Abstract
Background:
Anecdotal evidence suggests that the profile of midwifery clients in British Columbia has changed over the past 20 years and that midwives are increasingly caring for clients with moderate to high medical risk. We sought to compare perinatal outcomes with a registered midwife as the most responsible provider (MRP) versus outcomes among clients with physicians as their MRP across medical risk strata.
Methods:
This retrospective cohort study (2008–2018) used data from the BC Perinatal Data Registry. We included all births that had a family physician, obstetrician or midwife listed as the MRP (n = 425 056) and stratified the analysis by pregnancy risk status (low, moderate or high) according to an adapted perinatal risk scoring system. We estimated differences in outcomes between MRP groups by calculating adjusted absolute and relative risks.
Results:
The adjusted absolute and relative risks of adverse neonatal outcomes were consistently lower among those who chose midwifery care across medical risk strata, compared with clients who had a physician as MRP. Midwifery clients experienced higher rates of spontaneous vaginal births, vaginal births after cesarean delivery and breastfeeding initiation, and lower rates of cesarean deliveries and instrumental births, with no increase in adverse neonatal outcomes. We observed an increased risk of oxytocin induction among high-risk birthers with a midwife versus an obstetrician as MRP.
Interpretation:
Our findings suggest that compared with other providers in BC, midwives provide safe primary care for clients with varied levels of medical risk. Future research might examine how different practice and remuneration models affect clinical outcomes, client and provider experiences, and costs to the health care system.
In British Columbia, registered midwives are autonomous, primary health care providers, regulated and integrated into the publicly funded health care system. Midwives typically work in small-team continuity-of-care models, providing medical care during pregnancy, birth and up to 3 months postpartum in the community and in hospitals. Midwives hold hospital privileges and consult with physician colleagues as medically indicated.
Since the regulation of midwifery in BC in 1998, the number of pregnant people who are attended by midwives during birth has steadily increased, from 4.8% in 2004/051 to 15.6% in 2019/20.2 In 2018/19, 1 in 4 childbearing people in BC (25.4%) had a midwife involved in their care at some point during their pregnancy, birth or postpartum period.2
Several studies have examined the safety of midwifery care in BC after regulation. Janssen and colleagues analyzed the outcomes of low-risk clients from 2000 to 2004, providing important evidence for the safety of midwife-attended planned home births in the early years after regulation.3 Other researchers have described good perinatal outcomes for subsets of midwifery clients in BC, including those residing in rural areas4 and those planning vaginal births after cesarean (VBAC) at home.5 However, these studies focused on subsamples of childbearing people or did not use recent data.
The benefits of midwife-led care for clients with more complex needs are beginning to emerge in BC. Using BC perinatal data, McRae and colleagues6,7 demonstrated that those affected by low socioeconomic position, substance use and mental illness had lower odds of small-for-gestational-age babies, pretermbirth and low-birth-weight babies when they were cared for by midwives antenatally rather than by physicians.
This analysis is part of a larger mixed-methods study that aimed to better understand the changing profile of midwifery clients in BC and the implications this has for education, research and practice. The goal of the current analysis is to present complete and recent data from all births in BC that had a midwife, family physician or obstetrician listed as the most responsible provider (MRP). Specifically, we sought to document neonatal and maternal outcomes of childbearing people who had a mid-wife as their MRP compared with those who had a physician as the MRP, with similar medical risk profiles.
Methods
Study population
We acknowledge that not all pregnant birthers are women or mothers. We use gendered language when referring to the BC Perinatal Data Registry (BCPDR)8 in order to accurately represent the source. The study population comprised births in BC from 2008 to 2018 and was drawn from abstracted medical chart data from the BCPDR, a quality-controlled registry containing data for 99% of all births, including home births.9 We linked 4 data sets using a unique identifier: core mother data set, maternal health care providers and services, maternal diagnostic codes and the newborn data set. After each linkage, we checked the sample size and stratified by fiscal year, to verify the accuracy of the linkage and to ensure data were complete for each fiscal year.
Risk stratification
The antenatal risk score we used in this study is a validated scoring tool used by the Alberta Perinatal Health Program.10,11 The 45-item antenatal risk assessment tool includes prepregnancy demographics and health conditions, past obstetric history and problems in the current pregnancy. Higher scores show a strong correlation with perinatal mortality and morbidity.11
We extracted the components of the risk score from the maternal diagnostic International Classification of Diseases, 10th Revision codes and variables in the BCPDR. Three prepregnancy items (symptomatic heart disease with no effect on daily living, blood pressure 140/90 or greater, antihypertensive drug use) and 1 past obstetric history item (Rh isoimmunization with an affected infant) could not be included in our version of the risk tool as they were not recorded in the databases available to us. However, we included a prepregnancy history of symptomatic heart disease with an effect on daily living in our analysis, as well as indicators of hypertensive disorders in the current pregnancy (i.e., gestational hypertension, proteinuria, eclampsia) and an obstetric history of isoimmunization (Appendix 1, Supplemental Table 1, available at www.cmaj.ca/lookup/doi/10.1503/cmaj.220453/tab-related-content).
