Abstract
Background
Previous research suggests that racial and ethnic minority groups especially Black Americans showed stronger COVID-19 vaccine hesitancy and resistance, which may result from a lack of trust toward the government and vaccine manufacturers, among other sociodemographic and health factors.
Objectives
The current study explored potential social and economic, clinical, and psychological factors that may have mediated racial and ethnic disparities in COVID-19 vaccine uptake among US adults.
Methods
A sample of 6078 US individuals was selected from a national longitudinal survey administered in 2020–2021. Baseline characteristics were collected in December 2020, and respondents were followed up to July 2021. Racial and ethnic disparities in time to vaccine initiation and completion (based on a 2-dose regimen) were first assessed with the Kaplan-Meier Curve and log-rank test, and then explored with the Cox proportional hazards model adjusting for potential time-varying mediators, such as education, income, marital status, chronic health conditions, trust in vaccine development and approval processes, and perceived risk of infection.
Results
Prior to mediator adjustment, Black and Hispanic Americans had slower vaccine initiation and completion than Asian Americans and Pacific Islanders and White Americans (p’s < 0.0001). After accounting for the mediators, there were no significant differences in vaccine initiation or completion between each minoritized group as compared to White Americans. Education, household income, marital status, chronic health conditions, trust, and perceived infection risk were potential mediators.
Conclusion
Racial and ethnic disparities in COVID-19 vaccine uptake were mediated through social and economic conditions, psychological influences, and chronic health conditions. To address the racial and ethnic inequity in vaccination, it is important to target the social, economic, and psychological forces behind it.
Keywords: Disparity; Vaccine; COVID-19; Racial and ethnic minority, survival analysis
1. Introduction
The novel coronavirus (SARS-COV-2) has infected over 700 million people worldwide and caused nearly 7 million deaths in early 2023 [1]. In the United States (US), more than 100 million confirmed cases and over one million deaths have been reported [2]. Some racial and ethnic minority groups have been disproportionately impacted by the emergence of COVID-19, especially in the early pandemic, with non-Hispanic Black Americans (referred to as Black Americans) and Hispanic Americans experiencing disproportionately higher rates of morbidity and mortality compared to non-Hispanic White Americans (referred to as White Americans) [3], [4], [5].
The widespread COVID-19 vaccine uptake across the world is shown to be protective against COVID-19 related hospitalization and mortality. Repeated vaccination at 9- or 12-month intervals has been recommended by some scientists due to reduced vaccine efficacy over time and the emergence of new variants [6]. High vaccine uptake rates between 75% and 90% are required to achieve herd immunity [7], and equitable vaccine uptake among different racial and ethnic groups can reduce disparities in COVID-19 related mortality and morbidity [8]. According to the current data from Centers for Disease Control and Prevention (CDC), completion of the two-dose regimen is highest among Asian Americans (97%), similar among Black, Hispanic, and White Americans (84–85%), and lowest among American Indians and Alaska Natives (AIAN, 77%). However, the uptake of the booster dose is low in all groups, with the highest rate in White Americans (35%), followed by Asian (29%), AIAN(26%), Black (23%), and Hispanic (17%) Americans [2]. Racial and ethnic inequity in vaccine uptake was observed in the early phase of the vaccine rollout process. For instance, during the initial distribution phase of the vaccine in the State of Maryland in 2020, the vaccination rate was lowest in the predominantly Black Prince George County with highest COVID-19 incidence, but highest among the predominantly White and affluent Howard County with much lower COVID-19 incidence [3]. By the end of April 2021, vaccine uptake of at least 1 dose among Asian, White, Hispanic, and Black Americans was 70%, 59%, 47% and 46%, respectively [8]. The gaps narrowed by November 2021, with White, Hispanic, and Black Americans achieved equitable first dose coverage (78-81%).
Previous studies on social determinants of health proposed that social and economic factors likely mediate the pathways from race and ethnicity to health and healthcare disparities. For instance, maternal education and insurance status mediated the racial and ethnic disparities in congenital heart disease outcomes [9]; income and health behaviors mediated disparities in mortality among Black and White Americans [10]; social and economic conditions explained racial and ethnic disparities in COVID-19 infections [11]. In this work, we proposed three domains of mediators that may explain racial and ethnic disparities in vaccine uptake timelines. The first domain consists of social and economic mediators such as education level, household income, and health insurance type [12], [13]. The second domain of mediators includes chronic health conditions that may deter or expedite vaccine uptake. Some minoritized groups have a greater burden of chronic diseases, which put them at higher risk for mortality and severe illness from COVID-19. They may adopt the vaccine early to prevent infection and its complications or forgo the vaccine due to its potential side effects [14]. The third domain of mediators is referred to as psychological influences, such as concerns around social norms and the patient’s belief system [15]. Trust is a major factor in vaccine hesitancy, which may lead to delay and refusal of vaccines [16]. Racial and ethnic minorities especially Black Americans have reported resistance or hesitancy in their intention to adopt the COVID-19 vaccine [17], which may result from a lack of trust, among other factors, toward the government and manufacturers [18]. Mistrust in the healthcare system and concerns about the vaccine effectiveness and safety are factors behind the hesitancy of COVID vaccine uptake among the Black community [19].
In this study, we aimed to explore social and economic, clinical, and psychological factors that mediated the racial and ethnic disparities in COVID-19 vaccine uptake timelines among US adults. We distinguish mediators from confounders in that although both types of variables are associated with the exposure and the outcome, the mediators are on the pathway between the exposure and the outcome, whereas the confounders are not. Accordingly, age and gender behave as confounders of racial and ethnic disparities in vaccine uptake.
The research was approved by the University of Toledo Institutional Review Board. All authors declared no conflict of interests.
