Abstract
BACKGROUND AND OBJECTIVES:
Children who are deaf or hard of hearing (DHH) often have persistent language delays despite early identification and interventions. The technology-assisted language intervention (TALI), which incorporates augmentative and alternative communication technology into a speech-language therapy model, was designed to support language learning. The study objective was to evaluate the impact of the TALI on spoken language outcomes in DHH children.
METHODS:
Children aged 3 to 12 years with mild to profound bilateral hearing loss were enrolled in a single-site randomized controlled trial. Children were randomly assigned to receive the TALI or treatment as usual (TAU) (with no change in current care) and were followed for 24 weeks. Primary outcomes included spoken language measures elicited from language samples. Secondary outcomes included standardized assessments. Intention-to-treat analyses were used.
RESULTS:
Analyses focused on 41 children randomly assigned to TALI (n = 21) or TAU (n = 20). Among all participants, mean age was 6.3 years (SD 2.5). Over 24 weeks, children in the TALI group, compared with those in the TAU group, had significantly greater increases in the length of phrases they used to express themselves (β = .91 vs .15, respectively; P< .0001). Similar findings were seen with conversational turn-taking and number of different words spoken.
CONCLUSIONS:
Providing visual supports for language concepts that are typically challenging for DHH children to acquire allowed children to process and comprehend spoken language more fully. Such strategies can mitigate persistent language delays with the goal of improving lifelong outcomes and independence across settings.
Despite national efforts for early hearing loss identification and early intervention to improve language development,1–4 language deficits remain a pervasive problem for deaf or hard of hearing (DHH) children.3,5–13 Even with appropriate access to sound, DHH children do not have the same quality of auditory experience and do not perceive speech and acquire language in the same way as individuals with hearing.14,15 Research shows that ~40% of DHH children aged ≤6 years may have significant language gaps,16,17 which negatively affect social functioning and behavioral, academic, and employment outcomes.6,18–22 DHH adolescents have alarmingly high rates of low literacy and suboptimal educational attainment.23–25
Speech-language therapy is common for a DHH child and often initiated during infancy. In therapy, a speech-language pathologist (SLP) works directly with an infant and/or child, provides parent training for strategies, and fosters development of new skills to improve function.26 For DHH children, therapists frequently aim to improve speech and language skills. Even with substantial public health advances for DHH children, improvements in the development of language-specific interventions to support continued language development are necessary.27,28
Augmentative and alternative communication (AAC) is an evidence-based approach targeting core communication deficits in children with complex communication needs.29 Language interventions using AAC strategies have provided evidence for improving functional language growth30–34 and communication.35–38 AAC also increases speech production39,40 without interfering with the development of vocal or verbal communication.41 AAC strategies delivered via iPads positively impact spoken language outcomes for DHH children.42,43 Children participating in a small experimental study in which researchers leveraged AAC software had significant increases in spoken language measures and pragmatic skills.
Here, we report on a randomized controlled trial to examine the benefits of a therapy program, technology-assisted language intervention (TALI), which incorporates high-tech AAC strategies into speech-language therapy to improve expressive (spoken) language skills versus treatment as usual (TAU). Our primary hypothesis was that children receiving the TALI would make greater language gains, specifically syntax, semantics, and discourse, than in the TAU settings. Our intervention and hypotheses were informed by understanding the need for enhanced language development through augmented means,44,45 the importance of visual learning,46–48 and the role of graphic symbols in language development.49
METHODS
Participants
Participants were enrolled at a single tertiary pediatric institution from 2016 to 2019. Eligibility criteria included age 3 to 12 years, bilateral hearing loss (mild or worse), spoken English language as primary communication mode, and language delay or deficit (defined as language standard scores of 0.85 or less than the child’s nonverbal IQ (NVIQ) score or demonstrating deficits in spontaneous language skills compared with same-aged peers). Children with severe communication disorders (eg, autism spectrum disorder), significant motor impairments, or a NVIQ < 60 were excluded. Research coordinators obtained informed consent before participants completed eligibility and baseline assessments, which occurred before random assignment and intervention allocation. This trial was approved by the institution’s institutional review board and registered with ClinicalTrials.gov (NCT02998164).
Outcomes
The primary outcomes were language skills, specifically syntax, semantics, and discourse, analyzed from recorded language samples. Syntax was measured by the mean length of utterances in morphemes (MLUm), discourse by the child’s mean turn length (MTL) in words, and semantics by the number of different words (NDW) used in 50 consecutive and complete utterances.50 Secondary outcomes included receptive and expressive language standard scores taken from the Clinical Evaluation of Language Fundamentals, Fifth Edition51 (CELF-5) or the preschool edition.
Intervention Groups
After eligibility was determined, participants were randomly assigned to the TALI or TAU groups. Random assignment was done within 4 strata: age (3–6 and 6–12 years) and NVIQ (<100 and ≥100). A sealed envelope containing group assignment was opened after eligibility visit completion. See Supplemental Table 4 for an outline of general therapy components for both groups and supplemental material for in-depth descriptions.
TAU
TAU was defined as the therapy the child was currently receiving at the time of study enrollment. The TAU SLP, different from the TALI SLP, never delivered the TALI. During weekly, hour-long therapy sessions, the SLP targets language and communication skills (without AAC). Goals vary by child and can include development of awareness and discrimination of sounds and phonemes, segmentation of words, and understanding of words, phrases, and sentences in context (routines).
TALI
Details of the TALI have been published elsewhere.42,43 The SLP targets language and communication skills, leveraging AAC technology as a language-teaching tool. We incorporated evidence-based AAC strategies52 using the TouchChat HD - AAC with WordPower language program53 on iPads. The software company played no role in the study question, design, conduct, or analysis. The software is dynamic (grows in complexity with the child), provides visual support for abstract linguistic concepts, offers voice output for each selection, and provides a consistent model for verbalizations. The iPad was locked; the software was the only accessible application. The SLP uses AAC as a visual and audio tool to teach the child to construct longer and more complex messages. The child is encouraged to use the constructed message to verbalize the same message, actively self-monitor, and revise errors as needed. The TALI cycle included 6 SLP therapy weeks (hour-long, weekly sessions), 6 self-guided (at home) weeks, 6 SLP therapy weeks, and 6 self-guided weeks. All SLPs delivering either intervention were licensed and trained on the basis of national standards.
Baseline and Follow-up Visits
Figure 1 illustrates the assessment time line. Standardized assessments and parent-reported measures occurred at baseline (before random assignment) and 24 weeks (postintervention visit). Baseline nonverbal cognition was measured with the Leiter International Performance Scale, R,54 which provided a brief IQ. Parents completed a questionnaire regarding sex, race, school programs, intervention history, communication strategies, parental income, insurance status, and education. Audiograms and audiologic histories, including hearing-device use (hearing aids and cochlear implants), were reviewed from medical records. Language assessments were administered at baseline and 24 weeks. Language samples were taken at baseline and 12 and 24 weeks for all participants. After trial completion, parents in the TAU group could opt for their child to receive the TALI. At study completion, all children who completed the study received an iPad. Children completing the TALI kept the software on their iPads. We did not collect measures of parent engagement for either group.
FIGURE 1.
