Abstract
INTRODUCTION
Non-specific low back pain (NS-LBP) is one of the most common musculoskeletal conditions related to medical expenses and disability. Evidence suggests that changes in motion patterns could induce trunk instability and impaired postural control. Therefore, this systematic review investigated the effects of exercise on balance in patients with NS-LBP.
EVIDENCE ACQUISITION
A systematic review and meta-analysis were conducted. Findings were reported following the 2020 PRISMA statement and the main databases were searched for RCTs. Studies were independently screened through a standardized form and their internal validity assessed by using the Cochrane risk of bias (RoB) tool. Pooled effects were calculated at post-treatment and quality of evidence was assessed through the GRADE framework.
EVIDENCE SYNTHESIS
Twelve articles were included in the review, eight in the meta-analysis. None of the studies were judged at low RoB. There is very low-quality evidence that exercise is effective in reducing Centre of Pressure (CoP) displacement (-16.99 [-27.29, -6.68]; P=0.001) and in improving single-leg stance test performance (-28.7 [-48.84, -8.67]; P=0.005) and dynamic balance (-4.74 [-8.02, -1.46]; P=0.005). Conversely, no significant results were observed in “ellipse area” and in “limits of stability” indexes. Other results were summarized in a qualitative synthesis.
CONCLUSIONS
Exercise could be effective in improving both static and dynamic balance in patients with NS-LBP over a short-term period. However, quality of evidence was estimated as very low, hence further double-blinded, high-quality RCTs are needed to address clinical practice and research.
Key words: Low back pain, Exercise, Postural balance, Physical therapy modalities, Systematic review
Introduction
Low back pain (LBP) is the most common musculoskeletal condition, frequently related to medical expenses and disability.1, 2 It is considered the main cause of limitation in everyday activities and work absence in most countries, representing an important economic burden globally.3, 4
Despite its high prevalence, LBP frequently has a favorable prognosis. Although a specific cause of pain can seldom be identified, in most cases no pathology is present, and the prevalent form consists of mechanical, non-specific LBP (NS-LBP).5 Pain typically improves consistently within 6 weeks, even if many subjects - estimates varying from 2% to 34% – still experience pain after 3 months and later, turning this condition into a chronic state.6
Up to now, several hypotheses have been made about the mechanisms underlying the onset of NS-LBP. Many authors have suggested that changes in motion patterns and impairments in spine stability could play a role in spinal disorders.7, 8 Indeed, different studies have focused on the activity of the deep muscles of the trunk, typically showing delayed activation, diminished resistance and weakness, especially during episodes of pain.9
In this context, evidence suggests that these changes probably induce postural instability as well as impaired postural control; in fact, there is evidence that NS-LBP subjects show an increase in center of pressure (CoP) displacement and velocity10-12 and proprioceptive deficits, probably as a consequence of pain.13 Interestingly, a recent systematic review highlighted how balance is significantly impaired in individuals with chronic LBP, thus suggesting clinicians should carry out a proper balance assessment; this evaluation should be used to monitor and guide the treatment period.14 As a consequence, different instruments and motor-task tests have been adopted over the years, showing overall acceptable values of reliability and validity.15-17
To date, several randomized controlled trials (RCTs) have already investigated the effects of therapeutic exercise on pain and disability in patients with NS-LBP with conflicting results. Specifically, exercise seems to be slightly effective in improving pain levels and functional status in chronic LBP, while there is no evidence of its efficacy in the case of acute pain.18 However, no systematic reviews to date have established the effectiveness of exercise on balance outcomes19 in patients with NS-LBP, so a synthesis of evidence is still missing.
Based on the above line of reasoning, this systematic review aimed to investigate the effects of exercise on balance in patients with NS-LBP. Secondly, we explored which modality of exercise appeared to be superior to others and lastly, if effects are still present over a medium- or a long-term period.
Evidence acquisition
Protocol registration
The reporting of the current review followed the “2020 Preferred Reporting Items for Systematic Reviews and Meta-Analysis” (PRISMA 2020 checklist).20 A “PICO” strategy was used to state the research question (P: non-specific low back pain; I: therapeutic exercise; C: all the other therapies routinely applied; O: balance performance). The protocol was regularly approved and published in an international prospective register of systematic reviews (PROSPERO, https://www.crd.york.ac.uk/prospero/, registration ID: CRD42021236669).
Search strategy
A search process was carried out to assess the effects of exercise on balance performance in NS-LBP subjects. PubMed, Embase, Cochrane CENTRAL, Scopus and PEDro databases were consulted up to April 2021. To be thorough, we performed cross-referencing to retrieve any possible missing study and gray literature was also considered through Google web searching and ClinicalTrials.gov. Different search terms and keywords were used, such as “low back pain,” “non-specific low back pain,” “chronic low back pain,” “exercise,” “training,” “physical therapy,” “physiotherapy,” “balance,” “proprioception,” “equilibrium” and “posture.” These words were combined differently according to database functioning; details are provided in the Supplementary Digital Material 1: Supplementary Text File 1.
Eligibility criteria
Inclusion criteria for this review were the following: randomized, or quasi-randomized controlled clinical trials (RCTs or quasi-RCTs) also including feasibility or pilot studies; trials assessing the effects of active exercise on any balance performance indicator, both instrumental and motor-task tests, and studies which compared any other kind of control interventions, conducted in subjects presenting NS-LBP. Further considered criteria were adult population (18-70 years old) and papers written in English. Due to the intrinsic variability of exercise therapies, no restriction in terms of dosage was applied. Similarly, we did not apply any limitations regarding control groups, except for the exclusion of trials comparing two (or more) different types of exercise; control therapies included usual care, instrumental therapies, passive applications (e.g. manual/manipulative treatments, massage, hot and/or cold packs), waiting lists and educational/informative counselling. Although gait can be considered an indicator of balance performance, we opted to exclude studies focusing on gait analysis due to its complexity and peculiarities.
Study selection and data collection
Records obtained from databases were managed using “Rayyan, Intelligent Systematic Review” (www.rayyan.ai).21 Title, abstract and full texts were screened independently by three reviewers (MA, MC, EP) to identify eligible studies. Discrepancies were resolved through a discussion with another reviewer (FDF). Details of the study selection process are provided in the PRISMA 2020 flow diagram (Figure 1).
Figure 1.

—Flow diagram based on PRISMA statement.
