Abstract
Background
Globally, helminth infections and cardiometabolic diseases often overlap in populations and individuals. Neither the causal relationship between helminth infections and cardiometabolic diseases nor the effect of helminth eradication on cardiometabolic risk have been reviewed systematically in a large number of human and animal studies.
Methods
We conducted a systematic review assessing the reported effects of helminth infections and anthelmintic treatment on the development and/or severity of cardiometabolic diseases and risk factors. The search was limited to the most prevalent human helminths worldwide. This study followed PRISMA guidelines and was registered prospectively in PROSPERO (CRD42021228610). Searches were performed on December 10, 2020 and rerun on March 2, 2022 using Ovid MEDLINE ALL (1946 to March 2, 2022), Web of Science, Cochrane Library, Global Index Medicus, and Ovid Embase (1974 to March 2, 2022). Randomized clinical trials, cohort, cross-sectional, case-control, and animal studies were included. Two reviewers performed screening independently.
Results
Eighty-four animal and human studies were included in the final analysis. Most studies reported on lipids (45), metabolic syndrome (38), and diabetes (30), with fewer on blood pressure (18), atherosclerotic cardiovascular disease (11), high-sensitivity C-reactive protein (hsCRP, 5), and non-atherosclerotic cardiovascular disease (4). Fifteen different helminth infections were represented. On average, helminth-infected participants had less dyslipidemia, metabolic syndrome, diabetes, and atherosclerotic cardiovascular disease. Eleven studies examined anthelmintic treatment, of which 9 (82%) reported post-treatment increases in dyslipidemia, metabolic syndrome, and diabetes or glucose levels. Results from animal and human studies were generally consistent. No consistent effects of helminth infections on blood pressure, hsCRP, or cardiac function were reported except some trends towards association of schistosome infection with lower blood pressure. The vast majority of evidence linking helminth infections to lower cardiometabolic diseases was reported in those with schistosome infections.
Conclusions
Helminth infections may offer protection against dyslipidemia, metabolic syndrome, diabetes, and atherosclerotic cardiovascular disease. This protection may lessen after anthelmintic treatment. Our findings highlight the need for mechanistic trials to determine the pathways linking helminth infections with cardiometabolic diseases. Such studies could have implications for helminth eradication campaigns and could generate new strategies to address the global challenge of cardiometabolic diseases.
Author summary
Helminth infections are caused by parasitic worms and affect over 1.5 billion people worldwide. Helminth infections and cardiometabolic diseases are both common and overlap with one another in many parts of the world. Studies have separately examined the relationship between helminth infections and various cardiometabolic diseases, but the relationships overall, as well as the impact of treatment of parasitic worms, have not been studied systematically. The authors conducted a systematic review to assess the impact of helminth infections, and treatment of helminth infections, on cardiometabolic diseases and risk factors. Eighty-four total studies were analyzed and included in the final review. People and animals infected with helminths were generally found to have fewer cardiometabolic disease risk factors including better overall cholesterol profiles, less diabetes, and less atherosclerotic heart disease than uninfected study participants. After treatment of helminth infections, participants frequently experienced worsening in those cardiometabolic measurements. There were no consistent effects of helminth infections on blood pressure, high-sensitivity CRP (an inflammatory marker), or other cardiac function. In summary, helminth infections may offer protection against certain cardiometabolic diseases and risk factors. More studies are needed to elucidate the pathways linking helminth infections with cardiometabolic diseases as it may impact how we treat both disease processes in regions where both are prevalent.
Introduction
Cardiometabolic diseases, which include cardiovascular disease and diabetes, are the leading cause of death worldwide, accounting for 32% of global deaths [1]. The incidence of cardiometabolic diseases and well-recognized traditional risk factors for these diseases, such as hypertension and dyslipidemia, have been rising particularly in low- and middle-income countries (LMICs) [2]. Novel interactions with the environment may play a critical role in the development of cardiometabolic diseases and risk factors in these regions.
Helminths infect approximately one-quarter of the world’s population [3] and account for numerous neglected tropical diseases, causing significant morbidity and mortality mainly in LMICs. Given that helminths have co-existed with humans for millennia, it would not be surprising if coevolution has resulted in beneficial effects of helminth infections on human health. Previous systematic reviews have reported that helminth infections can be associated with favorable metabolic function and outcomes, but other cardiometabolic measures and the effects of anthelmintic treatment were not included [4,5]. Additionally, other studies have demonstrated inconsistency in the literature, with some showing that helminth infections worsened or had no effect on metabolic measures [6–8]. Against the backdrop of the World Health Organization’s efforts to eliminate helminth infections by 2030 [9] and these previous data, we sought systematically to review data to investigate: (1) associations between helminth infections and cardiometabolic diseases and risk factors, and (2) whether helminth eradication could alter the prevalence and incidence of cardiometabolic diseases and risk factors. Given a growing number of studies reporting relationships between helminths and cardiovascular health, we hypothesized that helminth infections would be associated with fewer cardiometabolic diseases and risk factors, and that anthelmintic treatment would increase the risk or development of these noncommunicable diseases and conditions.
Methods
We conducted a systematic review to assess the effects of helminth infections on the development and/or severity of cardiometabolic diseases and risk factors. This study was reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and was registered prospectively in PROSPERO (CRD42021228610).
Data sources and searches
A comprehensive search was developed and performed on December 10, 2020 and rerun on March 2, 2022 using Ovid MEDLINE ALL (1946 to March 2, 2022), Web of Science, Cochrane Library, Global Index Medicus, and Ovid Embase (1974 to March 2, 2022). Both English and foreign language papers were included. Databases were searched from inception. Authors were not contacted for further information. Studies were uploaded to the Covidence platform (Melbourne, Australia) for conduct of the screening and extraction phases.
Included study types were randomized clinical trials, cohort, cross-sectional, and case-control studies. Both human and animal studies were included. S1 Table summarizes our study’s predefined search terms, keywords, and study types included, with the full search strategy detailed in S1 Appendix.
Predefined search terms for cardiometabolic diseases and risk factors included systolic blood pressure, total cholesterol, high-density lipoprotein cholesterol (HDL), high-sensitivity C-reactive protein (hsCRP), coronary artery disease (CAD, which included myocardial infarction (MI) and large vessel atherosclerosis), cerebrovascular disease, peripheral vascular disease, heart failure, rheumatic heart disease, congenital heart disease, and cardiomyopathies. These terms were generated by identifying modifiable biomedical components included in 3 widely used calculated cardiac risk equations (Atherosclerotic Cardiovascular Disease 2013 (ASCVD 2013) Risk Calculator, Reynolds Risk Score, and the Framingham Risk Score with Lipids), as well as by including terms in the World Health Organization’s definition of cardiovascular disease [1].
Predefined search terms for metabolic syndrome included abdominal obesity, atherogenic dyslipidemia, raised blood pressure, insulin resistance, and glucose intolerance. These terms were generated according to the biomedical components that characterize metabolic syndrome, as defined by the National Cholesterol Education Program—Adult Treatment Panel (ATP) III report [10]. Prothrombotic and proinflammatory states, also components of the ATP III definition, were not included in the search as there is unclear guidance on how to apply these risk factors to clinical patient care [10]. Additionally, articles that reported host factors without any clear correlation to cardiometabolic diseases were excluded.
Predefined search terms for helminths pathogenic in humans included the soil-transmitted nematodes, filarial nematodes, platyhelminth flukes, and the platyhelminth tapeworm, Taenia solium, as shown in S1 Table. Corresponding diseases for these etiologic agents were also developed into the search (e.g., schistosomiasis for Schistosoma worm species). These helminths were chosen because they are the most prevalent human helminthiases worldwide [11].
Eligibility criteria and study selection
Studies were eligible if they fulfilled all of the following: 1) were a correct study type; 2) had a correct parasite genus and species; 3) had a correct cardiometabolic disease or risk factor; 4) described helminth infection as the exposure and cardiometabolic disease or risk factor as the outcome of the study, or vice versa; and 5) had available full texts or abstracts with enough information for further assessment. Excluded papers included review papers without original data and case reports or case series. Duplicate records were removed. Two investigators independently screened titles and abstracts to identify studies eligible for inclusion using the above criteria, and a third investigator independently resolved discrepancies.
Data extraction and quality assessment
After the completion of the screening methods, data were extracted and quality assessment was performed. Data extracted included helminth species and study type; country of origin; sample size; cardiometabolic outcomes; key findings; effects of anthelmintic therapy on outcomes, if applicable; and study limitations. Quality assessment of data was performed using the Downs and Black checklist [12]. Studies were categorized as “poor,” “fair,” “good,” or “excellent” based on a summative score derived from this checklist, and only those of “fair” quality or above were included in the final analysis.
Data synthesis and analysis
Data were synthesized and analyzed in Stata MP/Version 17 (College Station, Texas) and Microsoft Excel Version 16.53. Descriptive statistics were applied, using medians for continuous variables and proportions for categorical variables.
Cardiometabolic diseases and risk factors reported from included articles were categorized for analysis. These 7 categories included lipids, metabolic syndrome and related parameters, diabetes and related parameters, blood pressure and other cardiovascular hemodynamics, cardiovascular disease (which included CAD, MI, and large vessel atherosclerosis), hsCRP, and non-atherosclerotic cardiovascular disease. It was anticipated that some studies would report on more than one cardiometabolic outcome within the same study; if this occurred, then each outcome was grouped accordingly under the corresponding category (e.g., if study A reported on both lipids and diabetes, then we categorized study A under both the lipids and diabetes categories, highlighting the specific outcome under each corresponding category and incorporating study A in the analysis of each category). Because some components of metabolic syndrome overlap with other cardiometabolic categories, the metabolic syndrome category only included anthropometric measurements (e.g., body mass index (BMI), waist circumference (WC), and waist-to-hip ratio (WHR)), glucose intolerance, and insulin resistance. Other components of metabolic syndrome, such as blood pressure or dyslipidemia, were grouped into the blood pressure and lipids categories, respectively, and not included in the metabolic syndrome category.
Due to the heterogeneity of study designs and inclusion of different cardiometabolic measures and helminth infections, a meta-analysis was not possible.
Results
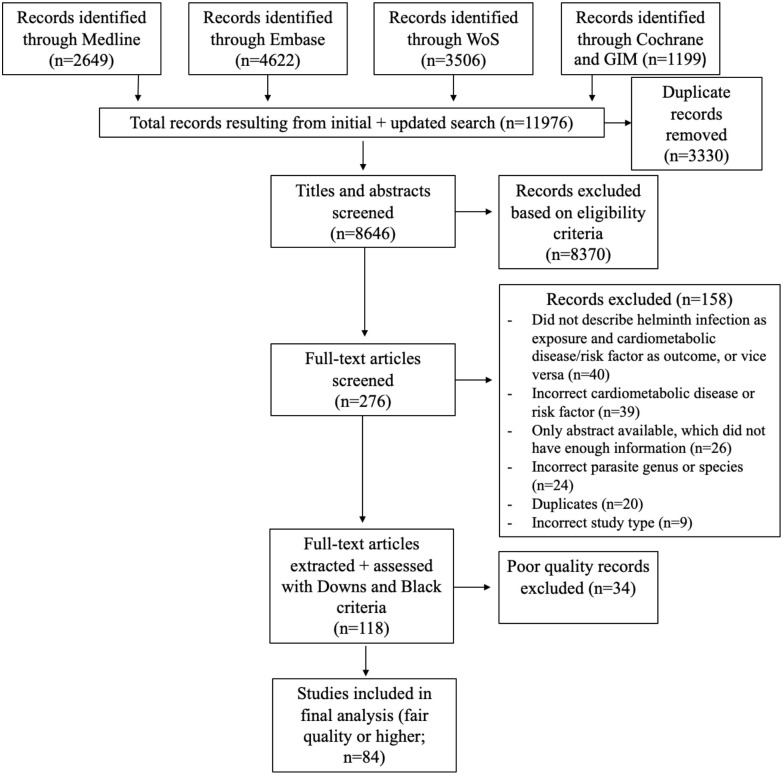
Titles and abstracts of 8,646 studies were screened, after which 276 full-text papers were assessed for inclusion. A total of 118 studies then underwent data extraction and quality assessment with 84, which were determined to be of fair quality or higher, included in the final analysis (Fig 1). Fifteen different helminth species were represented, and these included Ancylostoma duodenale, Ascaris lumbricoides, Brugia malayi, Clonorchis sinensis, Fasciola hepatica, Necator americanus, Onchocerca volvulus, Opisthorchis viverinni, Schistosoma species (including S. haematobium, japonicum, and mansoni), Strongyloides stercoralifigs, Taenia solium, Trichuris trichiura, and Wuchereria bancrofti. Schistosoma species were most represented (S. mansoni (26), S. japonicum (8), unspecified Schistosoma species (7), and S. haematobium (2)) and studied in 43 studies, followed by mixed helminths (12), Strongyloides stercoralis (9), and others (20). The 34 records that did not meet Downs and Black criteria of “fair” or better quality are reported in S1 Supplemental Table. The associations of helminths with each of the 7 categories of cardiometabolic diseases and risk factors are discussed in the following sections.
Fig 1. PRISMA flow diagram of systematic review.
Helminths and lipid profiles
Forty-five studies examined helminth infections and serum lipid profile, including total cholesterol, low-density lipoprotein cholesterol (LDL), HDL, and/or triglycerides (S2 Table). These studies comprised 27 human and 17 animal studies, and 1 mixed human/animal study.
