Abstract
Background
Cholesterol guidelines typically prioritize primary prevention statin therapy based on 10-year risk of cardiovascular disease. The advent of generic pricing may justify expansion of statin eligibility. Moreover, 10-year risk may not be the optimal approach for statin prioritization. We estimated the cost-effectiveness of expanding preventive statin eligibility and evaluated novel approaches to prioritization from a Scottish health sector perspective.
Methods
A computer simulation model predicted long-term health and cost outcomes in Scottish adults aged ≥40 years. Epidemiologic analysis was completed using the Scottish Heart Health Extended Cohort, Scottish Morbidity Records, and National Records of Scotland. A simulation cohort was constructed with data from the Scottish Health Survey 2011 and contemporary population estimates. Treatment and cost inputs were derived from published literature and health service cost data. The main outcome measure was the lifetime incremental cost-effectiveness ratio (ICER), evaluated as cost (GBP 2020) per quality-adjusted life year (QALY) gained.
Three approaches to statin prioritization were analyzed: 10-year risk scoring using the ASSIGN score, age-stratified (Age-Strat) risk thresholds to increase treatment rates in younger individuals, and absolute risk reduction (ARR)-guided therapy to increase treatment rates in individuals with elevated cholesterol levels. For each approach, two policies were considered: one which treats the same number of individuals as an ASSIGN score ≥20% (ASSIGN 20, Age-Strat 20, ARR 20) and one which treats the same number as an ASSIGN score ≥10% (ASSIGN 10, Age-Strat 10, ARR 10).
Results
Compared to ASSIGN 20, reducing the risk threshold for statin initiation to 10% expanded eligibility from 804,000 (32% of CVD-free adults aged ≥40 years) to 1,445,500 individuals (58%). This policy would be cost-effective (ICER: £12,300/QALY, 95% CI: £7,690/QALY-£26,500/QALY). Incremental to ASSIGN 20, ARR 20 produced around 8,800 QALYs and was cost-effective (£7,050/QALY, 95% CI: £4,560/QALY-£10,700/QALY). Incremental to ASSIGN 10, ARR 10 produced around 7,950 QALYs and was cost-effective (£11,700/QALY, 95% CI: £9,250/QALY-£16,900/QALY). Both age-stratified risk threshold strategies were dominated (i.e., more expensive and less effective than alternative treatment strategies).
Conclusions
Generic pricing has rendered preventive statin therapy cost-effective for many adults. Absolute risk reduction-guided therapy is more effective than 10-year risk scoring and is cost-effective.
Keywords: cardiovascular disease, risk, cost-effectiveness, cholesterol, statins
Introduction
Cardiovascular disease (CVD) is the leading cause of morbidity and mortality worldwide.1 In the U.K. more than 140,000 deaths were attributable to CVD in 2018 and rates are disproportionately high in Scotland.2,3 Hydroxymethylglutaryl–coenzyme A reductase inhibitors (statins) are a cornerstone treatment for the primary prevention of CVD. They are a first-line treatment for lipid-lowering therapy, their efficacy and safety has been established in high-quality clinical trials, and recent price reductions have made this drug class very affordable.
Individuals without CVD are often prioritized for preventive statin therapy based on 10-year risk of experiencing a primary CVD event, estimated using 10-year CVD risk scores.4–7 The National Institute for Health and Care Excellence (NICE) in England and Wales recommends statins for individuals aged 40 years and above with a 10-year CVD risk score ≥10%, type 1 diabetes mellitus, chronic kidney disease, or total cholesterol ≥ 7.5 mmol/L.5,8 The risk threshold for statin eligibility had previously been 20%.
Unlike NICE, the Scottish Intercollegiate Guidelines Network (SIGN) has retained a risk threshold of 20% for statin eligibility.6 SIGN recommends that risk is assessed using the ASSIGN risk score, which was developed with Scottish data. The risk factors included in the ASSIGN score are age, sex, diabetes, systolic blood pressure (SBP), total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), cigarettes per day (CPD), Scottish Index of Multiple Deprivation (SIMD), and family history of CVD.
Reducing the risk threshold in England and Wales was partly justified by the advent of generic pricing for most statin formulations. Generic statin pricing expanded the proportion of the population who would be cost-effective to treat.9–12 The cost-effectiveness of lowering the threshold or pursuing alternative prioritization strategies in Scotland has not been evaluated. Most other countries also still use 10-year risk thresholds.13
We aimed to (i) estimate the cost-effectiveness of lowering the 10-year CVD risk threshold for statin eligibility in Scotland, and (ii) estimate the cost-effectiveness of novel approaches to statin prioritization, an analysis highly relevant to future statin prescribing in many other countries worldwide.
Methods
The Scottish CVD Policy Model, the decision-analytic model employed in our analysis, and the program code used to run the model are publicly available and can be accessed at https://github.com/yiqiaoxin/CVDmodel. The Scottish Health Survey is publicly available from the UK Data Service and can be accessed at https://beta.ukdataservice.ac.uk/datacatalogue/series/series?id=2000047.
Novel Approaches to Statin Prioritization
Novel approaches to statin prioritization may be preferable to 10-year risk scoring. Two alternative approaches to statin prioritization are age-stratified risk thresholds and absolute risk reduction.
Age-stratified risk thresholds
The age-stratified risk threshold approach involves setting separate risk thresholds for statin initiation in different age-groups. This approach has been introduced in Norway and is predicated on the concept that risk scores are poorly calibrated for some subsets of the CVD-free population.14 This includes younger individuals who are at high-risk of developing CVD relative to their age-group peers.15
Some CVD risk factors are generic to a range of adverse health conditions. For example, age is a risk factor for CVD but is also predictive of non-CVD mortality. Ten-year CVD risk scores disregard the competing risk of non-CVD mortality and therefore may overstate potential benefit from preventive therapy. Using age-stratified risk thresholds to target treatment at younger individuals with unhealthy levels of modifiable risk factors may produce greater health benefits than current practice.
Absolute risk reduction
The absolute risk reduction (ARR) approach to statin prioritization recognizes that reduction in cholesterol is the major driver of statin benefit and that this can be estimated from baseline cholesterol.16 Several major clinical trials have analyzed the effect of statins on CVD risk. This enables powerful inference of statin effectiveness in patient subgroups. A key finding has been that relative risk reduction (RRR) of CVD from statin therapy is near constant at approximately 22% per 1.0 mmol/L reduction in low-density lipoprotein cholesterol (LDL-C) over five years.17 Further, statins tend to produce a greater reduction in individuals with higher baseline LDL-C. Combining these two findings – RRR applied to baseline absolute risk – suggests that individuals with higher baseline LDL-C achieve greater ARR from statin therapy.
Consider two individuals with same ASSIGN 10-year risk score, one with an LDL-C of 4.0 mmol/L and one with an LDL-C of 2.0 mmol/L. If atorvastatin 20mg reduces LDL-C by around 40%, giving it to these individuals yields reductions of a 1.6 mmol/L and 0.8 mmol/L, respectively. This translates to a 33% RRR for the former individual and an 18% RRR for the latter.
To prevent CVD events, we are ultimately concerned with absolute risk reduction. Thanassoulis et al. developed an equation to predict 10-year ARR from statin therapy.16 This equation predicts that ARR from statins is the product of an individual’s baseline 10-year risk and their baseline LDL-C (ldlb). The equation is as follows:
| (Equation 1) |
Sun and HR represent 10-year untreated survival and the hazard ratio associated with a unitary reduction in LDL-C, respectively. The equation assumes that statins produce a 40% reduction in LDL-C. We modified this equation to account for the effect of statins on non-HDL cholesterol (non-HDL-C) rather than LDL-C in our analysis.
