Abstract
Primary sclerosing cholangitis (PSC) is a rare autoimmune bile duct disease that is strongly associated with immune-mediated disorders. In this study, we implemented multitrait joint analyses to genome-wide association summary statistics of PSC and numerous clinical and epidemiological traits to estimate the genetic contribution of each trait and genetic correlations between traits and to identify new lead PSC risk-associated loci. We identified seven new loci that have not been previously reported and one new independent lead variant in the previously reported locus. Functional annotation and fine-mapping nominated several potential susceptibility genes such as MANBA and IRF5. Network-based in silico drug efficacy screening provided candidate agents for further study of pharmacological effect in PSC.
Subject terms: Genetic predisposition to disease, Genetic variation, Genome-wide association studies
The genetic basis of primary sclerosing cholangitis has only been partially uncovered. Here, the authors perform a multitrait genome-wide association study to provide insight into the genetic etiology of primary sclerosing cholangitis risk and possible therapeutic drug targets.
Introduction
Primary sclerosing cholangitis (PSC) is a chronic, progressive autoimmune disorder of the bile duct1–3. Individuals with PSC are at risk of severe liver problems including a lifetime risk of cholangiocarcinoma of between 5 and 20%4. PSC is often associated with inflammatory bowel disease (IBD). Approximately 75% of individuals with PSC have IBD2, most commonly ulcerative colitis (UC). Individuals with PSC are also more likely than those without PSC to have other autoimmune diseases, including type 1 diabetes, celiac disease, and thyroid disease. The shared etiology and underlying characteristics of these immune-mediated disorders remain incompletely understood.
Recent genome-wide association studies (GWAS) have identified ~19 loci associated with PSC among individuals of European ancestry2,5. Association analysis using the Immunochip genotype array data that specifically targeted known autoimmune-related disease regions identified three additional loci influencing PSC risk6. The development of PSC can be attributed to a combination of genetic and environmental factors7. Individuals with a family history of PSC have an increased risk of developing PSC suggesting that genetic influences play a critical role in susceptibility, which may act in concert with exposure to specific environmental factors. However, the genetic and environmental risk factors are not fully elucidated. As PSC is strongly associated with IBD2, examining two traits together may provide better genetic insight into a common genetic etiology8–11. Few studies have been conducted to understand the shared genetic underpinning between PSC and other associated medical conditions.
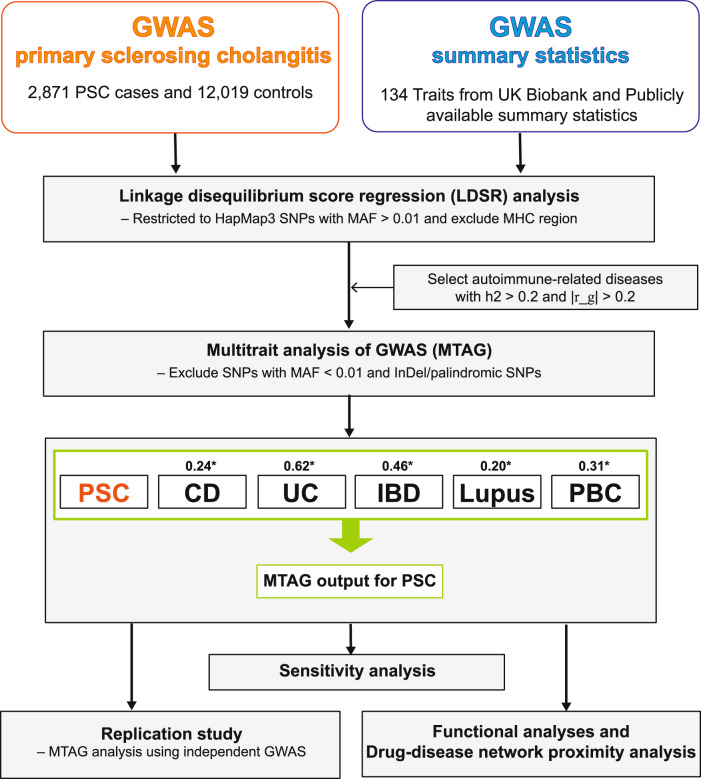
Leveraging publicly available GWAS summary-level data12–14 (Supplementary Data 1, “Methods”), we conducted cross-trait linkage disequilibrium (LD) score regression (LDSR) analysis15,16 to determine whether there was a shared genetic contribution between polygenic phenotypes for multiple diseases and traits. We explored the directionality and degree of these relationships, and whether the genetic architecture between two traits is correlated or inversely correlated17. We took advantage of the genetic overlap between traits to identify additional independent genetic variants for PSC alongside five immune-mediated disorders (Supplementary Data 2), highly correlated with PSC: Crohn’s disease18 (CD), UC18, IBD18, lupus19, and primary biliary cirrhosis20 (PBC) using multitrait analysis of GWAS21 (MTAG). Although IBD is the umbrella term that includes CD and UC, we also surveyed the pairwise genetic correlation of PSC for CD and UC, respectively. We then performed functional fine-mapping analyses on the newly identified loci to elucidate potential functional characterization and biological mechanisms affecting PSC susceptibility. Since there is no medication proven to be effective for PSC treatment, we conducted network-based drug–disease proximity analysis to identify potential agents suitable for repurposing to PSC from the previously reported13 and newly identified candidate genes in this study.
Results
PSC shows the shared genetic contributions among numerous clinical and epidemiological traits
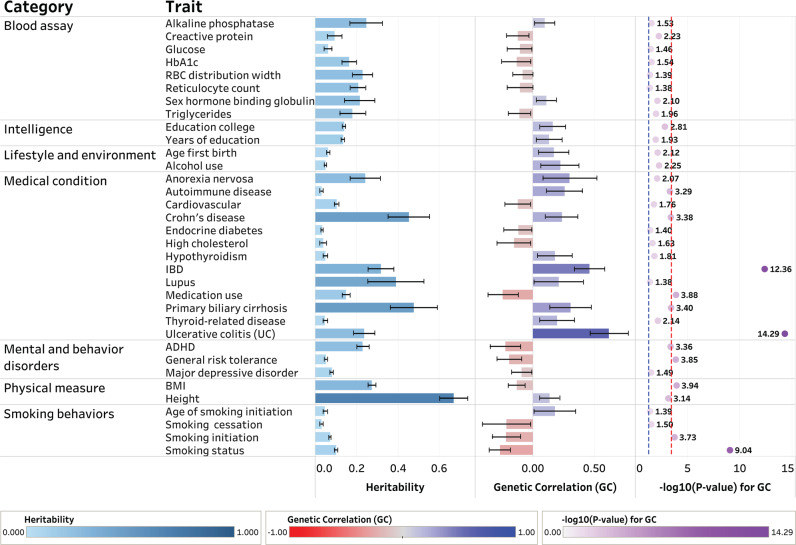
We investigated the proportion of phenotypic variance explained by all common single-nucleotide polymorphisms (SNPs) for 134 clinical and epidemiological traits to identify potential comorbid conditions and to uncover traits that are causally involved in clinical course and epidemiologic associations using LDSR (“Methods”). We identified numerous traits showing moderate SNP-heritability in the observed scale (h2). The study workflow shown in Fig. 1 summarizes the steps from data preparation to subsequent analyses in the present study. We estimated the SNP-heritability of PSC to be 0.23. Among serologic biomarkers, an increased alkaline phosphatase (ALP) level and conditions such as a blocked bile duct had an estimated SNP-heritability of 0.25. We also examined the magnitude and direction of shared genetic contribution between PSC and 134 polygenic traits of clinical and epidemiological parameters based on the cross-trait genetic correlation (r_g). We identified several polygenic traits showing moderate to strong genetic correlation with PSC at a Bonferroni-corrected significance level of P = 0.05/134 = 3.73 × 10−4. Since this is hypothesis-based research, we also considered P < 0.05 to identify nominally significant associations that could be examined in future studies. We considered P-values less than the Bonferroni-corrected significance level to be robustly associated in this study and the highlighted traits are displayed in Fig. 2. Our findings reported in Supplementary Data 3 demonstrated that the genetic architecture of PSC susceptibility was positively correlated with that of several immune-related diseases including IBD (r_g = 0.46; P = 4.41 × 10−13), UC (r_g = 0.62; P = 5.18 × 10−15), CD (r_g = 0.24; P = 4.16 × 10−4), lupus (r_g = 0.21; P = 0.04), and PBC (r_g = 0.31; P = 3.95 × 10−4). Overall shared genetic contribution between PSC and a behavior parameter, general risk tolerance defined as the willingness to take risks22, showed a significant negative correlation (r_g = −0.20; P = 1.41 × 10−4). Increased body mass index (BMI) had a significant negative genetic correlation with PSC susceptibility (r_g = −0.13; P = 1.16 × 10−4). In epidemiological studies7,23,24, the association between PSC and cigarette smoking has been inconsistent. Among traits related to smoking behaviors in this study, smoking status25 modeled in previous smokers versus current smokers showed a strong negative genetic correlation with PSC susceptibility (r_g = −0.27; P = 9.17 × 10−10) while smoking initiation26, which is a binary phenotype indicating whether an individual had ever smoked regularly (i.e., never-smokers versus ever-smokers), reported a significant negative genetic correlation with PSC (r_g = −0.20; P = 2.05 × 10−6).
Fig. 1. Flow chart of the analytical workflow in this study.
h2 represents SNP-based heritability in the observed scale. |r_g| represents the absolute value of the pairwise genetic correlation between PSC and the traits studied. MAF stands for a minor allele frequency. MHC region stands for the major histocompatibility complex region. The asterisk “*” indicates the genetic correlation between PSC and each tested trait. The imputed summary statistics for PBC were used for subsequent analyses.
Fig. 2. The shared heritability and genetic correlation of PSC among clinical and epidemiological traits.
