., Orie V.K., Williams T., Baker M.R., De Oliveira H.M., Polvikoski T., Silsby M., Menon P., van den Bos M., Halliday G.M., et al. TDP-43 proteinopathies: A new wave of neurodegenerative diseases. J. Neurol. Neurosurg. Psychiatry. 2020 doi: 10.1136/jnnp-2020-322983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Del Campo M., Zetterberg H., Gandy S., Onyike C.U., Oliveira F., Udeh-Momoh C., Lleo A., Teunissen C.E., Pijnenburg Y. New developments of biofluid-based biomarkers for routine diagnosis and disease trajectories in frontotemporal dementia. Alzheimers Dement. 2022;18:2292–22307. doi: 10.1002/alz.12643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Kwiatkowski T.J., Jr., Bosco D.A., Leclerc A.L., Tamrazian E., Vanderburg C.R., Russ C., Davis A., Gilchrist J., Kasarskis E.J., Munsat T., et al. Mutations in the FUS/TLS gene on chromosome 16 cause familial amyotrophic lateral sclerosis. Science. 2009;323:1205–1208. doi: 10.1126/science.1166066. [DOI] [PubMed] [Google Scholar]
- 120.Vance C., Rogelj B., Hortobagyi T., De Vos K.J., Nishimura A.L., Sreedharan J., Hu X., Smith B., Ruddy D., Wright P., et al. Mutations in FUS, an RNA processing protein, cause familial amyotrophic lateral sclerosis type 6. Science. 2009;323:1208–1211. doi: 10.1126/science.1165942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Chio A., Mazzini L., D’Alfonso S., Corrado L., Canosa A., Moglia C., Manera U., Bersano E., Brunetti M., Barberis M., et al. The multistep hypothesis of ALS revisited: The role of genetic mutations. Neurology. 2018;91:e635–e642. doi: 10.1212/WNL.0000000000005996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Pasetto L., Grassano M., Pozzi S., Luotti S., Sammali E., Migazzi A., Basso M., Spagnolli G., Biasini E., Micotti E., et al. Defective cyclophilin A induces TDP-43 proteinopathy: Implications for amyotrophic lateral sclerosis and frontotemporal dementia. Brain. 2021;144:3710–3726. doi: 10.1093/brain/awab333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Nardo G., Pozzi S., Pignataro M., Lauranzano E., Spano G., Garbelli S., Mantovani S., Marinou K., Papetti L., Monteforte M., et al. Amyotrophic lateral sclerosis multiprotein biomarkers in peripheral blood mononuclear cells. PLoS ONE. 2011;6:e25545. doi: 10.1371/journal.pone.0025545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Pasetto L., Callegaro S., Corbelli A., Fiordaliso F., Ferrara D., Brunelli L., Sestito G., Pastorelli R., Bianchi E., Cretich M., et al. Decoding distinctive features of plasma extracellular vesicles in amyotrophic lateral sclerosis. Mol. Neurodegener. 2021;16:52. doi: 10.1186/s13024-021-00470-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Lehmer C., Oeckl P., Weishaupt J.H., Volk A.E., Diehl-Schmid J., Schroeter M.L., Lauer M., Kornhuber J., Levin J., Fassbender K., et al. Poly-GP in cerebrospinal fluid links C9orf72-associated dipeptide repeat expression to the asymptomatic phase of ALS/FTD. EMBO Mol. Med. 2017;9:859–868. doi: 10.15252/emmm.201607486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Miller T.M., Cudkowicz M.E., Genge A., Shaw P.J., Sobue G., Bucelli R.C., Chio A., Van Damme P., Ludolph A.C., Glass J.D., et al. Trial of Antisense Oligonucleotide Tofersen for SOD1 ALS. N. Engl. J. Med. 2022;387:1099–1110. doi: 10.1056/NEJMoa2204705. [DOI] [PubMed] [Google Scholar]
- 127.Winer L., Srinivasan D., Chun S., Lacomis D., Jaffa M., Fagan A., Holtzman D.M., Wancewicz E., Bennett C.F., Bowser R., et al. SOD1 in cerebral spinal fluid as a pharmacodynamic marker for antisense oligonucleotide therapy. JAMA Neurol. 2013;70:201–207. doi: 10.1001/jamaneurol.2013.593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Eitan C., Hornstein E. Vulnerability of microRNA biogenesis in FTD-ALS. Brain Res. 2016;1647:105–111. doi: 10.1016/j.brainres.2015.12.063. [DOI] [PubMed] [Google Scholar]
