INTRODUCTION
Scope of the Problem
In recent years, there has been increased attention towards the importance of sleep and its essential role in athletic performance, cognition, health and mental well-being. Many of these studies examine “elite athletes” (e.g., Olympians, professionals, and/or players recruited to national and varsity teams) and some focus on athletes in general. Despite all the efforts expended, by any definition, numerous athletes still experience inadequate sleep (Lucidi, Lombardo, Russo, Devoto & Violani, 2007; Samuels., 2008; Swinbourne, Gill, Vaile & Smart., 2016). Compared to non-athletes, athletes tend to sleep less on average (Leeder, Glaister, Pizzoferro, Dawson & Pedlar, 2012). Furthermore, athletes’ quality of sleep appears to be lower than their non-athlete peers (Bleyer, Barbosa, Andrade, Teixeira & Felden., 2015; Tsunoda & al., 2015). Additionally, it has been suggested that certain types of athletes are more prone to developing sleep difficulties such as sleep apnea. For example, according to George, Kab & Levy (2003) and Albuquerque & al., (2010), National Football League (NFL) players have higher rates of obstructive sleep apnea, which has tremendous deleterious impacts on health and daytime sleepiness. Notably, there is increasing evidence that poor sleep is a good predictor for injuries and more importantly, concussion (Raikes, Athey, Alfonso-Miller, Killgore & Grandner, 2019).
Position Statements
Recently, the International Olympic Committee (IOC), has addressed, for the first time, sleep as a major contributor to athletic performance and as a fundamental feature of athlete mental health (Reardon & al., 2019). In addition, the National Collegiate Athletics Association (NCAA) included sleep health as part of their published mental health best practices (Kroshus & al., 2019), as well as their more recently published official position statement on the importance of sleep health for student athletes (Kroshus & al., 2019). These position statements from the NCAA and IOC represent the increased awareness of the importance of sleep health among organizations of elite athletes. Both of these documents were the result of a literature review, delphi process of iterative consensus-building, and subsequent revision, following exhaustive reviews of available literature.
The IOC mental health document (Reardon, et al., 2019) considers sleep health in terms of sufficiency (i.e., at least 7 hours for adults), proper circadian alignment, good overall perceived sleep quality, and absence of sleep disorders including insomnia disorder and sleep apnea. The document recommends that these dimensions of sleep be considered important for mental health, as well as physical health and functioning. Further, the document recommends education, proper assessment and screening, and treatment using evidence-based strategies – given the consideration that some treatments may impact safety and/or performance.
The NCAA document focused on sleep as an important aspect of health, performance, and mental functioning in collegiate student athletes (Kroshus et a., 2019). It addresses many identified barriers to sleep, including academic, athletic, and social time demands. Similarly, this document defines sleep health in terms of duration (at least 7 hours in adults), timing, overall quality, and absence of disorders including insomnia and sleep apnea. Particular attention is also paid to the role of tiredness, fatigue, and/or sleepiness as consequences of sleep loss and/or disturbances. The NCAA makes 5 recommendations in this document:
Conduct a collegiate athlete time demands survey annually.
Recommendation 2: Ensure that consumer sleep technology, if used, is compliant with Health Information Portability and Accountability Act (HIPAA) and Family Educational Rights and Privacy Act (FERPA) laws.
Recommendation 3: Incorporate sleep screening into the preparticipation exam.
Recommendation 4: Provide collegiate athletes with evidence-based sleep education that includes: (1) information on sleep best practices; (2) information about the role of sleep in optimising athletic and academic performance and overall well-being; and (3) strategies for addressing sleep barriers.
Recommendation 5: Provide coaches with evidence-based sleep education that includes: (1) information on sleep best practices; (2) information about the role of sleep in optimising athletic and academic performance and overall well-being; and (3) strategies to help optimise collegiate athlete sleep.
These efforts specifically recommend that sleep-related education should be provided, sleep difficulties and disorders should be routinely assessed and screened for, and sleep health promotion should be a goal of athletics programs.
EPIDEMIOLOGY OF SLEEP DISTURBANCES IN ATHLETES
Prevalence of Insufficient Sleep
Insufficient sleep duration can impact metabolism, endocrine function, athletic and cognitive outcomes, and, furthermore, increase perceived effort during exercise (Chase & al., 2017; Spiegel, Leproult & Van Cauter, 1999; Spiegel & al., 2004). When athletes are compared to non-athletes, they tend to sleep less and less efficiently. Leeder, Glaister, Pizzoferro, Dawson & Pedlar, (2012) compared the habits of 47 elite athletes over a four-day period to a group of non-athletes, using actigraphy; age of participants were not reported, but groups were matched for age and gender. On average, athletes slept 6.55 ± 0.43 vs 7.11 ± 0.25 hours in the non-athletes (p = 0.27). However, they did report lower sleep efficiency (80.6 ± 6.4 vs 88.7 ± 3.6., p < 0.05), higher time spent in bed (8:07 ± 0:20 vs 8:36 ± 0:.53., p < 0.05), wake after sleep onset (0:50 ± 0:16 vs 1:17 ± 0:31., p < 0.05), sleep onset latency (5.0 ± 2.5 vs 18.2 ± 16.5., p < 0.05) and sleep fragmentation (29.8 ± 9.0 vs 36.0 ± 12.4., p < 0.05) in athletes. Furthermore, Lastella, Roach, Halson & Sargent (2015) reported insufficient sleep duration among athletes, with 6.8 hours on average. Sargent, Lastella, Halson & Roach (2014) also reported that over 14 nights assessed with actigraphy, athletes recorded an average of 6.5 hours of sleep per night.
Taken together, these studies have investigated a total of 241 elite athletes and documented actigraphically-determined sleep durations of about 6 and a half hours in most cases. Recently, Mah and colleagues (2018) indicated that 39.1% of athletes reported insufficient sleep (< 7 hours) by self-report. And among a large sample of collegiate athletes in the US (N=8,312), Turner and colleagues reported that the mean number of nights per week that athletes did not think they got enough sleep was 3.8 (Turner et al 2019).
Prevalence of poor sleep quality
Hoshikawa, Uchida & Hirano (2018) investigated the quality of sleep of 817 Japanese elites’ athletes with the Pittsburgh Sleep Quality Index (PSQI), showing that 28% of the participants exhibit a score > 5, suggesting poor quality of sleep. Mah and colleagues (2018) reported that 42.2% of the 629 athletes in that study experienced poor sleep quality, also using the PSQI. In 2019, Turner and colleagues examined data from N=8,312 collegiate student athletes and found that 19.8% reported that “sleep difficulties” were particularly “traumatic or difficult to handle” over the past 12 months and that 21.8% reported extreme difficulty falling asleep at least 3 nights per week (Turner & al., 2019). Bleyer and colleagues reported that 38% of their 452 participants reported poor sleep (Bleyer, Barbosa, Andrade, Teixeira & Felden, 2015). Findings from a study conducted among elite rugby and cricket players (n = 175) showed that 50% of their participants’ PSQI score were > 5, and that 9% scored > 10 (Swinbourne, Gill, Vaile & Smart, 2016). Tsunoda and colleagues (2015) reported the PSQI scores of 14 wheelchair basketball athletes (mean = 5.8 ± 3.0) and compared their results with 103 non-athletes from the general population (mean = 4.51 ± 2.14). Regardless of total sleep time, the wheelchair athletes reported lower sleep quality and lower sleep efficiency than matched non-athletes.
In a cohort of 317 Rio Olympic athletes from eleven different sports, poor sleep quality (as assessed by the PSQI) was prevalent in more than 50% of the athletes following the Olympic Games (Drew & al., 2018). This recapitulates the earlier results with a similar cohort, in which up to 83% of athletes reach the cutoff indicating poor sleep (Drew & al., 2017). Of note, the higher proportion with a score >5 occurred in the leadup to the Olympics and the lower figure was recorded at the Games. Consequently, regardless of the type of sports, these results highlight the prevalence of poor sleep quality among athletes.
Prevalence of Daytime Sleepiness
Few studies have examined the prevalence of general fatigue and/or sleepiness among athletes. Turner and colleagues (2019) reported that 60.9% of collegiate athletes report that they experience feeling “tired, dragged out, or sleepy during the day” at least 3 days per week (as measured by self-report). Furthermore, 32.75% of these collegiate student athletes reported an inability to maintain wakefulness at least 3 times per week (by self-report). Mah and colleagues (2018) reported that 51% of student athletes in their study reported high scores (>=10) on the Epworth Sleepiness Scale. These findings indicate high levels of sleepiness in elite athletes.
Prevalence of circadian preferences and disruption
Data exploring chronotype among the general population suggest that about 25% are morning type, 50% are intermediate types and about 25% are evening types (Fischer, Lombardi, Marucci-Wellman & Roenneberg, 2017). Very few studies have explored the chronotype distribution among athletes. Two studies (Samuels, 2008; Silva & al., 2012) indicated that 51% of athletes were classified as morning types, 40% as intermediate types and only 9% were classified as evening types. One study examined athletes in wheelchairs and the other examined school-age athletes and may not be representative of the elite athlete population. Lastella, Roach, Halson & Sargent (2016) investigated 114 elite athletes emerging from 5 different sports. Their results indicated that 28% were morning types, 65% were intermediate types and only 6% were evening types, supporting previous findings that athletes tend to pursue and excel in sports that match their chronotype (Lastella, Roach, Hurem & Sargent, 2010).
Circadian rhythms can influence variations in performance, depending on the time of day and typical training schedules, which ultimately can affect competitive performance (Drust, Waterhouse, Atkinson, Edwards & Reilly, 2005). When athletes experience disturbances in their environments or routines such as overnight travel, repetitive time zone changes, evening training or late-night competition, endogenous circadian rhythms and normal sleep patterns may be out of synchrony (Beersma & Gordijn, 2007; Reilly & Edwards, 2007). Such disruptions in circadian and sleep patterns can increase homeostatic pressure and thus influence the regulation of emotions, body temperature, circulation of melatonin, and cause a significant increase in sleep latency (Lack & Wright, 2007). The sleep/wake behavior of athletes is often governed by their training schedule (Lastella, Roach, Halson, Martin, West & Sargent, 2015). Therefore, the role of chronotype among athletes may interact with the training schedule and should be considered to optimize training and performance (Drust, Waterhouse, Atkinson, Edwards & Reilly, 2005) and reduce the prevalence of chronobiologic disturbances.
Prevalence of sleep disorders
Insomnia
Gupta, Morgan & Gilchrist (2017) demonstrated that the relation between elite sport participation and insomnia symptomology is poorly systematized. Daytime impairment – a key part of insomnia diagnosis – can reflect a wide variety of experiences including fatigue, emotional fluctuation, and psychomotor and/or neuropsychological performance, which all are important for elite athletes. Given this particular sensitivity to performance impairment and high levels of sleepiness (which is not common in insomnia), there arise some challenges in insomnia assessment among elite athletes. Traditional insomnia models might poorly discriminate insomnia per se in this non-traditional population (Samuels, James, Lawson & Meeuwisse, 2016). The multifaceted demands of elite sport including a high level of training volume (Collette, Kellmann, Ferrauti, Meyer & Pfeiffer, 2018; Sargent, Halson & Roach, 2014), pre-competition anxiety (Erlacher, Ehrlenspiel, Adegbesan & Galal El-Din, 2011; Lastella & al., 2015) circadian challenges (jet lag) (Samuels, 2012) can all predispose and precipitate sleep disturbance, thus leading to or facilitating symptomology of insomnia.