The dotted lines in blue and red indicate nominally and Bonferroni-corrected significant levels of and , respectively. The error bar represents 95% confidence interval for the estimate of SNP-based heritability and pairwise genetic correlation of PSC in each trait, respectively. Sample sizes used to derive the estimates of SNP-based heritability and pairwise genetic correlation of PSC in each trait are shown in Supplementary Data 1. The dashboard for visualizing the results from LDSR was created using Tableau Desktop software (version 2022.2).
MTAG with immune-mediated diseases identifies new PSC-associated loci with evidence of replication
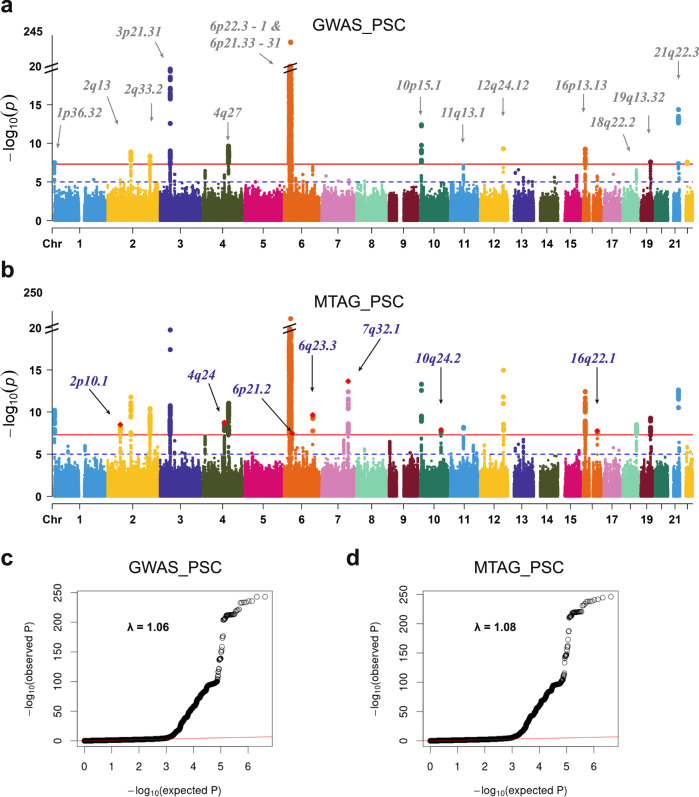
Based on findings from the genome-wide SNP-heritability and pairwise genetic correlation, we restricted our MTAG to the traits for which LDSR has suggested strong associations with PSC susceptibility, showing h2 > 0.20 and |r_g| > 0.20 (“Methods”, Supplementary Information). Five autoimmune-related disorders, CD (r_g = 0.24), UC (0.62), IBD (0.46), lupus (0.20), and PBC (0.31) were selected to identify new PSC risk loci using MTAG (Table 1). Compared to the conventional univariate GWAS, we detected more significant and stronger PSC-specific association signals when implementing MTAG. From MTAG combining PSC with five immune-related diseases; CD, UC, IBD, lupus, and PBC, we discovered seven loci (2p16.1, 4q24, 6q21.2, 6q23.3, 7q32.1, 10q24.2, and 16q22.1) that have not been previously reported or failed to reach the genome-wide significance level and one new independent significant variant of the reported locus (3p21.31) at the genome-wide significance level of 5.0 × 10−8 (Table 2 and Fig. 3). In addition, our MTAG-identified PSC-specific results confirmed 11 PSC-specific risk-associated variants that have been previously reported in a single-disease GWAS of PSC susceptibility. These include genetic variants from well-established risk loci at 1p36.32, 2q33.2, and 6p21.33-p21.32 that are strongly associated with autoimmune-related diseases2,20,27,28. We displayed a Manhattan plot for the MTAG-identified PSC-specific GWAS (MTAG_PSC, Fig. 3b) along with that from the previously published single-disease GWAS of PSC2 (GWAS_PSC, Fig. 3a). There was no substantial evidence for inflation of both GWAS test statistics (λGWAS_PSC = 1.06; λMTAG_PSC = 1.08) shown in Fig. 3c, d, respectively. MTAG-identified genomic risk variants associated with PSC susceptibility with a P < 5.0 × 10−8 are reported in Supplementary Data 4.
Table 1.
Estimate of genetic correlation among autoimmune-related diseases
| PSC | CD | UC | IBD | Lupus | PBC* | |
|---|---|---|---|---|---|---|
| Primary sclerosing cholangitis (PSC) | 1 | 0.24 (se = 0.07) | 0.62 (0.08) | 0.46 (0.06) | 0.20 (0.10) | 0.31 (0.09) |
| Crohn’s disease (CD) | 1 | 0.62 (0.03) | 0.92 (0.02) | 0.13 (0.055) | 0.18 (0.05) | |
| Ulcerative colitis (UC) | 1 | 0.90 (0.01) | 0.22 (0.07) | 0.23 (0.05) | ||
| Inflammatory bowel disease (IBD) | 1 | 0.19 (0.05) | 0.23 (0.04) | |||
| Lupus | 1 | 0.49 (0.06) | ||||
| Primary biliary cirrhosis (PBC)* | 1 |
The asterisk “*” indicates that imputed summary statistics were used to estimate the SNP-heritability and pairwise genetic correlation using the SSimp package. “se” stands for the standard error of the pairwise genetic correlation between PSC and each trait.
Table 2.
The MTAG-identified new associations of PSC
| SNP Information (Ji et al. 2017) | MTAG_PSC (Discovery) | MTAG_PSC⊥IBD (Sensitivity) | MTAG_PSC_R (Replication) | GWAS_PSC (Ji et al. 2017) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| SNP:A1/A2 | Chr:Position | Cytoband | Gene | OR | P | OR | P | OR | P | OR (EAF) | P |
| rs7608697:C/A | 2:61204641 | 2p16.1* | PUS10 | 1.07 | 3.11 × 10−9 | 1.07 | 3.04 × 10−9 | 1.01 | 9.24 × 10−1 | 1.14 (0.39) | 1.04 × 10−4 |
| rs6787808:C/T | 3:49079105 | 3p21.31# | QRICH1 | 1.08 | 1.20 × 10−9 | 1.08 | 1.08 × 10−9 | 1.01 | 1.79 × 10−2 | 1.04 (0.04) | 8.47 × 10−8 |
| rs228614:A/G | 4:103578637 | 4q24* | MANBA | 0.94 | 1.71 × 10−9 | 0.94 | 1.85 × 10−9 | 0.99 | 2.05 × 10−2 | 0.87 (0.53) | 1.26 × 10−6 |
| rs12198665:G/T | 6:39240796 | 6p21.2* | KCNK17 | 0.94 | 3.35 × 10−8 | 0.94 | 3.09 × 10−8 | 1.00 | 9.18 × 10−1 | 0.84 (0.30) | 7.99 × 10−8 |
| rs17780429:A/G | 6:138222588 | 6q23.3* | TNFAIP3 | 0.91 | 2.24 × 10−10 | 0.91 | 1.28 × 10−10 | 1.00 | 1.23 × 10−1 | 0.77 (0.85) | 1.16 × 10−7 |
| rs3757387:C/T | 7:128576086 | 7q32.1* | IRF5 | 1.08 | 2.19 × 10−14 | 1.08 | 1.54 × 10−14 | 1.01 | 1.39 × 10−8 | 1.13 (0.46) | 3.01 × 10−4 |
| rs7911680:C/A | 10:101293468 | 10q24.2* | NKX2-3 | 0.94 | 1.33 × 10−8 | 0.94 | 1.23 × 10−8 | 0.99 | 1.20 × 10−3 | 0.88 (0.49) | 1.28 × 10−5 |
| rs79390277:C/A | 16:68942590 | 16q22.1* | TANGO6 | 1.15 | 1.69 × 10−8 | 1.15 | 1.39 × 10−8 | 1.00 | 7.53 × 10−1 | 1.35 (0.05) | 1.86 × 10−6 |
Gene, the nearest genes ±200 kb of the genomic risk SNP (reference NCBI build37); A1/A2, effect allele/other allele; EAF effect allele frequency; OR odds ratio; P, P-value; MTAG_PSC, MTAG-identified PSC-specific association modeled in the discovery phase (6 GWAS in total); MTAG_PSC⊥IBD, MTAG-identified PSC-specific association modeled in the sensitivity analysis (5 GWAS in total); MTAG_PSC_R, MTAG-identified PSC-specific association modeled in replicate phase (6 GWAS in total); GWAS_PSC, single-disease PSC GWAS; ORs are calculated from a joint meta-analysis using MTAG; Two-sided raw P-values are reported; *, the new risk loci identified in this study; #, the new lead variant from a previously reported locus with r2 < 0.1.
Fig. 3. Manhattan plots and quantile-quantile plots for the single-trait GWAS and the multitrait GWAS of PSC.
a, c PSC single-trait GWAS (Ji et al., 2017, PMID:27992413; GWAS_PSC). b, d MTAG-identified PSC-specific GWAS against five immune-mediated disorders, CD, UC, IBD, lupus, and PBC (MTAG_PSC). The x-axis represents chromosomal location, and the y-axis represents the −log10(P-value). The cytoband annotations for the newly and previously identified loci are in purple (b) and gray (a), respectively. The solid lines in red and the dotted lines in blue indicate the genome-wide significant two-sided unadjusted P-value of and the suggestive significant two-sided unadjusted P-value of , respectively. P-values are derived using multitrait analysis of GWAS in the discovery study.
