Abstract
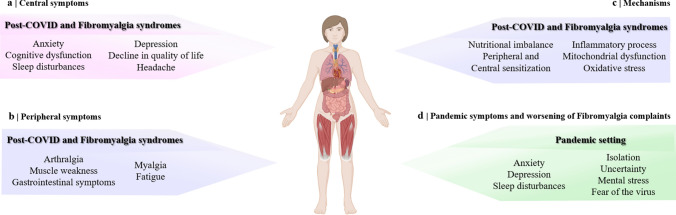
Fibromyalgia (FM) is a complex disease with an uncertain aetiology and intricate pathophysiology. Although its genesis is not fully explained, potential environmental factors, such as viral infections might trigger FM or worsen patients' clinical outcomes. The SARS-CoV-2 virus may affect central and peripheral nervous systems, leading to musculoskeletal, neurological, and psychological disturbances. These symptoms might persist at least 12 months beyond the recovery, often referred to as post-COVID syndrome, which resembles FM syndrome. In this sense, we argued the potential consequences of COVID-19 exclusively on FM syndrome. First, we have described post-COVID syndrome and its painful symptoms. Afterwards, we argued whether FM syndrome could be triggered or enhanced by COVID-19 infection or by numerous and persistent stressors imposed daily by the pandemic setting (isolation, uncertainty, depression, mental stress, generalized anxiety, and fear of the virus). In addition, we have demonstrated similarities between pathophysiological mechanisms and cardinal symptoms of FM and COVID-19, speculating that SARS-CoV-2 might represent a critical mediator of FM or an exacerbator of its symptoms once both syndromes share similar mechanisms and complaints. Therefore, pharmacologic and non-pharmacological approaches commonly used to treat FM could serve as strategic therapies to attenuate painful and neurological manifestations of post-COVID syndrome. Although it is still theoretical, clinicians and researchers should be alert of patients who develop symptoms similar to FM or those who had their FM symptoms increased post-COVID to manage them better.
Graphical Abstract
Keywords: SARS-CoV-2, Post-COVID syndrome, Musculoskeletal pain, Fatigue, Myalgia, Chronic pain
Introduction
Fibromyalgia (FM) is a common but intricate illness with unknown aetiology. It is classified as nociplastic pain, which arises from the altered function of pain-related sensory pathways in the nervous system, causing increased sensitivity (Fitzcharles et al. 2021). There are many potential triggering factors for FM, such as genetic predisposition, inactivity, obesity, stressful life events and environmental factors (Häuser et al. 2015; Sarzi-Puttini et al. 2020). The latter includes several infections of viral or bacterial origin that culminate in long febrile disorder, particularly if accompanied by long bed rest (Buskila et al. 2008; Häuser et al. 2015). Although the pathogenesis of FM is not fully understood, it is believed that abnormal host response due to the direct microorganism invasion or immunological process may be implicated in the development and chronicity of pain in chronic fatigue syndromes (Komaroff and Lipkin 2021). Besides, physical or mental stress related to infection is also a known factor associated with worsening FM pain (Häuser et al. 2015; Sarzi-Puttini et al. 2020). In light of the above, there is a growing idea that coronavirus disease (COVID) may impact the development or exacerbate FM syndrome.
The global pandemic of COVID 2019 has exhibited devastating potential, causing high morbidity and mortality rates worldwide (WHO 2023). Fortunately, due to the recent development of vaccines, the infection and mortality rates have decreased and are better controlled. Patients with COVID-19 experience acute symptoms during the early illness, with acute respiratory distress being the most problematic (Mahmudpour et al. 2020; Krynytska et al. 2021). However, musculoskeletal, neurological, and psychological disturbances might persist after recovery from COVID-19 (Carfì et al. 2020; Huang et al. 2021b; Nalbandian et al. 2021).
Most patients who recovered from COVID-19 carry a burden of sequelae after infection, which impacts their daily quality of life (Nalbandian et al. 2021; Elkan et al. 2021). Thus, it is essential to elucidate better the pandemic’s aftermath and COVID-19 on the population. Some studies point out that FM syndrome and other chronic painful conditions might be triggered or exacerbated by COVID-19 or due to the numerous and persistent stressors imposed daily by the pandemic setting (Clauw et al. 2020; Kemp et al. 2020; Attal et al. 2021). Furthermore, the COVID-caused widespread pain and symptoms associated with nervous system sensitization support the hypothesis that the syndrome that appears months after infection resembles features of a nociplastic origin condition (Kosek et al. 2021; Goudman et al. 2021; Fernández-de-las-Peñas et al. 2022).
Based on this, we reported on painful, musculoskeletal, and neurological symptoms caused by COVID-19, mainly in a recovery situation. We also argued the potential consequences of COVID-19 exclusively on FM syndrome, which might include: (i) COVID-19 as a trigger of FM syndrome; (ii) COVID-19 as an enhancer of FM syndrome; (iii) similar mechanisms between FM syndrome and COVID-19; (iv) potential FM treatments for post-COVID syndrome; and (v) therapies to inflammation, given the robust inflammation triggered by the infection. Although our review is quite speculative, our goal is to alert clinicians and researchers about the similarities between post-COVID syndrome and FM symptoms, to better treat this group of patients.
COVID-19 symptoms and their relation with chronic pain
As the pandemic of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) occurs, the number of patients recovered from COVID-19 grows worldwide (WHO 2023). Although many individuals remain asymptomatic throughout the infection of SARS-CoV-2, about 32%–85% of infected patients have a non-severe disease, and 15%–31% face a severe illness (Wiersinga et al. 2020a; Guan et al. 2020; Carfì et al. 2020; Tuzun et al. 2021). The severe illness usually occurs in vulnerable people, leading to a considerable rate of morbidity and mortality (Wiersinga et al. 2020a; Zamorano Cuervo and Grandvaux 2020). The most common clinical manifestations at the onset of illness have included signs of a typical cold, such as sore throat, nasal congestion, rhinorrhea (approx. 7%), dry cough (50%–86%), fever (60%–90%), dyspnoea (approx. 65%) or shortness of breath (53%–80%), anorexia (approx. 30%), and gastrointestinal symptoms (e.g., diarrhoea (15%–39%)) (Liguori et al. 2020; Wiersinga et al. 2020a; Wang et al. 2020; Guan et al. 2020; Mao et al. 2020; Landewé et al. 2020; Carfì et al. 2020).
SARS-CoV-2 may also infect skeletal muscle (Disser et al. 2020; Santos et al. 2022), causing musculoskeletal and pain-related symptoms (Mao et al. 2020). Among these symptoms are fatigue (38%–85%), weakness (approx. 25%), mild to moderate body pain resembling a pattern compatible with local or generalised myalgia (15%–68%), arthralgia (15%–55%; primarily notable at the wrist, ankle, and knee joints), chest pain (approx. 40%), back pain (approx. 20%), and abdominal pain (2%–5%) (Liguori et al. 2020; Nalleballe et al. 2020; Wang et al. 2020; Guan et al. 2020; Mao et al. 2020; Landewé et al. 2020; Carfì et al. 2020; Wiersinga et al. 2020b; Rowbotham and Arendt-Nielsen 2021; Kayaaslan et al. 2021). Thus, muscle involvement in COVID-19 appears to be a triangle of myalgia, physical fatigue, and muscle weakness (Tuzun et al. 2021). However, musculoskeletal symptoms do not seem to be associated with the severity of COVID-19 (Schett et al. 2020). They may have a longer duration when compared to other viral infections, being unresponsive to conventional analgesics (Kucuk et al. 2020).
More than one-third of patients with COVID-19 have experienced various neurologic manifestations due to the neuroinvasive potential of SARS-CoV-2 (Josephson and Kamel 2020; Shiers et al. 2020), which has affected both central and peripheral nervous systems (Nalleballe et al. 2020; Mao et al. 2020). Altered mental status, confusion, delirium, dizziness, nausea, vomiting, seizures and headache (4–45%) were the most common manifestations related to the central nervous system (CNS) (Nalleballe et al. 2020; Mao et al. 2020; Josephson and Kamel 2020; Harapan and Yoo 2021). Neuralgias (e.g., burning pain, numbness or paraesthesia), polyneuropathy, and sensory problems, such as allodynia (i.e., abnormal tenderness to light touch or pressure) (Nalleballe et al. 2020; Aksan et al. 2020; Gheita et al. 2021), dysgeusia (i.e., taste impairment; approx. 5%) and anosmia (i.e., smell impairment; approx. 5%) were the most frequent symptoms reported by patients and related to the peripheral nervous system (PNS) (Nalleballe et al. 2020; Wiersinga et al. 2020a; Mao et al. 2020; Tancheva et al. 2020; Rowbotham and Arendt-Nielsen 2021). Psychological disturbances were also present from the early phases of the disease. They included sleep impairment, anxiety, mood disorders such as depression, memory problems, suicidal ideation, and post-traumatic stress disorder (Valiuddin et al. 2020; Liguori et al. 2021).
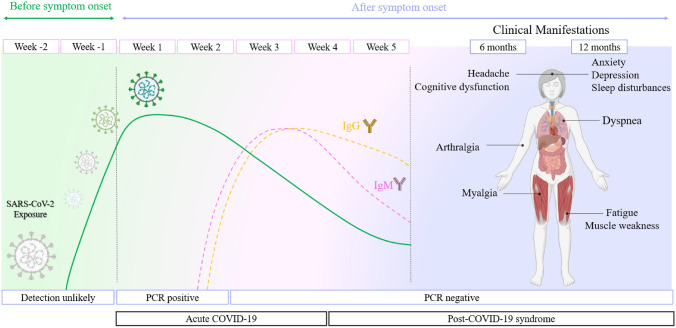
Due to the large portion of the population who have survived COVID-19, there is immense concern about the long-term sequelae. Although we have lived with it for more than three years, the lineup and incidence of long-term or persistent COVID-19-related symptoms are still unclear. Nevertheless, it is believed that people who have been infected with SARS-CoV-2 and recovered carry a burden of sequelae, regardless of their virus immunity (Scherlinger et al. 2021). As time passes, it has been possible to observe that the musculoskeletal, neurological, and psychological disorders that occur during the acute phase of the infection may persist beyond the recovery time. The terminology for this phenomenon is still evolving, and there is no standard clinical terminology, although it is often referred to as a post-COVID-19 syndrome (Fig. 1) (Carfì et al. 2020; Tancheva et al. 2020; Nalbandian et al. 2021; Kayaaslan et al. 2021). In this sense, a high proportion (70–90%) of individuals still complain about at least one symptom after recovery, including fatigue (76%), dyspnea (43.4%), arthralgia (27.3%), chest pain (21.7%), headache (10%), or myalgia (5%–8%) (Carfì et al. 2020; Nasserie et al. 2021; Elkan et al. 2021; Scherlinger et al. 2021; Moghimi et al. 2021; Kayaaslan et al. 2021).
Fig. 1.
Timeline from the SARS-CoV-2 exposure until the development of the post-COVID syndrome. The symptoms of acute COVID-19 usually last until 4 weeks from the onset of symptoms. However, these symptoms might persist beyond the acute phase of infection and are often referred to as a post-COVID syndrome. Post-COVID syndrome is defined as persistent symptoms and/or delayed or long-term complications, which may persist at least 6–12 months beyond the recovery. The common symptoms of post-COVID syndrome argued in this review were summarized on the right side. The Figure was adapted from Nalbandian et al. (2021) and Moghimi et al. (2021)
Altered psychological parameters of post-COVID patients have encompassed stress, cognitive dysfunction (67.5%), including memory and concentration impairment (approx. 9%), depression or anxiety (approx. 7%), and sleep impairment and insomnia (29.4%) (Nasserie et al. 2021; Elkan et al. 2021; Moghimi et al. 2021). Furthermore, restraints imposed by lockdown during the pandemic of COVID-19 have altered the social environment where people live and work, contributing to the worsening of these parameters (Varga et al. 2021).
It is clear that COVID-19 is associated with painful symptoms, and even those who face a non-severe disease may require strong analgesics for their pain management (Kemp et al. 2020). In the face of a high-severity pandemic (such as COVID-19), keeping patients alive is of absolute importance, and pain assessment may not be a priority. However, if patients' pain is undertreated and underestimated, it can become chronic and strongly interfere with their post-COVID lives (Kemp et al. 2020; Fernández-de-las-Peñas et al. 2021a, 2023). Although studies report days of hospitalization as a risk factor for the development of post-COVID-19 musculoskeletal pain symptoms (Kemp et al. 2019; Fernández-de-las-Peñas et al. 2021b, a), the chronic pain and persistent poor health after COVID-19 may not necessarily be associated with respiratory complications, initial disease severity, or the need for hospital care (Logue et al. 2021; Townsend et al. 2021). Thus, the health consequences of COVID-19 extend far beyond acute infection, even among those who experience mild illness (Logue et al. 2021).