- 129.Gascon E., Gao F.B. The emerging roles of microRNAs in the pathogenesis of frontotemporal dementia-amyotrophic lateral sclerosis (FTD-ALS) spectrum disorders. J. Neurogenet. 2014;28:30–40. doi: 10.3109/01677063.2013.876021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Freischmidt A., Muller K., Zondler L., Weydt P., Volk A.E., Bozic A.L., Walter M., Bonin M., Mayer B., von Arnim C.A., et al. Serum microRNAs in patients with genetic amyotrophic lateral sclerosis and pre-manifest mutation carriers. Brain. 2014;137:2938–2950. doi: 10.1093/brain/awu249. [DOI] [PubMed] [Google Scholar]
- 131.Kawahara Y., Mieda-Sato A. TDP-43 promotes microRNA biogenesis as a component of the Drosha and Dicer complexes. Proc. Natl. Acad. Sci. USA. 2012;109:3347–3352. doi: 10.1073/pnas.1112427109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Buratti E., De Conti L., Stuani C., Romano M., Baralle M., Baralle F. Nuclear factor TDP-43 can affect selected microRNA levels. FEBS J. 2010;277:2268–2281. doi: 10.1111/j.1742-4658.2010.07643.x. [DOI] [PubMed] [Google Scholar]
- 133.Freischmidt A., Muller K., Ludolph A.C., Weishaupt J.H. Systemic dysregulation of TDP-43 binding microRNAs in amyotrophic lateral sclerosis. Acta Neuropathol. Commun. 2013;1:42. doi: 10.1186/2051-5960-1-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Dolinar A., Koritnik B., Glavac D., Ravnik-Glavac M. Circular RNAs as Potential Blood Biomarkers in Amyotrophic Lateral Sclerosis. Mol. Neurobiol. 2019;56:8052–8062. doi: 10.1007/s12035-019-1627-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Gagliardi S., Zucca S., Pandini C., Diamanti L., Bordoni M., Sproviero D., Arigoni M., Olivero M., Pansarasa O., Ceroni M., et al. Long non-coding and coding RNAs characterization in Peripheral Blood Mononuclear Cells and Spinal Cord from Amyotrophic Lateral Sclerosis patients. Sci. Rep. 2018;8:2378. doi: 10.1038/s41598-018-20679-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Liu W., Wang Z., Liu L., Yang Z., Liu S., Ma Z., Liu Y., Ma Y., Zhang L., Zhang X., et al. LncRNA Malat1 inhibition of TDP43 cleavage suppresses IRF3-initiated antiviral innate immunity. Proc. Natl. Acad. Sci. USA. 2020;117:23695–23706. doi: 10.1073/pnas.2003932117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Matsukawa K., Kukharsky M.S., Park S.K., Park S., Watanabe N., Iwatsubo T., Hashimoto T., Liebman S.W., Shelkovnikova T.A. Long non-coding RNA NEAT1_1 ameliorates TDP-43 toxicity in in vivo models of TDP-43 proteinopathy. RNA Biol. 2021;18:1546–1554. doi: 10.1080/15476286.2020.1860580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Teunissen C.E., Elias N., Koel-Simmelink M.J., Durieux-Lu S., Malekzadeh A., Pham T.V., Piersma S.R., Beccari T., Meeter L.H., Dopper E.G., et al. Novel diagnostic cerebrospinal fluid biomarkers for pathologic subtypes of frontotemporal dementia identified by proteomics. Alzheimers Dement. (Amst) 2016;2:86–94. doi: 10.1016/j.dadm.2015.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Seelaar H., Rohrer J.D., Pijnenburg Y.A., Fox N.C., van Swieten J.C. Clinical, genetic and pathological heterogeneity of frontotemporal dementia: A review. J. Neurol. Neurosurg. Psychiatry. 2011;82:476–486. doi: 10.1136/jnnp.2010.212225. [DOI] [PubMed] [Google Scholar]
