Abstract
Objective
To describe and synthesise studies of SARS-CoV-2 seroprevalence by occupation prior to the widespread vaccine roll-out.
Methods
We identified studies of occupational seroprevalence from a living systematic review (PROSPERO CRD42020183634). Electronic databases, grey literature and news media were searched for studies published during January–December 2020. Seroprevalence estimates and a free-text description of the occupation were extracted and classified according to the Standard Occupational Classification (SOC) 2010 system using a machine-learning algorithm. Due to heterogeneity, results were synthesised narratively.
Results
We identified 196 studies including 591 940 participants from 38 countries. Most studies (n=162; 83%) were conducted locally versus regionally or nationally. Sample sizes were generally small (median=220 participants per occupation) and 135 studies (69%) were at a high risk of bias. One or more estimates were available for 21/23 major SOC occupation groups, but over half of the estimates identified (n=359/600) were for healthcare-related occupations. ‘Personal Care and Service Occupations’ (median 22% (IQR 9–28%); n=14) had the highest median seroprevalence.
Conclusions
Many seroprevalence studies covering a broad range of occupations were published in the first year of the pandemic. Results suggest considerable differences in seroprevalence between occupations, although few large, high-quality studies were done. Well-designed studies are required to improve our understanding of the occupational risk of SARS-CoV-2 and should be considered as an element of pandemic preparedness for future respiratory pathogens.
Keywords: COVID-19, public health, occupational & industrial medicine
STRENGTHS AND LIMITATIONS OF THIS STUDY.
We conducted a comprehensive search of the COVID-19 seroprevalence literature, including non-English articles, government reports, unpublished data.
Occupations were classified using the Standard Occupational Classification 2010 coding system to improve interpretability and facilitate comparison with other datasets.
Seroprevalence may underestimate the true prevalence of infection because antibody titres decline over time, but where possible we prioritised prevalence estimates for IgG antibodies, which appear to be more robust than other immunoglobulin types.
We did not adjust for differences in serological test performance.
Introduction
Occupation is a social determinant of health and an important risk factor for SARS-CoV-2 infection. Essential workers in health and social care occupations have an increased risk of COVID-19 compared with non-essential workers, but the risks for other occupations are not well defined.1–3 Studies using confirmed COVID-19 cases to examine occupational COVID-19 risk are affected by variable testing rates. For example, testing rates may be higher in workplaces offering testing or paid sick leave, and are impacted by geographic (eg, urban vs rural) and socioeconomic factors (eg, deprivation), potentially biasing results.4–6 Few high-quality, prospective studies using frequent, serial molecular or antigen testing covering a broad range of occupations have been conducted, in part due to the costs and administrative burden of such studies.7 8
Serological testing for SARS-CoV-2 antibodies provides evidence of previous infection and/or vaccination depending on vaccination status and the specific antigens targeted and can be used to obtain more accurate estimates of the cumulative incidence of infection.9 Accurate data on the occupational risks of COVID-19 and other respiratory infections are essential for informing the development of occupational safety guidelines and regulations, transmission control measures and resource allocation (testing, personal protective equipment (PPE), etc). The objectives of this review were to describe and synthesise studies of SARS-CoV-2 seroprevalence across a broad range of occupations globally prior to the widespread roll-out of vaccines.
Methods
We identified seroprevalence studies with sample frames or subgrouping variables related to occupation or employment status from a database compiled via a living systematic review (PROSPERO CRD42020183634). The database has been described previously and includes >1000 cohort and cross-sectional studies reporting antibody testing for SARS-CoV-2 in humans identified from electronic databases, grey literature and news media.10–12 We restricted the current review to studies published during January–December 2020 before vaccines were rolled-out, because differential vaccination rates by occupation may obscure results. We excluded studies that only reported seroprevalence for mixed occupation groups or workplaces (eg, ‘hospital staff’) rather than specific occupations, included children <18 years and that could not be machine-translated using Google Translate if unavailable in English or French (online supplemental file 1).
bmjopen-2022-063771supp001.pdf (193.7KB, pdf)
We extracted study information, sample characteristics, seroprevalence estimates and study-level risk of bias from the living review database. Risk of bias was assessed with a modified Joanna Briggs Institute Checklist for Prevalence Studies by one reviewer and verified independently as described previously. Overall risk of bias was assessed qualitatively based on whether seroprevalence estimates were very likely (corresponding to a low risk of bias), likely (moderate risk) or unlikely (low risk) to be correct for the author’s stated target population (online supplemental file 1).12 13 If multiple estimates were reported, the most recent estimate using laboratory-based methods (eg, ELISA) and anti-spike and/or IgG antibodies were prioritised, because non-IgG and anti-nucleocapsid antibodies may decline more rapidly.14 Free-text descriptions of occupations were extracted from the original studies by one researcher and reviewed by a second.
