Abstract
Objective
Situation awareness (SA) refers to people’s perception and understanding of their dynamic environment. In primary care, reduced SA among physicians increases errors in clinical decision-making and, correspondingly, patients’ risk of experiencing adverse outcomes. Our objective was to understand the extent to which electronic health records (EHRs) support primary care physicians (PCPs)’ SA during clinical decision-making.
Method
We conducted a metanarrative review of papers in selected academic databases, including CINAHL and MEDLINE. Eligible studies included original peer-reviewed research published between January 2012 and August 2020 on PCP–EHR interactions. We iteratively queried, screened, and summarized literature focused on EHRs supporting PCPs’ clinical decision-making and care management for adults. Then, we mapped findings to an established SA framework to classify external factors (individual, task, and system) affecting PCPs’ levels of SA (1–Perception, 2–Comprehension, and 3–Projection) and identified SA barriers.
Results
From 1504 articles identified, we included and synthesized 19 studies. Study designs were largely noninterventional. Studies described EHR workflow misalignments, usability issues, and communication challenges. EHR information, including lab results and care plans, was characterized as incomplete, untimely, or irrelevant. Unmet information needs made it difficult for PCPs to obtain even basic SA, Level 1 SA. Prevalent barriers to PCPs developing SA with EHRs were errant mental models, attentional tunneling, and data overload.
Conclusion
Based on our review, EHRs do not support the development of higher levels of SA among PCPs. Review findings suggest SA-oriented design processes for health information technology could improve PCPs’ SA, satisfaction, and decision-making.
Keywords: situation awareness, primary care, electronic health record, cognition, decision-making, safety
Background
Despite interventions such as patient-centered medical homes and electronic health records (EHRs), improvements in the quality and safety of primary care have not been consistently recognized (Beasley et al., 2020). As defined by the Institute of Medicine, primary care is “the provision of integrated, accessible health care services by clinicians who are accountable for addressing a large majority of personal health care needs, developing a sustained partnership with patients, and practicing in the context of family and community” (Fiscella & McDaniel, 2018; Institute of Medicine, 1996). Primary care ranges from disease prevention to end-stage disease and palliative care; it encompasses acute care, chronic disease management, and all organ systems, age ranges, and genders (Institute of Medicine, 1996). Increasingly, primary care physicians (PCPs) are addressing multiple patient issues in one visit, averaging less than 20 min (Fiscella & McDaniel, 2018; Temte et al., 2020). Before, during, and after visits, there is a critical need for care coordination among the primary care team, including physicians, nurses, medical assistants, and clerks. Additionally, this coordination must extend to specialists, hospitals, and long-term care facilities (Beasley et al., 2020; Savoy et al., 2019). Without comprehensive, accessible, timely, and accurate patient information, PCPs cannot make decisions related to prevention, diagnosis, or treatment, which are needed to deliver high-quality care to patients (Beasley et al., 2011; Savoy et al., 2021).
EHRs often refer to a digital version of a patient’s paper chart and the associated health information systems (Office of the National Coordinator for Health Information Technology, 2019). EHRs can improve primary care decision-making and delivery by enhancing access to detailed patient information, ensuring more reliable communication between providers and care teams, and facilitating clinical decision support. Over 10 years after the Health Information Technology for Economic and Clinical Health (HITECH) Act aimed to improve the quality, safety, and efficiency of health care by promoting health information technology adoption, persistent issues of poor usability have limited EHRs’ expected benefits (Beasley et al., 2011; Howe et al., 2018; Roman et al., 2017; Sinsky et al., 2014). Usability is the extent to which a product or service can be used to achieve goals with effectiveness, efficiency, and satisfaction (International Organization for Standardization, 2018). In primary care practices, where EHR adoption has progressed rapidly since HITECH’s passage, negative unintended consequences are evident (Beasley et al., 2011; Colicchio et al., 2019; Eikey et al., 2019; Institute of Medicine, 2012; Zheng et al., 2016).
EHR user interfaces do not fully support the dynamics of primary care workflows, such as facilitating management of multiple problems per encounter, efficient EHR interactions, teamwork, and longitudinal care (Berg, 1999; Carter, 2015; Karsh et al., 2010; Rittenhouse et al., 2020; Sinsky et al., 2014; Zulman et al., 2016). Clinical information in EHRs is organized primarily for billing and other administrative management (Savoy et al., 2021). Reviewing patient history may involve navigating through multiple sections of the EHR (Roman et al., 2017) to find only partial answers, both increasing review time and lowering the likelihood of finding an answer (Aakre et al., 2019; Daei et al., 2020; Dwairy et al., 2011; González-González et al., 2007; Gorman, 1995; Gorman & Helfand, 1995). This increases PCPs’ cognitive workload and decreases their situation awareness (SA), defined as “the perception of the elements in the environment, the comprehension of their meaning, and the projection of their status in the near future” (Beasley et al., 2011; Endsley, 1988). A lack or loss of SA related to the perception of clinical findings, comprehension of patient condition, and projection of possible outcomes and treatments negatively impacts decision-making (Singh et al., 2006).
From aviation to health care, including anesthesiology, surgery, acute nursing, and emergency medicine, the SA framework has been used to understand both decision-making and errors (Gaba et al., 1995; Hazlehurst et al., 2007; Nibbelink & Brewer, 2018; Risser et al., 1999; Sitterding et al., 2012; Wauben et al., 2011; Wright et al., 2004). Using the SA framework, individual (e.g., goals and objectives, abilities, training, experience), task (e.g., stress and workload, complexity), and system (e.g., EHR capability and interface design) factors have been identified and analyzed to determine their impact on developing and maintaining SA (Endsley & Jones, 2012c). Previous analyses of clinical scenarios in primary care have demonstrated that decreased awareness impeded activities ranging from clinical problem identification to treatment planning (Beasley et al., 2011; Murphy et al., 2019; Powell et al., 2020; Singh et al., 2012). While EHRs are expected to provide information that PCPs need to support SA, usability issues have hindered PCP–EHR interactions, and these usability issues have the potential to foster SA barriers (i.e., often labeled “SA demons”; Table 1) that can increase medical errors (Beasley et al., 2011; Singh et al., 2012). There is little evidence demonstrating relationships among these PCP–EHR interactions and the development or maintenance of SA.
Table 1.
Situation Awareness (SA) Barriers Types and Definitions (Endsley & Jones, 2012b)
| SA Barriers | Definition |
|---|---|
| Attentional tunneling | Fixating on one set of information to the exclusion of others. |
| Requisite memory trap | Over reliance on limited short-term memory. |
| Workload, fatigue, and other stressors | Contextual stressors that reduce a person’s capacity to process information. |
| Data overload | Large amounts of data or changes in data that overwhelm individuals by outpacing their sensory and cognitive systems. |
| Misplaced salience | Drawing user’s attention to irrelevant, low priority information. |
| Complexity creep | Systems with too many features, tabs, or menus. |
| Errant mental models | Use of wrong mental model for interpretation. |
| Out of the loop syndrome | Automation without user’s collaboration. |
We aimed to understand how EHRs support PCPs’ SA by providing information needed to make clinical decisions and manage care for adult patients. Our long-term goal was to outline corresponding gaps in SA support that could be targeted by interventions.
Methods
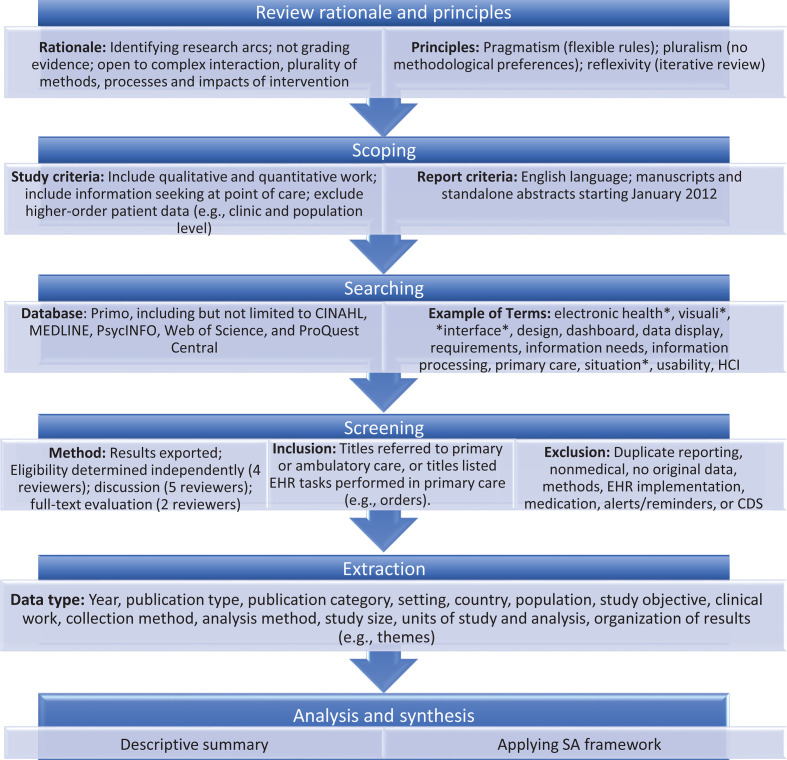
To understand how EHRs support PCPs’ SA, we performed a systematic review and metanarrative analysis (Greenhalgh et al., 2005; Wong et al., 2013) using the SA framework. In contrast to meta-analyses, the metanarrative analysis enabled the inclusion of heterogenous (e.g., quantitative, qualitative, and mixed methods) studies to provide a comprehensive description of the current state of PCPs’ SA supported by EHRs. The metanarrative approach also permitted an open-ended and iterative approach to planning, searching, and synthesis of literature mapped to the SA framework (Greenhalgh et al., 2005; Stanton et al., 2017). SA concepts (e.g., information presentation and cognition) guided the systematic searching, screening, extraction and synthesis of the existing research (Figure A1).
