Abstract
Background
Aboriginal Australians are reported to have a high burden of chronic airway diseases. However, prescribing patterns and related outcomes of airway directed inhaled pharmacotherapy, (short-acting beta agonists (SABA), short-acting muscarinic antagonists (SAMA), long-acting β-agonists (LABA), long-acting muscarinic antagonists (LAMA) and inhaled corticosteroids (ICS)) among Aboriginal Australian patients with chronic airway disease have been sparsely reported in the past.
Methods
A retrospective cohort study was conducted, using clinical, spirometry data, chest radiology, primary healthcare (PHC) presentations and hospital admission rates among Aboriginal patients identified to have been prescribed inhaled pharmacotherapy in remote and rural communities referred to the respiratory specialist service in the Top End, Northern Territory of Australia.
Results
Of the 372 identified active patients, 346 (93%) had inhaled pharmacotherapy prescribed (64% female, median age 57.7 years). ICS was the most common prescription (72% of the total cohort) and was recorded to be prescribed in 76% of patients with bronchiectasis, and 80% of patients with asthma or chronic obstructive pulmonary disease (COPD). Fifty-eight percent of patients had a respiratory hospital admission and 57% had a recorded PHC presentation for a respiratory issue during the study period, with a higher rate of hospital admissions among patients prescribed ICS compared with those on SAMA/SABA or LAMA/LABA without ICS (median rate (per person per year) 0.42 vs 0.21 and 0.21 (p=0.004). Regression models demonstrated that presence of COPD or bronchiectasis alongside ICS was associated with significantly increased hospitalisation rates (1.01 admissions/person/year (95% CI 0.15 to 1.87) and 0.71 admissions/person/year (95% CI 0.23 to 1.18) against patients without COPD/bronchiectasis, respectively).
Conclusions
This study demonstrates that among Aboriginal patients with chronic airway diseases, ICS is the most common inhaled pharmacotherapy prescribed. Although LAMA/LABA and concurrent ICS use may be appropriate among patients with asthma and COPD, the use of ICS may have detrimental effects among those with underlying bronchiectasis either in isolation or concurrent COPD and bronchiectasis, potentially leading to higher hospital admission rates.
Keywords: asthma, asthma pharmacology, Bronchiectasis, COPD pharmacology, imaging/CT MRI etc, inhaler devices, respiratory infection, respiratory measurement
WHAT IS ALREADY KNOWN ON THIS TOPIC
Inhaled pharmacotherapy is often used in the management of chronic airway diseases. However, despite overwhelming evidence in the literature to suggest chronic airway diseases are highly prevalent among the adult Aboriginal Australians, the prescribing pattern/practice and appropriateness is sparsely assessed in this population.
WHAT THIS STUDY ADDS
This study demonstrated that among a referred population, the majority of Aboriginal patients with chronic airway diseases are prescribed with inhaled pharmacotherapy—inhaled corticosteroids (ICS) being the most common. Patients prescribed with ICS containing inhaled pharmacotherapy had higher recurrent hospital admissions, particularly among those with underlying chronic obstructive pulmonary disease or bronchiectasis.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
ICS prescription is high, and in many cases appears inappropriate from the perspective of current guidelines, particularly concerning its use among patients with bronchiectasis. A more conservative approach should be adopted in prescription practice until prospective studies are undertaken among this population to assess safety and efficacy.
Introduction
Approximately one-third of Aboriginal Australians (Aboriginal Australian and Torres Strait Islander peoples) are diagnosed with a chronic respiratory condition, with chronic airways disease (asthma, chronic obstructive pulmonary disease (COPD) and bronchiectasis) reported to be the leading cause of morbidity and mortality in this population.1 In the Northern Territory (NT), Aboriginal Australians form 26% (approximately 60 000 people) of the overall NT population, which is the highest proportion compared with all other Australian states and territories.2 Moreover, 81% of Aboriginal people in the NT reside in remote/very remote geographic locations.2 3 Previous studies have demonstrated high rates of chronic airway diseases among NT Aboriginal people, in particular a higher burden of COPD, bronchiectasis and asthma.4 Concomitant presence of multiple respiratory conditions is also highly prevalent among NT Aboriginal people,5 specifically presence of combined COPD and bronchiectasis.6–8 Furthermore, lung function parameters are observed to be poorer among Aboriginal Australians,9–12 giving rise to considerable physical symptoms.13 In addition, hospital admission frequency/rates are reported to be much higher secondary to exacerbations of chronic airway diseases among Aboriginal Australians compared with non-Aboriginal Australians in the NT.14
Nonetheless, airway directed inhaled pharmacotherapy such as short-acting beta agonists (SABA), short-acting muscarinic antagonists (SAMA), long-acting β-agonists (LABA), long-acting muscarinic antagonists (LAMA) and inhaled corticosteroids (ICS)15 is often used/prescribed/recommended to improve symptoms, lung function parameters, reduce exacerbations and prevent hospitalisation among patients with chronic airway diseases. There are guidelines that have been established to direct appropriate prescription of inhaled pharmacotherapy, especially among patients with COPD and asthma.16 17 In the Australian context, the COPD-X Concise Guide is a widely adopted and recommended tool in the stepwise management of COPD, including use of inhaled pharmacotherapy.18–21 However, the majority of these recommendations and guidelines are drawn from studies based on non-Aboriginal/Indigenous populations and it is reasonable to speculate whether these recommendations and guidelines are applicable to Aboriginal Australians. Additionally, among patients residing in rural and remote locations, the majority of chronic medical conditions are managed at the primary healthcare (PHC) level. These services are usually provided through a remote health centre, with a nurse-based model of care supported by Aboriginal Health Practitioners and through visiting primary/medical specialists. There is often limited access to medical officers and virtually no direct access to pharmacists.22
Currently, there is sparse evidence in the literature assessing either the safety or efficacy of inhaled pharmacotherapy, or the prescribing patterns and related outcomes in the Aboriginal Australian population.23 Therefore, the aim of this retrospective study is to evaluate and to describe the clinical parameters, demographics, spirometry data, chest radiology, PHC utilisation and hospital admission frequency of Aboriginal Australians prescribed with inhaled pharmacotherapy residing in the rural and remote regions of the Top End Health Service (TEHS) region of the NT of Australia.
Methods
Setting, study participants and ethics
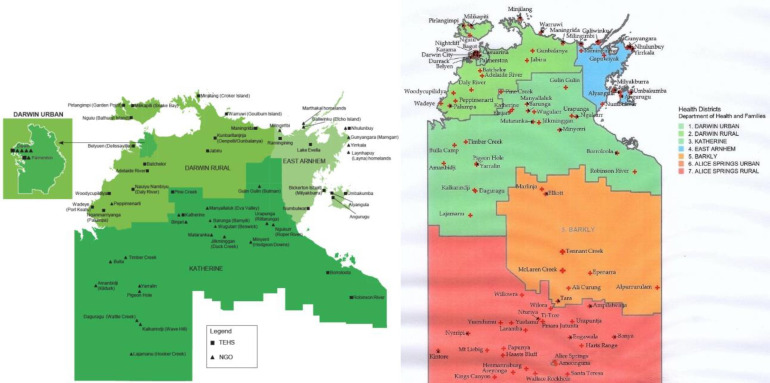
This retrospective cohort study was conducted at the respiratory and sleep service based at the Royal Darwin hospital (RDH) and Darwin Respiratory and sleep health (DRSH) at the Darwin private hospital in the TEHS region of the NT of Australia. The Top End region covers approximately 35% or 4 75 338 km2 of the total area of the NT, with an estimated population of 195 000 people representing 79% of the total NT population2 24 (figure 1). The study participants were Aboriginal patients residing in remote and regional Aboriginal communities referred to the respiratory and sleep outreach service by primary health practitioners and other health practitioners.4 The respiratory and sleep service at the Top End, NT has visited an average of 20 remote Aboriginal communities approximately 2–3 times a year since 2010, as a part of the respiratory outreach service in the TEHS region (prior to COVID-19 lockdown).4 9 Patients referred to the respiratory outreach service were identified through the database maintained by the respiratory and sleep outreach team at RDH. Patients included for this study were inclusive of only those patients identified to be currently marked as ‘active patients’ as per the updated outreach records at the end of 2020, or marked as ‘active’ at time of death if deceased prior to 2020.
Figure 1.
Top end health service map (TEHS), Northern Territory, Australia. Source: Department of Health—Innovation and Research—2018. Chondur R. Health Gains Planning. Department of Health and planning 2009.
The authors acknowledge the rights of Aboriginal people involved in this study, and as such conducted and reported according to strengthening and reporting of health research involving Aboriginal people.25
Patient and public involvement
As the study was retrospective in nature, patients’ participation or individual consent from the study participants was not required and the need for consent was waived by the research committee. In the public involvement perspective, Mr Izaak Thomas (Australian Aboriginal Luritja descendent) reviewed the study for its design, conduct, reporting, dissemination of our research work, in particular, the appropriateness and respect in relation to the Aboriginal context represented in this study.
Demographic, clinical, lung function and radiology data
Patients’ demographics, self-identified Aboriginal status and usual residence location according to post code were collected through hospital electronic medical records (EMRs). Patients’ EMRs were meticulously reviewed to extract information on the physician’s clinical diagnosis/documentation for the presence of chronic respiratory diseases, restricted to COPD bronchiectasis and asthma. When available, in order to confirm the presence/pattern and severity of airway disease, results of spirometry parameters; forced vital capacity (FVC), forced expiratory volume in one second (FEV1), FEV1/FVC ratio, including lower limit of normal (LLN) values were collected.