Scottish CVD Policy Model
The Scottish CVD Policy model was employed to estimate the cost-effectiveness of different statin policies (Supplemental Material, eTables 1-6). This open-source, decision-analytic model was developed in the R programming language (Version 4.0.4, R Core Team)18 and has been validated in the Scottish population (eFigures 1-2).19–21 The model predicts life expectancy, quality-adjusted life years (QALYs), and healthcare costs for individuals receiving care in the Scottish National Health Service based on their ASSIGN risk factors.
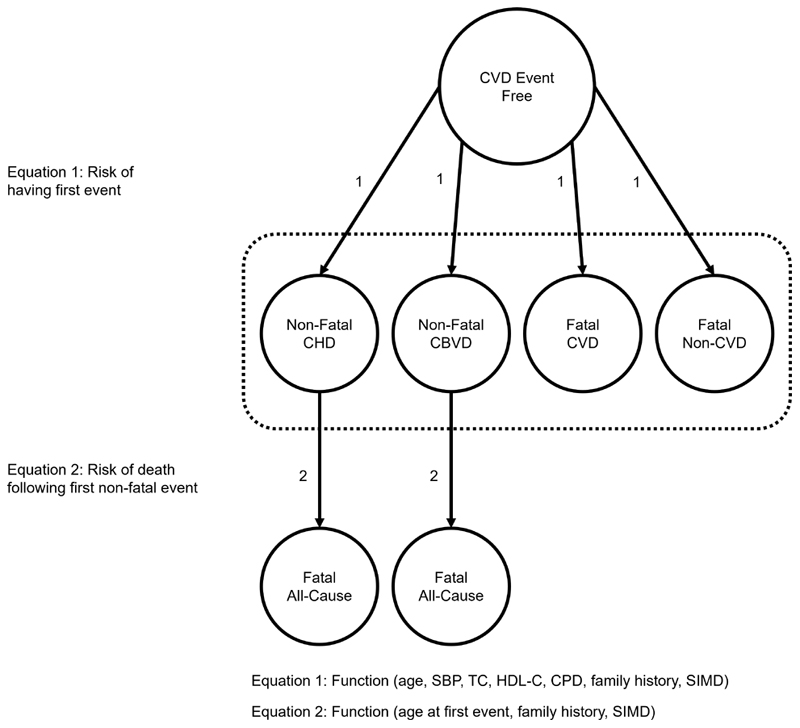
Figure 1 shows a diagram of the model. Individuals enter CVD-free and transition to one of four primary event types throughout their lives: non-fatal coronary heart disease (CHD), non-fatal cerebrovascular disease (CBVD), fatal CVD, or fatal non-CVD. After the occurrence of a non-fatal primary event, individuals progress to an absorbing state representing all-cause mortality.
Figure 1. Structure of the Scottish CVD Policy Model.
CBVD – Cerebrovascular Disease, CHD – Coronary Heart Disease, CPD – Cigarettes per Day, CVD – Cardiovascular Disease, HDL-C – High-Density Lipoprotein Cholesterol, SBP – Systolic Blood Pressure, SIMD – Scottish Index of Multiple Deprivation
Probability of state transition was determined by competing risk parametric survival analysis of a linked Scottish Heart Health Extended Cohort (SHHEC)-Scottish Morbidity Records (SMR) dataset.22,23 SHHEC was used in the construction of the ASSIGN risk score. Researchers collected baseline risk factor information for more than 13,000 Scottish adults commencing in 1986. The SMR is an electronic database which records all hospitalized events that occur in the Scottish NHS. Baseline risk factors were linked with the SMR via participants’ unique NHS identification number.
Each state in the model has an assigned disutility value, derived from a survey of the Scottish population. Individuals who have not experienced a primary CVD event are attributed a background health-related quality of life, disaggregated by age and sex. Individuals inhabiting one of the two non-fatal chronic CVD states are assigned a decrement to their background quality of life, determined by the type of primary event (CHD or CBVD). Within the chronic disease states, individuals may experience further utility decrements attributable to secondary CVD events (i.e., myocardial infarctions, strokes, transient ischemic attacks, heart failure, peripheral artery disease, and ‘other’ CVD events).
All states in the model are assigned healthcare costs, derived from a combination of SMR data and English tariffs for elective and non-elective hospitalizations.24 When the primary event is non-fatal, linear equations predict pre- and post-event hospitalization costs. These equations include age at primary event, SIMD, and family history of CVD as covariates.
The model estimates outcomes through cohort simulation. It deterministically assigns individuals to health states, based on the SHHEC-SMR risk functions and a profile of CVD risk factors. Health and cost estimates are produced for each risk factor profile by summing the probability-weighted outcomes associated with each health state that an individual may encounter. This process is outlined in the Supplemental Material. Heterogeneity in the population is reflected by simulating multiple risk factor profiles that are reflective of the CVD-free Scottish population.
Simulation data
To simulate the Scottish CVD-free population, information on risk factor and age distributions were required. Our analysis was completed using a combination of the Scottish Health Survey (SHS) 2011 and contemporary population estimates from the National Records of Scotland.25,26
The SHS is a study of public health and ASSIGN risk factors values can be derived for all respondents from the 2011 survey data. The SHS 2011 is the most contemporaneous dataset regarding the distribution of CVD risk factors in Scotland. Subsequent waves of the survey have not included a nurse visit so have not collected blood samples or recorded SBP.
We excluded individuals aged <40 years and those with existing CVD from our dataset. Individuals currently receiving statins were ‘detreated’, by modifying cholesterol levels according to treatment effects observed in randomized clinical trials.17 A relatively small number of respondents received nurse visits. This meant that data were sparse for three important covariates: TC, HDL-C, and SBP. For most individuals, we assumed these variables were missing at random and they were imputed with stochastic regression.27 For individuals who refused nurse visits, we performed multiple imputation (eTable 7).28 Individuals with familial hypercholesterolaemia, defined as TC ≥7.5 mmol/L and a family history of premature CVD or TC ≥8.0 mmol/L, are high priority for statin therapy and were omitted from the analysis.6 In a scenario analysis, we further excluded individuals with diabetes mellitus.
More information on the SHS and our imputation procedure is included in the Supplemental Material.
Treatment criteria
We first aimed to establish the cost-effectiveness of expanding statin eligibility. This was achieved by analyzing three treatment strategies in the SHS cohort: no treatment, statins for individuals with ASSIGN score ≥20% (ASSIGN 20), and statins for individuals with ASSIGN score ≥10% (ASSIGN 10).
Our second objective was to estimate the cost-effectiveness of novel approaches to statin prioritization. Age-stratified risk thresholds and ARR were analyzed. Two strategies were defined for each novel strategy: one which treated approximately the same number of people as ASSIGN 20 (Age-Strat 20, ARR 20) and one which treated approximately the same number of people as ASSIGN 10 (Age-Strat 10, ARR 10).
For age-stratified risk threshold policies, we set separate risk thresholds for five-year age-groups from ages 40 to 79 and individuals aged ≥80 years. These thresholds targeted treatment at individuals who were high-risk relative to their age-group peers, so increased the proportion of younger individuals who were treated (Supplemental Material).
We estimated ARR from statins for everyone in the SHS cohort using a modified form of Equation 1. Due to data limitations, LDL-C was replaced with non-HDL-C. The percentage reduction in non-HDL-C and HR per 1.0 mmol/L reduction were altered in the equation accordingly. We established ARR thresholds that would treat the same proportion of the population as ASSIGN 20 and ASSIGN 10, respectively.
