Abstract
Background
Young adults (YAs) experience higher uninsurance rates and more advanced stage at cancer diagnosis than older counterparts. We examined the association of the Affordable Care Act Medicaid expansion with insurance coverage and stage at diagnosis among YAs newly diagnosed with cancer.
Methods
Using the National Cancer Database, we identified 309 413 YAs aged 18-39 years who received a first cancer diagnosis in 2011-2016. Outcomes included percentages of YAs without health insurance at diagnosis, with stage I (early-stage) diagnoses, and with stage IV (advanced-stage) diagnoses. We conducted difference-in-difference (DD) analyses to examine outcomes before and after states implemented Medicaid expansion compared with nonexpansion states. All statistical tests were 2-sided.
Results
The percentage of uninsured YAs decreased more in expansion than nonexpansion states (adjusted DD = −1.0 percentage points [ppt], 95% confidence interval [CI] = −1.4 to −0.7 ppt, P < .001). The overall percentage of stage I diagnoses increased (adjusted DD = 1.4 ppt, 95% CI = 0.6 to 2.2 ppt, P < .001) in expansion compared with nonexpansion states, with greater improvement among YAs in rural areas (adjusted DD = 7.2 ppt, 95% CI = 0.2 to 14.3 ppt, P = .045) than metropolitan areas (adjusted DD = 1.3 ppt, 95% CI = 0.4 to 2.2 ppt, P = .004) and among non-Hispanic Black patients (adjusted DD = 2.2 ppt, 95% CI = −0.03 to 4.4 ppt, P = .05) than non-Hispanic White patients (adjusted DD = 1.4 ppt, 95% CI = 0.4 to 2.3 ppt, P = .008). Despite the non-statistically significant change in stage IV diagnoses overall, the percentage declined more (adjusted DD = −1.2 ppt, 95% CI = −2.2 to −0.2 ppt, P = .02) among melanoma patients in expansion relative to nonexpansion states.
Conclusions
We provide the first evidence, to our knowledge, on the association of Medicaid expansion with shifts to early-stage cancer at diagnosis and a narrowing of rural-urban and Black-White disparities in YA cancer patients.
Cancer is the leading disease causing death among young adults (YAs) in the United States (1). An estimated 83 700 YAs aged 20-39 years were diagnosed with cancer in the United States in 2020 (2). Compared with other age groups, YAs often experience higher uninsurance rates and present with more advanced stage of cancer at diagnosis (3,4). Among YA patients with cancer, those uninsured or underinsured, who are disproportionately concentrated in racial or ethnic minority YAs often present with advanced-stage disease and have inferior survival outcomes (5-7). Expanding health insurance coverage may improve access to care for timely detection, diagnosis, and treatment of cancer.
The Affordable Care Act (ACA) contains multiple provisions to enhance health insurance coverage for YA populations. Notably, the 2010 Dependent Coverage Expansion extended coverage up to age 26 years in all states, and Medicaid expansion encouraged states to expand Medicaid coverage to all low-income adults (8), including the entire age spectrum of YAs as defined by the National Cancer Institute (9). As of March 2021, 39 states (including Washington, DC) had opted to expand Medicaid through the ACA (10).
A growing body of research has shown insurance coverage gains associated with the ACA Medicaid expansion in patients aged younger than 65 years (11–17). However, findings of the few studies examining the downstream effect of Medicaid expansion on cancer stage at diagnosis or cancer survival in nonelderly patients are mixed (11–17). For example, whereas 2 analyses reported an increase in early-stage diagnoses in the first year post ACA (13,16), a more recent study found no change in breast cancer presentation in the 2-year period following ACA implementation (18). The short post ACA time used in many studies may explain, at least in part, the mixed findings because the health impact of policy changes may require longer time to manifest.
Notably, no studies to our knowledge have assessed the association of Medicaid expansion specifically among YAs with cancer, a group not age-eligible for application of most screening guidelines that affect early stage at presentation (ie, breast, colorectal, or lung cancer screening) (19). Insurance coverage for access to timely physical examination and diagnostic testing is essential to promptly recognize symptoms and identify cancer at an early stage for YAs. Although several studies focusing on nonelderly patients showed a narrowing of sociodemographic disparities in insurance coverage in states that expanded Medicaid (13,17,20), there have not been YA age group–specific analyses. The impact of Medicaid expansion on gaps in YAs' insurance coverage and cancer stage is poorly understood. Historically, this age group experienced disparities in health insurance coverage by race or ethnicity and rurality (21,22).
To fill these knowledge gaps, we used national data before and after the ACA to examine the association of Medicaid expansion with changes in insurance coverage and disease stage at initial diagnosis among YAs newly diagnosed with cancer, overall and by sociodemographic factors.
Methods
Data Source and Study Sample
We analyzed the 2011-2016 data from the National Cancer Database (NCDB), a hospital-based cancer registry cosponsored by the American College of Surgeons Commission on Cancer and the American Cancer Society (23). The NCDB provides sociodemographic, diagnosis, and treatment information for newly diagnosed cancer patients across the United States and accounts for over 70% of all incident cancer patients in the country (23). The use of the NCDB for this study was deemed exempt by the institutional review board of the Morehouse School of Medicine in Atlanta, Georgia.
We identified all male or female YA patients aged 18-39 years who were newly diagnosed with a first primary cancer between January 1, 2011, and December 31, 2016, in the United States. Patients with incomplete information on diagnosis date necessary to determine pre- or postexpansion status or with noninvasive (stage 0) cancers were excluded. These criteria yielded 309 413 patients for the analysis of health insurance coverage. For the analysis of stage at diagnosis, we restricted to 245 135 patients following additional exclusion of 1) 40 643 patients diagnosed with cancers without an applicable American Joint Committee Classification (AJCC) staging scheme (24) (eg, brain tumor, leukemia) and 2) 23 635 patients with testis cancer due to high percentages (12%-30% after 2014) of unknown stage observed exclusively among testis cancer patients. Notably, patients with unknown stage (5%) of all other cancers were included in our main analysis, because unknown stage often reflects a lack of staging evaluation. A sensitivity analysis excluding these patients was performed as a robustness check.
Outcome Measures
Primary outcomes are health insurance coverage and stage at cancer diagnosis. The NCDB provides information on patient primary payer or insurance carrier at the time of cancer diagnosis. Based on this information, patients were categorized as having no health insurance, Medicaid coverage, private insurance (including TRICARE and military), or other insurance (Medicare including dual-eligible and with supplement, Veterans Affairs, Indian or Public Health Service, or unknown).
Disease stage at diagnosis in the NCDB was categorized based on pathological stage or clinical stage if pathological stage was missing or unknown according to the AJCC tumor, nodes, and metastases staging scheme (24). Two dichotomous variables were derived to indicate whether YAs had stage I (early-stage) cancer and stage IV (advanced-stage) cancer at diagnosis according to the AJCC staging scheme.
Covariates
Sociodemographic factors included sex, age group (18-25 years, 26-34 years, 35-39 years), self-reported race or ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, non-Hispanic others, unknown race or ethnicity), and residence metropolitan statistical area (MSA) status (metropolitan, non-MSA urban, non-MSA rural, unknown). Consistent with previous studies (11,14), zip code–level median household income was used as a proxy of patient-level family income and converted to percent of the federal poverty level (FPL) by assuming a family size of 4. Income was then classified as low (≤138% of FPL), middle (139%-400% of FPL), or high (>400% of FPL).
