Abstract
Objectives
Knowledge on information needs in cardiac rehabilitation (CR) patients is scarce. This study investigates determinants of information needs in patients with coronary artery disease (CAD).
Design
Prospective observational study.
Participants
A total of 259 patients participated.
Setting
CR centre serving a general hospital in The Netherlands.
Methods
Patients with a coronary event and/or revascularisation referred for CR completed questionnaires assessing their level of information needs with respect to nutrition, physical activity, smoking, medication use and psychological well-being, and potential determinants of information needs (sociodemographic characteristics, health literacy, illness perceptions, anxiety, depression, Type D personality and quality of life).
Results
The majority (63%) of patients indicated a need for information on at least one of the four topics (nutrition, physical activity, medication use, psychological well-being), with considerable inter-individual variation. Female sex, being employed, higher socioeconomic status, higher levels of anxiety and higher illness perception were associated with higher information needs on specific topics.
Conclusions
The majority of CR patients with CAD have a need for information, with considerable inter-individual variability. Several demographic, socioeconomic and psychosocial characteristics were related to their preference for information topics. These results underline the need for personalised information strategies in patients undergoing CR.
Keywords: cardiology, coronary heart disease, rehabilitation medicine, preventive medicine
STRENGTHS AND LIMITATIONS OF THIS STUDY.
The study evaluated a broad range of potential predictors of information needs in patients entering cardiac rehabilitation (CR).
The study was conducted in a large patient cohort representative of the population entering CR in The Netherlands.
Selection bias may have occurred, possibly leading to lower study participation in patients with limited (health) literacy.
In the years after study completion, patients may have become more familiar with acquiring (health) information through digital resources, possibly influencing the interpretation of study results.
Introduction
Multidisciplinary cardiac rehabilitation (CR) reduces morbidity and mortality and increases quality of life in cardiac patients.1 Lifestyle educational interventions have become an integral part of CR,2 and the provision of information about lifestyle and risk factors is an important aspect in reducing the risk of new or recurring cardiovascular disease.3 In general, adequate education can lead to an improvement of self-efficacy, satisfaction and health-promoting behaviours.4 However, information on lifestyle behaviour provided in educational interventions often does not meet the needs of the individual patient.5 Whereas personalised education has been shown to improve medication compliance,6 lifestyle behaviour,7 8 patient satisfaction, mood and perception of disease control,9 information that is not tailored to the individual patient information needs reduces the effectiveness of educational interventions.10
In order to individually tailor lifestyle education programmes in the CR setting, it is crucial to know how sociodemographic, disease characteristics, health literacy and psychological characteristics influence patient information needs. For example, previous research has shown that negative emotions related to cardiac disease and anxiety are associated with higher information needs.11 12 Yet, research on the influence of other psychosocial characteristics, sociodemographic factors, disease characteristics and health literacy on information needs in the CR setting is scarce.
The present study aims to investigate the variability in information needs regarding lifestyle behaviours among patients entering a CR programme after myocardial infarction (MI) or coronary revascularisation, and to evaluate whether sociodemographic characteristics, disease characteristics, psychosocial characteristics and health literacy can be used to predict information needs and information seeking behaviour.
Methods
Design
This study was designed as a prospective observational study in patients who participated in the CR programme at Máxima Medical Center (MMC), Eindhoven, The Netherlands. For the present analyses cross-sectional data were used, collected in consecutive patients prior to the start of CR.
Study sample and data collection
Patients who were eligible for CR for the first time due to a non-ST segment elevation myocardial infarction or ST-segment elevation myocardial infarction and/or percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG) were invited to participate in the study. Exclusion criteria were: insufficient Dutch language skills, heart failure with reduced ejection fraction (ie, left ventricular ejection fraction (LVEF) <40% and New York Heart Association functional class II, III or IV) and recent treatment for psychiatric illness.
Before starting CR (ie, <2 weeks after hospital discharge), all patients were asked to complete questionnaires about information needs and potential determinants of information needs: sociodemographic, health literacy, internet use and psychological characteristics. Disease characteristics were extracted from the electronic patient records.
CR programme
Following the current Dutch CR guideline,13 patients entering outpatient CR were offered an individualised comprehensive multi-disciplinary rehabilitation programme with a typical duration of 6–12 weeks, consisting of one or more group based therapies (education, exercise training, relaxation therapy and lifestyle modification therapy) supplemented by individual counselling when indicated (eg, by a psychologist, dietician). Education in CR is usually organised in four group sessions provided by a cardiologist, a dietician, a psychologist and a sports doctor.14 To personalise the CR programme, participants were counselled to formulate personal lifestyle goals based on the SMART principle (Specific, Measurable, Achievable, Realistic and relevant, and Timed).15 An advanced nurse practitioner monitored each individual patient’s progress, with a final assessment and consultation taking place after 3 months.
Information needs
Information needs regarding the following topics were evaluated: risk behaviour (ie, nutrition, physical activity and smoking), medication use and psychological well-being. For each topic, patients were asked for their preference to receive information (‘yes’ or ‘no’).
Determinants of information needs
Sociodemographic characteristics
The following sociodemographic items were assessed: age, sex, marital status, country of birth, educational level and employment. Regarding educational level, patients were categorised as either ‘not highly educated’ or ‘highly educated’ (highly educated being defined as having completed academic or professional education at the equivalent of a bachelor degree level, or higher).
Health literacy and internet use
Health literacy was evaluated using the Dutch version of the Set of Brief Screening Questions.16 This questionnaire consists of three questions about reading and understanding medical information. Responses were scored on a 5-point Likert scale from 0 to 4.17 To assess patients’ reasons for internet use, a questionnaire was developed for the purposes of this study with seven topics adapted from previously used questionnaires on internet use for health-related information seekings.18 19 Patients were asked whether they had used internet to search for medical information about their own or someone else’s health.
