Abstract
IMPORTANCE
Perceived everyday discrimination is a psychosocial stressor linked to adverse health outcomes, including mortality.
OBJECTIVE
To assess the association of vision impairment (VI), hearing impairment (HI), and dual sensory impairments (DSI) with everyday discrimination.
DESIGN, SETTING, AND PARTICIPANTS
Cross-sectional analysis of the Health and Retirement Study 2006 and 2008 surveys, a US population-based survey that included noninstitutionalized adults 51 years and older. Analyses were weighted to account for complex sample design and differential nonresponse. Data were analyzed between October 2019 and November 2019.
EXPOSURES
Participants rated their vision and hearing, using eyeglasses and/or hearing aids if applicable, on a Likert scale (poor, fair, good, very good, and excellent). Sensory impairment was defined as poor or fair ability in the relevant modality, and sensory impairment was categorized as neither sensory impairment (NSI), VI alone, HI alone, and DSI.
MAIN OUTCOMES AND MEASURES
Perceived everyday discrimination was measured on the validated 5-question Williams scale (range 0 to 5). Linear regression models estimated differences in discrimination scores by sensory categories, adjusting for age, sex, race, ethnicity, non-US birth, body mass index, relationship status, net household wealth, and number of chronic diseases (among diabetes, hypertension, heart disease, stroke, lung disease, nonskin cancer, and arthritis).
RESULTS
The sample included 13 092 individuals. After weighting the sample to be representative of the US population, 11.7% had VI alone, 13.1% HI alone, and 7.9% DSI. In the fully adjusted model, participants with VI alone (β [change in discrimination score], 0.07; 95% CI, 0.02–0.13), HI alone (β = 0.07; 95% CI, 0.02–0.11), and DSI (β = 0.23; 95% CI, 0.16–0.29) perceived greater discrimination compared with participants with NSI. The DSI group perceived greater discrimination than VI alone or HI alone.
CONCLUSIONS AND RELEVANCE
Older adults with VI or HI in the United States perceive greater everyday discrimination than older adults with NSI, and those with DSI perceive even more discrimination than those with either VI or HI alone. These results provide insight into the social impact of sensory loss and highlight a need to identify and address reasons for discrimination toward older adults with VI and HI.
As the population ages,1 the prevalence of vision impairments (VIs) and hearing impairments (HIs), and dual sensory impairment (DSI; defined as concurrent VI and HI), will increase. One in 9 adults older than 80 years currently has DSI,2 which has been associated with poorer quality of life,3 independent living difficulty,4,5 anxiety,6 depression,6,7 cognitive impairment,5,8,9 and evenmortality.10,11 Further, these adverse outcomes are generally more strongly associated with DSI than with VI or HI alone.
Discrimination is the unjust treatment of individuals and groups regarded as inferior by more powerful and privileged groups in society. It can be categorized as systemic or everyday discrimination. Systemic discrimination refers to conditions or actions that lead to the preferential allocation of resources and rights to more privileged groups (eg, residential segregation), while everyday discrimination refers to relatively minor experiences that reproduce the effects of systemic discrimination (eg, receiving poorer service than others).12 Most reported discrimination is everyday discrimination, and more than 60% of the US population has experienced this type of discrimination.13,14 Individuals who experience discrimination are often aware of being treated differently, which can engender psychosocial stress.15,16
In addition to being morally wrong, perceived discrimination has been linked to a multitude of negative psychological and physical health outcomes, including worsening emotional well-being,17 psychological distress,14,16 chronic pain,18 poorer subjective health,17 higher rates of incident metabolic syndrome,19 impaired cognitive performance,18 and mortality.20,21 Previous studies on perceived discrimination have focused on discrimination on the basis of race, ethnicity, gender, sexual orientation, disability, and age.22
People with disabilities, including sensory disability, experience social disparities compared with people without disabilities, such as lower employment rates and incomes as well as higher rates of poverty.23,24 However, research on sensory disability and perceived discrimination has been limited. Increased perceived discrimination has been shown in individuals with VI in an English cohort and in a population of Spanish individuals with HI in a qualitative study.25,26 To our knowledge, the association between DSI and perceived discrimination has not been examined. In this study, we analyze perceived discrimination in individuals with sensory impairments (VI, HI, and DSI) using a nationally representative sample of the US older adult population. Further, we hypothesize that individuals with DSI perceive greater discrimination than individuals with VI or HI alone.