In this sense, a subset of patients who faced non-severe COVID-19 disease has reported persistent painful symptoms, which included fatigue/muscle weakness (70.6%), trouble with mobility (7%), headaches (68%), and myalgias (55%) (Graham et al. 2021; Nehme et al. 2021; Moghimi et al. 2021). Moreover, it has been shown that painful symptoms might persist for 7–12 months, ranging from one to five complaints (Huang et al. 2021b; Nehme et al. 2021; Fernández-de-las-Peñas et al. 2023). Some symptoms, such as myalgia, arthralgia, and fatigue, appear early in the infection and persist. While other symptoms, such as paraesthesia (60%), burning (43%), and musculoskeletal pain (40%), are rarely reported at the onset of infection but emerge and become prevalent for at least 6–12 months (Scherlinger et al. 2021; Fernández-de-las-Peñas et al. 2023).
The persistence of painful symptoms might also be related to hospital procedures (e.g., routine procedures in the intensive care unit (ICU)) or medications (e.g., antiretroviral drugs, neuromuscular blockers, and corticosteroids) (Kemp et al. 2020; Heesakkers et al. 2022). Furthermore, it is also important to note that the pain may cause rapid and shallow breathing, increasing the respiratory workload and oxygen consumption. In this way, the pain can negatively affect the course of the disease in patients with COVID-19 who have a respiratory failure (Pektas et al. 2021). Several studies have reported the persistence of at least one symptom in previously hospitalized patients, which can persist at least 6 (68%) and 12 (49%) months after infection (Huang et al. 2021b; Nasserie et al. 2021).
It is essential to highlight that COVID-19 may not only be related to trigger pain but also exacerbate the pain of patients who live with chronic pain, such as FM. Worsening of pre-existing pain might be associated with COVID-related physical or mental conditions (Clauw et al. 2020), social threats, discontinuation of therapy or reduced access to treatments, and hospitalization (Attal et al. 2021; Fernández-de-las-Peñas et al. 2023). Indeed, the patients living with chronic pain infected by COVID-19 reported that no new symptoms appeared, but clearly, their painful symptoms (e.g., intensity, duration, location, or frequency) worsened after hospitalization (Fernández-de-las-Peñas et al. 2023). Likewise, patients with chronic neuropathic pain exposed to SARS-CoV-2 appear to exacerbate their pain and deteriorate their neurological condition (Attal et al. 2021). Based on these data, we hypothesize that COVID-19 can also exacerbate symptoms of FM syndrome.
During the pandemic, people not infected with COVID-19 were also impacted. Evidence supports that painful symptoms can have been triggered or exacerbated during the worldwide lockdown, probably associated with emotional and social factors (such as fear, catastrophism, social alarm, and posttraumatic stress disorder) (Clauw et al. 2020; Karos et al. 2020; Meulders et al. 2022). Persistent and excessive stress can also lead to severe mental health consequences, triggering anxiety, depression, and sleep disorders, which are comorbidities frequently reported in chronic pain states (Choy 2015; Clauw et al. 2020; Karos et al. 2020).
Remarkably, the COVID-19 pandemic or the aftermath of restraints imposed by the lockdown during the pandemic could potentially increase the prevalence of chronic pain after a SARS-CoV-2 infection (Clauw et al. 2020). The widespread pain and symptoms associated with nervous system sensitization support the hypothesis that post-COVID syndrome resembles features of a nociplastic condition (Kosek et al. 2021; Goudman et al. 2021; Fernández-de-las-Peñas et al. 2023). Thus, our concern is mainly given to FM syndrome, a chronic pain condition of nociplastic origin. These approaches make us wonder: could the FM syndrome be impacted by COVID-19? To clarify this hypothesis, we focused our review on how symptoms of FM could be triggered or exacerbated by SARS-CoV-2.
Could fibromyalgia syndrome be impacted by COVID-19?
Fibromyalgia syndrome
FM is classified as chronic primary pain, considered the third most frequent musculoskeletal condition, affecting 2–3% of the world population (Treede et al. 2019; Sarzi-Puttini et al. 2020). This condition is characterized by polysymptomatology once it results from the interplay between many predisposing, triggering, and sustaining factors (Häuser et al. 2015; Sarzi-Puttini et al. 2020). Thus, the term FM includes a pathway of multiple somatic, psychological, and social contributions, and consequently, the severity and complaints of FM vary from patient to patient (Sarzi-Puttini et al. 2020).
The clinical manifestations of FM are mainly characterized by pain, fatigue, and sleep disturbances, which are currently considered diagnostic criteria (Häuser et al. 2015, 2017; Sarzi-Puttini et al. 2020). Patients with FM present with chronic widespread pain with a variable anatomical location that affects the entire body (Häuser et al. 2017; Sarzi-Puttini et al. 2020), spontaneous pain in the muscles or joints (Napadow et al. 2010), headache (Littlejohn and Guymer 2018), and a variety of sensory symptoms (Clauw 2014; Larson et al. 2014; Littlejohn and Guymer 2018). Furthermore, chronic widespread pain is the unanimous complaint among patients with FM, and fatigue is achieved by 70% of patients (Choy 2015). This fatigue might be physical or mental, varying from mild to severe tiredness (Sarzi-Puttini et al. 2020), morning stiffness (Häuser et al. 2015), muscle pain and weakness (Park et al. 2000), or restricted gait (Littlejohn and Guymer 2018). Sleep problems are also preponderant in patients with FM since approximately 90% of patients have insomnia or frequent awakenings (Sarzi-Puttini et al. 2020). Although the quality and duration of sleep are sometimes unchanged, patients with FM often report insufficient rest (Choy 2015; Sarzi-Puttini et al. 2020).
Patients with FM often present with other clinical symptoms non-pain-related (Choy 2015; Häuser et al. 2015; Sarzi-Puttini et al. 2020) that include cognitive dysfunction, mostly concentration problems or memory deficits (Sarzi-Puttini et al. 2020), anxiety (60%) or mood disturbances, such as depression (14–36%) (Choy 2015; Sarzi-Puttini et al. 2020), and variable gastrointestinal symptoms (Clauw 2015). Moreover, most symptoms of FM can be aggravated by physical or mental stress during the syndrome (Häuser et al. 2017), which leaves us intrigued if a pandemic situation could trigger or exacerbate the FM symptoms.
The FM pathophysiology is not fully understood, although it covers several pathological characteristics. The CNS plays a critical role in FM symptomatology, once occur altered pain processing (termed central sensitization henceforth), dysfunctional descending pain modulation, and structural and functional changes in the brain (Choy 2015; Häuser et al. 2015). However, FM has been also associated with abnormalities in peripheral systems. At least in a subset of patients with FM, the inflammatory process has been demonstrated, with altered levels of inflammatory and immunoregulatory cytokines, neuropeptides release and neurogenic inflammation (Littlejohn 2015; Littlejohn and Guymer 2018), inflammatory cells increase (Theoharides et al. 2019), and NLR Family Pyrin Domain Containing 3 (NLRP3) inflammasome activation (Cordero et al. 2014). Additionally, mitochondrial dysfunction has been observed in the blood, muscle, and skin biopsies of some patients with FM (Cordero et al. 2012b; Scherlinger et al. 2021). The imbalance of nutritional components, such as essential minerals and vitamins, also might play a critical role in FM (Bjørklund et al. 2018).
Even though several other mechanisms besides those punctuated here had been related to the pathophysiology of FM, we highlighted only the similar pathophysiological features between COVID-19 and FM. We focus on mechanisms that can help explain the development of similar symptomatology between these two conditions.
Could fibromyalgia syndrome be triggered by COVID-19?
The persistent symptoms post-COVID are becoming increasingly apparent over time and are known as post-COVID syndrome (Carfì et al. 2020; Nalbandian et al. 2021). Similarities between post-COVID syndrome and the FM syndrome raise the hypothesis that SARS-CoV-2 infection could trigger the development of FM once potential environmental factors generate it (Häuser et al. 2015; Sarzi-Puttini et al. 2020). Indeed, at least 30% of patients identify a preceding physical or psychological trigger of their syndrome (Fitzcharles et al. 2021). Some viral infections have been linked to the development of FM, including infection induced by the hepatitis C virus, human immunodeficiency virus (HIV), parvovirus, or Epstein–Barr virus (Buskila et al. 2008). The observation that such infectious agents are associated with FM syndrome suggests that abnormal host response to infection may be implicated (Komaroff and Lipkin 2021). Thus, the hypothesis that SARS-CoV-2 and its sequelae might play a role in the development of FM is encouraged.
Of note, clinical features of the FM syndrome, such as musculoskeletal pain, fatigue, sleep impairment, depression, and anxiety have been reported in one-third of patients with symptoms of the post-COVID syndrome (as presented in Table 1) (Sarzi-Puttini et al. 2020; Nalbandian et al. 2021; Fernández-de-las-Peñas et al. 2023). Based on this, web-centred research uncovered more than 600 patients that developed post-COVID syndrome (Ursini et al. 2021). Of them, about 30% of patients met the 2011 American College of Rheumatology (ACR) criteria for diagnosis of FM (Wolfe et al. 2010) at a mean of 6 months after their recovery from COVID-19. Therefore, they were referred to as post-COVID FM (Ursini et al. 2021).
Table 1.
Similar symptoms between FM and Post-COVID-19 syndromes
| Pain | Hypersensitivities | Muscle pain | Sleep disturbances | Headache | Cognitive dysfunction | Mood disorders | Anxiety |
|---|---|---|---|---|---|---|---|
| FM syndrome | |||||||
| Myalgia |
Sensory problems (e.g. allodynia, hyperalgesia, thermal and chemical hypersensitivity) |
Fatigue (e.g. physical and mental) |
Sleep impairment (e.g. insomnia or frequent awakenings) |
Headache (e.g. migraine or temporomandibular dysfunction) |
Memory problems |
Depression (enhance painful symptoms) |
Anxiety (e.g. palpitations and ↑ anxiety index) |
| Widespread pain |
Neuropathic-like pain (e.g. burning pain or dysesthesia) |
Weakness | Concentration impairment | ||||
| Chest and abdominal pain | |||||||
| Post-COVID-19 syndrome | |||||||
| Myalgia |
Sensory problems (i.e., allodynia, dysgeusia and anosmia) |
Fatigue |
Sleep impairment |
Headache | Memory problems | Depression |
Anxiety (e.g. ↑ anxiety index) |
| Widespread pain | |||||||
| Chest and abdominal pain |
Neuralgias (e.g., burning pain, numbness and paraesthesia) |
Weakness | Concentration impairment | ||||
| Arthralgia | |||||||
COVID-19 coronavirus disease 19, FM fibromyalgia
The comorbidity of obesity and male gender also seem to be risk factors for developing the post-COVID FM-like syndrome in this subgroup of interviewed patients (Ursini et al. 2021). The authors have suggested that patients who developed severe COVID-19 (with hospital admission and oxygen therapy need) are more suggestive of developing a post-COVID FM-like syndrome (Ursini et al. 2021). However, in another study, 56.7% of patients (17/30) who showed mild and moderate symptoms during COVID-19 were positive for FM-like symptoms 6 months after the infection (Scherlinger et al. 2021). Thus, the severity of the symptoms during the disease course seems not to be an essential factor for developing a post-COVID FM-like syndrome.
Strikingly, one case report published in April 2021 also demonstrated the strong relationship between FM symptoms and post-COVID syndrome (Gheita et al. 2021). Three female patients with no previous history of FM or any other rheumatic disease complained of persistent symptoms after recovery from COVID-19, such as generalized musculoskeletal pain, allodynia, fatigue, anxiety, depression, paraesthesia, and non-restorative sleep. General examination and several laboratory investigations, including an autoimmune profile and radiological investigation, were all normal. However, all women met the 2010 ACR criteria for a diagnosis of FM (Wolfe et al. 2010; Gheita et al. 2021). The standard clinical treatments of FM, including non-pharmacological and pharmacological management, were prescribed to them, such as physical exercise and therapies approved by Food and Drug Administration (FDA), including duloxetine ((serotonin and norepinephrine reuptake inhibitor (SNRI)) and gabapentin (gabapentinoid). All women reported improved well-being and mood after the onset of treatment, which contributed to confirming the diagnosis of a post-COVID FM-like syndrome (Gheita et al. 2021).
Another case published in 2020 reported a woman diagnosed with COVID-19 without a history of any previous painful condition but with some associated comorbidities (Aksan et al. 2020). The patient presented with pain symptoms very similar to the complaints reported by patients with FM (Häuser et al. 2017), which included: (i) constant neck and back pain (resembling generalized pain), (ii) and a burning quality (resembling a neuropathic-like FM pain), which was (iii) exacerbated by light touch and heat (resembling mechanical and thermal hypersensitivity). This patient presented with bilateral and generalized pain, which was not a pattern for viral neuropathic pain. Furthermore, the onset of the pain coincided with her SARS-CoV-2 infection, and there was no other likely explanation for the symptoms. Sleep problems, which are observed in many patients with FM, were also reported. The patient's treatment with acetaminophen, non-steroidal anti-inflammatory drugs (NSAIDs), and opioids did not alleviate her pain. It makes us hypothesize that this patient was going through a post-COVID FM-like syndrome once these usual treatment approaches are ineffective for patients with FM. On the other hand, gabapentinoids, a class of drugs recommended for the treatment of FM, attenuated the painful hypersensitivity and improved the sleep quality of this patient.