- 140.Patel R., Brophy C., Hickling M., Neve J., Furger A. Alternative cleavage and polyadenylation of genes associated with protein turnover and mitochondrial function are deregulated in Parkinson’s, Alzheimer’s and ALS disease. BMC Med. Genomics. 2019;12:60. doi: 10.1186/s12920-019-0509-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Koyama A., Sugai A., Kato T., Ishihara T., Shiga A., Toyoshima Y., Koyama M., Konno T., Hirokawa S., Yokoseki A., et al. Increased cytoplasmic TARDBP mRNA in affected spinal motor neurons in ALS caused by abnormal autoregulation of TDP-43. Nucleic Acids Res. 2016;44:5820–5836. doi: 10.1093/nar/gkw499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Osaka H., Wang Y.L., Takada K., Takizawa S., Setsuie R., Li H., Sato Y., Nishikawa K., Sun Y.J., Sakurai M., et al. Ubiquitin carboxy-terminal hydrolase L1 binds to and stabilizes monoubiquitin in neuron. Hum. Mol. Genet. 2003;12:1945–1958. doi: 10.1093/hmg/ddg211. [DOI] [PubMed] [Google Scholar]
- 143.Farrawell N.E., McAlary L., Lum J.S., Chisholm C.G., Warraich S.T., Blair I.P., Vine K.L., Saunders D.N., Yerbury J.J. Ubiquitin Homeostasis Is Disrupted in TDP-43 and FUS Cell Models of ALS. iScience. 2020;23:101700. doi: 10.1016/j.isci.2020.101700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Steinacker P., Feneberg E., Weishaupt J., Brettschneider J., Tumani H., Andersen P.M., von Arnim C.A., Bohm S., Kassubek J., Kubisch C., et al. Neurofilaments in the diagnosis of motoneuron diseases: A prospective study on 455 patients. J. Neurol. Neurosurg. Psychiatry. 2016;87:12–20. doi: 10.1136/jnnp-2015-311387. [DOI] [PubMed] [Google Scholar]
- 145.Gendron T.F., Chew J., Stankowski J.N., Hayes L.R., Zhang Y.J., Prudencio M., Carlomagno Y., Daughrity L.M., Jansen-West K., Perkerson E.A., et al. Poly(GP) proteins are a useful pharmacodynamic marker for C9ORF72-associated amyotrophic lateral sclerosis. Sci. Transl. Med. 2017;9 doi: 10.1126/scitranslmed.aai7866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Wilke C., Preische O., Deuschle C., Roeben B., Apel A., Barro C., Maia L., Maetzler W., Kuhle J., Synofzik M. Neurofilament light chain in FTD is elevated not only in cerebrospinal fluid, but also in serum. J. Neurol. Neurosurg. Psychiatry. 2016;87:1270–1272. doi: 10.1136/jnnp-2015-312972. [DOI] [PubMed] [Google Scholar]
- 147.van der Ende E.L., Meeter L.H., Poos J.M., Panman J.L., Jiskoot L.C., Dopper E.G.P., Papma J.M., de Jong F.J., Verberk I.M.W., Teunissen C., et al. Serum neurofilament light chain in genetic frontotemporal dementia: A longitudinal, multicentre cohort study. Lancet Neurol. 2019;18:1103–1111. doi: 10.1016/S1474-4422(19)30354-0. [DOI] [PubMed] [Google Scholar]
- 148.Silva-Spinola A., Lima M., Leitao M.J., Duraes J., Tabuas-Pereira M., Almeida M.R., Santana I., Baldeiras I. Serum neurofilament light chain as a surrogate of cognitive decline in sporadic and familial frontotemporal dementia. Eur. J. Neurol. 2022;29:36–46. doi: 10.1111/ene.15058. [DOI] [PubMed] [Google Scholar]
- 149.Delaby C., Alcolea D., Carmona-Iragui M., Illan-Gala I., Morenas-Rodriguez E., Barroeta I., Altuna M., Estelles T., Santos-Santos M., Turon-Sans J., et al. Differential levels of Neurofilament Light protein in cerebrospinal fluid in patients with a wide range of neurodegenerative disorders. Sci. Rep. 2020;10:9161. doi: 10.1038/s41598-020-66090-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Abu-Rumeileh S., Mometto N., Bartoletti-Stella A., Polischi B., Oppi F., Poda R., Stanzani-Maserati M., Cortelli P., Liguori R., Capellari S., et al. Cerebrospinal Fluid Biomarkers in Patients with Frontotemporal Dementia Spectrum: A Single-Center Study. J. Alzheimers Dis. 2018;66:551–563. doi: 10.3233/JAD-180409. [DOI] [PubMed] [Google Scholar]
