Abstract
Background:
Altered gut integrity is central to HIV-related immune activation. Opioids may promote similar changes in gut permeability and/or increase systemic inflammation potentially augmenting processes already occurring in people with HIV (PWH).
Setting:
Urban hospital systems in Cleveland, Ohio and surrounding communities.
Methods:
This is prospectively-enrolled, cross-sectional study including people with and without HIV using heroin, and people with and without HIV who have never used heroin matched by age, sex and CD4+ count (PWH only) to compare markers of gut integrity, microbial translocation, systemic inflammation, and immune activation.
Results:
100 participants enrolled. Active heroin use was associated with higher lipopolysaccharide binding protein (LBP), beta-D-glucan (BDG), high sensitivity C-reactive protein (hsCRP), soluble tumor necrosis factor-α receptors-I and –II, soluble CD163, inflammatory monocytes, and activated CD4+ lymphocytes in adjusted models. HIV status tended to modify the effect between heroin use and LBP, BDG, hsCRP, patrolling monocytes, and activated CD4+ lymphocytes (p<0.15 for interactions); however, not as expected. The effect of heroin on these markers (except patrolling monocytes) was greatest among those without HIV rather than those with HIV.
Conclusions:
Heroin use is associated with heightened microbial translocation, systemic inflammation, and immune activation. Concurrent HIV infection in virologically-suppressed individuals does not appear to substantially worsen effects heroin has on these markers.
Keywords: Heroin, HIV, Gut Integrity, Immune Activation, Systemic Inflammation
Introduction
People with HIV (PWH) whose mode of HIV acquisition was intravenous drug use are at higher risk of progression to AIDS, death due to AIDS, and all-cause mortality even when controlling for access to care, and antiretroviral therapy (ART) duration1–4. While high risk lifestyle or death from co-morbid conditions, such as bacterial infection or hepatitis C, certainly contribute, chronic immune activation may play an important role. In an observational study of people with a history of injecting drugs, an inflammatory index constructed from serum interleukin-6 (IL6) and soluble tumor necrosis factor-α receptor I (sTNF-RI) was associated with frailty and increased mortality in PWH and people without HIV who inject drugs5. Systemic inflammation associated with intravenous drug use is particularly relevant for PWH where chronic immune activation is already apparent and the added contribution of drug use is unclear.
It is plausible that HIV and heroin use together result in a synergistic effect on immune activation. Peripheral blood mononuclear cells (PBMCs) from healthy donors co-cultured with PBMCs from PWH in the presence of morphine have significantly greater p24 antigen release than PBMCs from controls or PMBCs in the presence of interleukin-2 which promotes HIV proliferation6. Heroin use is associated with lower gene expression and concentrations of antiviral restriction factors and type 1 interferon, in effect, limiting antiviral activity7. Morphine also downregulates β-chemokine production and upregulates CCR5 receptor expression resulting in enhanced R5-tropic HIV virus infection of macrophages that is not seen with X4 strains8. Last, altered gut integrity and resultant microbial translocation to the systemic circulation appears to be a central factor in HIV-related immune activation9,10; heroin use may further exacerbate this pathology11.
In this study, our aim was to evaluate associations between heroin use and gut integrity, microbial translocation, systemic and vascular inflammation, and immune activation and to understand how HIV infection modifies the effects of heroin on these factors. Our hypothesis was that heroin use would be associated with worse markers of gut integrity, microbial translocation, inflammation, and immune activation; and, the effects would be greatest in PWH.
Methods
Study Participants
The Impact of Heroin on Immune ACTIVATion in HIV study (or ACTIVATE) study is a prospective, observational cohort study designed to understand the effect of heroin use on innate and acquired immune activation and to assess the factors, such as gut integrity, that may mediate these associations in PWH who actively use heroin (HIV+ heroin+) and age-, sex- and CD4+ cell count-matched PWH who have never used heroin (HIV+ heroin-) in Cleveland, Ohio. People without HIV who actively use heroin (HIV- heroin+) and those who have never used heroin (HIV- heroin-) were enrolled for a single visit designed for cross-sectional analyses. Eligibility criteria included age ≥18 years, self-report of current injecting or snorting heroin for at least 1 month with cumulative use of at least 12 months in the past for the active heroin use groups, or no heroin use ever for groups that never use heroin. Participants with HIV were required to have HIV-1 RNA ≤400 copies/ml if on they were on ART. Presence of an inflammatory condition, active malignancy, infection in the past two weeks, pregnancy, uncontrolled diabetes, known cardiovascular disease, liver function tests greater than two and a half times the upper limit of normal, hemoglobin <9 g/dl, and creatinine clearance by Cockcroft-Gault <30 ml/min were exclusionary for all groups. Potential participants were recruited from the MetroHealth System (MHS), University Hospitals Cleveland Medical Center (UHCMC), and drug treatment facilities across Cleveland, Ohio and surrounding communities. All participants provided written informed consent. The study protocol and informed consent were approved by the MHS and UHCMC institutional review boards. The analysis presented herein was performed after the first 100 participants enrolled.