As instructed by the Alberta Perinatal Health Program,10,11 we assigned a weighted value to each risk variable, and the total score was the sum of these weighted values. We recoded the score into the recommended risk categories:10 low risk (scores of 0–2), moderate risk (scores of 3–6) and high risk (scores of 7 or higher).11
Group assignment
The focus of our analysis was perinatal outcomes of childbearing people for whom the MRP was a midwife, compared with outcomes of those with a family physician or obstetrician as MRP. Within the BCPDR, the MRP is defined as the care provider who is responsible for the care and treatment of the client for the greatest portion of time during the stay in the health care facility, including home births. The MRP assumes responsibility for any treatment resulting from their written or verbal orders.12 Findings from a Canadian validation study indicate that the MRP type during hospital stay aligns with the prenatal provider type in most cases. For obstetricians, the percent agreement was 93%; for family physicians, the percent agreement was 98%; and for midwives, it was 94%.13
The MRP type is a mandatory field abstracted from medical charts by trained coding and informatics professionals after the client is discharged from hospital. The data are then sent to the Canadian Institute for Health Information. Data pertaining to community-based midwifery care, including the planned and actual place of birth (home, hospital or unknown), are abstracted from midwifery charts and included in the BCPDR. The Canadian Institute for Health Information employs a rigorous quality control process, including verification of individual data elements, cross-referencing of interrelated data elements and regular validation studies.14 The BCPDR employs similar quality checks.15
Primary and secondary outcomes
We included 4 primary neonatal outcomes and 1 primary birth outcome: perinatal death (any stillbirth or neonatal death, as determined by the Canadian Institute for Health Information Discharge Abstract Database); low birth weight of less than 2500 g; preterm birth at less than 37 weeks; Apgar of less than 7 at 5 minutes; and cesarean delivery (all types). Secondary outcomes included labour induction with oxytocin, VBAC, assisted vaginal delivery (vacuum, forceps or both), spontaneous vaginal birth (SVB), third- or fourth-degree perineal tears, and breast- or chest-feeding initiation within 1 hour of birth.
Confounders
We used most maternal prenatal confounding variables available in the BCPDR to create the prenatal risk score. We examined the remaining variables and selected those that either have a known association with adverse neonatal outcomes (i.e., prenatal substance use, rural residence, antenatal hospital admissions, history of mental health condition) or are routinely controlled for in perinatal research studies (i.e., parity).
Statistical analysis
We present descriptive statistics for each outcome across exposure groups, followed by adjusted absolute differences and relative risks and 95% confidence intervals (CIs). We obtained adjusted absolute and relative risks using logistic regression modelling, which represent marginal values obtained by averaging estimates over the adjusting variables.16 We report relative risks rather than odds ratios to avoid inflated effects for common outcomes such as SVB.17,18 For each outcome, we present 8 comparisons. We applied the Tukey–Kramer correction to p values and CIs to maintain the family-wise error rate within each outcome.
Ethics approval
The study was approved by the University of British Columbia Behavioural Research Ethics Board (# H20-00806).
Results
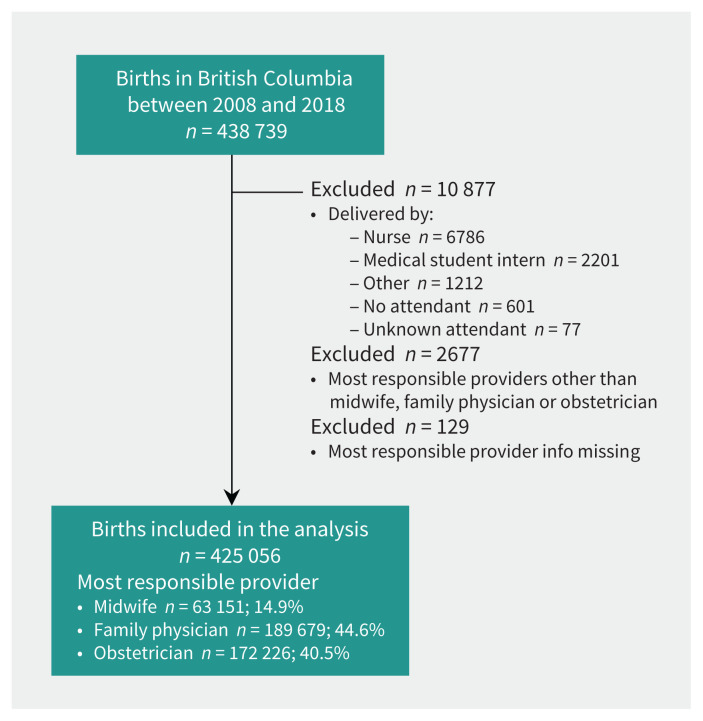
There were 438 739 linked mother–baby pairs during the study period. We excluded births that were not delivered by a midwife or physician and those with unknown or no attendants (Figure 1). Twins and multiples (n = 7098) were included and duplicate mother IDs removed from the analysis so that each mother was linked to only 1 baby.
Figure 1:
Flowchart showing selection of births used in the analysis.
Of the 425 056 births included in this study, 63 151 (14.9%) had a midwife as their MRP, 189 679 (44.6%) a family physician and 172 226 (40.5%) an obstetrician. Less than 1% (n = 2677) had other MRPs, such as general surgeons or maternal–fetal medicine specialists, and we excluded these clients from analysis. The antenatal risk score ranged from 0 to 23, with a median score of 2. The proportion of births that had a midwife listed as MRP increased from 9.2% to 19.8% over the study period. In 2018, midwives were listed as MRP for 24.3% of low-risk, 14.3% of moderate-risk and 7.9% of high-risk births in the province, representing an absolute increase of 9.1% (low risk), 7.7% (moderate risk) and 5.7% (high risk) between 2008 and 2018.