Statistical Analysis
We applied the difference-in-difference (DD) method to examine changes in the percentages of patients who had no insurance, Medicaid, or private insurance at diagnosis and the percentages of stage I diagnoses or stage IV diagnoses before and after the implementation of the expansion in states that expanded Medicaid coverage (“expansion states”) compared with states that did not (“nonexpansion states”). The DD method accounts for secular trends and common shocks (eg, provisions affecting all states) that may confound the association between Medicaid expansion and study outcomes (25,26).
More specifically, our DD analysis included 32 expansion states. Between January 2011 and December 2016 (our study period), 24 states and Washington, DC had expanded Medicaid by January 2014 and 7 states expanded later (Michigan: April 1, 2014; New Hampshire: August 15, 2014; Pennsylvania: January 1, 2015; Indiana: February 1, 2015; Alaska: September 1, 2015; Montana: January 1, 2016; Louisiana: July 1, 2016) (27). We also included 19 nonexpansion states that did not implement the expansion at any point during our study period. Medicaid expansion status was determined based on patients’ residence by state.
Consistent with prior studies (28–30), the years 2011 through 2013 were designated as the preexpansion period and 2014 through 2016 as the postexpansion period for states that expanded Medicaid in January 2014 and for nonexpansion states. For states that expanded Medicaid after January 2014, we used the month of the state’s implementation of Medicaid expansion as the beginning of the postexpansion period.
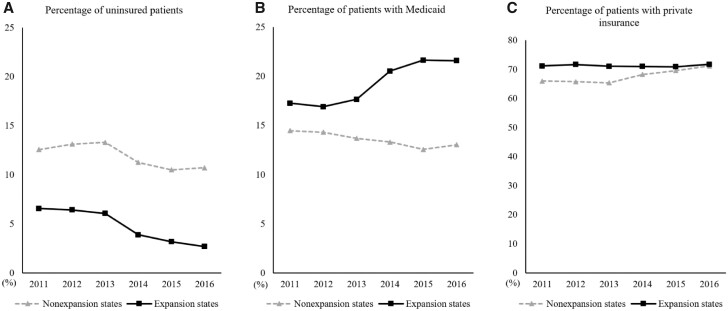
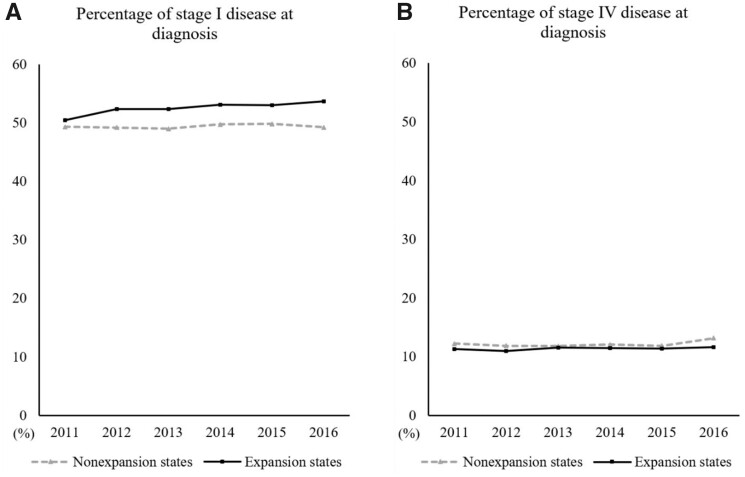
An assumption of the DD method is parallel trends between expansion and nonexpansion states in the preexpansion period (25). We tested this assumption graphically (Figures 1 and 2) and by performing a falsification test as suggested in previous DD studies (11,31). Non-statistically significant difference in outcomes between expansion and nonexpansion states when a pseudo-policy change year was used (detailed in Supplementary Table 1, available online) supported the parallel trends assumption, except in the cases of percentage uninsured and percentage with Medicaid where slightly divergent trends began preexpansion. This could be partly accounted for by including the secular trend in DD models (32).
Figure 1.
Trends in the percentages of uninsured patients, patients with Medicaid, and patients with private insurance among newly diagnosed cancer patients aged 18-39 years in Medicaid expansion states vs nonexpansion states, 2011-2016. A) The trend in the percentage of uninsured patients. B) The trend in the percentage of patients with Medicaid. C) The trend in the percentage of patients with private insurance.
Figure 2.
Trends in the percentage of stage I disease at diagnosis and the percentage of stage IV disease at diagnosis among newly diagnosed young adult cancer patients aged 18-39 years in Medicaid expansion states vs nonexpansion states, 2011-2016. A) The trend in the percentage of stage I disease at diagnosis. B) The trend in the percentage of stage IV disease at diagnosis.
Linear probability models were used in DD analysis (33). Crude percentages, pre-post differences, and crude and adjusted DD were estimated. Adjusted DD was calculated controlling for sex, age group, race or ethnicity, zip code–level income, and MSA. Consistent with prior DD analyses (32), we further adjusted for preexpansion linear time trends given the nonparallel trends in percentage uninsured and percentage with Medicaid. We also included residence state as a random effect to account for within-state clustering, consistent with previous studies on Medicaid expansion and health-care outcomes (28,34,35). DD analyses were conducted for YA patients overall and stratified by sociodemographic factors (ie, age groups, race or ethnicity, zip code–level income, and residence MSA status) to examine the differential effects of Medicaid expansion across YA subpopulations. When examining the expansion-associated change in cancer stage at diagnosis, DD analyses were performed for all cancers combined and then by cancer type for the 10 most prevalent cancers among the US YA population. P values from χ2 tests and regression models for crude and adjusted DD were calculated. All results were determined as statistically significant at P < .05. All statistical tests were 2-sided.
Results
Sample Characteristics
Of the 309 413 YAs, more than one-half were female (62.9%) and non-Hispanic White (67.4%), and nearly one-half (43.3%) were aged 26-34 years (Table 1). The most common types of cancer among YA patients were thyroid, female breast, testis, melanoma, colon or rectum, cervix, brain or other nervous system, and hematologic cancers.
Table 1.