2. Methods
2.1. Data source
Data were drawn from the Understanding America Study (UAS) conducted by the University of Southern California [20]. UAS is a probability-based Internet panel representative of the US adult population excluding institutionalized individuals and military personnel [21]. The online survey in response to the COVID-19 pandemic adopted a multi-phase (mail, web) address-based sampling frame. It was initiated in March 2020 and collected data around 6000 respondents biweekly up to wave 24 (March 2021) and every four weeks afterwards until the final wave (wave 29). The final wave of the survey was fielded from June 9 to July 21, 2021. Each wave maintained a similar number of respondents, with new respondents recruited to compensate for attrition in each wave. Internet access and a tablet were provided to the survey participants to minimize the barriers to online participation [22]. Poststratification weights were provided to address selection bias and to match the sociodemographic characteristics of external distributions. The survey encompassed a wide array of domains of information, such as psychosocial well-being during the pandemic, risk perception, preventive behaviors, and vaccination.
2.2. Design and Follow-Up
A few key attitudinal variables towards the vaccine that highly likely influenced the subsequent actual vaccination behavior were first collected in wave 20 (initiation date December 9, 2020). Thus, we selected this panel as our baseline cohort. The total number of respondents at baseline was 6078. The baseline survey field date was approximate to the start of the national distribution of the COVID-19 vaccine in December 2020. Thus we chose December 9, 2020 as the follow-up start date. Respondents were followed up until the final wave (wave 29, July 2021) or the last observed survey participation date if they dropped out early. Time to first (or second) dose was measured as the time from the start of the follow-up to the self-reported date of the first (or second) dose received. A case for a dose was considered censored when no date for the corresponding dose was recorded. The censoring point was set at the last observed survey date.
Time to first dose and time to second dose were compared between each racial and ethnic group and White Americans to assess inequity in vaccine uptake timelines.
2.3. Outcomes
This study mainly explored two outcomes based on the two-dose regimen: vaccine initiation – time to first dose, and vaccine completion – time to second dose. The two doses were not theoretically independent. However, for our analysis, they were treated as two separated outcomes.
2.4. Independent variable
Race and ethnicity were classified as White Americans, Black Americans, Hispanic Americans, Asian Americans and Pacific Islanders (AAPIs), and Other. Because the sample size of Native Americans was very small (N = 51, 0.84%) and may yield inadequate statistical power in estimates, this category was included in the Other category.
2.5. Potential mediators
Potential mediators assessed in each wave covered three domains: social and economic, clinical, and psychological. Social and economic variables were marital status (married vs. unmarried), education (1–16), household income (1–16), and current working status (yes/no). Chronic health conditions (each as a dichotomous yes/no response) included asthma, autoimmune diseases, cancer, COPD, diabetes, heart diseases, hypertension, kidney diseases, mental disorder, obesity, and disability. Due to small cell sizes of some chronic health conditions by racial and ethnic group, a sum of all chronic health conditions was calculated for each participant (0-9). Psychological factors referred to perceived COVID risk, trust of the vaccine, and experience of discrimination. Perceived COVID risk was based on a factor analysis of four questions assessing perceived risk of death from COVID-19, hospitalization from COVID-19, contracting COVID-19, and risk of running out of money in the next 3 months. The respondents rated each risk on a 0% to 100% scale. Cronbach alpha for this scale was 0.72. The final scale took the mean of these four items and multiplied it by 0.1 to keep the scale in a range comparable to other covariates. Trust of the vaccine development process and trust of governmental approval process were assessed by two separate questions: 1) How much do you trust the process in general (not just for COVID-19) to develop safe vaccines for the public? and 2) How much do you trust the governmental approval process to ensure the COVID-19 vaccine is safe for the public? Each response was a four-point Likert scale: fully trust, mostly trust, somewhat trust, and do not trust. These responses were reverse coded so that a higher score reflected stronger trust. Experience of discrimination was assessed with four questions (e.g., you were treated with less courtesy and respect than other people), with the original response scale of yes, no, and unsure. A respondent was classified as having experienced discrimination if a positive answer (yes) was recorded for any of the four questions; otherwise, the person was classified as having not experienced discrimination. These potential mediators were assessed in each wave and were included as time-varying variables.
2.6. Statistical analysis
We first looked at the baseline distribution of potential mediators by racial and ethnic group, and the statistical differences were expressed with the chi-square test for categorical variables or ANOVA for continuous variables.
In the unadjusted time to event analysis, the differences in each outcome, i.e., time to first dose and time to second dose, among different racial and ethnic groups were represented in the Kaplan-Meier (KM) curve and assessed with the log-rank test. Disparities between each racial and ethnic group as compared to White Americans were further assessed with the Cox proportional hazard model and expressed in hazard ratio (HR) and 95% confidence interval (CI). The proportional hazard assumption was checked to ensure the validity of the model results. To assess the racial and ethnic disparities in vaccine uptake with adjustment for time-varying mediators, we adopted the counting process for the Cox proportional hazards model. We created multiple intervals between two adjacent survey dates for each individual until a valid date of vaccination or censoring due to loss to follow-up or end of study, with covariates taken from the earlier survey at the start of each interval. The start date of the first interval was set at December 9, 2020, for all participants. This method resulted in 5968 unique individuals and 34,590 intervals for the time to first dose analysis with time-varying covariates, and 33,743 intervals had complete data, with 3954 events and 88.3% censoring. For the time to second dose analysis with time-varying mediators, the sample included 5995 unique individuals and 39,651 intervals, and 38,727 intervals had complete data, with 3251 events and 91.6% censoring. Survey weights were applied in all the time-to-event analyses. In the main adjusted time-to-event analysis, covariates included social and economic mediators, the sum of chronic health conditions, and psychological influences, as well as the confounders of age and gender. In the sensitivity analysis, individual chronic health conditions replaced the sum of chronic conditions. All time-to-event analysis excluded cases with missing on the covariates or the outcome variables and cases with inappropriate vaccination dates (e.g., vaccination dates prior to the start of the follow-up or the baseline survey, or the first dose date after second dose date). All analyses were done in SAS 9.4.