Main characteristics of included studies were extracted in a standardized form and summarized in a table (Supplementary Digital Material 2: Supplementary Table I) reporting first author name, main objective, outcomes, sample size, participants’ allocation and information regarding the intervention in terms of dosage. Another table (Supplementary Digital Material 3: Supplementary Table II) detailed the characteristics of compared interventions and results. As before, the same reviewers independently screened the included studies and resolved any disagreement with a consensus.
In case of missing data, investigators were contacted via e-mail.
Outcomes
The primary outcome of the current review was balance improvement, measured at postintervention and/or at medium- or long-term follow-up.
We considered any possible indicator of balance performance such as posturography, static and dynamic stabilometry and all types of measurement coming from a motor-task test.
Secondary outcome measures were changes in physical parameters (e.g. endurance, muscular strength, motor-task performances) and self-reported questionnaires related to psychological attitude such as fear-avoidance beliefs, pain-related fear and catastrophizing. Furthermore, patient care satisfaction was taken into account.
Risk of bias assessment
The updated version of the Cochrane Risk of Bias (RoB) tool in RCTs22 (13 item version) was used to assess the methodological quality of the included studies. Three blinded reviewers (MA, MC, EP) independently made their evaluation by reading full-text articles and a final discussion with two other reviewers (FDF, MM) resolved each discrepancy. This tool included six domains (selection bias, performance bias, attrition bias, detection bias, reporting bias, other sources of bias) made up of 13 criteria. Reviewers could make their judgement considering a three-point scale: low, unclear and high RoB.
Measures and synthesis of results
As measurements of treatment effect, we reported results and differences among groups in a descriptive way, by using mean±standard deviation (SD) and mean and 95% confidence interval (CI). In the case of data presented as median and interquartile range (IQR), median was assimilated to mean, and SD was obtained considering a 1.35:1 ratio.
A meta-analysis was performed using “Review Manager v 5.3.5” (The Nordic Cochrane Centre, http://ims.cochrane.org/revman) and alpha level was set at 0.05 to test for overall effect.
For continuous variables, mean difference (MD or Cohen’s “d”) or standardized mean difference (SMD or Hedges’ “g”) with 95% CI were calculated using a random effects model, to acknowledge the possible clinical and methodological diversity among included studies.
An effect size (ES) ranging from 0.2 to 0.49 was considered “small,” from 0.5 to 0.79 “moderate,” and a value of 0.8 or above “large.” Heterogeneity was measured through I2 statistics which explained how much of the variation between studies was due to heterogeneity rather than to chance. Values ranging from 0% to 40% suggest “not important” heterogeneity, from 30% to 60% indicate “moderate” levels, from 50% to 90% represent “substantial,” and from 75% to 100% “considerable” heterogeneity.23
The quality of evidence was assessed through the Grades of Recommendation, Assessment, Development and Evaluation (GRADE) method, as suggested by the Updated Cochrane Back Review Group method guidelines.24 Using this approach, it is possible to downgrade the quality of evidence from “high” to “moderate,” “low” or “very low” on the basis of 5 key-domains: risk of bias, inconsistency, indirectness, imprecision and publication bias.
Evidence synthesis
Selection of the studies
The search strategies led us to identify a total of 2262 studies, 478 of which were detected as duplicates and consequently removed. In a second stage, 1784 records were screened by reading title and abstract and 1758 were excluded since they were not pertinent. Finally, a total of 26 articles were assessed by reading the full text and 14 were subsequently excluded. As a consequence, 12 studies completely met the criteria we stated for the current review and were included in the final synthesis; 9 of these RCTs were also considered for meta-analysis. Further details of the study selection process are reported in the PRISMA 2020 flow-chart (Figure 1).
Description of the studies
All the included studies (N.=12)25-36 were RCTs. Interventions presented differences across studies, since four trials25, 29, 30, 34 investigated the effects of a Pilates training, two studies32, 35 focused on stability training and two others28, 36 on whole-body vibration therapy; functional resistance exercises, diaphragmatic training, therapeutic exercise and sensorimotor training were investigated by the other included studies.26, 27, 31, 33 Regarding control groups, most of the studies25, 26, 28-32, 34, 36 opted for “no intervention,” only suggesting daily normal activities; two trials27, 35 compared exercise to instrumental therapies such as TENS, ultrasounds and laser-therapy. Ghasemi et al.33 performed a three-arm trial, so that a comparison was possible with two different types of manual therapy (cranio-sacral treatment and muscle-energy techniques).
The overall sample size was 521 (mean: 43.41, SD=17.74), with a mean age of 38.77±10.04 years. The period of treatment varied from a minimum of 1 day (single session in Lopes’ study29), to a maximum of 14 weeks,30 resulting in a mean of 8.9±3.9 weeks. Frequency of treatments greatly varied (mean: 2.27±1.19 session/week), since Lopes29 investigated a single session and Karimi35 assessed a program of ten consecutive sessions performed on a daily basis. Treatments had an average duration of 34.11±20.08 minutes, although studies28, 36 investigating the whole-body vibration therapy had shorter duration (8 and 15 min.) with respect to the other exercise programs (range: 20-60 min.).
All the included studies considered assessments at post treatment, while only two RCTs31, 33 reported evaluations over a medium- or long-term period; specifically, Ghasemi33 considered 2-month and Kuukkanen et al.31 6- and 12-month follow-up assessment. The main characteristics of the included RCTs are reported in Supplementary Table I.
Outcomes
Although all the included trials investigated at least one outcome related to balance, only two of them29, 30 considered these as a primary outcome.
All the trials assessed static balance, whereas in two studies27, 29 dynamic balance was considered. The static balance performances were explored through different modalities: six studies29-33, 36 measured postural sway by using posturography, four trials25-27, 34 adopted different motor-task tests such as stork stand test,25 blind flamingo test,26 unilateral hip bridge endurance test27 and single limb stance test;34 finally, two RCTs28, 35 considered stability indices through the “Biodex Balance System.” In both the studies27, 29 assessing dynamic balance, the “star excursion balance test” was used.
Other considered outcome measures were related to physical parameters. Two studies25, 34 detected lumbar mobility, two others28, 36 investigated trunk muscle performances and another26 measured the physical fitness levels of the subjects.
Risk of bias
The RoB was evaluated for all twelve included studies and specific details are reported in Figure 225-36 and Figure 3.
Figure 2.

—Risk of bias summary: review authors’ judgement about each risk of bias item for included studies.25-36
Figure 3.
