Abstract
Introduction
Primary cam morphology is a mostly benign bony prominence that develops at the femoral head-neck junction of the hip, but it is highly prevalent in many athlete populations. In the small proportion of athletes for whom it is not benign, the resulting hip osteoarthritis can be debilitating. Clinicians, athletes, patients and researchers do not yet agree on important primary cam morphology elements. We aimed to ascertain and improve the level of agreement on primary cam morphology definitions, terminology, taxonomy and imaging outcome measures.
Methods
To collect and aggregate informed opinions, an expert panel—the Young Athlete’s Hip Research Collaborative—rated primary cam morphology definition, terminology, taxonomy and imaging outcome statements through an online Delphi exercise followed by an online meeting to explore areas of tension and dissent. Reporting followed Conducting and REporting DElphi Studies.
Results
A diverse and inclusive Delphi panel (n=65 for rounds 1 and 2, representing 18 countries; 6 stakeholder groups; 40% women) agreed on 35 of 47 statements in 4 domains, while surfacing areas of tension and dissent. This Delphi panel agreed on four key issues essential to moving research and clinical care forward around primary cam morphology. They agreed on: (1) definition, confirming its conceptual attributes (tissue type, size, location, shape and ownership); (2) terminology—use ‘morphology’ and not terms with a negative connotation like ‘lesion’, ‘abnormality’ or ‘deformity’; (3) taxonomy, distinguishing between primary and secondary cam morphology, and (4) imaging outcomes, a continuous bone/cartilage alpha angle on radial femoral head-neck MRI for primary cam morphology aetiology research.
Conclusion
This consensus provides athletes, patients, clinicians and researchers with a strong foundation to guide more precise communication, better clinical decision-making and higher value research about primary cam morphology and its natural history.
Keywords: Hip, Osteoarthritis, Consensus, Athletes, Sports medicine
Executive summary for clinicians and researchers
Primary cam morphology (PCM) is a mostly benign bony prominence that develops at the femoral head-neck junction of the hip and is highly prevalent in many athlete populations. In some athletes for whom it is not benign, the resulting symptoms and eventual hip osteoarthritis can be debilitating. The Oxford Consensus Study (part 1) equips clinicians and researchers in sport and exercise medicine, musculoskeletal rehabilitation and sports science fields to practice more precise communication, pursue better clinical decisions, and produce higher value research about PCM and its natural history. This study’s focus on the definitions, terminology, taxonomy and imaging outcome measures of PCM opens the door for clearer conversations about the morphology and its natural history with athletes, parents, coaches and patients; conversations that normalise what is happening with the athlete’s hip— ‘…a bony bump in your hip that is a common and normal response to training—the vast majority of athletes never have problems. However, some athletes living with this morphology could develop symptoms (femoroacetabular impingement (FAI) syndrome), and potentially hip osteoarthritis in the long term.’
Applying this consensus, clinicians and researchers should prioritise conversations with athletes and patients that:

|
Clarify the concept of primary cam morphology and its natural history, using a clear definition: primary cam morphology is a cartilage or bony prominence (bump) of varying size at any location around the femoral head-neck junction of the hip, which changes the shape of the femoral head from spherical to aspherical. Development likely begins in early adolescence, occurring most often in asymptomatic male athletes in both hips. |

|
Validate athletes’ and patients’ experiences through consistent, positive terminology; use ‘morphology’, ‘prominence’ or ‘bump’ when referring to the morphology; avoid ‘lesion’, ‘deformity’ and ‘abnormality’—words that could amplify the need for unnecessary interventions; consider the possible negative connotation of ‘syndrome’. |

|
Apply a consistent taxonomy for cam morphology that distinguishes between primary and secondary cam morphology: primary cam morphology develops during skeletal maturation in young adolescents (with no current or previous hip disease), as a normal physiological response to high-load sporting activity, and is largely benign; secondary cam morphology develops secondary to primary (hip) disease—an important distinction that empowers athletes and patients to embrace normality and their ‘happy hips’. |

|
Describe the alpha-angle on radiographs or 3D imaging, depending on the clinical and/or research context, to measure (operationalise) the morphology: the preferred outcome measure for research on primary cam morphology aetiology is a cartilage or bone alpha angle as a continuous variable on radial MRI along the axis of the femoral neck, using 30° intervals from 12 o'clock to 11 o'clock positions, reported per hip, per person or both. In addition to reporting the morphology as a continuous alpha angle (in degrees), a dichotomous alpha angle (using a threshold of ≥60°) can be useful in clinical practice or research. |
The Oxford Consensus Study mobilised an international and multidisciplinary community of clinicians, researchers, patient and public partners, research methodologists, journal editors and funders. This learning community—the Young Athlete’s Hip Research (YAHiR) Collaborative—will continue to collaborate to:
Coproduce knowledge, prioritising minoritised populations and focusing on questions that matter to athletes and patients.
Develop open and easy-access resources for clinicians, researchers, athletes and patients.
Implement the Oxford consensus while addressing areas of tension and dissent through respectful scholarly discourse.
Measure its performance based on realistic and coagreed deliverables.
Introduction
Although PCM is mostly an inconsequential bony prominence that develops at the femoral head-neck junction of the hip, it is highly prevalent in many athlete populations.1–3 In those few athletes for whom it is not benign, the resulting hip osteoarthritis can be debilitating.4 This predominantly benign morphology thus places existing and potential athlete-patients at risk of future hip disease.
Clinicians and researchers cannot currently predict with accuracy whose PCM will be inconsequential and who will end up with a total hip replacement, hence the need for research to determine the risk factors for poor outcome. Existing research is mired in confusion partly because clinicians, athlete-patients and researchers have not agreed on a conceptual or operational definition of PCM, key terminology or a taxonomy of subtypes.5
The YAHiR collaborative is an international multiprofessional stakeholder group that aims to add research value and reduce research waste on conditions affecting the young athlete’s hip. The current focus is PCM and its natural history. Some have defined ‘natural history’ as the ‘uninterrupted progression’6 of a person’s condition, including being asymptomatic for life. It is important to recognise that ‘progression’ for a person with PCM might also include the curtailment of hip disease by treatment. Therefore, we have included a broader range of outcomes in our use of the term natural history in this study. A preliminary concept analysis we recently published,5 identified four key areas for further attention: it (1) proposed a new conceptual definition for the morphology based on five defining attributes; (2) spotlighted inconsistent and troublesome terminology, while also commending the important Warwick Agreement from a small and selective expert panel7; (3) introduced taxonomy distinguishing between primary and secondary cam morphology; and (4) exposed the challenges of operationalising the hip morphology.
However, publication of a concept paper in isolation does not guarantee dissemination, clinical uptake, impact on research or benefit to patients. The urgent current need is for clinicians, athlete-patients and researchers to engage with, challenge and improve the above-mentioned four key elements and prioritise a research agenda for this field. If not, communication will remain imprecise, clinical decision-making will be compromised and research waste will continue.
Here, we report on our overarching aim to inform a more rigorous, inclusive and evidence-based approach to research on PCM and its natural history. The specific objectives of the research were to:
Ascertain the level of agreement among experts on definitions, terminology, taxonomy and imaging outcome measures for research on PCM.
Work towards agreement and highlight residual disagreements on a set of research priorities on conditions affecting the young person’s hip focusing primarily on PCM and its natural history.
-
Hold two education events to engage stakeholders, disseminate the latest evidence and stimulate debate.
Oxford-Aspetar-La Trobe Young Athlete’s Hip Webinar Series.
YAHiR Collaborative Symposium.
We report the results of objective one in this paper. A linked paper (Oxford consensus study, part 2) describes objectives 2 and 3.
Methods
We held a sequential, two-round online Delphi survey and two synchronous online mixed stakeholder group meetings (Interacting Group Process) to explore the level of agreement among a panel of experts, on PCM definitions, terminology, taxonomy and imaging outcome measures for research, and to work towards agreement on a set of research priorities on conditions affecting the young person’s hip.
This methods section focuses on objective 1 while the methods section in a linked paper (Oxford consensus study, part 2) describes the research priority setting methods. Online supplemental file 1 describes and elaborates on the combined Methods for Oxford consensus study, parts 1 and 2.
bjsports-2022-106085supp001.pdf (754.2KB, pdf)
Methodology
The Delphi method provides a less hierarchical and more ethical approach to conducting research, combined, in our study context, with transformative and knowledge coproduction lenses underpinned by pragmatism as the philosophical paradigm.8 As a pragmatic tool, the Delphi method is flexible, favouring diversity over statistical representativeness in sampling, relatively low resource and user-friendly.8 9 Given the focus on (research) transformation and knowledge coproduction, it was important to reflect on our positionality and identities (racial/ethnic, sex/gender). The Oxford Delphi consensus steering committee members, 5 women and 8 men, were English-speaking white academics (11 with PhDs); 4 were physicians, 6 allied healthcare practitioners and 3 health researchers. One resided in the Global South.
Study design: Delphi method and research priority setting process
Delphi method
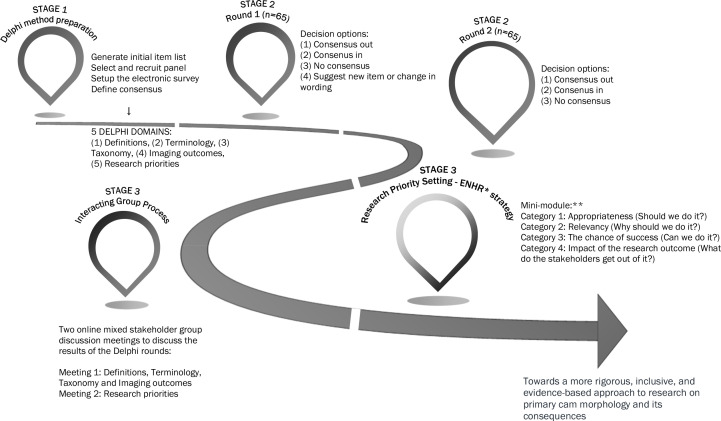
For this three-stage consensus study (figure 1), we modified the classical Delphi method slightly by replacing an open qualitative first round with a pre-selected list of statements based on a review of existing literature and a synthesis of the knowledge of steering group members.10–13 The Delphi method assesses consensus through an iterative multistage process of controlled online questionnaires, feedback, reflection and discussion, documenting both agreements and the nature and extent of residual disagreement.14–16 Multiple rounds allow panel members to work towards consensus as members are invited to amend their response in the light of the group average.17 18 The Delphi method allows panel members to participate anonymously to reduce the influence of dominant individuals.19 Reporting followed Conducting and REporting DElphi Studies20 (online supplemental file 2). We report in a linked paper (Oxford consensus study, part 2) how the prioritised research statements were further ranked according to the Council on Health Research for Development’s Essential National Health Research (ENHR) ranking method.21
Figure 1.