Given the absence of a validated sleep questionnaire specifically for athletes before the creation of the Athlete Sleep Screening Questionnaire (ASSQ) (Bender, Lawson, Werthner & Samuels, 2018), it is difficult to precisely indicate the insomnia prevalence in elite athletes. However, the systematic review conducted by Gupta Morgan & Gilchrist (2017) reported that sleep disturbance complaints range from 13 to 70% of the athletes and that overall, on average, 26% of the athletes significantly scored for insomnia symptoms using the Insomnia Severity Index (ISI) and Pittsburgh Sleep Questionnaire Index (PSQI). It should be noted that notwithstanding the popularity of these two questionnaires, none of them are specifically validated in an elite athlete population. Elite athletes are primarily selected on the basis of physiological predisposition but also psychological attributes (Allen, Greenlees & Jones, 2013). It is possible that personality traits that include a focus on success (e.g., perfectionism) may also predispose an elite athlete to insomnia (Harvey, Gehrman & Espie, 2014). Furthermore, the demands of elite sports, including an elevated frequency, intensity, and volume of activity and scheduling challenges (Sargent, Lastella, Halson & Roach, 2014; Sargent, Halson & Roach, 2014), coupled with pre-competition anxiety (Erlacher, Ehrlenspiel, Adegbesan & Galal El-Din, 2011) and jetlag/travel (Fowler, Duffield, Howle, Waterson & Vaile, 2015; Fowler, Duffield, Lu, Hickmans & Scott, 2016), all these factors may lead an individual toward sleep difficulties. Given that these challenges are uncommon among the general population and the relationship between risk factors and sleep may be fundamentally different in this group (e.g., distribution of muscle mass), tools not specifically validated in athletic populations should be used somewhat cautiously.
Sleep Apnea
The prevalence of sleep apnea may be high in certain type of sports, such as strength, power and high contact sports where athletes often present with a large body mass and neck circumference (Dunican & Eastwood, 2017; Emsellem & Murtagh, 2005; Swinbourne, Gill, Vaile & Smart, 2016). In the National Football League (NFL) and National Hockey League (NHL), two high-speed and contact sports, an elevated body mass index and a large neck circumference are considered protective assets, making athletes less injury-prone (Swinbourne, Gill, Vaile & Smart, 2016). However, these specific body traits, unfortunately, also predispose these athletes to an increased risk of obstructive sleep apnea (OSA) (Ahbab & al., 2013; Emsellem & Murtagh, 2005; Mihaere & al., 2009). Two studies carried out among NFL players illustrated that players with these specific physical traits appeared to have a higher incidence of OSA (George, Kab, Kab, Vila & Levy, 2003; Rice & al., 2010). Additionally, in line with the previous Football studies, Dobrosielski and colleagues (2016) illustrated that approximately 8% of the NCAA-I football players were at risk for OSA. Moreover, in professional hockey players, OSA was present in approximately 10% of athletes (Tuomilehto & al., 2017). It is reported that in most cases, the OSA severity was “mild” but even mild OSA might cause major disturbances in sleep (Jackson, Howard & Barnes, 2011), therefore potentially impacting athletic performance.
Other Disorders
Very few studies have been conducted on Restless Legs Syndrome (RLS) among athletes. Findings from a study assessing a population of runners, indicate prevalence is suggested to be around 13% (Fagundes & al., 2010). Among hockey players, prevalence is suggested to be around 5% (Tuomilehto & al., 2017); Finally, within a sample of rugby players, no participants reported RLS but 12% reported periodic limb movements (PLMs) (Dunican & al., 2019). These three studies have shown that sleep disorders such as RLS and PLMs are relatively common among elite athletes from a variety of sports.
IMPACT OF SLEEP ON PHYSICAL PERFORMANCE
Adverse effects of sleep restriction on athletic performance have been documented for many years, including cardiorespiratory and psychomotor effects, which require sustained and stable performance over time (Edwards & Waterhouse, 2009; Horne & Pettitt, 1984; Martin, 1981; Mougin & al., 1989; Mougin & al., 1991). Mougin (1991) observed 7 participants on a cycle ergometer, in a study that included a 10 minute warmup, then a 20 minute steady exercise corresponding to 75% of the predetermined maximal oxygen consumption, followed by an increased intensity exercise until exhaustion. This was done along with sleep restriction (3 hours of wakefulness in the middle of the night). In this study, physiological demands were significantly higher during the submaximal effort compared to a baseline night (10:30pm to 7:00am), (Mougin & al., 1991). Heart rate was significantly higher when measured after 9 minutes (167.1 ± 2.0 vs 171.3 ± 2.5) and after 20 minutes (176.0 ± 2.6 vs 179.1 ± 2.4). Also, ventilation (141.0 ± 5.7 vs 157.5 ± 6.4) and respiratory frequency (43.0 ± 1.6 vs 44.7 ± 1.7) were both altered following a sleep restriction when compared to baseline. Similarly, these same variables were significantly higher after the sleep restriction condition when performing a graded exercise stress test, until exhaustion, while the volume of maximal oxygen uptake (VO2max) decreased. Lactate accumulation was also greater at the 9th minutes (P < 0.01), at the 20th minutes (P < 0.05) of the steady power exercise and at maximal exercise (P < 0.05) following sleep restriction. These results from Mougin (1991) elegantly demonstrated that following a sleep restriction, physical performances would require a higher physiological demand, ultimately leading the athletes to exhaustion faster than he should have been. However, in a separate study there was no significant change in mean or maximal power in anaerobic tests after a 3:00am bedtime, compared to a 10:30pm bedtime (Mougin et al., 1996). Subsequent studies by Mougin showed that following 4-hours sleep restriction, the maximum work rate developed by the participants was reduced by 15 watts for cyclists in a 30-minute exercise at 75% of maximum power (Mougin et al., 2001). In agreement with some of the previous results, the average and maximum power of an anaerobic test decreases among students (Souissi et al., 2008), football players (Abedelmalek et al., 2013) and judokas (Souissi et al., 2013) following a single 4-hour sleep restriction. The reasoning behind the decrease in resistance to exercise is the alteration of the aerobic pathways (Mougin et al., 1989), or in the perceptual change (impression of a longer effort), since the physiological aspects remain predominantly unchanged (Horne & Pettitt 1984, Martin 1981). Indeed, the increase in perceived effort accompanied by a reduction in generated power supports the theory of neuromuscular fatigue (Abbiss & Laursen, 2005), possibly indicating a combination of central nervous system response and neural theory of sleep (Horne & Pettitt 1984, Stickgold, 2005, Walker & Stickgold 2005).
Other studies have also shown adverse impacts of sleep restriction on athletes’ anaerobic power (Taheri & Arabameri, 2012), tennis serving accuracy (Reyner & Horne, 2013), isometric force (Ben, Latiri, Dogui & Ben, 2017), and cortisol levels (Omisade, Buxton & Rusak, 2010). In addition, the average distance traveled by elite runners decreases (6.224 to 6.037 miles) in a treadmill exercise (30 minutes) at their own pace (Oliver, Costa, Laing, Bilzon & Walsh, 2009). Skein and colleagues (2011) reported lower average sprint times, reduced glycogen concentration in the muscles, decreased strength and activation during an isometric force test following a 30-hour total sleep deprivation with 10 athletes from team sports compared to a normal 8-hours of sleep. Submaximal-effort sports, such as running, might be more likely to be affected by total sleep deprivation than the maximum-effort sports, such as weightlifting, as they require more time, therefore negatively impacting the perception of effort throughout time and based on the higher physiological demand required (Mougin & al., 1991). After sleep restriction, the perception of effort increases exponentially increased completion time of the test (Oliver, Costa, Laing, Bilzon & Walsh, 2009). However, the differences in muscle contraction results (voluntary activation) can probably be explained by the sensitivity and accuracy of the electromyography equipment used. For example, previous studies have probably been limited in this aspect contrary to recent studies due to the technological advancement of equipment (Katirji, 2012; Skein, Duffield, Edge, Short & Muendel, 2011). In summary, although the effects of sleep deprivation on exercise are not completely understood, many converging results imply adverse effects of sleep deprivation on athletic performance.
Moreover, the balance of the energy substrate seems vulnerable to sleep deprivation. For instance, a 30-hour sleep deprivation compared to an 8-hour sleep opportunity, demonstrated the inability of the human body to fully recover (24 hours) muscle glycogen in an athletic population as shown by the muscle glycogen concentration before exercise (310 ± 67 mmol*kg−1 dw vs 209 ± 60 mmol*kg−1 dw) (Skein, Duffield, Edge, Short & Muendel, 2011). Inadequate glucose intake would hinder athletes' ability to compete for extended periods, as glycogen shortage is known to reduce muscle function and athletic stamina (Costill & al., 1988; Le Meur, Duffield & Skein, 2012). Indeed, it seems that a large energy imbalance leads to a deterioration in both aerobic and anaerobic power production when activity is sustained over several days and sleep is reduced (Guezennec, Satabin, Legrand & Bigard, 1994; Hausswirth & al., 2014; Jung & al., 2011; Markwald & al., 2013; Waterhouse, Atkinson, Edwards & Reilly, 2007). Prolonged periods of sleep deprivation are associated with increased sympathetic nervous system activity and decreases in parasympathetic nervous system activity as well as altered spontaneous baroreflex sensitivity during vigilance testing in healthy adults (Zhong & al., 2005). Since disturbances of sympathetic and parasympathetic equilibrium are associated with overtraining (Achten & Jeukendrup, 2003), it is possible that these disturbances of the autonomic nervous system following sleep deprivation may promote the development of a state of overtraining in athletes (Hynynen, Uusitalo, Konttinen & Rusko, 2006; Le Meur, Duffield & Skein, 2012). Despite this, several studies have reported that sleep deprivation has minimal impact on the cardiorespiratory variables during exercise (Azboy & Kaygisiz, 2009; Horne & Pettitt, 1984; Mougin et al., 1996) as oppose to the previous finding of Mougin and colleagues (1991). Differences are probably more attributable to the protocols administered and the exercise mode used (running, cycling, time of exhaustion) throughout these different studies. In addition to these results, there were no significant effects on cardiorespiratory or thermoregulatory function in athletes despite a reduction in the distance run for 30 minutes on a treadmill following sleep deprivation (Oliver, Costa, Laing, Bilzon & Walsh, 2009). Oliver (2009) hypothesized the minimal effects on cardiorespiratory function could be due to the influence of perceived effort during the final stages of prolonged high intensity exercise (described above).
IMPACT OF SLEEP ON INJURY RISK AND RECOVERY
Sleep and concussions
It is estimated that as many as 3.8 million concussions are sustained in the U.S. during competitive sports (Harmon & al., 2013). Regrettably, approximately 50% of concussions may go unreported (Harmon & al., 2013). As many as 1 million student-athletes reported having two or more concussions during a period of twelve months (Depadilla, Miller, Jones, Peterson & Breiding, 2018). A study indicated that 40% of athletes with a concussion reported that their coaches were not aware of their symptoms (Rivara & al., 2014). Moreover, it is suggested that athletes involved in team sports have significantly higher risk for one or more concussion than athletes in individual sports (Depadilla, Miller, Jones, Peterson & Breiding, 2018).
Sleep may play an important role as a risk factor for concussions. Participants were given sleep screening questionnaires and followed over a one-year period. Predictors of incident concussions included clinically moderate to severe insomnia (RR = 3.13, 95% CI: 1.320–7.424, p = 0.015) and excessive daytime sleepiness (RR = 2.856, 95% CI: 0.681–11.977, p = 0.037), in a study of N=190 NCAA athletes (Raikes, Athey, Alfonso-Miller, Killgore & Grandner, 2019), and these risk factors outperformed more traditional risk factors (e.g., high-risk sport, history of concussions) as predictors.
Post-concussion sleep is also important. Recently, a meta-analysis reported that sleep disturbances were reported following a concussion about 50% of the time (Mathias & Alvaro, 2012). The most common sleep disturbances reported following a concussion are daytime sleepiness and insomnia by 50% and 25%, respectively (Verma, Anand & Verma, 2007). In addition, sleep disturbance may be a prominent contributor to exacerbate comorbid features of depression, fatigue and pain following a concussion (Mathias & Alvaro, 2012) and worsen recovery because normal recuperative functions of sleep are altered (Weber, Webb & Killgore, 2013).