Studies examining serum lipids before and after anthelmintic treatment
Of the 45 studies, 6 reported on serum lipids both before and after anthelmintic treatment. Three of these studies were conducted in humans [8,13,14] and 3 were conducted in animal models [15–17].
Human studies examining serum lipids before and after anthelmintic treatment
One cluster-randomized trial of 1898 adults in Uganda reported lower total cholesterol and LDL at baseline in those with S. mansoni infection than those without [13]. The authors observed a dose-response relationship in which those with moderate to heavy S. mansoni infection had the lowest LDL and triglycerides. Similarly, individuals infected with S. stercoralis also had lower LDL than those without Strongyloides infection. In clusters that received community-wide intensive anthelminthic treatment with quarterly single-dose praziquantel and triple-dose albendazole, the mean LDL increased after 4 years of follow-up, as compared to the mean LDL in communities that received single-dose anthelmintic treatment, which was a significant trend (2.86 vs 2.60 mmol/L; adjusted mean difference, 0.26 [95% CI, −0.03 to 0.56]; P = .08). While this study provides robust evidence for LDL, it should also be noted that ongoing helminth transmission in both study arms at the end of the study and a cluster-randomized design with data reported as community means limited the study’s ability to investigate outcomes at an individual level.
A second human study reported significantly elevated HDL but no differences in serum total cholesterol, LDL, or triglycerides at baseline in 200 adults with O. viverrini infection versus 200 uninfected adults [14]. Six months after treatment with praziquantel, a further increase in HDL was observed.
In contrast, a household, cluster-randomized controlled trial [8] investigated lipid profiles in 1669 Indonesian persons with mixed helminth infections and found no significant associations between helminth infection and serum lipids either at baseline or 52 weeks post-anthelmintic treatment with albendazole.
In summary, 2 out of 3 human studies found that alterations in serum lipids were associated with helminth infections. Treatment of infection led to an increase in serum lipids in both studies [8,9].
Animal studies examining serum lipids before and after anthelmintic treatment
One mouse study examined lipid changes in male mice exposed to S. japonicum cercariae or soluble egg antigen (SEA) [15]. They reported no differences in lipid profiles between cercariae-exposed and unexposed mice at baseline, but mice that were effectively treated with praziquantel had developed elevated LDL and HDL levels by 9 weeks post-treatment, compared to uninfected or persistently infected mice.
One sheep study found lower LDL in Fasciola-infected animals at baseline that increased 28 days after anthelmintic treatment with triclabendazole and levamisole [16]. This was also accompanied by newly elevated total cholesterol and HDL after treatment of infection. This study also reported decreased serum triglycerides after anthelmintic treatment. Limitations included studying only 30 sheep of unclear sex distribution, and possible confounding effect of a peroxisome proliferator receptor alpha agonist, which can affect lipids and was included with the treatment of fasciolosis. Additionally, although infected sheep were treated and had a significant reduction in parasite eggs, sheep still had up to 100,000 eggs per gram of stool post-treatment, suggesting that infection was not completely eradicated.
In another animal study using F. hepatica-infected sheep, the serum total cholesterol, LDL, HDL, and triglycerides were all lower at baseline and remained low with only minor, non-significant increases on day 28 after treatment of infection with triclabendazole and levamisole when compared to uninfected sheep [17]. However, by day 56 post-treatment, differences in total cholesterol, LDL, and triglycerides were no longer present, supporting the hypothesis that anthelmintic treatment would remove the beneficial effects of helminth infection on cardiometabolic risk factors. Limitations of this study included small sample size of 25 sheep and that the study appeared to only compare pre-post treatment lipids in the infected group to baseline measurements obtained in the control group.
In summary, 2 out of 3 animal studies demonstrated that helminth infection was associated with lower lipid levels [16,17]. All 3 studies showed that anthelmintic treatment subsequently increased lipid levels in these animal models [15–17].
Summary of studies examining serum lipids before and after anthelmintic treatment
Taken together, 4 of these 6 studies (67%, 2 human, 2 animal) reported that helminth infection was associated with beneficial lipid levels at baseline [13,14,16,17], and the majority (5 of 6 studies, or 83%) demonstrated some increases in various serum lipids after anthelmintic therapy [13–17]. Lower LDL was the most frequently reported lipid measurement associated with helminth infections among these studies at baseline, with higher HDL, lower triglycerides, and lower total cholesterol reported less frequently. It should also be noted that HDL was consistently reported to increase after infected individuals were treated [14–16], which in practice could translate to a clinical benefit given that cardiovascular risk is known to increase sharply as HDL levels fall below 40 mg/dL [18] and that the risk of CAD increases by 13% for every 10% reduction in HDL [19]. This suggests that helminth infections and anthelmintic treatment may preferentially affect certain types of lipids through different mechanisms that warrant further investigation. Interestingly, these effects were observed predominantly in helminths that affect the liver, suggesting intra-hepatic processing of cholesterol may be altered by these liver flukes. No significant trends were noted when these studies with pre-post anthelmintic treatment data were stratified by age or sex.
Cross-sectional associations of helminth infections with serum lipids
Of the 45 studies cross-sectionally comparing serum lipids in human and animal studies, 36 reported lower lipids in association with helminth infection, 23 demonstrated no relationship, and 16 showed that helminth infection was associated with higher lipids. Given heterogeneity in lipid trends within many of the studies, each lipid measurement will be discussed separately with comparisons between human versus animal studies.
Forty-three of these studies reported on total cholesterol [6–8,13–17,20–55]. Of these, 28 reported on participants infected with Schistosoma species or with mixed helminths that included Schistosoma species [6,7,13,15,25–28,30,31,35,37,39–44,46,48–55]. These 28 studies mostly reported that infected individuals or those challenged with helminth products had lower total cholesterol than uninfected participants. Including all helminths in other studies, 96% (24 of 25 total studies, which consisted of 11 human and 13 animal studies with 1 mixed study) that reported a relationship between helminth infection and lower total cholesterol found this inverse association to be significant [13,17,24–31,33,35,38–41,44,46–51,54,55]. In contrast, 6 studies (14%, all with different helminths with 4 human and 2 animal studies) reported associations with increased total cholesterol [6,20,21,33,34,36], and 13 (30%, 10 human and 3 animal studies, of which 6 examined schistosome infections) demonstrated no effect of infection on total cholesterol [7,8,14–16,22,23,32,36,37,42,43,53]. Notably, some studies reported differences in total cholesterol depending on factors such as duration of infection, co-morbidities, type of helminth infection, route of exposure to infection, geographic locations (e.g., urban vs rural or endemic vs. non-endemic), and BMI. For example, rabbits infected with C. sinensis developed higher total cholesterol during the first week of infection which then decreased below baseline levels during weeks 2–8 of infection [33]. In contrast, S. mansoni-infected mice had significantly lower total cholesterol than uninfected mice after exposure to schistosome eggs or egg antigens, but not to cercariae [44]. In another study, S. haematobium infection was associated with lower total cholesterol and other lipids only in overweight and obese infected people [52]. Although such heterogeneity of potential confounders makes comparisons challenging, the majority of these studies (24 of 43, or 56%) found that helminth infections, mostly with schistosomes but including other helminths as well, were significantly associated with lower total cholesterol. These 24 studies included robust human (n = 10 with 1 mixed study) and animal (n = 13) studies with large sample sizes and diverse study designs and participants, suggesting that beneficial effects of helminth infections on total cholesterol may be generalizable.
Twenty-nine studies reported on LDL [6–8,13–17,22,25,27–30,34–36,39,42,43,45–48,50–54], and the majority of these [19] focused on those infected with Schistosoma species. Eighteen (10 human, 8 animal) of the 29 studies (62%) found infected participants to have lower LDL than uninfected participants [7,13,16,17,25,27–30,34,35,39,45–48,50,51,53], of which 11 were in those with schistosome infections. By comparison, 3 studies (10%; 2 human, 1 animal) reported higher LDL in those with different helminth infections [6,34,36], and 10 (34%; 8 human, 2 animal), including 6 on schistosomes, showed no effect [7,8,14,15,22,36,42,43,52,54]. Similar to studies of total cholesterol, differences in LDL also depended on additional factors in some studies. For instance, S. stercoralis was associated with lower LDL in people with alcoholism, but with higher LDL in people who were not alcoholics [34]. Similarly, O. viverrini-infected hamsters had higher LDL than uninfected hamsters during acute infection, but there were no differences in LDL between the two groups as the infected hamsters progressed to chronic infection [36]. In total, almost 2/3 of the studies that reported on LDL demonstrated lower LDL in infected versus uninfected participants. Similar to the observation with total cholesterol, there were strong human and animal studies representing a breadth of helminth infections and study designs that supported this trend.
More heterogeneity was observed for associations between helminth infection and HDL or triglycerides. Of the 31 studies investigating HDL [6–8,13–17,22,25,27–30,32,34–37,39,42,43,46–48,50–54,56], 13 (42%; 7 human, 6 animal) found lower HDL [6,17,27,29,36,37,39,46,48,50,52,54,56], 9 (29%; 7 human, 2 animal) reported higher HDL [14,25,28,30,34,42,43,51,53], and 9 (29%; 6 human, 3 animal) saw no association between helminth infections and HDL levels [7,8,13,15,16,22,32,35,47]. Notably, fewer than 50% of these studies showed lower HDL levels associated with infection, in contrast to high frequencies of studies that identified such inverse relationships between helminths and total cholesterol or LDL. Given the known association between lower HDL levels and increased CAD, it should be noted that this inverse relationship suggests that helminth infections may translate clinically to lower cardioprotection with respect to HDL [18,19]. In fact, only 29% of the studies showed a potentially protective effect with higher HDL levels in those with helminth infections. As with the other lipid measurements, the majority of the studies reporting either lower or higher HDL levels focused on schistosome infections, while those showing no effect had an even split between mixed helminth and schistosome infections.
Lastly, 35 studies reported on triglyceride levels with 20 showing lower triglycerides (57%; 12 human, 7 animal, 1 mixed study) [13,17,25,26,28,30,34,37,39,41–43,46,48,50–54,56], 3 (9%; 2 human, 1 animal) reporting higher triglycerides [29,32,36], and 15 (43%; 8 human, 7 animal) demonstrating no association with helminth infections [6–8,14–16,22,27,34–36,40,47–49]. The majority of these studies focused on schistosome infections. None of the 3 studies showing higher triglyceride levels investigated schistosome infection. Some of these studies reported varying trends of triglycerides in their same cohort of participants, similar to that observed in the total cholesterol and LDL studies. For example, one study documented significantly lower triglycerides in S. mansoni-infected mice that were fed normal diet, though not in those fed a high-fat diet (HFD), when compared to uninfected controls [37]. In a human study of S. mansoni infection in two regions of different schistosome endemicity in Ethiopia, no differences in triglyceride levels were seen between infected and uninfected individuals within the same region, but infected individuals in the highly endemic region had lower triglycerides than uninfected individuals in the S. mansoni-nonendemic region [48], possibly due to undiagnosed infections in the highly endemic region. The majority of these studies (57%) found lower triglycerides in infected versus uninfected individuals.
Summary: Overall, 45 studies reported on serum lipids with a median sample size of 167.5 study participants. Most (36 of 45 studies) demonstrated that helminth infections were associated with lower serum lipid levels cross-sectionally. Of the 6 that reported on the effects of anthelmintic treatment, 5 (2 human and 3 animal studies) showed that post-treatment serum lipid levels increased.
Of note, 12 human studies [7,8,13,21,26,32,34,39,45,47,48,52] focused on individuals with a median age of less than 50 years (38.5 [IQR 31.2–44.1]) and a median of 50% [46.5–59.1%] women. Among these, 6/11 reported lower total cholesterol, 6/8 reported lower LDL, and 5/9 reported lower triglycerides in those with helminth infections. Only 1/9 studies observed increased HDL associated with infection. Together, these studies suggest that the beneficial impact of helminth infections on unhealthy lipid levels may be highest in adults less than 50 years of age. In contrast, among the 8 human studies [6,22,25,28,42,43,53,56] with median participant ages ≥ 50 years (65.4 [54.2–69.5]) and fewer females (median 26% [16.2–40.8%]), only 2/7 studies observed lower total cholesterol and 3/7 observed lower LDL with helminth infections. However, helminth infections were associated with higher HDL in 5/8 studies and lower triglycerides in 6/8. Conclusions in older adults are more limited due to fewer studies, and are particularly limited for older women, who were underrepresented in these data. These data suggest that older men may derive more cardioprotection from helminth infections than older women, and that the beneficial lipid effects may be derived from different mechanisms in younger versus older adults with helminth infections. More rigorous studies, including those that control for infection intensity when examining effects of age and sex and those that have older female participants, are needed.
Helminths and metabolic syndrome
Thirty-eight studies reported on the associations of helminths with metabolic syndrome and related measures, such as BMI, WC, WHR, glucose intolerance, insulin level, and/or homeostatic model assessment for insulin resistance (HOMA-IR) (S3 Table). These studies comprised 24 human and 13 animal studies, and 1 mixed study.
Studies examining metabolic syndrome before and after anthelmintic treatment
Ten of the 38 studies investigated effects of helminth infections on metabolic syndrome measures before and after anthelmintic treatment [8,13–17,57–60]. Seven (4 animal, 3 human) of these reported an increase in metabolic syndrome and related measures and 3 (all human) demonstrated no effect on these factors after anthelmintic treatment.