The specific age-stratified risk threshold and ARR policies that we analyzed are shown in Table 1. The proportions of the Scottish population eligible for treatment under different risk and ARR thresholds are presented in Table 1 and eFigures 3-5. Ten-year risk, age-stratified risk threshold, and absolute risk reduction strategies which treated the same number of people were compared using traditional cost-effectiveness decision rules.29
Table 1. Statin eligibility criteria and percentage eligible for treatment under different treatment strategies.
|
10-Year CVD Risk
Threshold (% Eligible) |
10-Year ARR
Threshold (% Eligible) |
||||||
|---|---|---|---|---|---|---|---|
|
ASSIGN
20 |
ASSIGN
10 |
Age-Strat
20 |
Age-Strat
10 |
ARR
20 |
ARR
10 |
||
| Age-Group (Years) | 40-44 | 20.0 (0.2) | 10.0 (4.7) | 4.8 (32.1) | 3.3 (57.7) | 3.97 (0.8) | 2.00 (8.0) |
| 45-49 | 20.0 (1.2) | 10.0 (14.0) | 7.2 (32.1) | 4.9 (57.7) | 3.97 (2.6) | 2.00 (20.0) | |
| 50-54 | 20.0 (3.6) | 10.0 (33.9) | 10.3 (32.1) | 7.2 (57.7) | 3.97 (7.8) | 2.00 (39.2) | |
| 55-59 | 20.0 (13.4) | 10.0 (60.5) | 14.4 (32.1) | 10.4 (57.7) | 3.97 (20.5) | 2.00 (59.8) | |
| 60-64 | 20.0 (32.9) | 10.0 (81.6) | 20.4 (32.1) | 14.9 (57.7) | 3.97 (36.8) | 2.00 (76.0) | |
| 65-69 | 20.0 (57.6) | 10.0 (95.2) | 26.6 (32.1) | 20.0 (57.7) | 3.97 (54.1) | 2.00 (87.9) | |
| 70-74 | 20.0 (79.6) | 10.0 (100.0) | 36.4 (32.1) | 26.9 (57.7) | 3.97 (69.3) | 2.00 (95.5) | |
| 75-79 | 20.0 (96.0) | 10.0 (99.6) | 43.8 (32.1) | 34.8 (57.7) | 3.97 (86.9) | 2.00 (98.2) | |
| 80+ | 20.0 (100.0) | 10.0 (100.0) | 62.9 (32.1) | 48.8 (57.7) | 3.97 (91.2) | 2.00 (99.3) | |
| Overall | 20.0 (32.1) | 10.0 (57.7) | n/a (32.1) | n/a (57.7) | 3.97 (32.1) | 2.00 (57.7) | |
ARR – absolute risk reduction; Age-Strat – age-stratified risk thresholds; CVD – cardiovascular disease
Statin treatment parameters
Statins reduced risk of non-fatal CHD, non-fatal CBVD, and fatal CVD in the model. This was achieved by lowering individuals’ non-HDL-C levels (Table 2). Patients receiving statins incurred side effects and accumulated treatment and monitoring costs (eTable 8).
Table 2. Intermediate-intensity statin treatment parameters.
| Parameter |
Base
Case |
PSA
Distribution |
Lower | Upper | Source |
|---|---|---|---|---|---|
| Statin effectiveness | |||||
| Non-HDL cholesterol reduction (%) | -26.0 | Beta | -35.0 | -15.0 | 17 |
| Relative risk per 1.0 mmol/L reduction in non-HDL cholesterol | |||||
| Non-fatal coronary heart disease | 0.77 | Beta | 0.75 | 0.80 | 17 |
| Non-fatal stroke | 0.87 | Beta | 0.83 | 0.91 | 17 |
| Fatal cardiovascular disease | 0.90 | Beta | 0.86 | 0.92 | 17 |
| Any cardiovascular disease* | 0.79 | np | nt | nt | 17 |
| Side effects and treatment disutility | |||||
| Type-2 diabetes absolute risk increase (%) | 0.5 | Log-normal | 0.1 | 1.0 | 33 |
| Annual pill-taking disutility | 0.002 | Beta | 0.000 | 0.004 | 11 |
| Annual treatment-related costs (£) | |||||
| Atorvastatin 20mg/daily | 13.44 | Gamma | 12.65 | 26.35 | 35 |
| Monitoring, first year | 102.51 | Gamma | 63.51 | 141.51 | 5,34,36,38 |
| Monitoring, subsequent | 55.48 | Gamma | 16.48 | 94.48 | 5,34,36,38 |
| Other costs | |||||
| Risk assessment | 17.68 | Gamma | 10.68 | 24.68 | 5,34,36,38 |
| Annual type-2 diabetes treatment | 314.33 | Gamma | 156.50 | 469.50 | 5,34,36,38 |
| Annual discount rate (%) † | 3.5 | np | 1.5 | 5.5 | 37 |
Used to estimate individual-level absolute risk reduction from statin therapy
Assumed equal for health and cost outcomes
np – not included in probabilistic sensitivity analysis
nt – not included in traditional sensitivity analyses
The Scottish CVD Policy Model does not include LDL-C as a predictor of CVD risk. Instead, it includes TC and HDL-C. Similarly, the SHS only collected data on TC and HDL-C. Evidence suggests that statins produce a 26% reduction in non-HDL-C and are associated with relative risks of 0.77, 0.87, and 0.90 for non-fatal CHD, non-fatal stroke, and fatal CVD per 1.0 mmol/L reduction in non-HDL-C, respectively.17 These values were derived from secondary analysis of a Cholesterol Treatment Trialists’ meta-analysis and are likely conservative estimates of the impact of statins on CVD risk as mediated by non-HDL-C reduction.30
Statins are a relatively safe treatment with a well-established side effect profile.31,32 In the model, statins increased absolute risk of new onset diabetes by 0.5%.33 An annual pill-taking disutility of 0.002 QALYs was also applied.11
Statin costs were obtained from the British National Formulary.34 An annual cost of £13.44 was applied for every year on statin therapy, representing the annual NHS drug tariff price for generic atorvastatin 20mg.35 Alternative moderate-intensity statins are available, and their prices were used to define upper and lower limits in sensitivity analyses.
All individuals experienced screening costs upon entering the model. Patients prescribed statins were assigned monitoring costs which were largely obtained from a cost-effectiveness analysis of statin policy conducted for NICE and an analysis of unit costs for health and social care in England and Wales.5,36 Additional costs were added for each statin user attributable to their increased risk of diabetes.
Statistical Analysis
The Scottish CVD Policy Model simulated the cost-effectiveness of different risk- and absolute risk reduction-guided statin policies. A baseline simulation predicted treatment-free health and cost outcomes. Next, model parameters were altered to simulate the benefits, side effects, and costs associated with moderate-intensity statin therapy. If individuals in the SHS cohort met treatment criteria, they received the benefits and costs associated with statin therapy. Otherwise, they incurred no treatment costs or benefits. One ‘iteration’ of the model involved simulating every individual in the SHS cohort.
This study followed the Consolidated Health Economic Evaluation Reporting Standards reporting guideline (eTable 9). A health sector perspective was adopted which accounted for all screening, statin treatment, monitoring, CVD, and background healthcare costs incurred by the Scottish NHS. The primary outcome considered was the incremental cost (GBP 2020) per QALY gained for different treatment strategies with a lifetime horizon. Intermediate outcomes recorded were primary CVD events prevented, life years gained, and disaggregated healthcare costs. Future costs and health benefits were discounted at a rate of 3.5% annually.37 Model costs were inflated by 12.5% to account for health services pay and price inflation from 2014 to 2020.38 Cost-effectiveness analysis was performed with a health sector perspective and a strategy was deemed cost-effective if its incremental cost-effectiveness ratio (ICER) was below £20,000/QALY.39,40 This is a standard threshold used in cost-effectiveness analyses in Scotland and the U.K.6,37
Simulation analysis was completed by stochastically sampling Table 2 parameter distributions and risk factor hazard ratios, then estimating costs and QALYs for the respective treatment strategies in 1,000 independent iterations. Correlation between risk factor hazard ratios was accounted for with Cholesky decomposition.41 Base case results were derived from the mean values of the probabilistic analyses and 95% confidence intervals were presented as the 2.5th and 97.5th percentiles of the 1,000 iterations. Cost-effectiveness acceptability curves were produced with results from the probabilistic analysis.
