Abstract
Cognitive decline as part of mental ageing is typically assessed with standardized tests; below-average performance in such tests is used as an indicator for pathological cognitive aging. In addition, morphological and functional changes in the brain are used as parameters for age-related pathological decline in cognitive abilities. However, there is no simple link between the trajectories of changes in cognition and morphological or functional changes in the brain. Furthermore, below-average test performance does not necessarily mean a significant impairment in everyday activities. It therefore appears crucial to record individual everyday tasks and their cognitive (and other) requirements in functional terms. This would also allow reliable assessment of the ecological validity of existing and insufficient cognitive skills. Understanding and dealing with the phenomena and consequences of mental aging does of course not only depend on cognition. Motivation and emotions as well personal meaning of life and life satisfaction play an equally important role. This means, however, that cognition represents only one, albeit important, aspect of mental aging. Furthermore, creating and development of proper assessment tools for functional cognition is important. In this contribution we would like to discuss some aspects that we consider relevant for a holistic view of the aging mind and promote a strengthening of a multidisciplinary approach with close cooperation between all basic and applied sciences involved in aging research, a quick translation of the research results into practice, and a close cooperation between all disciplines and professions who advise and support older people.
Keywords: Cognitive aging, Mental aging, Functional cognition, Coping, Resilience, Life quality, ADL, Aging research
Introduction
Aging and cognitive decline appear often as inevitably linked in human aging research. According to the “mainstream” scientific perspective, cognitive decline is becoming an increasingly and almost mandatory characteristic for people over the age of 65 years [33]. It has been known since the seminal Seattle longitudinal study [118] that cognitive performance changes over the course of adult life. But the “decline” in cognitive performance is not fundamentally synonymous with actual cognitive impairment or disability but mostly reflects the normal development of cognition during adulthood. Possibly the rather pessimistic view on age-related cognitive decline is mainly based on laboratory results on cognitive performance but not on observations on the cognitive competence and cognitive behavior in everyday life conditions of the same individuals [113]. If there is cognitive decline, when in life has an individual reached the peak of cognition, from where the decline starts, and at what level of cognitive decline can one speak of a significant loss? There is no doubt that cognitive performance does not persist regardless of age, but rather shows an age-related decrease, which is also experienced and reported by older people [149] (Table 1).
Table 1.
Proposal for a possible comprehensive standard on mental aging studies with focus on non-biological (A) and involved disciplines (B).
| A Focus on functional mental aging |
| Perception: Vision, audition, somatosensory perception, olfactory and gustatory perception |
| Cognition: Attention (alertness, cognitive speed, sustained attention; focused and divided attention; spatial attention) |
| Memory (episodic, semantic and procedural memory; short-term, working and ling-term memory; prospective memory) |
| Executive functions (planning, problem solving, cognitive flexibility, adaptation of routines to changing task requirements) |
| Language/Speech: Language comprehension and expression; reading (incl. reading habits) and writing |
| Motivation: Engagement in daily and social activities |
| Emotion: Emotion recognition (social perception); expression of emotions |
| Mood: Symptoms of depression and anxiety |
| Subjective cognitive complaints |
| Instrumental activities of daily living: ideally performance-based measures plus an informant rating |
| Social networks |
| Sleep |
| Life quality |
| Physical activity |
| Aging perceptions |
| Biological variables: Health status (e.g., blood pressure, blood glucose status, hormonal status, alcohol consumption, smoking, drug abuse), current medications, BMI, medical history, neuroimaging, genetics (APOE status) |
| Demographic variables: Age, sex/gender, family status, level of education, regular earlier occupation, current occupation, living arrangement, ethnicity. |
| B Disciplines involved in the study of mental aging |
| Psychiatry |
| Neurology |
| (Neuro-) Psychology |
| Occupational therapy |
| Neuroimaging |
| Neuroendocrinology |
| Internal Medicine |
| Genetics |
An age-related decrease in functionality can also be found in other domains, such as emotion, motivation, language or motor skills. However, these domains are often neglected and not routinely assessed in research or clinical practice. This is all the more astonishing because cognition critically depends on motivation and emotional evaluation also in older age [88], [34]. However, the scientific literature of the past decade gives the impression that research on aging is somehow biased and has mainly focused on cognition and the underlying neurobiological factors. It seems like cognition is a major player among mental functions. In a certain way this may be true if cognition is understood as the ability to analytically reflect on one's own thinking, feeling and behavior and its social and moral evaluation, and to search for and find meaning in life as the highest mental level. On the other hand, cognition can also be understood as a universal set of tools for developing, executing and supervising mental and behavioral routines and habits that enable people to deal well with the personal challenges of life. Above all, this ability includes adaptive strategies to changing physical and social environments, but also to cope flexibly with unsolvable problems and challenges. Maintaining good health and independence while avoiding or coping appropriately with disability, functional and cognitive decline are key challenges of ageing. The meaning of one's own life and its realization may play a special role in older age, as meaningful factors in earlier life, e.g. occupation, care for one's own children and their development, or special social roles, do typically no longer exist. The individual definition of meaningfulness depends on one's own ideas, wishes and positive and negative life experiences and their evaluation [102]. Of course, good or at least sufficiently good physical and mental health, wellbeing, positive social contacts with family and friends, other social roles (e.g., grandparenthood, caregiver, volunteer), mobility, and the availability of sufficient financial resources are essential for assessing and experiencing one's own life in older age as meaningful [54], [62], [134]. In addition, values attributed to positive aging depend significantly also on cultural factors [75]. Aging research has also paid attention to aging perceptions which refer to the stereotypes and attitudes an individual holds towards aging, as well as their personal experiences associated with aging. Not surprisingly, negative aging perceptions are associated with decline in cognitive and functional performance [89], [148].
As already mentioned, cognition undoubtedly plays a decisive role when it comes to the development or planning, implementation and supervision as well as the proof of functional adaptation strategies [44], [136]. This applies to dealing with professional, economic, social and health challenges. A necessary mastery of the listed challenges includes not only the current handling of problems, but also preventive activities and measures. Of course, prevention should not and cannot only begin when mental, physical, economic or social difficulties are already visible or have arisen. The ability to plan and to solve foreseeable problems or to develop alternatives are necessary prerequisites for successful coping with difficulties in life in general [56].
Given a lack of reviews that include a holistic view of the aging mind, this selective narrative review aims to give an overview of different aspects of the aging mind that extend beyond cognitive decline. After a brief outline of morphological and functional changes of the aging brain, we will give an overview of brain and cognitive reserve, individual and general characteristics of cognitive aging, the interplay between mental health, cognition and influencing factors as well as resilience, meaning of life, and life quality in older people. We will describe the assessment and rehabilitation of older people with impaired cognition, outline the relationship between cognitive performance, as assessed in standardized tests, and functional cognition, defined as cognitive performance required to cope with individual activities of daily living, and finally, give recommendations for bridging interdisciplinary gaps in future research.
Morphological and functional changes of the aging brain
Research on the development of cognitive skills with age has consistently shown that cognitive performance decreases with age. The performance in the domains of perception, attention, memory and executive functions, in particular selective attention, planning, problem solving and multi-tasking, decreases with increasing age, largely independently of unfavorable influencing factors. In other domains, e.g. general knowledge and vocabulary and life experience (wisdom), is older adults’ performance as good as, or even superior to, that of young people [38].
The age-related decline in cognitive performance is mainly explained by morphological and functional changes in the brain. Not only does the number of cortical neurons and thus the thickness of the gray matter decrease [146], but also of intra- and intercortical connections, so that brain networks thin out [31]. As a consequence, exchange of information between and cooperation of local, regional and supra-regional brain structures is impaired or lost [95]. Frontal, temporal (including the hippocampus), and parietal structures show age-related loss of gray matter, while the primary sensory cortices are relatively or completely preserved in aging [37], [51], [105].This morphological brain aging pattern is called the ‘first-in, last-out’ hypothesis, which means that the brain regions that develop earlier are also less affected by age-related decline than those that develop later [74]. A similar picture emerges for age-related white matter changes, which are particularly pronounced in the prefrontal regions, as observed in a longitudinal study [111]. However, the trajectories of the gray matter and white matter alterations may differ; the loss of gray matter generally begins in early adulthood whereas the white matter volume decreases after middle age [35], [106]. The most consistent finding in aging is a general decline (or disconnection) in the connectivity within individual networks [30]. In his comprehensive overview, Kawagoe [74] has pointed out that there is still “no consensus about a comprehensive theory of the aging brain. Obtaining such a consensus remains a challenge because even the relationship between structural connectivity and functional connectivity is not clearly established, although the structural connectivity can be expected to be a basis for functional connectivity” (p. 14). In light of this conclusion, the claim of some authors is even more surprising, that one could derive the diagnosis of cognitive decline, mild cognitive impairment and (early) dementia with sufficient certainty from brain imaging alone [39], [128]. Such a far-reaching (diagnostic) conclusion would presuppose that there is a close connection between the trajectories of changes in cognition and of the morphological and functional changes in the brain.
The assumption that morphological brain changes in older people are basically always associated with a decline in cognition was seriously questioned already by the outcome of the pioneering study by Ince & colleagues in 2001 [69]. They showed that striking age-related morphological changes in the brain were not compulsorily associated with a loss of cognitive abilities. Later studies have confirmed this result and have shown that various compensation mechanisms can be responsible for this discrepancy (e.g., [96]). The assumption of takeover of impaired functions by other structures or by co-activation of additional structures within a functional network are among the preferred explanations [12].