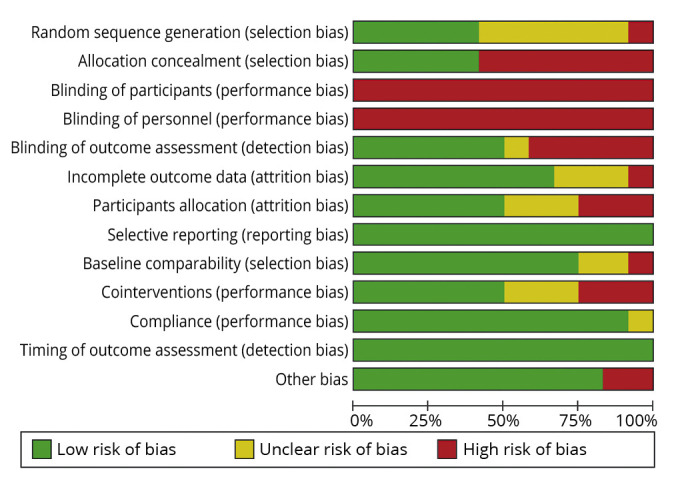
—Risk of bias assessment graph for the included studies.
None of these studies reported a low risk for all the items. Since the trials dealt with physical therapy modalities, a high RoB was attributed to “blinding of personnel” criterion; furthermore, none of the studies declared that the subjects were masked, so blinding of participants was also considered to be at high risk of bias. In addition, some issues were detected for selection bias: seven RCTs25-28, 31, 33, 35 were judged at high risk for allocation concealment, and one of these31 did not perform a proper random sequence generation. Other six studies25, 27, 32, 33, 35, 36 did not detail the randomization procedure sufficiently, so the risk was judged as unclear. Five26, 31-33, 35 out of twelve studies were considered at high RoB for detection bias, since assessors were not blinded; another one27 was considered at unclear risk for this point.
Three studies32, 33, 35 were evaluated at high risk of attrition bias, and for another three trials some details were missing (unclear RoB). Baseline comparability was not guaranteed in three RCTs25, 31, 36 and cointerventions management was not considered sufficiently performed in six studies;27, 28, 31, 33, 35, 36 in three of these works,28, 31, 35 the risk was judged as high.
Description of results
The overall effect of exercise on balance in NSLBP subjects was estimated through a qualitative synthesis; in addition, a meta-analysis was performed for some end-points, by including the studies25, 27-31, 33-35 which adopted comparable outcome measures.
Among RCTs investigating balance performance during a motor-task test, four studies25-27, 34 reported results in favor of exercise; however, only Cortell-Tormo26 and Otadi27 found a between-group significance (+58%, P≤0.05 during “blind flamingo test” and +65%, P≤0.05 during the “unilateral hip bridge endurance test”).
Concerning postural sway variables, results were different across the studies; only Keading36 did not find any significant difference in a pre-post comparison, neither in a “within-group” nor in a between-groups analysis. Rather, three trials reported effects of exercise for most of the assessed variables: Lopes29 and Patti30 found an overall reduction of postural sway registered in CoP displacements (-44.7 cm, P<0.001; -94.9 mm, P<0.001 respectively); Rhee32 observed a reduction in anterior-posterior sway (P=0.04), but not in medium-lateral sway (P=0.86). Kuukkanen et al.31 did not find any significant differences in displacements, although some pre-post changes were detected in CoP velocity (+1.5 mm/s, P=0.03). Ghasemi33 observed an overall improvement in posturographic parameters for all the groups of intervention, even if the most relevant changes were detected in the “craniosacral therapy group,” especially during a single-leg standing test with closed eyes (P<0.001 at post-treatment, P=0.03 at follow-up). Considering the large number of variables used to evaluate postural sway, a consultation of Supplementary Table I and Supplementary Table II is advised.
Two studies28, 35 considered limits of stability to evaluate balance performance; Karimi35 reported the overall stability index improving from 9.78±1.87 to 8.22±2.27, P≤0.05; Del Pozo Cruz28 found a significant improvement of 20.37% (–0.11°, P=0.031) over the anterior-posterior axis, but not over the medium-lateral one. However, no differences between groups were registered.
Regarding the two studies27, 29 investigating dynamic balance through SEBT, both found improvements in the exercise groups in the different directions (P≤0.05), however only Otadi27 reported significant changes between groups (P≤0.05).
Only two studies31, 33 considered follow-up assessments; Ghasemi33 reported mean CoP velocity and ellipse area improvements in the exercise group at 2 months after the end of the treatment period (-0.0002, P≤0.05 and -0.002, P≤0.05), Kuukkanen et al.31 found improvements only in the “home based exercise” group both at 6 and at 12 months follow-up (+1.0 and +1.6, P=0.01 and P=0.002, respectively).
Concerning secondary outcomes, two studies25, 34 reported superiority of exercise in increasing flexibility (Fingertip-to-floor test: +8.45, P=0.032 and +2.2 cm P≤0.05, respectively).
Cortell-Tormo26 considered a group of motor-task tests to assess physical fitness, finding improvements in all of these attributable to exercise intervention (P≤0.01). Del Pozo Cruz28 assessed lifting capacity through the PILE test, finding a significant improvement of 16.58% (P=0.008); however, the same author did not find the same results in walking endurance. In addition, Keading36 reported a positive trend in favor of intervention (P=0.056) concerning the isokinetic performance of trunk muscles.
Finally, no studies investigated psychological attitudes or levels of care satisfaction.
Effects of exercise on balance
Single leg stance test
Two trials25, 34 were included in the analysis, with a total sample size of 88 subjects. The forest plot in Figure 425, 34 shows how exercise significantly improves time of resistance in the single leg stance test in both of the trials included.
Figure 4.
—Forest plot of comparison: effect of exercise vs. control interventions for balance in NS-LBP.25, 34 Outcome: single-leg stance test. CI: Confidence interval; SD: standard deviation.
