Abstract
Objective
Epidemiological studies on the prevalence and associated factors of cardiovascular diseases (CVDs) representative of all states of India among middle-aged and elderly are not much reported. The present study estimates the prevalence and associated factors of cardiovascular diseases across Indian states among men and women aged ≥45 years.
Methods
We used data from the Longitudinal Ageing Study in India wave 1 (2017–2019), which included a final analytical sample size of 56,935 adults and their spouses aged 45 years and above. We estimated CVDs prevalence for sociodemographic and behavioural variables, and multivariable logistic regression was used to assess the association between behavioural factors and CVDs in both men and women.
Results
The prevalence of CVDs was 5.2% among adults ≥45 years (women: 4.6%; men: 5.9%), hypertension was 46.7% (women:48.9%; men:44%). Men and women have a similar prevalence of diabetes (11.9%) and cholesterol (2.3%). Prevalence of physical inactivity was 30.3% (women:27%; men:34.1%). Hypertension (adjusted odds ratio; aOR women:2.60, 95% CI: 2.08–3.25, men:1.88, 95% CI 1.54–2.29), hypercholesterolemia (aOR women:1.70; 95% CI 1.07–2.69, men 3.55; 95% CI 2.66–4.74), diabetes (aOR women:2.53; 95% CI 1.83–3.51, men:1.77 95% CI 1.44–2.17), obesity, physical inactivity, and smoking in men were significantly associated with CVDs.
Conclusion
The prevalence of CVDs and lifestyle risk factors among middle-aged and elderly poses severe concerns regarding noncommunicable disease (NCD) healthcare services provided in a lower-middle-income country like India. The key to preventing CVDs is controlling hypertension, diabetes, hypercholesterolemia, and increasing physical activity among adults aged ≥45 years.
Keywords: Prevalence, Risk factors, Cardiovascular disease, LASI, Hypertension, Diabetes
1. Introduction
Cardiovascular diseases (CVDs), mainly coronary heart disease and stroke, are the primary causes of disability and mortality worldwide in males and females aged 45 years and older.1,2 India contributes the most to the global burden of cardiovascular disease after China, with 71.13 million cases and 27% of total deaths according to the Global Disease Burden Study in 2019.3,4 In comparison to other races, South Asians, including people in India, have a higher incidence, more severe symptoms, and a younger onset of disease.5 The increasing trend in cardiovascular diseases is attributable to several lifestyle and metabolic factors such as physical inactivity, tobacco use, unhealthy diet, harmful alcohol use, hypertension, hyperglycemia, obesity, and dyslipidemia.6,7
According to the million-death study, nearly 42% of CVDs deaths in men and women happen in the age group 30–69, compared to 32.5% among 70 years or older.8 The higher CVDs prevalence and mortality in both middle and older adults may present a significant burden on the healthcare system.8,9 These CVDs cause a high prevalence of heart failure, arrhythmias, and other heart diseases due to functional, structural, cellular, and molecular changes in later life.10 A deeper understanding of the causes of CVDs in older adults is needed, given India's rapidly increasing elderly population.
CVDs and their risk factors vary by gender, income, and racial group and are significant causes of health inequality.11 Most studies on the prevalence of CVDs and its risk factors in India were not representative of the entire country,12 while a few available studies have focused on the high-risk population of men and women aged 45 years and older. Understanding the key preventable and modifiable risk factors of CVDs at the population level will enable clinicians and public health researchers to design and implement effective interventions to ensure healthy and productive ageing. Therefore this study aimed to understand the prevalence and the associated factors of CVDs among men and women aged 45 years and older in India using nationally representative data.
2. Methods
2.1. Data and participants
This study utilized data from the Longitudinal Ageing Survey of India (LASI) wave 1 (2017–2019) survey implemented by the International Institute of Population Sciences, India. This is a nationally representative survey across India's states and union territories. The details of the survey have been published widely before.13 Briefly, this was a multistage cluster sample survey to collect data from 72,262 non-institutional residents, 45 years and older. Data on social, economic, and medical conditions, such as heart diseases, were obtained. Our final analytical sample size for this study was 56,935 individuals after excluding survey respondents with missing values for biomarkers. This included 30,584 (54.2%) women and 26,351 (45.8%) men.
2.2. Outcome variable
Self-reported medical history of CVDs (heart attack, congestive heart failure, cardiac arrhythmias, and stroke) in men and women aged 45 years and older. The responses were coded as a dichotomous variable (no – 0, no CVDs, yes – 1, presence of CVDs).