Scoping and Searching
We used the SA framework to define the review’s scope, considering social dynamics of primary care and PCPs’ EHR interactions. We focused on common clinical decisions and tasks related to care management of adult patients that are often not supported by clinical decision support tools. For example, deciding whether to start palliative care, predicting quality of life and recovery time, and tracking progress toward patients’ stated goals are tasks for which clinical decision support tools do not exist. We systematically reviewed academic literature published between January 2012 and August 2020. By the end of 2011, initial findings related to HITECH’s implementation were published (Blumenthal, 2011). Thus, we chose 2012 as the starting year for our review. We included English-language manuscripts and standalone abstracts. Primary sources were the databases indexed by the metasearch product Primo (Ex Libris Group, 2020), including CINAHL, MEDLINE, PsycINFO, Web of Science, EBSCO, and ProQuest Central. Searches were simultaneous across these databases, and exact duplicates within a search were removed automatically.
A primary keyword search included situation awareness and primary care. To expand the search, two authors (AS, HP) built a compound query using related terms from the U.S. National Library of Medicine’s Medical Subject Headings. We tested and changed our search and screening processes iteratively. After estimating the relevance of results for each query, final queries included these terms: electronic health record, electronic medical record, patient record, electronic record, visuali*, interface, design, prototype, concept, dashboard, data display, requirements, information needs, information processing, primary care, healthcare, health care, situation* awareness, user-computer interface, presentation, salien*, usability, morae, and HCI.
Screening and Extraction
Search results were exported into reference management software (Center for History and New Media at George Mason University, 2013; Clarivate Analytics, 2016–2019). Four reviewers determined eligibility independently by working unblinded on separate subsets (205–217 articles per subset). Weekly meetings were held to review screening decisions. We included articles if their titles referred to primary or ambulatory care, or if the titles listed EHR tasks that may be performed in primary care (e.g., orders). We excluded articles based on abstracts. Types excluded were duplicate reporting (e.g., conference papers edited into journal papers), secondary work (e.g., position and review articles), and methods-oriented work (i.e., defining or reviewing protocols or metrics). Themes excluded were clinical decision support systems, migration from paper records, information needs from secondary uses of EHRs (i.e., not at the point of care), reminders used strictly as memory aids, decision support aids used strictly for prescribing, incidental (not central) findings about information needs, and usability evaluations of software interfaces that did not include information needs. The remaining papers were discussed in a consensus meeting with five reviewers (including AS). Then, two reviewers (AS, HP) reviewed the full-text of the included papers and extracted five elements: study focus, organization type, participants, analysis method, and results. In a series of consensus meetings, we excluded papers due to not reporting user attitudes (e.g., a software proof of concept), reporting only the needs of patients, or reporting needs in specialties other than primary care (Table A1).
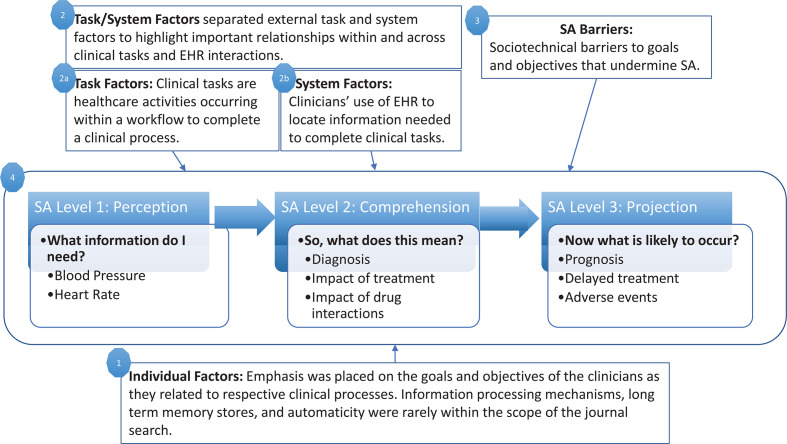
To understand how EHRs support PCPs’ SA, review findings were mapped (Figure 1) to SA framework concepts (Endsley, 1995; Singh et al., 2012). Based on this framework, three types of factors can affect primary care SA. Individual factors include PCPs’ goals and objectives for clinical processes. Task factors include clinical tasks within a workflow to complete those processes. System factors include PCPs’ experiences using EHRs when completing those tasks.
Figure 1.
Adaptation of SA framework (Singh et al., 2012; Wright et al., 2004) that guided mapping of findings. SA = situation awareness.
Results
Search Findings
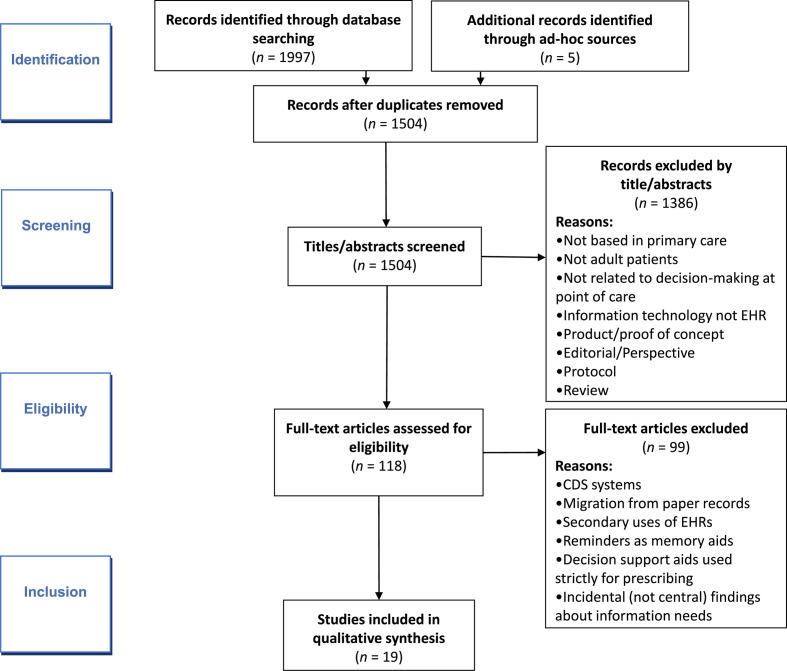
Our prepared and ad hoc searches identified 1504 unique papers (Figure 2). After applying our criteria iteratively to titles, abstracts, and full texts, 118 papers underwent review. In the majority of the studies that directly addressed SA, PCPs were not identified as primary stakeholders or users.
Figure 2.
Document flow. * Criteria listed in methods section.
Overview of Studies
The resultant literature sample consisted of 19 papers published between 2012 and 2020 (Appendix 2). Twelve of the papers were published in medical informatics journals (Clarivate Analytics, 2021). Although different health care organization types were represented (educational, government, and community health care organizations), most of this diversity was between studies, not within them. Four studies were conducted across multiple health care networks (Flanagan et al., 2013; Harle et al., 2019; Pet et al., 2019; Robelia et al., 2017). Seventeen studies were descriptive or interpretive; only two (11%) were interventional (Belden et al., 2017; Del Fiol et al., 2016). Fourteen studies (74%) used interview- or focus group-based qualitative and exploratory methods, three involved surveys (Menon et al., 2016; Robelia et al., 2017; Singh et al., 2013), and two involved controlled evaluation (Belden et al., 2017; Clarke et al., 2014). Of 16 non-survey studies, 13 involved fewer than 30 participants.
Mapping to SA Framework
Figure 3 illustrates the synthesized review findings mapped to the components of the SA framework. Specific individual (goals of clinical processes), task (information requirements), and system (EHR interactions) factors that affect SA are listed. Major SA barriers identified are also represented.
Figure 3.
Summary of mapping to SA framework. This figure illustrates the synthesis of literature findings mapped to the components of the SA framework. SA barriers related to individual, task, and system factors are depicted with dashed-line barricades near the respective factors. SA = situation awareness.