Psychological characteristics
The Hospital Anxiety and Depression Scale20 was used to assess the degree of anxiety and depressive symptoms.21 This scale has good psychometric properties (Cronbach’s alpha=0.89 and 0.83 for the anxiety and depression subscales), is commonly used in clinical settings and has been validated in cardiac populations.22
Because anxiety and depression might change over time, we also assessed stable personality traits relevant to these factors (ie, Type D personality). Type D personality was evaluated using the DS14, a 14-item questionnaire with two subscales: social inhibition and negative affectivity.23
Quality of life was evaluated using the Short Form 36 questionnaire,24 consisting of a generic tool of 36 items grouped into nine health-related aspects of patients’ lives. This scale has good psychometric properties and provides an index of general health-related quality of life,24 with reference values being available for patients with ischaemic heart disease.25
The Brief Illness Perception Questionnaire was used to assess illness perceptions during CR. It consists of eight questions that are scored on a 0–10 response scale. An additional question is placed at the end in which the patient has to name three causal factors related to his heart disease.26
Disease characteristics
We collected data from electronic patient records, including entry diagnosis (primary reason for referral to CR: MI, PCI or CABG), relevant comorbidities (ie, chronic obstructive pulmonary disease, cerebrovascular disease, hypertension, diabetes mellitus, hypercholesterolaemia, peripheral vascular disease) and LVEF. Body weight was measured in kilograms (kg) and used to calculate body mass index (BMI, kg/m2). Based on the international WHO guidelines, BMI was categorised as: normal weight (18.5–24.9 kg/m2), preobesity (25–29.9 kg/m2) and obesity (≥ 30kg/m2).27
Statistical analysis
Patient characteristics are described as frequencies/percentages for categorical variables, and as mean±SD for continuous normally distributed variables (as evaluated by the Shapiro-Wilk test) or median and IQR for non-normally distributed variables. To compare groups, χ2 tests were used for categorical variables, independent sample t-tests for normally distributed continuous variables and Mann-Whitney U tests for non-normally distributed continuous variables. The Phi coefficient was additionally exploited to quantify the strength of the associations between pairs of questionnaire items (ie, information needs).
Multivariable logistic regression analyses with logit link function were performed per topic (ie, nutrition, physical activity, smoking, medication use and psychological well-being) to analyse potentially associated factors for each topic of information needs. Due to the large amount of predictors, we adopted a two-step approach. First, we identified significant predictors for each information need. Explanatory variables with p value ≤0.1 were taken into account in further analyses. Second, these explanatory variables were included in a multivariable model for each topic separately. A backward elimination, based on likelihood ratio test, was used per topic for the selection of the relevant predictors. Variables with p value >0.10 were removed from the model, starting from the least significant effect. The percentage of accuracy in classification was used as a measure of the goodness of fit. The percentage of accuracy was calculated as the proportion of patients for which the predicted response coincided with a negative answer to the questionnaire item (ie, information need). Moreover, the Hosmer-Lemeshow test,28 at a fixed significance level of 0.05, was used as additional measure of goodness-of-fit. Finally, the model was tested with an area under the receiver operating characteristic (AUROC) curve. The statistical analyses were performed using the SPSS software (IBM, V.24.0).
Patient and public involvement
No patients were involved in the study design, conduct, evaluation or dissemination.
Results
Patient characteristics
Table 1 summarises the patient characteristics. A total of 259 patients were included between December 2011 and June 2013. The mean age was 65 years and 76% of the study sample was male. The level of education was high in 19% of participants, 51% were of relatively low socioeconomical status and 82% had a partner/spouse. Among the 259 participants, 58% was diagnosed with MI and 63% was treated with PCI prior to CR. Cardiovascular risk factors were common: 67% of the patients had a BMI >25 kg/m2, 51% had hypertension, 19% had hypercholesterolaemia, 7% had peripheral vascular disease and 12% had diabetes mellitus.
Table 1.
Patient characteristics
| Number of patients, n | 259 |
| Sociodemographic characteristics | |
| Age, mean, SD | 65±10 |
| Sex, n (%) | |
| Male | 198 (76) |
| Female | 61 (24) |
| Relationship status, n (%) | |
| Relationship | 212 (82) |
| No relationship | 47 (18) |
| Children, n (%) | 227 (88) |
| Education, n (%) | |
| Not highly educated | 203 (78) |
| Highly educated* | 50 (19) |
| Employment, n (%) | |
| Employed, working | 46 (18) |
| Employed, not yet returned to work | 71 (27) |
| Unemployed | 133 (51) |
| Ethnic group, n (%) | |
| Northern European descent | 247 (95) |
| Other | 8 (3) |
| Disease characteristics | |
| Diagnosed myocardial infarction, n (%) | 176 (58) |
| Treatment, n (%) | |
| Medication | 22 (9) |
| PCI | 163 (63) |
| CABG | 71 (27) |
| Other† | 2 (1) |
| Medication, n (%) | |
| Beta blockers | 230 (89) |
| ACE inhibitors | 191 (74) |
| Nitrates | 105 (41) |
| Calcium antagonists | 60 (23) |
| LVEF<40%, n (%) | 13 (5) |
| Comorbidities, n (%) | |
| COPD | 19 (7) |
| Cerebrovascular disease | 9 (4) |
| Hypertension | 86 (33) |
| Diabetes mellitus | 32 (12) |
| Hypercholesterolaemia | 49 (19) |
| Peripheral vascular disease | 17 (7) |
| Smoking, n (%) | 19 (7) |
| BMI, med (IQR) kg/m2 | 26 (24–29) |
| BMI categories, n (%) | |
| <25 kg/m2 | 87 (34) |
| 25–30 kg/m2 | 121 (47) |
| >30 kg/m2 | 51 (20) |
| Internet use | |
| Per topic, n (%) | |
| Diet | 76 (29) |
| Physical activity | 97 (38) |
| Smoking | 7 (3) |
| Psychological well-being | 66 (26) |
| Medication | 75 (29) |
| Internet users, n (%) | 108 (42) |
Patient characteristics are described with mean±SD for normally distributed continuous variables (evaluated by the Shapiro-Wilk test); median and IQR for non-normally distributed continuous variables and frequencies with percentages for categorical variables.
