Abstract
Mental health issues often result in significant impairment and financial challenges, both at home and in the workplace. Solutions vary widely in their usage and cost-effectiveness. This study presents an analysis of medical and prescription drug spending and utilization data for the employees of 4 companies who were eligible for an evidence-based workforce mental health program (WMHP). A variation of coarsened exact matching paired WMHP users to nonusers, based on demographics, location, and medical factors. Individuals included 2791 pairs of members whose medical claims were incurred in 2018 and 3883 pairs with claims in 2019. Using a cost efficiency measurement process, mean cost and utilization per person per year (PPPY) were compared. WMHP users had lower medical (−$2295 in 2018; −$2304 in 2019) and prescription drug spending (−$295 in 2018; −$312 in 2019). Over half of the cost reduction (−$1252 in 2018; −$1211 in 2019) resulted from shifting therapy services from the medical benefit to WMHP. WMHP users attended about 12 sessions PPPY, whereas the comparison group of nonusers attended about 7 mental health office visits PPPY under the medical benefit. WMHP users had more mental health-related visits in both years, but had fewer visits on the medical plan, and fewer emergency department visits for mental health than comparison group members. These results provide evidence that high-quality, evidence-based mental health services can reduce total expenditures and change utilization patterns. Evidence-based WMHP may represent a prudent investment for employers in providing mental health care to employees.
Keywords: mental health, workforce mental health, cost-effectiveness, employee assistance program, therapy, health care claims
Introduction
Mental health challenges present significant quality-of-life and financial burdens for employees and employers. Somewhere between 30% and 50% of adults experience mental illness over their lifetimes,1,2 resulting in more than $200 billion annually in health care utilization and lost work productivity.3,4 Mental health concerns remain among the top contributors of disability worldwide.5 Within the workplace, acute and chronic mental health conditions result in more days of work lost and a higher likelihood of working while impaired,6,7 as well as higher employee turnover.8 Providing appropriate mental health care to those in the workforce could help to alleviate these challenges and reduce suffering.9
For many employees, mental health care services are provided through employer-sponsored health insurance. Despite mandates of parity in the insurance coverage of physical and mental health services in the United States, disparities between mental and physical health care coverage and quality still exist.10 One significant barrier to obtaining mental health care is the significant financial burden that results, as individuals with mental health conditions experience high cost sharing and out-of-network spending responsibilities.11,12
In addition, many individuals have difficulty accessing mental health services in a timely manner due to mental health care provider shortages,13,14 logistical challenges presented by outdated or inaccurate insurance directories,15 and even discrimination within the search for care.16 If someone can find a provider within their health insurance plan network, they still may not have found a provider who performs evidence-based treatment (EBT), which is the gold standard17 for improvement in clinical outcomes and value-based care. Barriers to accessing high-quality care remain high,14 whereas the need for mental health services has increased, nearly doubling in the past 30 years.2
Inadequately treated mental health conditions, whether caused by access challenges or nonevidence-based practice, also impact physical functioning and disease-related spending. Even among individuals with similar levels of chronic physical illness, living with a mental health condition results in greater health care resource utilization and costs, due to more hospitalizations, longer hospital stays, and more emergency department (ED) visits.18 These increased costs are shared by individuals and employers. According to the Kaiser Family Foundation, the average employer-sponsored health care premium in 2021 ranged from roughly $7700 for individuals to about $22,000 for families, representing a 22% increase over the past 5 years and a 47% increase over the past 10 years.19
To alleviate the burden of workforce mental health challenges, employers continue to search for cost-effective or cost-savings solutions for employees. Workforce mental health programs (WMHPs) are comprehensive mental health and wellness programs targeted at employed populations that aim to fill this critical need and gap in the health care system. These programs aim to provide a focused investment in mental health, with the potential to shift ineffective spending for mental health concerns away from the medical insurance plan.
The broad value of a focused investment on employees' mental health has been described in the literature, with many traditional employee-assistance programs (EAPs) showing a positive return on investment for employers.3,20,21 Cost-savings and cost-effectiveness vary greatly, however, by type of intervention (eg, EBT or not evidence based), employer characteristics (eg, size, corporation type), and treatment focus (eg, diagnoses covered by the EAP).22 Providing evidence-based treatment for mental health conditions in general has been demonstrated as cost-effective,23,24 including preliminary evidence for cost-effectiveness for EBT for depression in the workplace.20
Challenges in methodology and analysis, however, limit the generalizability of these findings to WMHP. For example, many studies on EAPs and WMHP unreliably project savings from a small number of users over a brief period of time to an entire population over years,7,25 whereas a preferred method would be to examine actual usage of the WMHP and health care expenditure data over an extended period of time.
Despite high need and a general perception that these programs can be effective, the quality of care provided by WMHPs varies greatly, with many traditional EAPs mirroring the challenges of finding care through a health insurance plan (eg, troubles with access, session limits, providers who are not offering EBT).21,26,27 WMHPs providing EBT in psychotherapy show high rates of symptom reduction and clinical improvements for those who use their services.28,29 Services using exclusively EBT also demonstrate reductions in employee turnover, compared with individuals accessing usual care in the community.8
Although clinical improvements and impacts on workplace outcomes have been demonstrated by WMHP using EBT, more research is needed to demonstrate the financial value of providing EBT through WMHP using real-world data from health care claims. To that end, the objective of this study was to examine differences in medical, pharmacy, and mental health care utilization and expenditures between individuals who utilize a WMHP providing EBT and individuals who do not. The hypothesis is that individuals who utilize the evidence-based WMHP will have lower medical and pharmacy costs, for both mental health- and nonmental health-related claims.
Evidence-Based Workforce Mental Health Solution
Workforce mental health services were offered to eligible individuals through Lyra Health's WMHP, partnering with Lyra Clinical Associates, to self-referring individuals and their dependents, as a mental health benefit from their employers. Individuals seeking care accessed providers through an online portal that paired them with options for providers who provided EBT for their specific clinical needs. Appointments could be scheduled with a provider immediately through a connected calendar. All costs of care for these services were covered by the employer, with no cost sharing for the employee.
Providers are selected after rigorous evaluation and supervising processes to evaluate the quality of therapy and usage of EBTs, hiring only 4%–9% of applicants. All interventionists receive ongoing supervision, continuing education, and evaluation for performance in achieving clinical outcomes. The evidence-based services providing this WMHP are described in detail elsewhere.29
Study Design, Data Sources, and Methods
Study design
This study involved a third-party retrospective analysis conducted by Aon plc using deidentified data from 4 WMHP employer clients who together had over 50,000 eligible members. These data report eligibility for insurance coverage and insurance claims for health care services. Data were initially provided to Lyra Health using a fully executed business associate agreement. Deidentified data were transferred to Aon for independent review and analysis, with consent from employer clients. The use of deidentified data falls outside the regulatory definition of research involving human subjects, obviating the need for institutional review board (IRB) approval.