A newly identified association of an intronic variant, rs228614, was detected in MANBA on 4q24 (PMTAG_PSC = 1.71 × 10−9). Associations at MANBA have been previously reported for multiple sclerosis29, primary biliary cirrhosis30, psoriasis31, numerous hematologic traits32–35, asthma36,37, and major depressive disorders38. Another association at rs17780429 between TNFAIP3 and LINC02528 on 6q23.3 showed a strong genetic signal (PMTAG_PSC = 2.24 × 10−10) and many associations at TNFAIP3 have been observed in autoimmune-related diseases39–42 and multiple blood-cell traits34,43. We found a new intergenic variant, rs3757387 between KCP and IRF5 on 7q32.1 (PMTAG_PSC = 2.19 × 10−14). rs3757387 has been previously reported for significant associations with systematic lupus erythematosus among diverse populations44 and in a single population19,45, rheumatoid arthritis in multiple populations46,47, and Sjögren’s syndrome48. An NKX2-3 intronic variant, rs791168 on 10q24.2, was associated with PSC susceptibility and has been reported in many autoimmune-related and blood-cell traits13 (PMTAG_PSC = 1.33 × 10−8). LocusZoom regional plots of genome-wide associations for these newly identified loci are provided in Supplementary Fig. 1.
To assess whether our MTAG results were robust to strong genetic correlation and clinical relevance among IBD, UC, and CD, we repeated our MTAG analysis only including PSC, CD, UC, lupus, and PBC (MTAG_PSC⊥IBD) as a sensitivity analysis. The results from the MTAG-identified PSC-specific model excluding IBD were very similar to those from the inclusion model (MTAG_PSC) (Table 2 and Supplementary Fig. 2).
To replicate the new MTAG-identified PSC-specific associations, we downloaded GWAS summary statistics from FinnGen14 and GWAS Catalog13, which are independent GWAS from the discovery phase (Supplementary Data 2). Since we were interested in replicating eight new associations (seven newly identified loci and one independent significant variant in the reported locus), we did not apply multiple testing corrections. We replicated four PSC-specific associations (MTAG_PSC_R), rs6787808 in QRICH1 (PMTAG_PSC_R = 1.79 × 10−2), rs228614 in MANBA (PMTAG_PSC_R = 2.05 × 10−2), rs3757387 between KCP and IRF5 (PMTAG_PSC_R = 1.39 × 10−8), and rs791168 in NKX2-3 (PMTAG_PSC_R = 1.20 × 10−3) at the nominal significance level of 0.05 (Table 2 and Supplementary Fig. 2).
Fine-mapping and functional annotation nominates candidate variants within MTAG-identified loci
To pinpoint genomic risk loci and prioritize susceptibility variants underlying the MTAG-identified PSC-specific GWAS associations by functional annotation, positional, expression quantitative trait loci (eQTL), and chromatin interaction mappings, we exploited Functional Mapping and Annotation of GWAS (FUMA GWAS)49 using LD structure based on European ancestry of 1000 Genome Project phase 3 (“Methods”). We prioritized 406 unique genes from 20 PSC susceptibility loci reported in Supplementary Data 5 that functionally mapped and annotated using MTAG-identified GWAS, of which 109 genes were identified by position mapping of deleterious coding variants with the combined annotation-dependent depletion (CADD) score (posMapMaxCADD ≥ 12.37)50 (Supplementary Data 6). Out of 406 prioritized genes, 48 genes (12%) were detected by eQTL associated with the expression of 14 immune cell types51. In the chromatin interaction mapping, 278 genes (69%) are mapped to the regions interacting with the promoter of the listed gene and of which 90 genes (32%) were found in the liver tissue in which the chromatin interaction is observed (Supplementary Data 6). Either chromatin interactions or eQTLs within PSC risk loci (Supplementary Data 5) were shown on chromosomes 2, 3, 4, 6, 7, 11, 16, 19, and 21, respectively (Supplementary Figs. 3). Then, 158 genes were mapped by both eQTLs and chromatin interactions including IRF5 and TNPO3 genes (in red in Supplementary Fig. 3e) on the 7q32.1. In addition, we explored immune-related genes among 406 PSC-specific susceptibility genes prioritized by position, eQTL, or chromatin interaction mapping using InnateDB52 (“Methods”). We found five immune-related genes including IRF5 and SMO (7q32.1) and HAS3, SNTB2, and VPS4A (16q22.1), within newly identified loci that have not been previously reported (Supplementary Data 7).
To functionally characterize the 329 independent significant variants within 20 genomic risk loci generated from FUMA, we performed an integrated variant functional annotation approach using the Functional Annotation of Variants Online Resource (FAVOR) platform53–55 and the multidimensional annotation class integrative estimator56,57 (MACIE). Out of 168 noncoding genes, we observed 14 more likely deleterious genes (CADD PHRED ≥ 12.37) and 8 and 6 genes on promoter and permissive enhancer sites, respectively. (Supplementary Data 8 and 9). Of the SNPs investigated with MACIE, we find 80 variants with a regulatory class prediction greater than 95%. That is, these variants are highly likely to tangibly affect the behavior of certain gene expressions, most often nearby genes. We find four variants with a conserved class prediction greater than 95%, and three of these variants also possess a regulatory prediction greater than 95%. That is, the four variants are highly likely to belong to the class of evolutionarily conserved variants that are found in many living beings. The full predictions for each SNP can be found in Supplementary Data 10.
To nominate the candidate causal variants from each locus for further functional analysis, we implemented fine-mapping of MTAG-identified loci using FINEMAP58 and surveyed credible sets of plausible causal variants based on posterior inclusion probability (PIP). We then applied Conditional and Joint Analysis (COJO) using GCTA59 to refine independent associations with prioritized risk loci. Based on the single-SNP PIP with each locus, we identified 32 variants falling into the 95% credible set across eight MTAG-identified GWAS loci (Supplementary Data 11). We found that eight MTAG-identified PSC risk loci explained at least two independent association signals; 2p16.1 locus harboring PUS10, with five independent variants, 3p21.31 (QRICH1) and 4q24 (MANBA) with five variants, 6p21.2 (KCNK17) with two variants, 6q23.3 (TNFAIP3) and 7q32.1 (IRF5) with five variants, 10q24.2 (NKX2-3) with three variants and 16q22.1 (TANGO6) with two variants, respectively. There is no additional genome-wide significant association from GCTA-COJO analysis at the genome-wide significant level of 5 × 10−8.
eQTL-based colocalization prioritizes PSC susceptibility genes from the MTAG-identified new loci
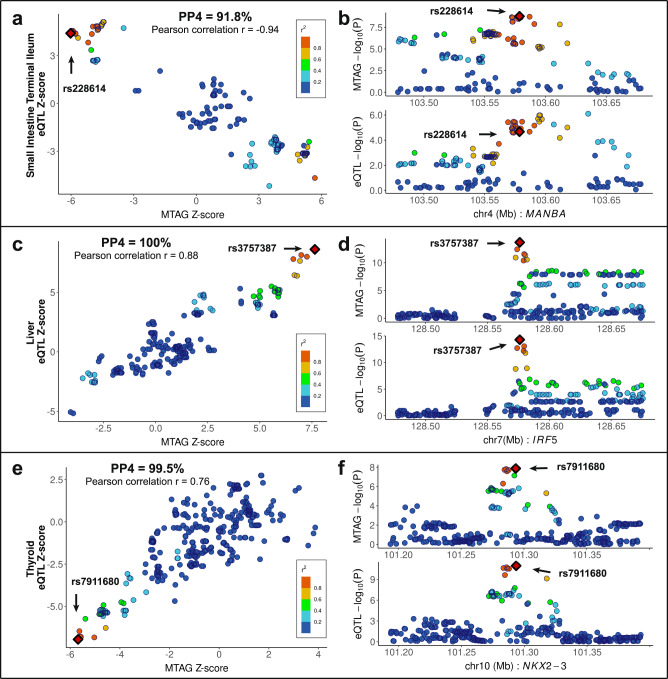
We carried out eQTL-based colocalization analysis to identify allelic-specific effects on gene expression and to examine colocalization of association signals from new MTAG-identified PSC risk-associated findings using eQTL summary statistics of 49 tissue types from GTEx v8. Among seven MTAG-identified new risk loci (2p16.1, 4q24, 6p21.2, 6q23.3, 7q32.1, 10q24.2, 16q22.1), colocalization nominated three candidate genes, MANBA at 4q24, IRF5 at 7q32.1, and NKX2-3 at 10q24.2, contributing to PSC risk (Supplementary Data 12). Notably, a newly MTAG-identified locus, IRF5, displayed the highest posterior probability scores indicating that both PSC and each of the 30 tissues are associated and share a single functional variant (PP4 > 0.80) using coloc60 package (Fig. 4, Supplementary Fig. 4, Supplementary Data 12).
Fig. 4. Functional validation of the MTAG-identified PSC-specific candidate genes.
a, c, e eQTL signals in GTEx v8 small intestine terminal ileum (n = 174) for MANBA (a), liver (n = 208) for IRF5 (c), and thyroid (n = 574) for NKX2-3 (e) colocalize with those of the MTAG-identified PSC-specific GWAS by coloc (posterior probability for the same causal variant shared between MTAG-identified GWAS and a tissue-specific eQTL (PP4) = 0.918 for rs228614, PP4 = 1.00 for rs3757387, and PP4 = 0.995 for rs7911680), respectively. Pearson correlation (r) is shown between the Z-score of eQTL (y-axis) and MTAG_PSC (x-axis). Variants are color-coded based on the LD r2 (1000 Genomes phase 3, EUR) with the candidate variants (red dot in a diamond shape). Variants with imputation quality scores >0.6 were plotted in this region. b, d, f Regional association plots of eQTL and MTAG_PSC within ±100kb of rs228614 (b), rs3757387 (d), and rs7911680 (f) are displayed.
