Summary
Background
Malnutrition and obesity are interdependent pathologies along the same spectrum. We examined global trends and projections of disability-adjusted life years (DALYs) and deaths from malnutrition and obesity until 2030.
Methods
Using data from the 2019 Global Burden of Disease study involving 204 countries and territories, trends in DALYs and deaths were described for obesity and malnutrition from 2000 to 2019, stratified by geographical regions (as defined by WHO) and Socio-Demographic Index (SDI). Malnutrition was defined according to the 10th revision of International Classification of Diseases codes for nutritional deficiencies, stratified by malnutrition type. Obesity was measured via body mass index (BMI) using metrics related to national and subnational estimates, defined as BMI ≥25 kg/m2. Countries were stratified into low, low-middle, middle, high-middle, and high SDI bands. Regression models were constructed to predict DALYs and mortality up to 2030. Association between age-standardised prevalence of the diseases and mortality was also assessed.
Findings
In 2019, age-standardised malnutrition-related DALYs was 680 (95% UI: 507–895) per 100,000 population. DALY rates decreased from 2000 to 2019 (−2.86% annually), projected to fall 8.4% from 2020 to 2030. Africa and low SDI countries observed highest malnutrition-related DALYs. Age-standardised obesity-related DALY estimates were 1933 (95% UI: 1277–2640). Obesity-related DALYs rose 0.48% annually from 2000 to 2019, predicted to increase by 39.8% from 2020 to 2030. Highest obesity-related DALYs were in Eastern Mediterranean and middle SDI countries.
Interpretation
The ever-increasing obesity burden, on the backdrop of curbing the malnutrition burden, is predicted to rise further.
Funding
None.
Keywords: Global burden, Obesity, Malnutrition, Mortality, Disability-adjusted life years
Research in context.
Evidence before this study
Increasing importance has been placed on viewing undernutrition and overnutrition not as two distinct conditions addressed in silos, but as interconnected issues sharing common pathophysiological processes that together contribute to the double burden of malnutrition. We searched the databases MEDLINE and Embase with the search terms “global burden”, “GBD”, “malnutrition”, and “obesity”, for articles published in English from database inception to 7th August, 2022; the search returned 2971 articles. While the changing burdens of malnutrition and obesity have been studied in target vulnerable groups, such as in children or in low and middle-income countries, the comprehensive analysis on to the global trends and predictions of the double burden of disease is lacking.
Added value of this study
This study utilises the Global Burden of Disease (GBD) 2019 data to estimate the distribution of the double burden of malnutrition and obesity. Progress in reducing disease burden stemming from undernutrition has been shown to have been more-than-offset by rapidly rising obesity-related disease burden, evidenced especially by the regions registering the greatest reductions in malnutrition-related outcomes also demonstrating the greatest exacerbations in obesity-related disease burden. The disparities in disease burden reveal the entrenched sex-regional-socioeconomic precursors, with obesity-related death rates rising with the level of social development, but only up to a point—high SDI countries demonstrated the lowest obesity-related deaths. Our projections suggest that the chiasm between malnutrition and obesity will widen further in the coming decade, driven primarily by rising obesity.
Implications of all the available evidence
Bringing together and examining the chiasm between malnutrition and obesity, stratified by sex, location and social development, allows for important, contextualised insights to be drawn for future decision-making on addressing the double burden of malnutrition as one entity. Our analysis provides evidence suggesting worsening disease burden related to obesity, especially pertinent in low and low-middle SDI countries that are in the midst of rapid nutrition transitions. Through this, we highlight the importance of population-specific interventions and policies, weighing measures addressing malnutrition against the obesity epidemic. Measures addressing malnutrition must be dynamic and have consideration for long-term unintended consequences, working to address common pathways involved in the progression of obesity as well, through empowering access to quality food and instilling healthy eating habits.
Introduction
The double burden of malnutrition and obesity, is one of the top priorities that the UN Decade of Action on Nutrition is trying to eradicate.1 This burden of disease manifests as either undernutrition or overnutrition, which has traditionally been viewed as two distinct conditions addressed in silos, whereas in fact they share similar pathophysiological processes at different ends of the spectrum.2 Previously, health and development policies have focused their attention on undernutrition and this has helped eradicate the life-threatening sequelae of acute malnutrition as well as curb the trajectory of chronic malnutrition. However, these policies have resulted in some countries undergoing a rapid nutritional transition, which has led to unhealthy diets and obesity.2,3 Hence, newer policies have pivoted to simultaneously tackle the burden of malnutrition and obesity with a more holistic approach.4
Previous studies have focused on the severe burden of disease particularly in vulnerable population groups such as in children and maternal malnutrition,5 as well as in low and middle-income countries.2,3 The disparate distribution of the global burden of malnutrition and obesity remains unclear given the paucity of data from other population groups such as those of higher-income countries. The Global Burden of Disease, Injuries, and Risk Factors Study (GBD) lends insights into the global trends through systematic estimates of the risk factors and causes of death in 204 different countries and territories, allowing important stratification based on sex, geographical, and socio-demographic index (SDI).6 The present study provides unique perspectives on the global estimates of the burden of disease, by examining the trends and projections of disability-adjusted life years (DALYs) and deaths from malnutrition and obesity until 2030, across sex, geographical regions and socioeconomic status. With the current obesogenic climate, there is a growing need to forecast these estimates that can help inform policy-making stakeholders in structuring and implementing effective health services to meet the future demand. This is in line with the Lancet Commission that recommends the understanding in the shift of paradigms and practices regarding obesity and nutrition, with the unified goal in advancing governmental action and accountability that will promote planetary health.7
Methods
Overview and definition
To the trends in deaths and DALYs of obesity and malnutrition from 2000 to 2019, estimates were retrieved from the GBD 2019 study coordinated by the Institute for Health Metrics and Evaluation, an independent global health research centre at the University of Washington.8 The GBD 2019 study is a multinational collaborative study consisting of 204 countries and territories, that provides annual data allowing for accurate comparisons across the years.9 The present study included the full set of data estimates derived from the GBD 2019 study, thus allowing for the study findings to be representative of the respective wider populations.10 The study reports death estimates from vital registration systems, verbal autopsies, as well as alternative surveillance systems,11 data from which can be generated from the Global Health Data Exchange website.8 For the purposes of this study, estimates of DALYs and deaths for obesity and malnutrition were retrieved. As the GBD database offers the ecological analysis of country-level estimates, it does not provide estimates of DALYs and death for individuals suffering from both obesity and malnutrition, thus the synergistic effects of the double burden of disease cannot be examined. The original GBD 2019 study utilised DisMod-MR 2.1, a Bayesian meta-regression method designed to address the limitations of descriptive epidemiological data, such as inconsistency, missing data, as well as any large variation in methodology between data sources. Natural history models, back calculation from mortality rates, or other methods were also applied for certain conditions as described in previous studies.12 The methods to generate the GBD estimates were previously described13 and can be found in Supplementary Material S1.
Death and DALYs estimation in the GBD 2019 study
Death and DALYs estimates were retrieved similar to the methods described by previous GBD studies.12 Estimates for age-standardised prevalence, death, and DALY were presented with their 95% uncertainty intervals (UIs).
Prevalence, socio-demographic index and world health organisation regions
The GBD study considers SDI on a scale from 0 to 1, representing a composite of average incomes per capita, education level, and fertility rates.14 This score was then used to stratify countries into low, low-middle, middle, high-middle and high SDI bands. Differences in prevalence, deaths, and DALYs based on socioeconomic development of countries was then evaluated using this data. The prevalence of obesity could not be obtained as it was classified as a risk factor instead of a cause of death or injury in the GBD study. Results were also stratified based on geographical locations as defined by WHO15—Africa, the Eastern Mediterranean, Europe, the Region of Americas, South-East Asia and the Western Pacific. Association between age-standardised prevalence of the diseases and mortality was also assessed.
