Abstract
Background
Full-scale implementation of lung cancer screening in the United States will increase detection of early stages. We aimed to assess the capacity required for treating those cancers.
Methods
A well-established microsimulation model was extended with treatment data from the National Cancer Database. We assessed changes in treatment demand when implementing lung cancer screening in 2018. Three policies were assessed: annual screening, ages 55–80, ≥30 pack-years, currently smoking or quit ≤15 years (A-55–80-30–15, USPSTF recommendations); A-55–77-30–15 (CMS); A-55–75-40–10 (Ontario). Base-case screening adherence was a constant 50%. Sensitivity analyses assessed other adherence levels, including a linear build-up to 50% between 2018–2027.
Results
The USPSTF policy requires 37.0% more lung cancer surgeries in 2015–2040 than no screening, 2.2% less radiotherapy, and 5.4% less chemotherapy. 5.7% more patients would require any therapy. The increase in surgical demand would be 96.1% in 2018, 46.0% in 2023, 38.3% in 2028, and 24.9% in 2040. Adherence strongly influenced results. By 2018, surgical demand would range from 52,619 (20% adherence) to 96,121 (80%). With gradual build-up of adherence, the increase in surgical demand would be 9.6% in 2018, 38.3% in 2023, 42.0% in 2028, and 24.4% in 2040. Results for the CMS and Ontario policies were similar, although changes compared to no screening were smaller.
Conclusions
Full-scale implementation of lung cancer screening causes a major increase in surgical demand, with a peak in the first 5 years. Gradual build-up of adherence can spread this peak over time. Careful surgical capacity planning is essential for successfully implementing screening.
Keywords: Lung Neoplasms, Early Detection of Cancer, Health Workforce, Health Resources, Therapy
Precis
Full-scale implementation of lung cancer screening in the United States will lead to a major increase in demand for thoracic surgery. Careful surgical capacity planning is essential for successfully implementing screening.
Introduction
Despite decreasing incidence rates, lung cancer is still the leading cause of cancer-related mortality in the United States (US).1 The National Lung Screening Trial (NLST) has shown that three annual Low-Dose Computed Tomography (LDCT) screenings for lung cancer can reduce lung cancer mortality by 20% compared to three annual chest radiography screenings.2 Since then, both the United States Preventive Task Force (USPSTF)3 and the Centers for Medicare & Medicaid Services (CMS)4 have issued recommendations for LDCT screening for lung cancer. The USPSTF recommendation has been partly based on modeling efforts.5
The standard of care is surgery for early-stage non-small cell lung cancer (NSCLC), a combination of chemotherapy and radiotherapy for locally-advanced NSCLC, and chemotherapy for advanced NSCLC.6 Consequently, early detection by lung cancer screening is expected to increase demand for surgery and decrease demand for radiotherapy and chemotherapy. The magnitude of this shift in treatment will depend on the number of screened individuals, which will reduce over time7 because younger birth cohorts smoke less.8
The benefits of early detection depend on the availability of adequate treatment. Hence, assessing the demand for treatment and planning for sufficient manpower are essential to successfully implementing screening. In screening programs where capacity (e.g. for follow-up) was limited, program implementation has been done gradually to take this into account.9 Therefore, the aim of this current study was to project the treatment capacity required for the full-scale implementation of LDCT screening for lung cancer in the US.
Materials and Methods
Simulation of lung cancer incidence rates
In this study we used the MIcrosimulation SCreening ANalysis Lung (MISCAN-Lung) model, which simulates individual life histories in the presence and absence of screening to project benefits and harms of different screening policies on a population level. MISCAN-Lung has been calibrated to individual-level incidence and mortality data from the NLST and the Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial.10,11 It accounts for differences in smoking behavior across birth cohorts by incorporating the National Cancer Institute’s Smoking History Generator.8 The model has been previously used to inform the USPSTF on the LDCT screening scenario with the most favorable ratio of benefits and harms for a 1950 US birth cohort.5 Also, it has been used to identify the most cost-effective scenario for Cancer Care Ontario.12
In this current analysis, we first simulated a scenario without lung cancer screening. Then, we simulated three scenarios with screening: [1] using the USPSTF recommendations, annually screening current and former smokers aged 55–80 with at least a 30 pack-years smoking history that quit fewer than 15 years ago3; [2] using the CMS recommendations, stopping screening three years earlier than the USPSTF scenario, at the age of 774; and [3] using the most cost-effective policy from a recent cost-effectiveness analysis for Cancer Care Ontario, annually screening current and former smokers aged 55–75 with at least a 40 pack-years smoking history that quit fewer than 10 years ago.12
The timeframe for this study was 2015 through 2040. We assumed that screening started in 2018 because the current uptake of lung cancer screening in the US is low.13 We simulated the full range of birth-year cohorts from 1916 (i.e. patients aged 99 years in 2015) through 2005 (i.e. patients aged 35 years in 2040). We assumed that no lung cancer occurred under the age of 35. We further assumed that the maximum age in the population was 99.