*Highly educated represents highest degree level, highest professional education or university.
†Treatment other, a combination of a PCI and CABG or a heart valve replacement.
BMI, body mass index; CABG, coronary artery bypass grafting; COPD, chronic obstructive pulmonary disease; LVEF, left ventricular ejection fraction; PCI, percutaneous coronary intervention.
Of all patients, 108 (42%) used internet to find information about their health and more than half (56%) indicated that they wanted to receive as much information as possible.
Variability of information needs in patients undergoing CR
Figure 1 shows the distribution (histogram) of the amount of information items needed by the interviewed patients: 89 patients (36%) did not need any kind of information, whereas 64% of the respondents indicated a need for further information about at least one of these topics. Only 3% had information needs on all four topics.
Figure 1.
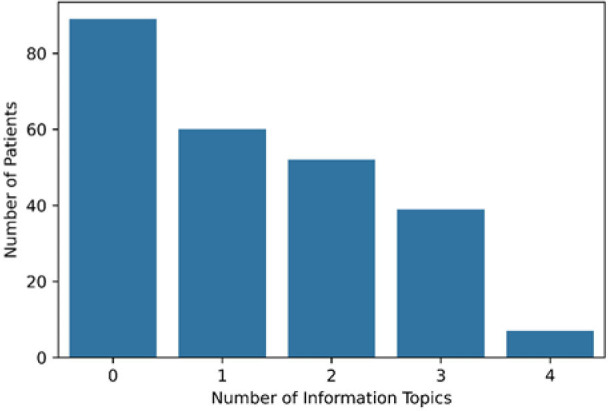
Distribution of the amount of topics on which patients needed information.
Table 2 presents the Phi coefficients associated with the need of smoking information and demonstrates that this item correlates very poorly with the others, that share instead moderate association sizes; that is, patients with information needs about nutrition also had information needs about physical activity and psychological well-being, patients with information needs about physical activity also had more information needs about medication use and nutrition. Patients with information needs on physical activity had the highest information needs with respect to medication.
Table 2.
Phi correlation matrix of the information needs
| Information need | Nutrition | Physical activity | Smoking | Psychological well-being | Medication use |
| Nutrition | 1 | ||||
| Physical activity | 0.31 | 1 | |||
| Smoking | 0.15 | 0.02 | 1 | ||
| Psychological well-being | 0.23 | 0.19 | −0.04 | 1 | |
| Medication use | 0.13 | 0.33 | 0.00 | 0.10 | 1 |
Variables associated with information needs
Tables 3 and 4 show sociodemographic, disease-related and psychosocial characteristics, which are broken down by information needs for different topics of health behaviour. Patients are divided into two groups based on the need (yes/no) for information per topic. For all the topics, the majority of the patients did not need information on that specific subject. Information needs on the topic ‘smoking’ was not included in the regression analysis because of the large number of missing data and the untreatable unbalance between the two subgroups (7 vs 246). For all the topics, we set up each model for predicting the probability of requiring no information about the inspected item.
Table 3.
Sociodemographic and disease characteristics per information topic according to information needs
| Information need | Nutrition | Physical activity | Smoking | Psychological well-being | Medication use | |||||
| Need (n=76) | No need (n=175) | Need (n=97) |
No need (n=156) |
Need (n=7) | No need (n=244) | Need (n=66) | No need (n=186) |
Need (n=75) | No need (n=178) | |
| Age, mean±SD | 64±11 | 65±10 | 63±11 | 66±10 | 62±13 | 65±10 | 61±11 | 66±10 | 63±10 | 65±10 |
| Sex, n (%) | ||||||||||
| Male | 51 (27) | 140 (73) | 76 (39) | 119 (61) | 5 (3) | 189(97) | 41 (21) | 153 (79) | 63 (32) | 131 (68) |
| Female | 25 (42) | 35 (58) | 21 (36) | 37 (64) | 2 (3) | 57 (97) | 25 (43) | 33 (57) | 12 (20) | 47 (80) |
| Education, n (%) | ||||||||||
| Not highly educated | 66 (33) | 133 (67) | 74 (37) | 128(6 3) | 7 (3) | 195 (97) | 49 (24) | 152 (76) | 54 (27) | 147 (73) |
| Highly educated* | 10 (20) | 40 (80) | 23 (46) | 27 (54) | 0 (0) | 49 (100) | 16 (32) | 34 (17) | 21 (42) | 29 (58) |
| Employment, n (%) | ||||||||||
| Employed, working | 11 (25) | 33 (75) | 19 (41) | 27 (59) | 0 (0) | 46 (100) | 14 (30) | 32 (70) | 21 (47) | 24 (53) |
| Employed, not working | 24 (34) | 46 (66) | 33 (46) | 38 (54) | 1 (1) | 70 (99) | 25 (35) | 46 (65) | 22 (31) | 49 (69) |
| Unemployed | 40 (30) | 92 (70) | 44 (34) | 87 (66) | 6 (46) | 125(95) | 26 (20) | 104 (80) | 31 (23) | 101 (77) |
| Relationship/living with partner or spouse, n (%) | 58 (28) | 150 (72) | 81 (38) | 130 (62) | 5 (2) | 205 (98) | 50 (24) | 160 (76) | 66 (31) | 144 (69) |