Characteristics of newly diagnosed young adult cancer patients aged 18-39 years, 2011-2016a
| Characteristics | Total, No. (%) | Medicaid expansion states, | Nonexpansion states, | P b |
|---|---|---|---|---|
| No. (%) | No. (%) | |||
| Total No. | 309 413 | 193 109 | 116 304 | |
| Sex | <.001 | |||
| Male | 114 901 (37.1) | 72 386 (37.5) | 42 515 (36.6) | |
| Female | 194 512 (62.9) | 120 723 (62.5) | 73 789 (63.4) | |
| Age, y | <.001 | |||
| 18-25 | 54 366 (17.6) | 34 733 (18.0) | 19 633 (16.9) | |
| 26-34 | 133 945 (43.3) | 83 763 (43.4) | 50 182 (43.1) | |
| 35-39 | 121 102 (39.1) | 74 613 (38.6) | 46 489 (40.0) | |
| Race or ethnicity | <.001 | |||
| Non-Hispanic White | 208 684 (67.4) | 132 768 (68.8) | 75 916 (65.3) | |
| Non-Hispanic Black | 36 668 (11.9) | 18 333 (9.5) | 18 335 (15.8) | |
| Hispanic | 40 033 (12.9) | 24 243 (12.6) | 15 790 (13.6) | |
| Non-Hispanic other | 20 273 (6.6) | 15 040 (7.8) | 5233 (4.5) | |
| Unknown | 3755 (1.2) | 2725 (1.4) | 1030 (0.9) | |
| Zip code–level median household income | <.001 | |||
| Low (≤138 FPL) | 22 314 (7.2) | 12 098 (6.3) | 10 216 (8.8) | |
| Middle (139-400 FPL) | 258 544 (83.6) | 159 592 (82.6) | 98 952 (85.1) | |
| High (>401 FPL) | 27 085 (8.8) | 20 259 (10.5) | 6826 (5.9) | |
| Unknown | 1470 (0.5) | 1160 (0.6) | 310 (0.3) | |
| Residence MSA status | <.001 | |||
| Metropolitan | 262 625 (84.9) | 166 841 (86.4) | 95 784 (82.4) | |
| Non-MSA urban | 35 022 (11.3) | 19 414 (10.1) | 15 608 (13.4) | |
| Non-MSA rural | 3786 (1.2) | 1716 (0.9) | 2070 (1.8) | |
| Unknown | 7980 (2.6) | 5138 (2.7) | 2842 (2.4) | |
| Year of cancer diagnosis | .02 | |||
| 2011 | 49 203 (15.9) | 30 674 (15.9) | 18 529 (15.9) | |
| 2012 | 50 570 (16.3) | 31 280 (16.2) | 19 290 (16.6) | |
| 2013 | 51 331 (16.6) | 32 138 (16.6) | 19 193 (16.5) | |
| 2014 | 52 573 (17.0) | 33 046 (17.1) | 19 527 (16.8) | |
| 2015 | 53 438 (17.3) | 33 246 (17.2) | 20 192 (17.4) | |
| 2016 | 52 298 (16.9) | 32 725 (16.9) | 19 573 (16.8) | |
| Cancer stage at diagnosis | <.001 | |||
| I | 139 855 (45.2) | 89 478 (46.3) | 50 377 (43.3) | |
| II | 49 335 (15.9) | 30 416 (15.8) | 18 919 (16.3) | |
| III | 35 399 (11.4) | 21 507 (11.1) | 13 892 (11.9) | |
| IV | 28 628 (9.3) | 17 397 (9.0) | 11 231 (9.7) | |
| Unknownc | 15 553 (5.0) | 9465 (4.9) | 6088 (5.2) | |
| Not applicabled | 40 643 (13.1) | 24 846 (12.9) | 15 797 (13.6) | |
| Cancer site | <.001 | |||
| Thyroid | 55 048 (17.8) | 36 403 (18.9) | 18 645 (16.0) | |
| Female breast | 46 687 (15.1) | 28 525 (14.8) | 18 162 (15.6) | |
| Testis | 23 699 (7.7) | 15 504 (8.0) | 8195 (7.0) | |
| Melanoma | 20 554 (6.6) | 13 303 (6.9) | 7251 (6.2) | |
| Colon or rectum | 15 161 (4.9) | 9121 (4.7) | 6040 (5.2) | |
| Non-Hodgkin lymphoma | 15 225 (4.9) | 9569 (5.0) | 5656 (4.9) | |
| Cervix | 14 445 (4.7) | 8171 (4.2) | 6274 (5.4) | |
| Hodgkin lymphoma | 14 600 (4.7) | 9298 (4.8) | 5302 (4.6) | |
| Other | 103 994 (33.6) | 63 215 (32.7) | 40 779 (35.1) | |
| Brain or other nervous system | 14 168 (4.6) | 8785 (4.5) | 5383 (4.6) | |
| Leukemia | 13 766 (4.4) | 8381 (4.3) | 5385 (4.6) | |
| Kidney | 10 375 (3.4) | 6140 (3.2) | 4235 (3.6) | |
| Uterus | 8007 (2.6) | 4708 (2.4) | 3299 (2.8) | |
| Soft tissue including heart | 7048 (2.3) | 4299 (2.2) | 2749 (2.4) | |
| Lung | 4502 (1.5) | 2758 (1.4) | 1744 (1.5) | |
| Ovary | 6204 (2.0) | 3777 (2.0) | 2427 (2.1) | |
| Oral cavity or pharynx | 5981 (1.9) | 3647 (1.9) | 2334 (2.0) | |
| Bones or joints | 3299 (1.1) | 1952 (1.0) | 1347 (1.2) | |
| Stomach | 3028 (1.0) | 1912 (1.0) | 1116 (1.0) | |
| All other rare cancers | 22 249 (7.2) | 13543 (7.0) | 8706 (7.5) | |
Authors’ analysis of the 2011-2016 National Cancer Database. FPL = federal poverty level; MSA = metropolitan statistical area.
P values were from 2-sided χ2 tests.
Included patients (<0.1%) with occult stage.
Cancers without an applicable American Joint Committee Classification (AJCC) staging scheme; these cancers were excluded in our analysis of stage at diagnosis.
Sociodemographic characteristics differed by state’s expansion status. Compared with YAs residing in expansion states, those in nonexpansion states were more likely to be non-Hispanic Black (15.8% vs 9.5%, P < .001) and to reside in zip codes with low-income level (8.8% vs 6.3%, P < .001) and less likely to reside in metropolitan areas (82.4% vs 86.4%, P < .001).
Expansion-Associated Changes in Insurance Coverage
From the preexpansion to postexpansion periods, the percentage of YAs with Medicaid increased (absolute percentage change [APC] = 4.6 percentage points [ppt]; 95% confidence interval [CI] = 4.3 to 5.0 ppt) in expansion states and decreased in nonexpansion states (APC = −1.2 ppt, 95% CI = −1.6 to −0.8 ppt); in contrast, the percentage of privately insured YAs did not change in expansion states and increased (APC = 4.0 ppt, 95% CI = 3.4 to 4.5 ppt) in nonexpansion states (Table 2; Figure 1). Consequently, the percentage of uninsured YAs decreased more in expansion states (APC = −3.2 ppt, 95% CI = −3.4 to −3.1 ppt) than nonexpansion states (APC = −2.2 ppt, 95% CI = −2.6 to −1.8 ppt), resulting in a relative reduction of 1.0 ppt (95% CI = −1.4 to −0.7 ppt, P < .001) in the percentage of uninsured YAs in expansion compared with nonexpansion states in adjusted DD models.
Table 2.
Changes in health insurance coverage associated with Medicaid expansion among newly diagnosed young adult cancer patients aged 18-39 years, 2011-2016a
| Outcomes | Expansion states |
Nonexpansion states |
Crude model |
Adjusted modelb |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre-ME, % | Post-ME, % | Absolute difference (95% CI), ppt | Pre-ME, % | Post-ME, % | Absolute difference (95% CI), ppt | DD (95% CI), ppt | P c | DD (95% CI), ppt | P c | |
| Uninsured | 6.3 | 3.0 | −3.2 (−3.4 to −3.1) | 13.0 | 10.8 | −2.2 (−2.6 to −1.8) | −1.1 (−1.5 to −0.7) | <.001 | −1.0 (−1.4 to −0.7) | <.001 |
| Medicaid | 17.1 | 21.7 | 4.6 (4.3 to 5.0) | 14.1 | 13.0 | −1.2 (−1.6 to −0.8) | 5.8 (5.3 to 6.3) | <.001 | 5.4 (4.8 to 5.9) | <.001 |
| Private | 71.4 | 71.0 | −0.4 (−0.8 to 0.02) | 65.7 | 69.7 | 4.0 (3.4 to 4.5) | −4.4 (−5.0 to −3.7) | <.001 | −4.2 (−4.8 to −3.5) | <.001 |
Authors’ analysis of the 2011-2016 National Cancer Database. CI = confidence interval; DD = difference in difference; ME = Medicaid expansion; ppt = percentage points.
Adjusted model: regression models also adjusted for age, sex, race or ethnicity, zip code–level income, residence metropolitan statistical area status, and linear time trends as well as state adjusted as a random effect.
P values were calculated from linear probability regression models and reflect 2-sided test of statistical significance.
