ABSTRACT
Policies and programs to increase vaccine coverage rates among adults 50 years of age or older are limited and vaccine uptake is often suboptimal. Our review evaluated evidence on the effectiveness and success of adult-targeted vaccination interventions and identified literature gaps. Literature was retrieved (2021) from PubMed, Embase, and Google Scholar databases. Outcomes assessed included data on an intervention’s effectiveness and impact on vaccine uptake. Interventions were characterized thematically: affordability (n = 9), awareness (n = 25), and vaccination access (n = 6); and included influenza, pneumococcal, tetanus-containing, and herpes zoster vaccines. Interactive interventions directed toward patients, including provider-led educational initiatives and provider recommendations showed more positive associations than less interactive interventions, such as posters and reminder-recall letters. Provider interventions, including awareness campaigns, incentives, affordability efforts, or vaccination site expansion generally showed positive associations. Combining interventions was found to be successful across several studies. Barriers and interventions varied for population subgroups, therefore, tailoring programs is critical.
KEYWORDS: Older adults, routine adult vaccination, vaccination program, intervention, evidence-based, policy
Introduction
Immunization is a critical public health intervention, with vaccinations preventing illness and death from more than 20 vaccine-preventable diseases.1 While most vaccination policies and programs target infants and young children, the benefits of adult vaccination, in terms of health and productivity, are significant.2 Prioritizing vaccination among older adults, individuals 50 years of age or older, is crucial, as the severity of vaccine-preventable disease and complications can increase with age due to waning antibody protection, immunosenescence, and chronic age-associated conditions which can reduce immunity.3 As the global population ages, increasing vaccine uptake among older adults will become even more important. By 2050, one in six people are expected to be over the age of 65, with rapid growth expected in certain regions of Northern Africa, Asia, and Latin America.4 This demographic trend demands investment into the establishment and delivery of national programs that target older adults.
Despite the importance of adult vaccination, vaccine coverage rates (VCRs) among older adults are suboptimal.5,6 Policies and programs addressing adult vaccination are fragmented and inconsistent; even when targets are set by collaborating global and national organizations (e.g., World Health Organization (WHO), National Immunization Technical Advisory Groups (NITAG)), vaccination policies set by governments may not align or provide sufficient support for targeted vaccination coverage goals.5,6 For example, of 30 European Union countries, 21 have general age-based recommendations for pneumococcal vaccination for adults, however only 12 of those provide funding through a national health system or national immunization program (NIP).7 Additionally, adult VCRs are inconsistently measured across countries, complicating comparative assessments of vaccine uptake.8,9 Adult immunization programs often lack the infrastructure to aggregate relevant data, which can lead to decreased understanding and underestimation of the burden and impact of coverage, particularly in low- and middle-income countries (LMICs).10
The COVID-19 pandemic strained already inadequate healthcare infrastructure and exposed the need to improve vaccine access for older adults. Adults in all countries reported missed and delayed immunizations, often due to clinics closing or infection concerns among immunosuppressed individuals; this burden fell harder on LMICs than high-income countries (9.6% vs. 3.4%, p < .05).11
Countries have implemented various policies and interventions designed to increase adult VCRs, reduce financial barriers, raise vaccination awareness, and improve access to vaccinations.12 However, few studies assess the effectiveness of these policies and programs, thereby slowing widespread adoption of effective solutions. Understanding the impact, and effectiveness of successful program and policy interventions can inform efforts to improve and sustain adult VCRs. This study builds on the current literature, reviewing evidence on impact, effectiveness, and drivers of targeted vaccination policies and programs and identifies gaps in the literature surrounding vaccination policies and programs for adults 50 years of age or older. This work also is in support of the WHO’s priority for a life-course approach to vaccination and their Immunization Agenda 2030 (IA2030) has built on a life-course approach to immunization (with the goal of all individuals benefiting from recommended vaccinations regardless of their age by vaccination services integrated with other essential health services), as a strategic priority. This is a critical step to investing in and building infrastructure and support for older adult vaccination.1
Methods
To characterize interventions aimed at increasing VCRs among older adult groups, defined as individuals 50 years of age and older, a systematic literature review was conducted on 1 February 2021, using PubMed and Embase, in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.13 To gain further insights into the policy and intervention literature, search criteria were expanded, and a subsequent search was conducted on 22 December 2021, using PubMed and Google Scholar. The subsequent search strategy attempted to capture interventions that were underrepresented in the initial review to further address gaps in relevant outcomes related to awareness and affordability. The subsequent search was conducted in accordance with the principles of narrative synthesis in systematic reviews and the PRISMA guidelines.13,14 The initial and subsequent search algorithms and keywords are shown in Supplementary Tables S1-S4.
Identified studies were screened to remove duplicates and determine eligibility using the inclusion and exclusion criteria outlined in Table 1. Studies were selected through a 2-phased process, which is illustrated in Figure 1. The first phase screened titles and abstracts to determine study design, vaccine(s) studied, policy or program(s) implemented, and geographic location. The second phase reviewed full-text publications with elements of interest extracted and stored in a repository. All inclusions and exclusions were confirmed by two different reviewers.
Table 1.
Inclusion and exclusion criteria.
| Inclusion criteria | Exclusion criteria | |
|---|---|---|
| Population | Human population 50 years of age and older | Less than 50 years of age; populations out of scope (e.g., pregnant women and healthcare professionals) |
| Intervention | Routine vaccination programs | Vaccines out of scope (e.g., travel vaccines) |
| Comparator | Not applicable | Not applicable |
| Outcomes | Barriers and drivers (e.g., access, behaviors and beliefs, availability of information, affordability, advocacy, policy) | Outcomes out of scope (e.g., studies investigating vaccine immunogenicity, efficacy, effectiveness); not about vaccines/vaccination or secondary outcomes |
| Study design | Any (except editorial or commentary paper) | Secondary research; editorial or commentary |
| Other | Written in English; published January 1, 2016 to December 22, 2021 |
Figure 1.