| Internet users, n (%) | 33 (69) | 72 (41) | 56 (52) | 52 (48) | 1 (1) | 106 (99) | 26 (76) | 82 (24) | 44 (41) | 64 (59) |
| Health literacy, med (IQR) | 10 (9–12) | 11 (10–13) | 11 (9–12) | 11 (9–12) | 10±3 | 11±2 | 10 (8–12) | 11 (10–13) | 11 (10–12) | 11 (9–12) |
| Diagnosed myocardial infarction, n (%) | 53 (31) | 118 (69) | 69 (40) | 103 (60) | 5 (3) | 186 (97) | 50 (29) | 121 (71) | 50 (29) | 122 (71) |
| Treatment, n (%) | ||||||||||
| Medication | 6 (30) | 14 (70) | 8 (38) | 13 (62) | 0 (0) | 21 (100) | 7 (33) | 14 (67) | 4 (19) | 17 (81) |
| PCI | 49 (31) | 109 (69) | 63 (40) | 95 (60) | 6 (4) | 153 (96) | 48 (31) | 109 (69) | 55 (35) | 103 (65) |
| CABG | 21 (30) | 50 (70) | 26 (36) | 4 (64) | 1 (1) | 70 (99) | 11 (15) | 61 (85) | 16 (22) | 56 (78) |
| Comorbidities, n (%) | ||||||||||
| COPD | 6 (33) | 12 (67) | 6 (32) | 13 (68) | 0 (0) | 19 (100) | 7 (37) | 12 (63) | 5 (28) | 13 (72) |
| Cerebrovascular disease | 3 (33) | 6 (67) | 2 (22) | 7 (78) | 0 (0) | 9 (100) | 3 (33) | 6 (67) | 1 (1) | 8 (99) |
| Hypertension | 27 (33) | 56 (67) | 29 (35) | 54 (65) | 1 (1) | 80 (99) | 17 (21) | 65 (79) | 18 (22) | 64 (78) |
| Diabetes mellitus | 11 (35) | 20 (65) | 11 (34) | 21 (66) | 0 (0) | 32 (100) | 8 (25) | 24 (75) | 6 (19) | 26 (81) |
| Hypercholesterolaemia | 15 (32) | 32 (68) | 18 (38) | 29 (62) | 0 (0) | 46 (100) | 11 (24) | 24 (76) | 13 (28) | 34 (72) |
| Peripheral vascular disease | 3 (19) | 13 (81) | 3 (19) | 13 (81) | 0 (0) | 15 (100) | 5 (31) | 11 (69) | 1 (6) | 15 (94) |
| Smoking, n (%) | 4 (21) | 15 (79) | 4 (22) | 14 (88) | 6 (32) | 13 (68) | 6 (33) | 12 (67) | 3 (16) | 16 (84) |
*Highly educated= highest degree level, highest professional education or university.
CABG, coronary artery bypass grafting; COPD, chronic obstructive pulmonary disease; PCI, percutaneous coronary intervention.
Table 4.
Psychosocial characteristics per information topic according to information needs
| Information need | Nutrition | Physical activity | Smoking | Psychological well-being | Medication | |||||
| Need (n=76) | No need (n=175) | Need (n=97) |
No need (n=156) |
Need (n=7) | No need (n=244) | Need (n=66) | No need (n=186) |
Need (n=75) | No need (n=178) | |
| Illness perception | ||||||||||
| Consequences | 8 (7-9) | 7 (5-8) | 7 (6-8) | 7 (5-8) | 7 (5-10) | 7±2 | 8 (7-9) | 7 (5-8) | 7 (5-8) | 7 (5-8) |
| Timeline | 8 (5-10) | 7 (5-10) | 7 (5-9) | 7 (5-10) | 7(5-10) | 8 (6-10) | 8 (6-10) | 7 (5-10) | 8 (5-10) | 8 (5-10) |
| Personal control | 6 (5-8) | 6 (5-7) | 6 (5-7) | 6 (5-7) | 5 (5-6) | 6 (5-7) | 6 (5-7) | 6 (5-7) | 6 (5-8) | 6 (5-7) |
| Treatment control | 8(7-9) | 8 (7-9) | 8 (7-9) | 8 (7-9) | 8 (6-10) | 8±2 | 8 (7-9) | 8 (7-9) | 8 (7-9) | 8 (7-9) |
| Identity | 6 (4-7) | 5 (3-7) | 5 (3-7) | 5 (3-7) | 6 (5-7) | 6 (3-8) | 7 (5-8) | 5 (2-7) | 5 (2-7) | 6 (3-7) |
| Concern | 7 (5-8) | 5 (3-7) | 7 (5-8) | 5(3-8) | 6 (4-7) | 8 (3-9) | 8 (7-9) | 5 (3-7) | 6 (3-8) | 6 (3-8) |
| Comprehensibility | 7 (5-8) | 7 (5-8) | 7 (6-8) | 7 (5-8) | 7 (5-8) | 8 (5-8) | 7 (5-8) | 7±2 | 7 (6-8) | 7 (5-8) |
| Emotion | 5 (3-8) | 4 (2-7) | 5 (3-7) | 5 (2-7) | 5 (2-6) | 7 (3-8) | 8 (7-9) | 3 (2-5) | 4 (2-7) | 5 (2-7) |
| HADS | ||||||||||
| Depression | 3 (1-7) | 3 (1-6) | 3 (1-6) | 3 (1-6) | 4 (3-10) | 5 (3-10) | 5 (3-9) | 2 (1-5) | 2 (1-7) | 4 (1-6) |
| Anxiety | 4 (1-8) | 3 (1-7) | 8 (2-9) | 4 (3-10) | 9 (4-13) | 2 (0–5) | 3 (1-8) | 3 (1-7) | ||
| Subscales Type D | 5 (1-10) | 3 (1-6) | ||||||||
| Negative affectivity | 7 (3-13) | 6 (2-11) | 7 (4-12) | 6 (2-11) | 13 (4-17) | 9 (2-13) | 11±6 | 6 (2-9) | 7 (2-12) | 7 (2-12) |
| Social inhibition | 9 (4-12) | 11 (3-13) | 10 (5-16) | 10±6 | 8 (4-11) | 8 (5-14) | 9 (4-12) | |||
| Quality of Life SF36 | 9 (5-12) | 9 (4-13) | 8 (5-13) | |||||||
| Physical functioning | 55 (35-75) | 75 (50-85) | 70 (45-80) | 70 (40-85) | 75 (48-85) | 62±25 | 60 (35-75) | 75 (45-85) | 70 (50-85) | 70 (45-85) |
| Social role functioning | 62 (38-88) | 75 (50-88) | 63 (50-88) | 75 (50-88) | 64±25 | 67±25 | 50 (38-75) | 75 (63-100) | 63 (50-88) | 63 (50-88) |
| Physical problem | 13 (0–50) | 25 (0–50) | 25 (0–50) | 25 (0–75) | 46±40 | 30±36 | 0 (0–25) | 25 (0–69) | 25 (0–50) | 25 (0–69) |