A return to baseline cognition and self-reported symptoms are key priorities that could be adopted to ensure player safety (McCrory & al., 2013; McCrory & al., 2017). However, it has been demonstrated that athletes sleeping fewer than 7 hours the previous night of testing would perform worse (McClure, Zuckerman, Kutscher, Gregory & Solomon, 2014). Considering that the decision of allowing a player back to play results from a comparison of pre and post concussion performance, a valid neurocognitive baseline is needed. In that sense, sleep should be monitored throughout the year to obtain an adequate neurocognitive performance and therefore a valid baseline. Moreover, the difference in symptomatic presentation following a concussion is highly divergent between males and females athletes (Brown, Elsass, Miller, Reed & Reneker, 2015). This highlights the existing gap between the type of athletes and the consideration that should be directed toward an individualize baseline assessment to better detect the symptomology of a concussion.
Concussion, regardless of severity, is an injury to the brain, and athletes who are suspected of such an injury should be carefully monitored (Graham & al., 2014; McCrory & al., 2013a). An increase in awareness has directly led to more interest into post-concussion symptoms (Eisenberg, Meehan & Mannix, 2014; Lau, Collins & Lovell, 2011). Research has specifically pointed out that the continuation of poor sleep symptoms following a concussion was a reliable predictor of prolonged recovery (Gosselin & al., 2009; Lau, Collins & Lovell, 2011a; Sufrinko, Howie, Elbin, Collins & Kontos, 2018). Additionally, Kostyun and colleagues (2015) demonstrated that during recovery, adolescents who reported greater sleep disturbance performed worse on neurocognitive testing.
Insufficient sleep as a risk factor for injury
Athletes aim to achieve peak performance for as long as possible, given typically short careers with high stakes. An online study of adolescent students (12 to 18 years old) reported that students sleeping less than 8.1 hours a night were 1.7 times more likely to have had an injury than their peers who slept more than 8.1 hours (Jones, Griffiths, Towers, Claxton & Mellalieu, 2018; Milewski & al., 2014). Furthermore, the same study also indicated that for each additional grade in school, students were 1.4 times more likely to have had an injury. Taken together, insufficient sleep duration may increase the risk of injury. Additionally, the summation of years of (accumulated) sleep debt may play a role in risk injury outcomes.
Nutrition plays a fundamental role in recovery and injury prevention (Drew & al., 2017; Mountjoy & al., 2018; Pyne, Verhagen & Mountjoy, 2014; Smyth, Newman, Waddington, Weissensteiner & Drew, 2019), and nutrition and sleep have a bidirectional relationship (Chaput & Dutil, 2016; Grandner, Jackson, Gerstner & Knutson, 2013; Grandner, Jackson, Gerstner & Knutson, 2014; Halson, 2014; Ordóñez, Oliver, Bastos, Guillén & Domínguez, 2017). There is an association between the number of hours slept and the intake of dietary nutriments categories (Grandner, Jackson, Gerstner & Knutson, 2014). Furthermore, individuals that have a later bedtime, tend to consume a higher percentage of carbohydrates, fat and protein than the average sleepers (Baron, Reid, Van Horn & Zee, 2013). On the other hand, some nutriment categories may have a positive effect on sleep such as tart cherries and kiwis that are believed to reduce the number of awakening and increasing the sleep time (Lin, Tsai, Fang & Liu, 2011). Although nutritional knowledge is assumed to be high among athletes (Heaney, O’Connor, Michael, Gifford & Naughton, 2011) data are sparse on the number of athletes who are following their diet on a regular basis, and this may be impacted by poor sleep, which influences food intake (Shechter, Grandner & St-Onge, 2014).
Adolescents sleeping fewer than 8 hours per night were more likely to sustain an injury (Von Rosen, Frohm, Friden & Heijne, 2017) compared to students sleeping greater than 8-hours. These results are in line with Milewski and colleagues (2014). This is interesting given that the results are replicated in a population of athletes. Additionally, Von Rosen and colleagues (2017) found that the recommended intake of fruits, vegetables and fish was not met for 20%, 39% and 43% of their athletes, respectively. Therefore, the hypothesis of combined effect of poor sleep and a poor nutrition needs to be further explored in order to better understand the mechanisms underlying injuries in athletes. Moreover, lack of sleep and poor sleep quality exacerbate depression and anxiety symptoms (Owens, 2014), which may also increase injury risk. In a study of N=958 athletes, 40.6% experienced an injury of various nature (Li, Moreland, Peek-Asa & Yang, 2017). At preseason, 28.8% of the 958 enrolled athletes in this study reported anxiety symptoms and 21.7% reported depressive symptoms. Those with anxiety symptoms were 2.3 times more likely to have had an injury (Li, Moreland, Peek-Asa & Yang, 2017). Given the strong association between poor sleep, anxiety and depression symptoms (Baglioni & al., 2011; Lee, Buxton, Andel & Almeida, 2019), it can be speculated that insufficient sleep may indirectly lead to an injury.
Insufficient sleep and recovery
Poor sleep quality and sleep deprivation impair brain functions that affect a wide array of cognitive functions (Killgore, 2010), which may directly or indirectly facilitate recovery from mental effort and/or physical injury. Furthermore, sleep deprived individuals might increase their intake of unhealthy foods which ultimately will impair glycogen repletion and protein synthesis (Morselli, Leproult, Balbo & Spiegel, 2010), which are critical for recovery in athletes. Additionally, impaired sleep directly affects growth hormone release and alters cortisol secretion (Mougin & al., 2001), therefore, impacting recovery from exercise and stress. Sleep deprivation also increases proinflammatory cytokines such as interleukin-6 (IL-6 and C-reactive Protein (CRP) level which are pain-facilitating agents (McMahon, Cafferty & Marchand, 2005), ultimately affecting the immune system, and hinders muscle recovery and repair from damages sustained in high intensity training and leads towards an imbalance of the autonomic nervous system (Haack, Sanchez & Mullington, 2007; Haack, Lee, Cohen & Mullington, 2009). Moreover, athletes who feel the need to push the boundaries of their capabilities may tend to develop poor sleep patterns, therefore increasing their chances of illness (i.e., medical symptoms) and this impacted their performance and recovery (Hausswirth & al., 2014).
IMPACT OF SLEEP ON MENTAL AND COGNITIVE PERFORMANCE
Vigilance and reaction time
Sleep restriction has been demonstrated to negatively impact attention and reaction time (Basner & Dinges, 2011; Dinges & al., 1997; Włodarczyk, Jaśkowski & Nowik, 2002). Furthermore, it has been demonstrated that reaction times are adversely impacted following only a one night, complete sleep deprivation (Taheri & Arabameri, 2012).
Sleep extension, conversely, has been shown to improve reaction times by 15% and also improve objective daytime sleepiness (Kamdar, Kaplan, Kezirian & Dement, 2004) in a study of student-athletes. Mah, Mah, Kezirian & Dement, (2011) extended the sleep of a college basketball team during a 5-7 week period. The average total sleep time increased from 7.50 to 10.25 hours of sleep over this period. Student athletes improved their reaction time scores (p <0.001) in morning and evening testing sessions. Given that athletes often experience at least mild sleep restriction (especially during intense periods of training or competition), sleep management becomes a priority to maximize reaction time. Consistent with the findings on sleep extension, there is evidence that we can “bank” sleep in order to optimize vigilance and reaction time (Arnal & al., 2015; Arnal & al., 2016; Rupp, Wesensten, Bliese & Balkin, 2009).
Executive function and decision making
Executive functions are one of the cornerstones to athletic performance (Marchetti & al., 2015; Micai, Kavussanu & Ring, 2015). These include the highest levels of thinking required to engineer a strategy, make a fast decision, demonstrate cognitive flexibility and manage the prioritization of attention. Deep sleep / slow-wave sleep seems to have different restorative functions both at the neurophysiologic and phenomenological level. Indeed, deep sleep appears to have a beneficial impact on the prefrontal cortex which will also have a positive impact on the functions directed by this cerebral region. (Goel, Rao, Durmer & Dinges, 2009; Wilckens, Erickson & Wheeler, 2012). Prioritization or inhibitory control ensures the control of the athlete’s concentration, attention, and thoughts, and suppresses the cognitive and behavioural external and internal distractions (Diamond, 2013; Lehto, Juujärvi, Kooistra & Pulkkinen, 2003). Cognitive flexibility is vital for athletes by ensuring efficiency and adaptation in changing tasks (Diamond, 2013; Kiesel & al., 2010). Adaptation is key in athletics; it prevents athletes from making a bad or a risky decision and this inhibitory control is highly linked to sleep deprivation (Killgore, Balkin & Wesensten, 2006; Rossa, Smith, Allan & Sullivan, 2014).
These studies underscore the deleterious effects of lack of sleep on executive functions. Too little sleep may alter an athlete’s ability to make a good decision versus a risky one in a split second, during the course of a game or event. Caffeine as been suggested as a countermeasure to protect against effects on risk-taking or poor decision-making (Killgore, Kamimori & Balkin, 2011). However, it has been demonstrated that caffeine does not replace a proper night of sleep for these functions (Clark & Landolt, 2017; Drake, Roehrs, Shambroom & Roth, 2013; Dunican & al., 2018; Reyner & Horne, 2013).
Learning and memory
Learning new skills is crucial for every athlete. The roots of memory consolidations are found in sleep (Huber, Ghilardi, Massimini & Tononi, 2004; Maquet, 2001; Stickgold, Hobson, Fosse & Fosse, 2001; Stickgold, 2005). The ability to recall information (Gais, Lucas & Born, 2006) is inevitably of interest for athletes. For example, the NFL requires emphasis on the playbook and the ability to recall complex plays is essential for participation in football. Moreover, learning and improving a motor skill is known to continue 24 hours following training (Karni & al., 1998). In healthy young adults, nonrapid eye movement (NREM) stage 2 (N2), typically represent about 45%-55% of total sleep time (Carskadon & Dement, 2011). It has been demonstrated that the duration of sleep stage 2 (NREM) is strongly correlated with the consolidation of motor skills (Albouy, King, Maquet & Doyon, 2013a; Doyon, Gabitov, Vahdat, Lungu & Boutin, 2018; Walker, Brakefield, Morgan, Hobson & Stickgold, 2002). Arguably, the sleep period following learning a new skill is crucial and it has been shown that sleep restriction can adversely impact the memory consolidation (Curcio, Ferrara & De Gennaro, 2006).
While it is true to a certain point that “practice makes perfect,” the results of several studies indicated that sleep after learning improves performance significantly, relative to sleep deprivation (Albouy & al., 2013b; Ashworth, Hill, Karmiloff-Smith & Dimitriou, 2014; Walker & Stickgold, 2006). So perhaps “sleep makes perfect.” It should also be noted that sleep restriction also negatively impacts the academic performance of student athletes (Huang & al., 2016). 56 students were either assigned to a 5-hours or 9-hours time in bed (TIB) for 14 consecutive days in which participants had to study for the Graduate Record Examination (GRE). Results showed that the sleep-restricted group were significantly impacted for the recall of massed item, which is fundamental in academic success.
Another group of elite athletes, student-athletes, not only need to be prepared for their competition but also for academics. Turner and colleagues found that general sleep difficulty, initial insomnia, daytime tiredness, daytime sleepiness, and insufficient sleep were all associated with decreased academic performance among student-athletes (Turner & al., 2019). It is partially the coach’s responsibility to mentor their student-athletes to be ready for any kind of test, either athletic or academic. Ultimately, assessing sleep on a regular basis, could provide crucial information for the coaching members and the athletes (Okano, Kaczmaryk, Dave, Gabrieli & Grossman, 2019). Furthermore, having a clear idea of how an athlete sleep may help the team medical specialist prevent injuries such as concussion (Raikes, Athey, Alfonso-Miller, Killgore & Grandner, 2019).
