Abstract
Cholesterol crystals (CC) are strong activators of complement and could potentially be involved in thromboinflammation through complement-coagulation cross-talk. To explore the coagulation inducing potential of CC, we performed studies in lepirudin-based human whole blood and plasma models. In addition, immunohistological examinations of brain thrombi and vulnerable plaque material from patients with advanced carotid atherosclerosis were performed using polarization reflected light microscopy to identify CC. In whole blood, CC exposure induced a time- and concentration dependent generation of prothrombin fragment 1+2 (PTF1.2), TF mRNA synthesis and monocyte tissue factor (TF) expression. Blocking antibodies against TF abolished CC-mediated coagulation, thus indicating involvement of the TF-dependent pathway. Blockade of FXII by corn trypsin inhibitor had a significant inhibitory effect on CC induced PTF1.2 in platelet free plasma, although the overall activation potential was low. CC exposure did not induce platelet aggregation, TF-microparticle induction, or TF on granulocytes or eosinophils. Inhibition of complement C3 by CP40 (compstatin), C5 by eculizumab or C5aR1 by PMX53 blocked CC-induced PTF1.2 by 90%, and reduced TF-positive monocytes from 18-20% to 1-2%. The physiologic relevance was supported by birefringent CC structures adjacent to monocytes (CD14), TF and activated complement iC3b and C5b-9 in a human brain thrombus. Furthermore, monocyte influx and TF induction in close proximity to CC rich regions with activated complement was found in a vulnerable plaque. In conclusion, CC could be active releasable contributors to thrombosis by inducing monocyte TF secondary to complement C5aR1 signalling.
Introduction
The World Health Organization (WHO) estimates that cardiovascular disease (CVD) causes more than 17 million deaths every year. Of these, 80% are due to myocardial infarction or ischemic stroke as a result of thrombosis obstructing blood flow to the heart or brain, respectively (1). Thrombosis occurs following atherosclerotic plaque rupture and involves lesion derived tissue factor (TF) from endothelial cells (2), plaque macrophages (3, 4) and blood monocytes following exposure to oxidized LDL (oxLDL) and C-reactive protein (CRP) (5, 6). Cholesterol crystals (CC) formed upon oxLDL accumulation at the lesion sites are hallmarks of atherosclerotic plaques. (7) Their sharp, needle-like structure promotes erosion of the fibrous cap and thereby plaque rupture with release into blood. (8) Except for their role in promoting plaque rupture, CC are considered passive participators in the thrombotic events.
CC activate the complement system, (9, 10) whereas their role as direct promoters of coagulation has not yet been investigated. The recent finding of CC being strong inducers of complement-dependent inflammatory processes (11) raises the question if CC could activate coagulation through thromboinflammation. This question is further justified in light of evidence of crosstalk between the complement and coagulation cascades (12-16).
The complement and coagulation cascades are first-line defense systems, mediating inflammation and clot formation, respectively. Both consist of circulating zymogens converting to reactive proteases upon proteolytic activation (12). Complement can be activated through the classical-, lectin- or alternative pathways, converging in the formation of C3 convertases. Downstream formation of C5 convertases cleaves C5 and leads to formation of C5a, a highly potent pro-inflammatory mediator (17), and the terminal complement complex (TCC, C5b-9). Of note, CC induce activation of all the three complement pathways (18).
The coagulation system is activated either through the intrinsic pathway, activating FXII to FXIIa on a surface, or through the extrinsic pathway by binding of FVIIa to cellular expressed TF. Both pathways converge in the activation of FX to FXa with subsequent cleavage of prothrombin to thrombin. This leads to the conversion of circulating fibrinogen to insoluble fibrin. Together with activated platelets, this process builds up a stable thrombus. TF is the major initiator of blood coagulation in vivo, and is under normal conditions only expressed on extravascular cells. However, circulating monocytes are capable of expressing TF on their surface when exposed to pro-inflammatory stimuli, including lipopolysaccharide (LPS), tumor necrosis factor (TNF), CRP and C5a (19). The latter demonstrates one of the most important points of crosstalk between the complement and coagulation systems (12).
Activated factors of complement and coagulation are evident within aspirates of human atherosclerotic plaques and thrombi. More specifically, TCC as well as mRNA of complement C1r, C1s, and C4 are found within atherosclerotic lesions (20). C3 has been detected in thrombi, (21) and C3a and C5a have been shown to be increased in surrounding plasma at the site of thrombus formation (22). This suggests local complement activation within the plaque and thrombi. Leukocyte-associated TF has also been found in thrombi, and is thought to contribute to clot propagation and growth (23).
Since CC activate complement, and there is an increased recognition of complement-coagulation crosstalk, the aim of the present study was to investigate the role of CC in thrombosis by studying their activation of coagulation and the dependency of complement activation in this process.
Materials and methods
Reagents
This work includes the following reagents; anticoagulant Lepirudin (Refludan®) from Celgene Europe (Boudry, Switzerland), sterile phosphate-buffered saline (PBS ± Ca2+ and Mg2+) and ethylenediaminetetraacetic acid (EDTA) from Sigma-Aldrich (St. Louis, MO). Human serum albumin (HSA) from Octapharma (Jessheim, Norway). Heat-inactivated E. coli strain LE392 (ATCC 33572) from American Type Culture Collection (Manassas, VA, USA). CryoTubes (polypropylene) from Nunc AS (Roskilde, Denmark). Complement inhibitors; Compstatin analog CP40 (sequence: 14-amino acid cyclic peptide ((D)Tyr-Ile-[Cys-Val-Trp(Me)-Gln-Asp-Trp-Sar-Ala-His-Arg-Cys]-mIle-NH2) and a control peptide (Sar-Sar-Trp(Me)-Ala-Ala-Asp-Ile-His-Val-Gln-Arg-mlle-Trp-Ala-NH2) synthesized as described (24), C5 inhibitor eculizumab (Soliris®) from Alexion Pharmaceuticals (New Haven, CT) and control rituximab (Roche, Basel, Switzerland), and cyclic peptide C5aR1 antagonist PMX53 (AcPhe-[Orn-Pro-dCha-Trp-Arg]) synthesized as described (25) . Tissue factor inhibitor; the functional grade purified inhibitory antibody against human TF (HTF-1) from eBioscience (San Diego, CA) and Ultra-leaf purified Mouse IgG1κ (MG1–45, 400165) from BioLegend (San Diego, CA). Factor XII inhibitor; Corn trypsin inhibitor (CTI-01) from Haematologic Technologies Inc. (Essex Junction, VT). Flow cytometry antibodies; anti-CD14 FITC (MΦP9) from BD Biosciences (345784), anti-HLA-DR APC-Cy7 (L243) from BioLegend (307602), anti-Siglec-8 APC (7C9) from BioLegend (347106), anti-tissue factor PE (CD142, NY2) from BioLegend (365204), and anti-mouse IgG1, κ PE (MOPC-21) BioLegend (981804). FACS™ Lysing Solution was from BD Biosciences. Antibodies for histology; murine monoclonal neo anti-human C9 (DIA011–01, clone E11, isotype IgG2a) from BioPorto Diagnostics A/S (DK-2820 Gentofte, Denmark), neo anti-human iC3b (A209, isotype IgG1) from Quidel (San Diego, CA), monoclonal antibody against human TF (CD142, ADG4509, clone IIID8, isotype IgG1) from Sekisui (American Diagnostica GmbH, Pfungstdt, Germany), a monoclonal anti-human CD14 (18D11, isotype IgG1) synthesized in-house, monoclonal mouse anti-human CD68 (clone KP1, M0814, isotype IgG1) and anti-human CD61 (clone Y2/51, M0753, isotype IgG1) from Dako (Glostrup, Denmark). Isotype controls were purified mouse immunoglobulins IgG1 (clone MOPC-21), IgG2a (clone MOPC-172), IgG2b (clone MPC-11) from BioLegend (San Diego, CA).
Preparation of CC and endotoxin measurement
CC were prepared as described by Samstad et al.(10). Briefly, ultrapure cholesterol (100 mg) was dissolved in 1-propanol (50 mL and aggregated by the addition of distilled water. CC were air dried and suspended in 0.05% (w/v) HSA/PBS. After preparation, the endotoxin contamination was measured in a Chromogenic LAL Assay (Lonza). The Lipopolysaccharide (LPS) was below the detection limit (0.1 EU/mL) in sample size of 50 mg/mL CC, and thus the endotoxin content would be below 0.18 pg/mg CC.
Experiments in human whole blood
Human whole blood from healthy volunteers anticoagulated with lepirudin (50 μg/mL) was used as first described by Mollnes et al. (26). Final concentrations of CC or controls; CC (500, 1000 and 2000 μg/mL), E. coli (1×107 particles/mL), or glass control (200 μL PBS with Ca2+/Mg2+ in BD Vacutainer glass tubes). Final concentrations of inhibitors; CP40 or its peptide control (20 μM), eculizumab and its antibody control (100 μg/mL), anti-TF (10 μg/mL) or control Ig (10 μg/mL), and PMX53 (10 μM). The incubation time was between 60–240 min, as stated for the individual experiments. Complement and coagulation activity was terminated by addition of EDTA (10 mM final concentration). Whole blood was retracted for flow cytometric analysis. Plasma was harvested after centrifugation at 2000 × g for 15 min, and stored in aliquots at −20 ºC for analyses of PTF1.2. After plasma harvesting, the pellets were added 350 μL PBS (equal to plasma harvesting) and further processed as under the paragraph for TF mRNA.