Study Evaluations
Demographics, medical and substance use history were obtained by self-report and a targeted physical exam, 8-hour fasting blood draw, and urine collection were performed. Plasma, urine and PBMCs were cryopreserved until thawed once and analyzed in batches.
Soluble Markers of Gut Integrity, Microbial Translocation, Inflammation and Monocyte Activation
Soluble markers of gut integrity (intestinal fatty acid binding protein or I-FABP), intestinal permeability (zonulin), bacterial translocation (LPS binding protein or LBP), fungal translocation (beta-D-glucan or BDG), systemic inflammation (high sensitivity C-reactive protein or hsCRP, IL6, sTNF-RI and -RII, and D-dimer], vascular inflammation (soluble vascular cell adhesion molecule-1 or sVCAM-1), and monocyte activation (soluble CD14 or sCD14 and soluble CD163 or sCD163) were quantified by ELISA as per manufacturers’ instructions (R&D Systems, Minneapolis, MN, USA, for all, except PromoCell GmbH, Heidelberg, Germany, for zonulin, Hycult Biotech Inc, Wayne, PA, USA, for LBP, MyBioSource, San Diego, CA, USA, for BDG, and Diagnostic Stago Inc, Parsippany, NJ, USA, for D-dimer).
Cellular Markers of Monocyte and T cell Activation
Cellular markers of immune activation were phenotyped from PBMCs by flow cytometry as previously described using a Miltenyi MACSQuant flow cytometer (Miltenyi Biotec, Bergisch Gladbach, Germany)12. Monocyte subsets including CD14+CD16+ (inflammatory) and CD14dimCD16+ (patrolling) were quantified as a percentage of the overall monocyte population. CD4+ and CD8+ lymphocytes expressing CD38 and HLA-DR (activated) were quantified as percentage of the overall CD4+ and CD8+ lymphocyte population, respectively.
Statistical Analysis
Demographics, clinical and HIV-related characteristics were compared by group using Kruskal-Wallis tests for continuous variables, and chi-square, Fisher’s exact, or Pearson exact chi-square tests for categorical variables, as appropriate. Outcomes including markers of gut integrity, microbial translocation, systemic and vascular inflammation, monocyte and T cell activation, were compared between groups in pairwise fashion. Comparisons planned a priori were between (1) HIV+, heroin+ and HIV+, heroin-; (2) HIV-, heroin+ and HIV-, heroin-; (3) HIV+, heroin+ and HIV-, heroin+. Unadjusted followed by adjusted pairwise comparisons of the least square means for each outcome variable were made using ANOVA (GLM procedure). Additional variables included were age, sex, race, trunk fat, smoking, and hepatitis C status. To evaluate for effect modification by HIV status, ANOVA models included heroin use status, HIV status and a heroin use-by-HIV status interaction term. A conservative p-value of <0.15 was considered a potentially important interaction effect. Last, markers were compared between heroin users with and without HIV after adjusting for route of heroin administration and intensity of heroin use, i.e. self-reported grams of heroin used per week and average number of days per week heroin used, separately. Outcome variables were transformed prior to analyses by using the natural logarithm. All analyses were performed using SAS, version 9.4 (Carey, North Carolina, USA). Statistical significance was defined by p <0.05 except where described above.
Results
Demographics and Clinical Characteristics
From July 2017 to August 2018, 100 participants were enrolled (19 HIV+ heroin+, 19 HIV+ heroin-, 38 HIV- heroin+, 24 HIV- heroin-). Overall, median (IQR) age was 42 (33–51) years and 75% were men. There were differences in race/ethnicity distribution among the groups (Table 1) with the majority of participants in each group being non-Hispanic white, except in the HIV+ heroin- group where most were non-Hispanic black. A high proportion of HIV+ heroin+ participants were Hispanic (37%) reflecting the demographics of heroin use among PWH in Cleveland, Ohio. BMI was lowest in the HIV+ heroin+ participants (p=0.02 among all groups). Participants using heroin were more likely to have chronic hepatitis C (56 vs 0%; p<0.0001), to be current smokers (98 vs 42%; p<0.0001), with a greater number of pack years (17 vs 6; p<0.01), and to currently use cocaine or amphetamines (49 vs 7%; p<0.0001, and 12 vs 0%; p=0.03, respectively) when compared to participants not using heroin. Current cannabis use among all participants was high, and similar between groups using heroin [53 vs 58% for HIV+ heroin+ vs HIV- heroin+ (p=0.71 between heroin+ groups), 73% for HIV+ heroin-, and 25% in HIV- heroin-; p=0.01 among all groups]. Among those who self-reported heroin use, 49% were positive for fentanyl, 35% for morphine, 18% for methadone, 16% for heroin metabolite, 5% oxycodone by urine toxicology. Multiple opioids were present in 39%. The distribution of opioids was similar between participants with and without HIV. More participants in the HIV+ heroin+ group reported using heroin exclusively through intranasal route than the HIV- heroin+ group (26 vs 0%; p<0.0001), but self-reported average grams of heroin used per week and number of days heroin used per week were similar (p=0.92 and 0.72, respectively).