| Emotional problem | 33 (0–100) | 67 (33-100) | 67 (0–100) | 67 (0–100) | 74 (0–100) | 72 (0–100) | 67 (0–67)] | 100 (33-100) | 67 (0–100) | 67 (0–100) |
| Mental health | 72 (56-84) | 80 (64-88) | 72 (60-88) | 80 (60-88) | 70 (51-77) | 74±25 | 56 (40-76) | 80 (72-91) | 76 (59-92) | 76 (60-88) |
| Vitality | 54±20 | 58±20 | 57±19 | 57±21 | 54±21 | 57±20 | 49±18 | 60 (45-75) | 60±21 | 56±20 |
| Bodily pain | 67 (45-90) | 67(55-90) | 67 (55-90) | 67 (55-90) | 64±22 | 55 (45-78) | 55 (45-84) | 67 (55-90) | 76 (55-88) | 67 (40-70) |
| General health perception | 55±21 | 65 (50-75) | 61±19 | 65 (45-75) | 53±11 | 61±20 | 53±20 | 65 (50-75) | 62±21 | 60 (50-75) |
| Health change | 25 (25-50) | 50 (25-50) | 50 (25-50) | 50 (25-50) | 25±22 | 41±26 | 25 (25-50) | 50 (25-50) | 50 (25-50) | 50 (25-50) |
Data are presented as median (IQR) and mean±SD.
HADS, Hospital Anxiety and Depression Scale; SF36, Short Form 36.
Multivariate analyses examining correlates of information needs
In the multivariable logistic regression analysis, we evaluated which factors were independently associated with information needs. Separate models were examined for each of the topics of information needs nutrition, physical activity, medication use and psychological well-being (smoking was not further analysed in multivariable models because of the small number of patients with current smoking status: n=7 out of 253).
Needs for information about nutrition
Multivariate analysis with backward removal of non-significant covariates showed that out of the 26 variables that displayed a bivariate association with nutrition-related information needs, educational level, ethnicity, subscales of illness perception and quality of life were independently related with information needs regarding nutrition. Specifically, a lower educational level and lower quality of life were associated with a lower need for information. Using this model, the absence of nutrition-related information needs could be predicted in 90.4% of cases with a good model fit and an AUC of the ROC curve of 0.73 (95% CI 0.67 to 0.80) (table 5).
Table 5.
Predictors for information need in the multivariable logistic model after backward elimination
| Topic | Variable | B | SE | Wald stat | P value | OR | 95% CI ratio |
| Nutrition | Education | ||||||
| Highly educated | −1.10 | 0.54 | 4.19 | 0.041 | 0.33 | 0.12 to 0.95 | |
| Not highly educated (ref) | – | – | – | – | – | – | |
| Ethnic group | |||||||
| Other | −2.40 | 1.46 | 2.69 | 0.10* | 0.09 | 0.01 to 1.60 | |
| Dutch (ref) | – | – | – | – | – | – | |
| Illness perception—consequences | 0.22 | 0.09 | 6.69 | 0.010 | 1.25 | 1.06 to 1.48 | |
| Illness perception—treatment control | 0.24 | 0.12 | 4.46 | 0.035 | 1.28 | 1.02 to 1.60 | |
| Illness perception—comprehensibility | −0.20 | 0.09 | 5.17 | 0.023 | 0.82 | 0.69 to 0.97 | |
| Quality of life—general health | −0.02 | 0.01 | 3.90 | 0.048 | 0.98 | 0.97 to 1.00 | |
| Perception | |||||||
| Intercept | 0.63 | 1.80 | 0.14 | 0.726 | 1.87 | ||
| Physical activity | Illness perception concern | 0.10 | 0.05 | 3.22 | 0.073* | 1.11 | 0.99 to 1.24 |
| Internet use | |||||||
| Yes (ref) | – | – | – | – | |||
| No | 0.73 | 0.31 | 5.73 | 0.017 | 2.08 | 1.14 to 3.79 | |
| Intercept | −1.93 | 0.66 | 8.69 | 0.003 | 0.15 | ||
| Psychological well-being | Gender | ||||||
| Male (ref) | – | – | – | – | |||
| Female | 0.96 | 0.53 | 3.23 | 0.072* | 2.61 | 0.92 to 7.41 | |
| Anxiety | 0.27 | 0.09 | 8.76 | 0.003 | 1.31 | 1.10 to 1.57 | |
| Illness perception—identity | −0.31 | 0.13 | 5.36 | 0.021 | 0.73 | 0.56 to 0.95 | |
| Illness perception—emotions | 0.83 | 0.17 | 23.75 | 0.000 | 2.28 | 1.64 to 3.18 | |
| Negative affectivity | −0.13 | 0.06 | 4.41 | 0.036 | 0.88 | 0.78 to 0.99 | |
| Quality of life—bodily pain | −0.3 | 0.01 | 7.78 | 0.005 | 0.97 | 0.95 to 0.99 | |
| Intercept | −2.57 | 1.11 | 5.32 | 0.021 | 0.08 | ||
| Medication | Sum of comorbidities | −0.38 | 0.17 | 4.96 | 0.026 | 0.69 | 0.49 to 0.96 |
| Employed | 7.07 | 0.29 | |||||
| Employed, working | 0.98 | 0.37 | 7.06 | 0.008 | 2.65 | 1.29 to 5.45 | |
| Employed, not yet returned to work | 0.28 | 0.33 | 0.68 | 0.408 | 1.32 | 0.69 to 2.54 | |
| Unemployed (ref) | – | – | – | – | – | – | |
| Intercept | −0.86 | 0.24 | 12.41 | 0.000 | 0.43 |
B denotes the estimated coefficient in the logit scale.