Experiments in platelet free plasma (PFP)
Platelet free plasma (PFP) anticoagulated with lepirudin (50 μg/mL) was made by centrifugation at 2500 × g for 15 min twice at RT. Each time the upper plasma fraction was retained, while discarding the lowest 0.5 mL rich fraction with platelets. The fresh plasma was incubated with or without corn trypsin inhibitor (CTI) at a final concentration of 40 μg/mL in the presence of CC (2000 μg/mL) or in glass vials with an incubation length of 60 and 240 min.
PTF1.2 quantification
PTF1.2 levels were quantified in duplicate using the Enzygnost Prothrombin F1+2 ELISA kit (Monoclonal OPBD03, Siemens Healthcare AS, Marburg, Germany) following the manufacturer’s instructions. Optical density was measured using PolarStar OMEGA plate reader (BMG Labtech, Ortenberg, Germany).
TF mRNA
Cell pellets (550 μL) were added 1.53 mL PaxGene Blood RNA tubes solution (PreAnalytiX (Hombrechtikon, Switzerland) and stored at −80 ºC until RNA extraction. Total RNA was extracted using the MagNA Pure 96 Cellular RNA large volume kit (Roche Diagnostics, Mannheim, Germany) by the manufacturer’s instructions, and the amount analysed using the NanoDrop 2000c spectrophotometer (Thermo Fisher Scientific, Wilmington, DE, USA). cDNA was synthesized using High Capacity cDNA reverse transcription kit and 2720 Thermal cycler (Applied Biosystems, Foster City, CA) and stored at −80 ºC. TF mRNA levels were measured using the StepOne Plus Real-Time PCR systems (Applied Biosystems). Gene expression was detected by TaqMan Fast Universal PCR Master Mix reagents and pre-developed TaqMan® gene expression assays using the target gene TF (TF, Hs 0017225) with reference gene human beta-2-microglobulin (TaqMan B2M Probe Dye Fam, 4333766 – 0804015) analyzed using qPCR with cycle conditions according to the manual.
TF-MP quantification
TF-bearing microparticles (TF-MP) with procoagulant activity were quantified using Aniara ZYMUPHEN MP-TF (521196, Hyphen BioMed, Neuville Sur Oise, France) according to producers protocol. Beforehand, whole blood samples were added sodium citrate 3.2% (from blood collection tubes Vacuette, Greiner bio-one) in 1:10 dilution, and thereafter centrifuged at 1500 × g 15 min RT, before the plasma fractions further were centrifuged at 13000 × g 2 min RT. Platelet free plasma was then harvested by retracting 400 μL from the uppermost plasma fraction. Samples were stored at −80 ºC until analysis.
Flow cytometry
EDTA-inactivated blood samples (50 μL) were added to a mixture of anti-CD14 FITC (2.5 μL), anti-Siglec-8 APC (1.25 μL), anti-HLA-DR APC-Cy7 (1.25 μL), anti-TF PE (IgG1) (1.25 μL) or isotype control (0.625 μL, concentration matched) for anti-TF (anti-mouse IgG1κ PE), red blood cells were lysed by 1 mL of FACS™ Lysing Solution (diluted 1:10 in H2O). Samples were analyzed using BD FACS Canto II flow cytometer, with data processing in FlowJo software (version 10, TreeStar, USA). To separate the monocytes from granulocytes and autofluorescencing eosinophils following CC exposure, a flow cytometric gating strategy based on the following settings was used; monocytes defined by SSC+(medium)/CD14+(high)/Siglec-8−/MHCII+; granulocytes by SSC+(high)/CD14+(low)/Siglec-8−/ MHCII−; eosinophils by SSC+(high)/Siglec-8+/MHCII−. The percentages of TF positive leukocytes were determined in a histogram-plot set by the control antibody. The gating-strategy is given in Fig. 1.
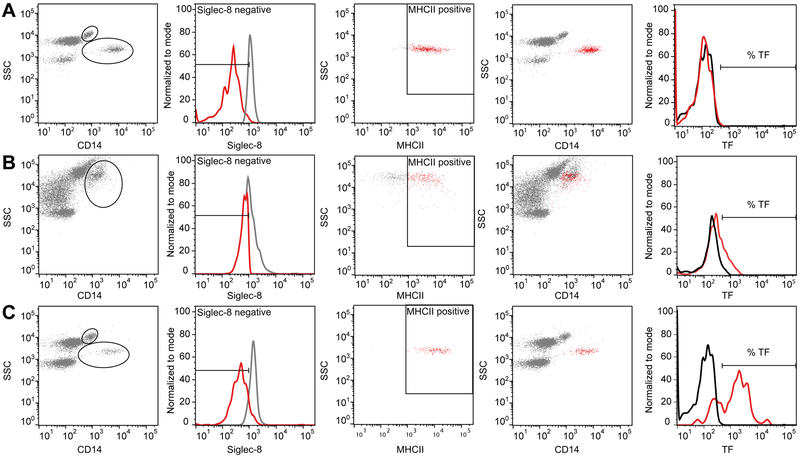
Figure 1. Flow cytometric gating strategy for separating monocytes from granulocytes and eosinophiles.
(A). Non-stimulated blood. Monocytes were easily distinguished as the SSC+(medium)/CD14+(high), Siglec-8− and MHCII+ population (red color in fourth picture) (B). Cholesterol crystals (CC)-stimulated blood. Monocyte and eosinophil populations merged in the CD14+/SSC+ plot, thus a large gate was set to include the most granular monocytes. Thereafter monocytes were selected by a negative selection of Siglec-8− population (based on settings from non-stimulated blood), and a positive selection of the MHCII+ cells (red color second and third picture), resulting in a distinguished monocyte population (red color in fourth picture). (C). E. coli stimulated blood. Monocytes and granulocytes were separated, and the monocytes distinguished further by Siglec-8− and MHCII+ staining. The percentage of TF positive cells were determined by a histogram plot of fluorescence intensity, determining baseline setting from non-stimulated blood and subtracted the isotype control from the positive staining obtained from the specific TF-antibody. The granulocytes and eosinophils were further distinguished by negative and positive selection of Siglec-8 stained cells, respectively (not shown) and further analyzed for TF expression.
Platelet aggregation assay
Platelet aggregation was analyzed on a Multiplate® electrical impedance aggregometry (Roche, Mannheim; Germany). Blood was collected in 4.5 mL plastic blood collection tubes containing the anticoagulant Hirudin (25 μg/mL) (Roche, Mannheim, Germany). After a 30-min rest at 20°C, the samples were diluted with 5% (v/v) PBS without Ca2+ and Mg2+ with 0.05% (w/v) human serum albumin (HSA, Albuminativ Octapharma) or CC (500–2000 μg/mL). The samples were analyzed as recommended by the manufacturer, adding 0.3 mL preheated (37°C) isotonic saline (0.9%) to 0.3 mL whole blood in the Multiplate test cell, followed by incubation for 3 min at 37°C. The aggregation response over 6 min was expressed by the area under the curve as arbitrary units (AU × min), either by the CC or its background control alone, or following additional stimulation with 20 μL of ADP or thrombin receptor activating peptide-6 (TRAP) test as described by the producer (Roche, Mannheim, Germany).
Human thrombus and plaque material
Intracranial thrombus material was obtained by arterial recanalization or thrombectomy (27) from a single center cohort study (28). Carotid plaques were obtained by carotid endarterectomy. Study inclusion criteria were acute stroke with clinical ischemic symptoms corresponding to an angiographically proven large intracranial vessel occlusion, absence of intracranial hemorrhage on computed tomography scan, and a clearly defined time of symptom onset within six hours of inclusion. Mechanical thrombectomy involved arterial catheterization from the groin artery to the level of the intracranial vessel occlusion and thrombus retraction with the use of a retrievable stent delivered through a microcatheter. After retraction the thrombi were stored at 4°C in Allprotect tissue reagent (Qiagen) or snap-frozen.