Methods
Study Design and Participants
This study included participants from the Health and Retirement Study (HRS), a longitudinal study of noninstitutionalized adults 51 years and older in the United States. The HRS is sponsored by the National Institute on Aging (grant U01AG009740) and is conducted by the University of Michigan.27 The HRS protocol has been approved by the institutional review board at the University of Michigan. All participants gave verbal consent prior to the interview, and they were provided token payments for participation. Participants are surveyed very 2 years. In 2006, half of HRS participants were randomly selected to receive a psychosocial and lifestyle questionnaire (PLQ), where they were asked about their everyday discrimination experiences, and in 2008, the other half of the HRS sample received the PLQ.28
Measures
Perceived Everyday Discrimination
The PLQ included a validated 5-item every day experiences with discrimination measure.29 Participants were asked how often they experienced the following occurrences in their day-to-day life:
You are treated with less courtesy or respect than otherpeople.
You receive poorer service than other people at restaurants or stores.
People act as if they think you are not smart.
People act as if they are afraid of you.
You are threatened or harassed.
There were 6 possible responses to each question that were converted to numerical values: never = 0, less than once a year = 1, a few times a year = 2, a few times a month = 3, at least once a week = 4, and almost every day = 5.
For the primary analysis, the responses from the 5 questions were averaged to create a discrimination score. This approach is consistent with prior work using this scale in HRS.21 The internal consistency (Cronbach α) of this measure was 0.80 for 2006 and 0.82 for the 2008 sample.28
Sensory Impairment
Sensory impairment was assessed using patient-reported functional measures. Visual ability was assessed on a single item: “Is your eyesight excellent, very good, good, fair, or poor using glasses or corrective lens as usual?” Hearing ability was similarly assessed on a single item: “Is your hearing excellent, very good, good, fair, or poor?” Participants who indicated using a hearing aid during the interview or any prior interview were asked to rate their hearing “using a hearing aid as usual.” Impairment was defined as reporting fair or poor sensory ability on the respective question(s). Dual sensory impairment was defined as having concurrent VI and HI.
Covariates
Demographic covariates were self-reported and included age, sex, race (modeled as White vs other races), ethnicity (Hispanic vs non-Hispanic), birth in the United States, relationship status (married, partnered, or other), and education (high school or less, some or full college, graduate level). Additionally, net household wealth was obtained from the RAND HRS Longitudinal File 2016 (V1),30 which included imputed values for missing wealth variables. Wealth was divided into quartiles that were modeled as categorical variables.
Health covariates included body mass index (BMI; calculated as weight in kilograms divided by height in meters squared) and chronic disease index. When either of these was missing (1862 participants), self-reported height or weight were used. Participants who had both measured and self-reported readings tended to underestimate their weight (mean difference, 1.37 kg; 95% CI, 1.29–1.44) and overestimate their height (mean difference, 2.4 cm; 95% CI, 2.3–2.5). Chronic disease index is the number of self-reported diagnoses among diabetes, hypertension, heart disease, stroke, lung disease, nonskin cancer, and arthritis.21
Presence of psychiatric conditions was based on self-report, “Have you ever had or has a doctor ever told you that you had any emotional, nervous, or psychiatric problems?” Presence of memory-related disease was based on self-report, “Has a doctor told you that you have a memory-related disease?” Finally, delayed recall of a 10-word list was included as the number of words recalled correctly.
Analysis
Data
This analysis combined data from the 2006 and 2008 study visits with responses to the PLQ. Overall, 13 825 were eligible and completed the PLQ (7232 in 2006 and 6593 in 2008). Participants who did not respond to 1 or more discrimination questions were excluded (n = 475). We also excluded nursing home residents (n = 67), legally blind participants (n = 57) or participants with missing vision or hearing ability (n = 18), and participants with missing BMI (n = 143). In total, 733 participants (5.3%) were excluded for 1 or more of the reasons mentioned above.
Statistical Approach
All analyses were weighted to account for HRS complex design and differential nonresponse to the PLQ. We performed 3 regression analyses to determine the association between sensory impairment and perceived everyday discrimination (1) using discrimination score (average of the 5 discrimination questions) as the outcome, (2) using question score as the outcome and repeating the analysis separately for each question, (3) using frequent perceived discrimination (defined as perceived discrimination a few times a month or more frequently on any of the 5 questions) as the outcome.
Line arregression was used to model discriminations core and log-binomial regression to calculate prevalence ratios of frequent discrimination by sensory impairment. Poisson regression with robust variance estimation was used when the log-binomial model failed to converge. Adjusted models controlled for age, sex, race, ethnicity, US birth, BMI, relationship status, education, wealth, and chronic disease index. Based on the exploratory analysis, age was modelled with a linear spline term at 70 years, and interaction terms were included among race, ethnicity, and sex. An additional linear model was fitted without interaction terms to determine the difference in perceived discrimination between non-White vs White individuals, thereby providing context to interpret the coefficients for sensory impairment.