We selected 406 prioritized genes to detect relevant groups of related genes involved in the regulation of specific biological pathways. Using STRING Protein–Protein Interaction (PPI) networks61, these candidate genes are highly enriched for protein–protein interactions (P < 1.00 × 10−16), with enrichment at false discovery rate (FDR) < 0.05 of the following pathways: immune receptor activity (FDR = 3.84 × 10−2), beta-2-microglobulin binding (1.10 × 10−2), cytokine-mediated signaling pathway (1.58 × 10−13), interferon-gamma-mediated signaling pathway (1.13 × 10−11), T-cell receptor signaling pathway(2.21 × 10−11), immune response-activating cell surface receptor signaling pathway (2.65 × 10−9), interleukin-7-mediated signaling pathway (9.21 × 10−9), TNFR2 noncanonical NF-kB pathway (7.90 × 10−3), Th17 cell differentiation (2.63 × 10−6), and Th1 and Th2 cell differentiation (1.94 × 10−5) (Supplementary Data 13, Supplementary Fig. 5). For comparison, we implemented enrichment analysis using the Database for Annotation, Visualization, and Integrated Discovery (DAVID) Bioinformatics Resources62,63 on the same candidate 406 genes. We observed T-cell receptor signaling pathway (FDR = 5.82 × 10−7), antigen processing and presentation (8.18 × 10−15), immunoglobulin production involved in immunoglobulin mediated immune response (6.30 × 10−14), cytokine Signaling in Immune system (3.48 × 0−5), interferon Signaling (2.62 × 10−9), and interferon alpha/beta signaling (6.60 × 10−4) (Supplementary Data 14).
In addition, we scrutinized the PPI network associated with each gene prioritized from newly MTAG-identified loci and found three genes (MANBA, IRF5, and NKX2-3) to be highly enriched for PPI at FDR < 0.05. Each prioritized gene of MANBA, IRF5, and NKX2-3 reported a PPI P-value of 5.16 × 10−14, 1.00 × 10−16, and 1.13 × 10−9, respectively. We observed B and T-cell receptors, chemokine, C-type lectin receptor, cytosolic DNA-sensing, HIF-1, IL-17, JAK-STAT, MAPK, metabolic, NF-kappa B, NOD-like receptor, PD-L1 expression and PD-1 checkpoint in cancer, RIG-I-like receptor, th1-th2 cell differentiation, th17 cell differentiation, thyroid hormone, TNF, and toll-like receptor signaling pathways in the KEGG pathways at FDR < 0.05 using STRING PPI networks (Supplementary Data 15, Supplementary Fig. 6).
Network-based proximity predicts drug-PSC associations for drug repurposing
Although there is no medication proven to treat PSC, ursodeoxycholic acid (UDCA) is a recommended treatment increasing the bile flow as well as preventing damage to liver cells. While UDCA is used to treat PBC and radiolucent gallstones with a functioning gall bladder, it does not appear to improve survival or reduce the need for liver transplant in PSC patients. From in silico network-based proximity analysis64, we estimated the shortest distance (d) between drug targets and PSC candidate genes (Supplementary Data 16, “Methods”) and the relative proximity measure(z) capturing the statistical significance of distance between drug and disease protein derived from a permutation test (Table 3, Supplementary Data 17, Supplementary information). The more negative the relative proximity between drug and disease, the closer the genetic relationship between them64. We identified many agents at the relative proximity threshold of −0.15, implying potential therapeutic effects on PSC. The top-ranked drugs suggestive for PSC included denileukin diftitox, interleukin-2-alpha binder used for cutaneous T-cell lymphoma (z = −5.443); vitamin E (z = −1.918); MLN0415, a small molecule IKK2 inhibitor downregulating the expression of a number of inflammatory proteins (z = −1.648). The proximity of UDCA showed 0.170 on PSC indicating that it may not be a genetically promising candidate drug for PSC. The FUMA platform facilitates gene mapping to the DrugBank database via GENE2FUNC reported in Supplementary Data 18. While network-based proximity predicts drug association based on the distance between drug targets and candidate genes, FUMA provides the gene table mapped to the drug database based on the prioritized genes by different mapping methods such as position, eQTL, and chromatin interaction.
Table 3.
Network-based in silico drug repurposing on PSC
| DrugBank id | Drug Name | Description | Indication | z | p |
|---|---|---|---|---|---|
| DB00004 | Denileukin diftitox | CD25-directed cytotoxin | Cutaneous T-cell lymphoma | −5.443 | 2.63 × 10−8 |
| DB05299 | Keyhole limpet hemocyanin* | Immune modulator | Bladder cancer, solid tumors | −4.020 | 2.91 × 10−5 |
| DB06584 | TG4010* | Cancer vaccine expressing MUC1/IL2 | Breast cancer, renal cell carcinoma, prostate cancer, non-small cell lung cancer. | −3.561 | 1.85 × 10−4 |
| DB05304 | Girentuximab* | Chimeric monoclonal antibody targeting carbonic anhydrase IX | Renal cell carcinoma | −3.526 | 2.11 × 10−4 |
| DB06083 | Tapinarof* | Aryl hydrocarbon receptor-modulating agent | Plaque psoriasis | −3.013 | 1.29 × 10−3 |
| DB04901 | Galiximab* | Anti-CD80 monoclonal antibody | Non-Hodgkin’s lymphoma, psoriasis | −2.740 | 3.07 × 10−3 |
| DB00163 | Vitamin E | Vitamin | Dietary supplement | −1.918 | 0.0276 |
| DB06421 | Declopramide* | DNA repair inhibitors | Colorectal cancer, inflammatory bowel disease. | −1.593 | 0.0556 |
| DB06362 | Becatecarin* | DNA intercalating agent, topoisomerase I and II inhibitor | Gastric cancer, adenocarcinoma of unknown origin, gall bladder or pancreatic tumors, breast cancer, renal cell cancer, colorectal cancer | −1.542 | 0.0615 |
| DB05022 | Amonafide* | DNA intercalating agent, topoisomerase II inhibitor | Breast cancer, ovarian cancer, prostate cancer, acute myeloid leukemia | −1.542 | 0.0616 |
| DB08934 | Sofosbuvir | N55B RNA polymerase inhibitor | Chronic hepatitis C infection | −1.342 | 0.0898 |
| DB05127 | ANA971* | Toll-like receptor 7 | Chronic hepatitis C infection | −1.338 | 0.0904 |
| DB04860 | Isatoribine* | Toll-like receptor 7 | Chronic hepatitis C infection | −1.338 | 0.0904 |
| DB11094 | Vitamin D | Vitamin | Osteoporosis prevention, Vitamin D insufficiency/deficiency, hypoparathyroidism, refractory rickets, familial hypophosphatemia | −0.515 | 0.3033 |
| DB01586 | Ursodeoxycholic acid | Gallstone dissolution agent | Gallstones, PBC | 0.170 | 0.5673 |
DrugBank id, DrugBank database identifier; Drug Name, drug name; Indication, current drug-treatment; z, relative proximity between PSC candidate genes and relevant drug of genes; p, P-value of the relative proximity. *Asterisk indicates not FDA-approved agent.
Discussion
We leveraged publicly available GWAS summary statistics to investigate the shared genetic architecture of PSC with a variety of clinical and epidemiological traits and to identify additional PSC-risk loci. We first scrutinized the patterns of genomic overlap between PSC and numerous phenotypes using LDSR. Cross-trait LDSR estimated the genetic correlation between traits to gain insights into common etiologies15,16. We identified significant phenotypic associations between different polygenic traits and PSC. The findings of this study enabled us to confirm previously well-established comorbid conditions and to identify polygenic traits for further study. Complementary approaches such as MTAG, which is a joint association analysis of genetically correlated traits, helped us to discover new susceptibility variants influencing PSC. In addition, LDSR-identified polygenic traits indicating a high correlation with PSC can be applied in Mendelian randomization analysis to unveil further causal relationships between PSC and the traits of interest.
We observed a significant positive correlation between the genomic architecture of each autoimmune-related disease and that of PSC using LDSR. In several genetic studies, PSC is driven by shared and distinct genetic determinants compared to immune-mediated diseases7,19,27,65,66. The shared structure of the genetic susceptibility to PSC is notably overlapped with immune-mediated disorders such as CD, IBD, lupus, PBC, and UC27, which have well-established associations with PSC67. In addition, these immune-mediated disorders showed large proportions of phenotypic variance explained by all common SNPs in this study.
Several epidemiological studies have reported inverse associations between smoking and PSC risk7,23,24,68,69. Our study found a strongly protective genetic correlation between the genomic architecture of smoking status modeled in former smokers versus current smokers and that of PSC, suggesting that the genetic contribution of current smoking is associated with a decreased risk of PSC compared to that of former smoking. Although it failed to meet the Bonferroni-corrected significance level of 3.73 × 10−4, the smoking cessation trait modeled in former smokers versus current smokers26 showed a consistent association with PSC implying that the genetic contribution of current smoking is associated with a decreased risk of PSC compared to that of former smoking23. The smoking initiation trait modeled in never-smokers versus ever-smokers26 showed a significant negative association with PSC suggesting that PSC risk among current and former smokers is significantly lower than that among never-smokers23. Smoking promotes chronic epithelial and tissue injury through chronic airway inflammation70,71 and the most common causes of chronic inflammation include immune-mediated disorders which could potentially contribute to PSC development. Therefore, the shared association of PSC with smoking behaviors makes disentangling such effects challenging.
Applying an orthogonal genomics-driven method complementing clinical epidemiologic research of PSC, we confirmed a link between PSC risk and elevated BMI and diabetes7,72–75. However, clinical studies have shown inconsistent associations between cardiovascular disease and PSC75,76. Pairwise genetic correlation between PSC and cardiovascular risk demonstrated a negative association at the nominal significance level of 0.05. We also identified several suggestive polygenic traits for which the pairwise genetic correlations were nominally significant at P < 0.05. We observed a nominally significant inverse genetic correlation between PSC and several serologic biomarkers including C-reactive protein, glucose, HbA1c, red blood cell distribution width, reticulocyte count, and triglycerides while alkaline phosphatase and sex hormone binding globulin were positively correlated with PSC risk. These findings through LDSR show good concordance with previous clinical and genetic epidemiologic studies7,75,77.