In stratified analyses, the changes in insurance coverage were observed across YA subgroups by race or ethnicity, levels of zip code income, MSA status, and age groups (Supplementary Table 2, available online). Specifically, the expansion-associated reductions in the percentage of uninsured YAs were larger in magnitude among non-Hispanic Black and Hispanic (vs non-Hispanic White) patients, rural (vs urban) areas, and poorer areas.
Expansion-Associated Changes in Stage at Diagnosis
Overall, the percentage of YAs with stage I disease at diagnosis did not change in nonexpansion states; in contrast, it increased from 51.6% to 53.5% in expansion states (APC = 1.9 ppt, 95% CI = 1.4 to 2.4 ppt) from the preexpansion to postexpansion periods (Table 3; Figure 2). This resulted in an increase (adjusted DD = 1.4 ppt, 95% CI = 0.6 to 2.2 ppt, P < .001) in the percentage of stage I diagnoses in expansion states compared with nonexpansion states. No statistically significant change was observed in the percentage of stage IV diagnoses in expansion relative to nonexpansion states (Table 4; Figure 2; Supplementary Table 3, available online).
Table 3.
Changes in the percentage of stage I disease at diagnosis associated with Medicaid expansion among newly diagnosed young adult cancer patients aged 18-39 years, 2011-2016a,b
| Cancer site | Expansion states |
Nonexpansion states |
Crude model |
Adjusted modelc |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre-ME, % | Post-ME, % | Absolute difference (95% CI), ppt | Pre-ME, % | Post-ME, % | Absolute difference (95% CI), ppt | DD (95% CI), ppt | P d | DD (95% CI), ppt | P d | |
| All cancer types combined | 51.6 | 53.5 | 1.9 (1.4 to 2.4) | 49.1 | 49.6 | 0.4 (−0.2 to 1.1) | 1.4 (0.6 to 2.2) | <.001 | 1.4 (0.6 to 2.2) | <.001 |
| Thyroid | 91.3 | 94.3 | 3.0 (2.5 to 3.6) | 88.6 | 92.0 | 3.4 (2.6 to 4.3) | −0.4 (−1.4 to 0.6) | .43 | −0.7 (−1.6 to 0.3) | .18 |
| Female breast | 32.2 | 34.9 | 2.7 (1.6 to 3.8) | 32.4 | 33.2 | 0.8 (−0.5 to 2.2) | 1.9 (0.1 to 3.6) | .04 | 1.8 (0.03 to 3.5) | .046 |
| Melanoma | 67.8 | 69.5 | 1.7 (0.1 to 3.2) | 64.8 | 64.7 | −0.2 (−2.4 to 2.0) | 1.8 (−0.9 to 4.5) | .18 | 2.0 (−0.6 to 4.7) | .13 |
| Colon and rectum | 17.0 | 17.4 | 0.4 (−1.1 to 2.0) | 15.9 | 15.4 | −0.5 (−2.4 to 1.3) | 0.9 (−1.5 to 3.3) | .45 | 0.9 (−1.6 to 3.3) | .49 |
| Non-Hodgkin lymphoma | 31.0 | 30.7 | −0.3 (−2.2 to 1.6) | 28.9 | 28.4 | −0.5 (−2.9 to 1.9) | 0.2 (−2.8 to 3.2) | .90 | 0.2 (−2.8 to 3.2) | .89 |
| Cervix | 62.1 | 61.4 | −0.7 (−2.8 to 1.4) | 58.5 | 57.3 | −1.2 (−3.7 to 1.2) | 0.5 (−2.7 to 3.8) | .74 | 0.3 (−3.0 to 3.5) | .87 |
| Hodgkin lymphoma | 10.1 | 9.8 | −0.3 (−1.5 to 0.9) | 11.7 | 10.1 | −1.6 (−3.3 to 0.05) | 1.3 (−0.8 to 3.4) | .21 | 1.3 (−0.8 to 3.3) | .23 |
| Other | 44.4 | 45.5 | 1.0 (0.02 to 2.0) | 45.2 | 45.3 | 0.2 (−1.1 to 1.4) | 0.8 (−0.7 to 2.4) | .30 | 1.1 (−0.5 to 2.7) | .16 |
Authors’ analysis of the 2011-2016 National Cancer Database. CI = confidence interval; DD = difference in difference; ME = Medicaid expansion; ppt = percentage points.
Cases without applicable stages (eg, leukemia, brain tumor) were excluded. Testicular cancer cases were excluded due to high percentage of unknown stage observed exclusively among patients with testicular cancer.
Adjusted model: regression models also adjusted for age, sex, race or ethnicity, zip code–level income, residence metropolitan statistical area status, and linear time trends as well as state adjusted as a random effect.
P values were calculated from linear probability regression models and reflect 2-sided test of statistical significance.
Table 4.
Changes in the percentage of stage IV disease at diagnosis associated with Medicaid expansion among newly diagnosed young adult cancer patients aged 18-39 years, 2011-2016a,b
| Cancer site | Expansion states |
Nonexpansion states |
Crude model |
Adjusted modelc |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre-ME, % | Post-ME, % | Absolute difference (95% CI), ppt | Pre-ME, % | Post-ME, % | Absolute difference (95% CI), ppt | DD (95% CI), ppt | P d | DD (95% CI), ppt | P d | |
| All cancer types combined | 11.3 | 11.4 | 0.1 (−0.2 to 0.4) | 12.0 | 12.4 | 0.4 (−0.03 to 0.8) | −0.3 (−0.8 to 0.2) | .24 | −0.4 (−0.9 to 0.1) | .14 |
| Thyroid | 0.3 | 0.4 | 0.01 (−0.1 to 0.1) | 0.4 | 0.4 | −0.03 (−0.2 to 0.1) | 0.03 (−0.2 to 0.2) | .76 | 0.03 (−0.2 to 0.2) | .79 |
| Female breast | 5.9 | 6.2 | 0.2 (−0.3 to 0.8) | 5.9 | 6.7 | 0.8 (0.1 to 1.5) | −0.5 (−1.4 to 0.4) | .24 | −0.5 (−1.4 to 0.4) | .28 |
| Melanoma | 2.9 | 3.2 | 0.3 (−0.3 to 0.8) | 2.9 | 4.3 | 1.4 (0.5 to 2.2) | −1.1 (−2.2 to −0.1) | .04 | −1.2 (−2.2 to −0.2) | .02 |
| Colon and rectum | 26.4 | 26.8 | 0.4 (−1.4 to 2.2) | 27.2 | 27.7 | 0.5 (−1.8 to 2.8) | −0.1 (−3.0 to 2.8) | .94 | 0.1 (−2.8 to 3.0) | .97 |
| Non-Hodgkin lymphoma | 30.9 | 32.0 | 1.1 (−0.8 to 3.0) | 32.3 | 32.8 | 0.6 (−1.9 to 3.0) | 0.5 (−2.6 to 3.6) | .74 | 0.6 (−2.5 to 3.7) | .72 |
| Cervix | 6.9 | 6.7 | −0.2 (−1.3 to 0.9) | 6.3 | 7.6 | 1.4 (0.1 to 2.6) | −1.6 (−3.3 to 0.1) | .06 | −1.6 (−3.3 to 0.1) | .06 |
| Hodgkin lymphoma | 17.8 | 20.1 | 2.3 (0.7 to 3.9) | 18.1 | 19.3 | 1.1 (−1.0 to 3.2) | 1.2 (−1.5 to 3.8) | .39 | 1.4 (−1.2 to 4.0) | .29 |
| Other | 19.7 | 18.8 | −0.9 (−1.7 to −0.1) | 19.5 | 19.0 | −0.5 (−1.4 to 0.5) | −0.4 (−1.7 to 0.8) | .49 | −0.7 (−2.0 to 0.5) | .25 |
Authors’ analysis of the 2011-2016 National Cancer Database. CI = confidence interval; DD = difference in difference; ME = Medicaid expansion; ppt = percentage points.