The studies published so far speculate that the development of FM might be occasioned in a subgroup of patients after SARS-CoV-2 infection (Gheita et al. 2021; Ursini et al. 2021). However, it is currently unknown what factors contribute to it. Potential processes have been suggested for the pathophysiology of post-COVID syndrome (Nalbandian et al. 2021). These processes might also be linked to the development of FM syndrome after the viral infection. Substantial mechanisms that may contribute to the trigger of an FM-like syndrome after COVID-19 are: (i) pathophysiologic changes caused by SARS-CoV-2 itself, mainly neuropsychiatric sequelae such as chronic malaise, diffuse myalgia, depressive and anxiety symptoms, non-restorative sleep, and cognitive impairment (Abdullahi et al. 2020; Nalbandian et al. 2021) and (ii) SARS-CoV-2 cell-to-cell inflammatory mechanisms (ie, cytokine storms) which might provoke hyperexcitability of PNS and CNS (Fernández-de-las-Peñas et al. 2023). Furthermore, the (iii) sequelae of post-critical illness are indirect processes responsible for worsening the physical, cognitive, and psychiatric domains after COVID-19. They can be caused by posttraumatic stress disorder, prolonged bed rest, ICU admission, and the necessity of sedation and ventilation (Häuser et al. 2015; Inoue et al. 2019; Hosey and Needham 2020; Heesakkers et al. 2022).
The co-existence of comorbidities or immunosuppressive diseases is a known factor for anticipating or developing chronic pain (Clauw et al. 2020; Kemp et al. 2020) and increasing severity and mortality related to COVID-19 (Nalbandian et al. 2021). Thus, it can also be suggested that the presence of these parameters might support the advancement of FM-like symptoms after COVID-19 (Nalbandian et al. 2021). However, more studies are necessary to understand the direct and indirect mechanisms of the pathophysiology of the FM-like syndrome triggered after COVID-19.
Although the long-term effects of the post-COVID syndrome and its similarity with FM syndrome remain actively debated, acknowledging the post-COVID FM-like syndrome is still a challenge. Moghimi et al. (2021), for example, proposed a diagnostic criterion for the neurological post-acute sequelae of SARS-CoV-2 infection. Among the proposed criteria, 60% of them (25 of 42 reported symptoms) match the criteria for FM diagnosis. The early recognition of the development of an FM-like syndrome after COVID-19 could lead to prompt and targeted treatment and, thus, mitigate the potential impact of chronic pain on health and the social environment.
Could fibromyalgia syndrome be exacerbated by COVID-19?
Based on the clinical manifestations of FM, it has been proposed that people living with FM are an extremely vulnerable population in the setting of COVID-19 (Mohabbat et al. 2020). As shown in Table 1, musculoskeletal pain, fatigue, myalgia, and sleep impairment are some of the common complaints in both diseases (Choy 2015; Abdullahi et al. 2020; Tuzun et al. 2021; Nasserie et al. 2021). In this sense, it has been demonstrated that patients with FM are subject to more significant mental stress and anxiety during COVID-19. Thus, these patients have exacerbated symptoms of pain, fatigue, and sleep quality compared to control patients (without FM) with COVID-19 (Salaffi et al. 2021). Therefore, the SARS-CoV-2 infection may be an essential factor in exacerbating the symptoms of FM patients.
It is worth mentioning that the acute symptoms of COVID-19 can persist in COVID-19 survivors after their recovery (Fig. 1) (Kucuk et al. 2020; Nalbandian et al. 2021). Thus, it is unclear if the exacerbation of FM symptoms returns to normal after patients with FM have recovered from COVID-19 (Salaffi et al. 2021). Nonetheless, it has been shown that patients suffering from pre-existing musculoskeletal pain conditions before COVID-19 seem to experience increased intensity, extension, or frequency of their symptoms for at least the first seven months after infection (Fernández-de-las-Peñas et al. 2021b, 2022). Thus, we might speculate that the enhanced FM symptoms in post-COVID situations can also last for an extended time. Patients with FM are at increased risk of mood disorders, even in non-pandemic situations (Clauw 2014, 2015; Häuser et al. 2017). During the COVID-19 pandemic, the social and economic environments where people live and work suffered changes (Karos et al. 2020). Thus, the COVID-19 pandemic prompted feelings of isolation, uncertainty, depression, mental stress, generalized anxiety, and fear of the virus, mainly in vulnerable subgroups (Liguori et al. 2020; Clauw et al. 2020; Varga et al. 2021). Indeed, some studies have revealed that fear and anxiety levels during the COVID-19 pandemic in patients with FM were higher than in control patients (without FM) (Cankurtaran et al. 2021). In another study, 67% of 32 patients with FM reported that their general health status (well-being) worsened during the lockdown imposed by the COVID-19 pandemic (Cavalli et al. 2021; Cankurtaran et al. 2021). Consequently, these feelings seem to be associated with the severity of painful symptoms of FM (Aloush et al. 2021; Cankurtaran et al. 2021). The lack of social interactions may also play an essential role in modulating pain and dealing with chronic pain (Mogil 2015). Furthermore, patients with FM appear to be more susceptible to mood disorders than patients with other rheumatic diseases in the settings imposed by the COVID-19 pandemic (Iannuccelli et al. 2021), reinforcing the need to care for patients suffering from FM.
FM symptoms can be substantially managed using non-pharmacological measures (Sarzi-Puttini et al. 2020). Multidisciplinary interventions and physical exercise are strongly recommended to treat pain and improve the well-being of patients with FM (Busch et al. 2002; Sarzi-Puttini et al. 2020). However, one of the consequences caused by the pandemic was the reduction in daily activities related to the health of individuals, as many patients avoided leaving home to prevent SARS-CoV-2 infection (Clauw et al. 2020; Attal et al. 2021). Indeed, a study in Israel showed that all 129 patients with FM who used non-pharmacological treatments interrupted their activities after restrictions imposed by the COVID-19 pandemic, and over half of the patients with FM lost contact with their physician (Aloush et al. 2021). Another study showed that in patients with FM, the most commonly self-reported cause of exacerbating symptoms was the inability to exercise during restrictions (Cavalli et al. 2021).
Although we have been living with it for more than three years, the long-term effects of the pandemic in patients with FM are still unknown. The findings so far indicate that FM symptoms might be exacerbated during COVID-19, at least in a subset of patients (Salaffi et al. 2021), and it can persist for months after recovery (Nalbandian et al. 2021). Furthermore, the numerous and persistent stressors imposed by the COVID-19 pandemic seem to aggravate FM disease (Aloush et al. 2021; Salaffi et al. 2021; Cavalli et al. 2021). Based on this, both the viral infection and scenario of the COVID-19 pandemic may collectively exacerbate FM symptoms in the short and possibly long term.
Similar mechanisms between fibromyalgia syndrome and COVID-19
FM and SARS-CoV-2 infection share mechanisms that could help us understand why both conditions culminate in the development of similar complaints. As these conditions are heterogeneous, and not all patients develop the same symptoms, multiple underlying mechanisms are likely to be implicated (Sarzi-Puttini et al. 2020; Scherlinger et al. 2021). Table 2 summarizes the similarities among the mechanisms of post-COVID and FM syndromes.
Table 2.
Similar mechanisms between post-COVID-19 and FM syndromes
| Inflammation | Peripheral sensitization | Central sensitization | Mitochondrial dysfunction | Oxidative stress | Nutritional imbalance |
|---|---|---|---|---|---|
| FM syndrome | |||||
|
Cytokines (e.g. ↑ IL-1, IL-6, and IL-8 and ↓ IL-4 and IL-10) |
Nociceptors sensibilization (e.g. spontaneous activity and sensitization of C-fibres) |
Increased excitatory NT (e.g. glutamate) |
Mitochondrial dysfunction (e.g. degenerated mitochondria, membrane permeabilization, ↓ complexes activity, ↓ coenzyme Q10) |
Oxidative stress (e.g. ↑ ROS, lipid peroxidation, ↓ endogenous antioxidants) |
Nutritional imbalance (e.g. ↓ minerals and vitamins) |
|
Chemokines (e.g., CX3CL1) |
Alteration monoamines levels | Antioxidant drugs are recommended | |||
| Mastocytosis and glial cell activation | Microglia activation | ||||
| Post-COVID-19 syndrome | |||||
|
Cytokines (e.g. ↑ TNF-α, IL-6, and IL-8) |
Nociceptors sensibilization (due cytokine storm) |
Increased excitatory NT * (e.g. glutamate) |
Mitochondrial dysfunction (e.g. ↓ ATP production, membrane permeabilization and mitophagy) |
Oxidative stress (e.g. ↑ malondialdehyde levels) |
Nutritional imbalance (e.g. ↓ vitamin D levels) |
| Chemokines | Alteration monoamines levels * | Antioxidant drugs are recommended | |||
| Microglia activation * | |||||
COVID-19 coronavirus Disease 19, CX3CL1 C-X3-C motif chemokine ligand 1, FM fibromyalgia, NLRP3 NLR Family Pyrin Domain Containing 3, NT neurotransmitter, ROS reactive oxygen species
*It is suspected to happen
Accumulating evidence has clarified how the host immune response reacts to SAR-CoV-2 infection and contributes to infectious symptoms. The “cytokine storm” is an excessive or uncontrolled innate immune response to severe COVID-19 associated with untoward pathological consequences (Mahmudpour et al. 2020). However, immunological reactions might also occur in milder cases of COVID-19, aiming to combat viral infection. In this case, some COVID-19 clinical features, mainly painful and fatigue symptoms, are believed to be caused by an inflammatory response due to the invasion of the virus in the muscle and joints (Widyadharma et al. 2020). Indeed, SARS-CoV-2 cell-to-cell inflammatory mechanisms (i.e., cytokine storm) provoke hyperexcitability of PNS and CNS leading to the development of painful symptoms post-COVID or exacerbating pre-existing pain symptoms (Goudman et al. 2021; Fernández-de-las-Peñas et al. 2023). A similar immunological response also occurs in a subset of patients with FM. Although the cause of FM is unknown, and in some patients, it is not caused after a viral infection, dysregulated immune processes have been proposed to mediate FM symptoms (Goebel et al. 2021). In agreement, cytokines such as TNF-α, IL-6, and IL-8 are found in higher levels in the serum of patients with COVID-19 or FM (Littlejohn and Guymer 2018; Mahmudpour et al. 2020).
It is complicated to establish whether the immunological responses in the acute phase of COVID-19 evolve or are correlated with long-term sequelae (Moghimi et al. 2021). However, Huang et al. (2021b) have demonstrated that some pro-and anti-inflammatory cytokines and chemokines gradually decreased from symptoms onset to 12 months, as the symptoms of fatigue, weakness, and sleep problems were attenuated. This statement supports the critical role of the inflammatory process in developing symptoms in patients with COVID-19.
Saleh et al. (2020) have suggested inflammatory responses of SARS-CoV-2 may modulate mitochondria metabolism. Additionally, the opposite also may happen. The mitochondrial metabolic manipulation by SARS-CoV-2 triggers an enhanced inflammatory response in patients with COVID-19 (Ajaz et al. 2021). Mitochondrial dysfunction has been implicated in numerous pathologies, including FM (Meeus et al. 2013) and SARS-CoV-2 infection (Saleh et al. 2020; Ajaz et al. 2021). In both diseases, there is impaired mitochondrial oxidative phosphorylation and production of ATP, which culminate in mitochondrial membrane permeabilization and mitophagy (Cordero et al. 2010; Saleh et al. 2020; Ajaz et al. 2021). Once patients with COVID-19 and FM cannot produce their required energy as in physiological conditions, increased glycolysis occurs to compensate for high energy demands (Eisinger et al. 1994; Moghimi et al. 2021). These impairments are associated with a higher inflammatory response and may lead to peripheral and central sensitization, explaining the pain and other systemic complaints in these patients (Meeus et al. 2013).
Mitochondria is the primary source of reactive oxygen species that contributes to normal cell function but is also linked to intracellular oxidative stress (Rinnerthaler et al. 2015). Besides, a heightened inflammatory state is associated with deleterious systemic events, including oxidative stress (Saleh et al. 2020). In this way, oxidative stress is indicated as an important player in the pathogenesis and severity of both COVID-19 (Saleh et al. 2020) and FM (Hung et al. 2020). Increased levels of malondialdehyde have been observed in patients with COVID-19 (Forcados et al. 2021) and FM (Meeus et al. 2013). Although literature data did not provide enough information on other oxidized substances in patients with COVID-19, antioxidant therapeutic strategies successfully reverted the severe symptoms of patients with COVID-19 (Cecchini and Cecchini 2020). Besides, the antioxidant therapeutic strategies also revert several symptoms of FM (Cordero et al. 2012a; Schweiger et al. 2020), suggesting that the oxidative status is implicated in the symptoms of both diseases.
