Abstract
To facilitate the interaction between the health professional and the patient, a framework to guide the rehabilitation process is needed. This framework would encompass three interwoven aspects: the rehabilitation management plan, Individual Rehabilitation Project (IRP), and rehabilitation cycle(s). All three framework aspects focus on the patient and on the aim of rehabilitation, i.e. to optimize a person’s functioning across the continuum of care. An IRP is a multi-element, person-centered rehabilitation management scheme, in which rehabilitation is generally provided by a multiprofessional team under the leadership of a physical and rehabilitation medicine (PRM) physician, working in an interdisciplinary manner and together with the patient (or proxy). A reference system for operationalizing functioning and standardizing the process is the International Classification of Functioning, Disability and Health (ICF) – for assessing functioning needs, defining rehabilitation goals and outcomes. The objective of this paper is to present the IRP as a framework for rehabilitation in Europe (EUR-IRP). The specific aims are: 1) to introduce the IRP; and 2) to describe the framework components, elements and variables of the IRP. Demonstration projects (case studies) using the EUR-IRP will be conducted. The present paper presents the efforts to date for developing the EUR-IRP, a key part of the action plan of the PRM Section and Board of the European Union of Medical Specialists to implement the ICF systemwide across the care continuum. This paper serves as another step to bring together practice, science and governance in calling for contribution from rehabilitation clinicians and researchers and professional societies in PRM and beyond.
Key words: Rehabilitation; International classification of functioning, disability and health; Patient-centered care
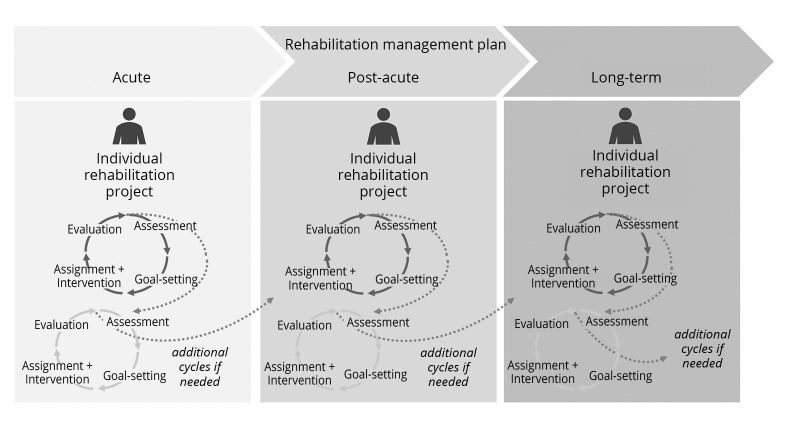
At the forefront of developing standards and frameworks for rehabilitation in Europe is the European Union of Medical Specialists Physical and Rehabilitation Medicine (UEMS-PRM) Section and Board.1 The UEMS-PRM has developed the European framework for rehabilitation service types2 (referred to as “European Framework” from now on) and corresponding clinical assessment schedules (CLASs).3 To facilitate the interaction between the health professional and the patient, a framework to guide the rehabilitation process is needed. This framework would encompass three interwoven aspects: the rehabilitation management plan, Individual Rehabilitation Project (IRP),4, 5 and rehabilitation cycle(s). See Table I2, 5-9 for a brief description of each aspect and Figure 1 illustrating the interface between them.
Table I. —Brief description of the aspects covered by the proposed framework to guide the rehabilitation process in the person-centered care continuum.