Oxford Consensus Study methods flow chart. Stage 1: prepare for Delphi method; stage 2: Delphi method online rounds; stage 3: Interacting Group Process and ENHR strategy for research priority setting. *Essential National Health Research; **Minimodule adapted from Okello et al.21 ENHR, Essential National Health Research.
bjsports-2022-106085supp002.pdf (154.2KB, pdf)
Stage 1: planning
Steering committee
The study steering committee included members of the YAHiR Collaborative. Avoiding the ‘good old boys sat around a table’ approach22 the steering committee ensured a representative Delphi panel, and a robust Delphi study process. Interpreting ‘diversity’ as more than representation of certain demographic groups, the steering committee ensured a diverse and informed Delphi panel, representing six multiprofession stakeholder groups, including previously minoritised groups relevant to this research field (eg, women, athletes, patients and the community, participants from the Global South). This study’s online Delphi method, with a specific focus on anonymity and access to adequate topic-specific resources, supported a more equitable and inclusive process. (Online supplemental file 3: steering committee terms of reference).
bjsports-2022-106085supp003.pdf (1.9MB, pdf)
Delphi panel
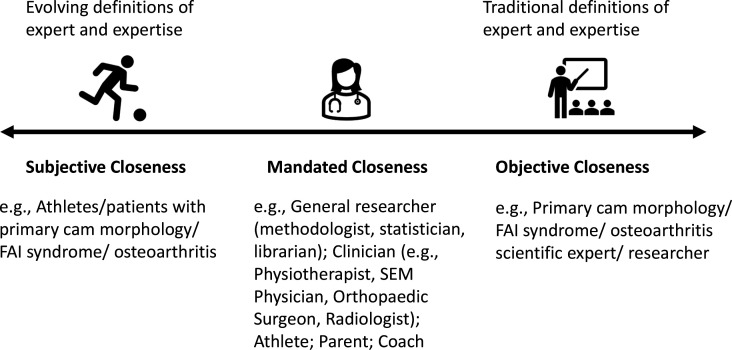
The concept of ‘expert’ is contested. We adapted and applied the ‘closeness continuum’ to purposively recruit 73 experts for this study (figure 2, table 1).23 The closeness continuum represents an inclusive expert population of individuals with subjective, mandated, and objective closeness to the topic of interest.23 24
Figure 2.
Applying the closeness continuum of experts to the Oxford Consensus Study.23 FAI, femoroacetabular impingement, SEM, sport and exercise medicine.
Table 1.
Delphi panel recruitment criteria
| Identification of Delphi panel and sample size | Panel members were identified through (1) expert knowledge of the steering committee and colleagues; (2) International Olympic Committee’s 11 research centres for the prevention of injury and protection of athlete health; (3) International Hip Pain Research Network Consensus Group; (4) a list of authors (lead/corresponding authors) with a track record of peer-review publications in sports medicine and science, preferably in the field of cam morphology/FAI syndrome over the past 15–20 years (2000–2021). We oversampled to compensate for possible attrition at a rate of 25% per round. |
| Researchers | Statisticians, methodologists, librarians and sport scientists |
| Clinicians and clinician researchers | Clinicians who treat patients with hip-related conditions and clinician-researchers with a peer reviewed publication record in the field (cam morphology and/or FAI aetiology, prognosis, treatment), including orthopaedic surgeons, physicians (including sports medicine physicians, physical medicine and rehabilitation physician, rheumatologist, family medicine), radiologists, physical therapists |
| Patient and public involvement (PPI) representatives |
|
| Journal editors, representatives of research funding bodies and policymakers | Journal editors (eg, BJSM and JOSPT); Sports organisations/federations for example, FIFA, IOC, IAAF |
BJSM, British Journal of Sports Medicine; FAI, femoroacetabular impingement; FIFA, Fédération Internationale de Football Association; IAAF, International Association of Athletics Federations; IOC, International Olympic Committee; JOSPT, Journal of Orthopaedic & Sports Physical Therapy.
Patient and public involvement
We involved patient and public partners in the planning, delivery and dissemination of the Delphi study through the YAHiR Collaborative’s patient and public involvement (PPI) group. The latter group was represented in the Delphi study steering committee. We supplied the PPI group with a glossary, mentored them on definition use and content (during online individual and PPI group meetings), and invited them to weigh in on each Delphi round.25 A panel information pack facilitated informed assessments. Members of the PPI group co-led and actively participated in the mixed stakeholder group discussions following the Delphi rounds.
Delphi software
We used DelphiManager, ‘a web-based system designed to facilitate the building and management of Delphi surveys’ for the Delphi Rounds and Microsoft Forms for the ENHR ranking exercise.26
Statement preparation
We created an extensive list of statements and a conceptual framework of all the potential definitions, terminology, taxonomy and research imaging outcome measures focused on PCM and its natural history. The initial list of statements was based on our concept analysis of PCM,5 and informed by the early results of a qualitative study to explore stakeholder perspectives on factors contributing to high-quality research on how PCM develops, and the Lisbon Agreement on Femoroacetabular Imaging.27–29 Steering committee members independently reviewed the initial statements, followed by an iterative, asynchronous online process to review, discuss, modify and approve the final statements. We provided additional descriptive information (‘Help Text’) where appropriate and asked stakeholders, including the PPI group, to provide feedback on the draft Delphi survey. Stakeholders examined the survey’s face validity and refined language, formatting and layout.
Panel information pack
All panel members had access from the outset of the project and throughout the Delphi process, to relevant study material, including recorded presentations of the first 8 webinars of the Oxford-Aspetar-La Trobe Young Athlete’s Hip Webinar Series (online supplemental file 4: webinar series agenda). Completion of the webinars and/or reading of the consensus statements was not required.
bjsports-2022-106085supp004.pdf (12.8MB, pdf)
Consensus definition
The steering committee agreed on a consensus definition prior to the Delphi rounds (table 2).
Table 2.
Definition of consensus
| Category | Definition | Action |
| Consensus in (high agreement) | Scored as very important (7–9) by ≥70% of panel members and not important (1–3) by <15% of panel members | Item retained for the next survey round/consensus meeting. |
| Consensus out (low agreement) | Scored as not important (1–3) by ≥70% of panel members and very important (7–9) by <15% of panel members | Item discarded after round 2 (to be ratified at the face-to-face consensus meeting). |
| No consensus | Neither criteria above are met | Item retained for the next survey round/consensus meeting. |
| Suggest rewording | Scored as important but must be reworded. | Provide the opportunity for panel members to suggest rewording. The study steering committee will consider retaining a reworded item for the next survey round. |
Stage 2: online Delphi rounds
Round 1
Invited participants provided informed consent and registered for the study in one of six stakeholder groups (table 3). Statements for the Delphi rounds were presented in order of five domains (definitions, terminology, taxonomy, imaging outcomes and research priorities).
Table 3.
Demographic characteristics of Delphi panel and Essential National Health Research (ENHR) ranking exercise participants
| Delphi exercise | ENHR ranking exercise (Oxford consensus study, part 2) | |||
| Round 1 and round 2 (n=65) |
Survey 1* (n=49) |
Survey 2† (n=44) |
Survey 3‡ (n=42) |
|
| Sex | ||||
| Male | 39 | No sex data collected for ENHR ranking exercise | ||
| Female | 26 | |||
| Stakeholder group: n=6 | ||||
| Orthopaedic surgeons | 11 | 7 | 4 | 4 |
| Patient and public involvement group | 10 | 7 | 6 | 6 |
| Physical therapists | 17 | 17 | 16 | 16 |
| Physicians | 13 | 8 | 8 | 7 |
| Radiologists | 6 | 4 | 4 | 4 |
| Researchers | 8 | 6 | 6 | 5 |
| Country of residence | ||||
| Australia | 8 | No country of residence data collected | ||
| Belgium | 1 | |||
| Brazil | 1 | |||
| Canada | 5 | |||
| Denmark | 4 | |||
| Germany | 1 | |||
| Ireland | 2 | |||
| Netherlands | 5 | |||
| Norway | 2 | |||
| Portugal | 1 | |||
| Qatar | 7 | |||
| South Africa | 3 | |||
| Spain | 1 | |||
| Sweden | 1 | |||
| Switzerland | 2 | |||
| Turkey | 1 | |||
| UK | 7 | |||
| USA | 8 | |||
*Survey 1: Statements 48–54.
†Survey 2: Statement 55–59.
‡Survey 3: Statements 64–69.
Panel members scored each statement using a 9-point Likert scale ranging from 1 (‘not important/disagree’) to 9 (‘critical/agree’), based on the Grading of Recommendations Assessment, Development and Evaluation scale for scoring the importance of including the item in the final list of statements.30 Round 1 included a free text section allowing participants to propose new or modified statements and provide feedback. The steering committee reviewed, discussed and considered the proposed new statements or statement modifications suggested by participants in round 1, and resolved any uncertainties. All statements were kept unchanged for round 2.
Round 2
Participants had access to the distribution of round 1 scores for each statement stratified by stakeholder group. Panel members saw their score and then rescored each statement on a scale of 1–9 (or not if they chose to defend their outlying score) based on the average scores of the group. We documented changes in scores from round to round, and panel members could provide reasons when their score boundaries changed between rounds 1 and 2 (online supplemental file 5).
bjsports-2022-106085supp005.pdf (1.8MB, pdf)
The steering committee and Delphi panellists explored and discussed outlying scores, disagreement and dissent (including statements with overall consensus) during the Interacting Group Process (stage 3). Multiple rounds can cause ‘group-think’ among participants via pressure to comply.31 We did not wish to force agreement among participants and chose to limit the Delphi process to a maximum of 3 rounds. However, two Delphi rounds resulted in high consensus and surfaced important disagreements and areas of dissent to focus on in online discussions. A third voting round was therefore not required. Following Delphi round 2, we included all statements voted ‘consensus in/agree’ and ‘consensus out/disagree’ in the final list of consensus statements.32 33
Stage 3: online Interacting Group Process (and research priority setting exercise discussed in Oxford consensus study, part 2)
Interacting Group Process
Delphi panellists discussed discordant items and areas of tension and dissent during two online mixed stakeholder group meetings—the Interacting Group Processes. This process supports sharing and evaluating information,34 stimulating participants to look at problems and solutions from different perspectives.34 35 The first meeting discussed the results of the Delphi rounds and ratified the consensus PCM definitions, terminology, taxonomy and imaging outcome measures statements (online supplemental file 8: agenda and discussion topics). The second meeting discussed the priority research statements. To create a safe space for panellists to share their views, the steering committee facilitated discussions in small zoom breakout rooms (6–8 panellists representing different stakeholder groups); the discussions were not recorded. Group leads documented discussions in a field diary, and maintained speaker anonymity.
bjsports-2022-106085supp008.pdf (930.3KB, pdf)
Data analysis
We entered and stored data using the DelphiManager electronic software tool and created Excel spreadsheets.26 We calculated descriptive statistics for each statement and stakeholder group for example, summary scores, ranges, percentage scoring for each statement ‘not important/disagree’ (score 1–3), ‘important but not critical/neutral’ (score 4–6) and ‘critical/agree’ (score 7–9). Specifically, we reported, per stakeholder group, the median and IQR for each statement between each round (online supplemental file 5). This central tendency and measure of distribution served to estimate the consistency of responses between successive rounds of the Delphi survey. Stability of response is an indication of whether agreement (or continuous dissensus or disagreement) is present throughout and whether it develops between rounds.36 37 The stability of group response between rounds 1 and 2 was determined using the intraclass correlation coefficient (ICC) type A, and an absolute agreement definition.38 39 ICC estimates and their 95% CI were calculated using SPSS statistical package V.23 (SPSS) based on two-way mixed-effects model.40 The lower bound 95% CI of the ICC estimate was used as the basis to evaluate the level of stability using the following general guideline: ICC values <0.5 (poor stability), 0.5–0.75 (moderate stability), 0.75–0.9 (good stability) and >0.9 (excellent stability).40
Table 2 represents the prior consensus definition for categorising statements in the five Delphi domains. The Delphi study steering committee retained all statements between rounds 1 and 2 to enable participants to re-score every statement after considering feedback from round 1. Acknowledging that certain statements might be more relevant to some panel members than others, stakeholders were given the choice not to score a specific statement. We did, however, analyse the data of different stakeholder groups separately in each round.32
Dissent analysis: To explore possible dissent, we applied outlier, bipolarity and stakeholder group analysis.41 42
Outlier analysis: We identified low outliers (data points that fall more than 1.5 times the IQR below the first quartile), and high outliers (data points that fall more than 1.5 times the IQR above the third quartile). In addition, we visually inspected histograms of round 2 stakeholder group scoring for outliers. We reanalysed consensus after eliminating outliers for all statements with marginal non-consensus to test if these had an impact on the group’s consensus.