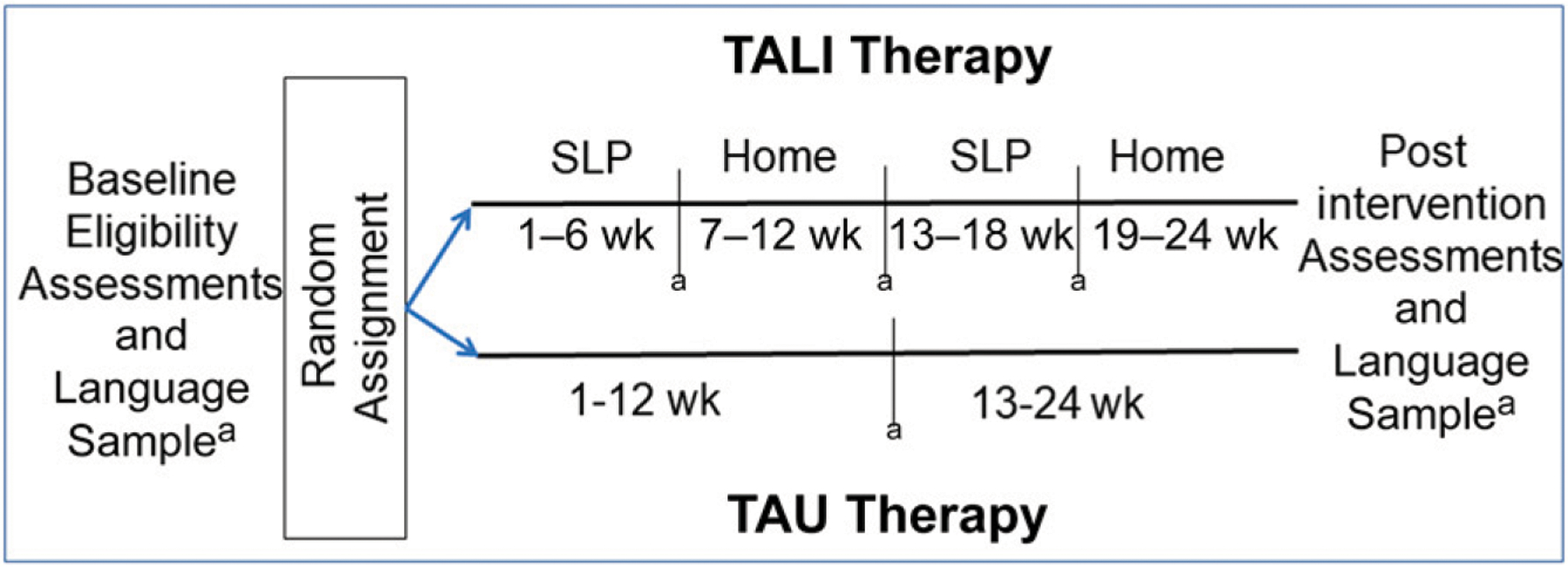
Study diagram of the follow-up of children randomly assigned to either the TALI or TAU therapy groups. a Time points at which language samples were obtained.
Language Sample Methods
Language samples were ~20 minutes in length, digitally audio- and video-recorded during a play- and/or conversation-based interaction with an SLP, and transcribed verbatim by someone blinded to group assignment. A second individual reviewed transcripts with recordings for accuracy. The iPad was not used during the language samples; all recordings were in the child’s own voice. Transcribed samples followed strict coding procedures compatible with the Systematic Analysis of Language Transcripts software.55 Variables elicited from samples included MLUm, MTL, and NDW spoken.
Sample Size and Statistical Analysis Methods
Sample size calculations were based on change in the primary outcomes over the 24-week intervention period. We hypothesized that children in the TALI group would have greater language gains in 24 weeks than children in the TAU group. On the basis of our preliminary pilot study findings,42 we estimated the need for 20 children per group to detect a 38% change in the MLUm between TALI and TAU using a two-group t test with a two-tailed α of .05% and 80% power, accounting for a possible 10% attrition rate.
Descriptive statistics were generated for each measured outcome. The distributions of these variables were examined for normality and potential outliers. Primary analysis was conducted with an intention-to-treat approach. The primary language outcomes over time (baseline and 12 and 24 weeks) were modeled as a function of intervention group assignment (TALI versus TAU) and investigated by using general linear models. Generalized estimating equations (GEEs) were used to account for the potential correlation inducted by the repeated-measures data. Three separate models were constructed for MLUm, MTL, and NDW by using a general linear model with an identity link function and exchangeable correlation matrix structure. An interaction term between group assignment and time was included in the model to test for a differential trajectory in the outcome between groups across time. Each model included the baseline outcome value as the only covariate. Least-square (LS) means were derived from the fitted models and graphically illustrated the trajectories for the TALI and TAU groups. To evaluate within-group change in receptive and expressive language standard scores preintervention to postintervention, the differences in scores were tested by using a paired t test for both the TALI and TAU groups separately. All analyses were conducted by using SAS version 9.4 (SAS Institute, Inc, Cary, NC).
RESULTS
Study Population
Sixty-one children were screened at an eligibility visit for language deficits; 42 were eligible and randomly assigned (Fig 2). Table 1 illustrates comparisons of eligible and noneligible children. Eligible children tended to be younger, non-Hispanic Black or African American, and used cochlear implants. Two randomly assigned children did not start the intervention, and a third child was deemed ineligible at the first intervention visit because of significant behavior issues. Table 2 includes characteristics of the TALI (n = 19) and TAU (n = 20) participants. Demographic characteristics were similar in both groups. Overall, the mean (SD) age of participants was 6.3 (2.5) years, 70% were white, 30% used a cochlear implant, and 48% of mothers had a college education. The mean (SD) NVIQ of the sample was 97 (18); the receptive and expressive language scores were 81 (15) and 78 (17.5), respectively.
FIGURE 2.