Human studies examining metabolic syndrome before and after anthelmintic treatment
In humans, two studies documented lower insulin levels and but no difference in random blood glucose levels in S. stercoralis-infected individuals when compared to uninfected people at baseline in two different cohorts: infected diabetic vs. uninfected diabetic individuals in one study [58], and infected, non-diabetic obese vs. uninfected, non-diabetic obese individuals in another study [59]. In individuals who received treatment with single-dose albendazole and ivermectin, both insulin and random blood glucose levels increased at 6 months of follow-up compared to pretreatment levels in those with known diabetes, and only insulin levels increased in those receiving the same anthelmintic regimen and duration of follow-up but who were obese and non-diabetic.
In a double-blind, household-cluster-randomized, placebo-controlled clinical trial of people with and without mixed helminth infections, no differences in levels of insulin or glucose or HOMA-IR were observed at baseline, but those with helminth infections who were randomized to receive albendazole treatment experienced a significant increase in insulin resistance (HOMA-IR) at 52 weeks compared to those randomized to placebo treatment (estimated treatment effect, 0.031 [95% CI, 0.004–0.059]; P = 0.04) [8]. Three other human studies showed no effect of helminth infection or anthelmintic treatment on measures of metabolic syndrome [13,14,57]
In summary, 50% (3 of 6) of human studies demonstrated increases in measures of metabolic syndrome after treatment of helminth infection.
Animal studies examining metabolic syndrome before and after anthelmintic treatment
Mouse models consistently showed negative associations of metabolic syndrome parameters with helminth infections. S. japonicum-infected male mice had lower body weight and less insulin resistance than uninfected mice at baseline. Nine weeks following treatment with praziquantel, body weight and HOMA-IR of previously-infected mice increased compared to chronically-infected, untreated mice [15]. In a second mouse model, S. mansoni-infected mice had significantly lower blood glucose than uninfected mice at baseline, which had increased 7 and 14 days after infected mice received praziquantel [60]. Two other animal studies, using sheep and investigating the effects of Fasciola infection, reported similar trends in blood glucose before and after anthelmintic treatment with triclabendazole and levamisole [16,17], as seen in the mouse studies.
In summary, all 4 animal studies showed inverse assocations (lower measures of metabolic syndrome) with helminth infection and a subsequent increase in these measures after infection was treated.
Summary of studies examining metabolic syndrome before and after anthelmintic treatment
Taken together, the majority of studies (7 of 10 (70%), with 4 animal and 3 human studies) reported lower body weight, blood glucose, insulin level, and insulin resistance in association with helminth infections [8,15,17,58–60]. Subsequently, these parameters seemed consistently to increase after treatment of infected study participants. The 3 studies demonstrating no effect of anthelmintic therapy on parameters of metabolic syndrome were all human studies and notably also did not show any baseline differences in metabolic syndrome between helminth-infected and uninfected people [13,14,57]. Of note, the human studies included in this section had median participant ages of < 50 years (39.3 [34–44.3]), with approximately equal distributions of men and women. Although few in number, these human studies mostly suggest that anthelmintic treatment may paradoxically predispose both men and women younger than 50 to an increased risk for metabolic syndrome.
Cross-sectional associations of helminth infections with metabolic syndrome
Thirty-eight studies examined the baseline associations between helminth infections on metabolic syndrome and related measures, of which 22 (58%; 12 animal, 9 human, 1 mixed human/animal) demonstrated lower metabolic syndrome and related measures [15–17,25,28,30,37,42,43,47,48,51,56,58–66], 14 (37%; 13 human, 1 animal) showed no relationship [7,8,13,14,20,21,26,32,45,52,53,57,67,68], and 3 (8%; 2 human, 1 animal) reported an increase or variable changes in metabolic syndrome and related measures in association with helminth infections [6,66,69]. A large proportion of these studies (21/38) reported on blood levels of glucose or insulin; some also measured glucose intolerance or insulin resistance. Some examined anthropometric measurements, such as BMI, WC, and WHR, as well as prevalence of metabolic syndrome.
Two studies in China focused on people with history of prior schistosome infection (PSI). The first showed a lower prevalence of obesity and abdominal obesity among 465 men with PSI (8.4% and 24.3%, respectively) when compared to a control group of 1132 never-infected men (16.4% and 41.8%, respectively) [43]. Women were also included in this study, but there were no differences in obesity or abdominal obesity when the smaller numbers of previously infected (n = 61) and uninfected (n = 284) women were compared to each other [43]. BMI was lower in both men and women, and fasting blood glucose was also lower in women with previous infection compared to their uninfected counterparts. In the second study of 1,597 men, the prevalence of metabolic syndrome and its components, including central obesity, hypertriglyceridemia, hypertension, and hyperglycemia, was lower in the group with PSI versus those never infected [42]. Although both studies included large sample sizes, women were underrepresented in the first study (17.8%) and not included at all in the second; both also included older individuals with an average age of ~65 years. Additionally, PSI was diagnosed as ultrasonographic liver abnormalities plus participants’ recall of past exposure to contaminated water and anthelmintic treatment, but other liver diseases were not reported as being excluded.
Other animal studies and human studies from Brazil, China, Egypt, Ethiopia, the Netherlands, and the United States reported similar inverse relationships between active schistosome infection and measures of metabolic syndrome [15,25,28,30,37,48,51,56,60–62,70]. Of note, 7 other studies did not demonstrate these associations, with 4 (3 human, 1 animal) showing no association [26,52,53,67], 2 (1 human, 1 animal) reporting increased insulin resistance, glucose intolerance, or insulinemia [6,66], and 1 (human) showing variable relationships between measures of metabolic syndrome and schistosome infection [69]. The latter, for instance, showed lower HOMA-IR and fasting insulin only in HIV-schistosome co-infected people not on ART, and not in those with HIV on ART or HIV-uninfected individuals with schistosome infection, when compared to normal controls [69]. This study also reported an increase in pancreatic beta cell function in those with schistosome infection who were HIV-uninfected.
Overall, studies investigating metabolic syndrome with non-schistosome helminth infections also reported similarly lower measures of metabolic syndrome-related parameters among infected individuals (n = 8) [16,17,47,58,59,63,65,69]. In contrast to the 22 total studies showing inverse associations between helminth infections and metabolic syndrome or parameters, 14 other studies showed no association [7,8,13,14,20,21,26,32,45,52,53,57,67,68]. These 14 studies included mostly human studies and investigated 4 Schistosoma, 4 mixed helminth, 3 Strongyloides, 1 Opisthorchis, 1 Fasciola, and 1 Ascaris infections.
Summary: In total, 38 studies reported on metabolic syndrome and related measures with a median sample size of 213.5 human and animal participants. Most (22 of 38, or 58%) demonstrated that helminth infections were associated with a lower frequency of metabolic syndrome, with most data coming from studies of Schistosoma infections. Of the 10 that reported on the effects of anthelmintic treatment, 7 showed that metabolic syndrome parameters increased after treatment of helminth infection.
When stratifying the human studies by age and sex, we conclude that in both men and women younger than 50 years, there was mostly no relationship (n = 9/15) versus lower measures of metabolic syndrome (n = 6/15) in association with helminth infections [7,8,13,21,26,32,45,47,48,52,58,59,65,68,69]. On the other hand, in 5 of the 7 human studies [6,25,28,42,43,53,56] with an average age of 50 or above, helminth infections were associated with lower prevalence of metabolic syndrome, suggesting that helminths may offer protection against metabolic syndrome in older individuals, particularly in men who were over-represented in these studies.
Helminths and diabetes
Thirty studies investigated helminths and diabetes or related measures, such as hemoglobin A1c or pancreatic inflammation by histopathological analysis (S4 Table).
Studies examining diabetes before and after anthelmintic treatment in humans
Five of these 30 investigated diabetes and related measures before and after anthelmintic treatment, all in humans [14,57–59,71]. The first of these followed up on a previous study [32] in which individuals with positive S. stercoralis serology had a significantly lower odds of prevalent type 2 diabetes (T2DM) [57]. Three years after testing and treatment for S. stercoralis infection, follow-up was successful in 80% of the original cohort participants (n = 207). Those who had been treated with ivermectin for Strongyloides infection had an unadjusted 7.7 times increased relative risk of being diagnosed with T2DM than the uninfected, untreated group [57]. After adjustment for age, sex, change in BMI and initial hemoglobin A1c, the relative risk for diabetes was lower but still trended towards significance (RR 5.85, 95% CI 0.75–39.5, p = 0.093).
In support of these findings, two prospective cohort studies also demonstrated worsened glycemic control after anthelmintic treatment. In O. viverrini-infected Thai individuals, who had a lower mean hemoglobin A1c (5.5%) than uninfected individuals (6.0%) at baseline, praziquantel treatment led to a significant increase in hemoglobin A1c (5.5%—>6.0%) over 6 months [14]. In a second study, individuals with T2DM and Strongyloides infection had similar hemoglobin A1c and random blood glucose levels, but lower insulin and glucagon levels, compared to uninfected individuals with T2DM at baseline [58]. Six months after albendazole and ivermectin treatment with confirmatory repeat parasitological examinations, previously infected individuals experienced increases in hemoglobin A1c by 25%, random blood glucose by 18%, and insulin level by 13% when compared to their pretreatment levels.
In contrast, another study led by the same first author found no effects of Strongyloides infection or anthelmintic treatment on hemoglobin A1c in non-diabetic, obese individuals 6 months after receiving albendazole and ivermectin [59]. Given a similar study design used by the same authors in these two studies [58,59], the different conclusions may reveal a preferential glycemic benefit of Strongyloides infection for people with known diabetes, and not for people without. Additionally, another study of children aged 9–14 years with mixed helminth infections in South Africa documented no differences in hemoglobin A1c at baseline or 6 months after treatment with albendazole [71]. However, potential selection bias and metabolic differences between children and adults may limit this study’s conclusions; it was also not reported whether the children were re-tested for infection or how many cleared their infection at follow-up.
No animal studies reported on diabetes and related measures before and after treatment of helminth infection.
In summary, 3 of 5 studies (60%; all human studies) that investigated markers of diabetes in people after anthelminthic treatment reported paradoxical worsening of diabetes and related measures after treatment [14,57,58]. Additional prospective data are warranted, particularly focusing on other helminth infections, clarifying post-treatment findings in children, and assessing whether age and sex affect the association between infection and diabetes.
Cross-sectional associations of helminth infections with diabetes, glucose, or pancreatic inflammation
In total, 29 studies compared baseline measures of diabetes or pancreatic inflammation in those with and without helminth infection. Seventeen studies (59%; 11 animal, 6 human) reported lower measures of diabetes or pancreatic inflammation [14,25,32,68,72–84], 6 (21%; all human) demonstrated higher measures of these factors [6,85–89], and 5 (17%; all human) showed no association with respect to helminth infections [53,58,59,71,90]. In the final study there was no difference in hemoglobin A1c or fasting glucose regardless of helminth infection or antiretroviral status among HIV-infected individuals, while among HIV-uninfected individuals, soil-transmitted helminth (STH) infection was inversely associated with hemoglobin A1c (5.2% vs. 5.5% in STH-uninfected controls) after adjustment for age and sex [69].
The 6 studies reporting higher measures of diabetes with helminth infections were all human studies with mixed helminths (2), Schistosoma species (2), and Strongyloides (2) represented. Among the 2 studies with mixed helminths, an increased odds of diabetes was reported for those with Taenia and Ascaris infections [86,87]. One case-control study among 300 people in Sudan found an increased odds of prevalent urogenital schistosome (aOR: 2.5, 95% CI: 0.8–7.8; p = 0.10) or intestinal parasite infection (aOR: 2.10, 95% CI: 0.97–4.5, p = 0.059) among diabetic participants, and the intensity of S. haematobium infection correlated with duration of T2DM (R = 0.666, p = 0.009) [85]. Similarly, the 5 studies showing no association were also all human studies, with 3 focused on Strongyloides infection. One study of 2867 Chinese participants with and without prior schistosome infection notably reported no difference in diabetes (19.2% vs. 22.4%, respectively; p = 0.063), although those with PSI had significantly lower lipids and CAD prevalence [53].
Of the 17 studies reporting lower measures of diabetes or pancreatic inflammation among helminth-infected participants, 6 involved humans [14,25,32,68,73,74]. In one study of 762 people, 2.6% of those with normal glucose tolerance, versus none of those with Type 1 diabetes, had positive antigen and antibody filarial tests for W. bancrofti and B. malayi [74]. A second study of 1416 participants demonstrated a dose-dependent inverse relationship between these filarial tests and T2DM, showing a lower prevalence of lymphatic filariasis among diabetic participants (both newly diagnosed [5.7%] and those under treatment [4.3%]) compared to pre-diabetic [9.1%, p = 0.0095) and non-diabetic participants [10.4%, p = 0.0463) [73]. Similar inverse relationships have also been described between those with PSI and diabetes in China [25], those with O. viverrini and hemoglobin A1c levels in Thailand [14], and those with prior S. stercoralis infection and diabetes among Aboriginal Australians [32].