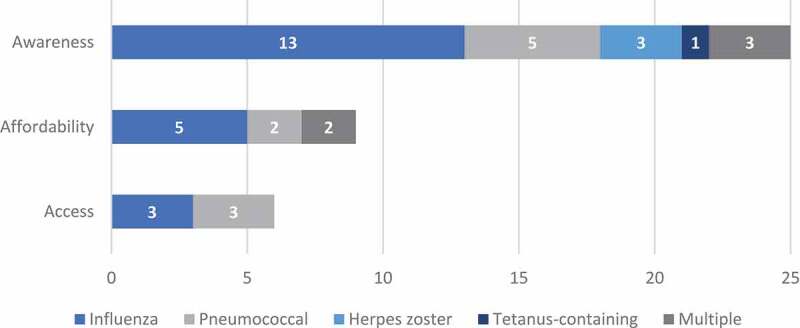
Number of studies per category and vaccine type (n = 40 studies).
We extracted the following items from each selected study: title, authors, country/countries of origin, study design, study setting, number of subjects, and analysis type. When available, the vaccine type(s) being studied and outcomes reported, including quantitative data on vaccine uptake, were captured. All data were logged into an Excel spreadsheet by two reviewers and checked for accuracy by a third reviewer. All included studies analyzed the impact of program or policy interventions on VCRs among adults 50 years of age and older. Significance values related to outcomes of interest were included when applicable; however, not all studies were designed to assess and include statistical analysis.
After initial data extraction, a thematic analysis was conducted and interventions were grouped into three categories: affordability, awareness, or vaccination access. Descriptions of intervention categories, including the types of interventions assessed, are detailed below and in Supplementary Table S5. Affordability intervention studies assessed government-funded vaccination programs, co-payment programs and monetary incentive programs. Awareness interventions included assessments patients and healthcare professionals (HCPs) and the role of vaccination reminders, media coverage of vaccines, and other education initiatives. Access interventions studies included the expansion of vaccination sites and vaccinators.
Results
The initial search identified 2,674 results, of which 85 were identified for further review. From this review, 24 studies reported policy/program-related determinants of vaccine uptake and were selected for full-text review. The subsequent literature review returned 6,864 results, of which 116 publications were identified for further review and 16 studies were subsequently selected for full-text review. Figure 1 describes the selection of the final 40 studies reporting policy/programmatic-related determinants of vaccine uptake included in this literature review. The studies were diverse in geographic region and included studies from North America (n = 17), Asia (n = 13), Europe (n = 6), and Africa and the Middle East (n = 4). Characterizations of vaccinations used and regions where the studies were conducted are included in Figure 1 and Supplementary Figures #1–3. Across the three thematic categories interventions for each category included: affordability (n = 9), awareness (n = 25), and access (n = 6). Characteristics of all selected studies (e.g., population size, location, study dates) are further detailed in Supplementary Table S6.
Affordability interventions
Government-funded vaccination programs
Government funded national vaccination programs have been found to increase older adult vaccination rates. Japan’s national pneumococcal vaccination program doubled VCRs (2–5% in 2009–2014 to 10–11% in 2014–2018) following implementation, and the six-month gradient of increase in cumulative VCRs rose from 2.2% to 3.7% (p < .001).15 In Korea, pneumococcal VCRs of adults ≥65 years old increased from 5% to 57.3% in the 20 months following the introduction of pneumococcal vaccination into the Korean National Immunization Program (p < .0001).16 Similar impacts were observed in Australia, where herpes zoster vaccinations recorded in SmartVax (an immunization data software) rose from an average of 1–18 per month in the 1.5 years before government funded vaccination program implementation to > 500 per month in the three-years following implementation.17 In Italy, influenza VCRs were 70–90% higher (p < .05) in adults eligible for government funded vaccination (aged ≥65) compared to those ineligible.18
Studies comparing vaccination rates in areas with and without government funded influenza vaccination programs provided mixed results. A comparison of 12 Chinese counties found that influenza VCRs among older adults were significantly higher in the six counties with government funded vaccination programs compared to the six without funding (81.1% vs 68.45%, p < .001).19 However, a similar study of 23 European countries found a correlation between government funded influenza vaccination programs and country level vaccination rates, though the finding was only borderline significant (r = 0.43, p = .053).20
Copay programs
Co-payment (fixed amount paid by the patient out-of-pocket after their deductible is paid) policies were found to have mixed results on VCRs. A US claims analysis of adults ≥65 found that increasing copays for tetanus, diphtheria, and pertussis (Tdap) and herpes zoster vaccinations was associated with higher “cancel status” (i.e., provider examined the persons’s coverage level but did not submit a claim), with adjusted odds ratios for a canceled claim estimated to be 1.19 ($1–25 copay), 1.76 ($26–50), 2.42 ($51–75) and 2.40 ($76–100) (all p < .001).21 However, another study of adults ≥65 enrolled in a US-based managed care organization found that increased herpes zoster VCRs among enrollees following removal of a $20–40 copay was not significantly different than increases observed in comparator populations where copay policies were unchanged (difference in rate ratio = 0.04, p > .05).22
Monetary incentives
Monetary incentives for individuals and providers were associated with higher vaccine uptake. A Singapore study offered adults ≥65 years of age shopping vouchers for returning a survey with proof of influenza vaccination. Increasing the shopping voucher amount from 10 to 20 Singaporean Dollars (SGD) increased survey return rates from 4.5% to 7.5% (p = .006), but a further increase from 20 to 30 SGD did not significantly change the return rate (7.5% to 9.2%, p > .05).23 A study comparing 23 European countries found that policies providing additional vaccine administration payments to providers correlated with higher influenza vaccination rates in older adults (age varied by country but individuals at least ≥59 years of age) at the country level (r = 0.53, p = .018).20
Awareness interventions
Reminders
