Abstract
Amyotrophic lateral sclerosis (ALS) is a progressive motor neuron disease that affects both upper and lower motor neurons and is fatal in its course. This evidence-based position paper represents the official position of the UEMS PRM Section. The aim of the paper is to define the role of the physical and rehabilitation medicine (PRM) physician and PRM professional practice for people with ALS. A systematic review of the literature and a consensus procedure by means of a Delphi process have been performed involving the delegates of all European countries represented in the UEMS PRM Section. The systematic literature review is reported together with thirty-two recommendations resulting from the Delphi procedure. The responsibility of the PRM physician is functional assessment of persons with ALS and delivering the optimal and most effective PRM program of care. The rehabilitation program of patients with ALS should be delivered and monitored by the multiprofessional team, with the PRM physician as principal coordinator.
Key words: Amyotrophic lateral sclerosis, Rehabilitation, Health planning guidelines
Neuromuscular diseases (NMD) refer to the wide heterogenous group of disorders and pathologies involving: peripheral nerves, anterior horn cells, neuromuscular junction (presynaptic or postsynaptic) and muscles.1 They can affect one or more of these sites leading to a wide group of disabilities. Neuromuscular diseases can be grouped into: acquired and hereditary.
Amyotrophic lateral sclerosis
Amyotrophic lateral sclerosis (ALS) refers to a progressive motor neuron disease that affects both upper and lower motor neurons and is in its course fatal.2 The estimated incidence of ALS is around two in 100,000 individuals per year, while the prevalence is estimated to be around 4.5 in 100,000 individuals.3 The median survival period of patients with the ALS is around 2-4 years from the disease onset, with 5-10% of them surviving beyond 10 years.2 Men are more likely to be affected with such condition.4 ALS affects motor neurons in brain and spinal cord resulting in loss of the motor function5 reducing the independence and quality of life. In a multicenter study it was shown that around 40% of ALS patients, have cognitive changes.6 Moreover, behavioral changes are described as well in these patients.6 Most individuals with diagnosed ALS are sporadic, however, rate of familial forms are pointed to be around 5-10%.7
Diagnosis of ALS is a very delicate, sensitive and challenging task. It is mainly based on clinical criteria that were defined in 1994 and revised in 1998 (El Escorial criteria).8 However, both EL Escorial criteria revised and Lambert criteria were found to be insufficient to secure the diagnosis of ALS particularly in early stages of the disease.9 Thus, Awaji-Shima criteria was introduced in 2008 improving diagnostic sensitivity.9 Given the difficulty of early diagnosis, there is a delay in addressing persons with ALS to rehabilitation services.10 The importance of rehabilitation interventions in ALS patients refers to the fact that they can positively affect the goals management of these patients.10 Therefore, better understanding of ALS etiology, disease course mechanisms along with potential risk factors will help to increase efficacy in delivering early diagnosis along with more effective and optimal management strategies in improving patients overall quality of life.
Physical and rehabilitation medicine (PRM) physicians are trained in postgraduate specialist studies to treat and implement rehabilitation programs for patients with neuromuscular diseases. However, uniformed standards across the Europe haven’t been established so far. The emerging need for optimal, up-to-date and evidence-based treatment of patients with ALS at all levels of medical care is the cornerstone of successful management of challenges arising for patients, their families/caregivers and the society. Therefore, the main goals of the PRM physician along with the multiprofessional team participating in the treatment of these patients should be to preserve and/or improve functioning and the quality of life of the patient, bearing in mind the needs of his family and/or caregivers.
The aim of this paper is to define the role of the physical and rehabilitation medicine (PRM) physician and PRM professional practice for people with ALS.
Methodology
This evidence-based position paper (EBPP) has been developed according to the methodology proposed by the Professional Practice Committee of the Section of Physical and Rehabilitation Medicine of the Union of European Medical Specialists (UEMS-PRM Section).11 It consisted of two parts: “Systematic review of the literature” and “consensus with Delphi procedure among UEMS PRM Section delegates.”
Literature search
The systematic review of the literature was done regarding the professional relevance for PRM physicians as judged by at least two authors of the paper (ML and DN). The search relevant to ALS was conducted using the search terms/strings and included articles extracted from the PubMed/MEDLINE. The main inclusion criteria were the relevance of articles/reviews for the PRM profession. Additionally, we included grey literature for other guidelines that are not published in Journals (online sources), as well as representative articles/reports/position papers in the searched field by major relevant international bodies (e.g. the WHO, the UEMS PRM Section and others). The grey literature was drawn from well-established and reputable organizations in the field of interest for the ALS and rehabilitation practice. The time period of searched articles was between 2006-2019 years. For the ICF classification, the WHO reference from 2001 was cited in recommendations. Our priority in systematic literature search were: Cochrane reviews, systematic reviews, meta-analyses, randomized controlled trials, evidence-based papers and guidelines, however other relevant papers were included as well.
Search strings in PubMed/MEDLINE: amyotrophic lateral sclerosis[All Fields] AND rehabilitation[All Fields] (String 1) #846; amyotrophic lateral sclerosis[All Fields] AND physical therapy[All Fields] (String 2) #303; amyotrophic lateral sclerosis[All Fields] AND exercise[All Fields] (String 3) #230; amyotrophic lateral sclerosis[All Fields] AND electrodiagnostics[All Fields] (String 4) #73; amyotrophic lateral sclerosis[All Fields] AND telemedicine[All Fields] (String 5) #38; amyotrophic lateral sclerosis[All Fields] AND pain[All Fields] (String 6) #336; amyotrophic lateral sclerosis[All Fields] AND spasticity[All Fields] (String 7) #290; amyotrophic lateral sclerosis[All Fields] AND epidemiology[All Fields] AND intervention[All Fields] (String 8) #955.
We also included additional articles in PubMed/MEDLINE from White Book on Physical and Rehabilitation Medicine (PRM) in Europe (#3), ICF (#2) and also grey literature (#3) (Supplementary materials).
The recommendations draft and consensus followed the five-step Delphi procedure (Table I) that was proposed by the Methodology paper.11 Strength of Recommendations (SoR) grading, and Strength of Evidence (SoE) grading was described as well in Methodology paper.11 Overall view of the recommendations was presented in Table II.