Histology
Histology processing was performed at the Cellular & Molecular Imaging Core Facility (CMIC) Histology lab at NTNU. We chose frozen tissue material without preservations, due to the possibility of preserving neoepitopes of activated complement and preserving the CC structures. Briefly, frozen thrombi tissue sections (4 μm) were stained for HES (Hematoxylin Erythrosine Saffron) or with specific antibodies. HES procedure in brief; rehydration through descending grades of ethanol to water (1 min), staining in aqueous Hematoxylin (5 min) followed by bluing in water (8 min), erythrosine treatment (5 min) and rinsing in water (1 min), dehydrating in ethanol (80%, 96%, 100%) and staining in Saffron (5 min) before rinsing in absolute ethanol and clearing in Tissue Clear. Cover slipping utilized Sakura Tissue-Tek© Glas™. Specific antibody staining in brief; frozen sections on SuperFrost Plus slides, dried (10 min) and washed (soaking in Dako S3006 buffer), quenched for endogenous peroxidase activity in Peroxydase block (Dako K4011), and treated with Protein Block Serum-Free (Dako X0909) for 20 min. The primary antibodies were diluted in Vendor code over night at 4 °C by following dilutions; anti-C9 (IgG2a 1 mg/mL) neoepitope in 1:10000 (plaque) and 1:5000 (thrombi) dilution, anti-iC3b neoepitope (IgG2b 1.04 mg/mL) in 1:1500 dilution, anti-TF (IgG1 0.5 mg/mL) in 1:1000 dilution, anti-CD14 (IgG1 165 μg/mL) in 1:200 dilution, anti-CD68 (IgG1 156 mg/L) in 1:5000 dilution, anti-CD61 (IgG1 647 mg/L) in 1:5000 dilution. Negative controls were isotype- and concentration matched. Lastly, washing buffer was added followed by 30 min in Labelled polymer HRP anti-mouse (Dako K4011), rinsing and incubation in DAB (Dako K4011). Counterstaining was by a non-alcoholic aqueous Hematoxylin (2 min) and mounting medium. Images were taken by an inverted fluorescence microscope Olympus IX71, using a polarization filter, and an Olympus XC30 CCD color camera and 4x-40x objectives and processed by with Cell^P Image visualization software and optimized in Adobe illustrator V 10.0.1 using linear stretch adjustments.
Statistical analysis
GraphPad Prism software (version 7.0a) was used for statistical analyses. Two-way ANOVA with multiple comparisons were used to evaluate the effects between stimuli, controls and inhibitors. Dunnett’s multiple comparisons test was used for the time course studies, Tukey’s multiple comparisons test when comparing each condition of CC with its inhibitor and inhibitor control, and Sidak’s multiple comparisons test was for additional data comparing each CC condition with inhibitor. The data generated by continuous scales were log-transformed on beforehand to ensure normal distribution. A Wilcoxon matched pairs-signed rank test was used for comparisons between two conditions.
Ethical approval
The use of human whole blood was approved and followed the guidelines as recommended by the Regional Committees for Medical and Health Research Ethics (REC) under REC Central [REK2009/2245], and in accordance with the Helsinki declaration. The use of thrombi and plaque material was approved by the South East Norway Regional Ethics Committee, REC South East [REK 2014/2078] and written informed consent were obtained from all patients.
Results
CC induce PTF1.2 in human lepirudin whole blood
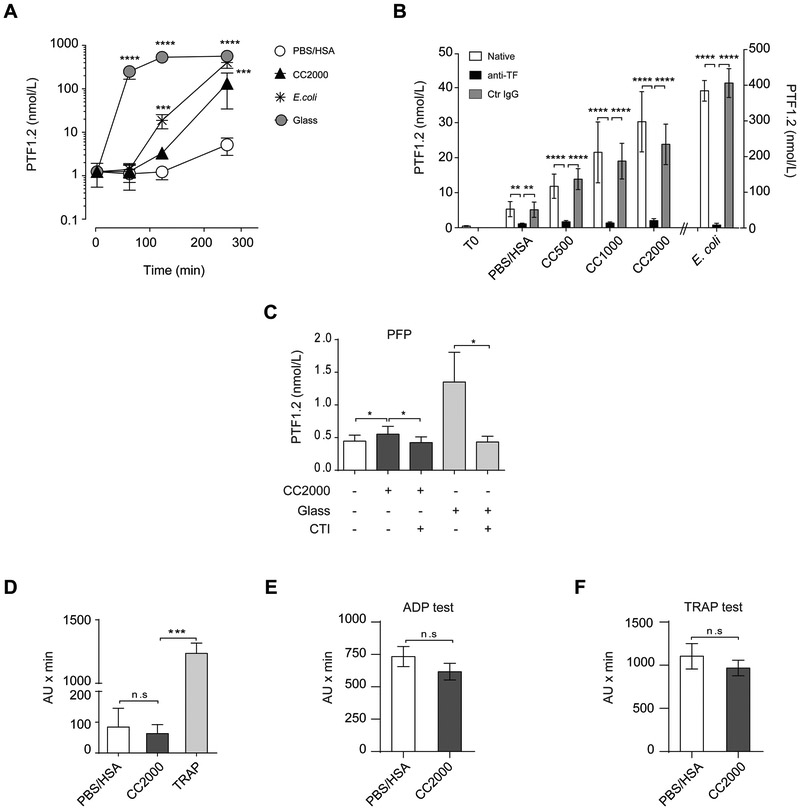
Lepirudin specifically inhibits thrombin and thus avoids fibrinogen activation and downstream coagulation, while still allowing the coagulation system to be activated upstream. Despite the inhibition of the thrombin feed-back loop, the up-stream coagulation proteins together with all complement proteins are able to be activated, thereby allowing interaction with leukocytes. The conversion of prothrombin to thrombin results in a cleavage product, PTF1.2, which serves as an indirect estimate on the initial coagulation activation by either of the two coagulation pathways. CC 2000 μg/mL induced a significant increase (P<0.001) of PTF1.2 compared to the PBS/HSA control following 240 min incubation (Fig. 2A). Significant elevation was achieved for CC 1000 μg/mL (P<0.05), whereas a non-significant (P>0.05) elevation was obtained under exposure to CC 500 μg/mL (data not shown). Glass significantly elevated PTF1.2 levels by 60 min (P<0.0001) and E. coli by 120 min (P<0.001) (Fig. 2A). Glass is a highly potent activator of coagulation FXII, and can be inhibited by corn trypsin inhibitor (CTI) (29), while E. coli activates TF that can be explored by TF inhibiting antibodies (14). Inhibiting TF prior to addition of CC using a TF blocking antibody efficiently and significantly (P<0.0001) blocked the CC and E. coli induced PTF1.2 (Fig. 2B). These data pointed to the TF-driven pathway to be most important for the CC-induced PTF1.2. To test for the FXII dependency, CC or glass were incubated in lepirudin PFP with or without blockage of FXII using CTI. In PFP the overall PTF1.2 induction by CC or glass was low (just above baseline), but could still be significantly (P<0.05) inhibited by CTI (Fig. 2C). The ability of CC to induce platelet aggregation was investigated by electrical impedance aggregometry (Fig. 2D-F). CC did not induce platelets aggregation as compared to its background control (HAS/PBS) and positive control TRAP (Fig. 2D). The CC did not induce additional activation or inhibition in activated platelets as investigated by the ADP test (Fig. 2E) or the TRAP test (Fig. 2F). Altogether, these data point to the TF pathway as the main pathway triggered by CC, with a small contribution from FXII.
Figure 2. Cholesterol crystals (CC) induce prothrombin fragment factor 1+2 (PTF1.2) dependent on the tissue factor pathway.
(A) PTF1.2 induction over time (60, 120 and 240 min) upon exposure to CC 2000 μg/mL, PBS/HSA, E. coli (1 × 107 particles/mL) or glass (N=7 donors) in human whole blood. (B) Effect of TF inhibition following exposure of CC (500, 1000 and 2000 μg/mL) or E.coli after addition of the functional grade inhibitory antibody against TF (anti-TF) or the corresponding ultra-leaf purified IgG1κ control antibody (Ctr IgG) for 240 min in human whole blood (N=6 donors). (C) Effect of factor XII inhibition by CTI (40 μg/mL) in platelets reduced plasma (PFP) following incubation with CC (2000 μg/mL) or glass for 60 min (N=5). Effect of CC on platelet aggregation in human whole blood measured by electrical impedance aggregometry in (D) by CC (2000 μg/mL) or its controls HSA/PBS or thrombin receptor activating peptide-6 (TRAP) (N=6), (E) by additional stimulation with ADP (N=3) and in (F) with TRAP following 6 min incubation (N=3) given as arbitrary units × min. Under all experiments thrombin was inhibited with lepirudin. All data are given as means ± SEM. The statistical differences are given by the following significance levels *P<0.05, **P<0.01, ***P<0.001, ****P<0.0001.
CC induce coagulation through monocytic TF
The pro-coagulant activity of TF detected in the inhibition studies (Fig. 2B) could be a consequence of cellular expressed TF or TF microparticles (TF-MP). Measuring TF at the transcriptional level (TF mRNA) after CC 2000 μg/mL exposure in the whole blood resulted in a highly significant (P<0.0001) increase as compared to the PBS/HSA control peaking after 60 min incubation (Fig. 3A). Similar patterns although less prominent were found following exposure of CC 1000 μg/mL and CC 500 μg/mL (Suppl. Table 1). In comparison, E. coli induced a significant (P<0.0001) and stronger response, but also peaking after 60 min (Fig. 3A). Measuring the TF-MP activity in human whole blood (Fig. 3B) resulted in the lack of activity following CC exposure, while the E. coli induction was in consistence with previous data (14).