Studies assessing the impact of reminder programs on vaccine uptake, including patient and provider reminders, found text messaging was minimally effective with adult patients. A UK study of adults at risk due to a chronic condition aged 18–64 years found that text message reminders increased vaccination uptake by 2.6% however, this value was not significant (p = .58). There were no differences for age groups in the subanalysis including those aged 51–64 years (OR = 1.10; 95% CI 0.98 to 1.24).24 However, another US study found that while patient portal (a secure website allowing patients online access to their health information) reminders had a significant impact on influenza VCRs among all patients (ages 0.5mo+), there was no significant impact on uptake among adults ≥65 year of age, with VCRs of 53.2, 53.1, 53.0, and 53.8% among individuals receiving 0, 1, 2, and 3 reminders, respectively (p = .31).25
Provider vaccination reminders had a positive impact on vaccine uptake in two US-based studies. In one study, some pharmacies received active reporting of individuals with vaccination gaps. Reports regarding gaps in vaccination were then entered into a system to remind pharmacists to provide additional vaccination consultation upon the person’s next presentation. Individuals 65–89 years of age visiting these pharmacies were 1.7 times more likely to receive the pneumococcal vaccine than those visiting control pharmacies (16.1% vs 10.2%, p < .0001).26 Additionally, following implementation of a vaccination reminder tool for providers, pneumococcal VCRs increased from 1.4% to 25% among hospitalized veterans ≥65 years of age (p = .0003).27
Implementing workflow redesign (i.e., pending vaccination orders prior to patient visit) paired with provider reminders had mixed impacts on vaccination rates in three North American studies. A study of herpes zoster vaccination among people ≥60 years of age living with HIV found that, starting from a baseline of 21.3% of eligible persons vaccinated, an additional 8.3% were vaccinated after implementing provider vaccination prompts. An additional 17.3% were vaccinated after prompts from the individuals electronic medical record (EMR).28 Persons ≥65 years of age consulting with providers who received pneumococcal vaccination EMR reminders were 2.61 times (95% CI 1.18–6.10) more likely to be vaccinated than those in the control group (20% vs 8.7%).29 Another study found that in three out of four groups studied, passive EMR health maintenance notifications (alerts staff when patient records are reviewed with the patient in the room) were more effective than best practice alerts (follow-up pop-up message) or workflow redesign in promoting pneumococcal vaccination series completion among immunocompetent adults ≥65 years of age.30
Media coverage
Both positive and negative media coverage of vaccines and vaccine-preventable diseases impact vaccination rates. Following monthly assessment of news reports between 2010–2017, one study found that for every additional 100 influenza media reports published in October, there was an associated 0.3% point increase in VCRs of adults ≥65 years of age.31 A study in Italy observed the inverse relationship between media coverage and vaccination, attributing a 6.2% decrease in influenza VCRs among adults ≥65 years of age to news reports of 10 deaths related to an influenza vaccine.32
Education
Educational initiatives with the aim of increasing VCRs, varied in methods such as using passive or active distribution of written education materials, discussions with providers, physician recommendations, and provider education. Reviewing the use of informational materials, one US study of Medicare beneficiaries >65 years of age found that individuals who received an informational letter about influenza vaccination were significantly more likely to be vaccinated than those who did not receive the information (adjusted Hazard Ratio between 0.4 and 0.5, p < .01).33 However, a French study found that informational pamphlets and posters in general practitioner (GP) waiting rooms had no significant impact on influenza VCRs among adults ≥65 years of age (RR = 1.01, p = .561).34
Seven studies found a positive association between vaccination and direct patient education by HCPs. Compared to control groups, influenza VCRs were higher in adults ≥65 years old who received provider-led education (i.e., face-to-face discussions about vaccination) in Hong Kong (33.6% vs 25.0%, p = .021)35 and in Beijing (average age 67.5 years) (45.8% vs 27.4%, p < .001).36 Similarly, implementing pharmacist-led vaccination education and counseling was associated with an increase in pneumococcal VCRs of adults ≥65 years old from 0.5% to 1.9% (p = .008) in Jordan.37 Influenza vaccine uptake rose 51% among adults ≥65 years old in Israel who initially indicated an unwillingness to receive an influenza vaccination (as measured during pre-intervention questioning), after provision of provider-led education on the relationship between influenza and vascular events.38 A pharmacist-led intervention in the US involving a formal presentation, live skit, action planning, and optional vaccination resulted in 37.2% of previously unvaccinated individuals reporting pneumococcal vaccination at three-month follow-up.39
Five studies evaluating the recommendation from a provider to be vaccinated and VCRs had significant positive associations. After implementing GP recommendations, pneumococcal VCRs increased from 2.5% to 73.5% among adults ≥65 years old in Turkey. Notably, 75.5% of study participants were unaware of the pneumococcal vaccine prior to the intervention (as measured in face-to-face and phone questionnaires).40 Another Turkish study found that in the year following a GP vaccination recommendation for pneumococcal (6% to 21%, p < .001), influenza (18% to 35%, p < .001), and Tdap (5% to 8%, p = .21) vaccination rates rose among adults ≥65 years old.41 Surveys in Japan and China also found a correlation between provider recommendation and vaccination among older adults for pneumococcal (age ≥60, OR = 8.50, p < .001)42 and influenza (age ≥65, OR = 2.647, p < .010) vaccinations, respectively.43 Expanding vaccination clinics with a physician recommendation further increased VCR. Residents of a Chinese neighborhood that had additional pop-up vaccination clinics had greater access to provider recommendations for influenza vaccination than a control neighborhood (19% vs 0.4%, p < .01).44