For each seroprevalence estimate, we identified the relevant Standard Occupational Classification (SOC) 2010 codes by applying the National Institute for Occupational Safety and National Institute for Health Industry and Occupation Computerised Coding System (NIOCCS) to occupation descriptions.15 NIOCCS was chosen, because many studies were conducted in the USA. Coding was manually verified if there was insufficient information for NIOCCS classification, or if the probability of correct classification to the six-digit level was <0.8 based on our review of a subset of the NIOCCS coded data (online supplemental file 1). Anticipating substantial heterogeneity and an insufficient number of estimates relative to covariates for meta-regression, we planned to summarise data using the median/IQR.
Patient and public involvement
It was not possible or appropriate to involve patients or the public in this study.
Results
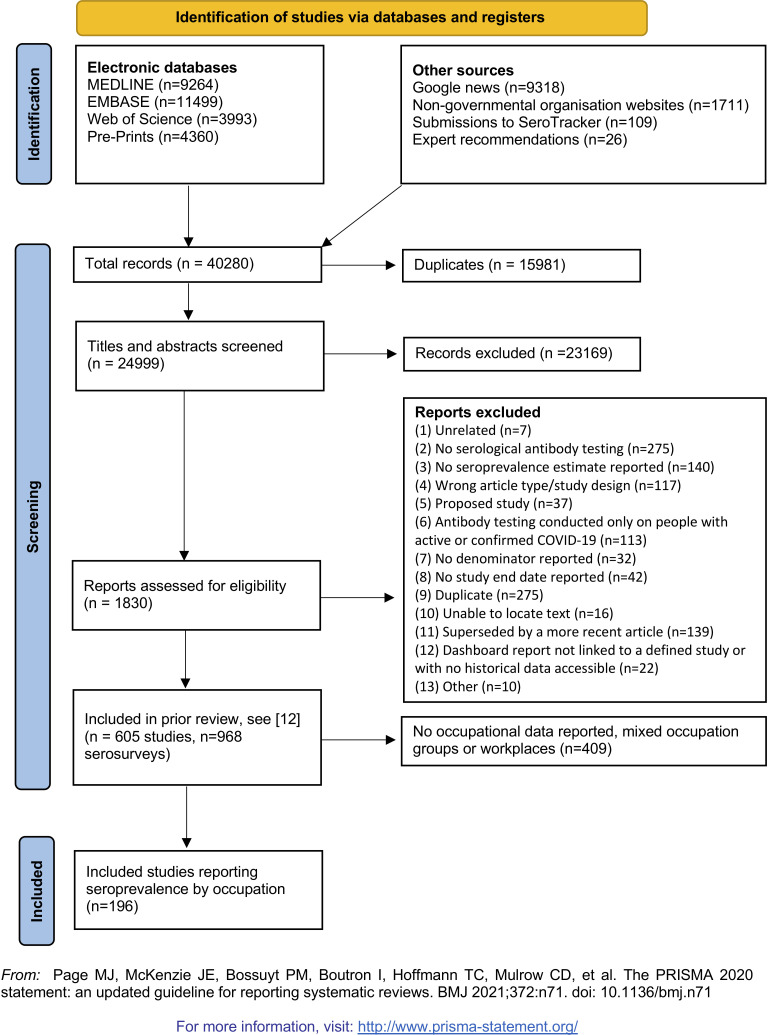
We identified 196 studies of occupational seroprevalence conducted in 2020 during the first and second waves of the pandemic (figure 1). There were 591 940 participants from 38 countries, including the USA (n=44 studies), UK (n=16) and Italy (n=15). Most studies (n=162; 83%) were conducted locally (eg, city, county) as opposed to regionally (eg, state; n=20; 10%) or nationally (n=14; 7%). Most were restricted to one occupational group (n=103), limiting direct comparisons (ie, using the same reference group). Sample sizes were often small (median=220, IQR 64–568 participants). Overall, 135 studies (69%) were at a high risk of bias, 47 moderate (24%), 2 low (1%) and 12 unclear (6%). Common reasons for bias were inadequate statistical analysis (ie, no adjustment for test or sample characteristics; 92%), non-probability sampling (74%) and small sample size (46%).
Figure 1.