| Rehabilitation management plan2, 6-8 | An overarching care provision structure, in which one or more IRP may be used. Rehabilitation can be provided at different stages across the care continuum from acute, to postacute, to long-term. The rehabilitation management plan can be operationalized using the European Framework for rehabilitation service types developed by the UEMS-PRM Section. |
| Individual Rehabilitation Project (IRP)5, 6 | A comprehensive approach for providing rehabilitation services that is inherently person-centered and interdisciplinary. Employed throughout the rehabilitation process, the IRP is developed for each individual patient and comprises one or more rehabilitation cycles. The IRP has a start and an end, and a separate IRP is developed for each service across the care continuum. To support continuity between services, the IRP would ideally incorporate relevant elements from the previous service that would facilitate transition from one service to the next. See Figure 1. |
| Rehabilitation cycle(s)7-9 | An ICF-based approach that facilitates the structuring, organization and documentation of the rehabilitation process. It encompasses the following phases: assessment [diagnosis of health condition and functioning assessment], goal-setting, assignment [of an intervention to specific health professionals] and [conducting] interventions, evaluation [of goal achievement]. Details are provided below. |
Figure 1.
—Interface between the rehabilitation management plan, Individual Rehabilitation Project, and rehabilitation cycles.
All three framework aspects focus on the patient and on the aim of rehabilitation, i.e. to optimize a person’s functioning across the continuum of care.10, 11 As the internationally recognized reference system for operationalizing functioning, the International Classification of Functioning, Disability and Health (ICF)12 can be employed in assessing functioning needs, defining rehabilitation goals and outcomes.
The UEMS-PRM Section is currently elaborating the ICF-based IRP framework to meet its implementation action plan item “development of measurement-for-improvement systems for clinical decision-making in individual patients (microlevel) and continuous improvement of a rehabilitation service (mesolevel)”.1 The objective of this paper is to present the IRP as a framework for rehabilitation in Europe. The specific aims are: 1) to introduce the IRP; and 2) to describe the framework components, elements and variables of the IRP.
Individual Rehabilitation Project
Reflecting the overall tenet of rehabilitation,10 an Individual Rehabilitation Project (IRP) is a multi-element, person-centered rehabilitation management scheme, in which rehabilitation is generally provided by a multi-professional team under the leadership of a physical and rehabilitation medicine (PRM) physician,6 working in an interdisciplinary manner and together with the patient (or proxy accordingly). Depending on the person’s needs, this team could also include non-rehabilitation health professionals. The focus here is on the “individual,” meaning that the rehabilitation provided is tailored to the needs and goals of the specific person for whom the IRP is developed. In a 2020 editorial that outlined a model to strengthen clinical rehabilitation in health systems worldwide, the authors introduced the IRP model developed in Italy as a potential model for other countries.4, 5 The IRP model is congruent with clinical rehabilitation as described in the White Book of PRM in Europe,6 and encompasses the setting of short, intermediate and long-term goals, together with the patient in shared decision-making, including the expected timeframe for achieving the goals, intervention planning and evaluation of goal achievement. Thus, the Italian IRP model is the starting point for the IRP being elaborated by the UEMS-PRM Section.
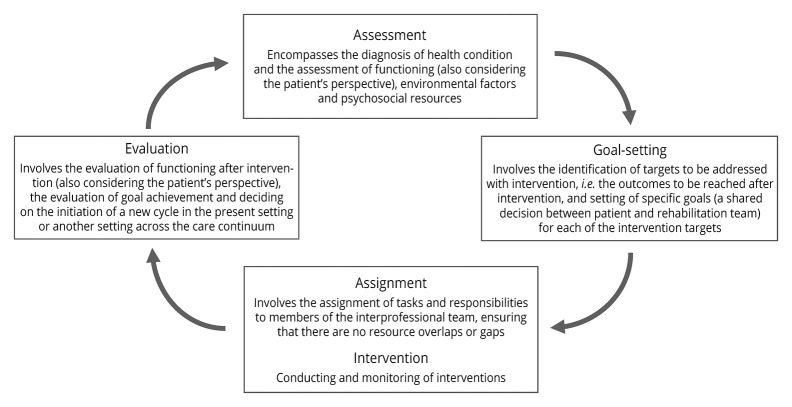
Rehab-Cycle
An essential component of the IRP model is the rehabilitation cycle, also called “Rehab-Cycle.” The Rehab-Cycle can facilitate the coordination of rehabilitation actions, the structuring, organization and documentation of the rehabilitation process, as well as support clinical decision-making, e.g. to plan interventions, to monitor progress and modify interventions, across the care continuum.7-9 Figure 2 outlines the phases of the Rehab-Cycle. The Rehab-Cycle can be iterative, i.e. at the end of each cycle, a new cycle can be initiated if needed to reach desired functioning outcomes, whereby the new cycle starts from the outcomes and learned lessons of the preceding cycle.7-9
Figure 2.