Creativity and thinking
Through sleep, the consolidation theory suggests that learning and memory consolidation would benefit creativity (Oudiette & al., 2011). The relationship between sleep and creativity stems from the direct influence of sleep on learning and formation of new concepts, ideas or solutions, and ultimately the genesis of creativity (Marguilho, Jesus, Viseu, Rus & Brandolim, 2014). It was demonstrated that REM sleep can improve creative problem solving (Cai, Mednick, Harrisson, Kanady & Mednick, 2009). REM sleep, according to Cai and colleagues (2009), enhanced creativity for items that are primed before sleep by over 40%. Another study showed that stage 1 sleep was associated with fluency and flexibility and slow wave sleep and REM sleep were associated with originality and global measure of figural creativity (Drago & al., 2011). Furthermore, in a Remote Associates Test (RAT) study, participants were faced with different levels of difficulty and the unsolved problems were re-presented after a period of sufficient sleep, wake or no delay (Sio, Monoghan & Ormerod, 2013). The sleep group solved a greater number of difficult RAT items than the other groups. These findings suggest that sleep facilitates creative thinking for harder problems. Creative problem solving is essential for elite athletes. Every game, every competition, elite athletes are faced with decisions that can either improve or lessen their chance of winning. Therefore, it would be essential to investigate how sleep can enhance problem solving within an environment filled with distractions, coupled with the rapidity of execution which is more typical for elite athletes.
IMPACT OF SLEEP ON MENTAL HEALTH
Sleep and anxiety/stress
Previous studies have pointed out the bidirectional associations between sleep, daily stressors and poor mood states (Lee, Crain, McHale, Almeida & Buxton, 2017; Sin & al., 2017). Moreover, poor sleep quality and short sleep duration were significantly associated with cognitive interferences related to stress the next day such as the experience eof intrusive, unwanted, off-task and potentially ruminated thoughts (Lee, Buxton, Andel & Almeida, 2019). Additionally, associations in the opposite direction were found such as stressful and cognitive interferences throughout the day would lead to an earlier bedtime and earlier wake time (Lee & al, 2019).
Prevalence of anxiety symptoms in adult athletes range from 7.1 to 26% (Gouttebarge, Frings-Dresen & Sluiter, 2015; Gulliver, Griffiths, Mackinnon, Batterham & Stanimirovic, 2015). Student-athletes report higher rates of anxiety, up to 37% (Li, Moreland, Peek-Asa & Yang, 2017; Storch, Storch, Killiany & Roberti, 2005). In a study by Lastella, Lovell and Sargent (2014), 21% of the athletes reported that anxiety was the primary reason for their awakening during the night. Additionally, Savis, Eliot, Gansneder & Rotella, 1997, reported, among student-athletes, a lower sleep quality the night before a competition. Student-athletes reported that the primary reason to their sleep difficulty was anxiety and that this greatly affected their performance the following day (Brassington, 2002; Lee, Buxton, Andel & Almeida, 2019; Walters, 2002). Moreover, Davenne (2009) reported that continuously being in a new sleep environment exacerbated the anxiety, thus negatively impacting sleep and therefore performance.
Athletes not getting sufficient sleep consistently show higher rates of anxiety, therefore leading to an increased difficulty coping with new environmental challenges and stressors, which is a key component to performance for every athlete (Brassington, 2002; Walters, 2002). Further studies are needed to clarify this bidirectional relation in athletes in order to develop appropriate plan of action and adaptative strategy to optimize performance.
INTERVENTIONS AT THE TEAM LEVEL
Promoting a culture of healthy sleep
Prioritizing sleep in athletes’ preparation and recovery routine is not an easy task. There is an omnipresent attitude in our society toward sleep that has been put forward where being able to tolerate insufficient sleep is a sign of mental strength and a “badge of honor” (Adler, 2009; Grandner, 2017). These attitudes may influence young elite athletes who are trying to reach the highest level performance in their respective sports. To counter this, teams can promote a culture of healthy sleep as a performance enhancer. This includes embracing the idea that sleep is essential to athletic performance and recovery and counteract the perception that getting sufficient sleep should produce a feeling of guilt. Several high-profile athletes have now publicly discussed the importance of sleep in their preparation and recovery (Schultz, 2014). Unfortunately, these athletes’ habits are not yet the norm and throughout the literature and sport culture; sleep is not yet a priority among elite athletes and professional team sports, though this may be changing.
Systematically screening for sleep problems
Systematically screening for sleep problems is required in order to understand the scope of the problem, identify areas that need improvement, and identify individuals at risk for sleep problems (Kroshus & al., 2019). Ideally, teams need to screen athletes at the beginning of the season and follow up with prospective sleep assessment. Challenges include integrating sleep assessments into existing programs, decisions about what tools to use, implementing sleep assessment at multiple timepoints, and strategies for assessing sleep disorders. In addition, developing collaborative relationships with sleep providers should be a priority (Grandner & al., 2016). Healthy sleep for student-athletes: A guide for athletics departments and coaches. NCAA Sport Science Institute Newsletter, 4(2).)
To date, only one sleep questionnaire has been validated in athletes; the Athlete Sleep Screening Questionnaire (ASSQ) (Bender, Lawson, Werthner & Samuels, 2018). Another promising tool is the Athlete Sleep Behavioral Questionnaire (ASBQ) (Driller, Mah & Halson, 2018), that mainly addresses poor sleep behavior.
Treating sleep disorders
In order to treat sleep disorders among elite athletes, proper sleep screening is essential. Different types of athletes may be differentially susceptible to certain types of sleep disorders. For example, American football players may have a higher prevalence of sleep apnea due to their physical attributes (George & Kab, 2011; Rogers & al., 2017), and swimmers may experience circadian rhythm problems due to their early practice schedules (Sargent, Halson & Roach, 2014).
Sports medicine teams should be educated on diagnosing and treating sleep disorders and referring to sleep specialists when appropriate (Grandner, 2014), and education about sleep disorders should be provided to both athletes and staff (Kroshus & al., 2019). Furthermore, the sport medicine specialist should also be the provider and the promoter of good sleep behavior and its beneficial effects on athletic and academic performance.
When sleep disorders are identified, appropriate evidence-based treatments should be applied, just as in non-athletes (Kroshus & al., 2019; Reardon & al., 2019), including positive airway pressure therapy and oral appliances for sleep apnea and cognitive behavioral therapy for insomnia. It should be noted, though, that sometimes evidence-based treatments of sleep disorders in athletes can be problematic. For example, sedating medications may be clinically indicated but may impede athletics performance, and some empirically supported treatments may actually be banned substances in sport (Reardon & al., 2019). For this reason, clinical providers may need to be sensitive to these issues and may need to consider whether sedating treatments impair performance or whether stimulating treatments are restricted because they are performance-enhancing.
Managing training and travel schedules
The relationship between training loads, timing, intensity, sleep and performance is likely quite complex and not entirely understood. An increase in training load and training intensity, and decrease in hours of sleep, is associated with increased injury risk (Von Rosen, Frohm, Kottorp, Fridén & Heijne, 2017a). Therefore, training more efficiently may be preferable to training longer or harder. This would be more preferable to the accumulation of training load without a profitable recovery, accompanied with a decrease in performance and the need for an extended period of recovery (Halson & Jeukendrup, 2004; Meeusen & al., 2013).
CONCLUSIONS AND FUTURE DIRECTIONS
Sleep health is an important consideration for athletic performance. Athletes are at high risk of insufficient sleep duration (i.e., less than 7–8 hours per night), poor sleep quality (e.g., difficulty initiating or maintaining sleep, or other sleep difficulties), daytime sleepiness and fatigue, suboptimal sleep schedules (e.g., too early or late), irregular sleep schedules, and sleep & circadian disorders (especially insomnia and sleep apnea). These issues, individually and in combination likely impact athletic performance via a number of domains. Sleep loss and/or poor sleep quality can impair muscular strength, speed, and other aspects of physical performance. Sleep issues can also increase risk of concussions and other injuries, and impair recovery following injury. Cognitive performance is also impacted in a number of domains, including vigilance, learning and memory, decision-making, and creativity. Sleep also plays important roles in mental health, which is important for not only athletic performance, but the well-being of athletes in general. Figure 1 depicts a summary of these findings. These relationships have begun to be formally incorporated into athletics organizations, with official position statements that address sleep health published by the NCAA and the IOC (Kroshus et al., 2019; Reardon et al., 2019).
Figure 1.
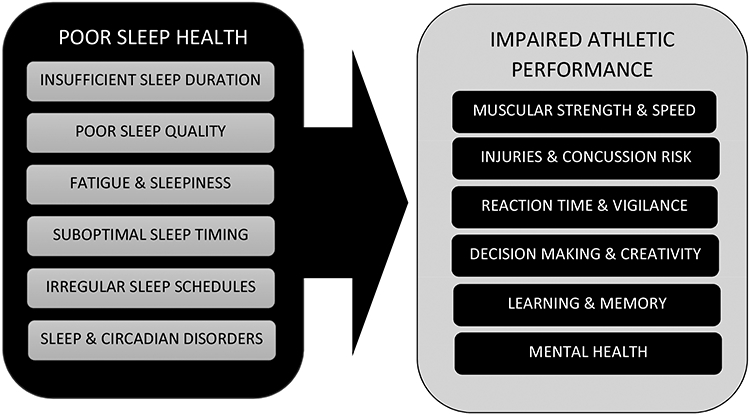
Relationships between Sleep Health and Athletics Performance
Much future research on sleep in athletes is needed. This is because athletes represent a very diverse group of individuals, and most studies in athletes are small, confined to a single team and/or sport, and include inconsistent measurement approaches. In particular, it is still not clear what the best strategy for assessing sleep parameters is in athletes and may likely depend on factors intrinsic to the sport or activity. Additionally, it is not known if standard approaches should be adapted. There is also a lack of trials of sleep interventions thought to positively impact sleep, and still an insufficient number of studies describing how improving sleep can improve performance. Still, there is a large and growing body of evidence that clearly establishes sleep health as an important factor in sport.
Improving sleep in athletes through sleep education at every level of sports organisations has significant implications for health, athletic performance, academic performance and beyond, given the influence each athlete has on the general population as role model. This will not only provide an opportunity to explore a crucial aspect of mental and physical health, but it will also pave the way for new interventions in the area of mental wellbeing. Tracking sleep through questionnaires, wearables and other objective devices is promising but there is still a lot of question marks remaining. It is therefore crucial to develop strategies to mitigate sleep difficulties, not only for physical performance, but also for mental well-being, which will require additional data for a better understanding of the science of sleep.
KEY POINTS.
Insufficient sleep and poor sleep quality are prevalent among athletes, potentially due to time demands, physical demands, and developmental needs.
Sleep disturbances among athletes adversely impacts physical performance, mental performance, injury risk and recovery, medical health, and mental health.
Sleep interventions among athletes have been shown to improve physical strength and speed, cognitive performance and reaction time, mental health, and other domains.
Sport organizations should incorporate sleep health promotion programs at individual, team, and system levels.
SYNOPSIS.
Previous research has characterised the sleep of elite athletes and has attempted to identify factors associated with athletic performance, cognition, health and mental well-being. Sleep is considered a fundamental component to performance optimization among elite athletes. Yet, sleep has only recently been embraced by sport organizations as an important part of the training and recovery process. Not only does sleep play a crucial role in physical and cognitive performance, it is also an important factor in reducing the risk of injury. Yet, there are still many gaps in the literature regarding how sleep can be optimized and what the mechanisms are that link sleep and circadian rhythms to performance and recovery. This article aims to highlight the prevalence of poor sleep, describe its impacts, and address the issue of sport culture surrounding healthy sleep.