In summary, age-related morphological and functional changes in the brain are often, but not always, associated with a decline in cognitive performance.
Brain reserve and cognitive reserve
In this context, the concepts of brain reserve and cognitive reserve play an important role in understanding and explaining the discrepancy between morphological and cognitive measures. Brain reserve refers more to the “passive” capacity of the aging brain to cope with morphological alterations and consequent functional losses, while cognitive reserve means that the brain actively tries to compensate for functional losses with the help of already established, successful cognitive processes and individual strategies [135]. The question remains which factors contribute to acquiring, increasing and conserving this cognitive reserve, or reducing or impairing it. Individual genetic factors or predispositions [64], [84], health, mood, lifestyle, and social factors play a significant role [16], [62], [117]. Activities and measures exist to maintain or regain mental health or at least to prevent the pathological consequences of unfavorable developments. In addition, there are ways to keep oneself mentally fit, including an engaged lifestyle [137], and regular physical [11], [140] and social activities [86]. The increased prevalence of multimorbidity in older age can lead to more rapid functional decline in individuals with less cognitive reserve and even relatively minor illness or injury may result in significant functional impairment. Maintaining physical fitness and building cognitive (and thus functional) reserve to optimise functional ability is a life-long journey that should be promoted and implemented early in life. It is important to note, that higher resilience levels earlier in life are associated with lower risk of progressive cognitive decline [17].
In summary, there are large interindividual differences in brain and cognitive reserve, which can at least partly explain the differences in cognitive performance between individuals with similar brain pathology.
Resilience, meaning of life, and life quality
The constructs of brain reserve, cognitive reserve, and functional compensation are used to explain the preservation of cognition in the presence of (pathological) brain alterations; this capacity is also called “resilience” [135]. In a psychological sense, resilience means the “ability to overcome the difficulties experienced in the different areas of one’s life with perseverance, as well as good awareness of oneself and one’s own internal coherence by activating a personal growth project” ([125], p. 1). Resilience plays an essential role in the entire development of life, but especially in the early [47] and late stages, when personality factors also come more into play [61]. Resilience shows a stronger positive relationship with openness and agreeableness, and a stronger negative relationship with neuroticism [101]. Undoubtedly, providing and supporting the acquisition of personally suitable resilience strategies is one of the most important processes in the first phase of human life. Finding an individual meaning in life and the resulting actions and evaluations seem to be decisive for how satisfied people are or can be with their own quality of life. The final reflection of the meaning of one’s own life takes often place in older age when special events or big changes are no longer expected [43]. Of course, concerns with the limited remaining time of life and with one’s legacy as well as health and financial issues may become key themes [102], [131]. Decisive for the evaluation of one's own quality of life and its subjective assessment (life satisfaction) seem to be the values and criteria used for it. These values and criteria are, of course, essentially personal in nature, and typically comprise health, functional capacity and autonomy, emotional comfort, leisure, environmental quality, level of satisfaction, social networks, and positive social interactions, spirituality, home and neighbourhood, and financial security [20], [57], [78], [112], [143]. These values depend on and play a key role in the respective culture, society, and religion [5], [75], [77]. Furthermore, gender differences [73], [82] and cross-cultural aspects of life quality that apply to all people, also have a significant impact, regardless of their ethnic, cultural or religious affiliation. Among these aspects are: the ability to perform activities of daily living (ADL), general health, sensory abilities, mobility and autonomy and energy [26], [91], [144]. The loss of independence in ADL is a key factor affecting the quality of life in older individuals and their families.
As already mentioned, the adoption of criteria and values regarding satisfaction with and quality of life and their implementation in one's own life as well as the development of strategies begin already in childhood [48], [161]. Therefore, these processes should also be imparted and practiced in this early development phase. In a broader sense, education should not only include the acquisition of the cultural techniques of reading, writing and arithmetic and knowledge of the world and of professional activities. From childhood on, knowledge about different forms of life quality and life satisfaction, and their influences on one's own long-term mental life development, should be passed on. This knowledge should include both the corresponding semantic and procedural components that are important for implementation of appropriate coping strategies in different life situations. Based on the combination of both forms of knowledge, personalized strategies can then be developed, which ultimately result in routines and habits. Such routines and habits make it easier to cope with the various demands of life. They represent mental and behavior programs that can be used flexibly according to the actual circumstances [127]. Routine learning and habit formation play an important role in behavior change [59], in particular in health behavior [58], health-related quality of life [66] and in developing and maintaining resilience [153] and stress tolerance [150]. However, habit formation may take quite a long time of systematic repetition of the desired behavior [79], [142]; rapid effects can therefore not be expected. But it seems more than worthwhile to guide and help children and adolescents to develop, learn, optimize and maintain routines and habits that are relevant for healthy mental aging and thus also for personal quality of life (an individual's perception of their position in life in the respective cultural context and in relation to their goals, expectations, standards and concerns [57], and life satisfaction (an individual's self-evaluation of their life quality using their personal criteria [5], [78]). It should, therefore, become and be an essential part of lifelong education to train and use different adaptive coping strategies, which suit changing contexts (internally or externally driven) [100]. We all agree that every-one should be happy according to their own way and values. Happiness is a purely subjective feeling and therefore depends on what personal values a person uses to judge it for themselves as long as it is not at the expense of others and affect others in a negative way. That is why every-one should also grow old happily according to their own lifestyle and evaluation [6]. Whatever individual values a person develops and relies on, mood and motivation play a crucial role in this [34], [72], [141]. Therefore, it seems very important that the development of mood disorders, especially depression, and apathy are early recognized as early as possible and treated properly.
In summary, resilience and satisfaction with life have an influence on brain aging and strategies to build resilience and life satisfaction should be part of early and lifelong education.
Individual and general characteristics of cognitive aging
Older, like younger people, individually show very different cognitive characteristics [22], [110], [129]. Trends and average changes of cognition in older people can be derived from large group studies, but these changes cannot be validly transferred to individual subjects. Cognitive performance of older people is often compared with that of younger people, but changes in cognition may be found across a larger range of adulthood [114], and performance in a complex cognitive task can overlap in older and younger subjects [159]. Older people may still have good ability in learning and memory, particularly in collaboration with social interactions [41], and may even show improvements in attention and executive function [44], [145]. However, an increased time requirement appears to be a typical “symptom” of cognitive aging and time-dependent cognitive test performance (‘power tests’) [162] as well as cognitive activities under time pressure are often less successful and can also show more errors [115]. However, the adaptation of the individual time schedule allows a personalized prospective time-pressure management [147] and can also enhance wellbeing [2]. Notably, centenarians can still have good cognitive skills that also ensure appropriate time and task management for a sufficiently independence in daily life [13], [105]. Empirical evidence suggests not only a large inter-individual variability in cognitive aging, but also significant intra-individual differences in the trajectories of the various cognitive domains [67]. Motivation can diminish in older subjects, when self-generated, while motivation-related cognitive performance enhancements are still present [157].
In summary, cognitive aging goes often along with a slowing down of cognitive processes but this does not necessarily lead to worse cognitive or functional performance.
Mental health, cognition, and influencing factors
Following Galderisi et al. ([55], p. 408), mental health can be defined as “a dynamic state of internal equilibrium which enables individuals to use their abilities in harmony with universal values of society. Basic cognitive and social skills; ability to recognize, express and modulate one’s own emotions, as well as empathize with others; flexibility and ability to cope with adverse life events and function in social roles; and harmonious relationship between body and mind represent important components of mental health which contribute, to varying degrees, to the state of internal equilibrium”. Thus cognition, emotion, resilience, life satisfaction and social skills represent some of the most important and essential factors contributing to mental health.
Mental health and cognitive function interact in many ways through the life span. Poorer mental health (defined as anxiety and depression), social dysfunction, and loss of confidence can be associated with lower cognitive function [21], and in particular cognitive skills in social processes and interactions contribute significantly to mental health [116]. A broad range of physical, biological, lifestyle, and psychological factors are known as either protective or risk factors [49], [117]. In addition, cognitive and social activities in older age appear to depend on education level [14], but of course also on motivation for cognitive activities in general [52], [88]. Mood trajectories may also change with aging, with the most extreme (positive and negative) subgroups in older adults [133]. Negative and positive events associate differently with cognition and psychological status. A study from Northern Portugal has shown that the vast majority of older individuals report more positive than negative life events. Individuals with more reported positive events also show better cognitive performance and lower depressive mood and perceived stress compared to those who report more negative life events [25]. Personality traits do not appear to change significantly with aging and do only modestly influence longitudinal changes in cognition [119].
Regular physical, cognitive and social activities and engagement are known to have protective effects [3], [23], [24], possibly via cardiovascular fitness [130]. Postponing retirement, if possible, particularly in cognitively and socially “enriched” occupations, can also be a favourable factor [63], [155].
Among diseases, which may affect cognition and mental health in older age, hyperglycemia (supraphysiological blood sugar levels) appears crucial [9]. An important aspect of mental health, not just, but also in older age, is coping with stressful conditions, so that chronic consequences remain as low as possible. It is known that chronic stress is associated with various biological alterations, including in the brain, and can have deleterious effects on cognition [94], [121], [108]. This also applies to daily stressors [98] and permanent social stress conditions, for example, in partnerships [15]. The acquisition of helpful strategies for dealing with stress and especially for preventing chronic consequences is therefore an important component of mental health maintenance, especially mood [27], [81] and belief in control and prevention of loss of control, which are not reduced in older age [4]. Sufficient cognitive, motivational and emotional resources act as protective reserves and have a very beneficial effect on the quality of life in older age. Studies on centenarians have shown, that despite biological risk factors, cognitive abilities [13], [104] and helpful stress coping strategies [68] are preserved and can reduce the severity of mental disability [28]. Of course, functional loss of vision [138], audition [53] or motor skills [65], [143] can limit social participation and mobility, but not necessarily prevent it.