PRISMA flow diagram, Page et al.18 PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
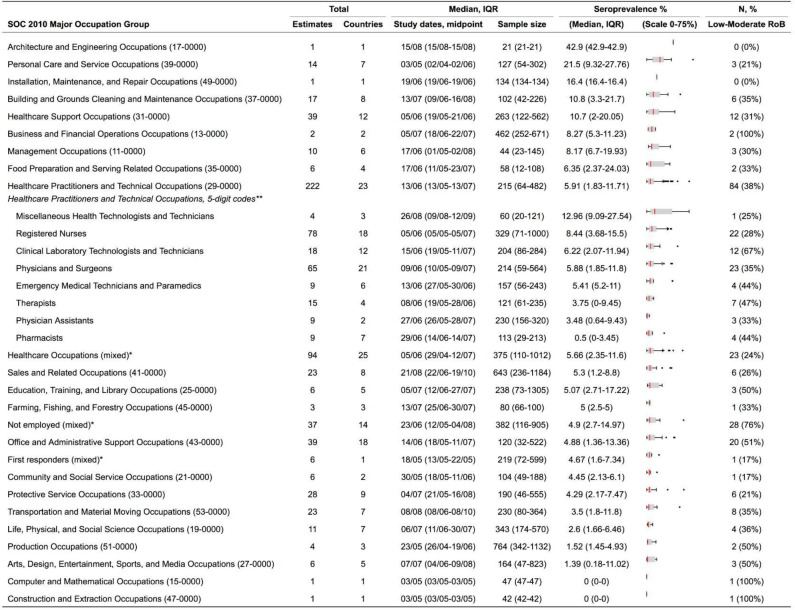
At least one estimate was available for all 23 major SOC occupation groups, except for ‘legal’ and ‘military-specific’ occupations (figure 2; all studies). Over half of the 600 estimates identified (n=359) were for healthcare-related occupations. For SOC groups with three or more estimates, the highest median seroprevalence was reported for ‘personal care and service occupations’ (median 22% (IQR 9%–28%); n=14, eg, ‘personal care aids’). The next highest was reported for ‘building and grounds cleaning and maintenance’ occupations (11% (3%–22%); n=17, for example, ‘maids and housekeeping cleaners’) and ‘healthcare support’ (11% (2%–20%); n=39, eg, ‘nursing assistants’) occupations. The lowest median seroprevalence was 1% (0%–11%; n=6, eg, ‘athletes’) for ‘arts, design, entertainment, sports and media occupations.’ Individual estimates are listed in online supplemental file 2.
Figure 2.
Seroprevalence by SOC 2010 major occupation group. *Estimates are a mix of ‘Healthcare Practitioners and Technical Occupations’ and ‘Healthcare Support Occupations’. SOC, Standard Occupational Classification.
bmjopen-2022-063771supp002.pdf (542.2KB, pdf)
Discussion
This review is the first comprehensive synthesis of occupational COVID-19 seroprevalence studies worldwide. We identified 196 studies representing 21 out of 23 major SOC groups conducted during the first and second waves of the SARS-CoV-2 pandemic in 2020, prior to the widespread roll-out of vaccines, and described occupational groups with high seroprevalence.
Seroprevalence studies may estimate the cumulative incidence of infection more accurately than diagnostic testing studies when access to testing and test performance are poor, and also can identify asymptomatic infections.6 8 The data identified suggest considerable differences in seroprevalence by occupation, though we did not statistically test for differences due to considerable variation in geography, study dates and workplace determinants of infection (eg, PPE, ventilation). ‘Caring and personal service’ occupations had the highest median seroprevalence (22%), which was four times higher than the unemployed (5%) and median seroprevalence across all occupational groups (5%). The UK Office for National Statistics reported a slightly lower cumulative incidence for positive diagnostic or rapid tests for COVID-19 across 25 occupational groups of 4% (mean),4 but the discrepancy between the true cumulative incidence and confirmed infections is likely greater in regions with less access to testing: some national, population-based serosurveys have estimated there are 10–20 serologically identifiable cases per 1 confirmed case.12
In future pandemics, large, well-reported, high-quality seroprevalence studies across a broad range of occupations are needed at an early stage to inform appropriate workplace policy. It has been suggested that 20% of the US workforce was exposed to disease or infection at work at least once a month prior to the pandemic.16 Accurate data on the occupational risks of respiratory infections, including SARS-CoV-2, are needed to inform understanding of transmission, occupational health and safety agency guidelines and allocation of resources (eg, PPE and vaccines) during outbreaks and pandemics. For governments, there are also issues of occupational disease recognition and compensation to be considered.