In comparison to the 6 human studies, 11 animal studies with mouse models using Schistosoma species (n = 7), Fasciola hepatica (n = 2), and filarial species (n = 2) also documented lower measures of diabetes or pancreatic inflammation among helminth-infected animals [72,75–84]. Seven of 11 documented histopathological changes of the pancreas in mice and found that helminth infection was associated with less pancreatic inflammation, degradation, and other architectural changes in mice who were infected or exposed to helminth antigens as compared to uninfected mice [72,76–81]. These studies also documented a lower incidence of diabetes between infected and uninfected mice, and via correlations with pancreatic histopathological changes suggested helminths may possibly protect against autoimmune diabetes. This potential insight into mechanistic causes of these inverse relationships is valuable given that human studies have been unable to examine for diabetes-related pancreatic changes.
Summary: In total, 30 studies reported on diabetes and related measures with a median sample size of 279.5 participants. Most (17 of 29, or 59%) demonstrated cross-sectional associations between helminth infections and lower frequency of diabetes or diabetes-related parameters. Infection with Schistosoma species were most represented in these studies. Of the 5 that reported on the effects of anthelmintic treatment, 3 (60%) showed that blood glucose increased after treatment of helminth infection. Among human studies that reported median age and sex distribution, 2 out of 5 [6,25,53,89,90] with median ages over 50 years observed a different cross-sectional trend and suggested that helminth infection may possibly increase diabetes risk in older women, although the sample size of studies is admittedly limited and women were over-represented in those 2 studies, which both focused on Strongyloides [89,90].
Helminths and atherosclerotic cardiovascular disease
Eleven studies investigated the associations of helminths on CAD, MI, and/or large-vessel atherosclerosis. None investigated the subsequent effect of anthelmintic treatment on these outcomes (S5 Table).
Cross-sectional associations between helminth infections and atherosclerotic cardiovascular disease in animals
Of the 6 mouse studies investigating effects of helminths on atherosclerosis [27,35,46,49,51,61], 5 showed fewer atherosclerotic plaques along the aorta and other arteries in schistosome-infected versus uninfected mice. One of these showed that S. mansoni-infected, ApoE-deficient mice had 50% less atherosclerosis in the aortic arch and brachiocephalic artery than uninfected mice [27]. Another reported similar findings, demonstrating that mice on HFD exposed to S. mansoni SEA had smaller aortic plaque size and 44% less progression of aortic root atherosclerosis versus mice on HFD exposed to phosphate buffered saline [49]. Additionally, a study investigating the effects of recombinant S. japonicum protein (rSj-Cys) showed that treatment with the protein significantly decreased atherosclerotic plaque along the entire aorta and aortic sinus, decreased fat deposition in the kidneys and glomerular damage, and improved blood flow to the heart in mice that were fed a HFD [51]. Two other studies [46,61] also found decreased aortic atherosclerosis in S. mansoni-infected mice, although the statistical significance was not clear in one of them. In contrast, a study in which mice received weekly S. mansoni egg exposure found that egg-exposed mice were not protected against the development or progression of atherosclerosis when fed a HFD, despite having lower total cholesterol and LDL, compared to unexposed mice on the same diet [35]. It should be noted that sex was not clearly described in the majority of these animal studies, that every animal study investigated the effects of schistosome infections, and that these studies examined only large-vessel atherosclerosis, not CAD or MI. Additionally, it should be noted that mouse studies are conducted in models with similar but altered physiology and under extreme conditions (e.g., genetically altered or fed extremely HFD) as compared to human studies.
Cross-sectional associations between helminth infections and atherosclerotic cardiovascular disease in humans
Similar to the mouse studies, 1 human autopsy study also found that Opisthorchis-infected cadavers had significantly less aortic atherosclerosis than the autopsy cases without infection, and this was magnified with increasing infection burden across all age ranges [38]. Only 12.2% of the cadavers were female. In contrast, two cross-sectional studies investigating the effects of mixed STH or filarial infections on carotid intimal thickness, a measure of carotid atherosclerotic vascular disease, found no association between infection and atherosclerotic plaque [22,47].
Only 3 studies reported on CAD or MI [22,53,91]. A cross-sectional study of 453 adults living in India showed no association between lymphatic filariasis and CAD [22]. Further, among those with CAD, there were no associations of lymphatic filariasis with ultrasound measurements of carotid intimal thickness, aligning with the mouse study mentioned above. In contrast, a second autopsy study also found less MI and atherosclerosis in autopsies with bilharzial cirrhosis compared to all other autopsies, but important possible confounders including age and sex of cadavers, and other types of cirrhosis, were not clearly described [91]. A third cross-sectional study of 2867 Chinese adults showed that prior schistosome infection was significantly associated with a lower prevalence of CAD, which remained significant even after adjusting for laboratory measures including serum lipids and hepatic dysfunction [53].
Summary: In total, 11 studies (6 animal, 5 human) reported on atherosclerotic cardiovascular disease with a median sample size of 319 study participants. None of these studies investigated the effects of anthelmintic treatment on these outcomes. Specifically, only 3 studies (all human) reported on CAD or MI [22,53,91], of which 2 (67%) found less CAD among those with schistosome infection. Of note, 7 of 10 studies (70%; 6 animal, 4 human) of large vessel atherosclerosis concluded that helminth infections were generally associated with less atherosclerosis, particularly in the aorta and carotid arteries [27,35,38,46,49,51,61]. Most demonstrating this inverse relationship were animal studies that investigated Schistosoma infections. When the human studies were stratified by age and sex, no notable trends were observed, though only a small number had clear reports of average age and proportion of women in their studies. Future studies should rigorously control for potential confounders, such as age, sex, physical activity, and other sociodemographic factors, that may be associated with both helminth infections and atherosclerotic cardiovascular disease.
Helminths, blood pressure, and cardiovascular hemodynamics
Eighteen studies investigated relationships between helminth infection, blood pressure, and cardiovascular hemodynamics, such as peripheral vascular resistance and mean arterial pressure (S6 Table).
Studies examining blood pressure and cardiovascular hemodynamics before and after anthelmintic treatment in humans
Three of the 18 studies investigated the effects of helminth infections on blood pressure before and after anthelmintic treatment, all in humans. One of these, a large prospective cohort study, found no differences in blood pressure before and 6 months after treatment of O. viverrini with praziquantel [14]. A second study was a cluster-randomized trial that demonstrated no differences in blood pressure before and after treatment of mixed helminth infections with albendazole at 52 weeks of follow-up [8]. The third, also a cluster-randomized trial, reported lower diastolic blood pressure in individuals with heavy S. mansoni infections compared to uninfected individuals at baseline [13]. However, follow-up blood pressures at 4 years were not affected by either quarterly or annual anthelmintic treatment with albendazole and praziquantel, although it should be noted that there were persistently high rates of infection in both treatment arms at follow-up. These studies mostly enrolled people younger than 50 years, limiting conclusions about older persons.
Cross-sectional associations of helminth infections with blood pressure or cardiovascular hemodynamics
Together with the above 3 studies, 14 other human studies also compared baseline measures of blood pressure and cardiovascular hemodynamics in those with and without helminths [7,23–25,32,42,43,47,48,53,56,68,91–92]. Of the studies investigating the associations of helminths with systolic blood pressure or hypertension, 13 human studies in a total of 18,807 people demonstrated no associations [7,8,13,14,24,25,32,42,43,47,48,53,68], 3 studies in a total of 781 people showed lower systolic blood pressure [23,56,91], and 1 reported higher systolic blood pressure in 213 pregnant women [92]. The three studies reporting inverse associations examined different helminth infections: O. volvulus (mean systolic blood pressure 105 mmHg vs. 113 mmHg in uninfected participants) [23], previous schistosome infection (mean systolic blood pressure 110 mmHg vs. 127 mmHg in those never infected) [56]; and autopsy cases with bilharzial cirrhosis (6.4% vs. 12.9% frequency of hypertension in all autopsy cases) [91]. In contrast, the single study with positive associations reported elevated systolic, diastolic, and mean arterial blood pressures in pregnant women with hookworm infection, and a 6-fold increased odds of elevated mean arterial pressure in those with Trichuris, of borderline significance [92]. However, the large majority of the studies, which included 95% of the human participants, indicated no associations of helminth infections with systolic blood pressure.
The same 17 human studies also investigated diastolic blood pressure with 11 showing no associations [7,8,14,23–25,32,47,48,53,68], 5 demonstrating lower diastolic blood pressure [13,42,43,56,91], and the same study of pregnant women showing higher diastolic blood pressure among infected participants [92]. Two of these studies, discussed in the prior paragraph, showed inverse associations between helminth infections and both systolic and diastolic blood pressure [56,91]. While helminth infection was not associated with systolic blood pressure, higher intensity of S. mansoni infection in a study of 1898 individuals from Uganda was associated with lower diastolic blood pressure (72.8 vs. 76.7 mmHg (heavy vs. light or moderate infection intensity, p = 0.01)) [13]. In further support of differential effects on diastolic versus systolic blood pressure, two cross-sectional studies of people with prior schistosome infection from China found lower diastolic pressure and less overall hypertension in men, but not women, and no differences in systolic blood pressure [42,43]. Notably, women were under-represented in both of these studies. Among 11 studies showing no association between helminth infection and diastolic blood pressure, helminths represented included mixed species (3), Schistosoma species (3), Strongyloides (2), Opisthorchis species (2), and O. volvulus (1). Countries where these studies were conducted were also diverse and included Australia, China, Indonesia, Thailand, Ethiopia, Republic of Chad, and Uganda. Similar to the trend seen with systolic blood pressure, however, diastolic blood pressure seemed mostly to be unaffected by helminth infections with 11 of 17 studies showing no association between helminth infection and diastolic blood pressure. Interestingly, in the 4 studies with discordant systolic and diastolic blood pressure outcomes [13,23,42,43], 3 found that active or previous schistosome infection was associated with lower diastolic blood pressures and no impact in systolic blood pressures—perhaps suggesting differential effects on diastolic versus systolic blood pressures could be limited to schistosome infection.
Other measures of cardiovascular hemodynamics were reported in the single mouse study, which showed that mice infected with S. mansoni had lower peripheral vascular resistance and mean arterial pressure than uninfected mice [93].
Summary: In total, 18 studies (17 human, 1 animal) reported on blood pressure and cardiovascular hemodynamics with a median sample size of 555 study participants. The effects of helminths on blood pressure and peripheral vascular resistance were mixed, with no effect reported cross-sectionally in 10 (56%) of those studies. Additionally, of the 3 studies that reported on the effects of anthelmintic treatment, none showed that treatment of helminth infection had effects on follow-up blood pressure. When the human studies were stratified by age and sex, helminth infections were not associated with differences in blood pressure in either men or women under the age of 50. In contrast, among the 5 studies [25,42,43,53,56] with older participants (median age 65.7 years [IQR 65.1–68.5] and 20.7% women [IQR 11.6%-27.7%]), helminth infection was consistently associated with lower diastolic blood pressure measurements. These data suggest that a possible beneficial effect of infection on diastolic blood pressure may occur more frequently in men over age 50 as compared to in women of the same age group.
Helminths and hsCRP
Five studies examined helminth infections and hsCRP, an inflammatory marker that is used clinically to evaluate cardiac risk (S7 Table).
Study examining hsCRP Before and after anthelmintic treatment in humans
Only 1 of the 5 studies, all in humans, reported on the subsequent effects of anthelmintic treatment on hsCRP [8]. This double-blind, cluster-randomized, placebo-controlled trial reported hsCRP measurements at baseline and post-treatment among participants who received 4 rounds of albendazole or matching placebo every 3 months for 3 consecutive days. Infected individuals had one or more infections with A. lumbricoides, T. trichiura, A. duodenale, and N. americanus. The trial reported no difference in hsCRP between treatment groups at baseline or after 52 weeks of follow-up.
Cross-sectional associations of helminth infections with hsCRP in humans
Among the 5 studies of helminths and hsCRP, 2 in Indonesia reported no differences in hsCRP between those with mixed STH infections and those without [47,65]. In both studies, the geometric mean hsCRP was 0.5 mg/L or below in all groups, well below the hsCRP threshold of 2 or higher typically recognized to be associated with an increased risk for cardiovascular events [94,95].
In another cross-sectional study looking at CAD-positive vs. CAD-negative individuals living in India with positive versus negative filarial (W. bancrofti and B. malayi) antigen tests, the geometric mean hsCRP in the CAD-positive group was not different [22]. A fourth study in S. haematobium-infected vs. uninfected individuals in Gabon also found no difference in median hsCRP measurements [52].
Summary: In total, 5 studies reported on hsCRP with a median sample size of 646 participants, all in humans. None of the 5 studies showed any cross-sectional association between helminth infections and hsCRP, nor were any trends observed when the studies were examined by age and sex. The single study that reported the effects of anthelmintic treatment failed to demonstrate any effect of treatment of helminth infection on hsCRP.
Helminths and non-atherosclerotic cardiovascular disease
Four studies examined the associations of helminths with non-atherosclerotic cardiovascular disease, defined in these studies as myocardial injury, myocardium lipid deposits, cardiac hypertrophy, eosinophilic myocarditis, or other endomyocardial manifestations of eosinophilia that may be related to helminth infections [46,96–98]. None of these studies investigated the subsequent effects of anthelmintic treatment on outcomes of non-atherosclerotic cardiovascular disease (S8 Table).
Cross-sectional associations between helminth infections and non-atherosclerotic cardiovascular disease
Of these 4 studies, 2 showed some increase in non-atherosclerotic cardiovascular disease [96,98], 1 reported less non-atherosclerotic cardiovascular disease [46], and 1 found no relationship between non-atherosclerotic cardiovascular disease [97] and helminth infections.