As a consequence, the overall effect was in favor of exercise (MD=-28.7 [-48.84, -8.67]; P=0.005). Heterogeneity was not important (I2=2%) and not significant (P=0.31). Quality of evidence was rated as “very low” (Table I).24
Table I. —Quality of evidence assessed through GRADE framework.24.
| Outcome | SMD (95% CI) | N. of subjects (Studies) | Comments | Quality of Evidence |
|---|---|---|---|---|
| CoP total displacement | -16,99 (-27.29, -6.68) | 84 (2 RCT) | Downgraded by one level for risk of bias Downgraded by two levels for imprecisiona,b |
Very Low |
| Ellipse area | -0.28 (-0.97, 0.41) | 114 (3 RCT) | Downgraded by one level for risk of bias Downgraded by one level for inconsistency (I2=70%) Downgraded by one level for imprecisiona |
Very Low |
| Limits of stability (antero-posterior) | -0.00 (-0.38, 0.38) | 87 (2 RCT) | Downgraded by one level for risk of bias Downgraded by two levels for imprecisiona,b |
Very Low |
| Limits of stability (medio-lateral) | 0.03 (-0.41, 0.48) | 87 (2 RCT) | Downgraded by one level for risk of bias Downgraded by one level for inconsistency (I2=81%) Downgraded by two levels for imprecisiona,b |
Very low |
| Dynamic balance (SEBT test) | -4.74 (-8.02, -1.46) | 70 (2 RCT) | Downgraded by one level for risk of bias Downgraded by two levels for imprecisiona,b |
Very Low |
| Single-leg stance test | -28.7 (-48.84, -8.67) | 88 (2 RCT) | Downgraded by one level for risk of bias Downgraded by two levels for imprecisiona,b |
Very Low |
aWide confidence interval; bsample size <100. GRADE criteria: high quality (we are very confident that the true effect lies close to that of the estimate of the effect); moderate quality (we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different); low quality (our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect); very low quality (we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect).
Postural sway
Centre of pressure total displacement
Two studies29, 30 were included in the analysis (Figure 5),29, 30 with an aggregate sample of 84 subjects. Both of the studies reported significant results in favor of exercise in reducing the CoP total displacement, as illustrated in Figure 4.25, 34 The pooled MD was of -16.99 (-27.29, - 6.68), P=0.001; heterogeneity was absent (I2=0%) and not significant (P=0.42). Quality of evidence was judged as “very low” (Table I).24
Figure 5.
—Forest plot of comparison: effect of exercise vs. control interventions for balance in NS-LBP.29, 30 Outcome: CoP displacement. CI: Confidence interval; SD: standard deviation.
Ellipse area
Three RCTs29, 30, 33 were included in the meta-analysis (Figure 6),29, 30, 33 with a total sample of 114 subjects; one study reported significant results in favor of exercise, one study found no significant effects in favor of exercise and another one no significant results in favor of the control group. The overall effect on the ellipse surface area was not significant in favor of exercise, resulting in a pooled effect size (SMD) of -0.28 (-0.97, 0.41), P=0.42. Heterogeneity was substantial (I2=70%) and significant (P=0.04). Quality of evidence was rated as “very low” (Table I).24
Figure 6.
—Forest plot of comparison: effect of exercise vs. control interventions for balance in NS-LBP.29, 30, 33 Outcome: ellipse area. CI: Confidence interval; SD: standard deviation.
Limits of stability
Anterior-Posterior Index
Two studies28, 35 were included in the analysis (Figure 7),28, 35 with an overall sample size of 87. One trial reported a non-significant effect of the control group compared to exercise group and the other one found a non-significant effect of exercise in improving antero-posterior stability index. The overall effect of exercise was indifferent, with a pooled effect (MD) of -0.00 (-0.38, 0.38), P=1.00. Heterogeneity was not important (I2=26%) and not significant (P=0.25). Quality of evidence was rated as “very low” (Table I).24
Figure 7.
—Forest plot of comparison: effect of exercise vs. control interventions for balance in NS-LBP.28, 35 Outcome: Anterior-Posterior Index (limits of stability). CI: Confidence interval; SD: standard deviation.
Medium-Lateral Index
Two studies28, 35 were considered for meta-analysis (Figure 8),28, 35 with an average sample of 87 subjects. One trial reported a non-significant effect on the control group and the other a non-significant effect of exercise in improving medium-lateral stability index. The overall effect was not significantly in favor of control interventions, resulting in a pooled effect (MD) of 0.03 (-0.41, 0.48), P=0.89; heterogeneity was considerable (I2=81%) and significant (P=0.02). Quality of evidence was “very low” (Table I).24
Figure 8.
—Forest plot of comparison: effect of exercise vs. control interventions for balance in NS-LBP.28, 35 Outcome: Medium-Lateral Index (limits of stability). CI: Confidence interval; SD: standard deviation.
Dynamic balance
Two studies27, 29 assessing dynamic balance through dynamic balance (SEBT) were considered for meta-analysis (Figure 9),27, 29 with a total sample size of 70. Both trials reported effects in favor of exercise, in one case not-significantly. The overall effect was significantly in favor of exercise, with a mean difference of -4.74 (-8.02, -1.46), P=0.005. Heterogeneity was absent (I2=0%) and not significant (P=0.86). Quality of evidence was judged as “very low” (Table I).24
Figure 9.
—Forest plot of comparison: effect of exercise vs. control interventions for balance in NS-LBP.27, 29 Outcome: dynamic balance (SEBT). CI: Confidence interval; SD: standard deviation.
Summary of evidence
To the best of our knowledge, this is the first systematic review investigating the effects of exercise on balance in patients with NS-LBP. In our opinion this aspect should be considered of particular importance since to date, several studies37-39 have demonstrated how balance could frequently be affected in NS-LBP; moreover, previous reviews invited clinicians to take into consideration a balance assessment in the context of NS-LBP.12, 14 However, an SR on the topic was missing.
Results of the current review highlighted that exercise seems to improve balance performance in NS-LBP individuals, since qualitative and quantitative synthesis showed how postural sway, motor-task tests and dynamic balance are positively influenced following a period of exercise training. Specifically, the most affected variables seem to be total CoP displacement, performance obtained during a single-leg stance test and dynamic balance, assessed through SEBT. However, conflicting results emerged in some parameters related to postural sway, such as total ellipse area, CoP velocity and limits of stability, in which only a positive trend (without any significant result) was observed. These findings are detectable at the end of the period of treatment, since most of the included studies only reported data concerning a “pre-post” evaluation; nevertheless, some positive cues are present in those trials which considered an evaluation over a medium-term period.31, 33
Results also gave some indication that balance improvements could be accompanied by some modifications of physical parameters such as lumbar flexibility, fitness levels, lifting capacity and the isokinetic performance of trunk muscles. This last aspect should be considered of particular importance if confirmed by additional evidence, since changes in physical function (especially regarding the performance of trunk muscles) may explain the improvements obtained in balance; unfortunately, the included studies (2) which explored such variables were very limited. Moreover, these outcomes were assessed by different modalities, so that conclusions should be drawn with care.