Cases without applicable stages (eg, leukemia, brain tumor) were excluded. Testicular cancer cases were excluded due to high percentage of unknown stage observed exclusively among patients with testicular cancer.
Adjusted model: regression models also adjusted for age, sex, race or ethnicity, zip code–level income, residence metropolitan statistical area status, and linear time trends as well as state adjusted as a random effect.
P values were calculated from linear probability regression models and reflect 2-sided test of statistical significance.
In subgroup analyses by cancer type, DD estimates showed a relative increase in stage I diagnoses in expansion compared with nonexpansion states across specific cancer types, except for thyroid; yet, the positive estimate was statistically significant only for female breast cancer (adjusted DD = 1.8 ppt, 95% CI = 0.03 to 3.5 ppt, P = .046) (Table 3). DD models also showed a statistically significant decrease in stage IV melanoma diagnoses (adjusted DD = −1.2 ppt, 95% CI = −2.2 to −0.2 ppt, P = .02) and a marginally statistically significant decrease in stage IV cervix cancer diagnoses (adjusted DD = −1.6 ppt, 95% CI = −3.3 to 0.1 ppt, P = .06) in expansion relative to nonexpansion states (Table 4).
In subgroup analyses by sociodemographic factors, expansion-associated changes in the percentage of stage I diagnoses varied across YA subgroups by age category, race or ethnicity, or residence MSA status (Table 5). Increases in stage I diagnoses were observed across all subgroups in expansion states and in most subgroups in nonexpansion states, although not all were statistically significant. Specifically, in expansion states, the percentage of stage I diagnoses increased the most among non-Hispanic Black patients (APC = 2.1 ppt [95% CI = 0.5 to 3.6 ppt] vs 1.8 ppt in both non-Hispanic White [95% CI = 1.2 to 2.4 ppt] and Hispanic patients [95% CI = 0.3 to 3.2 ppt]) and among YAs residing in rural areas (APC = 6.4 ppt [95% CI = 1.1 to 11.7 ppt] vs 1.8 ppt [95% CI = 1.3 to 2.4 ppt] in those residing in metropolitan areas). In contrast, in nonexpansion states, non-statistically significant changes were observed across these subgroups. Consequently, the relative increase in stage I diagnoses in expansion compared with nonexpansion states was larger in magnitude among non-Hispanic Black patients (adjusted DD = 2.2 ppt, 95% CI = −0.03 to 4.4 ppt, P = .05) than non-Hispanic White patients (adjusted DD = 1.4 ppt, 95% CI = 0.4 to 2.3 ppt, P = .008) and among YAs living in rural areas (adjusted DD = 7.2 ppt, 95% CI = 0.2 to 14.3 ppt, P = .045) compared with those living in metropolitan areas (adjusted DD = 1.3 ppt, 95% CI = 0.4 to 2.2 ppt, P = .004). Notably, DD models showed no statistically significant change (P > .1) in stage I diagnoses among Hispanic patients. Moreover, among YAs, we observed a larger expansion-associated shift to stage I diagnoses in younger patients aged 18-25 years (adjusted DD = 3.1 ppt, 95% CI = 1.0 to 5.1 ppt) compared with those aged 26-34 years (adjusted DD = 1.6 ppt, 95% CI = 0.3 to 2.8 ppt) and aged 35-39 years (adjusted DD = 0.6 ppt, 95% CI = −0.6 to 1.9 ppt).
Table 5.
Changes in the percentage of stage I disease at diagnosis associated with Medicaid expansion by sociodemographic factors among newly diagnosed cancer patients aged 18-39 years, 2011-2016a,b
| Characteristics | Expansion states |
Nonexpansion states |
Crude model |
Adjusted modelc |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre-ME, % | Post-ME, % | Absolute difference (95% CI), ppt | Pre-ME, % | Post-ME, % | Absolute difference (95% CI), ppt | DD (95% CI), ppt | P d | DD (95% CI), ppt | P d | |
| Age group | ||||||||||
| 18-25 y | 51.5 | 54.2 | 2.7 (1.5 to 4.0) | 49.8 | 49.5 | −0.2 (−2.0 to 1.5) | 3.0 (0.8 to 5.1) | .006 | 3.1 (1.0 to 5.1) | .004 |
| 26-34 y | 53.6 | 55.5 | 1.9 (1.2 to 2.7) | 51.1 | 51.5 | 0.4 (−0.5 to 1.4) | 1.5 (0.2 to 2.7) | .02 | 1.6 (0.3 to 2.8) | .01 |
| 35-39 y | 49.6 | 51.1 | 1.5 (0.7 to 2.2) | 47.0 | 47.7 | 0.7 (−0.3 to 1.6) | 0.8 (−0.4 to 2.0) | .21 | 0.6 (−0.6 to 1.9) | .33 |
| Race or ethnicitye | ||||||||||
| Non-Hispanic White | 54.1 | 55.9 | 1.8 (1.2 to 2.4) | 52.7 | 53.1 | 0.4 (−0.4 to 1.2) | 1.4 (0.4 to 2.4) | .006 | 1.4 (0.4 to 2.3) | .008 |
| Non-Hispanic Black | 37.7 | 39.7 | 2.1 (0.5 to 3.6) | 36.9 | 36.5 | −0.3 (−1.9 to 1.2) | 2.4 (0.2 to 4.6) | .03 | 2.2 (−0.03 to 4.4) | .05 |
| Hispanic | 47.6 | 49.3 | 1.8 (0.3 to 3.2) | 46.2 | 47.0 | 0.8 (−1.0 to 2.6) | 1.0 (−1.3 to 3.3) | .41 | 1.0 (−1.3 to 3.3) | .39 |
| Non-Hispanic other | 52.2 | 53.8 | 1.6 (−0.1 to 3.4) | 49.0 | 50.6 | 1.6 (−1.4 to 4.6) | −0.05 (−3.5 to 3.5) | 1.00 | 0.6 (−2.9 to 4.0) | .75 |
| Zip code–level median household incomee | ||||||||||
| High (>400 FPL) | 57.3 | 58.4 | 1.1 (−0.4 to 2.6) | 56.3 | 55.7 | −0.6 (−3.2 to 2.0) | 1.7 (−1.3 to 4.7) | .27 | 1.5 (−1.4 to 4.5) | .31 |
| Middle (139-400 FPL) | 51.6 | 53.3 | 1.7 (1.2 to 2.3) | 49.7 | 49.9 | 0.2 (−0.5 to 0.9) | 1.5 (0.6 to 2.4) | <.001 | 1.5 (0.7 to 2.4) | <.001 |
| Low (≤138 FPL) | 43.5 | 47.0 | 3.4 (1.4 to 5.5) | 38.7 | 42.3 | 3.5 (1.4 to 5.7) | −0.1 (−3.0 to 2.9) | .96 | −0.04 (−2.9 to 2.9) | .98 |
| Residence MSA statuse | ||||||||||
| Metropolitan | 51.7 | 53.6 | 1.8 (1.3 to 2.4) | 49.3 | 49.8 | 0.5 (−0.2 to 1.2) | 1.4 (0.5 to 2.2) | .003 | 1.3 (0.4 to 2.2) | .004 |
| Non-MSA urban | 50.8 | 52.7 | 1.9 (0.3 to 3.5) | 47.9 | 49.3 | 1.4 (−0.4 to 3.1) | 0.5 (−1.9 to 2.9) | .68 | 0.6 (−1.8 to 2.9) | .63 |
| Non-MSA rural | 46.6 | 53.0 | 6.4 (1.1 to 11.7) | 48.1 | 47.9 | −0.2 (−5.0 to 4.6) | 6.7 (−0.5 to 13.8) | .07 | 7.2 (0.2 to 14.3) | .045 |
Authors’ analysis of the 2011-2016 National Cancer Database. CI = confidence interval; DD = difference in difference; FPL = federal poverty level; ME = Medicaid expansion; MSA = metropolitan statistical area; ppt = percentage points.