In summary, mental health and cognitive function interact with each other throughout the life span and both can be influenced by a range of factors including stress and lifestyle.
The assessment and rehabilitation of older people with impaired cognition and related difficulties
As discussed earlier, aging of the brain is also associated with mental aging. In individual cases, this can lead to an impairment relevant to everyday life, e.g. if the previous level of cognitive performance is no longer available or if mild cognitive impairment is already present. Cognitive performance and its loss is assessed with the help of standardized test procedures. The comparison of the individual test result with normative data enables the classification of the individual result as ‘above average’, ‘average’ or ‘below average’. Normative values usually take age, gender and education into account. So-called cut-off scores are used to classify a test result as “below average”. This procedure applies in particular to the distinction between ‘normal’ age-related changes in cognitive performance from mild cognitive impairment or dementia. Whichever test procedure is used and which cut-off scores are set to characterize a test result as “below average”, it always relates to the cognitive performance under standardized conditions. It should be noted, however, that the conditions for cognitive assessment may have little or no commonality with the everyday conditions and requirements of the individual [113]. It is of course correct to speak of underperformance in a cognitive test; whether this performance also means an individual handicap under more ‘real’ everyday conditions can only be assumed very indirectly. Thus, cognitive test procedures have limited and often insufficient ecological validity for such a far-reaching diagnostic conclusion, for example ‘cognitive impairment’ or ‘disability’. According to the WHO, dementia “is a syndrome, usually of a chronic or progressive nature, caused by a variety of brain illnesses that affect memory, thinking, behaviour and ability to perform everyday activities” … “there is deterioration in cognitive function beyond what might be expected from the usual consequences of biological ageing” [154]. This characterization contains two main points: (1) the loss of cognition must be (significantly) greater than the “normal” age-related cognitive changes, and (2) this loss must also (in a significant way) affect individual everyday activities, i.e. represent a personal disability. The use of screening procedures alone is definitely not sufficient for this, and does not allow any statements about (still) average and (already) below average performance in the various cognitive domains [7], [123]. For standardized cognitive tests, appropriate age-related norms are essential for the classification into “average” and “sub-average” performance [90], and follow-up examinations are required to determine changes in individual test scores over time. The second characteristic can only be provided to a limited extent by cognitive tests alone in mild and moderate cases of cognitive changes, e.g. in mild cognitive impairment or mild to moderate forms of dementia. In severe forms of dementia, cognitive difficulties become manifest in nearly all everyday life activities, and standardized tests can no longer be carried out. Systematic behavior observations and surveys are important and helpful amendments for the evaluation of cognitive difficulties in everyday activities and requirements, whereby the latter should also include the family and caregivers [42], [103], [139], [158].
Cognitive rehabilitation of older subjects with cognitive impairment usually consists as a kind of mental exercise using guided practice with tasks that reflect particular cognitive functions, such as perception, attention, memory, problem-solving or multi-tasking. In neurorehabilitation after acquired brain injury, age is an important general predictor for long-term outcome [18], [70]. This statistical evidence does not mean, however, that there is no success even in very old subjects and that the rehabilitation effort is less justified than in younger patients [83]. Unfortunately, the influence of age is rarely considered in neuropsychological rehabilitation studies because of the statistical comparability between groups (e.g. treatment vs waiting group), and is even neglected in meta-analyses on neuropsychological treatment effects. Interestingly, some studies have shown no age-specific influence on the treatment outcome or the long-term course, e.g. in visual perception [160], attention and global functional capacities (ADL) [1], [10].
In case of reduced cognitive functions and resulting difficulties in ADL, i.e. in mild cognitive impairment and mild to moderate dementia, training may be supportive for improving cognition. However, evidence for the efficacy of such practice regimes is still preliminary and controversial [80], [156]. Technologies for the remediation of cognitive impairments may be useful, for specific personalized training, when optimized for portable devices, and user-friendly [71]. Music activities in the broadest sense can offer a rich mean for cognition (particularly attention and memory), health and wellbeing independent of age, background, and setting [46].
In summary, the assessment of cognitive function is based on standardized tests and cut-offs that not always reflect the ability to carry out everyday activities. Cognitive rehabilitation programs can be beneficial for improving cognition, but more research is needed on age-specific influence of these programs.
Cognitive performance and functional cognition
As mentioned above, cognitive performance as assessed with standardized tests alone, may not show meaningful ecological significance for the individual. Therefore, such test results cannot be used to reliably infer the availability or impairment of cognitive functions in ADL. In milder forms of cognitive decline, the determination of the “critical minimum” of cognition actually required in the individual life situation appears to be more suitable for the valid assessment of the degree of cognitive disability. For this, a systematic survey of the individual everyday requirements in the relevant areas of life is necessary, especially in the case of older people. Interestingly, even centenarians may still possess cognitive functional capacity for coping with everyday life challenges [87]. The systematic investigation of individual living conditions in older age and their cognitive requirements, taking into account the previous acquired executive strategies and habits, could lead to a catalog that focuses on functional cognition that is based on ecologically valid measures. Functional (or also instrumental) cognition can then be used to describe the actual use of a person's cognitive abilities in different situations and/or environments. The focus is therefore on the importance of the individually available cognitive abilities and skills in activities of daily life [93], [151]. Systematic observation and the diagnostic assessment should, therefore, be based on the specific use of the existing cognitive capacities in everyday situations without and/or with assistance. The assessment of functional cognition could be part of a more general functional assessment in older people [109]. While assessments of cognitive function are standardized with the use of objective neuropsychological tests, objective assessments of functional performance or functional cognition are limited and not standard in clinical practice, partly due to constraints in time and resources, and lack of standardised processes [97]. However, reliable and objective assessments of functional ability and change over time are critical to monitor decline to enable focussed support and intervention, and to monitor improvement after targeted interventions.
In summary, functional cognition refers to how an individual integrates cognition to accomplish everyday activities. Longitudinal assessments of functional cognition are important to monitor change over time.
Bridging the interdisciplinary gaps in future research strategies
Which central topics for mentally healthy aging seem important for future research, but also for social and health services and institutions and for health policy? From what has been said so far, it follows that non-pharmacological preventive measures can make a significant contribution to maintaining cognitive functions in older people. Preventive measures in the mental area include cognitive strategies, routines and habits that enable the individual to master the challenges of life and to acquire and maintain a good quality of life. These preventive measures refer to aspects of both, the physical and mental health. However, you shouldn't start when you've gotten old, but rather already in childhood and adolescence in an appropriate form [99]. But even if there is cognitive impairment in older age, improvements can be sometimes achieved through suitable treatment [8], [24], [76], [152], [156].
There are numerous scientific findings on mental aging in basic neurobiological research and in medical, psychological and social applications. For the future cognitive and mental age research it would be very desirable that all basic and applied disciplines engaged in aging research cooperate more closely to guarantee an early, successful translation of the scientific findings into more ‘real’ life conditions of older people. At the same time, bridges between science and in health and social policies should be increased in number and widened to further reduce the gaps between science and translation to the reality of older age [45], [50], [132]. The integration of brain, mind, and biological body factors with the aim of greater applicability, particularly in clinical conditions, appears a crucial prerequisite for future comprehensive research on aging [32]. Cox & Deary [36] recommend a “multidisciplinary openness”, whereby “the collaboration has to work; there is no point in collaborating with a specialism with which one cannot shake hands; there should be no understanding gap in the collaboration. Not all new variables will make a contribution (p. 7). In addition, these authors endorse the recruitment of large and more diverse subject samples, because only multiple small group effects are to be expected, and a broader search for explanatory variables. Large samples with large variation in variables would also allow specific subgroups to be discovered, defined and then examined separately with regard to special characteristics or profiles. The essential prerequisite for this is the consideration of as many biological and non-biological variables as possible in an approach that is as holistic as possible. This would mean setting a mandatory minimum of aging characteristics for multidisciplinary studies. In the second step, the individual disciplines can then use their respective subject-specific methods to characterize the subgroups defined in this way more precisely. As far as possible, all variables should be taken into account in order to be able to make general statements about the (favorable or unfavorable) influence of these variables on aging processes. Such an approach would also represent a valid basis for modeling aging processes and courses. For studies with large samples as well as for studies with smaller specific groups, a close linking of all research disciplines involved from planning to implementation, data analysis and classification of the results is desirable. Of course, each research discipline has its own specific approach and research methods, and pursues its own research goals with different outcome variables. However, the combination of the different, complementary approaches fits better to a complex topic such as mental aging because it focuses on the human being as a whole. Finally, the individual research contributions should (be able to) be classified in a higher-level, more holistic context of ageing. An important prerequisite for multidisciplinary and cooperative research this should be the interdisciplinary scientific training, especially of young scientists, and close networking between research groups of the disciplines involved. Of course, it must be taken into account that a broad research approach always requires a higher expenditure in terms of personnel, money and time and the establishment and safeguarding of the required project organization. On the other hand, in practice, it must be possible to reliably classify the individual test results for mental functions, taking into account the influencing variables. Of course, this means that these influencing variables are also known in individual cases.