Figure 3. Cholesterol crystals (CC) induce tissue factor (TF) mRNA and TF expression on the monocyte surface.
Human whole blood was incubated with cholesterol crystals CC (500, 1000 and 2000 μg/mL) or controls; PBS/HSA or E. coli (1 × 107 particles/mL) at different time points (60, 120 and 240 min). (A) TF mRNA in whole blood measured by RT qPCR (N=6 donors), additionally CC 1000 and 500 μg/mL are in Suppl. Table 2. (B) The pro-coagulant activity of tissue factor-microparticles (TF-MP) (N=3 donors). (C) Monocytes TF expression exemplified with flow cytometry histogram after 120 min, and quantified as percentage of monocytes expressing surface TF at all time points (N=6 donors). Additionally CC 1000 and 500 μg/mL are shown in Suppl. Table 2. (D) The lack of granulocytes TF expression exemplified with flow cytometry histogram after 120 min, and quantified as percentage of granulocytes expressing surface TF at all time points (N=6 donors). Histograms baseline (T0) are stippled lines, isotype controls as filled grey and the TF expression as black line. Graphs are given as means ± SEM. Significant difference between the stimuli and inhibitors at the given time-points **P<0.01, ***P<0.001, ****P<0.0001.
We further investigated the TF expression on the surface of the monocyte and granulocyte populations using flow cytometry. The monocytic population (CD14positive/Siglec-8negative/MHCIIpositive) histogram showed a clear shift to the right for TF following CC exposure (Fig. 3C), and stronger for E. coli. Quantification from six donors indicated an average of 23% of the monocytic population expressing TF at the surface upon CC 2000 μg/mL exposure, and between 18–20% at the lower concentrations (Suppl. Table 2). Of note, a significant increase was detected already after 60 min for CC 2000 μg/mL (P<0.001) and CC 1000 (P<0.05), and after 120 and 240 min for all concentrations of CC (Suppl. Table 2). E. coli induced the fastest and strongest TF expression involving between 70–80% of the monocyte population in agreement with previous findings. In contrast, no shift in TF was found on the surface of the granulocytes (SSChigh/CD14negative/Siglec-8negative) for either CC or E. coli stimulation (Fig. 3D) (14). Equally, no TF induction could be detected on the eosinophilic population (SSChigh/MHCIInegative/Siglec-8positive) (not shown). In conclusion, CC induces synthesis of TF mRNA, where only monocytes express TF at the surface.
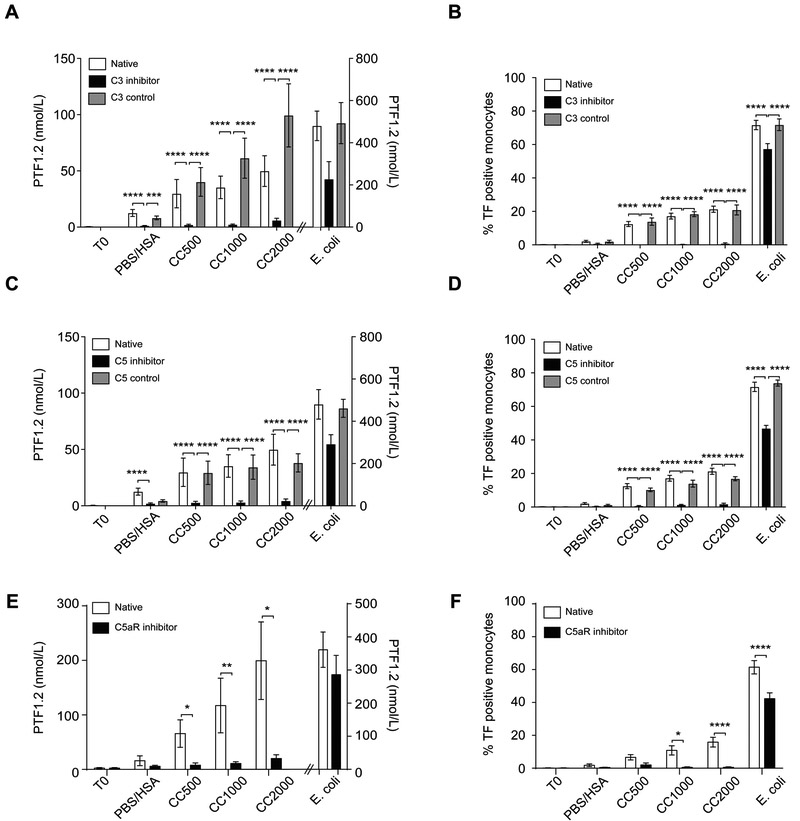
CC induce coagulation through an initial complement activation
CC are strong activators of complement leading to TCC formation (10). Complement-induced TF has previously been demonstrated (13-15), suggesting a possibility also for CC-induced coagulation. Inhibiting complement by blocking C3 (CP40) or C5 (eculizumab) significantly (P<0.0001) reduced the CC-induced PTF1.2 and monocyte TF expression close to baseline (Fig 4A-D). Of note, the percentage of monocytes expressing TF was less than 1% upon inhibition of C3 and less than 2% upon inhibition of C5. Upon E. coli exposure, the inhibition was less efficient in accordance with previous data demonstrating the need of dual blockage of CD14 and complement C5 to avoid E. coli-induced coagulation (14). Since the inhibition of CC was efficient also at the level of C5, we further investigated the involvement of the anaphylatoxin C5a receptor, C5aR1, using the inhibitor PMX53. The effective blocking of the CC-induced PTF1.2 and monocyte TF by PMX53 points to an important role of the C5a-C5aR1 axis in the CC-induced coagulation (Fig. 4E-F). In comparison, blocking of E. coli-induced PTF1.2 and monocytic TF by PMX53 was less effective (Fig. 4E-F). In conclusion, the CC-induced coagulation activation measured by PTF1.2 and monocytic TF is dependent on initial complement activation, where the anaphylatoxin receptor C5aR1 is central.
Figure 4. Cholesterol crystal (CC) induce coagulation activation dependent on an initial complement activation.
Whole blood was incubated with CC (500, 1000, 2000 μg/mL), PBS/HSA or E. coli (1 × 107 particles/mL) for 240 min with the C3 inhibitor (CP40), C5 inhibitor (eculizumab) or their respective controls (scrambled peptide for CP40 or rituximab as control for eculizumab). (A) PTF1.2 production following C3 inhibition (CP40) (N=7 donors). (B) Monocyte TF expression at 120 min incubation following C3 inhibition (N=6 donors). (C) PTF1.2 production following complement C5 inhibition (eculizumab) (N=7 donors). (D) Monocyte TF expression at 120 min incubation following C5 inhibition (N=6 donors). (E) PTF1.2 following inhibition of complement receptor C5aR1 with PMX53 after 240 min (N=5 donors). (F) Monocyte TF expression after 120 min incubation following inhibition of C5aR1 with PMX53 (N=5 donors). Data are given as means ± SEM. Significance levels are given as * P<0.05, *** P<0.001, **** P<0.0001.
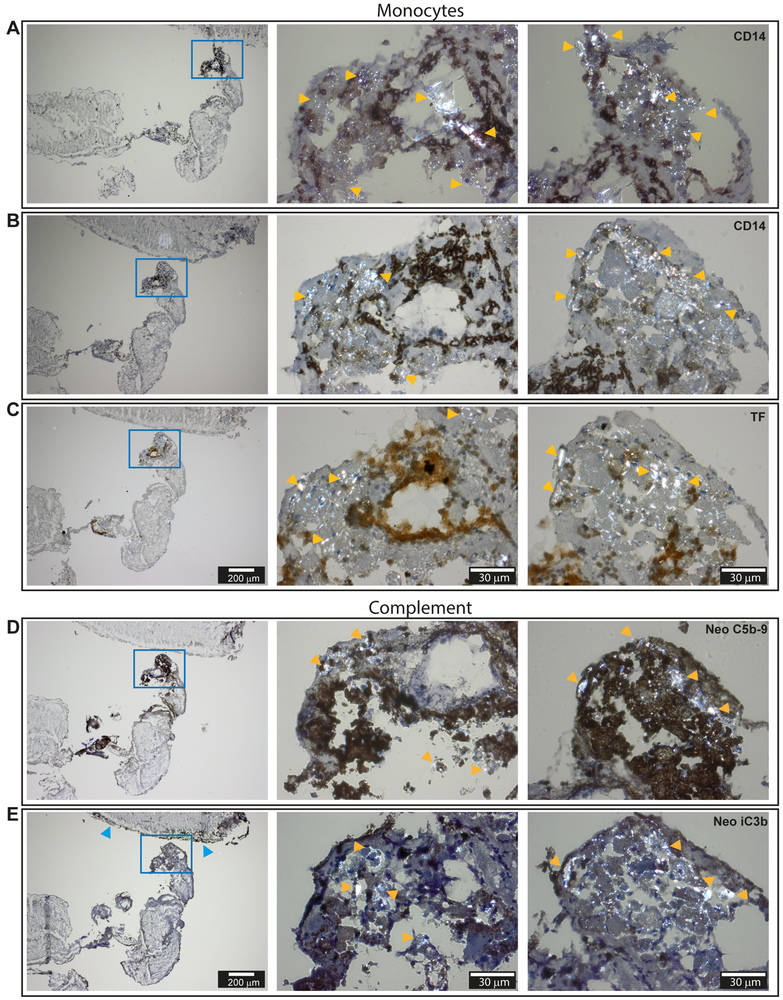
CC are found within human intracranial vessel thrombus material and are associated with activated complement, monocytes and TF positive leukocytes
Our studies in whole blood pointed to complement and monocytes to be essential participators in CC-induced coagulation. To further explore the physiological relevance of these findings, we next explored thrombi material retracted from the intracranial vessel of patients with advanced carotid atherosclerosis. First, we investigated the possibility of detecting CC structures within the thrombi material, and next in the association with complement and monocytes. Since CC are one of few materials showing birefringence in human tissue (30), it was possible to detect CC structures by polarization filter reflected light microscopy. Birefringent structures similar to CC were detected within hematoxylin stained samples (Fig. 5A and B). In the corresponding HES sections, the birefringent structures were absent (Fig. 5C and D). Crystalized cholesterol dissolves in ethanol (31), which is one of the constituents of HES. The disappearance of birefringent structures upon HES staining suggested that the structures could be of cholesterol origin.