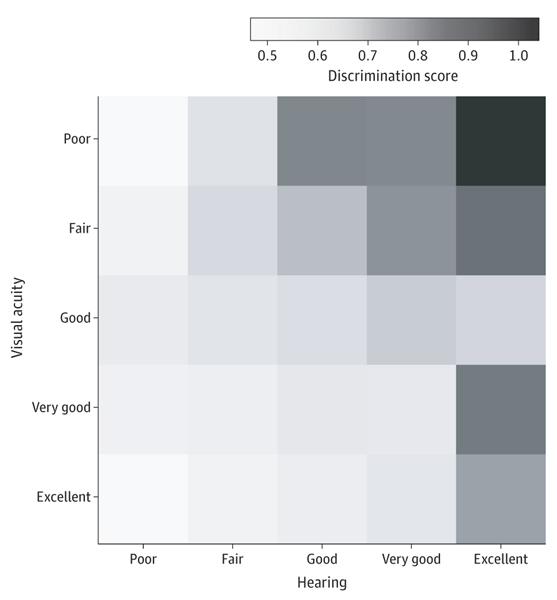
In the primary analysis, sensory impairment was categorized as neither sensory impairment (NSI), VI alone, HI alone, and DSI. Additionally, analysis1was repeated with hearing and vision abilities entered as categorical variables with interaction terms between them. Model marginal effects were calculated to determine the discrimination score for each combination of vision and hearing abilities after accounting for covariates. The marginal effects were displayed in a vision vs hearing ability tile plot. Two-sided P values were reported and values less than .05 were considered statistically significant. The analyses were conducted using the R statistical software package, version 3.5.3 (R Core Team 2019; R Foundation for Statistical Computing). Data were analyzed between October 2019 and December 2019.
Sensitivity Analysis
The regression model in analysis 1 was rerun while including psychiatric conditions, memory-related disease, and delayed recall. These measures of psychiatric and cognitive function were not included in the main analysis because they may act as mediators on the association between sensory impairment and discrimination or they may be consequential to perceived discrimination.17
Results
Study Population
The analysis included 13092 individuals: 1609 had VI alone, 1786 had HI alone, and 1061 had DSI. Participant characteristics are summarized in Table 1. After applying weights for survey design and nonresponse,11.7%hadVIalone,13.1%hadHI alone, and 7.9% had DSI (eTable 1 in the Supplement). Individuals with DSI were older than individuals with NSI and more likely to be male, non-White, Hispanic, or have been born outside the US. Individuals with DSI were also less likely to be married or partnered, less likely to have college or graduate education and had lower net household wealth compared with participants with NSI. Further, DSI participants had more chronic conditions than individuals with NSI. The frequency of perceived discrimination by sensory impairment across the 5 questions is shown in eFigure in the Supplement.
Table 1.
Description of the Study Population: the Health and Retirement Study 2006 and 2008
| %a | ||||
|---|---|---|---|---|
| Characteristic | NSI (n = 8636) | VI alone (n = 1609) | HI alone (n = 1786) | DSI (n = 1061) |
| Weighted proportion | 67.3 | 11.7 | 13.1 | 7.9 |
| Age, mean (SD), y | 65.2 (9.3) | 67.6 (10.8) | 69.5 (10.6) | 70.6 (11.8) |
| Female | 57.2 | 62.3 | 36.6 | 45.7 |
| Non-White race | 12.1 | 23.7 | 8.7 | 18.9 |
| Hispanic ethnicity | 5.4 | 13.6 | 7.7 | 14.6 |
| Born outside United States | 7.1 | 12.1 | 6.7 | 13.4 |
| Married or partnered | 69.1 | 57.3 | 68.7 | 57.6 |
| Education | ||||
| High school or less | 65.6 | 80.6 | 74.9 | 87.6 |
| College | 22.2 | 13.6 | 15.8 | 8.9 |
| Graduate | 12.1 | 5.9 | 9.3 | 3.5 |
| Net household wealth, median (IQR)b | 279 (90–660) | 106 (15–365) | 223 (64–601) | 76 (7–264) |
| BMI, mean (SD) | 29.4 (6.2) | 29.6 (6.9) | 29.4 (6.0) | 29.8 (6.8) |
| Chronic disease index, mean (SD)c | 1.68 (1.25) | 2.26 (1.41) | 2.07 (1.32) | 2.56 (1.44) |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared)
DSI, dual sensory impairment
HI, hearing impairment
IQR, interquartile range
NSI, neither sensory impairment
VI, vision impairment.