- 151.Suarez-Calvet M., Kleinberger G., Araque Caballero M.A., Brendel M., Rominger A., Alcolea D., Fortea J., Lleo A., Blesa R., Gispert J.D., et al. sTREM2 cerebrospinal fluid levels are a potential biomarker for microglia activity in early-stage Alzheimer’s disease and associate with neuronal injury markers. EMBO Mol. Med. 2016;8:466–476. doi: 10.15252/emmm.201506123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Woollacott I.O.C., Nicholas J.M., Heslegrave A., Heller C., Foiani M.S., Dick K.M., Russell L.L., Paterson R.W., Keshavan A., Fox N.C., et al. Cerebrospinal fluid soluble TREM2 levels in frontotemporal dementia differ by genetic and pathological subgroup. Alzheimers Res. Ther. 2018;10:79. doi: 10.1186/s13195-018-0405-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Cenik B., Sephton C.F., Kutluk Cenik B., Herz J., Yu G. Progranulin: A proteolytically processed protein at the crossroads of inflammation and neurodegeneration. J. Biol. Chem. 2012;287:32298–32306. doi: 10.1074/jbc.R112.399170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Sellami L., Rucheton B., Ben Younes I., Camuzat A., Saracino D., Rinaldi D., Epelbaum S., Azuar C., Levy R., Auriacombe S., et al. Plasma progranulin levels for frontotemporal dementia in clinical practice: A 10-year French experience. Neurobiol. Aging. 2020;91:167-e1. doi: 10.1016/j.neurobiolaging.2020.02.014. [DOI] [PubMed] [Google Scholar]
- 155.Kortvelyessy P., Heinze H.J., Prudlo J., Bittner D. CSF Biomarkers of Neurodegeneration in Progressive Non-fluent Aphasia and Other Forms of Frontotemporal Dementia: Clues for Pathomechanisms? Front. Neurol. 2018;9:504. doi: 10.3389/fneur.2018.00504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Cooper Y.A., Nachun D., Dokuru D., Yang Z., Karydas A.M., Serrero G., Yue B., Alzheimer’s Disease Neuroimaging I., Boxer A.L., Miller B.L., et al. Progranulin levels in blood in Alzheimer’s disease and mild cognitive impairment. Ann. Clin. Transl. Neurol. 2018;5:616–629. doi: 10.1002/acn3.560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Portelius E., Olsson B., Hoglund K., Cullen N.C., Kvartsberg H., Andreasson U., Zetterberg H., Sandelius A., Shaw L.M., Lee V.M.Y., et al. Cerebrospinal fluid neurogranin concentration in neurodegeneration: Relation to clinical phenotypes and neuropathology. Acta Neuropathol. 2018;136:363–376. doi: 10.1007/s00401-018-1851-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Janelidze S., Hertze J., Zetterberg H., Landqvist Waldo M., Santillo A., Blennow K., Hansson O. Cerebrospinal fluid neurogranin and YKL-40 as biomarkers of Alzheimer’s disease. Ann. Clin. Transl. Neurol. 2016;3:12–20. doi: 10.1002/acn3.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Clarke M.T.M., Brinkmalm A., Foiani M.S., Woollacott I.O.C., Heller C., Heslegrave A., Keshavan A., Fox N.C., Schott J.M., Warren J.D., et al. CSF synaptic protein concentrations are raised in those with atypical Alzheimer’s disease but not frontotemporal dementia. Alzheimers Res. Ther. 2019;11:105. doi: 10.1186/s13195-019-0564-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Brinkmalm A., Brinkmalm G., Honer W.G., Frolich L., Hausner L., Minthon L., Hansson O., Wallin A., Zetterberg H., Blennow K., et al. SNAP-25 is a promising novel cerebrospinal fluid biomarker for synapse degeneration in Alzheimer’s disease. Mol. Neurodegener. 2014;9:53. doi: 10.1186/1750-1326-9-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Davidsson P., Westman-Brinkmalm A., Nilsson C.L., Lindbjer M., Paulson L., Andreasen N., Sjogren M., Blennow K. Proteome analysis of cerebrospinal fluid proteins in Alzheimer patients. Neuroreport. 2002;13:611–615. doi: 10.1097/00001756-200204160-00015. [DOI] [PubMed] [Google Scholar]