In a mouse model, acute S. mansoni infection was associated with abnormally lower density of cardiomyocytes, increased area of injury indicative of more myocarditis, and increased collagen deposition on histopathological examination when compared to uninfected mice [98]. Further, as infection became more chronic, mice developed progressively worsening myocardial disease that was characterized by a further decrease in total cardiomyocytes. Notably, this study included only 20 mice, all of which were females. Another animal study reported an inverse relationship between S. mansoni infection and myocardium lipid deposits and cardiac hypertrophy in mice fed HFD or standard diet (SD) [46]. Investigators first showed that HFD versus SD led to abnormal myocardial deposits and cardiac hypertrophy on histopathology, then found that mice that were fed HFD and exposed to S. mansoni cercariae or soluble egg antigen developed fewer myocardial lipid deposits and cardiac hypertrophic changes than unexposed mice fed a HFD. Only male mice were used in this study.
In a third study, 50 young adult immigrants who had come from sub-Saharan Africa were stratified into those with mixed helminth infection and/or eosinophilia (study group) versus those without (control group) to evaluate for the presence of endomyocardial lesions [97]. The study group had thickened posterior mitral valve leaflets on both qualitative and quantitative echocardiography. No associations were observed between the type of helminth infection and valvular involvement or with degree of eosinophilia. Additionally, one other human study showed that Opisthorchis infection was associated with eosinophilic myocarditis in cadavers, but there were several limitations, including that it was not clear how infection was determined, whether a control group was used, or whether the reported outcomes reached statistical significance [96].
Summary: In total, 4 studies (2 animal, 2 human) reported on non-atherosclerotic cardiovascular disease with a median sample size of 45 study participants. The effects of helminths on non-atherosclerotic cardiovascular disease were mixed, with 2 studies showing more endomyocardial pathology, 1 demonstrating less, and 1 reporting no association between non-atherosclerotic cardiovascular disease and helminth infection. No studies investigated the effects of helminth eradication on non-atherosclerotic cardiovascular disease, which could provide helpful data to guide understanding of this area. Interestingly, the 2 mouse studies—both studying S. mansoni—had either all female or all male mice and came to different conclusions concerning the association between infection and cardiac changes. Further studies in this area are needed and should investigate whether sex and age may play a role in the relationship between helminth infections and non-atherosclerotic cardiovascular disease.
S9 Table summarizes the major findings for each category of cardiometabolic diseases and risk factors.
Discussion
Our robust synthesis of 84 human and animal studies consistently demonstrates that helminth infections may protect against dyslipidemia, metabolic syndrome, diabetes, and atherosclerotic cardiovascular disease. This is particularly strengthened by the existence of longitudinal studies in which these parameters paradoxically increased after elimination of helminth infections. We posit that the ability of helminth infections to lower atherosclerotic cardiovascular disease risk seems to be mostly explained by a reduction in metabolic risk factors, such as dyslipidemia and diabetes, and may also be partly explained by the type of helminth infection. Our review confirms the findings of prior systematic reviews on metabolic outcomes [4,5] and extends them to examine post-treatment effects. Further, to our knowledge, this is the first systematic review to comprehensively evaluate the effects of a variety of helminth infections and anthelmintic treatments on multiple cardiometabolic diseases and risk factors. Importantly, these data show that the burden of cardiometabolic diseases and risk factors may paradoxically worsen as the World Health Organization and global community strive to eliminate human helminthiases worldwide, which would have implications for at least 24% of the world’s population [9,99].
Our data indicate that metabolic effects, rather than immune alterations, may explain the observed associations between helminth infections and lower cardiometabolic diseases. This is a notable finding given that helminth infections are well-known to induce type 2 and T regulatory immune responses while downregulating proinflammatory type 1 immune responses that are critical to the pathogenesis of some cardiometabolic diseases [99–104]. If lower cardiometabolic diseases were driven by helminth-induced immune changes, one might expect that hsCRP, which is elevated in cardiovascular disease and is used to stratify cardiac risk [94,95], would be lower in those with helminth infections [101,105,106]. Instead, we found no difference in hsCRP levels but strong, consistent differences in lipid and metabolic factors. We note that CRP is a nonspecific inflammatory marker [107] and we cannot conclude that lack of differences in CRP indicates lack of contribution of immune findings to our observations. However given the key role of the liver in lipid and glucose metabolism and the predilection of many helminths to affect this organ, we posit that altered intra-hepatic or other metabolic functioning may also contribute to the associations we have observed. One other important caveat is that we cannot exclude other immunologic mechanisms, including the liver’s role in host immune responses [108], in analyzing the etiologies that may explain the inverse associations that we have reported.
Helminth infections are known to affect several metabolic pathways that could ultimately contribute to lowering cardiometabolic disease risk. For instance, it has been postulated that helminths could decrease serum lipids by parasitizing host dietary nutrients for their own survival, by altering the gut microbiota and thereby affecting intestinal lipid metabolism, or by regulating lipid metabolism in the liver or peripheral adipose tissue [52,109]. Helminths use host lipids for their own biosynthetic purposes, such as for membrane formation during larval stages and by incorporating fatty acids into parasite eggs [110]. An alternative hypothesis is that the lower adiposity in individuals with helminth infections could explain the inverse relationships observed between helminth infections with dyslipidemia and diabetes. Either of these hypotheses could be supported by our findings of little or no association between helminth infections and hypertension or non-atherosclerotic cardiovascular disease. One possible exception could be the association of helminth infections with lower diastolic blood pressure. A potential explanation for the lower diastolic blood pressure in people living with helminth infection could be arterial stiffness. Helminth infection may reduce diastolic blood pressure through either metabolic [111] or immunomodulatory effects [112–114]. The beneficial effect of helminth infection on lower diastolic blood pressure may be particularly profound in older adults [115], as 2 of the 3 positive studies for diastolic blood pressure enrolled participants with a mean age above 65 years [42,43].
Different helminths may have distinct effects on cardiometabolic diseases, potentially through direct physiologic or local metabolic effects on the liver. In support of this, over 90% (38 of 42) of studies with Schistosoma species, blood flukes that can affect the liver and intestines, demonstrated an association between infection and lower frequencies of cardiometabolic diseases and risk factors with infected participants generally having lower serum lipids, glucose, and other metabolic parameters than uninfected participants. In contrast, only 33% (4 of 12) of the studies with mixed helminths, 67% (6 of 9) of those with Strongyloides, and 75% (15 of 20) of those with all other helminths reported some inverse relationships between helminth infection and cardiometabolic risk. Given the smaller number of studies focused on other helminths compared to those that reported on Schistosoma species, future studies investigating the relationship between helminth infections and cardiometabolic diseases may consider focusing on these other helminths.
The mechanistic pathways that connect helminth infections with cardiometabolic diseases could provide new drug targets or other strategies to manage the global burgeoning of these cardiometabolic diseases. In particular, LDL was more consistently altered than HDL in helminth-infected participants, which may be similar to trends seen with the use of statin drugs [116]. This suggests that helminths may perhaps affect a specific aspect of the common pathway of lipoproteins [117] that preferentially alters LDL levels while relatively conserving HDL levels. Given the known clinical benefit of elevated HDL in lowering cardiovascular risk [18,19] and its inclusion in commonly used calculated risk equations (ASCVD 2013 Risk Calculator, Reynolds Risk Score, and the Framingham Risk Score with Lipids), several questions remain in our comprehensive literature assessment. First, do alterations in LDL lower cardiovascular risk in helminth-infected individuals chronically if HDL levels are largely unaffected? Second, given that LDL is more frequently altered in helminth infections, should calculation of cardiac risk in helminth-endemic areas be tailored to consider LDL, instead of HDL, levels?
Mechanistic clinical trials with translational components are needed to illuminate these pathways and answer these questions. Studies in which helminth infections are treated can incorporate measures of cardiometabolic diseases, which could guide future clinical screening and management for cardiometabolic diseases as we work towards global eradication of helminths. Prospective studies in humans must also account for crucial sociodemographic and clinical confounders that may be associated with both helminth infections and cardiometabolic diseases, which dramatically affected outcomes in some studies [42,52,69], particularly when women were under-enrolled. Examining trends seen in animal versus human studies further supports the need for rigorous control of potential confounding variables. Over 85% of animal studies reported less cardiometabolic diseases or risk factors in the setting of helminth infections, as compared to only ~64% of human studies, which suggests the presence of important confounders.
Our study has limitations. First, diagnostics used in the included studies vary by sensitivity and host characteristics, and in some studies were based on clinical history and subject to recall bias. Further, other studies did not document the clearance of helminth infections after treatment. These scenarios may lead to infections being underrepresented at baseline or overrepresented at follow-up, and may have influenced reported outcomes. Second, it is possible that medications could contribute to observed post-treatment effects. Praziquantel and albendazole, the two anthelmintics used in the majority of the included studies, do not have known direct effects on host glucose or lipid metabolism. However, ivermectin has been shown to decrease serum glucose and cholesterol levels in a few experiments [118,119]. Contrary to the results of those experiments, the 3 studies in this review that used ivermectin all reported increases in diabetes and/or metabolic syndrome, though the total sample sizes were small. Third, as with any systematic review, the risk of publication bias could have led to under-reporting of studies that did not find associations between helminth infections and cardiometabolic diseases. Our systematic review was also limited to only the most prevalent human helminths, which may have excluded other important work examining the effects of non-human helminths on cardiometabolic diseases. Finally, due to the heterogeneity of the data with diverse study types, helminths, and cardiometabolic diseases and risk factors represented, a meta-analysis was not possible, which limits our ability to estimate overall effect sizes or to examine more comprehensively for the effects of confounders.
In summary, this rigorous, comprehensive systematic review demonstrates consistent interactions of helminths with dyslipidemia, diabetes, and atherosclerotic cardiovascular disease. Our data suggest that increased preventive care may be needed for individuals at moderate or high risk for cardiometabolic disease who receive mass drug administration for helminth infections. Providing these individuals with regular screening for diabetes, lipids, and atherosclerotic cardiovascular disease could mitigate possible increased cardiometabolic risk after anthelmintic treatment in highly endemic areas, particularly those in which routine preventive primary care may not be available. Our findings highlight the need for further cross-disciplinary research, which would have implications for both individual and population health and could point towards ground-breaking new strategies to address the intersection between helminthiases and non-communicable diseases globally in regions where both commonly overlap.
Supporting information
(DOCX)
Abbreviations: IQR, interquartile range; STH, soil-transmitted helminths; HDL, high-density lipoprotein; TC, total cholesterol; LDL, low-density lipoprotein; trig, triglycerides; PCR, polymerase chain reaction; RCT, randomized controlled trial; PZQ, praziquantel; SEA, soluble egg antigen; CAD, coronary artery disease; PSI, previous schistosome infection; T2DM, type 2 diabetes; HFD, high-fat diet; BMI, body mass index. #study investigated other outcome measures that will be included in other tables. *denotes statistical significance, p<0.05.
(DOCX)
Abbreviations: IQR, interquartile range; STH, soil-transmitted helminths; PCR, polymerase chain reaction; BMI, body mass index; T2DM, type 2 diabetes; WC, waist circumference; PZQ, praziquantel; IR, insulin resistance; RCT, randomized controlled trial; HOMA-IR, homeostatic model assessment for insulin resistance; SEA, soluble egg antigen; PSI, previous schistosome infection; FBG, fasting blood glucose;; ART, antiretroviral therapy; HFD, high-fat diet; WHR, waist-hip ratio. #study investigated other outcome measures that will be included in other tables. *denotes statistical significance, p<0.05.
(DOCX)
Abbreviations: IQR, interquartile range; STH, soil-transmitted helminths; PCR, polymerase chain reaction; T2DM, type 2 diabetes mellitus; HbA1c, hemoglobin A1c; PZQ, praziquantel; LF, lymphatic filariasis; T1DM, type 1 diabetes mellitus; PSI, previous schistosome infection; DM, diabetes mellitus; ART, antiretroviral therapy; STZ, streptozotocin; NOD, non-obese diabetic; SEA, soluble egg antigen; PBS, phosphate buffered saline; SWA, soluble extracts of worms. #study investigated other outcome measures that will be included in other tables. *denotes statistical significance, p<0.05.
(DOCX)
Abbreviations: CAD, coronary artery disease; MI, myocardial infarction; IQR, interquartile range; STH, soil-transmitted helminths; LF, lymphatic filariasis; PCR, polymerase chain reaction; PSI, previous schistosome infection; SEA, soluble egg antigen; HFD, high-fat diet; PBS, phosphate buffered saline. #study investigated other outcome measures that will be included in other tables. *denotes statistical significance, p<0.05.
(DOCX)
Abbreviations: IQR, interquartile range; STH, soil-transmitted helminths; SBP, systolic blood pressure; DBP, diastolic blood pressure; PZQ, praziquantel; PCR, polymerase chain reaction; RCT, randomized controlled trial; BP, blood pressure; PSI, previous schistosome infection; MAP, mean arterial pressure; PVR, peripheral vascular resistance; #study investigated other outcome measures that will be included in other tables. *denotes statistical significance, p<0.05.
(DOCX)
Abbreviations: hsCRP, high-sensitivity C-reactive protein; IQR, interquartile range; STH, soil-transmitted helminths; PCR, polymerase chain reaction; RCT, randomized controlled trial; LF, lymphatic filariasis; CAD, coronary artery disease. #study investigated other outcome measures that will be included in other tables. *denotes statistical significance, p<0.05.