Based on the existing empirical evidence, prevention and exercise programs also appear to have a beneficial effect in old age. It seems important, however, that such programs are also checked for ecological validity and functional significance. Smart technologies can assist older people and can help to facilitate and maintain their own independence [92], but their ecological validity must be demonstrated. In addition, a valid measurement of reserve/resilience in aging may help to better assess and understand this obviously important factor, and to implement early measures for prevention [17]. Finally, for as complete an understanding as possible, the influence of genetic factors in addition to environmental factors on diverse trajectories of human aging, and their interaction, should also be taken into account in aging research [40].
As discussed earlier, cultural factors play an important role in understanding and dealing with mental aging and values about quality of life. Cultural differences should therefore be considered when evaluating differing research results, because they cannot be compared directly. However, differing study outcomes can be used to gain valuable suggestions for one's own cultural area. Interestingly, there are shared cross-cultural meanings of quality of life, both in personal and in more general terms. Personal indicators include emotional and physical well-being, interpersonal relations and social inclusion, financial well-being, and self-determination [120]. The more general indicators include spiritual qualities on meaning in life, awe and wonder, wholeness and integration, and kindness to others [126]. In contrast, in mental health the different cultural factors play a major role [60], [124]. Taking these criteria into account would certainly also be helpful when dealing with older people and their problems, especially under pathological conditions, e.g. dementia, and should be included especially in applied aging research as well as in clinical practice. Health systems need to ensure access to assessment and care focusing on the needs, rights, culture, and capabilities of older individuals.
A higher age is associated with cognitive, mental and physical changes, but older people can retain their individuality and personality, which is also made up of their life history and individual experiences. That is why personalized programs are important for maintaining functionality in everyday life. However, this also implies that older people accept such offers and (are able to) translate them into their personal lives. To be curious about and interested in problem solving and flexible adjustments of routines and habits to the age-related requirements is supportive for coping with everyday challenges. This attitude is acquired at an early stage in life, but should be further developed, depending on the respective individual requirements and necessities. The development and adaptation of routines and habits, and their continuous optimization in the context of current living conditions and their challenges requires the flexible use of cognitive reserves under the guidance of executive functions, including development, selection and use of current problem solutions and adaptation strategies, error control and, if necessary, error correction. Motivation for cognition and the emotional (positive and negative) evaluation of one’s own routines and habits play a powerful role in this groundbreaking developmental process. The positive or negative confirmation of successful action acts as an amplifier in reinforcement learning of action routines [19] and is based on a widespread system of potential reward in the brain [85]. In this context, the assessment of aging attitudes of an individual may assist in the holistic assessment of mental aging. Aging attitudes can be changed and are a potential target for intervention to reduce negative aging attitudes and enforce positive aging experiences [122].
The functional adaptation to the various objective and subjective challenges of life is a highly complex, dynamic process that requires appropriate mental resources. The magic word is learning; learning means regular practice, which is seldom possible without exertion. Learning in terms of adaptation of functional abilities to changing life conditions is still possible in older age [29], [107]. However, it is important that learning goals are set in such a way that they are individually meaningful and necessary, and remain feasible. Despite the age-related biological and mental changes, growing older is a normal process, which can be positively influenced and does not have to be negative, fateful process.
In summary, interdisciplinary collaboration in aging research and closing the gap between research findings and their application in practice and policy is crucial to advance progress in this area.
Conclusion
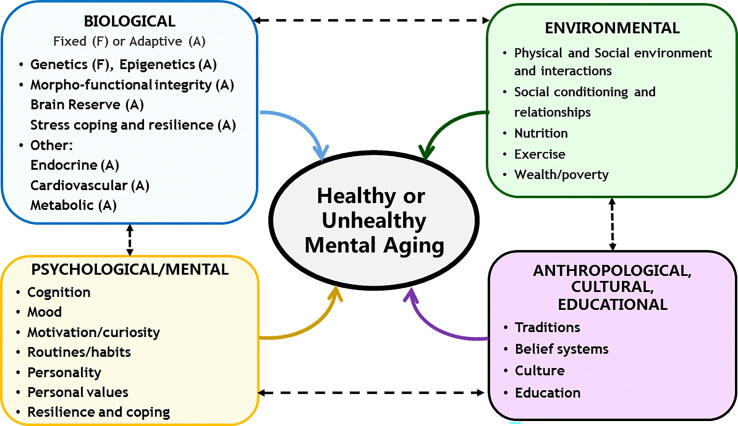
This contribution aimed to provide a holistic overview of the aging mind. When assessing the aging mind and brain, cognition is just one of many mental functions. Cognitive reserve, resilience, functional cognition, and life satisfaction, but also biological, mental, environmental and anthropological, cultural and educational factors are important aspects that have an impact of an individual’s brain aging. In Fig. 1, some of the main factors contributing to healthy and unhealthy mental aging, and their interactions, are summarized. Each of these factors contributes significantly to aging of the mind, however, the various direct and indirect interactions between these factors are just as decisive for the favorable or unfavorable development of mental health in aging. The success of the joint interdisciplinary efforts to understand the various processes involved in mental aging will also determine how well these complex relationships can be dealt with in research and practice.
Fig. 1.
Some of the main factors contributing to healthy and unhealthy mental aging, and their interactions.
Promotion and funding of multidisciplinary research is an important step to advance knowledge and progress in this area. Not only collaboration between basic and applied research and professions but also timely knowledge translation to clinical practice and policy is recommended.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Abd-Elaziz S A-E, Khedr EM, Ahmed HAE, Ibrahim HDF (2015) Effect of cognitive rehabilitation on improving cognitive function and activities of daily living among elderly patients with stroke at Assiut University Hospital. J Educ Practice 6: 24. ISSN (Paper) 2222-1735 ISSN (Online) 2222-288X.
- 2.Aeon B, Faber A, Panaccio A (2021) Does time management work? A meta-analysis. PLoS One. 16: e0245066. doi: 10.1371/journal.pone.0245066. [DOI] [PMC free article] [PubMed]
- 3.Aftab A., Lee E.E., Klaus F., Daly R., Wu T.-C., Tu X., et al. Meaning in life and its relationship with physical, mental, and cognitive functioning: A study of 1,042 community-dwelling adults across the lifespan. J Clin Psychiatry. 2019;81(1) doi: 10.4088/JCP.19m13064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aldwin Does age affect the stress and coping process? Implications of age differences in perceived control. J Gerontol. 1991;46:174–180. doi: 10.1093/geronj/46.4.p174. [DOI] [PubMed] [Google Scholar]
- 5.Angelini V., Cavapozzi D., Corazzini L., Paccagnella O. Age, health and life satisfaction among older Europeans. Soc Indic Res. 2012;105:293–308. doi: 10.1007/s11205-011-9882-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Araujo L., Teixeira L., Afonso R.M., Ribeiro O. To live or to die: What to wish at 100 years and older. Front Psychol. 2021;12 doi: 10.3389/fpsyg.2021.726621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arevalo-Rodriguez I, Smailagic N, Roqué i Figuls M, Ciapponi A, Sanchez-Perez E, et al. (2015) Mini-Mental State Examination (MMSE) for the detection of Alzheimer’s disease and other dementias in people with mild cognitive impairment (MCI). Cochrane Database Syst Rev 3: CD010783. doi: 10.1002/14651858.CD010783.pub2. [DOI] [PMC free article] [PubMed]
- 8.Arida R.M., Teixeira-Machado L. The contribution of physical exercise to brain resilience. Front Behav Neurosci. 2021;14 doi: 10.3389/fnbeh.2020.626769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Assuncao N, Sudo FK, Drummond C, Guarina de Felice F, Mattos P (2018) Metabolic Syndrome and cognitive decline in the elderly: A systematic review. PLoS ONE 13(3): e0194990. doi. org/10.1371/journal.pone.0194990. [DOI] [PMC free article] [PubMed]
- 10.Bagg S., Pombo A.P., Hopman W. Effect of age on functional outcomes after stroke rehabilitation. Stroke. 2002;33:179–185. doi: 10.1161/hs0102.101224. [DOI] [PubMed] [Google Scholar]
- 11.Bangsbo J., Blackwell J., Boraxbekk C.-J., Caserotti P., Dela F., Evans A.B., et al. Copenhagen Consensus statement 2019: Physical activity and ageing. Br J Sports Med. 2019;53(14):856–858. doi: 10.1136/bjsports-2018-100451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barulli D., Stern Y. Efficiency, capacity, compensation, maintenance, plasticity: emerging concepts in cognitive reserve. Trends Cogn Sci. 2013;17(10):502–509. doi: 10.1016/j.tics.2013.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Beker N, Sikkes SAM, Hulsman M, Tesi N, van der Lee SJ, et al. Longitudinal maintenance of cognitive health in centenarians in the 100-plus study. JAMA Network Open 2020;3(2):e200094. doi: 10.1001/jamanetworkopen.2020.0094. [DOI] [PMC free article] [PubMed]
- 14.Belo P., Navarro-Pardo E., Pocinho R., Carrana P., Margarido C. Relationship between mental health and the education level in elderly people: Mediation of leisure attitude. Front Psychol. 2020;11:573. doi: 10.3389/fpsyg.2020.00573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Birditt K.S., Newton N., Hope S. Implications of marital/partner relationship quality and perceived stress for blood pressure among older adults. J Gerontol B Psychol Sci Soc Sci. 2014;69:188–198. doi: 10.1093/geronb/gbs123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bjørkløf G.H., Engedal K., Selbæk G., Kouwenhoven S.E., Helvik A.S. Coping and depression in old age: A literature review. Dement Geriatr Cogn Disord. 2013;35:121–154. doi: 10.1159/000346633. [DOI] [PubMed] [Google Scholar]