- 162.Ruetschi U., Zetterberg H., Podust V.N., Gottfries J., Li S., Hviid Simonsen A., McGuire J., Karlsson M., Rymo L., Davies H., et al. Identification of CSF biomarkers for frontotemporal dementia using SELDI-TOF. Exp. Neurol. 2005;196:273–281. doi: 10.1016/j.expneurol.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 163.Gloeckner S.F., Meyne F., Wagner F., Heinemann U., Krasnianski A., Meissner B., Zerr I. Quantitative analysis of transthyretin, tau and amyloid-beta in patients with dementia. J. Alzheimers Dis. 2008;14:17–25. doi: 10.3233/JAD-2008-14102. [DOI] [PubMed] [Google Scholar]
- 164.Yang C., Wang H., Li C., Niu H., Luo S., Guo X. Association between clusterin concentration and dementia: A systematic review and meta-analysis. Metab Brain Dis. 2019;34:129–140. doi: 10.1007/s11011-018-0325-0. [DOI] [PubMed] [Google Scholar]
- 165.Jiang C., Hopfner F., Katsikoudi A., Hein R., Catli C., Evetts S., Huang Y., Wang H., Ryder J.W., Kuhlenbaeumer G., et al. Serum neuronal exosomes predict and differentiate Parkinson’s disease from atypical parkinsonism. J. Neurol. Neurosurg. Psychiatry. 2020;91:720–729. doi: 10.1136/jnnp-2019-322588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Mohanty L., Henderson R.D., McCombe P.A., Lee A. Levels of clusterin, CD5L, ficolin-3, and gelsolin in ALS patients and controls. Amyotroph Lateral Scler Front. Degener. 2020;21:631–634. doi: 10.1080/21678421.2020.1779303. [DOI] [PubMed] [Google Scholar]
- 167.Meeter L.H.H., Vijverberg E.G., Del Campo M., Rozemuller A.J.M., Donker Kaat L., de Jong F.J., van der Flier W.M., Teunissen C.E., van Swieten J.C., Pijnenburg Y.A.L. Clinical value of neurofilament and phospho-tau/tau ratio in the frontotemporal dementia spectrum. Neurology. 2018;90:e1231–e1239. doi: 10.1212/WNL.0000000000005261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Pijnenburg Y.A., Verwey N.A., van der Flier W.M., Scheltens P., Teunissen C.E. Discriminative and prognostic potential of cerebrospinal fluid phosphoTau/tau ratio and neurofilaments for frontotemporal dementia subtypes. Alzheimers Dement. (Amst) 2015;1:505–512. doi: 10.1016/j.dadm.2015.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Junttila A., Kuvaja M., Hartikainen P., Siloaho M., Helisalmi S., Moilanen V., Kiviharju A., Jansson L., Tienari P.J., Remes A.M., et al. Cerebrospinal Fluid TDP-43 in Frontotemporal Lobar Degeneration and Amyotrophic Lateral Sclerosis Patients with and without the C9ORF72 Hexanucleotide Expansion. Dement. Geriatr. Cogn. Dis. Extra. 2016;6:142–149. doi: 10.1159/000444788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Noto Y., Shibuya K., Sato Y., Kanai K., Misawa S., Sawai S., Mori M., Uchiyama T., Isose S., Nasu S., et al. Elevated CSF TDP-43 levels in amyotrophic lateral sclerosis: Specificity, sensitivity, and a possible prognostic value. Amyotroph Lateral Scler. 2011;12:140–143. doi: 10.3109/17482968.2010.541263. [DOI] [PubMed] [Google Scholar]
- 171.Katisko K., Huber N., Kokkola T., Hartikainen P., Kruger J., Heikkinen A.L., Paananen V., Leinonen V., Korhonen V.E., Helisalmi S., et al. Serum total TDP-43 levels are decreased in frontotemporal dementia patients with C9orf72 repeat expansion or concomitant motoneuron disease phenotype. Alzheimers Res. Ther. 2022;14:151. doi: 10.1186/s13195-022-01091-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Steinacker P., Hendrich C., Sperfeld A.D., Jesse S., von Arnim C.A., Lehnert S., Pabst A., Uttner I., Tumani H., Lee V.M., et al. TDP-43 in cerebrospinal fluid of patients with frontotemporal lobar degeneration and amyotrophic lateral sclerosis. Arch. Neurol. 2008;65:1481–1487. doi: 10.1001/archneur.65.11.1481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Suarez-Calvet M., Dols-Icardo O., Llado A., Sanchez-Valle R., Hernandez I., Amer G., Anton-Aguirre S., Alcolea D., Fortea J., Ferrer I., et al. Plasma phosphorylated TDP-43 levels are elevated in patients with frontotemporal dementia carrying a C9orf72 repeat expansion or a GRN mutation. J. Neurol. Neurosurg. Psychiatry. 2014;85:684–691. doi: 10.1136/jnnp-2013-305972. [DOI] [PubMed] [Google Scholar]