Treatment capacity requirements
For each screening scenario, we adjusted the year, gender, age, stage and histology specific lung cancer incidence rates estimated by MISCAN-Lung to the projected US population by using the Census National Population Projections.14 Therefore, we account for growth and aging of the population. Next, we obtained lung cancer treatment patterns from the National Cancer Database (NCDB) Participant User File for 440,566 lung cancer cases diagnosed between years 2010–2014. The NCDB, established in 1989, is a nationwide, facility-based, comprehensive clinical surveillance resource oncology data set that currently captures 70% of all newly diagnosed malignancies in the US annually, from more than 1500 affiliated facilities. The NCDB is a joint project of the Commission on Cancer of the American College of Surgeons and the American Cancer Society. Analysis of individual-level NCDB data was performed on site at the University of Michigan Medical School. Details of the analysis of the NCDB data, including case selection and data cleaning are provided as Supplementary Methods in the Supporting Information. In short, we obtained the gender, age, stage, and histology specific proportions of lung cancer patients that received surgery, radiotherapy, chemotherapy, and any therapy as first course treatment. As treatment patterns among lung cancer patients in the NCDB remained stable over time (see Supporting Figure 1), the mean treatment proportions across years 2010–2014 were used in this study (see Supporting Table 1). For each scenario that we simulated, we then calculated the required lung cancer treatment capacity by multiplying the year, gender, age, stage and histology specific Census-adjusted incidence from MISCAN-Lung with the mean gender, age, stage and histology specific treatment proportions from the NCDB. In the base-case analysis, the same treatment proportions were applied to screen-detected cases and clinically detected cases. As screen-detected cases may have less comorbidity than clinically detected cases, a sensitivity analysis was also performed that uses stage-specific treatment proportions from the LDCT arm of the NLST for screen-detected cases (see Supporting Table 2).2
Effect of adherence
Based on the results of an implementation study of lung cancer screening in the US Veterans Affairs Administration, we assumed a constant screening adherence of 50% for the base-case analysis.15 Another study in the Stanford Health Care system reported an adherence level of 60%.16 That study also reported national adherence rates of 69% for colorectal cancer screening, 79% for breast cancer screening, and 75% for cervical cancer screening in the US. We assume that it is unlikely that adherence to lung cancer screening will surpass that of existing screening programs in the near future. Therefore, we assessed the effect of constant adherence levels of 20%, 35%, 65% and 80% in a sensitivity analysis. In a second sensitivity analysis, we assessed the effect of a linear build-up of screening adherence from 5% in 2018 to a plateau of 50% from 2027 onwards.
Statistical Analysis
All analyses were performed using the MISCAN-Lung model and R software version 3.4.1.17
Results
Simulation of lung cancer incidence rates
In 2018, the projected number of screening eligible persons in the US population would be 11,816,790 for the USPSTF scenario, 11,258,937 for the CMS scenario, and 6,505,609 for the Ontario scenario (Supporting Fig. 2). By 2023, screening eligibility would decrease to 10,192,541 (USPSTF), 9,574,244 (CMS), and 5,548,430 (Ontario). By 2040, 4,710,017 persons would be eligible in the USPSTF scenario, 4,145,176 in the CMS scenario, and 2,322,388 in the Ontario criteria.
In the absence of screening, annual Census-adjusted lung cancer incidence would increase to 215,392 cases by 2033 and would then then gradually decrease (see Supporting Fig. 3). The implementation in 2018 of a screening program with a constant 50% adherence would lead to an immediate peak in incidence compared to no screening. This peak would be highest for the USPSTF scenario (n=253,938), followed by the CMS scenario (n=247,556) and the Ontario scenario (n=233,841). With a gradual build-up of adherence, this peak would be lower but last longer (Supporting Fig. 4).
Over the entire study period, the cumulative number of lung cancer cases would be 5,525,593 for the USPSTF scenario, 5,495,049 for the CMS scenario, 5,462,657 for the Ontario scenario, and 5,402,854 for the no screening scenario (Supporting Table 3).The proportion of screen-detected cases would be 16.8% (USPSTF), 14.3% (CMS), and 10.1% (Ontario). In the absence of screening, 22.2% of clinically detected cases would be diagnosed in stage I, 5.9% in stage II, 25.5% in stage III, and 46.3% in stage IV (see Figure 1A). Among screen-detected cases in the USPSTF scenario, 65.6% would be diagnosed in stage I, 6.8% in stage II, 16.5% in stage III, and 11.1% in stage IV (see Figure 1B). For both clinically detected and screen-detected cases, differences in stage distribution across scenarios were minimal. Overall, the proportion of cases diagnosed in stage I would be 30.6% in the USPSTF scenario, 29.4% in the CMS scenario, and 27.3% in the Ontario scenario, compared to 22.2% without screening (see Fig. 1C). Conversely, the proportion of cases diagnosed in stage IV decreased due to screening: from 46.3% without screening to 38.9% (USPSTF), 40.0% (CMS), and 41.8% (Ontario).
Figure 1.