Statistical analysis
The study included all cases of malnutrition and obesity within the GBD 2019 study. Malnutrition was defined based on the 10th revision International Classification of Diseases (ICD) codes for nutritional deficiencies, stratified based on protein-energy malnutrition (ICD-10 codes E40-E46.9, E64.0), iodine deficiencies (E00-E02), vitamin A deficiencies (E50-E50.9, E64.1), dietary iron deficiencies (D50-D50.9), and other nutritional deficiencies such as vitamin deficiency anaemias, thiamine, niacin, vitamin D, vitamin C, calcium, selenium, and folate deficiency (D51-D53.9, E51-E61.9, E63-E64, E64.2-E64.9),16 with the full definitions used reported in the original GBD 2019 report.11 Obesity was measured by body mass index (BMI) using metrics related to national and subnational estimates, and defined as a high BMI of ≥25 kg/m2.17
The Joinpoint Regression Model version 4.9.1.018 was used to compare annual percentage changes (APC) in rates, through which trends in obesity and malnutrition, stratified by sex, geographical location, and SDI were observed. APCs of the age-standardised rates from 2000 to 2019 were presented with 95% confidence intervals (CIs). An APC value which is large in magnitude represents an increasing (worsening) or decreasing (improving) trend.
STATA version 17.0 was used to project the obesity and malnutrition-related burden of deaths and DALYs using historical data from 2000 to 2019 to test for linear and quadratic trends. Based on visual inspection and evaluation of the models, the most appropriate model with the best fit for each disease entity was chosen. Using the predictions from the regression models and the Institute for Health Metrics and Evaluation projection19 of population counts for years 2020–2030, we projected the burden of mortality and DALYs through to year 2030 for obesity and malnutrition. We also stratified the projections by sex for comparison. To examine the percentage change for obesity and malnutrition, the following equation was used:
The methods used to project the GBD estimates have been described previously.20 No sensitivity or post-hoc analyses were performed.
Ethics
The study was exempted from IRB review as the publicly available data did not contain any confidential patient information.
Role of the funding source
This research did not receive additional support from organisations beyond the authors’ academic institutions. Therefore, no funders had any role in the study design, data collection, data analyses, data interpretation, or writing of the report.
Results
Malnutrition
Global prevalence of malnutrition
In 2019, the global age-standardised prevalence rate for malnutrition was 16,835 (95% UI: 16,337–17,313) per 100,000 population (Supplementary Table S1). The prevalence per 100,000 population was higher in females (18,222 [95% UI: 17,681–18,790]) than in males (15,499 [95% UI 15,028–15,965]). From 2000 to 2019, there was an annual reduction in age-standardised prevalence rates worldwide (−0.39% [95% CI: −0.41 to −0.37]; −0.55% [95% CI: −0.57 to −0.53] for males, −0.25% [95% CI: −0.26 to −0.25] for females).
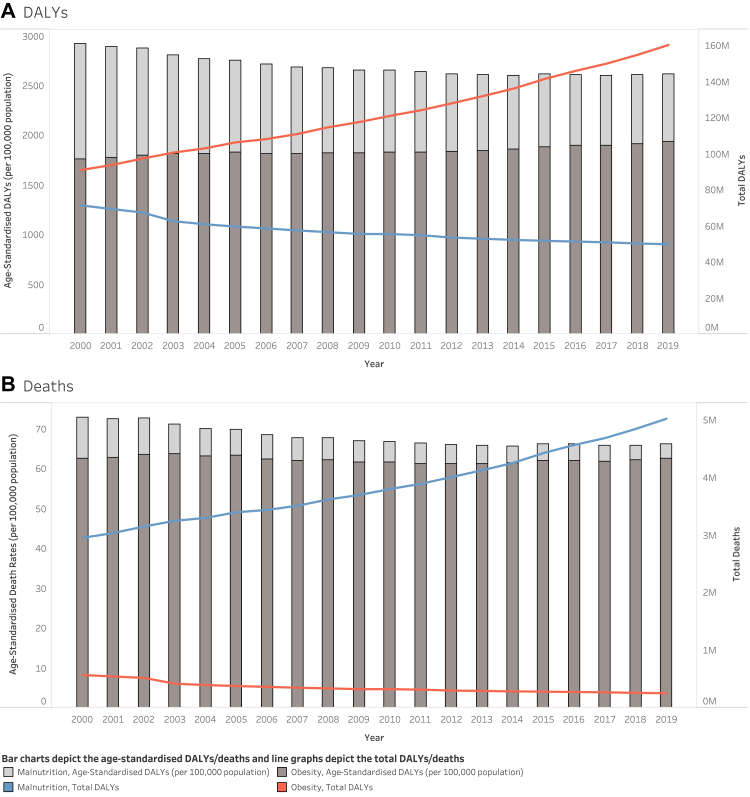
Overall malnutrition-related DALYs
Approximately 50 million DALYs were related to malnutrition in 2019 (Table 1), with an age-standardised DALY rate of 680 (95% UI: 507–895) per 100,000 population (Fig. 1A). Malnutrition-related DALY rates were higher in females (778 [95% UI: 579–1029]) compared to males (584 [95% UI: 441–763]); and a larger decrease in DALYs was observed in males (−3.22% [95% CI: −3.41 to −3.03]) than in females (−2.57% [95% CI: −2.73 to −2.42]) from 2000 to 2019. Across the years, there was an overall annual reduction in age-standardised DALY rates related to malnutrition (−2.86% [95% CI: −3.03 to −2.70]).
Table 1.
Disability-adjusted life years and mortality of individuals with malnutrition.
| DALYs |
Mortality |
|||||||
|---|---|---|---|---|---|---|---|---|
| Number 2019 | Age-standardised DALYs per 100,000 in 2019 | Annual percentage change 2000–2019 (%) | p-value | Number 2019 | Age-standardised death rate per 100,000 in 2019 | Annual percentage change 2000–2019 (%) | p-value | |
| Overall | 49,775,124 (36,889,950–65,839,422) | 680 (507–895) | −2.86 (−3.03 to −2.70) | <0.001 | 251,577 (221,150–289,040) | 3.52 (3.09–4.06) | −5.71 (−6.22 to −5.20) | <0.001 |
| Sex | ||||||||
| Male | 21,318,569 (16,030,317–27,817,401) | 584 (441–763) | −3.22 (−3.41 to −3.03) | <0.001 | 113,594 (99,257–129,012) | 3.45 (3.04–3.90) | −5.89 (−6.36 to −5.41) | <0.001 |
| Female | 28,456,555 (21,132,186–37,721,021) | 778 (579–1029) | −2.57 (−2.73 to −2.42) | <0.001 | 137,983 (118,651–165,844) | 3.64 (3.09–4.40) | −5.57 (−6.12 to −5.01) | <0.001 |
| WHO region | ||||||||
| Africa | 15,067,357 (11,792,113–18,890,743) | 1142 (893–1431) | −3.39 (−3.58 to −3.20) | <0.001 | 98,704 (79,248–124,293) | 11.63 (9.76–14.03) | −4.70 (−4.84 to −4.57) | <0.001 |
| Eastern Mediterranean | 5,836,326 (4,366,093–7,646,904) | 770 (577–1012) | −1.41 (−1.70 to −1.11) | <0.001 | 27,165 (20,780–34,574) | 4.62 (3.70–5.66) | −2.40 (−3.12 to −1.68) | <0.001 |
| Europe | 1,873,495 (1,298,031–2,579,991) | 202 (137–281) | −1.41 (−1.57 to −1.24) | <0.001 | 10,551 (8728–11,808) | 0.61 (0.51–0.68) | −1.34 (−1.55 to −1.13) | <0.001 |
| Region of Americas | 2,830,651 (2,160,366 to 3,740,292) | 292 (222–386) | −2.74 (−2.86 to −2.62) | <0.001 | 33,718 (29,633–37,002) | 2.82 (2.48–3.12) | −3.75 (−4.00 to −3.50) | <0.001 |
| South-East Asia | 20,097,893 (14,181,237–27,528,035) | 1059 (755–1444) | −3.79 (−4.17 to −3.41) | <0.001 | 55,979 (47,135–67,846) | 4.03 (3.43–4.80) | −9.63 (−11.45 to −7.77) | <0.001 |
| Western Pacific | 4,004,705 (2,839,008–5,483,388) | 209 (147–283) | −3.32 (−3.46 to −3.19) | <0.001 | 25,100 (22,107–27,519) | 1.19 (1.05–1.31) | −3.84 (−4.20 to −3.47) | <0.001 |
| SDI | ||||||||
| High | 1,456,034 (1,049,926–1,973,130) | 131 (91–181) | −0.55 (−0.78 to −0.32) | <0.001 | 16,051 (13,336–17,672) | 0.68 (0.58–0.75) | −1.37 (−1.75 to −0.99) | <0.001 |
| High-middle | 3,777,225 (2,628,068–5,243,542) | 275 (190–385) | −1.96 (−2.05 to −1.88) | <0.001 | 17,140 (15,215–18,564) | 0.98 (0.87–1.06) | −2.80 (−3.06 to −2.54) | <0.001 |
| Middle | 10,018,418 (7,136,818–13,547,619) | 446 (320–601) | −2.16 (−2.28 to −2.04) | <0.001 | 54,705 (49,551–59,490) | 3.00 (2.68–3.29) | −3.58 (−3.69 to −3.47) | <0.001 |
| Low-middle | 16,197,717 (11,889,740–21,765,779) | 946 (697–1264) | −4.08 (−4.51 to −3.65) | <0.001 | 59,226 (50,936–70,362) | 4.51 (3.94–5.28) | −9.54 (−10.39 to −8.68) | <0.001 |
| Low | 18,299,217 (14,184,880–23,321,623) | 1412 (1090–1802) | −3.12 (−3.27 to −2.96) | <0.001 | 104,285 (83,825–130,287) | 11.56 (9.75–13.97) | −5.03 (−5.30 to −4.76) | <0.001 |
Data in the parentheses are 95% uncertainty intervals· DALYs disability-adjusted life year; SDI Socio-Demographic Index; WHO World Health Organisation.