Table I. —Results of the consensus procedure.
| Round | N. of recommendations | Accept | Accept with changes | Reject |
|---|---|---|---|---|
| 1 | 30 | 40% | 56.7% | 3.3% |
| 2 | 32* | 25% | 75% | 0% |
| 3 | 32 | 100% | 0% | |
| 4 | 32 | 100% | 0% | |
| 5 | 32 | 100% | 0% |
*One rejected, three added after 1st round.
Table II. —Overall view of the recommendations.
| Content | N. of recommendations | Strength of recommendations | Strength of evidence | ||||||
|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | I | II | III | IV | ||
| Overall general recommendation | 1 | 100% | 0 | 0 | 0 | 0 | 0 | 100% | 0 |
| Recommendations on PRM physician’s role in Medical diagnosis according to ICD | 4 | 50% | 50% | 0 | 0 | 0 | 0 | 0 | 100% |
| Recommendations on PRM physician’s role in PRM diagnosis and assessment according to ICF | 4 | 75% | 25% | 0 | 0 | 0 | 0 | 25% | 75% |
| Recommendations on PRM management and process | 22 | 68.18% | 27.27% | 4.55% | 0 | 0 | 0 | 13.64% | 86.36% |
| Recommendations on future research on PRM professional practice Project definition | 1 | 100% | 0 | 0 | 0 | 100% | 0 | 0 | 0 |
| Total | 32 | 68.75% | 28.12% | 3.13% | 0 | 3.13% | 0 | 15.62% | 81.25% |
Results
Systematic review
The electronic search of the literature identified 3076 papers and three references from grey literature, from which 759 abstracts with three references from grey literature, and finally 77 articles of them as well as three papers from grey literature were considered to produce this paper. The flow chart of the selection process is presented in Figure 1.
Figure 1.
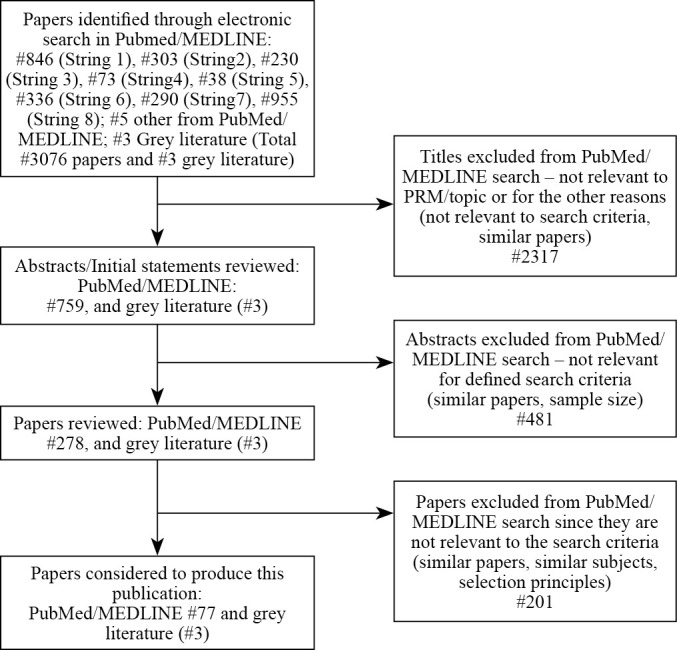
—Flow chart of the study.
The synthesis of literature evidence is presented in Supplementary Digital Material 1 (Supplementary Table I).
Recommendations were prepared according to the chapters proposed in the Methodology paper11 as defined by the Professional Practice Committee of the UEMS-PRM Section:
overall general recommendation;
recommendations on PRM physicians’ role in Medical Diagnosis according to ICD;
recommendations on PRM physicians’ role in PRM diagnosis and assessment according to ICF;
recommendations on PRM management and process;
recommendations on future research about best PRM professional practice in persons with ALS.
Final recommendations
A. Overall general recommendation
1. The professional role of the PRM physician as a part of the multiprofessional (different rehabilitation professions) and/or interdisciplinary medical team for patients with ALS, is to improve optimally (or maintain) functional capacities and health condition, prevent complications, treat existing complications, and enable optimal integration of the individual into the community as well as better quality of life.12-15 The PRM physicians should follow evidence-based interventions and guidelines when planning and creating rehabilitation treatment in patients with ALS [SoR: A; SoE: III].
B. Recommendations on the PRM physician’s role in Medical diagnosis according to ICD
2. It is recommended that PRM physicians make a thorough integration of the assessments and diagnoses made by the neurologist and/or other medical specialists relevant to the individual with ALS in order to supplement these evaluations with PRM functional analyses of capacity and participation and to build the rehabilitation care plan. The PRM role in ALS diagnosis can be to perform and interpret the electromyoneurography (EMNG) findings or this may be done by clinical neurophysiologist [SoR: B; SoE: IV].
3. It is recommended that PRM physicians consider age and severity of illness, taking into account the patient’s advance directives since such dimensions very often influence complex decisions that have to be taken. Some age groups (particularly elderly) have increased multimorbidity and thus higher risks of invasive diagnostic procedures and modified treatment responses16, 17 [SoR: A; SoE: IV].
4. It is recommended that the PRM physician applies treatment modalities (physical medicine and rehabilitation medicine strategies, medication and adjunctive treatments) in patients with ALS according to the presence and the degree of expression of clinical signs and symptoms, bearing in mind patients’ functional boundaries’ with the consent of the patient or caregiver’s18 [SoR: A; SoE: IV].
5. It is recommended that the PRM physician has knowledge to interpret electrodiagnostic tests (electromyoneurography-EMNG) in order to follow disease progression and establish severity degree of neurogenic lesion.19-22 Additionally, it is recommended that PRM physicians gain expertise for such diagnostic method. Alternatively clinical neurophysiologist may provide the testing [SoR: B; SoE: IV].