Spirometry parameters were assessed for presence of restrictive impairment (prebronchodilator (BD), FVC<LLN and post-BD FEV1/FVC≥0.7), mixed impairment (post-BD FEV1/FVC<0.7 and pre-BD FVC<LLN) or airflow obstruction (AO) (post-BD FEV1/FVC<0.717 26). For the presence of significant BD response (BDR), both traditional (BDRT)16 17 27 and updated (BDRU) American thoracic society/European respiratory society criteria (BDRT, BDRU) (change of ≥12% and ≥200 mL on FVC or FEV1 pre-BD to post-BD or change ≥10%, respectively) were used.28 Severity of AO was graded as per Global Initiative for Chronic Obstructive Lung Disease (GOLD) criteria.17 Information on height, weight and body mass index (BMI) was recorded while patients were undergoing spirometry testing. If patients were observed to have undergone multiple spirometry tests during this study period, the earliest test acceptable and reproducible for session quality were used to assess spirometry impairments. Radiology reports were assessed for evidence of COPD and bronchiectasis.29 30 In the case of discrepancy between the EMR and chest radiology for presence of COPD or bronchiectasis, results from chest radiology were taken in preference. In the case of patients having both CT and chest X-ray (CXR) recorded, results of CT were taken in preference to CXR. The following airway diagnosis criteria was applied:
COPD was defined when chest radiology demonstrated evidence of; emphysema, bullous disease or bronchial/bronchiolar inflammation or thickening 29 or in the absence of imaging, physicians clinical EMR documentation of COPD.
Bronchiectasis was defined when chest radiology demonstrated evidence of bronchiectasis30 or in the absence of imaging, physicians clinical EMR documentation of bronchiectasis.
Asthma or ‘potential asthma’ was defined when physicians clinical EMR documented asthma and/or spirometry demonstrated presence of significant BDRT.16
Inhaled pharmacotherapy data
All available EMRs were searched to document the details of any type or combination of airway directed inhaled pharmacotherapy prescribed, more specifically—SABA (salbutamol); SAMA (ipratropium); LABA (formaterol, indacaterol, olodaterol, salmeterol, vilanterol); LAMA (aclidinium, glycopyronium, tiotropium, umeclidinium) and ICS (beclomethasone, budesonide, fluticasone). If the patients were identified to have been prescribed multiple/change in similar class of inhaled pharmacotherapy during the study period, the most recent/last prescribed type of therapy was included in the analysis. Patients inhaled pharmacotherapy use was defined as:
SAMA/SABA with no recording of either LAMA/LABA or ICS.
LAMA/LABA with or without SAMA/SABA and without ICS.
Any use of ICS.
PHC utilisation and hospital admission data
Hospital admissions data were extracted via the electronic hospital information system using International Classification of Diseases (ICD) code specifically for chronic respiratory admissions (asthma, bronchiectasis or COPD, ICD codes J44–47). When assessable and available all respiratory related remote and rural community PHC presentations were also extracted through the hospital electronic information systems using international classification of primary care codes (PHC presentation data were not available for all patients). An end date of hospital/PHC presentation data collection was set at 1 January 2020 in order to avoid the potential influence of local COVID-19-related measures on hospital and PHC presentations, aside from patients who were deceased prior to this, in which case the end date of hospital collection was set at date of death. From this final date a retrospective 10-year window was applied, excluding all presentations outside of this window. Hospital admissions and PHC presentation data was reported in the following three manners:
A binary variable detailing if the patient ever had a hospital admission/PHC presentation during the 10-year window.
As the total number of hospital admissions/PHC presentations during the 10-year window per patient.
As the rate of hospital admissions/PHC presentations per year per person (calculated as number of presentations divided by the length of time (in years) from the patients first presentation to the collection end date (for this cohort median time between first presentation and the defined end date was 8.9 years (IQR 7.7–9.7)).
Statistical analysis
Demographic and clinical parameters including respiratory presentation rates were presented as medians (IQR), and categorical parameters presented as numbers (%). Presence of airway disease via EMRs, radiology or spirometry was compared between inhaler combinations (SAMA/SABA, LAMA/LABA or +ICS) via two-tailed χ2 test, using Fisher’s exact test in cases with cell counts <10. Differences in the proportion of patients with any respiratory presentation, PHC presentation or hospital admission between inhaler combinations were assessed via two-tailed χ2 tests. Total number of and rate of total respiratory presentations, hospital admissions and PHC presentations between inhaler combinations were tested via Kruskal-Wallis rank test. Univariate and multivariate logistic regression models were used to define the odds of having a hospital admission among patients on SAMA/SABA or LAMA/LABA compared with+ICS (used as the reference group), adjusting for age at the start of the 10-year window, sex, BMI and chronic airway diseases (asthma, bronchiectasis or COPD—in separate models) reporting results as ORs (95% CIs). Univariate and multivariate Poisson regression models were used to define hospital admission rates (number per person per year) among patients on SAMA/SABA or LAMA/LABA compared with +ICS (used as the reference group), using the same models as for the logistic regressions, reporting betas (95% CIs). A secondary subanalysis was conducted looking specifically at hospital admission rates for COPD with lower respiratory tract infection (ICD code J44.0), using the same logistic and Poisson regression models. In cases of patients missing any of the outcome or adjusting variables, they were dropped from the regression models. Alpha was set to p=0.05 throughout, and all analyses were conducted in STATA IC V.15.
Results
Clinical and demographic characteristics
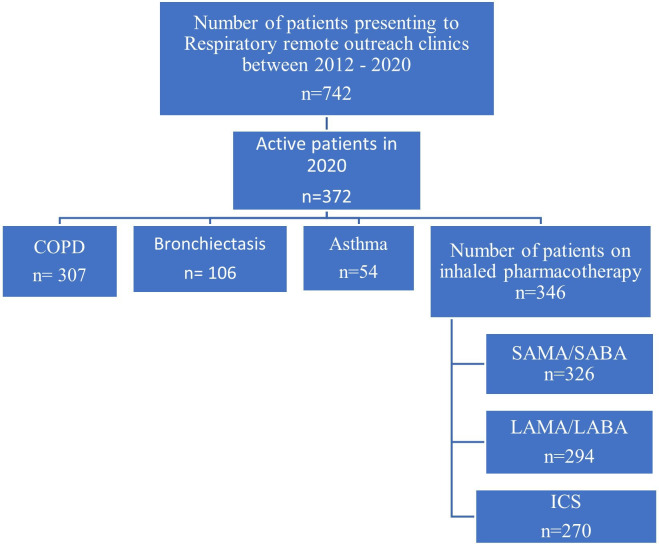
A total of 372 active Aboriginal patients were identified through the respiratory outreach database, of whom 346 (93%) had recorded current use of inhaled pharmacotherapy. The majority of patients were female (64%), with a BMI in the normal or underweight range (58%) and a high proportion reporting a history of smoking (92%). Physician EMR documentation for the presence of chronic airway disease was observed in 97% of the study participants (COPD, bronchiectasis and asthma 92%, 32%,16%, respectively) (table 1) (figure 2). Only a minority of patients were not recorded to have any form of chronic airway disease on EMR (3%, n=12), of whom six had spirometry and four did not show any spirometric impairment.
Table 1.
Patients’ clinical and demographic details
| Demographics | Clinical parameters | Patients (n=346) |
| Sex | Female | 223 (64%) |
| Age | Years* | 57.76 (50.95, 65.83) |
| Corpulence | Height (m) (n=271) | 1.64 (1.58, 1.7) |
| Weight (kg) (n=268) | 64.75 (52.7, 76) | |
| BMI (n=268) | 23.86 (19.95, 29.4) | |
| Underweight | 48 (18%) | |
| Normal weight | 107 (40%) | |
| Overweight | 52 (19%) | |
| Obese | 61 (23%) | |
| Smoking | Ever smoker | 314 (92%) |
| Pack years (n=91) | 20 (8, 33.75) | |
| Spirometry | Had PFT | 283 (82%) |
| Restrictive impairment (n=272) | 89 (33%) | |
| Airway obstruction | 183 (65%) | |
| Mixed impairment (n=272) | 165 (58%) | |
| BDRT (n=227) | 55 (24%) | |
| BDRU (n=227) | 101 (44%) | |
| Comorbidities recorded on EMR | Any chronic airway disease | 334 (97%) |
| COPD | 307 (92%) | |
| Bronchiectasis | 106 (32%) | |
| Asthma | 54 (16%) | |
| Radiology | Had radiology report available | 335 (97%) |
| COPD | 96 (29%) | |
| Bronchiectasis | 44 (13%) | |
| COPD and bronchiectasis | 46 (14%) | |
| No COPD and no bronchiectasis | 149 (44%) | |
| Healthcare data | Any respiratory presentation | 288 (83%) |
| PHC respiratory presentation | 198 (57%) | |
| Hospital respiratory admission | 201 (58%) | |
| Mortality | 28 (8%) |
Data displayed as n (%) or median (IQR).
Underweight: BMI <18.5 kg/m2.
Normal weight: BMI 18.5 to <25 kg/m2.
Overweight: BMI 25 to <30 kg/m2.
Obese: BMI ≥30 kg/m2.
*Current age defined as age at data collection.
BDRT, traditional bronchodilator response criteria; BDRU, updated BDR; BMI, body mass index; COPD, chronic obstructive pulmonary disease; EMR, electronic medical record; PFT, pulmonary function test; PHC, primary healthcare.