Population estimates from the National Records of Scotland were used to project results onto the wider Scottish population.25 The number of individuals in each age-group was derived from these estimates. This number was multiplied by the respective proportion of CVD-free individuals in each age-group in SHS 2011 to obtain the number of individuals eligible for preventive treatment. The outcomes observed in the simulation were projected onto the Scottish population by multiplying average age-group-level outcomes in the simulation by the number of eligible patients in the wider population.
Sensitivity Analyses
Sensitivity analyses assessed the impact of key modelling parameters on cost-effectiveness estimates. Table 2 lists the lower and upper values employed in these analyses. Results from the sensitivity analysis were synthesized in tornado diagrams. These diagrams showed the impact of modelling assumptions on the cost-effectiveness of a treatment policy, represented by change in net monetary benefit (NMB). Unlike the ICER, NMB is a continuously defined, linear measure of cost-effectiveness and an increase represents increased cost-effectiveness.42 We estimated the NMB for all strategies at a range of values between the lower and upper limits defined in Table 2.
In our base case, we assumed ‘full adherence’ to statin therapy (i.e., effect size equal to effects observed in clinical trials). In a scenario analysis, we assumed 67% of patients would continue treatment in the first, 53% in the second, and 50% in subsequent years of statin initiation.43 Treatment efficacy, side effects, and monitoring costs were only experienced by persistent statin users. In a further scenario analysis, we excluded individuals with diabetes from the prospective patient population and assumed that they would be treated regardless of prioritization criteria. We additionally considered the net monetary benefit of each treatment strategy over a wide range of values for pill-taking disutility to establish optimal treatment strategies dependent on a patient’s aversion to daily pill-taking.
While the primary analysis was limited to two ASSIGN score thresholds for statin initiation, we considered the cost-effectiveness of reducing the threshold below ASSIGN 10 in a sensitivity analysis. Specifically, we considered the incremental cost-effectiveness of reducing the threshold at 1% increments from ASSSIGN 20 to treatment of the entire CVD-free adult population.
Institutional review board approval was not required as the study was a secondary analysis of publicly available and de-identified data.
Results
Descriptive statistics for the final dataset and treatment-eligible populations are displayed in eTable 10. The overall population was disproportionately female, likely because we excluded individuals with established CVD. Age-stratified risk thresholds and ARR strategies reduced the average age of treatment compared to standard 10-year risk scoring. The ARR strategies treated patients with higher TC, higher non-HDL-C, and lower HDL-C compared to the alternatives.
Our first objective was to estimate the cost-effectiveness of extending preventive statin therapy eligibility (Table 3). ASSIGN 20 was cost-effective compared to no treatment (ICER: £3,850/QALY; 95% CI: £957/QALY-£6,770/QALY). Implementing ASSIGN 10 would also be cost-effective (ICER vs. ASSIGN 20: £12,300/QALY; 95% CI: £7,690/QALY-£26,500/QALY).
Table 3. Cost-effectiveness of statin treatment strategies, mean and 95% confidence intervals from probabilistic analysis.
| Policy |
Number
Treated |
Primary CVD
Events Prevented |
Undiscounted
Life Years |
Discounted
QALYs Gained |
Discounted
Cost (£1000’s) |
ICER
(£/QALY) |
|---|---|---|---|---|---|---|
| Expanding treatment eligibility | ||||||
| No Treatment | 0 | Reference | ||||
| ASSIGN 20 | 804,000 | 34,400 (21,000-49,600) | 240,000 (106,000-405,000) | 103,000 (49,100-168,000) | 397,000 (46,800-791,000) | 3,850 (957-10,100) |
| ASSIGN 10 | 1,445,500 | 62,100 (38,500-89,000) | 463,000 (202,000-792,000) | 172,000 (78,000-282,000) | 1,240,000 (590,000-2,050,000) | 12,300 (7,690-26,500) |
| Policies comparable to ASSIGN 20 | ||||||
| ASSIGN 20 | 804,000 | Reference | ||||
| ARR 20 | 804,000 | 2,740 (1,750-3,990) | 26,600 (6,410-51,300) | 8,800 (3,870-14,400) | 62,000 (27,600-104,000) | 7,050 (4,560-10,700) |
| Age-Strat 20 | 804,000 | 1,700 (764-3,120) | 24,900 (-83,900-115,000) | -5,390 (-21,600-10,400) | 417,000 (230,000-625,000) | Dominated* (Dominated-Dominated) |
| Policies comparable to ASSIGN 10 | ||||||
| ASSIGN 10 | 1,445,500 | Reference | ||||
| ARR 10 | 1,445,500 | 2,760 (1,790-4,000) | 31,800 (6,830-58,400) | 7,950 (3,660-13,000) | 93,500 (54,500-138,000) | 11,700 (9,250-16,900) |
| Age-Strat 10 | 1,445,500 | 2,510 (1,360-4,120) | 34,800 (-63,800-124,000) | -7,090 (-21,300-5,960) | 450,000 (269,000-660,000) | Dominated* (Dominated-Dominated) |
ARR – absolute risk reduction; Age-Strat – age-stratified risk thresholds; CVD – cardiovascular disease; ICER – Incremental cost-effectiveness ratio; QALYs – quality-adjusted life years
More expensive and less effective than comparator
Reducing the ASSIGN risk threshold from 20% to 10% would extend statin eligibility by approximately 641,500 individuals, from 804,000 to 1,445,500. Statin eligibility would increase from 32% to 58% of Scottish CVD-free population aged ≥40 years. Reducing the threshold would prevent around 27,700 primary CVD events and produce around 223,000 life years and 69,000 discounted QALYs. Sensitivity analysis showed that it would be cost-effectiveness to further reduce the threshold to approximately 8.0% (eTable 11).
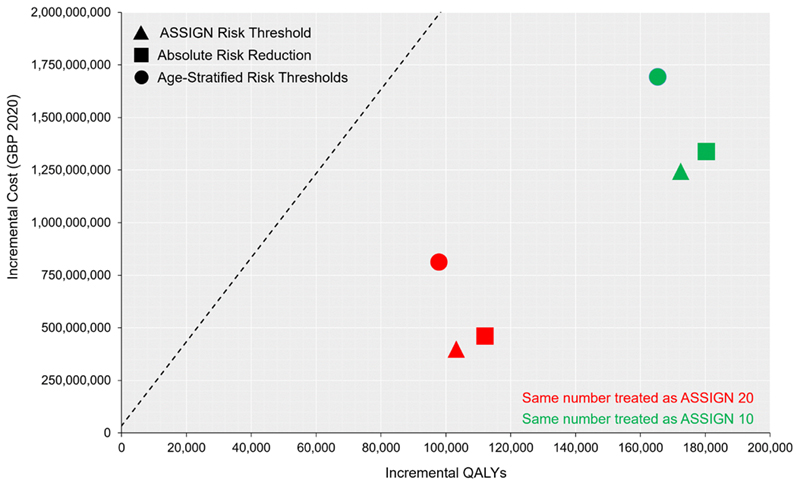
Our second objective was to estimate the cost-effectiveness of novel approaches to statin prioritization (Figure 2). Both age-stratified risk policies were dominated, meaning they were more expensive and less effective than alternative treatment options. Incremental to ASSIGN 20, ARR 20 treated approximately the same number of individuals, produced around 8,800 QALYs, and had an ICER of £7,050/QALY (95% CI: £4,560/QALY-£10,700/QALY). Incremental to ASSIGN 10, ARR 10 treated approximately the same number of individuals, produced around 7,950 QALYs, and had an ICER of £11,700/QALY (95% CI: £9,250/QALY-£16,900/QALY).