(DOCX)
Abbreviations: IQR, interquartile range; STH, soil-transmitted helminths; HFD, high-fat diet; SD, standard diet; SEA, soluble egg antigen. #study investigated other outcome measures that will be included in other tables. *denotes statistical significance, p<0.05.
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(CSV)
Acknowledgments
We thank the librarian team at Weill Cornell Medicine for their assistance with searching and retrieving study records for this systematic review. We also thank Drs. Mary Charlson, Carol Mancuso, and Martin Shapiro, who all lead the Master’s Program in Clinical Epidemiology and Health Services Research at the Weill Cornell Graduate School of Medical Sciences, for their valuable input which helped to shape the direction of this study.
Registration
A review protocol was registered with PROSPERO (registration number CRD42021228610). It is available online (https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=228610).
Data Availability
All relevant data are within the manuscript and its Supporting information files.
Funding Statement
The study received support from NewYork-Presbyterian Hospital (NYPH) and Weill Cornell Medical College (WCMC), including the Clinical and Translational Science Center (CTSC) (UL1 TR000457) and Joint Clinical Trials Office (JCTO), as well as the Weill Cornell T32 training grant (T32AI007613 Research Training in Infectious Diseases). KP is supported by the Burroughs Wellcome Fund/American Society of Tropical Medicine & Hygiene Postdoctoral Fellowship in Tropical Infectious Diseases. RP is supported by the National Heart, Lung, and Blood Institute (R01 HL160332). JD is supported by the National Institute of Allergy and Infectious Diseases (R01 AI 168306). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.W H O. Cardiovascular diseases (CVDs) [Internet]. 2021 [cited 2022 Apr 20]. https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds)
- 2.Collaborators GBD. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020. Oct 17;396(10258):1204–22. doi: 10.1016/S0140-6736(20)30925-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.W H O. Soil-transmitted helminth infections [Internet]. 2022 [cited 2022 Apr 20]. https://www.who.int/news-room/fact-sheets/detail/soil-transmitted-helminth-infections#:~:text=Approximately%201.5%20billion%20people%20are,soil%20contamination%20with%20infective%20eggs
- 4.Rennie C, Fernandez R, Donnelly S, McGrath KC. The Impact of Helminth Infection on the Incidence of Metabolic Syndrome: A Systematic Review and Meta-Analysis. Front Endocrinol (Lausanne). 2021. Aug 12;12:728396. doi: 10.3389/fendo.2021.728396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tracey EF, McDermott RA, McDonald MI. Do worms protect against the metabolic syndrome? A systematic review and meta-analysis. Diabetes Res Clin Pract. 2016. Oct;120:209–20. doi: 10.1016/j.diabres.2016.08.014 [DOI] [PubMed] [Google Scholar]
- 6.Li Y, Yang G, Qiang J, Cai S, Zhou H. Incidence of insulin resistance and diabetes in patients with portosystemic shunts without liver dysfunction. J Int Med Res. 2016. Oct;44(5):1040–8. doi: 10.1177/0300060516659392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sanya RE, Andia Biraro I, Nampijja M, Zziwa C, Nanyunja C, Nsubuga D, et al. Contrasting impact of rural, versus urban, living on glucose metabolism and blood pressure in Uganda. Wellcome Open Res. 2020. Aug 24;5:39. doi: 10.12688/wellcomeopenres.15616.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tahapary DL, de Ruiter K, Martin I, Brienen EAT, van Lieshout L, Cobbaert CM, et al. Effect of Anthelmintic Treatment on Insulin Resistance: A Cluster-Randomized, Placebo-Controlled Trial in Indonesia. Clin Infect Dis. 2017. Sep 1;65(5):764–71. doi: 10.1093/cid/cix416 [DOI] [PubMed] [Google Scholar]
- 9.W H O. 2030 targets for soil-transmitted helminthiases control programmes [Internet]. 2020 [cited 2022 Apr 20]. https://apps.who.int/iris/bitstream/handle/10665/330611/9789240000315-eng.pdf
- 10.Grundy SM, Brewer HB, Cleeman JI, Smith SC, Lenfant C, American Heart Association, et al. Definition of metabolic syndrome: Report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation. 2004. Jan 27;109(3):433–8. doi: 10.1161/01.CIR.0000111245.75752.C6 [DOI] [PubMed] [Google Scholar]
- 11.Hotez PJ, Brindley PJ, Bethony JM, King CH, Pearce EJ, Jacobson J. Helminth infections: the great neglected tropical diseases. J Clin Invest. 2008. Apr;118(4):1311–21. doi: 10.1172/JCI34261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998. Jun;52(6):377–84. doi: 10.1136/jech.52.6.377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sanya RE, Webb EL, Zziwa C, Kizindo R, Sewankambo M, Tumusiime J, et al. The Effect of Helminth Infections and Their Treatment on Metabolic Outcomes: Results of a Cluster-Randomized Trial. Clin Infect Dis. 2020. Jul 27;71(3):601–13. doi: 10.1093/cid/ciz859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Muthukumar R, Suttiprapa S, Mairiang E, Kessomboon P, Laha T, Smith JF, et al. Effects of Opisthorchis viverrini infection on glucose and lipid profiles in human hosts: A cross-sectional and prospective follow-up study from Thailand. Parasitol Int. 2020. Apr;75:102000. doi: 10.1016/j.parint.2019.102000 [DOI] [PubMed] [Google Scholar]
- 15.Luo X, Zhu Y, Liu R, Song J, Zhang F, Zhang W, et al. Praziquantel treatment after Schistosoma japonicum infection maintains hepatic insulin sensitivity and improves glucose metabolism in mice. Parasit Vectors. 2017. Oct 2;10(1):453. doi: 10.1186/s13071-017-2400-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yuksek N, Altug N, Denizhan V, Ceylan E, Agaoglu Z. Enhancement of the glucose metabolism and the reverse cholesterol transport by a peroxisome proliferator receptor alpha (PPAR alpha) agonist included in the fasciolosis treatment in naturally infested sheep. Revue De Medecine Veterinaire. 2013;164(4):163–72. [Google Scholar]
- 17.Kozat S, Denizhan V. Glucose, lipid, and lipoprotein levels in sheep naturally infected with Fasciola hepatica. J Parasitol. 2010. Jun;96(3):657–9. doi: 10.1645/GE-2104.1 [DOI] [PubMed] [Google Scholar]
- 18.Castelli WP. Incidence of coronary heart disease and lipoprotein cholesterol levels. The Framingham Study. JAMA: The Journal of the American Medical Association. 1986. Nov 28;256(20):2835–8. [PubMed] [Google Scholar]
- 19.Després JP, Lemieux I, Dagenais GR, Cantin B, Lamarche B. HDL-cholesterol as a marker of coronary heart disease risk: the Québec cardiovascular study. Atherosclerosis. 2000. Dec;153(2):263–72. [DOI] [PubMed] [Google Scholar]
- 20.Afshan K, Kabeer S, Firasat S, Jahan S, Qayyum M. Seroepidemiology of human fascioliasis and its relationship with anti-Fasciola IgG and liver enzymes as biomarkers of pathogenicity. Afr Health Sci. 2020. Mar;20(1):208–18. doi: 10.4314/ahs.v20i1.26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zaman S, Afshan K, Firasat S, Jahan S, Qayyum M. Measurement of Ascaris lumbricoides IgG antibody, associated risk factors and identification of serum biochemical parameters as biomarkers of pathogenicity: among patients with gastrointestinal complains in Pakistan. Trop Biomed. 2018. Mar 1;35(1):10–25. [PubMed] [Google Scholar]
- 22.Aravindhan V, Mohan V, Surendar J, Rao MM, Anuradha R, Deepa M, et al. Effect of filarial infection on serum inflammatory and atherogenic biomarkers in coronary artery disease (CURES-121). Am J Trop Med Hyg. 2012. May;86(5):828–33. doi: 10.4269/ajtmh.2012.11-0773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Buck AA, Anderson RI, Colston JA, Wallace CK, Connor DH, Harman LE, et al. Microfilaruria in onchocerciasis. A clinical and epidemiological follow-up study in the Republic of Chad. Bull World Health Organ. 1971;45(3):353–69. [PMC free article] [PubMed] [Google Scholar]
- 24.Changbumrung S, Ratarasarn S, Hongtong K, Migasena P, Vutikes S, Migasena S. Lipid composition of serum lipoprotein in opisthorchiasis. Annals of tropical medicine and parasitology. 1988;82(3):263–9. doi: 10.1080/00034983.1988.11812242 [DOI] [PubMed] [Google Scholar]
- 25.Chen Y, Lu J, Huang Y, Wang T, Xu Y, Xu M, et al. Association of previous schistosome infection with diabetes and metabolic syndrome: a cross-sectional study in rural China. J Clin Endocrinol Metab. 2013. Feb;98(2):E283–7. doi: 10.1210/jc.2012-2517 [DOI] [PubMed] [Google Scholar]
- 26.Dessie N, Lema W, Aemero M. Hematological and Biochemical Profile of Patients Infected with Schistosoma mansoni in Comparison with Apparently Healthy Individuals at Sanja Town, Northwest Ethiopia: A Cross-Sectional Study. J Trop Med. 2020. May 6;2020:4083252. doi: 10.1155/2020/4083252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Doenhoff MJ, Stanley RG, Griffiths K, Jackson CL. An anti-atherogenic effect of Schistosoma mansoni infections in mice associated with a parasite-induced lowering of blood total cholesterol. Parasitology. 2002. Nov;125(Pt 5):415–21. doi: 10.1017/s0031182002002275 [DOI] [PubMed] [Google Scholar]
- 28.Duan Q, Xiong L, Liao C, Liu Z, Xiao Y, Huang R, et al. Population based and animal study on the effects of Schistosoma japonicum infection in the regulation of host glucose homeostasis. Acta Trop. 2018. Apr;180:33–41. doi: 10.1016/j.actatropica.2018.01.002 [DOI] [PubMed] [Google Scholar]
- 29.El-Shazly AM, Azab MS, El-Beshbishi SN, Sakr TI, El-Fayoumy KN, El-Ghareeb AS, et al. Biochemical parameters in chronic fascioliasis. Journal of the Egyptian Society of Parasitology. 2008;38(3):977–90. [PubMed] [Google Scholar]
- 30.da Silva Filomeno CE, Costa-Silva M, Corrêa CL, Neves RH, Mandarim-de-Lacerda CA, Machado-Silva JR. The acute schistosomiasis mansoni ameliorates metabolic syndrome in the C57BL/6 mouse model. Exp Parasitol. 2020. May;212:107889. doi: 10.1016/j.exppara.2020.107889 [DOI] [PubMed] [Google Scholar]
- 31.Gillett MP, Carvalho VC. Schistosoma mansoni: a comparative study of plasma and erythrocyte lipid alterations in the experimentally infected mouse and in selected human patients. Experimental parasitology. 1978;44(2):173–80. doi: 10.1016/0014-4894(78)90095-4 [DOI] [PubMed] [Google Scholar]
- 32.Hays R, Esterman A, Giacomin P, Loukas A, McDermott R. Does Strongyloides stercoralis infection protect against type 2 diabetes in humans? Evidence from Australian Aboriginal adults. Diabetes Res Clin Pract. 2015. Mar;107(3):355–61. doi: 10.1016/j.diabres.2015.01.012 [DOI] [PubMed] [Google Scholar]
- 33.Hong SJ, Woo HC, Chung MH, Ahn JH, Moon YS, Choi CH. Liver function in Clonorchis sinensis-infected rabbits. The Korean journal of parasitology. 1994;32(3):177–83. doi: 10.3347/kjp.1994.32.3.177 [DOI] [PubMed] [Google Scholar]
- 34.de Jesus Inês E, Sampaio Silva ML, de Souza JN, Galvão AA, Aquino Teixeira MC, Soares NM. Alterations in serum paraoxonase-1 activity and lipid profile in chronic alcoholic patients infected with Strongyloides stercoralis. Acta Trop. 2017. Feb;166:1–6. doi: 10.1016/j.actatropica.2016.10.013 [DOI] [PubMed] [Google Scholar]
- 35.La Flamme AC, Harvie M, Kenwright D, Cameron K, Rawlence N, Low YS, et al. Chronic exposure to schistosome eggs reduces serum cholesterol but has no effect on atherosclerotic lesion development. Parasite Immunol. 2007. May;29(5):259–66. doi: 10.1111/j.1365-3024.2007.00942.x [DOI] [PubMed] [Google Scholar]
- 36.Laothong U, Pinlaor P, Boonsiri P, Hiraku Y, Khoontawad J, Hongsrichan N, et al. α-Tocopherol and lipid profiles in plasma and the expression of α-tocopherol-related molecules in the liver of Opisthorchis viverrini-infected hamsters. Parasitol Int. 2013. Apr;62(2):127–33. [DOI] [PubMed] [Google Scholar]