Fig. 1.
A) Disability-adjusted life year (DALYs) and age-standardised DALYs and B) number of deaths and age-standardised death rates at the global level by obesity and malnutrition, 2000–2019. Bar charts depict the age-standardised DALYs/deaths and line graphs depict the total DALYs/deaths.
Malnutrition-related differences in DALYs based on geographical region
In 2019, age-standardised malnutrition-related DALYs were highest in the Africa (1142 [95% UI: 893–1431]), followed by South-East Asia (1059 [95% UI: 755–1444]), and Eastern Mediterranean regions (770 [95% UI: 577–1012]). In contrast, Europe had the lowest age-standardised malnutrition-related DALYs (202 [95% UI: 137–281]), followed by Western Pacific (209 [95% UI: 147–283]) and Region of Americas (292 [95% UI: 222–386]). All geographical regions observed decreases in malnutrition-related DALY rates, with the largest reductions in South-East Asia (−3.79% [95% CI: −4.17 to −3.41]) and Africa (−3.39% [95% CI: −3.58 to −3.20]), and the smallest reductions seen in the Eastern Mediterranean region (−1.41% [95% CI: −1.70 to −1.11]) and Europe (−1.41% [95% CI: −1.57 to −1.24]).
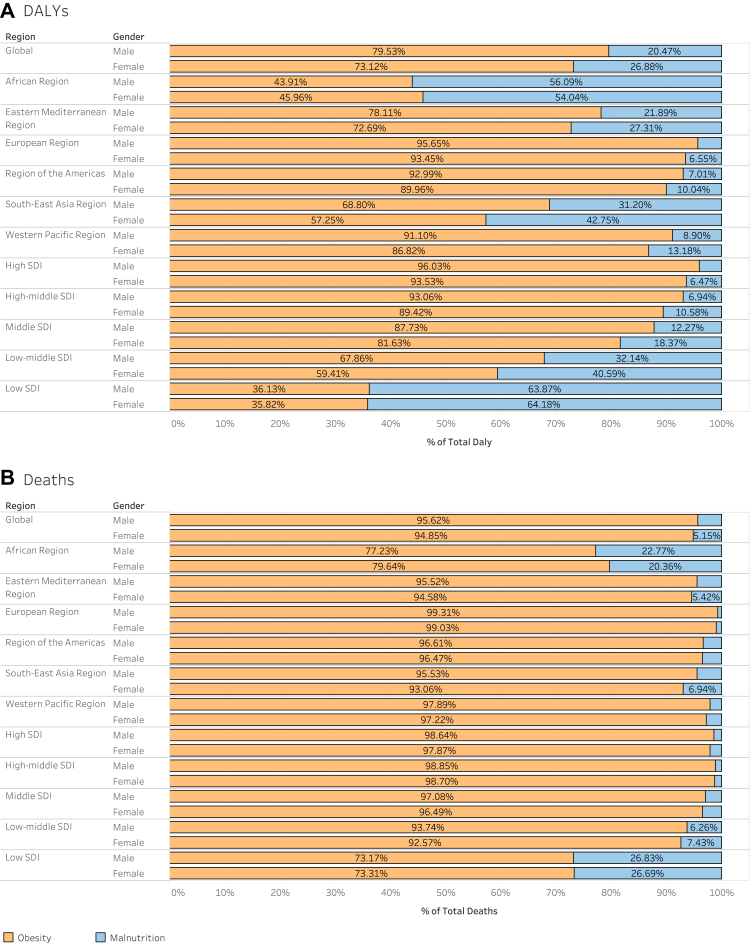
Malnutrition-related differences in DALYs based on socio-demographic index (SDI)
The malnutrition-related age-standardised DALYs decreased with increasing SDI, with low SDI countries observing the highest DALYs associated with malnutrition (1412 [95% UI: 1090–1802]), to high SDI countries with the lowest DALYs associated with malnutrition (131 [95% UI: 91–181]). There were increasing malnutrition-related age-standardised DALY rates in countries with decreasing SDI quintiles. Low (−3.12% [95% CI: −3.27 to −2.96]), low-middle (−4.08% [95% CI: −4.51 to −3.65]) and middle (−2.16% [95% CI: −2.28 to −2.04]) SDI countries observed the largest decreases in annual age-standardised DALY rates related to malnutrition, with the smallest reductions observed in high SDI countries (−0.55% [95% CI: −0.78 to −0.32]). Importantly, in 2019, malnutrition predominantly contributed to the burden of disease in the low SDI countries and in the African regions, whilst the burden of obesity was the largest across the remaining SDI quintiles and geographical regions (Fig. 2).
Fig. 2.
A) Proportion of deaths and, B) Proportion of disability-adjusted life years (DALYs) due to obesity and malnutrition, at global and regional levels by sex, 2019. SDI, Socio-Demographic Index.
Overall malnutrition-related mortality
In 2019, the global estimate of malnutrition-related deaths was 251,577 (95% UI: 221,150–289,040) (Table 1). The ASDR in individuals with malnutrition in 2019 was 3.52 (95% UI: 3.09–4.06) per 100,000 population (Fig. 1B). The ASDR per 100,000 population was higher in females (3.64 [95% UI: 3.09–4.40]) than in males (3.45 [95% UI: 3.04–3.90]). From 2000 to 2019, there was annual reduction in malnutrition-related mortality rates (−5.71% [95% CI: −6.22 to −5.20]), with similar reductions seen in both males and females (−5.89% [95% CI: −6.36 to −5.41] for males, −5.57% [95% CI: −6.12 to −5.01] for females).