Of the 12 169 births that took place at home during the study period, 9776 (80.3%) had low medical risk, 2329 (19.1%) moderate risk, and 64 (0.5%) were in the high-risk category. As the risk score increased, so did the proportion of midwifery and family physician clients who were delivered by obstetricians (Table 1). More family physician than midwifery clients had babies delivered by obstetricians across all risk strata (Table 1). Characteristics of clients across MRP groups are presented in Table 2.
Table 1:
Proportion of clients who were delivered by obstetricians across most responsible provider* groups (n = 425 056)
| Risk category | No. (%) of midwife MRPs | No. (%) of family physician MRPs | No. (%) of obstetrician MRPs |
|---|---|---|---|
| All | 10 229/63 151 (16.2) | 40 567/189 679 (21.4) | 169 044/172 226 (98.2) |
| Low risk (0–2) | 6268/46 632 (13.4) | 23 125/132 309 (17.5) | 74 931/76 694 (97.7) |
| Moderate risk (3–6) | 3438/15 437 (22.3) | 14 449/51 519 (28.0) | 75 934/77 142 (98.4) |
| High risk (≥ 7) | 523/1082 (48.3) | 2993/5851 (51.2) | 18 179/18 390 (98.9) |
Note: MRP = most responsible provider.
MRP definition: a provider who is responsible for the care and treatment of the client for the greatest portion of the clieint’s length of stay in the health care facility. The MRP assumes responsibility for any treatment provided resulting from their written or verbal orders. They may not be physically present in the health care facility. 2022 DAD Abstracting Manual: https://secure.cihi.ca/estore/productSeries.htm?pc=PCC78.
Table 2:
Characteristics of clients across most responsible provider groups (n = 425 056)
| Characteristic | No. (%) of midwife MRPs n = 63 151 |
No. (%) of family physician MRPs n = 189 679 |
No. (%) of obstetrician MRPs n = 172 226 |
|---|---|---|---|
| Nulliparous | 29 156 (46.3) | 90 705 (48.1) | 78 781 (46.0) |
| Maternal residence* | |||
| Northern Health Authority | 2022 (3.2) | 21 803 (11.5) | 8583 (5.0) |
| Interior Health | 8103 (12.8) | 32 931 (17.4) | 18 846 (10.9) |
| Island Health | 17 395 (27.5) | 32 159 (17.0) | 12 035 (7.0) |
| Fraser Health | 19 380 (30.7) | 69 943 (36.9) | 76 987 (44.7) |
| Vancouver Coastal Health | 16 016 (25.4) | 31 061 (16.4) | 54 410 (31.6) |
| Unknown health authority, or out-of-country or out-of-province residence | 235 (0.4) | 1782 (0.9) | 1365 (0.8) |
| History of mental health condition† | 17 564 (27.8) | 34 722 (18.3) | 25 280 (14.7) |
| Substance use during pregnancy‡ | 1600 (2.5) | 10 284 (5.4) | 5083 (3.0) |
| Antenatal hospital admissions (1 or more)§ | 2474 (3.9) | 15 594 (8.2) | 17 073 (9.9) |
| Prenatal medical risk category | |||
| Low risk (0–2) | 46 632 (73.8) | 132 309 (69.8) | 76 694 (44.5) |
| Moderate risk (3–6) | 15 437 (24.4) | 51 519 (27.2) | 77 142 (44.8) |
| High risk (≥ 7) | 1082 (1.7) | 5851 (3.1) | 18 390 (10.7) |
Note: MRP = most responsible provider.
The Health Authority of usual residence, as determined by resident postal code.
Any history of mental illness (depression, previous postpartum depression, anxiety, bipolar disorder, other, or unknown type) before or during the current pregnancy.
Mother used any of the following substances at any time during the current pregnancy: heroin or opioids, cocaine, methadone, solvents or marijuana; or care provider lists use of prescription, “other,” or unknown other drug as a risk to the pregnancy.
Total previous inpatient hospital admissions, to any facility, for any reason, during the current pregnancy (excluding current delivery admission).
Primary outcomes
The risk of perinatal death for midwifery clients across risk strata was similar to the risk of those under the care of family physicians (Table 3). Compared with obstetrician-led care, low- and moderate-risk clients with midwife-led care were significantly less likely to experience a perinatal death (Table 3), but the adjusted absolute risk differences were very small (Appendix 2, Supplemental Table 2, available at www.cmaj.ca/lookup/doi/10.1503/cmaj.220453/tab-related-content). In the high-risk group, there was no significant difference in the rate of perinatal death between midwife-led and physician-led care (Table 3).