In the following sections, we discuss PCPs’ information needs published in our literature sample and associated with levels of SA. Then, we discuss the individual, task, and system factors that affect SA and expound on the EHR’s impact on SA. Lastly, we discuss barriers to SA.
Information Needed From EHRs to Support Levels of SA for PCPs
Most studies focused on information needed to acquire the basic level of SA, SA Level 1 (Perception), and involved methods for gathering information from EHRs for review. Individual PCPs’ information needs included new symptoms, previous care plans (Singh et al., 2012; Wright et al., 2004), and changes in social determinants of health (Friedman et al., 2014; Koopman et al., 2015; Weir et al., 2015). Clinical teams’ information needs were driven by care transitions. Advanced levels of SA—Level 2 (Comprehension) and Level 3 (Projection)—were identified in 11 studies (Clarke et al., 2014; Friedman et al., 2014; Harle et al., 2019; Koopman et al., 2015; Menon et al., 2016; Pet et al., 2019; Robelia et al., 2017; Rogers et al., 2012; Rotenstein et al., 2016; Savoy et al., 2019; Weir et al., 2015). Achieving these advanced levels of SA is often based on the synthesis and interpretation of information gathered from the EHR and is important for clinical decision-making and care management. For example, PCPs needed previous assessment and plan documents (Clarke et al., 2014; Koopman et al., 2015) to better comprehend patients’ medical conditions and aid care coordination (SA Level 2). For SA Level 3, genomic labs (Pet et al., 2019) were the main reference of information considered for patient health projection or forecasting. Table 2 displays information needs specified across the studies and links them to the three SA Levels.
Table 2.
Information Needed From EHRs to Support PCPs and Their Teams’ Clinical Decision-Making, Organized by SA Level
| SA Level | Information Needs | References |
|---|---|---|
| SA Level 1 |
|
(Ahluwalia et al., 2015; Dillon et al., 2017; Flanagan et al., 2013; Friedman et al., 2014; Harle et al., 2019; Koopman et al., 2015; Menon et al., 2016; Robelia et al., 2017; Rogers et al., 2012; Rotenstein et al., 2016; Savoy et al., 2019; Singh et al., 2013; Smith et al., 2019; Weir et al., 2015) |
| SA Level 2 |
|
(Clarke et al., 2014; Friedman et al., 2014; Harle et al., 2019; Koopman et al., 2015; Menon et al., 2016; Pet et al., 2019; Robelia et al., 2017; Rogers et al., 2012; Rotenstein et al., 2016; Savoy et al., 2019; Smith et al., 2019; Weir et al., 2015) |
| SA Level 3 |
|
(Clarke et al., 2014; Harle et al., 2019; Koopman et al., 2015; Pet et al., 2019; Rogers et al., 2012; Rotenstein et al., 2016; Savoy et al., 2019) |
Note. *Information needed by more than one person on the care team. EHRs = electronic health records; PCP = primary care physician; SA = situation awareness.
PCP–EHR Interactions: Classification of Individual, Task, and System Factors That Affect SA
SA individual factors: Ineffective EHR-integrated clinical processes
Common goals for clinical processes included efficient communication and effective decision-making. These were classified as individual factors in SA because they shape the determination of important information. PCPs attempted to use the EHR to communicate and collaborate, relying on notes and alerts/notifications for information transfer, which would increase SA. However, findings across studies consistently indicated that EHRs were not effective tools for communication or collaborations (Ahluwalia et al., 2015; Flanagan et al., 2013; Koopman et al., 2015; Robelia et al., 2017; Rotenstein et al., 2016; Smith et al., 2019). Similarly, EHRs did not adequately support individual or team decision-making (Clarke et al., 2014; Harle et al., 2019; Koopman et al., 2015; Pet et al., 2019; Robelia et al., 2017; Weir et al., 2015). Contents of progress notes related to administrative reporting and metrics rather than information needed for clinical tasks and decision-making (Koopman et al., 2015). Insufficient information timeliness, quality, and access inhibited SA. Unmet information needs preceding a clinical decision were associated with medical errors (Singh et al., 2013). In an attempt to mitigate these medical errors, physicians across institutions established workarounds—actions addressing real or perceived limitations in technology (Cresswell et al., 2012)—in their clinical processes. Four papers described workarounds to EHRs, addressing SA Levels 1 and 2 (Flanagan et al., 2013; Friedman et al., 2014; Menon et al., 2016; Smith et al., 2019). EHR workarounds aimed to aid memory and increase awareness and efficiency (Flanagan et al., 2013; Smith et al., 2019). Decreased SA may have explained negative outcomes in care coordination (Clarke et al., 2014; Koopman et al., 2015), advance care planning (Ahluwalia et al., 2015; Dillon et al., 2017), and referrals (Harle et al., 2019; Savoy et al., 2019). For example, not knowing whether a specialty-care referral led to a consultation (Harle et al., 2019; Savoy et al., 2019) inhibited decision-making.
SA task factors: Inconsistent quality of EHR information
EHR information had attributes that positively or negatively affected PCPs’ SA and associated clinical tasks, decisions, or outcomes. With every clinical decision and task, PCPs regularly decided which information to pursue and use. Weir et al. (2015) identified six attributes of patient information—informativeness, goal language, temporality, source attribution, retrieval effort, and information quality—supporting a patient-centered medical home model of care (Table A4). We linked these attributes to clinical tasks done with the EHR across the studies. To achieve Level 1 SA, retrieval effort—time to determine the usefulness of information—was influential. This effort appeared to increase with case complexity, time since last visit, and EHR unavailability (Koopman et al., 2015; Singh et al., 2013). With this increase, it was harder for PCPs to gather and review recent notes and lab results. For Level 2 SA, temporality and information quality were vital for PCPs to identify a baseline status of interest and identify notable deviations or trends from that baseline (Belden et al., 2017; Del Fiol et al., 2016). This was particularly important for medication reconciliation (Robelia et al., 2017). For Level 3 SA, poor relevance, language, and quality of information caused issues with advanced care planning, which involved projection of outcomes and mapping of care concordant with accepted practices and with the patients’ preferences (Ahluwalia et al., 2015; Dillon et al., 2017).
SA system factors: Poor EHR usability
Although EHRs demonstrate increased usefulness over paper records, literature described poor EHR usability, identified negative experiences, or limited interventions. As a result, PCPs’ stress and workload increased, which decreases SA (Belden et al., 2017; Del Fiol et al., 2016; Flanagan et al., 2013; Friedman et al., 2014; Rotenstein et al., 2016).
PCPs’ experiences using EHRs included redundant interaction and information overload. Redundant interaction was described as repeated actions using one or more interfaces to complete a single task, including documenting information in multiple systems (Friedman et al., 2014). Related outcomes included increased time needed to review of patient records and clinical references (Del Fiol et al., 2016; Robelia et al., 2017), slower ordering of medication tapers (Friedman et al., 2014), and duplicated documentation (Friedman et al., 2014; Menon et al., 2016). Information overload was related to an inability to manipulate filters or sort EHR information. Tools to limit information overload via filtering, sorting, or querying remained unused (Singh et al., 2013). Outcomes associated with information overload included (1) increased time and effort for retrieval (Belden et al., 2017; Clarke et al., 2014; Koopman et al., 2015; Weir et al., 2015) and (2) increased difficulty in prioritizing information (Menon et al., 2016; Singh et al., 2013; Smith et al., 2019).
SA Barriers Present in PCP–EHR Interactions
Table 3 describes the link between social and technical (i.e., sociotechnical) and SA barriers. Social barriers to communication were related to ambiguities of physician expectations and responsibilities (Ahluwalia et al., 2015; Dillon et al., 2017; Smith et al., 2019). This ambiguity was amplified by the absence of messaging capabilities in EHRs, demonstrating errant mental models among EHR designers and care teams (Ahluwalia et al., 2015). Technical barriers to communication related to computing infrastructure and human–computer interfaces included EHR downtime (Flanagan et al., 2013), lack of interoperability among vendors limiting access to clinical information (Friedman et al., 2014), and inadequate support for managing notifications (Del Fiol et al., 2016; Menon et al., 2016; Singh et al., 2013; Smith et al., 2019). These were often associated with attentional tunneling, misplaced salience, and data overload, which decrease Level 1 SA. One illustration described the organization and presentation of progress notes (Belden et al., 2017; Clarke et al., 2014; Koopman et al., 2015), which facilitated billing and reimbursement more than building patient narratives (Ahluwalia et al., 2015; Clarke et al., 2014; Weir et al., 2015). Based on the literature sample, errant mental model, requisite memory trap, attention tunneling, and data overload were the most evident SA barriers.
Table 3.