Clinical implications
In light of the abovementioned findings, some considerations are necessary. Firstly, the highlighted efficacy of exercise can probably confirm some theories underlying balance impairment in NS-LBP; indeed, the most acknowledged mechanism seems to be the altered proprioceptive function deriving from faulty muscular responses and leading to deficit in trunk repositioning, postural control and balance.40-43 Moreover, it is largely known that multiple sensory information is involved in the organization of postural control, so that in addition to visual and vestibular cues, somatosensory information arising from the musculoskeletal system has an important role in posture.44 In this context, exercise could act on different physical parameters and mechanisms such as muscle endurance, functional stabilization, proprioception, coordination and flexibility, thus ensuring an improved postural control both in static and in dynamic conditions. Evidence suggests how this is possible through a continuous sensorial re-weighting coming from the integration of somatosensory information, processed by the central nervous system.45-47 This point can also explain the reason why different types of exercise (e.g. functional resistance training, Pilates, sensorimotor training, active vibration therapy) all appeared to be effective in improving balance.
Secondly, due to the huge variability of the methods applied in the RCTs, a subgroup analysis for type of exercise was not possible. Despite this, the studies investigating exercises targeted on stabilization25, 29, 30, 32, 34, 35 (e.g. core stability, Pilates, spinal stabilization) were definitely prevailing (50%) compared to other trials: more specifically, these trials reported improvements in at least one of the static balance parameters and in three studies those changes were significantly greater in the intervention group. Moreover, Lopes et al. also found a significant change in the dynamic balance assessment. Concerning the remaining studies, results were overall in favor of exercise as well. However, it is important to point out that three26, 27, 31 of these studies included, in their intervention, a number of exercises oriented towards stabilization mechanisms or, at least, movements involving the activation of the spinal core. Conversely, these improvements were not observed in the other two trials,28, 36 where whole-body vibration and sensorimotor training were considered. We can hypothesize that exercise, when specifically targeted to stability mechanisms, could lead to larger effects in improving balance. Furthermore, our assumption seems to be in line with previous literature, reporting positive effects on balance and a reduction in falls in healthy people and in the elderly following a Pilates training.48-51
Despite the above-mentioned importance of a proper balance assessment in NS-LBP, some issues emerge if we consider the clinical relevance of the measures employed in the different studies. Although posturography is to be considered a reliable method to evaluate balance in NS-LBP,15, 52 this examination is strictly addressed to a static performance and it does not provide any information concerning the dynamic skills of the people;53, 54 moreover, this assessment is not performed in an ecological environment with respect to the activities of daily living.15, 55 The same reasoning should be done for the single leg stance test, in which many confounding factors can affect the validity of this test.56 On the other hand, both the studies that used the SEBT, a more dynamic reliable test,57, 58 reported clinical significant changes after the exercise therapy. As a consequence, this fact represents, once again, indirect proof that balance is impaired in NS-LBP, thus leading to a worsening of dynamic performances. Besides, exercise training can positively influence such aspects, presumably through proper proprioceptive stimulation and improvement in the stability of trunk muscles.
Implications for research and healthcare policies
Methods applied in the included studies appeared to be characterized by a certain degree of heterogeneity. This aspect is mostly related to the interventions. Exercise is de facto a kind of active therapy for the patient; however, the manner in which different modalities can imply different forms of physical stimulation should be considered.59-61 Moreover, not all the protocols were described following the proper checklist suggested for exercise trials,62 with subsequent issues in terms of reproducibility.
Similarly, the comparison intervention also presented some differences, varying from usual care to instrumental therapies (e.g. electrotherapy). Furthermore, the authors adopted different outcome measures and, sometimes, various settings. Another point of interest should be the possible correlation between balance impairments and levels of pain or disability: so far, no studies have confirmed this aspect. Finally, only two of the included trials29, 30 chose balance as the primary outcome.
For all these issues, it becomes hard to generalize our results, so that relative considerations should be taken carefully. Therefore, research should move in this direction by ensuring higher levels of uniformity in methods and better levels of consistency in results. In this way, it would be possible to properly inform clinicians and lead to updates in healthcare policies.
Quality of evidence
The quality of evidence was “very low,” according to GRADE criteria.24 The reasons for downgrading were mostly similar for each considered outcome.
Primarily, we downgraded for risk of bias. Since the included studies dealt with exercise therapy, blinding of personnel was not possible at all and masking of participants was unlikely, so these criteria were judged at high RoB. Besides, most of the studies did not perform an allocation concealment,25-28, 31, 33, 35 thus a form of selection bias was possible. In some cases, the outcome assessor was not blinded either,26, 27, 31-33, 35 and the “intention to treat” analysis was not always performed:26, 28, 31-33, 35 consequently, detection and attrition biases were also suspected. Other potential sources of bias were related to an unsure baseline comparability (selection bias)25, 31, 35 and to missing details concerning cointerventions (performance bias);27, 28, 31, 33, 35, 36 in addition, degrees or specializations of personnel (e.g. certified pilates instructor) were sometimes not clearly specified (performance bias)27, 28, 31, 33, 35, 36 (Figure 2).25-36
Another critical aspect was the imprecision of the assessments; indeed, all the data obtained from the analyses were characterized by wide confidence intervals and a small sample size.
Finally, two out of the six comparisons reported considerable levels of heterogeneity, leading us to downgrade for inconsistency.33, 34
Limitations of the study
This research presents some limitations. We performed a search including all the typologies of therapeutic exercise. On the one hand, this allowed us to consider, as a whole, all the active interventions frequently applied in the context of physical therapy. On the other hand, we had to summarize evidence considering an intrinsic degree of heterogeneity.
Only articles in English were admitted even if, according to our research, no studies written in other languages were found. Furthermore, our search strategy was performed on the main databases, aware that some studies of interest could have been overlooked. As previously stated, we performed meta-analysis only when data were aggregable and assessment modalities were almost equivalent. In some cases, the procedures of evaluation were not fully described, or they presented some minimal differences. Hence, it is possible that such variability can affect the pooled effect size of some comparisons. Finally, publication bias is another possible issue; as is known, there is no statistical tool able to accurately detect it.63
Conclusions
Exercise could be effective in improving both static and dynamic balance in patients with NS-LBP over a short-term period. However, quality of evidence is very low, and some methodological issues were detected in the included studies. Further double-blinded, high-quality RCTs, comparing different subgroups of exercise and assessing balance through standardized and uniform modalities are needed. This could improve the quality of evidence and properly address clinicians and researchers in this field.
Supplementary Digital Material 1
Supplementary Text File 1
Search strategy.