- 174.Foulds P., McAuley E., Gibbons L., Davidson Y., Pickering-Brown S.M., Neary D., Snowden J.S., Allsop D., Mann D.M. TDP-43 protein in plasma may index TDP-43 brain pathology in Alzheimer’s disease and frontotemporal lobar degeneration. Acta Neuropathol. 2008;116:141–146. doi: 10.1007/s00401-008-0389-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Foulds P.G., Davidson Y., Mishra M., Hobson D.J., Humphreys K.M., Taylor M., Johnson N., Weintraub S., Akiyama H., Arai T., et al. Plasma phosphorylated-TDP-43 protein levels correlate with brain pathology in frontotemporal lobar degeneration. Acta Neuropathol. 2009;118:647–658. doi: 10.1007/s00401-009-0594-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Khalil M., Teunissen C.E., Otto M., Piehl F., Sormani M.P., Gattringer T., Barro C., Kappos L., Comabella M., Fazekas F., et al. Neurofilaments as biomarkers in neurological disorders. Nat. Rev. Neurol. 2018;14:577–589. doi: 10.1038/s41582-018-0058-z. [DOI] [PubMed] [Google Scholar]
- 177.Verde F., Steinacker P., Weishaupt J.H., Kassubek J., Oeckl P., Halbgebauer S., Tumani H., von Arnim C.A.F., Dorst J., Feneberg E., et al. Neurofilament light chain in serum for the diagnosis of amyotrophic lateral sclerosis. J. Neurol. Neurosurg. Psychiatry. 2019;90:157–164. doi: 10.1136/jnnp-2018-318704. [DOI] [PubMed] [Google Scholar]
- 178.Gendron T.F., Group C.O.N.S., Daughrity L.M., Heckman M.G., Diehl N.N., Wuu J., Miller T.M., Pastor P., Trojanowski J.Q., Grossman M., et al. Phosphorylated neurofilament heavy chain: A biomarker of survival for C9ORF72-associated amyotrophic lateral sclerosis. Ann. Neurol. 2017;82:139–146. doi: 10.1002/ana.24980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Steinacker P., Anderl-Straub S., Diehl-Schmid J., Semler E., Uttner I., von Arnim C.A.F., Barthel H., Danek A., Fassbender K., Fliessbach K., et al. Serum neurofilament light chain in behavioral variant frontotemporal dementia. Neurology. 2018;91:e1390–e1401. doi: 10.1212/WNL.0000000000006318. [DOI] [PubMed] [Google Scholar]
- 180.Zhang J.V., Irwin D.J., Blennow K., Zetterberg H., Lee E.B., Shaw L.M., Rascovsky K., Massimo L., McMillan C.T., Chen-Plotkin A., et al. Neurofilament Light Chain Related to Longitudinal Decline in Frontotemporal Lobar Degeneration. Neurol. Clin. Pract. 2021;11:105–116. doi: 10.1212/CPJ.0000000000000959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Thompson A.G., Turner M.R. Untangling neuroinflammation in amyotrophic lateral sclerosis. J. Neurol. Neurosurg. Psychiatry. 2019;90:1303–1304. doi: 10.1136/jnnp-2019-320442. [DOI] [PubMed] [Google Scholar]
- 182.Abdelhak A., Foschi M., Abu-Rumeileh S., Yue J.K., D’Anna L., Huss A., Oeckl P., Ludolph A.C., Kuhle J., Petzold A., et al. Blood GFAP as an emerging biomarker in brain and spinal cord disorders. Nat. Rev. Neurol. 2022;18:158–172. doi: 10.1038/s41582-021-00616-3. [DOI] [PubMed] [Google Scholar]
- 183.Oeckl P., Anderl-Straub S., Von Arnim C.A.F., Baldeiras I., Diehl-Schmid J., Grimmer T., Halbgebauer S., Kort A.M., Lima M., Marques T.M., et al. Serum GFAP differentiates Alzheimer’s disease from frontotemporal dementia and predicts MCI-to-dementia conversion. J. Neurol. Neurosurg. Psychiatry. 2022;93:659–667. doi: 10.1136/jnnp-2021-328547. [DOI] [PubMed] [Google Scholar]