Four studies assessed educational initiatives directed toward US providers to help increase vaccination uptake. Following a nurse practitioner-directed vaccination best practices educational initiative at two clinics, VCRs among their patients ≥65 year old rose significantly for pneumococcal (13-valent 52.4% to 55.6% at clinic one, 10.7% to 15.3% at clinic two; 23-valent 41.8% to 45.9% at clinic one, 28.0% to 32.7% at clinic two, p < .01) and Tdap (19.8% to 22.2% at clinic one, 20.7% to 27.3% at clinic two, p < .001) but non-significantly for influenza and herpes zoster (p > .05).45 An initiative including both patient (i.e., television public announcements, mailings) and provider education (i.e., lectures, case studies, workflow redesign) increased VCRs among adults ≥65 years old for influenza (35% to 53%, p < .01) and pneumococcal (23-valent formulation, 62.5% to 64%, p = .12 and 13-valent formulation 40% to 60%, p < .01).46 Implementing the HCP 4 Pillars Program47 which prioritizes convenient vaccination, communication with patients, enhanced office systems to facilitate immunization, and motivation through an office vaccination champion, produced mixed results. The program increased VCRs from baseline among adults 18–64 years old with high-risk conditions for pneumococcal (+12.2 PP), Tdap (+11.4 PP), and influenza (+4.8 PP) vaccinations (p < .001 for all) and vaccination was significantly associated with older age.48 However, a study evaluating the impact on adults ≥50 years old found that after adjusting for clustering and demographic factors, the program implementation did not increase pneumococcal vaccination rates in Pittsburgh, PA (HR = 1.03, p = .830) or Houston, TX (HR = 1.33, p = .110).49
Access interventions
Expanding vaccination sites and vaccinators
The impact of expanding vaccination sites varied by country and study
After increasing vaccine administration sites from one to seven sites on a small Japanese island, influenza VCRs for adults ≥60 years old increased significantly more than the national average (38% to 58% vs 49% to 53%) over a 10-year period.50 However, a study across regions in Italy found no significant association between the ratio of vaccine clinics to adult ≥65 year old population and influenza VCRs across regions.51 Additionally, an effort in Korea to encourage influenza vaccination uptake by increasing provider choice and expanding vaccination sites from publicly-run health clinics only to both publicly- and privately-run health clinics at no cost to the patient did not increase overall VCRs among adults aged ≥55 years.52
Other expansion efforts, such as the increase in vaccinator and provider choice, and the extension of vaccination offered at other types of presentation for care (e.g., medical encounters) were positively associated with increased VCRs. In Canada, influenza VCRs among adults ≥65 years old increased from 61.8% (95% CI = 61.5–62.0%) to 71.6% (95% CI = 71.6–71.8%) following implementation of pharmacist vaccination policy.53 Influenza vaccination rates were higher in provinces with a pharmacist vaccinator policy compared with those without (adjusted prevalence ratio = 1.13, 95% CI = 1.02–1.08).54 Further, offering vaccination to patients seeking medical care for other reasons was also impactful; within one French hospital, VCRs among hospitalized patients aged ≥65 years of age who were offered Td-IPV (tetanus, diphtheria, and polio) vaccination during their visit increased more than the control group VCRs (56.2–80.8% vs 38.1–40.5%).55
Discussion
The studies reviewed assessed a wide array of interventions across various countries, populations, and vaccines. While the heterogeneity of study designs and study contexts limits our ability to directly compare studies or broadly generalize study findings, several significant themes emerged.
Among interactive interventions targeting individuals, provider-led educational initiatives35–39 and direct provider recommendations40–44 showed positive associations across multiple studies, populations, and vaccine types, more so than less interactive interventions (i.e., posters, reminders). The display of educational materials (i.e., posters) did not influence uptake,34 and text messages 24 resulted in weak or non-significant increases in VCRs. Notably, one study found patient portal reminders increased self-reported VCRs among individuals aged 18–64 years but had no significant impact on adults aged ≥65 years old,25 highlighting the importance of population-specific interventions. A Cochrane review conducted in 2018 that evaluated recall and reminder studies found that of all reminder types studied, person-to-person phone call reminders had the greatest impact (pooled RR = 1.75) and postcards (RR = 1.18), and auto-dialer (RR = 1.17) reminders had the smallest impact on VCRs.56 Authors concluded that overall reminder systems were likely effective at increasing vaccine uptake; however, for the adult population (all ages included) the evidence for influenza uptake was moderate (RR 1.29, 95% CI 1.17 to 1.43) compared to non-influenza vaccines, which had a low certainty of evidence (RR 2.08, 95% CI 0.91 to 4.78).56 The combination of our findings and these results suggest that although utilizing technology-based reminders may help increase uptake, active, face-to-face interactions generally have a greater impact on VCRs for older adults.
Interventions targeting providers generally showed positive results, highlighting the important role HCPs play in vaccination and the need for more provider-directed intervention research and funding. Provider vaccine administration incentives were associated with higher influenza VCRs, potentially demonstrating impact of reimbursement policies on provider behavior.20 Implementing provider awareness interventions, including workflow redesign,28,30 reminders26,27 and education programs,45,48,49 generally increased uptake, with some exceptions. The success of provider-directed interventions has also been observed in other populations; for example, studies have found that clinical reminder tools directed at clinicians and providers effectively increased adolescent male HPV vaccination rates.57 Overall, provider reminders were found to increase VCRs more effectively than educational programs, contrary to what was observed for patient-directed interventions. Designing interventions based on the needs of both the target population and providers is critical.