Supplementary Digital Material 2
Supplementary Table I
Main characteristics of the included studies
Supplementary Digital Material 1
Supplementary Table II
Description of interventions and main results.
References
- 1.Woolf AD, Zeidler H, Haglund U, Carr AJ, Chaussade S, Cucinotta D, et al. Musculoskeletal pain in Europe: its impact and a comparison of population and medical perceptions of treatment in eight European countries. Ann Rheum Dis 2004;63:342–7. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=15020325&dopt=Abstract 10.1136/ard.2003.010223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Andersson GB. Epidemiology of low back pain. Acta Orthop Scand Suppl 1998;281:28–31. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=9771538&dopt=Abstract 10.1080/17453674.1998.11744790 [DOI] [PubMed] [Google Scholar]
- 3.Rapoport J, Jacobs P, Bell NR, Klarenbach S. Refining the measurement of the economic burden of chronic diseases in Canada. Chronic Dis Can 2004;25:13–21. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=15298484&dopt=Abstract [PubMed] [Google Scholar]
- 4.Hoy D, March L, Brooks P, Blyth F, Woolf A, Bain C, et al. The global burden of low back pain: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis 2014;73:968–74. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=24665116&dopt=Abstract 10.1136/annrheumdis-2013-204428 [DOI] [PubMed] [Google Scholar]
- 5.Deyo RA, Weinstein JN. Low back pain. N Engl J Med 2001;344:363–70. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=11172169&dopt=Abstract 10.1056/NEJM200102013440508 [DOI] [PubMed] [Google Scholar]
- 6.Steenstra IA, Verbeek JH, Heymans MW, Bongers PM. Prognostic factors for duration of sick leave in patients sick listed with acute low back pain: a systematic review of the literature. Occup Environ Med 2005;62:851–60. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=16299094&dopt=Abstract 10.1136/oem.2004.015842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hodges PW, Richardson CA. Inefficient muscular stabilization of the lumbar spine associated with low back pain. A motor control evaluation of transversus abdominis. Spine 1996;21:2640–50. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=8961451&dopt=Abstract 10.1097/00007632-199611150-00014 [DOI] [PubMed] [Google Scholar]
- 8.Kienbacher T, Kollmitzer J, Anders P, Habenicht R, Starek C, Wolf M, et al. Age-related test-retest reliability of isometric trunk torque measurements in patiens with chronic low back pain. J Rehabil Med 2016;48:893–902. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27735987&dopt=Abstract 10.2340/16501977-2164 [DOI] [PubMed] [Google Scholar]
- 9.Hodges PW. Is there a role for transversus abdominis in lumbo-pelvic stability? Man Ther 1999;4:74–86. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=10509061&dopt=Abstract 10.1054/math.1999.0169 [DOI] [PubMed] [Google Scholar]
- 10.Caffaro RR, França FJ, Burke TN, Magalhães MO, Ramos LA, Marques AP. Postural control in individuals with and without non-specific chronic low back pain: a preliminary case-control study. Eur Spine J 2014;23:807–13. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=24570125&dopt=Abstract 10.1007/s00586-014-3243-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Oyarzo CA, Villagrán CR, Silvestre RE, Carpintero P, Berral FJ. Postural control and low back pain in elite athletes comparison of static balance in elite athletes with and without low back pain. J Back Musculoskeletal Rehabil 2014;27:141–6. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=23963269&dopt=Abstract 10.3233/BMR-130427 [DOI] [PubMed] [Google Scholar]
- 12.Ruhe A, Fejer R, Walker B. Center of pressure excursion as a measure of balance performance in patients with non-specific low back pain compared to healthy controls: a systematic review of the literature. Eur Spine J 2011;20:358–68. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=20721676&dopt=Abstract 10.1007/s00586-010-1543-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Plowman SA. Physical activity, physical fitness, and low back pain. Exerc Sport Sci Rev 1992;20:221–42. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=1385572&dopt=Abstract [PubMed] [Google Scholar]
- 14.Berenshteyn Y, Gibson K, Hackett GC, Trem AB, Wilhelm M. Is standing balance altered in individuals with chronic low back pain? A systematic review. Disabil Rehabil 2019;41:1514–23. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29382241&dopt=Abstract 10.1080/09638288.2018.1433240 [DOI] [PubMed] [Google Scholar]
- 15.Leitner C, Mair P, Paul B, Wick F, Mittermaier C, Sycha T, et al. Reliability of posturographic measurements in the assessment of impaired sensorimotor function in chronic low back pain. J Electromyogr Kinesiol 2009;19:380–90. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=18023594&dopt=Abstract 10.1016/j.jelekin.2007.09.007 [DOI] [PubMed] [Google Scholar]
- 16.Ageberg E, Roberts D, Holmström E, Fridén T. Balance in single-limb stance in healthy subjects—reliability of testing procedure and the effect of short-duration sub-maximal cycling. BMC Musculoskelet Disord 2003;4:14. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=12831402&dopt=Abstract 10.1186/1471-2474-4-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ganesh GS, Chhabra D, Mrityunjay K. Efficacy of the star excursion balance test in detecting reach deficits in subjects with chronic low back pain. Physiother Res Int 2015;20:9–15. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=24619777&dopt=Abstract 10.1002/pri.1589 [DOI] [PubMed] [Google Scholar]
- 18.Hayden JA, van Tulder MW, Malmivaara A, Koes BW. Exercise therapy for treatment of non-specific low back pain. Cochrane Database Syst Rev 2005;(3):CD000335. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=16034851&dopt=Abstract 10.1002/14651858.CD000335.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Areeudomwong P, Buttagat V. Proprioceptive neuromuscular facilitation training improves pain-related and balance outcomes in working-age patients with chronic low back pain: a randomized controlled trial. Braz J Phys Ther 2019;23:428–36. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30361077&dopt=Abstract 10.1016/j.bjpt.2018.10.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. J Clin Epidemiol 2021;134:178–89. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33789819&dopt=Abstract 10.1016/j.jclinepi.2021.03.001 [DOI] [PubMed] [Google Scholar]
- 21.Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev 2016;5:210. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27919275&dopt=Abstract 10.1186/s13643-016-0384-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. Cochrane Bias Methods Group . Cochrane Statistical Methods Group. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011;343:5928. 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane Handbook for Systematic Reviews of Interventions. Second Edition. Chichester: John Wiley & Sons, 2011. [Google Scholar]