As such, future population-based studies on respiratory infections should collect data on occupation. In the case of epidemic infection, collaboration between academic centres with the capacity to conduct large-scale studies and government agencies with expertise in disease surveillance and access to workplace data (eg, public health, occupational health and safety) may be beneficial.12 Other authors have suggested the utility of occupational surveillance systems.17 However, the routine completion of the occupation field in electronic health records would also serve this purpose as well as informing patient reported outcome measures.
Strengths and limitations
Despite the large number of studies of occupational seroprevalence conducted, many studies had methodological limitations. Only two studies were at a low risk of bias and most occupational subgroups had small sample sizes (median 220 participants). Many were limited to one major SOC group (n=103 studies), which precluded comparisons. Detailed descriptions of occupations were often lacking, potentially contributing to coding errors and misclassification, and workplace determinants of infection (eg, use of PPE) were poorly reported.
In conclusion, our review shows that a large number of seroprevalence studies covering a broad range of occupations were published in the first year of the pandemic. Results suggest considerable differences in seroprevalence between occupations, although few large, well-reported, high-quality studies were done. Carefully designed, adequately powered seroprevalence studies with coverage of a broad range of occupations could improve our understanding of the occupational risk of SARS-CoV-2 and other respiratory infections and should be considered an element of pandemic preparedness and response.
Supplementary Material
Footnotes
Twitter: @doctorsdilemma, @nikbobrovitz
Collaborators: SeroTracker Consortium: Cheng Matthew P, Donnici Claire, Illincic Natasha, Liu Michael, Papenburg Jesse, Segal Mitchell J, Penny Lucas J, Perlman-Arrow Sara, Rahim Hannah P, Yan Tingting, Yanes-Lane Mercedes.
Contributors: This secondary analysis of the SeroTracker database was conceived by NB, EB, DK and AA. Senior authors on this paper were NB, DK, RA and AA. The protocol was developed by EB, NB and DK. Data cleaning was performed by CC, CD, NataD, SD'M and EB and verification by EB, SD, NathD and GB. Analysis was performed by EB and RA. The first draft of the manuscript was written by EB and revised by EB, RA, NB, NathD, GB, S'M, CC, AA, DK. The SeroTracker Consortium maintained the living systematic review database used in the study. All authors reviewed and agreed to the findings, and also provided critical revisions to the paper. EB accepts full responsibility for the work and/or the conduct of the study, had access to the data, and controlled the decision to publish.
Funding: SeroTracker receives funding for SARS-CoV-2 seroprevalence study evidence synthesis from the Public Health Agency of Canada through Canada’s COVID-19 Immunity Task Force (Grant Number 2021-HQ-000056), the WHO Health Emergencies Programme, the Robert Koch Institute and the Canadian Medical Association Joule Innovation Fund.
Disclaimer: No funding source had any role in the design of this study, its execution, analyses, interpretation of the data, or decision to submit results. This manuscript does not necessarily reflect the views of the WHO or any other funder.
Competing interests: RA was previously a Technical Consultant for the Bill and Melinda Gates Foundation Strategic Investment Fund, is a minority shareholder of Alethea Medical and was a former Senior Policy Advisor at Health Canada. Each of these relationships is unrelated to the present work. JP reports grants to his institution from MedImmune, Sanofi Pasteur, Merck and AbbVie, and personal fees for lectures from AbbVie and Astra-Zeneca, all outside of the submitted work. MPC reports grants from McGill Interdisciplinary Initiative in Infection and Immunity, grants from Canadian Institutes of Health Research, during the conduct of the study; personal fees from GEn1E Lifesciences, personal fees from nplex biosciences, personal fees from Kanvas biosciences, personal fees from AstraZeneca, non-financial support from Cidara therapeutics, non-financial support from Scynexis, non-financial support from Amplyx Pharmaceutics, outside the submitted work. In addition, MPC has a patent for methods detecting tissue damage, graft versus host disease, and infections using cell-free DNA profiling pending, a patent for methods assessing the severity and progression of SARS-CoV-2 infections using cell-free DNA pending, a patent for rapid identification of antimicrobial resistance and other microbial phenotypes using highly multiplexed fluorescence in situ hybridisation pending, and a patent highly multiplexed detection of gene expression with hybridisation chain reaction pending, all outside the submitted work.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Contributor Information