2.3. Independent variables
2.3.1. Sociodemographic variables
The sociodemographic variables used in this study are age group (45–59 years and ≥60 years), sex (male/female), residence location (rural or urban), educational attainment (less than ten years of schooling or more than or equal to ten years of schooling) and caste (categorised as scheduled caste (SC) or scheduled tribe (ST), other backward classes (OBC), and forward castes). Respondents were classified as poorest, poor, middle, rich, and richest based on the Monthly Per Capita Consumption Expenditure (MPCE).13 States and union territories were categorised into six regions (North, Central, East, Northeast, West, and South).
2.4. Behavioural variables
We used respondents' self-reported data on hypercholesterolemia and diabetes mellitus. Hypertension prevalence was calculated using both self-reported and measured data. Respondents were considered to have a positive family history of CVDs if their mother, father, brother, or sister has a history of heart disease or stroke. Smoking and alcohol variables were grouped into ever-users and never-users. The participants in this study were categorised as physically active if they engaged in moderate or vigorous physical activities more than once a week or physically inactive if they did so only once a week or less. Respondents were classified into four categories basing on their body mass index (BMI) values; underweight (<18.5 kg/m2), normal BMI (18.5–24.9 kg/m2), overweight (25–29.9 kg/m2), and obese (≥30 kg/m2). BMI is calculated as weight in kg/(height in metre2). Sleep health has been added as the eighth component of the American Heart Association's definition of cardiovascular health, making it one of the vital components needed to prevent CVDs.14 We used the inability to fall asleep as one of the proxy measures of sleep health, which we defined as an inability to fall asleep more than or equal to three nights a week.
2.5. Statistical analysis
A frequency and percentage distribution table were constructed for all the study variables according to men, women, and the total sample. The prevalence of CVDs was stratified across sociodemographic and lifestyle factors. We used Pearson chi-squared test to test for statistically significant differences in CVDs prevalence between groups. The adjusted odds ratios (aOR) were estimated by employing the multivariable logistic regression model with the following variables in the model: age group, sex, rural/urban, education, MPCE quintile, caste, state-region, hypertension, high cholesterol, diabetes, physical inactivity, BMI, sleep, family history of CVDs, smoke and alcohol use. We have presented the aORs and their corresponding 95% Confidence Intervals (CIs) graphically for men, women and the total sample. Survey weights provided in the dataset were applied during the data analysis to obtain accurate estimates. The level of statistical significance was set at p < 0.05, and two-tailed test values were presented. We used the Stata MP statistical software version 16 (StataCorp, TX, USA) for all statistical analyses.
2.6. Ethical clearance
All the participants provided informed consent at the time of data collection.
3. Results
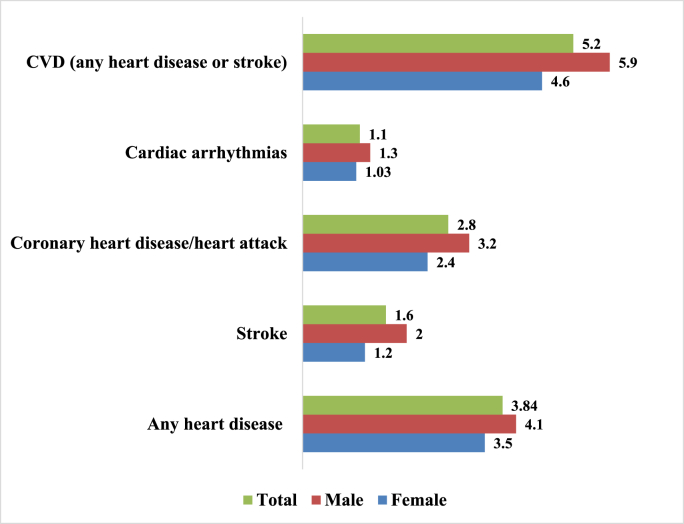
The prevalence of hypertension was 46.7% (women:48.9%; men:44.0%), physical inactivity was 30.3% (women:27%; men:34.1%) smoking was 17.2% (women:3.6%; men 33.3%), and obesity was 6.8% (women:9.6%; men 3.4%). Poor sleep was reported by 39.3% (women:44.2%; men 33.6%). Men and women had a similar prevalence of diabetes (11.9%) and high cholesterol levels (2.3%) (Table 1). The overall prevalence of cardiovascular disease was 5.2% (women: 4.6%; men: 5.9%), coronary heart disease/heart attacks was 2.8% (women: 2.4%; men: 3.2%), and stroke was 1.6% (women: 1.2%; men: 2.0%) (Fig. 1).
Table 1.