*Not-significant variables (p>0.05) were kept in the model according to the improved prediction accuracy determined by backward elimination.
Needs for information about physical activity
A parallel approach was used to evaluate independent predictors of the need for information regarding physical activity. As shown in table 5, a higher illness perception and no internet use were independently related to a higher need for information on physical activity. Correct prediction of no information need was estimated at 71.7%. The Hosmer and Lemeshow test could not reject the null hypothesis of good fit of the proposed model. The AUC of the ROC curve was 0.61 (95% CI 0.53 to 0.69) (table 5).
Needs for information about psychological well-being
Women were more likely (OR 2.61) to have need for information on psychological well-being than men. Also, higher anxiety levels were associated with higher information needs on psychological well-being. Whereas higher illness perception with regard to ‘physical complaints’ and negative affectivity were associated with lower information needs, higher illness perception in emotional response was associated with a greater need for information. Correct prediction of no information needs was 92.8%. with a good fit for the proposed model and an AUC of the ROC of 0.92 (0.87 to 0.97) (table 5).
Needs for information about medication use
A higher sum of comorbidities was associated with lower information needs on medication. Employed patients were more likely to need information than those who were not employed (OR of 2.65 for employed patients and 1.32 for employed patients not yet returned to work). Correct prediction of no information needs was calculated 94.2% with a good model fit and an AUC of the ROC curve of 0.63 (0.56 to 0.71) (table 5).
Discussion and conclusion
Discussion
This study investigated the variation in and potential determinants of information needs on lifestyle behaviour and medication use in CR patients with coronary artery disease (CAD). We showed that the majority of patients (63%) indicated a need for information on at least one of the topics with considerable inter-individual variation. Demographic, socioeconomic and psychosocial characteristics were related to the preference for specific information topics, underlining the need for personalised education strategies in CR programmes.
In this study, we evaluated patients’ information needs with respect to different topics. Although a minority had information needs on more than one topic, most patients expressed information needs on either nutrition, physical activity, medication use or psychological well-being. Correlation analysis revealed that an overlap in information needs was observed most frequently for the combinations physical activity-medication and physical activity-nutrition. In line with these findings, Drenowatz et al29 also showed an independent association between information needs on nutrition and physical activity. Although research on specific information needs in patients referred for CR is limited, recent studies have analysed general information needs among patients with MI, PCI or CABG.30 31 In accordance with our findings, information needs were generally high with a decline over time, highlighting the need for structuring of educational programmes based on individual and evolving information needs.
Disease characteristics were not associated with information needs in the present study, but several demographic factors were evidently related to information needs. Importantly, we observed that women were more likely to have information needs regarding nutrition and psychological well-being than men. Although the role of sex and gender in medical information needs is largely unexplored, it has been shown previously, in line with our results, that women have higher information needs than men, possibly due to a more proactive attitude and engagement in seeking health-related issues.31 Although the reason for this finding is not well established, an explanation may be that women have a stronger social motive and they often experience greater enjoyment in health-related information searches, explained by social role interpretations.32 Other demographic factors that were indicative for information needs were educational level and employment status, with highly educated and employed patients being more likely to have a need for information on medication. In contrast, Greco et al31 observed lower information needs about pharmacological treatments in patients with CAD. Although the number of participants was comparable to our study, the mean age was lower (57 vs 65 years), fewer people were married (71% vs 82%), people were more often highly educated (51% vs 19%) and mainly employed (58% vs 45%). A possible explanation for the discrepancy with our study may therefore be that these younger participants with a higher education, income and better self-reported general and mental health status, were more active consumers and more likely to seek and use health information themselves than the participants in the present study.33 Although research in the relation between employment/socioeconomic status and information needs on nutrition is scarce, the same explanation may account for higher information needs on nutrition in this specific group. Therefore, we recommend that in addition to sex and gender, educational level and employment status should be taken into account in the design of personalised education programmes.
Our results revealed that several psychosocial characteristics were related to specific information needs. Patients with higher anxiety levels showed higher levels of information needs on psychological well-being. Also, patients with higher scores on Type D personality subscales (negative affectivity and social inhibition), had lower information needs on psychological well-being. It is generally known that Type D personality is associated with poor mental health problems and an unhealthy lifestyle.21 34 35 Other studies also reported the need to include psychosocial factors in the identification of patients at risk for cardiac events.36 The present data suggest that psychological factors are related to the way cardiac patients perceive the need for information and education with regard to cardiovascular risk factors. These factors may be useful in the development of tailored interventions for cardiac patients.24 29 In addition to anxiety and personality traits, we found that health literacy also was an important determinant of information needs. In our study, patients with higher illness perception in several domains (consequences, treatment control, emotions), showed higher information needs. In particular, a strong positive relation was observed between illness perceptions on the emotional domain and information needs on psychological well-being. In conclusion, this study showed that anxiety, illness perception and personality traits are important factors to take into account in the design of education programmes.
Strengths and limitations
This study was one of the first evaluating the influence of sociodemographic factors, health literacy, disease characteristics and psychological characteristics on information needs of patients entering CR. The study was conducted in a large patient cohort that is representative of the population entering CR in The Netherlands, with a mean age of 65 years, the majority of patients being male, and most patients having undergone a cardiac intervention (either PCI or CABG).29 36 37 The relatively large sample size (n=259) is a strength of this study, but selection bias may have occurred since patients with limited (health) literacy may have had more difficulties in completing questionnaires and were therefore less likely to participate in the study. This limitation may have caused an overestimation of health literacy in the present study.