Bipolarity analysis: Opposing groups of experts with an important and insoluble cleft of opinion, might result in non-consensus. Bimodal data distribution is therefore a possible explanation for dissent. To test for bipolarity, we investigated potential bimodal distribution (two or more answer options had the same mode frequency) and visually inspected histograms for round 2 scores of each statement.41
Stakeholder group analysis: To compare the scores from round 2 between the six stakeholder groups, we performed Kruskal-Wallis tests. To account for multiple post hoc comparisons, we adjusted the statistical significance threshold P value to 0.0033 according to Bonferroni method. We are conscious of the limitations of ‘statistical significance’43; therefore, substantial stakeholder group differences (p<0.0033) prompted us to further scrutinise individual and group opinions for the specific statement.
Qualitative analysis
The lead investigator (HPD) immersed himself in the details of participants’ comments provided during Delphi rounds, Interacting Group Process and ENHR ranking exercise.44 After developing a framework based on recurrent and important themes, the free text comments were grouped into categories, iteratively discussed between the lead investigator and second author (SMA). The lead authors (HPD and SMA) then undertook thematic analysis to identify, group and agree on common threads within these categories, further refining themes and subthemes.45 46 We provided summarised feedback of quantitative and qualitative open responses to panel members during Webinars 10 and 11 of the Oxford-Aspetar-La Trobe Young Athlete’s Hip Webinar Series. The two webinars preceded the online synchronous mixed stakeholder group discussions.
Results
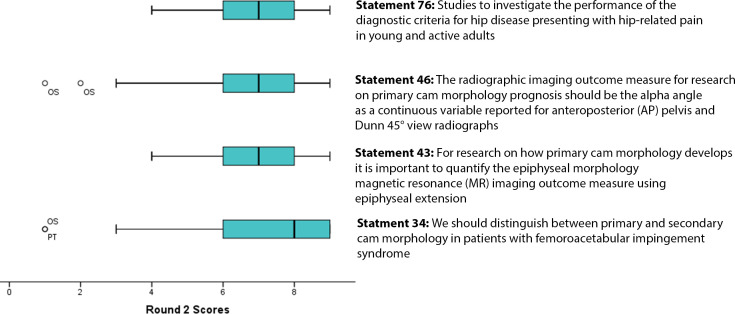
Of the 73 experts invited to participate in this study, 65 completed rounds 1 and 2 of the Delphi exercise. The Delphi panel from 18 countries represented 6 stakeholder groups—26 were female (table 3). The Delphi panel scored 85 statements (12 definition, 19 terminology, 4 taxonomy, 12 imaging outcome and 38 research statements), and reached consensus on 43 of 85 statements in round 1, and 53 of 85 statements in round 2 (table 4 and online supplemental file 5). Online supplemental file 5 also lists the reasons for score boundary changes between rounds 1 and 2 for each statement; twelve statements did not reach stability (table 4). There were four marginally non-consensus statements after round 2 (figure 3).
Table 4.
Results of two survey rounds showing the level of agreement with primary cam morphology definition, terminology, taxonomy and imaging outcomes statements
| Statments | Round 1 | Round 2 | ICC* | ICC 95% CI | ||||
| Not important/disagree | Critical/agree | Not important/disagree | Critical/agree | Lower bound | Upper bound | |||
| No | Definitions | |||||||
| 1 | Primary cam morphology develops during skeletal maturation as a normal physiological response to load | 3.3% | 80.3% | 1.6% | 85.9% | 0.69 | 0.53 | 0.80 |
| 2 | Primary cam morphology is not caused by previous disease, injury or an acute event; it represents a normal physiological response of the maturing skeleton to load | 3.3% | 72.1% | 1.6% | 81.3% | 0.79 | 0.68 | 0.87 |
| 3 | Secondary cam morphology develops due to existing hip disease or acute trauma, including Perthes disease, slipped capital femoral epiphysis, healed proximal femoral fractures or acute fracture | 0% | 73.8% | 1.6% | 81.0% | 0.54 | 0.34 | 0.70 |
| 4 | Primary cam morphology develops in young and active individuals, including athletes, likely due to load (eg, sporting activity) during prepubertal and pubertal skeletal maturation (load during growth) and its (physiological) effect on the proximal femoral growth plate | 0% | 87.1% | 0% | 96.9% | 0.69 | 0.53 | 0.80 |
| 5 | Primary cam morphology is common in young and active males, including athletes, likely due to sporting activity during prepubertal and pubertal skeletal maturation (load during growth) and its (physiological) effect on the proximal femoral growth plate | 4.9% | 73.8% | 0% | 79.4% | 0.80 | 0.68 | 0.88 |
| 6 | Primary cam morphology includes cam morphology of unknown origin | 8.8% | 49.1% | 9.5% | 52.4% | 0.52 | 0.30 | 0.69 |
| 7 | Cam morphology that develops in young and active individuals without any symptoms (eg, hip-related pain, stiffness) or history of previous/existing hip disease, is primary cam morphology until proven otherwise | 3.4% | 55.9% | 4.7% | 53.1% | 0.83 | 0.73 | 0.90 |
| 8 | Cam morphology is a cartilage or bony prominence (bump) of varying size at any location around the femoral head-neck junction, which changes the shape of the femoral head from spherical to aspherical | 1.6% | 90.5% | 1.5% | 92.3% | 0.47 | 0.26 | 0.64 |
| 9 | Primary cam morphology often occurs in male athletes in both hips | 5.1% | 50.8% | 3.2% | 45.2% | 0.89 | 0.83 | 0.94 |
| 10 | The most common outcome measure for cam morphology is a cartilage or bone alpha angle as a dichotomised or continuous variable on radiographs, CT scans or MRI, reported per hip, per person or both | 0% | 72.6% | 0% | 74.6% | 0.72 | 0.58 | 0.82 |
| 11 | Primary cam morphology likely develops during maturation in young adolescents (with no current or previous hip disease), possibly due to high-load sporting activity and other unconfirmed risk factors | 1.6% | 82.3% | 0% | 93.8% | 0.60 | 0.41 | 0.74 |
| 12 | A comprehensive definition for primary cam morphology would be: Primary cam morphology is a cartilage or bony prominence (bump) of varying size at any location around the femoral head-neck junction, which changes the shape of the femoral head from spherical to aspherical. It often occurs in male athletes in both hips. The most common outcome measure is a cartilage or bone alpha angle as a dichotomised or continuous variable on radiographs, CT scans or MRI, reported per hip, per person or both. Primary cam morphology likely develops during maturation in young adolescents (with no current or previous hip disease), possibly due to high-load sporting activity and other unconfirmed risk factors. | 0% | 93.7% | 1.6% | 96.9% | 0.44 | 0.21 | 0.62 |
| Terminology | ||||||||
| 13 | Cam morphology is the preferred term to use for a bone/ cartilage bump at any location around the femoral head-neck junction | 1.6% | 87.5% | 1.5% | 87.7% | 0.56 | 0.36 | 0.71 |
| 14 | Cam lesion is the preferred term to use for a bone/ cartilage bump at any location around the femoral head-neck junction | 75.8% | 6.5% | 83.1% | 4.6% | 0.84 | 0.69 | 0.91 |
| 15 | Cam deformity is the preferred term to use for a bone/cartilage bump at any location around the femoral head-neck junction | 71.0% | 12.9% | 81.5% | 7.7% | 0.67 | 0.50 | 0.79 |
| 16 | Cam abnormality is the preferred term to use for a bone/cartilage bump at any location around the femoral head-neck junction | 80.6% | 4.8% | 86.2% | 4.6% | 0.70 | 0.54 | 0.81 |
| 17 | Cam-type deformity is the preferred term to use for a bone/cartilage bump at any location around the femoral head-neck junction | 79.0% | 3.2% | 84.6% | 4.6% | 0.8 | 0.69 | 0.87 |
| 18 | Cam-type abnormality is the preferred term to use for a bone/ cartilage bump at any location around the femoral head-neck junction | 79.0% | 6.5% | 87.7% | 3.1% | 0.64 | 0.45 | 0.77 |
| 19 | Cam-type lesion is the preferred term to use for a bone/cartilage bump at any location around the femoral head-neck junction | 77.4% | 3.2% | 89.2% | 1.5% | 0.69 | 0.48 | 0.82 |
| 20 | Pistol grip deformity is the preferred term to use for a bone/cartilage bump at any location around the femoral head-neck junction | 85.2% | 1.6% | 92.2% | 0.0% | 0.64 | 0.40 | 0.78 |
| 21 | Pistol grip lesion is the preferred term to use for a bone/cartilage bump at any location around the femoral head-neck junction | 85.2% | 3.3% | 92.2% | 1.6% | 0.59 | 0.37 | 0.74 |
| 22 | Pistol grip abnormality is the preferred term to use for a bone/ cartilage bump at any location around the femoral head-neck junction | 85.2% | 4.9% | 92.2% | 1.6% | 0.44 | 0.22 | 0.63 |
| 23 | Cam-type impingement is the preferred term to use for hip-related pain due to a bony bump at any location around the femoral head-neck junction | 56.5% | 16.1% | 56.3% | 10.9% | 0.78 | 0.65 | 0.86 |
| 24 | Cam femoroacetabular impingement (FAI) is the preferred term to use for hip-related pain due to a bony bump at any location around the femoral head-neck junction | 53.2% | 27.4% | 51.6% | 20.3% | 0.83 | 0.74 | 0.90 |
| 25 | Cam-type FAI is the preferred term to use for hip-related pain due to a bony bump at any location around the femoral head-neck junction | 59.7% | 19.4% | 51.6% | 20.3% | 0.82 | 0.72 | 0.89 |
| 26 | FAI Syndrome with cam morphology is the preferred term to use for hip-related pain due to a bony bump at any location around the femoral head-neck junction | 7.9% | 69.8% | 7.8% | 75.0% | 0.65 | 0.47 | 0.77 |
| 27 | FAI Syndrome with cam deformity is the preferred term to use for hip-related pain due to a bony bump at any location around the femoral head-neck junction | 71.0% | 6.5% | 81.5% | 4.6% | 0.81 | 0.66 | 0.89 |
| 28 | FAI Syndrome with cam abnormality is the preferred term to use for hip-related pain due to a bony bump at any location around the femoral head-neck junction | 74.2% | 4.8% | 81.5% | 4.6% | 0.82 | 0.70 | 0.89 |
| 29 | FAI Syndrome with cam lesion is the preferred term to use for hip-related pain due to a bony bump at any location around the femoral head-neck junction | 71.0% | 4.8% | 83.1% | 4.6% | 0.72 | 0.52 | 0.84 |
| 30 | FAI Syndrome with cam-type abnormality is the preferred term to use for hip-related pain due to a bony bump at any location around the femoral head-neck junction | 74.2% | 6.5% | 84.6% | 1.5% | 0.72 | 0.55 | .83 |
| 31 | FAI Syndrome with cam-type deformity is the preferred term to use for hip-related pain due to a bony bump at any location around the femoral head-neck junction | 69.4% | 9.7% | 81.5% | 4.6% | 0.75 | 0.56 | 0.85 |
| Taxonomy | ||||||||
| 32 | We should distinguish between primary and secondary cam morphology in clinical practice | 6.5% | 74.2% | 6.2% | 83.1% | 0.87 | 0.79 | 0.92 |
| 33 | We should distinguish between primary and secondary cam morphology in research | 4.6% | 90.8% | 4.6% | 92.3% | 0.71 | 0.57 | .815 |
| 34 | We should distinguish between primary and secondary cam morphology in patients with FAI syndrome | 6.5% | 66.1% | 4.7% | 68.8% | 0.82 | 0.72 | 0.89 |
| 35 | We should distinguish between primary and secondary cam morphology in research participants with FAI syndrome | 4.7% | 84.4% | 4.6% | 90.8% | 0.69 | 0.53 | 0.80 |
| Imaging outcomes | ||||||||
| 36 | The main imaging modality for research on how primary cam morphology develops should be MR with radial imaging (1.5T or 3 T) | 1.9% | 75.9% | 1.8% | 89.3% | 0.81 | 0.59 | 0.90 |
| 37 | The minimum acceptable number of radial sequence MRI slices for research on how primary cam morphology develops should be 12 slices (30° intervals in all 12 clock face positions from 12 o'clock to 11 o'clock positions) | 0% | 60.0% | 0% | 81.6% | 0.7 | 0.49 | 0.83 |
| 38 | Referring to precisely quantifying the asphericity of the femoral head-neck junction on radial sequence MRI: use either radial sequences along the axis of the femoral neck (providing higher resolution images) or radial reconstructions from 3-dimensional acquisitions | 0% | 75.0% | 0% | 87.0% | 0.84 | 0.70 | 0.92 |
| 39 | The MRI protocol for research on how primary cam morphology develops should include: (1) unilateral small field-of-view sequences and radial images of a randomly selected or both hips; as well as (2) femoral torsion assessment (fast axial sequences of the distal knee—femoral condyles—and proximal femoral neck); and (3) a fluid sensitive sequence covering the whole pelvis (in axial or coronal planes; to screen for soft-tissue and bone marrow oedema beyond the hip) | 5.9% | 64.7% | 0% | 78.4% | 0.71 | 0.47 | 0.85 |
| 40 | The MRI for prospective research on how primary cam morphology develops should be repeated every 18 to 24 months | 11.3% | 56.6% | 7.3% | 56.4% | 0.86 | 0.78 | 0.92 |