- 24.Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE Working Group . GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336:924–6. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=18436948&dopt=Abstract 10.1136/bmj.39489.470347.AD [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gladwell V, Head S, Haggar M, Beneke R. Does a program of Pilates improve chronic non-specific low back pain? J Sport Rehabil 2006;15:338–50. 10.1123/jsr.15.4.338 [DOI] [Google Scholar]
- 26.Cortell-Tormo JM, Sánchez PT, Chulvi-Medrano I, Tortosa-Martínez J, Manchado-López C, Llana-Belloch S, et al. Effects of functional resistance training on fitness and quality of life in females with chronic nonspecific low-back pain. J Back Musculoskeletal Rehabil 2018;31:95–105. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=28826168&dopt=Abstract 10.3233/BMR-169684 [DOI] [PubMed] [Google Scholar]
- 27.Otadi K, Nakhostin Ansari N, Sharify S, Fakhari Z, Sarafraz H, Aria A, et al. Effects of combining diaphragm training with electrical stimulation on pain, function, and balance in athletes with chronic low back pain: a randomized clinical trial. BMC Sports Sci Med Rehabil 2021;13:20. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33663607&dopt=Abstract 10.1186/s13102-021-00250-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.del Pozo-Cruz B, Hernández Mocholí MA, Adsuar JC, Parraca JA, Muro I, Gusi N. Effects of whole body vibration therapy on main outcome measures for chronic non-specific low back pain: a single-blind randomized controlled trial. J Rehabil Med 2011;43:689–94. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=21687923&dopt=Abstract 10.2340/16501977-0830 [DOI] [PubMed] [Google Scholar]
- 29.Lopes S, Correia C, Félix G, Lopes M, Cruz A, Ribeiro F. Immediate effects of Pilates based therapeutic exercise on postural control of young individuals with non-specific low back pain: A randomized controlled trial. Complement Ther Med 2017;34:104–10. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=28917361&dopt=Abstract 10.1016/j.ctim.2017.08.006 [DOI] [PubMed] [Google Scholar]
- 30.Patti A, Bianco A, Paoli A, Messina G, Montalto MA, Bellafiore M, et al. Pain Perception and Stabilometric Parameters in People With Chronic Low Back Pain After a Pilates Exercise Program: A Randomized Controlled Trial. Medicine (Baltimore) 2016;95:e2414. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=26765419&dopt=Abstract 10.1097/MD.0000000000002414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kuukkanen TM, Mälkiä EA. An experimental controlled study on postural sway and therapeutic exercise in subjects with low back pain. Clin Rehabil 2000;14:192–202. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=10763797&dopt=Abstract 10.1191/026921500667300454 [DOI] [PubMed] [Google Scholar]
- 32.Rhee HS, Kim YH, Sung PS. A randomized controlled trial to determine the effect of spinal stabilization exercise intervention based on pain level and standing balance differences in patients with low back pain. Med Sci Monit 2012;18:CR174–81. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=22367128&dopt=Abstract 10.12659/MSM.882522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ghasemi C, Amiri A, Sarrafzadeh J, Dadgoo M, Jafari H. Comparative study of muscle energy technique, craniosacral therapy, and sensorimotor training effects on postural control in patients with nonspecific chronic low back pain. J Family Med Prim Care 2020;9:978–84. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32318454&dopt=Abstract 10.4103/jfmpc.jfmpc_849_19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Valenza MC, Rodríguez-Torres J, Cabrera-Martos I, Díaz-Pelegrina A, Aguilar-Ferrándiz ME, Castellote-Caballero Y. Results of a Pilates exercise program in patients with chronic non-specific low back pain: a randomized controlled trial. Clin Rehabil 2017;31:753–60. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27260764&dopt=Abstract 10.1177/0269215516651978 [DOI] [PubMed] [Google Scholar]
- 35.Karimi N, Ebrahimi I, Ezzati K, Kahrizi S, Torkaman G, Arab AM. The Effects of consecutive supervised stability training on postural balance in patients with chronic low back pain. Pak J Med Sci 2009;25:177–81. [Google Scholar]
- 36.Kaeding TS, Karch A, Schwarz R, Flor T, Wittke TC, Kück M, et al. Whole-body vibration training as a workplace-based sports activity for employees with chronic low-back pain. Scand J Med Sci Sports 2017;27:2027–39. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=28185300&dopt=Abstract 10.1111/sms.12852 [DOI] [PubMed] [Google Scholar]
- 37.da Silva RA, Vieira ER, Fernandes KB, Andraus RA, Oliveira MR, Sturion LA, et al. People with chronic low back pain have poorer balance than controls in challenging tasks. Disabil Rehabil 2018;40:1294–300. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=28282992&dopt=Abstract 10.1080/09638288.2017.1294627 [DOI] [PubMed] [Google Scholar]
- 38.Hooper TL, James CR, Brismée JM, Rogers TJ, Gilbert KK, Browne KL, et al. Dynamic balance as measured by the Y-Balance Test is reduced in individuals with low back pain: A cross-sectional comparative study. Phys Ther Sport 2016;22:29–34. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27579805&dopt=Abstract 10.1016/j.ptsp.2016.04.006 [DOI] [PubMed] [Google Scholar]
- 39.Ge L, Wang C, Zhou H, Yu Q, Li X. Effects of low back pain on balance performance in elderly people: a systematic review and meta-analysis. Eur Rev Aging Phys Act 2021;18:8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34090345&dopt=Abstract 10.1186/s11556-021-00263-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Panjabi MM. A hypothesis of chronic back pain: ligament subfailure injuries lead to muscle control dysfunction. Eur Spine J 2006;15:668–76. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=16047209&dopt=Abstract 10.1007/s00586-005-0925-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.O’Sullivan PB, Burnett A, Floyd AN, Gadsdon K, Logiudice J, Miller D, et al. Lumbar repositioning deficit in a specific low back pain population. Spine 2003;28:1074–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=12768152&dopt=Abstract 10.1097/01.BRS.0000061990.56113.6F [DOI] [PubMed] [Google Scholar]
- 42.Brumagne S, Cordo P, Lysens R, Verschueren S, Swinnen S. The role of paraspinal muscle spindles in lumbosacral position sense in individuals with and without low back pain. Spine 2000;25:989–94. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=10767813&dopt=Abstract 10.1097/00007632-200004150-00015 [DOI] [PubMed] [Google Scholar]