C. Recommendations on PRM physicians’ role in PRM diagnosis and assessment according to ICF
6. It is recommended that PRM physicians perform a complete physical evaluation of the patients with ALS with particular attention to the identification of all clinical signs and symptoms as well as all functional impairments including: presence and the degree of skeletal muscles including respiratory muscles dysfunction, pain, spasticity, contractures, postural control/balance function, spine deformities, presence of fatigue, dysphagia, communication functions and diet14, 23 [SoR: A; SoE: IV].
7. It is recommended that PRM physicians use the International Classification of Functioning, Disability and Health (ICF) as a framework for information collection regarding activity and participation problems due to the impairment in body structure and function in patients with ALS, according to specific environmental components and taking into account personal factors of these patients.24 Additionally, such tool might be recommended for proposing, planning, and implementing of the optimal rehabilitation treatment [SoR: A; SoE: III].
8. It is recommended that PRM physicians use the ICF Core Sets for neuromuscular diseases for patients with ALS to plan and target PRM interventions25 [SoR: B; SoE: IV].
9. It is recommended that PRM physicians pay particular attention to lifestyle and participation (e.g. environmental factors) of patients with ALS in order to identify barriers and facilitators that could have influence in the involvement in numerous life situations14 [SoR: A; SoE: IV].
D. Recommendations on PRM management and process
Inclusion criteria (e.g. when and why to prescribe PRM interventions)
10. It is recommended that PRM physicians define an optimal and adequate rehabilitation program in close collaboration with the neurologist, internist, gastroenterologist, nutritionist, pneumologist, otolaryngologist, intensivist, and/or other physicians, if needed, within the multidisciplinary and/or interdisciplinary team in every stage of the disease13 [SoR: B; SoE: IV].
11. It is recommended that PRM physicians prescribe PRM interventions whenever it is justified and needed throughout the continuum of care for persons with ALS, thus reducing impairments in body structures and functions, maintaining and/or facilitating individuals’ activities and participation in their environments26, 27 [SoR: A; SoE: IV].
Project definition (definition of the overall aims and strategy of PRM interventions)
12. It is recommended that rehabilitation interventions are provided by a coordinated multiprofessional team. The PRM physician’s role is to: manage and coordinate patient rehabilitation, to plan and monitor proposed PRM programs tailored to the individual’s needs, educate and advise patients, family and/or caregivers, refer ALS patients to the multidisciplinary clinic for health care delivery optimization and prolong survival28-30 [SoR: A; SoE: IV].
13. It is recommended that PRM treatment modalities be implemented over all the phases of the health condition: in acute care settings including intensive care units, in post-acute care settings, in specialized rehabilitation centers, at home or in the community with the main purpose of reducing activity limitations and participation restrictions in specific environments.31-33 Further, it is recommended to implement telemedicine as supplementary tool in multidisciplinary care of patients with ALS34-36 [SoR: B; SoE: IV].
14. It is recommended that PRM physicians participate in discussions, and propose recommendations on policies, interventions and programs, as well as good practice statements to health-policy makers, stakeholders, academic institutions and international organizations in order to meet the needs of persons with ALS37 [SoR: A; SoE: IV].
Team work (professionals involved and specific modalities of team work)
15. It is recommended that rehabilitation for patients with ALS is performed by a multiprofessional expert team working in multi-, inter- or trans-disciplinary way in different rehabilitation settings. The team should include: PRM physicians, neurologists, psychiatrists, internal medicine specialists, pneumologist, otorhinolaryngologist, gastroenterologists, geriatricians, and other medical specialists as well as other rehabilitation professionals: physiotherapists, exercise physiologists, occupational therapists, speech and language therapists, nurses, psychologists, social workers, prosthetists, orthotists, rehabilitation engineers, vocational counsellors, behavioral therapists, and other health professionals: nutritionists and social care services or community-based workers, with mandatory inclusion of family members or caregivers34, 38-41 [SoR: B; SoE: IV].
PRM interventions
16. It is recommended that the PRM physicians adopt adequate and effective communication skills with patients and family members or caregivers and adequately respond to patients’ demands regarding concerns and important information. Furthermore, PRM physicians should take active involvement in continuous medical education in order to adopt adequate theoretical knowledge, evidence based clinical and therapeutic skills (pharmacological therapy and rehabilitation) guidelines for best optimal planning and performing PRM treatment through all stages of rehabilitation in patients with ALS42-44 [SoR: A; SoE: IV].
17. It is recommended that the PRM physician in a multidisciplinary setting be responsible of the prescription, supervise the implementation and follow-up of individually designed exercise programs that can be safely performed without any deterioration of patients with ALS functional outcome45-47 [SoR: A; SoE: III].
18. It is recommended that PRM physicians consider telemedicine assisted and integrated care in patients with ALS48, 49 [SoR: B; SoE: IV].
19. It is recommended that PRM physicians plan and supervise the delivery of specific interventions in respiratory rehabilitation that include: inspiratory muscle training, lung volume recruitment training and manually assisted cough, that are considered as effective for respiratory outcome measures improvement along with increased survival of patients with ALS. Instrumental coughing is advised as mandatory tool in rehabilitation planning as well, if the respiratory muscle controls are too weak50-52 [SoR: A; SoE: III].
20. It is recommended that the PRM physician participates in multidisciplinary treatment and rehabilitation plan for pain symptom in ALS patients including: pharmacological treatment, physical therapy, cognitive behavioral therapy and assistive devices according to the actual evidence23, 53-55 [SoR: A; SoE: III].
21. It is recommended that patients with ALS and dysphagia are provided with adequate periodic dysphagia evaluation (protective and propulsion stages) and nutritional assessment with individually designed dietary regimes and tools56 [SoR: A; SoE: IV].
22. It is recommended that PRM physician participates in a multiprofessional team for ALS patients in the management of dysarthria. The goal is to optimize the intelligibility of speech, focusing as well on communication between people. The management of dysarthria should be individually assessed, planned and evaluated57, 58 [SoR: A; SoE: IV].
23. It is recommended to include active music therapy in improvement of anxiety, depression and quality of life of patients with ALS59 [SoR: C; SoE: IV].
24. It is recommended that patients with ALS participate in home-based exercise program for functional improvement associated with telemedicine if necessary.60 Furthermore, the PRM physicians role is significant in designing, implementing and regularly following every stage of the home based exercise program in order to monitor evolution of the patients’ overall health condition in conjunction with the physiotherapist [SoR: B; SoE: IV].