Figure 5. Histology from frozen sections of human intracranial thrombus retracted from a patient with advanced carotid atherosclerosis explored by polarization filter reflected light microscopy.
(A-B) Hematoxylin stained sections with easily identifiable birefringent cholesterol crystals (CC) marked with orange arrows. (C-D) HES stained sections of corresponding areas. Corresponding areas are A/D and B/C. The thicknesses of the sections are 4 μm. Images were taken with 40x objective by a polarization filter to visualize birefringent structures. Scale bars are 30 μm.
Of note, the CC areas were richly populated with cells having bean-shaped nuclei typical for monocytes (Fig. 5A-D). Immunohistochemistry staining confirmed the presence of monocytes within the CC rich areas as marked by yellow arrows (Fig. 6A-B). The corresponding adjacent section stained prominently for TF (Fig.6C, middle picture). Furthermore, complement neoepitopes C5b-9 (Fig. 5D) were densely present and strongly associated with the birefringent CC-like structures (yellow arrows). The neoepitope iC3b was also found within the CC rich areas (Fig. 5E), in addition to being present in the outermost regions of the thrombus (Fig. 5E, left picture, blue arrows). The presence of monocytes/macrophages in the thrombus was further confirmed by positive staining for CD68 in areas rich in CC (Suppl. S1A). Platelets (CD61) on the other hand were present throughout the thrombus (Suppl. S1B). The antibody specificities were manifested both by the areas free of staining and further confirmed by the lack of staining by their respective isotype control IgG1 (Suppl. S1C), IgG2a and IgG2b (not shown). In conclusion, the histological examinations pointed to a physiological relevance of CC and complement in thrombosis through the activation of monocytic TF.
Figure 6. Immunohistochemistry of frozen sections of human intracranial thrombus retracted from a patient with advanced carotid atherosclerosis explored with polarization filter reflected light microscopy.
(A and B) Staining against the monocyte marker CD14. (C) Staining against TF. (D) Staining against the complement neo epitope C5b-9. (E) Staining against the complement neoepitope iC3b. The thicknesses of the sections are 4 μm. Pictures in the left column are taken by 4x objective and the cholesterol crystal (CC) rich area (blue frame) is further augmented with a 40x objective (middle and right columns). Examples of birefringent structures are shown by yellow arrows, whereas blue arrows points to the outer thrombi sections stained heavily for neoepitopes iC3b. Scale bars are 200 μm for pictures in left column and 30 μm for pictures in middle and in right column.
Monocyte TF/CD14 expression patterns are connected to CC and activated complement in a vulnerable plaque and in whole blood.
Vulnerable plaques were examined for ruptures, the presence of CC, complement and monocytes. One sample showed signs of an open lumen and had large CC present near the adventitia (Fig. 7A and Suppl. S2). Briefly, within the open lumen bright staining with the monocyte marker CD14 (CD14bright) suggested monocyte influx and blood exposure (Fig. 7A, yellow arrows). In the innermost region of the lumen a layer of CD14low staining monocytes was detected (Fig. 7A, first picture, blue arrows). The corresponding layer stained positive for TF (second picture, blue arrows). Of note, bright CC-like structures were observed in the adjacent region (marked CC). The CC rich areas stained heavily for complement iC3b and C5b-9 (Fig. 7A, third and fourth picture). The monocytic origin of the TF+ cells was further confirmed by positive staining for the monocyte/macrophage marker CD68 and negative staining for CD34 and CD61 in corresponding areas (Suppl. S2A). Larger magnifications confirmed the monocytes origin by its presence of bean shaped nuclei (Suppl. S2B) both for the CD14bright and the CD14low/TF+ areas (Suppl. S2C-D). The precence of CC in the adjacent area to the CD14low/TF+ cells are clearly shown (Suppl. S2C-E). Endothelial staining was only found in the are of CD14bright monocytes, with irregular staining patterns typical for endothelial renewing (Suppl. S2E). The antibody specificities were confirmed by negative controls (not shown).
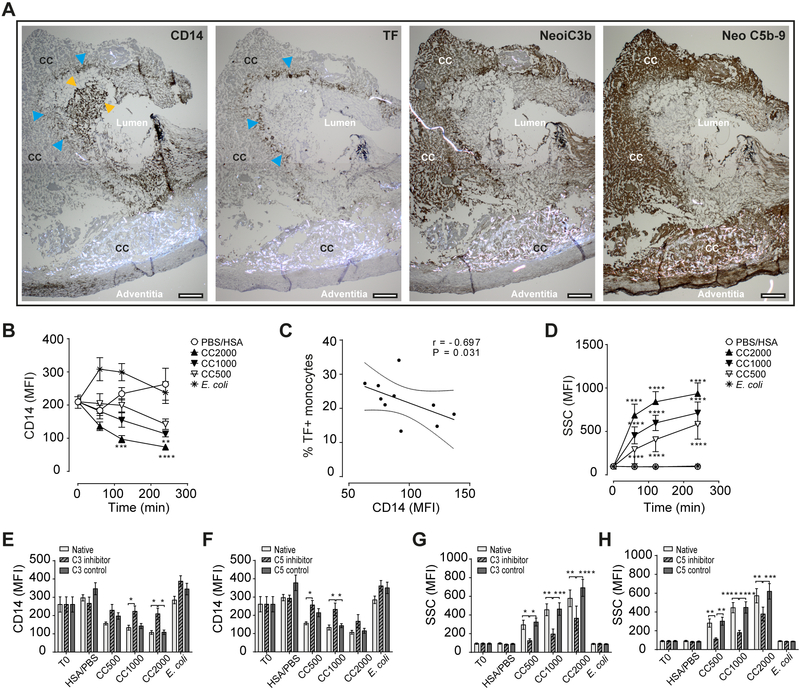
Figure 7. Human vulnerable plaque and whole blood show corresponding patterns in monocytes TF/CD14 expression and complement activation to CC.
(A) Immunohistochemistry of the vulnerable plaque with the monocyte marker CD14, tissue factor (TF), and activated complement neo iC3b and neo C5b-9. Staining areas for CD14bright monocytes are marked with yellow arrows, and CD14low/TF+ expressing monocytes by blue arrows, specified are also the CC rich areas, lumen and adventitia. Sections are 4 μm and are taken by 4x objective. Scale bars are 200 μm. Whole blood following cholesterol crystals (CC) exposure showing effects on (B) monocytes CD14 expression, (C) correlation between CD14 and TF in monocytes, (D) the increase in monocytes granularity, (E) monocyte CD14 following inhibition of complement C3 (120 min), (F) monocyte CD14 following inhibition of complement C5 inhibition (120 min), (G) monocytes granularity following inhibition of C3 (120 min) and (G) monocytes granularity following inhibition of C5 (120 min). Data are given as mean fluorescence intensity (MFI), mean± SEM, N=6 donors. Significance levels are * P<0.05, ** P < 0.01, *** P<0.001, **** P<0.0001.
The findings of CD14low/TF+ expressing leukocytes within the plaque could be explained by further obeservations in whole blood upon CC exposure (Fig. 7B-H). Briefly explained, in the monocytes a reduction of CD14 from the initial expression level by time was observed, with a significant lowering for CC2000 (μg/mL) after 120 and 240 min (P<0.001–0.0001), and for CC 1000 (μg/mL) after 240 min (P<0.01) (Fig. 7B). Moreover, a negative correlation (r= −0.697) between CD14 expression and the TF positive monocytes (percentage) was identified (Fig. 7C). The CC exposure led to a substantial and significant (P<0.0001) increase in the granularity indicating phagocytosis (10) (Fig. 7D). The reduction in CD14 (Fig. 7E-F) and increase in granularity (Fig. 7G-H) could be inhibited by blocking complement at the level of C3 and C5, thus linking both events to complement. From these findings, we would suggest that CC in a vulnerable plaque situation activates complement with a subsequent influx of monocytes, phagocytosis of CC and induction of TF in monocytes. During this process, CD14 is internalized, in part through complement mediated activity.