Figure 2.
Flow diagram of patient inclusion in study. COPD, chronic obstructive pulmonary disease; ICS, inhaled corticosteroid; LABA, long-acting β-agonist; LAMA, long-acting muscarinic antagonist; SABA, short-acting beta agonist; SAMA, short-acting muscarinic antagonist.
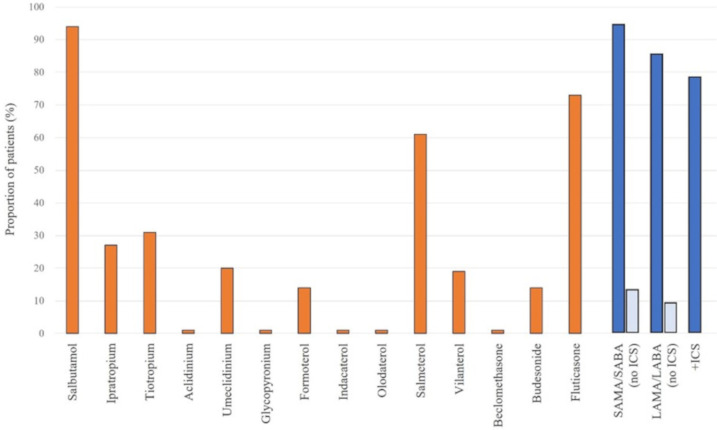
Inhaled pharmacotherapy prescription data
Of the 346 patients with an inhaled pharmacotherapy prescription recorded, 326/346 (94%) had SAMA/SABA recorded, and 45/346 (13%) had only either SAMA or SABA recorded, 294/346 (85%) had LAMA/LABA recorded and 31/346 (9%) had only either LAMA or LABA or a combination of LAMA/LABA+SAMA/SABA recorded, and 270/346 (78%) had ICS recorded (figure 3).
Figure 3.
Proportion of patients with individual pharmacotherapy prescriptions, and those grouped by SAMA/SABA, LAMA/LABA or+ICS. ICS, inhaled corticosteroid; LABA, long-acting β-agonist; LAMA, long-acting muscarinic antagonist; SABA, short-acting beta agonist; SAMA, short-acting muscarinic antagonist.
Inhaled pharmacotherapy use as per EMR and chest radiology
COPD was the most common respiratory comorbidity recorded for each of SAMA/SABA, LAMA/LABA and +ICS patients (71% (32/45), 90% (28/31) and 92% (247/270) respectively, Fisher’s exact test p=0.001) (table 2). The majority of patients prescribed LAMA/LABA alone had only COPD listed in their EMRs (71%, 22/31) compared with SAMA/SABA or+ICS patients (51 (23/45) and 50% (136/270), respectively). A greater proportion of+ICS patients, however, had COPD and bronchiectasis listed compared with SAMA/SABA or LAMA/LABA patients (28% (76/270) vs 13% (6/45) and 16% (5/31), respectively).
Table 2.
Inhaler prescriptions by comorbidity as recorded on electronic medical records, or as identified on radiology
| Clinical parameters | SAMA/SABA | LAMA/LABA | +ICS | P value |
| Electronic medical record of airway disease (n=334) | ||||
| Any COPD (n=307) | 32/45 (71%) | 28/31 (90%) | 247/270 (92%) | 0.001* |
| Any bronchiectasis (n=106) | 11/45 (24%) | 7/31 (23%) | 88/270 (33%) | 0.364 |
| Any asthma (n=54) | 7/45 (16%) | 1/31 (3%) | 46/270 (17%) | 0.122 |
| Comorbidity breakdown | ||||
| COPD (alone) (n=181) | 23/45 (51%) | 22/31 (71%) | 136/270 (50%) | 0.008* |
| COPD+bronchiectasis (n=87) | 6/45 (13%) | 5/31 (16%) | 76/270 (28%) | |
| COPD+asthma (n=34) | 3/45 (7%) | 1/31 (3%) | 30/270 (11%) | |
| Bronchiectasis (alone) (n=12) | 4/45 (9%) | 2/31 (7%) | 6/270 (2%) | |
| Bronchiectasis+asthma (n=2) | 1/45 (2%) | 0/31 (0%) | 1/270 (0%) | |
| Asthma (alone) (n=13) | 3/45 (7%) | 0/31 (0%) | 10/270 (4%) | |
| COPD+bronchiectasis+asthma (n=5) | 0/45 (0%) | 0/31 (0%) | 5/270 (2%) | |
| Clinical comorbidities not recorded (n=12) | 5/45 (11%) | 1/31 (3%) | 6/270 (2%) | |
| Radiology (n=335) | ||||
| Any bronchiectasis (n=90) | 11/38 (29%) | 10/30 (33%) | 69/267 (26%) | 0.587 |
| Any COPD (n=142) | 12/38 (32%) | 12/30 (40%) | 118/267 (44%) | 0.328 |
| Bronchiectasis (alone) (n=44) | 6/38 (16%) | 5/30 (17%) | 33/267 (12%) | 0.693 |
| COPD (alone) (n=96) | 7/38 (18%) | 7/30 (23%) | 82/267 (31%) | |
| COPD+Bronchiectasis (n=46) | 5/38 (13%) | 5/30 (17%) | 36/267 (14%) | |
| No COPD or Bronchiectasis (n=149) | 20/38 (53%) | 13/30 (43%) | 116/267 (44%) | |
P value obtained via χ2 or Fisher’s exact test (cases where cells values were <10).
*p<0.05.
COPD, chronic obstructive pulmonary disease; ICS, inhaled corticosteroids; LABA, long-acting β-agonists; LAMA, long-acting muscarinic antagonists; SABA, short-acting bronchodilator; SAMA, short-acting muscarinic antagonists.
Radiology reports were available for 335 patients to determine radiological evidence of airway diseases. COPD was the most common, recorded in 142/335 (42%), with 90/335 (27%) showing bronchiectasis and 46/335 (14%) recording concurrent COPD and bronchiectasis (table 1). Of the 44 patients with isolated bronchiectasis on radiology, the majority (75%, 33/44) had a recorded prescription of+ICS, while among patients with isolated bronchiectasis on EMR (n=12), half (50%, 6/12) had recorded use of+ICS (table 2). This proportion rose to 87% among patients with bronchiectasis plus COPD via EMR (76/87), 50% in plus asthma via EMR (1/2) and 100% in patients with all three present via EMR (5/5). Among patients with radiologically defined bronchiectasis plus COPD the proportion was 78% (36/46). Of the 96 patients with radiologically defined isolated COPD, the majority (85%, 82/96) recorded use of+ICS, as did the majority (75%, 136/181) of those with isolated COPD on EMR.
Inhaled pharmacotherapy use as per pulmonary function test results
The majority of patients (n=283/346, 82%) had spirometry recorded, though 44/283 (16%) did not have post-BD spirometry to assess for AO or BDR, and an additional 12 (total 56/283) were missing percent predicted and percentage change values. However, among the 239 who had both pre-BD and post-BD spirometry values available, there was no significant difference in pre to post values for FEV1/FVC (0.634 (95% CI 0.615 to 0.653) vs 0.636 (95% CI 0.617 to 0.655), p=0.569), therefore pre-BD FEV1/FVC was used for AO in these 44 patients. AOs were common, noted in two-thirds of patients (65%, 183/283), though these often occurred alongside an FVC below the LLN resulting in a mixed impairment (58%, 165/283) (table 3). Only 3% (8/283) of the cohort did not show any evidence of spirometric impairment. A greater proportion of patients with mixed impairment were prescribed with+ICS (85%, 140/165) compared with those with a restrictive impairment (78%, 69/89). A greater proportion of patients with a SAMA/SABA prescription showed no significant impairments on spirometry compared with LAMA/LABA or+ICS (14% (4/29) vs 0 (0/27) and 2% (4/227), respectively (Fisher’s exact p=0.014). A greater proportion of patients with+ICS who showed airway obstruction were at GOLD stages III or IV (88%, 128/146), compared with patients with SAMA/SABA (77%, 10/13) or LAMA/LABA (60%, 9/15). Presence of BDR ‘potential asthma’ was observed in 55 patients (23%, 55/227) on spirometry, with the majority of these patients (80%, 44/55) observed to have a+ICS prescription.
Table 3.
Inhaler prescriptions by spirometry result
| Spirometry and COPD stages | SAMA/SABA | LAMA/LABA | +ICS | P value |
| Restrictive impairment (n=89) | 11/28 (39%) | 9/24 (38%) | 69/220 (31%) | 0.577 |
| +BDR (n=9) | 0/25 (0%) | 2/22 (9%) | 7/180 (4%) | 0.202 |
| Airway obstruction (n=183) | 14/29 (48%) | 17/27 (63%) | 152/227 (67%) | 0.138 |
| +BDR (n=46) | 4/25 (16%) | 5/22 (23%) | 37/180 (21%) | 0.871 |
| Mixed impairment (n=165) | 12/28 (43%) | 13/24 (54%) | 140/220 (64%) | 0.077 |
| +BDR (n=46) | 4/25 (16%) | 5/22 (23%) | 37/180 (21%) | 0.871 |
| BDR (total) (n=55) | 4/25 (16%) | 7/22 (32%) | 44/180 (24%) | 0.440 |
| Any impairment (n=275) | 25/29 (86%) | 27/27 (100%) | 223/227 (98%) | 0.014* |
| GOLD | ||||
| GOLD I (n=2) | 0/13 (0%) | 1/15 (7%) | 1/146 (1%) | 0.085 |
| GOLD II (n=25) | 3/13 (23%) | 5/15 (33%) | 17/146 (12%) | |
| GOLD III (n=92) | 7/13 (54%) | 5/15 (33%) | 80/146 (55%) | |
| GOLD IV (n=55) | 3/13 (23%) | 4/15 (27%) | 48/146 (33%) | |
| COPD-X | ||||
| NA (FEV1>80%) (n=11) | 1/14 (7%) | 3/17 (18%) | 7/152 (5%) | 0.114 |
| Mild (n=12) | 1/14 (7%) | 3/17 (18%) | 8/152 (5%) | |
| Moderate (n=57) | 5/14 (36%) | 4/17 (24%) | 48/152 (32%) | |
| Severe (n=103) | 7/14 (50%) | 7/17 (41%) | 89/152 (59%) |
GOLD stages.