However, significant efforts were made to maintain data and individual confidentiality, consistent with data privacy and security safeguards described in the Health Insurance Portability and Accountability Act and the Health Information Technology for Economic and Clinical Health Act.
The study used eligibility and health care claims data to compare medical and prescription drug spending in 2018 and 2019 between 2 groups of people: those who utilized the WMHP services (WMHP users) and those who did not (the comparison group, also referred to as nonusers). Within these 2 groups, matched pairs were generated based on over 40 measures of geography, demographics, and medical and mental health comorbidities (Tables 1 and 2). The analysis utilized Aon's member-level cost efficiency measurement process, which is described in more detail below.
Table 1.
Sample Characteristics Before and After Matching for 2018
| |
2018 Before matching |
2018 After matching |
||||||
|---|---|---|---|---|---|---|---|---|
| |
WMHP users group |
Comparison group |
|
|
WMHP users group |
Comparison group |
|
s |
| Variable | n = 2990 |
n = 40,027 |
Standardized differences | P | n = 2791 |
n = 2791 |
Standardized differences | P |
| Mean or % | Mean or % | Mean or % | Mean or % | |||||
| Age | 31.08 | 27.29 | 0.311 | <0.001 | 30.81 | 31.44 | −0.078 | 0.004 |
| Adult (%) | 92.8% | 67.9% | 0.659 | <0.001 | 92.8% | 89.8% | 0.104 | <0.001 |
| Female (%) | 52.7% | 42.6% | 0.203 | <0.001 | 52.6% | 50.6% | 0.040 | 0.141 |
| MSA 1 | 31.3% | 25.8% | 0.122 | <0.001 | 31.9% | 29.6% | 0.051 | 0.056 |
| MSA 2 | 15.2% | 15.9% | −0.018 | 0.334 | 15.4% | 17.1% | −0.045 | 0.095 |
| MSA 3 | 12.0% | 9.0% | 0.096 | <0.001 | 11.7% | 12.4% | −0.021 | 0.434 |
| MSA 4 | 5.0% | 2.9% | 0.110 | <0.001 | 5.1% | 4.9% | 0.008 | 0.758 |
| MSA 5 | 5.2% | 2.6% | 0.130 | <0.001 | 4.8% | 3.7% | 0.059 | 0.028 |
| All other MSAs | 31.3% | 43.7% | −0.259 | <0.001 | 31.1% | 32.5% | −0.030 | 0.262 |
| Mood disorders (%) | 36.6% | 3.1% | 0.927 | <0.001 | 36.0% | 36.0% | 0.000 | 1.000 |
| Anxiety (%) | 64.2% | 4.0% | 1.646 | <0.001 | 64.3% | 54.2% | 0.208 | <0.001 |
| Adjustment disorders (%) | 42.3% | 1.9% | 1.115 | <0.001 | 42.5% | 24.3% | 0.394 | <0.001 |
| Attention-deficit disorders (%) | 5.0% | 1.7% | 0.182 | <0.001 | 4.7% | 4.7% | 0.000 | 1.000 |
| Alcohol/substance disorders (%) | 2.1% | 0.5% | 0.144 | <0.001 | 1.5% | 1.5% | 0.000 | 1.000 |
| Asthma(%) | 2.7% | 2.4% | 0.019 | 0.345 | 2.1% | 2.1% | 0.000 | 1.000 |
| Blood cell disease (%) | 0.4% | 0.3% | 0.019 | 0.365 | 0.1% | 0.1% | 0.000 | 1.000 |
| Cancer (%) | 0.7% | 0.5% | 0.016 | 0.438 | 0.1% | 0.1% | 0.000 | 1.000 |
| Secondary cancer (%) | 0.0% | 0.1% | −0.035 | 0.330 | 0.0% | 0.0% | 0.000 | 1.000 |
| Cardiovascular (%) | 2.8% | 2.6% | 0.012 | 0.545 | 1.7% | 1.7% | 0.000 | 1.000 |
| Lower back/disk diseases (%) | 16.9% | 8.4% | 0.257 | <0.001 | 14.7% | 14.7% | 0.000 | 1.000 |
| Diabetes (%) | 0.7% | 0.9% | −0.021 | 0.352 | 0.5% | 0.5% | 0.000 | 1.000 |
| Diabetes with complications (%) | 0.8% | 0.8% | 0.002 | 1.000 | 0.4% | 0.4% | 0.000 | 1.000 |
| Esophageal/upper GI diseases (%) | 2.2% | 1.4% | 0.055 | 0.002 | 1.2% | 1.2% | 0.000 | 1.000 |
| Hypertension (%) | 1.6% | 1.8% | −0.009 | 0.681 | 1.5% | 1.2% | 0.028 | 0.352 |
| Metabolic disorders (%) | 2.8% | 2.4% | 0.023 | 0.230 | 1.7% | 1.7% | 0.000 | 1.000 |
| Migraine/headache (%) | 4.8% | 2.5% | 0.128 | <0.001 | 3.6% | 3.6% | 0.000 | 1.000 |
| Multiple sclerosis (%) | 0.1% | 0.1% | 0.006 | 1.000 | 0.0% | 0.0% | 0.000 | 1.000 |
| Neurological disorders (%) | 4.4% | 2.9% | 0.078 | <0.001 | 2.8% | 2.8% | 0.000 | 1.000 |
| Osteoarthritis (%) | 0.7% | 0.6% | 0.014 | 0.500 | 0.1% | 0.1% | 0.000 | 1.000 |
| Pregnancy and labor (%) | 3.4% | 3.0% | 0.020 | 0.301 | 3.1% | 3.1% | 0.000 | 1.000 |
| Rheumatoid arthritis (%) | 0.3% | 0.2% | 0.012 | 0.628 | 0.1% | 0.1% | 0.000 | 1.000 |
GI, gastrointestinal; MSA, metropolitan statistical area; WMHP, workforce mental health program.
Table 2.