- 184.Guerreiro R., Wojtas A., Bras J., Carrasquillo M., Rogaeva E., Majounie E., Cruchaga C., Sassi C., Kauwe J.S., Younkin S., et al. TREM2 variants in Alzheimer’s disease. N. Engl. J. Med. 2013;368:117–127. doi: 10.1056/NEJMoa1211851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Jonsson T., Stefansson H., Steinberg S., Jonsdottir I., Jonsson P.V., Snaedal J., Bjornsson S., Huttenlocher J., Levey A.I., Lah J.J., et al. Variant of TREM2 associated with the risk of Alzheimer’s disease. N. Engl. J. Med. 2013;368:107–116. doi: 10.1056/NEJMoa1211103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Heslegrave A., Heywood W., Paterson R., Magdalinou N., Svensson J., Johansson P., Ohrfelt A., Blennow K., Hardy J., Schott J., et al. Increased cerebrospinal fluid soluble TREM2 concentration in Alzheimer’s disease. Mol. Neurodegener. 2016;11:3. doi: 10.1186/s13024-016-0071-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Piccio L., Deming Y., Del-Aguila J.L., Ghezzi L., Holtzman D.M., Fagan A.M., Fenoglio C., Galimberti D., Borroni B., Cruchaga C. Cerebrospinal fluid soluble TREM2 is higher in Alzheimer disease and associated with mutation status. Acta Neuropathol. 2016;131:925–933. doi: 10.1007/s00401-016-1533-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Suarez-Calvet M., Morenas-Rodriguez E., Kleinberger G., Schlepckow K., Araque Caballero M.A., Franzmeier N., Capell A., Fellerer K., Nuscher B., Eren E., et al. Early increase of CSF sTREM2 in Alzheimer’s disease is associated with tau related-neurodegeneration but not with amyloid-beta pathology. Mol. Neurodegener. 2019;14:1. doi: 10.1186/s13024-018-0301-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Wilke C., Gillardon F., Deuschle C., Hobert M.A., Jansen I.E., Metzger F.G., Heutink P., Gasser T., Maetzler W., Blauwendraat C., et al. Cerebrospinal Fluid Progranulin, but Not Serum Progranulin, Is Reduced in GRN-Negative Frontotemporal Dementia. Neurodegener Dis. 2017;17:83–88. doi: 10.1159/000448896. [DOI] [PubMed] [Google Scholar]
- 190.Sleegers K., Brouwers N., Maurer-Stroh S., van Es M.A., Van Damme P., van Vught P.W., van der Zee J., Serneels S., De Pooter T., Van den Broeck M., et al. Progranulin genetic variability contributes to amyotrophic lateral sclerosis. Neurology. 2008;71:253–259. doi: 10.1212/01.wnl.0000289191.54852.75. [DOI] [PubMed] [Google Scholar]
- 191.Philips T., De Muynck L., Thu H.N., Weynants B., Vanacker P., Dhondt J., Sleegers K., Schelhaas H.J., Verbeek M., Vandenberghe R., et al. Microglial upregulation of progranulin as a marker of motor neuron degeneration. J. Neuropathol. Exp. Neurol. 2010;69:1191–1200. doi: 10.1097/NEN.0b013e3181fc9aea. [DOI] [PubMed] [Google Scholar]
- 192.Halbgebauer S., Steinacker P., Hengge S., Oeckl P., Abu Rumeileh S., Anderl-Straub S., Lombardi J., Von Arnim C.A.F., Giese A., Ludolph A.C., et al. CSF levels of SNAP-25 are increased early in Creutzfeldt-Jakob and Alzheimer’s disease. J. Neurol. Neurosurg. Psychiatry. 2022;93:1059–1065. doi: 10.1136/jnnp-2021-328646. [DOI] [PubMed] [Google Scholar]
- 193.Serot J.M., Christmann D., Dubost T., Couturier M. Cerebrospinal fluid transthyretin: Aging and late onset Alzheimer’s disease. J. Neurol. Neurosurg. Psychiatry. 1997;63:506–508. doi: 10.1136/jnnp.63.4.506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Poulsen K., Bahl J.M., Tanassi J.T., Simonsen A.H., Heegaard N.H. Characterization and stability of transthyretin isoforms in cerebrospinal fluid examined by immunoprecipitation and high-resolution mass spectrometry of intact protein. Methods. 2012;56:284–292. doi: 10.1016/j.ymeth.2011.12.009. [DOI] [PubMed] [Google Scholar]
- 195.Ranganathan S., Williams E., Ganchev P., Gopalakrishnan V., Lacomis D., Urbinelli L., Newhall K., Cudkowicz M.E., Brown R.H., Jr., Bowser R. Proteomic profiling of cerebrospinal fluid identifies biomarkers for amyotrophic lateral sclerosis. J. Neurochem. 2005;95:1461–1471. doi: 10.1111/j.1471-4159.2005.03478.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Brettschneider J., Lehmensiek V., Mogel H., Pfeifle M., Dorst J., Hendrich C., Ludolph A.C., Tumani H. Proteome analysis reveals candidate markers of disease progression in amyotrophic lateral sclerosis (ALS) Neurosci. Lett. 2010;468:23–27. doi: 10.1016/j.neulet.2009.10.053. [DOI] [PubMed] [Google Scholar]