Another limitation is the gap between the period of data collection (2011–2013) and the presentation of study results, which was mainly due to logistical and personnel-related reasons. In the years after data collection, the need for information may have changed because of an increase in patients’ possibilities and skills for gaining (health) information through digital resources, especially after the COVID-19 pandemic. In 2011, 94% of Dutch households already had an internet connection,38 but regular internet use has since increased in the general Dutch population, including people aged 65 years or older,39 which should be considered when interpreting our study results.
Finally, the cross-sectional design of the analysis interferes with causal inferences that can be made. For example, it is possible that people who have a high need for information will become more anxious if such information is not available. Although this ‘reverse pathway’ is less likely for the observed association with personality traits, future longitudinal studies and clinical trials are needed to improve our understanding of the observed associations.
Current and future implications
Based on our results, the development and implementation of personalised—instead of ‘one size fits all’—educational programmes seems essential. It is expected that information needs in general will expand due to an increase in patients’ possibilities and skills to collect (health) information digitally via internet and other sources. In addition, digital solutions, including smartphone applications, smart watches and (wearable) devices (eg, activity/sleep trackers, blood pressure monitors and glucose sensors; whether or not connected to online applications) increasingly dominate the process in which we gain and seek (health) information. Future research should not only aim at increased understanding of differences in information need, but should also evaluate how technological advances can be implemented in health educational programmes, the ultimate goal being to design and implement data-driven personalised education strategies.
Conclusion
We demonstrated that information needs in CR patients are generally high, but vary with respect to specific information topics. Female sex, being employed, higher socioeconomic status, higher levels of anxiety and higher illness perception were associated with higher information needs on specific topics. These results underline the need for personalised information strategies in patients undergoing CR.
Supplementary Material
Footnotes
Contributors: Study conception and design: ST, HK. Acquisition of data: NT, ST. Analysis and interpretation of data: NT, IvA, AB. Drafting the article: NT, IvA, RWMB, AB, HK. Revising the article critically for important intellectual content: ST, RFS, YL, WK. Final approval of the article: NT, IvA, ST, RWMB, RFS, YL, AB, WK, HK. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Guarantor: HK.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
No data are available.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by the Institutional Review Board of Máxima Medical Center (protocol ID 37193.015.11) and all participants provided written informed consent.
References
- 1.Dibben G, Faulkner J, Oldridge N, et al. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev 2021;11:CD001800. 10.1002/14651858.CD001800.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bellmann B, Lin T, Greissinger K, et al. The beneficial effects of cardiac rehabilitation. Cardiol Ther 2020;9:35–44. 10.1007/s40119-020-00164-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zare-Farashbandi F, Lalazaryan A. A review of models and theories of health information seeking behavior. Int J Health Syst Disaster Manage 2014;2:193. 10.4103/2347-9019.144371 [DOI] [Google Scholar]
- 4.Zeguers M, de Haes HCJM, Zandbelt LC, et al. The information needs of new radiotherapy patients: how to measure? do they want to know everything? and if not, why? Int J Radiat Oncol Biol Phys 2012;82:418–24. 10.1016/j.ijrobp.2010.09.032 [DOI] [PubMed] [Google Scholar]
- 5.Shoemaker SJ, Wolf MS, Brach C. Development of the patient education materials assessment tool (pemat): a new measure of understandability and actionability for print and audiovisual patient information. Patient Educ Couns 2014;96:395–403. 10.1016/j.pec.2014.05.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vosbergen S, Mulder-Wiggers JMR, Lacroix JP, et al. Using personas to tailor educational messages to the preferences of coronary heart disease patients. J Biomed Inform 2015;53:100–12. 10.1016/j.jbi.2014.09.004 [DOI] [PubMed] [Google Scholar]
- 7.Shaw A, Ibrahim S, Reid F, et al. Patients’ perspectives of the doctor-patient relationship and information giving across a range of literacy levels. Patient Educ Couns 2009;75:114–20. 10.1016/j.pec.2008.09.026 [DOI] [PubMed] [Google Scholar]
- 8.Hawkins RP, Kreuter M, Resnicow K, et al. Understanding tailoring in communicating about health. Health Educ Res 2008;23:454–66. 10.1093/her/cyn004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kreuter MW, Wray RJ. Tailored and targeted health communication: strategies for enhancing information relevance. Am J Health Behav 2003;27:S227–32. 10.5993/ajhb.27.1.s3.6 [DOI] [PubMed] [Google Scholar]
- 10.Pelle AJ, Schiffer AA, Smith OR, et al. Inadequate consultation behavior modulates the relationship between type D personality and impaired health status in chronic heart failure. Int J Cardiol 2010;142:65–71. 10.1016/j.ijcard.2008.12.086 [DOI] [PubMed] [Google Scholar]
- 11.Beckie TM, Beckstead JW. The effects of a cardiac rehabilitation program tailored for women on global quality of life: a randomized clinical trial. J Womens Health (Larchmt) 2010;19:1977–85. 10.1089/jwh.2010.1937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harrington NG, Noar SM. Reporting standards for studies of tailored interventions. Health Educ Res 2012;27:331–42. 10.1093/her/cyr108 [DOI] [PubMed] [Google Scholar]