Discussion
CC have emerged as important contributors to atherosclerotic inflammation (11), but their potential role in thrombosis is unexplored. Here we show that CC induce coagulation through a complement-dependent expression of TF in monocytes, by using an experimental whole blood model. The physiological relevance of these findings is supported by human intracranial vessel thrombus and vulnerable plaque histology, demonstrating CC in association with monocyte TF (CD14/TF positive leukocytes) and activated complement (iC3b and C5b-9). The present data thus point to an active role of CC and complement in thrombosis.
Atherosclerotic plaques can contain dense amounts of CC (32), suggesting relatively high concentrations of CC at the releasing site. Herein we show that CC in concentrations of 500–2000 μg/ml induces coagulation by cleavage product PTF1.2 mediated mainly through the TF pathway and TF surface expression by monocytes. Our data indicate a time-span of CC induced TF expression of one to two hours, with TF mRNA peaking after one hour and a full surface expression after two hours. Although endothelial damage could induce a faster response in concert with platelets, these findings point to releasable CC as active contributors in thrombus formation and growth. The demonstration of monocyte influx and TF expressing monocytes in a vulnerable human plaque further support monocytes as important effectors in thrombosis. The time-frame from plaque debris release to clinical symptoms is not well defined, and depends on thrombus size and localization. According to clinical guidelines (33), patients with advanced carotid atherosclerosis should undergo carotid endarterectomy preferably within 48 hours after a transient ischemic attack (TIA) due to the high risk of recurrent infarction. The clinical picture with small ischemic occlusions such as TIA promote a high-risk period for up to two months where patients are particularly vulnerable for new and often larger attacks. The release of CC during this period could thus promote thrombosis by inducing TF expression on monocytes.
Cholesterol embolization syndrome is a phenomenon characterized by a multitude of small emboli occurring over time in association with CC, with an incidence of 22–27% during surgical treatment of atherosclerosis (34). Of note, this phenomenon was connected to complement consumption, which fits well with the complement dependent CC induced coagulation activation demonstrated herein. Our data might contribute to a mechanistic explanation, by demonstrating that the coagulation activation is mediated predominantly by complement, with more than 90% inhibition at either the level of C3 or C5. The efficient prevention of coagulation by inhibiting the anaphylatoxin receptor C5aR1 points to an essential role of the C5a-C5aR1 signalling axis in CC induced coagulation. This clear effect was in contrast to the partial inhibition of coagulation by C5aR1 under exposure to E. coli, and clearly point to a specific complement-mediated activation by CC. Bacteria induced coagulation is in addition to complement also dependent on CD14 (26), and further connected to the toll-like receptor (TLR) pathway (35). The lack of direct activation of CD14/TLRs by CC might explain the lower potency of CC to induce TF mRNA, the lower number of TF positive monocytes and the lack of TF-MP activity presently demonstrated. We observed however a rapid loss of CD14 in correlation with TF induction following CC exposure. This phenomenon was concentration dependent and linked to complement, and could possibly be the consequence of phagocytosis of CC. Whether CD14 is involved in the signal induction leading to TF expression remains to be elucidated. Previous exploration by our group has shown that the CC induced complement activation mediates upregulation of CR3 (CD11b/CD18) through C5a/C5aR1 (10). The additional opsonization with complement fragments at the level of C3 leads to efficient phagocytosis of CC. This was also demonstrated in the current study by the concentration-dependent granulation in monocytes after CC exposure that could be blocked by the complement inhibitors both at the level of C3 and C5. Although we did not explore the link between monocytes TF and the phagocytic events, the rapid phagocytosis prior to TF mRNA synthesis, as well as the complement dependency for both, could indicate that these events are connected.
The inflammatory cytokines TNF and IL-1β among others are triggered by CC exposure (10). The induction of TF has also been connected to TNF (36), which could suggest its involvement in CC mediated coagulation. However, the time-span between CC exposure and TF mRNA induction of one hour points to a shorter induction time than is needed for activation of TNF. It is thus more likely that these processes are initiated in parallel in connection to complement, than that TNF plays a central role in the initial TF induction by CC. The NLRP3 inflammasome has been linked to CC induced IL-1β secretion mediated by C5a (10). Further on, NLRP3 has been linked to induction of TF-bearing microparticles. However, our investigation in whole blood using the specific NLRP3 inhibitor MCC950, caspase-1 inhibitor VX-765 and pan-caspase inhibitor Z-VAD-FMK did not provide evidences for its involvement in CC induced TF expression or downstream coagulation activation (data not shown). Additionally, no induction of TF bearing microparticles by CC were observed in our system. As regulation of TF has been shown to occur mainly on the transcriptional level (37), our findings imply that CC induced generation of C5a activates the C5a-C5aR1 axis to drive synthesis of TF mRNA, which has been shown to occur both in monocytes (38) and endothelial cells (39).
From the present and previous data, CC can be regarded as participators in thromboinflammation with a strong dependency on complement. Our investigation points to the monocytes as the only leukocytes able to induce TF upon exposure to CC, as surface expression on granulocytes and eosinophils was absent. CR3 expression is in contrast induced both on the monocytes and granulocytes (10), and our explorations also revealed increased granulocyte granularity upon CC exposure (data not shown). This further points to the ability of CC to activate the granulocytes, but not induce surface expression of TF. While there is an agreement regarding the capability of monocytes to express TF, the expression of TF on other cell types is debated (40-42). These discrepancies in cellular sources could be related to health status of the donors as well as the type of stimuli (36, 42, 43). Platelets contribute in the initial clot-formation process by binding to damaged vascular endothelium (44) and connections between platelets and monocyte TF are commonly accepted (45). We found no direct effect of CC on platelet aggregation, nor in the induction of PTF1.2 following CC exposure in platelet containing plasma (data not shown). The tiny induction of PTF1.2 following CC exposure in platelets-free plasma which was still significantly inhibited by CTI, opens for a small contribution of FXII in CC induced coagulation. This could also explain the approximately 10% of PTF1.2 activity remaining following complement inhibition. A limitation of the lepirudin anticoagulant is the inhibition of thrombin, the major platelet activator (46). However, since the platelets also contain complement receptors (47), a complement-dependent coagulation activation by the platelets could be possible. The presence of iC3b in the outermost parts of the thrombus also opens for a role for complement-platelet interactions in thrombus growth, as previously described (22, 48).
CC are normally observed as imprints (CC clefts) in plaques due to their dissolution when specimens are treated with ethanol during regular immunohistochemical staining (49). CC accumulation over time gives rise to cleft structures within atherosclerotic plaques that are easily observed under the microscope. However, upon plaque rupture CC will be subjected to blood flow, and therefore more challenging to detect during thrombus formation. CC can be observed using polarized filter reflected light microscopy due to their high birefringence (30). The detection of complement products is also more efficient in frozen samples as used herein. A recent paper suggests that freezing of biopsies from atherosclerotic plaques may produce birefringent structures in frozen section samples that do not represent CC (50). An exclusion of such artifacts from the present images is not possible, but still several findings support the birefringent structures being of CC origin: (1) the birefringent structures were associated with activated complement, monocytes and TF; (2) monocytes or TF positive cells were adjacent to CC-structures; (3) the shape of the birefringent structures resembled the in vitro made square CC for the smaller structures, while the larger needle shaped or larger assemblies were similar to those seen in atherosclerotic plaques; and (4) upon HES staining of step-wise ethanol treatment, the birefringent structures disappeared, thereby supporting that the structures contained cholesterol. Altogether, these findings point to a CC nature of the birefringent structures.
Based on the efficiency of complement inhibition in reducing CC induced coagulation, targeting complement warrants further exploration as a future treatment option for prevention of thrombosis. Currently, the complement C3 inhibitor CP40 is under clinical development (51) whereas the C5 inhibitor eculizumab is in clinical use for treatment of paroxysomal nocturnal hemoglobinuria (PNH) (52). These patients often suffer from thromboembolism, and targeted treatment of C5 has proven to reduce the thrombotic events by 81% (52). In a pre-clinical porcine model of myocardial infarction, C5 treatment also reduced the infarction size (53). Targeting interleukin-1β (IL-1β) has recently been proven to reduce the incidence of thrombosis in patients with underlying atherosclerosis (54). Of note, complement activation is an up-stream event to the inflammatory cytokines including IL-1β (10) and thus targeting complement could represent an alternative strategy. This might also avoid a compromised immune activation upon infections, as is the concern with anti-IL-1β therapy (54).