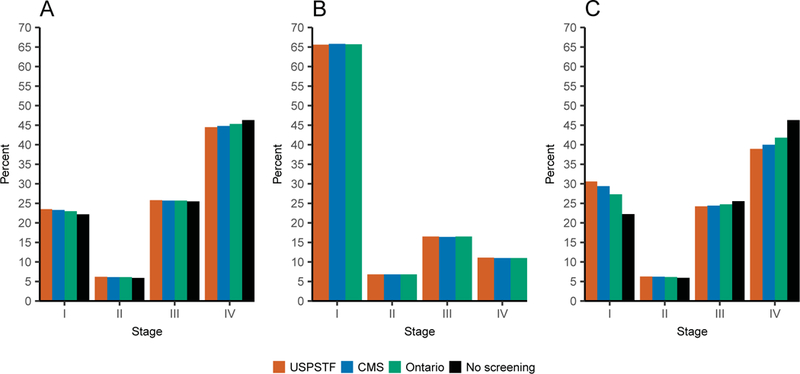
Distribution of stage at diagnosis for (A) clinically detected lung cancer cases; (B) screen-detected cases; and (C) all cases in the United States between 2015–2040 in the absence of Low-Dose Computed Tomography screening and for three screening policies implemented in 2018. All policies assumed a constant 50% adherence to screening. USPSTF, United States Preventive Task Force recommendations, annually screening current and former smokers aged 55–80 with at least a 30 pack-years smoking history that quit fewer than 15 years ago; CMS, the Centers for Medicare & Medicaid Services recommendations, annually screening current and former smokers aged 55–77 with at least a 30 pack-years smoking history that quit fewer than 15 years ago; Ontario, the most cost-effective policy from a study for Cancer Care Ontario, annually screening current and former smokers aged 55–75 with at least a 40 pack-years smoking history that quit fewer than 10 years ago.
Treatment capacity requirements
Figure 2 shows the change in lung cancer therapy due to the implementation of LDCT screening in 2018. The main change would be a large cumulative increase in demand for lung cancer surgery. At the base-case adherence of 50%, demand for lung cancer surgery would increase compared to no screening by 37.0% (USPSTF), 32.1% (CMS), and 22.8% (Ontario). However, demand for radiotherapy would decrease by 2.2% (USPSTF), 2.6% (CMS), and 2.1% (Ontario). Demand for chemotherapy would decrease by 5.4% (USPSTF), 5.1% (CMS), and 3.8% (Ontario). Finally, the number of patients that would receive any therapy would increase by 5.7% (USPSTF), 4.5% (CMS), and 3.0% (Ontario). When assuming that screen-detected cases receive stage-specific treatment as reported in the NLST, the increase in surgery compared to no screening would be 55.3% (USPSTF), 46.3% (CMS), and 32.3% (Ontario) (Supporting Figure 5). Demand for radiotherapy would decrease by 7.4% (USPSTF), 6.8% (CMS), and 5.1% (Ontario). Chemotherapy demand would decrease by 4.3% (USPSTF), 4.7% (CMS), and 3.7% (Ontario). Finally, demand for any therapy would increase by 7.6% (USPSTF), 5.9% (CMS), and 3.9% (Ontario).
Figure 2.
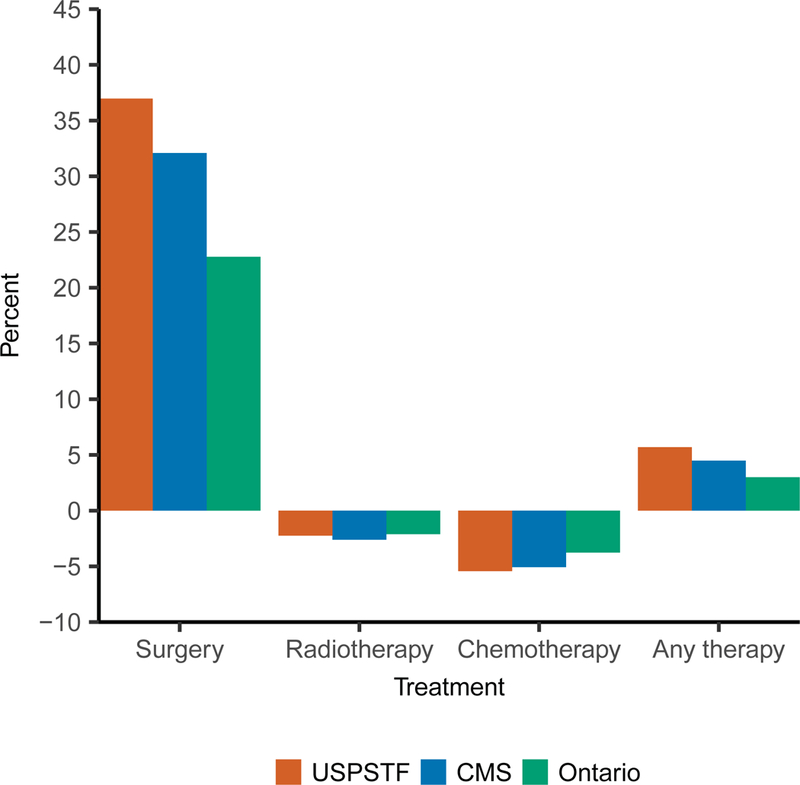
Cumulative change in demand for lung cancer therapy in the United States between 2015–2040 when implementing Low-Dose Computed Tomography screening for lung cancer in 2018. Expressed as cumulative percentage change compared to no screening. All policies assumed a constant 50% adherence to screening. USPSTF, United States Preventive Task Force recommendations, annually screening current and former smokers aged 55–80 with at least a 30 pack-years smoking history that quit fewer than 15 years ago; CMS, the Centers for Medicare & Medicaid Services recommendations, annually screening current and former smokers aged 55–77 with at least a 30 pack-years smoking history that quit fewer than 15 years ago; Ontario, the most cost-effective policy from a study for Cancer Care Ontario, annually screening current and former smokers aged 55–75 with at least a 40 pack-years smoking history that quit fewer than 10 years ago.