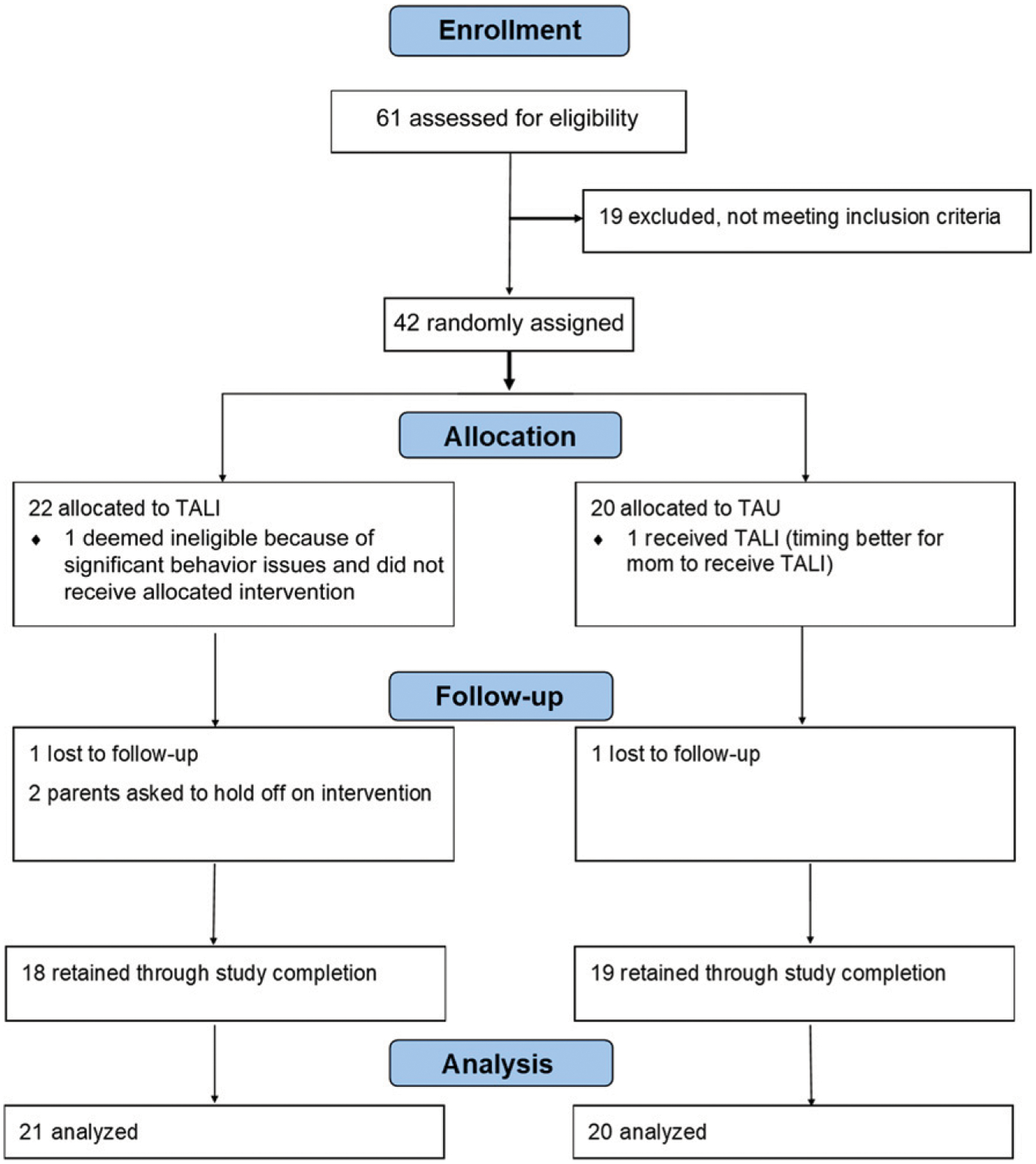
Consolidated Standards of Reporting Trials flowchart. Longitudinal analyses included all available data from each subject through lost to follow-up or study completion.
TABLE 1.
Demographic Characteristics Between DHH Children Who Were Eligible Compared and Children Who Were Ineligible for Study Participation
| Characteristics | Eligible (n = 41) | Ineligible (n = 19) | P |
|---|---|---|---|
| Age at visit, y, mean (SD) | 6.2 (2.5) | 9.1 (2.4) | <.0001 |
| Age of identification of hearing loss, mo, median (IQR) | 19 (2–48) | 49.5 (16–84) | .015a |
| Sex, n (%) | .30 | ||
| Girls | 20 (49) | 12 (63) | |
| Boys | 21 (51) | 7 (37) | |
| Race and/or ethnicity, n (%) | .045a | ||
| Non-Hispanic white | 29 (71) | 18 (95) | |
| Non-Hispanic Black or African American | 12 (29) | 1 (5) | |
| Health insurance, n (%) | .96 | ||
| Private only | 17 (41) | 8 (42) | |
| Public only or combined | 24 (59) | 11 (58) | |
| Maternal education level, n (%) | .65 | ||
| Less than college education | 22 (54) | 9 (47) | |
| College graduate or higher | 19 (46) | 10 (53) | |
| Household income <$20 000, n (%) | 11 (27) | 1 (5) | .08a |
| Use cochlear implants, n (%) | 12 (30) | 1 (5) | .045a |
| Use hearing aids, n (%) | 36 (88) | 17 (94) | .66a |
| NVIQ, mean (SD) | 97.2 (17.8) | 95.7 (16.7) | .76 |
IQR, interquartile range.
Fisher’s exact test or Wilcoxon rank test.
TABLE 2.
Demographic Characteristics of Participants
| Characteristics | TALI (n = 21) | TAU (n = 20) |
|---|---|---|
| Age at visit, y, mean (SD) | 6.0 (2.5) | 6.5 (2.5) |
| Age of identification of hearing loss, mo, median (IQR) | 35 (2–48) | 17 (2–37) |
| Sex, n (%) | ||
| Girls | 9 (43) | 11 (55) |
| Boys | 12 (57) | 9 (45) |
| Race and/or ethnicity, n (%) | ||
| Non-Hispanic white | 14 (74) | 13 (65) |
| Non-Hispanic Black or African American | 5 (26) | 7 (35) |
| Health insurance, n (%) | ||
| Private only | 8 (40) | 9 (45) |
| Public only or combined | 13 (62) | 11 (55) |
| Maternal education level, n (%) | ||
| Less than college education | 13 (62) | 9 (45) |
| College graduate or higher | 8 (38) | 11 (55) |
| Household income <$20 000, n (%) | 7 (33) | 4 (20) |
| Use cochlear implants, n (%) | 6 (29) | 6 (30) |
| Use hearing aids, n (%) | 18 (86) | 18 (90) |
| Unaided pure-tone average thresholds, median (IQR) | 56 (45–84) | 51 (43–55) |
| Aided thresholds,a median (IQR) | 20 (15–25) | 15 (12.5–20) |
| Reported receiving speech therapy in school, n (%) | 13 (62) | 15 (75) |
| NVIQ, mean (SD) | 96.9 (18.4) | 97.7 (17.6) |
| Baseline CELF receptive standard score, mean (SD) | 80.0 (15.2) | 82.1 (14.5) |
| Baseline CELF expressive standard score, mean (SD) | 77.6 (16.0) | 77.5 (19.6) |
Intervention assignment according to intention-to-treat. IQR, interquartile range.
Based on aided values of speech awareness and/or speech reception thresholds.
Primary Outcomes: MLUm, MTL, and NDW
Table 3 includes the GEE model results. Children in the TALI group made significantly greater progress regarding MLUm compared with children in the TAU group (β = .91 vs .15, respectively; P < .0001 for differences in slopes). Every 12 weeks, children in the TALI group increased their MLUm by 0.91, whereas TAU children increased their MLUm by 0.15. The mean MLUm (derived from the LS means of the GEE model) for TALI children increased from 4.23 at baseline to 6.06 at 24 weeks; the mean MLUm for TAU children increased from 4.23 at baseline to 4.49 at 24 weeks (Fig 3). Similar results were seen with MTL; TALI children made significantly more progress than TAU children over time (β = 1.21 vs .26, respectively; P = .005 for differences in slopes). MTL increased (baseline to 24 weeks) from 4.91 to 7.26 for TALI children and from 4.90 to 5.42 for TAU children (Fig 4). Finally, TALI children significantly increased their NDW spoken over time compared with TAU children (β = 11.04 vs 2.65, respectively; P = .007 for differences in slopes). Across 24 weeks, TALI children increased their NDW spoken from 82 to 104 words, whereas TAU children increased their NDW from 82 to 87 words (Fig 5). See Supplemental Table 5 for the LS means for each primary and secondary outcome.
TABLE 3.