In conclusion, the current study reveals a role for CC in thromboinflammation. CC possess a pro-coagulant feature dependent on complement and monocytic TF, and following plaque rupture releasable CC might contribute to thrombosis. The use of complement inhibitors targeting either C3, C5, or C5aR1 could be an alternative clinical strategy for prophylactic treatment of atherosclerotic plaques or after thrombosis, and warrants further exploration.
Supplementary Material
Key-points:
Cholesterol crystals induce coagulation through monocyte tissue factor (TF)
Monocyte TF induction is blocked by complement inhibitors to C3, C5 or C5aR1
Monocyte TF induction is dependent on complement C5aR1
Acknowledgments
We acknowledge the Cellular & Molecular Imaging Core Facility (CMIC) at NTNU, Ingunn Nervik for the immunohistochemistry and Bjørnar Sporsheim for image optimization. Liv Ryan and Hilde Fure is acknowledged for technical help/ and valuable discussions in the initial experimental phase. Technical assistance on the electrical impedance aggregometry by Judith Krey Ludviksen is also greatly acknowledged as well as the production of CC by Nathalie Niyonzima. We are grateful to the department head of pathology Harald Aarset for evaluating our prepared samples from vulnerable plaque histology.
Grant support
The studies were funded by The Liaison Committee for Education, Research and Innovation in Central Norway (RHA, Samarbeidsorganet) under grant 46056819 and the Joint Research Committee between St. Olavs Hospital and the Faculty of Medicine and Health Science, NTNU, under grant 46082800; The Research Council of Norway through its Centers of Excellence funding scheme, project number 223255, and by the European Community\s Seventh Framework Program under grant agreement n° 602699 (DIREKT); by National Institutes of Health Grants AI068730 and AI030040, and by The Odd Fellow Foundation [OFF-2014]; The Simon Fougner Hartmann Family Fund [SFHF-12/14].
Footnotes
Disclosures
J.D.L. is the inventor of patents and/or patent applications that describe the use of complement inhibitors for therapeutic purposes, the founder of Amyndas Pharmaceuticals, which is developing complement inhibitors (i.e. 3rd generation compstatins) for clinical applications, and the inventor of the compstatin technology licensed to Apellis Pharmaceuticals (i.e., 4(1MeW)7W/POT-4/APL-1 and PEGylated derivatives). The authors declare no competing financial interest beyond this.
References
- 1.World Health Organization. 2016. Cardiovascular diseases (CVDs). [Google Scholar]
- 2.Breitenstein A, Camici GG, and Tanner FC. 2009. Tissue factor: beyond coagulation in the cardiovascular system. Clin Sci (Lond) 118: 159–172. [DOI] [PubMed] [Google Scholar]
- 3.Nishi K, Itabe H, Uno M, Kitazato KT, Horiguchi H, Shinno K, and Nagahiro S. 2002. Oxidized LDL in carotid plaques and plasma associates with plaque instability. Arterioscler Thromb Vasc Biol 22: 1649–1654. [DOI] [PubMed] [Google Scholar]
- 4.Yasojima K, Schwab C, McGeer EG, and McGeer PL. 2001. Generation of C-reactive protein and complement components in atherosclerotic plaques. Am J Pathol 158: 1039–1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Owens AP 3rd, Byrnes JR, and Mackman N. 2014. Hyperlipidemia, tissue factor, coagulation, and simvastatin. Trends Cardiovasc Med 24: 95–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cai H, Song C, Lim IG, Krilis SA, Geczy CL, and McNeil HP. 2005. Importance of C-reactive protein in regulating monocyte tissue factor expression in patients with inflammatory rheumatic diseases. J Rheumatol 32: 1224–1231. [PubMed] [Google Scholar]
- 7.Grebe A, and Latz E. 2013. Cholesterol crystals and inflammation. Curr Rheumatol Rep 15: 313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Abela GS, Aziz K, Vedre A, Pathak DR, Talbott JD, and Dejong J. 2009. Effect of cholesterol crystals on plaques and intima in arteries of patients with acute coronary and cerebrovascular syndromes. Am J Cardiol 103: 959–968. [DOI] [PubMed] [Google Scholar]
- 9.Vogt W, von Zabern I, Damerau B, Hesse D, Luhmann B, and Nolte R. 1985. Mechanisms of complement activation by crystalline cholesterol. Mol Immunol 22: 101–106. [DOI] [PubMed] [Google Scholar]
- 10.Samstad EO, Niyonzima N, Nymo S, Aune MH, Ryan L, Bakke SS, Lappegard KT, Brekke OL, Lambris JD, Damas JK, Latz E, Mollnes TE, and Espevik T. 2014. Cholesterol crystals induce complement-dependent inflammasome activation and cytokine release. J Immunol 192: 2837–2845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Niyonzima N, Halvorsen B, Sporsheim B, Garred P, Aukrust P, Mollnes TE, and Espevik T. 2017. Complement activation by cholesterol crystals triggers a subsequent cytokine response. Mol Immunol 84: 43–50. [DOI] [PubMed] [Google Scholar]
- 12.Markiewski MM, Nilsson B, Ekdahl KN, Mollnes TE, and Lambris JD. 2007. Complement and coagulation: strangers or partners in crime? Trends Immunol 28: 184–192. [DOI] [PubMed] [Google Scholar]
- 13.Gravastrand C, Hamad S, Fure H, Steinkjer B, Ryan L, Oberholzer J, Lambris JD, Lacik I, Mollnes TE, Espevik T, Brekke OL, and Rokstad AM. 2017. Alginate microbeads are coagulation compatible, while alginate microcapsules activate coagulation secondary to complement or directly through FXII. Acta Biomater 58: 158–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Landsem A, Fure H, Christiansen D, Nielsen EW, Osterud B, Mollnes TE, and Brekke OL. 2015. The key roles of complement and tissue factor in Escherichia coli-induced coagulation in human whole blood. Clin Exp Immunol 182: 81–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Langer F, Spath B, Fischer C, Stolz M, Ayuk FA, Kroger N, Bokemeyer C, and Ruf W. 2013. Rapid activation of monocyte tissue factor by antithymocyte globulin is dependent on complement and protein disulfide isomerase. Blood 121: 2324–2335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ovstebo R, Hellum M, Aass HCD, Troseid AM, Brandtzaeg P, Mollnes TE, and Henriksson CE. 2014. Microparticle-associated tissue factor activity is reduced by inhibition of the complement protein 5 in Neisseria meningitidis-exposed whole blood. Innate Immun-London 20: 552–560. [DOI] [PubMed] [Google Scholar]
- 17.Ricklin D, Hajishengallis G, Yang K, and Lambris JD. 2010. Complement: a key system for immune surveillance and homeostasis. Nat Immunol 11: 785–797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pilely K, Rosbjerg A, Genster N, Gal P, Pal G, Halvorsen B, Holm S, Aukrust P, Bakke SS, Sporsheim B, Nervik I, Niyonzima N, Bartels ED, Stahl GL, Mollnes TE, Espevik T, and Garred P. 2016. Cholesterol Crystals Activate the Lectin Complement Pathway via Ficolin-2 and Mannose-Binding Lectin: Implications for the Progression of Atherosclerosis. J Immunol 196: 5064–5074. [DOI] [PubMed] [Google Scholar]
- 19.Chu AJ 2011. Tissue factor, blood coagulation, and beyond: an overview. Int J Inflam 2011: 367284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yasojima K, Schwab C, McGeer EG, and McGeer PL. 2001. Complement components, but not complement inhibitors, are upregulated in atherosclerotic plaques. Arterioscler Thromb Vasc Biol 21: 1214–1219. [DOI] [PubMed] [Google Scholar]
- 21.Howes JM, Richardson VR, Smith KA, Schroeder V, Somani R, Shore A, Hess K, Ajjan R, Pease RJ, Keen JN, Standeven KF, and Carter AM. 2012. Complement C3 is a novel plasma clot component with anti-fibrinolytic properties. Diab Vasc Dis Res 9: 216–225. [DOI] [PubMed] [Google Scholar]
- 22.Distelmaier K, Adlbrecht C, Jakowitsch J, Winkler S, Dunkler D, Gerner C, Wagner O, Lang IM, and Kubicek M. 2009. Local complement activation triggers neutrophil recruitment to the site of thrombus formation in acute myocardial infarction. Thromb Haemost 102: 564–572. [DOI] [PubMed] [Google Scholar]