Policies designed to remove financial barriers or expand vaccination sites have been found to improve vaccination rates, according to the studies reviewed. Government funded national vaccine programs in Japan,15 Australia,17 Italy,18 and Korea16 all increased vaccine uptake. These results, compared to other financial interventions (e.g., copay policies, monetary incentives), indicate that national payment policies may be effective due to their ability to circumvent barriers related to an individuals’ lack of willingness or ability to pay. However, non-financial barriers to vaccination exist and must be addressed. These include expanding vaccination settingssuch as opening additional vaccination clinics,50 vaccinating during hospitalizations,55 or expanding pharmacist scope of practice to vaccinate53,54, which have been found to increase uptake. The efficacy of interventions that increase vaccination access has been previously demonstrated in other studies, including a meta-analysis that found a 24% increase in vaccination rates among individuals of all ages receiving pharmacy-based interventions; however, when evaluating subgroups, adults aged ≥65 years old only had a 3% increase in VCR, which was not statistically significant.58 The overall success of these interventions across studies and vaccine types indicates that increasing access to vaccination is a key strategy to improving uptake; however, interventions must be tailored to the target population as outcomes can vary by population.
In some studies where a single intervention did not have the greatest impact, combination interventions had more success. One study found that government-funded vaccination policies have a “borderline significant” impact on vaccination rates of older adults when assessed alone; however, assessing government funded vaccination policies in combination with HCP financial incentives (r = 0.49, p = .047) and mailings to HCPs (r = 0.79, p = .034) was statistically significant.20 Another review assessing combined interventions, such as patient-directed reminders in addition to mail notices, patient reminders with supplemental outreach, and patient reminders plus provider reminders reported increased VCRs (RR = 1.28; RR = 1.22; RR = 2.91, respectively), suggesting combinations of interventions may improve the receipt of vaccination.12,56 The success of combination interventions has been noted by guideline development groups such as the US’s Community Preventive Services Task Force, which recommends that multiple different community-based interventions for vaccination be implemented in combination. In an evidence review and meta-analysis of 14 studies, combination interventions resulted in a median 16% point increase in VCRs.59,60
The WHO’s IA2030 framework for action specifically defined key areas that need to be focused on if the goal and objectives of a life-course approach to vaccination and integration of vaccination services into essential health services are to be achieved.1 Although the core principles of the IA2030 span childhood through adult vaccination, several findings from this review are aligned with the IA3030’s key areas of focus. The most notable are raising awareness of the benefits of vaccination, which in the context of this review could be achieved through expanding provider-led educational initiatives, using data to inform decision making, and evidence-based delivery practices. These were also the foundational objectives of the review: a people-centered approach with a deliberate focus on adult vaccination; and promoting changes in immunization policy and legislation, which is partly captured by the importance of government initiatives, especially when combined with other interventions.
Though these reviews have assessed the value of coordinated interventions, age-disaggregated findings are not well understood, specifically for older adults. Investigation of the degree to which different combinations improve outcomes, particularly in different regions or countries, would be beneficial. Further, though this literature accounted for influence on VCRs among older adults, it did not assess cost-effectiveness or implementation factors. Resources needed to implement interventions, either in isolation or combination, may vary greatly.
In conclusion, increasing vaccination rates, especially among older adults, is important but complex. Government-funded vaccination programs for older adults have demonstrated large positive impacts on vaccination rates, however vaccination targets are typically unmet. Combined efforts addressing barriers such as affordability, awareness, and access will likely have the greatest impact on vaccination rates. However, regional, country, and other geographical factors may influence the ability to address some barriers. Barriers to vaccination also differ by population, and tailoring interventions to specific populations is critical. Existing literature gaps, especially surrounding the most effective and cost-effective interventions limits the ability to develop and implement evidence-based policies and practices. Collaboration between policymakers, healthcare professionals, public health workers, and researchers to design and implement interventions in a way that supports rigorous impact assessment may enhance the intervention understanding we need to increase vaccination access and uptake among older adults.
Supplementary Material
Acknowledgments
The authors thank Elif Alyanak, MPH and Margretta Kruger for their research assistance and thoughtful contributions to the development of the manuscript.
Funding Statement
This work was funded by Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ, USA.
Disclosure statement
AE is currently an employee of Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ, USA and is a shareholder in Merck & Co., Inc., Rahway, NJ, USA. Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ, USA manufactures and sells vaccines used in routine immunization programs globally. MN was an employee of Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ, USA and a shareholder at Merck & Co., Inc., Rahway, NJ, USA when the study was performed. JB reported that the organization International Federation on Aging has agreements contracts with Bayer, AbbVie, BioGen, Pfizer Inc, GlaxoSmithKline, Seqirus, Merck & Co, Inc.
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website at https://doi.org/10.1080/21645515.2022.2157164.
References
- 1.World Health Organization (WHO) . Immunization Agenda 2030: a global strategy to leave no one behind; 2022. [accessed 2022 Nov 18]. https://www.who.int/teams/immunization-vaccines-and-biologicals/strategies/ia2030#:~:text=The%20World%20Health%20Assembly%2C%20with,save%20over%2050%20million%20lives.