Figure 2. Cost-effectiveness plane for all treatment strategies.
QALY – Quality-Adjusted Life Year
Dashed line represents cost-effectiveness threshold of £20,000/QALY
Compared to no treatment, all statin strategies led to large reductions in CVD-related healthcare costs (eTable 12). However, these were offset by non-CVD healthcare, statin, monitoring, and risk assessment costs.
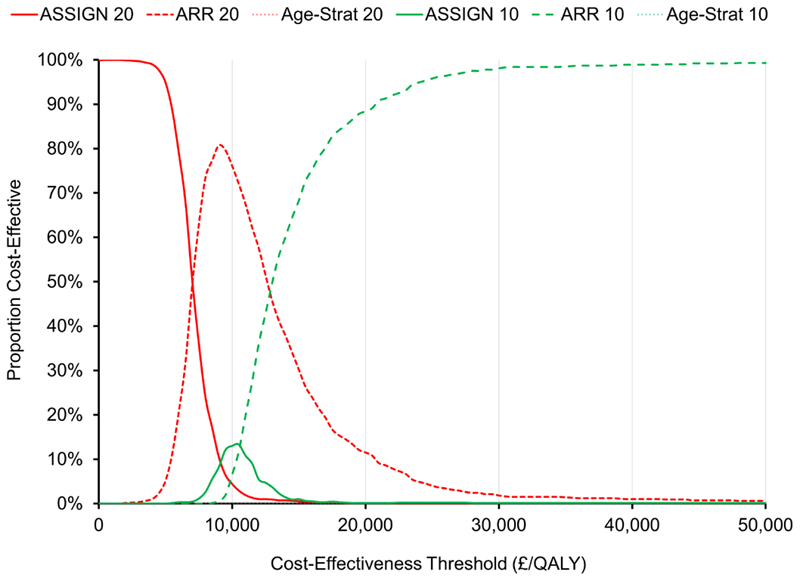
At cost-effectiveness thresholds less than £50,000/QALY, ARR-based prioritization was optimal in most probabilistic iterations of the model (Figure 3). When all treatment strategies were considered together, ARR 10 was optimal 88% of the time at a threshold of £20,000/QALY.
Figure 3. Cost-effectiveness acceptability curves for all treatment strategies.
QALY – Quality-Adjusted Life Year
The curves for Age-Strat-10 and Age-Strat-20 are indistinguishable from the 0% line
Reduction in non-HDL cholesterol, discount rate, the impact of statins on CVD mortality, pill-taking disutility, and ongoing monitoring costs had the greatest impact on cost-effectiveness estimates (Figure 4, eFigures 6-7). Absolute risk reduction remained the optimal approach to statin prioritization in most sensitivity analyses. However, at high levels of pill-taking disutility, treating fewer individuals was optimal (i.e., ARR 20 had greater NMB than ARR 10) (eFigure 8). Neither accounting for reduced patient adherence nor removing patients with diabetes from the simulation cohort greatly affected cost-effectiveness results, with ARR 10 remaining the optimal treatment strategy at a cost-effectiveness threshold of £20,000/QALY in both these analyses (eTables 13-14).
Figure 4. Tornado diagrams for most influential model parameters.
A. Strategies treating same number as ASSIGN 20
B. Strategies treating same number as ASSIGN 10
Quality-adjusted life years valued at £20,000
Increased net monetary benefit indicates increased cost-effectiveness
Discussion
The objectives of this study were to estimate the cost-effectiveness of expanding statin eligibility in Scotland and to estimate the cost-effectiveness of novel approaches to statin prioritization, relevant to all nations. Expanding statin eligibility in Scotland would be cost-effective and population health would be improved by using ARR, based on both 10-year CVD risk and non-HDL-C levels, to guide statin treatment decisions. This means, guideline committees should consider new ways to allocate statins based on ARR and not simply 10-year risk thresholds.
Absolute risk reduction may be more clinically acceptable than 10-year risk scoring. Some physicians were dismayed by NICE’s decision to reduce the risk threshold for statin initiation to 10%.44 Polypharmacy, ‘labelling’ and treatment of relatively healthy individuals, and potential adverse events were cited as concerns. These concerns may partly explain poor clinical adherence to statin guidelines.45 The absolute risk reduction approach treats patients with measurably unhealthy levels of a modifiable risk factor and may be more palatable to clinicians.
The benefits associated with age-stratified risk thresholds may also have been underestimated. Atherosclerosis is a cumulative process. Reducing exposure to risk factors that exacerbate atherosclerotic build-up in early life will have an outsized effect on averting later life CVD events.46,47 We did not account for cumulative exposure to risk factors in our analysis and estimated statin-related risk reduction from medium-term cardiovascular outcomes trials. Accounting for cumulative exposure would require access to a longitudinal dataset that regularly tracked participants’ risk factors. Such a dataset does not currently exist for the general Scottish population. Combining information on patients’ lifetime CVD risk and current cholesterol levels may allow clinicians to better target treatment at younger patients with a high capacity-to-gain from early statin initiation.48,49
In a validation exercise, the Scottish CVD Policy Model simulated individuals from the placebo and treatment arms of the West of Scotland Coronary Prevention Study (eFigures 1-2). The model was well-matched to CVD event rates in most comparisons. However, rates of CHD were lower in the simulated placebo arm compared to trial data. If the model systematically underestimates CVD event rates in the untreated CVD-free population, intensive lipid-lowering strategies will be more cost-effective than simulated. Event rates in the model were recalibrated to replicate contemporary Scottish life tables, which should ensure a better fit with contemporary CVD event rates than observed in the validation exercise.19
As with all decision modelling studies, uncertainty in model parameters propagates into uncertainty in modelled outcomes. While the efficacy and side effects of statins have been studied extensively, more research could be conducted to assess statin pill-taking disutility and establish optimal treatment monitoring procedures. Pill-taking disutility is a loosely defined and under-researched phenomenon, with most available evidence coming from small sample studies and online surveys of select populations.50,51 The results of our sensitivity analyses suggest that benefits of statins do not outweigh the costs for patients that are highly averse to regularly pill-taking. The necessary frequency of patient monitoring also likely varies substantially between patients. Our results show that reducing monitoring costs greatly increases the cost-effectiveness of statin therapy.
Conclusion
The advent of generic pricing has rendered preventive statin therapy cost-effective for many adults in Scotland. Eligibility for statin therapy should be expanded to ensure more individuals who could benefit from statins are treated. More importantly, novel mechanisms for statin prioritization may further improve population health. Absolute risk reduction synthesizes information on a patient’s absolute CVD risk with their relative risk reduction from statin therapy; it is a cost-effective approach to statin prioritization and may be more appealing to clinicians than recommendations based solely on 10-year risk thresholds.
Supplementary Material
Clinical Perspective.
What is new?
The advent of generic pricing has rendered preventive statin therapy cost-effective for many adults.
Absolute risk reduction-guided statin therapy, which is based on 10-year cardiovascular disease risk and non-high-density lipoprotein cholesterol levels, is cost-effective and would improve population health.
Age-stratified risk thresholds were more expensive and less effective than alternative approaches to statin prioritization.
What are the clinical implications?
Guideline committees should expand statin eligibility and consider new ways to allocate statins based on absolute risk reduction rather than 10-year risk thresholds.