- 37.Lira DGD, de Oliveira DC, Brayner FA, de L Aires A, Albuquerque MCPA, Vieira LD, et al. Superimposing a high-fat diet on Schistosoma mansoni infection affects renin-angiotensin system components in the mouse kidney. Rev Soc Bras Med Trop. 2019. Mar 7;52:e20180371. doi: 10.1590/0037-8682-0371-2018 [DOI] [PubMed] [Google Scholar]
- 38.Magen E, Bychkov V, Ginovker A, Kashuba E. Chronic Opisthorchis felineus infection attenuates atherosclerosis—an autopsy study. Int J Parasitol. 2013. Sep;43(10):819–24. doi: 10.1016/j.ijpara.2013.04.008 [DOI] [PubMed] [Google Scholar]
- 39.Onuegbu JA, Olisekodiaka JM, Oladele HA, Opeyemi US, Igbeneghu CA, Adeyeye AD. Lipid profile of subjects infected with Schistosoma Haematobium in South-Western Nigeria. Pakistan Journal of Medical Sciences. 2011;27(1):44–7. [Google Scholar]
- 40.Owen JS, Costa JC, Carvalho V, Gillett MP. Effect of experimental schistosomiasis mansoni on plasma and erythrocyte lipids and on plasma lecithin: cholesterol acyltransferase in the mouse. Revista brasileira de biologia. 1978;38(4):913–8. [PubMed] [Google Scholar]
- 41.Ramos TM de B, de Vasconcelos AS, de Carvalho VCO, Lima VL de M. [Alterations in cholesterol, triglyceride and total phospholipid levels in plasma of Callithrix jacchus (sagüi) reinfected by Schistosoma mansoni]. Rev Soc Bras Med Trop. 2004. Feb;37(1):37–40. [DOI] [PubMed] [Google Scholar]
- 42.Shen SW, Lu Y, Li F, Shen ZH, Xu M, Yao WF, et al. The potential long-term effect of previous schistosome infection reduces the risk of metabolic syndrome among Chinese men. Parasite Immunol. 2015. Jul;37(7):333–9. doi: 10.1111/pim.12187 [DOI] [PubMed] [Google Scholar]
- 43.Shen S-W, Lu Y, Li F, Shen Z-H, Xu M, Yao W-F, et al. The potential long-term effect of previous schistosome infection may reduce the risk factors for cardiovascular diseases. Int J Cardiol. 2014. Dec 15;177(2):566–8. doi: 10.1016/j.ijcard.2014.08.128 [DOI] [PubMed] [Google Scholar]
- 44.Stanley RG, Jackson CL, Griffiths K, Doenhoff MJ. Effects of Schistosoma mansoni worms and eggs on circulating cholesterol and liver lipids in mice. Atherosclerosis. 2009. Nov;207(1):131–8. doi: 10.1016/j.atherosclerosis.2009.04.037 [DOI] [PubMed] [Google Scholar]
- 45.Tahapary DL, de Ruiter K, Kurniawan F, Djuardi Y, Wang Y, Nurdin SME, et al. Impact of rural-urban environment on metabolic profile and response to a 5-day high-fat diet. Sci Rep. 2018. May 25;8(1):8149. doi: 10.1038/s41598-018-25092-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Toulah FH, El-Aswad BEW, Harba NM, Naguib YM. Therapeutic effects of Schistosoma mansoni soluble egg antigen in high fat diet induced dyslipidemia, hepatic and cardiovascular pathology in mice. Tropical Biomedicine. 2018;35(4):893–907. [PubMed] [Google Scholar]
- 47.Wiria AE, Wammes LJ, Hamid F, Dekkers OM, Prasetyani MA, May L, et al. Relationship between carotid intima media thickness and helminth infections on Flores Island, Indonesia. PLoS ONE. 2013. Jan 24;8(1):e54855. doi: 10.1371/journal.pone.0054855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wolde M, Berhe N, Medhin G, Chala F, van Die I, Tsegaye A. Inverse Associations of Schistosoma mansoni Infection and Metabolic Syndromes in Humans: A Cross-Sectional Study in Northeast Ethiopia. Microbiol Insights. 2019. May 22;12:1178636119849934. doi: 10.1177/1178636119849934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wolfs IMJ, Stöger JL, Goossens P, Pöttgens C, Gijbels MJJ, Wijnands E, et al. Reprogramming macrophages to an anti-inflammatory phenotype by helminth antigens reduces murine atherosclerosis. FASEB J. 2014. Jan;28(1):288–99. doi: 10.1096/fj.13-235911 [DOI] [PubMed] [Google Scholar]
- 50.Xue Y-F, Shen L. [Effect of Schistosoma japonicum infection on serum lipid status in mice]. Zhongguo ji sheng chong xue yu ji sheng chong bing za zhi = Chinese journal of parasitology & parasitic diseases. 2014;32(1):12–6. [PubMed] [Google Scholar]
- 51.Yang H, Li H, Chen W, Mei Z, Yuan Y, Wang X, et al. Therapeutic Effect of Schistosoma japonicum Cystatin on Atherosclerotic Renal Damage. Front Cell Dev Biol. 2021. Nov 25;9:760980. doi: 10.3389/fcell.2021.760980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zinsou JF, Janse JJ, Honpkehedji JY, Dejon-Agobe JC, Garcia-Tardon N, Hoekstra PT, et al. Schistosoma haematobiuminfection is associated with lower serum cholesterol levels and improved lipid profile in overweight/obese individuals. Plos Neglected Tropical Diseases. 2020;14(7). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zou Z-Q, Liu M, Zhong H-Q, Guan G-Y. Association of previous schistosome infection with fatty liver and coronary heart disease: A cross-sectional study in china. Parasite Immunol. 2021. Apr;43(4):e12822. doi: 10.1111/pim.12822 [DOI] [PubMed] [Google Scholar]
- 54.da Silva FL, Del-Rei RP, Fraga DBM, Leony LM, de Souza AMGC, Santos FLN. Alterations in the lipid profiles and circulating liver enzymes in individuals infected by Schistosoma mansoni. Rev Soc Bras Med Trop. 2018. Dec;51(6):795–801. doi: 10.1590/0037-8682-0113-2018 [DOI] [PubMed] [Google Scholar]
- 55.de Oliveira DNG, de M. Costa J. Schistosoma mansoni: Cholesteryl ester profiles of plasma and liver in experimentally infected mice. Exp Parasitol. 1977. Oct;43(1):244–7. [DOI] [PubMed] [Google Scholar]
- 56.Mohamed SMA, Saber T, Taha AA, Roshdy HS, Shahien NE. RELATION BETWEEN SCHISTOSOME PAST INFECTION AND METABOLIC SYNDROME. Journal of the Egyptian Society of Parasitology. 2017;47(1):137–43. [PubMed] [Google Scholar]
- 57.Hays R, Giacomin P, Olma L, Esterman A, McDermott R. The relationship between treatment for Strongyloides stercoralis infection and type 2 diabetes mellitus in an Australian Aboriginal population: A three-year cohort study. Diabetes Res Clin Pract. 2017. Dec;134:8–16. doi: 10.1016/j.diabres.2017.09.012 [DOI] [PubMed] [Google Scholar]
- 58.Rajamanickam A, Munisankar S, Bhootra Y, Dolla C, Thiruvengadam K, Nutman TB, et al. Metabolic Consequences of Concomitant Strongyloides stercoralis Infection in Patients With Type 2 Diabetes Mellitus. Clin Infect Dis. 2019. Aug 1;69(4):697–704. doi: 10.1093/cid/ciy935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Rajamanickam A, Munisankar S, Thiruvengadam K, Menon PA, Dolla C, Nutman TB, et al. Impact of Helminth Infection on Metabolic and Immune Homeostasis in Non-diabetic Obesity. Front Immunol. 2020. Sep 16;11:2195. doi: 10.3389/fimmu.2020.02195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Shaheen AA, Ebeid FA, Fahim AT. Effect of praziquantel on some aspects of carbohydrate metabolism in mice infected with Schistosoma mansoni. Pharmacol Res. 1989. Jun;21(3):263–70. doi: 10.1016/s1043-6618(89)80004-0 [DOI] [PubMed] [Google Scholar]
- 61.Cortes-Selva D, Elvington AF, Ready A, Rajwa B, Pearce EJ, Randolph GJ, et al. Schistosoma mansoni Infection-Induced Transcriptional Changes in Hepatic Macrophage Metabolism Correlate With an Athero-Protective Phenotype. Front Immunol. 2018. Nov 12;9:2580. doi: 10.3389/fimmu.2018.02580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hussaarts L, García-Tardón N, van Beek L, Heemskerk MM, Haeberlein S, van der Zon GC, et al. Chronic helminth infection and helminth-derived egg antigens promote adipose tissue M2 macrophages and improve insulin sensitivity in obese mice. FASEB J. 2015. Jul;29(7):3027–39. doi: 10.1096/fj.14-266239 [DOI] [PubMed] [Google Scholar]
- 63.Phiri IK, Phiri AM, Harrison LJS. The serum glucose and beta-hydroxybutyrate levels in sheep with experimental Fasciola hepatica and Fasciola gigantica infection. Vet Parasitol. 2007. Feb 28;143(3–4):287–93. doi: 10.1016/j.vetpar.2006.09.001 [DOI] [PubMed] [Google Scholar]
- 64.Tang C-L, Yu X-H, Li Y, Zhang R-H, Xie J, Liu Z-M. Schistosoma japonicum Soluble Egg Antigen Protects Against Type 2 Diabetes in Lepr db/db Mice by Enhancing Regulatory T Cells and Th2 Cytokines. Front Immunol. 2019. Jun 26;10:1471. doi: 10.3389/fimmu.2019.01471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wiria AE, Hamid F, Wammes LJ, Prasetyani MA, Dekkers OM, May L, et al. Infection with Soil-Transmitted Helminths Is Associated with Increased Insulin Sensitivity. PLoS ONE. 2015. Jun 10;10(6):e0127746. doi: 10.1371/journal.pone.0127746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Saule P, Vicogne J, Delacre M, Macia L, Tailleux A, Dissous C, et al. Host glucose metabolism mediates T4 and IL-7 action on Schistosoma mansoni development. J Parasitol. 2005. Aug;91(4):737–44. doi: 10.1645/GE-3402.1 [DOI] [PubMed] [Google Scholar]
- 67.Thabet HS, Saleh NKM, Thabet SS, Abdel-Aziz M, Kalleny NK. Decreased basal non-insulin-stimulated glucose uptake by diaphragm in streptozotocin-induced diabetic mice infected with Schistosoma mansoni. Parasitol Res. 2008. Aug;103(3):595–601. doi: 10.1007/s00436-008-1016-2 [DOI] [PubMed] [Google Scholar]
- 68.Talukder MR, Pham H, Woodman R, Wilson K, Taylor K, Kaldor J, et al. The Association between Diabetes and Human T-Cell Leukaemia Virus Type-1 (HTLV-1) with Strongyloides stercoralis: Results of a Community-Based, Cross-Sectional Survey in Central Australia. Int J Environ Res Public Health. 2022. Feb 13;19(4). doi: 10.3390/ijerph19042084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.PrayGod G, Filteau S, Range N, Ramaiya K, Jeremiah K, Rehman AM, et al. The association of Schistosoma and geohelminth infections with β-cell function and insulin resistance among HIV-infected and HIV-uninfected adults: A cross-sectional study in Tanzania. PLoS ONE. 2022. Jan 25;17(1):e0262860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Tang C-L, Liu Z-M, Gao YR, Xiong F. Schistosoma Infection andSchistosoma-Derived Products Modulate the Immune Responses Associated with Protection against Type 2 Diabetes. Front Immunol. 2017;8:1990. doi: 10.3389/fimmu.2017.01990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Htun NSN, Odermatt P, Müller I, Yap P, Steinmann P, Schindler C, et al. Association between gastrointestinal tract infections and glycated hemoglobin in school children of poor neighborhoods in Port Elizabeth, South Africa. PLoS Negl Trop Dis. 2018. Mar 15;12(3):e0006332. doi: 10.1371/journal.pntd.0006332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Amdare NP, Khatri VK, Yadav RSP, Tarnekar A, Goswami K, Reddy MVR. Therapeutic potential of the immunomodulatory proteins Wuchereria bancrofti L2 and Brugia malayi abundant larval transcript 2 against streptozotocin-induced type 1 diabetes in mice. J Helminthol. 2017. Sep;91(5):539–48. doi: 10.1017/S0022149X1600064X [DOI] [PubMed] [Google Scholar]
- 73.Aravindhan V, Mohan V, Surendar J, Muralidhara Rao M, Pavankumar N, Deepa M, et al. Decreased prevalence of lymphatic filariasis among diabetic subjects associated with a diminished pro-inflammatory cytokine response (CURES 83). PLoS Negl Trop Dis. 2010. Jun 15;4(6):e707. doi: 10.1371/journal.pntd.0000707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Aravindhan V, Mohan V, Surendar J, Rao MM, Ranjani H, Kumaraswami V, et al. Decreased prevalence of lymphatic filariasis among subjects with type-1 diabetes. Am J Trop Med Hyg. 2010. Dec;83(6):1336–9. doi: 10.4269/ajtmh.2010.10-0410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Cooke A, Tonks P, Jones FM, O’Shea H, Hutchings P, Fulford AJ, et al. Infection with Schistosoma mansoni prevents insulin dependent diabetes mellitus in non-obese diabetic mice. Parasite Immunol. 1999. Apr;21(4):169–76. doi: 10.1046/j.1365-3024.1999.00213.x [DOI] [PubMed] [Google Scholar]
- 76.El-Gebaly N, Rehan M, Abdelfattah D. Immunomodulating effect of Schistosoma mansoni soluble egg antigen on course of induced diabetes mellitus in experimental mice. Parasitol United J. 2019. Apr 1;12(1):45–52. [Google Scholar]