Sample Characteristics Before and After Matching for 2019
| |
2019 Before matching |
2019 After matching |
||||||
|---|---|---|---|---|---|---|---|---|
| |
WMHP users group |
Comparison group |
|
|
WMHP users group |
Comparison group |
|
|
| Variable | n = 4182 |
n = 41,437 |
|
|
n = 3883 |
n = 3883 |
|
|
| Mean or % | Mean or % | Standardized differences | P | Mean or % | Mean or % | Standardized differences | P | |
| Age | 31.36 | 27.21 | 0.342 | <0.001 | 31.11 | 31.81 | −0.088 | <0.001 |
| Adult (%) | 93.6% | 67.6% | 0.698 | <0.001 | 93.6% | 91.5% | 0.081 | <0.001 |
| Female (%) | 56.0% | 43.0% | 0.261 | <0.001 | 55.7% | 53.4% | 0.046 | 0.047 |
| MSA 1 | 30.9% | 26.6% | 0.094 | <0.001 | 31.4% | 28.8% | 0.056 | 0.013 |
| MSA 2 | 14.0% | 14.9% | −0.024 | 0.138 | 14.2% | 16.1% | −0.054 | 0.018 |
| MSA 3 | 10.2% | 8.5% | 0.059 | <0.001 | 9.7% | 11.0% | −0.043 | 0.057 |
| MSA 4 | 5.9% | 3.3% | 0.123 | <0.001 | 5.9% | 5.0% | 0.041 | 0.072 |
| MSA 5 | 5.6% | 2.5% | 0.155 | <0.001 | 5.2% | 3.2% | 0.096 | <0.001 |
| All other MSAs | 33.5% | 44.2% | −0.221 | <0.001 | 33.6% | 35.8% | −0.046 | 0.043 |
| Mood disorders (%) | 33.9% | 3.4% | 0.849 | <0.001 | 33.8% | 33.8% | 0.000 | 1.000 |
| Anxiety (%) | 67.0% | 4.4% | 1.726 | <0.001 | 66.6% | 54.2% | 0.254 | <0.001 |
| Adjustment disorders (%) | 35.4% | 2.0% | 0.949 | <0.001 | 35.6% | 25.5% | 0.219 | <0.001 |
| Attention-deficit disorders (%) | 5.0% | 1.7% | 0.183 | <0.001 | 4.0% | 4.0% | 0.000 | 1.000 |
| Alcohol/substance disorders (%) | 1.8% | 0.5% | 0.120 | <0.001 | 1.1% | 1.1% | 0.000 | 1.000 |
| Asthma (%) | 2.7% | 2.4% | 0.020 | 0.237 | 1.9% | 1.9% | 0.000 | 1.000 |
| Blood cell disease (%) | 0.4% | 0.4% | 0.005 | 0.859 | 0.1% | 0.1% | 0.000 | 1.000 |
| Cancer (%) | 0.6% | 0.6% | −0.005 | 0.823 | 0.2% | 0.2% | 0.000 | 1.000 |
| Secondary cancer (%) | 0.1% | 0.0% | 0.025 | 0.126 | 0.0% | 0.0% | 0.000 | 1.000 |
| Cardiovascular (%) | 3.5% | 2.6% | 0.050 | 0.001 | 2.2% | 2.2% | 0.000 | 1.000 |
| Lower back/disk diseases (%) | 18.6% | 9.2% | 0.276 | <0.001 | 17.2% | 17.2% | 0.000 | 1.000 |
| Diabetes (%) | 0.9% | 0.9% | −0.004 | 0.865 | 0.5% | 0.5% | 0.000 | 1.000 |
| Diabetes with complications (%) | 0.9% | 0.7% | 0.026 | 0.108 | 0.4% | 0.4% | 0.000 | 1.000 |
| Esophageal/upper GI diseases (%) | 2.7% | 1.4% | 0.093 | <0.001 | 1.6% | 1.6% | 0.000 | 1.000 |
| Hypertension (%) | 2.3% | 1.8% | 0.032 | 0.044 | 2.0% | 2.1% | −0.009 | 0.749 |
| Metabolic disorders (%) | 3.5% | 2.5% | 0.054 | <0.001 | 2.4% | 2.4% | 0.000 | 1.000 |
| Migraine/headache (%) | 5.3% | 2.6% | 0.140 | <0.001 | 3.9% | 3.9% | 0.000 | 1.000 |
| Multiple sclerosis (%) | 0.2% | 0.1% | 0.027 | 0.081 | 0.0% | 0.0% | 0.000 | 1.000 |
| Neurological disorders (%) | 4.7% | 3.1% | 0.082 | <0.001 | 2.9% | 2.9% | 0.000 | 1.000 |
| Osteoarthritis (%) | 0.6% | 0.6% | −0.004 | 0.882 | 0.3% | 0.3% | 0.000 | 1.000 |
| Pregnancy and labor (%) | 3.6% | 3.0% | 0.030 | 0.061 | 3.3% | 3.3% | 0.000 | 1.000 |
| Rheumatoid arthritis (%) | 0.2% | 0.2% | −0.008 | 0.747 | 0.0% | 0.0% | 0.000 | 1.000 |
GI, gastrointestinal; MSA, metropolitan statistical area; WMHP, workforce mental health program.
Study participants
Lyra Health's WMHP services were offered to all eligible employees and dependents by their employers. Engagement with WMHP services was voluntary and self-selected by the employee. For group assignment, individuals assigned to the WMHP users group included those who had at least 1 visit with the WMHP providers within a given year. Individuals in the comparison group were matched to WMHP users as mentioned above, to adjust for many nonprogram-related factors that might influence the cost of care. Individuals in both groups were able to use their medical benefit plans to engage in mental health care outside of the WMHP, if desired, and all such claims were included in the analyses.
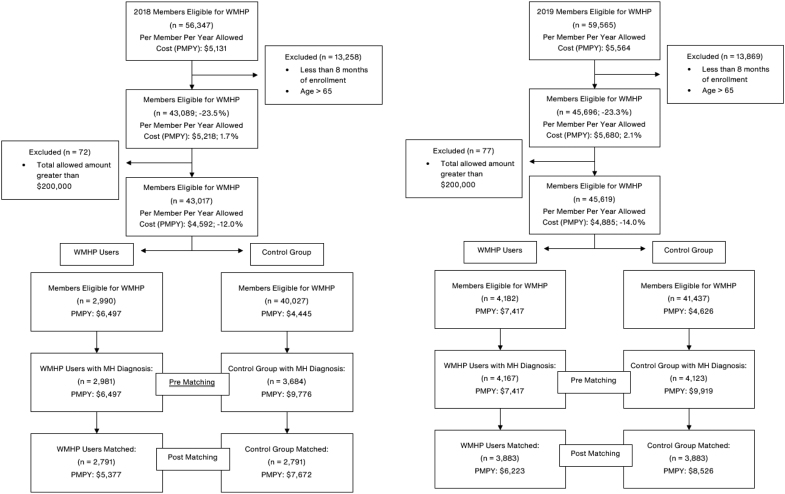
To be included in the analysis, individuals must have been under the age of 65 years with at least 8 months of access to the WMHP in the given year. Members whose cumulative medical spend over $200,000 per year (medical and pharmacy combined) were excluded (comprising <0.1% of members) from the main analysis, as their utilization patterns were statistical outliers that did not represent the overall population. Additional sensitivity analyses were conducted to evaluate the impact of different outlier cutoffs of $50,000 and $100,000 on the primary outcome of total medical, mental health, and prescription spending. Figure 1 shows a visualization of inclusion and exclusion criteria used for the study.
FIG. 1.
Participant flow diagram of inclusion and exclusion for 2018 and 2019. MH, mental health; WMHP, workforce mental health program.
Data sources
Eligibility data
The 4 employers who contributed data for this study worked within the technology, manufacturing, consumer goods, and transportation industries. As of 2019, the companies included in the analysis employed an average of 6000 employees. These employers provided Lyra Health with monthly data files, sharing up-to-date information on over 50,000 covered individuals who were eligible for health care services during 2018 or 2019, including demographic and geographic information. These covered individuals lived in 38 states around the country.