The optimal prevalence of statin eligibility is sensitive to patient preference for daily pill-taking.
Funding/Support
CKL is supported by the Medical Research Council, Swindon (MR/K501335/1) and the National Institute for Disability, Independent Living, and Rehabilitation Research (610-5441030-60057402). NS is supported by the British Heart Foundation Research Excellence Award (RE/18/6/34217).
Non-Standard Abbreviations and Acronyms
- CVD
Cardiovascular Disease
- NICE
National Institute for Health and Care Excellence
- SIGN
Scottish Intercollegiate Guidelines Network
- SBP
Systolic Blood Pressure
- TC
Total Cholesterol
- HDL-C
High-Density Lipoprotein Cholesterol
- SIMD
Scottish Index of Multiple Deprivation
- ARR
Absolute Risk Reduction
- RRR
Relative Risk Reduction
- LDL-C
Low-Density Lipoprotein Cholesterol
- QALY
Quality-Adjusted Life Year
- CHD
Coronary Heart Disease
- CBVD
Cerebrovascular Disease
- SHHEC
Scottish Heart Health Extended Cohort
- SMR
Scottish Morbidity Records
- SHS
Scottish Health Survey
- NMB
Net Monetary Benefit
- ICER
Incremental Cost-Effectiveness Ratio
Footnotes
Conflict of Interest Disclosures: Naveed Sattar discloses the following relationships: Personal fees from Afimmune, Amgen, AstraZeneca, Boehringer Ingelheim, Eli Lilly, Hanmi Pharmaceuticals, Merck Sharp and Dohme, Novartis, Novo Nordisk, Pfizer and Sanofi, and grant funding paid to his University from AstraZeneca, Boehringer Ingelheim and Roche Diagnostics. No other disclosures were reported.
Role of the Funder/Sponsor: The sponsors had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
References
- 1.Roth GA, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, Abbastabar H, Abd-Allah F, Abdela J, Abdelalim A, et al. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. The Lancet. 2018;392:1736–1788. doi: 10.1016/S0140-6736(18)32203-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Deaths Registered in England and Wales. London, England: Office for National Statistics; 2019. [accessed October 12, 2021]. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/datasets/deathsregisteredinenglandandwalesseriesdrreferencetables . [Google Scholar]
- 3.Vital Events Reference Tables 2018. Edinburgh, Scotland: National Records of Scotland; 2019. [accessed November 19, 2019]. https://webarchive.nrscotland.gov.uk/20210314054215/https://www.nrscotland.gov.uk/statistics-and-data/statistics/statistics-by-theme/vital-events/general-publications/vital-events-reference-tables/2018 . [Google Scholar]
- 4.Woodward M, Brindle P, Tunstall-Pedoe H, SIGN group on risk estimation Adding social deprivation and family history to cardiovascular risk assessment: the ASSIGN score from the Scottish Heart Health Extended Cohort (SHHEC) Heart Br Card Soc. 2007;93:172–176. doi: 10.1136/hrt.2006.108167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.National Clinical Guideline Centre (UK) Lipid Modification: Cardiovascular Risk Assessment and the Modification of Blood Lipids for the Primary and Secondary Prevention of Cardiovascular Disease. National Institute for Health and Care Excellence; 2014. [accessed March 23, 2021]. http://www.ncbi.nlm.nih.gov/books/NBK248067/ [PubMed] [Google Scholar]
- 6.Risk estimation and the prevention of cardiovascular disease. Edinburgh, Scotland: Scottish Intercollegiate Guidelines Network; 2017. [accessed March 23, 2021]. https://www.sign.ac.uk/assets/sign149.pdf . [Google Scholar]
- 7.Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, Braun LT, de Ferranti S, Faiella-Tommasino J, Forman DE, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018:25709. doi: 10.1016/j.jacc.2018.11.003. [DOI] [Google Scholar]
- 8.Summary of National Guidance for Lipid Management. London, England: National Institute for Health and Care Excellence; 2020. [accessed November 1, 2021]. https://www.england.nhs.uk/aac/publication/summary-of-national-guidance-for-lipid-management/ [Google Scholar]
- 9.Rabar S, Harker M, O’Flynn N, Wierzbicki AS. Lipid modification and cardiovascular risk assessment for the primary and secondary prevention of cardiovascular disease: summary of updated NICE guidance. BMJ. 2014;349:g4356. doi: 10.1136/bmj.g4356. [DOI] [PubMed] [Google Scholar]
- 10.Kohli-Lynch CN, Bellows BK, Thanassoulis G, Zhang Y, Pletcher MJ, Vittinghoff E, Pencina MJ, Kazi D, Sniderman AD, Moran AE. Cost-effectiveness of Low-density Lipoprotein Cholesterol Level-Guided Statin Treatment in Patients With Borderline Cardiovascular Risk. JAMA Cardiol. 2019;4:969–977. doi: 10.1001/jamacardio.2019.2851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pandya A, Sy S, Cho S, Weinstein MC, Gaziano TA. Cost-effectiveness of 10-Year Risk Thresholds for Initiation of Statin Therapy for Primary Prevention of Cardiovascular Disease. JAMA. 2015;314:142–150. doi: 10.1001/jama.2015.6822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kohli-Lynch CNK-LN, Briggs AHBH. Oxf Encycl Health Econ. Oxford University Press; 2020. Heterogeneity in Cost-Effectiveness Analysis. [Google Scholar]
- 13.Nayor M, Vasan RS. Recent Update to the US Cholesterol Treatment Guidelines. Circulation. 2016;133:1795–1806. doi: 10.1161/CIRCULATIONAHA.116.021407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Norheim OF, Gjelsvik B, Klemsdal TO, Madsen S, Meland E, Narvesen S, Negård A, Njølstad I, Tonstad S, Ulvin F, et al. Norway’s new principles for primary prevention of cardiovascular disease: age differentiated risk thresholds. BMJ. 2011;343:d3626. doi: 10.1136/bmj.d3626. [DOI] [Google Scholar]
- 15.Navar-Boggan AM, Peterson ED, D’Agostino RB, Pencina MJ, Sniderman AD. Using Age- and Sex-Specific Risk Thresholds to Guide Statin Therapy: One Size May Not Fit All. J Am Coll Cardiol. 2015;65:1633–1639. doi: 10.1016/j.jacc.2015.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thanassoulis G, Williams K, Altobelli KK, Pencina MJ, Cannon CP, Sniderman AD. Individualized Statin Benefit for Determining Statin Eligibility in the Primary Prevention of Cardiovascular Disease. Circulation. 2016;133:1574–1581. doi: 10.1161/CIRCULATIONAHA.115.018383. [DOI] [PubMed] [Google Scholar]
- 17.Mihaylova B, Emberson J, Blackwell L, Keech A, Simes J, Barnes EH, Voysey M, Gray A, Collins R, Baigent C. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet Lond Engl. 2012;380:581–590. doi: 10.1016/S0140-6736(12)60367-5. p 588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2014. [Google Scholar]