Estimated Slopes, With SEs in Parentheses, Reported Indicating Change in Outcomes Occurring at Each 12-Week Interval
| TALI | TAU | P | |
|---|---|---|---|
| MLUm | 0.91 (0.12) | 0.15 (0.14) | <.0001 |
| MTL | 1.21 (0.24) | 0.26 (0.20) | .004 |
| NDW spokena | 11.04 (1.86) | 2.65 (2.45) | .007 |
P values represent test of differences in slopes (test of interaction) between TALI and TAU.
Occurring in 50 utterances.
FIGURE 3.
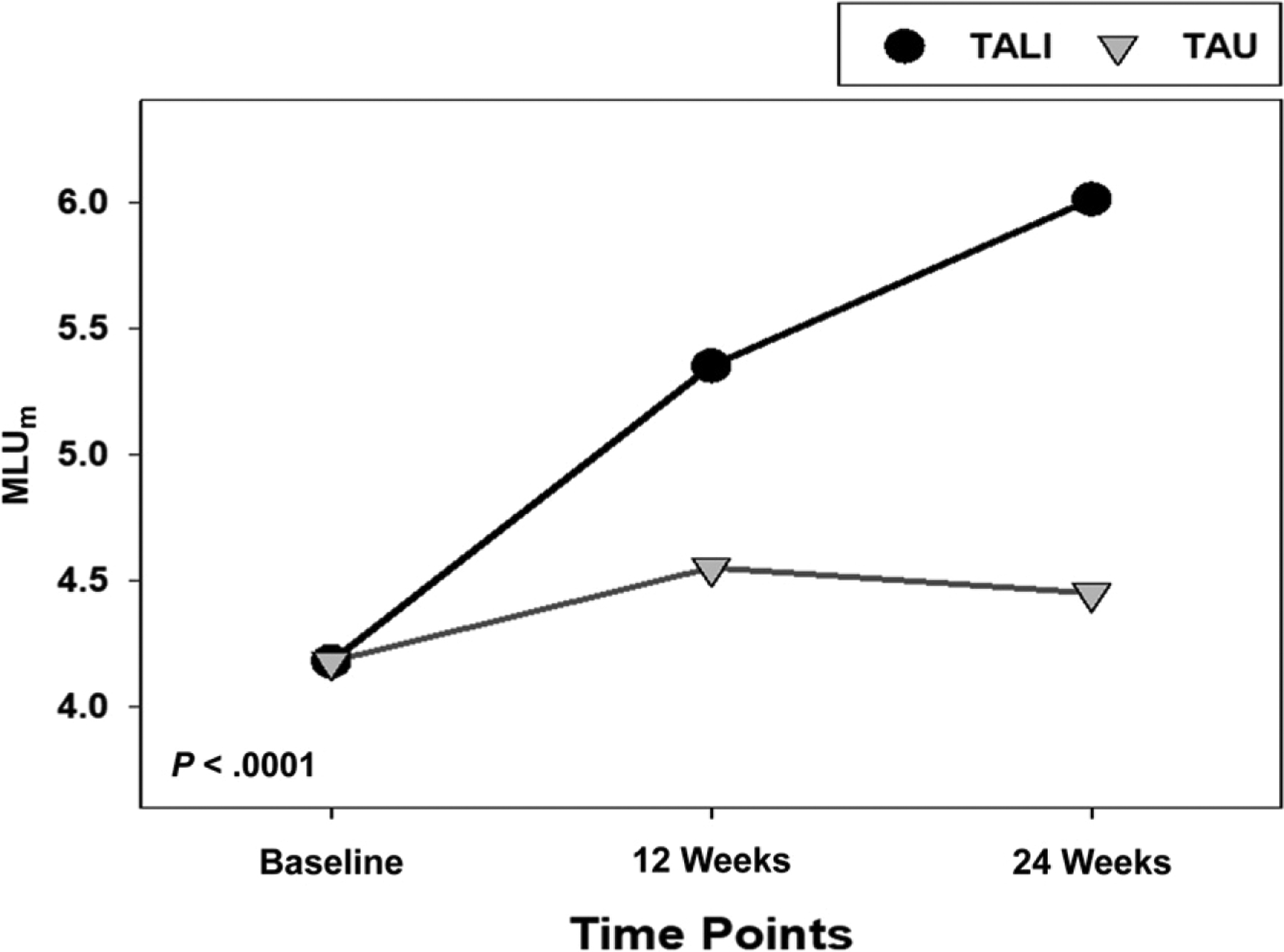
Change in MLUm over the study period for children randomly assigned to the TALI group and children randomly assigned to the TAU group. Group by time interaction was statistically significant in the model (P < .0001), indicating that the trajectories for the 2 groups were statistically different.
FIGURE 4.
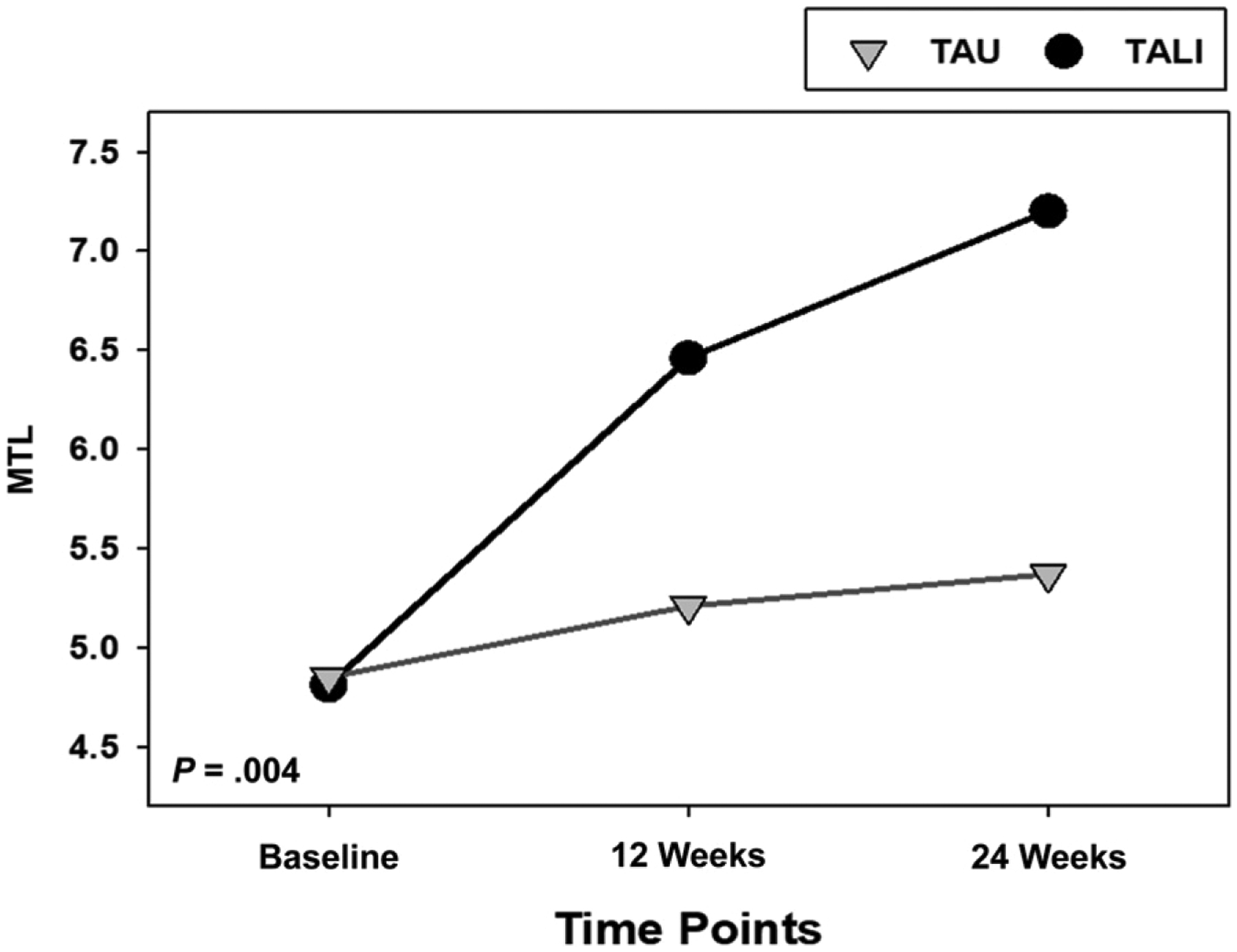
Change in MTL during the study period for children randomly assigned to the TALI and children randomly assigned to the TAU group. Group by time interaction was statistically significant in the model (P = .004), indicating that the trajectories for the 2 groups were statistically different.