- 17.Bocancea D.I., van Loenhoud A.C., Groot C., Barkhof F., van der Flier W.M., Ossenkoppele R. Measuring resilience and resistance in aging and Alzheimer Disease using residual methods. A systematic review and meta-analysis. Neurology. 2021;97(10):474–488. doi: 10.1212/WNL.0000000000012499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Boltzmann M., Schmidt S.B., Gutenbrunner C., Krauss J.K., Höglinger G.U., et al. One-year outcome of brain injured patients undergoing early neurological rehabilitation: A prospective observational study. BMC Neurol. 2022;22:30. doi: 10.1186/s12883-022-02549-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Botvinick M.M., Niv Y., Barto A.C. Hierarchically organized behavior and its neural foundations: A reinforcement-learning perspective. Cognition. 2009;113:262–280. doi: 10.1016/j.cognition.2008.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bowling A. Enhancing later life: How older people perceive active ageing? Aging Ment Health. 2008;12:293–301. doi: 10.1080/13607860802120979. [DOI] [PubMed] [Google Scholar]
- 21.Bunce D., Tzur M., Ramchurn A., Gain F., Bond F.W. Mental health and cognitive function in adults aged 18 to 92 years. J Gerontol B Psychol Sci Soc Sci. 2008;63:67–74. doi: 10.1093/geronb/63.2.P67. [DOI] [PubMed] [Google Scholar]
- 22.Cabeza R., Albert M., Belleville S., Craik F.I.M., Duarte A., Grady C.L., et al. Maintenance, reserve and compensation: The cognitive neuroscience of healthy ageing. Nat Rev Neurosci. 2018;19(11):701–710. doi: 10.1038/s41583-018-0068-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Carr K., Weir P. A conceptual model of engagement profiles throughout the decades of older adulthood. Front Psychol. 2019;10:2535. doi: 10.3389/fpsyg.2019.02535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Carvalho A, Rea IM, Parimon T, Cusack, BJ. Physical activity and cognitive function in individuals over 60 years of age: A systematic review. Clin Interv Aging 2014;9:661–682. dx.doi.org/10.2147/CIA.S55520. [DOI] [PMC free article] [PubMed]
- 25.Castanho TC, Santos NC, Meleiro-Neves C, Neto S, Moura GR, et al. Association of positive and negative life events with cognitive performance and psychological status in late life: A cross-sectional study in Northern Portugal. Aging Brain 2021;1:100020. doi.org/10.1016/j.nbas.2021.100020. [DOI] [PMC free article] [PubMed]
- 26.Cené C.W., Dilworth-Anderson P., Leng I., Garcia L., Benavente V., Rosal M., et al. Correlates of successful aging in racial and ethnic minority women age 80 years and older: Findings from the Women's Health Initiative. J Gerontol A Biol Sci Med Sci. 2016;71(Suppl 1):S87–S99. doi: 10.1093/gerona/glv099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chen Y., Peng Y., Xu H., O’Brien W.H. Age differences in stress and coping: Problem-focused strategies mediate the relationship between age and positive affect. Int J Aging Hum Dev. 2018;86:347–363. doi: 10.1177/0091415017720890. [DOI] [PubMed] [Google Scholar]
- 28.Christensen K, McGue M, Petersen I, Jeune B, Vaupel JW. Exceptional longevity does not result in excessive levels of disability. PNAS 2008;105:13274–13279. doi.org/10.1073_pnas.0804931105. [DOI] [PMC free article] [PubMed]
- 29.Clark R., Freedberg M., Hazeltine E., Voss M.W. Are there age-related differences in the ability to learn configural responses? PLoS One. 2015;10(8):e0137260. doi: 10.1371/journal.pone.0137260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Coelho A., Fernandes H.M., Magalhães R., Moreira P.S., Marques P., Soares J.M., et al. Reorganization of brain structural networks in aging: A longitudinal study. J Neurosci Res. 2021;99(5):1354–1376. doi: 10.1002/jnr.24795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Coelho A., Fernandes H.M., Magalhães R., Moreira P.S., Marques P., Soares J.M., et al. Signatures of white-matter microstructure degradation during aging and its association with cognitive status. Sci Rep. 2021;11(1) doi: 10.1038/s41598-021-83983-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cole J.H., Marioni R.E., Harris S.E., Deary I.J. Brain age and other bodily ‘ages’: Implications for neuropsychiatry. Mol Psychiatry. 2019;24:266–281. doi: 10.1038/s41380-018-0098-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cornelis MC, Wang Y, Holland T, Agarwal P, Weintraub S et al. Age and cognitive decline in the UK Biobank. PLoS ONE 2019;14(3):e0213948. doi.org/10.1371/journal. [DOI] [PMC free article] [PubMed]
- 34.Cotter D.L., Walters S.M., Fonseca C., Wolf A., Cobigo Y., Fox E.C., et al. Aging and positive mood: Longitudinal neurobiological and cognitive correlates. Am J Geriatr Psychiatry. 2020;28(9):946–956. doi: 10.1016/j.jagp.2020.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Coupé P., Catheline G., Lanuza E., Manjón J.V. Towards a unified analysis of brain maturation and aging across the entire lifespan: A MRI analysis. Hum Brain Mapp. 2017;38(11):5501–5518. doi: 10.1002/hbm.23743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cox S.R., Deary I.J. Brain and cognitive ageing: The present, and some predictions (. about the future) Aging Brain. 2022;2 doi: 10.1016/j.nbas.2022.100032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Crivello F, Tzourio-Mazoyer N, Tzourio C, Mazoyer B. Longitudinal assessment of global and regional rate of grey matter atrophy in 1,172 healthy older adults: Modulation by sex and age. PLoS ONE 2014;9:e114478. doi: 10.1371/journal.pone.0114478. [DOI] [PMC free article] [PubMed]
- 38.Davidson PSR, Winocur G. Aging and cognition. In Reference Module in Neuroscience and Biobehavioral Psychology, Elsevier; 2017. doi: 10.1016/B978-0-12-809324-5.00252-2.
- 39.Debette St, Markus HS. The clinical importance of white matter hyperintensities on brain magnetic resonance imaging: Systematic review and meta-analysis. BMJ 2010;341:c3666. doi: 10.1136/bmj.c3666. [DOI] [PMC free article] [PubMed]
- 40.Demeneix B.A. Environmental influences on brain aging. Aging Brain. 2021;1 doi: 10.1016/j.nbas.2020.100003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Derksen B.J., Duff M.C., Weldon K., Zhang J., Zamba K.D., Tranel D., et al. Older adults catch up to younger adults on a learning and memory task that involves collaborative social interaction. Memory. 2015;23(4):612–624. doi: 10.1080/09658211.2014.915974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Devi J. The scales of functional assessment of Activities of Daily Living in geriatrics. Age Ageing. 2018;47:500–502. doi: 10.1093/ageing/afy050. [DOI] [PubMed] [Google Scholar]
- 43.Dewitte L., Dezutter J. Meaning reflectivity in later life: The relationship between reflecting on meaning in life, presence and search for meaning, and depressive symptoms in older adults over the age of 75. Front Psychol. 2021;12 doi: 10.3389/fpsyg.2021.726150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Diamond A. Executive functions. Annu Rev Psychol. 2013;64:135–168. doi: 10.1146/annurev-psych-113011-143750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Di Luca M., Destrebecq F., St K. Future of the ageing brain: Bridging the gap between research and policy. Aging Brain. 2021;1 doi: 10.1016/j.nbas.2020.100002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dingle G.A., Sharman L.S., Bauer Z., Beckman E., Broughton M., Bunzli E., et al. How do music activities affect health and well-being? A scoping review of studies examining psychosocial mechanisms. Front Psychol. 2021;12 doi: 10.3389/fpsyg.2021.713818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ellis B.J., Bianchi J.M., Griskevicius V., Frankenhuis W.E. Beyond risk and protective factors: An adaptation-based approach to resilience. Perspect Psychol Sci. 2017;12:561–587. doi: 10.1177/1745691617693054. [DOI] [PubMed] [Google Scholar]
- 48.Eschenbeck H., St S., Schroeder I., Wasserfall N., Kohlmann C.-W. Development of coping strategies from childhood to adolescence: Cross-sectional and longitudinal trends. Eur J Health Psychol. 2015;25:18–30. doi: 10.1027/2512-8442/a000005. [DOI] [Google Scholar]
- 49.Feng Z, Lugtenberg M, Franse C, Fang X, Hu S, et al. Risk factors and protective factors associated with incident or increase of frailty among community-dwelling older adults: A systematic review of longitudinal studies. PLoS ONE 2017;12(6):e0178383. doi.org/10.1371/journal.pone.0178383. [DOI] [PMC free article] [PubMed]
- 50.Fishman J.R., Binstock R.H., Lambrix R.H. Anti-aging science: The emergence, maintenance, and enhancement of a discipline. J Aging Stud. 2008;22:295–303. doi: 10.1016/j.jaging.2008.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fjell AM, Westlye LT, Grydeland H, Amlien I, Espeseth T, et al. Accelerating cortical thinning: Unique to dementia or universal in aging? Cereb Cortex 2014;24:919–934. doi: 10.1093/cercor/bhs379. [DOI] [PMC free article] [PubMed]
- 52.Forstmeier S., Maercker A. Motivational Reserve: Lifetime motivational abilities contribute to cognitive and emotional health in old age. Psychol Aging. 2008;23:886–899. doi: 10.1037/a0013602. [DOI] [PubMed] [Google Scholar]
- 53.Fortunato S., Forli F., Guglielmi V., De Corso E., Paludetti G., et al. A review of new insights on the association between hearing loss and cognitive decline in ageing. Acta Otorhinolaryngol Ital. 2016;36:155–166. doi: 10.14639/0392-100X-993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Friedman V.A., Carr D., Cornman J.C., Lucas R.E. Aging, mobility impairments and subjective wellbeing. Disabil Health J. 2017;10:525–531. doi: 10.1016/j.dhjo.2017.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Galderisi S., Heinz A., Kastrup M., Beezhold J., Sartorius N. A proposed new definition of mental health. Psychiatr Pol. 2017;51:407–411. doi: 10.12740/PP/74145. [DOI] [PubMed] [Google Scholar]
- 56.Galiana L., Tomás J.M., Fernández I., Oliver A. Predicting well-being among the elderly: The role of coping strategies. Front Psychol. 2020;11:616. doi: 10.3389/fpsyg.2020.00616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Garcia L.M.R., Navarrro J.M.R. The impact of quality of life on the health of older people from a multidimensional perspective. J Aging Res. 2018;2018:4086294. doi: 10.1155/2018/4086294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gardner B., Lally P.h., Wardle J. Making health habitual: The psychology of ‘habit- formation’ and general practice. Br J Gen Pract. 2012;62(605):604–666. doi: 10.3399/bjgp12X659466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Gardner B, Rebar AL. Habit formation and behaviour change. In OREs, Psychology. Oxford: Oxford University Press; 2019. doi.org/10.1093/acrefore/9780190236557.013.129.