| 41 | In primary cam morphology epidemiological research (eg, when regression is being used in aetiology or prognosis research) continuous imaging outcome measures (variables) like the alpha angle should be kept continuous | 3.6% | 72.7% | 0% | 89.3% | 0.77 | 0.58 | 0.87 |
| 42 | The cam morphology MRI outcome measure for research on how primary cam morphology develops (aetiology) should be the alpha angle for bone and cartilage as a continuous variable reported for all the o’clock locations around the femoral head-neck junction regardless of the symptomatic state of the research participant. | 5.4% | 66.1% | 0% | 80.7% | 0.81 | 0.68 | 0.89 |
| 43 | For research on how primary cam morphology develops it is important to quantify the epiphysial morphology MRI outcome measure using epiphysial extension | 4.8% | 57.1% | 0% | 65.9% | 0.83 | 0.68 | 0.91 |
| 44 | For research on how primary cam morphology develops the epiphysial morphology MRI outcome measure should also be quantified using epiphysial tilt | 5.1% | 43.6% | 0% | 44.2% | 0.81 | 0.67 | 0.90 |
| 45 | The main imaging modality for longitudinal primary cam morphology prognosis research should be anteroposterior (AP) pelvis and Dunn 45° view radiographs repeated at least every 5 years | 20.4% | 44.9% | 15.4% | 42.3% | 0.91 | 0.84 | 0.95 |
| 46 | The radiographic imaging outcome measure for research on primary cam morphology prognosis should be the alpha angle as a continuous variable reported for AP pelvis and Dunn 45° view radiographs | 15.7% | 56.9% | 11.3% | 67.9% | 0.90 | 0.83 | 0.94 |
| 47 | In addition to reporting alpha angles as continuous in studies on aetiology or prognosis the following quantitative and qualitative imaging outcome measures to categorise cam morphology can be useful in research or clinical practice: (1) Alpha angle ≥60° (preferred) (2) Head-neck offset <8 mm and head-neck offset ratio ≤0.15 usually at the anterior (3 o’clock) location around the femoral head-neck junction (in addition to (1)); Osseous or cartilage convexity of the femoral head neck junction at any location (in addition to (1) and (2)) | 2.1% | 52.1% | 0% | 72.5% | 0.81 | 0.68 | 0.89 |
Green (high agreement on ‘consensus in’): Statement scored as critical (7–9) by ≥70% of panel members and not important (1–3) by <15% of panel members.
Red (high agreement on ‘consensus out’): Scored as not important (1–3) by ≥70% of panel members and critical (7–9) by <15% of panel members.
Yellow (non-consensus): Neither of the ‘consensus in’ or ‘consensus out’ criteria were met.
ICC is an indication of the level of agreement (within-subject variation and between-subject variance of individual statement scores between round 1 and round 2.) We used the lower bound 95% CI of the ICC estimate as the basis to evaluate the level of reliability using the following general guideline: values <0.5 were classified as poor reliability ICC values 0.5–0.75 moderate reliability and 0.75–0.9 indicated good reliability and ICC values >0.9 indicated excellent reliability.
*Type A ICC coefficients using an absolute agreement definition; two-way mixed effects model where people effects are random and measures effects are fixed.
ICC, intraclass correlation coefficient.
Figure 3.
Marginally non-consensus statements 34, 43 and 46 (and statement 76 relevant to Delphi exercise domain 5; Oxford consensus study, part 2). Recalculating consensus after removing the four outliers for statements 34 and 46 resulted in consensus. OS, orthopaedic surgeon; PT, physical therapist.
Here, we report the quantitative results, analysis of qualitative feedback and dissent analysis of the Delphi rounds for definition, terminology, taxonomy and imaging outcomes statements. An online Interacting Group Process followed the Delphi exercise; six mixed stakeholder groups of 5–8 panellists (n=43), discussed the Delphi exercise results on 22 September 2021. We summarise the discussions in boxes 1–4 and online supplemental file 8.
Box 1. Interacting Group Process: mixed stakeholder group discussion summary—definition domain.
Mixed stakeholder groups agreed on the importance of primary cam morphology (PCM) as a concept. This taxonomy, differentiating between primary and secondary cam morphology (SCM), offers several advantages that offset its drawbacks—‘their origins are important to distinguish’, and ‘it has utility in research, prognosis and treatment.’ In research the taxonomy is ‘important for classification’, while the prognosis is often worse for SCM. Treatment maybe distinctly different as most individuals with PCM will never present with any symptoms. The panel contended more work is needed to authentically engage a small group that is not yet convinced that PCM is an important concept.
Although there is agreement, albeit ‘based on the (limited) available literature’, that PCM is more common in males and mostly asymptomatic, female athletes also develop this morphology and ‘longer-term consequences of PCM seem to affect women as much as men.’ More inclusive research is needed involving minoritised female cohorts.
Although there is agreement that PCM, unlike SCM, often occurs bilaterally, and this distinction ‘is the defining element for PCM versus SCM, and important for patients’, this is not always the case. Some patients might have unilateral PCM while others might present with a combination of primary and SCM.
The mixed stakeholder groups agreed that PCM also include the group where no clear aetiology ‘at an individual level’ exists. It is likely that a ‘complex relationship’ between PCM and ‘a genetic susceptibility’ exists. Genetics as risk factor, and ‘the interplay between genetic risk and load relationship’ should therefore be considered and researched.
Despite strong consensus that PCM develops during skeletal maturation ‘as a normal physiological response to load’ (statement 1) further qualified as ‘high-load sporting activity’ (statement 11), some panellists, during the online discussions, felt ‘normal’ is ‘potentially problematic.’ However, the high prevalence of PCM in largely asymptomatic professional athletes—‘several studies showed >80% prevalence’—begs the question: ‘when does it [physiological response] become abnormal? …when it’s very painful?’ Furthermore, high-load sporting activity for one athlete might be normal-load sporting activity for another; load type (‘torsion, varus/valgus’) and skeletal maturation status are both important variables to consider in clinical practice and research.
Box 2. Interacting Group Process: mixed stakeholder group discussion summary—terminology domain.
The Delphi panel achieved strong consensus on using the term ‘morphology’ and to abandon ‘lesion’, ‘deformity’ and ‘abnormality’: ‘large foreign words set the tone for fear, unknown, not in control, especially about [the] outcome.’ Although the majority agreed, some felt that ‘language didn’t necessarily change things for patients’, and that the consequences (‘the pathology part’) of primary cam morphology ‘is the bigger problem and needs to be part of the file, but the patient doesn’t necessarily need to know about this [wording].’ Others thought that ‘morphology should be avoided in patient consultations as it’s unfriendly, not well understood and likely medical "jargon".’ A further problem is that ‘morphology’ doesn’t always translate well into other languages.
Although ‘bump’ is easy for patients to understand and visualise (‘I use "bump" to make it easy for patients’), some felt primary cam morphology is ‘likely more complex than "bump".’ ‘Morphology and syndrome sound more scientific. Bump totally not.’ Another group warned about the possible ‘nociceptive response in patients’ caused by associating the term ‘bump’ with ‘bumping bones’, or of ‘things hitting.’ ‘Therefore we may need to take care with using this term [bump] too.’ One mixed stakeholder group concluded that the ‘language we use in patient-facing consultations should be tailored to the person’ and mentioned alternatives like ‘bumpy-shape’ and ‘egg-shape.’ There was agreement to use ‘less threatening’ language supported by visual aids ‘images/figures.’ While it might be appropriate to ‘tailor terms to three different target audiences: researchers, clinicians and patients and public’, stakeholder groups suggested that patient and public involvement group should inform further research on this.
Validating the Warwick Agreement, the Delphi panel achieved strong consensus on using the ‘much preferred scientifically’ term, ‘femoroacetabular impingement (FAI) Syndrome’ for FAI in patients with symptoms (pain/stiffness etc). However, some felt that ‘syndrome’ sounds ‘too serious.’ Arguing that ‘words matter’ panellists discussed the importance to ‘tailor language to the individual’, and distinguish between a ‘research discussion vs talking with patients.’ Commenting on the 2016 Warwick Agreement, a member of that panel mentioned ‘we considered whether "syndrome" might apply a negative label to patients, but the expert patient member of the panel did not feel this would be the case, but could be good to bounce this off more patients too.’ We therefore need ‘further patient-orientated research to assess whether it [syndrome] has negative consequences and whether FAI used in isolation may be a better term when communicating with patients.’
Box 3. Interacting Group Process: mixed stakeholder group discussion summary—taxonomy domain.
The general agreement was that it is important (and not necessarily difficult) to distinguish between primary and secondary cam morphology in clinical practice and in research: ‘Where we can, we should make the differential diagnosis as it affects the prognosis and therefore the management of the problem.’ A librarian panellist emphasised the benefit of ‘consistent terminology’ when reviewing the literature: ‘using primary versus secondary allowed searching the literature more clear.’ Although most panellists felt that ‘history is key’ to distinguish between primary and secondary cam morphology, others felt that ‘obtaining a detailed history and discussion with patient is more important than a label of primary and secondary.’
It can be clinically challenging when a combination of primary and secondary cam morphology exists in the same patient as ‘there are some cases where primary cam morphology exists prior to a secondary injury (eg, SCFE), and these cases can be a little more difficult to diagnose but are less commonly observed.’
SCFE, Slipped capital femoral epiphysis
Box 4. Interacting Group Process: mixed stakeholder group discussion summary—imaging outcomes domain.
Commenting on the ‘obvious ethical consideration for the amount or frequency of imaging’, a radiologist in one of the mixed stakeholder groups felt ‘the more the better in terms of insight’, and raised the possible benefit of radial vs block imaging—‘block images may allow you to evaluate the images later through the use of novel techniques such as artificial intelligence.’ While one group felt that yearly MRI is appropriate when investigating how primary cam morphology develops in boys (from 11 to 16 years) and girls (from 9 to 14 years), another commented that ‘the time interval should be much shorter if it is to be truly "ideal" (eg, every 3 months). This would capture periods of considerably faster growth or considerable changes in load’, while ‘more frequent imaging will help in periods of rapid growth but it is also important to have frequent serial imaging even in periods without rapid growth to assess the influence of growth spurts.’ However, the value of serial imaging was questioned, as, for example, ‘positions [of primary cam morphology] might vary making it impossible to use them to track changes over time.’ One group warned that the use of serial radiographs to investigate primary cam morphology aetiology constitutes research waste: ‘if you can’t do serial MRIs at short enough intervals, don’t waste time and money; don’t do the study.’