0—FEV1/FVC post-BD ≥0.7.
I—FEV1/FVC post-BD <0.7 and FEV1 post-BD (% predicted) ≥80%.
II—FEV1/FVC post-BD <0.7 and FEV1 post-BD (% predicted) ≥50% and <80%.
III—FEV1/FVC post-BD <0.7 and FEV1 post-BD (% predicted) ≥30% and <50%.
IV—FEV1/FVC post-BD <0.7 and FEV1 post-BD (% predicted) <30%.
Denominators in the above table show the number of SAMA/SABA, LAMA/LABA or +ICS patients with information available to categorise into each spirometry impairment category.
P value obtained via χ2 or Fisher’s exact test (cases where cells values were <10).
*p<0.05.
†In the absence of post- BD values, pre-BD values were used.
BD, bronchodilator; BDR, BD response; COPD-X, Australian concise tool for chronic obstructive pulmonary disease; FEV1, forced expiratory volume in 1 s; FVC, forced vital capacity; GOLD, Global Initiative for Chronic Obstructive Lung Disease; ICS, inhaled corticosteroids; LABA, long-acting β-agonists; LAMA, long-acting muscarinic antagonists; NA, not available; SABA, short-acting bronchodilator; SAMA, short-acting muscarinic antagonists.
Inhaled pharmacotherapy prescription with bronchiectasis
A further analysis was undertaken to understand the pattern of inhaler prescription for the 142 patients with a diagnosis of bronchiectasis (either in EMR or via radiology) (table 4). Among patients with a diagnosis of bronchiectasis, 76% (108/142) had a prescription for +ICS. Breaking it down further, to exclude patients with other potential comorbidities, 29/142 (20%) did not have any evidence of AO, asthma or COPD on radiology. Of these 29 patients, 21 (72%) recorded+ICS prescription. Of the five patients with no evidence of asthma, AO, or COPD via any of spirometry, radiology or recorded in patients’ EMRs, all had a prescription for+ICS. The rate of+ICS prescription among patients with bronchiectasis was comparable to patients with evidence of asthma (78/97) or COPD (249/313) (80% each).
Table 4.
Inhaler use according to underlying airway disease (bronchiectasis)
| Airway disease | SAMA/SABA | LAMA/LABA | +ICS |
| Bronchiectasis specific patients | |||
| Bronchiectasis (radiology or EMR) (n=142) | 22/142 (16%) | 12/142 (8%) | 108/142 (76%) |
| Bronchiectasis (radiology or EMR) with no asthma/BDR (n=124) | 19/124 (15%) | 11/124 (9%) | 94/124 (76%) |
| Bronchiectasis (radiology or EMR) with no asthma/BDR and no airway obstruction (n=31) | 5/31 (16%) | 3/31 (10%) | 23/31 (74%) |
| Bronchiectasis (radiology or EMR) with no asthma/BDR and no airway obstruction and no COPD (radiology) (n=29) | 5/29 (17%) | 3/29 (10%) | 21/29 (72%) |
| Bronchiectasis (radiology or EMR) with no asthma/BDR and no airway obstruction and no COPD (any) (n=5) | 0/5 (0%) | 0/5 (0%) | 5/5 (100%) |
| Total cohort of patients | |||
| Asthma (EMR or BDR on PFT) (n=97) | 11/97 (12%) | 8/97 (8%) | 78/97 (80%) |
| COPD (radiology or EMR) (n=313) | 36/313 (12%) | 28/313 (9%) | 249/313 (80%) |
BDR, bronchodilator response; COPD, chronic obstructive pulmonary disease; EMR, electronic medical record; GOLD, Global Initiative for Chronic Obstructive Lung Disease; ICS, inhaled corticosteroids; LABA, long-acting β-agonists; LAMA, long-acting muscarinic antagonists; PFT, pulmonary function test; SABA, short-acting bronchodilator; SAMA, short-acting muscarinic antagonists.
Inhaled pharmacotherapy prescription relationship to hospital admissions and PHC presentations
Healthcare presentations due to respiratory conditions were common, with 83% (288/346) of patients recording at least one presentation (either PHC or hospital). Hospital admissions were recorded in 58% (201/346) (table 5). Respiratory hospital admissions were significantly more common among patients using +ICS, with 62% (167/270) having at least one hospital admission compared with 52% (16/31) of LAMA/LABA and 40% (18/45) of SAMA/SABA (p=0.017). The total number of presentations was additionally significantly greater among the +ICS group with a median 3 hospital admissions per patient compared with 2 for SAMA/SABA and LAMA/LABA. Furthermore, the median rate of presentations (/person/year) among patients who presented at least once was twice as high among the+ICS group compared with the SAMA/SABA or LAMA/LABA groups (p=0.004). The total number of patients deceased in the ICS group was higher compared with SAMA/SABA or LAMA/LABA groups (n=22/270 (8%) vs n=2/45 (4%) and n=4/31 (13%), respectively). However, with low numbers (<5) in the SAMA/SABA or LAMA/LABA group compared with ICS group, the statistical power is low.
Table 5.
Presentations to PHC or hospital admissions secondary to exacerbation of airway disease or lower respiratory tract infections
| Hospital and PHC presentation | SAMA/SABA (n=45) | LAMA/LABA (n=31) | +ICS (n=270) |
P value |
| Any respiratory presentation | 29 (64%) | 25 (81%) | 234 (87%) | 0.002* |
| Total number of respiratory presentations | 2 (1, 3) (1, 24) | 2 (1, 2) (1, 6) | 3 (2, 7) (1, 74) | <0.001* |
| Total presentation rate | 0.22 (0.13, 0.35) | 0.22 (0.13, 0.34) | 0.4 (0.21, 0.73) | <0.001* |
| Any respiratory presentation to hospital | 18 (40%) | 16 (52%) | 167 (62%) | 0.017* |
| Total no of respiratory presentations to hospital | 2 (1, 3) (1, 25) | 2 (1, 2) (1, 5) | 3 (2, 7) (1, 74) | 0.001* |
| Hospital presentation rate | 0.21 (0.13, 0.51) | 0.21 (0.12, 0.28) | 0.42 (0.21, 0.78) | 0.004* |
| Any respiratory presentation to PHC | 20 (44%) | 15 (48%) | 163 (60%) | 0.079 |
| Total no of respiratory presentations to PHC | 1 (1, 2) (1, 3) | 2 (1, 2) (1, 2) | 2 (1, 2) (1, 8) | 0.141 |
| PHC presentation rate | 0.14 (0.11, 0.21) | 0.2 (0.11, 0.23) | 0.2 (0.12, 0.27) | 0.428 |
| Mortality | 2 (4%) | 4 (13%) | 22 (8%) | 0.399 |
Parameters displayed as number (%), median (IQR) (minimum, maximum).
P value obtained via χ2 or Fisher’s exact test (cases where cells values were <10) for categorical parameters, Kruskal-Wallis rank test for continuous parameters.
*p<0.05.
ICS, inhaled corticosteroids; LABA, long-acting β-agonists; LAMA, long-acting muscarinic antagonists; PHC, primary health centre; SABA, short-acting bronchodilator; SAMA, short-acting muscarinic antagonists.
Regression analyses for respiratory healthcare presentations/utilisation
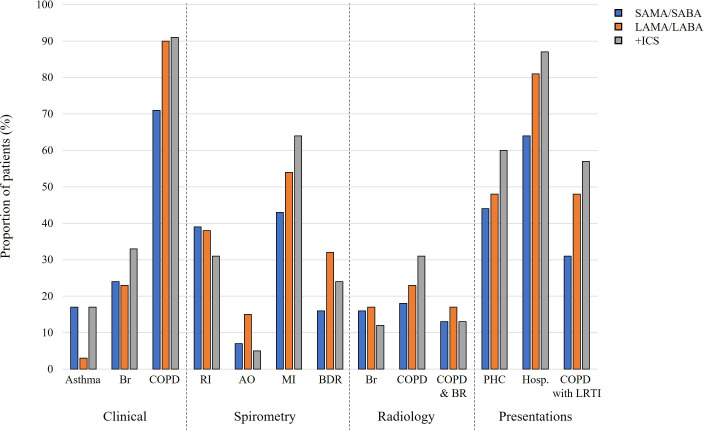
In logistic regression models, the odds of having a hospital admission (any of ICD J44-J47) were significantly reduced among patients who were prescribed only SAMA/SABA compared with+ICS, with no significant difference between LAMA/LABA and+ICS (table 6). However, the rate of hospital admissions was significantly reduced among patients on LAMA/LABA compared with+ICS in all adjusted models. In the respiratory disease adjusted models (models A, B and C (models as detailed under table 6)), there was a difference in the effect of the presence of each disease. Presence of asthma did not significantly change the hospitalisation rate (−0.34 (95% CI −0.8 to 0.12)), while presence of bronchiectasis (0.71 (95% CI 0.23 to 1.18)) or presence of COPD (1.01 (95% CI 0.15 to 1.88)) were associated with significantly increased hospitalisation rates. When the model was refined to only COPD admissions with a lower respiratory tract infection (ICD-J44.0), the results remained the same, with patients on+ICS recording a significantly greater rate of hospital admissions than those on LAMA/LABA without ICS. Figure 4 illustrates the inhaled pharmacotherapy prescribing patterns as per clinical, spirometry, radiology, including hospital and PHC presentations.