- 19.Lewsey JD, Lawson KD, Ford I, Fox KaA, Ritchie LD, Tunstall-Pedoe H, Watt GCM, Woodward M, Kent S, Neilson M, et al. A cardiovascular disease policy model that predicts life expectancy taking into account socioeconomic deprivation. Heart. 2015;101:201–208. doi: 10.1136/heartjnl-2014-305637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lawson KD, Lewsey JD, Ford I, Fox K, Ritchie LD, Tunstall-Pedoe H, Watt GCM, Woodward M, Kent S, Neilson M, et al. A cardiovascular disease policy model: part 2-preparing for economic evaluation and to assess health inequalities. Open Heart. 2016;3:e000140. doi: 10.1136/openhrt-2014-000140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xin Y, Gray E, Robles-Zurita JA, Haghpanahan H, Heggie R, Kohli-Lynch C, Briggs A, McAllister DA, Lawson KD, Lewsey J. From Spreadsheets to Script: Experiences From Converting a Scottish Cardiovascular Disease Policy Model into R. Appl Health Econ Health Policy. 2021 doi: 10.1007/s40258-021-00684-y. [DOI] [PubMed] [Google Scholar]
- 22.Tunstall-Pedoe H, Peters SAE, Woodward M, Struthers AD, Belch JJF. Twenty‐Year Predictors of Peripheral Arterial Disease Compared With Coronary Heart Disease in the Scottish Heart Health Extended Cohort (SHHEC) J Am Heart Assoc. 6:e005967. doi: 10.1161/JAHA.117.005967. n.d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Scottish Morbidity Records. Edinburgh, Scotland: NHS Scotland Information Services Division; 2018. [accessed October 19, 2019]. http://www.ndc.scot.nhs.uk/Data-Dictionary/SMR-Datasets//Episode-Management/SMR-Record-Type/ [Google Scholar]
- 24.Lawson KD. The Scottish Cardiovascular Disease Policy Model. University of Glasgow; 2013. [Google Scholar]
- 25.Mid-Year Population Estimates, Scotland Mid-2019. Edinburgh, Scotland: National Records of Scotland; 2020. [accessed April 25, 2021]. https://www.nrscotland.gov.uk/files//statistics/population-estimates/mid-19/mid-year-pop-est-19-report.pdf . [Google Scholar]
- 26.The Scottish Health Survey 2011: Volume 1 - Adults. Edinburgh, Scotland: Scottish Government; 2012. [accessed October 10, 2019]. https://www.gov.scot/Publications/2012/09/7854 . [Google Scholar]
- 27.Van Buuren S, Groothuis-Oudshoorn K. mice: Multivariate Imputation by Chained Equations in R. J Stat Softw. 2011;45:1–67. doi: 10.18637/jss.v045.i03. [DOI] [Google Scholar]
- 28.Van Buuren S, Boshuizen HC, Knook DL. Multiple imputation of missing blood pressure covariates in survival analysis. Stat Med. 1999;18:681–694. doi: 10.1002/(sici)1097-0258(19990330)18:6<681::aid-sim71>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 29.Karlsson G, Johannesson M. The Decision Rules of Cost-Effectiveness Analysis. PharmacoEconomics. 1996;9:113–120. doi: 10.2165/00019053-199609020-00003. [DOI] [PubMed] [Google Scholar]
- 30.Brunner FJ, Waldeyer C, Ojeda F, Salomaa V, Kee F, Sans S, Thorand B, Giampaoli S, Brambilla P, Tunstall-Pedoe H, et al. Application of non-HDL cholesterol for population-based cardiovascular risk stratification: results from the Multinational Cardiovascular Risk Consortium. The Lancet. 2019;394:2173–2183. doi: 10.1016/S0140-6736(19)32519-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.He Y, Li X, Gasevic D, Brunt E, McLachlan F, Millenson M, Timofeeva M, Ioannidis JPA, Campbell H, Theodoratou E. Statins and Multiple Noncardiovascular Outcomes: Umbrella Review of Meta-analyses of Observational Studies and Randomized Controlled Trials. Ann Intern Med. 2018;169:543–553. doi: 10.7326/M18-0808. [DOI] [PubMed] [Google Scholar]
- 32.Newman Connie B, David Preiss, Tobert Jonathan A, Jacobson Terry A, Page Robert L, Goldstein Larry B, Clifford Chin, Tannock Lisa R, Michael Miller, Geetha Raghuveer, et al. Statin Safety and Associated Adverse Events: A Scientific Statement From the American Heart Association. Arterioscler Thromb Vasc Biol. 2019;39:e38–e81. doi: 10.1161/ATV.0000000000000073. [DOI] [PubMed] [Google Scholar]
- 33.Finegold JA, Manisty CH, Goldacre B, Barron AJ, Francis DP. What proportion of symptomatic side effects in patients taking statins are genuinely caused by the drug? Systematic review of randomized placebo-controlled trials to aid individual patient choice. Eur J Prev Cardiol. 2014;21:464–474. doi: 10.1177/2047487314525531. [DOI] [PubMed] [Google Scholar]
- 34.Joint Formulary Committee. British National Formulary. London, England: BMJ Group and Pharmaceutical Press; 2022. [Google Scholar]
- 35.Scottish Drugs Tariff: Prescribing and Medicines. Edinburgh, Scotland: Public Health Scotland; 2021. [accessed October 10, 2021]. https://www.isdscotland.org/Health-Topics/Prescribing-and-Medicines/Scottish-Drug-Tariff/ [Google Scholar]
- 36.Curtis LA, Burns A. PSSRU. University of Kent; 2020. Unit Costs of Health & Social Care 2020. [Google Scholar]
- 37.National Institute for Health and Care Excellence. Guide to the Methods of Technology Appraisal 2013. London, England: National Institute for Health and Care Excellence; 2013. [accessed June 3, 2019]. https://www.nice.org.uk/process/pmg9/resources/guide-to-the-methods-of-technology-appraisal-2013-pdf-2007975843781 . [PubMed] [Google Scholar]
- 38.Consumer price inflation, UK: December 2021. London, England: Office for National Statistics; 2021. [accessed November 1, 2021]. https://www.ons.gov.uk/economy/inflationandpriceindices/timeseries/chzw/mm23 . [Google Scholar]
- 39.A Guide to QALYs. Edinburgh, Scotland: Healthcare Improvement Scotland; 2018. [accessed October 23, 2019]. https://www.scottishmedicines.org.uk/media/2839/guide-to-qalys.pdf . [Google Scholar]
- 40.Kim DD, Silver MC, Kunst N, Cohen JT, Ollendorf DA, Neumann PJ. Perspective and Costing in Cost-Effectiveness Analysis, 1974–2018. PharmacoEconomics. 2020;38:1135–1145. doi: 10.1007/s40273-020-00942-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Loveman E, Jones J, Clegg AJ, Picot J, Colquitt JL, Mendes D, Breen DJ, Moore E, George S, Poston G, et al. The clinical effectiveness and cost-effectiveness of ablative therapies in the management of liver metastases: systematic review and economic evaluation: Variables included in probabilistic sensitivity analysis, sampling distributions and parameterisation of sampling distributions. Southampton, England: NIHR Journals Library; 2014. [accessed January 1, 2019]. https://www.ncbi.nlm.nih.gov/books/NBK261554/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Messori A, Trippoli S. The results of a pharmacoeconomic study: incremental cost-effectiveness ratio versus net monetary benefit. Heart. 2017;103:1746-1746. doi: 10.1136/heartjnl-2017-311816. [DOI] [PubMed] [Google Scholar]
- 43.Greving JP, Visseren FLJ, de Wit G, Algra A. Statin treatment for primary prevention of vascular disease: whom to treat? Cost-effectiveness analysis. BMJ. 2011;342:d1672. doi: 10.1136/bmj.d1672. [DOI] [PubMed] [Google Scholar]
- 44.Wise J. Open letter raises concerns about NICE guidance on statins. BMJ. 2014;348:g3937. doi: 10.1136/bmj.g3937. [DOI] [PubMed] [Google Scholar]