Geographic data and social determinants of health
Geographic information was summarized by incorporating the Area Deprivation Index (ADI)30,31 into the analyses. The ADI was calculated at the 5-digit ZIP code level, as a proxy of an individual's socioeconomic status (SES) and social determinants of health (SDOH). SES and SDOH factors related to education levels, income/employment rates, housing values, and household characteristics in a geographic area often influence cost and utilization analyses, so it was important to adjust for the impact of these factors.
Health insurance claims data
Detailed medical and pharmacy claims were collected from 2018 and 2019 on all WMHP users and nonusers. At least 3 months elapsed after the end of the year before claims data were obtained, to allow for processing. Pharmacy rebate data were not available and were not incorporated. Mental health-related spending was identified through primary diagnostic codes in the ICD-10 F-series, at the claim-line level. For WMHP users, mental health conditions were identified through both WMHP sessions and health plan benefit claims. Mental health service use among the comparison group was identified through medical and pharmaceutical claims only.
Participant and nonparticipant matching procedures
WMHP users were coded as such in this study based upon their use of at least 1 WMHP service. WMHP providers submitted diagnostic impressions that were then mapped to ICD-10 diagnosis codes by Lyra Health clinicians. A detailed mapping from diagnostic impression to ICD-10 diagnosis codes is included in the Appendix Table A1.
To apply the Aon cost efficiency measurement process, WMHP users were matched with a comparison group of nonusers, composed of eligible members at the same employers with closely matched geography, demographics, and medical and mental health comorbidities, for the same time periods. A derivation of coarsened exact matching32 was used to match cohorts. As originally described by Iacus et al, coarsened exact matching first involves dividing members into meaningful categories selected for each matching factor of interest.
Specifically, members were first divided into age groups, gender categories, geographic area categories, and according to the existence or not of several medical conditions, as noted below. Then, all members of the treatment and comparison groups who fell into the same categories were retained for the analysis; the rest were excluded. The Iacus et al32 method also suggests using case weights to account for the proportion of treatment and comparison group members who are in each factor category, then using their original data values (not the indicators of which factor categories they fell into) in the subsequent statistical analyses.
The Iacus et al method was simplified for this analysis, by avoiding the use of case weights. Age is the only continuous measure in this data set, so individuals were matched on tightly constructed age groups, which still produced a highly balanced set of WMHP users and comparison group members for analysis. More specifically, individuals were matched by gender first; then they were matched to others within ±3 years of their ages.
Individuals were then matched on presence or absence of 22 diagnosed medical conditions (Tables 1 and 2), and combinations of selected conditions. The chronic condition indicators considered for each member were based on primary (first listed) medical diagnostic codes, using the Chronic Condition Indicator and Clinical Classifications Software developed by the Agency for Healthcare Research and Quality Healthcare Cost and Utilization Project.33 When members had more than 1 mental health condition, a hierarchy was applied.
Specifically, when 2 or more disorders were present, members were coded according to the one that is typically thought to be more impactful in nature, resulting in greater levels of disability and incurring the most cost. Based upon the existing literature,2,4,5 mood disorders were anticipated to incur more costs than anxiety and adjustment disorders, which were in turn anticipated to incur more costs than attention-deficit disorders.
Next, WMHP users were matched to nonusers in the same geographic areas, when possible. First, an attempt was made to match members residing in the same metropolitan statistical area (MSA), based on a list of over 200 such areas across the United States. When a within-MSA match could not be found, members were matched at the state level. When that was not possible, members were not matched geographically, but were matched on the other factors mentioned above, searching across the country for the best demographic and condition level matches.
When no matches could be found (typically when members had a rare combination of disease and location values), individuals were removed from further analysis. For WMHP users who could have matched to more than 1 comparison group member, only 1 matching comparison group member was randomly selected for inclusion into the analyses. See Figure 1 for other inclusion and exclusion criteria and associated sample size reductions.
Statistical analyses
After matching was complete, mean health care expenditure values were calculated for all types of service, then for individual or combinations of multiple service types based on site or type of care. Differences in expenditures between groups were also examined by age, gender, and the ADI used as a proxy for their SDOH. Mean differences in expenditures between WMHP users and comparison group members were tested for statistical significance at the 95% confidence level, using 2-sample t-tests, assuming unequal variances; this is consistent with the approach recommended by Iacus et al.32
Results
Matching results
Matching resulted in 2791 member pairs in 2018 and 3883 member pairs in 2019. Overall, 93.3% of all WMHP users were matched with comparison group members in 2018, and 92.9% of all WMHP users were matched in 2019. The most challenging variable to match on was geography. In 2019, of the total population, 69.2% of the WMHP users were matched to comparison group members in the same MSA, an additional 9.1% of WMHP users were matched outside their MSA but within the same state, and 14.6% of WMHP users were matched nationally.
The remaining 7.1% were not matched and dropped from the study. Similar geography matching results were observed for 2018. Select smaller MSAs were combined with adjacent large MSAs in high-density areas (eg, New York, San Francisco, Denver, and Salt Lake City) to improve local sample sizes.
Pre- and postmatching results are presented in Tables 1 and 2 to describe the samples. Matching greatly reduced differences in means and percentages between all the variables used in the matching analyses. Standardized differences for all variables except 2 were below 0.10, which is commonly taken as a benchmark for adequate balance. The 2 exceptions were adjustment disorders and anxiety, which were 40%–60% higher among WMHP users than potential comparison group members before matching, but only about 10%–20% higher after matching.
Claims analyses
Results given in Tables 3 and 4 compare health expenditures between WMHP users and comparison group members. In both 2018 and 2019, WMHP users had significantly lower medical and pharmaceutical expenditures overall, as well as lower expenditures for mental health and nonmental health problems. In particular, WMHP users' mental health expenditures were about $1200–$1400 lower per member per year than comparison group members. This includes a significant difference in both inpatient and outpatient facility-related dollars in 2019, but not in 2018.
Table 3.