Table 6.
Logistic and Poisson regression models exploring the effect of inhaler prescription on odds of healthcare presentation and rate of presentations, using patients on +ICS as baseline
| SAMA/SABA | P value | LAMA/LABA | P value | +ICS | |
| Total respiratory hospital admissions (ICD J44–J47) | |||||
| Logistic | |||||
| Model 1 (n=346) | 0.41 (0.22, 0.78) | 0.007* | 0.66 (0.31, 1.39) | 0.271 | Reference |
| Model 2 (n=268) | 0.47 (0.21, 1.04) | 0.064 | 0.53 (0.22, 1.27) | 0.153 | |
| Model 2 A (n=268) | 0.46 (0.2, 1.03) | 0.057 | 0.53 (0.22, 1.23) | 0.154 | |
| Model 2 B (n=268) | 0.43 (0.19, 0.98) | 0.043* | 0.57 (0.23, 1.39) | 0.217 | |
| Model 2 C (n=268) | 0.46 (0.20, 1.04) | 0.063 | 0.52 (0.21, 1.25) | 0.144 | |
| Poisson (rate) | |||||
| Model 1 (n=201) | −0.57 (−1.25, 0.12) | 0.105 | −0.93 (−1.42, –0.45) | <0.001* | Reference |
| Model 2 (n=157) | −0.43 (−1.27, 0.41) | 0.314 | −0.77 (−1.35, –0.19) | 0.010* | |
| Model 2 A (n=157) | −0.45 (−1.33, 0.44) | 0.323 | −0.79 (−1.37, –0.21) | 0.008* | |
| Model 2 B (n=157) | −0.38 (−1.24, 0.48) | 0.382 | −0.74 (−1.33, –0.16) | 0.013* | |
| Model 2 C (n=157) | −0.48 (−1.32, 0.35) | 0.258 | −0. 8 (−1.4 to –0.2) | 0.009* | |
| COPD with LRTI hospital admission (ICD J44.0) | |||||
| Logistic | |||||
| Model 1 (n=346) | 0.34 (0.17, 0.66) | 0.002* | 0.7 (0.33, 1.47) | 0.339 | Reference |
| Model 2 (n=268) | 0.46 (0.2, 1.05) | 0.066 | 0.61 (0.25, 1.47) | 0.271 | |
| Model 2 A (n=268) | 0.45 (0.2, 1.04) | 0.061 | 0.61 (0.25, 1.48) | 0.272 | |
| Model 2 B (n=268) | 0.42 (0.18, 0.98) | 0.043* | 0.67 (0.27, 1.65) | 0.383 | |
| Model 2 C (n=268) | 0.45 (0.19, 1.06) | 0.068 | 0.59 (0.24, 1.45) | 0.252 | |
| Poisson (Rate) | |||||
| Model 1 (n=184) | −0.61 (−1.11, –0.11) | 0.016* | −0.81 (−1.35, –0.27) | 0.003* | Reference |
| Model 2 (n=143) | −0.53 (−1.15, 0.09) | 0.096 | −0.59 (−1.15, –0.02) | 0.042* | |
| Model 2 A (n=143) | −0.51 (−1.14, 0.13) | 0.117 | −0.62 (−1.19, –0.05) | 0.034* | |
| Model 2 B (n=143) | −0.52 (−1.14, 0.11) | 0.105 | −0.55 (−1.1, 0) | 0.050* | |
| Model 2 C (n=143) | −0.53 (−1.15, 0.09) | 0.094 | −0.59 (−1.16, –0.03) | 0.039 | |
Model 1—Univariate logistic or Poisson regression model showing the effect of inhaler prescriptions against the reference group of patients using +ICS.
Model 2—Model 1 additionally adjusted for age, sex and BMI.
Model 2 A/B/C—Model 2 additionally adjusted for asthma, bronchiectasis or COPD respectively.
Note that observations with high absolute residuals are dropped from the robust regression.
*p-value <0.05.
BMI, body mass index; COPD, chronic obstructive pulmonary disease; ICD, international classification of disease; ICS, inhaled corticosteroids; LABA, long-acting β-agonists; LAMA, long-acting muscarinic antagonists; LRTI, lower respiratory tract infection; SABA, short-acting bronchodilator; SAMA, short-acting muscarinic antagonists.
Figure 4.
Clinical factors and outcomes of patients by inhaler prescription. AO, airflow obstruction; BDR, bronchodilator response; Br, bronchiectasis; COPD, chronic obstructive pulmonary disease; +ICS, plus inhaled corticosteroids; MI, mixed impairment; PHC, primary healthcare; RI, restrictive impairment; LABA, long-acting β-agonists; LAMA, long-acting muscarinic antagonists; LRTI, lower respiratory tract infection; SABA, short-acting bronchodilators; SAMA, short-acting muscarinic antagonists.
Discussion
To the best of the authors’ knowledge, this is the first study that used clinical, spirometry and radiology data to comprehensively assess the prescribing pattern of inhaled pharmacotherapy and its related outcomes in an Aboriginal Australian population with chronic airway disease. This study highlights several key findings:
Almost 93% of remote residing Aboriginal patients with chronic respiratory conditions who were referred to the respiratory and sleep outreach service were noted to have been prescribed with one form or another airway directed inhaled pharmacotherapy.
ICS containing inhaled pharmacotherapy was by far the most frequently prescribed inhaled pharmacotherapy.
COPD was the most common condition recorded among study patients prescribed with inhaled pharmacotherapy, with the majority being prescribed LAMA or LABA either alone or in conjunction with ICS.
Irrespective of what impairment was observed on spirometry, ICS containing inhaled pharmacotherapy prescription is the most common.
ICS was observed to be prescribed in up to 76% of patients with bronchiectasis.
Patients with a prescription of ICS showed almost double the hospital admission rate, especially with COPD or bronchiectasis compared with asthma.
ICS prescription was also significantly associated with increased hospital admission rates secondary to lower respiratory tract infections.
Despite overwhelming evidence in the literature to indicate that chronic airway diseases are highly prevalent among Aboriginal/Indigenous people, not only among Aboriginal Australians,4–8 but also among other Indigenous people globally,31–36 there is little evidence in the literature examining the efficacy, safety or prescribing patterns and related outcomes of inhaled pharmacotherapy. Hence, the current study addresses this gap in knowledge and could be viewed as an invaluable addition to the literature.
In this study, we observed that COPD was the most common condition among patients being prescribed inhaled pharmacotherapy. This is not surprising though, as it reflects the high prevalence of COPD in the remote residing NT Aboriginal population, as well as the high smoking rates (>90%) noted in the current and previous studies.4–6 While there is evidence to suggest either LAMA or LABA in combination or in isolation are beneficial in the management of patients with COPD,37–39 the use of ICS in the management of patients with COPD is controversial and continues to be debated.40–42 In our study, the majority of patients diagnosed with COPD were observed to be prescribed with LAMA/LABA containing inhaled pharmacotherapy, in line with the beneficial outcomes noted in previous reports.37–39 However, a significant proportion of patients with COPD were also noted to be prescribed with ICS.
Among patients presenting with chronic airway diseases, spirometry alongside other clinical parameters, including exacerbation frequency are often used in clinical decision making, including when considering inhaled pharmacotherapy in day-to-day clinical practice.17 18 In the absence of spirometry reference norms among adult Indigenous people,43 there are substantial challenges in the accurate diagnosis and classification of the severity of airway disease,44 45 in order to guide inhaled pharmacotherapy appropriately. Health practitioners caring for Indigenous/Aboriginal people undoubtably rely on and adopt evidence established in non-Aboriginal/Indigenous ethnic populations that may or may not be appropriate for Indigenous/Aboriginal people. A previous study from our centre found that among Aboriginal patients with COPD, irrespective of which severity classification is used (GOLD, COPD-X or Global lung function initiative-2012), the majority of patients will likely be classified as having either severe or very severe disease.46 Hence why, with spirometry demonstrating a high proportion of patients classified to have severe COPD, and in line with current recommended guidelines,20 we observed a significant proportion of patients with COPD having an ICS prescription. However, a recent study has demonstrated that there could be excessive decline in lung function parameters, in particular for FEV1 values, associated with ICS use among Aboriginal Australians with chronic airway diseases.47 Hence, caution has to be exercised while considering ICS containing pharmacotherapy among an Aboriginal Australian population with a high prevalence of concomitant airway disease.