25. It is recommended that PRM physicians be responsible of prescription and follow-up devices such as: walkers, wheelchairs, transfer devices, adaptive seating and positioning, assistive technology in feeding and ventilation, environment control systems, personal emergency response systems and communication technology for patients with ALS61-63 [SoR: A; SoE: IV].
Outcome criteria
26. It is recommended that PRM physicians decide on the outcome criteria during the assessment and goal-setting processes using physical examination and suitable disability scales (as suggested below) as minimal set of assessments within the ICF framework.25, 64-68
-
ICF-based measure for neuromuscular disease related disabilities:
Neuromuscular Disease Impact Profile (NMDIP);
-
Generic health measures:
SF-36;
World Health Organization WHOQOL-BREF quality of life assessment;
Groningen Activity Restriction Scale (GARS);
Impact on Participation and Autonomy Questionnaire (IPAQ);
-
specific health measures:
Amyotrophic Lateral Sclerosis Functional Rating Scale-revised (ALSFRS-R);
Muscle Cramp Scale (MCS)
[SoR: A; SoE: IV].
27. It is recommended that PRM physicians follow updated consensus statements, guidelines and protocols regarding rehabilitation and management of patients with ALS in order to make evidence-based decision for outcome criteria in this group of patients5, 69, 70 [SoR: A; SoE: IV].
Length/duration/intensity of treatment (overall practical PRM approach)
28. It is recommended that the PRM physician leads and coordinates length, duration and intensity of the rehabilitation treatment within a multidisciplinary setting, taking into consideration specific needs and desired goals, along with the physical and psychological conditions of the patient with ALS71, 72 [SoR: A; SoE: IV].
Discharge criteria (e.g. when and why to end PRM interventions)
29. It is recommended that the multiprofessional rehabilitation team that is led and coordinated by the PRM physician decides on the discharge criteria from inpatient rehabilitation facilities taking into consideration the patients’ physical and psychological conditions and their needs including but not limited to: nursing and medical requirements, rehabilitation goal attainment, home and community settings and family or caregiver situation. Transition to and rehabilitation implementation in palliative care is also important PRM point [SoR: A; SoE: IV].
30. It is recommended that PRM physicians participates in multiprofessional team in advanced care planning as a professional communication process and be familiar with diseases course, common acute care planning decisions as well as end-of-life care for patients with ALS. The goal should be to improve the quality of life both for ALS patients and caregivers and to reduce physical and psychosocial stress73-75 [SoR: A; SoE: IV].
Follow-up criteria and agenda
31. It is recommended that PRM physicians plan and organize the post-discharge follow-up plan on regular basis bearing in mind the patient’s clinical and functional status, thus ensuring the optimal continuity of all aspects of care of patients with ALS [SoR: B; SoE: IV].
E. Recommendations on future research about best PRM professional practice in persons with ALS
32. It is recommended that PRM physicians participate in multidisciplinary projects within systematic research regarding the effects and benefits of certain conservative rehabilitation modalities and interventions in patients with ALS. Better understanding of epidemiology, pathophysiology, risk and prognostic factors as well as survival rates will help in better optimization of rehabilitation resources and more effective short- and long-term treatment planning76-80 [SoR: A; SoE: I].
Conclusions
The responsibility of the PRM physician is functional assessment of persons with ALS and delivering the optimal and most effective PRM program of care that is oriented to the patients, their family and caregivers, and society. The PRM physician should focus on early detection of functional impairments in order to promote patients’ and caregivers’ education so that they timely adapt to functional decline and are collaborative in the adoption of aids for mobility and communication as well as for ventilation and safe feeding. The ultimate goal is to maintain quality of life, trying to avoid pain and suffering in people who exhibit a rapidly progressing motor impairment and have a very short life expectancy. Moreover, the PRM physician, through rehabilitation procedures, should avoid and anticipate complications (dysphagia, nutrition, respiratory, etc.), and support home care. The rehabilitation program of patients with ALS should be delivered and monitored by the multiprofessional team, with the PRM physician as principal coordinator.
This EBPP represents the official position of the UEMS PRM section and describes the professional role of PRM physicians in ALS.
Supplementary Digital Material 1
Supplementary Table I
Evidence synthesis of the literature.