Cases without applicable stages (eg, leukemia, brain tumor) were excluded. Testicular cancer cases were excluded due to high percentage of unknown stage observed exclusively among patients with testicular cancer.
Adjusted model: regression models also adjusted for linear time trends, age, sex, race or ethnicity, zip code–level income, and residence MSA status, when applicable, as well as state as a random effect.
P values were calculated from linear probability regression models and reflect 2-sided test of statistical significance.
Data for unknown categories not shown.
Findings were similar in the sensitivity analysis that excluded patients with unknown stage (Supplementary Tables 4-7, available online).
Discussion
Using a nationwide large sample of YAs newly diagnosed with cancer, our DD analyses demonstrated a statistically significant reduction in the percentage of uninsured YA patients associated with Medicaid expansion. Medicaid coverage gains in expansion states were greater than private insurance gains in nonexpansion states (potentially through private coverage options under the ACA) (8). Moreover, DD analyses revealed an expansion-associated shift to presentation with early stage at diagnosis, especially among YAs living in rural areas and non-Hispanic Black patients. Importantly, our findings of reduced disparities in expansion states suggest a widening of geographic disparities between YA cancer patients residing in expansion states and those residing in nonexpansion states.
These findings are consistent with cancer-specific studies reporting reductions in noninsurance following Medicaid expansion (11,12,17) and the few studies reporting increases in early-stage diagnoses among patients younger than 65 years old (13,16). For example, Medicaid expansion was associated with small increases in early-stage diagnoses among nonelderly cancer patients during the first year following expansion (13). However, the magnitude of the association was larger in our study, likely reflecting a longer time horizon postexpansion, different data sources, and the specific impact on a younger population for which most screening guidelines do not exist. In particular, our study focused on YAs aged 18-39 years, a population with the highest uninsurance rate across age groups before the ACA (36).
Given the lower overall incidence of cancer in YAs compared with older adults, there are no regular screening guidelines (ie, mammograms, colorectal screening) for common cancers in the YA population. The notable exception is the application of Pap smears and human papillomavirus screening for early detection of cervical cancer (19). Accordingly, the shift toward stage I disease at diagnosis observed for all cancers combined, as well as the statistically significant drop in stage IV melanoma diagnoses, all suggest improved access to health-care services for timely symptom assessment, following Medicaid expansion (6,37). It is also possible that increased access to routine primary care visits lead to incidental detection following the expansion (6,37). The shift to stage I diagnoses observed among YAs living in rural areas and non-Hispanic Black patients further highlights the role of the ACA in narrowing sociodemographic disparities in access to cancer care. Of note, although the postexpansion shift towards stage I diagnoses was high for all YA cancers combined, the DD estimates for stage I diagnoses were suggestive but only statistically significant for breast cancer, potentially due to limited power given the smaller sample sizes of other specific cancer sites.
Importantly, YAs diagnosed at an earlier stage may require less aggressive therapies, have lower risks for subacute or late morbidity related to cancer therapies, and bear lower out-of-pocket burden of medical costs (38). Earlier cancer stage at diagnosis was historically associated with better survival outcomes (39) and will need to be confirmed in this population in the future. In addition, as described in a recent study (40), Medicaid expansion can also enhance individuals’ ability to maintain health insurance and reduce coverage disruptions, which would be associated with improvements in access to care post diagnosis and treatment and, ultimately, better survival (41,42). This is germane to YA cancers where survivorship care is imperative for mitigating the late effects of cancer therapy. Thus, future studies should quantify the impact of the ACA Medicaid expansion on maintaining insurance coverage post cancer diagnosis and longer-term outcomes such as late morbidity, financial hardship, and survival rates, as well as sociodemographic disparities in these outcomes, among YA cancer survivors.
Besides the lack of health insurance, other barriers to early cancer diagnosis may exist for YA cancer patients. We found that although expansion-associated reductions in uninsurance rates were observed among Hispanic patients and those residing in low-income areas (Supplementary Table 2, available online), the insurance gains have not translated to an increase in stage I diagnoses among these YA groups (Table 5). This finding suggests that studies of other barriers to receiving timely care for cancer detection are needed. These include barriers related to culture, language, health literacy, immigration status, and competing obligations during young adulthood (43,44). Future efforts beyond expanding insurance coverage are needed to improve the delivery and quality of health care for early detection of YA cancers.
This study had some limitations. Although the patient sample from our data was not population based, the NCDB—a hospital-based cancer registry with data from American College of Surgeons Commission on Cancer–accredited facilities across all states and territories—captures over 70% of all new cancer cases in the United States, with the highest case coverage of nearly 80% for YAs (45). Furthermore, previous comparisons between the NCDB and population-based cancer registries have shown similarity in patient characteristics (45,46). As in other studies using cancer registry data, patients’ health insurance status was documented only once in the NCDB, with no indication of when Medicaid enrollment occurred. More research is needed to distinguish YAs with Medicaid preceding a cancer diagnosis from those who gained Medicaid on diagnosis and to assess the effects of insurance continuity on health outcomes subsequent to a cancer diagnosis, including cancer treatment, survivorship care, and mortality.
Prior research has suggested that Medicaid status might be underreported in cancer registries (47). However, in a DD framework, we were interested in outcome changes over time; any systematic error associated with Medicaid underreporting would not affect our findings. Another limitation was the lack of individual-level income in the NCDB. Any nondifferential measurement error from using zip code–level income (as a proxy for individual income) would bias results toward the null, potentially underestimating the reduction in disparities of insurance coverage and early diagnoses following the ACA. Future studies with information on individual-level income are needed to better understand the changes in YA cancer disparities post ACA. Additionally, causality could not be determined given the observational nature of this study; it is possible that aspects of the ACA other than expanding Medicaid eligibility may differentially affect expansion vs nonexpansion states. Moreover, given the smaller sample sizes for subgroup analyses, there was less power to detect statistical significance within or across strata. Lastly, our ability to determine the severity of illness at presentation was limited for patients with brain tumors and leukemia, which have a high incidence in YAs but do not have staging criteria akin to other cancers (48).
Despite these limitations, this study provides compelling evidence on the benefit of Medicaid expansion under the ACA, with statistically significant increases in health insurance coverage and early-stage diseases at diagnosis in YAs with cancer and with greater increases among vulnerable populations, including non-Hispanic Black patients and those living in rural areas. This is a large initial step in addressing the disparities that YA patients, a group with unique health-care needs, have faced in cancer care and outcomes. As states consider expanding Medicaid eligibility or continuing the current expansion, our findings highlight the benefits of public health insurance for early cancer diagnoses among medically vulnerable populations in the United States. As newer data become available, future research should monitor changes associated with the expansion beyond 2016 as well as the downstream survival benefit from insurance coverage gains and earlier stage at diagnosis. Future research should also investigate the differential or synergistic effects of multiple provisions (such as Medicaid expansion and Dependent Coverage Expansion) under the ACA on YA cancer outcomes (49,50).
Funding
This work was supported by grant R03CA259665 (Ji, Castellino, Mertens, Han) from the National Cancer Institute of the National Institutes of Health.