3. Results
3.1. Distributions of mediators by racial and ethnic group
The mediator distributions by racial and ethnic group at baseline are listed in Table 1 . The baseline sample consisted of 4064 White Americans, 479 Black Americans, 897 Hispanic Americans, 332 Asian Americans and Pacific Islanders, and 296 Others, with weighted percent as 62.6 %, 12.0 %, 16.7%, 5.4%, and 3.3% for each group, respectively. It is shown that Black and Hispanic Americans reported lower education, household income, and trust in the development and approval processes of safe vaccine, and perceived greater COVID risk, compared to other racial and ethnic groups. Black Americans were less likely to be married, or to be working, and reported a greater number of health conditions, compared to the other groups. Asian Americans and Pacific Islanders reported highest education, household income, and trust in the vaccine development and approval processes, and perceived lowest risk from COVID.
Table 1.
Baseline distributions of potential mediators and confounders by race and ethnicity, N = 6078.
| Variables | Class | Total |
Race and Ethnicity |
P-value | |||||
|---|---|---|---|---|---|---|---|---|---|
| White | Black | Hispanic | AAPI | Other | |||||
| Mediators: Social and Economic Conditions |
Married | Yes | 3395 (55.7) | 2494 (60.8) | 147 (31.8) | 435 (55.3) | 175 (59.7) | 144 (41.6) | <0.0001 |
| Education | * | 10.83 (0.04) | 10.82 (0.05) | 10.31 (0.13) | 10.74 (0.13) | 12.11 (0.23) | 11.26 (0.21) | <0.0001 | |
| Household Income | * | 10.88 (0.08) | 11.38 (0.08) | 8.15 (0.26) | 10.76 (0.23) | 11.77 (0.33) | 10.68 (0.45) | <0.0001 | |
| Work Status | Yes | 3385 (56.8) | 2172 (55.0) | 263 (53.5) | 560 (62.6) | 224 (67.8) | 166 (56.7) | 0.0016 | |
| Mediators: Chronic Health Conditions |
Asthma | Yes | 702 (11.9) | 468 (11.6) | 66 (15.7) | 87 (9.3) | 32 (11.8) | 49 (16.8) | 0.0527 |
| Autoimmune Disease | Yes | 379 (5.5) | 295 (6.7) | 26 (4.8) | 34 (3.5) | 7 (1.4) | 17 (3.4) | 0.0027 | |
| Cancer | Yes | 428 (6.0) | 336 (6.9) | 29 (5.9) | 23 (3.3) | 14 (5.2) | 26 (4.3) | 0.0462 | |
| COPD | Yes | 237 (4.1) | 202 (5.3) | 12 (3.2) | 8 (1.2) | 2 (1.1) | 13 (3.2) | 0.0010 | |
| Diabetes | Yes | 738 (12.3) | 482 (11.5) | 84 (16.9) | 106 (13.5) | 21 (6.1) | 45 (14.7) | 0.0087 | |
| Heart Disesase | Yes | 392 (6.2) | 326 (8.0) | 18 (3.5) | 13 (2.1) | 9 (2.5) | 26 (7.7) | <0.0001 | |
| Hypertension | Yes | 1926 (31.0) | 1405 (32.7) | 200 (40.1) | 159 (22.7) | 60 (16.7) | 102 (30.1) | <0.0001 | |
| Kidney Disease | Yes | 163 (2.7) | 114 (2.6) | 24 (3.9) | 12 (2.4) | 3 (0.8) | 10 (4.9) | 0.2051 | |
| Mental Disorders | Yes | 661 (11.1) | 482 (12.9) | 40 (8.6) | 76 (7.3) | 23 (6.0) | 40 (13.7) | 0.0009 | |
| Obesity | Yes | 1070 (16.4) | 723 (16.4) | 92 (18.2) | 168 (17.0) | 22 (6.4) | 65 (23.7) | 0.0036 | |
| Disability | Yes | 509 (9.3) | 346 (9.6) | 75 (16.3) | 49 (5.5) | 4 (2.0) | 35 (9.5) | <0.0001 | |
| Sum of Chronic Conditions | * | 1.14 (0.02) | 1.22 (0.03) | 1.32 (0.08) | 0.85 (0.07) | 0.59 (0.08) | 1.28 (0.15) | <0.0001 | |
| Mediators: Psychological Factors |
Trust 1 | * | 2.48 (0.02) | 2.57 (0.02) | 2.02 (0.05) | 2.38 (0.05) | 2.68 (0.06) | 2.52 (0.09) | <0.0001 |
| Trust 2 | * | 2.30 (0.02) | 2.37 (0.02) | 1.90 (0.05) | 2.23 (0.05) | 2.56 (0.06) | 2.30 (0.09) | <0.0001 | |
| COVID Risk | * | 1.92 (0.04) | 1.79 (0.04) | 2.29 (0.12) | 2.20 (0.11) | 1.66 (0.15) | 1.94 (0.18) | <0.0001 | |
| Discrimination | Yes | 344 (6.0) | 190 (5.3) | 31 (7.4) | 76 (7.4) | 26 (7.1) | 21 (5.1) | 0.3334 | |
| Confounders | Age | * | 48.76 (0.29) | 50.86 (0.36) | 47.40 (0.83) | 43.84 (0.74) | 44.97 (1.44) | 45.31 (1.43) | <0.0001 |
| Gender | F | 3571 (51.7) | 2286 (47.9) | 333 (62.1) | 586 (58.6) | 193 (48.5) | 173 (54.5) | <0.0001 | |
| Total | 6068 (100) | 4064 (62.6) | 479 (12.0) | 897 (16.7) | 332 (5.4) | 296 (3.3) | |||
Note. Except the Hispanic group, all listed racial and ethnic groups are non-Hispanic. *: continuous variables. For continuous variables, each cell shows weighted mean and standard error; for categorical variables, each cell shows raw number and weighted percent. Total in the variable column refers to total sample distribution by race/ethnicity, with raw number and weighted percent for each race or ethnicity. Trust1 refers to trust in the vaccine development process and trust2 refers to trust in vaccine approval process. F refers to female.