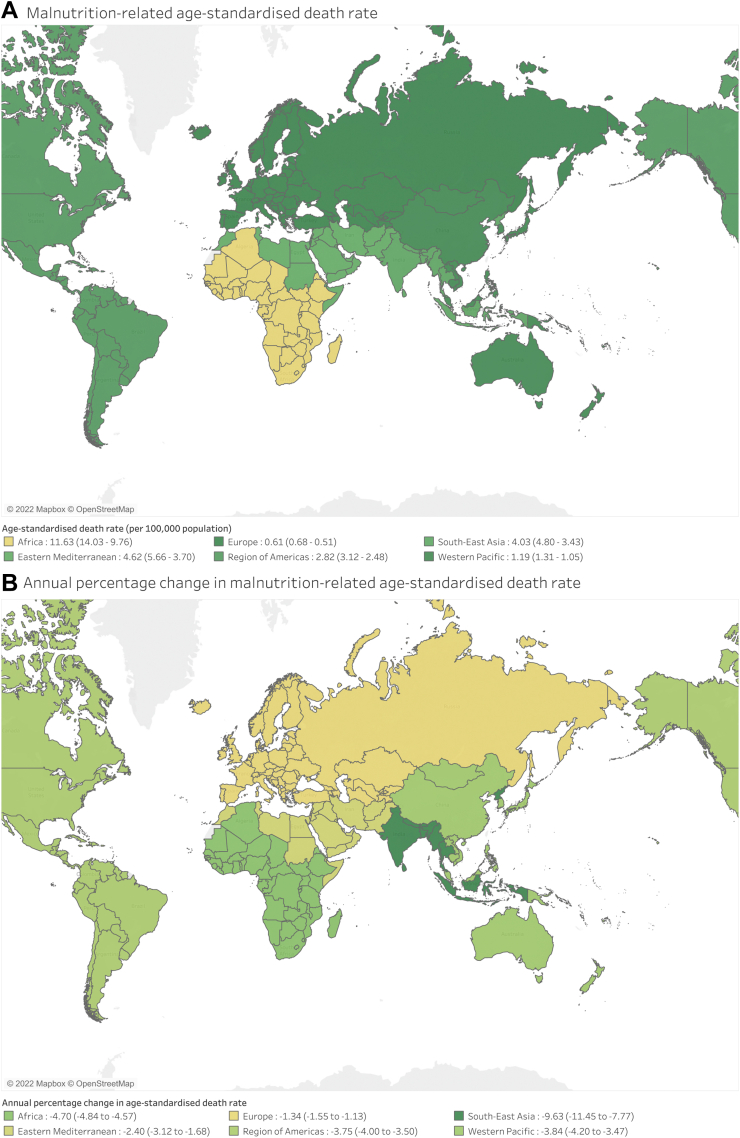
In 2019, Africa had the highest ASDR of 11.63 (95% UI: 9.76–14.03), followed by the Eastern Mediterranean (4.62 [95% UI: 3.70–5.66]) and South-East Asia regions (4.03 [95% UI: 3.43–4.80]). On the contrary, Europe had the lowest malnutrition-related ASDR (0.61 [95% UI: 0.51–0.68]), followed by Western Pacific (1.19 [95% UI: 1.05–1.31]). From 2000 to 2019, ASDR reductions in individuals with malnutrition were observed across all geographical regions (Fig. 3), with the largest decrease in South-East Asia (−9.63% [95% CI: −11.45 to −7.77]), followed by Africa (−4.70% [95% CI: −4.84 to −4.57]). Furthermore, 235,356 malnutrition-related deaths (93.6% of all deaths) occurred in low to high-middle SDI countries. The malnutrition-related ASDR decreased with increasing SDI, with low SDI countries observing the highest death rates associated with malnutrition (11.56 [95% UI: 9.75–13.97]), and the lowest death rates in high SDI countries (0.68 [95% UI: 0.58–0.75]). Countries from all SDI quintiles reported reductions in malnutrition-related ASDR from 2000 to 2019, with the largest reductions observed in low-middle SDI (−9.54% [95% CI: −10.39 to −8.68]), and low SDI countries (−5.03% [95% CI: −5.30 to −4.76]) across the years.
Fig. 3.
The global trends of A) obesity related age-standardised mortality and B) annual percentage change in malnutrition-related age-standardised death rate.
Obesity
Overall obesity-related DALYs
There was a global estimate of 160 million DALYs related to obesity in 2019 (Table 2), with an age-standardised DALY rate of 1933 (95% UI: 1277–2640) per 100,000 population (Fig. 1A). The obesity-related DALY rate was higher in males (2070 [95% UI: 1312–2889]) than in females (1790 [95% UI: 1229–2417]). From 2000 to 2019, there was a 0.48% (95% CI: 0.38–0.58) annual increase in age-standardised DALY rates related to obesity, with a larger increase observed in males (0.74% [95% CI: 0.63–0.85]) compared to females (0.25% [95% CI: 0.17–0.34]).
Table 2.
Disability-adjusted life years and mortality of individuals with obesity.
| DALYs |
Mortality |
|||||||
|---|---|---|---|---|---|---|---|---|
| Number 2019 | Age-standardised DALYs per 100,000 in 2019 | Annual percentage change 2000–2019 (%) | p-value | Number 2019 | Age-standardised death rate per 100,000 in 2019 | Annual percentage change 2000–2019 (%) | p-value | |
| Overall | 160,265,357 (105,969,034–218,870,439) | 1933 (1277–2640) | 0.48 (0.38–0.58) | <0.001 | 5,019,360 (3,223,364–7,110,736) | 62.59 (39.92–89.13) | −0.01 (−0.13 to0.11) | 0.881 |
| Sex | ||||||||
| Male | 82,840,928 (52,774,866–115,149,374) | 2070 (1312–2889) | 0.74 (0.63–0.85) | <0.001 | 2,477,387 (1,515,677–3,568,860) | 66.55 (39.76–97.21) | 0.33 (0.15–0.52) | <0.001 |
| Female | 77,424,429 (53,176,344–104,577,664) | 1790 (1229–2417) | 0.25 (0.17–0.34) | <0.001 | 2,541,973 (1,683,590–3,561,055) | 58.14 (38.53–81.39) | −0.27 (−0.38 to −0.16) | <0.001 |
| WHO region | ||||||||
| Africa | 12,324,913 (8,371,480–16,578,508) | 2221 (1486–3025) | 0.87 (0.80–0.95) | <0.001 | 361,539 (237,293–499,448) | 79.20 (50.92–111.98) | 0.86 (0.78–0.94) | <0.001 |
| Eastern Mediterranean | 17,923,202 (12,584,59–23,768,056) | 3721 (2591–4954) | 1.04 (0.92–1.15) | <0.001 | 522,392 (352,647–707,166) | 130.97 (87.38–179.78) | 1.01 (0.87–1.14) | <0.001 |
| Europe | 32,474,360 (22,183,037–43,473,404) | 2206 (1519–2946) | −0.90 (−1.10 to −0.70) | <0.001 | 1,243,937 (810,492–1,717,794) | 75.41 (49.74–103.02) | −1.16 (−1.41 to−0.89) | <0.001 |
| Region of Americas | 30,395,450 (21,207,720–39,622,411) | 2457 (1725–3200) | 0.17 (0.09–0.26) | <0.001 | 940,265 (625,116–1,268,476) | 72.83 (48.62–97.90) | −0.27 (−0.44 to −0.10) | 0.002 |
| South-East Asia | 33,558,095 (20,816,783–46,899,343) | 1786 (1096–2513) | 2.63 (2.48–2.77) | <0.001 | 918,795 (550,880–1,327,038) | 53.60 (31.54–78.85) | 2.37 (1.93–2.81) | <0.001 |
| Western Pacific | 33,058,032 (16,759,032–52,761,895) | 1229 (624–1963) | 1.22 (0.98–1.46) | <0.001 | 1,015,716 (483,041–1,701,367) | 38.38 (18.10–64.89) | 0.87 (0.48–1.26) | <0.001 |
| SDI | ||||||||
| High | 26,809,080 (18,213,631–36,348,663) | 1631 (1121–2198) | −0.14 (−0.19 to −0.09) | <0.001 | 901,712 (573,462–1,289,616) | 45.65 (29.76–63.76) | −1.02 (−1.20 to −0.84) | <0.001 |
| High-middle | 39,587,645 (26,141,026–54,009,607) | 1982 (1312–2706) | −0.91 (−1.09 to −0.73) | <0.001 | 1,376,628 (877,166–1,953,869) | 69.14 (44.00–98.24) | −1.21 (−1.44 to −0.99) | <0.001 |
| Middle | 55,465,889 (36,710,764–75,810,218) | 2119 (1388–2920) | 1.26 (1.18–1.35) | <0.001 | 1,647,281 (1,051,542–2,333,137) | 68.92 (43.02–99.26) | 1.05 (0.92–1.19) | <0.001 |
| Low-middle | 28,007,122 (17,469,919–39,227,162) | 1892 (1174–2682) | 2.41 (2.18–2.63) | <0.001 | 804,748 (490,930–1,158,654) | 60.34 (36.27–88.37) | 2.07 (1.79–2.36) | <0.001 |
| Low | 10,276,830 (6,088,926–14,897,027) | 1698 (990–2492) | 1.87 (1.79–1.94) | <0.001 | 285,468 (162,714–429,330) | 55.55 (31.38–85.09) | 1.68 (1.59–1.78) | <0.001 |
Data in the parentheses are 95% uncertainty intervals· DALYs disability-adjusted life year; SDI Socio-Demographic Index; WHO World Health Organisation.
Obesity-related differences in DALYs based on geographical region
Age-standardised obesity-related DALYs was highest in the Eastern Mediterranean region (3721 [95% UI: 2591–4954]) followed by Region of Americas (2457 [95% UI: 1725–3200]), Africa (2221 [95% UI: 1486–3025]), Europe (2206 [95% UI: 1519–2946]). On the contrary, the lowest age-standardised obesity-related DALYs were observed in the Western Pacific (1229 [95% UI: 624–1963]) and South-East Asia (1786 [95% UI: 1096–2513]). South-East Asia (2.63% [95% CI: 2.48–2.77]), Western Pacific (1.22% [95% CI: 0.98–1.46]), Eastern Mediterranean (1.04% [95% CI: 0.92–1.15]), Africa (0.87% [95% CI: 0.80–0.95]), and the Region of Americas (0.17% [95% CI: 0.09–0.26]) observed increases in age-standardised DALY rates from 2000 to 2019, with only Europe observing a decrease (−0.90% [95% CI: −1.10 to −0.70]).