Distribution of variables by women and men aged ≥45 years, LASI (2017–2019).
| Women |
Men |
Total |
||||
|---|---|---|---|---|---|---|
| % | n | % | n | % | n | |
| Total | 54.2 | 30,584 | 45.8 | 26,351 | 100.0 | 56,935 |
| Hypertension | ||||||
| Yes | 48.9 | 15,420 | 44.0 | 12,433 | 46.7 | 27,853 |
| Family History of CVDs | ||||||
| Yes | 10.9 | 3212 | 11.8 | 2820 | 11.3 | 6032 |
| Physically active | ||||||
| No | 27.0 | 8448 | 34.1 | 9516 | 30.3 | 17,964 |
| Diabetes Mellitus | ||||||
| Yes | 11.9 | 3780 | 11.9 | 3414 | 11.9 | 7194 |
| High cholesterol | ||||||
| Yes | 2.3 | 1157 | 2.3 | 841 | 2.3 | 1998 |
| Smoke | ||||||
| Ever User | 3.6 | 1403 | 33.3 | 9083 | 17.2 | 10,486 |
| Alcohol | ||||||
| Ever user | 2.7 | 1292 | 30.4 | 9174 | 15.4 | 10,466 |
| Body Mass Index | ||||||
| Underweight | 20.4 | 5517 | 22.7 | 5112 | 21.5 | 10,629 |
| Normal | 47.8 | 14,825 | 56.0 | 15,007 | 51.5 | 29,832 |
| Overweight | 22.2 | 7125 | 17.9 | 5156 | 20.2 | 12,281 |
| Obesity | 9.6 | 3117 | 3.4 | 1076 | 6.8 | 4193 |
| Sleep problem | ||||||
| Yes | 44.2 | 13,508 | 33.6 | 8869 | 39.3 | 22,377 |
| Age-Group (in years) | ||||||
| 45–59 | 51.6 | 16,563 | 48.3 | 13,295 | 50.1 | 29,858 |
| ≥60 | 48.4 | 14,021 | 51.7 | 13,056 | 49.9 | 27,077 |
| Residence | ||||||
| Rural | 69.0 | 20,004 | 71.4 | 17,555 | 70.1 | 37,559 |
| Urban | 31.0 | 10,580 | 28.6 | 8796 | 29.9 | 19,376 |
| MPCE Quintile | ||||||
| Poorest | 21.4 | 6146 | 21.0 | 5229 | 21.2 | 11,375 |
| Poorer | 21.1 | 6188 | 21.4 | 5308 | 21.2 | 11,496 |
| Middle | 20.4 | 6191 | 20.2 | 5301 | 20.3 | 11,492 |
| Richer | 19.8 | 6124 | 19.5 | 5363 | 19.6 | 11,487 |
| Richest | 17.4 | 5935 | 17.9 | 5150 | 17.6 | 11,085 |
| Education (in years) | ||||||
| Less than ten | 89.9 | 27,211 | 73.8 | 19,291 | 82.5 | 46,502 |
| Ten or more | 10.1 | 3373 | 26.2 | 7059 | 17.5 | 10,432 |
| Caste | ||||||
| Scheduled castes/tribes | 29.0 | 10,929 | 28.5 | 9336 | 28.8 | 20,265 |
| Other Backward classes | 46.7 | 11,885 | 46.8 | 10,336 | 46.7 | 22,221 |
| Forward castes | 24.3 | 7718 | 24.7 | 6654 | 24.5 | 14,372 |
| State-Region | ||||||
| North | 13.0 | 5754 | 12.5 | 4873 | 12.8 | 10,627 |
| Central | 20.3 | 4158 | 22.8 | 3908 | 21.4 | 8066 |
| East | 22.4 | 5366 | 24.1 | 4844 | 23.2 | 10,210 |
| West | 16.3 | 3994 | 15.2 | 3329 | 15.8 | 7323 |
| Northeast | 2.9 | 3697 | 3.2 | 3395 | 3.1 | 7092 |
| South | 25.1 | 7615 | 22.2 | 6002 | 23.7 | 13,617 |
MPCE: monthly per capita consumption expenditure, CVDs: cardiovascular diseases.
Fig. 1.
Prevalence (%) of cardiovascular diseases (CVDs) in men and women aged 45 years and older, LASI (2017–2019).
The CVDs prevalence was higher among patients with hypertension (women 7.4%; men 8.8%) compared to patients without hypertension (women 1.9%; men 3.5%), and among patients with Diabetes mellitus patients (women 13.6%; men 12.9%) compared to patients without diabetes mellitus (women 3.4%; men 4.9%). Respondents with high cholesterol, males who reported as ever smokers, obese women and men, and physically inactive women and men reported higher CVDs rates compared to others (Table 2).