- 77.El-Wakil HS, Aboushousha TSE, El Haddad O, Gamil NB, Mansour T, El-Said H. Effect of schistosoma mansoni egg deposition on multiple low doses streptozotocin induced insulin dependent diabetes. J Egypt Soc Parasitol. 2002. Dec;32(3):987–1002. [PubMed] [Google Scholar]
- 78.Lund ME, O’Brien BA, Hutchinson AT, Robinson MW, Simpson AM, Dalton JP, et al. Secreted proteins from the helminth Fasciola hepatica inhibit the initiation of autoreactive T cell responses and prevent diabetes in the NOD mouse. PLoS ONE. 2014. Jan 21;9(1):e86289. doi: 10.1371/journal.pone.0086289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Lund ME, Greer J, Dixit A, Alvarado R, McCauley-Winter P, To J, et al. A parasite-derived 68-mer peptide ameliorates autoimmune disease in murine models of Type 1 diabetes and multiple sclerosis. Sci Rep. 2016. Nov 24;6:37789. doi: 10.1038/srep37789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Osada Y, Fujiyama T, Kamimura N, Kaji T, Nakae S, Sudo K, et al. Dual genetic absence of STAT6 and IL-10 does not abrogate anti-hyperglycemic effects of Schistosoma mansoni in streptozotocin-treated diabetic mice. Exp Parasitol. 2017. Jun;177:1–12. doi: 10.1016/j.exppara.2017.03.008 [DOI] [PubMed] [Google Scholar]
- 81.Reddy SM, Reddy PM, Amdare N, Khatri V, Tarnekar A, Goswami K, et al. Filarial Abundant Larval Transcript Protein ALT-2: An Immunomodulatory Therapeutic Agent for Type 1 Diabetes. Indian J Clin Biochem. 2017. Mar;32(1):45–52. doi: 10.1007/s12291-016-0572-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Wang L, Gao Y, Pan Q, Tang C, Zhang R, Li Y, et al. Protective effect and mechanism of Schistosoma japonicum soluble egg antigen against type 1 diabetes in NOD mice. Int J Diabetes Dev Ctries. 2021. Jul 29; [Google Scholar]
- 83.Yan K, Wang B, Zhou H, Luo Q, Shen J, Xu Y, et al. Amelioration of type 1 diabetes by recombinant fructose-1,6-bisphosphate aldolase and cystatin derived from Schistosoma japonicum in a murine model. Parasitol Res. 2020. Jan;119(1):203–14. doi: 10.1007/s00436-019-06511-7 [DOI] [PubMed] [Google Scholar]
- 84.Zaccone P, Fehérvári Z, Jones FM, Sidobre S, Kronenberg M, Dunne DW, et al. Schistosoma mansoni antigens modulate the activity of the innate immune response and prevent onset of type 1 diabetes. Eur J Immunol. 2003. May;33(5):1439–49. doi: 10.1002/eji.200323910 [DOI] [PubMed] [Google Scholar]
- 85.Almugadam BS, Ibrahim MK, Liu Y, Chen S-M, Wang C-H, Shao C-Y, et al. Association of urogenital and intestinal parasitic infections with type 2 diabetes individuals: a comparative study. BMC Infect Dis. 2021. Jan 7;21(1):20. doi: 10.1186/s12879-020-05629-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Htun NSN, Odermatt P, Paboriboune P, Sayasone S, Vongsakid M, Phimolsarn-Nusith V, et al. Association between helminth infections and diabetes mellitus in adults from the Lao People’s Democratic Republic: a cross-sectional study. Infect Dis Poverty. 2018. Nov 6;7(1):105. doi: 10.1186/s40249-018-0488-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Machado ER, Matos NO, Rezende SM, Carlos D, Silva TC, Rodrigues L, et al. Host-Parasite Interactions in Individuals with Type 1 and 2 Diabetes Result in Higher Frequency of Ascaris lumbricoides and Giardia lamblia in Type 2 Diabetic Individuals. J Diabetes Res. 2018. Feb 6;2018:4238435. doi: 10.1155/2018/4238435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.McGuire E, Welch C, Melzer M. Is Strongyloides seropositivity associated with diabetes mellitus? A retrospective case-control study in an East London NHS Trust. Trans R Soc Trop Med Hyg. 2019. Apr 1;113(4):189–94. doi: 10.1093/trstmh/try132 [DOI] [PubMed] [Google Scholar]
- 89.Mendonça SCL, Gonçalves-Pires M do RF, Rodrigues RM, Ferreira A, Costa-Cruz JM. Is there an association between positive Strongyloides stercoralis serology and diabetes mellitus? Acta Trop. 2006. Aug;99(1):102–5. doi: 10.1016/j.actatropica.2006.06.006 [DOI] [PubMed] [Google Scholar]
- 90.Kalantari N, Darbandi Z, Bayani MA, Sharbatkhori M, Bayani M, Ghaffari S. Prevalence and associated risk factors of strongyloides sp. infection in diabetic patients in the central part of mazandaran, northern iran. Arch Clin Infect Dis. 2019. Aug 14;14(4). [Google Scholar]
- 91.Shalaby ES, Zaki SA, Fahmy SA. Incidence of atherosclerosis, hypertension & myocardial infarction in bilharzial cirrhosis. J Egypt Med Assoc. 1963;46:53–6. [PubMed] [Google Scholar]
- 92.González-Fernández D, Pons EDC, Rueda D, Sinisterra OT, Murillo E, Scott ME, et al. Identification of High-Risk Pregnancies in a Remote Setting Using Ambulatory Blood Pressure: The MINDI Cohort. Front Public Health. 2020. Mar 24;8:86. doi: 10.3389/fpubh.2020.00086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Sarin SK, Mosca P, Sabbà C, Groszmann RJ. Hyperdynamic circulation in a chronic murine schistosomiasis model of portal hypertension. Hepatology. 1991. Mar;13(3):581–4. [PubMed] [Google Scholar]
- 94.Quispe R, Michos ED, Martin SS, Puri R, Toth PP, Al Suwaidi J, et al. High-Sensitivity C-Reactive Protein Discordance With Atherogenic Lipid Measures and Incidence of Atherosclerotic Cardiovascular Disease in Primary Prevention: The ARIC Study. J Am Heart Assoc. 2020. Feb 4;9(3):e013600. doi: 10.1161/JAHA.119.013600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Carrero JJ, Andersson Franko M, Obergfell A, Gabrielsen A, Jernberg T. hsCRP Level and the Risk of Death or Recurrent Cardiovascular Events in Patients With Myocardial Infarction: a Healthcare-Based Study. J Am Heart Assoc. 2019. Jun 4;8(11):e012638. doi: 10.1161/JAHA.119.012638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Bychkov VG, Zolotukhin VM, Khadieva ED, Kulikova SV, Petrov IM, Berdinskih SG, et al. Hypereosinophilic syndrome, cardiomyopathies, and sudden cardiac death in superinvasive opisthorchiasis. Cardiol Res Pract. 2019. May 9;2019:4836948. doi: 10.1155/2019/4836948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Carranza-Rodríguez C, San-Román-Sánchez D, Marrero-Santiago H, Hernández-Cabrera M, Gil-Guillén C, Pisos-Álamo E, et al. Endomyocardial involvement in asymptomatic sub-Saharan immigrants with helminth-related eosinophilia. PLoS Negl Trop Dis. 2017. Feb 24;11(2):e0005403. doi: 10.1371/journal.pntd.0005403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Góes VC, Neves RH, Alencar ACMB, Oliveira AV, Gomes DC, Machado-Silva JR. Effects of high-fat chow on heart tissue in acute and chronic experimental murine schistosomiasis mansoni. Parasitology. 2012. Sep;139(11):1462–70. [DOI] [PubMed] [Google Scholar]
- 99.Ji Q, Cheng G, Ma N, Huang Y, Lin Y, Zhou Q, et al. Circulating th1, th2, and th17 levels in hypertensive patients. Dis Markers. 2017. Jul 5;2017:7146290. doi: 10.1155/2017/7146290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Fairweather D. Regulating inflammation in the heart. Int J Biomed Sci. 2007. Mar;3(1):9–13. [PMC free article] [PubMed] [Google Scholar]
- 101.Szodoray P, Timar O, Veres K, Der H, Szomjak E, Lakos G, et al. TH1/TH2 imbalance, measured by circulating and intracytoplasmic inflammatory cytokines—immunological alterations in acute coronary syndrome and stable coronary artery disease. Scand J Immunol. 2006. Sep;64(3):336–44. doi: 10.1111/j.1365-3083.2006.01816.x [DOI] [PubMed] [Google Scholar]
- 102.Madhumitha H, Mohan V, Deepa M, Babu S, Aravindhan V. Increased Th1 and suppressed Th2 serum cytokine levels in subjects with diabetic coronary artery disease. Cardiovasc Diabetol. 2014. Jan 3;13:1. doi: 10.1186/1475-2840-13-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Norlander AE, Madhur MS, Harrison DG. The immunology of hypertension. J Exp Med. 2018. Jan 2;215(1):21–33. doi: 10.1084/jem.20171773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Yu Q, Watson RR, Marchalonis JJ, Larson DF. A role for T lymphocytes in mediating cardiac diastolic function. Am J Physiol Heart Circ Physiol. 2005. Aug;289(2):H643–51. doi: 10.1152/ajpheart.00073.2005 [DOI] [PubMed] [Google Scholar]
- 105.Trial J, Potempa LA, Entman ML. The role of C-reactive protein in innate and acquired inflammation: new perspectives. Inflamm Cell Signal. 2016. Sep 5;3(2). [PMC free article] [PubMed] [Google Scholar]
- 106.Sproston NR, Ashworth JJ. Role of C-Reactive Protein at Sites of Inflammation and Infection. Front Immunol. 2018. Apr 13;9:754. doi: 10.3389/fimmu.2018.00754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Pepys MB, Hirschfield GM. C-reactive protein: a critical update. J Clin Invest. 2003. Jun;111(12):1805–12. doi: 10.1172/JCI18921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Robinson MW, Harmon C, O’Farrelly C. Liver immunology and its role in inflammation and homeostasis. Cell Mol Immunol. 2016. May;13(3):267–76. doi: 10.1038/cmi.2016.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Guigas B, Molofsky AB. A worm of one’s own: how helminths modulate host adipose tissue function and metabolism. Trends Parasitol. 2015. Sep;31(9):435–41. doi: 10.1016/j.pt.2015.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Brouwers JF, Smeenk IM, van Golde LM, Tielens AG. The incorporation, modification and turnover of fatty acids in adult Schistosoma mansoni. Mol Biochem Parasitol. 1997. Sep;88(1–2):175–85. doi: 10.1016/s0166-6851(97)00091-1 [DOI] [PubMed] [Google Scholar]
- 111.Urbina EM, Gao Z, Khoury PR, Martin LJ, Dolan LM. Insulin resistance and arterial stiffness in healthy adolescents and young adults. Diabetologia. 2012. Mar;55(3):625–31. doi: 10.1007/s00125-011-2412-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Witteman JC, Grobbee DE, Valkenburg HA, van Hemert AM, Stijnen T, Burger H, et al. J-shaped relation between change in diastolic blood pressure and progression of aortic atherosclerosis. Lancet. 1994. Feb 26;343(8896):504–7. doi: 10.1016/s0140-6736(94)91459-1 [DOI] [PubMed] [Google Scholar]
- 113.Ikonomidis I, Kadoglou N, Tsiotra PC, Kollias A, Palios I, Fountoulaki K, et al. Arterial stiffness is associated with increased monocyte expression of adiponectin receptor mRNA and protein in patients with coronary artery disease. Am J Hypertens. 2012. Jul;25(7):746–55. doi: 10.1038/ajh.2012.42 [DOI] [PubMed] [Google Scholar]
- 114.Mozos I, Malainer C, Horbańczuk J, Gug C, Stoian D, Luca CT, et al. Inflammatory markers for arterial stiffness in cardiovascular diseases. Front Immunol. 2017. Aug 31;8:1058. doi: 10.3389/fimmu.2017.01058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Laurent S, Boutouyrie P. Arterial stiffness and hypertension in the elderly. Front Cardiovasc Med. 2020. Oct 29;7:544302. doi: 10.3389/fcvm.2020.544302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Rashid S, Uffelman KD, Barrett PHR, Lewis GF. Effect of atorvastatin on high-density lipoprotein apolipoprotein A-I production and clearance in the New Zealand white rabbit. Circulation. 2002. Dec 3;106(23):2955–60. doi: 10.1161/01.cir.0000038303.84249.4a [DOI] [PubMed] [Google Scholar]
- 117.Feingold KR, Grunfeld C. Introduction to Lipids and Lipoproteins. In: De Groot LJ, Beck-Peccoz P, Chrousos G, Dungan K, Grossman A, Hershman JM, et al., editors. Endotext. South Dartmouth (MA): MDText.com, Inc.; 2000. [Google Scholar]
- 118.Jin L, Feng X, Rong H, Pan Z, Inaba Y, Qiu L, et al. The antiparasitic drug ivermectin is a novel FXR ligand that regulates metabolism. Nat Commun. 2013;4:1937. doi: 10.1038/ncomms2924 [DOI] [PubMed] [Google Scholar]
- 119.Yang JS, Qi W, Farias-Pereira R, Choi S, Clark JM, Kim D, et al. Permethrin and ivermectin modulate lipid metabolism in steatosis-induced HepG2 hepatocyte. Food Chem Toxicol. 2019. Mar;125:595–604. doi: 10.1016/j.fct.2019.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. doi: 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]