Table 3:
Primary outcomes — descriptive statistics and adjusted relative risks comparing midwives with family physicians and obstetricians (95% confidence intervals)
| Risk score | No. (%) of midwife MRPs | No. (%) of family physician MRPs | No. (%) of obstetrician MRPs | Midwife compared with family physician | Midwife compared with obstetrician | ||
|---|---|---|---|---|---|---|---|
| Numerator/denominator | N | RR (95% CI)* | N | RR (95% CI)* | |||
| Perinatal death | |||||||
| Low risk | 115/46 632 (0.2) | 321/132 309 (0.2) | 403/76 694 (0.5) | 178 941 | 1.046 (0.811–1.350) | 123 326 | 0.482 (0.376–0.618) |
| Moderate risk | 72/15 437 (0.5) | 319/51 519 (0.6) | 531/77 142 (0.7) | 66 956 | 0.789 (0.581–1.071) | 92 579 | 0.675 (0.503–0.906) |
| High risk | 19/1082 (1.8) | 127/5851 (2.2) | 352/18 390 (1.9) | 6933 | 0.863 (0.488–1.525) | 19 472 | 0.941 (0.545–1.624) |
| All | 206/63 151 (0.3) | 767/189 679 (0.4) | 1286/172 226 (0.7) | 252 830 | 0.833 (0.693–1.002) | 235 377 | 0.437 (0.366–0.521) |
| Low birth weight (< 2500 g) | |||||||
| Low risk | 448/46 438 (1.0) | 1967/131 562 (1.5) | 2096/76 299 (2.7) | 178 000 | 0.694 (0.614–0.784) | 122 737 | 0.392 (0.347–0.443) |
| Moderate risk | 498/15 334 (3.2) | 2899/50 866 (5.7) | 5594/76 534 (7.3) | 66 200 | 0.617 (0.552–0.690) | 91 868 | 0.460 (0.414–0.513) |
| High risk | 178/1066 (16.7) | 1348/5693 (23.7) | 5296/18 098 (29.3) | 6759 | 0.755 (0.640–0.890) | 19 164 | 0.609 (0.520–0.713) |
| All | 1124/62 838 (1.8) | 6214/188 121 (3.3) | 12 986/170 931 (7.6) | 250 959 | 0.574 (0.532–0.619) | 233 769 | 0.244 (0.227–0.262) |
| Preterm birth (< 37 wk) | |||||||
| Low risk | 1476/46 005 (3.2) | 5298/130 363 (4.1) | 4297/75 587 (5.7) | 176 368 | 0.823 (0.769–0.881) | 121 592 | 0.593 (0.553–0.636) |
| Moderate risk | 1136/15 168 (7.5) | 5469/50 193 (10.9) | 9435/75 450 (12.5) | 65 361 | 0.720 (0.669–0.774) | 90 618 | 0.607 (0.566–0.651) |
| High risk | 260/1049 (24.8) | 1818/5566 (32.7) | 6889/17 548 (39.3) | 6615 | 0.794 (0.698–0.904) | 18 597 | 0.649 (0.573–0.735) |
| All | 2872/62 222 (4.6) | 12 585/186 122 (6.8) | 20 621/168 585 (12.2) | 248 344 | 0.708 (0.676–0.743) | 230 807 | 0.387 (0.370–0.405) |
| Apgar < 7 at 5 min | |||||||
| Low risk | 756/45 966 (1.6) | 2737/130 326 (2.1) | 1696/75 604 (2.2) | 176 292 | 0.778 (0.707–0.856) | 121 570 | 0.734 (0.663–0.812) |
| Moderate risk | 303/15 157 (2.0) | 1381/50 167 (2.8) | 1868/75 481 (2.5) | 65 324 | 0.735 (0.635–0.851) | 90 638 | 0.763 (0.661–0.881) |
| High risk | 48/1048 (4.6) | 325/5557 (5.8) | 937/17 548 (5.3) | 6605 | 0.781 (0.547–1.115) | 18 596 | 0.791 (0.562–1.113) |
| All | 1107/62 171 (1.8) | 4443/186 050 (2.4) | 4501/168 633 (2.7) | 248 221 | 0.741 (0.686–0.802) | 230 804 | 0.633 (0.586–0.685) |
| Cesarean delivery | |||||||
| Low risk | 3356/46 632 (7.2) | 16 171/132 309 (12.2) | 32 476/76 694 (42.3) | 178 941 | 0.579 (0.555–0.605) | 123 326 | 0.167 (0.160–0.174) |
| Moderate risk | 2396/15 437 (15.5) | 13 328/51 519 (25.9) | 52 907/77 142 (68.6) | 66 956 | 0.593 (0.566–0.622) | 92 579 | 0.228 (0.218–0.239) |
| High risk | 411/1082 (38.0) | 2848/5851 (48.7) | 14 783/18 390 (80.4) | 6933 | 0.779 (0.709–0.855) | 19 472 | 0.492 (0.450–0.538) |
| All | 6163/63 151 (9.8) | 32 347/189 679 (17.1) | 100 166/172 226 (58.2) | 252 830 | 0.564 (0.547–0.582) | 235 377 | 0.169 (0.164–0.175) |
Note: CI = confidence interval, MRP = most responsible provider, RR = relative risk.
Adjusted for parity, maternal residence, history of mental health condition, substance use during pregnancy and antenatal hospital admissions (see Table 2 for definitions). RR > 1.0 denotes a higher risk in midwives; RR < 1.0 denotes a lower risk in midwives.