Use of inhaled pharmacotherapy may be appropriate among patients with asthma or selected patients with COPD,16–21 yet among those with bronchiectasis, consensus guidelines are far more individualised and depend on the frequency of exacerbations, prior medication response and comorbidity of asthma and/or COPD.48–51 As ICS reduces the local (pulmonary) immune response, there is potential for deleterious effect of ICS use among patients with bronchiectasis, as the disease is typically underlined by long term bacterial colonisation, perpetuating a vicious cycle of recurrent infective exacerbations and further airway inflammation, alongside a decline in lung function, which may be exacerbated by long term use of ICS.47 52 In our study, we noted a significant proportion of patients with underlying bronchiectasis had ICS prescribed—even in the absence of evidence of comorbid lung conditions—and moreover, patients prescribed with ICS had higher rates of hospital presentations. Hence, it may be reasonable to presume the overlap of bronchiectasis and ICS prescription could be at least partially driving the higher hospital admission rates seen among our patients. Contrary to international guidelines recommending against the use of ICS among patients with bronchiectasis unless there are clear clinical justification,53 ICS containing pharmacotherapy continues to be prescribed frequently/liberally even among the non-Aboriginal Australian population,54 with data suggesting unprecedently 6.3% of Australians have a current ICS prescription,55 potentially inappropriately in certain circumstances. Furthermore, more recent studies have raised serious concerns in relation to ICS use and its association with risk of pneumonia among patients with airway diseases, more specifically with fluticasone containing inhaled pharmacotherapy.56–59 The results of our study potentially add to this body of evidence, with the high rate of hospitalisations among patients with a prescription of ICS, and fluticasone was by far the single most prescribed ICS among our study participants.
The current study also found that ICS prescription, regardless of underlying respiratory condition, was associated with significantly higher overall hospital admission rates and more specifically with higher COPD with lower respiratory tract infection admission rates (ICD-J44.0), in particular in the presence of bronchiectasis. Due to the retrospective study design, we cannot ascertain if ICS prescription contributed to excessive hospital admission rates or if the excessive hospital admission rates triggered ICS prescriptions, and nor could the exact point of initiation of therapy compared with hospital or PHC presentations be determined accurately. Nonetheless, healthcare utilisation for respiratory disorders is generally observed to be higher for Indigenous people globally, especially in high-income countries such as Australia, New Zealand and Canada.14 60–62 It is unclear at this stage if the high healthcare utilisation rates observed are related to the adoption of therapeutic interventions established among non-Aboriginal/Indigenous populations, or if it is related to a higher prevalence of chronic and more severe respiratory disease burden.
Nevertheless, in the Australian context, it appears that inhaled pharmacotherapy is liberally and extensively used to treat chronic airway diseases among Aboriginal Australians, despite the lack of clear evidence or guidelines. Several previous studies have reported on the use of airway directed inhaled pharmacotherapy in other ethnic populations, indeed highlighting rather inappropriate prescribing patterns on several fronts, more particularly in the excessive use of ICS among patients with airway disease, including at the PHC level.63–66 This trend appears to be true for the current study, as we noted that inhaled pharmacotherapy prescribing patterns did not clearly align with spirometry results, particularly among patients demonstrating restrictive or mixed impairments. This is despite the Australian rural guidelines manual (CARPA) recommending to consider ICS only if the spirometry demonstrates BDR among patients with bronchiectasis.51 It is imperative to acknowledge that there are substantial differences in the way in which respiratory diseases manifests in Aboriginal people in comparison to non-Aboriginal Australian counterparts.67–77 In this vein, recent studies have recommended to take a personalised and tailored approach, by adopting clinical, spirometry and radiology in the accurate diagnosis, alongside advocating cautious use of inhaled pharmacotherapy in the management of chronic respiratory conditions among Aboriginal people.47 78 Moreover, following locally developed prescribing guidelines that have been specifically developed for patients residing in remote and rural communities is vital,51 in order to reduce treatment emergent morbidity and mortality.42 59 Currently, there is limited access to comprehensive medication review services for Aboriginal people79 and in remote communities.80 Studies have shown that the involvement of Aboriginal Health Workers and Consultant pharmacists can have a positive impact on appropriate prescribing patterns.81 82 These types of services could be established and evaluated in this setting.
Limitations
The authors acknowledge that this study has several limitations. The participants included in this study were drawn from referred patients to a specialist respiratory service in the TEHS region of the NT, hence, the outcomes represented in this study cannot be generalised, neither to other Aboriginal Australians residing in the NT nor to those living in other Australian states or territory or Indigenous people globally. The reason we observed a high proportion of patients being on inhaled pharmacotherapy is likely related to this. Moreover, medication adherence data were not available to be assessed, which would have had an impact on hospital and PHC presentations. Furthermore, spirometry, radiology and pharmacotherapy prescriptions did not all occur at the same time point, but rather were spread through the study window, and indeed some patients may have swapped between therapies and dosages in this time period, including during exacerbations, thus curtailing the potential for this study to truly assess any time course effect. In addition, medical services provision for patients residing in remote communities can be variable and transient, swapping between primary/visiting general practitioners/visiting specialist health work force, hence, choice and treatment initiation or ceasing are often dependent on the individual medical practitioner’s discretion. On a similar note, we did not collect data on length of hospital admission or care provided during hospital admissions, which may have affected propensity for future visits, nor the exacerbation history of the patient which limits our ability to define the appropriateness of+ICS prescription. In other underserved populations medication sharing is commonly reported, however, whether this is the case in the current population and study sample is not known. We also did not include or compare the prescribing practice between Aboriginal and non-Aboriginal patients in this study, in order not to introduce bias. As such, previous studies have demonstrated significant difference in the way chronic respiratory diseases manifests Aboriginal patients compared with non-Aboriginal Australians. Nevertheless, this is the first study to assess the prescription and associations of inhaled pharmacotherapy in a predominantly adult Aboriginal Australian population, highlighting opportunities for prospective further research to exploring avenues in the better management of chronic respiratory conditions.
Conclusion
This study has demonstrated that airway directed inhaled pharmacotherapy was observed to be substantially used in the management of chronic airway diseases among Aboriginal patients being referred to the respiratory service in the NT. ICS containing inhaled pharmacotherapy appears to be prescribed extensively, rather inappropriately in certain respiratory conditions, which may be detrimental for overall outcomes. Strategies are required for advocating appropriate inhaled pharmacotherapy prescribing practice among Aboriginal people with chronic airway diseases.
Acknowledgments
We sincerely thank Mrs Raelene L Messenger, respiratory clinical nurse consultant respiratory form RDH and Ms Ara Joy Perez form DRSH/DPH in contributing towards this study. We also extend our sincere appreciation to our Aboriginal health workers and primary care physicians in co-ordinating respiratory care for Aboriginal people residing in the TEHS region of the NT of Australia. We also thank the division of medicine and the research committee members at RDH for supporting funding for this study.
Footnotes
Contributors: All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work. SH is the guarantor and accepts full responsibility for the work and/or the conduct of the study, had access to the data, and controlled the decision to publish.
Funding: This study received internal funding/support from the Division of Medicine, Royal Darwin Hospital, Darwin, Australia.
Map disclaimer: The inclusion of any map (including the depiction of any boundaries therein), or of any geographic or locational reference, does not imply the expression of any opinion whatsoever on the part of BMJ concerning the legal status of any country, territory, jurisdiction or area or of its authorities. Any such expression remains solely that of the relevant source and is not endorsed by BMJ. Maps are provided without any warranty of any kind, either express or implied.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available on reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study was approved by the Human Research Ethics governance/committee of the NT, TEHS and Menzies School of Health Research (Reference: HREC 2020-3840).