References
- 1.McDonald CM. Clinical approach to the diagnostic evaluation of hereditary and acquired neuromuscular diseases. Phys Med Rehabil Clin N Am 2012;23:495–563. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=22938875&dopt=Abstract 10.1016/j.pmr.2012.06.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chiò A, Logroscino G, Traynor BJ, Collins J, Simeone JC, Goldstein LA, et al. Global epidemiology of amyotrophic lateral sclerosis: a systematic review of the published literature. Neuroepidemiology 2013;41:118–30. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=23860588&dopt=Abstract 10.1159/000351153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Weil C, Zach N, Rishoni S, Shalev V, Chodick G. Epidemiology of Amyotrophic Lateral Sclerosis: A Population-Based Study in Israel. Neuroepidemiology 2016;47:76–81. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27617889&dopt=Abstract 10.1159/000448921 [DOI] [PubMed] [Google Scholar]
- 4.Ilieva H, Maragakis NJ. Motoneuron Disease: clinical. Adv Neurobiol 2017;15:191–210. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=28674982&dopt=Abstract 10.1007/978-3-319-57193-5_7 [DOI] [PubMed] [Google Scholar]
- 5.Janssens AI, Ruytings M, Al-Chalabi A, Chio A, Hardiman O, Mcdermott CJ, et al. ; ALS-CARE Consortium. A mapping review of international guidance on the management and care of amyotrophic lateral sclerosis (ALS). Amyotroph Lateral Scler Frontotemporal Degener 2016;17:325–36. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27078045&dopt=Abstract 10.3109/21678421.2016.1167911 [DOI] [PubMed] [Google Scholar]
- 6.Rabkin J, Goetz R, Murphy JM, Factor-Litvak P, Mitsumoto H, ALS COSMOS Study Group . Cognitive impairment, behavioral impairment, depression, and wish to die in an ALS cohort. Neurology 2016;87:1320–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27496520&dopt=Abstract 10.1212/WNL.0000000000003035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Krewski D, Barakat-Haddad C, Donnan J, Martino R, Pringsheim T, Tremlett H, et al. Determinants of neurological disease: synthesis of systematic reviews. Neurotoxicology 2017;61:266–89. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=28410962&dopt=Abstract 10.1016/j.neuro.2017.04.002 [DOI] [PubMed] [Google Scholar]
- 8.Soofi AY, Bello-Haas VD, Kho ME, Letts L. The impact of rehabilitative interventions on quality of life: a qualitative evidence synthesis of personal experiences of individuals with amyotrophic lateral sclerosis. Qual Life Res 2018;27:845–56. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29204783&dopt=Abstract 10.1007/s11136-017-1754-7 [DOI] [PubMed] [Google Scholar]
- 9.Orsini M, Oliveira AB, Nascimento OJ, Reis CH, Leite MA, de Souza JA, et al. Amyotrophic Lateral Sclerosis: New Perpectives and Update. Neurol Int 2015;7:5885. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=26487927&dopt=Abstract 10.4081/ni.2015.5885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Corcia P, Meininger V. Management of amyotrophic lateral sclerosis. Drugs 2008;68:1037–48. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=18484797&dopt=Abstract 10.2165/00003495-200868080-00003 [DOI] [PubMed] [Google Scholar]
- 11.Negrini S, Kiekens C, Zampolini M, Wever D, Varela Donoso E, Christodoulou N. Methodology of “Physical and Rehabilitation Medicine practice, Evidence Based Position Papers: the European position” produced by the UEMS-PRM Section. Eur J Phys Rehabil Med 2016;52:134–41. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=26681647&dopt=Abstract [PubMed] [Google Scholar]
- 12.Simmons Z. Rehabilitation of motor neuron disease. Handb Clin Neurol 2013;110:483–98. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=23312666&dopt=Abstract 10.1016/B978-0-444-52901-5.00041-1 [DOI] [PubMed] [Google Scholar]
- 13.Majmudar S, Wu J, Paganoni S. Rehabilitation in amyotrophic lateral sclerosis: why it matters. Muscle Nerve 2014;50:4–13. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=24510737&dopt=Abstract 10.1002/mus.24202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Andersen PM, Abrahams S, Borasio GD, de Carvalho M, Chio A, Van Damme P, et al. EFNS Task Force on Diagnosis and Management of Amyotrophic Lateral Sclerosis . EFNS guidelines on the clinical management of amyotrophic lateral sclerosis (MALS)—revised report of an EFNS task force. Eur J Neurol 2012;19:360–75. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=21914052&dopt=Abstract 10.1111/j.1468-1331.2011.03501.x [DOI] [PubMed] [Google Scholar]
- 15.Hulisz D. Amyotrophic lateral sclerosis: disease state overview. Am J Manag Care 2018;24(Suppl):S320–6. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30207670&dopt=Abstract [PubMed] [Google Scholar]
- 16.Mandrioli J, Ferri L, Fasano A, Zucchi E, Fini N, Moglia C, et al. Cardiovascular diseases may play a negative role in the prognosis of amyotrophic lateral sclerosis. Eur J Neurol 2018;25:861–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29512869&dopt=Abstract 10.1111/ene.13620 [DOI] [PubMed] [Google Scholar]
- 17.Sathasivam S. Managing patients with amyotrophic lateral sclerosis. Eur J Intern Med 2009;20:355–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=19524172&dopt=Abstract 10.1016/j.ejim.2008.09.002 [DOI] [PubMed] [Google Scholar]
- 18.Paganoni S, Karam C, Joyce N, Bedlack R, Carter GT. Comprehensive rehabilitative care across the spectrum of amyotrophic lateral sclerosis. NeuroRehabilitation 2015;37:53–68. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=26409693&dopt=Abstract 10.3233/NRE-151240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Howard IM, Rad N. Electrodiagnostic Testing for the Diagnosis and Management of Amyotrophic Lateral Sclerosis. Phys Med Rehabil Clin N Am 2018;29:669–80. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30293622&dopt=Abstract 10.1016/j.pmr.2018.06.003 [DOI] [PubMed] [Google Scholar]
- 20.American Association of Neuromuscular and Electrodiagnostic Medicine. Who is qualified to practice electrodiagnostic medicine? 2012 [Internet]. Available from: https://www.aanem.org/getmedia/1e53beb2-987d-4f06-b091-ebe56148a8b9/Who-is-Qualifed-to-Practice-EDX-2012.pdf [cited 2021, Nov 18].