—Phases of the Rehab-Cycle with descriptions.
The Rehab-Cycle relies on the use of the ICF. Documentation templates can be developed for use in each of the Rehab-Cycle phases. ICF-based templates are already available: the ICF Assessment Sheet, Categorical Profile, Intervention Table and Evaluation Display.7-9 The Assessment Sheet is an at-a-glance overview of the person’s functioning problems and resources documented from the perspective of the patient as well as the health professional (rehabilitation team). The Categorical Profile is a visual depiction of the person’s functioning problems based on the cumulative results of the assessment. These problems are depicted with a rating of the problem in respective ICF categories. The Categorical Profile also shows the long-term global goal(s), and the short-term cycle and intermediate service-program goal(s) that the rehabilitation team and the patient want to achieve with interventions. The Intervention Table can be used to document the interventions planned to address specific intervention targets (identified with the categories and goals documented in the Categorical Profile) and the team member(s) assigned to perform specific interventions. The Evaluation Display is basically a before-after depiction of the person’s functioning, showing the Categorical Profile before and another profile after intervention and identifying which goals have been achieved. See the Supplementary Digital Material 1: Supplementary Table I, Supplementary Table II for examples of the Intervention Table and Evaluation Display. The templates can be downloaded from www.icf-research-branch.org.
Like the Rehab-Cycle, the Italian IRP model is seen as a way to structure rehabilitation while also promoting its individualization to address specific person’s functioning outcomes and goals.5
On the path to standardization: the process for refining the IRP
The UEMS-PRM Section systemwide quality management implementation initiative not only promotes the use of the ICF in rehabilitation management, it also aims to facilitate clinical quality management in rehabilitation at the macro-, meso- and micro-levels of care.1 Key to clinical quality management in rehabilitation is the standardized documentation and reporting of functioning outcomes and goals.1, 13, 14 On the path to standardization, the IRP in Italy evolved, and a first proposal for an ICF-based IRP sheet has been developed.15 This unpublished document “Individual Rehabilitation Pathway Sheet” allows the rehabilitation team to document a patient’s diagnoses, and positive (facilitator) and/or negative (barrier) impact of selected environmental factors, create a functioning profile based on ratings of problems in selected functioning domains, set goals based on the functioning profile and propose a post-discharge care pathway. This documentation sheet can inform the development of an IRP scheme for Europe and beyond.
To advance the development of the IRP scheme for Europe (EUR-IRP), the UEMS-PRM Section IRP working group has proposed a list of components, i.e. basic information, Rehab-Cycle and discharge plan, and their corresponding elements and variables (Table II,2, 16-21 Table III,3, 12, 22, 23 Table IV2) that align with the general characteristics of the IRP based on the Italian model ‒ individualized, person-centered, interdisciplinary, optimization of functioning as the aim of rehabilitation, thus ICF-based.
Table II. —BASIC INFORMATION. Proposed elements and corresponding variables of the component “basic information” – all information that are relevant for the rehabilitation process outlined in the Rehab-Cycle component (Table III).