Figure 3 shows the absolute annual number of lung cancer treatments required between 2015 and 2040 for the base-case scenario. Supporting Table 4 additionally shows the percentage change compared to no screening in 2018, 2023, 2028, and 2040. In the absence of screening, the annual required number of lung cancer surgeries would remain relatively constant: 37,964 in 2018, 38,903 in 2023, 38,876 in 2028, and 34,021 in 2040. Implementing the USPSTF recommendations would increase demand for lung cancer surgery compared to no screening by 96.1% in 2018, 46.0% in 2023, 38.3% in 2028, and 24.9% in 2040. In the CMS scenario, the increase compared to no screening would be 87.5% (2018), 41.2% (2023), 33.0% (2028), and 19.7% (2040). Finally, implementing the Ontario recommendations would increase demand compared to no screening by 64.5% in 2018, 30.1% in 2023, 23.7% in 2028, and 13.1% in 2040.
Figure 3.
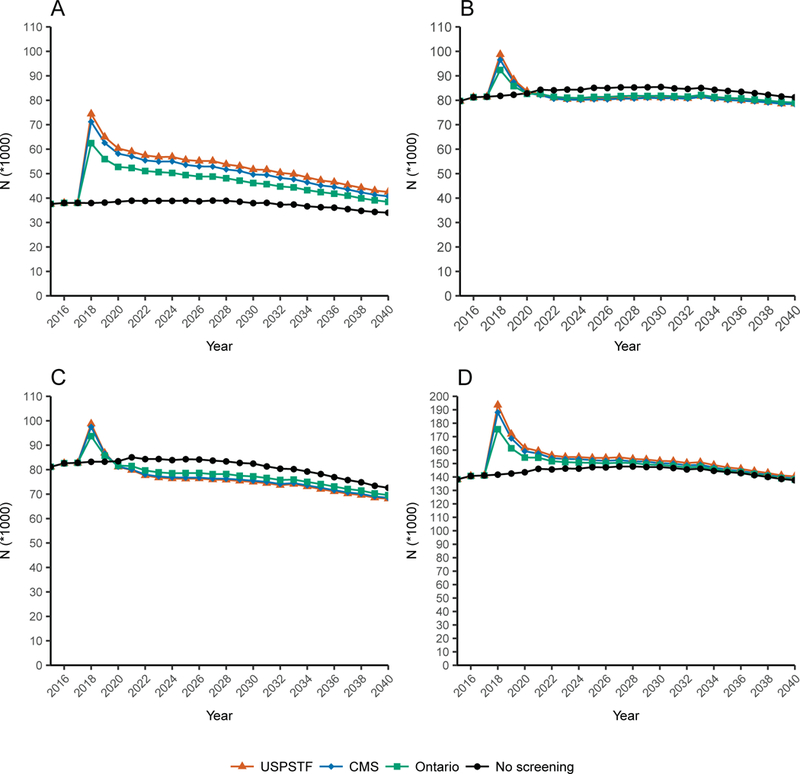
Absolute annual number of lung cancer patients in the United States requiring (A) surgery; (B) radiotherapy; (C) chemotherapy; and (D) any therapy when implementing Low-Dose Computed Tomography screening for lung cancer in 2018. All policies assumed a constant 50% adherence to screening. USPSTF, United States Preventive Task Force recommendations, annually screening current and former smokers aged 55–80 with at least a 30 pack-years smoking history that quit fewer than 15 years ago; CMS, the Centers for Medicare & Medicaid Services recommendations, annually screening current and former smokers aged 55–77 with at least a 30 pack-years smoking history that quit fewer than 15 years ago; Ontario, the most cost-effective policy from a study for Cancer Care Ontario, annually screening current and former smokers aged 55–75 with at least a 40 pack-years smoking history that quit fewer than 10 years ago.
In the absence of screening, the annual number lung cancer patients requiring radiotherapy would increase from 81,802 in 2018 to 84,378 in 2023 and 85,242 in 2028, after which it would gradually decrease to 81,219 in 2040. Implementing the USPSTF recommendations would first increase demand for radiotherapy by 20.7% in 2018. However, demand would decrease compared to no screening shortly after that, by 4.7% in 2023, 5.1% in 2028, and 3.3% in 2040. Results for the CMS and Ontario scenarios were similar, although differences compared to no screening were less pronounced.
We found a similar pattern for the number of cases that required chemotherapy. In the absence of screening, demand for chemotherapy would be 83,221 in 2018, 84,351 in 2023, 83,366 in 2028, and 72,586 in 2040. In the USPSTF scenario, demand would first increase by 18.7% in 2018, followed by a relative decrease compared to no screening of 9.0% in 2023 and 2028, and 6.2% in 2040.
Finally, the number of lung cancer cases that would receive any therapy in the no screening scenario would increase from 141,751 in 2018 to 146,288 in 2023, and 147,815 in 2028. Then, it would decrease to 137,607 in 2040. For each screening scenario, the number of cases receiving any therapy peaked in 2018: +36.5% compared to no screening (USPSTF), +32.7% (CMS), and +23.8% (Ontario). The difference compared to no screening would then get smaller within five years after implementation. For the USPSTF scenario, the increase compared to no screening would be 5.9% in 2023, 3.8% in 2028, and 2.1% in 2040.