Associations Among Sociotechnical Barriers and SA Barriers in Primary Care Medicine
| SA Barriers | Affected SA Level | Published Sociotechnical Barriers | References | |
|---|---|---|---|---|
| Errant mental model | Level 1 |
|
Ahluwalia et al. (2015); Flanagan et al. (2013); Rogers et al. (2012); Savoy et al. (2019) | |
|
||||
| Attentional tunneling | Level 1 |
|
Ahluwalia et al. (2015); Dillon et al. (2017); Flanagan et al. (2013); Friedman et al. (2014); Harle et al. (2019); Robelia et al. (2017); Rogers et al. (2012); Rotenstein et al. (2016); Savoy et al. (2019); Smith et al. (2019) | |
| Misplaced salience and data overload | Level 1 |
|
Menon et al. (2016); Singh et al. (2013); Smith et al. (2019) | |
| Workload, anxiety, fatigue, and other stressors | Level 1 |
|
Pet et al. (2019) | |
| Level 2 |
|
|||
| Requisite memory trap | Level 2 |
|
Flanagan et al. (2013); Friedman et al. (2014); Savoy et al. (2019); Smith et al. (2019) | |
|
||||
|
Note. EHRs = electronic health records; PCPs = primary care physicians; SA = situation awareness.
Discussion
The SA framework enabled us to analyze published findings using a systems approach that considered the combined effect of PCPs’ goals for clinical processes, information attributes required to complete clinical tasks, and usability requirements for physician–EHR interactions on PCPs’ SA. Based on our results, we discuss implications for SA in primary care and considerations for future research below.
Implications of SA in Primary Care
Finding patient events, lab values, and clinical status required redundant efforts and high mental workloads for PCPs and their teams. If perception of this information is hindering Level 1 SA, then higher levels of SA are not supported. With respect to the SA framework, existing research largely focuses on Level 1 SA. Our study suggests that there is a gap between PCP-pursued needs and EHR information and visualizations. EHRs are not capturing or presenting information in a manner that allow PCPs to efficiently use it in the context of their clinical workflow. More recently, technological workarounds and interventions are not integrated into the EHR and require PCPs to use additional user interfaces (e.g., Metke-Jimenez et al., 2019). Furthermore, there is a lack of focus on team SA, which is important given the widely adopted patient-centered medical home model in primary care. Without higher levels of SA, PCPs and their teams are prone to delayed action, inaction, or inappropriate action.
Requisite memory trap, attention tunneling, and data overload were the most common barriers examined. When EHRs are unable to support higher levels of SA and contain widespread SA barriers, PCPs are forced to create workarounds due to requisite memory traps, make decisions with limited information due to attention tunneling, or experience high levels of mental workload due to data overload. To build and maintain SA, researchers and designers need to ensure accurate mental models for PCPs, which guides their information interpretation. These models would inform aggregation of disparate elements of information to support comprehension and projections of patient conditions or treatment. Although PCPs’ expertise and workarounds resolve some sociotechnical barriers, there is tension between PCPs’ determination to care for patients and EHR issues. This makes health care delivery susceptible to medical errors, patients susceptible to safety risks, and providers susceptible to burnout (National Academy of Medicine, 2019). Clinical decision-making is forced to occur at the intersection of competing goals and priorities, high levels of uncertainty, and EHRs that do not support SA adequately.
From this review, major barriers for obtaining high levels of SA stemmed from errant mental models. These barriers persist when technology-centered designs are implemented rather than user-centered designs. When mental models are discussed, it is about the users of systems applying the wrong mental model for data perception. However, we propose another perspective of errant mental model, where EHR developers apply the wrong mental model. Major EHR vendors have challenges implementing a user-centered design process, and one of those challenges is their inability to conduct contextually rich studies of clinical workflow (Ratwani et al., 2015; Zheng et al., 2020). Additionally, communication breakdowns among interdisciplinary groups or research and practice contribute to errant mental models among EHR developers and the lack of successful user interfaces (Hettinger et al., 2021). These breakdowns invoked by ineffective deliverables have created difficulties in translating user requirements into implemented software features (Saleem et al., 2016).
Human Factors Approach to Improve EHRs’ Support of SA
Implementing a human factors approach for the (re)design of EHR user interfaces can improve PCP-EHR interactions. A recent review by Carayon and Hoonakker (2019) concluded that this approach positively affects not only the usability of systems but also the quality-of-care processes and outcomes. Based on our findings, the SA-oriented design process has the potential to improve EHRs’ ability to support higher levels of SA for PCPs. This particular human factors approach is a user-centered design process that consists of three main components: SA requirements analysis, SA design principles, and SA measurement and validation (Endsley & Jones, 2012a).
SA requirements analysis can be used to mitigate the knowledge gaps and ambiguity demonstrated across workflows in our literature sample. This type and similar analyses have been used to define the information needed for PCPs and supporting roles in healthcare teams for specific workflows or tasks (Militello et al., 2020; Savoy et al., 2019). For example, Savoy et al. (2019) described information needs for referring PCPs during the referral process. Their specification of distinct goals, tasks, and decision points throughout workflows identified information needs and how they shifted across decisions. Ostropolets et al. (2020) identified clinicians’ unmet information needs that arose from gaps in medical evidence to inform requirements for the design of future clinical decision support systems.
With these requirements, SA design principles (Endsley & Jones, 2012a) developed to combat the SA barriers identified by our metanarrative analysis can be applied to future EHR (re)designs. These SA design principles include general and specific guidelines to support higher levels of SA. For example, SA Design Principles 1 and 2 posit organizing EHR information based on PCPs’ goals (SA Design Principle 1) and directly presenting SA Level 2 information (SA Design Principle 2) to minimize demands on PCPs’ working memory. Emerging literature demonstrated the application of these and other human factors principles in the design of user interfaces for clinicians (Fischer et al., 2020; Harle et al., 2019; Savoy et al., 2018). For example, Fischer et al. (2020) used human factors design principles to create a visualization supporting decision-making about chronic diseases, increasing PCPs’ satisfaction.
Furthermore, SA measurement and validation provide feedback for iterative design and continuous improvement. Associated methods (e.g., SAGAT, SART, simulations, interviews, observations, rating scales) can be used before and after implementation of designs. Methods can also be adapted for remote and pragmatic evaluations to reduce potential PCP participation burden and provide evidence of impact on outcomes (Sauer et al., 2019; Woodward et al., 2020). For example, Woodward et al. (2020) used field observation and stakeholder input to inform the design of a neurosurgery referral system, which was put into practice; a pre-post implementation evaluation indicated the new system improved referral outcomes.
Limitations
This review has some limitations. Our primary keyword search was limited to academic publications published in English and indexed by commonly used databases, including MEDLINE and PsycINFO. In addition, we limited the review to PCP workflows and EHR interactions. Thus, we did not include articles with alternative methods of addressing SA, cognitive workload, or information needs. However, the combination of our search strategies helped to identify key literature with implications for SA in primary care. With a metanarrative approach, we could not define or calculate a standard effect. Additionally, our ability to assess the quality of each study was limited. As with other reviews, we denote the possibility of selective reporting and publication bias among individual papers.
Conclusion
Based on our review, current EHRs are unable to support the development of high levels of SA among PCPs. The SA framework advances our thinking about PCPs’ interaction with EHRs by considering the impact of social and technical factors on developing and maintaining SA needed to provide quality care. In various workflows, there are key barriers hindering PCPs’ development of Level 1 SA, upon which higher levels of SA depend. What information and how information is presented to PCPs through EHRs greatly influences SA and clinical decision-making. New research and implementation methods should be investigated to incorporate SA principles into health information technology design and evaluation to increase PCPs’ level of SA.
Key Points
With the SA framework, this metanarrative study advanced our understanding of PCPs’ interaction with EHRs and found that EHRs do not support the development of higher levels (Levels 2–3) of SA among PCPs.
Requisite memory traps, errant mental models, attention tunneling, and data overload were the most prevalent SA barriers present during PCP–EHR interactions.
Findings suggest that PCP decision-making is forced to occur at the intersection of competing goals and priorities, high levels of uncertainty, and EHRs that do not support SA adequately, which has negative implications for PCP mental workload and patient safety.
Based on our results, incorporation of SA-oriented design principles into future EHR and relevant health information technology design, development, and evaluation is recommended to increase PCPs’ level of SA.
Acknowledgments
Special thanks to our research team and student assistants, Zeba Kokan and Anna Mathew. This work was funded by the Human Factors Engineering Directorate in the Office of Health Informatics, U.S. Department of Veterans Affairs (VA), who helped define this work’s original scope. April Savoy and Himalaya Patel are supported in part by VA Health Services Research and Development (HSR&D) Center for Health Information and Communication (CIN 13–416). April Savoy is also supported in part by the following grants KL2TR002530 (A Carroll, PI), and UL1TR002529 (A. Shekhar, PI) from the National Institutes of Health, National Center for Advancing Translational Sciences, Clinical and Translational Sciences Award. Daniel Murphy, Ashley Meyer, and Hardeep Singh are supported in part by the Houston VA HSR&D Center for Innovations in Quality, Effectiveness and Safety (CIN 13–413). Additionally, Ashley Meyer is supported by a VA HSR&D Career Development Award (CDA 17–167).