- 21.Joyce NC, Carter GT. Electrodiagnosis in persons with amyotrophic lateral sclerosis. PM R 2013;5(Suppl):S89–95. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=23523708&dopt=Abstract 10.1016/j.pmrj.2013.03.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.de Carvalho M, Dengler R, Eisen A, England JD, Kaji R, Kimura J, et al. Electrodiagnostic criteria for diagnosis of ALS. Clin Neurophysiol 2008;119:497–503. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=18164242&dopt=Abstract 10.1016/j.clinph.2007.09.143 [DOI] [PubMed] [Google Scholar]
- 23.Bartolo M, Chiò A, Ferrari S, Tassorelli C, Tamburin S, Avenali M, et al. Italian Consensus Conference on Pain in Neurorehabilitation (ICCPN) . Assessing and treating pain in movement disorders, amyotrophic lateral sclerosis, severe acquired brain injury, disorders of consciousness, dementia, oncology and neuroinfectivology. Evidence and recommendations from the Italian Consensus Conference on Pain in Neurorehabilitation. Eur J Phys Rehabil Med 2016;52:841–54. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27579582&dopt=Abstract [PubMed] [Google Scholar]
- 24.Organization WH. International Classification of Functioning, Disability and Health: ICF. World Health Organization; 2001. [Google Scholar]
- 25.Bos I, Stallinga HA, Middel B, Kuks JB, Wynia K. Validation of the ICF core set for neuromuscular diseases. Eur J Phys Rehabil Med 2013;49:179–87. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=23172408&dopt=Abstract [PubMed] [Google Scholar]
- 26.Lui AJ, Byl NN. A systematic review of the effect of moderate intensity exercise on function and disease progression in amyotrophic lateral sclerosis. J Neurol Phys Ther 2009;33:68–87. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=19556916&dopt=Abstract 10.1097/NPT.0b013e31819912d0 [DOI] [PubMed] [Google Scholar]
- 27.Chen A, Montes J, Mitsumoto H. The role of exercise in amyotrophic lateral sclerosis. Phys Med Rehabil Clin N Am 2008;19:545–57, ix–x. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=18625415&dopt=Abstract 10.1016/j.pmr.2008.02.003 [DOI] [PubMed] [Google Scholar]
- 28.Bello-Haas VD. Physical therapy for individuals with amyotrophic lateral sclerosis: current insights. Degener Neurol Neuromuscul Dis 2018;8:45–54. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30890895&dopt=Abstract 10.2147/DNND.S146949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Howard I, Potts A. Interprofessional Care for Neuromuscular Disease. Curr Treat Options Neurol 2019;21:35. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=31264031&dopt=Abstract 10.1007/s11940-019-0576-z [DOI] [PubMed] [Google Scholar]
- 30.Shoesmith CL, Strong MJ. Amyotrophic lateral sclerosis: update for family physicians. Can Fam Physician 2006;52:1563–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=17279237&dopt=Abstract [PMC free article] [PubMed] [Google Scholar]
- 31.Soriani MH, Desnuelle C. Care management in amyotrophic lateral sclerosis. Rev Neurol (Paris) 2017;173:288–99. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=28461024&dopt=Abstract 10.1016/j.neurol.2017.03.031 [DOI] [PubMed] [Google Scholar]
- 32.Kitano K, Asakawa T, Kamide N, Yorimoto K, Yoneda M, Kikuchi Y, et al. Effectiveness of Home-Based Exercises Without Supervision by Physical Therapists for Patients With Early-Stage Amyotrophic Lateral Sclerosis: A Pilot Study. Arch Phys Med Rehabil 2018;99:2114–7. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29608902&dopt=Abstract 10.1016/j.apmr.2018.02.015 [DOI] [PubMed] [Google Scholar]
- 33.Bach JR. Noninvasive Respiratory Management of Patients With Neuromuscular Disease. Ann Rehabil Med 2017;41:519–38. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=28971036&dopt=Abstract 10.5535/arm.2017.41.4.519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Van De Rijn M, Paganoni S, Levine-Weinberg M, Campbell K, Swartz Ellrodt A, Estrada J, et al. Experience with telemedicine in a multi-disciplinary ALS clinic. Amyotroph Lateral Scler Frontotemporal Degener 2018;19:143–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29250986&dopt=Abstract 10.1080/21678421.2017.1392577 [DOI] [PubMed] [Google Scholar]
- 35.Section of Physical and Rehabilitation Medicine Union Européenne des Médecins Spécialistes (UEMS) European Board of Physical and Rehabilitation Medicine . Académie Européenne de Médecine de Réadaptation; European Society for Physical and Rehabilitation Medicine. White book on physical and rehabilitation medicine in Europe. Eura Medicophys 2006;42:292–332. [PubMed] [Google Scholar]
- 36.Galea MD. Telemedicine in Rehabilitation. Phys Med Rehabil Clin N Am 2019;30:473–83. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30954160&dopt=Abstract 10.1016/j.pmr.2018.12.002 [DOI] [PubMed] [Google Scholar]
- 37.Rehabilitation in Health Systems. Geneva: World Health Organization; 2017. License: CC BY-NC-SA 3.0 IGO. https://apps.who.int/iris/bitstream/handle/10665/254506/9789241549974-eng.pdf?sequence=8&isAllowed=y
- 38.Güell MR, Antón A, Rojas-García R, Puy C, Pradas J; en representación de todo el grupo interdisciplinario. Comprehensive care of amyotrophic lateral sclerosis patients: a care model. Arch Bronconeumol 2013;49:529–33. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=23540596&dopt=Abstract https://doi.org/ 10.1016/j.arbr.2013.09.011 [DOI] [PubMed] [Google Scholar]
- 39.Budinčević H, Marčinko Budinčević A, Kos M, Vlašić S, Bartolović J, Benko S, et al. [Multidisciplinary Management and Neurorehabilitation of Patients with Amyotrophic Lateral Sclerosis]. Acta Med Croatica 2016;70:111–6. Croatian. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=28722839&dopt=Abstract [PubMed] [Google Scholar]
- 40.Lewis M, Rushanan S. The role of physical therapy and occupational therapy in the treatment of amyotrophic lateral sclerosis. NeuroRehabilitation 2007;22:451–61. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=18198431&dopt=Abstract 10.3233/NRE-2007-22608 [DOI] [PubMed] [Google Scholar]
- 41.Mayadev AS, Weiss MD, Distad BJ, Krivickas LS, Carter GT. The amyotrophic lateral sclerosis center: a model of multidisciplinary management. Phys Med Rehabil Clin N Am 2008;19:619–31, xi. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=18625420&dopt=Abstract 10.1016/j.pmr.2008.04.004 [DOI] [PubMed] [Google Scholar]