Effect of adherence
Figure 4 shows the effect of different levels of constant screening adherence on the number of patients requiring lung cancer surgery for the USPSTF scenario. In 2018, the required surgical capacity would be 52,619 (20% adherence), 63,623 (35%), 74,437 (50%), 85,312 (65%), and 96,121 (80%). When considering a lower limit of 20% adherence and 80% adherence as the upper limit, the number of surgeries would range from 47,790 to 62,849 in 2023, from 46,213 to 58,752 in 2028, and from 38,259 to 45,172 in 2040. Results for the CMS and Ontario scenarios are shown in Supporting Figure 6 and Supporting Figure 7, respectively.
Figure 4.

Absolute annual number of lung cancer patients in the United States requiring surgery when implementing Low-Dose Computed Tomography screening for lung cancer in 2018 using the United States Preventive Task Force criteria at different constant screening adherence levels. USPSTF, United States Preventive Task Force recommendations, annually screening current and former smokers aged 55–80 with at least a 30 pack-years smoking history that quit fewer than 15 years ago.
Figure 5 and Supporting Table 5 show the effect of a linear build-up of screening adherence from 5% in 2018 to a constant 50% from 2027. In 2018, the increase in surgical demand compared to no screening would be 9.6% (USPSTF), 8.7% (CMS), and 7.9% (Ontario). In 2023, the increase would be 38.3% (USPSTF), 34.2% (CMS), and 30.4% (Ontario). In 2028, the increase would be 42.0% (USPSTF), 36.1% (CMS), and 31.6% (Ontario). Finally, in 2040 the increase would be 24.4% (USPSTF), 19.4% (CMS), and 16.1% (Ontario). For the USPSTF scenario, demand for radiotherapy would change compared to no screening by +2.1% (in year 2018), +1.7% (2023), −2.9% (2028), and −3.4% (2024). Demand for chemotherapy would change by +1.9% (2018), −0.6% (2023), −6.8% (2028), and −6.2% (2040). Finally, demand for any therapy would change by +3.7% (2018), +9.3% (2023), +6.3% (2028), and +1.9% (2040). Changes in demand for radiotherapy, chemotherapy, and any therapy for the CMS and Ontario scenarios were similar to the USPSTF scenario but less pronounced.
Figure 5.
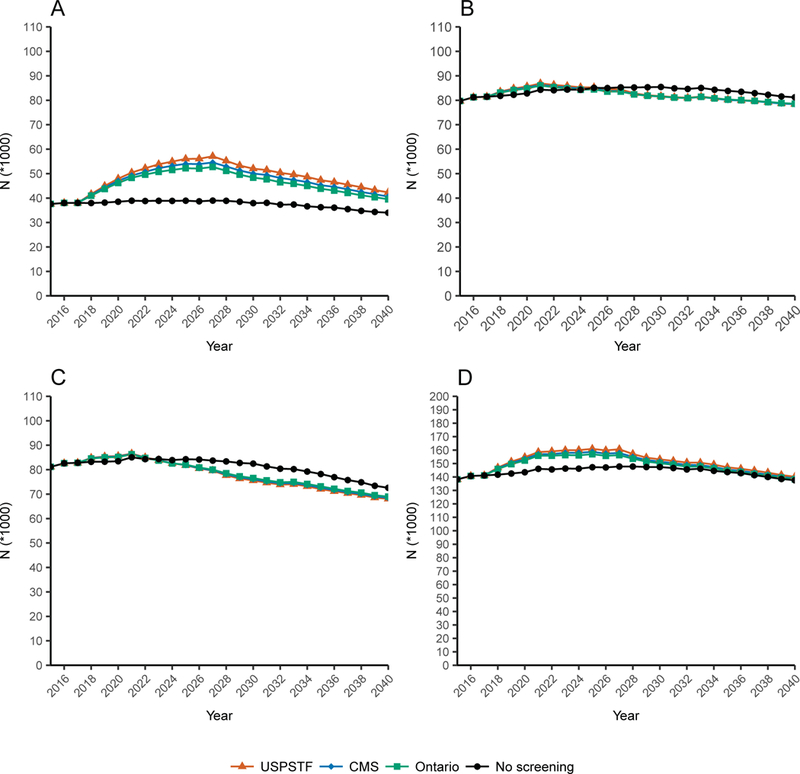
Absolute annual number of lung cancer patients in the United States requiring (A) surgery; (B) radiotherapy; (C) chemotherapy; and (D) any therapy when implementing Low-Dose Computed Tomography screening for lung cancer in 2018. All policies assume an adherence level of 5% in 2018, with an annual 5 percentage point increase until a constant adherence of 50% is reached in 2027.USPSTF, United States Preventive Task Force recommendations, annually screening current and former smokers aged 55–80 with at least a 30 pack-years smoking history that quit fewer than 15 years ago; CMS, the Centers for Medicare & Medicaid Services recommendations, annually screening current and former smokers aged 55–77 with at least a 30 pack-years smoking history that quit fewer than 15 years ago; Ontario, the most cost-effective policy from a study for Cancer Care Ontario, annually screening current and former smokers aged 55–75 with at least a 40 pack-years smoking history that quit fewer than 10 years ago.