Discussing long-term prognosis studies, groups agreed MRI trumps radiography and ‘should be the investigation of choice where at all possible in adolescent populations.’ The quality of imaging is better, it better quantifies cartilaginous progression in adolescents where ‘the use of alpha-angle on X-ray can be misleading and therefore inaccurate’, and, as it does not pose a (cumulative) radiation risk ‘ethics committees are more likely to accept MRI based studies.’ However, there are at least three issues with MRI: cost, availability (equipment and expert radiologists), and the burden of procedure (time, claustrophobia, etc). MRI is challenging in young adolescents ‘due to difficulty remaining still, that is, movement artefact.’
The group agreed that further work is needed to develop and refine consensus on the specific and standardised imaging protocol: ‘If X-rays are used then it has to be reinforced on the views that are valuable and this message should be repeated in order to support this becoming routine practice; not all facilities are skilled with specific radiograph images for example, Dunn.’
It is further important to consider dissemination of findings: ‘Do athletes want to know the results? How, what, and when do we communicate imaging results to participants or parents? Do we consider positive/negative response by athletes/parents, and provide them with the ‘opt in’ opportunity not to be informed of their individual imaging results?’ Group members raised four important points from the athlete/parent’s perspective. First, parents ‘were not comfortable’ with cumulative radiation exposure associated with serial radiographs. Radiation exposure is an ‘ethical dilemma in this area’ with ‘a need to be up front and transparent with information so parents are aware.’ Second, sharing of imaging results is a ‘hugely important area’ and research teams should carefully consider the possibility that ‘parents may pick up the information or interpret it differently than healthcare practitioners.’ Third, research teams should consider ‘an "opt-in" option for participants and parents where, except if there is an issue with an imaging finding, they will not be informed of the results.’ Last, research teams should carefully consider how they communicate periodic imaging results and suggested a ‘common approach to dissemination of results/imaging is needed.’
Definitions: Delphi domain 1
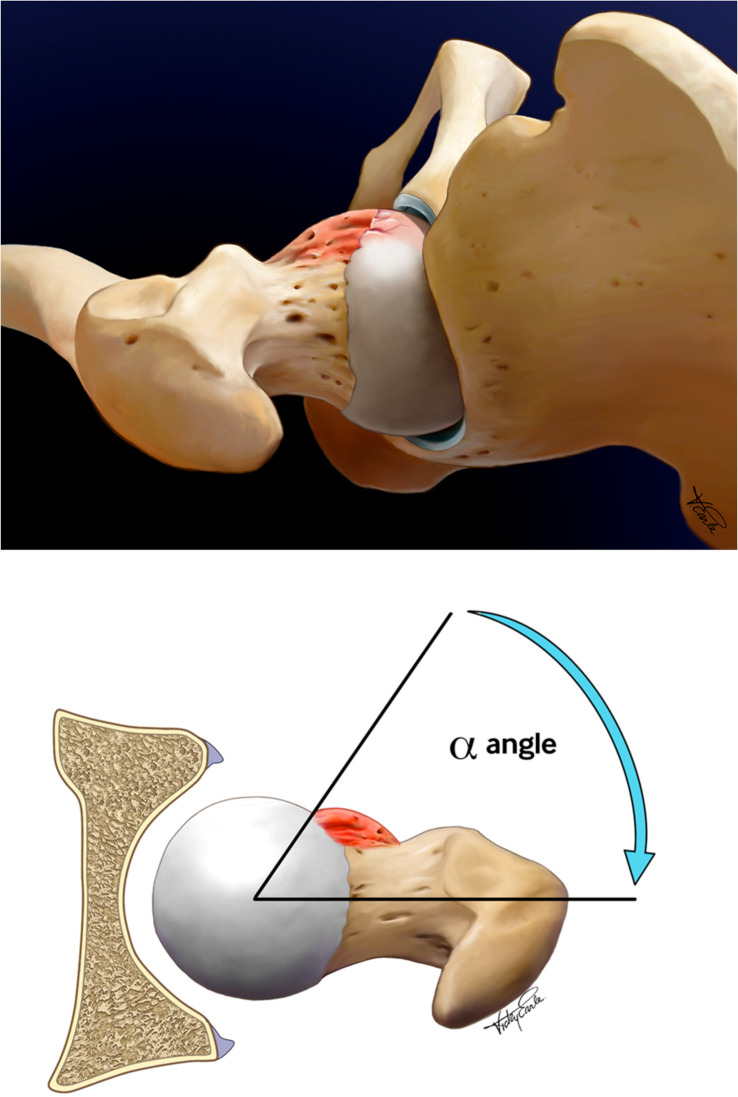
The Delphi panel reached consensus on 9 of 12 definition statements in rounds 1 and 2 (table 4; online supplemental file 5). The panel agreed on a comprehensive definition for PCM, based on its five proposed conceptual attributes (figure 4; statements 1, 2, 4, 5, 8, 10–12). The panel also agreed that secondary cam morphology develops due to existing and/or pre-existing hip disease (statement 3).
Figure 4.
Primary cam morphology definition. Primary cam morphology is a cartilage or bony prominence (bump) of varying size at any location around the femoral head-neck junction of the hip, which changes the shape of the femoral head from spherical to aspherical. It occurs most often in asymptomatic male athletes in both hips. The preferred outcome measure for research on primary cam morphology aetiology is a cartilage or bone alpha angle as a continuous variable on radial MRI along the axis of the femoral neck, using 30° intervals from 12 o'clock to 11 o'clock positions, reported per hip, per person or both. In addition to a continuous alpha angle, a dichotomous alpha angle (using a threshold of ≥60°) can be useful in clinical practice or research. Primary cam morphology develops during skeletal maturation in young adolescents (with no current or previous hip disease), as a normal physiological response to high-load sporting activity and other unconfirmed risk factors. Illustrations from Dijkstra et al. (2021)5
Qualitative analysis identified 12 themes (online supplemental files 5 and 6). The first four themes illuminated tension and dissent related to three non-consensus definition statements (statements 6, 7 and 9).
bjsports-2022-106085supp006.pdf (226.2KB, pdf)
First, some Delphi panel members commented that PCM’s origin is not ‘entirely "unknown" [but] likely due to variable loading demands’ (statement 6). However, ‘at an individual level not all PCM has [a] clear cause.’ Second, the Delphi panel did not agree that ‘all cam morphology in young and active adults without any symptoms or history of previous hip disease is PCM until proven otherwise’ (statement 7). Some found the ‘concept of primary and secondary cam morphology’ challenging. Third, the statement ‘PCM is more common in male athletes in both hips’ (statement 9) created the impression that this morphology was a ‘male-only problem’ while the reality is ‘females [are] often left out of research.’ Last, while the Delphi panel agreed that PCM usually occurs bilaterally, representing ‘a defining element for primary vs secondary cam morphology and important for patients’, some athletes might have unilateral PCM.
Dissent analysis (online supplemental file 7). Outlier analysis: Although outliers were identified for ten of twelve definition statements in round 2, they did not influence group consensus or non-consensus. None of the outliers provided qualitative comments. One physical therapist ‘did not agree that the concept of primary and secondary CAM is commonly agreed and established’, choosing ‘Unable to score’ for most of the definition statements in rounds 1 and 2. Bipolarity analysis: There was no bimodal distribution in the overall scoring of definition statements. Stakeholder group analysis: There was no significant difference in how stakeholder groups scored definition statements in rounds 1 and 2.
bjsports-2022-106085supp007.pdf (1.6MB, pdf)
Terminology: Delphi domain 2
The Delphi panel reached consensus on 14 of 19 terminology statements in round 1 and 16 in round 2—consensus on two statements to include (‘consensus in/agree’), and consensus on 14 statements to exclude (‘consensus out/disagree’) certain terms. The panel agreed that ‘cam morphology’ is the preferred term to use for a bone/cartilage bump at any location around the femoral head-neck junction (statement 13), and ‘FAI syndrome with cam morphology’ (statement 26) for hip-related pain due to a bony bump at any location around the femoral head-neck junction. The Delphi panel agreed to avoid (‘consensus out’) terms ‘lesion’, ‘deformity’ and ‘abnormality’ (statements 14–22 and 27–31).
Three statements related to the terms proposed for hip-related pain due to a bony bump at any location around the femoral head-neck junction, did not reach consensus: ‘cam-type impingement’ (statement 23), ‘cam FAI’ (statement 24) and ‘cam-type FAI’ (statement 25).
Qualitative analysis identified four themes (online supplemental files 5 and 6). First, warning that ‘abnormality is not a very optimistic term’, panellists preferred the term ‘morphology’: ‘We’ve agreed it is a "normal physiological response" and therefore shouldn’t be called a lesion/ deformity with their connotations of abnormality.’ Second, a panellist suggested replacing ‘bump’ with ‘prominence’ as ‘not every cam morphology has a "bump". It might only be decreased offset and that certainly does not constitute a "bump".’ Third, although ‘FAI syndrome’ is the agreed term for hip-related pain due to a bony bump at any location around the femoral head-neck junction, one panellist warned that other causes for hip-related pain exist, and ‘(FAI syndrome) is one type of pathology’ in the hip. Last, one panellist disagreed with the term ‘any location’, as ‘an inferior bony bump may not lead to FAI.’
Dissent analysis (online supplemental file 7). Outlier analysis: Outliers (present in 16 of the 19 terminology statements) in round 2, did not influence group consensus or non-consensus. The orthopaedic surgeon outlier for statements 13 and 26 did not agree that PCM refers to a bump ‘at any location’ around the femoral head-neck junction. One physician chose ‘unable to score’ for most of the terminology statements in round 1 as they misinterpreted the statement wording. Feedback after round 1 clarified the misunderstanding. Bipolarity analysis: There was no bimodal distribution in the overall scoring of terminology statements. Stakeholder group analysis: The average terminology statement scores were significantly different for the physical therapist stakeholder group compared with the researcher stakeholder group (statement 23, round 1; statement 24, rounds 1 and 2), and for the radiologist stakeholder group compared with the researcher stakeholder group (statement 24, round 2).
Taxonomy: Delphi domain 3
The Delphi panel reached consensus in rounds 1 and 2 on three of four statements in the taxonomy domain. There is consensus that we should distinguish between primary and secondary cam morphology in clinical practice and in research (statements 32 and 33), and in research participants with FAI syndrome (statement 35). However, there was marginal non-consensus on the importance of distinguishing between primary and secondary cam morphology in patients (clinical practice) with FAI syndrome (statement 34).
Qualitative analysis of individual panellist feedback identified six themes (online supplemental files 5 and 6). First, although not agreed as critical by the panel, distinguishing between primary and secondary cam morphology in patients with FAI syndrome (statement 34) is important as ‘secondary CAM morphology has a poorer prognosis and therefore should be distinguished to improve treatment planning.’ Second, the taxonomy is important for diagnosis. Third, the taxonomy is important for treatment. Fourth, the taxonomy is important for prognosis. Fifth, distinguishing between primary and secondary cam morphology is age dependent and perhaps ‘less relevant if someone is 30 years old.’ Last, panellists commented on the challenge ‘where a patient has a mix of both’ primary and secondary cam morphology.
Dissent analysis (online supplemental file 7). Outlier analysis: Although strong consensus was achieved for statements 32, 33 and 35, few outliers (mainly orthopaedic surgeons and a physical therapist) were not convinced. After removing two outliers for statement 34, the Delphi panel reached consensus on the importance of distinguishing between primary and secondary cam morphology in patients with FAI syndrome (figure 3 and online supplemental files 5 and 7). Bipolarity analysis: There was no bimodal distribution in the overall scoring of taxonomy statements. Stakeholder group analysis: The average scores for taxonomy statement 32 were significantly different for PPI group compared with the: (1) orthopaedic surgeon stakeholder group (round 2); (2) physical therapist stakeholder group (rounds 1 and 2); (3) radiologist stakeholder group (rounds 1 and 2) and (4) researcher stakeholder group (round 2). PPI stakeholder group compared with the physical therapist stakeholder group scored statement 34 significantly different (rounds 1 and 2).