| Element | Variable | Specific information | |
|---|---|---|---|
| Service context | Type of rehabilitation service (using the European Framework)2 | Rehabilitation in acute care General postacute rehabilitation Specialized postacute rehabilitation General outpatient rehabilitation Specialized outpatient rehabilitation General day rehabilitation Specialized day rehabilitation Vocational rehabilitation |
Rehabilitation in the community Rehabilitation services at home Rehabilitation for specific groups of persons with disability Rehabilitation in social assistance Specialized lifelong follow-up rehabilitation Rehabilitation in medical health resorts |
| Information about the service (using ICSO-R)16 | Target group(s), location of service delivery, setting, time & intensity of services, etc. | ||
| Referral information | Referral from which type of health or rehabilitation service2 | Also see above | |
| Mode of referral (using ICSO-R) | Self-referral, referral by health professional, by health service (institution), etc. | ||
| Additional information | To be determined by the service provider as needed | ||
| Patient information | Socio-demographics | Age Gender Civil status (single, married, etc.) Living situation (living alone, living with family, etc.) Work status (employed, self-employed, homemaker, retired, in training, etc.) |
Work incapacity level Reason for work incapacity Education level (primary school, secondary school, trade school, university, etc.) Funding source Other information to be determined by the service provider as needed |
| Primary health condition | International Classification of Diseases (ICD) Code17 | ||
| Comorbidities | International Classification of Diseases (ICD) Code | ||
| Pre-admission documentation on functioning | CLASs (ICF Core Sets18, 19 and ICF Generic Sets20, 21) and other outcomes | ||
| Pre-admission disability level | If disability level is established | ||
ICSO-R: International Classification of Service Organization in Rehabilitation.
Table III. —REHAB-CYCLE. Proposed elements and corresponding variables of the component “Rehab-Cycle.”.
| Element | Variable |
|---|---|
| Assessment | Diagnosis of health condition in detail |
| Functioning status with focus on limitations in body functions and structures and the person’s ability to engage in everyday activities in interaction with environmental factors | |
| Developmental stage for pediatric patients | |
| Environmental factors (barriers and facilitators) | |
| Psychosocial resources that can promote or hinder functioning | |
| Person’s expectations, priorities and desired outcome of rehabilitation (and of caregivers, e.g. for pediatric patients and other patients unable to make decisions on their own) | |
| Rehabilitation potential and functional prognosis | |
| Use of diverse assessment tools (clinical tests and diagnostic tools, patient-reported outcome measures, clinical-administered questionnaires and anamnesis/case history) for gathering evidence on the aforementioned patient data | |
| Documentation of the person’s functioning status according to the designated CLASs3 when possible and using an ICF-based clinical tool, e.g. ClinFIT22 and the service provider’s health information system | |
| Goal-setting | If relevant for the service provider, documentation of the differences in functioning status between capacity (what a person can do with little or no influence of environmental factors on functioning) and performance (what a person can actually do with the support of environmental factors12 |
| Results of the assessment tools and sources of information | |
| Intervention targets (functioning outcomes) using ICF sets employed in the assessment documentation | |
| Shared decision-making between patient (or proxy) and the rehabilitation team on short-term and long-term goals | |
| Involvement of patient proxies, e.g. family, designated caregiver, if relevant | |
| Short-term goals, i.e. goals to be achieved within the present IRP cycle “cycle goals” and goals to be achieve during the episode of care provided by the present rehabilitation service provider “service program goals;” long-term goals “global goals” | |
| Goal setting in consideration of the patient’s psychosocial resources that promote functioning | |
| Documentation of intervention targets and corresponding short-term goals using the service provider’s health information system (if possible) | |
| Assignment and intervention | If relevant for the service provider, capacity and performance goals are set separately and accordingly, the documentation of intervention targets |
| Under the leadership of a PRM physician | |
| Documentation of interventions to be performed and the corresponding rehabilitation team member(s) who is (are) assigned to address each intervention target, possibly using WHO’s International Classification of Health Interventions (ICHI)23 | |
| Monitoring and documentation using the service provider’s health information system (if possible) | |
| Use of the patient’s psychosocial resources to promote functioning | |
| Information on involvement of patient proxies in performing interventions | |
| Evaluation | Mode of collaboration (e.g. interdisciplinary versus multi-disciplinary) |
| Use of diverse assessment tools (clinical tests and diagnostic tools, patient-reported outcome measures, clinical-administered questionnaires and anamnesis/case history) for gathering evidence on the aforementioned patient data | |
| Achievement of goals set | |
| Change in functioning profile, environmental factors, psychosocial resources based on information collected and observed during the whole rehabilitation process | |
| Change in primary health condition and comorbidities if relevant | |
| Presence of complications | |
| Documentation of change in functioning status and goal achievement using the service provider’s health information system (if possible) | |
| If relevant for the service provider, achievement of the capacity and performance goals are documented |
Table IV. —DISCHARGE PLAN. Proposed elements and corresponding variables of the component “discharge plan.”.