Author Biographies
April Savoy is an assistant professor at Indiana University-Purdue University Indianapolis in the Purdue School of Engineering and Technology. She is a faculty investigator at the Regenstrief Institute and at the Center for Health Information and Communication at Richard L. Roudebush VA Medical Center in Indiana, where she also directs the Human Computer Interaction and Simulation Lab. She received her PhD in industrial engineering in 2008 from Purdue University.
Himalaya Patel is a researcher at the VA Health Services Research and Development Center for Health Information and Communication at Richard L. Roudebush VA Medical Center in Indianapolis, Indiana, where he manages the Human-Computer Interaction and Simulation Lab. He received his PhD in informatics in 2015 from Indiana University.
Daniel Murphy is the medical director and an assistant professor at Baylor College of Medicine in the Department of Medicine. He is an investigator at the Center for Innovations in Quality, Effectiveness and Safety at Michael E. DeBakey VA Medical Center. Dr. Murphy received his MD from the University of Miami School of Medicine in 2004. He received his MBA in 2006 from the University of Miami School of Business.
Ashley N. D. Meyer is an assistant professor at Baylor College of Medicine. She is a cognitive psychologist at the Center for Innovations in Quality, Effectiveness and Safety at Michael E. DeBakey VA Medical Center. Dr. Meyer co-directs the VA Patient Safety Center of Inquiry - Diagnosis Improvement Safety Center in Houston, Texas. She received her PhD in cognitive psychology/neuroscience in 2011 from Rice University.
Jennifer Herout is a program manager in the VA’s Office of Connected Care (OCC), where she oversees field testing prior to release of OCC tools. She received her PhD in industrial and systems engineering in 2008 from the University of Wisconsin.
Hardeep Singh is a professor at Baylor College of Medicine in the Department of Medicine. He is the chief of health policy, quality, and informatics program at the Center for Innovations in Quality, Effectiveness and Safety based at the Michael E. DeBakey VA Medical Center and Baylor. Dr. Singh received his MD in 1994 from All India Institute of Medical Sciences. He received his MPH in 2004 from Medical College of Wisconsin.
Appendix 1. Review Steps
Figure A1.
Adapted metanarrative review (Greenhalgh et al., 2005; Wong et al., 2013) with synthesis using SA framework (Endsley, 1995). To explore the literature and synthesize the data from existing scholarly work, we conducted a metanarrative review of recent academic literature and applied the situation awareness framework to organize our findings. Our review concerned information-seeking activity at the point of care (i.e., between encounters), excluding higher-order patient data (e.g., at the clinic and population level). The focus of our review was not on grading the evidence, but rather on identifying research arcs. Our approach accepted both quantitative and qualitative methods, and it facilitated investigating both the processes and impacts of interventions (Pawson et al., 2005).
Appendix 2. Studies Included in Literature Sample
Table A1.
Summary of the Studies Included in the Review
| Reference | Focus | Participants | Analytic Method | Result |
|---|---|---|---|---|
| Ahluwalia et al. (2015) | Coordination: Advance directives | 20 | Thematic analysis, consensus coding | Identified three barriers to practice, which related to social and technical aspects of communication about advance care planning and two strategies to overcome the barriers. |
| Rogers et al. (2012) | Coordination | 26 | Participatory design, strategic rationale diagramming, strategic dependency diagramming | Identified information needs of clinicians to support knowledge sharing and distributed decision-making. Suggested improvements to the EHR included documenting and sharing patient information related to behavioral, emotional, and spiritual factors that influence physical health and disease. |
| Clarke et al. (2014) | Review notes | 15 | Nonparametric statistical inference | In progress notes, sections frequently identified as important were History of Present Illness (HPI) and Assessment, and Plan (A&P). Usefulness of Review of Systems (ROS) was low typically but higher in some contexts. |
| Weir et al. (2015) | Coordination | 17 | Cognitive task analysis; critical incident technique | Identified six key attributes of contextual information about patients: informativeness, goal language, temporality, source attribution, retrieval effort, and information quality. |
| Koopman et al. (2015) | Review notes | 16 | Cognitive task analysis | Assessment and Plan was the most important and usually reviewed first. History of Present Illness could provide supporting information, especially in narrative form. Review of Systems did not match physicians’ information needs. A patient summary view made past notes partially redundant. |
| Friedman et al. (2014) | Routine; Coordination | 19 | Grounded | Workarounds addressed problems with the EHR user interface, barriers to health information exchange, and difficulty integrating new technology. Dimensions of workarounds were temporary/routinized, avoidable/unavoidable, and chosen/unplanned. |
| Singh et al. (2013) | Review test results | 2590 | Descriptive statistics | Identified sociotechnical barriers to notifying patients and providers about test results. PCPs supported new features to improve tracking and visualization of result notifications. |
| Flanagan et al. (2013) | Routine; Coordination | 120 | Consensus coding, hybrid | Identified computer- and paper-based workarounds for efficiency, memory, and awareness at three institutions. Identified a new workaround category, no correct path, for computer-based workarounds. |
| Belden et al. (2017) | Review notes | 16 | Descriptive statistics, inferential statistics | One- and two-column collapsible Assessment, Plan, Subjective, Objective (APSO)-formatted notes were significantly faster than Subjective, Objective, Assessment, and Plan (SOAP) and noncollapsible APSO notes for the Review of Systems and Physical Examination tasks. Usability ratings for SOAP format were worse than for three other note styles. |
| Del Fiol et al. (2016) | Clinical decisions | 10 | Descriptive statistics, inferential statistics | New computerized clinical knowledge summarization tool that summarizes patient-specific and actionable clinical recommendations from PubMed and UpToDate was compared with usual practice (manual searching). Although difference in search time was not significant, perceived decision quality was significantly greater with the new tool |
| Farrell et al. (2017) | Routine; Coordination | 10 (est.) | Goal-directed task analysis (cognitive task analysis) | Although high-level goals are fundamentally different between physicians and nurses, shared goals were identified. Groups share level 3 SA in projecting that the education they provide will improve patients’ health and compliance |
| Pet et al. (2019) | Clinical decisions: Unsolicited genomic results | 25 | Thematic analysis | Concerns about work disruption, patient stress, validity of screening, importance of actionable information |
| Robelia et al. (2017) | Review: Discharge summaries | 474 | Descriptive statistics | Discharge summaries are sometimes missing or incomplete, even when other hospital records are accessible |
| Dillon et al. (2017) | Coordination: Advance directives | 13 (interviews) 437 (chart review) | Descriptive statistics, thematic analysis | PCPs sought advance care planning (ACP) information more than specialists did, PCP workflows involved ACP information more than specialist workflows did, and PCPs documented ACP more than specialists did |
| Rotenstein et al. (2016) | Coordination: Complex patients | 20 | Thematic analysis; descriptive statistics | Identified key principles that health care software developers can integrate into PC and patient-centered electronic care planning tools. |
| Menon et al. (2016) | Review test result management | 2554 | Descriptive statistics; inferential statistics | Workarounds to manage EHR-based test results are common and indicate unmet needs |
| Harle et al. (2019) | Review: treat chronic pain | 10 | Thematic analysis | Identified four key goals, eight supporting information needs, and four design elements |
| Smith et al. (2019) | Test result management to inform HIT requirements | 37 | Content analysis | Identified challenges and methods used to overcome challenges; HIT should support team/ task status tracking for test result management |
| Savoy et al. (2019) | Coordination: Referrals for specialty consults | 62 | Hierarchical task analysis; goal-directed task analysis | Identified goal hierarchy with one main goal, two sub-goals, and four major tasks; identified 22 information needs which PCPs satisfied through different sources |
Table A2.
Clinical Processes (Individual Factors), Task-Related Information Attributes (Task Factors), and EHR Interactions (System Factors) Identified as Affecting PCPs’ SA When Using the EHR
| Factor | Reference | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ahluwalia et al. (2015) | Rogers et al. (2012) | Clarke et al. (2014) | Weir et al. (2015) | Koopman et al. (2015) | Singh et al. (2013) | Flanagan et al. (2013) | Friedman et al. (2014) | Belden et al. (2017) | Del Fiol et al. (2016) | Farrell et al. (2017) | Pet et al. (2019) | Robelia et al. (2017) | Dillon et al. (2017) | Rotenstein et al. (2016) | Menon et al. (2016) | Harle et al. (2019) | Smith et al. (2019) | Savoy et al. (2019) | |
| Individual: Clinical Processes | |||||||||||||||||||
| Communication | X | X | X | X | X | X | X | X | X | X | X | ||||||||
| Decision-making | X | X | X | X | X | X | X | X | X | X | X | X | |||||||
| Workarounds | X | X | X | X | X | ||||||||||||||
| Tasks: Information Attributes | |||||||||||||||||||
| Informativeness | X | X | X | X | X | X | X | X | X | X | X | ||||||||
| Goal language | X | X | X | X | X | X | |||||||||||||
| Temporality | X | X | X | X | X | ||||||||||||||
| Source attribution | X | X | |||||||||||||||||
| Retrieval effort | X | X | X | X | X | X | X | ||||||||||||
| Quality | X | X | X | X | X | X | X | ||||||||||||
| System: EHR Interactions | |||||||||||||||||||
| Multiple systems | X | X | X | X | X | X | |||||||||||||
| Information overload | X | X | X | X | X | X | X | ||||||||||||
| Features not found | X | X | X | X | |||||||||||||||
Table A3.