Obesity-related differences in DALYs based on socio-demographic index (SDI)
The obesity-related age-standardised DALYs rose with increasing SDI from low (1698 [95% UI: 990–2492]) to low-middle (1892 [95% UI: 1174–2682]) and reaching the peak in middle (2119 [95% UI: 1388–2920]) SDI countries. The trend then reversed with age-standardised DALYs decreases in high-middle (1982 [95% UI: 1312–2706]) and high (1631 [95% UI: 1121–2198]) SDI countries. From 2000 to 2019, low (1.87% [95% CI: 1.79–1.94]), low-middle (2.41% [95% CI: 2.18–2.63]) and middle (1.26% [95% CI: 1.18–1.35]) SDI countries noted increases in annual age-standardised DALY rates related to obesity; whilst high-middle (−0.91% [95% CI: −1.09 to −0.73]) and high (−0.14% [95% CI: −0.19 to −0.09]) SDI countries experienced annual decreases in obesity-related DALY rates.
Overall obesity-related mortality
In 2019, there was an estimated 5.0 million obesity-related deaths worldwide. The age-standardised death rate (ASDR) for obesity was 62.59 (95% UI: 39.92–89.13) per 100,000 population (Fig. 1B), with higher rates (66.55 [95% UI: 39.76–97.21]) in males than in females (58.14 [95% UI: 38.53–81.39]). From 2000 to 2019, the overall ASDR remained relatively constant with an annual percentage decrease of 0.01% (95% CI: −0.13–0.11). An annual increase in obesity-related death rates was observed in males (0.33% [95% CI: 0.15–0.52]), whilst an annual reduction was seen amongst females (−0.27% [95% CI: −0.38 to −0.16]).
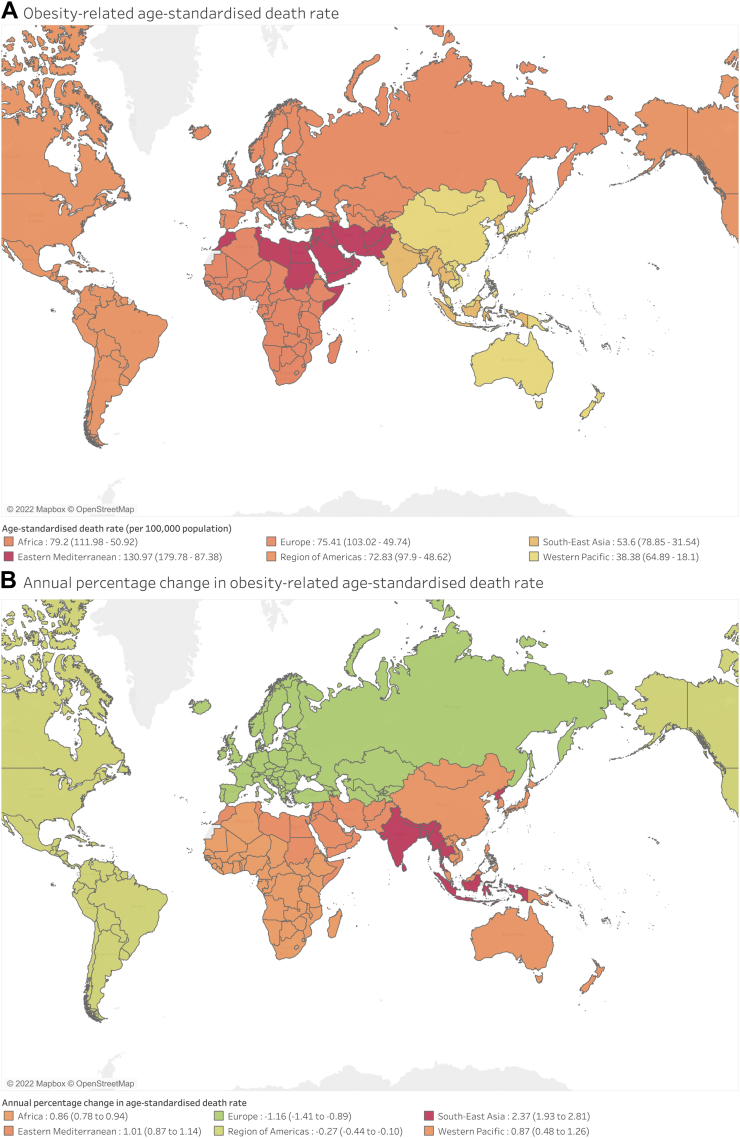
Obesity-related ASDR was highest in the Eastern Mediterranean region (130.97 [95% UI: 87.38–179.78]), followed by Africa (79.20 [95% UI: 50.92–111.98]), Europe (75.41 [95% UI: 49.74–103.02]), the Region of Americas (72.83 [95% UI: 48.62–97.90]). On the contrary, the lowest obesity-related ASDR was observed in the South-East Asia (53.60 [95% UI: 31.54–78.85), and the Western Pacific regions (38.38 [95% UI: 18.10–64.89]). Trends in the annual percentage change of ASDR from 2000 to 2019 varied across regions, with South-East Asia (2.37% [95% CI: 1.93–2.81]), the Eastern Mediterranean (1.01% [95% CI: 0.87–1.14]), the Western Pacific (0.87% [95% CI: 0.48–1.26]) and Africa (0.86% [95% CI: 0.78–0.94]) facing increases in obesity-related ASDR annually. On the contrary, there were annual decreases in ASDR in Europe (−1.16% [95% CI: −1.41 to −0.89]) and the Region of Americas (−0.27% [95% CI: −0.44 to −0.10]) from 2000 to 2019 (Fig. 4). Furthermore, 4,114,125 obesity-related deaths (82.0% of all deaths) occurred in low to high-middle SDI countries. The obesity-related ASDR rose with increasing SDI, from low (55.55 [95% UI 31.38–85.09]) to high-medium SDI countries (69.14 [95% UI: 44.00–98.24]). Notably, this trend was not observed in high SDI countries, which revealed the lowest ASDR related to obesity (45.65 [95% UI: 29.76–63.76]). From 2000 to 2019, low (1.68% [95% CI: 1.59–1.78]), low-middle (2.07% [95% CI: 1.79–2.36]), and middle (1.05% [95% CI: 0.92–1.19]) SDI countries experienced increasing annual ASDR; whilst high (−1.02% [95% CI: −1.20 to −0.84]) and high-middle (−1.21% [95% CI: −1.44 to −0.99]) SDI countries had decreasing annual obesity-related ASDR across the years.
Fig. 4.
The global trends of A) obesity related age-standardised mortality and B) annual percentage change in obesity-related age-standardised death rate.
Projected DALYs and deaths
From 2020 to 2030, the global estimates of malnutrition-related DALYs are projected to decrease by 8.4%, albeit a lesser extent than the reduction in malnutrition-related mortality (Supplementary Table S2). The decrease in DALYs is predicted to be larger in males (−12.8%) than in females (−5.0%).
The overall malnutrition-related mortality is also projected to decrease by 27.3% (Supplementary Table S3), from 254,276 to 184,801 cases worldwide (Supplementary Table S4). This percentage change is estimated to be greater in males (−28.4%) than in females (−26.4%).