| Element | Variable |
|---|---|
| Discharge information | Shared decision-making between patient (and proxies, if relevant) and the rehabilitation team about a potential new cycle or decision to discharge |
| Pharmacological therapy and indication of the activity of daily living to be maintained (in case of home setting discharge) | |
| Non-pharmacological interventions related to lifestyle, habits, diet, use of devices, etc.) | |
| Results of diverse assessment tools (clinical tests and diagnostic tools, patient-reported outcome measures, clinical-administered questionnaires and anamnesis/case history) | |
| Functional profile at discharge | |
| Discharge setting (home or nursing facility, rehabilitation service) | |
| Type of rehabilitation service2 if continued services are planned | |
| Information on funding source | |
| Guidance and training of patient and family | |
| Provision of prosthetic, orthotic and/or assistive devices | |
| Potential architectural arrangements for home and/or work as well as car adaptations, if needed | |
| Other discharge information to be determined by service provider as needed |
The use of the ICF on the path to standardization has been well documented in scientific literature.13, 14, 24-28 Reflected in the proposed Rehab-Cycle elements of the EUR-IRP, standardized reporting of functioning outcomes employs ICF Core Sets and ICF Generic Sets.18-21 These ICF Sets (accessible at www.icf-core-sets.org) can be applied using the aforementioned ICF-based documentation tools developed for the Rehab-Cycle.7-9
Discussion
This paper has outlined the building blocks of the EUR-IRP, a person-centered and interdisciplinary ICF-based rehabilitation management scheme for the assessment and reporting of patient functioning across the care continuum. Until now, there is no rehabilitation management scheme that is comparable to the comprehensiveness of the EUR-IRP in Europe.
Crossing frontiers
The EUR-IRP envisioned by UEMS-PRM Section crosses several frontiers. First, it crosses the boundaries of use. The EUR-IRP can also be used across various rehabilitation types across the continuum of care and along the life course.1, 2 Moreover, the UEMS-PRM Section envisions that the EUR-IRP can be tailored for specific purposes, such as rehabilitation in emergency and disaster relief.1 And in light of COVID-19, the EUR-IRP has potential in assessing and reporting functioning outcomes related to post-intensive care syndrome in acute rehabilitation and in tele-rehabilitation in the postacute and long-term context. It also crosses “geo-socioeconomic” frontiers. Although UEMS-PRM is developing the EUR-IRP for Europe, it can be tailored for countries outside of Europe and low- and middle-income countries as well.1, 5 The application of the IRP can range from being simple to more comprehensive depending on the complexity of the patient’s health situation and on the specific context in which the IRP is being applied.
Demonstration projects are needed to test the versatility of the IRP scheme and its applicability in diverse areas.
Demonstration projects
The UEMS-PRM Section has planned demonstration projects (case studies) using the EUR-IRP described in this paper to be conducted by UEMS-PRM country delegates. Non-UEMS-PRM societies, including professional societies beyond PRM are also welcomed to join the efforts in conducting demonstration projects. In an initial step, the IRP working group will develop an instructions manual that will outline the demonstration project steps as well as detail how to employ the EUR-IRP in different rehabilitation service types. The demonstration projects are expected to showcase how the EUR-IRP can be implemented in countries all over Europe, across rehabilitation service types according to the European Framework,2 by different rehabilitation professionals, and in different use cases as exemplified in the previous section.