Studies have shown significantly lower levels of vitamin D in patients with COVID-19, which can be correlated with disease progression (Forcados et al. 2021). Similarly, some patients with FM may have health problems associated with low levels of vitamin D (Bjørklund et al. 2018). It is important to emphasize that deficiency of vitamin D is related to the development of myopathy and severe muscle weakness, depression, and anxiety (Shipton and Shipton 2015), similar to the complaints of patients with COVID-19 and FM. In this way, therapy with vitamin D could improve the FM patient’s quality of life (Bjørklund et al. 2018), reduce the progression of COVID-19 and enhance the survival rate (Forcados et al. 2021). Thus, patients with COVID-19 could benefit from vitamin D supplementation.
Another mechanism shared by FM and COVID-19 is peripheral and central sensitization. More than one-third of patients with COVID-19 have experienced several neurologic manifestations (Josephson and Kamel 2020). Dorsal root ganglion (DRG) sensory neurons are a potential target for SARS-CoV-2 invasion, and viral infection of nociceptors may be responsible for causing some of the persistent neurological effects seen in COVID-19 (Shiers et al. 2020). Besides, neuropilin 1, expressed in nociceptors, was recently reported as a host entry receptor for SARS-CoV-2 (Cantuti-Castelvetri et al. 2020). Similar to COVID-19, neuronal alterations also occur in some patients with FM, which are associated with abnormalities in peripheral sensory afferents fibres, triggering spontaneous activity and sensitization of C-fibres, and loss of epidermal innervation (Üçeyler et al. 2013; Evdokimov et al. 2019; Fasolino et al. 2020).
More recently, it was demonstrated that dysregulated immune processes produce autoreactive antibodies (e.g., IgG) that bind antigens expressed in the DRG of patients with FM and may cause an increased noxious peripheral input (Goebel et al. 2021). Similarly, immune dysregulation was also observed in patients with COVID-19. The presence of autoantibodies against cytokines and chemokines seems to perturb the immune function and impair virological control (Wang et al. 2021). Thus, the lack of host immunological control might be correlated with the occurrence of peripheral sensitization and the development and maintenance of painful symptoms in both diseases (Goebel et al. 2021; Komaroff and Lipkin 2021).
Systemic inflammation leads to decreased monoamine levels and activation of microglia, resulting in increased levels of glutamate and N-methyl-D-aspartate receptor and excitotoxicity, which are suspected to happen in SARS-CoV-2 systemic inflammation (Boldrini et al. 2021). It has been recently suggested that alterations of the dopamine and serotonin synthetic pathways might be involved in the pathophysiology of COVID-19, culminating in reduced levels of neurotransmitters (Nataf 2020). In this way, neuropsychiatric disorders that affect patients with COVID-19 could be explained, at least in part, by neurotransmission dysfunction or dysregulation (Boldrini et al. 2021). Quite similar processes also happen in FM, such as activation of glial cells (Littlejohn and Guymer 2018; Albrecht et al. 2019), increased excitatory neurotransmitters (glutamate, substance P, and others), and reduced inhibitory neurotransmitters (biogenic amines and gamma aminobutiric acid (GABA)) (Sarzi-Puttini et al. 2020). Together, these mechanisms suggest the development of central sensitization in FM syndrome and COVID-19.
Patients with FM have enhanced pain-specific brain processing (named neurologic pain signature) (López-Solà et al. 2017) and brain glial activation (Albrecht et al. 2019), while decreased cortical and subcortical grey-matter density (Choy 2015). SARS-CoV-2 is known to penetrate the olfactory mucosa, causing loss of smell, and may enter the brain. However, definitive evidence for SARS-CoV-2 penetrating the blood–brain barrier (BBB) is lacking. Inflammatory cytokines induce BBB instability, and once across the BBB, cytokines can activate glial cells (Boldrini et al. 2021). Given the propensity for cytokines (e.g., TNF-α and IL-6) and oxidative substances to contribute to peripheral and central neuronal sensitization, it was already hypothesized by some studies that the increased prevalence of neurological manifestations seen in severe cases of COVID-19 may be associated with elevations of these markers (McFarland et al. 2021). Besides, stressors, whether physical (e.g., viral infection), mental, emotional, or financial (i.e., common stressors observed in a pandemic situation), directly and negatively affect the underlying process of central sensitization, exacerbating the symptoms of FM and COVID-19 (Mohabbat et al. 2020).
As described in detail, FM and COVID-19 share many similar mechanisms (Table 2). However, we strongly encourage further studies to elucidate better the analogy between the development and maintenance of both diseases.
Could fibromyalgia drugs be used to treat post-COVID symptoms?
More than three years after the start of the COVID-19 pandemic, it is time to recognize (i) the possibility of an FM-related syndrome in SARS-CoV-2-infected patients and (ii) the achievability of SARS-CoV-2 infection or pandemic situation (isolation, uncertainty, depression, mental stress, generalized anxiety, and fear of the virus) to exacerbate FM symptoms. Recognizing these approaches might encourage addressed treatments and strategies to alleviate the impact of COVID-19 on overall health. Nowadays, no standard protocols are available for treating post-COVID-19 symptoms. However, due to the similar symptoms between post-COVID and FM syndrome, as well as the often-post-COVID FM-like syndrome diagnosis, it is possible to hypothesize that medications already approved to treat FM syndrome may be repositioned and efficacious for treating FM-related symptoms in post-COVID-19 patients.
The clinical treatments of FM are based only on symptom management and involve pharmacological or non-pharmacological approaches (Sarzi-Puttini et al. 2020). The first-line drugs for the treatment of FM approved by the FDA are gabapentinoids (pregabalin) and SNRIs (duloxetine and milnacipran) (Clauw 2015; Sarzi-Puttini et al. 2020). Studies about the beneficial effects of pregabalin in patients with COVID-19 have already been published (Oh et al. 2021; Pektas et al. 2021; Oddy et al. 2021; Jena et al. 2022). Jena et al. (2022) demonstrated that pregabalin, associated or not with antidepressants, relieved pain symptoms in hospitalized patients with COVID-19. Besides, a case report described the effects of pregabalin use in two patients with COVID-19 and pneumonia who were admitted to the ICU with complaints of pain and cough. The patients received treatment with acetaminophen, tramadol, and pregabalin. Immediately after adding pregabalin, the patients related a significant reduction in cough complaints, chest pain, and myalgia. Furthermore, the patients began to tolerate more non-invasive mechanical ventilation and prone position due to the absence of such complaints (Pektas et al. 2021). Evidence indicates that pregabalin use is not associated with increased in-hospital mortality among patients with COVID-19 (Oh et al. 2021; Oddy et al. 2021).
Additionally, pregabalin seemed to be an attractive therapeutic alternative to treat pain in patients during and after COVID-19. In addition to its pain-reducing effects, pregabalin has sedative properties and can reduce anxiety and chronic cough (Vertigan et al. 2016; Bach et al. 2018; Slee et al. 2019). Pregabalin is also effective in reducing pain and anxiety symptoms in FM patients (Clauw 2015; Salaffi et al. 2021). Pregabalin also presents advantages over other medications, and it causes minimal respiratory depression, has a low drug-drug interaction potential and has minor metabolism (Ben-Menachem 2004; Pektas et al. 2021), which is relevant to critical patients. Since the treatment with pregabalin showed positive effects during cases with severe COVID-19, and this subset of patients is considered more susceptible to developing post-COVID syndrome, we wonder: could early treatment with pregabalin or another gabapentinoid attenuate the progression of COVID-19 symptoms and, therefore, prevent the development of post-COVID syndrome?
In this sense, Aksan et al. (2020) published a case report of a 40-year-old woman diagnosed with COVID-19 with acute symptoms quite similar to the complaints reported by patients with FM, including constant pain, mechanical and thermal hypersensitivities, and sleep problems (Häuser et al. 2017). Acetaminophen, NSAIDs, and opioids, which usually are ineffective in relieving the pain of patients with FM, did not alleviate this patient’s pain. On the other hand, gabapentin gradually reduced the pain, mechanical and thermal hypersensitivity, sleep impairment, and respiratory symptoms during hospitalization. One month later, the pain had decreased slightly and continued to be relieved by gabapentin. It is worth noting that gabapentin is also a gabapentinoid drug, with a somewhat similar pharmacokinetic profile but more slowly and variably absorbed than pregabalin (Bockbrader et al. 2010). Additionally, gabapentin and pregabalin are safe treatment options with no significant interactions with treatments for COVID-19 (Plasencia-García et al. 2021).
Duloxetine, another drug approved by the FDA as a therapy for FM, decreased the incidence of COVID-19 in patients (Blanch-Rubió et al. 2020), and seems to be less likely to interact with treatments recommended for COVID-19 (Plasencia-García et al. 2021). Furthermore, it is among the most commonly prescribed drugs annually in the United States, has an established safety profile, and is generally well-tolerated (Fanelli et al. 2021). In contrast, milnacipran, another SNRI used as a first-line treatment for FM (Sarzi-Puttini et al. 2020), has not been evaluated in the COVID-19 setting. However, milnacipran may represent a good therapeutic alternative since it lacks interaction with the cytochrome P450 enzymes (frequently involved in the metabolism of antidepressants) (Fanelli et al. 2021). Therefore, milnacipran is less likely to interact with antiretroviral drugs used in patients with COVID-19 (Plasencia-García et al. 2021).
Although tricyclic antidepressants, selective serotonin reuptake inhibitors, and muscle relaxants are prescribed by clinicians and have strong clinical evidence (level I, A) for use in FM, they are not FDA-approved drugs for this purpose (Clauw 2014, 2015; Sarzi-Puttini et al. 2020). Some of these drugs have also been tested for repositioning for COVID-19. The antidepressants amitriptyline, imipramine, paroxetine, and sertraline have potential anti-viral activities and deserve studies targeting COVID-19, especially for those patients suffering from depression (Kutkat et al. 2022). Additionally, amitriptyline has potential benefit in patients with post-COVID-19 headaches (Gonzalez-Martinez et al. 2022) and, when associated with pregabalin, relieves pain symptoms in hospitalized patients with COVID-19 (Jena et al. 2022). In the same way, the muscle relaxant tizanidine, used for treating myofascial pain disorders and FM (McLain 2000; Sarzi-Puttini et al. 2020), could be repositioned for treating post-COVID-19 symptoms (Kumar et al. 2021).
Nonetheless, there is a need to carefully evaluate the use of the therapeutic approaches commonly used in FM for treating some complaints of COVID-19 patients. A study demonstrates the contradictory effects of pregabalin, including an increased incidence of COVID-19 in patients that use it (Blanch-Rubió et al. 2020). Besides, serotonin syndrome (i.e., a serotoninergic overactivity at synapses of the CNS and PNS) has to be considered when using drugs metabolized by cytochrome P450 enzymes, such as duloxetine, in patients with COVID-19 on antiretroviral therapy with lopinavir-ritonavir (Plasencia-García et al. 2021). However, serotoninergic syndrome seems to disappear when duloxetine is stopped (Sabe et al. 2021). Therefore, until now, the literature data have not provided enough backing to confirm whether patients with COVID-19 will benefit or be harmed using gabapentinoids or SNRIs during the infection. The hypotheses must be considered, and double-blinded, controlled, and randomized clinical trials of these drugs in patients with COVID-19 and post-COVID are needed to better understand their benefits in this disease.
Non-pharmacological interventions used for FM treatment, such as psychotherapy, physical exercise, and acupuncture, should be considered for patients with post-COVID syndrome. Studies have demonstrated that exercise therapy might be a safe and effective relief for post-COVID19 syndrome (Hernando-Garijo et al. 2021; Dotan et al. 2022). Indeed, a telerehabilitation program based on aerobic exercise relieved the painful symptoms and psychological distress in women with FM during the COVID-19 pandemic (Hernando-Garijo et al. 2021). Although it may be laborious to transpose non-pharmacological FM treatments to post-COVID syndrome, telerehabilitation, neuromodulation, and resistance exercises have improved primary complaints in post-viral syndromes (Perez et al. 2021; Chandan et al. 2022; Gentil et al. 2022).
Pharmacotherapies to inflammation treatment
Although therapies focusing on inflammation are not recommended for treating FM, we cannot disregard their prominent use in the post-COVID syndrome, given all the solid inflammatory mechanisms triggered by the infection. The immune responses against SARS-CoV-2 are one of the main features of disease pathogenesis (van de Veerdonk et al. 2022), leading to the recruitment and activation of leukocyte subsets and the release of inflammatory cytokines (such as IL-6, IL-2, IL-8, interferon (IFN)-γ, IFN-α, and TNF-α), featuring the “cytokine storm” in the COVID-19 (Mahmudpour et al. 2020). Additionally, the IL-1–IL-6 axis represents one of the most important signalling pathways in the SARS-CoV-2-induced hyperinflammatory reaction (Chen et al. 2020a, b; Giamarellos-Bourboulis et al. 2020). All these mechanisms contribute to an inflammatory response that is associated with different clinical features and symptoms of COVID-19 (Chang et al. 2021; Huang et al. 2021a), such as painful symptoms since increased cytokines can induce hyperalgesia and allodynia and, therefore, sustain widespread chronic pain (Ji et al. 2018; Goudman et al. 2021). Furthermore, post-COVID-19 painful symptoms may be caused by an inflammatory response due to the invasion of the virus in the neurons, muscles, and joints (Shiers et al. 2020; Widyadharma et al. 2020). Thus, preventing viral progression or limiting the cytokine storm could help re-establishing health, eliminate or alleviate pain, and assuage the impact of COVID on patients.