Clients who had a midwife as the MRP were significantly less likely to experience preterm birth and have a low-birth-weight baby across all risk strata, compared with those with a physician as the MRP. The adjusted relative risk of an Apgar score of less than 7 at 5 minutes was significantly lower for clients of midwives than for clients with physicians as MRP, for 7 of the 8 comparisons (Table 3). The cesarean delivery rate among midwifery clients in the low-risk group was 7.2% compared with 12.2% for family physician clients and 42.3% for obstetrician clients. Cesarean delivery rates increased for midwifery clients as medical risk increased, and were significantly lower than physician rates across all risk strata (Table 3). Low-risk clients had an absolute risk reduction of 34.4% for cesarean delivery when their MRP was a midwife compared with an obstetrician. The absolute risk difference increased to 55.3% for clients with moderate prenatal risk and 42.2% for high-risk clients (Appendix 2, Supplemental Table 2).
Secondary outcomes
The analysis of secondary outcomes demonstrated that low-risk midwifery clients were significantly less likely to experience labour induction with oxytocin; however, high-risk midwifery clients were more than twice as likely to be induced with oxytocin than obstetrician clients (adjusted absolute difference 11.3%). Midwifery clients were significantly less likely to have an assisted vaginal birth across most risk levels than physician clients (Table 4) and they were significantly more likely to have an SVB across all risk strata. For example, low-risk clients who had a midwife as MRP were nearly twice as likely to have an SVB (adjusted absolute difference 42.7%) than obstetrician clients, and clients of moderate risk were nearly 4 times as likely to have an SVB (adjusted absolute difference 58.3%). Rates of VBAC among eligible individuals were significantly higher if a midwife was the MRP compared with a physician in 7 of 8 comparisons reported in Table 4. The relative and absolute differences were small when comparing midwifery with family physician clients, but larger when comparing midwives as MRP to obstetricians. For example, among childbearing people with low risk, the VBAC rate was 85.3% among midwifery clients, compared with 78.6% among family physician clients and 51.5% among obstetrician clients. The prevalence of adverse maternal outcomes (blood transfusion, intensive care unit admissions, uterine rupture and postpartum wound infection) were very low for midwifery clients across risk strata (Appendix 3, Supplemental Table 3, available at www.cmaj.ca/lookup/doi/10.1503/cmaj.220453/tab-related-content). Breast- or chest-feeding at birth was significantly more common among midwifery clients across all risk strata (Table 4). There were few significant differences in perineal tears across MRP groups.
Table 4:
Secondary outcomes — descriptive statistics and adjusted relative risks comparing midwives with family physicians and obstetricians (95% confidence intervals)
| Risk score | No. (%) of midwife MRPs | No. (%) of family physician MRPs | No. (%) of obstetrician MRPs | Midwife compared with family physician | Midwife compared with obstetrician | ||
|---|---|---|---|---|---|---|---|
| Numerator/denominator | N | RR (95% CI)* | N | RR (95% CI)* | |||
| Labour induction with oxytocin | |||||||
| Low risk | 2986/46 632 (6.4) | 13 859/132 309 (10.5) | 10 758/76 694 (14.0) | 178 941 | 0.609 (0.582–0.638) | 123 326 | 0.474 (0.452–0.497) |
| Moderate risk | 1898/15 437 (12.3) | 8559/51 519 (16.6) | 9411/77 142 (12.2) | 66 956 | 0.741 (0.701–0.783) | 92 579 | 0.994 (0.941–1.051) |
| High risk | 198/1082 (18.3) | 1089/5851 (18.6) | 1541/18 390 (8.4) | 6933 | 0.972 (0.827–1.142) | 19 472 | 2.202 (1.878–2.581) |
| All | 5082/63 151 (8.0) | 23 507/189 679 (12.4) | 21 710/172 226 (12.6) | 252 830 | 0.644 (0.622–0.667) | 235 377 | 0.622 (0.600–0.644) |
| Assisted vaginal delivery (vacuum, forceps or both) | |||||||
| Low risk | 2600/46 632 (5.6) | 15 985/132 309 (12.1) | 11 316/76 694 (14.8) | 178 941 | 0.463 (0.440–0.486) | 123 326 | 0.408 (0.388–0.430) |
| Moderate risk | 788/15 437 (5.1) | 5106/51 519 (9.9) | 5482/77 142 (7.1) | 66 956 | 0.520 (0.476–0.568) | 92 579 | 0.732 (0.670–0.800) |
| High risk | 51/1082 (4.7) | 393/5851 (6.7) | 884/18 390 (4.8) | 6933 | 0.676 (0.476–0.959) | 19 472 | 1.031 (0.734–1.448) |
| All | 3439/63 151 (5.4) | 21 484/189 679 (11.3) | 17 682/172 226 (10.3) | 252 830 | 0.477 (0.457–0.498) | 235 377 | 0.524 (0.501–0.547) |