In addition to testing the applicability and potential utility of EUR-IRP, the demonstration projects could also serve other purposes. For example, demonstration projects that focus on specific health conditions and different age groups from children to the geriatric population, if sufficient in numbers, may help clarify potential condition-specific care pathways and needs of different age groups. In principle, the EUR-IRP, possibly with some modifications, can be applied to each and every individual experiencing disability or at risk of developing disability at any age.
The case studies may also be useful for teaching purposes, e.g. in the training of health professionals on clinical decision-making and interdisciplinary teamwork.
Future demonstration projects or research could explore methods that may further strengthen the patient centeredness of the EUR-IRP, such as narrative medicine, an emerging method of translating patient’s stories and patient-health professional discussions into outcomes and the foundation for clinical decisions. This method combined with the use of functioning-based questions was exemplified in a study that differentiated between capacity and performance of patients with amyotrophic lateral sclerosis (ALS) and highlighted the environmental factors that were either facilitators or barriers to patient functioning at home and in the community.29 A similar project in the context of an implemented EUR-IRP could be conducted in the future.
Conclusions
The present paper presents the efforts to date for developing the EUR-IRP, a framework for rehabilitation in Europe and a key part of UEMS-PRM’s action plan to implement the ICF systemwide across the care continuum. The UEMS-PRM envisions the EUR-IRP as a tool for documenting patients’ functioning outcomes, rehabilitation needs and prognosis in a more nuanced way, as well as for individualizing rehabilitation management, and in supporting meso-level clinical quality management in rehabilitation and efforts to improve national policy on rehabilitation. This paper serves as another step “to bring together practice, science and governance”1 in calling for contribution from rehabilitation clinicians and researchers and professional societies in PRM and beyond.
Supplementary Digital Material 1
Supplementary Table I
Intervention table (excerpt from an ICF-based case study of a person with spinal cord injury).a
Supplementary Table II
Evaluation display: includes the categorical profile (excerpt from an ICF-based case study of a person with spinal cord injury).
References
- 1.Stucki G, Zampolini M, Juocevicius A, Negrini S, Christodoulou N. Practice, science and governance in interaction: European effort for the system-wide implementation of the International Classification of Functioning, Disability and Health (ICF) in Physical and Rehabilitation Medicine. Eur J Phys Rehabil Med 2017;53:299–307. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27882907&dopt=Abstract 10.23736/S1973-9087.16.04436-1 [DOI] [PubMed] [Google Scholar]
- 2.Stucki G, Zampolini M, Selb M, Ceravolo MG, Delargy M, Varela Donoso E, et al. Study Group European Framework of Rehabilitation Service Types . European Framework of Rehabilitation Services Types: the perspective of the Physical and Rehabilitation Medicine Section and Board of the European Union of Medical Specialists. Eur J Phys Rehabil Med 2019;55:411–7. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30868836&dopt=Abstract 10.23736/S1973-9087.19.05728-9 [DOI] [PubMed] [Google Scholar]