In this sense, several drugs with immunomodulatory properties have been strongly recommended by the panel for COVID-19 treatments, which vary according to the disease severity (mild, severe, or critical) (Lamontagne et al. 2020). These drugs include systemic corticosteroids (dexamethasone), IL-6 inhibitors (tocilizumab and sarilumab), and janus kinase inhibitors (baricitinib, tofacitinib, and ruxolitinib) (Lamontagne et al. 2020).
Corticosteroids are among the drugs recommended to manage patients with COVID-19 and are widely used for treating other diseases closely related to COVID, such as Severe Acute Respiratory Syndrome and Middle Eastern Respiratory Syndrome (Caiazzo et al. 2022). This drug class inhibits many inflammation-associated molecules, such as cytokines (IL-6, IFN-γ, and TNF-α), chemokines, arachidonic acid metabolites, and adhesion molecules, besides up-regulating anti-inflammatory mediators (Barnes 2011). Corticosteroids are recommended for severe or critical COVID-19 to counteract excessive inflammation, but not for non-severe patients (Lamontagne et al. 2020). Indeed, clinical large-scale randomized trials have proposed that corticosteroids contribute to the recovery of severe or critically ill patients infected with SARS-CoV-2 (Sterne et al. 2020; RECOVERY 2021; Cano et al. 2021). Its long-term use might help control post-disease complications, especially in patients with persistent respiratory distress (Kostorz-Nosal et al. 2021). However, the long-term corticosteroid treatment must be carefully evaluated as it might contribute to adverse effects involving the gastrointestinal, cardiovascular, endocrine, nervous, ocular, and immune systems (Oray et al. 2016).
The IL-6 released by macrophages is one of the key factors in initiating cytokine storms, and its increase is associated with the severity of COVID-19 (Chen et al. 2020a; McGonagle et al. 2020; Huang et al. 2021b). Thus, it is suggested that blocking the action of IL-6 may alter the course of the disease and benefit critically ill patients (Zhang et al. 2022). Tocilizumab and sarilumab are monoclonal antibodies that act as immunomodulatory, directly targeting IL-6 via the IL-6 receptor (Xu et al. 2021). Both are approved by the FDA for rheumatoid arthritis treatment and have recently been approved in the United States and United Kingdom for use in patients with severe COVID-19 (Department of Health and NHS 2021; Salama et al. 2021). Although the effectiveness of IL-6 inhibitors on the SARS-CoV-2-triggered immune response has been proven (Abani et al. 2021; Godolphin et al. 2022), its usage as a sole drug and the optimal timing to introduce it to the patient treatment regimen remains controversial (Huang and Jordan 2020; Abidi et al. 2022).
The IL-6 is one of the primary activators of janus kinase (JAK)/signal transducer and activator of the transcription (STAT) pathway (Kamimura et al. 2003). The activation of JAK/STAT pathways orchestrates important biological processes, including cell proliferation, differentiation, apoptosis, and immunomodulation (Xin et al. 2020). By exerting effects in controlling immune regulation and inflammation in the cells, and reducing inflammatory cytokines, some JAK inhibitors have been approved by FDA, such as baricitinib and tofacitinib for treating rheumatoid arthritis (Harrington et al. 2020) and ruxolitinib for treating haematological diseases (Kirito 2022). In this sense, many clinical trials have researched the role of JAK inhibitors in COVID-19 treatment (Cao et al. 2020; Bronte et al. 2020; Kalil et al. 2021; Marconi et al. 2021; Ely et al. 2022). The effectiveness of JAK inhibitors in critically ill patients with COVID-19 has been proven (Cao et al. 2020; Bronte et al. 2020). However, inconsistent conclusions in relation to its efficacy, especially for the reduction of COVID-19 mortality were reported (Kalil et al. 2021; Marconi et al. 2021; Ely et al. 2022).
In addition to the drugs listed above, several drug classes with anti-inflammatory properties have been tested to manage COVID-19, which include colchicine (Tardif et al. 2021; Horby et al. 2021), inhaled corticosteroids (budesonide and ciclesonide) (Yu et al. 2021; Clemency et al. 2022), IL-1 inhibitor (anakinra) (Cavalli et al. 2020; Huet et al. 2020), Bruton’s tyrosine kinase (BTK) inhibitors (acalabrutinib and ibrutinib) (Roschewski et al. 2020; Rada et al. 2021) and NSAIDs (indomethacin and aspirin) (Perico et al. 2022). However, it is essential to point out that all of these drugs are currently under investigation in clinical trials and the treatment regimen remains controversial. Until now, they were not recommended by the panel for COVID-19 treatments or still need to be approved by the FDA.
Finally, it is worth noting that pharmacotherapies recommended by the panel for COVID-19 treatments need to be evaluated, especially for their use on painful parameters in post-COVID syndrome. More medical evidence is still required to demonstrate their rational application, including dosage, course of treatment, the timing of administration, and combination with other drugs. Future clinical studies are also relevant to investigate whether these therapies effectively treat FM-related symptoms in post-COVID patients. Moreover, clinicians should investigate whether these therapies could also reduce COVID-19-caused intense inflammation and, consequently, improve patients' general health.
Conclusions
Given the global scale of this pandemic, it is apparent that the healthcare needs for patients with sequelae of COVID-19 will continue to increase for the foreseeable future. Current evidence raises several interesting questions about whether FM syndrome, a chronic pain condition, might be triggered or potentiated by COVID-19. Based on the collected evidence in this review, we could assume the following:
Post-COVID syndrome in some people may be recognized as an FM-like syndrome once these patients are increasingly meeting the criteria for the diagnosis of FM. Thus, clinical diagnosis of post-COVID sequelae must be made and it is encouraged the recognition of the post-COVID FM-like syndrome;
The exacerbation or occurrence of FM symptoms might happen during a COVID-19 or be due to the numerous and persistent stressors imposed daily by the pandemic setting;
COVID and FM syndrome share some mechanisms, which help explain why both conditions culminate in the development of similar complaints;
Awareness among the general population and care professionals about developing an FM-like syndrome after COVID-19 could lead to prompt and targeted treatment. Thus, the clinical treatments for FM may potentially be repositioned, aiming to prevent or treat FM-related symptoms in post-COVID patients; and
Therapies focusing on inflammation could be effective in post-COVID patients, given all the solid inflammatory mechanisms triggered by the infection, even though they are not recommended in FM syndrome.
Altogether, these actions can contribute to re-establishing pre-COVID-19 health and assuage the potential impact of chronic pain on physical and mental health, family and community life, and the social and economic environments. However, it is important to emphasize that current studies of post-COVID symptoms persistence are highly heterogeneous. Therefore, future research with longer follow-ups, improved quality, and more standardized designs are encouraged.
Abbreviations
- ACR
American College of Rheumatology
- BBB
Blood–brain barrier
- CNS
Central nervous system
- COVID-19
Coronavirus disease 19
- DRG
Dorsal root ganglia
- FM
Fibromyalgia
- FDA
Food and Drug Administration
- GABA
Gamma aminobutiric acid
- HIV
Human immunodeficiency virus
- ICU
Intensive care units
- IFN
Interferon
- IL
Interleukin
- JAK
Janus kinase
- NLRP3
NLR Family pyrin domain containing 3
- NSAIDs
Nonsteroidal anti-inflammatory drugs
- PNS
Peripheral nervous system
- SNRIs
Serotonin and noradrenaline reuptake inhibitors
- SARS-CoV-2
Severe acute respiratory syndrome coronavirus 2
- STAT
Signal transducer and activator of the transcription
- TNF-α
Tumour necrosis factor alpha
Author contributions
All the authors equally contributed to this study. Study concept and design: S.M.O., M.F.P.F., and E.S.B. Acquisition of data M.F.P.F., and E.S.B. Analysis and interpretation of data: S.M.O., M.F.P.F., and E.S.B. Study supervision: S.M.O
Funding
This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior—Brasil (CAPES)—Finance Code 001; by the Fundação de Amparo à Pesquisa do Estado do Rio Grande do Sul-FAPERGS (Grant #21/2551-0001966-2) (Brazil); and by Conselho Nacional de Desenvolvimento Científico (CNPq). CAPES/Programa de Excelência Acadêmica (PROEX) (process #23038.002125/2021-85; Grant #0036/2021). S.M.O and E.S.B. are recipients of a fellowship from CNPq (Grant #304985/2020-1 and #150611/2022-6, respectively). M.F.P.F. is a recipient of a fellowship from CAPES/PROEX (process #88882.182170/2018-01).
Declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval and consent to participate
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Maria Fernanda Pessano Fialho and Evelyne Silva Brum equally contributed to the development of this review article.