- 2.Bloom D, Fan V, Sevilla J.. The broad socioeconomic benefits of vaccination. Sci Transl Med. 2018;10(441):eaaj234. doi: 10.1126/scitranslmed.aaj2345. [DOI] [PubMed] [Google Scholar]
- 3.Dorrington M, Bowdish D.. Immunosenescence and novel vaccination strategies for the elderly. Front Immunol. 2013;4:171. doi: 10.3389/fimmu.2013.00171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.United Nations Department of Economic and Social Affairs, Population Division . World population prospects 2019: highlights. United Nations Department of Economic and Social Affairs | Multimedia Library; 2019. Jun 17 [accessed 2022 Mar 10]. https://www.un.org/development/desa/publications/world-population-prospects-2019-highlights.html. [Google Scholar]
- 5.Peck M, Gacic-Dobo M, Diallo M, Nedelec Y, Sodha S, Wallace A. Global routine vaccination coverage, 2018. MMWR Morb Mortal Wkly Rep. 2019;68(42):937–8. doi: 10.15585/mmwr.mm6842a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Patel M, Dumolard L, Nedelec Y, Sodha S, Steulet C, Gacic-Dobo M, Kretsinger K, McFarland J, Rota P, Goodson J. Progress toward regional measles elimination — worldwide, 2000–2018. Morb Mortal Wkly Rep. 2019;68(48):1105–11. doi: 10.15585/mmwr.mm6848a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.European Centers for Disease Control and Prevention (ECDC) . Vaccine scheduler | vaccine schedules in all countries in the EU/EEA. Vaccine scheduler; 2022. [accessed 2022 Mar 25]. https://vaccine-schedule.ecdc.europa.eu. [Google Scholar]
- 8.Wu L, Kanitz E, Crumly J, D’Ancona F, Strikas R. Adult immunization policies in advanced economies: vaccination recommendations, financing, and vaccination coverage. Int J Public Health. 2013;58(6):865–74. doi: 10.1007/s00038-012-0438-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Privor-Dumm L, Vasudevan P, Kobayashi K, Gupta J. Archetype analysis of older adult immunization decision-making and implementation in 34 countries. Vaccine. 2020;38(26):4170–82. doi: 10.1016/j.vaccine.2020.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sauer M, Vasudevan P, Meghani A, Luthra K, Garcia C, Knoll M, Privor-Dumm L. Situational assessment of adult vaccine preventable disease and the potential for immunization advocacy and policy in low- and middle-income countries. Vaccine. 2021;39(11):1556–64. doi: 10.1016/j.vaccine.2021.01.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shapiro G, Gottfredson N, Leask J, Wiley K, Ganter-Restrepo F, Jones S, Menning L, Brewer N. COVID-19 and missed or delayed vaccination in 26 middle- and high-income countries: an observational survey. Vaccine. 2022;40(6):945–52. doi: 10.1016/j.vaccine.2021.12.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thomas R, Lorenzetti D. Interventions to increase influenza vaccination rates of those 60 years and older in the community. Cochrane Database Syst Rev. 2018;5. doi: 10.1002/14651858.CD005188.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tricco A, Lillie E, Zarin W, O’Brien K, Colquhoun H, Levac D, Moher D, Peters M, Horsley T, Weeks L, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 14.Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, Britten N, Roen K, Duffy S. Guidance on the conduct of narrative synthesis in systematic reviews: a product from the ESRC methods programme. Lanc Univ. 2016;92. doi: 10.13140/2.1.1018.4643. [DOI] [Google Scholar]
- 15.Naito T, Suzuki M, Fujibayashi K, Kanazawa A, Takahashi H, Yokokawa H, Watanabe A. The estimated impact of the 5-year national vaccination program on the trend of 23-valent pneumococcal polysaccharide vaccine vaccination rates in the elderly in Japan, 2009–2018. J Infect Chemother. 2020;26(4):407–10. doi: 10.1016/j.jiac.2019.12.011. [DOI] [PubMed] [Google Scholar]
- 16.Yang J, Atkins K, Feng L, Pang M, Zheng Y, Liu X, Cowling B, Yu H. Seasonal influenza vaccination in China: landscape of diverse regional reimbursement policy, and budget impact analysis. Vaccine. 2016;34(47):5724–35. doi: 10.1016/j.vaccine.2016.10.013. [DOI] [PubMed] [Google Scholar]
- 17.Litt J, Booy R, Bourke D, Dwyer D, Leeb A, McCloud P, Stein A, Woodward M, Cunningham A. Early impact of the Australian national shingles vaccination program with the herpes zoster live attenuated vaccine. Hum Vaccines Immunother. 2020;16(12):3081–89. doi: 10.1080/21645515.2020.1754702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brilli Y, Lucifora C, Russo A, Tonello M. Vaccination take-up and health: evidence from a flu vaccination program for the elderly. J Econ Behav Organ. 2020;179:323–34. doi: 10.1016/j.jebo.2020.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jiang X, Shang X, Lin J, Zhao Y, Wang W, Qiu Y. Impacts of free vaccination policy and associated factors on influenza vaccination behavior of the elderly in China: a quasi-experimental study. Vaccine. 2021;39(5):846–52. doi: 10.1016/j.vaccine.2020.12.040. [DOI] [PubMed] [Google Scholar]
- 20.Blank P, Essen G, Lejarazu R, Nitsch-Osuch A, Kuchar E, Falup-Percurariu O, Maltezou H, Zavadska D, Kristufkova Z, Kassianos G. Impact of European vaccination policies on seasonal influenza vaccination coverage rates: an update seven years later. Hum Vaccines Immunother. 2018. Aug;14(11):2706–14. doi: 10.1080/21645515.2018.1489948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yan S, DerSarkissian M, Bhak R, Lefebvre P, Duh M, Krishnarajah G. Relationship between patient copayments in medicare part D and vaccination claim status for herpes zoster and tetanus-diphtheria-acellular pertussis. Curr Med Res Opin. 2018;34(7):1261–69. doi: 10.1080/03007995.2017.1416347. [DOI] [PubMed] [Google Scholar]