FIGURE 5.
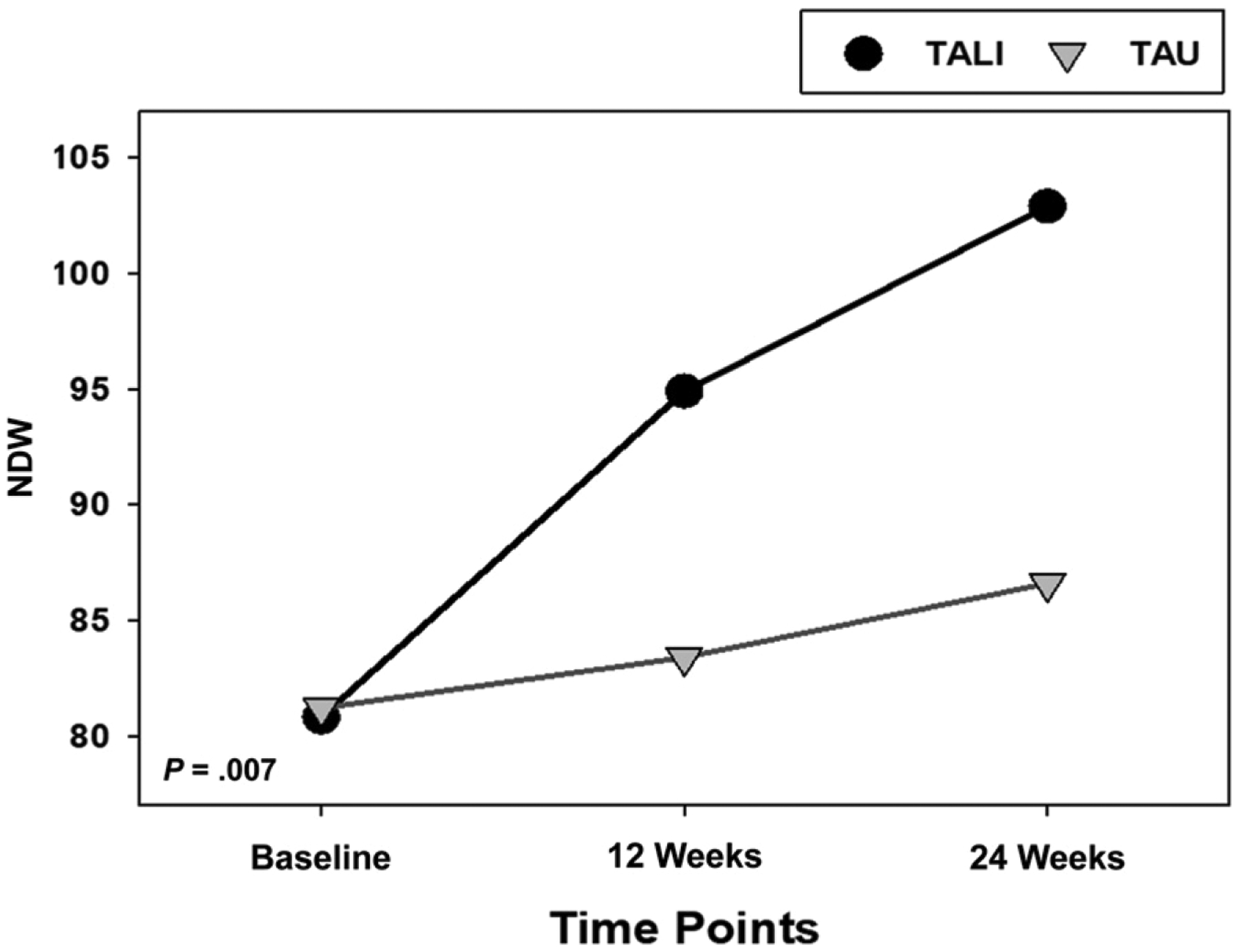
Change in NDW spoken in 50 utterances during study period for children randomly assigned to the TALI group and children randomly assigned to the TAU group. Group by time interaction was statistically significant in the model (P = .007), indicating that the trajectories for the 2 groups were statistically different.
Secondary Outcomes
At baseline, mean (SD) receptive scores were 80.0 (15.2) and 82.1 (14.5) for the TALI and TAU groups, respectively, whereas mean expressive scores were 77.6 (16.0) and 77.5, respectively (19.6). At 24 weeks, the mean receptive and expressive scores for children in the TALI group significantly increased to 90.6 (15.7) (P = .008) and 86.1 (15.8) (P = .01), respectively. The TAU group did not have significant improvements in mean receptive (83.6 [15.7]; P = .09) or expressive scores (79.9 [18.5]; P = .21).
DISCUSSION
This study is the first to our knowledge to show improvements in spoken language metrics and standard language scores among DHH children after incorporating AAC technology into speech-language therapy compared to a control (no change in current care). Changes in MLUm, MTL, and NDW were encouraging, particularly considering the time interval of the intervention and the impact on quality and depth of communication. Children in the TALI group increased MLUm by 43%, whereas children in the TAU group increased by only 6%. Increases in MTL and NDW spoken for children in the TALI group were 48% and 27%, respectively, whereas increases for children in the TAU group were 11% and 6%, respectively. Our current findings are consistent with a previous report on the TALI,42 as well as other studies in which AAC was shown to increase length of utterances, vocabulary, and grammatical development in young children, with moderate to large effect sizes.29,31,56
We obtained measures of naturalistic language from recorded language samples. Increases in the MLUm indicate increasing complexity of sentences and phrases (syntax and morphology). DHH children often struggle with word endings that can change the overall meaning of a sentence; thus, we measured MLU in morphemes (the smallest meaningful element of language). The increases seen in the MTL (the speaker’s mean length of conversational turn in words) indicate improvements in conversational turn-taking by holding, expanding on, and increasing involvement in the conversation. Expansion of the NDW used demonstrates an expanding vocabulary (syntax), enhancing the depth of communication. TALI participants also showed improvements in receptive and expressive language assessment scores (a secondary outcome), which indicate significant language growth within a relatively short time interval (24 weeks).