- 45.Homer K, Boomla K, Hull S, Dostal I, Mathur R, Robson J. Statin prescribing for primary prevention of cardiovascular disease: a cross-sectional, observational study. Br J Gen Pract. 2015;65:e538–e544. doi: 10.3399/bjgp15X686113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zhang Y, Vittinghoff E, Pletcher MJ, Allen NB, Zeki Al Hazzouri A, Yaffe K, Balte PP, Alonso A, Newman AB, Ives DG, et al. Associations of Blood Pressure and Cholesterol Levels During Young Adulthood With Later Cardiovascular Events. J Am Coll Cardiol. 2019;74:330–341. doi: 10.1016/j.jacc.2019.03.529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ference BA, Yoo W, Alesh I, Mahajan N, Mirowska KK, Mewada A, Kahn J, Afonso L, Williams KA, Flack JM. Effect of Long-Term Exposure to Lower Low-Density Lipoprotein Cholesterol Beginning Early in Life on the Risk of Coronary Heart Disease: A Mendelian Randomization Analysis. J Am Coll Cardiol. 2012;60:2631–2639. doi: 10.1016/j.jacc.2012.09.017. [DOI] [PubMed] [Google Scholar]
- 48.Kohli-Lynch CN, Bellows BK, Zhang Y, Spring B, Kazi DS, Pletcher MJ, Vittinghoff E, Allen NB, Moran AE. Cost-Effectiveness of Lipid-Lowering Treatments in Young Adults. J Am Coll Cardiol. 2021;78:1954–1964. doi: 10.1016/j.jacc.2021.08.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Heidenreich PA, Clarke SL, Maron DJ. Time to Relax the 40-Year Age Threshold for Pharmacologic Cholesterol Lowering∗. J Am Coll Cardiol. 2021;78:1965–1967. doi: 10.1016/j.jacc.2021.08.072. [DOI] [PubMed] [Google Scholar]
- 50.Hutchins R, Pignone MP, Sheridan SL, Viera AJ. Quantifying the utility of taking pills for preventing adverse health outcomes: a cross-sectional survey. BMJ Open. 2015;5:e006505. doi: 10.1136/bmjopen-2014-006505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fontana M, Asaria P, Moraldo M, Finegold J, Hassanally K, Manisty CH, Francis DP. Patient-accessible tool for shared decision making in cardiovascular primary prevention: balancing longevity benefits against medication disutility. Circulation. 2014;129:2539–2546. doi: 10.1161/CIRCULATIONAHA.113.007595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Thanassoulis G, Williams K, Altobelli KK, Pencina MJ, Cannon CP, Sniderman AD. Individualized Statin Benefit for Determining Statin Eligibility in the Primary Prevention of Cardiovascular Disease. Circulation. 2016 doi: 10.1161/CIRCULATIONAHA.115.018383. [DOI] [PubMed] [Google Scholar]
- 53.Clark TG, Bradburn MJ, Love SB, Altman DG. Survival Analysis Part I: Basic concepts and first analyses. Br J Cancer. 2003;89:232–238. doi: 10.1038/sj.bjc.6601118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Blonde L, Khunti K, Harris SB, Meizinger C, Skolnik NS. Interpretation and Impact of Real-World Clinical Data for the Practicing Clinician. Adv Ther. 2018;35:1763–1774. doi: 10.1007/s12325-018-0805-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Xin Y. The Scottish Cardiovascular Disease (CVD) Policy Model [Electronic Resource: R Source Code] 2021 [Google Scholar]
- 56.Tunstall-Pedoe H, Smith WC, Crombie IK, Tavendale R. Coronary risk factor and lifestyle variation across Scotland: results from the Scottish Heart Health Study. Scott Med J. 1989;34:556–560. doi: 10.1177/003693308903400604. [DOI] [PubMed] [Google Scholar]
- 57.Scottish Morbidity Record Completeness - Scottish Health and Social Care Open Data. Edinburgh, Scotland: Public Health Scotland; 2022. [accessed February 11, 2022]. https://www.opendata.nhs.scot/nl/dataset/scottish-morbidity-record-completeness . [Google Scholar]
- 58.Andersen PK, Geskus RB, de Witte T, Putter H. Competing risks in epidemiology: possibilities and pitfalls. Int J Epidemiol. 2012;41:861–870. doi: 10.1093/ije/dyr213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Crowther MJ, Lambert PC. Simulating Complex Survival Data. Stata J. 2012;12:674–687. doi: 10.1177/1536867X1201200407. [DOI] [Google Scholar]
- 60.StataCorp. Stata Statistical Software. College Station, TX: StataCorp LP; 2012. [Google Scholar]
- 61.Lawder R, Harding O, Stockton D, Fischbacher C, Brewster DH, Chalmers J, Finlayson A, Conway DI. Is the Scottish population living dangerously? Prevalence of multiple risk factors: the Scottish Health Survey 2003. BMC Public Health. 2010;10:330. doi: 10.1186/1471-2458-10-330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sullivan PW, Ghushchyan V. Mapping the EQ-5D Index from the SF-12. Med Decis Mak Int J Soc Med Decis Mak. 2006;26:401–409. doi: 10.1177/0272989X06290496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Geue C, Lewsey J, Lorgelly P, Govan L, Hart C, Briggs A. Spoilt for choice: implications of using alternative methods of costing hospital episode statistics. Health Econ. 2012;21:1201–1216. doi: 10.1002/hec.1785. [DOI] [PubMed] [Google Scholar]
- 64.The Health Resource Group v3.5 Toolkit [Electronic Resource: Excel Document] London, England: NHS Information Centre; 2013. [Google Scholar]
- 65.Street A, Dawson D. Costing hospital activity: the experience with healthcare resource groups in England. Eur J Health Econ HEPAC Health Econ Prev Care. 2002;3:3–9. doi: 10.1007/s10198-001-0086-1. [DOI] [PubMed] [Google Scholar]
- 66.Lloyd-Jones DM. Cardiovascular Risk Prediction: Basic Concepts, Current Status, and Future Directions. Circulation. 2010;121:1768–1777. doi: 10.1161/CIRCULATIONAHA.109.849166. [DOI] [PubMed] [Google Scholar]
- 67.West of Scotland Coronary Prevention Group. West of Scotland Coronary Prevention Study: identification of high-risk groups and comparison with other cardiovascular intervention trials. The Lancet. 1996;348:1339–1342. doi: 10.1016/S0140-6736(96)04292-4. [DOI] [PubMed] [Google Scholar]
- 68.Hotchkiss JW, Davies CA, Dundas R, Hawkins N, Jhund PS, Scholes S, Bajekal M, O’Flaherty M, Critchley J, Leyland AH, et al. Explaining trends in Scottish coronary heart disease mortality between 2000 and 2010 using IMPACTSEC model: retrospective analysis using routine data. BMJ. 2014;348:g1088. doi: 10.1136/bmj.g1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Life Expectancy in Scotland: 2018-2020. Edinburgh, Scotland: National Records of Scotland; 2021. [accessed February 11, 2022]. https://www.nrscotland.gov.uk/files//statistics/life-expectancy-in-scotland/18-20/life-expectancy-18-20-report.pdf . [Google Scholar]
- 70.Sampford MR. On Sampling Without Replacement with Unequal Probabilities of Selection. Biometrika. 1967;54:499–513. doi: 10.2307/2335041. [DOI] [PubMed] [Google Scholar]
- 71.Taylor RS, Brown A, Ebrahim S, Jolliffe J, Noorani H, Rees K, Skidmore B, Stone JA, Thompson DR, Oldridge N. Exercise-based rehabilitation for patients with coronary heart disease: systematic review and meta-analysis of randomized controlled trials. Am J Med. 2004;116:682–692. doi: 10.1016/j.amjmed.2004.01.009. [DOI] [PubMed] [Google Scholar]
- 72.Janssen KJM, Donders ART, Harrell FE, Vergouwe Y, Chen Q, Grobbee DE, Moons KGM. Missing covariate data in medical research: to impute is better than to ignore. J Clin Epidemiol. 2010;63:721–727. doi: 10.1016/j.jclinepi.2009.12.008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.