Clinical Tasks and Attributes of Related Information Needed to Support Point-of-Care Decisions in Primary Care
| Relevant Clinical Task | Representative Quotations | Attribute (Weir et al., 2015) |
References |
|---|---|---|---|
| Assessment and planning | When dealing with the information overload of cluttered notes, there is tension between the need to display the bare minimum to set the context versus the need to “see it all” and be assured nothing has been missed (Koopman et al., 2015). | Informativeness: Relevance, vividness, usefulness, and clarity | Del Fiol et al. (2016); Harle et al. (2019); Pet et al. (2019); Savoy et al. (2019); Smith et al. (2019) |
| Deciding whether to start palliative care | Providers expressed frustration over the absence or inaccessibility of information about a patient’s health care values and goals and described this gap as a function of current approaches to capturing advanced care planning (ACP) information (Ahluwalia et al., 2015). | Goal language: Patients’ values, preferences, and goals | Ahluwalia et al. (2015); Dillon et al. (2017); Rogers et al. (2012); Rotenstein et al. (2016) |
| Detecting and describing changes from baseline |
One advantage of low-tech
media such as paper notes and white boards is that they
allow for efficiency and adaptability. Users can quickly
and easily create prospective memory aids for
non-routine events, reconfigure data to highlight
elements that are important in a specific context, or
track data over time that may become important later in
solving a specific problem (Flanagan et al.,
2013) “Medication list with changes” was regarded as most important (94% “very important”), followed by “list of diagnoses/problems” (89%) and “treatment provided” (87%; Robelia et al., 2017). |
Temporality: Onset, end, baseline, and changes | Flanagan et al. (2013); Robelia et al. (2017) |
| Deciding whether to start palliative care | Providers earlier in the care continuum, for example, primary care, described [advance care planning] much more broadly than acute care providers closer to the end-of-life (EOL), for example, intensive care, and consequently identified different types of ACP tasks (Ahluwalia et al., 2015) | Source attribution: Implicit evaluation of the message source’s role, setting, and responsibilities | Ahluwalia et al. (2015) |
| Writing and reading a persistent
record of a patient’s health goals Acting on lab results |
Providers also discussed
how the structure of the EMR discouraged more robust
documentation of patient values and goals, in particular
because it was designed to capture point-of-care events
rather than a more unified narrative about the patient’s
health (Ahluwalia et al.,
2015) [When] primary care physicians did not have time to process all notifications, printing them to highlight abnormal results and creating paper logs/lists to place high-priority notifications on the top of the list helped them manage them more efficiently (Menon et al., 2016). |
Retrieval effort: Time to determine relevance, source, temporal attributes, and quality | Ahluwalia et al. (2015); Flanagan et al. (2013); Koopman et al. (2015); Menon et al. (2016); Pet et al. (2019) |
| Detecting abnormal lab results | If the labels of abnormality are not consistently reliable, users will not trust the information display, and its utility will suffer dramatically. Our erroneous note (note model D the with the faulty Physical Examination values) vividly illustrated that erosion of trust once a test subject discovered the discrepancy between the header summary and the remainder of the section hidden by default (Belden et al., 2017). | Information quality: Consistency, completeness, and accuracy | Belden et al. (2017); Del Fiol et al. (2016); Flanagan et al. (2013); Robelia et al. (2017) |
ORCID iD
April Savoy https://orcid.org/0000-0001-9002-9234
References
- Aakre C. A., Maggio L. A., Fiol G. D., Cook D. A. (2019). Barriers and facilitators to clinical information seeking: A systematic review. Journal of the American Medical Informatics Association, 26, 1129–1140. 10.1093/jamia/ocz065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahluwalia S. C., Bekelman D. B., Huynh A. K., Prendergast T. J., Shreve S., Lorenz K. A. (2015). Barriers and strategies to an iterative model of advance care planning communication. American Journal of Hospice and Palliative Medicine, 32, 817–823. 10.1177/1049909114541513 [DOI] [PubMed] [Google Scholar]
- Beasley J. W., Holden R. J., Ötleş E., Green L. A., Steege L. M., Wetterneck T. B. (2020). It’s time to bring human factors to primary care policy and practice. Applied Ergonomics, 85, 103077. 10.1016/j.apergo.2020.103077 [DOI] [PubMed] [Google Scholar]
- Beasley J. W., Wetterneck T. B., Temte J., Lapin J. A., Smith P., Rivera-Rodriguez A. J., Karsh B.-T. (2011). Information chaos in primary care: Implications for physician performance and patient safety. Journal of the American Board of Family Medicine, 24, 745–751. 10.3122/jabfm.2011.06.100255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belden J. L., Koopman R. J., Patil S. J., Lowrance N. J., Petroski G. F., Smith J. B. (2017). Dynamic electronic health record note prototype: Seeing more by showing less. Journal of the American Board of Family Medicine, 30, 691–700. 10.3122/jabfm.2017.06.170028 [DOI] [PubMed] [Google Scholar]
- Berg M. (1999). Patient care information systems and health care work: A sociotechnical approach. International Journal of Medical Informatics, 55, 87–101. 10.1016/S1386-5056(99)00011-8 [DOI] [PubMed] [Google Scholar]
- Blumenthal D. (2011). Implementation of the federal health information technology initiative. New England Journal of Medicine, 365, 2426–2431. 10.1056/NEJMsr1112158 [DOI] [PubMed] [Google Scholar]
- Carayon P., Hoonakker P. (2019). Human factors and usability for health information technology: Old and new challenges. Yearbook of Medical Informatics, 28, 071–077. 10.1055/s-0039-1677907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter J. H. (2015, September 21). A usability conundrum: Whether it is EHRs or hospital gowns, one size never fits all…. EHR Science: Explorations in the Design and Implementation of Clinical Information Systems. https://www.ehrscience.com/2015/09/21/a-usability-conundrum-whether-it-is-ehrs-or-hospital-gowns-one-size-never-fits-all/
- Center for History and New Media at George Mason University . (2013). Zotero (Version 4). George Mason University. https://www.zotero.org/
- Clarivate Analytics . (2016–2019). EndNote (Version X7-X9). Clarivate Analytics. http://endnote.com/
- Clarivate Analytics . (2021). Journal citation reports. Clarivate Analytics. https://jcr.clarivate.com. [Google Scholar]
- Clarke M. A., Steege L. M., Moore J. L., Koopman R. J., Belden J. L., Kim M. S. (2014). Determining primary care physician information needs to inform ambulatory visit note display. Applied Clinical Informatics, 05, 169–190. 10.1055/s-0037-1619454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colicchio T. K., Cimino J. J., Del Fiol G. (2019). Unintended consequences of nationwide electronic health record adoption: Challenges and opportunities in the post-Meaningful use era. Journal of Medical Internet Research, 21, e13313. 10.2196/13313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cresswell K. M., Worth A., Sheikh A. (2012). Integration of a nationally procured electronic health record system into user work practices. BMC Medical Informatics and Decision Making, 12, 15. 10.1186/1472-6947-12-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daei A., Soleymani M. R., Ashrafi-Rizi H., Zargham-Boroujeni A., Kelishadi R. (2020). Clinical information seeking behavior of physicians: A systematic review. International Journal of Medical Informatics, 139, 104144. 10.1016/j.ijmedinf.2020.104144 [DOI] [PubMed] [Google Scholar]
- Del Fiol G., Mostafa J., Pu D., Medlin R., Slager S., Jonnalagadda S. R., Weir C. R. (2016). Formative evaluation of a patient-specific clinical knowledge summarization tool. International Journal of Medical Informatics, 86, 126–134. 10.1016/j.ijmedinf.2015.11.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dillon E., Chuang J., Gupta A., Tapper S., Lai S., Yu P., Ritchie C., Tai-Seale M. (2017). Provider perspectives on advance care planning documentation in the electronic health record: The experience of primary care providers and specialists using advance health-care directives and physician orders for life-sustaining treatment. American Journal of Hospice and Palliative Medicine, 34, 918–924. 10.1177/1049909117693578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dwairy M., Dowell A. C., Stahl J. -C. (2011). The application of foraging theory to the information searching behaviour of general practitioners. BMC Family Practice, 12, 90. 10.1186/1471-2296-12-90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eikey E., Chen Y., Zheng K. (2019). Unintended adverse consequences of health IT implementation: Workflow issues and their cascading effects. In Zheng K., Westbrook J., Kannampallil T. G., Patel V. L. (Eds.), Cognitive informatics: Reengineering clinical workflow for safer and more efficient care (pp. 31–43). Springer International Publishing. 10.1007/978-3-030-16916-9_3. [DOI] [Google Scholar]