- 42.European Physical and Rehabilitation Medicine Bodies Alliance . White Book on Physical and Rehabilitation Medicine (PRM) in Europe. Chapter 1. Definitions and concepts of PRM. Eur J Phys Rehabil Med 2018;54:156–65. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29565102&dopt=Abstract [DOI] [PubMed] [Google Scholar]
- 43.European Physical and Rehabilitation Medicine Bodies Alliance . White Book on Physical and Rehabilitation Medicine (PRM) in Europe. Chapter 6. Knowledge and skills of PRM physicians. Eur J Phys Rehabil Med 2018;54:214–29. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29565107&dopt=Abstract [DOI] [PubMed] [Google Scholar]
- 44.de Wit J, Bakker LA, van Groenestijn AC, van den Berg LH, Schröder CD, Visser-Meily JM, et al. Caregiver burden in amyotrophic lateral sclerosis: A systematic review. Palliat Med 2018;32:231–45. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=28671483&dopt=Abstract 10.1177/0269216317709965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Clawson LL, Cudkowicz M, Krivickas L, Brooks BR, Sanjak M, Allred P, et al. ; neals consortium. A randomized controlled trial of resistance and endurance exercise in amyotrophic lateral sclerosis. Amyotroph Lateral Scler Frontotemporal Degener 2018;19:250–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29191052&dopt=Abstract 10.1080/21678421.2017.1404108 [DOI] [PubMed] [Google Scholar]
- 46.Lunetta C, Lizio A, Sansone VA, Cellotto NM, Maestri E, Bettinelli M, et al. Strictly monitored exercise programs reduce motor deterioration in ALS: preliminary results of a randomized controlled trial. J Neurol 2016;263:52–60. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=26477027&dopt=Abstract 10.1007/s00415-015-7924-z [DOI] [PubMed] [Google Scholar]
- 47.Lisle S, Tennison M. Amyotrophic lateral sclerosis: the role of exercise. Curr Sports Med Rep 2015;14:45–6. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=25574882&dopt=Abstract 10.1249/JSR.0000000000000122 [DOI] [PubMed] [Google Scholar]
- 48.Vitacca M, Comini L, Tentorio M, Assoni G, Trainini D, Fiorenza D, et al. A pilot trial of telemedicine-assisted, integrated care for patients with advanced amyotrophic lateral sclerosis and their caregivers. J Telemed Telecare 2010;16:83–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=20139136&dopt=Abstract 10.1258/jtt.2009.090604 [DOI] [PubMed] [Google Scholar]
- 49.Tenforde AS, Hefner JE, Kodish-Wachs JE, Iaccarino MA, Paganoni S. Telehealth in Physical Medicine and Rehabilitation: A Narrative Review. PM R 2017;9(5S):S51–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=28527504&dopt=Abstract 10.1016/j.pmrj.2017.02.013 [DOI] [PubMed] [Google Scholar]
- 50.Macpherson CE, Bassile CC. Pulmonary Physical Therapy Techniques to Enhance Survival in Amyotrophic Lateral Sclerosis: A Systematic Review. J Neurol Phys Ther 2016;40:165–75. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27164308&dopt=Abstract 10.1097/NPT.0000000000000136 [DOI] [PubMed] [Google Scholar]
- 51.Ferreira GD, Costa AC, Plentz RD, Coronel CC, Sbruzzi G. Respiratory training improved ventilatory function and respiratory muscle strength in patients with multiple sclerosis and lateral amyotrophic sclerosis: systematic review and meta-analysis. Physiotherapy 2016;102:221–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27026167&dopt=Abstract 10.1016/j.physio.2016.01.002 [DOI] [PubMed] [Google Scholar]
- 52.Plowman EK, Tabor-Gray L, Rosado KM, Vasilopoulos T, Robison R, Chapin JL, et al. Impact of expiratory strength training in amyotrophic lateral sclerosis: results of a randomized, sham-controlled trial. Muscle Nerve 2019;59:40–6. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29981250&dopt=Abstract 10.1002/mus.26292 [DOI] [PubMed] [Google Scholar]
- 53.Chiò A, Mora G, Lauria G. Pain in amyotrophic lateral sclerosis. Lancet Neurol 2017;16:144–57. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27964824&dopt=Abstract 10.1016/S1474-4422(16)30358-1 [DOI] [PubMed] [Google Scholar]
- 54.McClelland S, 3rd, Bethoux FA, Boulis NM, Sutliff MH, Stough DK, Schwetz KM, et al. Intrathecal baclofen for spasticity-related pain in amyotrophic lateral sclerosis: efficacy and factors associated with pain relief. Muscle Nerve 2008;37:396–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=17894358&dopt=Abstract 10.1002/mus.20900 [DOI] [PubMed] [Google Scholar]
- 55.Delpont B, Beauvais K, Jacquin-Piques A, Alavoine V, Rault P, Blanc-Labarre C, et al. Clinical features of pain in amyotrophic lateral sclerosis: A clinical challenge. Rev Neurol (Paris) 2019;175:11–5. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30131172&dopt=Abstract 10.1016/j.neurol.2017.11.009 [DOI] [PubMed] [Google Scholar]
- 56.González-Fernández M, Daniels SK. Dysphagia in stroke and neurologic disease. Phys Med Rehabil Clin N Am 2008;19:867–88, x. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=18940646&dopt=Abstract 10.1016/j.pmr.2008.07.001 [DOI] [PubMed] [Google Scholar]
- 57.Tomik B, Guiloff RJ. Dysarthria in amyotrophic lateral sclerosis: A review. Amyotroph Lateral Scler 2010;11:4–15. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=20184513&dopt=Abstract 10.3109/17482960802379004 [DOI] [PubMed] [Google Scholar]
- 58.Körner S, Sieniawski M, Kollewe K, Rath KJ, Krampfl K, Zapf A, et al. Speech therapy and communication device: impact on quality of life and mood in patients with amyotrophic lateral sclerosis. Amyotroph Lateral Scler Frontotemporal Degener 2013;14:20–5. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=22871079&dopt=Abstract 10.3109/17482968.2012.692382 [DOI] [PubMed] [Google Scholar]
- 59.Raglio A, Giovanazzi E, Pain D, Baiardi P, Imbriani C, Imbriani M, et al. Active music therapy approach in amyotrophic lateral sclerosis: a randomized-controlled trial. Int J Rehabil Res 2016;39:365–7. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27437724&dopt=Abstract 10.1097/MRR.0000000000000187 [DOI] [PubMed] [Google Scholar]
- 60.Arbesman M, Sheard K. Systematic review of the effectiveness of occupational therapy-related interventions for people with amyotrophic lateral sclerosis. Am J Occup Ther 2014;68:20–6. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=24367951&dopt=Abstract 10.5014/ajot.2014.008649 [DOI] [PubMed] [Google Scholar]