Collaborators: SeroTracker Consortium, Matthew P Cheng, Claire Donnici, Natasha Illincic, Michael Liu, Jesse Papenburg, Mitchell J Segal, Lucas J Penny, Sara Perlman-Arrow, Hannah P Rahim, Tingting Yan, and Mercedes Yanes-Lane
Data availability statement
SeroTracker data are available in a public, open access repository. All data relevant to the study are included in the article or uploaded as online supplemental information. Seroprevalence data can be downloaded (or requested) from https://serotracker.com.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Magnusson K, Nygård K, Methi F, et al. Occupational risk of COVID-19 in the first versus second epidemic wave in Norway, 2020. Euro Surveill 2021;26:2001875. 10.2807/1560-7917.ES.2021.26.40.2001875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mutambudzi M, Niedwiedz C, Macdonald EB, et al. Occupation and risk of severe COVID-19: prospective cohort study of 120 075 UK biobank participants. Occup Environ Med 2020;78:307–14. 10.1136/oemed-2020-106731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nguyen LH, Drew DA, Graham MS, et al. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health 2020;5:e475–83. 10.1016/S2468-2667(20)30164-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Seo E, Mun E, Kim W, et al. Fighting the COVID-19 pandemic: onsite mass workplace testing for COVID-19 in the Republic of Korea. Ann Occup Environ Med 2020;32:e22. 10.35371/aoem.2020.32.e22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tan TQ, Kullar R, Swartz TH, et al. Location matters: geographic disparities and impact of coronavirus disease 2019. J Infect Dis 2020;222:1951–4. 10.1093/infdis/jiaa583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Duarte N, D’Mello S, Duarte NA, et al. Uptake of SARS-cov-2 workplace testing programs, march 2020 to march 2021. Occupational and Environmental Health 21259730. [Preprint]. 10.1101/2021.06.29.21259730 [DOI] [Google Scholar]
- 7.Office for National Statistics . Coronavirus (COVID-19) infection survey: characteristics of people testing positive for COVID-19 in england. 2021. Available: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/articles/coronaviruscovid19infectionsinthecommunityinengland/characteristicsofpeopletestingpositiveforcovid19inengland22february2021
- 8.Pearce N, Rhodes S, Stocking K, et al. Occupational differences in COVID-19 incidence, severity, and mortality in the united kingdom: available data and framework for analyses. Wellcome Open Res 2021;6:102. 10.12688/wellcomeopenres.16729.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Duarte N, Yanes-Lane M, Arora RK, et al. Adapting serosurveys for the SARS-cov-2 vaccine era. Open Forum Infect Dis 2022;9:ofab632. 10.1093/ofid/ofab632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arora RK, Joseph A, Van Wyk J, et al. SeroTracker: a global SARS-cov-2 seroprevalence dashboard. Lancet Infect Dis 2021;21:e75–6. 10.1016/S1473-3099(20)30631-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.SeroTracker Consortium . Data from: our data. 2021. Available: https://serotracker.com/data
- 12.Bobrovitz N, Arora RK, Cao C, et al. Global seroprevalence of SARS-cov-2 antibodies: a systematic review and meta-analysis. PLoS ONE 2021;16:e0252617. 10.1371/journal.pone.0252617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Munn Z, Moola S, Lisy K, et al. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int J Evid Based Healthc 2015;13:147–53. 10.1097/XEB.0000000000000054 [DOI] [PubMed] [Google Scholar]
- 14.Isho B, Abe KT, Zuo M, et al. Persistence of serum and saliva antibody responses to SARS-cov-2 spike antigens in COVID-19 patients. Sci Immunol 2020;5:eabe5511. 10.1126/sciimmunol.abe5511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.NIOSH. NIOSH Industry and Occupation Computerized Coding System (NIOCCS) . U.S. department of health and human services, public health service, centers for disease control and prevention, national institute for occupational safety and health, division of field studies & engineering, health informatics branch. Available: https://csams.cdc.gov/nioccs/About.aspx [Accessed 1 Sep 2021].
- 16.Baker MG, Peckham TK, Seixas NS. Estimating the burden of United States workers exposed to infection or disease: a key factor in containing risk of COVID-19 infection. PLoS ONE 2020;15:e0232452. 10.1371/journal.pone.0232452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marinaccio A, Boccuni F, Rondinone BM, et al. Occupational factors in the COVID-19 pandemic in Italy: compensation claims applications support establishing an occupational surveillance system. Occup Environ Med 2020;77:818–21. 10.1136/oemed-2020-106844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-063771supp001.pdf (193.7KB, pdf)
bmjopen-2022-063771supp002.pdf (542.2KB, pdf)
Data Availability Statement
SeroTracker data are available in a public, open access repository. All data relevant to the study are included in the article or uploaded as online supplemental information. Seroprevalence data can be downloaded (or requested) from https://serotracker.com.