In our study, AAC technology was used as a language-teaching tool to enhance speech and language therapy; it offers stationary and spatially based visual supports and repeated listening opportunities for key aspects of verbal language that are often difficult for DHH children (ie, low-emphasis language constructs, word endings, verb tense, plurality, and possessives). To learn and produce spoken language, children require adequate access to spoken language models, traditionally relying on auditory input and vocal output channels, both of which are temporally based (ie, sequences in time) and dynamic (ie, a rapidly fading nature). TALI provides a consistent model for verbalizations, offers feedback for self-monitoring,57–59 uses visual and recognition memory, and leverages multisensory input (both auditory and visual input). Because the TALI promotes initiation and development of more advanced communication skills, children were empowered to be independent communicators, with increased ability to actively participate across settings. Significant structured involvement of families during therapy may have facilitated additional practice between therapy sessions. By providing access to consistent vocabulary, sentence structures, and repeated listening opportunities, AAC technology enabled DHH children to more fully access and process information,60–62 thus improving spoken language, comprehension, and pragmatic skills.
In addition to language outcomes, families reported qualitative improvements in their child’s communication skills in natural settings as a result of the TALI.63 Families noted some challenges in implementing the TALI in different settings, such as school. Some challenges with implementation, such as time spent in treatment, are universal for any therapeutic approach (time in treatment, travel, and fitting in practice at home). Increased understanding of these challenges will help improve adherence and outcomes for children and families.
The consequences of persistent language deficits among DHH children include social and academic struggles that often continue into adulthood.18–22 Unfortunately, we lack novel approaches to speech-language therapy for DHH children, making it difficult to improve this outcome for many. The significant boost in both spoken and receptive language our DHH children experienced as a result of the TALI could potentially help mitigate the social and academic struggles related to language deficits. At study entry, the average age of our participants was 6 years, yet the average MLUm was 4.23, aligning with the MLU of a 4 year-old child.64,65 This discrepancy indicates a significant gap in spoken language skills that could impact longer-term outcomes. By 24 weeks, MLUm increased to 6.06 for the TALI participants, on par with children aged 6 years.64,65 Although it is premature to know whether the TALI could prevent a language gap, we targeted children as young as age 3 years to engage children at risk as early as possible. We do not know whether children younger than age 3 years can meaningfully engage in TALI because it requires the cognitive skill of assigning linguistic meaning to graphic symbols. There may also be other unidentified high-risk populations for whom this approach could effectively promote improved language development.
Although we used a randomized design, which is a major strength of this work, this study had several limitations. Because of the targeted sample size, we were unable to conduct subgroup analyses to understand for whom the TALI may be most beneficial. We were also unable to fully appreciate the effectiveness of the TALI in younger versus older children nor were we able to investigate differences in intervention responders versus nonresponders. Children as young as 3 years successfully completed the intervention, indicating feasibility of implementing the TALI in young children. We did not capture parent and/or caregiver engagement level at home. It is possible that TALI parents demonstrated increased engagement because of the nature of the intervention, possibly impacting outcomes. If the TALI was successful in improving only engagement, which in turn improved outcomes at the levels we witnessed in our study, one could argue the intervention was still a success. Future research will incorporate measures of parental engagement. Logistically, it was difficult to consistently blind assessors to group membership at the postintervention CELF-5 assessment (a secondary outcome). All providers were experienced on administration and scoring rules. Because of high interrater reliability, different providers administering the CELF-5 should arrive at comparable scores for a child. From a clinical perspective, accuracy and consistency of the administration and scoring of standardized assessments relies on the SLP’s ability to administer these assessments in a standardized manner with every child. Additionally, research coordinators randomly observed evaluations to cross-check and confirm that assessments were provided in a standardized manner. We were not powered to address CELF score differences between groups. In our ongoing research, we will better incorporate this measure. We also did not collect details regarding the quality or intensity of the TAU therapies. Rates of school therapy were similar between groups, indicating that group differences in outcomes were likely not due to additional interventions. Finally, we were unable to examine the effectiveness of the TALI on sign-language development. Future work includes expansion to include more diverse populations of children across different settings (multiple study sites) with a larger sample size.
CONCLUSIONS
Our data reveal that speech and language therapy supplemented with AAC technology strategies is an effective treatment for improving spoken language outcomes in DHH children. The marked improvements in language skills witnessed in this study highlight that DHH children have the capacity to develop better communication skills than we have historically expected. With appropriate visual supports and language-teaching tools, as used in TALI, DHH children are capable of developing language skills more commensurate with their cognitive abilities and flourishing in previously challenging communicative situations. Effective language and communication skills are foundational for many areas of lifelong success; DHH children are in great need of evidence-based approaches that support robust language growth. Although our study findings require further exploration, they bring excitement to the potential for improved outcomes for DHH children.
Supplementary Material
WHAT’S KNOWN ON THIS SUBJECT:
Early identification of and intervention for hearing loss have led to improved language skills in children who are deaf or hard of hearing. Despite this progress, children continue to experience language underperformance that can negatively impact other developmental domains.
WHAT THIS STUDY ADDS:
This randomized clinical trial in deaf or hard of hearing children evaluates a novel approach to language learning. Findings reveal that adding assistive technology to traditional speech-language therapy closes gaps in spoken language.
FUNDING:
Funded by the National Institute on Disability, Independent Living, and Rehabilitation Research (90IF0122) and in part by the National Institute on Deafness and Other Communication Disorders (1R01DC018550) and the National Institutes of Health Clinical and Translational Science Award Program (2UL1TR001425-05A). The funders had no role in the design and conduct of the study. Funded by the National Institutes of Health (NIH).
ABBREVIATIONS
- AAC
augmentative and alternative communication
- CELF
Clinical Evaluation of Language Fundamentals
- DHH
deaf or hard of hearing
- GEE
generalized estimating equation
- LS
least-square
- MLUm
mean length of utterance in morphemes
- MTL
mean turn length
- NDW
number of different words
- NVIQ
nonverbal IQ
- SLP
speech-language pathologist
- TALI
technology-assisted language intervention
- TAU
treatment as usual
Footnotes
Deidentified individual participant data will not be made available.
This trial has been registered at www.clinicaltrials.gov (identifier NCT02998164).
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
COMPANION PAPER: A companion to this article can be found online at www.pediatrics.org/cgi/doi/10.1542/peds.2020-032508.