3.2. Racial and ethnic disparities in vaccine uptake
3.2.1. Time to first dose
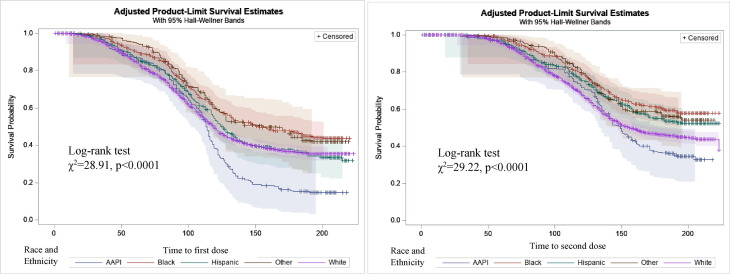
The Kaplan-Meier curves of time to first dose among different racial ethnic groups are shown in the left panel of Fig. 1 . A significant difference among these survival curves was indicated by the log-rank test (χ2 = 28.91, df = 4, p < 0.0001). As shown in Table 2 , the median number of days (95% CIs) to the first dose was 119 (115, 122) for White Americans, 153 (132, 193) for Black Americans, 126 (119, 135) for Hispanic Americans, 113 (108, 117) for Asian Americans and Pacific Islanders, and 156 (118, N/A) for the Other group. Asian Americans and Pacific Islanders were the earliest to get the first dose, followed by White, Hispanic, and Black Americans. The non-adoption rates of the first dose by the end of follow-up was lowest for Asian Americans and Pacific Islanders (15%) followed by Hispanic, White, and Black Americans (32%, 35%, and 44% respectively).
Fig. 1.
Time to first dose (left panel) and time to second dose (right panel) by racial and ethnic group. Note. Except the Hispanic group, all listed racial and ethnic groups are non-Hispanic. AAPI = Asian American and Pacific Islanders.
Table 2.
Hazard ratios (HRs) and 95% confidence intervals (CIs) of time to first dose, median number of days to first dose, and non-adoption rates of the first dose by the end of study by racial and ethnic group, N = 5964.
| Time to 1st dose HR (95% CI) |
Median Number of Days (95% CI) | Non-Adoption Rates (95% CI) | |
|---|---|---|---|
| White Americans | 1 | 119 (115, 122) | 35% (33%, 38%) |
| Black Americans | 0.74 (0.64, 0.87) | 153 (132, 193) | 44% (38%, 50%) |
| Hispanic Americans | 0.96 (0.83, 1.10) | 126 (119, 135) | 32% (24%, 40%) |
| Asian American and Pacific Islanders | 1.45 (1.24, 1.69) | 113 (108, 117) | 15% (9%, 21%) |
| Other | 0.76 (0.60, 0.97) | 156 (118, N/A) | 42% (32%, 52%) |
Note. Except the Hispanic group, all listed racial and ethnic groups are non-Hispanic. HR results should be interpreted with caution, as proportional hazard assumption did not hold (p < 0.0001). N/A = median survival not reached.
Cox proportional hazards model results for time to first dose were reported in Table 2. Black Americans and the Other group were slower in the first-dose uptake as compared to White Americans, with HR (95% CI) as 0.74 (0.64, 0.87) and 0.76 (0.60, 0.97) respectively, whereas Asian Americans and Pacific Islanders were faster, with HR (95% CI) as 1.45 (1.24, 1.69). However, these results should be interpreted with caution, as the proportional hazard assumption was not met.
3.2.2. Time to second dose
The Kaplan-Meier curves of time to second dose by racial and ethnic group are shown in the right panel of Fig. 1. The log-rank test showed a significant difference among these survival curves (χ2 = 29.22, df = 4, p < 0.0001). As shown in Table 3 , the median number of days (95% CI) to the second dose was 156 (149, 166) for White Americans, 149 (137, 161) for Asian Americans and Pacific Islanders, and not reached for Black Americans, Hispanic Americans, and Other. By the end of the study, Asian Americans and Pacific Islanders and White Americans had lower non-adoption rates of the second dose (33% and 38% respectively), compared to Hispanic and Black Americans (52% and 58% respectively).
Table 3.
Hazard ratios (HRs) and 95% confidence intervals (CIs) of time to second dose, median number of days to second dose, and non-adoption rates of the second dose by the end of study by racial and ethnic group, N = 5985.
| Time to 2nd Dose HR (95% CI) | Median Number of Days (95% CI) | Non-Adoption Rates (95% CI) | |
|---|---|---|---|
| White Americans | 1 | 156 (149, 166) | 38% (18%, 58%) |
| Black Americans | 0.65 (0.55, 0.78) | N/A (N/A, N/A) | 58% (52%, 63%) |
| Hispanic Americans | 0.77 (0.65, 0.91) | N/A (171, N/A) | 52% (46%, 58%) |
| Asian American and Pacific Islanders | 1.17 (0.96, 1.42) | 149 (137, 161) | 33% (24%, 41%) |
| Other | 0.71 (0.54, 0.94) | N/A (151, N/A) | 54% (43%, 64%) |
Note. Except the Hispanic group, all listed racial and ethnic groups are non-Hispanic. HR results should be interpreted with caution, as the proportional hazard assumption did not hold (p = 0.0098). N/A = median survival not reached.
The Cox proportional hazards model results shown in Table 3 indicate that Black Americans, Hispanic Americans, and the Other group were slower in the second-dose uptake compared to White Americans, with HRs (95% CIs) as 0.65 (0.55, 0.78), 0.77 (0.65, 0.91), and 0.71 (0.54, 0.94). These results should be interpreted with caution as the proportional hazard assumption was not met.
After confounder adjustment, Black Americans were slower and Asian Americans and Pacific Islanders were faster in their uptake of each dose, compared to White Americans (See Appendix Table 1).
3.3. Vaccine uptake after mediator adjustment
3.3.1. Outcome analysis time to first dose — Time to initiation
The results from the Cox proportional hazards model with potential time-varying mediators are shown in Table 4 . There was no significant difference in time to first dose between each racial and ethnic minority group and White Americans, with HR (95% CI) as 1.07 (0.88, 1.30), 1.15 (0.96, 1.37), 1.08 (0.93, 1.26), and 0.85 (0.65, 1.10) for Asian Americans and Pacific Islanders, Black Americans, Hispanic Americans, and the Other group, as compared to White Americans, respectively. Potential mediators were marital status, education, household income, number of health conditions, trust, and perceived COVID risk. Thus, being married, higher education and income, a greater number of health conditions, greater trust in vaccine development and approval processes, and greater perceived COVID risk all contributed to earlier adoption of the first dose. Note that perceived discrimination was not included as a mediator because it was not associated with race and ethnicity, even though it was associated with time to first dose. The results from the sensitivity analysis (Appendix Table 2) were largely consistent with the main analysis. Being female and older age also contributed to earlier first vaccination.