- 3.Selb M, Zampolini M, Delargy M, Kiekens C, Stucki G, Study Group Clinical Assessment Schedule . Specifying clinical assessment schedules for the European framework of rehabilitation service types: the perspective of the physical and rehabilitation medicine Section and Board of the European Union of Medical Specialists. Eur J Phys Rehabil Med 2019;55:834–44. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=31583877&dopt=Abstract 10.23736/S1973-9087.19.05961-6 [DOI] [PubMed] [Google Scholar]
- 4.S.I.M.F.E.R. (Italian Society of Physical and Rehabilitation Medicine) . Guidelines for rehabilitation services in Italy. Eura Medicophys 2005;41:95–109. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=16175774&dopt=Abstract [PubMed] [Google Scholar]
- 5.Zampolini M, Stucki G, Giustini A, Negrini S. The individual rehabilitation project: a model to strengthen clinical rehabilitation in health systems worldwide. Eur J Phys Rehabil Med 2020;56:1–4. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=31797660&dopt=Abstract 10.23736/S1973-9087.19.06110-0 [DOI] [PubMed] [Google Scholar]
- 6.European Physical and Rehabilitation Medicine Bodies Alliance . White Book on Physical and Rehabilitation Medicine (PRM) in Europe. Chapter 3. A primary medical specialty: the fundamentals of PRM. Eur J Phys Rehabil Med 2018;54:177–85. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29565104&dopt=Abstract 10.23736/S1973-9087.18.05146-8 [DOI] [PubMed] [Google Scholar]
- 7.Rauch A, Cieza A, Stucki G. How to apply the International Classification of Functioning, Disability and Health (ICF) for rehabilitation management in clinical practice. Eur J Phys Rehabil Med 2008;44:329–42. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=18762742&dopt=Abstract [PubMed] [Google Scholar]
- 8.Stucki G, Bickenbach J, Selb M, Melvin J. Chapter 9: The International Classification of Functioning, Disability and Health. In: Frontera W, DeLisa J, Gans B, Robinson L, Bockeneck W, Chase J, editors. DeLisa’s Physical medicine and rehabilitation: principles and practice. Sixth Edition. Philadelphia, PA: Wolters Kluwer; 2019. p.208–26. [Google Scholar]
- 9.Swiss Paraplegic Research. Translating interventions into real-life gains - A Rehab-Cycle Approach. ICF; [Internet]. Available from: www.icf-casestudies.org [cited 2022, Feb 08].
- 10.World Health Organization. Rehabilitation fact sheet. Geneva, Switzerland: World Health Organization; 2021 [Internet]. Available from: https://www.who.int/news-room/fact-sheets/detail/rehabilitation [cited 2022, Feb 08].
- 11.Cieza A, Causey K, Kamenov K, Hanson SW, Chatterji S, Vos T. Global estimates of the need for rehabilitation based on the Global Burden of Disease study 2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2021;396:2006–17. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33275908&dopt=Abstract 10.1016/S0140-6736(20)32340-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.World Health Organization. International Classification of Functioning, Disability and Health. Geneva: World Health Organization; 2001. [Google Scholar]
- 13.Stucki G, Prodinger B, Bickenbach J. Four steps to follow when documenting functioning with the International Classification of Functioning, Disability and Health. Eur J Phys Rehabil Med 2017;53:144–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=28118697&dopt=Abstract 10.23736/S1973-9087.17.04569-5 [DOI] [PubMed] [Google Scholar]
- 14.Prodinger B, Tennant A, Stucki G. Standardized reporting of functioning information on ICF-based common metrics. Eur J Phys Rehabil Med 2018;54:110–7. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=28534606&dopt=Abstract 10.23736/S1973-9087.17.04784-0 [DOI] [PubMed] [Google Scholar]
- 15.Regione Umbria. Scheda percorso riabilitativo unico. Regione Umbria; [Internet]. Available from: https://www.regione.umbria.it/home [cited 2022, Feb 08].