DISCLOSURE STATEMENT
Dr. Grandner has received grants from Jazz Pharmaceuticals, Nexalin Technology, and Kemin Foods. He has performed consulting activities for Fitbit, Natrol, Casper, Curaegis, Thrive, Pharmavite, SPV, NightFood, and Merck. This work was supported by R01MD011600 and an Innovation Grant from the National Collegiate Athletics Association.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abbiss CR, & Laursen PB (2005). Models to explain fatigue during prolonged endurance cycling. Sports medicine, 35(10), 865–898. [DOI] [PubMed] [Google Scholar]
- Abedelmalek S, Souissi N, Chtourou H, Denguezli M, Aouichaoui C, Ajina M, … & Tabka Z (2013). Effects of partial sleep deprivation on proinflammatory cytokines, growth hormone, and steroid hormone concentrations during repeated brief sprint interval exercise. Chronobiology international, 30(4), 502–509. [DOI] [PubMed] [Google Scholar]
- Achten J, & Jeukendrup AE (2003). Heart rate monitoring. Sports medicine, 33(7), 517–538. [DOI] [PubMed] [Google Scholar]
- Adler M In today’s world, the well-rested lose respect. (2009). Morning edn. Washington, DC: National Public Radio. [Google Scholar]
- Ahbab S, Ataoğlu HE, Tuna M, Karasulu L, Çetin F, Temiz LÜ , & Yenigün M (2013). Neck circumference, metabolic syndrome and obstructive sleep apnea syndrome; evaluation of possible linkage. Medical science monitor: international medical journal of experimental and clinical research, 19, 111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albouy G, King BR, Maquet P, & Doyon J (2013a). Hippocampus and striatum: Dynamics and interaction during acquisition and sleep-related motor sequence memory consolidation. Hippocampus, 23(11), 985–1004. [DOI] [PubMed] [Google Scholar]
- Albouy G, Vandewalle G, Sterpenich V, Rauchs G, Desseilles M, Balteau E, … & Maquet P (2013b). Sleep stabilizes visuomotor adaptation memory: a functional magnetic resonance imaging study. Journal of sleep research, 22(2), 144–154. [DOI] [PubMed] [Google Scholar]
- Albuquerque FN, Kuniyoshi FHS, Calvin AD, Sierra-Johnson J, Romero-Corral A, Lopez-Jimenez F, … & Goldman ME (2010). Sleep-disordered breathing, hypertension, and obesity in retired National Football League players. Journal of the American College of Cardiology, 56(17), 1432–1433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen MS, Greenlees I, & Jones M (2013). Personality in sport: A comprehensive review. International Review of Sport and Exercise Psychology, 6(1), 184–208. [Google Scholar]
- American Academy of Sleep Medicine. International Classification of Sleep Disorders; 2014. 3rd ed. Darien: American Academy of Sleep Medicine. [Google Scholar]
- American College Health Association. American College Health Association-National College Health Assessment, Fall 2015, Spring 2016, Fall 2016, Spring 2017, Fall 2017 [data file]. Hanover, MD: American College Health Association. [producer and distributor] 2018-11–15. [Google Scholar]
- Arnal PJ, Sauvet F, Leger D, Van Beers P, Bayon V, Bougard C, … & Chennaoui M (2015). Benefits of sleep extension on sustained attention and sleep pressure before and during total sleep deprivation and recovery. Sleep, 38(12), 1935–1943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnal PJ, Lapole T, Erblang M, Guillard M, Bourrilhon C, Leger D, … & Millet GY (2016). Sleep extension before sleep loss: effects on performance and neuromuscular function. Med Sci Sports Exerc, 48(8), 1595–1603. [DOI] [PubMed] [Google Scholar]
- Ashworth A, Hill CM, Karmiloff-Smith A, & Dimitriou D (2014). Sleep enhances memory consolidation in children. Journal of Sleep Research, 23(3), 304–310. [DOI] [PubMed] [Google Scholar]
- Azboy O, & Kaygisiz Z (2009). Effects of sleep deprivation on cardiorespiratory functions of the runners and volleyball players during rest and exercise. Acta Physiologica Hungarica, 96(1), 29–36. [DOI] [PubMed] [Google Scholar]
- Baglioni C, Battagliese G, Feige B, Spiegelhalder K, Nissen C, Voderholzer U, … & Riemann D (2011). Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. Journal of affective disorders, 135(1-3), 10–19. [DOI] [PubMed] [Google Scholar]
- Baron KG, Reid KJ, Van Horn L, & Zee PC (2013). Contribution of evening macronutrient intake to total caloric intake and body mass index. Appetite, 60, 246–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basner M, & Dinges DF (2011). Maximizing sensitivity of the psychomotor vigilance test (PVT) to sleep loss. Sleep, 34(5), 581–591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beersma DG, & Gordijn MC (2007). Circadian control of the sleep–wake cycle. Physiology & behavior, 90(2-3), 190–195. [DOI] [PubMed] [Google Scholar]
- Bender AM, Lawson D, Werthner P, & Samuels CH (2018). The clinical validation of the athlete sleep screening questionnaire: an instrument to identify athletes that need further sleep assessment. Sports medicine-open, 4(1), 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergeron MF, Mountjoy M, Armstrong N, Chia M, Côté J, Emery CA, … & Malina RM (2015). International Olympic Committee consensus statement on youth athletic development. Br J Sports Med, 49(13), 843–851. [DOI] [PubMed] [Google Scholar]
- Bleyer FTDS, Barbosa DG, Andrade RD, Teixeira CS, & Felden ÉPG (2015). Sleep and musculoskeletal complaints among elite athletes of Santa Catarina. Revista Dor, 16(2), 102–108. [Google Scholar]
- Bonnet MH (1986). Performance and sleepiness following moderate sleep disruption and slow wav sleep deprivation. Physiology & behavior, 37(6), 915–918. [PubMed] [Google Scholar]
- Bonnet MH, & Arand DL (2010). Hyperarousal and insomnia: state of the science. Sleep medicine reviews, 14(1), 9–15. [DOI] [PubMed] [Google Scholar]
- Brassington GS (2002). Sleep problems. In Mostofsky DL & Zaichkowsky LD (Eds.), Medical and psychological aspects of sport and exercise (193–204). Morgantown, WV: Fitness Information Technology. [Google Scholar]
- Brown DA, Elsass JA, Miller AJ, Reed LE, & Reneker JC (2015). Differences in symptom reporting between males and females at baseline and after a sports-related concussion: a systematic review and meta-analysis. Sports medicine, 45(7), 1027–1040. [DOI] [PubMed] [Google Scholar]
- Buysse DJ, Angst J, Gamma A, Ajdacic V, Eich D, & Rössler W (2008). Prevalence, course, and comorbidity of insomnia and depression in young adults. Sleep, 31(4), 473–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai DJ, Mednick SA, Harrison EM, Kanady JC, & Mednick SC (2009). REM, not incubation, improves creativity by priming associative networks. Proceedings of the National Academy of Sciences, 106(25), 10130–10134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carskadon MA, Dement WC, 2011. Normal human sleep: an overview. In: Kryger MH, Roth T, Dement WC (Eds.), Principles and Practice of Sleep Medicine. St. Louis, Missouri: Saunders/Elsevier; pp. 16e26. [Google Scholar]
- Chaput JP, & Dutil C (2016). Lack of sleep as a contributor to obesity in adolescents: impacts on eating and activity behaviors. International Journal of Behavioral Nutrition and Physical Activity, 13(1), 103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chase JD, Roberson PA, Saunders MJ, Hargens TA, Womack CJ, & Luden ND (2017). One night of sleep restriction following heavy exercise impairs 3-km cycling time-trial performance in the morning. Applied Physiology, Nutrition, and Metabolism, 42(9), 909–915. [DOI] [PubMed] [Google Scholar]
- Clark I, & Landolt HP (2017). Coffee, caffeine, and sleep: A systematic review of epidemiological studies and randomized controlled trials. Sleep medicine reviews, 31, 70–78. [DOI] [PubMed] [Google Scholar]
- Collette R, Kellmann M, Ferrauti A, Meyer T, & Pfeiffer M (2018). Relation between training load and recovery-stress state in high-performance swimming. Frontiers in physiology, 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costill DL, Flynn MG, Kirwan JP, Houmard JA, Mitchell JB, Thomas R, & Park SH (1988). Effects of repeated days of intensified training on muscle glycogen and swimming performance. Med Sci Sports Exerc, 20(3), 249–254. [DOI] [PubMed] [Google Scholar]
- Curcio G, Ferrara M, & De Gennaro L (2006). Sleep loss, learning capacity and academic performance. Sleep medicine reviews, 10(5), 323–337. [DOI] [PubMed] [Google Scholar]
- Davenne D (2009). Sleep of athletes–problems and possible solutions. Biological Rhythm Research, 40(1), 45–52. [Google Scholar]
- Depadilla L, Miller GF, Jones SE, Peterson AB, & Breiding MJ (2018). Self-reported concussions from playing a sport or being physically active among high school students—United States, 2017. Morbidity and Mortality Weekly Report, 67(24), 682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drago V, Foster PS, Heilman KM, Aricò D, Williamson J, Montagna P, & Ferri R (2011). Cyclic alternating pattern in sleep and its relationship to creativity. Sleep medicine, 12(4), 361–366. [DOI] [PubMed] [Google Scholar]
- Drust B, Waterhouse J, Atkinson G, Edwards B, & Reilly T (2005). Circadian rhythms in sports performance—an update. Chronobiology international, 22(1), 21–44. [DOI] [PubMed] [Google Scholar]
- Diamond A (2013). Executive functions. Annual review of psychology, 64, 135–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinges DF, Pack F, Williams K, Gillen KA, Powell JW, Ott GE, … & Pack AI, (1997). Cumulative sleepiness, mood disturbance, and psychomotor vigilance performance decrements during a week of sleep restricted to 4–5 hours per night. Sleep, 20(4), 267–277. [PubMed] [Google Scholar]
- Dobrosielski DA, Nichols D, Ford J, Watts A, Wilder JN, & Douglass-Burton T (2016). Estimating the prevalence of sleep-disordered breathing among collegiate football players. Respiratory care, 61(9), 1144–1150. [DOI] [PubMed] [Google Scholar]
- Doyon J, Gabitov E, Vahdat S, Lungu O, & Boutin A (2018). Current issues related to motor sequence learning in humans. Current opinion in behavioral sciences, 20, 89–97. [Google Scholar]
- Drake C, Roehrs T, Shambroom J, & Roth T (2013). Caffeine effects on sleep taken 0, 3, or 6 hours before going to bed. Journal of Clinical Sleep Medicine, 9(11), 1195–1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drew MK, Vlahovich N, Hughes D, Appaneal R, Peterson K, Burke L, … & Praet S (2017). A multifactorial evaluation of illness risk factors in athletes preparing for the Summer Olympic Games. Journal of science and medicine in sport, 20(8), 745–750. [DOI] [PubMed] [Google Scholar]
- Drew M, Vlahovich N, Hughes D, Appaneal R, Burke LM, Lundy B, … & Praet S (2018). Prevalence of illness, poor mental health and sleep quality and low energy availability prior to the 2016 Summer Olympic Games. Br J Sports Med, 52(1), 47–53. [DOI] [PubMed] [Google Scholar]
- Driller MW, Dixon ZT, & Clark MI (2017). Accelerometer-based sleep behavior and activity levels in student athletes in comparison to student non-athletes. Sport Sciences for Health, 13(2), 411–418. [Google Scholar]
- Driller MW, Mah CD, & Halson SL (2018). Development of the athlete sleep behavior questionnaire: a tool for identifying maladaptive sleep practices in elite athletes. Sleep Science, 11(1), 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Driller MW, Lastella M, & Sharp AP (2019). Individualized sleep education improves subjective and objective sleep indices in elite cricket athletes: A pilot study. Journal of sports sciences, 1–5. [DOI] [PubMed] [Google Scholar]