REFERENCES
- 1.Yoshinaga-Itano C Levels of evidence: universal newborn hearing screening (UNHS) and early hearing detection and intervention systems (EHDI). J Commun Disord. 2004;37(5):451–465 [DOI] [PubMed] [Google Scholar]
- 2.McCann DC, Worsfold S, Law CM, et al. Reading and communication skills after universal newborn screening for permanent childhood hearing impairment. Arch Dis Child. 2009;94(4): 293–297 [DOI] [PubMed] [Google Scholar]
- 3.Moeller MP. Early intervention and language development in children who are deaf and hard of hearing. Pediatrics. 2000;106(3). Available at: www.pediatrics.org/cgi/content/full/106/3/E43 [DOI] [PubMed] [Google Scholar]
- 4.Meinzen-Derr J, Wiley S, Choo DI. Impact of early intervention on expressive and receptive language development among young children with permanent hearing loss. Am Ann Deaf. 2011;155(5):580–591 [DOI] [PubMed] [Google Scholar]
- 5.Yoshinaga-Itano C Early Identification, Communication Modality, and the Development of Speech and Spoken Language Skills: Patterns and Considerations In: Spencer PE, Marschark MS, eds. Advances in the Spoken Language Development of Deaf and Hard-of-Hearing Children. New York, NY: Oxford University Press; 2006:298–327 [Google Scholar]
- 6.Meinzen-Derr J, Wiley S, Grether S, et al. Functional communication of children who are deaf or hard-of-hearing. J Dev Behav Pediatr. 2014;35(3):197–206 [DOI] [PubMed] [Google Scholar]
- 7.Meinzen-Derr J, Wiley S, Grether S, Choo DI. Children with cochlear implants and developmental disabilities: a language skills study with developmentally matched hearing peers. Res Dev Disabil. 2011;32(2):757–767 [DOI] [PubMed] [Google Scholar]
- 8.Stevenson J, McCann DC, Law CM, et al. The effect of early confirmation of hearing loss on the behaviour in middle childhood of children with bilateral hearing impairment. Dev Med Child Neurol. 2011;53(3):269–274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Holt RF, Beer J, Kronenberger WG, Pisoni DB, Lalonde K. Contribution of family environment to pediatric cochlear implant users’ speech and language outcomes: some preliminary findings. J Speech Lang Hear Res. 2012; 55(3):848–864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Meinzen-Derr J, Wiley S, Grether S, Choo DI. Functional performance among children with cochlear implants and additional disabilities. Cochlear Implants Int. 2013;14(4):181–189 [DOI] [PubMed] [Google Scholar]
- 11.Ching TY, Crowe K, Martin V, et al. Language development and everyday functioning of children with hearing loss assessed at 3 years of age. Int J Speech Lang Pathol. 2010;12(2):124–131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lund E, Schuele CM. Synchrony of maternal auditory and visual cues about unknown words to children with and without cochlear implants. Ear Hear. 2015;36(2):229–238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tomblin JB, Harrison M, Ambrose SE, Walker EA, Oleson JJ, Moeller MP. Language outcomes in young children with mild to severe hearing loss. Ear Hear. 2015;36(suppl 1):76S–91S [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harkins JE, Bakke M. Technologies for Communication: Status and Trends In: Marschark M, Spencer PE, eds. Oxford Handbook of Deaf Studies, Language, and Education, 2nd ed, vol. Vol. 1 New York, NY: Oxford University Press; 2011: 425–438 [Google Scholar]
- 15.Koehlinger KM, Van Horne AJ, Moeller MP. Grammatical outcomes of 3- and 6-year-old children who are hard of hearing. J Speech Lang Hear Res. 2013; 56(5):1701–1714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Meinzen-Derr J, Sheldon R, Grether S, et al. Language underperformance in young children who are deaf or hard-of-hearing: are the expectations too low? J Dev Behav Pediatr. 2018;39(2):116–125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yoshinaga-Itano C, Sedey AL, Wiggin M, Chung W. Early hearing detection and vocabulary of children with hearing loss. Pediatrics. 2017;140(2):e20162964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Calderon R, Greenberg M. Social and Emotional Development of Deaf Children: Family, School, and Program Effects In: Marschark M, Spencer PE, eds. Deaf Studies, Language, and Education, 2nd ed, vol. Vol. 1 New York, NY: Oxford University Press; 2011: 188–199 [Google Scholar]
- 19.Justice LM, Bowles RP, Pence Turnbull KL, Skibbe LE. School readiness among children with varying histories of language difficulties. Dev Psychol. 2009; 45(2):460–476 [DOI] [PubMed] [Google Scholar]
- 20.Antia SD, Jones PB, Reed S, Kreimeyer KH. Academic status and progress of deaf and hard-of-hearing students in general education classrooms. J Deaf Stud Deaf Educ. 2009;14(3):293–311 [DOI] [PubMed] [Google Scholar]
- 21.Beitchman JH, Wilson B, Brownlie EB, Walters H, Inglis A, Lancee W. Long-term consistency in speech/language profiles: II. Behavioral, emotional, and social outcomes. J Am Acad Child Adolesc Psychiatry. 1996;35(6):815–825 [DOI] [PubMed] [Google Scholar]
- 22.Beitchman JH, Wilson B, Brownlie EB, Walters H, Lancee W. Long-term consistency in speech/language profiles: I. Developmental and academic outcomes. J Am Acad Child Adolesc Psychiatry. 1996;35(6):804–814 [DOI] [PubMed] [Google Scholar]
- 23.Luckner JL, Sebald AM, Cooney J, Young J III, Muir SG. An examination of the evidence-based literacy research in deaf education. Am Ann Deaf. 2005;150(5):443–456 [DOI] [PubMed] [Google Scholar]
- 24.Traxler CB. The Stanford Achievement Test, 9th Edition: National Norming and Performance Standards for Deaf and Hard-of-Hearing Students. In: J Deaf Stud Deaf Educ, vol. 5 2000:337–348 [DOI] [PubMed] [Google Scholar]
- 25.Van Naarden Braun K, Yeargin-Allsopp M, Lollar D. A multi-dimensional approach to the transition of children with developmental disabilities into young adulthood: the acquisition of adult social roles. Disabil Rehabil. 2006; 28(15):915–928 [DOI] [PubMed] [Google Scholar]
- 26.American Speech-Language-Hearing Association. Roles and responsibilities of speech-language pathologists in early intervention: technical report. 2008. Available at: https://www.asha.org/policy/TR2008-00290/. Accessed May 1, 2017
- 27.Law J, Garrett Z, Nye C. Speech and language therapy interventions for children with primary speech and language delay or disorder. Cochrane Database Syst Rev. 2003;(3):CD004110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brennan-Jones CG, White J, Rush RW, Law J. Auditory-verbal therapy for promoting spoken language development in children with permanent hearing impairments. Cochrane Database Syst Rev. 2014;3(3): CD010100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Romski M, Sevcik RA, Adamson LB, et al. Randomized comparison of augmented and nonaugmented language interventions for toddlers with developmental delays and their parents. J Speech Lang Hear Res. 2010; 53(2):350–364 [DOI] [PubMed] [Google Scholar]
- 30.Schlosser RW, Wendt O. Effects of augmentative and alternative communication intervention on speech production in children with autism: a systematic review. Am J Speech Lang Pathol. 2008;17(3):212–230 [DOI] [PubMed] [Google Scholar]