- 22.Hechter R, Qian L, Yan S, Luo Y, Krishnarajah G, Tseng H. Impact of the change of copay policy in medicare part D on zoster vaccine uptake among medicare beneficiaries in a managed care organization. BMC Health Serv Res. 2017. Jul;17(1):503. doi: 10.1186/s12913-017-2441-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yue M, Wang Y, Low C, Yoong J, Cook A. Optimal design of population-level financial incentives of influenza vaccination for the elderly. Value Health. 2020;23(2):200–08. doi: 10.1016/j.jval.2019.08.006. [DOI] [PubMed] [Google Scholar]
- 24.Herrett E, Williamson E, Staa T, Ranopa M, Free C, Chadborn T, Goldacre B, Smeeth L. Text messaging reminders for influenza vaccine in primary care: a cluster randomised controlled trial (TXT4FLUJAB). BMJ Open. 2016;6(2):e010069. doi: 10.1136/bmjopen-2015-010069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Szilagyi P, Albertin C, Casillas A, Valderrama R, Duru O, Ong M, Vangala S, Tseng C-H, Rand C, Humiston S, et al. Effect of patient portal reminders sent by a health care system on influenza vaccination rates. JAMA Intern Med. 2020;180(7):962–70. doi: 10.1001/jamainternmed.2020.1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sheer R, Nau D, Dorich N, Boyer A, Pickering M, Campbell P, Pasquale M. Medicare advantage-pharmacy partnership improves influenza and pneumococcal vaccination rates. Am J Manag Care. 2021;27(10):425–31. doi: 10.37765/ajmc.2021.88760. [DOI] [PubMed] [Google Scholar]
- 27.Burka A, Fann J, Lamb K, Salvig B, Smith T, Wallace J. Evaluation of a novel discharge reminder tool on pneumococcal vaccination in hospitalized elderly veterans. JACCP J Am Coll Clin Pharm. 2019;2(5):462–67. doi: 10.1002/jac5.1078. [DOI] [Google Scholar]
- 28.Erlandson K, Streifel A, Novin A, Hawkins K, Foster C, Langness J, Bessesen M, Falutz J, Moanna A, Looney D, et al. Low rates of vaccination for herpes zoster in older people living with HIV. AIDS Res Hum Retroviruses. 2018;34(7):603–06. doi: 10.1089/aid.2017.0315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McGreevy S, McGowan C, Gillenwater K, Opole R, Veluri M, Stehle K, Ramm B, Gibson C. Improving population health in resident clinics: increasing pneumonia vaccination rates in adults 65 years and older. BMJ Open Qual. 2020;9(4):e000830. doi: 10.1136/bmjoq-2019-000830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McAdam-Marx C, Tak C, Petigara T, Jones N, Yoo M, Briley M, Gunning K, Gren L. Impact of a guideline-based best practice alert on pneumococcal vaccination rates in adults in a primary care setting. BMC Health Serv Res. 2019; 19: 1; 474. doi: 10.1186/s12913-019-4263-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chen W, Stoecker C. Mass media coverage and influenza vaccine uptake. Vaccine. 2020;38(2):271–77. doi: 10.1016/j.vaccine.2019.10.019. [DOI] [PubMed] [Google Scholar]
- 32.Rosselli R, Martini M, Fluad Effect Working Group, Bragazzi N, Watad A. The public health impact of the so-called ‘fluad effect’ on the 2014/2015 influenza vaccination campaign in Italy: ethical implications for health-care workers and health communication practitioners. Adv Exp Med Biol. 2017;973:125–34. doi: 10.1007/5584_2017_39. [DOI] [PubMed] [Google Scholar]
- 33.Yokum D, Lauffenburger J, Ghazinouri R, Choudhry N. Letters designed with behavioural science increase influenza vaccination in medicare beneficiaries. Nat Hum Behav. 2018;2(10):10. doi: 10.1038/s41562-018-0432-2. [DOI] [PubMed] [Google Scholar]
- 34.Berkhout C, Willefert-Bouche A, Chazard E, Zgorska-Maynard-Moussa S, Favre J, Peremans L, Ficheur G, Royen P. Randomized controlled trial on promoting influenza vaccination in general practice waiting rooms. PLoS ONE. 2018;13(2):e0192155. doi: 10.1371/journal.pone.0192155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Leung K, Mui C, Chiu W, Ng Y, Chen M, Ho P, Kwok C, Lam S, Wong C, Wong K, et al. Impact of patient education on influenza vaccine uptake among community-dwelling elderly: a randomized controlled trial. Health Educ Res. 2017;32(5):455–64. doi: 10.1093/her/cyx053. [DOI] [PubMed] [Google Scholar]
- 36.Tao L, Lu M, Wang X, Han X, Li S, Wang H. The influence of a community intervention on influenza vaccination knowledge and behavior among diabetic patients. BMC Public Health. 2019;19:1747. doi: 10.1186/s12889-019-8101-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Abu-Rish E, Barakat N. The impact of pharmacist-led educational intervention on pneumococcal vaccine awareness and acceptance among elderly in Jordan. Hum Vaccines Immunother. 2020;17(4):1181–89. doi: 10.1080/21645515.2020.1802973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schattner A. Cardiovascular-targeted patient education and uptake of influenza vaccination in elderly patients. Patient Educ Couns. 2020;103(5):1052–54. doi: 10.1016/j.pec.2019.12.008. [DOI] [PubMed] [Google Scholar]
- 39.Pizzi L, Prioli K, Harris L, Cannon-Dang E, Marthol-Clark M, Alcusky M, McCoy M, Schafer J. Knowledge, activation, and costs of the Pharmacists’ Pneumonia Prevention Program (PPPP): a novel senior center model to promote vaccination. Ann Pharmacother. 2018;52(5):446–53. doi: 10.1177/1060028017745566. [DOI] [PubMed] [Google Scholar]
- 40.Biyik M, Arslan I, Taci D. Study to increase the pneumococcal vaccination rates of individuals aged 65 years and older. Prim Health Care Res Dev. 2020;21:e37. doi: 10.1017/S1463423620000389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yuruyen M, Ayan G, Demirdağ F, Kara Z, Avcı S, Yavuzer H, Doventas A, Erdinçler D. Why is vaccination frequency low in elderly patients? Ann Clin Anal Med. 2018;9:2. doi: 10.4328/JCAM.5611. [DOI] [Google Scholar]