Notes
Role of the funder: The funder had no role in the design of the study; collection, analysis, and interpretation of the data; writing of the manuscript; and decision to submit the manuscript for publication.
Disclosures: The authors have no conflicts of interest to disclose.
Author contributions: XJ, SMC, ACM, KRY, XH: Scientific design, conceptualization, and project administration. XH: Formal analysis. XJ, SMC, ACM, JZ, LN, AJ, KRY, XH: Interpretation of results. XJ: Drafting of the initial manuscript. XJ, SMC, ACM, JZ, LN, AJ, KRY, XH: Review and critical revision. SMC, ACM, KRY: Supervision.
Disclaimer: The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Data Availability
The data underlying this article were provided by the American College of Surgeons and accessed at the American Cancer Society by permission. The data cannot be shared publicly per the Data User Agreement. The National Cancer Database Participant User Files are available through application to investigators associated with the Commission on Cancer accredited cancer programs (https://www.facs.org/quality-programs/cancer/ncdb/puf).
Supplementary Material
Contributor Information
Xu Ji, Department of Pediatrics, Emory University School of Medicine, Atlanta, GA, USA; Aflac Cancer and Blood Disorders Center, Children's Healthcare of Atlanta, Atlanta, GA, USA.
Sharon M Castellino, Department of Pediatrics, Emory University School of Medicine, Atlanta, GA, USA; Aflac Cancer and Blood Disorders Center, Children's Healthcare of Atlanta, Atlanta, GA, USA.
Ann C Mertens, Department of Pediatrics, Emory University School of Medicine, Atlanta, GA, USA; Aflac Cancer and Blood Disorders Center, Children's Healthcare of Atlanta, Atlanta, GA, USA; Department of Epidemiology, Emory University Rollins School of Public Health, Atlanta, GA, USA.
Jingxuan Zhao, Surveillance and Health Equity Science, American Cancer Society, Atlanta, GA, USA.
Leticia Nogueira, Surveillance and Health Equity Science, American Cancer Society, Atlanta, GA, USA.
Ahmedin Jemal, Surveillance and Health Equity Science, American Cancer Society, Atlanta, GA, USA.
K Robin Yabroff, Surveillance and Health Equity Science, American Cancer Society, Atlanta, GA, USA.
Xuesong Han, Surveillance and Health Equity Science, American Cancer Society, Atlanta, GA, USA.
References
- 1.Centers for Disease Control and Prevention. 10 Leading causes of death by age group, United States – 2010. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control, Office of Statistics and Programming. https://www.cdc.gov/injury/wisqars/pdf/10lcid_all_deaths_by_age_group_2010-a.pdf. Accessed May 6, 2020.
- 2.American Cancer Society. Cancer facts and figures 2020. Atlanta, GA: American Cancer Society. 2020. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2020/cancer-facts-and-figures-2020.pdf. Accessed April 29, 2020.
- 3. Martin S, Ulrich C, Munsell M, Taylor S, Lange G, Bleyer A. Delays in cancer diagnosis in underinsured young adults and older adolescents. Oncologist. 2007;12(7):816–824. [DOI] [PubMed] [Google Scholar]
- 4. Berchick E. Who are the uninsured? Most uninsured were working-age adults. Washington, DC: U.S. Census Bureau. September 12, 2018. https://www.census.gov/library/stories/2018/09/who-are-the-uninsured.html. Accessed April 29, 2020.
- 5. Rosenberg AR, Kroon L, Chen L, Li CI, Jones B. Insurance status and risk of cancer mortality among adolescents and young adults. Cancer. 2015;121(8):1279–1286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Robbins AS, Lerro CC, Barr RD. Insurance status and distant‐stage disease at diagnosis among adolescent and young adult patients with cancer aged 15 to 39 years: National Cancer Data Base, 2004 through 2010. Cancer. 2014;120(8):1212–1219. [DOI] [PubMed] [Google Scholar]
- 7. Moke DJ, Tsai K, Hamilton AS, et al. Emerging cancer survival trends, disparities, and priorities in adolescents and young adults: California Cancer Registry-based study. JNCI Cancer Spectrum. 2019;3(2):pkz031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kaiser Family Foundation. Summary of the Affordable Care Act. Menlo Park, CA: Kaiser Family Foundation. 2013. http://files.kff.org/attachment/fact-sheet-summary-of-the-affordable-care-act. Accessed December 14, 2019.
- 9. Geiger AM, Castellino SM. Delineating the age ranges used to define adolescents and young adults. J Clin Oncol. 2011;29(16):e492–e493. [DOI] [PubMed] [Google Scholar]
- 10.Kaiser Family Foundation. Status of state action on the Medicaid expansion decision. Menlo Park, CA: Kaiser Family Foundation. 2020. https://www.kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act/. Accessed November 14, 2020.
- 11. Jemal A, Lin CC, Davidoff AJ, Han X. Changes in insurance coverage and stage at diagnosis among nonelderly patients with cancer after the Affordable Care Act. J Clin Oncol. 2017;35(35):3906–3915. [DOI] [PubMed] [Google Scholar]
- 12. Soni A, Sabik LM, Simon K, Sommers BD. Changes in insurance coverage among cancer patients under the Affordable Care Act. JAMA Oncol. 2018;4(1):122–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Han X, Yabroff KR, Ward E, Brawley OW, Jemal A. Comparison of insurance status and diagnosis stage among patients with newly diagnosed cancer before vs after implementation of the Patient Protection and Affordable Care Act. JAMA Oncol. 2018;4(12):1713–1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Sineshaw HM, Ellis MA, Yabroff KR, et al. Association of Medicaid expansion under the Affordable Care Act with stage at diagnosis and time to treatment initiation for patients with head and neck squamous cell carcinoma. JAMA Otolaryngol Head Neck Surg. 2020;146(3):247–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Barnes JM, Barker AR, King AA, Johnson KJ. Association of Medicaid expansion with insurance coverage among children with cancer. JAMA Pediatr. 2020;174(6):581. doi:10.1001/jamapediatrics.2020.0052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Soni A, Simon K, Cawley J, Sabik L. Effect of Medicaid expansions of 2014 on overall and early-stage cancer diagnoses. Am J Public Health. 2018;108(2):216–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Moss HA, Wu J, Kaplan SJ, Zafar SY. The Affordable Care Act’s Medicaid expansion and impact along the cancer-care continuum: a systematic review. J Natl Cancer Inst. 2020;112(8):779–791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Satyananda V, Ozao-Choy J, Dauphine C, Chen KT. Effect of the Affordable Care Act on breast cancer presentation at a safety net hospital. Am J Surg. 2019;217(4):764–766. [DOI] [PubMed] [Google Scholar]
- 19. Smith RA, Andrews KS, Brooks D, et al. Cancer screening in the United States, 2019: a review of current American Cancer Society guidelines and current issues in cancer screening. CA Cancer J Clin. 2019;69(3):184–210. [DOI] [PubMed] [Google Scholar]
- 20. Moss HA, Havrilesky LJ, Zafar SY, Suneja G, Chino J. Trends in insurance status among patients diagnosed with cancer before and after implementation of the Affordable Care Act. J Oncol Pract. 2018;14(2):e92–e102. [DOI] [PubMed] [Google Scholar]
- 21. Gunja MZ, Collins SR. Who are the remaining uninsured, and why do they lack coverage? Findings from the Commonwealth Fund Biennial Health Insurance Survey, 2018. New York, NY: Commonwealth Fund. 2019. https://www.commonwealthfund.org/publications/issue-briefs/2019/aug/who-are-remaining-uninsured-and-why-do-they-lack-coverage?redirect_source=/publications/2019/aug/who-are-remaining-uninsured-and-why-do-they-lack-coverage. Accessed January 2, 2021. [Google Scholar]
- 22. Randolph R, Holmes M. Running the numbers health insurance coverage in North Carolina: the rural-urban uninsured gap. N C Med J. 2018;79(6):397–401. [DOI] [PubMed] [Google Scholar]
- 23. Boffa DJ, Rosen JE, Mallin K, et al. Using the National Cancer Database for outcomes research: a review. JAMA Oncol. 2017;3(12):1722–1728. [DOI] [PubMed] [Google Scholar]
- 24. Edge SB, Byrd DR, Carducci MA, et al. AJCC Cancer Staging Manual. 7th ed. New York, NY: Springer; 2010. [Google Scholar]
- 25. Wooldridge JM. Econometric Analysis of Cross Section and Panel Data. Cambridge, MA: MIT Press; 2002. [Google Scholar]
- 26. Ryan AM, Burgess JF Jr, Dimick JB. Why we should not be indifferent to specification choices for difference‐in‐differences. Health Serv Res. 2015;50(4):1211–1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kaiser Family Foundation. Status of state Medicaid expansion decisions: interactive map. Menlo Park, CA: Kaiser Family Foundation. 2020. https://www.kff.org/medicaid/issue-brief/status-of-state-medicaid-expansion-decisions-interactive-map/. Accessed April 15, 2020.