Imaging outcomes: Delphi domain 4
The Delphi panel reached consensus on 3 of 12 imaging outcomes statements in round 1 and 7 of 12 in round 2. Radial sequence 1.5 T or 3 T MRI should be used for research on how PCM develops (statements 36–38), with continuous bone and/or cartilage alpha angles as the agreed outcome measure reported for all the o’clock locations around the femoral head-neck junction regardless of the symptomatic state of the research participant (statements 41 and 42). MRI protocols for research on how PCM develops should include: (1) unilateral small field-of-view sequences and radial images of a randomly selected or both hips, as well as (2) femoral torsion assessment (fast axial sequences of the distal knee—femoral condyles—and proximal femoral neck), and (3) a fluid sensitive sequence covering the whole pelvis (in axial or coronal planes to screen for soft-tissue and bone marrow oedema beyond the hip) (statement 39).
In addition to reporting alpha angles as continuous in studies on aetiology or prognosis, other quantitative and qualitative imaging outcome measures to categorise cam morphology can be useful in research or clinical practice (statement 47).
The Delphi panel did not reach consensus on five imaging outcomes statements. First, panellists did not agree that ‘every 18–24 months’ is the preferred time interval for serial MRI in prospective research on how PCM develops. Some commented ‘it really depends on the research question’, while others suggested it should be ‘more often’, acknowledging that ‘it will be difficult but if there is a critical window that we want to identify, 2-year intervals would not be frequent enough’ (statement 40). Second, although it is ‘probably critical’, panellists felt ‘insufficient data’ exist to support using epiphysial extension or epiphysial tilt to quantify epiphysial morphology on MRI (statements 43 and 44). Third, questioning the evidence for a 5-year imaging interval, panellists did not agree on the main imaging modality for longitudinal PCM prognosis research nor how often to repeat the imaging. While some suggested frog-leg lateral or Dunn view radiographs, and others ‘any lateral head-neck view depending on the particular centre’, a few panellists preferred MRI with all clock positions (statement 45). Last, the panel failed to agree that, for prognosis studies, radiographs (anteroposterior, AP pelvis and Dunn 45° views) should be used to calculate the alpha angle. Some preferred MRI with all clock positions and others felt AP pelvis alpha angles are ‘too imprecise.’ Panellists reminded that, to date, ‘there is no consensus on optimum threshold for dichotomising this [alpha angle] variable. It makes comparing across studies very difficult when different thresholds are used.’ Despite this, a diagnostic threshold might be important for clinicians (statement 46).
In addition to the above, qualitative analysis of individual panellist feedback identified nine more themes (online supplemental files 5 and 6): (1) the ‘huge cost aspect’ of MRI is an important consideration, especially for minoritised and marginalised research populations; (2) disagreement on PCM as a concept; (3) the importance of qualifying ‘type of radial MRI’; (4) ‘fluid sensitive pelvis images’ are unnecessary when studying PCM development because ‘the rationale for this is to find pathological processes elsewhere’; (5) research question will determine the preferred imaging; (6) confusion created by alternative PCM imaging outcome measures; (7) importance of standardising imaging across research; (8) concern about radiation exposure of serial radiographs. While radiographs are ‘cheap’ with ‘little time costs’, the concerns are ‘radiation and less detail’; (9) lack of knowledge to score imaging statements.
Dissent analysis (online supplemental file 7). Outlier analysis: Six of 12 imaging outcomes statements (statements 36, 39, 42, 44, 45 and 46) had outliers. After eliminating the two orthopaedic surgeon outliers for marginally non-consensus statement 46, the Delphi panel reached consensus that alpha angle as a continuous variable, reported for AP pelvis and Dunn 45° view radiographs, should be the radiographic imaging outcome measure for research on PCM prognosis (figure 3). Bipolarity analysis: There was no bimodal distribution in the overall scoring of imaging outcomes statements. Stakeholder group analysis: There was no statistically significant difference in how stakeholder groups scored the imaging outcomes statements in rounds 1 and 2.
Discussion
An international Delphi panel of expert clinicians, athletes, patients and their representatives, and researchers—representing the YAHiR collaborative—agreed on four key PCM elements (definition, terminology, taxonomy and imaging outcome measures). In what follows, we discuss the Delphi panel’s opinions on these key elements and summarise how agreement and areas of tension and dissent inform a more rigorous, inclusive and evidence-based approach to research on PCM and its natural history.
Definitions: Delphi domain 1
The Delphi panel agreed on a comprehensive conceptual and operational definition for PCM (figure 4).
The conceptual definition equips all stakeholders, especially athletes and patients, with meaningful language to describe an abstract concept in their hip. It is a bony or cartilage prominence (or ‘bump’), with shape (aspherical), size (most are small; some are large), location (anywhere around the head-neck junction of the hip but predominantly anterolateral) and ownership (it is more prevalent in male athletes compared with females and non-athletes, and more common in both hips).5 Ownership also implies ‘lived with’—opening the door for conversations and qualitative research with athletes and patients on their experiences.
While celebrating consensus, tension and dissent spotlighted three areas for future research. First, although this morphology is more prevalent in male versus female athletes, very little research involves female athletes, and no research has been done in para-athlete cohorts—researchers must cast a much broader net to involve minoritised and marginalised groups. Second, although the vast majority of athletes with PCM will never develop symptoms or hip disease, some do. Yet, we cannot predict with confidence who these athletes are. While important to investigate the morphology’s prognosis, we should take care not to medicalise a common, mostly benign morphology. The key messages are: (1) this largely benign morphology develops as a ‘normal physiological response’ to ‘high-load’ physical activity, and (2) childhood physical activity and sport are important. Third, we should investigate the tension between ‘normal and abnormal’ as it relates to the capital femoral growth plate’s physiological response to load. Bone is a dynamic tissue; how mechanical loading influences the epiphysial growth plate is physiologically complex depending, for example, on the load type, and physical and physiological maturity. What might be a normal load for one athlete is abnormal or high-load for another.
Terminology: Delphi domain 2
Confirming the Warwick Agreement’s recommendations,7 this much larger, more inclusive and diverse panel agreed that PCM is a ‘morphology’ and not a ‘lesion’, ‘abnormality’ or ‘deformity’; in athlete-patients presenting with symptoms the agreed term is ‘FAI syndrome.’ However, while these are acceptable scientific terms, ‘morphology’ and ‘syndrome’ do not resonate with everyone. These terms are not necessarily patient-friendly and ‘morphology’ does not translate well into at least some other languages (of expert panel members). With patient and public partners, more work is needed to further refine preferred patient-friendly terms.
Taxonomy: Delphi domain 3
PCM, in contrast with secondary cam morphology, is a predominantly benign hip morphology that develops during maturation in many athletes. The Delphi panel agreed with this cam morphology taxonomy.5 Distinguishing between primary and secondary cam morphology offers advantages. First, a cam morphology taxonomy provides clarity and consistent terminology with utility in research; researchers describe their populations better with more specific inclusion and exclusion criteria. Second, primary and secondary cam morphology have distinctly different aetiology and prognosis. Contrary to secondary cam morphology, PCM develops during maturation due to load and is largely benign—an important distinction that empowers athletes and patients to embrace normality and their ‘happy hips’. Third, the clinical approach to an athlete with FAI syndrome and PCM is different to a patient with FAI syndrome and secondary cam morphology. The general agreement was that ‘it is not difficult to distinguish between primary and secondary cam morphology.’ However, some patients might have both types while in others, a clear distinction might only be possible later in the disease process.
Imaging outcomes: Delphi domain 4
Acknowledging that operationalising PCM remains challenging, the panel agreed to report a continuous alpha angle—the primary imaging outcome variable for aetiology and prognosis research (figure 4). In agreement with a recent systematic review,47 and the Lisbon Agreement,27–29 and mainly for clinical research, a 60° alpha angle cut-off value can be used to classify PCM. However, alpha angle should be reported as a specific number (continuous variable).
Although the panel agreed that serial MRI (radial imaging) is needed in studies to investigate how PCM develops during maturation, opinions on how often this should be done varied. Some experts suggested MRI every 3 months during the growth spurt, while others opined that every 6–24 months would suffice. MRI, however, is expensive and access to it limited. Not everyone agreed to use AP pelvis and lateral radiographs in long term prognosis studies of PCM or FAI syndrome; however, anything but radiographs will exclude the vast majority of minoritised populations with limited access to expensive three-dimensional imaging (MRI or CT scans) and expert radiologists.
Imaging findings could confuse and worry patients. Researchers should therefore consider how potentially sensitive imaging findings are communicated to athletes, patients and other stakeholders (eg, parents, coaches, club managers). A discussion paper on athlete data in professional sport by the Australian Academy of Sport describes some of the important aspects.48
How this consensus informs research on PCM and its natural history
Having standard PCM conceptual and operational definitions, taxonomy and terminology, empowers researchers, including patient and public partners, to do more rigorous research—research that is more credible, consistent, replicable, and valid, and of a higher quality.49–51 Although the panel reached strong consensus on key elements, this consensus study illuminates challenges relevant to the minoritised, including athletes and patients. It invites authentic collaboration on a level playing field, setting the scene for a more inclusive approach to clinical decision-making and research.
Inclusive PCM research should address issues that matter to patients and improve their lives, ‘access and represent’ the patient’s views and experiences, and treat them with respect.52 To date, research on PCM and its natural history, continue to minoritise important patient-athlete populations—women, children and parents, para-athletes, and athletes from the Global South. Patient partners are to a large extent absent from the research process. While emphasising the importance of meaningful inclusion of patients, giving them an active voice in research, Frankena et al emphasised partnerships that value each other’s skills.53 This consensus study served the inclusive agreement-seeking agenda well—not only did the pragmatic online approach limit travel, it also invited the minoritised and marginalised into the room. PPI colleagues voiced their opinions on improving conceptual and operational elements of the morphology’s definition, using more patient-friendly terminology, and applying a taxonomy that reflects their needs. This inclusive partnership strengthens evidence-based research.
Evidence-based research uses ‘prior research in a systematic and transparent way to inform a new study so that it is answering questions that matter in a valid, efficient and accessible manner’, minimising clinical health research that is unnecessary, irrelevant, unscientific, wasteful and unethical.54–56 While this consensus on the key elements of PCM will help researchers to produce research that is more ‘searchable’ in a systematic and transparent way, it is also a catalyst for a fresh look at evidence—a strong foundation for higher research value and less research waste.
Strengths and limitations
External validity of the Delphi method is often contested. Delphi panel judgements might differ from another equally diverse expert panel. However, many authors have argued that the Delphi method provides evidence of content and face validity—group opinion is more valid than that of a single person, and ‘real-world’ expertise provides confirmative judgement(s) on the subject/phenomenon/concept. Although we applied the ‘closeness continuum’ to purposively recruit a large and diverse expert panel (in terms of sex, geographical representation and profession/stakeholder group), this study’s panel and steering committee could have been more representative of communities that are not widely represented in this field. While making explicit progress on diversity, equity and inclusion, including actively involving a PPI stakeholder group (also as coauthors), we acknowledge that more could be done. This study, and the hip-and-groin research field in general, would benefit from actively involving researchers and participants from minoritised communities (diversity) ‘…including Black, Indigenous, and people of colour, people from the LGBTQIA2S+Community, people with disabilities, people with complex/chronic illnesses, people from the Global South or Far North, people from low-income or middle-income nations, people from stateless communities’ (BJSM Equity, Diversity and Inclusion Guiding Document: https://bjsm.bmj.com/pages/bjsm-key-publishing-resources). However, diversity in isolation is not enough. Clinicians and researchers should work to level the playing field (equity), and actively practice inclusivity (by creating, eg, a welcoming atmosphere, including a positive and supportive experience) to a diverse group of research participants. We used a modified (close ended) Delphi method—the classic open first round may create unambiguous, broad statements leading to bias from the outset. An open first round might also compromise assessment of reliability.57
Although anonymity of the Delphi method and large panels have many advantages, we acknowledge that it has limitations too. These include low compliance, lack of responsibility for the end result and loss of flexibility and richness of non-verbal communication—important elements of unstructured, direct group interaction.31 This study benefited from a closed first round and group interactions that were both anonymous for the Delphi surveys and direct, although online, for the Interactive Group Process. Larger panels, however, might introduce more variation of opinion and false ‘consensus’ as panellists are ‘forced’ to reach consensus without any opportunity to debate the issues or areas of tension and dissent.10 58
The increase in consensus between rounds 1 and 2 can be ascribed to iteration of judgement and partly to an artificial by-product of the pressure to conformity caused by feedback; we provided stakeholder group-specific histograms to all participants between rounds 1 and 2. In addition to anonymous feedback during the Delphi rounds, online mixed stakeholder group discussion meetings were opportunities to deliberate. Here it was possible for certain voices in the online room to dominate; however, group leads were carefully selected to guide conversations, guard against dominance and to give minoritised groups a voice.