Table 4.
Proportional hazards model of racial and ethnic disparities in vaccination, with adjustment for mediators and confounders.
| Time to first dose HR (95% CI) |
Time to second dose HR (95% CI) |
||||||
|---|---|---|---|---|---|---|---|
| HR | Lower bound | Upper bound | HR | Lower bound | Upper bound | ||
| Race and Ethnicity (Ref: White) |
AAPI | 1.07 | 0.88 | 1.30 | 0.83 | 0.66 | 1.05 |
| Black | 1.15 | 0.96 | 1.37 | 1.03 | 0.85 | 1.24 | |
| Hispanic | 1.08 | 0.93 | 1.26 | 0.92 | 0.77 | 1.09 | |
| Other | 0.85 | 0.65 | 1.10 | 0.80 | 0.60 | 1.06 | |
| Social and Economic Conditions | Married (ref: No) |
1.14 | 1.03 | 1.26 | 1.21 | 1.08 | 1.36 |
| Education | 1.07 | 1.05 | 1.10 | 1.09 | 1.06 | 1.11 | |
| Household income | 1.05 | 1.03 | 1.07 | 1.04 | 1.02 | 1.05 | |
| Working status (ref: No) |
1.03 | 0.92 | 1.14 | 1.04 | 0.92 | 1.17 | |
| Chronic Health Conditions |
Number of chronic conditions | 1.07 | 1.03 | 1.11 | 1.09 | 1.06 | 1.13 |
| Psychological Factors |
Trust 1 | 1.37 | 1.23 | 1.52 | 1.52 | 1.36 | 1.70 |
| Trust 2 | 1.61 | 1.45 | 1.78 | 1.46 | 1.31 | 1.62 | |
| Perceived risk | 1.05 | 1.02 | 1.08 | 0.99 | 0.96 | 1.02 | |
| Discrimination | 0.73 | 0.56 | 0.94 | 0.98 | 0.74 | 1.30 | |
| Confounders | Gender (Ref: male) |
1.11 | 1.01 | 1.22 | 1.15 | 1.04 | 1.27 |
| Age | 1.02 | 1.02 | 1.03 | 1.02 | 1.02 | 1.03 | |
Note. Except the Hispanic group, all listed racial and ethnic groups are non-Hispanic. AAPI = Asian Americans and Pacific Islanders. HR (95% CI) refers to hazard ratio and its 95% confidence interval. Chronic health conditions include disability, asthma, autoimmune disease, cancer, COPD, diabetes, heart disease, hypertension, kidney disease, mental disorder, and obesity. Trust1 refers to trust in the vaccine development process and trust2 refers to trust in vaccine approval process. Significant results are in bold.
3.3.2. Outcome analysis time to second dose – Time to completion
Also shown in Table 4, the HR (95% CI) of time to second dose derived from the covariate-adjusted Cox proportional hazards model shows no significant difference for each racial and ethnic minority group as compared to White Americans, with HR (95% CI) as 0.83 (0.66, 1.05), 1.03 (0.85, 1.24), 0.92 (0.77, 1.09), and 0.80 (0.60, 1.06) for Asian Americans and Pacific Islanders, Black Americans, Hispanic Americans, and the Other group, as compared to White Americans. Potential mediators included marital status, education, household income, number of health conditions, and trust. Thus, being married, higher education and income, a greater number of health conditions, and greater trust in vaccine development and approval processes all contributed to earlier adoption of the second dose. The sensitivity analysis (Appendix Table 2) generated consistent results. Being female and older age also led to earlier second vaccination.
4. Discussion
In this study, we compared the COVID-19 vaccine uptake timelines up to July 2021 among different racial and ethnic groups and explored potential mediators of racial and ethnic disparities in vaccine uptake. In the unadjusted time-to-event analysis (KM curves), the results are consistent with findings reported in literature, i.e., racial and ethnic minority groups such as Black and Hispanic Americans demonstrated slower uptake of the COVID-19 vaccine compared to White Americans and Asian Americans and Pacific Islanders. The disparities in actual vaccine uptake timelines correspond to vaccine hesitancy levels and trajectories in minoritized groups reported previously. Among all racial and ethnic groups, Black Americans have reported higher COVID-19 vaccine hesitancy in multiple studies [4], [23], [24], [25], [26], [27], [28]. Significant differences in the trajectories of intention to get a COVID-19 vaccine among different racial and ethnic groups existed between April 2020 and January 2021[29]: Asian Americans and Pacific Islanders had the highest intention to get a COVID-19 vaccine at baseline and Black Americans exhibited the lowest intention. Between October 2020 and March 2021, concurrent with COVID vaccine approval and mass distribution of vaccine programs, significant declines in vaccine hesitancy were observed across these groups, with the largest among Black and Hispanic respondents, while public trust in the vaccine increased, with the highest increase reported by Black and Hispanic respondents, although hesitancy was still high among Black respondents [18]. Asian Americans however showed highest vaccine intention among all racial and ethnic groups [25].
In identifying potential mediators of inequitable vaccine uptake, the three domains of mediators were derived from previous research on drivers for vaccine hesitancy, such as perceived risk of infection [30], trust of the government and vaccine developers in the vaccine manufacturing and approval processes[28], side effects of the vaccine, health conditions of the potential receivers [31], and educational attainment and income [17], [18], [25], [26], [32], [33]. In our sample, we assessed racial and ethnic disparities in potential mediators, which may influence vaccine uptake. Black and Hispanic Americans reported lower education and income that may affect vaccine access. Black Americans were less likely to be married and to be working, which may have contributed to no or delayed vaccination due to lack of social support and absence of work-related requirements and exposures. Black and White Americans experienced a higher number of chronic health conditions than other groups, which may have affected their decisions to be vaccinated. Black and Hispanic Americans perceived higher risk of COVID but reported lower trust in the development and approval processes for safe vaccines, consistent with reports that minoritized groups experienced higher morbidity and mortality from COVID-19 but held greater hesitancy and resistance toward the COVID vaccine especially in the early pandemic [17], [18], [34], [35], [36].