Percentage unless indicated otherwise. All figures are weighted for sampling probabilities and differential nonresponse.
Thousand of US dollars.
Number of chronic conditions among hypertension, diabetes mellitus, cancer other than skin, lung disease, heart disease, stroke, and arthritis. Range, 0 to 7.
Overall Discrimination Score
In a fully adjusted model, participants with VI alone (β = 0.07; 95% CI, 0.02–0.13) and HI alone (β = 0.07; 95% CI, 0.02–0.11) had higher discrimination cores (meaning greater levels of discrimination) compared with the NSI group, but this difference was greatest for those with DSI (β = 0.23; 95% CI, 0.16–0.29). Additionally, the differences between DSI and each of VI alone (β = 0.16; 95% CI, 0.08–0.23) and HI alone (β = 0.16; 95%CI, 0.09–0.23) were significant (Table 2). To provide context for these β coefficients, individuals who identified as non-White perceived greater discrimination (β = 0.11; 95%CI, 0.05–0.17) than individuals who identified as White after adjusting for all covariates.
Table 2.
Regression Analysis of Everyday Discrimination Score by Sensory Impairment: the Health and Retirement Study 2006 and 2008
| Variable | Discrimination score, mean | Unadjusted model | Adjusted modela | ||
|---|---|---|---|---|---|
| β (95% CI)b | P value | β (95% CI)b | P value | ||
| NSI | 0.63 | 1 [Reference] | NA | 1 [Reference] | NA |
| VI alone | 0.71 | 0.08 (0.02 to 0.14) | .008 | 0.07 (0.02 to 0.13) | .03 |
| HI alone | 0.67 | 0.04 (−0.004 to 0.08) | .08 | 0.07 (0.02 to 0.11) | .005 |
| DSI | 0.86 | 0.23 (0.17 to 0.29) | <.001 | 0.23 (0.16 to 0.29) | <.001 |
Abbreviations: DSI, dual sensory impairment; HI, hearing impairment; NA, not applicable; NSI, neither sensory impairment; VI, vision impairment.
Model adjusted for age, sex, race, ethnicity, US birth, body mass index, relationship status, education, wealth, and chronic disease index.
β Can be interpreted as the difference in everyday discrimination score comparing a sensory impairment group to the reference group of no sensory impairment.
Among those with VI and after accounting for the covariates, participants who also had HI reported higher discrimination scores. Similarly, among those with HI, participants who also had VI perceived greater discrimination (Figure).
Figure. Discrimination Score by Self-Reported Hearing and Vision Ability.
Vision and hearing abilities are modeled as categorical variables. Discrimination scores were obtained from the marginal effects of a linear regression model adjusted for age, sex, race, ethnicity, US birth, body mass index, relationship status, wealth, and chronic disease index. Possible range for the discrimination score is 0 to 5.
Question-Specific Discrimination
In fully adjusted models, perceived discrimination item score was higher in VI alone and HI alone compared with NSI for questions asking about being treated with less respect and if people act as if they think the individual is not smart. For those with HI alone, perceived discrimination item score was additionally higher for the questions about receiving poorer service. Perceived discrimination score was higher in DSI compared with NSI for all 5 questions, with the increase being most pronounced for questions asking about being treated with less respect (β = 0.28; 95% CI, 0.19–0.38) and if people act as if they think the individual is not smart (β = 0.39; 95% CI, 0.28–0.50). For all 5 questions, participants with DSI perceived greater discrimination than both VI alone and HI alone participants in fully adjusted models (values for questions A through E, respectively:β = 0.18;95%CI,0.07–0.29;P = .002; β = 0.12; 95% CI, 0.02–0.21; P = 0.02; β = 0.23; 95% CI, 0.110.36; P = .001;β = 0.12; 95% CI, 0.02–0.21; P = 0.02; β = 0.14; 95% CI, 0.05–0.23; P = 0.003) (Table 3).
Table 3.