References
- 1.Australian Institute of Health and Welfare (AIHW) . Aboriginal and torres strait islander health performance framework 2017 report: northern territory. 2022. Available: https://www.aihw.gov.au
- 2.Australian Bureau of Statistics . Northern territory: aboriginal and torres strait islander population summary. 2022. Available: https://www.abs.gov.au/articles/northern-territory-aboriginal-and-torres-strait-islander-population-summary
- 3.Australian Institute of Health Welfare . Profile of indigenous australians. 2021. Available: https://www.aihw.gov.au/reports/australias-welfare/profile-of-indigenous-australians
- 4.Kruavit A, Fox M, Pearson R, et al. Chronic respiratory disease in the regional and remote population of the Northern Territory top end: a perspective from the specialist respiratory outreach service. Aust J Rural Health 2017;25:275–84. 10.1111/ajr.12349 [DOI] [PubMed] [Google Scholar]
- 5.Heraganahally SS, Howarth TP, Sorger L. Chest computed tomography findings among adult Indigenous Australians in the Northern Territory of Australia. J Med Imaging Radiat Oncol 2022;66:337–44. 10.1111/1754-9485.13295 [DOI] [PubMed] [Google Scholar]
- 6.Heraganahally SS, Wasgewatta SL, McNamara K, et al. Chronic obstructive pulmonary disease in Aboriginal patients of the Northern Territory of Australia: a landscape perspective. Int J Chron Obstruct Pulmon Dis 2019;14:2205–17. 10.2147/COPD.S213947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mehra S, Chang AB, Lam CK, et al. Bronchiectasis among Australian Aboriginal and non-Aboriginal patients in the regional and remote population of the Northern Territory of Australia. Rural Remote Health 2021;21:6390. 10.22605/RRH6390 [DOI] [PubMed] [Google Scholar]
- 8.Heraganahally SS, Wasgewatta SL, McNamara K, et al. 2004 chronic obstructive pulmonary disease with and without bronchiectasis in aboriginal australians: a comparative study. Intern Med J 2020;50:1505–13. 10.1111/imj.14718 [DOI] [PubMed] [Google Scholar]
- 9.Schubert J, Kruavit A, Mehra S, et al. Prevalence and nature of lung function abnormalities among indigenous australians referred to specialist respiratory outreach clinics in the northern territory. Intern Med J 2019;49:217–24. 10.1111/imj.14112 [DOI] [PubMed] [Google Scholar]
- 10.Heraganahally SS, Howarth T, Mo L, et al. Critical analysis of Spirometric patterns in correlation to chest computed tomography among adult Indigenous Australians with chronic airway diseases. Expert Rev Respir Med 2021;15:1229–38. 10.1080/17476348.2021.1928496 [DOI] [PubMed] [Google Scholar]
- 11.Howarth T, Saad HB, Perez AJ, et al. Comparison of diffusing capacity of carbon monoxide (DLCO) and total lung capacity (TLC) between Indigenous Australians and Australian Caucasian adults. PLoS ONE 2021;16:e0248900. 10.1371/journal.pone.0248900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Heraganahally SS, Howarth T, Sorger L, et al. n.d. Sex differences in pulmonary function parameters among Indigenous Australians with and without chronic airway disease. PLoS ONE;17:e0263744. 10.1371/journal.pone.0263744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Heraganahally SS, Mortimer N, Howarth T, et al. Utility and outcomes among Indigenous and non-Indigenous patients requiring domiciliary oxygen therapy in the regional and rural Australian population. Aust J Rural Health 2021;29:918–26. 10.1111/ajr.12782 [DOI] [PubMed] [Google Scholar]
- 14.Heraganahally SS, Ghimire RH, Howarth T, et al. Comparison and outcomes of emergency department presentations with respiratory disorders among Australian Indigenous and non-Indigenous patients. BMC Emerg Med 2022;22:11.:11. 10.1186/s12873-022-00570-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jenkins C. Drugs for chronic obstructive pulmonary disease. Aust Prescr 2017;40:15–9. 10.18773/austprescr.2017.003 Available: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Global Initiative for Asthma . Global strategy for asthma management and prevention. 2021. Available: www.ginasthma.org
- 17.Global initiative for chronic obstructive lung disease . Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. 2021. Available: http://www.goldcopd.org
- 18.Yang IA, George J, Jenkins S, et al. The COPD-X plan: australian and new zealand guidelines for the management of chronic obstructive pulmonary disease 2021.COPD guidelines committee – version 2. 63 (2021). 2022. Available: https://copdx.org.au
- 19.Dabscheck E, McDonald CF, Yang IA. Concise guidance for COPD. Respirology 2020;25:1129–32. 10.1111/resp.13934 [DOI] [PubMed] [Google Scholar]
- 20.Walters J. Copd-diagnosis, management and the role of the GP. Aust Fam Physician 2010;39:100–3. [PubMed] [Google Scholar]
- 21.Reddel HK, Valenti L, Easton KL, et al. Assessment and management of asthma and chronic obstructive pulmonary disease in australian general practice. Aust Fam Physician 2017;46:413–9. [PubMed] [Google Scholar]
- 22.Jones MP, Zhao Y, Guthridge S, et al. Effects of turnover and stability of health staff on quality of care in remote communities of the northern territory, australia: a retrospective cohort study. BMJ Open 2021;11:e055635. 10.1136/bmjopen-2021-055635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thynne T, Gabb GM. Therapeutic drug safety for indigenous australians: how do we close the gap? Medical Journal of Australia 2016;204:16–7. 10.5694/mja15.00937 Available: https://onlinelibrary.wiley.com/toc/13265377/204/1 [DOI] [PubMed] [Google Scholar]
- 24.Department of Health, Northern Territory Government . The 2017-18 annual report for the department of health and the health services. 2018. Available: www.health.nt.gov.au
- 25.National Health Medical Research Council . Ethical conduct in research with aboriginal and torres strait islander peoples and communities: guidelines for researchers and stakeholders. Canberra: Commonwealth of Australia; 2018. Available: https://www.nhmrc.gov.au [Google Scholar]
- 26.Johnson JD, Theurer WM. A stepwise approach to the interpretation of pulmonary function tests. Am Fam Physician 2014;89:359–66. [PubMed] [Google Scholar]
- 27.Sim YS, Lee J-H, Lee W-Y, et al. Spirometry and bronchodilator test. Tuberc Respir Dis (Seoul) 2017;80:105–12. 10.4046/trd.2017.80.2.105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stanojevic S, Kaminsky DA, Miller MR, et al. ERS/ATS technical standard on interpretive strategies for routine lung function tests. Eur Respir J 2022;60:2101499. 10.1183/13993003.01499-2021 [DOI] [PubMed] [Google Scholar]
- 29.Pipavath SNJ, Schmidt RA, Takasugi JE, et al. Chronic obstructive pulmonary disease: radiology-pathology correlation. J Thorac Imaging 2009;24:171–80. 10.1097/RTI.0b013e3181b32676 [DOI] [PubMed] [Google Scholar]
- 30.Gaillard F, Weerakkody Y. Bronchiectasis. reference article, radiopaedia. 2022. Available: 10.53347/rID-1021 [DOI]
- 31.Ospina MB, Voaklander DC, Stickland MK, et al. Prevalence of asthma and chronic obstructive pulmonary disease in Aboriginal and non-Aboriginal populations: a systematic review and meta-analysis of epidemiological studies. Can Respir J 2012;19:355–60. 10.1155/2012/825107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bird Y, Moraros J, Mahmood R, et al. Prevalence and associated factors of COPD among Aboriginal peoples in Canada: a cross-sectional study. Int J Chron Obstruct Pulmon Dis 2017;12:1915–22. 10.2147/COPD.S138304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ospina MB, Voaklander D, Senthilselvan A, et al. Incidence and prevalence of chronic obstructive pulmonary disease among Aboriginal peoples in Alberta, Canada. PLoS ONE 2015;10:e0123204. 10.1371/journal.pone.0123204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Koleade A, Farrell J, Mugford G, et al. Prevalence and risk factors of ACO (asthma-COPD overlap) in Aboriginal people. Journal of Environmental and Public Health 2018;2018:1–9. 10.1155/2018/4657420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Blackall SR, Hong JB, King P, et al. Bronchiectasis in Indigenous and non-Indigenous residents of Australia and New Zealand. Respirology 2018;23:743–9. 10.1111/resp.13280 [DOI] [PubMed] [Google Scholar]
- 36.de Boer S, Lewis CA, Fergusson W, et al. Ethnicity, socioeconomic status and the severity and course of non-cystic fibrosis bronchiectasis. Intern Med J 2018;48:845–50. 10.1111/imj.13739 [DOI] [PubMed] [Google Scholar]
- 37.Kew KM, Mavergames C, Walters JAE. Long-Acting beta2-agonists for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2013:CD010177. 10.1002/14651858.CD010177.pub2 [DOI] [PubMed] [Google Scholar]
- 38.Koarai A, Sugiura H, Yamada M, et al. Treatment with LABA versus Lama for stable COPD: a systematic review and meta-analysis. BMC Pulm Med 2020;20:111.:111. 10.1186/s12890-020-1152-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Oba Y, Keeney E, Ghatehorde N, et al. Dual combination therapy versus long-acting bronchodilators alone for chronic obstructive pulmonary disease (COPD): a systematic review and network meta-analysis. Cochrane Database Syst Rev 2018;12:CD012620. 10.1002/14651858.CD012620.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Agusti A, Fabbri LM, Singh D, et al. Inhaled corticosteroids in COPD: friend or foe? Eur Respir J 2018;52:1801219. 10.1183/13993003.01219-2018 [DOI] [PubMed] [Google Scholar]
- 41.Photopoulos J. Should physicians still be prescribing steroid inhalers as a first-line treatment for COPD? Nature 2020;581:S12–3. 10.1038/d41586-020-01376-8 [DOI] [Google Scholar]
- 42.Heraganahally SS, Ghataura AS, Er XY, et al. Excessive dynamic airway collapse: a COPD/asthma mimic or a treatment-emergent consequence of inhaled corticosteroid therapy: case series and brief literature review. Clin Pulm Med 2020;27:175–82. 10.1097/CPM.0000000000000382 [DOI] [Google Scholar]
- 43.Blake TL, Chang AB, Petsky HL, et al. Spirometry reference values in Indigenous Australians: a systematic review. Med J Aust 2016;205:35–40. 10.5694/mja16.00226 [DOI] [PubMed] [Google Scholar]