In the proportional hazards model after adjusting for potential mediators and confounders, the racial and ethnic disparities in vaccine uptake disappeared. Thus, certain social and economic, clinical, and psychological factors potentially mediated vaccine uptake inequity. Racial and ethnic groups with higher education and household income reported earlier vaccine adoption, consistent with previous research on COVID-19 vaccine intention [17], [18], [25], [26]. Education and income may affect individuals’ knowledge about COVID-19, their assessment of vaccine effectiveness, as well as their access to the vaccine. Being married, a proxy for social support, also positively contributed to quicker vaccine uptake. Previous studies found that social support played a role in people’s intention of COVID-19 vaccination and testing [37]. Accordingly, Black Americans’ slower uptake of the COVID-19 vaccine can be partially explained by their disparities in socioeconomic conditions and marital support. Clinically, US adults with underlying medical conditions were more likely to be vaccinated compared to their healthier counterparts [38]. Individuals with more health conditions may have greater concerns about the complications of COVID-19 infection, thus expediting vaccination to minimize the chance of hospitalization and mortality. Although Black Americans experienced a greater number of health conditions than other groups, which could have shortened their vaccination timeline, gaps in other mediators (e.g., education, income, and trust) slowed down their vaccine uptake.
Trust in vaccine development and approval processes and perceived COVID risk are identified as psychological mediator. Disparities in vaccination timelines among minoritized groups may be mediated through their lower trust in vaccine development and approval processes. Previous research on COVID-19 vaccine uptake intention reported that trusting the safety of the vaccine was a strong predictor of vaccine intention [39], and a lack of trust in the vaccine development and approval processes explained most of the demographic variation in self-reported vaccination likelihood [28]. Black Americans’ lack of trust in the government-sponsored medical interventions has historical origins [40]. Institutionalized medical racism negatively impacts the access and quality of care for Black Americans [29], reducing their chance to receive effective treatments for conditions as leading causes of death. In a study of uptake of the influenza and pneumococcal vaccine, Black Americans were more likely to be vaccinated when their confidence or trust in their physician was higher [41]. The misinformation about COVID-19 and its vaccine disseminated in traditional news media and social media also fueled fear and distrust of the COVID-19 vaccine [31]. As some scholars claimed, the key in ending the pandemic is building trust [28]. Additionally, we found that higher perceived risk of COVID-19 led to earlier uptake of the first dose, but not the second dose. The uptake of the second dose may depend on additional factors related to the first dose, such as experienced adverse events from the first dose, which were not included in our analysis. Nonetheless, part of this finding was consistent with previous reports that perceived risk was positively associated with vaccination intention or acceptance [37], [39], [42]. Although Black and Hispanic Americans perceived higher risk of COVID-19 than other groups, which could have motivated quicker vaccine uptake, their actual uptake was deferred due to disparities in social and economic conditions and lower trust. Therefore healthcare interventions and health communication campaigns that solely target risk perceptions without integrating social and economic dimensions and other psychological influencers can be prone to pitfalls.
Age and gender were considered confounders. As expected, people in older age tended to get the vaccine sooner, due to the nation-wide policy that made the vaccine first available for the older individuals to better protect the vulnerable populations. Women also tended to get the vaccine earlier than men, which offers intervention opportunities addressing gender difference in vaccination.
Previous research shows that access barriers (in the social and economic domain) to the vaccine and structural racism can be deterrents to vaccine uptake, especially in underserved areas and among minoritized groups [31], [43]. For instance, individuals living alone or living in isolated rural areas may experience transportation difficulty traveling to vaccination sites. Those without access to the Internet or lacking skills to navigate the online scheduling platforms may have difficulty making an appointment. Language requirements for understanding guidelines and lack of translation services at clinics may create barriers for immigrants. Decreased access to vaccination has been observed in minoritized, lower-income, or rural communities, as vaccine administration locations were less likely to exist in these areas in the early vaccine rollout process [44], [45]. These access barriers are related to socioeconomic conditions, but are distinct influences on vaccine uptake and should be investigated further.
As some medical scientists have proposed repeated vaccination against COVID-19, future population vaccination patterns may bear resemblance of influenza vaccination [6]. Influenza and pneumococcal disease are major contributors to morbidity and mortality despite widespread availability of effective immunization in the US [41]. Racial and ethnic disparities exist in influenza hospitalizations and mortality rates, yet rates of vaccination among racial and ethnic minority groups continue to be sub-optimal [46], with lower influenza vaccination among Black Americans compared to their White counterparts [15]. These long-term vaccination disparities can be viewed through the lens of three domains of mediators, which can inform future intervention programs.
4.1. Strengths and limitations
Based on a three-domain mediation framework, our study provides empirical data-driven evidence to address disparities in COVID-19 vaccine uptake among at-risk subgroups of the population. Reducing inequities in social and economic conditions and psychological influences creates viable pathways to minimizing disparities in COVID-19 vaccination. Our outcome analysis used time-to-event analysis (KM curve and Cox proportional model) and incorporated the time-varying nature of mediators, especially psychological mediators such as trust and perceived COVID risk, in the proportional hazards model to assess vaccine uptake inequity. Use of an Internet-based national longitudinal panel has some inherent limitations in terms of variable selection and representativeness of the US population. Native Americans have lower vaccination rates than other minoritized groups [2], but they were not identified as a distinct group in our analysis due to a very small sample size. The vaccination dates were self-reported, which may not accurately reflect the actual dates. The mediators representing access barriers were not collected in the survey, thus not incorporated into our analysis. Future studies may explore ways to overcome these limitations.