- 61.Creemers H, Beelen A, Grupstra H, Nollet F, van den Berg LH. The provision of assistive devices and home adaptations to patients with ALS in the Netherlands: patients’ perspectives. Amyotroph Lateral Scler Frontotemporal Degener 2014;15:420–5. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=24899120&dopt=Abstract 10.3109/21678421.2014.920031 [DOI] [PubMed] [Google Scholar]
- 62.Elliott MA, Malvar H, Maassel LL, Campbell J, Kulkarni H, Spiridonova I, et al. Eye-controlled, power wheelchair performs well for ALS patients. Muscle Nerve 2019;60:513–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=31397910&dopt=Abstract 10.1002/mus.26655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Guy V, Soriani MH, Bruno M, Papadopoulo T, Desnuelle C, Clerc M. Brain computer interface with the P300 speller: usability for disabled people with amyotrophic lateral sclerosis. Ann Phys Rehabil Med 2018;61:5–11. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29024794&dopt=Abstract 10.1016/j.rehab.2017.09.004 [DOI] [PubMed] [Google Scholar]
- 64.Burns TM, Graham CD, Rose MR, Simmons Z. Quality of life and measures of quality of life in patients with neuromuscular disorders. Muscle Nerve 2012;46:9–25. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=22644588&dopt=Abstract 10.1002/mus.23245 [DOI] [PubMed] [Google Scholar]
- 65.Bos I, Kuks JB, Wynia K. Development and testing psychometric properties of an ICF-based health measure: The Neuromuscular Disease Impact Profile. J Rehabil Med 2015;47:445–53. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=25679115&dopt=Abstract 10.2340/16501977-1938 [DOI] [PubMed] [Google Scholar]
- 66.Simmons Z. Patient-Perceived Outcomes and Quality of Life in ALS. Neurotherapeutics 2015;12:394–402. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=25502407&dopt=Abstract 10.1007/s13311-014-0322-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bakker LA, Schröder CD, van Es MA, Westers P, Visser-Meily JM, van den Berg LH. Assessment of the factorial validity and reliability of the ALSFRS-R: a revision of its measurement model. J Neurol 2017;264:1413–20. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=28608303&dopt=Abstract 10.1007/s00415-017-8538-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Mitsumoto H, Chiuzan C, Gilmore M, Zhang Y, Ibagon C, McHale B, et al. A novel muscle cramp scale (MCS) in amyotrophic lateral sclerosis (ALS). Amyotroph Lateral Scler Frontotemporal Degener 2019;20:328–35. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=31007059&dopt=Abstract 10.1080/21678421.2019.1603310 [DOI] [PubMed] [Google Scholar]
- 69.Hobson EV, McDermott CJ. Supportive and symptomatic management of amyotrophic lateral sclerosis. Nat Rev Neurol 2016;12:526–38. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27514291&dopt=Abstract 10.1038/nrneurol.2016.111 [DOI] [PubMed] [Google Scholar]
- 70.Malik R, Lui A, Lomen-Hoerth C. Amyotrophic lateral sclerosis. Semin Neurol 2014;34:534–41. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=25520025&dopt=Abstract 10.1055/s-0034-1396007 [DOI] [PubMed] [Google Scholar]
- 71.de Almeida JP, Silvestre R, Pinto AC, de Carvalho M. Exercise and amyotrophic lateral sclerosis. Neurol Sci 2012;33:9–15. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=22228269&dopt=Abstract 10.1007/s10072-011-0921-9 [DOI] [PubMed] [Google Scholar]
- 72.Valadi N. Evaluation and management of amyotrophic lateral sclerosis. Prim Care 2015;42:177–87. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=25979579&dopt=Abstract 10.1016/j.pop.2015.01.009 [DOI] [PubMed] [Google Scholar]
- 73.Seeber AA, Pols AJ, Hijdra A, Grupstra HF, Willems DL, de Visser M. Advance care planning in progressive neurological diseases: lessons from ALS. BMC Palliat Care 2019;18:50. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=31196046&dopt=Abstract 10.1186/s12904-019-0433-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Karam CY, Paganoni S, Joyce N, Carter GT, Bedlack R. Palliative Care Issues in Amyotrophic Lateral Sclerosis: An Evidenced-Based Review. Am J Hosp Palliat Care 2016;33:84–92. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=25202033&dopt=Abstract 10.1177/1049909114548719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Connolly S, Galvin M, Hardiman O. End-of-life management in patients with amyotrophic lateral sclerosis. Lancet Neurol 2015;14:435–42. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=25728958&dopt=Abstract 10.1016/S1474-4422(14)70221-2 [DOI] [PubMed] [Google Scholar]
- 76.Dal Bello-Haas V, Florence JM. Therapeutic exercise for people with amyotrophic lateral sclerosis or motor neuron disease. Cochrane Database Syst Rev 2013;(5):CD005229. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=23728653&dopt=Abstract 10.1002/14651858.CD005229.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ashworth NL, Satkunam LE, Deforge D. Treatment for spasticity in amyotrophic lateral sclerosis/motor neuron disease. Cochrane Database Syst Rev 2012;(2):CD004156. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=22336799&dopt=Abstract 10.1002/14651858.CD004156.pub4 [DOI] [PubMed] [Google Scholar]
- 78.Radunovic A, Annane D, Rafiq MK, Brassington R, Mustfa N. Mechanical ventilation for amyotrophic lateral sclerosis/motor neuron disease. Cochrane Database Syst Rev 2017;10:CD004427. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=28982219&dopt=Abstract 10.1002/14651858.CD004427.pub4 [DOI] [PMC free article] [PubMed]
- 79.Ng L, Khan F, Young CA, Galea M. Symptomatic treatments for amyotrophic lateral sclerosis/motor neuron disease. Cochrane Database Syst Rev 2017;1:CD011776. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=28072907&dopt=Abstract 10.1002/14651858.CD011776.pub2 [DOI] [PMC free article] [PubMed]
- 80.Schell WE, Mar VS, Da Silva CP. Correlation of falls in patients with Amyotrophic Lateral Sclerosis with objective measures of balance, strength, and spasticity. NeuroRehabilitation 2019;44:85–93. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30714981&dopt=Abstract 10.3233/NRE-182531 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table I
Evidence synthesis of the literature.