- 28. Khatana SAM, Bhatla A, Nathan AS, et al. Association of Medicaid expansion with cardiovascular mortality. JAMA Cardiol. 2019;4(7):671–679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Gooptu A, Moriya AS, Simon KI, Sommers BD. Medicaid expansion did not result in significant employment changes or job reductions in 2014. Health Aff (Millwood). 2016;35(1):111–118. [DOI] [PubMed] [Google Scholar]
- 30. Brown CC, Moore JE, Felix HC, et al. Association of state Medicaid expansion status with low birth weight and preterm birth. JAMA. 2019;321(16):1598–1609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Hampton M, Lenhart O. The effect of the Affordable Care Act preexisting conditions provision on marriage. Health Econ. 2019;28(11):1345–1355. [DOI] [PubMed] [Google Scholar]
- 32. Takvorian SU, Oganisian A, Mamtani R, et al. Association of Medicaid expansion under the Affordable Care Act with insurance status, cancer stage, and timely treatment among patients with breast, colon, and lung cancer. JAMA Netw Open. 2020;3(2):e1921653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hellevik O. Linear versus logistic regression when the dependent variable is a dichotomy. Qual Quant. 2009;43(1):59–74. [Google Scholar]
- 34. Bell A, Jones K. Explaining fixed effects: random effects modeling of time-series cross-sectional and panel data. Pol Sci Res Meth. 2015;3(1):133–153. [Google Scholar]
- 35. Young GJ, Flaherty S, Zepeda ED, Singh S, Rosenbaum S. Impact of ACA Medicaid expansion on hospitals’ financial status. J Healthc Manag. 2019;64(2):91–102. [DOI] [PubMed] [Google Scholar]
- 36. Garrett AB, Gangopadhyaya A. Who Gained Health Insurance Coverage Under the ACA, and Where Do They Live? Washington, DC: Urban Institute; 2016. http://www.urban.org/sites/default/files/publication/86761/2001041-who-gained-health-insurance-coverage-under-the-aca-and-where-do-they-live.pdf. Accessed June 9, 2020. [Google Scholar]
- 37. Tsao H, Olazagasti JM, Cordoro KM, et al. ; American Academy of Dermatology Ad Hoc Task Force for the ABCDEs of Melanoma. Early detection of melanoma: reviewing the ABCDEs. J Am Acad Dermatol. 2015;72(4):717–723. [DOI] [PubMed] [Google Scholar]
- 38.World Health Organization (WHO). Guide to cancer early diagnosis. Geneva, Switzerland: World Health Organization. https://www.who.int/cancer/publications/cancer_early_diagnosis/en/. Accessed May 1, 2020. [Google Scholar]
- 39.American Cancer Society. Cancer facts and figures 2019. Atlanta, GA: American Cancer Society. 2019. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2019/cancer-facts-and-figures-2019.pdf. Accessed December 2, 2019.
- 40. Goldman AL, Sommers BD. Among low-income adults enrolled in Medicaid, churning decreased after the affordable care act: this study examines whether the Affordable Care Act’s expansion of Medicaid eligibility had an impact on coverage disruptions-known as “churning”-among Medicaid enrollees. Health Aff (Millwood). 2020;39(1):85–93. [DOI] [PubMed] [Google Scholar]
- 41. Yabroff KR, Reeder-Hayes K, Zhao J, et al. Health insurance coverage disruptions and cancer care and outcomes: systematic review of published research. J Natl Cancer Inst. 2020;112(7):671–687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Zhao J, Han X, Nogueira L, Zheng Z, Jemal A, Yabroff KR. Health insurance coverage disruptions and access to care and affordability among cancer survivors in the United States. Cancer Epidemiol Biomarkers Prev. 2020;29(11):2134–2140. [DOI] [PubMed] [Google Scholar]
- 43. Nonzee NJ, Ragas DM, Ha Luu T, et al. Delays in cancer care among low-income minorities despite access. J Womens Health (Larchmt). 2015;24(6):506–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Lazar M, Davenport L. Barriers to health care access for low income families: a review of literature. J Community Health Nurs. 2018;35(1):28–37. [DOI] [PubMed] [Google Scholar]
- 45. Mallin K, Browner A, Palis B, et al. Incident cases captured in the National Cancer Database compared with those in US population based central cancer registries in 2012-2014. Ann Surg Oncol. 2019;26(6):1604–1612. [DOI] [PubMed] [Google Scholar]
- 46.46. Surveillance, Epidemiology, and End Results (SEER) Program. SEERStat Database: Incidence - SEER 21 Regs Limited-Field Research Data + Hurricane Katrina Impacted Louisiana Cases, Nov 2018 Sub (2000-2016) <Katrina/Rita Population Adjustment> - Linked To County Attributes - Total U.S., 1969-2017 Counties. National Cancer Institute, DCCPS, Surveillance Research Program, released April 2019, based on the November 2018 submission. National Cancer Institute, DCCPS, Surveillance Research Program, Surveillance Systems Branch. http://www.seer.cancer.gov. Accessed June 10, 2020.
- 47. Chan JK, Gomez SL, O'Malley CD, Perkins CI, Clarke CA. Validity of cancer registry Medicaid status against enrollment files: implications for population-based studies of cancer outcomes. Med Care. 2006;44(10):952–955. [DOI] [PubMed] [Google Scholar]
- 48. Close AG, Dreyzin A, Miller KD, Seynnaeve BK, Rapkin LB. Adolescent and young adult oncology—past, present, and future. CA A Cancer J Clin. 2019;69(6):485–496. [DOI] [PubMed] [Google Scholar]
- 49. Nogueira LM, Chawla N, Han X, Jemal A, Yabroff KR. Patterns of coverage gains among young adult cancer patients following the Affordable Care Act. JNCI Cancer Spectrum. 2019;3(1):pkz001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Zhao J, Mao Z, Fedewa SA, et al. The Affordable Care Act and access to care across the cancer control continuum: a review at 10 years. CA A Cancer J Clin. 2020;70(3):165–117. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article were provided by the American College of Surgeons and accessed at the American Cancer Society by permission. The data cannot be shared publicly per the Data User Agreement. The National Cancer Database Participant User Files are available through application to investigators associated with the Commission on Cancer accredited cancer programs (https://www.facs.org/quality-programs/cancer/ncdb/puf).