In conclusion, our study used a mediation framework to explain the racial and ethnic disparities in COVID-19 vaccine uptake with a national longitudinal survey. Studies on racial and ethnic disparities without exploring mediating mechanisms can perpetuate harmful myths and misunderstandings that eventually make health promotion efforts fruitless [47]. Our study will inform health policy makers, public health scientists, and health care practitioners to steer their efforts towards upstream social, economic, and political forces behind racial and ethnic inequality and target the real causes of disparate outcomes.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.vaccine.2023.02.079.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
Data availability
Public Data.
References
- 1.World Health Organization. WHO Coronavirus (COVID-19) Dash Board. Accessed February 13, 2023. https://covid19.who.int/.
- 2.Centers for Disease Control and Prevention. COVID Data Tracker. Accessed February 10, 2023. https://covid.cdc.gov/covid-data-tracker/#new-hospital-admissions.
- 3.Cardona S., Felipe N., Fischer K., Sehgal N.J., Schwartz B.E. Vaccination Disparity: Quantifying Racial Inequity in COVID-19 Vaccine Administration in Maryland. J Urban Health. 2021;1–5 doi: 10.1007/s11524-021-00551-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kricorian K., Turner K. COVID-19 Vaccine Acceptance and Beliefs among Black and Hispanic Americans. PLoS One. 2021;16(8) doi: 10.1371/journal.pone.0256122. e0256122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baker D.W. Breaking links in the chain of racial disparities for COVID-19. JAMA Netw Open. 2021;4(6) doi: 10.1001/jamanetworkopen.2021.12879. e2112879-e2112879. [DOI] [PubMed] [Google Scholar]
- 6.Thompson M.G., Cowling B.J. How repeated influenza vaccination effects might apply to COVID-19 vaccines. Lancet Respir Med. 2022;10(7):636–638. doi: 10.1016/S2213-2600(22)00162-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Anderson R.M., Vegvari C., Truscott J., Collyer B.S. Challenges in creating herd immunity to SARS-CoV-2 infection by mass vaccination. Lancet. 2020;396(10263):1614–1616. doi: 10.1016/S0140-6736(20)32318-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kriss J.L., Hung M.-C., Srivastav A., et al. COVID-19 vaccination coverage, by race and ethnicity—national immunization survey adult COVID module, United States, December 2020–November 2021. Morb Mortal Wkly Rep. 2022;71(23):757. doi: 10.15585/mmwr.mm7123a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Peyvandi S., Baer R.J., Moon-Grady A.J., et al. Socioeconomic mediators of racial and ethnic disparities in congenital heart disease outcomes: a population-based study in California. J Am Heart Assoc. 2018;7(20):e010342. doi: 10.1161/JAHA.118.010342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Luo J., Hendryx M., Wang F. Mortality disparities between Black and White Americans mediated by income and health behaviors. SSM-Population Health. 2022;17 doi: 10.1016/j.ssmph.2021.101019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee H., Andrasfay T., Riley A., Wu Q., Crimmins E. Do social determinants of health explain racial/ethnic disparities in COVID-19 infection? Soc Sci Med. 2022;306 doi: 10.1016/j.socscimed.2022.115098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kawai K., Kawai A.T. Racial/Ethnic and Socioeconomic Disparities in Adult Vaccination Coverage. Am J Prev Med. 2021;61(4):465–473. doi: 10.1016/j.amepre.2021.03.023. [DOI] [PubMed] [Google Scholar]
- 13.Lu P.-j., O’Halloran A., Williams W.W., Lindley M.C., Farrall S., Bridges C.B. Racial and ethnic disparities in vaccination coverage among adult populations in the US. Vaccine. 2015;33:D83–D91. doi: 10.1016/j.vaccine.2015.09.031. [DOI] [PubMed] [Google Scholar]
- 14.Al-Hanawi M.K., Ahmad K., Haque R., Keramat S.A. Willingness to receive COVID-19 vaccination among adults with chronic diseases in the Kingdom of Saudi Arabia. J Infect Public Health. 2021;14(10):1489–1496. doi: 10.1016/j.jiph.2021.08.002. [DOI] [PubMed] [Google Scholar]
- 15.Bazargan M., Wisseh C., Adinkrah E., et al. Influenza vaccination among underserved African-American older adults. Biomed Res Int. 2020;2020 doi: 10.1155/2020/2160894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Freimuth V.S., Jamison A.M., An J., Hancock G.R., Quinn S.C. Determinants of trust in the flu vaccine for African Americans and Whites. Soc Sci Med. 2017;193:70–79. doi: 10.1016/j.socscimed.2017.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Daly M., Robinson E. Willingness to vaccinate against COVID-19 in the US: representative longitudinal evidence from April to October 2020. Am J Prev Med. 2021;60(6):766–773. doi: 10.1016/j.amepre.2021.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Daly M., Jones A., Robinson E. Public Trust and Willingness to Vaccinate Against COVID-19 in the US From October 14, 2020, to March 29, 2021. JAMA. 2021 doi: 10.1001/jama.2021.8246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Momplaisir F, Haynes N, Nkwihoreze H, Nelson M, Werner RM, Jemmott J. Understanding drivers of COVID-19 vaccine hesitancy among Blacks. Clin infect dis: off publ Infect Dis Soc Am. 2021; [DOI] [PMC free article] [PubMed]
- 20.Understanding America Study. Understanding Coronavirus in America. Accessed Feb 3, 2021. https://uasdata.usc.edu/index.php.
- 21.Angrisani M., Kapteyn A., Meijer E., Wah S.H. Sampling and weighting the understanding America study. CESR-Schaeffer Working Paper. 2019:(004). [Google Scholar]
- 22.Understanding America Study. N.D. https://uasdata.usc.edu/index.php?r=eNpLtDKyqi62MrFSKkhMT1WyLrYyslwwskuTcjKT9VLyk0tzU_NKEksy8_NS8svzcvITU0BqgMrzEnPByg3NrJRCHYMVnIrykzNKi1L1ClLSlKxrAQ89HTk.