Table 2.
Prevalence of CVDs in women and men aged ≥45 years, LASI (2017–2019).
| Women CVDs |
Men CVDs |
|||||
|---|---|---|---|---|---|---|
| Hypertension | No | Yes | p-value | No | Yes | p-value |
| No | 98.1 | 1.9 | 96.5 | 3.5 | ||
| Yes | 92.6 | 7.4 | <0.001 | 91.2 | 8.8 | <0.001 |
| Family History of CVDs | ||||||
| No | 95.9 | 4.2 | 94.7 | 5.3 | ||
| Yes | 92.0 | 8.0 | <0.001 | 90.2 | 9.8 | <0.001 |
| Physically active | ||||||
| Yes | 95.9 | 4.1 | 95.3 | 4.7 | ||
| No | 94.1 | 5.9 | 0.014 | 92 | 8 | <0.001 |
| Diabetes Mellitus | ||||||
| No | 96.7 | 3.4 | 95.1 | 4.9 | ||
| Yes | 86.4 | 13.6 | <0.001 | 87.1 | 12.9 | <0.001 |
| High cholesterol | ||||||
| No | 95.6 | 4.4 | 94.6 | 5.4 | ||
| Yes | 86.9 | 13.1 | <0.001 | 74.2 | 25.8 | <0.001 |
| Smoke | ||||||
| Never User | 95.4 | 4.6 | 94.6 | 5.4 | ||
| Ever User | 95.7 | 4.3 | 0.699 | 93.3 | 6.7 | 0.006 |
| Alcohol | ||||||
| Never User | 95.4 | 4.6 | 93.9 | 6.1 | ||
| Ever user | 97.5 | 2.5 | 0.050 | 94.6 | 5.4 | 0.204 |
| Body Mass Index | ||||||
| Underweight | 97.6 | 2.4 | 96.1 | 3.9 | ||
| Normal | 95.7 | 4.3 | 94.2 | 5.8 | ||
| Overweight | 95.6 | 4.4 | 92.6 | 7.4 | <0.001 | |
| Obesity | 89.0 | 11.0 | 0.004 | 88.1 | 11.9 | |
| Sleep problem | ||||||
| No | 96.0 | 4.0 | 95.0 | 5.0 | ||
| Yes | 94.7 | 5.3 | 0.019 | 92.5 | 7.5 | <0.001 |
| Age-Group (in years) | ||||||
| 45–59 | 97.1 | 2.9 | 96.6 | 3.4 | ||
| ≥60 | 93.7 | 6.3 | <0.001 | 91.9 | 8.1 | <0.001 |
| Residence | ||||||
| Rural | 96.3 | 3.7 | 94.9 | 5.1 | ||
| Urban | 93.4 | 6.6 | 0.001 | 92.3 | 7.7 | <0.001 |
| MPCE quintile | ||||||
| Poorest | 96.6 | 3.4 | 96.2 | 3.8 | ||
| Poorer | 96.6 | 3.4 | 94.6 | 5.4 | ||
| Middle | 96.5 | 3.6 | 93.8 | 6.3 | ||
| Richer | 95.7 | 4.3 | 94.1 | 5.9 | ||
| Richest | 91.0 | 9.0 | 0.001 | 91.8 | 8.2 | <0.001 |
| Education (in years) | ||||||
| Less than ten | 95.9 | 4.1 | 94.5 | 5.5 | ||
| Ten or more | 91.4 | 8.7 | 0.045 | 93.2 | 6.8 | 0.038 |
| Caste | ||||||
| Scheduled castes/tribes | 96.3 | 3.7 | 95.4 | 4.6 | ||
| Other backward classes | 95.3 | 4.7 | 94.3 | 5.7 | ||
| Forward castes | 94.6 | 5.4 | 0.199 | 92.4 | 7.6 | <0.001 |
| State-Region | ||||||
| North | 96.3 | 3.7 | 93.1 | 6.9 | ||
| Central | 97.6 | 2.4 | 96.7 | 3.3 | ||
| East | 94.9 | 5.1 | 93.5 | 6.5 | ||
| West | 94.5 | 5.5 | 91.4 | 8.6 | ||
| Northeast | 96.8 | 3.2 | 96.7 | 3.3 | ||
| South | 94.1 | 5.9 | 0.010 | 94.3 | 5.7 | <0.001 |
MPCE: monthly per capita consumption expenditure, CVDs: cardiovascular diseases.