- Drust B, Waterhouse J, Atkinson G, Edwards B, & Reilly T (2005). Circadian rhythms in sports performance—an update. Chronobiology international, 22(1), 21–44. [DOI] [PubMed] [Google Scholar]
- Dunican IC, Martin DT, Halson SL, Reale RJ, Dawson BT, Caldwell JA, … & Eastwood PR (2017). The effects of the removal of electronic devices for 48 hours on sleep in elite judo athletes. The Journal of Strength & Conditioning Research, 31(10), 2832–2839. [DOI] [PubMed] [Google Scholar]
- Dunican IC, Higgins CC, Jones MJ, Clarke MW, Murray K, Dawson B, … & Eastwood PR (2018). Caffeine use in a super rugby game and its relationship to post-game sleep. European journal of sport science, 18(4), 513–523. [DOI] [PubMed] [Google Scholar]
- Dunican IC, Walsh J, Higgins CC, Jones MJ, Maddison K, Caldwell JA, … & Eastwood PR (2019). Prevalence of sleep disorders and sleep problems in an elite super rugby union team. Journal of sports sciences, 37(8), 950–957. [DOI] [PubMed] [Google Scholar]
- Edwards BJ, & Waterhouse J (2009). Effects of one night of partial sleep deprivation upon diurnal rhythms of accuracy and consistency in throwing darts. Chronobiology international, 26(4), 756–768. [DOI] [PubMed] [Google Scholar]
- Eisenberg MA, Meehan WP, & Mannix R (2014). Duration and course of post-concussive symptoms. Pediatrics, 133(6), 999–1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emsellem HA, & Murtagh KE (2005). Sleep apnea and sports performance. Clinics in sports medicine, 24(2), 329–341. [DOI] [PubMed] [Google Scholar]
- Erlacher D, Ehrlenspiel F, Adegbesan OA, & Galal El-Din H (2011). Sleep habits in German athletes before important competitions or games. Journal of sports sciences, 29(8), 859–866. [DOI] [PubMed] [Google Scholar]
- Fagundes SB, Fagundes DJ, Carvalho LB, Coin-Carvalho J, Prado LF, & Prado GF (2010, January). Prevalence of restless legs syndrome in runners. In Sleep (Vol. 33, pp. A252–A252). One Westbrook Corporate CTR, STE 920, WESTCHESTER, IL 60154 USA: AMER ACAD SLEEP MEDICINE. [Google Scholar]
- Fischer D, Lombardi DA, Marucci-Wellman H, & Roenneberg T (2017). Chronotypes in the US–influence of age and sex. PloS one, 12(6), e0178782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fowler P, Duffield R, Howle K, Waterson A, & Vaile J (2015). Effects of northbound long-haul international air travel on sleep quantity and subjective jet lag and wellness in professional Australian soccer players. International journal of sports physiology and performance, 10(5), 648–654. [DOI] [PubMed] [Google Scholar]
- Fowler PM, Duffield R, Lu D, Hickmans JA, & Scott TJ (2016). Effects of long-haul transmeridian travel on subjective jet-lag and self-reported sleep and upper respiratory symptoms in professional rugby league players. International journal of sports physiology and performance, 11(7), 876–884. [DOI] [PubMed] [Google Scholar]
- Gais S, Lucas B, & Born J (2006). Sleep after learning aids memory recall. Learning & Memory, 13(3), 259–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- George CF, Kab V, Kab P, Villa JJ, & Levy AM (2003). Sleep and breathing in professional football players. Sleep medicine, 4(4), 317–325. [DOI] [PubMed] [Google Scholar]
- George CF, & Kab V (2011). Sleep-disordered breathing in the National Football League is not a trivial matter. Sleep, 34(3), 245–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goel N, Rao H, Durmer JS, & Dinges DF (2009, September). Neurocognitive consequences of sleep deprivation. In Seminars in neurology (Vol. 29, No. 04, pp. 320–339). © Thieme Medical Publishers. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gosselin N, Lassonde M, Petit D, Leclerc S, Mongrain V, Collie A, & Montplaisir J (2009). Sleep following sport-related concussions. Sleep medicine, 10(1), 35–46. [DOI] [PubMed] [Google Scholar]
- Gouttebarge V, Frings-Dresen MHW, & Sluiter JK (2015). Mental and psychosocial health among current and former professional footballers. Occupational medicine, 65(3), 190–196. [DOI] [PubMed] [Google Scholar]
- Graham R, Rivara FP, Ford MA, Spicer CM, Committee on Sports-Related Concussions in Youth, & National Research Council. (2014). Sports-related concussions in youth: improving the science, changing the culture. National Academies Press (US). [PubMed] [Google Scholar]
- Grandner MA, Jackson N, Gerstner JR, & Knutson KL (2013). Dietary nutrients associated with short and long sleep duration. Data from a nationally representative sample. Appetite, 64, 71–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grandner M (2014). Sleeping disorders. Mind, Body, and Sport. Understanding and Supporting Student-Athlete Mental Wellness. 51–53 [Google Scholar]
- Grandner MA, Jackson N, Gerstner JR, & Knutson KL (2014). Sleep symptoms associated with intake of specific dietary nutrients. Journal of sleep research, 23(1), 22–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grandner MA, Alfonso-Miller P, Fernandez-Mendoza J, Shetty S, Shenoy S, & Combs D (2016). Sleep: important considerations for the prevention of cardiovascular disease. Current opinion in cardiology, 31(5), 551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grandner MA (2017). Sleep, health, and society. Sleep medicine clinics, 12(1), 1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grandner MA, Athey A, Killgore WD, & Alfonso-Miller P (2017, April). Preliminary results of a sleep health intervention in student athletes; Changes in sleep, energy level, and mental well-being and body weight. In Sleep (Vol. 40, pp. A294–A294). Journals Dept, 2001 Evans RD, Cary, NC 27513 USA: OXFORD UNIV PRESS INC. [Google Scholar]
- Gulliver A, Griffiths KM, & Christensen H (2012). Barriers and facilitators to mental health help-seeking for young elite athletes: a qualitative study. BMC psychiatry, 12(1), 157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gulliver A, Griffiths KM, Mackinnon A, Batterham PJ, & Stanimirovic R (2015). The mental health of Australian elite athletes. Journal of science and medicine in sport, 18(3), 255–261. [DOI] [PubMed] [Google Scholar]
- Gupta L, Morgan K, & Gilchrist S (2017). Does elite sport degrade sleep quality? A systematic review. Sports Medicine, 47(7), 1317–1333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guezennec CY, Satabin P, Legrand H, & Bigard AX (1994). Physical performance and metabolic changes induced by combined prolonged exercise and different energy intakes in humans. European journal of applied physiology and occupational physiology, 68(6), 525–530. [DOI] [PubMed] [Google Scholar]
- Haack M, Sanchez E, & Mullington JM (2007). Elevated inflammatory markers in response to prolonged sleep restriction are associated with increased pain experience in healthy volunteers. Sleep, 30(9), 1145–1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haack M, Lee E, Cohen DA, & Mullington JM (2009). Activation of the prostaglandin system in response to sleep loss in healthy humans: potential mediator of increased spontaneous pain. PAIN®, 145(1–2), 136–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halson SL (2014). Monitoring training load to understand fatigue in athletes. Sports medicine, 44(2), 139–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harmon KG, Drezner JA, Gammons M, Guskiewicz KM, Halstead M, Herring SA, … & Roberts WO (2013). American Medical Society for Sports Medicine position statement: concussion in sport. Br J sports med, 47(1), 15–26. [DOI] [PubMed] [Google Scholar]
- Hausswirth C, Louis J, Aubry A, Bonnet G, Duffield R, & Le Meur Y (2014). Evidence of disturbed sleep and increased illness in overreached endurance athletes. Medicine and science in sports and exercise. [DOI] [PubMed] [Google Scholar]
- Harvey CJ, Gehrman P, & Espie CA (2014). Who is predisposed to insomnia: a review of familial aggregation, stress-reactivity, personality and coping style. Sleep medicine reviews, 18(3), 237–247. [DOI] [PubMed] [Google Scholar]
- Heaney S, O’Connor H, Michael S, Gifford J, & Naughton G (2011). Nutrition knowledge in athletes: a systematic review. International journal of sport nutrition and exercise metabolism, 21(3), 248–261. [DOI] [PubMed] [Google Scholar]
- Horne JA, & Pettitt AN (1984). Sleep deprivation and the physiological response to exercise under steady-state conditions in untrained subjects. Sleep, 7(2), 168–179. [DOI] [PubMed] [Google Scholar]
- Hoshikawa M, Uchida S, & Hirano Y (2018). A Subjective Assessment of the Prevalence and Factors Associated with Poor Sleep Quality Amongst Elite Japanese Athletes. Sports medicine-open, 4(1), 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang S, Deshpande A, Yeo SC, Lo JC, Chee MW, & Gooley JJ (2016). Sleep restriction impairs vocabulary learning when adolescents cram for exams: the need for sleep study. Sleep, 39(9), 1681–1690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huber R, Ghilardi MF, Massimini M, & Tononi G (2004). Local sleep and learning. Nature, 430(6995), 78. [DOI] [PubMed] [Google Scholar]
- Hynynen ESA, Uusitalo A, Konttinen N, & Rusko H (2006). Heart rate variability during night sleep and after awakening in overtrained athletes. Medicine and science in sports and exercise, 38(2), 313. [DOI] [PubMed] [Google Scholar]
- Jackson ML, Howard ME, & Barnes M (2011). Cognition and daytime functioning in sleep-related breathing disorders. Brain research (Vol. 190, pp. 53–68). Elsevier. [DOI] [PubMed] [Google Scholar]
- Jones C, Griffiths P, Towers P, Claxton J, & Mellalieu SD (2018). Pre-season injury and illness associations with perceptual wellness, neuromuscular fatigue, sleep and training load in elite rugby union. [Google Scholar]
- Jung CM, Melanson EL, Frydendall EJ, Perreault L, Eckel RH, & Wright KP (2011). Energy expenditure during sleep, sleep deprivation and sleep following sleep deprivation in adult humans. The Journal of physiology, 589(1), 235–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamdar BB, Kaplan KA, Kezirian EJ, & Dement WC (2004). The impact of extended sleep on daytime alertness, vigilance, and mood. Sleep medicine, 5(5), 441–448. [DOI] [PubMed] [Google Scholar]
- Karni A, Meyer G, Rey-Hipolito C, Jezzard P, Adams MM, Turner R, & Ungerleider LG (1998). The acquisition of skilled motor performance: fast and slow experience-driven changes in primary motor cortex. Proceedings of the National Academy of Sciences, 95(3), 861–868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katirji B Clinical neurophysiology: clinical electromyography. Philadelphia: Saunders Elsevier; 2012. [Google Scholar]
- Kiesel A, Steinhauser M, Wendt M, Falkenstein M, Jost K, Philipp AM, & Koch I (2010). Control and interference in task switching—A review. Psychological bulletin, 136(5), 849. [DOI] [PubMed] [Google Scholar]
- Killgore WD, Balkin TJ, & Wesensten NJ (2006). Impaired decision making following 49 h of sleep deprivation. Journal of sleep research, 15(1), 7–13. [DOI] [PubMed] [Google Scholar]
- Killgore WD (2010). Effects of sleep deprivation on cognition. In Progress in brain research (Vol. 185, pp. 105–129). Elsevier. [DOI] [PubMed] [Google Scholar]