Implementing MTAG, we discovered seven new susceptibility loci that have not been previously reported in GWAS_PSC and, of these, we replicated three lead associations in other GWAS independent from the discovery phase. Two of the new MTAG PSC loci, MANBA on 4q24 and IRF5 on 7q32.1 were previously shown to be associated with several hematology-related traits and immune-mediated disorders20,44–48. The previously identified phenotypes have also been reported in PSC. In addition, we prioritized candidate genes for PSC susceptibility through MTAG and inferred biological pathways identified through eQTL-colocalization analyses. PPI networks showed that candidate genes were often part of biological pathways involving metabolic processes and immune response.
Recently, the identification of targets for drug repurposing (repositioning) using genome-wide approaches has become popular20. In this study, we implemented network-based in silico drug efficacy screening to predict agents potentially suitable for repurposing to PSC. Generally, UDCA is recommended for the treatment of cholestatic liver diseases including PSC, but it does not show any effect on the progression and survival of PSC patients78. Interestingly, the proximity of UDCA shows that it may not be a genetically promising candidate drug for PSC. In clinical trials in the U.S., UDCA did not improve the management of PSC79 and its use has been discouraged in the U.S. providers80, indicating a correct prediction of our drug screening analysis. The identified candidate drugs are relevant to lymphoma (Denileukin diftitox, Galiximab), various cancers (Keyhole limpet hemocyanin, TG4010, Girentuximab, Amonafide), psoriasis and psoriatic disorders (Tapinarof), vitamin E, IBD (Declopramide), metabolic disorders (Girentuximab), rheumatoid arthritis, liver cancer (Becatecarin), chronic hepatitis C virus (HCV) (Sofosbuvir, ANA971, Isatoribine). Poch et al. reported a single-cell atlas of intrahepatic T-cell landscape in PSC81. The top-ranked drug, Denileukin diftitox, which is involved in the regulation of immune tolerance by controlling regulatory T-cells activity, could be a candidate agent for further study of pharmacological effect.
Integration, harmonization, and optimization of the existing large-scale GWAS datasets have become a popular analytical strategy to identify new genetic associations. However, access to individual-level GWAS datasets remains limited due to data use restrictions. Although LDSR can quantify the shared genetic architecture of traits having undergone GWAS analysis without requiring GWAS individual-level data, it assumes an absence of population stratification in the underlying summary statistics of the tested traits and necessitates the incorporation of GWAS data from populations expected to have homogeneous genetic structure. Furthermore, GWAS summary statistics with small sample sizes or low SNP-heritability are not amenable to LDSR. One caveat of implementing LDSR is that nonsignificant associations could be due to limited statistical power, rather than a lack of shared heritability, as cross-trait LDSR requires larger sample sizes of GWAS summary-level data to achieve equivalent standard error compared to methods that use individual-level data15. Another limitation of LDSR is that the analysis includes only common genetic variants with MAF >0.01 and therefore fails to capture shared heritability due to underlying rare variants between PSC and multiple polygenic traits.
MTAG21 can substantially improve statistical power for detecting susceptibility loci relative to separate GWAS for the traits tested and allows potential sample overlap in numerous trait-specific summary statistics from large-scale cohort GWAS. However, replication or validation analysis is recommended to assess the credibility of each SNP association when MTAG is applied to low-powered GWAS or to GWAS that are considerably heterogeneous in statistical power. Since MTAG uses overlapping SNPs across all GWAS summary statistics, combining summary statistics with a smaller number of SNPs with those with a larger number of SNPs can reduce statistical power.
In conclusion, our findings from LDSR confirm the associations between immune-mediated disorders and PSC, and epidemiological parameters associated with PSC susceptibility. We also identified and replicated the newly MTAG-identified PSC risk loci and through eQTL-colocalization analysis helped to prioritize candidate genes for PSC susceptibility. This study emphasizes the strong evidence that exists for the shared genetic underpinning among immune-mediated diseases. While PSC GWAS have identified a few risk-associated variants, the function and identity of the causal variants are not fully explored. To address the impact of PSC risk-associated variants in the immune system and within less-well-established noncoding regions, we highlighted several in silico functional approaches to map and prioritize the variants identified. Furthermore, we exploited an immune-related gene database for deciphering how PSC risk-associated variants may alter immune networks. We also utilized the integrative functional annotations platform to functionally characterize the prioritized genes including both coding and noncoding genes, which provide numerous information on variant and indel functional annotations. Since there is no medication proven to treat PSC, we predicted many potential agents at the relative proximity capturing the statistically significant relationship between a potential drug and putative disease-associated proteins. We further carried out gene mapping to the drug database with the broad range of genes prioritized by position, eQTL, and chromatin interaction mapping. These analytical pipelines, which utilize activity maps of noncoding regions help us pinpoint their role in specific cell types. These findings can provide better functional insight into the genetic etiology of PSC susceptibility and improve our understanding of how PSC risk-associated variants alter the immune system. Finally, future studies using causal inference approaches such as Mendelian randomization or genetic instrumental variable methods may help to elucidate the causal relationship between the risk of PSC and other potential candidate phenotypes to reveal surrogate biomarkers that may improve the predictive power of polygenic risk scores.
Methods
Ethics statement
All participants for each GWAS were recruited following protocols approved by the local Ethics Committee/Institutional Review Boards. Written informed consent was obtained from each participant included in the study. All methods were performed in accordance with the ethical guidelines of the 1975 Declaration of Helsinki.
GWAS summary statistics and imputation
We obtained the GWAS summary statistics for PSC2 and 134 clinical and epidemiological traits from existing data resources12,13. More details are shown in Supplementary Data 1 and Supplementary Information. We restricted the study populations to individuals of European ancestry to align with the homogeneous ancestry background of participants in GWAS of the traits tested in our downstream analyses. To enhance adequate statistical power in this study, GWAS summary statistics were imputed using the SSimp software82 (v.0.5.6; https://github.com/zkutalik/ssimp_software) when the number of SNPs in a trait was considerably smaller compared to that in other traits, thus becoming less informative. Detailed methods are provided in Supplementary Information.
Analyses of multitrait GWAS
We estimated SNP-heritability (h2) on the observed scale and pairwise genetic correlation (r_g) between multiple polygenic traits using LDSR8–11,15,16 (v1.0.1; https://github.com/bulik/ldsc). We conservatively set the test-wise significance level using Bonferroni correction to be 0.05/134, adjusting for the analysis of 134 polygenic traits in total (Supplementary Information).
The commonly used conventional GWAS approach is to analyze the univariate association test for a single trait/phenotype. This does not permit leveraging of genetic information from other polygenic traits. Integrating associations from other traits highly correlated with PSC can improve the statistical power to identify new polygenic variants21,83–85. We conducted MTAG (v1.0.8; https://github.com/JonJala/mtag) combining PSC with immune-mediated disorders selected by h2 > 0.20 and |r_g| > 0.20. MTAG was modeled for PSC versus five polygenic autoimmune-related traits: CD, UC, IBD, lupus, and PBC (MTAG_PSC). Additionally, we performed a sensitivity analysis excluding IBD (⊥IBD) from the MTAG analysis (MTAG_PSC⊥IBD) since IBD is the umbrella term mainly comprising of medical conditions under which both CD and UC fall86. The sensitivity analysis included only five autoimmune-related diseases; PSC, CD, UC, lupus, and PBC.
To replicate MTAG-identified PSC risk-associated new loci, we implemented MTAG (MTAG_PSC_R) using PSC (FinnGen phenocode:K11_CHOLANGI), CD (K11_CD_NOUC), UC (K11_UC_NOCD), IBD (K11_IBD), and lupus (M13_SLE) from FinnGen repository14, and PBC87 from GWAS catalog, which are independent of those in the discovery phase. Details are reported in Supplementary Data 2.
Characterization of genomic risk loci using FUMA
We mapped the genomic regions of associations by the most significant variants using FUMA GWAS49 (v1.4.1; https://fuma.ctglab.nl/) platform computing LD structure, annotating functions to SNPs, and prioritizing candidate genes from MTAG-derived summary statistics49. To define genomic risk loci for MTAG-identified PSC susceptibility, we used linkage disequilibrium structure based on the European ancestry of the 1000 Genome Project phase 3. Genomic risk loci and the subsets of significant SNPs within each locus were identified using the SNP2GENE function applying the default thresholds: (1) independent significant SNPs, defined as P < 5 × 10−8 and independent from each other at r2 ≥ 0.6 (2) lead SNPs, defined as independently significant SNPs and independent from each other at r2 ≥ 0.1; (3) genomic risk loci, defined by merging lead SNPs within physically overlapped LD blocks and all SNPs in linkage disequilibrium of r2 ≥ 0.6 with one of the independent SNPs. Prioritized susceptibility variants from MTAG GWAS were mapped by positional, eQTL, and chromatin interaction mappings using the FUMA SNP2GENE function with default settings. Finally, FUMA maps the prioritized genes given by the SNP2GENE function to the drug database (DrugBank88) via the GENE2FUNC function in the FUMA platform. The gene table mapped to the DrugBank database provides gene information and the relevant DrugBank IDs that can be found at https://go.drugbank.com/drugs with the details.