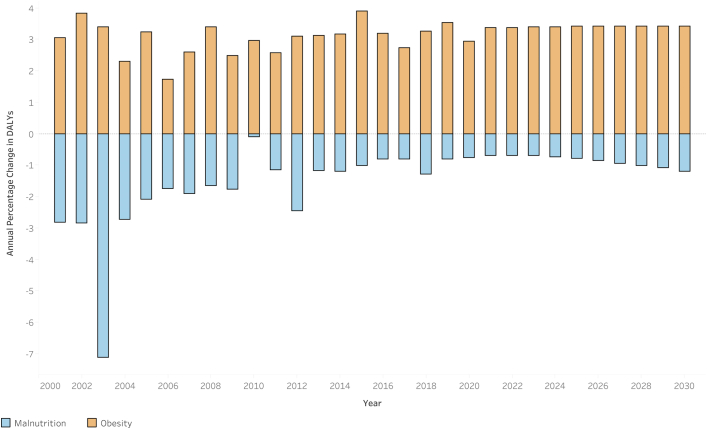
Obesity-related DALYs are projected to increase by 39.8% in the coming decade with a larger rise in females (41.3%) than in males (38.4%). Fig. 5 depicts the constant positive annual percentage change in obesity-related DALYs across the years, with a projected 3.4% annual increase from 2022 to 2030, and this increasing burden is not expected to change in the years to come. On the other hand, malnutrition-related DALYs observed the least reduction from 2016 to 2022, but is predicted to have a larger reduction from 2022 to 2030, with a projected annual reduction range from −0.7% to −1.2%. The global double burden of disease is projected to widen further in the coming decade, with obesity observing a 262% increased DALY burden compared to malnutrition in 2022, with almost doubled the obesity-malnutrition gap by 2030 (409% increased DALY burden; Supplementary Table S2). Projections of overall obesity-related mortality also suggest a 42.7% increase from 2020 to 2030, from 5,185,364 to 7,397,615 cases globally, with a greater percentage change seen in females (43.8%) compared to males (41.5%).
Fig. 5.
Bar graphs of Annual Percentage Change of Disability-adjusted Life Years (DALYs) by disease from 2000 to 2030.
Discussion
The current GBD study unravels temporal trends and predictions of the global burden of malnutrition and obesity, now and in the future. This offers an invaluable resource for long-term strategy development to tackle these challenging public health problems that often coexist interdependently (Central Illustration). Though the ubiquitous reductions in malnutrition-related DALYs and mortality worldwide give reason for optimism, this must be viewed against the backdrop of rising morbidities related to obesity.
Central illustration.
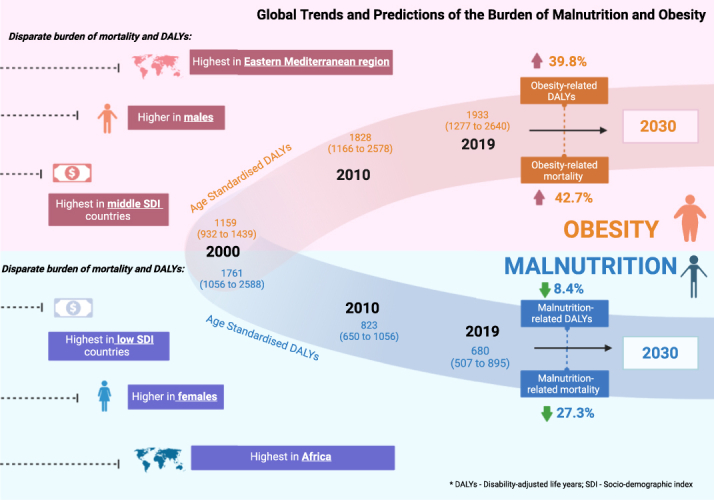
Global trends and predictions of the burden of malnutrition and obesity.
Our analysis portrays concerning disparities in mortality and DALYs across sex, geographical and socioeconomic factors: (1) Progress made in reducing malnutrition-related DALYs and mortality has been offset by the more-than-proportionately rising burden of obesity, with a widening chiasm observed between the two components of the double burden of malnutrition. This is especially evidenced by the regions registering the greatest reductions in malnutrition-related outcomes also demonstrating the greatest exacerbations in obesity-related disease burden. (2) Considerable spatial variations in the burden of disease across geographical regions parallel differences in social and cultural factors, with the highest mortality and DALY rates for both malnutrition and obesity seen in the Eastern Mediterranean and Africa. African countries are still burdened predominantly by malnutrition, while every other region has experienced the growing obesity epidemic as a larger driver of disease burden. (3) This geographical disparity is exacerbated by the SDI gradient, with the greatest malnutrition-related DALY and death rates found in lower SDI countries. This is in contrast with obesity-related death rates that generally rose with increasing SDI, with the exception of high SDI countries that benefitted from the lowest obesity-related death rates. (4) The forecasting analysis provides important insights as the burden of malnutrition and obesity is projected to widen further in the coming decade, with almost doubled the obesity-malnutrition gap by 2030. It also predicts a larger rise in the burden of obesity amongst females than males in the coming decade, highlighting the imperative need for policymakers to develop targeted sex-specific population-based strategies to reverse this trend before the projected exponential rise in the obesity burden leads to an epidemic that becomes irreversibly entrenched in society. As such, in this changing nutritional reality, malnutrition cannot be limited to addressing just undernutrition, but there is an urgency to increase awareness of the double burden of disease given the rising obesity rates, especially in areas where malnutrition was historically most widespread.
While malnutrition-related DALYs and mortality decreased from 2000 to 2019, obesity-related mortality and DALY rates trended in the opposite direction. These overall trends in the burden of malnutrition and obesity have been attributed mainly to rapid transitions in diets globally.3 Entire food systems consolidated under large businesses and manufacturers have heavily pushed the retail availability of highly processed foods, leading to relatively inexpensive but energy-dense options that dominate core parts of diets worldwide. These changes are not inherently detrimental – food processing has allowed for longer shelf-lives, inactivation of food-borne pathogens and better palatability.21 However, this has led to the formation of food deserts, areas characterised by an abundance of highly processed, high calorie, nutrient-poor foods while simultaneously facing a lack of nutrient-rich foods. Living in such dietary environments, coupled with a lack of financial resources, have resulted in individuals increasing their consumption of food that is energy-dense but low in micronutrients, evident in the increased adoption of sugary beverages and snacks, ultra-processed foods, and heavily salted, fried foods. This has been accompanied by a decrease in consumption of high fibre foods including fruit and vegetables, that are typically low in calories and high in micronutrients. This phenomenon has directly led to the increasing prevalence of obesity, surfacing difficult questions on the risk-benefit balance afforded by this new nutrition reality.3 The significant interplay between these two conditions deserves its due attention, with globalisation and social development accelerating the modern obesogenic environments that precede the obesity epidemic and the incidence of non-communicable diseases.22
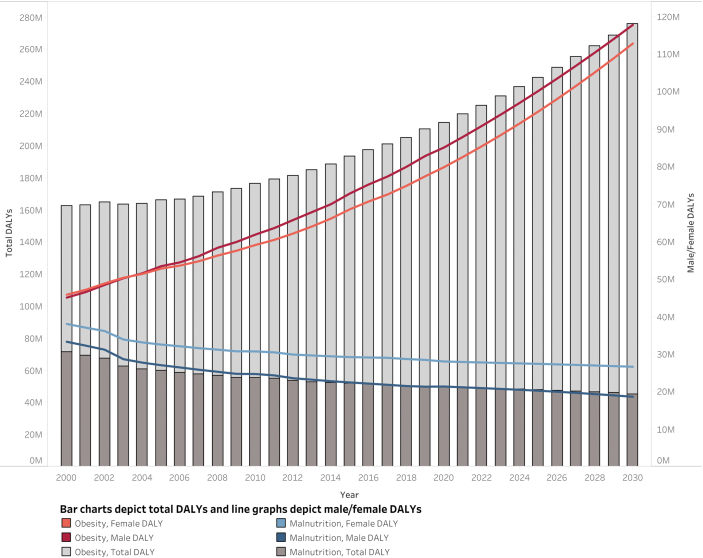
An interesting finding was the sex-specific disparity in obesity-related mortality predominantly affecting males, whilst the opposite was observed with the disparate malnutrition-related mortality rates unfavourably impacting females. This gap in obesity-malnutrition between males and females is projected to widen further in the years to come (Fig. 6). At the same BMI, men have been shown to demonstrate greater incident diabetes, insulin resistance, and ectopic fat levels, which may contribute to higher rates of obesity-related morbidity and mortality.23 Conversely, the higher rates of malnutrition-related outcomes in females emphasise several biological and social underpinnings. Food insecurity has been shown to be more prevalent in women than in men across the world, with increased nutritional demands secondary to menstruation, pregnancy and lactation.24 Moreover, discriminatory customs and practices prioritising men's dietary requirements also leave women to eat last, and eat less.25 As such, both obesity and malnutrition need to be addressed through the development of targeted, sex-specific strategies that effectively address the specific mechanisms underlying this disparity.26
Fig. 6.
Projection of Disability-adjusted Life Years (DALYs) by disease from 2000 to 2030. Bar charts depict total DALYs and line graphs depict male/female DALYs.