- Killgore WD, Kamimori GH, & Balkin TJ (2011). Caffeine protects against increased risk-taking propensity during severe sleep deprivation. Journal of sleep research, 20(3), 395–403. [DOI] [PubMed] [Google Scholar]
- Kostyun RO, Milewski MD, & Hafeez I (2015). Sleep disturbance and neurocognitive function during the recovery from a sport-related concussion in adolescents. The American journal of sports medicine, 43(3), 633–640. [DOI] [PubMed] [Google Scholar]
- Lack LC, & Wright HR (2007). Chronobiology of sleep in humans. Cellular and molecular life sciences, 64(10), 1205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lastella M, Roach GD, Hurem DC, & Sargent C (2010). Does chronotype affect elite athletes’ capacity to cope with the training demands of elite triathlon. Living in a, 24(7), 25–28. [Google Scholar]
- Lastella M, Lovell GP, & Sargent C (2014). Athletes' precompetitive sleep behaviour and its relationship with subsequent precompetitive mood and performance. European Journal of Sport Science, 14(sup1), S123–S130. [DOI] [PubMed] [Google Scholar]
- Lastella M, Roach GD, Halson SL, Gore CJ, Garvican-Lewis LA, & Sargent C (2014). The effects of transmeridian travel and altitude on sleep: preparation for football competition. Journal of sports science & medicine, 13(3), 718. [PMC free article] [PubMed] [Google Scholar]
- Lastella M, Roach GD, Halson SL, & Sargent C (2015)., 15(2), 94–100. [DOI] [PubMed] [Google Scholar]
- Lastella M, Roach GD, Halson SL, Martin DT, West NP, & Sargent C (2015). Sleep/wake behaviour of endurance cyclists before and during competition. Journal of sports sciences, 33(3), 293–299. [DOI] [PubMed] [Google Scholar]
- Lastella M, Roach GD, Halson SL, & Sargent C (2016). The chronotype of elite athletes. Journal of human kinetics, 54(1), 219–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau BC, Collins MW, & Lovell MR (2011). Cutoff scores in neurocognitive testing and symptom clusters that predict protracted recovery from concussions in high school athletes. Neurosurgery, 70(2), 371–379. [DOI] [PubMed] [Google Scholar]
- Lau BC, Collins MW, & Lovell MR (2011a). Sensitivity and specificity of subacute computerized neurocognitive testing and symptom evaluation in predicting outcomes after sports-related concussion. The American journal of sports medicine, 39(6), 1209–1216. [DOI] [PubMed] [Google Scholar]
- Lee S, Crain TL, McHale SM, Almeida DM, & Buxton OM (2017). Daily antecedents and consequences of nightly sleep. Journal of sleep research, 26(4), 498–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S, Buxton OM, Andel R, & Almeida DM (2019). Bidirectional associations of sleep with cognitive interference in employees' work days. Sleep health. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leeder J, Glaister M, Pizzoferro K, Dawson J, & Pedlar C (2012). Sleep duration and quality in elite athletes measured using wristwatch actigraphy. Journal of sports sciences, 30(6), 541–545. [DOI] [PubMed] [Google Scholar]
- Lehto JE, Juujärvi P, Kooistra L, & Pulkkinen L (2003). Dimensions of executive functioning: Evidence from children. British Journal of Developmental Psychology, 21(1), 59–80. [Google Scholar]
- Le Meur Y, Duffield R, Skein M. (2012). Sleep. In: Recovery for performance in sport. Champaign: Human Kinetics. [Google Scholar]
- Li H, Moreland JJ, Peek-Asa C, & Yang J (2017). Preseason anxiety and depressive symptoms and prospective injury risk in collegiate athletes. The American journal of sports medicine, 45(9), 2148–2155. [DOI] [PubMed] [Google Scholar]
- Lin HH, Tsai PS, Fang SC, & Liu JF (2011). Effect of kiwifruit consumption on sleep quality in adults with sleep problems. Asia Pacific journal of clinical nutrition, 20(2), 169. [PubMed] [Google Scholar]
- Lucidi F, Lombardo C, Russo PM, Devoto A, & Violani C (2007). Sleep complaints in Italian Olympic and recreational athletes. Journal of Clinical Sport Psychology, 1(2), 121–129. [Google Scholar]
- Mah CD, Mah KE, Kezirian EJ, & Dement WC (2011). The effects of sleep extension on the athletic performance of collegiate basketball players. Sleep, 34(7), 943–950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mah CD, Kezirian EJ, Marcello BM, & Dement WC (2018). Poor sleep quality and insufficient sleep of a collegiate student-athlete population. Sleep health, 4(3), 251–257. [DOI] [PubMed] [Google Scholar]
- Maquet P (2001). The role of sleep in learning and memory. science, 294(5544), 1048–1052. [DOI] [PubMed] [Google Scholar]
- Marchetti R, Forte R, Borzacchini M, Vazou S, Tomporowski PD, & Pesce C (2015). Physical and motor fitness, sport skills and executive function in adolescents: a moderated prediction model. Psychology, 6(14), 1915. [Google Scholar]
- Marguilho R, Jesus SN, Viseu J, Rus C, & Brandolim N (2014). Sleep and creativity: A quantitative review. In Milcu M, Krall H, & Dan P (Eds.), Prospecting interdisciplinarity in health, education and social sciences (pp. 117–126). [Google Scholar]
- Markwald RR, Melanson EL, Smith MR, Higgins J, Perreault L, Eckel RH, & Wright KP (2013). Impact of insufficient sleep on total daily energy expenditure, food intake, and weight gain. Proceedings of the National Academy of Sciences, 110(14), 5695–5700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin BJ (1981). Effect of sleep deprivation on tolerance of prolonged exercise. European journal of applied physiology and occupational physiology, 47(4), 345–354. [DOI] [PubMed] [Google Scholar]
- Mathias JL, & Alvaro PK (2012). Prevalence of sleep disturbances, disorders, and problems following traumatic brain injury: a meta-analysis. Sleep medicine, 13(7), 898–905. [DOI] [PubMed] [Google Scholar]
- McClure DJ, Zuckerman SL, Kutscher SJ, Gregory AJ, & Solomon GS (2014). Baseline neurocognitive testing in sports-related concussions: the importance of a prior night’s sleep. The American journal of sports medicine, 42(2), 472–478. [DOI] [PubMed] [Google Scholar]
- McCrory P, Meeuwisse WH, Aubry M, Cantu RC, Dvořák J, Echemendia RJ, … & Sills A (2013). Consensus statement on concussion in sport—the 4th International Conference on Concussion in Sport held in Zurich, November 2012. PM&R, 5(4), 255–279. [DOI] [PubMed] [Google Scholar]
- McCrory P, Meeuwisse WH, Echemendia RJ, Iverson GL, Dvorak J, & Kutcher JS (2013a). What is the lowest threshold to make a diagnosis of concussion?. Br J Sports Med, 47(5), 268–271. [DOI] [PubMed] [Google Scholar]
- McCrory P, Meeuwisse W, Dvorak J, Aubry M, Bailes J, Broglio S, … & Davis GA (2017). Consensus statement on concussion in sport—the 5th international conference on concussion in sport held in Berlin, October 2016. Br J Sports Med, 51(11), 838–847. [DOI] [PubMed] [Google Scholar]
- Meeusen R, Duclos M, Foster C, Fry A, Gleeson M, Nieman D, … & Urhausen A (2013). Prevention, diagnosis, and treatment of the overtraining syndrome: joint consensus statement of the European College of Sport Science and the American College of Sports Medicine. Medicine and science in sports and exercise, 45(1), 186–205. [DOI] [PubMed] [Google Scholar]
- Micai M, Kavussanu M, & Ring C (2015). Executive function is associated with antisocial behavior and aggression in athletes. Journal of sport and exercise psychology, 37(5), 469–476. [DOI] [PubMed] [Google Scholar]
- Mihaere KM, Harris R, Gander PH, Reid PM, Purdie G, Robson B, & Neill A (2009). Obstructive sleep apnea in New Zealand adults: prevalence and risk factors among Māori and non-Māori. Sleep, 32(7), 949–956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milewski MD, Skaggs DL, Bishop GA, Pace JL, Ibrahim DA, Wren TA, & Barzdukas A (2014). Chronic lack of sleep is associated with increased sports injuries in adolescent athletes. Journal of Pediatric Orthopaedics, 34(2), 129–133. [DOI] [PubMed] [Google Scholar]
- Morselli L, Leproult R, Balbo M, & Spiegel K (2010). Role of sleep duration in the regulation of glucose metabolism and appetite. Best practice & research Clinical endocrinology & metabolism, 24(5), 687–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mougin F, Davenne D, Simon-Rigaud ML, Renaud A, Garnier A, & Magnin P (1989). Disturbance of sports performance after partial sleep deprivation. Comptes rendus des seances de la Societe de biologie et de ses filiales, 183(5), 461–466. [PubMed] [Google Scholar]
- Mougin F, Simon-Rigaud ML, Davenne D, Renaud A, Garnier A, Kantelip JP, & Magnin P (1991). Effects of sleep disturbances on subsequent physical performance. European journal of applied physiology and occupational physiology, 63(2), 77–82. [DOI] [PubMed] [Google Scholar]
- Mougin F, Bourdin H, Simon-Rigaud ML, Didier JM, Toubin G, & Kantelip JP (1996). Effects of a selective sleep deprivation on subsequent anaerobic performance. International journal of sports medicine, 17(02), 115–119. [DOI] [PubMed] [Google Scholar]
- Mougin F, Bourdin H, Simon-Rigaud ML, Nhu UN, Kantelip JP, & Davenne D (2001). Hormonal responses to exercise after partial sleep deprivation and after a hypnotic drug-induced sleep. Journal of sports sciences, 19(2), 89–97. [DOI] [PubMed] [Google Scholar]
- Mountjoy M, Sundgot-Borgen JK, Burke LM, Ackerman KE, Blauwet C, Constantini N, … & Sherman RT (2018). IOC consensus statement on relative energy deficiency in sport (RED-S): 2018 update. Br J Sports Med, bjsports-2018. [DOI] [PubMed] [Google Scholar]
- NCAA. The Student-Athlete Perspective of the College Experience Findings from the NCAA GOALS and SCORE Studies, 2008. [Available from: https://www.ncaa.org/sites/default/files/The%20StudentAthlete%20Perspective%20of%20the%20College%20Experience.pdf
- NCAA. Defining Countable Athletically Related Activities, 2009. [Available from: https://www.ncaa.org/sites/default/files/Charts.pdf
- NCAA. How Student-Athletes Feel About Time Demands, 2017. [Available from: https://www.ncaa.org/sites/default/files/2017GOALS_Time_demands_20170628.pdf
- NCAA. NCAA Sports Sponshirship and Participation Rates Report, 2018. [Available from: https://ncaaorg.s3.amazonaws.com/research/sportpart/Oct2018RES_2017-18SportsSponsorshipParticipationRatesReport.pdf
- Nixdorf I, Frank R, Hautzinger M, & Beckmann J (2013). Prevalence of depressive symptoms and correlating variables among German elite athletes. Journal of Clinical Sport Psychology, 7(4), 313–326. [Google Scholar]
- Okano K, Kaczmaryk J, Dave N, Gabrieli J & Grossman J, (2019). "Sleep quality, duration, and consistency are associated with better academic performance in college students." npj Science of Learning 4(1): 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliver SJ, Costa RJ, Laing SJ, Bilzon JL, & Walsh NP (2009). One night of sleep deprivation decreases treadmill endurance performance. European journal of applied physiology, 107(2), 155–161. [DOI] [PubMed] [Google Scholar]
- Omisade A, Buxton OM, & Rusak B (2010). Impact of acute sleep restriction on cortisol and leptin levels in young women. Physiology & behavior, 99(5), 651–656. [DOI] [PubMed] [Google Scholar]
- Ordóñez FM, Oliver AJS, Bastos PC, Guillén LS, & Domínguez R (2017). Sleep improvement in athletes: use of nutritional supplements. Am. J. Sports Med, 34, 93–99. [Google Scholar]