Because the aim of this study was not to pursue consensus at all cost, but rather to obtain reasonable consensus while mapping the level of agreement, the panel did not vote again on non-consensus statements during online meetings. Statistical consensus or non-consensus was therefore unchanged but enriched by including deliberations from multiple perspectives.
Although the Delphi panel reached consensus on many statements, we acknowledge that consensus relies on ‘expert judgement’ with possible group pressure to conform. Consensus in a Delphi could therefore be seen as suspect.31
A third Delphi round might have resulted in an even higher overall consensus, although limited to a small number of statements. After removing outliers and reanalysing panellists’ scores, the panel reached consensus on two statements (statements 34 and 46) with marginal non-consensus after round 2.
Conclusion
A diverse and inclusive Delphi panel agreed on four key issues essential to moving clinical practice and research forward in the area of PCM and its natural history: (1) definition, confirming its proposed conceptual attributes (tissue type, size, location, shape and ownership); (2) terminology—use ‘morphology’ and not doom-and-gloom terms ‘lesion’, ‘abnormality’ or ‘deformity’; (3) taxonomy, distinguishing between primary and secondary cam morphology, and (4) imaging outcomes, continuous bone and/or cartilage alpha angles on radial femoral head-neck MRI for research on how PCM develops.
This broad consensus provides athletes, patients, clinicians and researchers with a strong foundation for more precise communication, better clinical decision-making and higher value research on PCM and its natural history.
Acknowledgments
The lead author (HPD) received a Kellogg College, Oxford Research Support Grant to the value of £1000.
Footnotes
Twitter: @DrPaulDijkstra, @Seaniemc89, @clare_ardern, @JoanneLKemp, @AndreaBMosler, @blazey85, @TO_dpr, @azizfar, @aserner, @rwilly2003, @oke_jason, @KarimKhan_IMHA
Collaborators: Young Athlete's Hip Research (YAHiR) Collaborative: Rintje Agricola; Thor Einar Andersen; Olufemi Ayeni; Ian Beasley; Mario Bizzini; Marco Cardinale; Tafadzwa Chiokwindo; Richard de Villiers (deceased); Lars Engebretsen; Tom Entwisle; Emin Ergen; Scott Fernquest; Celeste Geertsema; Mo Gimpel; Fares Haddad; David Hanff; Joshua Heerey; Per Holmich; Franco Milko Impellizzeri; Julie Sandell Jacobsen; Christa Janse van Rensburg; Ara Kassarjian; Vikas Khanduja; Stephanie Kliethermes; Cara Lewis; Travis Maak; Susan Mayes; Inger Mechlenburg; Nonhlanhla Mkumbuzi; Sofie Nelis; Antony Palmer; Theodora Papadopoulou; Marc Philippon; Lauren Pierpoint; Lindsey Plass; Noel Pollock; Michael Reiman; Nia Roberts; Nikki Rommers; Nisrine Sawaya; Toni-Jane Snoxell; Jomar Souza; Louise Strickland; Tina Taseska; Kristian Thorborg; Jane Thornton; Johannes Tol; Larissa Trease; Pim van Klij; Pieter Volcke; Adam Weir; Fiona Wilson; Mara Yamauchi
Contributors: HPD proposed the idea of a Delphi consensus study on the topic, planned and coordinated the study as part of his DPhil Evidence-Based Health Care studies. TG, MC, JLO, KMK and SG-J supervise the lead author’s DPhil studies and provided oversight to the study with other members of the Delphi Study Steering Committee (SMA, CLA, JK, ABM, AP, PB and AS). All steering committee members contributed to, revised and refined the list of Delphi statements. AP co-led the Patient and Public Involvement Group with HPD and, with DR and RWW, facilitated an authentic patient’s voice throughout. AF, with oversight by JLO, contributed to the statistical analysis of the study. Although EM and VM contributed to all stages of the Delphi study, their focus was the imaging- and research priorities domains. CLA and KMK co-chaired with HPD the Interactive Group Process while ABM, AP, JLO, SG-J, DR, SMA, EM, PB, RWW, AS and MC acted as group leads for the 6 small multistakeholder groups. HPD wrote the first draft of the manuscript; all listed authors contributed to reviewing, editing and revising the manuscript, and have read and agreed to the submitted version of the manuscript. The Young Athlete’s Hip Research (YAHiR) Collaborative listed as 'collaborators' were all Delphi panel members and contributed to the online Interactive Group Process and the ENHR ranking exercise.
Competing interests: HPD is a BJSM Associate Editor; CLA is Editor-in-Chief of Journal of Orthopaedic & Sports Physical Therapy (JOSPT); SM, PB, DR, AF, AS, EM, VM, RWW, KMK, JLO, SG-J, MC and TG—none to declare; JK is an editor of BJSM; ABM is BJSM Deputy Editor; AP is an editor at BMJ;
KMK was Editor-in-Chief of BJSM from 2008 to 2020 but holds no position with BJSM or BMJ Group at present (June 2022).
Collaborator group: JT and NM are editors of BJSM; KT and FW are BJSM Deputy Editors; LE is BJSM IPHP Editor; SB, CJvR, JoT, AW, SK and FW are BJSM Associate Editors.
Patient and public involvement statement: We involved patient and public partners in the planning, delivery, and dissemination phases of the Delphi study through the YAHiR Collaborative’s patient and public involvement (PPI) group. The latter group was represented in the Delphi study steering committee. We supplied all members of the PPI group with a glossary, mentored them on definition use and content (during online individual and PPI group meetings), and invited them to weigh in on each Delphi round. They had access to the recordings of the Oxford-Aspetar-La Trobe Young Athlete’s Hip Webinar Series, providing a good knowledge base including the current evidence, and issues, allowing an informed assessment. Members of the PPI group led and actively participated in the mixed stakeholder group discussions following the Delphi rounds (Delphi study, Stage 3).
Provenance and peer review: Not commissioned; externally peer reviewed.
Author note: Equity, diversity and inclusion: The Oxford consensus steering committee (HPD, SMA, CLA, JK, ABM, AP, PB, AS, JLO, KMK, SG-J, MK and TG), 5 women and 8 men, were English-speaking (as a first- or second language) white academics (11 with PhDs); 4 were physicians, 6 allied healthcare practitioners, and 3 health researchers. AP represented the Young Athlete’s Hip Research (YAHiR) Collaborative’s Patient and Public Involvement Group. One resided in the Global South. Interpreting ‘diversity’ as more than representation of certain demographic groups, the steering committee ensured a diverse and informed Delphi panel, representing six multi-profession stakeholder groups, including previously minoritised groups relevant to this research field (eg, women, athletes, patients and the community, participants from the Global South). This study’s online Delphi method, with a specific focus on anonymity and access to adequate topic-specific resources, supported a more equitable and inclusive process. First, the study’s online Delphi method was more equitable (as opposed to an in-person meeting) as traditionally underrepresented groups had similar opportunities to participate—levelling the playing field (they didn’t need to travel and could share their opinion in a ‘safe space’). Second, the study’s online Delphi method was more inclusive (referring to a positive and supportive experience) as our efforts included online meetings to share and discuss study resources and topic-specific information, and giving patient and public involvement partners leading roles in all aspects of the study (including steering committee membership, active involvement in study design, leading roles in online discussions, and co-authorship of study reports, including peer reviewed papers). Finally, in addition to the steering committee members, the main authors included a biostatistician (AF), two radiologists (EMcN and VM), and two additional members of the YAHiR Collaborative’s Patient and Public Involvement Group (DR and RWW). The 18 main authors include six women (including the senior author, TG).
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Contributor Information
Young Athlete’s Hip Research (YAHiR) Collaborative:
Rintje Agricola, Thor Einar Andersen, Olufemi Ayeni, Ian Beasley, Mario Bizzini, Marco Cardinale, Tafadzwa Chiokwindo, Richard de Villiers, Lars Engebretsen, Tom Entwisle, Emin Ergen, Scott Fernquest, Celeste Geertsema, Mo Gimpel, Fares Haddad, David Hanff, Joshua Heerey, Per Holmich, Franco Milko Impellizzeri, Julie Sandell Jacobsen, Christa Janse van Rensburg, Ara Kassarjian, Vikas Khanduja, Stephanie Kliethermes, Cara Lewis, Travis Maak, Susan Mayes, Inger Mechlenburg, Nonhlanhla Mkumbuzi, Sofie Nelis, Antony Palmer, Theodora Papadopoulou, Marc Philippon, Lauren Pierpoint, Lindsey Plass, Noel Pollock, Michael Reiman, Nia Roberts, Nikki Rommers, Nisrine Sawaya, Toni-Jane Snoxell, Jomar Souza, Louise Strickland, Tina Taseska, Kristian Thorborg, Jane Thornton, Johannes Tol, Larissa Trease, Pim van Klij, Pieter Volcke, Adam Weir, Fiona Wilson, and Mara Yamauchi
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by The University of Oxford’s Medical Sciences Interdivisional Research Ethics Committee (MS IDREC) provided ethics approval for the study—R73576/RE001. Participants gave informed consent to participate in the study before taking part.