Medical, Nonmental Health, Mental Health, and Prescription Drug Expenditures for WMHP Users and Matched Comparison Group Members for 2018 and 2019
| |
2018 |
2019 |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Per participant per year spend | WMHP user (n = 2791) | Comparison group (n = 2791) | Difference | P | WMHP user (n = 3883) | Comparison group (n = 3883) | Difference | P | ||
| Medical spend | $4197 | $6196 | −$1999 | <0.0001 | $4960 | $6952 | −$1992 | <0.0001 | ||
| Medical nonmental health claims | $3663 | $4397 | −$734 | 0.0068 | $4510 | $5097 | −$586 | 0.0403 | ||
| Mental health spend | $534 | $1799 | −$1265 | <0.0001 | $450 | $1855 | −$1405 | <0.0001 | ||
| Facility mental health claim | $275 | $289 | −$13 | 0.8947 | $166 | $360 | −$194 | 0.0021 | ||
| Inpatient mental health claim | $81 | $136 | −$55 | 0.2262 | $70 | $174 | −$104 | 0.0113 | ||
| Outpatient mental health claim | $194 | $152 | $42 | 0.4354 | $96 | $186 | −$89 | 0.0045 | ||
| Professional mental health claim | $258 | $1510 | −$1252 | <0.0001 | $284 | $1495 | −$1211 | <0.0001 | ||
| Prescription drug claim | $1180 | $1476 | −$295 | <0.0001 | $1262 | $1574 | −$312 | <0.0001 | ||
| Total | $5377 | $7672 | −$2295 | <0.0001 | $6223 | $8526 | −$2304 | <0.0001 | ||
| Outlier threshold evaluation | n | Lyra utilizer | Control group | Difference | P | n | Lyra utilizer | Control group | Difference | P |
|---|---|---|---|---|---|---|---|---|---|---|
| Total—$50K threshold |
2711 |
$4307 |
$6376 |
−$2069 |
<0.0001 |
3730 |
$4772 |
$6408 |
−$1635 |
<0.0001 |
| Total—$100K threshold | 2776 | $5130 | $7236 | −$2106 | <0.0001 | 3851 | $5805 | $7712 | −$1907 | <0.0001 |
Expenditure amounts in dollars represent per person per year mean spending.
WMHP, workforce mental health program.
Table 4.
Medical and Prescription Drug Expenditures and Utilization for WMHP Users and Matched Comparison Group Members for 2018 and 2019
| |
2018 |
2019 |
||||||
|---|---|---|---|---|---|---|---|---|
| ED detail | WMHP utilizer (n = 2791) | Comparison group (n = 2791) | Difference | P | WMHP utilizer (n = 3883) | Comparison group (n = 3883) | Difference | P |
| Mental health ED | $9 | $27 | −$18 | 0.002 | $10 | $19 | −$9 | 0.109 |
| Nonmental health ED | $152 | $163 | −$11 | 0.634 | $169 | $209 | −$40 | 0.063 |
| Total ED spend | $162 | $190 | −$29 | 0.185 | $179 | $227 | −$49 | 0.029 |
| Mental health ED util/1000 | 5.6 | 20.2 | −14.6 | <0.001 | 6.7 | 11.5 | −4.8 | 0.036 |
| Nonmental health ED util/1000 | 115.4 | 136.0 | −20.6 | 0.109 | 118.4 | 144.4 | −26.0 | 0.018 |
| Total ED util/1000 | 121.0 | 156.2 | −35.2 | 0.009 | 125.1 | 155.9 | −30.8 | 0.006 |
| Prescription drug detail | ||||||||
| Generic drug | $188 | $284 | −$97 | <0.001 | $221 | $296 | −$75 | <0.001 |
| Brand drug | $388 | $457 | −$70 | 0.078 | $313 | $346 | −$34 | 0.215 |
| Specialty drug | $605 | $734 | −$130 | 0.352 | $728 | $931 | −$203 | 0.111 |
| Total prescription drug spend | $1180 | $1476 | −$296 | <0.001 | $1262 | $1574 | −$312 | <0.001 |
| Generic drug scripts/1000 | 3719.2 | 4770.8 | −1051.6 | <0.001 | 4034.6 | 5067.6 | −1033.0 | <0.001 |
| Brand drug scripts/1000 | 792.1 | 815.2 | −23.1 | 0.641 | 489.7 | 530.8 | −41.1 | 0.072 |
| Specialty drug scripts/1000 | 73.8 | 74.2 | −0.4 | 0.970 | 108.3 | 125.8 | −17.5 | 0.124 |
| Total prescription drug scripts/1000 | 4585.1 | 5660.2 | −1075.1 | <0.001 | 4632.6 | 5724.2 | −1091.6 | <0.001 |
Expenditure amounts in dollars represent per person per year spending; “util/1,000” represents the number of visits utilized per 1000 eligible people; “Generic Drug Scripts/1000,” “Brand Drug Scripts/1,000,” “Specialty Drug Scripts/1000” and “Total Prescription Drug Scripts/1,000” represent the number of prescriptions written per 1000 eligible people.
ED, emergency department; WMHP, workforce mental health program.
The overall directionality, magnitude, and statistical significance of results were maintained in the sensitivity analyses. Using a cutoff of cumulative spending of over $50,000 per year, WMHP users still had lower total spending on average (−$2069 in 2018, n = 2711; −$1635 in 2019, n = 3730; P's < 0.0001) than nonusers. Using a cutoff of cumulative spending of over $100,000 per year, WMHP users again had lower total spending on average (−$2106 in 2018, n = 2776; −$1907 in 2019, n = 3851; P's < 0.0001). Given the consistent pattern of results, and the desire to account for a very high proportion of spending, the threshold of $200,000 was maintained in the results shown below.
Regarding utilization, WMHP users engaged in an average of 12.7 visits with the WMHP in 2018 and 11.9 in 2019, compared with 1.2 and 1.4 visits, respectively, on the medical plan's mental health benefit. Individuals in the comparison group who did not use the WMHP services engaged in an average of 7.4 and 6.9 visits on the medical plan's mental health benefit in 2018 and 2019, respectively. WMHP users engaged in significantly more mental health-related visits both years, with a mean difference of 6.5 more visits in 2018 (P < 0.001) and a mean difference of 6.4 more visits in 2019 (P < 0.001). WHMP users had fewer visits on the medical plan's mental health benefit than comparison group members.
Utilization of the ED (Table 5) varied by year and specific outcome. Although total claims spending for mental health-related concerns was significantly lower per member per year in 2018 for WMHP users than among comparison group members, this was not the case in 2019. Total ED claims costs were, however, lower in 2019 for WMHP users than for comparison group members, but this was not the case in 2018. For both years, ED utilization for mental health concerns per 1000 members was significantly lower for WMHP users than for comparison group members. Nonmental health ED utilization was also significantly lower for WMHP users than for comparison group members in 2019.
Table 5.