- 23.Fisher K.A., Bloomstone S.J., Walder J., Crawford S., Fouayzi H., Mazor K.M. Attitudes toward a potential SARS-CoV-2 vaccine: a survey of US adults. Ann Intern Med. 2020;173(12):964–973. doi: 10.7326/M20-3569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kreps S., Prasad S., Brownstein J.S., et al. Factors associated with US adults’ likelihood of accepting COVID-19 vaccination. JAMA Netw Open. 2020;3(10) doi: 10.1001/jamanetworkopen.2020.25594. e2025594-e2025594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Malik A.A., McFadden S.M., Elharake J., Omer S.B. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine. 2020;26 doi: 10.1016/j.eclinm.2020.100495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Szilagyi P.G., Thomas K., Shah M.D., et al. National trends in the US public’s likelihood of getting a COVID-19 vaccine—April 1 to December 8, 2020. JAMA. 2021;325(4):396–398. doi: 10.1001/jama.2020.26419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Willis D.E., Andersen J.A., Bryant-Moore K., et al. COVID-19 vaccine hesitancy: Race/ethnicity, trust, and fear. Clin Transl Sci. 2021 doi: 10.1111/cts.13077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Szilagyi P.G., Thomas K., Shah M.D., et al. The role of trust in the likelihood of receiving a COVID-19 vaccine: Results from a national survey. Prev Med. 2021;153 doi: 10.1016/j.ypmed.2021.106727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Niño M.D., Hearne B.N., Cai T. Trajectories of COVID-19 vaccine intentions among US adults: The role of race and ethnicity. SSM-population health. 2021 doi: 10.1016/j.ssmph.2021.100824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Viswanath K., Bekalu M., Dhawan D., Pinnamaneni R., Lang J., McLoud R. Individual and social determinants of COVID-19 vaccine uptake. BMC Public Health. 2021;21(1):1–10. doi: 10.1186/s12889-021-10862-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hooper M.W., Nápoles A.M., Pérez-Stable E.J. No populations left behind: Vaccine hesitancy and equitable diffusion of effective COVID-19 vaccines. J Gen Intern Med. 2021:1. doi: 10.1007/s11606-021-06698-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Quinn S.C., Jamison A., Freimuth V.S., An J., Hancock G.R., Musa D. Exploring racial influences on flu vaccine attitudes and behavior: Results of a national survey of White and African American adults. Vaccine. 2017;35(8):1167–1174. doi: 10.1016/j.vaccine.2016.12.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shapiro G.K., Tatar O., Dube E., et al. The vaccine hesitancy scale: Psychometric properties and validation. Vaccine. 2018;36(5):660–667. doi: 10.1016/j.vaccine.2017.12.043. [DOI] [PubMed] [Google Scholar]
- 34.Romano S.D., Blackstock A.J., Taylor E.V., et al. Trends in racial and ethnic disparities in COVID-19 hospitalizations, by region—United States, March–December 2020. Morb Mortal Wkly Rep. 2021;70(15):560. doi: 10.15585/mmwr.mm7015e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Song Z., Zhang X., Patterson L.J., Barnes C.L., Haas D.A. American Medical Association; 2021. Racial and ethnic disparities in hospitalization outcomes among Medicare beneficiaries during the COVID-19 pandemic. e214223-e214223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Price-Haywood E.G., Burton J., Fort D., Seoane L. Hospitalization and mortality among black patients and white patients with Covid-19. N Engl J Med. 2020;382(26):2534–2543. doi: 10.1056/NEJMsa2011686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jaspal R., Breakwell G.M. Social support, perceived risk and the likelihood of COVID-19 testing and vaccination: cross-sectional data from the United Kingdom. Curr Psychol. 2022;41(1):492–504. doi: 10.1007/s12144-021-01681-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Havers F.P., Pham H., Taylor C.A., et al. COVID-19-associated hospitalizations among vaccinated and unvaccinated adults 18 years or older in 13 US States, January 2021 to April 2022. JAMA Intern Med. 2022;182(10):1071–1081. doi: 10.1001/jamainternmed.2022.4299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Karlsson L.C., Soveri A., Lewandowsky S., et al. Fearing the disease or the vaccine: The case of COVID-19. Pers Individ Differ. 2021;172 doi: 10.1016/j.paid.2020.110590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Frazier C. It's more than just news: Print media, the tuskegee syphilis study and collective memory among african Americans. J Hist Sociol. 2020;33(3):280–296. [Google Scholar]
- 41.Hughes M.M., Saiyed N.S., Chen T.S. Local-level adult influenza and pneumococcal vaccination disparities: Chicago, Illinois, 2015–2016. Am J Public Health. 2018;108(4):517–523. doi: 10.2105/AJPH.2017.304257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Caserotti M., Girardi P., Rubaltelli E., Tasso A., Lotto L., Gavaruzzi T. Associations of COVID-19 risk perception with vaccine hesitancy over time for Italian residents. Soc Sci Med. 2021;272 doi: 10.1016/j.socscimed.2021.113688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Njoku A., Joseph M., Felix R. Changing the narrative: structural barriers and racial and ethnic inequities in COVID-19 vaccination. Int J Environ Res Public Health. 2021;18(18):9904. doi: 10.3390/ijerph18189904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hernandez I., Dickson S., Tang S., Gabriel N., Berenbrok L.A., Guo J. Disparities in distribution of COVID-19 vaccines across US counties: A geographic information system–based cross-sectional study. PLoS Med. 2022;19(7) doi: 10.1371/journal.pmed.1004069. e1004069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rader B., Astley C.M., Sewalk K., et al. Spatial modeling of vaccine deserts as barriers to controlling SARS-CoV-2. Communications Medicine. 2022;2(1):141. doi: 10.1038/s43856-022-00183-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Webb N.S., Dowd-Arrow B., Taylor M.G., Burdette A.M. Racial/ethnic disparities in influenza vaccination coverage among US adolescents, 2010–2016. Public Health Rep. 2018;133(6):667–676. doi: 10.1177/0033354918805720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chowkwanyun M., Reed A.L., Jr Racial health disparities and Covid-19—caution and context. N Engl J Med. 2020;383(3):201–203. doi: 10.1056/NEJMp2012910. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Public Data.