- 60.Gopalkrishnan N. Cultural diversity and mental health: Considerations for policy and practice. Front Public Health. 2018;6:179. doi: 10.3389/fpubh.2018.00179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Graham EK, James BD, Jackson KL, Willroth EC, Boyle P, et al. Associations between personality traits and cognitive resilience in older adults. J Gerontol B Psychol Sci Soc Sci 2021;76:6–19. doi: 10.1093/geronb/gbaa135. [DOI] [PMC free article] [PubMed]
- 62.Green A.F., Rebok G., Lyketsos C.G. Influence of social network characteristics on cognition and functional status with aging. Int J Geriatr Psychiatry. 2008;23:972–978. doi: 10.1002/gps.2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hale J.M., Bijlsma M.J., Lorenti A. Does postponing retirement affect cognitive function? A counterfactual experiment to disentangle life course risk factors. SSM - Population Health. 2021;15 doi: 10.1016/j.ssmph.2021.100855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hjelmborg J.vB., Iachine I., Skytthe A., Vaupel J.W., McGue M., Koskenvuo M., et al. Genetic influence on human lifespan and longevity. Hum Genet. 2006;119(3):312–321. doi: 10.1007/s00439-006-0144-y. [DOI] [PubMed] [Google Scholar]
- 65.Hoogendam Y.Y., van der Lijn F., Vernooij M.W., Hofman A., Niessen W.J., van der Lugt A., et al. Older age relates to worsening of fine motor skills: A population-based study of middle-aged and elderly Persons. Front Aging Neurosci. 2014;6 doi: 10.3389/fnagi.2014.00259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hörder H., Skoog I., Frändin K. Health-related quality of life in relation to walking habits and fitness: A population-based study of 75-year-olds. Qual Life Res. 2013;22:1213–1223. doi: 10.1007/s11136-012-0267-7. [DOI] [PubMed] [Google Scholar]
- 67.Hülür G., Ram N., Willis L., Schaie K.W., Gerstorf D. Cognitive aging in the Seattle Longitudinal Study: Within-person associations of primary mental abilities with psychomotor speed and cognitive flexibility. J Intell. 2016;4:12. doi: 10.3390/jintelligence4030012. [DOI] [Google Scholar]
- 68.Hutnik N., Smith P., Koch T. Using cognitive behaviour therapy to explore resilience in the life-stories of 16 UK centenarians. NursingOpen. 2016;23:110–118. doi: 10.1002/nop2.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ince P.G. Pathological correlates of late-onset dementia in a multicentre, community-based population in England and Wales. Neuropathology Group of the Medical Research Council Cognitive Function and Ageing Study (MRC CFAS) Lancet. 2001;357(9251):169–175. doi: 10.1016/s0140-6736(00)03589-3. [DOI] [PubMed] [Google Scholar]
- 70.Iosa M., Morone G., Antonucci G., Paolucci S. Prognostic factors in neurorehabilitation of stroke: A comparison among regression, neural network, and cluster analyses. Brain Sci. 2021;11:1147. doi: 10.3390/brainsci11091147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Irazoki E., Contreras-Somoza L.M., Toribio-Guzmán J.M., Jenaro-Rio C., van der Roest H., et al. Technologies for cognitive training and cognitive rehabilitation for people with mild cognitive Impairment and dementia. A systematic review. Front Psychol. 2020;11:648. doi: 10.3389/fpsyg.2020.00648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Jenkins A., Tree J.J., Thornton I.M., Tales A. Subjective cognitive impairment in 55–65-year-old adults is associated with negative affective symptoms, neuroticism, and poor quality of life. J Alzheimer’s Dis. 2019;67:1367–1378. doi: 10.3233/JAD-180810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kaplan R.M., Anderson J.P., Wingard D.L. Gender differences in health-related quality of life. Health Psychol. 1991;10:86–93. doi: 10.1037//0278-6133.10.2.86. [DOI] [PubMed] [Google Scholar]
- 74.Kawagoe T. Overview of (f)MRI Studies of cognitive aging for non-experts: Looking through the lens of neuroimaging. Life. 2022;12:416. doi: 10.3390/life12030416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kitayama S., Berg M., Chopick W. Culture and wellbeing in late adulthood: Theory and Evidence. Am Psychol. 2020;75:567–576. doi: 10.1037/amp0000614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Klimova B., Valis M., Kuca K. Cognitive decline in normal aging and its prevention: A review on non-pharmacological lifestyle strategies. Clin Interv Aging. 2017;12:903–910. doi: 10.2147/CIA.S132963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kraal A.Z., Sharifian N., Zaheed A.B., Sol K., Zahodne L.B. Dimension of religious involvement represent positive pathways in cognitive ageing. Res Aging. 2019;41:868–890. doi: 10.1177/0164027519862745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kutubaeva R.Z. Analysis of life satisfaction of the elderly population on the example of Sweden, Austria and Germany. Popul Econ. 2019;3:102–116. doi: 10.3897/popecon.3.e47192. [DOI] [Google Scholar]
- 79.Lally P.h., van Jaarsveld C.H.M., Potts H.W.W., Wardle J. How are habits formed: Modelling habit formation in the real world. Eur J Soc Psychol. 2009;40:998–1009. doi: 10.1002/ejsp.674. [DOI] [Google Scholar]
- 80.Langa K.M., Levine D.A. The diagnosis and management of mild cognitive impairment: A clinical review. JAMA. 2014;312:2551–2561. doi: 10.1001/jama.2014.13806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Lazarus R.S., DeLongis A. Psychological stress and coping in aging. Am Psychol. 1983;38:245–254. doi: 10.1037/0003-066X.38.3.245. [DOI] [PubMed] [Google Scholar]
- 82.Lee K.H., Hanzhang X., Wu B. Gender differences in quality of life among community-dwelling older adults in low- and middle-income countries: Results from the Study on global AGEing and adult health (SAGE) BMC Public Health. 2020;20:114. doi: 10.1186/s12889-020-8212-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Lieberman D., Lieberman D. Rehabilitation following stroke in patients aged 85 and above. JRRD. 2005;42:47–54. doi: 10.1682/JRRD.2004.01.0001. [DOI] [PubMed] [Google Scholar]
- 84.Lin C., Lin E., Lane H.Y. Genetic biomarkers on age-related cognitive decline. Front Psychiatry. 2017;8:247. doi: 10.3389/fpsyt.2017.00247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Lowet A.S., Zheng Q., Matias S., Drugowitsch J., Uchida N. Distributional reinforcement learning in the brain. Trends Neurosci. 2020;43:980–997. doi: 10.1016/j.tins.2020.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Marcum C.S. Age differences in daily social activities. Res Aging. 2014;35:612–640. doi: 10.1177/0164027512453468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Martin P., MacDonald M., Margrett J., Siegler I., Poon L.W. Correlates of functional capacity among centenarians. J Appl Gerontol. 2013;32:324–346. doi: 10.1177/0733464811420563. [DOI] [PubMed] [Google Scholar]
- 88.Mather M., Carstensen L.L. Aging and motivated cognition: The positivity effect in attention and memory. Trends Cogn Sci. 2005;9:496–502. doi: 10.1016/j.tics.2005.08.005. [DOI] [PubMed] [Google Scholar]
- 89.McGarrigle C.A., Ward M., Kenny R.A. Negative aging perceptions and cognitive and functional decline: Are you as old as you feel? J Am Geriatr Soc. 2022;70:777–788. doi: 10.1111/jgs.17561. [DOI] [PubMed] [Google Scholar]
- 90.Melikyan Z.A., Corrada M.M., Dick M.B., Whittle C., Paganini-Hill A., Kawas C.H. Neuropsychological test norms in cognitively intact oldest-old. J Int Neuropsychol Soc. 2019;25(05):530–545. doi: 10.1017/S1355617719000122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Molzahn A.E., Kalfoss M., Schick Makaroff K., Skevington S.M. Comparing the importance of different aspects of quality of life to older adults across diverse cultures. Age Ageing. 2011;40:192–199. doi: 10.1093/ageing/afq156. [DOI] [PubMed] [Google Scholar]
- 92.Morris M.E., Adair B., Miller K., Ozanne E., Hansen R., et al. Smart-home technologies to assist older people to live at home. Aging Sci. 2013;1:1. doi: 10.4172/jasc.1000101. [DOI] [Google Scholar]
- 93.Muir Giles G, Farrar Edwards D, Baum C, Furniss J, Skidmore E, et al. Health Policy Perspectives – Making functional cognition a professional priority. Am J Occup Ther 2020;74:7401090010p1–7401090010p6. doi.org/10.5014/ajot.2020.741002. [DOI] [PMC free article] [PubMed]
- 94.Munoz E, Sliwinki MJ, Scott SB, Hofer S. Global perceived stress predicts cognitive change among older adults. Psychol Aging 2015;30:487–499. doi: 10.37/pag0000036. [DOI] [PMC free article] [PubMed]
- 95.Nakagawa T, Jirsa VK, Spiegler A, McIntosh AR, Deco G. Bottom up modeling of the connectome: Linking structure and function in the resting brain and their changes in aging. NeuroImage 2013;80:318–329. dx.doi.org/10.1016/j.neuroimage.2013.04.055. [DOI] [PubMed]