References
- Abani O, Abbas A, Abbas F, et al. Tocilizumab in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial. Lancet. 2021;397:1637–1645. doi: 10.1016/S0140-6736(21)00676-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abdullahi A, Candan SA, Abba MA, et al. Neurological and musculoskeletal features of COVID-19: a systematic review and meta-analysis. Front Neurol. 2020;11:72–83. doi: 10.3389/fneur.2020.00687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abidi E, El Nekidy WS, Alefishat E, et al. Tocilizumab and COVID-19: timing of administration and efficacy. Front Pharmacol. 2022;13:1–12. doi: 10.3389/fphar.2022.825749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ajaz S, McPhail MJ, Singh KK, et al. Mitochondrial metabolic manipulation by SARS-CoV-2 in peripheral blood mononuclear cells of patients with COVID-19. Am J Physiol Physiol. 2021;320:C57–C65. doi: 10.1152/ajpcell.00426.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aksan F, Nelson EA, Swedish KA. A COVID-19 patient with intense burning pain. J Neurovirol. 2020;26:800–801. doi: 10.1007/s13365-020-00887-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albrecht DS, Forsberg A, Sandström A, et al. Brain glial activation in fibromyalgia—a multi-site positron emission tomography investigation. Brain Behav Immun. 2019;75:72–83. doi: 10.1016/j.bbi.2018.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aloush V, Gurfinkel A, Shachar N, et al. Physical and mental impact of COVID-19 outbreak on fibromyalgia patients. Clin Exp Rheumatol. 2021;130:108–114. doi: 10.55563/clinexprheumatol/rxk6s4. [DOI] [PubMed] [Google Scholar]
- Attal N, Martinez V, Bouhassira D. Potential for increased prevalence of neuropathic pain after the COVID-19 pandemic. PAIN Reports. 2021;6:884. doi: 10.1097/PR9.0000000000000884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bach DR, Korn CW, Vunder J, Bantel A. Effect of valproate and pregabalin on human anxiety-like behaviour in a randomised controlled trial. Transl Psychiatry. 2018;8:157. doi: 10.1038/s41398-018-0206-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes PJ. Glucocorticosteroids: current and future directions. Br J Pharmacol. 2011;163:29–43. doi: 10.1111/J.1476-5381.2010.01199.X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Menachem E. Pregabalin pharmacology and its relevance to clinical practice. Epilepsia. 2004;45:13–18. doi: 10.1111/j.0013-9580.2004.455003.x. [DOI] [PubMed] [Google Scholar]
- Bjørklund G, Dadar M, Chirumbolo S, Aaseth J. Fibromyalgia and nutrition: therapeutic possibilities? Biomed Pharmacother. 2018;103:531–538. doi: 10.1016/j.biopha.2018.04.056. [DOI] [PubMed] [Google Scholar]
- Blanch-Rubió J, Soldevila-Domenech N, Tío L, et al. Influence of anti-osteoporosis treatments on the incidence of COVID-19 in patients with non-inflammatory rheumatic conditions. Aging. 2020;12:19923–19937. doi: 10.18632/aging.104117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bockbrader HN, Wesche D, Miller R, et al. A comparison of the pharmacokinetics and pharmacodynamics of pregabalin and gabapentin. Clin Pharmacokinet. 2010;49:661–669. doi: 10.2165/11536200-000000000-00000. [DOI] [PubMed] [Google Scholar]
- Boldrini M, Canoll PD, Klein RS. How COVID-19 Affects the Brain. JAMA Psychiat. 2021;78:682. doi: 10.1001/jamapsychiatry.2021.0500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronte V, Ugel S, Tinazzi E, et al. Baricitinib restrains the immune dysregulation in patients with severe COVID-19. J Clin Invest. 2020;130:6409–6416. doi: 10.1172/JCI141772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Busch A, Barber K, Overend T, et al. Exercise for treating fibromyalgia syndrome. In: Busch A, et al., editors. The cochrane database of systematic reviews (Protocol) Chichester: John Wiley & Sons, Ltd; 2002. p. 3786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buskila D, Atzeni F, Sarzi-Puttini P. Etiology of fibromyalgia: the possible role of infection and vaccination. Autoimmun Rev. 2008;8:41–43. doi: 10.1016/j.autrev.2008.07.023. [DOI] [PubMed] [Google Scholar]
- Caiazzo E, Rezig AOM, Bruzzese D, et al. Systemic administration of glucocorticoids, cardiovascular complications and mortality in patients hospitalised with COVID-19, SARS, MERS or influenza: a systematic review and meta-analysis of randomised trials. Pharmacol Res. 2022;176:106053. doi: 10.1016/J.PHRS.2021.106053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cankurtaran D, Tezel N, Ercan B, et al. The effects of COVID-19 fear and anxiety on symptom severity, sleep quality, and mood in patients with fibromyalgia: a pilot study. Adv Rheumatol. 2021;61:41. doi: 10.1186/s42358-021-00200-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cano EJ, Fonseca Fuentes X, Corsini Campioli C, et al. Impact of corticosteroids in coronavirus disease 2019 outcomes. Chest. 2021;159:1019–1040. doi: 10.1016/j.chest.2020.10.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cantuti-Castelvetri L, Ojha R, Pedro LD, et al. Neuropilin-1 facilitates SARS-CoV-2 cell entry and infectivity. Science. 2020;370:856–860. doi: 10.1126/science.abd2985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao Y, Wei J, Zou L, et al. Ruxolitinib in treatment of severe coronavirus disease 2019 (COVID-19): a multicenter, single-blind, randomized controlled trial. J Allergy Clin Immunol. 2020;146:137–146.e3. doi: 10.1016/J.JACI.2020.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carfì A, Bernabei R, Landi F. Persistent symptoms in patients after acute COVID-19. JAMA. 2020;324:603–605. doi: 10.1001/jama.2020.12603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavalli G, De Luca G, Campochiaro C, et al. Interleukin-1 blockade with high-dose anakinra in patients with COVID-19, acute respiratory distress syndrome, and hyperinflammation: a retrospective cohort study. Lancet Rheumatol. 2020;2:e325–e331. doi: 10.1016/S2665-9913(20)30127-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavalli G, Cariddi A, Ferrari J, et al. Living with fibromyalgia during the COVID-19 pandemic: mixed effects of prolonged lockdown on the well-being of patients. Rheumatol. 2021;60:465–467. doi: 10.1093/rheumatology/keaa738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cecchini R, Cecchini AL. SARS-CoV-2 infection pathogenesis is related to oxidative stress as a response to aggression. Med Hypotheses. 2020;143:110102. doi: 10.1016/J.MEHY.2020.110102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandan JS, Brown K, Simms-Williams N, et al. Protocol: non-pharmacological therapies for postviral syndromes, including Long COVID: a systematic review and meta-analysis protocol. BMJ Open. 2022;12:57885. doi: 10.1136/BMJOPEN-2021-057885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang S, Minn D, Kim S-W, Kim Y. Inflammatory Markers and Cytokines in Moderate and Critical Cases of COVID-19. Clin Lab. 2021 doi: 10.7754/Clin.Lab.2021.210142. [DOI] [PubMed] [Google Scholar]
- Chen G, Wu D, Guo W, et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J Clin Invest. 2020;130:2620–2629. doi: 10.1172/JCI137244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen X, Zhao B, Qu Y, et al. Detectable serum severe acute respiratory syndrome coronavirus 2 viral load (RNAemia) is closely correlated with drastically elevated interleukin 6 level in critically Ill patients with coronavirus disease 2019. Clin Infect Dis. 2020;71:1937–1942. doi: 10.1093/cid/ciaa449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choy EHS. The role of sleep in pain and fibromyalgia. Nat Rev Rheumatol. 2015;11:513–520. doi: 10.1038/nrrheum.2015.56. [DOI] [PubMed] [Google Scholar]
- Clauw DJ. Fibromyalgia. JAMA. 2014;311:1547. doi: 10.1001/jama.2014.3266. [DOI] [PubMed] [Google Scholar]
- Clauw DJ. Fibromyalgia and related conditions. Mayo Clin Proc. 2015;90:680–692. doi: 10.1016/j.mayocp.2015.03.014. [DOI] [PubMed] [Google Scholar]
- Clauw DJ, Häuser W, Cohen SP, Fitzcharles M-A. Considering the potential for an increase in chronic pain after the COVID-19 pandemic. Pain. 2020;161:1694–1697. doi: 10.1097/j.pain.0000000000001950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clemency BM, Varughese R, Gonzalez-Rojas Y, et al. Efficacy of inhaled ciclesonide for outpatient treatment of adolescents and adults with symptomatic COVID-19: a randomized clinical trial. JAMA Intern Med. 2022;182:42–49. doi: 10.1001/JAMAINTERNMED.2021.6759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cordero MD, De Miguel M, Moreno Fernández AM, et al. Mitochondrial dysfunction and mitophagy activation in blood mononuclear cells of fibromyalgia patients: implications in the pathogenesis of the disease. Arthritis Res Ther. 2010;12:R17. doi: 10.1186/ar2918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cordero MD, Cano-García FJ, Alcocer-Gómez E, et al. Oxidative stress correlates with headache symptoms in fibromyalgia: coenzyme Q 10 effect on clinical improvement. PLoS ONE. 2012;7:6–11. doi: 10.1371/journal.pone.0035677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cordero MD, Cotán D, del-Pozo-Martín Y, et al. Oral coenzyme Q10 supplementation improves clinical symptoms and recovers pathologic alterations in blood mononuclear cells in a fibromyalgia patient. Nutrition. 2012;28:1200–1203. doi: 10.1016/j.nut.2012.03.018. [DOI] [PubMed] [Google Scholar]
- Cordero MD, Alcocer-Gómez E, Culic O, et al. NLRP3 inflammasome is activated in fibromyalgia: the effect of coenzyme Q 10. Antioxid Redox Signal. 2014;20:1169–1180. doi: 10.1089/ars.2013.5198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Disser NP, De Micheli AJ, Schonk MM, et al. Musculoskeletal consequences of COVID-19. J Bone Jt Surg - Am. 2020;102:1197–1204. doi: 10.2106/JBJS.20.00847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- dos Santos AAC, Rodrigues LE, Alecrim-Zeza AL, et al. Molecular and cellular mechanisms involved in tissue-specific metabolic modulation by SARS-CoV-2. Front Microbiol. 2022;13:4553. doi: 10.3389/FMICB.2022.1037467/BIBTEX. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dotan A, David P, Arnheim D, Shoenfeld Y. The autonomic aspects of the post-COVID19 syndrome. Autoimmun Rev. 2022 doi: 10.1016/J.AUTREV.2022.103071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisinger J, Plantamura A, Ayavou T. Glycolysis abnormalities in fibromyalgia. J Am Coll Nutr. 1994;13:144–148. doi: 10.1080/07315724.1994.10718387. [DOI] [PubMed] [Google Scholar]
- Elkan M, Dvir A, Zaidenstein R, et al. Patient-reported outcome measures after hospitalization during the COVID-19 pandemic: a survey among COVID-19 and non-COVID-19 patients. Int J Gen Med. 2021;14:4829–4836. doi: 10.2147/IJGM.S323316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ely EW, Ramanan AV, Kartman CE, et al. Efficacy and safety of baricitinib plus standard of care for the treatment of critically ill hospitalised adults with COVID-19 on invasive mechanical ventilation or extracorporeal membrane oxygenation: an exploratory, randomised, placebo-controlled trial. Lancet Respir Med. 2022;10:327–336. doi: 10.1016/S2213-2600(22)00006-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evdokimov D, Frank J, Klitsch A, et al. Reduction of skin innervation is associated with a severe fibromyalgia phenotype. Ann Neurol. 2019;86:504–516. doi: 10.1002/ana.25565. [DOI] [PubMed] [Google Scholar]
- Fanelli D, Weller G, Liu H. New serotonin-norepinephrine reuptake inhibitors and their anesthetic and analgesic considerations. Neurol Int. 2021;13:497–509. doi: 10.3390/NEUROLINT13040049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fasolino A, Di Stefano G, Leone C, et al. Small-fibre pathology has no impact on somatosensory system function in patients with fibromyalgia. Pain Publish Ah: 2020 doi: 10.1097/j.pain.0000000000001920. [DOI] [PubMed] [Google Scholar]
- Fernández-de-las-Peñas C, De-la-Llave-Rincón AI, Ortega-Santiago R, et al. Prevalence and risk factors of musculoskeletal pain symptoms as long-term post-COVID sequelae in hospitalized COVID-19 survivors. Pain. 2021 doi: 10.1097/j.pain.0000000000002564. [DOI] [PubMed] [Google Scholar]
- Fernández-de-las-Peñas C, Rodríguez-Jiménez J, Fuensalida-Novo S, et al. Myalgia as a symptom at hospital admission by severe acute respiratory syndrome coronavirus 2 infection is associated with persistent musculoskeletal pain as long-term post-COVID sequelae: a case-control study. Pain. 2021;162:2832–2840. doi: 10.1097/j.pain.0000000000002306. [DOI] [PubMed] [Google Scholar]
- Fernández-de-las-Peñas C, Navarro-Santana M, Plaza-Manzano G, et al. Time course prevalence of post-COVID pain symptoms of musculoskeletal origin in patients who had survived severe acute respiratory syndrome coronavirus 2 infection: a systematic review and meta-analysis. Pain. 2022;163:1220–1231. doi: 10.1097/j.pain.0000000000002496. [DOI] [PubMed] [Google Scholar]
- Fernández-de-las-Peñas C, Cancela-Cilleruelo I, Moro-López-Menchero P, et al. Exploring the trajectory curve of long-term musculoskeletal post-COVID pain symptoms in hospitalized COVID-19 survivors: a multicenter study. Pain. 2023;164:413–420. doi: 10.1097/j.pain.0000000000002718. [DOI] [PubMed] [Google Scholar]
- Fitzcharles M-A, Cohen SP, Clauw DJ, et al. Nociplastic pain: towards an understanding of prevalent pain conditions. Lancet. 2021;397:2098–2110. doi: 10.1016/S0140-6736(21)00392-5. [DOI] [PubMed] [Google Scholar]