Regression Analysis of Everyday Discrimination Question Responses by Sensory Impairment: the Health and Retirement Study 2006 and 2008
| Variable | Discrimination question, adjusted p (95% CI)a,b | ||||
|---|---|---|---|---|---|
| Treated with less respect than others | Receive poorer service at restaurants and stores | People act as if they think you are not smart | People act as if afraid of you | Threatened or harassed | |
| NSI | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| VI alone | 0.10 (0.02 to 0.19) | 0.04 (−0.04 to 0.11) | 0.16 (0.07 to 0.24) | 0.04 (−0.03 to 0.12) | 0 (−0.05 to 0.05) |
| HI alone | 0.10 (0.03 to 0.18) | 0.06 (0.02 to 0.11) | 0.14 (0.07 to 0.22) | 0.04 (−0.02 to 0.10) | −0.01 (−0.06 to 0.04) |
| DSI | 0.28 (0.19 to 0.38)c | 0.15 (0.08 to 0.23)c | 0.39 (0.28 to 0.50)c | 0.16 (0.09 to 0.23)c | 0.14 (0.06 to 0.22)c |
Abbreviations: DSI, dual sensory impairment; HI, hearing impairment; NSI, neither sensory impairment; VI, vision impairment.
Models adjusted for age, sex, race, ethnicity, US birth, body mass index, relationship status, education, wealth, and chronic disease index.
See Methods for full question text. Each discrimination question is scaled from 0 (never) to 5 (almost every day).
There are statistically significant (P < .05) differences comparing DSI with both VI alone and HI alone. Values for questions A through E, respectively: β = 0.18; 95% CI, 0.07–0.29; P = .002; β = 0.12; 95% CI, 0.02–0.21; P = 0.02; β = 0.23; 95% CI, 0.11–0.36; P = .001; β = 0.12; 95% CI, 0.02–0.21; P = 0.02; β = 0.14; 95% CI, 0.05–0.23; P = 0.003.
Frequent Discrimination
After adjusting for covariates, the prevalence of frequent discrimination was higher by 38% (95% CI, 20%−58%) for VI alone, by 21% (95% CI, 3%−43%) for HI alone, and by 72% (95% CI, 47%−100%) for DSI when compared with NSI (Table 4). The prevalence of frequent discrimination was higher in DSI than in VI alone by 25% (95% CI, 9%−43%) and higher than in HI alone by 41% (95% CI, 15%−73%).
Table 4.
Regression Analysis of the Proportion Experiencing Frequent Everyday Discrimination by Sensory Impairment: the Health and Retirement Study 2006 and 2008a
| Variable | Frequent discrimination, %a | Unadjusted model | Adjusted modelb | ||
|---|---|---|---|---|---|
| PrR (95% CI) | P value | PrR (95% CI) | P value | ||
| NSI | 15.2 | 1 [Reference] | NA | 1 [Reference] | NA |
| VI alone | 24.0 | 1.58 (1.39–1.80) | <.001 | 1.38 (1.20–1.58) | <.001 |
| HI alone | 17.4 | 1.14(0.98–1.34) | .10 | 1.21 (1.03–1.43) | .02 |
| DSI | 29.3 | 1.93 (1.68–2.22) | <.001 | 1.72 (1.47–2.00) | <.001 |
Abbreviations: DSI, dual sensory impairment; HI, hearing impairment; NA, not applicable; NSI, neither sensory impairment; PrR, prevalence ratio; VI, vision impairment.
Frequent discrimination is defined as experiencing discrimination few times a month or more frequently on any of the 5 everyday discrimination questions. Percentages are weighted for survey design and nonresponse.
Model adjusted for age, sex, race, ethnicity, US birth, body mass index, relationship status, education, wealth, and chronic disease index.
Sensitivity Analysis
The same inferences were obtained after adjusting for psychiatric conditions with or without measures of cognitive function (eTable 2 in the Supplement).
Discussion
In a nationally representative sample of 13 092 older adults in the United States, we found that those who reported hearing or vision loss perceived greater every day discrimination than older adults with out these impairments. Moreover, older adults with DSI perceived even more discrimination than those with either hearing or vision loss alone. Having DSI increased perceived discrimination about twice as much as being of non-White race. Perceived everyday discrimination is a multidomain construct, and DSI increased perceived discrimination across the 5 domains tested in this analysis. However, the greatest increases were in the perception of being treated with less respect and the perception that people act as if the individual with DSI was “not smart.”
Compared with older adults with NSI, the prevalence of frequent perceived discrimination was higher in VI alone by 38% after accounting for potential confounders. Vision impairment was also associated with perceived everyday discrimination in an English cohort of older adults, where the increase in odds of perceived discrimination for individuals with VI in that study was similar to the current estimate in the US HRS cohort.25 In our study, VI was associated with increased discrimination in the domains of being treated with less respect and others acting as if the individual with VI was not smart. These findings are consistent with previous qualitative research from Spain,26 where those with VI reported mockery, bullying, (corresponds to being treated with less respect), and over protection is min the family and public settings (corresponds to people acting as if an individual with VI is not smart).