Discussion
The aim of this study was to quantify the expected treatment capacity required for the full-scale implementation of LDCT screening for lung cancer in the US.
Simulation of lung cancer incidence rates
The introduction of screening caused an immediate peak in lung cancer incidence. This initial peak is due to the lead-time of screen-detected preclinical cases, which would have otherwise been clinically detected later in time.
We found that screening caused a shift in stage at diagnosis from stage IV to stage I. This stage shift was more pronounced for scenarios with less stringent eligibility criteria (i.e. stage shift for USPSTF > CMS > Ontario), which may be explained by the higher number (and proportion) of screen-detected cases in those scenarios (see Supporting Table 3). In the NLST, which followed participants from 2002–2009, the proportion of stage I lung cancers in the LDCT arm was 50.0%.2 This is much higher than the 30.6% that we found in the USPSTF scenario. This difference may be explained by three reasons. Most importantly, our simulation of the general population included all lung cancer cases, not just those detected in the screen-eligible population. Second, we conducted our model under assumptions of much lower (and perhaps more realistic) screening adherence (50%) than was achieved in the NLST (>90%).2 Third, our results are projected from 2015–2040, and therefore include younger cohorts than the NLST. A previous MISCAN-Lung simulation of the 1950 cohort found that 48% of lung cancer cases were diagnosed in stage I-II when implementing the USPSTF recommendations.5 In our current analysis, this proportion was only 36.9%. This may be explained by declining smoking trends for younger birth cohorts,8 which causes fewer individuals to be eligible for screening.7 These findings underline the necessity of modeling multiple birth cohorts when assessing lung cancer interventions over a time period.
Treatment capacity requirements
We found that the implementation of lung cancer screening would lead to a substantial increase in demand for lung cancer surgery. A previous study that investigated the radiological capacity requirements for implementing lung cancer screening in the US defined capacity constraints as “a greater than 5% and (alternatively) greater than 25% projected increase in scans”.18 If we apply the 5% increase criterion to our base-case estimates, surgical capacity would be restrained in every year, for each scenario, and at each adherence level. If we apply the 25% increase criterion to our base-case estimates, capacity would be restrained for each scenario and adherence level in 2018. By 2023, capacity would be restrained for the USPSTF and CMS scenarios with ≥35% adherence and for the Ontario scenarios with ≥50% adherence. Finally, by 2040 capacity would only be restrained for the USPSTF scenarios with ≥65% adherence and the CMS scenario with 80% adherence. When using the treatment proportions from the NLST for screen-detected cases, surgical capacity constraints would be even more pronounced. However, as the NLST was conducted under selective and controlled circumstances, these estimates should be considered an upper bound. Finally, when we apply the 5% criterion to the results of the sensitivity analysis with a gradual build-up of adherence, surgical capacity would still be restrained in each year for each scenario. If we apply the 25% increase criterion to the same analysis, capacity would be not be restrained in 2018. However, capacity would still be restrained in 2023 and 2028 for each scenario.
Thoracic surgeons have lower operative and postoperative mortality rates for lung cancer surgery than general surgeons.19,20 Consequently, guidelines state that thoracic surgeons should be involved in treating screen-detected lung cancer.21,22 However, earlier research projected that future demand for thoracic surgeons will increase while supply will decline.23 Moffatt-Bruce and colleagues reported that by 2035 the caseload per thoracic surgeon may increase by 121%, without taking into account lung cancer screening.24 Additionally, Edwards and colleagues reported that implementing LDCT lung cancer screening in Canada in 2014 could increase the number of operable (i.e. stage I and II) lung cancer cases per thoracic surgeon by 19.8% in 2030.25 However, our analysis of NCDB data indicates that many stage I and II NSCLC cases in fact do not receive surgery. Nevertheless, these studies provide indications that the current workforce of thoracic surgeons may not be able to cope with the additional demand caused by lung cancer screening.
Residency training of additional thoracic surgeons takes on average 8.7 years26. However, the projected surgical demand peaked in the first 5 years after the implementation of screening. This peak would be more spread out over time with a gradual build-up of adherence. However, delaying the full-scale implementation of lung cancer screening may reduce the potential health benefits because smoking trends have been declining.7 Therefore, our data suggest that training of additional thoracic surgeons should start as soon as possible. In the meantime, careful assessment and allocation of available capacity should be undertaken to ensure maximum benefits of lung cancer screening.
We found that the overall reduction in demand for radiotherapy (−2.2%) and chemotherapy (−5.4%) was smaller than the overall increase in demand for surgery (+37.0%). This is due to three reasons. First, patients could receive multiple treatments. Second, radiotherapy and chemotherapy demand first increased due to the large incidence peak, and then decreased. Third, demand for surgery in the absence of screening was much lower than demand for radiotherapy and chemotherapy. The initial peak in demand for radiotherapy would only exceed a 25% increase compared to no screening by 2018, and only for the base-case USPSTF scenarios with ≥65% adherence and the CMS scenario with 80% adherence. Similarly, the initial increase in demand for chemotherapy compared to no screening would only surpass the 25% mark in 2018 for the base-case USPSTF and CMS scenarios with 80% adherence. Therefore, it is unlikely that the implementation of lung cancer screening will cause a major shortage of radiation oncology or chemotherapy services.