| Spontaneous vaginal birth | |||||||
| Low risk | 40 676/46 632 (87.2) | 100 153/132 309 (75.7) | 32 902/76 694 (42.9) | 178 941 | 1.135 (1.129–1.141) | 123 326 | 1.919 (1.892–1.945) |
| Moderate risk | 12 253/15 437 (79.4) | 33 085/51 519 (64.2) | 18 753/77 142 (24.3) | 66 956 | 1.265 (1.248–1.282) | 92 579 | 3.846 (3.758–3.936) |
| High risk | 620/1082 (57.3) | 2610/5851 (44.6) | 2723/18 390 (14.8) | 6933 | 1.366 (1.259–1.481) | 19 472 | 4.529 (4.163–4.927) |
| All | 53 549/63 151 (84.8) | 135 848/189 679 (71.6) | 54 378/172 226 (31.6) | 252 830 | 1.189 (1.182–1.196) | 235 377 | 2.882 (2.838–2.926) |
| VBAC† | |||||||
| Low risk | 864/1013 (85.3) | 1183/1506 (78.6) | 669/1299 (51.5) | 2519 | 1.101 (1.049–1.155) | 2312 | 1.716 (1.575–1.869) |
| Moderate risk | 1943/2353 (82.6) | 3659/4659 (78.5) | 2447/4545 (53.8) | 7012 | 1.063 (1.030–1.096) | 6898 | 1.584 (1.499–1.674) |
| High risk | 167/213 (78.4) | 525/685 (76.6) | 524/901 (58.2) | 898 | 1.027 (0.928–1.137) | 1114 | 1.388 (1.238–1.557) |
| All | 2974/3579 (83.1) | 5367/6850 (78.4) | 3640/6745 (54.0) | 10 429 | 1.072 (1.045–1.099) | 10 324 | 1.590 (1.513–1.671) |
| Third- or fourth-degree perineal tears‡ | |||||||
| Low risk | 1674/28 554 (5.9) | 4708/77 367 (6.1) | 2941/31 814 (9.2) | 105 921 | 0.964 (0.901–1.031) | 60 368 | 0.650 (0.605–0.699) |
| Moderate risk | 545/8551 (6.4) | 1470/24 877 (5.9) | 1263/16 755 (7.5) | 33 428 | 1.107 (0.984–1.245) | 25 306 | 0.910 (0.807–1.026) |
| High risk | 22/407 (5.4) | 85/1705 (5.0) | 153/2219 (6.9) | 2112 | 1.136 (0.651–1.982) | 2626 | 0.936 (0.550–1.593) |
| All | 2241/37 512 (6.0) | 6263/103 949 (6.0) | 4357/50 788 (8.6) | 141 461 | 0.993 (0.937–1.053) | 88 300 | 0.703 (0.661–0.747) |
| Breast- or chest-feeding initiation at birth | |||||||
| Low risk | 30 137/46 545 (64.7) | 75 160/131 746 (57.0) | 34 509/76 461 (45.1) | 178 291 | 1.134 (1.122–1.146) | 123 006 | 1.429 (1.409–1.448) |
| Moderate risk | 9822/15 350 (64.0) | 26 003/50 989 (51.0) | 30 397/76 744 (39.6) | 66 339 | 1.267 (1.243–1.291) | 92 094 | 1.664 (1.632–1.697) |
| High risk | 567/1057 (53.6) | 2117/5704 (37.1) | 4969/18 207 (27.3) | 6761 | 1.464 (1.345–1.594) | 19 264 | 2.000 (1.848–2.165) |
| All | 40 526/62 952 (64.4) | 103 280/188 439 (54.8) | 69 875/171 412 (40.8) | 251 391 | 1.180 (1.169–1.191) | 234 364 | 1.618 (1.599–1.637) |
Note: CI = confidence interval, MRP = most responsible provider, RR = relative risk, VBAC = vaginal birth after cesarean.
Adjusted for parity, maternal residence, history of mental health condition, substance use during pregnancy, and antenatal hospital admissions (see Table 2).
Denominator includes people with a previous cesarean scar who were identified as eligible for VBAC or eligibility is unknown or not documented, and current delivery was singleton, vertex presentation. Denominator excludes people with a delivery episode and a history of cesarean who were not eligible for VBAC per the chart or people with a previous scar and unknown or not documented VBAC eligibility who did not have a singleton vertex pregnancy.
Analysis is restricted to those with a vaginal birth.
Interpretation
We found that midwives and family physicians in BC were the MRPs for similar proportions of low-, moderate- and high-risk pregnant people, countering the common impression that mid-wives care for predominantly low-risk clients. As medical risk increases, both midwives and family physicians collaborate increasingly and appropriately with obstetrician specialists. The study provides evidence for the safety and efficacy of midwifeled care across medical risk strata in BC. These findings align with evidence from meta-analyses of midwife-led continuity models and the global literature on the medical benefits of midwifery care.19,20
We used different strategies to enhance the internal validity and interpretation of the study’s findings. We stratified prenatal medical risk to reduce bias caused by the unequal distribution of medical risk factors across MRP groups; we adjusted each model for parity, maternal residence and other factors outlined in Table 2 that have the potential to bias the association between MRP and perinatal outcomes; we reported relative risks rather than odds ratios to avoid an inflation of effects for more prevalent outcomes like cesarean delivery or SVB; and we reported adjusted absolute risk differences in addition to relative risks, to help interpret the clinical importance of findings.