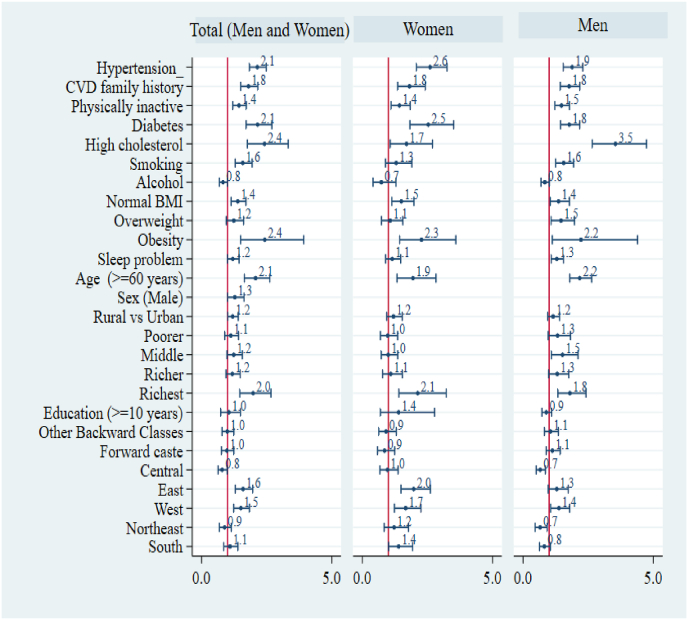
Hypertensives had two times higher odds for CVDs than non-hypertensives (aOR women:2.60, 95% CI: 2.08–3.25, men: 1.88, 95% CI 1.54–2.29). Diabetes mellitus patients (aOR women:2.53; 95% CI 1.83–3.51, men:1.77 95% CI 1.44–2.17) have a higher likelihood of CVDs than non-diabetics. Those respondents who reported hypercholesterolemia (aOR women:1.70; 95% CI 1.07–2.69, men 3.55; 95% CI 2.66–4.74) were more likely to have CVDs than those without that condition. Physically inactive have higher odds for CVDs (aOR women:1.43; 95% CI 1.11–1.84, men 1.47; 95% CI 1.22–1.78) than physically active men and women. Participants who are obese have a higher likelihood of CVDs (aOR women:2.27; 95% CI 1.44–3.59, men 2.22; 95% CI 1.12–4.39) than those in the underweight category. Smoking and sleep disorder variables were significantly associated with CVDs only in men (Fig. 2).
Fig. 2.
Adjusted odds ratios (with 95% CIs) of behavioural and sociodemographic variables associated with cardiovascular disease (CVDs) among men and women aged 45 years and older, LASI (2017–2019).
4. Discussion
This study provides the most recent prevalence estimates of CVDs and their associated factors in Indian men and women aged 45 years and older. Using the nationally representative LASI survey data, we found the following modifiable risk factors for CVDs: hypertension, diabetes mellitus, high cholesterol, obesity, and physical inactivity.
The overall CVDs prevalence is 5.4%, with men (6.2%) reporting a higher rate than women (4.8%). The national noncommunicable disease monitoring survey (NNMS) 2017–2018 reported a slightly lower proportion of CVDs in men (3.6%) and women (3.5%) in individuals aged 30–69 years compared to our results.15 The difference could be due to the variations in the age groups in the LASI survey (≥45 years) and NNMS Survey (30–69 years). A systematic review for the period 1969–2012 had shown that the prevalence of coronary heart disease in India ranged from 1.4% to 12.6% (rural: 1.4%–4.5% and urban 2.5%–12.6%).12 The Indian human development survey 2011–2012 reported a 1.1% prevalence of coronary heart in adults ≥15 years.16 The study on the global ageing survey (SAGE), 2007–2010, reported a 2% prevalence of stroke among older adults 50 years and above, similar to our study result.17
Our study findings agree with existing literature6,7,17 that hypertension is the main risk factor for CVDs in India. In this study, nearly 50% of individuals aged 45 years and older have hypertension. A study by Kiran et al4 has shown that the mean systolic blood pressure (mmHg) increased by one mmHg in women (123.3–124.3) and by two mmHg in men (125.5–127.3) between 2000 and 2016. Other studies have shown poor awareness, treatment and control rates among hypertensives, for example, the study by Mohanty et al18 in 2021 reported that among those with hypertension aged 45 years and older, 54.4% were aware of their medical condition, 50.8% were taking antihypertensive drugs, and only 28.8% had their blood pressure under control. This demonstrates that a significant proportion of older persons do not receive prompt treatment, which makes CVDs prevention challenging.