Limitations
There are several potential limitations to this current study. First, earlier research has identified treatment disparities among US lung cancer patients by race27 and insurance status.28 While these disparities are implicitly accounted for by using the NCDB data, which covers 70% of incident cancer cases in the US, MISCAN-Lung currently does not explicitly model the effect of these variables.
Second, our model is currently unable to estimate lung cancer incidence on a state level, while lung cancer incidence rates have been shown to vary by state.29 This should be the subject of future research, so that policy makers can plan treatment capacity on a local level. Policy makers should also note that simply increasing the number of trained thoracic surgeons may not be sufficient if patients at the highest risk for lung cancer are also encumbered by geographical (distance) or financial (health insurance) barriers to access.
Third, we do not model recurrent tumors. Also, the NCDB records only the first course of therapy, defined as all methods of treatment recorded in the treatment plan and administered to the patient before disease progression or recurrence. This might lead to an underestimation of the total number treatments required for the implementation of lung cancer screening.
Finally, as we project demand in the future there may be some future developments that could alter our estimates. For instance, we could not project the demand for targeted or immunotherapy agents because these are very recent developments. Furthermore, while current guidelines only recommend Stereotactic Body Radiotherapy for medically inoperable early-stage NSCLC patients,6 there is an ongoing debate on its appropriateness in operable patients.30,31. Therefore, the proportion of early-stage cases that require radiotherapy could increase in the future. Two other developments that may possibly alter our estimates are the introduction of risk models to select individuals for screening and the use of nodule management strategies such as Lung-RADS. Finally, If future developments would allow clinicians to distinguish indolent screen-detected cancers which would never cause symptoms from more aggressive cancers, overdiagnosis could decrease. In turn this could decrease treatment demand.
Conclusion
We show that full-scale implementation of lung cancer screening in the US will cause a major increase in demand for lung cancer surgery, with a peak within the first 5 years. The current workforce of thoracic surgeons may not be able to cope with this increased demand. The question is whether this could jeopardize the benefits of screening. Although a gradual build-up of adherence can spread the peak in surgical demand over time, a delayed implementation of screening may reduce the potential health benefits. Therefore, implementation of lung cancer screening can only be done with careful assessment and allocation of surgical capacity.
Supplementary Material
Acknowledgments
Disclosure of funding
This work was funded by Grant 1U01CA199284–01 from the National Cancer Institute as part of the Cancer Intervention and Surveillance Modelling Network (CISNET). The National Cancer Institute had no involvement in the study design, analysis and interpretation of data, in the writing of the report, or in the decision to submit the article for publication.
Footnotes
Conflicts of interest
HJdK, KtH and EFB are members of the Cancer Intervention and Surveillance Modeling Network (CISNET) Lung working group (grant 1U01CA199284–01 from the National Cancer Institute). HJdK is the principal investigator of the Dutch-Belgian Lung Cancer Screening Trial (Nederlands-Leuvens Longkanker Screenings onderzoek; the NELSON trial). KtH and EFB are researchers affiliated with the NELSON trial. HJdK and KtH received a grant from the University of Zurich to assess the cost- effectiveness of computed tomographic lung cancer screening in Switzerland. HJdK took part in a one-day advisory meeting on biomarkers organized by M.D. Anderson/Health Sciences during the 16th World Conference on Lung Cancer. KtH was an invited speaker at the 4th IASLC SSAC CT Screening workshop on Saturday 3rd December 2016, prior to the IASLC World Conference on lung cancer in Vienna. Travel expenses in part paid by the IASLC SSAC Organizing Committee. HJdK and KtH were involved in the Cancer Care Ontario Health Technology Assessment Study for CT Lung Cancer Screening in Canada. DAA was part of a paid medical advisory board for Nucleix, convened at the IASLC World Conference on lung cancer in Vienna, and is a member of the IASLC Smoking Cessation and Tobacco Control Committee.
References
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68:7–30. [DOI] [PubMed] [Google Scholar]
- 2.Aberle DR, Adams AM, Berg CD, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365:395–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moyer VA. Screening for Lung Cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2014;160:330–338. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Medicare & Medicaid Services. Decision Memo for Screening for Lung Cancer with Low Dose Computed Tomography (LDCT) (CAG-00439N). https://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId=274 Accessed July 7, 2018.