We also found a significant increase in the perception of discrimination in individuals with hearing loss. The prevalence of frequent discrimination increased by 21% in HI alone compared with NSI after accounting for confounders. While the increase in frequent discrimination for HI was lower than VI, the increase in overall discrimination score was similar to VI. This may indicate that a greater number of older adults with hearing loss perceive discrimination than older adults with vision loss, but that discrimination is experienced less often by individuals with HI over the course of a year. Hearing impairment was associated with the same 2 discrimination domains that were associated with VI; HI was also associated with increased perception of receiving poorer service at restaurants and stores. Receiving poorer service may correspond to the finding in the Spanish study that individuals with HI were highly concerned regarding poor access to leisure activities.26
The most pronounced increase in the perception of every day discrimination was experienced by individuals with DSI, who reported 72% more frequent discrimination compared with individuals with NSI. Discrimination was significantly higher in DSI compared with either VI or HI alone. Further-more, DSI was associated with increased discrimination across all 5 domains of the scale used in our analysis. In addition to the 3 domains mentioned previously, individuals with DSI also perceived that people act afraid of them and that people harass or bother them.
The relationship among sensory impairment, discrimination, and adverse health is poorly understood. Sensory impairment can reduce quality of life,3 cause difficulty navigating the activities of daily living,4 and negatively affect psychiatric and cognitive health.6–8 Everyday discrimination is an important stressor16,22 that can compound the emotional and cognitive difficulties of sensory impairment, thereby increasing adverse health outcomes. For example, older adults with VI who reported perceived discrimination had increased incident depression compared with older adults with VI who did not report discrimination.25 This is an argument that perceived discrimination amplifies (that is, act as an effect-measure modifier) the effect of sensory impairment on adverse health.
On the other hand, perceived discrimination is a psychosocial stressor that causes chronic low-grade inflammation and unhealthy coping behaviors,16,31 resulting in adverse health outcomes.22 Taken together, the adverse health effects of sensory impairment and our findings herein supported by other studies25 raise the question as to whether perceived discrimination mediates part of the association between sensory impairment and adverse health outcomes. Further research is needed to elucidate the role of discrimination in the sensory impairment and adverse health relationship.
Our analysis demonstrates that for those rating their hearing as “good” or better, an individual did not perceive increased discrimination even when they had poor vision. Perceived discrimination owing to sensory impairment mainly occurred when hearing was poor or both vision and hearing deteriorated in the same individual. Individuals with poor vision and poor hearing experienced twice as much discrimination as individuals with excellent vision and excellent hearing. Sensory substitution may help individuals with sensory impairment cope with a singular sensory loss, and concurrent loss of both vision and hearing may limit an individual’s ability to navigate society,32 thereby creating a communication barrier between the individual with DSI and others, rein forcing the perception of discrimination.
Limitations
The limitations of this study should be considered when interpreting our results. First, our results are limited by the cross sectional analytic approach, and future studies should explore the effect of sensory impairment on subsequent onset or increase in perceived discrimination. Second, given the self reported nature of both exposure and outcome, we cannot rule out an association caused by individual factors that concurrently lead to the perceptions of greater discrimination and poorer sensory function. Therefore, studies should seek to replicate our findings using objective measures of hearing and vision. Third, discrimination is based on recollection of past experiences and may be subject to problems with incorrect recall. Further, while this study adjusted for the most relevant covariates, there remains a risk of residual or unmeasured confounding. Despite these limitations, this study is, to our knowledge, the first large, population-based study examining discrimination among older adults with VI, HI, and DSI and documents an understudied association.
Conclusions
Overall, these results indicate that older adults with vision and hearing loss experience more discrimination than those without these impairments, and those with concurrent hearing and vision loss (DSI) perceive the greatest discrimination across many aspects of their day-to-day lives. Therefore, discrimination may be an important, yet under recognized, implication of sensory loss in late life. More work is needed to address this discrimination, which may help to mitigate some of the negative consequences of vision and hearing loss among older adults.
Supplementary Material
Key Points.
Question
How is sensory impairment associated with increased discrimination among older adults?
Findings
In a US population-based survey, older adults reporting vison or hearing loss perceived greater discrimination than older adults not reporting these impairments, and older adults with dual sensory impairment (concurrent vison and hearing loss) perceived the greatest levels of discrimination.
Meaning
These results suggest that older adults with sensory impairments perceive greater levels of discrimination than older adults without these impairments.