We also found that hypercholesterolemia is a major associated risk factor for CVDs. Previous studies have shown that high total cholesterol significantly contributed to disability-adjusted life years of CVDs.19 Similarly, diabetes mellitus, the prevalence of which increased significantly in the last two decades in both men and women,4 were also found to be significantly associated with CVDs in our analysis. Further, the national noncommunicable disease monitoring survey data (2017–2018) found that only 45.8% of diabetes patients were aware of the disease, 36.1% were on treatment, and only 15.7% of them had sugar levels under control.20 This signifies the importance of having a good noncommunicable disease control program with adequate components for diabetes and CVDs as the latter is the main cause of morbidity and mortality in type 2 diabetes mellitus patients.7
Obesity is a significant modifiable risk factor for CVDs in both men and women.21 According to four waves of national family health surveys conducted between 1998 and 2016, in both urban and rural areas, the prevalence of overweight and obesity has increased among both men and women.22 Our study also reiterated that physically inactive individuals were more likely to have CVDs than physically active, and our analysis found that nearly 30% of the Indian population is physically inactive. Furthermore, individuals in India seem to draw most of their physical activity from their occupations.23 Leisure-time physical activity is essential and has been shown to have a negative linear association with the risk of cardiovascular mortality regardless of age, gender, and cardiovascular disease presence.24
Smoking is associated with CVDs only in men in our study. According to a longitudinal study conducted in Iran, smoking is a more significant risk factor for CVDs in men than women.25 Also, men predominantly smoke in India more than women.26 Despite the rise in co-morbid cardiovascular disease risk factors in low- and middle-income nations, such as hyperlipidemia and hypertension, tobacco control is likely to continue to be a highly effective method of lowering cardiovascular deaths.27 Sleep problem was significantly associated with CVDs in men in our data. A cohort study of Taiwanese citizens from 1996 to 2014 found that short sleep duration and poor sleep quality were both independently linked to an increased risk of heart disease.28
Many cardiovascular diseases can be averted by addressing behavioural factors such as tobacco consumption, unhealthy diet, overweight/obesity, physical inactivity, and harmful use of alcohol.29 In a study in an urban area, NCDs were found triggered by unhealthy eating habits, high salt intake, inadequate fruit and vegetable intake, and increased waist circumference.30 India's ageing population, driven by multimorbidity, means a costly and complex burden of illness. Another critical factor to consider is that most health programs in India take a vertical, disease-specific approach rather than addressing individual health as a whole.31
India needs to increase its focus on limiting risk factors and preventing them from developing into CVDs, both through primary and secondary prevention. Primordial prevention measures include addressing social determinants, public health financing, population policies for smoking cessation, and promoting a healthy diet and physical activity, and these measures provide the most significant benefit in terms of CVDs reduction. Primary prevention techniques that are implemented in clinics that focus on cholesterol, blood pressure, and diabetes management are crucial. Reducing CVDs mortality also involves managing chronic CVDs with secondary and tertiary preventive strategies and treating acute CVDs events.32,33
Our study has a few limitations. CVDs and many of the predictors were self-reported in the survey. This might have resulted in recall bias and affected the validity of the results. The cross-sectional nature of data limits the interpretation of an association between explanatory and outcome variables.
5. Conclusion
This study provides national-level estimates of CVDs and the risk factors among a high-risk age group of ≥45 years old men and women using a large nationally representative survey. The study shows that, with the narrowing sex and urban-rural differences in the prevalence of CVDs and their risk factors, there is a need to strengthen the National Program for Prevention and Control of Cancer, Diabetes, Cardio-vascular diseases, and Stroke in the rural areas and giving equal importance to women in CVDs services and care. Such programs should provide preventive and counselling services to improve physical activity, smoking cessation, and essential drugs to control hypertension, diabetes mellitus and cholesterol.
Funding
The authors received no financial support for the research, authorship and/or publication of this article.
Author contributions
NVK and LDB have full access to all the data in the study and take responsibility for the integrity and accuracy of the data analysis. Concept and design: NVK, LDB, and SFK. Acquisition of data: NVK, NEP and LDB. Acquisition, analysis, or interpretation of data: NVK, NEP, LDB, and SFK. Drafting of the manuscript: NVK and NEP. Critical revision of the manuscript for important intellectual content: LDB, NEP and SFK. Statistical analysis: NVK, LDB and SFK. Administrative, technical, or material support: LDB. Supervision: LDB and SFK.