- Forcados GE, Muhammad A, Oladipo OO, et al. Metabolic implications of oxidative stress and inflammatory process in SARS-CoV-2 pathogenesis: therapeutic potential of natural antioxidants. Front Cell Infect Microbiol. 2021;11:654813. doi: 10.3389/fcimb.2021.654813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gentil P, de Lira CAB, Vieira CA, et al. Resistance training before, during, and after COVID-19 infection: what have we learned so far? Int J Environ Res Public Health. 2022 doi: 10.3390/IJERPH19106323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gheita TA, Fathi HM, Eladle SS, et al. Coronavirus disease 2019 ( COVID-19) an emerging trigger for primary fibromyalgia syndrome : a tale of three cases post-COVID-19. Int J Clin Rheumtol. 2021;16:129–135. [Google Scholar]
- Giamarellos-Bourboulis EJ, Netea MG, Rovina N, et al. Complex immune dysregulation in COVID-19 patients with severe respiratory failure. Cell Host Microbe. 2020;27:992–1000.e3. doi: 10.1016/J.CHOM.2020.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godolphin PJ, Fisher DJ, Berry LR, et al. Association between tocilizumab, sarilumab and all-cause mortality at 28 days in hospitalised patients with COVID-19: a network meta-analysis. PLoS ONE. 2022;17:e0270668. doi: 10.1371/JOURNAL.PONE.0270668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goebel A, Krock E, Gentry C, et al. Passive transfer of fibromyalgia symptoms from patients to mice. J Clin Invest. 2021;131:144201. doi: 10.1172/JCI144201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez-Martinez A, Guerrero-Peral ÁL, Arias-Rivas S, et al. Amitriptyline for post-COVID headache: effectiveness, tolerability, and response predictors. J Neurol. 2022;269:5702–5709. doi: 10.1007/S00415-022-11225-5/TABLES/4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goudman L, De Smedt A, Noppen M, Moens M. Is central sensitisation the missing link of persisting symptoms after COVID-19 infection? J Clin Med. 2021 doi: 10.3390/JCM10235594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham EL, Clark JR, Orban ZS, et al. Persistent neurologic symptoms and cognitive dysfunction in non-hospitalized Covid-19 “long haulers”. Ann Clin Transl Neurol. 2021;8:1073–1085. doi: 10.1002/acn3.51350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guan W, Ni Z, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harapan BN, Yoo HJ. Neurological symptoms, manifestations, and complications associated with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease 19 (COVID-19) J Neurol. 2021;268:3059–3071. doi: 10.1007/s00415-021-10406-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrington R, Al Nokhatha SA, Conway R. JAK inhibitors in rheumatoid arthritis: an evidence-based review on the emerging clinical data. J Inflamm Res. 2020;13:519. doi: 10.2147/JIR.S219586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Häuser W, Ablin J, Fitzcharles M-A, et al. Fibromyalgia. Nat Rev Dis Prim. 2015;1:15022. doi: 10.1038/nrdp.2015.22. [DOI] [PubMed] [Google Scholar]
- Häuser W, Perrot S, Sommer C, et al. Diagnostic confounders of chronic widespread pain: not always fibromyalgia. PAIN Reports. 2017;2:598. doi: 10.1097/PR9.0000000000000598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heesakkers H, Van Der Hoeven JG, Corsten S, et al. Clinical outcomes among patients with 1-year survival following intensive care unit treatment for COVID-19. JAMA. 2022;327:559–565. doi: 10.1001/JAMA.2022.0040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernando-Garijo I, Ceballos-Laita L, Mingo-Gómez MT, et al. Immediate effects of a telerehabilitation program based on aerobic exercise in women with fibromyalgia. Int J Environ Res Public Health. 2021;18:1–12. doi: 10.3390/IJERPH18042075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horby PW, Martin P, Landray J. Colchicine in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial. Lancet Respir Med. 2021;9:1419–1426. doi: 10.1016/S2213-2600(21)00435-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hosey MM, Needham DM. Survivorship after COVID-19 ICU stay. Nat Rev Dis Prim. 2020;6:60. doi: 10.1038/s41572-020-0201-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang E, Jordan SC. Tocilizumab for Covid-19 — the ongoing search for effective therapies. N Engl J Med. 2020;383:2387–2388. doi: 10.1056/NEJME2032071/SUPPL_FILE/NEJME2032071_DISCLOSURES.PDF. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang C, Huang L, Wang Y, et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet. 2021;397:220–232. doi: 10.1016/S0140-6736(20)32656-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang L, Yao Q, Gu X, et al. 1-year outcomes in hospital survivors with COVID-19: a longitudinal cohort study. Lancet. 2021;398:747–758. doi: 10.1016/S0140-6736(21)01755-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huet T, Beaussier H, Voisin O, et al. Anakinra for severe forms of COVID-19: a cohort study. Lancet Rheumatol. 2020;2:e393–e400. doi: 10.1016/S2665-9913(20)30164-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hung C-H, Lee C-H, Tsai M-H, et al. Activation of acid-sensing ion channel 3 by lysophosphatidylcholine 16:0 mediates psychological stress-induced fibromyalgia-like pain. Ann Rheum Dis. 2020;79:1644–1656. doi: 10.1136/annrheumdis-2020-218329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iannuccelli C, Lucchino B, Gioia C, et al. Mental health and well-being during the COVID-19 pandemic: stress vulnerability, resilience and mood disturbances in fibromyalgia and rheumatoid arthritis. Clin Exp Rheumatol. 2021;39:153–160. doi: 10.55563/clinexprheumatol/4nb0ku. [DOI] [PubMed] [Google Scholar]
- Inoue S, Hatakeyama J, Kondo Y, et al. Post-intensive care syndrome: its pathophysiology, prevention, and future directions. Acute Med Surg. 2019;6:233–246. doi: 10.1002/ams2.415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jena D, Sahoo J, Barman A, et al. Neuropathic pain in hospitalized patients with COVID-19: a prospective case series. Arch Rehabil Res Clin Transl. 2022;4:100188. doi: 10.1016/J.ARRCT.2022.100188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ji RR, Nackley A, Huh Y, et al. Neuroinflammation and central sensitization in chronic and widespread pain. Anesthesiology. 2018;129:343–366. doi: 10.1097/ALN.0000000000002130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Josephson SA, Kamel H. Neurology and COVID-19. JAMA. 2020;324:1139. doi: 10.1001/jama.2020.14254. [DOI] [PubMed] [Google Scholar]
- Kalil AC, Patterson TF, Mehta AK, et al. Baricitinib plus remdesivir for hospitalized adults with Covid-19. N Engl J Med. 2021;384:795–807. doi: 10.1056/NEJMOA2031994/SUPPL_FILE/NEJMOA2031994_DATA-SHARING.PDF. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamimura D, Ishihara K, Hirano T. IL-6 signal transduction and its physiological roles: the signal orchestration model. Rev Physiol Biochem Pharmacol. 2003;149:1–38. doi: 10.1007/S10254-003-0012-2. [DOI] [PubMed] [Google Scholar]
- Karos K, McParland JL, Bunzli S, et al. The social threats of COVID-19 for people with chronic pain. Pain. 2020;161:2229–2235. doi: 10.1097/j.pain.0000000000002004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kayaaslan B, Eser F, Kalem AK, et al. Post-COVID syndrome: a single-center questionnaire study on 1007 participants recovered from COVID-19. J Med Virol. 2021;93:6566–6574. doi: 10.1002/jmv.27198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kemp HI, Laycock H, Costello A, Brett SJ. Chronic pain in critical care survivors : a narrative review. Br J Anaesth. 2019;123:e372–e384. doi: 10.1016/j.bja.2019.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kemp HI, Corner E, Colvin LA. Chronic pain after COVID-19: implications for rehabilitation. Br J Anaesth. 2020;125:436–440. doi: 10.1016/j.bja.2020.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirito K. Recent progress of JAK inhibitors for hematological disorders. Immunol Med. 2022 doi: 10.1080/25785826.2022.2139317. [DOI] [PubMed] [Google Scholar]
- Komaroff AL, Lipkin WI. Insights from myalgic encephalomyelitis/chronic fatigue syndrome may help unravel the pathogenesis of postacute COVID-19 syndrome. Trends Mol Med. 2021;27:895–906. doi: 10.1016/j.molmed.2021.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kosek E, Clauw D, Nijs J, et al. Chronic nociplastic pain affecting the musculoskeletal system: clinical criteria and grading system. Pain. 2021;162:2629–2634. doi: 10.1097/J.PAIN.0000000000002324. [DOI] [PubMed] [Google Scholar]
- Kostorz-Nosal S, Jastrzębski D, Chyra M, et al. A prolonged steroid therapy may be beneficial in some patients after the COVID-19 pneumonia. Eur Clin Respir J. 2021 doi: 10.1080/20018525.2021.1945186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krynytska I, Marushchak M, Birchenko I, et al. COVID-19-associated acute respiratory distress syndrome versus classical acute respiratory distress syndrome (a narrative review) Iran J Microbiol. 2021;13:737. doi: 10.18502/IJM.V13I6.8072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kucuk A, Cumhur Cure M, Cure E. Can COVID-19 cause myalgia with a completely different mechanism? A hypothesis. Clin Rheumatol. 2020;39:2103–2104. doi: 10.1007/s10067-020-05178-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar A, Loharch S, Kumar S, et al. Exploiting cheminformatic and machine learning to navigate the available chemical space of potential small molecule inhibitors of SARS-CoV-2. Comput Struct Biotechnol J. 2021;19:424–438. doi: 10.1016/J.CSBJ.2020.12.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kutkat O, Moatasim Y, Al-Karmalawy AA, et al. Robust antiviral activity of commonly prescribed antidepressants against emerging coronaviruses: in vitro and in silico drug repurposing studies. Sci Rep. 2022;121(12):1–12. doi: 10.1038/s41598-022-17082-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamontagne F, Agarwal A, Rochwerg B, et al. A living WHO guideline on drugs for covid-19. BMJ. 2020;370:m3379. doi: 10.1136/bmj.m3379. [DOI] [PubMed] [Google Scholar]
- Landewé RBM, Machado PM, Kroon F, et al. EULAR provisional recommendations for the management of rheumatic and musculoskeletal diseases in the context of SARS-CoV-2. Ann Rheum Dis. 2020;79:851–858. doi: 10.1136/annrheumdis-2020-217877. [DOI] [PubMed] [Google Scholar]
- Larson AA, Pardo JV, Pasley JD. Review of overlap between thermoregulation and pain modulation in fibromyalgia. Clin J Pain. 2014;30:544–555. doi: 10.1097/AJP.0b013e3182a0e383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liguori C, Pierantozzi M, Spanetta M, et al. Subjective neurological symptoms frequently occur in patients with SARS-CoV2 infection. Brain Behav Immun. 2020;88:11–16. doi: 10.1016/j.bbi.2020.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liguori C, Pierantozzi M, Spanetta M, et al. Depressive and anxiety symptoms in patients with SARS-CoV2 infection. J Affect Disord. 2021;278:339–340. doi: 10.1016/j.jad.2020.09.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Littlejohn G. Neurogenic neuroinflammation in fibromyalgia and complex regional pain syndrome. Nat Rev Rheumatol. 2015;11:639–648. doi: 10.1038/nrrheum.2015.100. [DOI] [PubMed] [Google Scholar]
- Littlejohn G, Guymer E. Neurogenic inflammation in fibromyalgia. Semin Immunopathol. 2018;40:291–300. doi: 10.1007/s00281-018-0672-2. [DOI] [PubMed] [Google Scholar]
- Logue JK, Franko NM, McCulloch DJ, et al. Sequelae in adults at 6 months after COVID-19 infection. JAMA Netw Open. 2021;4:e210830. doi: 10.1001/jamanetworkopen.2021.0830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- López-Solà M, Woo C-W, Pujol J, et al. Towards a neurophysiological signature for fibromyalgia. Pain. 2017;158:34–47. doi: 10.1097/j.pain.0000000000000707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahmudpour M, Roozbeh J, Keshavarz M, et al. COVID-19 cytokine storm: the anger of inflammation. Cytokine. 2020;133:155151. doi: 10.1016/j.cyto.2020.155151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mao L, Jin H, Wang M, et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020;77:683. doi: 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marconi VC, Ramanan AV, de Bono S, et al. Efficacy and safety of baricitinib for the treatment of hospitalised adults with COVID-19 (COV-BARRIER): a randomised, double-blind, parallel-group, placebo-controlled phase 3 trial. Lancet Respir Med. 2021;9:1407–1418. doi: 10.1016/S2213-2600(21)00331-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McFarland AJ, Yousuf MS, Shiers S, Price TJ. Neurobiology of SARS-CoV-2 interactions with the peripheral nervous system: implications for COVID-19 and pain. Pain Reports. 2021;6:e885. doi: 10.1097/PR9.0000000000000885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGonagle D, Sharif K, O’Regan A, Bridgewood C. The role of cytokines including interleukin-6 in COVID-19 induced pneumonia and macrophage activation syndrome-like disease. Autoimmun Rev. 2020 doi: 10.1016/J.AUTREV.2020.102537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLain D. The effects of tizanidine HCL (Zanaflex®) in patients with fibromyalgia. Pain Med. 2000;1:207–207. doi: 10.1046/j.1526-4637.2000.000024-48.x. [DOI] [Google Scholar]
- Meeus M, Nijs J, Hermans L, et al. The role of mitochondrial dysfunctions due to oxidative and nitrosative stress in the chronic pain or chronic fatigue syndromes and fibromyalgia patients: peripheral and central mechanisms as therapeutic targets? Expert Opin Ther Targets. 2013;17:1081–1089. doi: 10.1517/14728222.2013.818657. [DOI] [PubMed] [Google Scholar]
- Meulders A, Vlaeyen JWS, Evers AWM, et al. Chronic primary pain in the COVID-19 pandemic: how uncertainty and stress impact on functioning and suffering. Pain. 2022;163:604–609. doi: 10.1097/J.PAIN.0000000000002428. [DOI] [PubMed] [Google Scholar]