- 5.de Koning HJ, Meza R, Plevritis SK, et al. Benefits and harms of computed tomography lung cancer screening strategies: a comparative modeling study for the U.S. Preventive Services Task Force. Ann Intern Med. 2014;160:311–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Comprehensive Cancer Network. Clinical Practice Guidelines in Oncology: Non-Small Cell Lung Cancer Version 5.2017. https://www.nccn.org/professionals/physician_gls/pdf/nscl.pdf Accessed April 20, 2017. [DOI] [PubMed]
- 7.Criss SD, Sheehan DF, Palazzo L, Kong CY. Population impact of lung cancer screening in the United States: Projections from a microsimulation model. PLOS Med. 2018;15:e1002506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Holford TR, Levy DT, McKay LA, et al. Patterns of birth cohort-specific smoking histories, 1965–2009. Am J Prev Med. 2014;46:e31–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.van Hees F, Zauber AG, van Veldhuizen H, et al. The value of models in informing resource allocation in colorectal cancer screening: the case of The Netherlands. Gut. 2015;64:1985–1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Meza R, ten Haaf K, Kong CY, et al. Comparative analysis of 5 lung cancer natural history and screening models that reproduce outcomes of the NLST and PLCO trials. Cancer. 2014;120:1713–1724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.ten Haaf K, van Rosmalen J, de Koning HJ. Lung cancer detectability by test, histology, stage, and gender: estimates from the NLST and the PLCO trials. Cancer Epidemiol Biomarkers Prev. 2015;24:154–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.ten Haaf K, Tammemägi MC, Bondy SJ, et al. Performance and Cost-Effectiveness of Computed Tomography Lung Cancer Screening Scenarios in a Population-Based Setting: A Microsimulation Modeling Analysis in Ontario, Canada. PLOS Med. 2017;14:e1002225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jemal A, Fedewa SA. Lung Cancer Screening With Low-Dose Computed Tomography in the United States-2010 to 2015. JAMA Oncol. 2017;3:1278–1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Unites States Census Bureau. 2014. National Population Projections Tables. https://www.census.gov/data/tables/2014/demo/popproj/2014-summary-tables.html Released December, 2014 Accessed January 1, 2018.
- 15.Kinsinger LS, Anderson C, Kim J, et al. Implementation of Lung Cancer Screening in the Veterans Health Administration. JAMA Intern Med. 2017;177:399–406. [DOI] [PubMed] [Google Scholar]
- 16.Duong DK, Shariff-Marco S, Cheng I, et al. Patient and primary care provider attitudes and adherence towards lung cancer screening at an academic medical center. Prev Med Rep. 2017;6:17–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.R: A Language and Environment for Statistical Computing [computer program]. Version 3.4.1. Vienna, Austria: R Foundation for Statistical Computing; 2017. [Google Scholar]
- 18.Smieliauskas F, MacMahon H, Salgia R, Shih YC. Geographic variation in radiologist capacity and widespread implementation of lung cancer CT screening. J Med Screen. 2014;21:207–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goodney PP, Lucas FL, Stukel TA, Birkmeyer JD. Surgeon specialty and operative mortality with lung resection. Ann Surg. 2005;241:179–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.von Meyenfeldt EM, Gooiker GA, van Gijn W, et al. The relationship between volume or surgeon specialty and outcome in the surgical treatment of lung cancer: a systematic review and meta-analysis. J Thorac Oncol. 2012;7:1170–1178. [DOI] [PubMed] [Google Scholar]
- 21.Jaklitsch MT, Jacobson FL, Austin JH, et al. The American Association for Thoracic Surgery guidelines for lung cancer screening using low-dose computed tomography scans for lung cancer survivors and other high-risk groups. J Thorac Cardiovasc Surg. 2012;144:33–38. [DOI] [PubMed] [Google Scholar]
- 22.Pedersen JH, Rzyman W, Veronesi G, et al. Recommendations from the European Society of Thoracic Surgeons (ESTS) regarding computed tomography screening for lung cancer in Europe. Eur J Cardiothorac Surg. 2017;51:411–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Grover A, Gorman K, Dall TM, et al. Shortage of cardiothoracic surgeons is likely by 2020. Circulation. 2009;120:488–494. [DOI] [PubMed] [Google Scholar]
- 24.Moffatt-Bruce S, Crestanello J, Way DP, Williams TE Jr., Providing cardiothoracic services in 2035: Signs of trouble ahead. J Thorac Cardiovasc Surg. 2018;155:824–829. [DOI] [PubMed] [Google Scholar]
- 25.Edwards JP, Datta I, Hunt JD, et al. The impact of computed tomographic screening for lung cancer on the thoracic surgery workforce. Ann Thorac Surg. 2014;98:447–452. [DOI] [PubMed] [Google Scholar]
- 26.Ikonomidis JS. The Society of Thoracic Surgeons Thoracic Surgery Practice and Access Task Force: 2014 Workforce Report. Ann Thorac Surg. 2016;102:2118–2125. [DOI] [PubMed] [Google Scholar]
- 27.Bach PB, Cramer LD, Warren JL, Begg CB. Racial differences in the treatment of early-stage lung cancer. N Engl J Med. 1999;341:1198–1205. [DOI] [PubMed] [Google Scholar]
- 28.Groth SS, Al-Refaie WB, Zhong W, et al. Effect of insurance status on the surgical treatment of early-stage non-small cell lung cancer. Ann Thorac Surg. 2013;95:1221–1226. [DOI] [PubMed] [Google Scholar]
- 29.U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute. U.S. Cancer Statistics Data Visualizations Tool, based on November 2017 submission data (2011–2015). https://gis.cdc.gov/Cancer/USCS/DataViz.html Accessed July 3, 2018.
- 30.Senan S, Paul MA, Lagerwaard FJ. Treatment of early-stage lung cancer detected by screening: surgery or stereotactic ablative radiotherapy? Lancet Oncol. 2013;14:e270–274. [DOI] [PubMed] [Google Scholar]
- 31.Tandberg DJ, Tong BC, Ackerson BG, Kelsey CR. Surgery versus stereotactic body radiation therapy for stage I non-small cell lung cancer: A comprehensive review. Cancer. 2018;124:667–678. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