Declaration of competing interest
The authors declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
Acknowledgements
We have acquired the data for this study from the Gateway to Global Aging Data website (https://g2aging.org/) available for researchers on request and we thank the Program on Global Aging, Health, and Policy, University of Southern California, Dornsife Center for Economic and Social Research, for providing access to this data.
References
- 1.Roth G.A., Mensah G.A., Johnson C.O., et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J Am Coll Cardiol. 2020;76(25):2982–3021. doi: 10.1016/j.jacc.2020.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zou Z., Cini K., Dong B., et al. Time trends in cardiovascular disease mortality across the BRICS. Circulation. 2020;141(10):790–799. doi: 10.1161/CIRCULATIONAHA.119.042864. [DOI] [PubMed] [Google Scholar]
- 3.Gbd Results. Institute for health metrics and evaluation. https://vizhub.healthdata.org/gbd-results.Accessed 7 June, 2022.
- 4.Kiran G., Mohan I., Kaur M., Ahuja S., Gupta S., Gupta R. Escalating ischemic heart disease burden among women in India: insights from GBD, NCDRisC and NFHS reports. Am J Prev Cardiol. 2020;2 doi: 10.1016/j.ajpc.2020.100035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Volgman A.S., Palaniappan L.S., Aggarwal N.T., et al. Atherosclerotic cardiovascular disease in South Asians in the United States: epidemiology, risk factors, and treatments: a scientific statement from the American heart association. Circulation. 2018;138(1):e1–e34. doi: 10.1161/CIR.0000000000000580. [DOI] [PubMed] [Google Scholar]
- 6.Yusuf S., Joseph P., Rangarajan S., et al. Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (PURE): a prospective cohort study. Lancet. 2020;395(10226):795–808. doi: 10.1016/S0140-6736(19)32008-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.O'Donnell M.J., Chin S.L., Rangarajan S., et al. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): a case-control study. Lancet. 2016;388(10046):761–775. doi: 10.1016/S0140-6736(16)30506-2. [DOI] [PubMed] [Google Scholar]
- 8.Gomes M., Begum R., Sati P., et al. Nationwide mortality studies to quantify causes of death: relevant lessons from India's million death study. Health Aff. 2017;36(11):1887–1895. doi: 10.1377/hlthaff.2017.0635. [DOI] [PubMed] [Google Scholar]
- 9.Yazdanyar A., Newman A.B. The burden of cardiovascular disease in the elderly: morbidity, mortality, and costs. Clin Geriatr Med. 2009;25(4):563–577. doi: 10.1016/j.cger.2009.07.007. [vii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Steenman M., Lande G. Cardiac aging and heart disease in humans. Biophys Rev. 2017;9(2):131–137. doi: 10.1007/s12551-017-0255-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kanchi R., Perlman S.E., Chernov C., et al. Gender and race disparities in cardiovascular disease risk factors among New York city adults: New York city health and nutrition examination survey (NYC HANES) 2013–2014. J Urban Health Bull N Y Acad Med. 2018;95(6):801–812. doi: 10.1007/s11524-018-0287-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rao M., Xavier D., Devi P., et al. Prevalence, treatments and outcomes of coronary artery disease in Indians: a systematic review. Indian Heart J. 2015;67(4):302–310. doi: 10.1016/j.ihj.2015.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.International Institute for Population Sciences (IIPS) National programme for health care elderly (NPHCE), MoHFW, harvard T. H. Chan school of public health (HSPH), the university of southern California (USC). Longitudinal ageing Study in India (LASI) wave 1, 2017-18, India report. IIPS. 2020:23–48. https://www.iipsindia.ac.in/content/lasi-publications Accessed. [Google Scholar]
- 14.Lloyd-Jones D.M., Allen N.B., Anderson C.A.M., et al. Life's essential 8: updating and enhancing the American heart association's construct of cardiovascular health: a presidential advisory from the American heart association. Circulation. 2022;146(5):e18–e43. doi: 10.1161/CIR.0000000000001078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National Centre for Disease Informatics and Research, Bengaluru . 2020. NATIONAL NONCOMMUNICABLE DISEASE MONITORING SURVEY (NNMS) 2017-18.https://www.ncdirindia.org/nnms/resources/Initial_Content.pdf Accessed. [Google Scholar]