Differences in Expenditures by Demographics and Area Deprivation Indices
| 2018 |
2019 |
|||||||
|---|---|---|---|---|---|---|---|---|
| WMHP utilizer (n = 2791) | Comparison group (n = 2791) | Difference | P | WMHP utilizer (n = 3883) | Comparison group (n = 3883) | Difference | P | |
| Male: age group in years | ||||||||
| 1–18 | $3091 | $6039 | −$2948 | 0.065 | $3371 | $4005 | −$634 | 0.491 |
| 19–29 | $3427 | $4950 | −$1523 | 0.003 | $4232 | $7896 | −$3664 | <0.001 |
| 30–39 | $4398 | $7010 | −$2612 | <0.001 | $5524 | $6865 | −$1341 | 0.051 |
| 40–49 | $7078 | $8109 | −$1031 | 0.628 | $6652 | $7473 | −$821 | 0.621 |
| 50–64 | $8189 | $6194 | $1995 | 0.606 | $10,423 | $6034 | $4389 | 0.224 |
| Total | $4327 | $6419 | −$2092 | <0.001 | $5178 | $7101 | −$1923 | <0.001 |
| Female: age group in years | ||||||||
| 1–18 | $2598 | $7819 | −$5221 | 0.006 | $2980 | $5878 | −$2898 | 0.022 |
| 19–29 | $4446 | $6362 | −$1916 | 0.001 | $4894 | $6902 | −$2008 | <0.001 |
| 30–39 | $7756 | $10,931 | −$3175 | 0.001 | $8983 | $11,872 | −$2889 | 0.002 |
| 40–49 | $10,842 | $10,269 | $573 | 0.698 | $9932 | $12,378 | −$2446 | 0.267 |
| 50–64 | $7264 | $8204 | −$940 | 0.713 | $8920 | $9705 | −$785 | 0.790 |
| Total | $6328 | $8914 | −$2586 | <0.001 | $7057 | $9775 | −$2718 | <0.001 |
| Area deprivation index groupings (higher values refer to greater deprivation related to social determinants of health) | ||||||||
| 0–20 | $5727 | $8383 | −$2656 | <0.001 | $6616 | $9564 | −$2948 | <0.001 |
| 21–40 | $4813 | $6469 | −$1656 | 0.015 | $6028 | $7261 | −$1233 | 0.114 |
| 41–60 | $4789 | $6696 | −$1907 | 0.018 | $4841 | $6612 | −$1771 | 0.034 |
| 61–80 | $4070 | $5732 | −$1662 | 0.376 | $5425 | $5857 | −$432 | 0.702 |
| 81–100 | $6946 | $4891 | $2055 | 0.431 | $5628 | $3177 | $2451 | 0.344 |
| Total | $5377 | $7672 | −$2295 | <0.001 | $6223 | $8526 | −$2303 | <0.001 |
Expenditure amounts in dollars represent per person per year mean spending.
WMHP, workforce mental health program.
WMHP users had lower overall prescription drug spending and a lower number of prescriptions filled per 1000 members than did comparison group members. By prescription subtype, this finding appeared to be driven primarily by generic drug costs and prescriptions.
When examined by age group (Table 5), all age groups showed lower health expenditures among WMHP user members than among comparison group members; differences were statistically significant among those under 40 years of age (P < 0.001). Differences in health care expenditures by ADI were seen only in areas with fewer deprivations related to SDOH, with WMHP users in these groups having lower expenditures.
Discussion
Overall, lower health care claims costs were found for individuals who used Lyra Health's WMHP services providing EBT than among the comparison group members who did not use these services. WMHP users also engaged in a greater number of visits specifically for mental health concerns with the WMHP, demonstrating that accessing EBT through the WMHP was feasible and sustained for many members, a factor previous research has shown can be a significant barrier in traditional EAPs and mental health care through a medical plan.11,21
Lower spending related to mental health-related ED visits, as well as ED utilization rates for mental health conditions, suggests that individuals receiving services through the WMHP may also have experienced fewer mental health emergencies because of engaging in care with the WMHP. Although these results were not consistently statistically significant across years, the lack of statistical significance could be a result of sample size or lower utilization rates of the ED.
Given the increasing burden of ED visits for mental health issues in the community,34,35 the alleviation of this burden reflects significant societal benefit of reduced utilization of this limited resource. WMHP users also had lower prescription costs and fewer prescriptions filled and claimed during the year, despite being matched on their medical conditions. This finding is consistent with other research stating that alleviation of mental health concerns can reduce spending overall for medical concerns.36,37
Differences in spending by age and program usage were only found for those under the age of 40 years. Overall spending increased after age 40 years, for both the WMHP and comparison groups. For older adults, it may be that other health care expenses (eg, those due to chronic illnesses such as diabetes or cardiac issues) make it more difficult to demonstrate the financial gains of treating mental health concerns. Given the average age of 31 years in this overall sample, sample sizes in the older age groups also may be too small to detect significant differences by age group.
Regarding the SDOH analysis, differences in spending were found among WMHP and comparison group members living in areas with lower ADI scores (ie, in those areas where relatively fewer deprivations related to SDOH). This pattern could be attributed to differences in care-seeking behavior by individuals who had better access to care and greater financial resources than those who are represented in areas with greater deprivation of SDOH. Future research is needed to examine and understand patterns of WMHP usage by SDOH.
Although participant matching procedures closely adhered to established procedures for coarsened exact matching, there were some discrepancies in the distribution of mental health diagnoses before matching that were challenging to overcome. WMHP users were more likely to have adjustment disorders and to also have comorbid diagnoses (eg, both depression and anxiety) than the comparison group members. These discrepancies may also represent diagnostic challenges for individuals seeking care outside of the WMHP.
This challenge was approached using a research-informed hierarchical matching process to generate matches for people with multiple mental health conditions; however, the process had limitations. WMHP users likely had superior diagnostic data and labels before matching, due to their engagement with evidence-based mental health services that recommend diagnostic assessment and clarity for selecting the right treatment modality.17,38
Also, ICD-10 diagnosis codes for the WMHP were derived from expert reviews of clinical documentation in patients' medical records. Although research suggests this is a valid approach for categorizing diagnoses,39 diagnoses made for WMHP users may have differed in unknown ways from diagnoses that would have been made if these patients had sought care through the health plan.
A few more limitations of this study are worth noting. First, there are unmeasured factors, such as socioeconomic variables and differences in job types, even within employers, that may have impacted study outcomes. In addition, unmeasured cultural factors and engagement preferences may have influenced differential care-seeking behaviors and, therefore, the observed cost patterns. WMHP users and comparison group members pursued different forms of care for their mental health conditions. Matching reduced some of the impact of known influential factors driving their choices, however, unmeasured factors likely played a role as well.
For example, factors such as urgency for treatment or schedule flexibility may have impacted the selection of 1 service over another. Mental health care sought from some health plans may require waiting days to weeks for appointments, whereas the WHMP typically scheduled visits within 1 to 2 days of request.
Next, research suggests that stigma and privacy concerns surrounding mental health care may prevent some people from engaging with a WMHP, even when it is available.40 Those concerns were not measured in this study and could have played a role in service selection.
An additional factor that may impact differential treatment choices is the out-of-pocket cost of mental health care that would be obtained through the health plan. This cost may be prohibitive for some due to limited financial resources, resulting in them seeking care through the WMHP at no out-of-pocket cost. A more comprehensive study would leverage randomization to treatment type (eg, a randomized controlled trial comparing a WMHP with health plan-provided treatment) to help account for these unmeasured factors.
Next, the analyses did not account for the cost of the WMHP to employers, so a return on investment in the WMHP is not presented. However, it is important to note that there was no cost to the employees to use the WMHP, which is a facilitating factor in seeking appropriate mental health care for employees.41 The reduction of this financial barrier may have resulted in more appropriate utilization of mental health services by WMHP users living with mental health conditions. Their return on investment (ie, better care at zero cost) was clearly positive. Whether this translated to a positive return on investment for their employers is still unknown.