- 31.Barker RM, Akaba S, Brady NC, Thiemann-Bourque K. Support for AAC use in preschool, and growth in language skills, for young children with developmental disabilities. Augment Altern Commun. 2013;29(4):334–346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Light J, Drager K. AAC technologies for young children with complex communication needs: state of the science and future research directions. Augment Altern Commun. 2007;23(3): 204–216 [DOI] [PubMed] [Google Scholar]
- 33.Lund SK, Light J. Long-term outcomes for individuals who use augmentative and alternative communication: part II-communicative interaction. Augment Altern Commun. 2007;23(1):1–15 [DOI] [PubMed] [Google Scholar]
- 34.Sevcik RA, Romski MA, Adamson LB. Research directions in augmentative and alternative communication for preschool children. Disabil Rehabil. 2004;26(21–22):1323–1329 [DOI] [PubMed] [Google Scholar]
- 35.Romski M, Sevcik RA, Barton-Hulsey A, Whitmore AS. Early intervention and AAC: what a difference 30 years makes. Augment Altern Commun. 2015;31(3): 181–202 [DOI] [PubMed] [Google Scholar]
- 36.McCarthy J, Light J, Drager K, et al. Re-designing scanning to reduce learning demands: the performance of typically developing 2-year-olds. Augment Altern Commun. 2006;22(4):269–283 [DOI] [PubMed] [Google Scholar]
- 37.Drager KD, Light JC, Speltz JC, Fallon KA, Jeffries LZ. The performance of typically developing 2 1/2-year-olds on dynamic display AAC technologies with different system layouts and language organizations. J Speech Lang Hear Res. 2003;46(2):298–312 [DOI] [PubMed] [Google Scholar]
- 38.Olin AR, Reichle J, Johnson L, Monn E. Examining dynamic visual scene displays: implications for arranging and teaching symbol selection. Am J Speech Lang Pathol. 2010;19(4):284–297 [DOI] [PubMed] [Google Scholar]
- 39.Millar DC, Light JC, Schlosser RW. The impact of augmentative and alternative communication intervention on the speech production of individuals with developmental disabilities: a research review. J Speech Lang Hear Res. 2006; 49(2):248–264 [DOI] [PubMed] [Google Scholar]
- 40.DeThorne LS, Johnson CJ, Walder L, Mahurin-Smith J. When “Simon says” doesn’t work: alternatives to imitation for facilitating early speech development. Am J Speech Lang Pathol. 2009;18(2):133–145 [DOI] [PubMed] [Google Scholar]
- 41.Cress CJ, Marvin CA. Common questions about AAC services in early intervention. Augment Altern Commun. 2003;19(4):254–272 [Google Scholar]
- 42.Meinzen-Derr J, Sheldon RM, Henry S, et al. Enhancing language in children who are deaf/hard-of-hearing using augmentative and alternative communication technology strategies. Int J Pediatr Otorhinolaryngol. 2019;125: 23–31 [DOI] [PubMed] [Google Scholar]
- 43.Meinzen-Derr J, Wiley S, McAuley R, Smith L, Grether S. Technology-assisted language intervention for children who are deaf or hard-of-hearing; a pilot study of augmentative and alternative communication for enhancing language development. Disabil Rehabil Assist Technol. 2017;12(8):808–815 [DOI] [PubMed] [Google Scholar]
- 44.Romski MA, Sevcik RA, Adamson LB. Framework for studying how children with developmental disabilities develop language through augmented means. Augment Altern Commun. 1997;13: 172–178 [Google Scholar]
- 45.Bedrosian JL. Framework for studying how children with developmental disabilities develop language through augmented means. Augment Altern Commun. 1997;13:179–185 [Google Scholar]
- 46.Stredler-Brown A Communication Choices and Outcomes during the Early Years: An Assessment and Evidence-Based Approach In: Marschark M, Spencer PE, eds Deaf Studies, Language, and Education, vol. Vol. 2 Oxford, NY: Oxford University Press, Inc; 2010:292–315 [Google Scholar]
- 47.Harris M Early Communication in Sign and Speech In: Marschark M, Spencer PE, eds Deaf Studies, Language, and Education, vol. Vol. 2 Oxford, NY: Oxford University Press, Inc; 2010:316–330 [Google Scholar]
- 48.Allen TE, Letteri A, Choi SH, Dang D. Early visual language exposure and emergent literacy in preschool deaf children: findings from a national longitudinal study. Am Ann Deaf. 2014; 159(4):346–358 [DOI] [PubMed] [Google Scholar]
- 49.Sevcik RA, Romski M, Wilkinson KM. Roles of graphic symbols in the language acquisition process for persons with severe cognitive disabilities. Augment Altern Commun. 1991;7:161–170 [Google Scholar]
- 50.Heilmann J, Nockerts A, Miller JF. Language sampling: does the length of the transcript matter? Lang Speech Hear Serv Sch. 2010;41(4):393–404 [DOI] [PubMed] [Google Scholar]
- 51.Wiig EH, Semel E, Seord WA. Clinical Evaluation of Language Fundamentals, 5th ed New York, NY: The Psychological Corporation; 2013 [Google Scholar]
- 52.Kent-Walsh J, Binger C. Fundamentals of the ImPAACT program. Perspect Augment Altern Commun. 2013;22:51–58 [Google Scholar]
- 53.Silver Kite. TouchChat HD - AAC with WordPower. Available at: http://touchchatapp.com/apps/touchchat-hd-aac-with-wordpower. Accessed June 14, 2014
- 54.Roid GH, Miller LJ, Pomplun M, Koch C. Leiter International Performance Scale, 3rd ed Wood Dale, IL: Stoelting; 2013 [Google Scholar]
- 55.Salt: Systematic Analysis of Language Transcripts [computer program]. Madison, WI: Salt Software, LLC; 2000 [Google Scholar]
- 56.Binger C, Light J. The effect of aided AAC modeling on the expression of multi-symbol messages by preschoolers who use AAC. Augment Altern Commun. 2007;23(1):30–43 [DOI] [PubMed] [Google Scholar]
- 57.Blischak D, Lombardino L, Dyson A. Use of speech-generating devices: in support of natural speech. Augment Altern Commun. 2003;19(1):29–35 [DOI] [PubMed] [Google Scholar]
- 58.Romski MA, Sevcik RA, Robinson BF, Mervis CB, Bertrand J. Mapping the meanings of novel visual symbols by youth with moderate or severe mental retardation. Am J Ment Retard. 1996; 100(4):391–402 [PubMed] [Google Scholar]
- 59.Smith M, Grove N. Asymmetry in Input and Output for Individuals Who Use AAC In: Light J, Beukelman D, Reichle J, eds Communicative Competence for Individuals Who Use Augmentative and Alternative Communication: From Research to Effective Practice. Baltimore, MD: Brooks Publishing; 2003: 163–195 [Google Scholar]
- 60.Doosti A, Jalalipour M, Ahmadi T, Hashemi SB, Haghjou S, Bakhshi E. Enhancing working memory capacity in Persian cochlear implanted children: a clinical trial study. Iran J Otorhinolaryngol. 2018;30(97):77–83 [PMC free article] [PubMed] [Google Scholar]
- 61.Mann VA, Liberman IY. Phonological awareness and verbal short-term memory. J Learn Disabil. 1984;17(10): 592–599 [DOI] [PubMed] [Google Scholar]
- 62.Nittrouer S, Caldwell-Tarr A, Lowenstein JH. Working memory in children with cochlear implants: problems are in storage, not processing. Int J Pediatr Otorhinolaryngol. 2013;77(11): 1886–1898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Grether S, Hunter LL, Gibler RC, et al. Social validity of technology assisted language intervention for deaf and hard-of-hearing children. J Early Hear Detect Interv. 2019;4(3):9–19 [Google Scholar]
- 64.Miller JF. Eliciting Procedures for Language In: Miller JF, ed Assessing Language Production in Children. London, United Kingdom: Edward Arnold; 1981 [Google Scholar]
- 65.Miller JF, Chapman RS. The relation between age and mean length of utterance in morphemes. J Speech Hear Res. 1981;24(2):154–161 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