Clear trends in malnutrition could be observed with SDI as a comparator, with both DALYs and mortality falling substantially in countries with increasing SDI quintiles. This does not come as a surprise—the SDI is a composite measure of a region's per-capita income, fertility rates and average education levels,14 all three of which have links to malnutrition. All SDI quintiles saw reductions in malnutrition-related deaths and DALYs, with the largest decreases observed in low and low-middle SDI quintile countries. Low and low-middle SDI countries are reportedly in the midst of their nutrition transition partly as a result of general economic growth,27 as well as the concerted efforts in targeted and deliberate interventions aimed at tackling undernutrition.28 Opposite trends were observed with increasing obesity-related DALYs and mortality in countries of higher SDI quintiles. This may be well characterised by the stages of nutritional change model,29 in which low-middle SDI countries transitioning to stage 2 depict the shift from receding famine to degenerative disease–urbanisation, economic growth and technological changes result in a greater prevalence of obesity and its associated non-communicable diseases.3 On the other hand, high-middle SDI regions show progression to stage 3 of the nutrition transition,29 observing positive behavioural change with increased awareness of and adherence to balanced diets, combined with more active lifestyles that help combat obesity.
Nonetheless, there remain large disparities in obesity and malnutrition-related DALYs and mortality across various geographical regions, with the largest burden borne by the Eastern Mediterranean and African regions. The reasons underpinning the burden of malnutrition and obesity are likely multifaceted and deeply entrenched. These factors have been described in several studies, which include differences in the prevalence of poverty, the effects of climate change on agriculture, the level of education, the readiness of governmental responses, as well as biological processes such as differences in fat patterning, body composition and cardiometabolic effects of BMI.30 Notably, the largest decrease in malnutrition-related mortality and increase in obesity-related mortality were observed in South-East Asia. This can be largely tied back to economic growth in the region, with increasing urbanisation has led to a more sedentary lifestyle and unhealthy diets. For example, Malaysia, which is the country with the highest prevalence of obesity in South-East Asia, has seen fat and sugar intake increase by 80% and 33% respectively over the past decades; with only a third of the population having ever exercised. The cost of obesity has seen healthcare spending in Malaysia being the highest in the region.31 Nevertheless, its government has taken steps in an attempt to reverse this rise in obesity by introducing a sugar tax levy to transition the country away from high calorie, nutrient-poor foods to nutrient-rich foods, as well as providing subsidies for fruits and vegetables.32 On the other hand, Europe had the second highest burden of obesity in 2000, and was the only region that observed decrease in age-standardised obesity-related DALY rates over the past 2 decades. Its implementation of the WHO European Childhood Obesity Surveillance Initiative (COSI)33 not only improved the understanding of obesity as a public health challenge, but also helped to inform and drive public policy in promoting physical activity and healthy diets across Europe.33
Policies can aim to promote a healthy diet through promotional campaigns that increase the consumption of plant-based foods. This should be accompanied by shifting the agricultural priorities from supplying high quantities of food to producing healthy food along with the sustainable intensification of food production to support the high-quality output. This will require strong and coordinated governance of both the land and seas as well as concrete plans to reduce food wastes from both the production and consumption sides in accordance to the EAT lancet commission diet.34 At the individual level, it is important to inculcate positive exercise and dietary habits in the public from a young age, based on either national recommendations or targets such as the WHO healthy diet35 or the EAT lancet commission diet.34 Building good habits in children is essential to reduce future burden of disease and healthcare costs, as they grow up a more informed and healthy populace.35
The unique design of the present study consolidates both malnutrition and obesity into a single framework, utilising historical trends to project the incoming burden of disease, and this has led to several key messages. It is prudent for healthcare policies to focus the attention on addressing the combined challenges of malnutrition and obesity, rather than each individual entity in isolation, mitigating the risk of compromising one global health issue for the other. The study highlights the danger of viewing the drivers of malnutrition as independent causative factors distinct from the underlying causes of obesity that can—and has—led to approaches targeting malnutrition that inadvertently exacerbate obesity.4 In addition, approaches in addressing malnutrition must be tailored and weighed against the obesity epidemic, with strategies to overcome the global disparity, empower access to quality food and instilling healthy eating-habits in populations through a combination of policy, education, and healthcare improvements.4 The study demonstrates that the low-middle SDI communities undergoing rapid development and growth have seen sharp reductions in malnutrition accompanied by spikes in obesity. In fact, the increasing rates of obesity-related DALYs are predicted to remain unchanged in the years to come, with a larger increase in DALYs expected to be borne by females. The concerning forecast of the obesogenic climate can generate momentum for change with the collective efforts in initiating effective population-specific interventions to tackle the widening burden of malnutrition and obesity, through equitable access to environmentally sustainable diets, food security, eating patterns, and diet quality.7
This study has several limitations. Firstly, the combined estimates of obesity and malnutrition would serve as a more accurate indicator of the double burden of malnutrition. However, individual patient data could not be retrieved as the Global Health Data Exchange only provides estimates of individual disease entities. Secondly, estimates made are highly dependent on primary data, and where not available, GBD estimates rely on modelling processes, predictive covariates and temporal trends derived from neighbouring countries that may lead to inherent biases. As such, inherent bias from the different adopted metrics and methods used may also affect the accuracy of the prediction model. Thirdly, there could be potential data quality concerns with regards to the mortality data acquisition due to inherent challenges of ascertaining deaths related to specific causes such as malnutrition. Moreover, these concerns are likely to have a larger effect on countries with lower levels of development and record keeping. This may lead to potential underestimation of the global burden of disease, as well as the geographical and socioeconomic disparity in mortality.36
The ubiquitous reduction in the burden of malnutrition has been offset by the more-than-proportionately rising burden of obesity, with the obesity-malnutrition chiasm predicted to widen further in the coming decade. This evokes a sense of urgency for effective sex-regional-socioeconomic tailored strategies to derail the projected trajectory of the burden of malnutrition and obesity, with heightened vigilance amongst stakeholders in avoiding compromising one disease entity for the other.
Contributors
BC, JJ, YHC, RF, MYC, MAM, GKD, CLR, and NWSC were responsible for conceptualisations and methodology of the study. BC, JJ, GK, YHC, YHC, RG, SK, SL, MTWK, CHN, CL, VVA, ELCZ, JC, DJHT, KEC, RF, MYC, MAM, GKD, CLR, and NWSC were responsible for investigation and data curation. BC, JJ, GK, YHC, YHC, RG, SK, SL, MTWK, CHN, CL, VVA, ELCZ, JC, DJHT, KEC, RF, MYC, MAM, GKD, CLR, and NWSC were responsible for formal analysis and software. YHC, JWW, MM, DJH, AM, GL, RF, MYC, MAM, GKD, CLR, and NWSC were responsible for supervision. BC, JJ, GK, YHC, YHC, RG, SK, SL, MTWK, CHN, CL, VVA, ELCZ, JC, DJHT, KEC, JWW, MM, DJH, AM, GL, RF, MYC, MAM, GKD, CLR, and NWSC were responsible for validation. BC, JJ, and NWSC were responsible for writing the original draft. BC, JJ, GK, YHC, YHC, RG, SK, SL, MTWK, CHN, CL, VVA, ELCZ, JC, DJHT, JWW, MM, DJH, AM, GL, RF, MYC, MAM, GKD, CLR, and NWSC were responsible for writing, preparation, review and editing drafts. BC, JJ, and NWSC accessed and verified the underlying data. All authors read and approved the final version of the manuscript.
Data sharing statement
All data and codes used in analysis and projections are available upon request to the corresponding author.
Editor note
The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Declaration of interests
GYHL is a consultant and speaker for BMS/Pfizer, Boehringer Ingelheim, Daiichi-Sankyo, Anthem; no fees are received personally. GYHL is also co-principal investigator of the AFFIRMO project on multimorbidity in AF, which has received funding from the European Union's Horizon 2020 research and innovation programme (under grant agreement no. 899871). MYC receives speaker's fees and research grants from Astra Zeneca, Abbott Technologies and Boston Scientific. CWlR reports grants from the Irish Research Council, Science Foundation Ireland, Anabio, and the Health Research Board; serves on advisory boards of Novo Nordisk, Herbalife, GI Dynamics, Eli Lilly, Johnson & Johnson, Glia, and Boehringer Ingelheim; is a member of the Irish Society for Nutrition and Metabolism outside the area of work commented on here; and was the chief medical officer and director of the Medical Device Division of Keyron in 2011 (both are unremunerated positions). CWlR was a previous investor in Keyron, which develops endoscopically implantable medical devices intended to mimic the surgical procedures of sleeve gastrectomy and gastric bypass. The product has only been tested in rodents and none of Keyron's products are currently licensed. They do not have any contracts with other companies to put their products into clinical practice. No patients have been included in any of Keyron's studies and they are not listed on the stock market. CWlR was also gifted stock holdings in September 2021 and divested all stock holdings in Keyron in September, 2021; CWlR continues to provide scientific advice to Keyron for no remuneration. All other authors declare no competing interests.