Also, although nearly all claim totals and utilization metrics found lower health care claims cost and utilization rates for WMHP users than for comparison group members, the analyses performed here describe the experiences limited to 4 employer clients who allowed their data to be used in the study. This limits the generalizability of these findings to the populations described within this analysis. Future research should be conducted on the cost implications of WMHP use among employers in all industry categories.
In addition, the collection of detailed demographic information, such as race, ethnicity, and income, would facilitate future statements about the generalizability and applicability of the sample's findings. At the time of analysis, these data were not available.
Although the limitations described above are important, the results of this study still provide preliminary support for the hypothesis that using WMHP services for mental health concerns can be cost-effective, especially for individual users. With regard to quality clinical care, the services provided by Lyra's WMHP focus on EBT, resulting in superior rates of clinical symptom improvement and recovery not demonstrated by other solutions.28,29 Future research should evaluate the net cost of WMHP services to many more employers, to help inform decision making and enhance generalizability of the findings. Future research might also address the impact of WMHP providing EBT on employee productivity and turnover.
Many workforce mental health solutions now also involve a suite of services targeted at supporting mental health wellness,42 from prevention to treatment. Future research should expand the scope of evaluation to additional services offered through these programs and investigate potential savings and return on investment. In conclusion, this study provides support for the statement that EBT through a WMHP for mental health care may reduce overall medical insurance spending for those who make use of these services.
Acknowledgments
The authors express their appreciation for the Lyra providers who work every day to support clients in leading more fulfilling, productive lives.
Appendix
Appendix Table A1.
Mapping from Diagnostic Impression to ICD-10 Diagnosis Codes
| Lyra impression | ICD-10 | ICD-10 description | CCS categories |
|---|---|---|---|
| Anger management | f4320 | Adjustment disorder, unspecified | Adjustment disorders |
| Behavioral problems | f4320 | Adjustment disorder, unspecified | Adjustment disorders |
| Career issues | f4320 | Adjustment disorder, unspecified | Adjustment disorders |
| Communication problems | f4320 | Adjustment disorder, unspecified | Adjustment disorders |
| Divorce | f4320 | Adjustment disorder, unspecified | Adjustment disorders |
| Family conflict | f4320 | Adjustment disorder, unspecified | Adjustment disorders |
| Grief | f4320 | Adjustment disorder, unspecified | Adjustment disorders |
| Life transition | f4320 | Adjustment disorder, unspecified | Adjustment disorders |
| Life purpose | f4320 | Adjustment disorder, unspecified | Adjustment disorders |
| Other | f4320 | Adjustment disorder, unspecified | Adjustment disorders |
| Parenting | f4320 | Adjustment disorder, unspecified | Adjustment disorders |
| Parenting child behavior issues | f4320 | Adjustment disorder, unspecified | Adjustment disorders |
| Relationship issues | f4320 | Adjustment disorder, unspecified | Adjustment disorders |
| Self-esteem | f4320 | Adjustment disorder, unspecified | Adjustment disorders |
| Substance abuse | f1010 | Alcohol abuse, uncomplicated | Alcohol-related disorders |
| Anxiety | f419 | Anxiety disorder, unspecified | Anxiety disorders |
| OCD | f429 | Obsessive-compulsive disorder, unspecified | Anxiety disorders |
| Panic | f419 | Anxiety disorder, unspecified | Anxiety disorders |
| Stress | f419 | Anxiety disorder, unspecified | Anxiety disorders |
| Trauma | f4310 | Post-traumatic stress disorder, unspecified | Anxiety disorders |
| ADHD | f909 | Attention-deficit hyperactivity disorder, unspecified type | Attention-deficit conduct and disruptive behavior disorders Mental |
| Bipolar disorder | f319 | Bipolar disorder, unspecified | Mood disorders |
| Depression sadness | f329 | Major depressive disorder, single episode, unspecified | Mood disorders |
ADHD, attention deficit hyperactivity disorder; CCS, Clinical Classifications Software; OCD, obsessive compulsive disorder.
Authors' Contributions
Mr Penev contributed to funding acquisition, methodology, project administration, software, and writing—review and editing. Ms Zhao contributed to data curation, formal analysis, investigation, project administration, software, validation, visualization, writing—original draft, and writing—review and editing. Dr. Lee contributed to conceptualization, project administration, writing—original draft and revised drafts, and writing—review and editing.
Dr. Chen contributed to conceptualization, funding acquisition, investigation, methodology, resources, supervision, writing—original draft and revised drafts, and writing—review and editing. Dr. Metcalfe contributed to methodology, formal analysis, investigation, supervision, validation, visualization, writing—original draft, and writing—review and editing. Dr. Ozminkowski contributed to formal analysis, methodology, supervision, visualization, writing—original and revised drafts, and writing—review and editing.
Author Disclosure Statement
Mr Penev, Ms Zhao, Dr. Metcalfe, and Dr. Ozminkowski are employed by Aon plc, and receive income and/or equity from Aon plc. Dr. Lee is employed by Lyra Health, receives income from Lyra Health, and has been granted equity in Lyra Health. Dr. Chen is employed by Lyra Health and Lyra Clinical Associates, receives income from Lyra Health and Lyra Clinical Associates, and has been granted equity in Lyra Health. Their employment status and incomes were not affected by participation in this study.
Funding Information
The study was funded by Lyra Health. The funder of the study was involved in study design, data interpretation, and writing of the report, and informed during data collection and data analysis. Aon plc coauthors lead had full access to all the data in the study and take joint responsibility for the decision to submit the article for publication.