Although the proportion of clients with a midwife as their MRP in BC increased more than twofold from 2008/09 to 2017/18, Canada has among the lowest rates of midwifery coverage in the world21 and rates of cesarean delivery continue to climb. In 2019/20, the cesarean delivery rate in BC was 36.6%, the highest in Canada.2 Our findings suggest that more continuity-based midwife-led care in BC may have contributed to keeping operative delivery rates low without compromising safety. Provincial midwifery workforce surveys have identified numerous barriers to the expansion of midwifery in BC, including dissatisfaction with pay and working conditions, scope restrictions and lack of support when caring for clients with complex social and medical needs.22,23 Midwifery expansion must therefore be accompanied by policies and payment structures that support retention, integration and interprofessional collaboration between midwives and their physician colleagues — what the International Confederation of Midwives considers an “enabling environment for midwives.”24
Future research might examine how different practice and remuneration models affect clinical outcomes, client and provider experiences, and costs to the health care system.
Limitations
It is possible that the severity of risk is not adequately captured by the prenatal risk scoring system, which could lead to more clients in the obstetrician MRP group having more complex medical conditions not captured by this tool, explaining differences in outcomes. The MRP was determined by the provider who was responsible for the greatest proportion of care and treatment at the time of delivery, and not throughout the pregnancy. However, a Canadian validation study found that the MRP at the time of delivery was the prenatal provider in more than 90% of cases. Another unmeasured factor is the choice of childbearing people. Individuals who want a medicalized birth (including a cesarean delivery on request) are more likely to seek care from obstetricians, while those with physiologic birth intentions typically seek out midwifery care.21,25 This self-selection bias is a major limitation in any study of this nature. Other unmeasured factors include additional biological, genetic, epigenetic and environ-mental risk factors that are associated with adverse perinatal outcomes. Finally, the prenatal risk scoring tool was not validated with childbearing people in BC and included 4 fewer components than the Alberta Perinatal Health Program scoring tool.
Conclusion
With this study we report midwifery outcomes at the population level in BC, without restricting analysis to childbearing people with low or moderate risk or disaggregating midwifery outcomes by place of birth. As such, the study provides population-level evidence that midwives provide safe primary care for clients with varied levels of medical risk. If scaled up, the expansion of midwifery in BC holds potential for meeting national mandates to lower obstetric intervention rates26 and to increase access to midwifery care to under-served communities.27
Supplementary Material
Acknowledgement
The authors thank Arianne Albert PhD from Women’s Health Research Institute at BC Women’s Hospital, for her guidance during the statistical analysis of findings.
See related article at www.cmaj.ca/lookup/doi/10.1503/cmaj.230113
Footnotes
Competing interests: Kathrin Stoll reports membership of the Midwives Association Contract Negotiation Advisory Council (since Feb. 2020; unpaid role). In December 2019, MABC contributed $2000 toward the Sustainable Midwifery Practice Taskforce, led by Dr. Stoll in 2019 and 2020. The funds were used to pay honoraria for 6 taskforce members and contributed to the salary of a project assistant. No other competing interests were declared.
This article has been peer reviewed.
Contributors: Kathrin Stoll, Reena Titoria and Luba Butska contributed to the conception and design of the work. Kathrin Stoll and Reena Titoria contributed to the acquisition and analysis of data. All of the authors interpreted the data. Kathrin Stoll drafted the manuscript. All of the authors revised the manuscript critically for important intellectual content, led by Michelle Turner. All of the authors gave final approval of the version to be published and agreed to be accountable for all aspects of the work.
Funding: The authors are grateful for the financial support from the University of British Columbia Stollery Fund and the University of British Columbia Work Learn Program, which provided a salary subsidy for this project. The funders had no role in the project.
Data sharing: Data used for this study can be requested through Perinatal Services BC at http://www.perinatalservicesbc.ca/our-services/data-surveillance/perinatal-data-registry/data-requests#Research. The first author can be contacted with a request to share the data access application that contains the data fields used for the current analysis.
Disclaimer: All inferences, opinions and conclusions drawn in this publication are those of the authors, and do not reflect the opinions or policies of Perinatal Services BC.