References
- 1. Doran C, Pettit M, Singh Y, et al. Does the type of sport influence morphology of the hip? A systematic review. Am J Sports Med 2022;50:1727–41. 10.1177/03635465211023500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Dickenson E, Wall PDH, Robinson B, et al. Prevalence of cam hip shape morphology: a systematic review. Osteoarthritis Cartilage 2016;24:949–61. 10.1016/j.joca.2015.12.020 [DOI] [PubMed] [Google Scholar]
- 3. Nepple JJ, Vigdorchik JM, Clohisy JC. What is the association between sports participation and the development of proximal femoral CAM deformity? A systematic review and meta-analysis. Am J Sports Med 2015;43:2833–40. 10.1177/0363546514563909 [DOI] [PubMed] [Google Scholar]
- 4. Beaulé PE, Grammatopoulos G, Speirs A, et al. Unravelling the hip pistol grip/cam deformity: origins to joint degeneration. J Orthop Res 2018;36:3125–35. 10.1002/jor.24137 [DOI] [PubMed] [Google Scholar]
- 5. Dijkstra HP, Ardern CL, Serner A, et al. Primary cam morphology; bump, burden or bog-standard? A concept analysis. Br J Sports Med 2021;55:1212–21. 10.1136/bjsports-2020-103308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bhopal RS. Interrelated concepts in the epidemiology of disease: Natural history, spectrum, iceberg, population patterns, and screening. In: Bhopal R, ed. Concepts of epidemiology: integrating the ideas, theories, principles and methods of epidemiology. 0. Oxford University Press, 2008. [Google Scholar]
- 7. Griffin DR, Dickenson EJ, O'Donnell J, et al. The Warwick agreement on femoroacetabular impingement syndrome (FAI syndrome): an international consensus statement. Br J Sports Med 2016;50:1169–76. 10.1136/bjsports-2016-096743 [DOI] [PubMed] [Google Scholar]
- 8. Brady SR. Utilizing and adapting the Delphi method for use in qualitative research. Int J Qual Methods 2015;14:160940691562138. 10.1177/1609406915621381 [DOI] [Google Scholar]
- 9. J. Skulmoski G, T. Hartman F, Krahn J. The Delphi method for graduate research. JITE:Research 2007;6:001–21. 10.28945/199 [DOI] [Google Scholar]
- 10. Hasson F, Keeney S. Enhancing rigour in the Delphi technique research. Technol Forecast Soc Change 2011;78:1695–704. 10.1016/j.techfore.2011.04.005 [DOI] [Google Scholar]
- 11. McKenna HP. The Delphi technique: a worthwhile research approach for nursing? J Adv Nurs 1994;19:1221–5. 10.1111/j.1365-2648.1994.tb01207.x [DOI] [PubMed] [Google Scholar]
- 12. Greenhalgh T, Wong G, Westhorp G, et al. Protocol--realist and meta-narrative evidence synthesis: evolving standards (RAMESES). BMC Med Res Methodol 2011;11:115. 10.1186/1471-2288-11-115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wong G, Greenhalgh T, Westhorp G, et al. RAMESES publication standards: realist syntheses. BMC Med 2013;11:21. 10.1186/1741-7015-11-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Murphy MK, Black NA, Lamping DL, et al. Consensus development methods, and their use in clinical Guideline development. Health Technol Assess 1998;2:1–88. 10.3310/hta2030 [DOI] [PubMed] [Google Scholar]
- 15. Hasson F, Keeney S, McKenna H. Research guidelines for the Delphi survey technique. J Adv Nurs 2000;32:1008–15. [PubMed] [Google Scholar]
- 16. Brown BB. Delphi process: a methodology used for the elicitation of opinions of experts. Rand Corporation, 1968. Available: https://www.rand.org/pubs/papers/P3925.html [Accessed 13 Feb 2022].
- 17. Sinha IP, Smyth RL, Williamson PR. Using the Delphi technique to determine which outcomes to measure in clinical trials: recommendations for the future based on a systematic review of existing studies. PLoS Med 2011;8:e1000393. 10.1371/journal.pmed.1000393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Li S-A, Yousefi-Nooraie R, Guyatt G, et al. A few panel members dominated Guideline development meeting discussions: social network analysis. J Clin Epidemiol 2022;141:1–10. 10.1016/j.jclinepi.2021.09.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Williamson PR, Altman DG, Bagley H, et al. The comet Handbook: version 1.0. Trials 2017;18:280. 10.1186/s13063-017-1978-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Jünger S, Payne SA, Brine J, et al. Guidance on conducting and reporting Delphi studies (CREDES) in palliative care: recommendations based on a methodological systematic review. Palliat Med 2017;31:684–706. 10.1177/0269216317690685 [DOI] [PubMed] [Google Scholar]
- 21. Okello D, Chongtrakul P, Datta M. A manual for research priority setting using the ENHR strategy. The Council on health research for development (COHRED). document 2000.3. 2000;52. [Google Scholar]
- 22. Miller J, Petrie J. Development of practice guidelines. The Lancet 2000;355:82–3. 10.1016/S0140-6736(99)90326-4 [DOI] [PubMed] [Google Scholar]
- 23. Needham RD, Loë RC. The policy Delphi: purpose, structure, and application. Canadian Geographer 1990;34:133–42. 10.1111/j.1541-0064.1990.tb01258.x [DOI] [Google Scholar]
- 24. Donohoe HM, Needham RD. Moving best practice forward: Delphi characteristics, advantages, potential problems, and solutions. Int. J. Tourism Res. 2009;11:415–37. 10.1002/jtr.709 [DOI] [Google Scholar]
- 25. Alper BS, Price A, van Zuuren EJ, et al. Consistency of recommendations for evaluation and management of hypertension. JAMA Netw Open 2019;2:e1915975. 10.1001/jamanetworkopen.2019.15975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Comet DelphiManager. Available: http://www.comet-initiative.org/delphimanager/ [Accessed 10 Jul 2018].
- 27. Mascarenhas VV, Castro MO, Rego PA, et al. The Lisbon agreement on femoroacetabular impingement Imaging-part 1: overview. Eur Radiol 2020;30:5281–97. 10.1007/s00330-020-06822-9 [DOI] [PubMed] [Google Scholar]
- 28. Mascarenhas VV, Castro MO, Afonso PD. The Lisbon agreement on femoroacetabular impingement imaging—part 2: general issues, parameters, and reporting. Eur Radiol. 10.1007/s00330-020-07432-1 [DOI] [PubMed] [Google Scholar]
- 29. Castro MO, Mascarenhas VV, Afonso PD. The Lisbon agreement on femoroacetabular impingement Imaging—part 3: imaging techniques. Eur Radiol 2021. 10.1007/s00330-020-07501-5 [DOI] [PubMed] [Google Scholar]
- 30. Guyatt GH, Oxman AD, Kunz R, et al. Grade guidelines: 2. framing the question and deciding on important outcomes. J Clin Epidemiol 2011;64:395–400. 10.1016/j.jclinepi.2010.09.012 [DOI] [PubMed] [Google Scholar]
- 31. Woudenberg F. An evaluation of Delphi. Technol Forecast Soc Change 1991;40:131–50. 10.1016/0040-1625(91)90002-W [DOI] [Google Scholar]
- 32. Avery K, Blazeby J, Wilson N, et al. Development of reporting guidance and core outcome sets for seamless, standardised evaluation of innovative surgical procedures and devices: a study protocol for content generation and a Delphi consensus process (cohesive study). BMJ Open 2019;9:e029574. 10.1136/bmjopen-2019-029574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Ma C, Panaccione R, Fedorak RN, et al. Development of a core outcome set for clinical trials in inflammatory bowel disease: study protocol for a systematic review of the literature and identification of a core outcome set using a Delphi survey. BMJ Open 2017;7:e016146. 10.1136/bmjopen-2017-016146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Van de Ven AH, Delbecq AL. Nominal versus interacting group processes for Committee decision-making effectiveness. Acad Manage J 1971;14:203–12. 10.2307/255307 [DOI] [Google Scholar]
- 35. Delbecq AL, Van de Ven AH. A group process model for problem identification and program planning. J Appl Behav Sci 1971;7:466–92. 10.1177/002188637100700404 [DOI] [Google Scholar]
- 36. Belton I, MacDonald A, Wright G, et al. Improving the practical application of the Delphi method in group-based judgment: a six-step prescription for a well-founded and defensible process. Technol Forecast Soc Change 2019;147:72–82. 10.1016/j.techfore.2019.07.002 [DOI] [Google Scholar]
- 37. von der Gracht HA. Consensus measurement in Delphi studies: review and implications for future quality assurance. Technol Forecast Soc Change 2012;79:1525–36. 10.1016/j.techfore.2012.04.013 [DOI] [Google Scholar]
- 38. Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull 1979;86:420–8. 10.1037//0033-2909.86.2.420 [DOI] [PubMed] [Google Scholar]
- 39. Trevelyan EG, Robinson PN. Delphi methodology in health research: how to do it? Eur J Integr Med 2015;7:423–8. 10.1016/j.eujim.2015.07.002 [DOI] [Google Scholar]
- 40. Koo TK, Li MY,. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 2016;15:155–63. 10.1016/j.jcm.2016.02.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Beiderbeck D, Frevel N, von der Gracht HA, et al. Preparing, conducting, and analyzing Delphi surveys: Cross-disciplinary practices, new directions, and advancements. MethodsX 2021;8:101401. 10.1016/j.mex.2021.101401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Beiderbeck D, Frevel N, von der Gracht HA, et al. The impact of COVID-19 on the European football ecosystem – a Delphi-based scenario analysis. Technol Forecast Soc Change 2021;165:120577. 10.1016/j.techfore.2021.120577 [DOI] [Google Scholar]
- 43. Wasserstein RL, Schirm AL, Lazar NA. Moving to a World Beyond “p. Am Stat 2019;73:1–19. [Google Scholar]
- 44. Ritchie J, Lewis J. Analysis: Principles and Processes. In: Qualitative research practice: a guide for social science students and researchers. London: SAGE, 2014: 269–93. [Google Scholar]
- 45. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77–101. 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- 46. Ziebland S, McPherson A. Making sense of qualitative data analysis: an introduction with illustrations from DIPEx (personal experiences of health and illness). Med Educ 2006;40:405–14. 10.1111/j.1365-2929.2006.02467.x [DOI] [PubMed] [Google Scholar]
- 47. van Klij P, Reiman MP, Waarsing JH, et al. Classifying Cam Morphology by the Alpha Angle: A Systematic Review on Threshold Values. Orthop J Sports Med 2020;8:2325967120938312. 10.1177/2325967120938312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Australian Academy of Science . Getting ahead of the game: athlete data in professional sport, 2022. Available: https://www.science.org.au/supporting-science/science-policy-and-analysis/reports-and-publications/getting-ahead-of-the-game-athlete-data-in-professional-sport [Accessed 11 Jun 2022].
- 49. Ioannidis JPA, Greenland S, Hlatky MA, et al. Increasing value and reducing waste in research design, conduct, and analysis. Lancet 2014;383:166–75. 10.1016/S0140-6736(13)62227-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Macleod MR, Michie S, Roberts I, et al. Biomedical research: increasing value, reducing waste. The Lancet 2014;383:101–4. 10.1016/S0140-6736(13)62329-6 [DOI] [PubMed] [Google Scholar]
- 51. Rowe G, Frewer LJ. A typology of public engagement mechanisms. Sci Technol Human Values 2005;30:251–90. 10.1177/0162243904271724 [DOI] [Google Scholar]
- 52. Johnson K, Walmsley J. Inclusive research with people with learning disabilities: past, present and futures. London, UNITED KINGDOM: Jessica Kingsley Publishers, 2003. http://ebookcentral.proquest.com/lib/oxford/detail.action?docID=290818 [Google Scholar]
- 53. Frankena TK, Naaldenberg J, Cardol M, et al. A consensus statement on how to conduct inclusive health research. J Intellect Disabil Res 2019;63:1–11. 10.1111/jir.12486 [DOI] [PubMed] [Google Scholar]
- 54. Robinson KA, Brunnhuber K, Ciliska D. What evidence-based research is and why is it important? J Clin Epidemiol 2020. 10.1016/j.jclinepi.2020.07.020 [DOI] [PubMed] [Google Scholar]
- 55. Lund H, Juhl CB, Nørgaard B. Using an evidence-based research approach before a new study is conducted to ensure value. J Clin Epidemiol 2020. 10.1016/j.jclinepi.2020.07.019 [DOI] [PubMed] [Google Scholar]
- 56. Lund H, Juhl CB, Nørgaard B. Using an evidence-based research approach to place your results into context after the study is performed to ensure usefulness of the conclusion. J Clin Epidemiol 2020. 10.1016/j.jclinepi.2020.07.021 [DOI] [PubMed] [Google Scholar]
- 57. Loo R. The Delphi method: a powerful tool for strategic management. Polic Int J Police Strateg Manag 2002;25:762–9. 10.1108/13639510210450677 [DOI] [Google Scholar]
- 58. Mullen PM. Delphi: myths and reality. J Health Organ Manag 2003;17:37–52. 10.1108/14777260310469319 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bjsports-2022-106085supp001.pdf (754.2KB, pdf)
bjsports-2022-106085supp002.pdf (154.2KB, pdf)
bjsports-2022-106085supp003.pdf (1.9MB, pdf)
bjsports-2022-106085supp004.pdf (12.8MB, pdf)
bjsports-2022-106085supp005.pdf (1.8MB, pdf)
bjsports-2022-106085supp008.pdf (930.3KB, pdf)
bjsports-2022-106085supp006.pdf (226.2KB, pdf)
bjsports-2022-106085supp007.pdf (1.6MB, pdf)