Acknowledgements
All authors have made substantial contributions to the following: (1) the conception and design of the study, or acquisition of data, or analysis and interpretation of data, (2) drafting the article or revising it critically for important intellectual content, (3) final approval of the version to be submitted. No writing assistance was obtained in the preparation of the manuscript.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.eclinm.2023.101850.
Appendix A. Supplementary data
References
- 1.United Nations System Standing Committee. The UN decade of action on nutrition 2016-2025. Available from: https://www.unscn.org/en/topics/un-decade-of-action-on-nutrition. Accessed October 11, 2022.
- 2.Wells J.C., Sawaya A.L., Wibaek R., et al. The double burden of malnutrition: aetiological pathways and consequences for health. Lancet. 2020;395(10217):75–88. doi: 10.1016/S0140-6736(19)32472-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Popkin B.M., Corvalan C., Grummer-Strawn L.M. Dynamics of the double burden of malnutrition and the changing nutrition reality. Lancet. 2020;395(10217):65–74. doi: 10.1016/S0140-6736(19)32497-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hawkes C., Ruel M.T., Salm L., Sinclair B., Branca F. Double-duty actions: seizing programme and policy opportunities to address malnutrition in all its forms. Lancet. 2020;395(10218):142–155. doi: 10.1016/S0140-6736(19)32506-1. [DOI] [PubMed] [Google Scholar]
- 5.Melaku Y.A., Gill T.K., Taylor A.W., et al. Trends of mortality attributable to child and maternal undernutrition, overweight/obesity and dietary risk factors of non-communicable diseases in sub-Saharan Africa, 1990-2015: findings from the Global Burden of Disease Study 2015. Public Health Nutr. 2019;22(5):827–840. doi: 10.1017/S1368980018002975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Five insights from the global burden of disease study 2019. Lancet. 2020;396(10258):1135–1159. doi: 10.1016/S0140-6736(20)31404-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Swinburn B.A., Kraak V.I., Allender S., et al. The global syndemic of obesity, undernutrition, and climate change: the lancet commission report. Lancet. 2019;393(10173):791–846. doi: 10.1016/S0140-6736(18)32822-8. [DOI] [PubMed] [Google Scholar]
- 8.The Institute for Health Metrics and Evaluation GBD results. 2019. https://vizhub.healthdata.org/gbd-results/ Available from:
- 9.Roth G.A., Mensah G.A., Johnson C.O., et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J Am Coll Cardiol. 2020;76(25):2982–3021. doi: 10.1016/j.jacc.2020.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Murray C.J.L. The global burden of disease study at 30 years. Nat Med. 2022;28(10):2019–2026. doi: 10.1038/s41591-022-01990-1. [DOI] [PubMed] [Google Scholar]
- 11.Vos T., Lim S.S., Abbafati C., et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet. 2020;396(10258):1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Global, regional, and national burden of colorectal cancer and its risk factors, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet Gastroenterol Hepatol. 2022;7(7):627–647. doi: 10.1016/S2468-1253(22)00044-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.The Institute for Health Metrics and Evaluation. Socio-demographic index (SDI). Available from: https://www.healthdata.org/taxonomy/glossary/socio-demographic-index-sdi#:∼:text=A%20summary%20measure%20that%20identifies,areas%20in%20the%20GBD%20study. Accessed November 2, 2022.
- 15.World Health Organisation. WHO regions. Available from: https://ourworldindata.org/grapher/who-regions. Accessed November 2, 2022.
- 16.Institute for Health Metrics and Evaluation (IHME). Global burden of disease study 2019 (GBD 2019) cause list mapped to ICD codes. Available from: https://ghdx.healthdata.org/record/ihme-data/gbd-2019-cause-icd-code-mappings. Accessed November 11, 2022.
- 17.Stanaway J.D., Afshin A., Gakidou E., et al. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet. 2018;392(10159):1923–1994. doi: 10.1016/S0140-6736(18)32225-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Statistical Methodology and Applications Branch SRP, National Cancer Institute . 2022. Joinpoint regression program, Version 4.9.1.0. [Google Scholar]
- 19.The Institute for Health Metrics and Evaluation. Population forecasting. Available from: https://vizhub.healthdata.org/population-forecast/. Accessed August 8, 2022.
- 20.Mohebi R., Chen C., Ibrahim Nasrien E., et al. Cardiovascular disease projections in the United States based on the 2020 census estimates. J Am Coll Cardiol. 2022;80(6):565–578. doi: 10.1016/j.jacc.2022.05.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.van Boekel M., Fogliano V., Pellegrini N., et al. A review on the beneficial aspects of food processing. Mol Nutr Food Res. 2010;54(9):1215–1247. doi: 10.1002/mnfr.200900608. [DOI] [PubMed] [Google Scholar]
- 22.Llewellyn D.C., Logan Ellis H., Aylwin S.J.B., et al. The efficacy of GLP-1RAs for the management of postprandial hypoglycemia following bariatric surgery: a systematic review. Obesity (Silver Spring) 2023;31(1):20–30. doi: 10.1002/oby.23600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Di Angelantonio E., Bhupathiraju S.N., Wormser D., et al. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet. 2016;388(10046):776–786. doi: 10.1016/S0140-6736(16)30175-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.World Food Program USA These are the top 6 reasons women are hungrier than men today. 2022. https://www.wfpusa.org/articles/women-in-crisis-top-ways-women-are-hungrier/ Available from:
- 25.Fu C.E., Ng C.H., Chew N.W.S., et al. A poor perspective of self weight significantly increases adverse outcomes in non-alcoholic fatty liver disease (NAFLD) Front Med (Lausanne) 2022;9 doi: 10.3389/fmed.2022.977552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Quek J., Chan K.E., Wong Z.Y., et al. Global prevalence of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in the overweight and obese population: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2023;8(1):20–30. doi: 10.1016/S2468-1253(22)00317-X. [DOI] [PubMed] [Google Scholar]
- 27.O'Connell S.A., Smith C. Economic growth and child undernutrition. Lancet Glob Health. 2016;4(12):e901–e902. doi: 10.1016/S2214-109X(16)30250-9. [DOI] [PubMed] [Google Scholar]
- 28.Gillespie S., Haddad L., Mannar V., Menon P., Nisbett N. The politics of reducing malnutrition: building commitment and accelerating progress. Lancet. 2013;382(9891):552–569. doi: 10.1016/S0140-6736(13)60842-9. [DOI] [PubMed] [Google Scholar]
- 29.Popkin B.M. An overview on the nutrition transition and its health implications: the Bellagio meeting. Public Health Nutr. 2002;5(1A):93–103. doi: 10.1079/phn2001280. [DOI] [PubMed] [Google Scholar]
- 30.Consultation WE Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363(9403):157–163. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 31.The Economist Intelligence Unit . 2017. Tackling obesity in ASEAN: prevalence, impact, and guidance on interventions. [Google Scholar]
- 32.Goh E.V., Azam-Ali S., McCullough F., Roy Mitra S. The nutrition transition in Malaysia; key drivers and recommendations for improved health outcomes. BMC Nutr. 2020;6(1):32. doi: 10.1186/s40795-020-00348-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Buoncristiano M., Spinelli A., Williams J., et al. Childhood overweight and obesity in Europe: changes from 2007 to 2017. Obes Rev. 2021;22(S6) doi: 10.1111/obr.13226. [DOI] [PubMed] [Google Scholar]
- 34.Willett W., Rockström J., Loken B., et al. Food in the Anthropocene: the EAT-Lancet commission on healthy diets from sustainable food systems. Lancet. 2019;393(10170):447–492. doi: 10.1016/S0140-6736(18)31788-4. [DOI] [PubMed] [Google Scholar]
- 35.World Health Organization . Regional Office for the Eastern Mediterranean; 2019. Healthy diet. World health organization. [Google Scholar]
- 36.Huibers M.H.W., Manda G., Silverstein A., et al. The burden of malnutrition in childhood cancer in Malawi—risk regardless of age. Nutr Cancer. 2022;74(9):3322–3328. doi: 10.1080/01635581.2022.2076888. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.