- 13.Nederlandse Vereniging Voor Cardiologie (NVVC) . Beslisboom poliklinische indicatiestelling hartrevalidatie 2012. Utrecht: Nederlandse Vereniging voor Cardiologie; 2012. Available: https://www.nvvc.nl/Richtlijnen/Beslisboom%20Hartrevalidatie%202012%20-website-.pdf [Google Scholar]
- 14.Rehabilitation Committee: Netherlands Society for Cardiology (NVVC) and Netherlands Heart Foundation (NHS) . Multidisciplinary guidelines for cardiac rehabilitation (in Dutch). Utrecht: Netherlands Society for Cardiology (NVVC), 2011. Available: https://www.nvvc.nl/Richtlijnen/Multidisciplinaire%20Richtlijn%20Hartrevalidatie%202011%2023052011.pdf [Google Scholar]
- 15.Bovend’Eerdt TJH, Botell RE, Wade DT. Writing smart rehabilitation goals and achieving goal attainment scaling: a practical guide. Clin Rehabil 2009;23:352–61. 10.1177/0269215508101741 [DOI] [PubMed] [Google Scholar]
- 16.Fransen MP, Van Schaik TM, Twickler TB, et al. Applicability of internationally available health literacy measures in the netherlands. J Health Commun 2011;16:134–49. 10.1080/10810730.2011.604383 [DOI] [PubMed] [Google Scholar]
- 17.Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med 2004;36:588–94. [PubMed] [Google Scholar]
- 18.Dumitru RC, Bürkle T, Potapov S, et al. Use and perception of internet for health related purposes in Germany: results of a national survey. Int J Public Health 2007;52:275–85. 10.1007/s00038-007-6067-0 [DOI] [PubMed] [Google Scholar]
- 19.Ybarra ML, Suman M. Help seeking behavior and the Internet: a national survey. Int J Med Inform 2006;75:29–41. 10.1016/j.ijmedinf.2005.07.029 [DOI] [PubMed] [Google Scholar]
- 20.Bjelland I, Dahl AA, Haug TT, et al. The validity of the hospital anxiety and depression scale. J Psychosom Res 2002;52:69–77. 10.1016/S0022-3999(01)00296-3 [DOI] [PubMed] [Google Scholar]
- 21.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361–70. 10.1111/j.1600-0447.1983.tb09716.x [DOI] [PubMed] [Google Scholar]
- 22.Watkins LL, Koch GG, Sherwood A, et al. Association of anxiety and depression with all-cause mortality in individuals with coronary heart disease. J Am Heart Assoc 2013;2:e000068. 10.1161/JAHA.112.000068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Denollet J. DS14: standard assessment of negative affectivity, social inhibition, and type D personality. Psychosom Med 2005;67:89–97. 10.1097/01.psy.0000149256.81953.49 [DOI] [PubMed] [Google Scholar]
- 24.Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. conceptual framework and item selection. Med Care 1992;30:473–83. [PubMed] [Google Scholar]
- 25.Huber A, Oldridge N, Höfer S. International SF-36 reference values in patients with ischemic heart disease. Qual Life Res 2016;25:2787–98. 10.1007/s11136-016-1316-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Broadbent E, Petrie KJ, Main J, et al. The brief illness perception questionnaire. J Psychosom Res 2006;60:631–7. 10.1016/j.jpsychores.2005.10.020 [DOI] [PubMed] [Google Scholar]
- 27.WHO Expert Committee . Physical status: the use and interpretation of anthropometry. 1995. Available: https://pubmed.ncbi.nlm.nih.gov/8594834/ [PubMed]
- 28.Hosmer DW, Hosmer T, Le Cessie S, et al. A comparison of goodness-of-fit tests for the logistic regression model. Statist Med 1997;16:965–80. [DOI] [PubMed] [Google Scholar]
- 29.Drenowatz C, Prasad VK, Hand GA, et al. Effects of moderate and vigorous physical activity on fitness and body composition. J Behav Med 2016;39:624–32. 10.1007/s10865-016-9740-z [DOI] [PubMed] [Google Scholar]
- 30.Tsoulou V, Vasilopoulos G, Kapadohos T, et al. Information needs in percutaneous coronary artery intervention: validation and reliability analysis of NPCI-10 item scale. Cureus 2021;13:e12718. 10.7759/cureus.12718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Greco A, Cappelletti ER, Monzani D, et al. A longitudinal study on the information needs and preferences of patients after an acute coronary syndrome. BMC Fam Pract 2016;17:136. 10.1186/s12875-016-0534-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bidmon S, Terlutter R. Gender differences in searching for health information on the Internet and the virtual patient-physician relationship in Germany: exploratory results on how men and women differ and why. J Med Internet Res 2015;17:e156. 10.2196/jmir.4127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nijman J, Hendriks M, Brabers A, et al. Patient activation and health literacy as predictors of health information use in a general sample of Dutch health care consumers. J Health Commun 2014;19:955–69. 10.1080/10810730.2013.837561 [DOI] [PubMed] [Google Scholar]
- 34.Pedersen SS, Denollet J. Type D personality, cardiac events, and impaired quality of life: a review. Eur J Cardiovasc Prev Rehabil 2003;10:241–8. 10.1097/00149831-200308000-00005 [DOI] [PubMed] [Google Scholar]
- 35.Kupper N, Denollet J. Type D personality as a risk factor in coronary heart disease: a review of current evidence. Curr Cardiol Rep 2018;20:104. 10.1007/s11886-018-1048-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vaartjes I, van Dis I, Visseren FLJ, et al. Hart- en vaatziekten in nederland 2011, cijfers over leefstijl- en risicofactoren, ziekte en sterfte. The Hague: Dutch Heart Foundation, 2011. Available: https://core.ac.uk/reader/29231290 [Google Scholar]
- 37.De Vries H, Van den Broek I, Van Dis I, et al. Hart- en vaatziekten in nederland 2017, cijfers over leefstijl, risicofactoren, ziekte en sterfte. In: Van Dis I, Visseren FLJ, Vaartjes I, et al., eds. Kenmerken van deelnemers aan hartrevalidatieprogramma’s. Den Haag: Hartstichting, 2017. Available: https://docplayer.nl/69393248-Cijfers-over-leefstijl-risicofactoren-ziekte-en-sterfte-hart-en-vaatziekten-in-nederland-2017.html [Google Scholar]
- 38.Centraal Bureau voor Statistiek (CBS) . Home internet access rate highest in the netherlands. n.d. Available: https://www.cbs.nl/en-gb/news/2012/24/home-internet-access-rate-highest-in-the-netherlands
- 39.Centraal Bureau voor Statistiek (CBS) . Internetgebruik van huishoudens en personen. n.d. Available: https://longreads.cbs.nl/ict-kennis-en-economie-2021/internetgebruik-van-huishoudens-en-personen/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No data are available.