- 16.Gutenbrunner C, Nugraha B, Gimigliano F, Meyer T, Kiekens C. International Classification of Service Organization in Rehabilitation: an updated set of categories (ICSO-R 2.0). J Rehabil Med 2020;52:jrm00004. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=31720692&dopt=Abstract 10.2340/16501977-2627 [DOI] [PubMed]
- 17.World Health Organization. International Classification of Diseases. Eleventh Revision. Geneva: World Health Organization; 2021. [Google Scholar]
- 18.Selb M, Escorpizo R, Kostanjsek N, Stucki G, Üstün B, Cieza A. A guide on how to develop an International Classification of Functioning, Disability and Health Core Set. Eur J Phys Rehabil Med 2015;51:105–17. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=24686893&dopt=Abstract [PubMed] [Google Scholar]
- 19.Selb M, Cieza A. ICF Core Sets. In: Bickenbach J, Cieza A, Selb M, Stucki G, editors. ICF Core Sets: manual for clinical practice. Second Edition. Göttingen: Hogrefe Publishing; 2020. p.15–22. [Google Scholar]
- 20.Cieza A, Oberhauser C, Bickenbach J, Chatterji S, Stucki G. Towards a minimal generic set of domains of functioning and health. BMC Public Health 2014;14:218. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=24588794&dopt=Abstract 10.1186/1471-2458-14-218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Prodinger B, Cieza A, Oberhauser C, Bickenbach J, Üstün TB, Chatterji S, et al. Toward the International Classification of Functioning, Disability and Health (ICF) Rehabilitation Set: A Minimal Generic Set of Domains for Rehabilitation as a Health Strategy. Arch Phys Med Rehabil 2016;97:875–84. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=26827829&dopt=Abstract 10.1016/j.apmr.2015.12.030 [DOI] [PubMed] [Google Scholar]
- 22.Frontera W, Gimigliano F, Melvin J, Li J, Li L, Lains J, et al. ClinFIT: ISPRM’s Universal Functioning Information Tool based on the WHO’s ICF. J Int Soc Phys Rehabil Med 2019;2:19–21. 10.4103/jisprm.jisprm_36_19 [DOI] [Google Scholar]
- 23.Fortune N, Madden R, Almborg AH. Use of a New International Classification of Health Interventions for Capturing Information on Health Interventions Relevant to People with Disabilities. Int J Environ Res Public Health 2018;15:145. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29342077&dopt=Abstract 10.3390/ijerph15010145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dorjbal D, Cieza A, Gmünder HP, Scheel-Sailer A, Stucki G, Üstün TB, et al. Strengthening quality of care through standardized reporting based on the World Health Organization’s reference classifications. Int J Qual Health Care 2016;28:626–33. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27566981&dopt=Abstract 10.1093/intqhc/mzw078 [DOI] [PubMed] [Google Scholar]
- 25.Prodinger B, Ballert CS, Brach M, Brinkhof MW, Cieza A, Hug K, et al. ; SwiSCI Study Group. Toward standardized reporting for a cohort study on functioning: The Swiss Spinal Cord Injury Cohort Study. J Rehabil Med 2016;48:189–96. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=26926922&dopt=Abstract 10.2340/16501977-2026 [DOI] [PubMed] [Google Scholar]
- 26.Prodinger B, Stamm T, Peterson D, Stucki G, Tennant A, International Classification of Functioning, Disability, and Health Info Network . Toward a Standardized Reporting of Outcomes in Hand Osteoarthritis: Developing a Common Metric of Outcome Measures Commonly Used to Assess Functioning. Arthritis Care Res (Hoboken) 2016;68:1115–27. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=26663476&dopt=Abstract 10.1002/acr.22816 [DOI] [PubMed] [Google Scholar]
- 27.Maritz R, Ehrmann C, Prodinger B, Tennant A, Stucki G. The influence and added value of a Standardized Assessment and Reporting System for functioning outcomes upon national rehabilitation quality reports. Int J Qual Health Care 2020;32:379–87. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32472134&dopt=Abstract 10.1093/intqhc/mzaa058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Maritz R, Tennant A, Fellinghauer C, Stucki G, Prodinger B. Creating a common metric based on existing activities of daily living tools to enable standardized reporting of functioning outcomes achieved during rehabilitation. J Rehabil Med 2020;52:jrm00085. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32719883&dopt=Abstract 10.2340/16501977-2711 [DOI] [PubMed]
- 29.Ciotti S, Bianconi F, Saraceni VM, Vulpiani MC, Rinonapoli G, Caraffa A, et al. Narrative Medicine in Amyotrophic Lateral Sclerosis and a Rehabilitation Project Based on International Classification of Functioning, Disability and Health. Am J Phys Med Rehabil 2018;97:832–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29870404&dopt=Abstract 10.1097/PHM.0000000000000978 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table I
Intervention table (excerpt from an ICF-based case study of a person with spinal cord injury).a
Supplementary Table II
Evaluation display: includes the categorical profile (excerpt from an ICF-based case study of a person with spinal cord injury).