Acknowledgments
Funding/Support: This work is supported by Research to Prevent Blindness and The National Institute on Aging (K01AG052640).
Role of the Funder/Sponsor: The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Conflict of Interest Disclosures: Dr Ehrlich reported grants from National Institutes of Health during the conduct of the study. Dr Reed reported grants from National Institute on Aging (1K23AG065443-01) during the conduct of the study; and Scientific Advisory Board (no financial compensation) for Shoebox Inc and Good Machine Studio. No other disclosures were reported.
REFERENCES
- 1.He W, Goodkind D, Kowal P. U.S. Census Bureau, International Population Reports, P95/16–1, An Aging World: 2015. U.S. Government Publishing Office: 2016. [Google Scholar]
- 2.Swenor BK, Ramulu PY, Willis JR, Friedman D, Lin FR. The prevalence of concurrent hearing and vision impairment in the United States. JAMA Intern Med. 2013;173(4):312–313. doi: 10.1001/jamainternmed.2013.1880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tseng YC, Liu SH, Lou MF, Huang GS. Quality of life in older adults with sensory impairments: a systematic review. Qual Life Res. 2018;27(8): 1957–1971. doi: 10.1007/s11136-018-1799-2 [DOI] [PubMed] [Google Scholar]
- 4.Bouscaren N, Yildiz H, Dartois L, Vercambre MN, Boutron-Ruault MC. Decline in instrumental activities of daily living over 4-year: the association with hearing, visual and dual sensory impairments among non-institutionalized women. J Nutr Health Aging. 2019;23(8):687–693. doi: 10.1007/s12603-019-1231-9 [DOI] [PubMed] [Google Scholar]
- 5.Fuller SD, Mudie LI, Siordia C, Swenor BK, Friedman DS. Nationwide prevalence of self-reported serious sensory impairments and their associations with self-reported cognitive and functional difficulties. Ophthalmology. 2018;125(4): 476–485. doi: 10.1016/j.ophtha.2017.11.003 [DOI] [PubMed] [Google Scholar]
- 6.Simning A, Fox ML, Barnett SL, Sorensen S, Conwell Y. Depressive and anxiety symptoms in older adults with auditory, vision, and dual sensory impairment. J Aging Health. 2019;31(8):1353–1375. doi: 10.1177/0898264318781123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Han JH, Lee HJ, Jung J, Park EC. Effects of self-reported hearing or vision impairment on depressive symptoms: a population-based longitudinal study. Epidemiol Psychiatr Sci. 2019;28 (3):343–355. doi: 10.1017/S2045796018000045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maharani A, Dawes P, Nazroo J, Tampubolon G, Pendleton N; Sense-Cog WP1 Group. Associations between self-reported sensory impairment and risk of cognitive decline and impairment in the health and retirement study cohort. J Gerontol B Psychol Sci Soc Sci. 2020;75(6):1230–1242. [DOI] [PubMed] [Google Scholar]
- 9.Liljas AEM, Walters K, de Oliveira C, Wannamethee SG, Ramsay SE, Carvalho LA. Self-reported sensory impairments and changes in cognitive performance: a longitudinal 6-year follow-up study of english community-dwelling adults aged 50 years. J Aging Health. 2020;32 (5–6):243–251. doi: 10.1177/0898264318815391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gopinath B, Schneider J, McMahon CM, Burlutsky G, Leeder SR, Mitchell P. Dual sensory impairment in older adults increases the risk of mortality: a population-based study. PLoS One. 2013;8(3):e55054. doi: 10.1371/journal.pone.0055054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fisher D, Li CM, Chiu MS, et al. Impairments in hearing and vision impact on mortality in older people: the AGES-Reykjavik Study. Age Ageing. 2014;43(1):69–76. doi: 10.1093/ageing/aft122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Essed Philomena. Understanding Everyday Racism: An Interdisciplinary Theory. Sage Publications, Inc; 1991. [Google Scholar]
- 13.American Psychological Association. Stress in America: The impact of discrimination. Stress in America™ Survey. Published 2016. Accessed September 2, 2020. https://www.apa.org/news/press/releases/stress/2015/impact-ofdiscrimination.pdf
- 14.Kessler RC, Mickelson KD, Williams DR. The prevalence, distribution, and mental health correlates of perceived discrimination in the United States. J Health Soc Behav. 1999;40(3):208–230. doi: 10.2307/2676349 [DOI] [PubMed] [Google Scholar]