- 44.Heraganahally SS, Howarth T, White E, et al. Lung function parameters among Australian Aboriginal “ apparently healthy ” adults: an Australian Caucasian and global lung function initiative (GLI-2012) various ethnic norms comparative study. Expert Rev Respir Med 2021;15:833–43. 10.1080/17476348.2021.1847649 [DOI] [PubMed] [Google Scholar]
- 45.White E, James A, de Klerk N, et al. Selection of appropriate spirometry reference values in aboriginal australians. Australian Indigenous Health Bulletin 2019;19. [Google Scholar]
- 46.Heraganahally S, Howarth TP, White E, et al. Implications of using the GLI-2012, gold and Australian COPD-X recommendations in assessing the severity of airflow limitation on spirometry among an Indigenous population with COPD: an Indigenous Australians perspective study. BMJ Open Respir Res 2021;8:e001135. 10.1136/bmjresp-2021-001135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Heraganahally SS, Ponneri TR, Howarth TP, et al. The effects of inhaled airway directed pharmacotherapy on decline in lung function parameters among Indigenous Australian adults with and without underlying airway disease. Int J Chron Obstruct Pulmon Dis 2021;16:2707–20. 10.2147/COPD.S328137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Polverino E, Goeminne PC, McDonnell MJ, et al. European respiratory Society guidelines for the management of adult bronchiectasis. Eur Respir J 2017;50:1700629. 10.1183/13993003.00629-2017 [DOI] [PubMed] [Google Scholar]
- 49.Kapur N, Petsky HL, Bell S, et al. Inhaled corticosteroids for bronchiectasis. Cochrane Database Syst Rev 2018;5:CD000996. 10.1002/14651858.CD000996.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hill AT, Sullivan AL, Chalmers JD, et al. British thoracic society guideline for bronchiectasis in adults. Thorax 2019;74:1–69. 10.1136/thoraxjnl-2018-212463 [DOI] [PubMed] [Google Scholar]
- 51.Remote Primary Health Care Manuals . CARPA standard treatment manual. 7th edition. Alice Springs, NT: Centre for Remote Health, 2017. [Google Scholar]
- 52.Borekci S, Halis AN, Aygun G, et al. Bacterial colonization and associated factors in patients with bronchiectasis. Ann Thorac Med 2016;11:55–9. 10.4103/1817-1737.172297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rhee CK, Chau NQ, Yunus F, et al. Management of COPD in asia: A position statement of the asian pacific society of respirology. Respirology 2019;24:1018–25. 10.1111/resp.13633 [DOI] [PubMed] [Google Scholar]
- 54.Visser SK, Bye PTP, Fox GJ, et al. Management of Australian adults with bronchiectasis in tertiary care: evidence-based or access-driven? Lung 2019;197:803–10. 10.1007/s00408-019-00280-x [DOI] [PubMed] [Google Scholar]
- 55.AIHW . Respiratory medication use in australia 2003–2013: treatment of asthma and COPD. cat. no: ACM 31:85. 2015. Available: https://www.aihw.gov.au›reports›respiratory-medica
- 56.Choi J-H, Jeong K-B, Park YH, et al. Comparison of risk of pneumonia caused by fluticasone propionate versus budesonide in chronic obstructive pulmonary disease: a nationwide retrospective cohort study. Int J Chron Obstruct Pulmon Dis 2021;16:3229–37. 10.2147/COPD.S332151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Janson C, Stratelis G, Miller-Larsson A, et al. Scientific rationale for the possible inhaled corticosteroid intraclass difference in the risk of pneumonia in COPD. Int J Chron Obstruct Pulmon Dis 2017;12:3055–64. 10.2147/COPD.S143656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Henkle E, Curtis JR, Chen L, et al. Comparative risks of chronic inhaled corticosteroids and macrolides for bronchiectasis. Eur Respir J 2019;54:1801896. 10.1183/13993003.01896-2018 [DOI] [PubMed] [Google Scholar]
- 59.Håkansson KEJ, Fjaellegaard K, Browatzki A, et al. Inhaled corticosteroid therapy in bronchiectasis is associated with all-cause mortality: a prospective cohort study. Int J Chron Obstruct Pulmon Dis 2021;16:2119–27. 10.2147/COPD.S311236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Vigneault L-P, Diendere E, Sohier-Poirier C, et al. Acute health care among Indigenous patients in Canada: a scoping review. International Journal of Circumpolar Health 2021;80:1. 10.1080/22423982.2021.1946324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Roberts ME, Lowndes L, Milne DG, et al. Socioeconomic deprivation, readmissions, mortality and acute exacerbations of bronchiectasis. Intern Med J 2012;42:e129–36. 10.1111/j.1445-5994.2011.02444.x [DOI] [PubMed] [Google Scholar]
- 62.Nader F, Kolahdooz F, Sharma S. Assessing health care access and use among Indigenous peoples in Alberta: a systematic review. J Health Care Poor Underserved 2017;28:1286–303. 10.1353/hpu.2017.0114 [DOI] [PubMed] [Google Scholar]
- 63.Casas A, Montes de Oca M, Menezes AM, et al. Respiratory medication used in COPD patients from seven Latin American countries: the LASSYC study. Int J Chron Obstruct Pulmon Dis 2018;13:1545–56. 10.2147/COPD.S154097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Jardim JR, Stirbulov R, Moreno D, et al. Respiratory medication use in primary care among COPD subjects in four Latin American countries. Int J Tuberc Lung Dis 2017;21:458–65. 10.5588/ijtld.16.0633 [DOI] [PubMed] [Google Scholar]
- 65.Lucas AEM, Smeenk FWJM, Smeele IJ, et al. Overtreatment with inhaled corticosteroids and diagnostic problems in primary care patients, an exploratory study. Fam Pract 2008;25:86–91. 10.1093/fampra/cmn006 [DOI] [PubMed] [Google Scholar]
- 66.Tavakoli H, Johnson KM, FitzGerald JM, et al. Trends in prescriptions and costs of inhaled medications in chronic obstructive pulmonary disease: a 19-year population-based study from Canada. Int J Chron Obstruct Pulmon Dis 2019;14:2003–13. 10.2147/COPD.S210897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sze DFL, Howarth TP, Lake CD, et al. Differences in the spirometry parameters between Indigenous and non-Indigenous patients with COPD: a matched control study. Int J Chron Obstruct Pulmon Dis 2022;17:869–81. 10.2147/COPD.S361839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Heraganahally SS, Silva SAMS, Howarth TP, et al. Comparison of clinical manifestation among Australian Indigenous and non-Indigenous patients presenting with pleural effusion. Intern Med J 2022;52:1232–41. 10.1111/imj.15310 [DOI] [PubMed] [Google Scholar]
- 69.Seyedshahabedin MM, Howarth TP, Mo L, et al. Flexible bronchoscopy indications and outcomes between Indigenous and non-Indigenous patients in the Northern Territory of Australia. Intern Med J 5, 2022. 10.1111/imj.15865 [DOI] [PubMed] [Google Scholar]
- 70.Heraganahally SS, Kruavit A, Oguoma VM, et al. Sleep apnoea among Australian Aboriginal and non-Aboriginal patients in the Northern Territory of australia-a comparative study. Sleep 2020;43:zsz248. 10.1093/sleep/zsz248 [DOI] [PubMed] [Google Scholar]
- 71.Howarth TP, Gentin N, Reyes-Chicuellar N, et al. Sleep quality and obstructive sleep apnoea in indigenous and non-indigenous australian children. Sleep Med 2022;98:68–78. 10.1016/j.sleep.2022.06.014 [DOI] [PubMed] [Google Scholar]
- 72.Pal A, Howarth TP, Rissel C, et al. Copd disease knowledge, self-awareness and reasons for hospital presentations among a predominately indigenous australian cohort: a study to explore preventable hospitalisation. BMJ Open Respir Res 2022;9:e001295. 10.1136/bmjresp-2022-001295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.LaGrappe D, Massey L, Kruavit A, et al. Sleep disorders among Aboriginal Australians with Machado-Joseph disease: quantitative results from a multiple methods study to assess the experience of people living with the disease and their caregivers. Neurobiol Sleep Circadian Rhythms 2022;12:100075. 10.1016/j.nbscr.2022.100075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Mehra S, Ghimire RH, Mingi JJ, et al. Gender differences in the clinical and polysomnographic characteristics among Australian Aboriginal patients with obstructive sleep apnea. Nat Sci Sleep 2020;12:593–602. 10.2147/NSS.S258330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Benn E, Wirth H, Short T, et al. n.d. The top end sleepiness scale (Tess): a new tool to assess subjective daytime sleepiness among Indigenous Australian adults. NSS;Volume 13:315–28. 10.2147/NSS.S298409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Heraganahally SS, Howarth TP, Wirth H, et al. Validity of the new “top end sleepiness scale” against the STOP-bang tool in predicting obstructive sleep apnoea among indigenous australian adults. Intern Med J 20, 2021. 10.1111/imj.15633 [DOI] [PubMed] [Google Scholar]
- 77.Garg H, Er XY, Howarth T, et al. Positional sleep apnea among regional and remote australian population and simulated positional treatment effects. Nat Sci Sleep 2020;12:1123–35. 10.2147/NSS.S286403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Heraganahally SS, Howarth TP, Lloyd A, et al. The prevalence of bronchodilator responsiveness “asthma” among adult indigenous australians referred for lung function testing in the top end northern territory of australia. J Asthma Allergy 2022;15:1305–19. 10.2147/JAA.S376213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Swain L, Griffits C, Pont L, et al. Attitudes of pharmacists to provision of home medicines review for indigenous australians. Int J Clin Pharm 2014;36:1260–7. 10.1007/s11096-014-0030-y [DOI] [PubMed] [Google Scholar]
- 80.Vaughan F. Accredited pharmacist special interest group: hmr in remote indigenous communities. Australian Pharmacist 2017;36:16–7. [Google Scholar]
- 81.Hamrosi K, Taylor SJ, Aslani P. Issues with prescribed medications in Aboriginal communities: Aboriginal health workers’ perspectives. Rural Remote Health 2006;6:557. [PubMed] [Google Scholar]
- 82.Gormley C, Spargo M, Fleming G, et al. Medicines optimisation for respiratory patients: the establishment of a new consultant respiratory pharmacist role in Northern Ireland. Pharmacy (Basel) 2021;9:177. 10.3390/pharmacy9040177 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available on reasonable request.