Functional annotation within immune-related genes using InnateDB Innate Immunity Genes
We examined 406 prioritized genes to nominate innate immune genes associated with PSC using 7476 genes involved in innate immune responses from the InnateDB52 portal. InnateDB provides the manually-curated list of genes and signaling responses involved in human innate immunity from publicly available databases including the Immunology Database and Analysis Portal (ImmPort) system, Immunogenetic Related Information Source (IRIS), MAPK/NFKB Network, and Immunome Database. The details can be found elsewhere at https://www.innatedb.com/redirect.do?go=resourcesGeneLists.
Integrative multi-omic annotation analysis
We annotated the 406 prioritized genes using FAVOR platform53–55 (v2.0; https://favor.genohub.org/) which is an open-access variant functional annotation portal for whole WGS/WES data. FAVOR provides functional annotation information of 8,812,917,339 SNVs across the human genome and 79,997898 indels from the Trans-Omics for Precision Medicine (TOPMed) BROVO variant set (Build GRCh38) based on a collection of databases such as variant category, evidence of chromatin, protein function, conservation, and Clinvar information. The details have been described elsewhere55.
Annotation-informed function prediction
We utilized the multidimensional annotation class integrative estimator56,57 (MACIE, https://github.com/ryanrsun/lungCancerMACIE/tree/master/MACIE_pipeline) to analyze functional annotation data and understand the possible mechanistic roles of individual SNPs. For each variant, MACIE utilizes a generalized linear mixed model that specifies annotation values as outcomes and unobserved latent functional classes as predictors. The posterior probabilities of these unobserved classes are then calculated for each SNP to estimate the probabilities of possessing certain functions. The calculation proceeds through an expectation-maximization (EM) algorithm until convergence. The final posterior expected value of a class is taken as the MACIE prediction. Specifically, we applied MACIE with two latent classes, (1) regulatory class informed by 28 annotations such as H3K27Ac levels and (2) conserved class informed by eight phylogenetic conservational algorithms. Predictions were only made for noncoding variants.
Fine-mapping and gene-based enrichment analyses
We implemented FINEMAP58 (v1.4.1; http://www.christianbenner.com) to survey credible sets of plausible causal variants based on the posterior inclusion probability (PIP). We carried out the FINEMAP package with the options “--sss” to specify the “fine-mapping with shotgun stochastic search” and “--n-causal-snps 5” to set the maximum number of causal variants allowed within a locus to 5. We performed Conditional and Joint analysis using GCTA59 (v1.9.4; https://cnsgenomics.com/software/gcta/) to select independent association signals within the prioritized risk loci with the option “--cojo-cond”.
The Genotype-Tissue Expression (GTEx_v8)89 database consists of data from 49 normal tissues from 838 donors (Supplementary Data 5, Supplementary information). Colocalization between the seven MTAG_PSC associations within the newly identified loci and eQTL signals was calculated using the coloc package (v5.1.0; https://cran.r-project.org/web/packages/coloc/)60. We focused on the colocalizations when coloc suggested a plausible posterior probability that both PSC and a tissue from GTEx_v8 are associated and share a single functional variant (PP4 > 0.80).
We utilized the STRING Database61 (v11.5; https://string-db.org/cgi/input?sessionId=bmwWOuutn8ZR) to explore the functional enrichment of protein–protein interaction (PPI) networks and to scrutinize the enrichment of various pathways among the prioritized genes (proteins). In addition, we surveyed the DAVID Bioinformatics Resources62,90 (v6.8; https://david.ncifcrf.gov/) to look for enrichment of various functional annotations on the 416 prioritized genes after excluding 9 overlapped genes from 19 newly MTAG-identified and previously reported PSC risk-associated genes and 406 genes mapped from position mapping, eQTL mapping, and chromatin interaction mapping provided from FUMA.
Network-based proximity between drugs and disease-identified proteins for drug repurposing
Drug–disease proximity measures, distance (d), and the corresponding relative proximity (z), quantifying the network-based relationship between drugs and proteins encoded by genes associated with the disease while correcting for the known biases of the interactome64, were estimated (Supplementary Information). To elucidate the effectiveness of proximity as an unbiased measure of drug–disease relatedness, we defined a drug to be proximal to a disease when the closest proximity, z ≤ −0.15, and not proximal otherwise64. We downloaded detailed drug data with comprehensive drug target information from the DrugBank database (v5.1.9, released 2022-01-04)88.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Supplementary information
Description of Additional Supplementary Files
Acknowledgements
We thank all individuals who have contributed their samples and clinical data for the PSC study, and we also thank the international PSC study group for sharing GWAS summary statistics of PSC. We want to acknowledge the participants and investigators of the FinnGen study. The Genotype-Tissue Expression (GTEx) Project was supported by the Common Fund of the Office of the Director of the National Institutes of Health, and by NCI, NHGRI, NHLBI, NIDA, NIMH, and NINDS. The data used for the analyses described in this manuscript were obtained from the GTEx Portal on 10/25/2021. Our study was supported by NIH/NCI under award P50 CA210964, by the Cholangiocarcinoma Foundation, and by PSC Partners Seeking a Cure to L.R.R.. C.I.A. is a Research Scholar of the Cancer Prevention Research Interest of Texas (CPRIT) award RR170048. J.Ra. was partially supported by NHLBI under award K25 HL152006 and by Artificial Intelligence/Machine Learning Consortium to Advance Health Equity and Researcher Diversity (AIM-AHEAD) award OD032581-01S1.
Author contributions
Y.H., J.B., and C.I.A. conceived and designed the study; Y.H. prepared and curated data; Y.H. and J.B. carried out the analyses and wrote the first draft of the manuscript; R.S. performed multi-omic annotation analysis; J.Y.R. assisted the description of results from drug repositioning analysis; C.Z., H.J.C., H.L., S.W.K., J.Ra., V.R.S., M.A.C., M.M.H., K.A.M., and L.R.R., C.I.A. contributed to interpretation of the results; T.F., D.E., A.B., S.M.R., A.F., T.H.K., K.N.L., and IPSCSG provided the summary statistics of PSC GWAS; H.J.C. and K.A.S. provided the summary statistics of PBC GWAS; Y.H., J.B., and C.I.A. supervised the study; all authors provided critical feedback and revised the manuscript for important intellectual content.
Peer review
Peer review information
Nature Communications thanks the anonymous reviewers for their contribution to the peer review of this work. Peer reviewer reports are available.
Data availability
The summary statistics of PSC from MTAG are publicly available at https://github.com/biomedicaldatascience/PSC_MTAG. The GWAS summary-level data analyzed in this study are available in the NHGRI-EBI GWAS Catalog [https://www.ebi.ac.uk/gwas/] and the MRC IEU OpenGWAS database [https://gwas.mrcieu.ac.uk/] for previously published GWAS summary statistics, Neale’s lab repository for UK Biobank GWAS summary statistics [https://github.com/Nealelab/UK_Biobank_GWAS], and FinnGen repository for Finnish Biobank GWAS summary statistics r6 [https://finngen.gitbook.io/documentation/v/r6/data-download]. The accessible links and reference information for the GWAS summary-level data (mapped to Genome Assembly GRCh37) used in this study can be found in Supplementary Data 1 and 2. Non-commercial DrugBank datasets (v5.1.9) are available and access can be obtained by the academic license [https://go.drugbank.com/releases/latest]. The data including all variant-gene cis-eQTL associations tested in each tissue (GTEx v8) are available in a requester pays bucket on Google Cloud Platform (GCP) [https://gtexportal.org/home/datasets; https://console.cloud.google.com/storage/browser/gtex-resources]. The immune-related genes can be obtained in the InnateDB portal [https://www.innatedb.com/redirect.do?go=resourcesGeneLists].
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Younghun Han, Jinyoung Byun.
A list of authors and their affiliations appears at the end of the paper.
A full list of members and their affiliations appears in the Supplementary Information.
Contributor Information
Christopher I. Amos, Email: Chris.Amos@bcm.edu
The International PSC Study Group:
Supplementary information
The online version contains supplementary material available at 10.1038/s41467-023-36678-8.
References
- 1.Karlsen TH, Schrumpf E, Boberg KM. Primary sclerosing cholangitis. Best. Pr. Res. Clin. Gastroenterol. 2010;24:655–666. doi: 10.1016/j.bpg.2010.07.005. [DOI] [PubMed] [Google Scholar]
- 2.Ji SG, et al. Genome-wide association study of primary sclerosing cholangitis identifies new risk loci and quantifies the genetic relationship with inflammatory bowel disease. Nat. Genet. 2017;49:269–273. doi: 10.1038/ng.3745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chung BK, Hirschfield GM. Immunogenetics in primary sclerosing cholangitis. Curr. Opin. Gastroenterol. 2017;33:93–98. doi: 10.1097/MOG.0000000000000336. [DOI] [PubMed] [Google Scholar]
- 4.Blechacz B. Cholangiocarcinoma: current knowledge and new developments. Gut Liver. 2017;11:13–26. doi: 10.5009/gnl15568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Melum E, et al. Genome-wide association analysis in primary sclerosing cholangitis identifies two non-HLA susceptibility loci. Nat. Genet. 2011;43:17–19. doi: 10.1038/ng.728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liu JZ, et al. Dense genotyping of immune-related disease regions identifies nine new risk loci for primary sclerosing cholangitis. Nat. Genet. 2013;45:670–675. doi: 10.1038/ng.2616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Andersen IM, et al. Effects of coffee consumption, smoking, and hormones on risk for primary sclerosing cholangitis. Clin. Gastroenterol. Hepatol. 2014;12:1019–1028. doi: 10.1016/j.cgh.2013.09.024. [DOI] [PubMed] [Google Scholar]
- 8.Byun J, et al. The shared genetic architectures between lung cancer and multiple polygenic phenotypes in genome-wide association studies. Cancer Epidemiol. Biomark. Prev. 2021;30:1156–1164. doi: 10.1158/1055-9965.EPI-20-1635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pettit RW, et al. The shared genetic architecture between epidemiological and behavioral traits with lung cancer. Sci. Rep. 2021;11:17559. doi: 10.1038/s41598-021-96685-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ostrom QT, et al. Partitioned glioma heritability shows subtype-specific enrichment in immune cells. Neuro Oncol. 2021;23:1304–1314. doi: 10.1093/neuonc/noab072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Byun J, et al. Shared genomic architecture between COVID-19 severity and numerous clinical and physiologic parameters revealed by LD score regression analysis. Sci. Rep. 2022;12:1891. doi: 10.1038/s41598-022-05832-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Elsworth, B. et al. The MRC IEU OpenGWAS data infrastructure. Preprint at bioRxiv. 10.1101/2020.08.10.244293 (2020).