- Oudiette D, Constantinescu I, Leclair-Visonneau L, Vidailhet M, Schwartz S, & Arnulf I (2011). Evidence for the re-enactment of a recently learned behavior during sleepwalking. PloS one, 6(3), e18056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owens J, & Adolescent Sleep Working Group. (2014). Insufficient sleep in adolescents and young adults: an update on causes and consequences. Pediatrics, 134(3), e921–e932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raikes AC, Athey A, Alfonso-Miller P, Killgore WD, & Grandner MA (2019). Insomnia and daytime sleepiness: risk factors for sports-related concussion. Sleep Medicine. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reardon CL, Hainline B, Aron CM, Baron D, Baum AL, Bindra A, … & Derevensky JL (2019). Mental health in elite athletes: International Olympic Committee consensus statement (2019). British journal of sports medicine, 53(11), 667–699. [DOI] [PubMed] [Google Scholar]
- Reilly T, Waterhouse J, & Budgett R (2005). Sport, exercise and environmental physiology. Elsevier Churchill Livingstone. [Google Scholar]
- Reilly T, & Edwards B (2007). Altered sleep–wake cycles and physical performance in athletes. Physiology & behavior, 90(2-3), 274–284. [DOI] [PubMed] [Google Scholar]
- Reyner LA, & Horne JA (2013). Sleep restriction and serving accuracy in performance tennis players, and effects of caffeine. Physiology & behavior, 120, 93–96. [DOI] [PubMed] [Google Scholar]
- Rice TB, Dunn RE, Lincoln AE, Tucker AM, Vogel RA, Heyer RA, … & Newman AB (2010). Sleep-disordered breathing in the National Football League. Sleep, 33(6), 819–824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rivara FP, Schiff MA, Chrisman SP, Chung SK, Ellenbogen RG, & Herring SA (2014). The effect of coach education on reporting of concussions among high school athletes after passage of a concussion law. The American journal of sports medicine, 42(5), 1197–1203. [DOI] [PubMed] [Google Scholar]
- Rogers AJ, Xia K, Soe K, Sexias A, Sogade F, Hutchinson B, … & Jean-Louis G (2017). Obstructive sleep apnea among players in the National Football League: a scoping review. Journal of sleep disorders & therapy, 6(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossa KR, Smith SS, Allan AC, & Sullivan KA (2014). The effects of sleep restriction on executive inhibitory control and affect in young adults. Journal of Adolescent Health, 55(2), 287–292. [DOI] [PubMed] [Google Scholar]
- Rupp TL, Wesensten NJ, Bliese PD, & Balkin TJ (2009). Banking sleep: realization of benefits during subsequent sleep restriction and recovery. Sleep, 32(3), 311–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samuels C (2008). Sleep, recovery, and performance: the new frontier in high-performance athletics. Neurologic clinics, 26(1), 169–180. [DOI] [PubMed] [Google Scholar]
- Samuels CH (2012). Jet lag and travel fatigue: a comprehensive management plan for sport medicine physicians and high-performance support teams. Clinical Journal of Sport Medicine, 22(3), 268–273. [DOI] [PubMed] [Google Scholar]
- Samuels C, James L, Lawson D, & Meeuwisse W (2016). The Athlete Sleep Screening Questionnaire: a new tool for assessing and managing sleep in elite athletes. Br J Sports Med, 50(7), 418–422. [DOI] [PubMed] [Google Scholar]
- Sargent C, Halson S, & Roach GD (2014). Sleep or swim? Early-morning training severely restricts the amount of sleep obtained by elite swimmers. European Journal of Sport Science, 14(sup1), S310–S315. [DOI] [PubMed] [Google Scholar]
- Sargent C, Lastella M, Halson SL, & Roach GD (2014). The impact of training schedules on the sleep and fatigue of elite athletes. Chronobiology International, 31(10), 1160–1168. [DOI] [PubMed] [Google Scholar]
- Sargent C, Lastella M, Romyn G, Versey N, Miller DJ, & Roach GD (2018). How well does a commercially available wearable device measure sleep in young athletes?. Chronobiology international, 35(6), 754–758. [DOI] [PubMed] [Google Scholar]
- Savis JC, Eliot JF, Gansneder B, & Rotella RJ (1997). A subjective means of assessing college athletes' sleep: a modification of the morningness/eveningness questionnaire. International Journal of Sport Psychology, 28(2), 157–170. [Google Scholar]
- Schultz J These famous athletes rely on sleep for peak performance, Huffington Post, 2014. Available at: http://www.huffingtonpost.com/2014/08/13/these-famous-athletes-rely-on-sleep_n_5659345.html (accessed October 1st, 2019). [Google Scholar]
- Shechter A, Grandner MA, & St-Onge MP (2014). The role of sleep in the control of food intake. American journal of lifestyle medicine, 8(6), 371–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva A, Queiroz SS, Winckler C, Vital R, Sousa RA, Fagundes V, … & de Mello MT (2012). Sleep quality evaluation, chronotype, sleepiness and anxiety of Paralympic Brazilian athletes: Beijing 2008 Paralympic Games. Br J Sports Med, 46(2), 150–154. [DOI] [PubMed] [Google Scholar]
- Sin NL, Almeida DM, Crain TL, Kossek EE, Berkman LF, & Buxton OM (2017). Bidirectional, temporal associations of sleep with positive events, affect, and stressors in daily life across a week. Annals of Behavioral Medicine, 51(3), 402–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sio UN, Monaghan P, & Ormerod T (2013). Sleep on it, but only if it is difficult: effects of sleep on problem solving. Memory & cognition, 41(2), 159–166. [DOI] [PubMed] [Google Scholar]
- Skein M, Duffield R, Edge J, Short MJ, & Muendel T (2011). Intermittent-sprint performance and muscle glycogen after 30 h of sleep deprivation. Medicine & Science in Sports & Exercise, 43(7), 1301–1311. [DOI] [PubMed] [Google Scholar]
- Smyth EA, Newman P, Waddington G, Weissensteiner JR, & Drew MK (2019). Injury prevention strategies specific to pre-elite athletes competing in Olympic and professional sports—A systematic review. Journal of science and medicine in sport. [DOI] [PubMed] [Google Scholar]
- Souissi N, Souissi M, Souissi H, Chamari K, Tabka Z, Dogui M, & Davenne D (2008). Effect of time of day and partial sleep deprivation on short-term, high-power output. Chronobiology International, 25(6), 1062–1076. [DOI] [PubMed] [Google Scholar]
- Souissi N, Chtourou H, Aloui A, Hammouda O, Dogui M, Chaouachi A, & Chamari K (2013). Effects of time-of-day and partial sleep deprivation on short-term maximal performances of judo competitors. The Journal of Strength & Conditioning Research, 27(9), 2473–2480. [DOI] [PubMed] [Google Scholar]
- Spiegel K, Leproult R, & Van Cauter E (1999). Impact of sleep debt on metabolic and endocrine function. The lancet, 354(9188), 1435–1439. [DOI] [PubMed] [Google Scholar]
- Spiegel K, Leproult R, L’Hermite-Balériaux M, Copinschi G, Penev PD, & Van Cauter E (2004). Leptin levels are dependent on sleep duration: relationships with sympathovagal balance, carbohydrate regulation, cortisol, and thyrotropin. The Journal of clinical endocrinology & metabolism, 89(11), 5762–5771. [DOI] [PubMed] [Google Scholar]
- Stickgold R, Hobson JA, Fosse R, & Fosse M (2001). Sleep, learning, and dreams: off-line memory reprocessing. Science, 294(5544), 1052–1057. [DOI] [PubMed] [Google Scholar]
- Stickgold R (2005). Sleep-dependent memory consolidation. Nature, 437(7063), 1272. [DOI] [PubMed] [Google Scholar]
- Storch EA, Storch JB, Killiany EM, & Roberti JW (2005). Self-reported psychopathology in athletes: a comparison of intercollegiate student-athletes and non-athletes. Journal of sport behavior, 28(1). [Google Scholar]
- Sufrinko AM, Howie EK, Elbin RJ, Collins MW, & Kontos AP (2018). A preliminary investigation of accelerometer-derived sleep and physical activity following sport-related concussion. The Journal of head trauma rehabilitation, 33(5), E64–E74. [DOI] [PubMed] [Google Scholar]
- Swinbourne R, Gill N, Vaile J, & Smart D (2016). Prevalence of poor sleep quality, sleepiness and obstructive sleep apnea risk factors in athletes. European journal of sport science, 16(7), 850–858. [DOI] [PubMed] [Google Scholar]
- Taheri M, & Arabameri E (2012). The effect of sleep deprivation on choice reaction time and anaerobic power of college student athletes. Asian journal of sports medicine, 3(1), 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsunoda K, Hotta K, Mutsuzaki H, Tachibana K, Shimizu Y, & Fukaya T (2015). Sleep status in male wheelchair basketball players on a Japanese national team. J Sleep Disord Ther, 4(210), 2167–0277. [Google Scholar]
- Tuomilehto H, Vuorinen VP, Penttilä E, Kivimäki M, Vuorenmaa M, Venojärvi M, … & Pihlajamäki J (2017). Sleep of professional athletes: underexploited potential to improve health and performance. Journal of sports sciences, 35(7), 704–710. [DOI] [PubMed] [Google Scholar]
- Turner RW, Vissa K, Hall C, Poling K, Athey A, Alfonso-Miller P, … & Grandner MA (2019). Sleep problems are associated with academic performance in a national sample of collegiate athletes. Journal of American College Health, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verma A, Anand V, & Verma NP (2007). Sleep disorders in chronic traumatic brain injury. Journal of Clinical Sleep Medicine, 3(04), 357–362. [PMC free article] [PubMed] [Google Scholar]
- Von Rosen P, Frohm A, Kottorp A, Friden C, & Heijne A (2017). Too little sleep and an unhealthy diet could increase the risk of sustaining a new injury in adolescent elite athletes. Scandinavian journal of medicine & science in sports, 27(11), 1364–1371. [DOI] [PubMed] [Google Scholar]
- Von Rosen P, Frohm A, Kottorp A, Fridén C, & Heijne A (2017a). Multiple factors explain injury risk in adolescent elite athletes: Applying a biopsychosocial perspective. Scandinavian journal of medicine & science in sports, 27(12), 2059–2069. [DOI] [PubMed] [Google Scholar]
- Walker MP, Brakefield T, Morgan A, Hobson JA, & Stickgold R (2002). Practice with sleep makes perfect: sleep-dependent motor skill learning. Neuron, 35(1), 205–211. [DOI] [PubMed] [Google Scholar]
- Walker MP, & Stickgold R (2005). It's practice, with sleep, that makes perfect: implications of sleep-dependent learning and plasticity for skill performance. Clinics in sports medicine, 24(2), 301–317. [DOI] [PubMed] [Google Scholar]
- Walker MP, & Stickgold R (2006). Sleep, memory, and plasticity. Annu. Rev. Psychol, 57, 139–166. [DOI] [PubMed] [Google Scholar]
- Walters PH (2002). Sleep, the athlete, and performance. Strength & Conditioning Journal, 24(2), 17–24. [Google Scholar]
- Weber M, Webb CA, & Killgore WD (2013). A brief and selective review of treatment approaches for sleep disturbance following traumatic brain injury. J Sleep Disorders Ther, 2(110), 2167–0277. [Google Scholar]
- Wilckens KA, Erickson KI, & Wheeler ME (2012). Age-related decline in controlled retrieval: the role of the PFC and sleep. Neural plasticity, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Włodarczyk D, Jaśkowski P, & Nowik A (2002). Influence of sleep deprivation and auditory intensity on reaction time and response force. Perceptual and motor skills, 94(3_suppl), 1101–1112. [DOI] [PubMed] [Google Scholar]
- Wolanin A, Hong E, Marks D, Panchoo K, & Gross M (2016). Prevalence of clinically elevated depressive symptoms in college athletes and differences by gender and sport. British journal of sports medicine, 50(3), 167–171. [DOI] [PubMed] [Google Scholar]
- Zhong X, Hilton HJ, Gates GJ, Jelic S, Stern Y, Bartels MN, … & Basner RC (2005). Increased sympathetic and decreased parasympathetic cardiovascular modulation in normal humans with acute sleep deprivation. Journal of applied physiology, 98(6), 2024–2032. [DOI] [PubMed] [Google Scholar]