- Endsley M. R. (1988). Design and evaluation for situation awareness enhancement. Proceedings of the Human Factors Society Annual Meeting, 32, 97–101. 10.1177/154193128803200221 [DOI] [Google Scholar]
- Endsley M. R. (1995). Toward a theory of situation awareness in dynamic systems. Human Factors, 37, 32–64. 10.1518/001872095779049543 [DOI] [Google Scholar]
- Endsley M. R., Jones D. G. (2012. a). Designing for situation awareness: An approach to user-centered design (2nd ed.). CRC Press. [Google Scholar]
- Endsley M. R., Jones D. G. (2012. b). SA demons: The enemies of situation awareness. In Endsley M. R., Jones D. G. (Eds.), Designing for situation awareness: An approach to user-centered design (2nd ed.). CRC Press. [Google Scholar]
- Endsley M. R., Jones D. G. (2012. c). What is situation awareness? In Endsley M. R., Jones D. G. (Eds.), Designing for situation awareness: An approach to user-centered design (2nd ed.,pp. 13–29). CRC Press. [Google Scholar]
- Ex Libris Group . (2020). Primo. ProQuest. https://purdue-primo-prod.hosted.exlibrisgroup.com/primo-explore/search?vid=PURDUE&mode=advanced&sortby=rank. [Google Scholar]
- Farrell L. J., Du S., Steege L. M., Cartmill R. S., Wiegmann D. A., Wetterneck T. B., Hoffmann A. E., Endsley M. R. (2017). Understanding cognitive requirements for EHR design for primary care teams. Proceedings of the International Symposium on Human Factors and Ergonomics in Health Care, 6, 15–16. 10.1177/2327857917061005 [DOI] [Google Scholar]
- Fiscella K., McDaniel S. H. (2018). The complexity, diversity, and science of primary care teams. American Psychologist, 73, 451–467. 10.1037/amp0000244 [DOI] [PubMed] [Google Scholar]
- Fischer S. H., Safran C., Gajos K. Z., Wright A. (2020). Visualization of electronic health record data for decision-making in diabetes and congestive heart failure. ACI Open, 4, e35–e43. 10.1055/s-0040-1702213 [DOI] [Google Scholar]
- Flanagan M. E., Saleem J. J., Millitello L. G., Russ A. L., Doebbeling B. N. (2013). Paper- and computer-based workarounds to electronic health record use at three benchmark institutions. Journal of the American Medical Informatics Association, 20, e59–e66. 10.1136/amiajnl-2012-000982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman A., Crosson J. C., Howard J., Clark E. C., Pellerano M., Karsh B. -T., Crabtree B., Jaén C. R., Cohen D. J. (2014). A typology of electronic health record workarounds in small-to-medium size primary care practices. Journal of the American Medical Informatics Association, 21, e78–e83. 10.1136/amiajnl-2013-001686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaba D. M., Howard S. K., Small S. D. (1995). Situation awareness in anesthesiology. Human Factors, 37, 20–31. 10.1518/001872095779049435 [DOI] [PubMed] [Google Scholar]
- González-González A., Dawes M., Sánchez-Mateos J., Riesgo-Fuertes R., Escortell-Mayor E., Sanz-Cuesta T., Hernández-Fernández T. (2007). Information needs and information-seeking behavior of primary care physicians. The Annals of Family Medicine, 5, 345–352. 10.1370/afm.681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorman P. N. (1995). Information needs of physicians. Journal of the American Society for Information Science, 46, 729–736. [DOI] [Google Scholar]
- Gorman P. N., Helfand M. (1995). Information seeking in primary care: How physicians choose which clinical questions to pursue and which to leave unanswered. Medical Decision Making, 15, 113–119. 10.1177/0272989X9501500203 [DOI] [PubMed] [Google Scholar]
- Greenhalgh T., Robert G., Macfarlane F., Bate P., Kyriakidou O., Peacock R. (2005). Storylines of research in diffusion of innovation: A meta-narrative approach to systematic review. Social Science & Medicine, 61, 417–430. 10.1016/j.socscimed.2004.12.001 [DOI] [PubMed] [Google Scholar]
- Harle C. A., DiIulio J., Downs S. M., Danielson E. C., Anders S., Cook R. L., Hurley R. W., Mamlin B. W., Militello L. G. (2019). Decision-centered design of patient information visualizations to support chronic pain care. Applied Clinical Informatics, 10, 719–728. 10.1055/s-0039-1696668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hazlehurst B., McMullen C. K., Gorman P. N. (2007). Distributed cognition in the heart room: How situation awareness arises from coordinated communications during cardiac surgery. Journal of Biomedical Informatics, 40, 539–551. 10.1016/j.jbi.2007.02.001 [DOI] [PubMed] [Google Scholar]
- Hettinger A. Z., Melnick E. R., Ratwani R. M. (2021). Advancing electronic health record vendor usability maturity: Progress and next steps. Journal of the American Medical Informatics Association, 319. 10.1093/jamia/ocaa329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howe J. L., Adams K. T., Hettinger A. Z., Ratwani R. M. (2018). Electronic health record usability issues and potential contribution to patient harm. JAMA, 319, 1276–1278. 10.1001/jama.2018.1171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine . (1996). Primary care: America’s health in a new era. The National Academies Press. 10.17226/5152. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine . (2012). Health it and patient safety: Building safer systems for better care. National Academies Press (US). 10.17226/13269. [DOI] [PubMed] [Google Scholar]
- International Organization for Standardization . (2018). Usability: Definitions and concepts. International Organization for Standardization. [Google Scholar]
- Karsh B.-T., Weinger M. B., Abbott P. A., Wears R. L. (2010). Health information technology: Fallacies and sober realities. Journal of the American Medical Informatics Association, 17, 617–623. 10.1136/jamia.2010.005637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koopman R. J., Steege L. M. B., Moore J. L., Clarke M. A., Canfield S. M., Kim M. S., Belden J. L. (2015). Physician information needs and electronic health records (EHRs): Time to reengineer the clinic note. The Journal of the American Board of Family Medicine, 28, 316–323. 10.3122/jabfm.2015.03.140244 [DOI] [PubMed] [Google Scholar]
- Menon S., Murphy D. R., Singh H., Meyer A. N. D., Sittig D. F. (2016). Workarounds and test results follow-up in electronic health record-based primary care. Applied Clinical Informatics, 7, 543–559. 10.4338/ACI-2015-10-RA-0135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metke-Jimenez A., Harrap K., Conlan D., Gibson S., Pearson J., Hansen D. (2019). A smart on FHIR prototype for genomic test ordering. Studies in Health Technology and Informatics, 266, 121–126. 10.3233/SHTI190783 [DOI] [PubMed] [Google Scholar]
- Militello L. G., Hurley R. W., Cook R. L., Danielson E. C., Diiulio J., Downs S. M., Anders S., Harle C. A. (2020). Primary care clinicians’ beliefs and strategies for managing chronic pain in an era of a national opioid epidemic. Journal of General Internal Medicine, 35, 3542–3548. 10.1007/s11606-020-06178-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy D. R., Giardina T. D., Satterly T., Sittig D. F., Singh H. (2019). An exploration of barriers, facilitators, and suggestions for improving electronic health record inbox-related usability: A qualitative analysis. JAMA Network Open, 2, e1912638. 10.1001/jamanetworkopen.2019.12638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Academy of Medicine . (2019). Taking action against clinician burnout: A systems approach to professional well-being. The National Academies Press. 10.17226/25521. [DOI] [PubMed] [Google Scholar]
- Nibbelink C. W., Brewer B. B. (2018). Decision-making in nursing practice: An integrative literature review. Journal of Clinical Nursing, 27, 917–928. 10.1111/jocn.14151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office of the National Coordinator for Health Information Technology . (2019, September 10). What is an electronic health record (EHR)? Retrieved February 1, 2021 from https://www.healthit.gov/faq/what-electronic-health-record-ehr
- Ostropolets A., Chen R., Zhang L., Hripcsak G. (2020). Characterizing physicians’ information needs related to a gap in knowledge unmet by current evidence. JAMIA Open, 3, 281–289. 10.1093/jamiaopen/ooaa012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pawson R., Greenhalgh T., Harvey G., Walshe K. (2005). Realist review--a new method of systematic review designed for complex policy interventions. Journal of Health Services Research & Policy, 10 Suppl 1, 21–34. 10.1258/1355819054308530 [DOI] [PubMed] [Google Scholar]