- 42.Higuchi M, Narumoto K, Goto T, Inoue M. Correlation between family physician’s direct advice and pneumococcal vaccination intention and behavior among the elderly in Japan: a cross-sectional study. BMC Fam Pract. 2018;19(1):153. doi: 10.1186/s12875-018-0841-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lv M, Fang R, Wu J, Pang X, Deng Y, Lei T, Xie Z. The free vaccination policy of influenza in Beijing, China: the vaccine coverage and its associated factors. Vaccine. 2016;34(18):2135–40. doi: 10.1016/j.vaccine.2016.02.032. [DOI] [PubMed] [Google Scholar]
- 44.Yi B, Zhou S, Song Y, Chen F, Xuyin L, Cai J, Greene C, Feng L, Zheng J, Dong H, et al. Innovations in adult influenza vaccination in China, 2014–2015: leveraging a chronic disease management system in a community-based intervention. Hum Vaccines Immunother. 2018;14(4):947–51. doi: 10.1080/21645515.2017.1403704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wright W, Bruns D, Feeney A, Strowman S. Improving vaccination rates in older adults: a quality improvement project. Nurse Pract. 2019;44(4):40–49. doi: 10.1097/01.NPR.0000554085.13073.37. [DOI] [PubMed] [Google Scholar]
- 46.Healy A, Svendsen M, Reynolds A, Heisler J, Huntington M. Enhancing immunization rates for senior citizens in South Dakota family medicine residency practices. S D Med J S D State Med Assoc. 2019;72(4):164–67. PMID: 31436929. [PubMed] [Google Scholar]
- 47.Nowalk M, Nolan B, Nutini J, Ahmed F, Albert S, Susick M, Zimmerman R. Success of the 4 pillars toolkit for influenza and pneumococcal vaccination in adults. J Healthc Qual off Publ Natl Assoc Healthc Qual. 2014;36(6):5–15. doi: 10.1111/jhq.12020. [DOI] [PubMed] [Google Scholar]
- 48.Nowalk M, Moehling K, Zhang S, Raviotta J, Zimmerman R, Lin C. Using the 4 pillarsTM to increase vaccination among high-risk adults: who benefits? Am J Manag Care. 2017;23(11):651–55. doi: 10.1186/s12879-016-1940-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zimmerman R, Brown A, Pavlik V, Moehling K, Raviotta J, Lin C, Zhang S, Hawk M, Kyle S, Patel S, et al. Using the 4 pIllars practice transformation program to increase pneumococcal immunizations for older adults: a cluster-randomized trial. J Am Geriatr Soc. 2017;65(1):114–22. doi: 10.1111/jgs.14451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Itamochi T, Mieno M, Hatakeyama S. Influenza vaccination coverage in Chiburijima Island, Japan: impact of diversification of vaccination place. J Gen Fam Med. 2020;21(5):178–84. doi: 10.1002/jgf2.335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Restivo V, Orsi A, Ciampini S, Messano G, Trucchi C, Ventura G, Casuccio A, Vitale F, the Leadership in Public Health Group . How should vaccination services be planned, organized, and managed? Results from a survey on the Italian vaccination services. Ann Ig Med Prev E Comunita. 2019;31(2):45–53. doi: 10.7416/ai.2019.2276. [DOI] [PubMed] [Google Scholar]
- 52.Ko H, Kim M. Impacts of expanding provider choice for free flu vaccination among the elderly in Korea. Health Policy (New York). 2020;24(10):1115–20. doi: 10.1016/j.healthpol.2020.07.014. [DOI] [PubMed] [Google Scholar]
- 53.Isenor J, Killen J, Billard B, McNeil S, MacDougall D, Halperin B, Slayter K, Bowles S. Impact of pharmacists as immunizers on influenza vaccination coverage in the community-setting in Nova Scotia, Canada: 2013-2015. J Pharm Policy Pract. 2016;9(1):32. doi: 10.1186/s40545-016-0084-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Buchan S, Rosella L, Finkelstein M, Juurlink D, Isenor J, Marra F, Patel A, Russell M, Quach S, Waite N, et al. Impact of pharmacist administration of influenza vaccines on uptake in Canada. CMAJ Can Med Assoc J. 2017;189(4):E146–52. doi: 10.1503/cmaj.151027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Blanchi S, Vaux J, Toqué J, Héry L, Laforest S, Piccoli G, Crochette N. Impact of a catch-up strategy of DT-IPV vaccination during hospitalization on vaccination coverage among people over 65 years of age in France: the HOSPIVAC study (vaccination during hospitalization). Vaccines. 2020;8(2):292. doi: 10.3390/vaccines8020292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Vann J, Jacobson R, Coyne-Beasley T, Asafu-Adjei J, Szilagyi P. Patient reminder and recall interventions to improve immunization rates. Cochrane Database Syst Rev. 2018;1(1). CD003941. doi: 10.1002/14651858.CD003941.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bae J, Ford E, Wu S, Huerta T. Electronic reminder’s role in promoting human papillomavirus vaccine use. Am J Manag Care. 2017;23(11):e353–59. PMID: 29182355. [PubMed] [Google Scholar]
- 58.Murray E, Bieniek K, Aguila M, Egodage S, Litzinger S, Mazouz A, Mills H, Liska J. Impact of pharmacy intervention on influenza vaccination acceptance: a systematic literature review and meta-analysis. Int J Clin Pharm. 2021;43(5):1163–72. doi: 10.1007/s11096-021-01250-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Community Preventative Services Task Force (CPSTF) . Increasing appropriate vaccination: community-based interventions implemented in combination. Community Guide; 2015. Feb. https://www.thecommunityguide.org/sites/default/files/assets/Vaccination-Community-Based-in-Combination.pdf. [Google Scholar]
- 60.Community Preventative Services Task Force (CPSTF) . Vaccination programs: community-based interventions implemented in combination. Community Guide; 2014. Oct. https://www.thecommunityguide.org/findings/vaccination-programs-community-based-interventions-implemented-combination. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