- 16.Biswas A., Singh S.K., Singh R.K. Linkages between hypertension and coronary heart disease in India: evidence from India human development survey-2 (2011–2012) Indian J Community Med. 2017;42(4):200. doi: 10.4103/ijcm.IJCM_168_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ruan Y., Guo Y., Zheng Y., et al. Cardiovascular disease (CVD) and associated risk factors among older adults in six low-and middle-income countries: results from SAGE Wave 1. BMC Publ Health. 2018;18(1):778. doi: 10.1186/s12889-018-5653-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mohanty S.K., Pedgaonkar S.P., Upadhyay A.K., et al. Awareness, treatment, and control of hypertension in adults aged 45 years and over and their spouses in India: a nationally representative cross-sectional study. PLoS Med. 2021;18(8) doi: 10.1371/journal.pmed.1003740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Prabhakaran D., Jeemon P., Sharma M., et al. The changing patterns of cardiovascular diseases and their risk factors in the states of India: the Global Burden of Disease Study 1990–2016. Lancet Global Health. 2018;6(12):e1339–e1351. doi: 10.1016/S2214-109X(18)30407-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mathur P., Leburu S., Kulothungan V. Prevalence, awareness, treatment and control of diabetes in India from the countrywide national NCD monitoring survey. Front Public Health. 2022;10 doi: 10.3389/fpubh.2022.748157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Riaz H., Khan M.S., Siddiqi T.J., et al. Association between obesity and cardiovascular outcomes: a systematic review and meta-analysis of mendelian randomization studies. JAMA Netw Open. 2018;1(7) doi: 10.1001/jamanetworkopen.2018.3788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Luhar S., Mallinson P.A.C., Clarke L., Kinra S. Trends in the socioeconomic patterning of overweight/obesity in India: a repeated cross-sectional study using nationally representative data. BMJ Open. 2018;8(10) doi: 10.1136/bmjopen-2018-023935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Anjana R.M., Pradeepa R., Das A.K., et al. Physical activity and inactivity patterns in India - results from the ICMR-INDIAB study (Phase-1) [ICMR-INDIAB-5] Int J Behav Nutr Phys Activ. 2014;11(1):26. doi: 10.1186/1479-5868-11-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cheng W., Zhang Z., Cheng W., Yang C., Diao L., Liu W. Associations of leisure-time physical activity with cardiovascular mortality: a systematic review and meta-analysis of 44 prospective cohort studies. Eur J Prev Cardiol. 2018;25(17):1864–1872. doi: 10.1177/2047487318795194. [DOI] [PubMed] [Google Scholar]
- 25.Amiri P., Mohammadzadeh-Naziri K., Abbasi B., et al. Smoking habits and incidence of cardiovascular diseases in men and women: findings of a 12 year follow up among an urban Eastern-Mediterranean population. BMC Publ Health. 2019;19:1042. doi: 10.1186/s12889-019-7390-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chhabra A., Hussain S., Rashid S. Recent trends of tobacco use in India. J Public Health. 2021;29(1):27–36. [Google Scholar]
- 27.Basu S., Glantz S., Bitton A., Millett C. The effect of tobacco control measures during a period of rising cardiovascular disease risk in India: a mathematical model of myocardial infarction and stroke. PLoS Med. 2013;10(7) doi: 10.1371/journal.pmed.1001480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yang X., Chen H., Li S., Pan L., Jia C. Association of sleep duration with the morbidity and mortality of coronary artery disease: a meta-analysis of prospective studies. Heart Lung Circ. 2015;24(12):1180–1190. doi: 10.1016/j.hlc.2015.08.005. [DOI] [PubMed] [Google Scholar]
- 29.Who. Cardiovascular diseases (CVDs). https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds). Accessed 22 August, 2022.
- 30.Selvaraj K., Kar S.S., Ramaswamy G., Premarajan K.C., Saya G.K., Kalidoss V. Clustering of cardiovascular disease risk factors – syndemic approach: is sit a time to shift toward integrated noncommunicable disease clinic? Indian J Publ Health. 2019;63(3):186. doi: 10.4103/ijph.IJPH_158_18. [DOI] [PubMed] [Google Scholar]
- 31.Sahoo H., Govil D., James K.S., Prasad R.D. Health issues, health care utilization and health care expenditure among elderly in India: thematic review of literature. Aging Health Res. 2021;1(2) [Google Scholar]
- 32.Gupta R., Guptha S., Joshi R., Xavier D. Translating evidence into policy for cardiovascular disease control in India. Health Res Pol Syst. 2011;9(1):1–12. doi: 10.1186/1478-4505-9-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Abdul-Aziz A.A., Desikan P., Prabhakaran D., Schroeder L.F. Tackling the burden of cardiovascular diseases in India. Circ Cardiovasc Qual Outcomes. 2019;12(4) doi: 10.1161/CIRCOUTCOMES.118.005195. [DOI] [PubMed] [Google Scholar]