- Pet D. B., Holm I. A., Williams J. L., Myers M. F., Novak L. L., Brothers K. B., Wiesner G. L., Clayton E. W. (2019). Physicians’ perspectives on receiving unsolicited genomic results. Genetics in Medicine, 21, 311–318. 10.1038/s41436-018-0047-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell L., Sittig D. F., Chrouser K., Singh H. (2020). Assessment of health information technology–related outpatient diagnostic delays in the US Veterans Affairs health care system: A qualitative study of aggregated root cause analysis data. JAMA Network Open, 3, e206752. 10.1001/jamanetworkopen.2020.6752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ratwani R. M., Benda N. C., Hettinger A. Z., Fairbanks R. J. (2015). Electronic health record vendor adherence to usability certification requirements and testing standards. JAMA, 314, 1070–1071. 10.1001/jama.2015.8372 [DOI] [PubMed] [Google Scholar]
- Risser D. T., Rice M. M., Salisbury M. L., Simon R., Jay G. D., Berns S. D. (1999). The potential for improved teamwork to reduce medical errors in the emergency department. Annals of Emergency Medicine, 34, 373–383. 10.1016/s0196-0644(99)70134-4 [DOI] [PubMed] [Google Scholar]
- Rittenhouse D. R., Wiley J. A., Peterson L. E., Casalino L. P., Phillips R. L. (2020). Meaningful use and medical home functionality in primary care practice. Health Affairs, 39, 1977–1983. 10.1377/hlthaff.2020.00782 [DOI] [PubMed] [Google Scholar]
- Robelia P. M., Kashiwagi D. T., Jenkins S. M., Newman J. S., Sorita A. (2017). Information transfer and the hospital discharge summary: National primary care provider perspectives of challenges and opportunities. Journal of the American Board of Family Medicine, 30, 758–765. 10.3122/jabfm.2017.06.170194 [DOI] [PubMed] [Google Scholar]
- Rogers M., Zach L., An Y., Dalrymple P. (2012). Capturing information needs of care providers to support knowledge sharing and distributed decision making. Applied Clinical Informatics, 3, 1–13. 10.4338/ACI-2011-08-CR-0053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roman L. C., Ancker J. S., Johnson S. B., Senathirajah Y. (2017). Navigation in the electronic health record: A review of the safety and usability literature. Journal of Biomedical Informatics, 67, 69–79. 10.1016/j.jbi.2017.01.005 [DOI] [PubMed] [Google Scholar]
- Rotenstein L., Tucker S., Kakoza R., Tishler L., Zai A., Wu C. (2016). The critical components of an electronic care plan tool for primary care: An exploratory qualitative study. Journal of Innovation in Health Informatics, 23, 529–533. 10.14236/jhi.v23i2.836 [DOI] [PubMed] [Google Scholar]
- Saleem J. J., Herout J., Wilck N. R. (2016). Function-specific design principles for the electronic health record. Proceedings of the Human Factors and Ergonomics Society Annual Meeting, 60, 578–582. 10.1177/1541931213601133 [DOI] [Google Scholar]
- Sauer J., Sonderegger A., Heyden K., Biller J., Klotz J., Uebelbacher A. (2019). Extra-laboratorial usability tests: An empirical comparison of remote and classical field testing with lab testing. Applied Ergonomics, 74, 85–96. 10.1016/j.apergo.2018.08.011 [DOI] [PubMed] [Google Scholar]
- Savoy A., Frankel R., Weiner M. (2021). Clinical thinking via electronic note templates: Who benefits? Journal of General Internal Medicine, 36, 577–579. 10.1007/s11606-020-06376-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savoy A., Militello L., Diiulio J., Midboe A. M., Weiner M., Abbaszadegan H., Herout J. (2019). Cognitive requirements for primary care providers during the referral process: Information needed from and interactions with an electronic health record system. International Journal of Medical Informatics, 129, 88–94. 10.1016/j.ijmedinf.2019.05.027 [DOI] [PubMed] [Google Scholar]
- Savoy A., Militello L. G., Patel H., Flanagan M. E., Russ A. L., Daggy J. K., Weiner M., Saleem J. J. (2018). A cognitive systems engineering design approach to improve the usability of electronic order forms for medical consultation. Journal of Biomedical Informatics, 85, 138–148. 10.1016/j.jbi.2018.07.021 [DOI] [PubMed] [Google Scholar]
- Singh H., Giardina T. D., Petersen L. A., Smith M. W., Paul L. W., Dismukes K., Bhagwath G., Thomas E. J. (2012). Exploring situational awareness in diagnostic errors in primary care. BMJ Quality & Safety, 21, 30–38. 10.1136/bmjqs-2011-000310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh H., Petersen L. A., Thomas E. J. (2006). Understanding diagnostic errors in medicine: A lesson from aviation. Quality and Safety in Health Care, 15, 159–164. 10.1136/qshc.2005.016444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh H., Spitzmueller C., Petersen N. J., Sawhney M. K., Smith M. W., Murphy D. R., Espadas D., Laxmisan A., Sittig D. F. (2013). Primary care practitioners’ views on test result management in EHR-enabled health systems: A national survey. Journal of the American Medical Informatics Association, 20, 727–735. 10.1136/amiajnl-2012-001267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinsky C. A., Beasley J. W., Simmons G. E., Baron R. J. (2014). Electronic health records: Design, implementation, and policy for higher-value primary care. Annals of Internal Medicine, 160, 727–728. 10.7326/M13-2589 [DOI] [PubMed] [Google Scholar]
- Sitterding M. C., Broome M. E., Everett L. Q., Ebright P. (2012). Understanding situation awareness in nursing work: A hybrid concept analysis. Advances in Nursing Science, 35, 77–92. [DOI] [PubMed] [Google Scholar]
- Smith M. W., Hughes A. M., Brown C., Russo E., Giardina T. D., Mehta P., Singh H. (2019). Test results management and distributed cognition in electronic health record-enabled primary care. Health Informatics Journal, 25, 1549–1562. 10.1177/1460458218779114 [DOI] [PubMed] [Google Scholar]
- Stanton N. A., Salmon P. M., Walker G. H., Salas E., Hancock P. A. (2017). State-of-science: Situation awareness in individuals, teams and systems. Ergonomics, 60, 449–466. 10.1080/00140139.2017.1278796 [DOI] [PubMed] [Google Scholar]
- Temte J. L., Beasley J. W., Holden R. J., Karsh B. -T., Potter B., Smith P., O’Halloran P. (2020). Relationship between number of health problems addressed during a primary care patient visit and clinician workload. Applied Ergonomics, 84, 103035. 10.1016/j.apergo.2019.103035 [DOI] [PubMed] [Google Scholar]
- Wauben L. S. G. L., Dekker-van Doorn C. M., van Wijngaarden J. D. H., Goossens R. H. M., Huijsman R., Klein J., Lange J. F. (2011). Discrepant perceptions of communication, teamwork and situation awareness among surgical team members. International Journal for Quality in Health Care, 23, 159–166. 10.1093/intqhc/mzq079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weir C. R., Staggers N., Gibson B., Doing-Harris K., Barrus R., Dunlea R. (2015). A qualitative evaluation of the crucial attributes of contextual information necessary in EHR design to support patient-centered medical home care. BMC Medical Informatics and Decision Making, 15, 1–8. 10.1186/s12911-015-0150-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong G., Greenhalgh T., Westhorp G., Buckingham J., Pawson R. (2013). RAMESES publication standards: Meta-narrative reviews. BMC Medicine, 11, 20. 10.1186/1741-7015-11-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodward M., De Pennington N., Grandidge C., McCulloch P., Morgan L. (2020). Development and evaluation of an electronic Hospital referral system: A human factors approach. Ergonomics, 63, 710–723. 10.1080/00140139.2020.1748232 [DOI] [PubMed] [Google Scholar]
- Wright M. C., Taekman J. M., Endsley M. R. (2004). Objective measures of situation awareness in a simulated medical environment. Quality and Safety in Health Care, 13, i65–i71. 10.1136/qshc.2004.009951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng K., Abraham J., Novak L. L., Reynolds T. L., Gettinger A. (2016). A survey of the literature on unintended consequences associated with health information technology: 2014–2015. Yearbook of Medical Informatics, 25, 13–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng K., Ratwani R. M., Adler-Milstein J. (2020). Studying workflow and workarounds in electronic health record–supported work to improve health system performance. Annals of Internal Medicine, 172, S116–S122. 10.7326/M19-0871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zulman D. M., Shah N. H., Verghese A. (2016). Evolutionary pressures on the electronic health record: Caring for complexity. JAMA: The Journal of the American Medical Association, 316, 923–924. [DOI] [PubMed] [Google Scholar]