References
- 1.Surveillance perinatal indicators: annual report — British Columbia residents delivering in BC. Vancouver: Perinatal Services BC; 2015. Available: www.perinatalservicesbc.ca/Documents/Data-Surveillance/Indicators/Annual/AnnualIndicatorsResidence_2013_14_BC.pdf (accessed 2021 July 20). [Google Scholar]
- 2.Perinatal health report: British Columbia 2019/20. Vancouver: Perinatal Services BC; 2021. Available: www.perinatalservicesbc.ca/Documents/Data-Surveillance/Reports/PHR/Perinatal%20Health%20Report%20BC%20201920.pdf (accessed 2022 Jan. 15). [Google Scholar]
- 3.Janssen PA, Saxell L, Page LA, et al. Outcomes of planned home birth with registered midwife versus planned hospital birth with midwife or physician. CMAJ 2009;181:377–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stoll K, Kornelsen J. Midwifery care in rural and remote British Columbia: a retrospective cohort study of perinatal outcomes of rural parturient women with a midwife involved in their care, 2003 to 2008. J Midwifery Womens Health 2014;59:60–6. [DOI] [PubMed] [Google Scholar]
- 5.Bayrampour H, Lisonkova S, Tamana S, et al. Perinatal outcomes of planned home birth after cesarean and planned hospital vaginal birth after cesarean at term gestation in British Columbia, Canada: a retrospective population-based cohort study. Birth 2021;48:301–8. [DOI] [PubMed] [Google Scholar]
- 6.McRae DN, Janssen PA, Vedam S, et al. Reduced prevalence of small-for-gestational-age and preterm birth for women of low socioeconomic position: a population-based cohort study comparing antenatal midwifery and physician models of care. BMJ Open 2018;8:e022220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McRae DN, Muhajarine N, Janssen PA. Improving birth outcomes for women who are substance using or have mental illness: a Canadian cohort study comparing antenatal midwifery and physician models of care for women of low socioeconomic position. BMC Pregnancy Childbirth 2019;19:279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Perinatal Data Registry. Vancouver: Perinatal Services BC; 2022. Available: www.perinatalservicesbc.ca/our-services/data-surveillance/perinatal-data-registry (accessed 2022 Sept. 1). [Google Scholar]
- 9.Frosst G, Hutcheon J, Joseph KS, et al. Validating the British Columbia Perinatal Data Registry: a chart re-abstraction study. BMC Pregnancy Childbirth 2015;15:123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Delivery record: Part one. Edmonton: Alberta Health Services; 2013. Available: https://www.yumpu.com/en/document/read/12005860/delivery-record-part-one-alberta-perinatal-health-program (accessed 2021 July 5). [Google Scholar]
- 11.Burstyn I. Antepartum risk score predicts adverse birth outcomes. J Obstet Gynaecol Can 2010;32:16–20. [DOI] [PubMed] [Google Scholar]
- 12.DAD Abstracting Manual (for use with ICD-10-CA/CCI), 2022–2023. Ottawa: Canadian Institute for Health Information; 2022. Available: https://secure.cihi.ca/estore/productSeries.htm?pc=PCC78 (accessed 2022 Oct. 1). [Google Scholar]
- 13.Thiessen K, Nickel N, Prior HJ, et al. Understanding the allocation of caesarean outcome to provider type: a chart review. Healthc Policy 2018;14:22–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Data quality documentation, Discharge Abstract Database: multi-year information. Ottawa: Canadian Institute for Health Information; 2012. Available: https://www.cihi.ca/sites/default/files/dad_multi-year_en_0.pdf (accessed 2022 Oct. 1). [Google Scholar]
- 15.BCPDR Data Quality: reference guide for coders — 2017. Vancouver: Perinatal Services BC. Available: http://www.perinatalservicesbc.ca/Documents/Data-Surveillance/PDR/Resources-Coders/DQGuide.pdf (accessed 2022 Oct. 1). [Google Scholar]
- 16.Lenth R. emmeans: estimated marginal means, aka least-squares means. Version 1.8.2: CRAN, R; 2022. Available: https://CRAN.R-project.org/package=emmeans (accessed 2022 Oct. 1).
- 17.McNutt L-A, Wu C, Xue X, et al. Estimating the relative risk in cohort studies and clinical trials of common outcomes. Am J Epidemiol 2003;157:940–3. [DOI] [PubMed] [Google Scholar]
- 18.Robbins AS, Chao SY, Fonseca VP. What’s the relative risk? A method to directly estimate risk ratios in cohort studies of common outcomes. Ann Epidemiol 2002;12:452–4. [DOI] [PubMed] [Google Scholar]
- 19.Sandall J, Soltani H, Gates S, et al. Midwife-led continuity models versus other models of care for childbearing women. Cochrane Database Syst Rev 2015;(9): CD004667. [DOI] [PubMed] [Google Scholar]
- 20.Renfrew MJ, McFadden A, Bastos MH, et al. Midwifery and quality care: findings from a new evidence-informed framework for maternal and newborn care. Lancet 2014;384:1129–45. [DOI] [PubMed] [Google Scholar]
- 21.Stoll KH, Downe S, Edmonds J, et al. ICAPP Study Team. A survey of university students’ preferences for midwifery care and community birth options in 8 high-income countries. J Midwifery Womens Health 2020;65:131–41. [DOI] [PubMed] [Google Scholar]
- 22.Stoll K, Gallagher J. A survey of burnout and intentions to leave the profession among Western Canadian midwives. Women Birth 2019;32:e441–9. [DOI] [PubMed] [Google Scholar]
- 23.Butska L, Stoll K. When midwives burn out: differences in the experiences of midwives in British Columbia and Alberta. Canadian Journal of Midwifery Research & Practice 2020;19:20–30. [Google Scholar]
- 24.ICM Enabling Environment Policy Brief (2021). The Hague (Netherlands): International Confederation of Midwives. The Hague: ICM. Available: https://internationalmidwives.org/our-work/other-resources/icm-enabling-environment-policy-brief-(2021).html (accessed 2022 Feb. 22). [Google Scholar]
- 25.Stoll KH, Hauck YL, Downe S, et al. International Childbirth Attitudes — Prior to Pregnancy (ICAPP) Study Team. Preference for cesarean section in young nulligravid women in eight OECD countries and implications for reproductive health education. Reprod Health 2017;14:116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Halpern S. SOGC joint policy statement on normal childbirth. J Obstet Gynaecol Can 2009;31:602. [DOI] [PubMed] [Google Scholar]
- 27.Society of Obstetricians and Gynaecologists of Canada. SOGC policy statement. No. 251, December 2010. Returning birth to aboriginal, rural, and remote communities. J Obstet Gynaecol Can 2010;32:1186–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.