- 197.Gregory J.M., Whiten D.R., Brown R.A., Barros T.P., Kumita J.R., Yerbury J.J., Satapathy S., McDade K., Smith C., Luheshi L.M., et al. Clusterin protects neurons against intracellular proteotoxicity. Acta Neuropathol. Commun. 2017;5:81. doi: 10.1186/s40478-017-0481-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Pijnenburg Y.A., Janssen J.C., Schoonenboom N.S., Petzold A., Mulder C., Stigbrand T., Norgren N., Heijst H., Hack C.E., Scheltens P., et al. CSF neurofilaments in frontotemporal dementia compared with early onset Alzheimer’s disease and controls. Dement. Geriatr. Cogn. Disord. 2007;23:225–230. doi: 10.1159/000099473. [DOI] [PubMed] [Google Scholar]
- 199.Schoonenboom N.S., Reesink F.E., Verwey N.A., Kester M.I., Teunissen C.E., van de Ven P.M., Pijnenburg Y.A., Blankenstein M.A., Rozemuller A.J., Scheltens P., et al. Cerebrospinal fluid markers for differential dementia diagnosis in a large memory clinic cohort. Neurology. 2012;78:47–54. doi: 10.1212/WNL.0b013e31823ed0f0. [DOI] [PubMed] [Google Scholar]
- 200.Hu W.T., Watts K., Grossman M., Glass J., Lah J.J., Hales C., Shelnutt M., Van Deerlin V., Trojanowski J.Q., Levey A.I. Reduced CSF p-Tau181 to Tau ratio is a biomarker for FTLD-TDP. Neurology. 2013;81:1945–1952. doi: 10.1212/01.wnl.0000436625.63650.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Feneberg E., Steinacker P., Lehnert S., Schneider A., Walther P., Thal D.R., Linsenmeier M., Ludolph A.C., Otto M. Limited role of free TDP-43 as a diagnostic tool in neurodegenerative diseases. Amyotroph Lateral Scler Front. Degener. 2014;15:351–356. doi: 10.3109/21678421.2014.905606. [DOI] [PubMed] [Google Scholar]
- 202.Kuiperij H.B., Versleijen A.A., Beenes M., Verwey N.A., Benussi L., Paterlini A., Binetti G., Teunissen C.E., Raaphorst J., Schelhaas H.J., et al. Tau Rather than TDP-43 Proteins are Potential Cerebrospinal Fluid Biomarkers for Frontotemporal Lobar Degeneration Subtypes: A Pilot Study. J. Alzheimers Dis. 2017;55:585–595. doi: 10.3233/JAD-160386. [DOI] [PubMed] [Google Scholar]
- 203.Tan R.H., Shepherd C.E., Kril J.J., McCann H., McGeachie A., McGinley C., Affleck A., Halliday G.M. Classification of FTLD-TDP cases into pathological subtypes using antibodies against phosphorylated and non-phosphorylated TDP43. Acta Neuropathol. Commun. 2013;1:33. doi: 10.1186/2051-5960-1-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Kasai T., Kojima Y., Ohmichi T., Tatebe H., Tsuji Y., Noto Y.I., Kitani-Morii F., Shinomoto M., Allsop D., Mizuno T., et al. Combined use of CSF NfL and CSF TDP-43 improves diagnostic performance in ALS. Ann. Clin. Transl. Neurol. 2019;6:2489–2502. doi: 10.1002/acn3.50943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Kojima Y., Kasai T., Noto Y.I., Ohmichi T., Tatebe H., Kitaoji T., Tsuji Y., Kitani-Morii F., Shinomoto M., Allsop D., et al. Amyotrophic lateral sclerosis: Correlations between fluid biomarkers of NfL, TDP-43, and tau, and clinical characteristics. PLoS ONE. 2021;16:e0260323. doi: 10.1371/journal.pone.0260323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Sproviero D., La Salvia S., Colombo F., Zucca S., Pansarasa O., Diamanti L., Costa A., Lova L., Giannini M., Gagliardi S., et al. Leukocyte Derived Microvesicles as Disease Progression Biomarkers in Slow Progressing Amyotrophic Lateral Sclerosis Patients. Front. Neurosci. 2019;13:344. doi: 10.3389/fnins.2019.00344. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are openly available in [Pubmed].