- Moghimi N, Di Napoli M, Biller J, et al. The neurological manifestations of post-acute sequelae of SARS-CoV-2 infection. Curr Neurol Neurosci Rep. 2021;21:44. doi: 10.1007/s11910-021-01130-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mogil JS. Social modulation of and by pain in humans and rodents. Pain. 2015;156:S35–S41. doi: 10.1097/01.j.pain.0000460341.62094.77. [DOI] [PubMed] [Google Scholar]
- Mohabbat AB, Mohabbat NML, Wight EC. Fibromyalgia and chronic fatigue syndrome in the age of COVID-19. Mayo Clin Proc Innov Qual Outcomes. 2020;4:764–766. doi: 10.1016/j.mayocpiqo.2020.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nalbandian A, Sehgal K, Gupta A, et al. Post-acute COVID-19 syndrome. Nat Med. 2021;27:601–615. doi: 10.1038/s41591-021-01283-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nalleballe K, Reddy Onteddu S, Sharma R, et al. Spectrum of neuropsychiatric manifestations in COVID-19. Brain Behav Immun. 2020;88:71–74. doi: 10.1016/j.bbi.2020.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Napadow V, LaCount L, Park K, et al. Intrinsic brain connectivity in fibromyalgia is associated with chronic pain intensity. Arthritis Rheum. 2010;62:2545–2555. doi: 10.1002/art.27497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nasserie T, Hittle M, Goodman SN. Assessment of the frequency and variety of persistent symptoms among patients with COVID-19. JAMA Netw Open. 2021;4:e2111417. doi: 10.1001/jamanetworkopen.2021.11417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nataf S. An alteration of the dopamine synthetic pathway is possibly involved in the pathophysiology of COVID-19. J Med Virol. 2020;92:1743–1744. doi: 10.1002/jmv.25826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nehme M, Braillard O, Chappuis F, et al. Prevalence of symptoms more than seven months after diagnosis of symptomatic COVID-19 in an outpatient setting. Ann Intern Med. 2021;174:1252–1260. doi: 10.7326/M21-0878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Health, NHS (2021) Interim Clinical Commissioning Policy: IL-6 inhibitors (tocilizumab or sarilumab) for hospitalised patients with COVID-19 (adults). Rapid Policy Statement 1–5
- Oddy C, McCaul J, Keeling P, et al. Pharmacological predictors of morbidity and mortality in COVID-19. J Clin Pharmacol. 2021;61:1286–1300. doi: 10.1002/jcph.1878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oh T-K, Song I-A, Lee J, et al. Musculoskeletal disorders, pain medication, and in-hospital mortality among patients with COVID-19 in South Korea: a population-based cohort study. Int J Environ Res Public Health. 2021;18:6804. doi: 10.3390/ijerph18136804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oray M, Abu Samra K, Ebrahimiadib N, et al. Long-term side effects of glucocorticoids. Expert Opin Drug Saf. 2016;15:457–465. doi: 10.1517/14740338.2016.1140743. [DOI] [PubMed] [Google Scholar]
- Park JH, Niermann KJ, Olsen NJ. Evidence for metabolic abnormalities in the muscles of patients with fibromyalgia. Curr Rheumatol Rep. 2000;2:131–140. doi: 10.1007/s11926-000-0053-3. [DOI] [PubMed] [Google Scholar]
- Pektas S, Gursoy C, Demirbilek SG. The use of pregabalin in Intensive Care Unit in the treatment of Covid-19-related pain and cough. J Coll Physicians Surg Pak. 2021;31:S143–S143. doi: 10.29271/jcpsp.2021.Supp2.S143. [DOI] [PubMed] [Google Scholar]
- Perez J, Niburski K, Stoopler M, Ingelmo P. Telehealth and chronic pain management from rapid adaptation to long-term implementation in pain medicine: a narrative review. PAIN Reports. 2021;6:e912. doi: 10.1097/pr9.0000000000000912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perico N, Cortinovis M, Suter F, Remuzzi G. Home as the new frontier for the treatment of COVID-19: the case for anti-inflammatory agents. Lancet Infect Dis. 2022;23:e22–e33. doi: 10.1016/S1473-3099(22)00433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plasencia-García BO, Rico-Rangel MI, Rodríguez-Menéndez G, et al. Drug-drug Interactions between COVID-19 treatments and antidepressants, mood stabilizers/anticonvulsants, and benzodiazepines: integrated evidence from 3 databases. Pharmacopsychiatry. 2021 doi: 10.1055/a-1492-3293. [DOI] [PubMed] [Google Scholar]
- Rada M, Qusairy Z, Massip-Salcedo M, Macip S. Relevance of the bruton tyrosine kinase as a target for COVID-19 therapy. Mol Cancer Res. 2021;19:549–554. doi: 10.1158/1541-7786.MCR-20-0814. [DOI] [PubMed] [Google Scholar]
- RECOVERY CG, Dexamethasone in hospitalized patients with Covid-19. N Engl J Med. 2021;384:693–704. doi: 10.1056/NEJMoa2021436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rinnerthaler M, Bischof J, Streubel MK, et al. Oxidative stress in aging human skin. Biomolecules. 2015;5:545–589. doi: 10.3390/biom5020545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roschewski M, Lionakis MS, Sharman JP, et al. Inhibition of Bruton tyrosine kinase in patients with severe COVID-19. Sci Immunol. 2020 doi: 10.1126/SCIIMMUNOL.ABD0110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowbotham MC, Arendt-Nielsen L. A year like no other: introduction to a special issue on COVID-19 and pain. PAIN Rep. 2021;6:e915. doi: 10.1097/PR9.0000000000000915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabe M, Dorsaz O, Huguelet P, Kaiser S. Toxicity of psychotropic drugs in patients with COVID-19: a systematic review. Gen Hosp Psychiatry. 2021;70:1–9. doi: 10.1016/J.GENHOSPPSYCH.2021.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salaffi F, Giorgi V, Sirotti S, et al. The effect of novel coronavirus disease-2019 (COVID-19) on fibromyalgia syndrome. Clin Exp Rheumatol. 2021;39:S72–S77. doi: 10.55563/clinexprheumatol/dnxtch. [DOI] [PubMed] [Google Scholar]
- Salama C, Han J, Yau L, et al. Tocilizumab in patients hospitalized with Covid-19 pneumonia. N Engl J Med. 2021;384:20–30. doi: 10.1056/NEJMOA2030340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saleh J, Peyssonnaux C, Singh KK, Edeas M. Mitochondria and microbiota dysfunction in COVID-19 pathogenesis. Mitochondrion. 2020;54:1–7. doi: 10.1016/j.mito.2020.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarzi-Puttini P, Giorgi V, Marotto D, Atzeni F. Fibromyalgia: an update on clinical characteristics, aetiopathogenesis and treatment. Nat Rev Rheumatol. 2020;16:645–660. doi: 10.1038/s41584-020-00506-w. [DOI] [PubMed] [Google Scholar]
- Scherlinger M, Felten R, Gallais F, et al. Refining “Long-COVID” by a prospective multimodal evaluation of patients with long-term symptoms attributed to SARS-CoV-2 infection. Infect Dis Ther. 2021;10:1747–1763. doi: 10.1007/s40121-021-00484-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schett G, Manger B, Simon D, Caporali R. COVID-19 revisiting inflammatory pathways of arthritis. Nat Rev Rheumatol. 2020;16:465–470. doi: 10.1038/s41584-020-0451-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schweiger V, Secchettin E, Castellani C, et al. Comparison between acupuncture and nutraceutical treatment with migratens® in patients with fibromyalgia syndrome: a prospective randomized clinical trial. Nutrients. 2020;12:821. doi: 10.3390/nu12030821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiers S, Ray PR, Wangzhou A, et al. ACE2 and SCARF expression in human dorsal root ganglion nociceptors: implications for SARS-CoV-2 virus neurological effects. Pain. 2020;161:2494–2501. doi: 10.1097/j.pain.0000000000002051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shipton EE, Shipton EA. Vitamin D deficiency and pain: clinical evidence of low levels of vitamin D and supplementation in chronic pain states. Pain Ther. 2015;4:67. doi: 10.1007/S40122-015-0036-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slee A, Nazareth I, Bondaronek P, et al. Pharmacological treatments for generalised anxiety disorder: a systematic review and network meta-analysis. Lancet. 2019;393:768–777. doi: 10.1016/S0140-6736(18)31793-8. [DOI] [PubMed] [Google Scholar]
- Sterne JAC, Murthy S, Diaz JV, et al. Association between administration of systemic corticosteroids and mortality among critically Ill patients with COVID-19: a meta-analysis. JAMA. 2020;324:1330–1341. doi: 10.1001/jama.2020.17023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tancheva L, Petralia MC, Miteva S, et al. Emerging neurological and psychobiological aspects of COVID-19 infection. Brain Sci. 2020;10:852. doi: 10.3390/brainsci10110852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tardif JC, Bouabdallaoui N, L’Allier PL, et al. Colchicine for community-treated patients with COVID-19 (COLCORONA): a phase 3, randomised, double-blinded, adaptive, placebo-controlled, multicentre trial. Lancet Respir Med. 2021;9:924–932. doi: 10.1016/S2213-2600(21)00222-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Theoharides TC, Tsilioni I, Bawazeer M. Mast cells, neuroinflammation and pain in fibromyalgia syndrome. Front Cell Neurosci. 2019;13:1–8. doi: 10.3389/fncel.2019.00353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Townsend L, Dowds J, O’Brien K, et al. Persistent poor health after COVID-19 is not associated with respiratory complications or initial disease severity. Ann Am Thorac Soc. 2021;18:997–1003. doi: 10.1513/AnnalsATS.202009-1175OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Treede R-D, Rief W, Barke A, et al. Chronic pain as a symptom or a disease: the IASP classification of chronic pain for the International Classification of Diseases (ICD-11) Pain. 2019;160:19–27. doi: 10.1097/j.pain.0000000000001384. [DOI] [PubMed] [Google Scholar]
- Tuzun S, Keles A, Okutan D, et al. Assessment of musculoskeletal pain, fatigue and grip strength in hospitalized patients with COVID-19. Eur J Phys Rehabil Med. 2021;57:653–662. doi: 10.23736/S1973-9087.20.06563-6. [DOI] [PubMed] [Google Scholar]
- Üçeyler N, Zeller D, Kahn AK, et al. Small fibre pathology in patients with fibromyalgia syndrome. Brain. 2013;136:1857–1867. doi: 10.1093/brain/awt053. [DOI] [PubMed] [Google Scholar]
- Ursini F, Ciaffi J, Mancarella L, et al. Fibromyalgia: a new facet of the post-COVID-19 syndrome spectrum? Results from a web-based survey. RMD Open. 2021;7:e001735. doi: 10.1136/rmdopen-2021-001735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valiuddin H, Skwirsk B, Paz-Arabo P. Acute transverse myelitis associated with SARS-CoV-2: a case-report. Brain, Behav Immun Heal. 2020;5:100091. doi: 10.1016/j.bbih.2020.100091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van de Veerdonk FL, Giamarellos-Bourboulis E, Pickkers P, et al. A guide to immunotherapy for COVID-19. Nat Med. 2022;28:39–50. doi: 10.1038/s41591-021-01643-9. [DOI] [PubMed] [Google Scholar]
- Varga TV, Bu F, Dissing AS, et al. Loneliness, worries, anxiety, and precautionary behaviours in response to the COVID-19 pandemic: a longitudinal analysis of 200,000 Western and Northern Europeans. Lancet Reg Heal Eur. 2021;2:100020. doi: 10.1016/j.lanepe.2020.100020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vertigan AE, Kapela SL, Ryan NM, et al. Pregabalin and speech pathology combination therapy for refractory chronic cough a randomized controlled trial. Chest. 2016;149:639–648. doi: 10.1378/chest.15-1271. [DOI] [PubMed] [Google Scholar]
- Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang EY, Mao T, Klein J, et al. Diverse functional autoantibodies in patients with COVID-19. Nature. 2021;595:283–288. doi: 10.1038/s41586-021-03631-y. [DOI] [PubMed] [Google Scholar]
- WHO (2023) Globally confirmed cases of COVID-19. World Health Organization. https://covid19.who.int/. Accessed 13 Dec 2021
- Widyadharma IPE, Dewi PR, Wijayanti IAS, Utami DKI. Pain related viral infections: a literature review. Egypt J Neurol Psychiatry Neurosurg. 2020;56:105. doi: 10.1186/s41983-020-00238-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiersinga WJ, Rhodes A, Cheng AC, et al. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): a review. JAMA. 2020;324:782–793. doi: 10.1001/jama.2020.12839. [DOI] [PubMed] [Google Scholar]
- Wiersinga WJ, Rhodes A, Cheng AC, et al. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19) JAMA. 2020;324:782. doi: 10.1001/jama.2020.12839. [DOI] [PubMed] [Google Scholar]
- Wolfe F, Clauw DJ, Fitzcharles M-A, et al. The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res (hoboken) 2010;62:600–610. doi: 10.1002/acr.20140. [DOI] [PubMed] [Google Scholar]
- Xin P, Xu X, Deng C, et al. The role of JAK/STAT signaling pathway and its inhibitors in diseases. Int Immunopharmacol. 2020 doi: 10.1016/J.INTIMP.2020.106210. [DOI] [PubMed] [Google Scholar]
- Xu C, Rafique A, Potocky T, et al. Differential binding of sarilumab and tocilizumab to IL-6Rα and effects of receptor occupancy on clinical parameters. J Clin Pharmacol. 2021;61:714–724. doi: 10.1002/JCPH.1795. [DOI] [PubMed] [Google Scholar]
- Yu LM, Bafadhel M, Dorward J, et al. Inhaled budesonide for COVID-19 in people at high risk of complications in the community in the UK (PRINCIPLE): a randomised, controlled, open-label, adaptive platform trial. Lancet. 2021;398:843–855. doi: 10.1016/S0140-6736(21)01744-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zamorano Cuervo N, Grandvaux N. ACE2: Evidence of role as entry receptor for SARS-CoV-2 and implications in comorbidities. Elife. 2020;9:61390. doi: 10.7554/eLife.61390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang W, Qin C, Fei Y, et al. Anti-inflammatory and immune therapy in severe coronavirus disease 2019 (COVID-19) patients: an update. Clin Immunol. 2022;239:109022. doi: 10.1016/J.CLIM.2022.109022. [DOI] [PMC free article] [PubMed] [Google Scholar]