References
- 1. Takayanagi Y, Spira AP, Roth KB, et al. Accuracy of Reports of Lifetime Mental and Physical Disorders: results from the Baltimore Epidemiological Catchment Area Study. JAMA Psychiatry 2014;71:273–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. GBD 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry 2022;9:137–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Goetzel RZ, Ozminkowski RJ, Sederer LI, et al. The business case for quality mental health services: why employers should care about the mental health and well-being of their employees. J Occup Environ Med 2002;44:320–330. [DOI] [PubMed] [Google Scholar]
- 4. Roehrig C. Mental disorders top the list of the most costly conditions in the United States: $201 billion. Health Aff (Millwood) 2016;35:1130–1135. [DOI] [PubMed] [Google Scholar]
- 5. Greenberg PE, Fournier A-A, Sisitsky T, et al. The economic burden of adults with major depressive disorder in the United States (2010 and 2018). Pharmacoeconomics 2021;39:653–665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Grasso JR, Chen SY, Schneider R. Examining changes in presenteeism and clinical symptoms in a workforce mental health benefits program. J Workplace Behav Health 2022;0:1–14. [Google Scholar]
- 7. Joseph B, Walker A, Fuller-Tyszkiewicz M. Evaluating the effectiveness of employee assistance programmes: a systematic review. Eur J Work Organ Psychol 2018;27:1–15. [Google Scholar]
- 8. Falcon M, Chen CE, Bandari R, et al. Impact of evidence-based psychotherapy on employee retention. Med Res Arch 2021;9. DOI: 10.18103/mra.v9i11.2574. [DOI] [Google Scholar]
- 9. Chisholm D, Sweeny K, Sheehan P, et al. Scaling-up treatment of depression and anxiety: a global return on investment analysis. Lancet Psychiatry 2016;3:415–424. [DOI] [PubMed] [Google Scholar]
- 10. Creedon TB, Cook BL. Access to mental health care increased but not for substance use, while disparities remain. Health Aff (Millwood) 2016;35:1017–1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Xu WY, Song C, Li Y, et al. Cost-sharing disparities for out-of-network care for adults with behavioral health conditions. JAMA Netw Open 2019;2:e1914554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Benson NM, Song Z. Prices and cost sharing for psychotherapy in network versus out of network in the United States. Health Aff (Millwood) 2020;39:1210–1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Malowney M, Keltz S, Fischer D, et al. Availability of outpatient care from psychiatrists: a simulated-patient study in three U.S. Cities. Psychiatr Serv 2015;66:94–96. [DOI] [PubMed] [Google Scholar]
- 14. Peterson E, Busch S. Achieving mental health and substance use disorder treatment parity: a quarter century of policy making and research. Annu Rev Public Health 2018;39:421–435. [DOI] [PubMed] [Google Scholar]
- 15. Busch SH, Kyanko KA. Incorrect provider directories associated with out-of-network mental health care and outpatient surprise bills. Health Aff (Millwood) 2020;39:975–983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kugelmass H. “Sorry, I'm Not Accepting New Patients”: an audit study of access to mental health care. J Health Soc Behav 2016;57:168–183. [DOI] [PubMed] [Google Scholar]
- 17. APA Presidential Task Force on Evidence-Based Practice. Evidence-based practice in psychology. Am Psychol 2006;61:271–285. [DOI] [PubMed] [Google Scholar]
- 18. Sporinova B, Manns B, Tonelli M, et al. Association of mental health disorders with health care utilization and costs among adults with chronic disease. JAMA Netw Open 2019;2:e199910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kaiser Family Foundation. Kaiser Family Foundation 2021 Employer Health Benefits Survey. 2021. http://kff.org/report-section/ehbs-2021-summary-of-findings/#figurea Accessed January 31, 2023.
- 20. de Oliveira C, Cho E, Kavelaars R, et al. Economic analyses of mental health and substance use interventions in the workplace: a systematic literature review and narrative synthesis. Lancet Psychiatry 2020;7:893–910. [DOI] [PubMed] [Google Scholar]
- 21. Csiernik R, Cavell M, Csiernik B. EAP evaluation 2010–2019: what do we now know? J Workplace Behav Health 2021;36:105–124. [Google Scholar]
- 22. Goetzel RZ, Henke RM, Tabrizi M, et al. Do workplace health promotion (wellness) programs work? J Occup Environ Med 2014;56:927–934. [DOI] [PubMed] [Google Scholar]
- 23. Brettschneider C, Djadran H, Härter M, et al. Cost-utility analyses of cognitive-behavioural therapy of depression: a systematic review. Psychother Psychosom 2015;84:6–21. [DOI] [PubMed] [Google Scholar]
- 24. World Health Organization. WHO menu of cost-effective interventions for mental health. 2021. https://apps.who.int/iris/handle/10665/343074 Accessed January 31, 2023.
- 25. Bondar J, Babich Morrow C, Gueorguieva R, et al. Clinical and financial outcomes associated with a workplace mental health program before and during the COVID-19 pandemic. JAMA Netw Open 2022;5:e2216349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Langlieb AM, Langlieb ME, Xiong W. EAP 2.0: reimagining the role of the employee assistance program in the new workplace. Int Rev Psychiatry 2021;33:699–710. [DOI] [PubMed] [Google Scholar]
- 27. Attridge M. A Global perspective on promoting workplace mental health and the role of employee assistance programs. Am J Health Promot 2019;33:622–629. [DOI] [PubMed] [Google Scholar]
- 28. Owusu JT, Wang P, Wickham RE, et al. Real-world evaluation of a large-scale blended care-cognitive behavioral therapy program for symptoms of anxiety and depression. Telemed J E Health 2022;28:1412–1420. DOI: 10.1089/tmj.2021.0590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lungu A, Jun JJ, Azarmanesh O, et al. Blended care-cognitive behavioral therapy for depression and anxiety in real-world settings: pragmatic retrospective study. J Med Internet Res 2020;22:e18723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Maroko AR, Doan TM, Arno PS, et al. Integrating social determinants of health with treatment and prevention: a new tool to assess local area deprivation. Prev Chronic Dis 2016;13:E128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kind AJH, Buckingham WR. Making neighborhood-disadvantage metrics accessible—the neighborhood atlas. N Engl J Med 2018;378:2456–2458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Iacus SM, King G, Porro G. Causal inference without balance checking: coarsened exact matching. Polit Anal 2012;20:1–24. [Google Scholar]
- 33. Healthcare Cost and Utilization Project (HCUP) CCS. Clinical Classifications Software for ICD-9-CM. 2017.
- 34. Lo CB, Bridge JA, Shi J, et al. Children's mental health emergency department visits: 2007–2016. Pediatrics 2020;145:e20191536. [DOI] [PubMed] [Google Scholar]
- 35. Holland KM, Jones C, Vivolo-Kantor AM, et al. Trends in US emergency department visits for mental health, overdose, and violence outcomes before and during the COVID-19 pandemic. JAMA Psychiatry 2021;78:372–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Ross KM, Gilchrist EC, Melek SP, et al. Cost savings associated with an alternative payment model for integrating behavioral health in primary care. Transl Behav Med 2019;9:274–281. [DOI] [PubMed] [Google Scholar]
- 37. Highland J, Nikolajski C, Kogan J, et al. Impact of behavioral health homes on cost and utilization outcomes. Psychiatr Serv 2020;71:796–802. [DOI] [PubMed] [Google Scholar]
- 38. Scott K, Lewis CC. Using measurement-based care to enhance any treatment. Cogn Behav Pract 2015;22:49–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. First MB, Rebello TJ, Keeley JW, et al. Do mental health professionals use diagnostic classifications the way we think they do? A global survey. World Psychiatry 2018;17:187–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Newell CJ, Ricciardelli R, Czarnuch SM, et al. Police staff and mental health: barriers and recommendations for improving help-seeking. Police Pract Res 2022;23:111–124. [Google Scholar]
- 41. Walker ER, Cummings JR, Hockenberry JM, et al. Insurance status, use of mental health services, and unmet need for mental health care in the United States. Psychiatr Serv 2015;66:578–584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Wu A, Roemer EC, Kent KB, et al. Organizational best practices supporting mental health in the workplace. J Occup Environ Med 2021;63:e925–e931. [DOI] [PMC free article] [PubMed] [Google Scholar]