- 96.Negash S., Wilson R.S., Leurgans S.E., Wolk D.A., Schneider J.A., et al. Resilient brain aging: Characterization of discordance between Alzheimer’s Disease pathology and cognition. Curr Alzheimer Res. 2013;10:844–851. doi: 10.2174/15672050113109990157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Nicosia F.M., Spar M.J., Steinman M.A., Lee S.J., Brown R.T. Making Function Part of the Conversation: Clinician Perspectives on Measuring Functional Status in Primary Care. J Am Geriatr Soc. 2019;67:493–502. doi: 10.1111/jgs.15677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.O’Brien EL, Torres GE, Neupert SD. Cognitive interference in the context of daily stressors, daily awareness of age-related change, and general aging attitudes. J Gerontol B Psychol Sci Soc Sci 2021;76:920–929. doi: 10.1093/geronb/gbaa155. [DOI] [PMC free article] [PubMed]
- 99.O’Connor C, Dyson J, Cowdell F, Watson R. Do universal school-based mental health promotion programmes improve the mental health and emotional wellbeing of young people? A literature review. J Clin Nurs 2018;27:e412-e426. doi: 10.1111/jocn.14078. [DOI] [PubMed]
- 100.O’Reilly Svirydzenka N., Adams S., Dogra N. Review of mental health promotion interventions in school. Soc Psychiatry Psychiatr Epidemiol. 2018;53:647–662. doi: 10.1007/s00127-018-1530-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Oshio A., Taku K., Hirano M., Saeed G. Resilience and Big Five personality traits: A meta-analysis. Pers Individ Differ. 2018;127:54–60. doi: 10.1016/j.paid.2018.01.048. [DOI] [Google Scholar]
- 102.Pachana N.A., Baumeister R.F. Better later than never: Meaning in late life. Front Psychol. 2021;12 doi: 10.3389/fpsyg.2021.693116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Pashmdarfard M., Azad A. Assessment tools to evaluate Activities of Daily Living (ADL) and Instrumental Activities of Daily Living (IADL) in older adults: A systematic review. Med J Islam Repub Iran. 2020;34:33. doi: 10.34171/mjiri.34.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Perls T. Centenarians who avoid dementia. Trends Neurosci. 2004;27:633–636. doi: 10.1016/j.tins.2004.07.012. [DOI] [PubMed] [Google Scholar]
- 105.Perls T.T. Cognitive trajectories and resilience in centenarians—findings from the 100-plus study. JAMA Netw Open. 2021;4(1):e2032538. doi: 10.1001/jamanetworkopen.2020.32538. [DOI] [PubMed] [Google Scholar]
- 106.Pfefferbaum A., Rohlfing T., Rosenbloom M.J., Chu W., Colrain I.M., Sullivan E.V. Variation in longitudinal trajectories of regional brain volumes of healthy men and women (ages 10 to 85years) measured with atlas-based parcellation of MRI. Neuroimage. 2013;65:176–193. doi: 10.1016/j.neuroimage.2012.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Poon L.W., Jazwinski M., Green R.C., Woodard J., Martin P., et al. Methodological considerations in studying centenarians: Lessons learned from the Georgia Centenarian Studies. Annu Rev Gerontol Geriatr. 2007;27:231–264. PMCID: PMC3156654. [PMC free article] [PubMed] [Google Scholar]
- 108.Prenderville J.A., Kennedy P.J., Dinan T.G., Cryan J.F. Adding fuel to the fire: The impact of stress on the ageing brain. Trends Neurosci. 2015;38:13–25. doi: 10.1016/j.tins.2014.11.001. [DOI] [PubMed] [Google Scholar]
- 109.Quinn TJ, McArthur K, Ellis G, Scott DJ. Functional assessment in older people. BMJ 2011;343:d4681. doi: 10.1136/bmj.d4681. [DOI] [PubMed]
- 110.Raz N., Rodrigue K.M. Differential aging of the brain: Patterns, cognitive correlates and modifiers. Neurosci Biobehav Rev. 2006;30:730–748. doi: 10.1016/j.neubiorev.2006.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Raz N, Lindenberger U, Rodrigue KM, Kennedy KM, Head D, et al. Regional brain changes in aging healthy adults: General trends, individual differences and modifiers. Cereb Cortex 2005;15:1676–1689. doi.org/10.1093/cercor/bhi044. [DOI] [PubMed]
- 112.Röcke C., Lachman M.E. Perceived trajectories of life satisfaction across past, present, and future: Profiles and correlates of subjective change in young, middle-aged, and older adults. Psychol Aging. 2008;23:833–847. doi: 10.1037/a0013680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Salthouse T. Consequences of age-related cognitive declines. Annu Rev Psychol. 2012;63:201–226. doi: 10.1146/annurev-psych-120710-100328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Salthouse T.A. Trajectories of normal cognitive aging. Psychol Aging. 2019;34:17–24. doi: 10.1037/pag0000288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Salthouse T.A., Ferrer-Caja E. What needs to be explained to account for age-related effects on multiple cognitive variables? Psychol Aging. 2003;18:91–110. doi: 10.1037/0882-7974.18.1.91. [DOI] [PubMed] [Google Scholar]
- 116.Santamaría-García H., Baez S., Gómez C., Odir Rodríguez-Villagra O., Huepe D., et al. The role of social cognition skills and social determinants of health in predicting symptoms of mental illness. Transl Psychiatry. 2020;10:165. doi: 10.1038/s41398-020-0852-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Santos N.C., Costa P.S., Cunha P., Portugal-Nunes C., Amorim L., Cotter J., et al. Clinical, physical and lifestyle variables and relationship with cognition and mood in aging: A cross-sectional analysis of distinct educational groups. Front Aging Neurosci. 2014;6 doi: 10.3389/fnagi.2014.00021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Schaie K.W. In: Longitudinal studies of adult psychological development. Schaie K.W., editor. Guilford Press; New York: 1983. The Seattle Longitudinal Study: A twenty-one year exploration of psychometric intelligence in adulthood; pp. 64–135. [Google Scholar]
- 119.Schaie K.W., Willis S.L., Caskie G.I.L. The Seattle Longitudinal Study: Relationship between personality and cognition. Aging Neuropsychol Cogn. 2004;11:304–324. doi: 10.1080/13825580490511134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Schalock R.L., Verdugo M.A., Jenaro C., Wang M., Wehmeyer M. Cross-cultural study of quality of life indicators. AJMR. 2005;110:298–311. doi: 10.1352/0895-8017(2005)110[298:CSOQOL]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 121.Scott S.B., Graham-Engeland J.E., Engeland C.G., Smyth J.M., Almeida D.M., Katz M.J., et al. The effects of stress on cognitive aging, physiology and emotion (ESCAPE) project. BMC Psychiatry. 2015;15(1) doi: 10.1186/s12888-015-0497-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Seow P.S., Byrne G.J., Arnold E., Pachana N.A. Relationships Between Aging Attitudes and Successful Aging Outcomes in Middle-age and Older Women. Clin Gerontol. 2022;20:1–13. doi: 10.1080/07317115.2022.2072791. [DOI] [PubMed] [Google Scholar]
- 123.Sheehan B. Assessment scales in dementia. Ther Adv Neurol Disord. 2012;5:349–358. doi: 10.1177/1756285612455733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Sheikh S., Furnham A. A cross-cultural study of mental health beliefs and attitudes towards seeking professional help. Soc Psychiatry Psychiatr Epidemiol. 2000;35:326–334. doi: 10.1007/s001270050246. [DOI] [PubMed] [Google Scholar]
- 125.Sisto A., Vicinanza F., Campanozzi L.L., Ricci G., Tartaglini D., Tambone V. Towards a transversal definition of psychological resilience: A literature review. Medicina. 2019;55(11):745. doi: 10.3390/medicina55110745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Skevington S.M., The WHOQOL SRPB Group Is culture important to the relationship between quality of life and resilience? Global implications for preparing communities for environmental and health disasters. Front Psychol. 2020;11:1492. doi: 10.3389/fpsyg.2020.01492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Skinner E., Zimmer-Gembeck M.J. The development of coping. Annu Rev Psychol. 2007;58:119–144. doi: 10.1146/annurev.psych.58.110405.085705. [DOI] [PubMed] [Google Scholar]
- 128.Smith E.E., Egorova S., Blacker D., Killiany R.J., Muzikansky A., Dickerson B.C., et al. Magnetic resonance imaging white matter hyperintensities and brain volume in the prediction of mild cognitive impairment and dementia. Arch Neurol. 2008;65(1) doi: 10.1001/archneurol.2007.23. [DOI] [PubMed] [Google Scholar]
- 129.Smith J., Baltes P. Differential psychological ageing: Profiles of the old and very old. Ageing Soc. 1993;13:551–587. doi: 10.1017/S0144686X00001367. [DOI] [Google Scholar]