- 13.Buniello A, et al. The NHGRI-EBI GWAS Catalog of published genome-wide association studies, targeted arrays and summary statistics 2019. Nucleic Acids Res. 2019;47:D1005–d1012. doi: 10.1093/nar/gky1120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.FinnGen. Documentation of R6 release, vol. 2022 (2022).
- 15.Bulik-Sullivan B, et al. An atlas of genetic correlations across human diseases and traits. Nat. Genet. 2015;47:1236–1241. doi: 10.1038/ng.3406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bulik-Sullivan BK, et al. LD score regression distinguishes confounding from polygenicity in genome-wide association studies. Nat. Genet. 2015;47:291–295. doi: 10.1038/ng.3211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.van Rheenen W, Peyrot WJ, Schork AJ, Lee SH, Wray NR. Genetic correlations of polygenic disease traits: from theory to practice. Nat. Rev. Genet. 2019;20:567–581. doi: 10.1038/s41576-019-0137-z. [DOI] [PubMed] [Google Scholar]
- 18.de Lange KM, et al. Genome-wide association study implicates immune activation of multiple integrin genes in inflammatory bowel disease. Nat. Genet. 2017;49:256–261. doi: 10.1038/ng.3760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bentham J, et al. Genetic association analyses implicate aberrant regulation of innate and adaptive immunity genes in the pathogenesis of systemic lupus erythematosus. Nat. Genet. 2015;47:1457–1464. doi: 10.1038/ng.3434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cordell HJ, et al. An international genome-wide meta-analysis of primary biliary cholangitis: novel risk loci and candidate drugs. J. Hepatol. 2021;75:572–581. doi: 10.1016/j.jhep.2021.04.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Turley P, et al. Multi-trait analysis of genome-wide association summary statistics using MTAG. Nat. Genet. 2018;50:229–237. doi: 10.1038/s41588-017-0009-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Karlsson Linner R, et al. Genome-wide association analyses of risk tolerance and risky behaviors in over 1 million individuals identify hundreds of loci and shared genetic influences. Nat. Genet. 2019;51:245–257. doi: 10.1038/s41588-018-0309-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wijarnpreecha K, et al. Association between smoking and risk of primary sclerosing cholangitis: a systematic review and meta-analysis. U. Eur. Gastroenterol. J. 2018;6:500–508. doi: 10.1177/2050640618761703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mitchell SA, et al. Cigarette smoking, appendectomy, and tonsillectomy as risk factors for the development of primary sclerosing cholangitis: a case control study. Gut. 2002;51:567–573. doi: 10.1136/gut.51.4.567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Loh PR, Kichaev G, Gazal S, Schoech AP, Price AL. Mixed-model association for biobank-scale datasets. Nat. Genet. 2018;50:906–908. doi: 10.1038/s41588-018-0144-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liu M, et al. Association studies of up to 1.2 million individuals yield new insights into the genetic etiology of tobacco and alcohol use. Nat. Genet. 2019;51:237–244. doi: 10.1038/s41588-018-0307-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ellinghaus D, et al. Analysis of five chronic inflammatory diseases identifies 27 new associations and highlights disease-specific patterns at shared loci. Nat. Genet. 2016;48:510–518. doi: 10.1038/ng.3528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Qiu F, et al. A genome-wide association study identifies six novel risk loci for primary biliary cholangitis. Nat. Commun. 2017;8:14828. doi: 10.1038/ncomms14828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.International Multiple Sclerosis Genetics Consortium et al. Genetic risk and a primary role for cell-mediated immune mechanisms in multiple sclerosis. Nature. 2011;476:214–219. doi: 10.1038/nature10251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cordell HJ, et al. International genome-wide meta-analysis identifies new primary biliary cirrhosis risk loci and targetable pathogenic pathways. Nat. Commun. 2015;6:8019. doi: 10.1038/ncomms9019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zuo X, et al. Whole-exome SNP array identifies 15 new susceptibility loci for psoriasis. Nat. Commun. 2015;6:6793. doi: 10.1038/ncomms7793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chen VL, et al. Genome-wide association study of serum liver enzymes implicates diverse metabolic and liver pathology. Nat. Commun. 2021;12:816. doi: 10.1038/s41467-020-20870-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Emilsson V, et al. Co-regulatory networks of human serum proteins link genetics to disease. Science. 2018;361:769–773. doi: 10.1126/science.aaq1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sinnott-Armstrong N, et al. Genetics of 35 blood and urine biomarkers in the UK Biobank. Nat. Genet. 2021;53:185–194. doi: 10.1038/s41588-020-00757-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kachuri L, et al. Genetic determinants of blood-cell traits influence susceptibility to childhood acute lymphoblastic leukemia. Am. J. Hum. Genet. 2021;108:1823–1835. doi: 10.1016/j.ajhg.2021.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhu Z, et al. Shared genetics of asthma and mental health disorders: a large-scale genome-wide cross-trait analysis. Eur. Respir. J. 2019;54:1901507. doi: 10.1183/13993003.01507-2019. [DOI] [PubMed] [Google Scholar]
- 37.Johansson A, Rask-Andersen M, Karlsson T, Ek WE. Genome-wide association analysis of 350 000 Caucasians from the UK Biobank identifies novel loci for asthma, hay fever and eczema. Hum. Mol. Genet. 2019;28:4022–4041. doi: 10.1093/hmg/ddz175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Peyrot WJ, Price AL. Identifying loci with different allele frequencies among cases of eight psychiatric disorders using CC-GWAS. Nat. Genet. 2021;53:445–454. doi: 10.1038/s41588-021-00787-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Morris DL, et al. Genome-wide association meta-analysis in Chinese and European individuals identifies ten new loci associated with systemic lupus erythematosus. Nat. Genet. 2016;48:940–946. doi: 10.1038/ng.3603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Baurecht H, et al. Genome-wide comparative analysis of atopic dermatitis and psoriasis gives insight into opposing genetic mechanisms. Am. J. Hum. Genet. 2015;96:104–120. doi: 10.1016/j.ajhg.2014.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Patrick MT, et al. Causal relationship and shared genetic loci between psoriasis and type 2 diabetes through trans-disease meta-analysis. J. Invest Dermatol. 2021;141:1493–1502. doi: 10.1016/j.jid.2020.11.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Laufer VA, et al. Genetic influences on susceptibility to rheumatoid arthritis in African-Americans. Hum. Mol. Genet. 2019;28:858–874. doi: 10.1093/hmg/ddy395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chen MH, et al. Trans-ethnic and ancestry-specific blood-cell genetics in 746,667 individuals from 5 global populations. Cell. 2020;182:1198–1213.e14. doi: 10.1016/j.cell.2020.06.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Langefeld CD, et al. Transancestral mapping and genetic load in systemic lupus erythematosus. Nat. Commun. 2017;8:16021. doi: 10.1038/ncomms16021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yin X, et al. Meta-analysis of 208370 East Asians identifies 113 susceptibility loci for systemic lupus erythematosus. Ann. Rheum. Dis. 2021;80:632–640. doi: 10.1136/annrheumdis-2020-219209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ishigaki K, et al. Large-scale genome-wide association study in a Japanese population identifies novel susceptibility loci across different diseases. Nat. Genet. 2020;52:669–679. doi: 10.1038/s41588-020-0640-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ha E, Bae SC, Kim K. Large-scale meta-analysis across East Asian and European populations updated genetic architecture and variant-driven biology of rheumatoid arthritis, identifying 11 novel susceptibility loci. Ann. Rheum. Dis. 2021;80:558–565. doi: 10.1136/annrheumdis-2020-219065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lessard CJ, et al. Variants at multiple loci implicated in both innate and adaptive immune responses are associated with Sjogren’s syndrome. Nat. Genet. 2013;45:1284–1292. doi: 10.1038/ng.2792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Watanabe K, Taskesen E, van Bochoven A, Posthuma D. Functional mapping and annotation of genetic associations with FUMA. Nat. Commun. 2017;8:1826. doi: 10.1038/s41467-017-01261-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kircher M, et al. A general framework for estimating the relative pathogenicity of human genetic variants. Nat. Genet. 2014;46:310–315. doi: 10.1038/ng.2892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Schmiedel BJ, et al. Impact of genetic polymorphisms on human immune cell gene expression. Cell. 2018;175:1701–1715.e16. doi: 10.1016/j.cell.2018.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Breuer K, et al. InnateDB: systems biology of innate immunity and beyond-recent updates and continuing curation. Nucleic Acids Res. 2013;41:D1228–D1233. doi: 10.1093/nar/gks1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Li X, et al. Dynamic incorporation of multiple in silico functional annotations empowers rare variant association analysis of large whole-genome sequencing studies at scale. Nat. Genet. 2020;52:969–983. doi: 10.1038/s41588-020-0676-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Li, Z. et al. A framework for detecting noncoding rare variant associations of large-scale whole-genome sequencing studies. Nat. Methods19, 1599–1611 (2021). [DOI] [PMC free article] [PubMed]