- 23.Palmerini T, Tomasi L, Barozzi C, Della Riva D, Mariani A, Taglieri N, Leone O, Ceccarelli C, De Servi S, Branzi A, Genereux P, Stone GW, and Ahamed J. 2013. Detection of tissue factor antigen and coagulation activity in coronary artery thrombi isolated from patients with ST-segment elevation acute myocardial infarction. PLoS One 8: e81501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Qu HC, Magotti P, Ricklin D, Wu EL, Kourtzelis I, Wu YQ, Kaznessis YN, and Lambris JD. 2011. Novel analogues of the therapeutic complement inhibitor compstatin with significantly improved affinity and potency. Molecular Immunology 48: 481–489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kumar V, Lee JD, Clark RJ, and Woodruff TM. 2018. Development and validation of a LC-MS/MS assay for pharmacokinetic studies of complement C5a receptor antagonists PMX53 and PMX205 in mice. Sci Rep 8: 8101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mollnes TE, Brekke OL, Fung M, Fure H, Christiansen D, Bergseth G, Videm V, Lappegard KT, Kohl J, and Lambris JD. 2002. Essential role of the C5a receptor in E coli-induced oxidative burst and phagocytosis revealed by a novel lepirudin-based human whole blood model of inflammation. Blood 100: 1869–1877. [PubMed] [Google Scholar]
- 27.Powers ER 2016. Aspiration Thrombectomy: The Possible Importance of Effective Thrombus Removal and Minimal Residual Thrombus Burden. JACC Cardiovasc Interv 9: 2012–2013. [DOI] [PubMed] [Google Scholar]
- 28.Skagen K, Skjelland M, Russell D, and Jacobsen EA. 2015. Large-Vessel Occlusion Stroke: Effect of Recanalization on Outcome Depends on the National Institutes of Health Stroke Scale Score. J Stroke Cerebrovasc Dis 24: 1532–1539. [DOI] [PubMed] [Google Scholar]
- 29.Hansson KM, Nielsen S, Elg M, and Deinum J. 2014. The effect of corn trypsin inhibitor and inhibiting antibodies for FXIa and FXIIa on coagulation of plasma and whole blood. J Thromb Haemost 12: 1678–1686. [DOI] [PubMed] [Google Scholar]
- 30.James J, and Tanke HJ. 2012. Biomedical Light Microscopy. Springer Netherlands. [Google Scholar]
- 31.Nasiri M, Janoudi A, Vanderberg A, Frame M, Flegler C, Flegler S, and Abela GS. 2015. Role of cholesterol crystals in atherosclerosis is unmasked by altering tissue preparation methods. Microscopy Research and Technique 78: 969–974. [DOI] [PubMed] [Google Scholar]
- 32.Janoudi A, Shamoun FE, Kalavakunta JK, and Abela GS. 2016. Cholesterol crystal induced arterial inflammation and destabilization of atherosclerotic plaque. Eur Heart J 37: 1959–1967. [DOI] [PubMed] [Google Scholar]
- 33.Kernan WN, Ovbiagele B, Black HR, Bravata DM, Chimowitz MI, Ezekowitz MD, Fang MC, Fisher M, Furie KL, Heck DV, Johnston SC, Kasner SE, Kittner SJ, Mitchell PH, Rich MW, Richardson D, Schwamm LH, Wilson JA, C. o. C. American Heart Association Stroke Council, C. o. C. C. Stroke Nursing, and D. Council on Peripheral Vascular. 2014. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 45: 2160–2236. [DOI] [PubMed] [Google Scholar]
- 34.Kronzon I, and Saric M. 2010. Cholesterol embolization syndrome. Circulation 122: 631–641. [DOI] [PubMed] [Google Scholar]
- 35.Barratt-Due A, Pischke SE, Brekke OL, Thorgersen EB, Nielsen EW, Espevik T, Huber-Lang M, and Mollnes TE. 2012. Bride and groom in systemic inflammation - The bells ring for complement and Toll in cooperation. Immunobiology 217: 1047–1056. [DOI] [PubMed] [Google Scholar]
- 36.Kambas K, Markiewski MM, Pneumatikos IA, Rafail SS, Theodorou V, Konstantonis D, Kourtzelis I, Doumas MN, Magotti P, Deangelis RA, Lambris JD, and Ritis KD. 2008. C5a and TNF-alpha up-regulate the expression of tissue factor in intra-alveolar neutrophils of patients with the acute respiratory distress syndrome. J Immunol 180: 7368–7375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gregory SA, Morrissey JH, and Edgington TS. 1989. Regulation of tissue factor gene expression in the monocyte procoagulant response to endotoxin. Mol Cell Biol 9: 2752–2755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Skjeflo EW, Christiansen D, Fure H, Ludviksen JK, Woodruff TM, Espevik T, Nielsen EW, Brekke OL, and Mollnes TE. 2018. Staphylococcus aureus-induced complement activation promotes tissue factor-mediated coagulation. J Thromb Haemost 16: 905–918. [DOI] [PubMed] [Google Scholar]
- 39.Ikeda K, Nagasawa K, Horiuchi T, Tsuru T, Nishizaka H, and Niho Y. 1997. C5a induces tissue factor activity on endothelial cells. Thromb Haemost 77: 394–398. [PubMed] [Google Scholar]
- 40.Nakamura S, Imamura T, and Okamoto K. 2004. Tissue factor in neutrophils: yes. J Thromb Haemost 2: 214–217. [DOI] [PubMed] [Google Scholar]
- 41.Osterud B 2004. Tissue factor in neutrophils: no. J Thromb Haemost 2: 218–220. [DOI] [PubMed] [Google Scholar]
- 42.Maugeri N, and Manfredi AA. 2015. Tissue Factor Expressed by Neutrophils: Another Piece in the Vascular Inflammation Puzzle. Semin Thromb Hemost 41: 728–736. [DOI] [PubMed] [Google Scholar]
- 43.Ritis K, Doumas M, Mastellos D, Micheli A, Giaglis S, Magotti P, Rafail S, Kartalis G, Sideras P, and Lambris JD. 2006. A novel C5a receptor-tissue factor cross-talk in neutrophils links innate immunity to coagulation pathways. J Immunol 177: 4794–4802. [DOI] [PubMed] [Google Scholar]
- 44.Palta S, Saroa R, and Palta A. 2014. Overview of the coagulation system. Indian J Anaesth 58: 515–523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Losche W 2005. Platelets and tissue factor. Platelets 16: 313–319. [DOI] [PubMed] [Google Scholar]
- 46.Kahn ML, Zheng YW, Huang W, Bigornia V, Zeng D, Moff S, Farese RV Jr., Tam C, and Coughlin SR. 1998. A dual thrombin receptor system for platelet activation. Nature 394: 690–694. [DOI] [PubMed] [Google Scholar]
- 47.Patzelt J, Mueller KA, Breuning S, Karathanos A, Schleicher R, Seizer P, Gawaz M, Langer HF, and Geisler T. 2015. Expression of anaphylatoxin receptors on platelets in patients with coronary heart disease. Atherosclerosis 238: 289–295. [DOI] [PubMed] [Google Scholar]
- 48.Del Conde I, Cruz MA, Zhang H, Lopez JA, and Afshar-Kharghan V. 2005. Platelet activation leads to activation and propagation of the complement system. J Exp Med 201: 871–879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nasiri M, Janoudi A, Vanderberg A, Frame M, Flegler C, Flegler S, and Abela GS. 2015. Role of cholesterol crystals in atherosclerosis is unmasked by altering tissue preparation methods. Microsc Res Tech 78: 969–974. [DOI] [PubMed] [Google Scholar]
- 50.Ho-Tin-Noe B, Vo S, Bayles R, Ferriere S, Ladjal H, Toumi S, Deschildre C, Ollivier V, and Michel JB. 2017. Cholesterol crystallization in human atherosclerosis is triggered in smooth muscle cells during the transition from fatty streak to fibroatheroma. J Pathol 241: 671–682. [DOI] [PubMed] [Google Scholar]
- 51.Ricklin D, Reis ES, Mastellos DC, Gros P, and Lambris JD. 2016. Complement component C3 - The “Swiss Army Knife” of innate immunity and host defense. Immunol Rev 274: 33–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hillmen P, Muus P, Roth A, Elebute MO, Risitano AM, Schrezenmeier H, Szer J, Browne P, Maciejewski JP, Schubert J, Urbano-Ispizua A, de Castro C, Socie G, and Brodsky RA. 2013. Long-term safety and efficacy of sustained eculizumab treatment in patients with paroxysmal nocturnal haemoglobinuria. Br J Haematol 162: 62–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pischke SE, Gustavsen A, Orrem HL, Egge KH, Courivaud F, Fontenelle H, Despont A, Bongoni AK, Rieben R, Tonnessen TI, Nunn MA, Scott H, Skulstad H, Barratt-Due A, and Mollnes TE. 2017. Complement factor 5 blockade reduces porcine myocardial infarction size and improves immediate cardiac function. Basic Res Cardiol 112: 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ridker PM, Everett BM, Thuren T, MacFadyen JG, Chang WH, Ballantyne C, Fonseca F, Nicolau J, Koenig W, Anker SD, Kastelein JJP, Cornel JH, Pais P, Pella D, Genest J, Cifkova R, Lorenzatti A, Forster T, Kobalava Z, Vida-Simiti L, Flather M, Shimokawa H, Ogawa H, Dellborg M, Rossi PRF, Troquay RPT, Libby P, Glynn RJ, and C. T. Group. 2017. Antiinflammatory Therapy with Canakinumab for Atherosclerotic Disease. N Engl J Med 377: 1119–1131. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.