- 130.Sokolowski D.R., Hansen T.I., Rise H.H., Reitlo L.S., Wisløff U., Stensvold D., et al. 5 years of exercise intervention did not benefit cognition compared to the physical activity guidelines in older adults, but higher cardiorespiratory fitness did. A Generation 100 Substudy. Front Aging Neurosci. 2021;13 doi: 10.3389/fnagi.2021.742587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Sørensen T., Hestad K., Ellen Karine Grov E.K. Relationships of sources of meaning and resilience with meaningfulness and satisfaction with life: A population-based study of Norwegians in late adulthood. Front Psychol. 2021;12 doi: 10.3389/fpsyg.2021.685125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Sousa N. Clinical studies in the elderly – Why and how should we care? Aging Brain. 2021;1 doi: 10.1016/j.nbas.2020.100001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Stanley J.T., Isaacowitz D.M. Age-related differences in profiles of mood-change trajectories. Dev Psychol. 2011;47:318–330. doi: 10.1037/a0021023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Steptoe A., Deaton A., Stone A.A. Psychological wellbeing, health and ageing. Lancet. 2015;385(9968):640–648. doi: 10.1016/S0140-6736(13)61489-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Stern Y., Barnes C.A., Grady C., Jones R.N., Raz N. Brain reserve, cognitive reserve, compensation, and maintenance: Operationalization, validity, and mechanisms of cognitive resilience. Neurobiol Aging. 2019;83:124–129. doi: 10.1016/j.neurobiolaging.2019.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Sternberg R.J. Intelligence. Dialogues Clin Neurosci. 2012;14:19–27. doi: 10.31887/DCNS.2012.14.1/rsternberg. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Stine-Morrow E.A.L., Parisi J.M., Park D.C., Morrow D.G. The effects of an engaged lifestyle on cognitive vitality: A field experiment. Psychol Aging. 2008;23:778–786. doi: 10.1037/a0014341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Swenor BK, Lee MJ, Varadaraj V, Whitson HE, Ramulu PY. Aging with vision loss: A framework for assessing the impact of visual impairment on older adults. Gerontologist 2020;60:989–995. doi: 10.1093/geront/gnz117. [DOI] [PMC free article] [PubMed]
- 139.Tabira T., Hotta M., Murata M., Yoshiura K., Han G., Ishikawa T., et al. Age-related changes in Instrumental and Basic Activities of Daily Living impairment in older adults with very mild Alzheimer’s Disease. Dement Geriatr Cogn Disord Extra. 2020;10(1):27–37. doi: 10.1159/000506281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Treyer V, Meyer RS, Buchmann A, Crameri G, Studer S, et al. Physical activity is associated with lower cerebral beta-amyloid and cognitive function benefits from lifetime experience – a study in exceptional aging. PLoS ONE 2021;16:e0247225. doi.org/10.1371/journal.pone.0247225. [DOI] [PMC free article] [PubMed]
- 141.Van Dalen JW, Van Wanrooij LL, Moll van Charante EP, Richard E, Van Gool WA. Apathy is associated with incident dementia in community-dwelling older people. Neurology 2018;90:e82-89. doi: 10.1212/WNL.0000000000004767. [DOI] [PMC free article] [PubMed]
- 142.Van der Weiden A., Benjamins J., Gillebaart M., Ybema J.F., de Ridder D. How to form good habits? A longitudinal field study on the role of self-control in habit formation. Front Psychol. 2020;11:560. doi: 10.3389/fpsyg.2020.00560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Van Leeuwen KM, van Loon MS, van Nes FA, Bosmans JE, de Vet HCW, et al. What does quality of life mean to older adults? A thematic synthesis. PLoS One 2019;14(3):e0213263. doi: 10.1371/journal.pone.0213263. [DOI] [PMC free article] [PubMed]
- 144.Van Swearingen J.M., Studenski S.A. Aging, motor skill, and the energy cost of walking: Implications for the prevention and treatment of mobility decline in older persons. J Gerontol A. 2014;69:1429–1436. doi: 10.1093/gerona/glu153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Veríssimo J., Verhaeghen P., Goldman N., Weinstein M., Ullman M.T. Evidence that ageing yields improvements as well as declines across attention and executive functions. Nat Hum Behav. 2022;6:97–110. doi: 10.1038/s41562-021-01169-7. [DOI] [PubMed] [Google Scholar]
- 146.Viviano R.P., Damoiseaux J.S. Functional neuroimaging in subjective cognitive decline: Current status and a research path forward. Alzheimer’s Res Ther. 2020;12:23. doi: 10.1186/s13195-020-00591-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Waldum E.R., McDaniel M.A. Why are you late? Investigating the role of time management in time-based prospective memory. J Exp Psychol Gen. 2016;145:1049–1061. doi: 10.1037/xge0000183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Warmoth K., Tarrant M., Abraham C., Lang I.A. Older adults’ perceptions of ageing and their health and functioning: A systematic review of observational studies. Psychol Health Med. 2016;21:531–550. doi: 10.1080/13548506.2015.1096946. [DOI] [PubMed] [Google Scholar]
- 149.Wasef S., Laksono I., Kapoor P., Tang-Wei D., Gold D., Saripella A., et al. Screening for subjective cognitive decline in the elderly via subjective cognitive complaints and informant-reported questionnaires: A systematic review. BMC Anesthesiol. 2021;21(1) doi: 10.1186/s12871-021-01493-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Welle P.D., Graf H.M. Effective lifestyle habits and coping strategies for stress tolerance among college students. Am J Health Educ. 2011;42:96–105. doi: 10.1080/19325037.2011.10599177. [DOI] [Google Scholar]
- 151.Wesson J., Clemson L., Brodaty H., Reppermund S. Estimating functional cognition in older adults using observational assessments of task performance in complex everyday activities: A systematic review and evaluation of measurement properties. Neurosci Biobehav Rev. 2016;68:335–360. doi: 10.1016/j.neubiorev.2016.05.024. [DOI] [PubMed] [Google Scholar]
- 152.Whitson H.E., Duan-Porter W., Schmader K.E., Morey M.C., Cohen H.J., Colón-Emeric C.S. Physical resilience in older adults: Systematic review and development of an emerging construct. J Gerontol A Biol Sci Med Sci. 2016;71(4):489–495. doi: 10.1093/gerona/glv202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Wister A.V., Coatta K.L., Schuurman N., Lear S.A., Rosin M., MacKey D. A lifecourse model of multimorbidity resilience: Theoretical and research developments. Int J Aging Hum Dev. 2016;82(4):290–313. doi: 10.1177/0091415016641686. [DOI] [PubMed] [Google Scholar]
- 154.WHO. Dementia Fact Sheet; 2021. Assessed 20.12.2021. www.who.int/news-room/fact-sheets/detail/dementia.
- 155.Windsor T.D., Gerstorf D., Pearson E., Ryan L.H., Anstey K.J. Positive and negative social exchanges and cognitive aging in young-old adults: Differential associations across family, friend, and spouse domains. Psychol Aging. 2014;29:28–43. doi: 10.1037/a0035256. [DOI] [PubMed] [Google Scholar]
- 156.Yao S., Liu Y., Zheng X., Zhang Y.u., Cui S., Tang C., et al. Do nonpharmacological interventions prevent cognitive decline? A systematic review and meta-analysis. Transl Psychiatry. 2020;10(1) doi: 10.1038/s41398-020-0690-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Yee D.M., Adams S., Beck A., Braver T.S. Age-related differences in motivational integration and cognitive control. Cogn Affect Behav Neurosci. 2019;19:692–714. doi: 10.3758/s13415-019-00713-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Zhang Y., Xiong Y., Yu Q., Shen S., Chen L., et al. The activity of daily living (ADL) subgroups and health impairment among Chinese elderly: A latent profile analysis. BMC Geriatr. 2021;21:30. doi: 10.1186/s12877-020-01986-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Zihl J, Fink Th, Pargent F, Ziegler M, Bühner M. Cognitive reserve in young and old healthy subjects: Differences and similarities in a testing-the-limits paradigm with DSST. PLoS One 2014;9(1):e84590. doi: 10.1371/journal.pone.0084590. [DOI] [PMC free article] [PubMed]
- 160.Zihl J., Kentridge R.W., Pargent F., Heywood C.A. Aging and the rehabilitation of homonymous hemianopia: The efficacy of compensatory eye-movement training techniques and a five-year follow up. Brain Aging. 2021;1:10012. doi: 10.1016/j.nbas.2021.100012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Zimmer-Gembeck M.J., Skinner E. The development of coping across childhood and adolescence: An integrative review and critique of research. Int J Behav Dev. 2011;35:1. doi: 10.1177/0165025410384923. [DOI] [Google Scholar]
- 162.Zimprich D., Hofer S.M., Aartsen M.J. Short-term versus long-term longitudinal changes in processing speed. Gerontology. 2004;50:17–21. doi: 10.1159/000074384. [DOI] [PubMed] [Google Scholar]