- 43.Radebold A, Cholewicki J, Polzhofer GK, Greene HS. Impaired postural control of the lumbar spine is associated with delayed muscle response times in patients with chronic idiopathic low back pain. Spine 2001;26:724–30. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=11295888&dopt=Abstract 10.1097/00007632-200104010-00004 [DOI] [PubMed] [Google Scholar]
- 44.O’Connor SM, Kuo AD. Direction-dependent control of balance during walking and standing. J Neurophysiol 2009;102:1411–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=19553493&dopt=Abstract 10.1152/jn.00131.2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bent LR, Inglis JT, McFadyen BJ. When is vestibular information important during walking? J Neurophysiol 2004;92:1269–75. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=15102904&dopt=Abstract 10.1152/jn.01260.2003 [DOI] [PubMed] [Google Scholar]
- 46.Bonnì S, Ponzo V, Tramontano M, Martino Cinnera A, Caltagirone C, Koch G, et al. Neurophysiological and clinical effects of blindfolded balance training (BBT) in Parkinson’s disease patients: a preliminary study. Eur J Phys Rehabil Med 2019;55:176–82. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29745627&dopt=Abstract 10.23736/S1973-9087.18.05126-2 [DOI] [PubMed] [Google Scholar]
- 47.Perry SD, McIlroy WE, Maki BE. The role of plantar cutaneous mechanoreceptors in the control of compensatory stepping reactions evoked by unpredictable, multi-directional perturbation. Brain Res 2000;877:401–6. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=10986360&dopt=Abstract 10.1016/S0006-8993(00)02712-8 [DOI] [PubMed] [Google Scholar]
- 48.Pata RW, Lord K, Lamb J. The effect of Pilates based exercise on mobility, postural stability, and balance in order to decrease fall risk in older adults. J Bodyw Mov Ther 2014;18:361–7. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=25042305&dopt=Abstract 10.1016/j.jbmt.2013.11.002 [DOI] [PubMed] [Google Scholar]
- 49.Bird ML, Hill KD, Fell JW. A randomized controlled study investigating static and dynamic balance in older adults after training with Pilates. Arch Phys Med Rehabil 2012;93:43–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=21975148&dopt=Abstract 10.1016/j.apmr.2011.08.005 [DOI] [PubMed] [Google Scholar]
- 50.Barker AL, Bird ML, Talevski J. Effect of pilates exercise for improving balance in older adults: a systematic review with meta-analysis. Arch Phys Med Rehabil 2015;96:715–23. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=25511371&dopt=Abstract 10.1016/j.apmr.2014.11.021 [DOI] [PubMed] [Google Scholar]
- 51.Bjerkefors A, Ekblom MM, Josefsson K, Thorstensson A. Deep and superficial abdominal muscle activation during trunk stabilization exercises with and without instruction to hollow. Man Ther 2010;15:502–7. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=20570549&dopt=Abstract 10.1016/j.math.2010.05.006 [DOI] [PubMed] [Google Scholar]
- 52.Ruhe A, Fejer R, Walker B. The test-retest reliability of centre of pressure measures in bipedal static task conditions—a systematic review of the literature. Gait Posture 2010;32:436–45. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=20947353&dopt=Abstract 10.1016/j.gaitpost.2010.09.012 [DOI] [PubMed] [Google Scholar]
- 53.O’Neill DE, Gill-Body KM, Krebs DE. Posturography changes do not predict functional performance changes. Am J Otol 1998;19:797–803. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=9831157&dopt=Abstract [PubMed] [Google Scholar]
- 54.Furman JM. Posturography: uses and limitations. Baillieres Clin Neurol 1994;3:501–13. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=7874405&dopt=Abstract [PubMed] [Google Scholar]
- 55.Visser JE, Carpenter MG, van der Kooij H, Bloem BR. The clinical utility of posturography. Clin Neurophysiol 2008;119:2424–36. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=18789756&dopt=Abstract 10.1016/j.clinph.2008.07.220 [DOI] [PubMed] [Google Scholar]
- 56.Omaña H, Bezaire K, Brady K, Davies J, Louwagie N, Power S, et al. Functional Reach Test, Single-Leg Stance Test, and Tinetti Performance-Oriented Mobility Assessment for the Prediction of Falls in Older Adults: A Systematic Review. Phys Ther 2021;101:173. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34244801&dopt=Abstract 10.1093/ptj/pzab173 [DOI] [PubMed] [Google Scholar]
- 57.Gribble PA, Kelly SE, Refshauge KM, Hiller CE. Interrater reliability of the star excursion balance test. J Athl Train 2013;48:621–6. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=24067151&dopt=Abstract 10.4085/1062-6050-48.3.03 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hyong IH, Kim JH. Test of intrarater and interrater reliability for the star excursion balance test. J Phys Ther Sci 2014;26:1139–41. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=25202168&dopt=Abstract 10.1589/jpts.26.1139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hwang JA, Bae SH, Do Kim G, Kim KY. The effects of sensorimotor training on anticipatory postural adjustment of the trunk in chronic low back pain patients. J Phys Ther Sci 2013;25:1189–92. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=24259943&dopt=Abstract 10.1589/jpts.25.1189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Chok B, Lee R, Latimer J, Tan SB. Endurance training of the trunk extensor muscles in people with subacute low back pain. Phys Ther 1999;79:1032–42. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=10534796&dopt=Abstract 10.1093/ptj/79.11.1032 [DOI] [PubMed] [Google Scholar]
- 61.Bagheri R, Parhampour B, Pourahmadi M, Fazeli SH, Takamjani IE, Akbari M, et al. The Effect of Core Stabilization Exercises on Trunk-Pelvis Three-Dimensional Kinematics During Gait in Non-Specific Chronic Low Back Pain. Spine 2019;44:927–36. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=31205170&dopt=Abstract 10.1097/BRS.0000000000002981 [DOI] [PubMed] [Google Scholar]
- 62.Boutron I, Altman DG, Moher D, Schulz KF, Ravaud P, CONSORT NPT Group . CONSORT Statement for Randomized Trials of Nonpharmacologic Treatments: A 2017 Update and a CONSORT Extension for Nonpharmacologic Trial Abstracts. Ann Intern Med 2017;167:40–7. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=28630973&dopt=Abstract 10.7326/M17-0046 [DOI] [PubMed] [Google Scholar]
- 63.Sun J, Freeman BD, Natanson C. Meta-analysis of clinical trials. In: Gallin JI, Ognibene FP, Johnson LL, editors. Principles and practice of clinical research. Fourth Edition. Amsterdam: Elsevier; 2018. p.17–327. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Text File 1
Search strategy.
Supplementary Table I
Main characteristics of the included studies
Supplementary Table II
Description of interventions and main results.