- 55.Zhou, H. et al. FAVOR: functional annotation of variants online resource and annotator for variation across the human genome. Nucleic Acids Res. 6, D1300–D1311 (2022). [DOI] [PMC free article] [PubMed]
- 56.Sun R, et al. Integration of multiomic annotation data to prioritize and characterize inflammation and immune-related risk variants in squamous cell lung cancer. Genet. Epidemiol. 2021;45:99–114. doi: 10.1002/gepi.22358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Li X, et al. A multi-dimensional integrative scoring framework for predicting functional variants in the human genome. Am. J. Hum. Genet. 2022;109:446–456. doi: 10.1016/j.ajhg.2022.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Benner C, et al. FINEMAP: efficient variable selection using summary data from genome-wide association studies. Bioinformatics. 2016;32:1493–1501. doi: 10.1093/bioinformatics/btw018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yang J, Lee SH, Goddard ME, Visscher PM. GCTA: a tool for genome-wide complex trait analysis. Am. J. Hum. Genet. 2011;88:76–82. doi: 10.1016/j.ajhg.2010.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wallace C. Eliciting priors and relaxing the single causal variant assumption in colocalisation analyses. PLoS Genet. 2020;16:e1008720. doi: 10.1371/journal.pgen.1008720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Szklarczyk D, et al. STRING v11: protein–protein association networks with increased coverage, supporting functional discovery in genome-wide experimental datasets. Nucleic Acids Res. 2019;47:D607–D613. doi: 10.1093/nar/gky1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Huang da W, Sherman BT, Lempicki RA. Systematic and integrative analysis of large gene lists using DAVID bioinformatics resources. Nat. Protoc. 2009;4:44–57. doi: 10.1038/nprot.2008.211. [DOI] [PubMed] [Google Scholar]
- 63.Sherman BT, et al. DAVID: a web server for functional enrichment analysis and functional annotation of gene lists (2021 update) Nucleic Acids Res. 2022;50:W216–W221. doi: 10.1093/nar/gkac194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Guney E, Menche J, Vidal M, Barabasi AL. Network-based in silico drug efficacy screening. Nat. Commun. 2016;7:10331. doi: 10.1038/ncomms10331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Denoth L, et al. Modulation of the mucosa-associated microbiome linked to the PTPN2 risk gene in patients with primary sclerosing cholangitis and ulcerative colitis. Microorganisms. 2021;9:1752. doi: 10.3390/microorganisms9081752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ellinghaus D, et al. Genome-wide association analysis in primary sclerosing cholangitis and ulcerative colitis identifies risk loci at GPR35 and TCF4. Hepatology. 2013;58:1074–1083. doi: 10.1002/hep.25977. [DOI] [PubMed] [Google Scholar]
- 67.Aranake-Chrisinger J, Dassopoulos T, Yan Y, Nalbantoglu I. Primary sclerosing cholangitis associated colitis: characterization of clinical, histologic features, and their associations with liver transplantation. World J. Gastroenterol. 2020;26:4126–4139. doi: 10.3748/wjg.v26.i28.4126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Bastida G, Beltrán B. Ulcerative colitis in smokers, non-smokers and ex-smokers. World J. Gastroenterol. 2011;17:2740–2747. doi: 10.3748/wjg.v17.i22.2740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Aune D, Sen A, Norat T, Riboli E, Folseraas T. Primary sclerosing cholangitis and the risk of cancer, cardiovascular disease, and all-cause mortality: a systematic review and meta-analysis of cohort studies. Sci. Rep. 2021;11:10646. doi: 10.1038/s41598-021-90175-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lee J, Taneja V, Vassallo R. Cigarette smoking and inflammation: cellular and molecular mechanisms. J. Dent. Res. 2012;91:142–149. doi: 10.1177/0022034511421200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Rodríguez, É. G. & Morán, G. A. G. in Autoimmunity: From Bench to Bedside (eds Anaya J. M. et al.) Ch. 8 (El Rosario University Press, 2013). https://www.ncbi.nlm.nih.gov/books/NBK459469/. [PubMed]
- 72.Poonawala A, Nair SP, Thuluvath PJ. Prevalence of obesity and diabetes in patients with cryptogenic cirrhosis: a case-control study. Hepatology. 2000;32:689–692. doi: 10.1053/jhep.2000.17894. [DOI] [PubMed] [Google Scholar]
- 73.Tana MM, et al. The significance of autoantibody changes over time in primary biliary cirrhosis. Am. J. Clin. Pathol. 2015;144:601–606. doi: 10.1309/AJCPQV4A7QAEEFEV. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Reyes JL, et al. Neutralization of IL-15 abrogates experimental immune-mediated cholangitis in diet-induced obese mice. Sci. Rep. 2018;8:3127. doi: 10.1038/s41598-018-21112-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ludvigsson JF, Bergquist A, Montgomery SM, Bahmanyar S. Risk of diabetes and cardiovascular disease in patients with primary sclerosing cholangitis. J. Hepatol. 2014;60:802–808. doi: 10.1016/j.jhep.2013.11.017. [DOI] [PubMed] [Google Scholar]
- 76.Suraweera D, Fanous C, Jimenez M, Tong MJ, Saab S. Risk of cardiovascular events in patients with primary biliary cholangitis—systematic review. J. Clin. Transl. Hepatol. 2018;6:119–126. doi: 10.14218/JCTH.2017.00064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.de Vries EM, et al. Alkaline phosphatase at diagnosis of primary sclerosing cholangitis and 1 year later: evaluation of prognostic value. Liver Int. 2016;36:1867–1875. doi: 10.1111/liv.13110. [DOI] [PubMed] [Google Scholar]
- 78.Iravani S, et al. An update on treatment options for primary sclerosing cholangitis. Gastroenterol. Hepatol. Bed Bench. 2020;13:115–124. [PMC free article] [PubMed] [Google Scholar]
- 79.Rahimpour S, et al. A triple blinded, randomized, placebo-controlled clinical trial to evaluate the efficacy and safety of oral vancomycin in primary sclerosing cholangitis: a pilot study. J. Gastrointestin Liver Dis. 2016;25:457–464. doi: 10.15403/jgld.2014.1121.254.rah. [DOI] [PubMed] [Google Scholar]
- 80.Chapman R, et al. Diagnosis and management of primary sclerosing cholangitis. Hepatology. 2010;51:660–678. doi: 10.1002/hep.23294. [DOI] [PubMed] [Google Scholar]
- 81.Poch T, et al. Single-cell atlas of hepatic T cells reveals expansion of liver-resident naive-like CD4(+) T cells in primary sclerosing cholangitis. J. Hepatol. 2021;75:414–423. doi: 10.1016/j.jhep.2021.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Rueger S, McDaid A, Kutalik Z. Evaluation and application of summary statistic imputation to discover new height-associated loci. PLoS Genet. 2018;14:e1007371. doi: 10.1371/journal.pgen.1007371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Emdin CA, et al. Association of genetic variation with cirrhosis: a multi-trait genome-wide association and gene-environment interaction study. Gastroenterology. 2021;160:1620–1633.e13. doi: 10.1053/j.gastro.2020.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Ong, J. S. et al. Multitrait genetic association analysis identifies 50 new risk loci for gastro-oesophageal reflux, seven new loci for Barrett’s oesophagus and provides insights into clinical heterogeneity in reflux diagnosis. Gut71, 1053–1061 (2022). [DOI] [PMC free article] [PubMed]
- 85.Liu L, et al. Twelve new genomic loci associated with bone mineral density. Front Endocrinol. (Lausanne) 2020;11:243. doi: 10.3389/fendo.2020.00243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Chandan JS, Thomas T. The impact of inflammatory bowel disease on oral health. Br. Dent. J. 2017;222:549–553. doi: 10.1038/sj.bdj.2017.318. [DOI] [PubMed] [Google Scholar]
- 87.Jiang L, Zheng Z, Fang H, Yang J. A generalized linear mixed model association tool for biobank-scale data. Nat. Genet. 2021;53:1616–1621. doi: 10.1038/s41588-021-00954-4. [DOI] [PubMed] [Google Scholar]
- 88.Wishart DS, et al. DrugBank 5.0: a major update to the DrugBank database for 2018. Nucleic Acids Res. 2018;46:D1074–D1082. doi: 10.1093/nar/gkx1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Consortium G. The Genotype-Tissue Expression (GTEx) project. Nat. Genet. 2013;45:580–585. doi: 10.1038/ng.2653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Dennis G, Jr., et al. DAVID: Database for Annotation, Visualization, and Integrated Discovery. Genome Biol. 2003;4:P3. doi: 10.1186/gb-2003-4-5-p3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Description of Additional Supplementary Files
Data Availability Statement
The summary statistics of PSC from MTAG are publicly available at https://github.com/biomedicaldatascience/PSC_MTAG. The GWAS summary-level data analyzed in this study are available in the NHGRI-EBI GWAS Catalog [https://www.ebi.ac.uk/gwas/] and the MRC IEU OpenGWAS database [https://gwas.mrcieu.ac.uk/] for previously published GWAS summary statistics, Neale’s lab repository for UK Biobank GWAS summary statistics [https://github.com/Nealelab/UK_Biobank_GWAS], and FinnGen repository for Finnish Biobank GWAS summary statistics r6 [https://finngen.gitbook.io/documentation/v/r6/data-download]. The accessible links and reference information for the GWAS summary-level data (mapped to Genome Assembly GRCh37) used in this study can be found in Supplementary Data 1 and 2. Non-commercial DrugBank datasets (v5.1.9) are available and access can be obtained by the academic license [https://go.drugbank.com/releases/latest]. The data including all variant-gene cis-eQTL associations tested in each tissue (GTEx v8) are available in a requester pays bucket on Google Cloud Platform (GCP) [https://gtexportal.org/home/datasets; https://console.cloud.google.com/storage/browser/gtex-resources]. The immune-related genes can be obtained in the InnateDB portal [https://www.innatedb.com/redirect.do?go=resourcesGeneLists].