- 15.Clark R, Anderson NB, Clark VR, Williams DR. Racism as a stressor for African Americans: a biopsychosocial model. Am Psychol. 1999;54(10): 805–816. doi: 10.1037/0003-066X.54.10.805 [DOI] [PubMed] [Google Scholar]
- 16.Pascoe EA, Smart Richman L. Perceived discrimination and health: a meta-analytic review. Psychol Bull. 2009;135(4):531–554. doi: 10.1037/a0016059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sutin AR, Stephan Y, Carretta H, Terracciano A. Perceived discrimination and physical, cognitive, and emotional health in older adulthood. Am J Geriatr Psychiatry. 2015;23(2):171–179. doi: 10.1016/j.jagp.2014.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brown TT, Partanen J, Chuong L, Villaverde V, Chantal Griffin A, Mendelson A. Discrimination hurts: the effect of discrimination on the development of chronic pain. Soc Sci Med. 2018; 204:1–8. doi: 10.1016/j.socscimed.2018.03.015 [DOI] [PubMed] [Google Scholar]
- 19.Beatty Moody DL, Chang Y, Brown C, Bromberger JT, Matthews KA. Everyday discrimination and metabolic syndrome incidence in a racially/ethnically diverse sample: Study of Women’s Health Across the Nation. Psychosom Med. 2018;80(1):114–121. doi: 10.1097/PSY.0000000000000516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barnes LL, de Leon CF, Lewis TT, Bienias JL, Wilson RS, Evans DA. Perceived discrimination and mortality in a population-based study of older adults. Am J Public Health. 2008;98(7):1241–1247. doi: 10.2105/AJPH.2007.114397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Farmer HR, Wray LA, Thomas JR. Do race and everyday discrimination predict mortality risk? evidence from the Health and Retirement Study. Gerontol Geriatr Med. 2019;5:2333721419855665. doi: 10.1177/2333721419855665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. J Behav Med. 2009;32(1):20–47. doi: 10.1007/s10865-008-9185-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.National Research Council Committee on Disability Determination for Individuals with Visual Impairments; Lennie P, Van Hemel SB, eds. Visual Impairments: Determining Eligibility for Social Security Benefits. National Academies Press; 2002. [PubMed] [Google Scholar]
- 24.Brucker DL, Houtenville AJ. People with disabilities in the United States. Arch Phys Med Rehabil. 2015;96(5):771–774. doi: 10.1016/j.apmr.2015.02.024 [DOI] [PubMed] [Google Scholar]
- 25.Jackson SE, Hackett RA, Pardhan S, Smith L, Steptoe A. Association of perceived discrimination with emotional well-being in older adults with visual impairment. JAMA Ophthalmol. 2019;137(7): 825–832. doi: 10.1001/jamaophthalmol.2019.1230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pérez-Garín D, Recio P, Magallares A, Molero F, García-Ael C. perceived discrimination and emotional reactions in people with different types of disabilities: a qualitative approach. Span J Psychol. 2018;21:E12. doi: 10.1017/sjp.2018.13 [DOI] [PubMed] [Google Scholar]
- 27.Fisher GG, Ryan LH. Overview of the health and retirement study and introduction to the special issue. Work Aging Retire. 2018;4(1):1–9. doi: 10.1093/workar/wax032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Smith J, Ryan LH, Fisher GG, Sonnega A, Weir DR. HRS Psychosocial and Lifestyle Questionnaire 2006–2016. Published 2017. Accessed September 2, 2020. https://hrs.isr.umich.edu/sites/default/files/biblio/HRS%202006-2016%20SAQ%20Documentation_07.06.17.pdf
- 29.Williams DR, Yan Yu, Jackson JS, Anderson NB. Racial differences in physical and mental health: socio-economic status, stress and discrimination. J Health Psychol. 1997;2(3):335–351. doi: 10.1177/135910539700200305 [DOI] [PubMed] [Google Scholar]
- 30.RAND Center for the Study of Aging. RANDHRS Longitudinal File 2016, version 1. Published May 2019. Accessed September 2, 2020. https://www.rand.org/content/dam/rand/www/external/labor/aging/dataprod/randhrs1992_2016v1.pdf
- 31.Jackson JS, Knight KM, Rafferty JA. Race and unhealthy behaviors: chronic stress, the HPA axis, and physical and mental health disparities over the life course. Am J Public Health. 2010;100(5):933–939. doi: 10.2105/AJPH.2008.143446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Brennan M, Bally SJ. Psychosocial adaptations to dual sensory loss in middle and late adulthood. Trends Amplif. 2007;11(4):281–300. doi: 10.1177/1084713807308210 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.