Table 1.
Baseline Demographics and HIV-Related Characteristics by Group
| HIV+ heroin+ n=19 |
HIV+ Heroin− n=19 |
HIV− heroin+ n=38 |
HIV− heroin− n=24 |
p-value overall* |
p-value HIV+ vs HIV−* |
p-value heroin+ vs heroin−* |
|
|---|---|---|---|---|---|---|---|
| Age, years | 47 (32.9, 54.9) |
46.5 (32.4, 53.8) |
37.5 (34.1, 50.5) |
44.3 (32.6, 52.3) |
0.61 | 0.28 | 0.56 |
|
| |||||||
| Male | 14 (74) | 15 (79) | 27 (71) | 19 (79) | 0.88 | 0.81 | 0.41 |
|
| |||||||
| Race/ethnicity | <0.0001 | <0.001 | <0.001 | ||||
| White, not Hispanic | 10 (53) | 2 (11) | 26 (68) | 17 (71) | |||
| Black, not Hispanic | 2 (11) | 15 (79) | 5 (13) | 5 (21) | |||
| Asian, not Hispanic | 0 (0) | 1 (5) | 2 (5) | 1 (4) | |||
| Hispanic | 7 (37) | 1 (5) | 5 (13) | 1 (4) | |||
|
| |||||||
| Current smoker | 19 (100) | 11 (58) | 37 (97) | 7 (29) | <0.0001 | 0.38 | <0.0001 |
|
| |||||||
| BMI, kg/m2 | 23.6 (21.6, 25.2) |
26 (23.5, 29.8) |
25.8 (22.9, 28.3) |
26.6 (22.9, 29.7) |
0.02 | 0.12 | 0.06 |
| Trunk fat, g | 6839 (5561, 9452) |
11576 (8460, 15969) |
9126 (6632, 14819) |
12136 (7233, 14623) |
<0.01 | 0.17 | <0.01 |
|
| |||||||
| Hepatitis C | 11 (58) | 0 (0) | 21 (55) | 0 (0) | <0.0001 | 0.61 | <0.0001 |
|
| |||||||
| HIV duration, years | 11.8 (2.3, 18.9) |
13.2 (8.1, 16.7) |
- | - | - | - | 0.82 |
|
| |||||||
| ART duration, years | 4.5 (1.8, 9.4) |
8.7 (6.8, 13.8) |
- | - | - | - | 0.02 |
| On ISTI | 10 (53) | 13 (68) | - | - | - | - | 0.32 |
| On PI | 6 (32) | 3 (16) | - | - | - | - | 0.25 |
| On NNRTI | 1 (5) | 7 (37) | - | - | - | - | 0.02 |
|
| |||||||
| CD4+, cells/mm3 | 562 (276, 799) |
767 (623, 1035) |
- | - | - | - | 0.02 |
|
| |||||||
| Nadir CD4+, cells/mm3 | 201 (42, 301) |
212 (110, 280) |
- | - | - | - | 0.83 |
|
| |||||||
| HIV-1 RNA <200 cps/ml | 16 (84) | 19 (100) | - | - | - | - | 0.07 |
|
| |||||||
| Heroin route | - | <0.0001 | - | ||||
| Intravenous | 14 (74) | - | 38 (100) | - | |||
| Intranasal | 5 (26) | - | 0 (0) | - | |||
|
| |||||||
| Amount heroin per week, grams | 7 (2, 7) |
6 (3.5, 7) |
0.92 | ||||
|
| |||||||
| Current substance use | |||||||
| Cannabis | 10 (53) | 14 (73) | 22 (58) | 6 (25) | 0.01 | 0.08 | 0.34 |
| Cocaine | 9 (47) | 1 (5) | 19 (50) | 2 (8) | <0.001 | 0.43 | <0.0001 |
| Methamphetamine | 3 (16) | 0 (0) | 4 (11) | 0 (0) | 0.16 | >0.99 | 0.04 |
Values shown are median (interquartile range) and frequency (column percent)
Kruskal-Wallis or Pearson exact chi-square tests for comparisons of more than two groups, Wilcoxon rank sum or chi-square tests for comparison between two groups
BMI, body mass index; ART, antiretroviral therapy; ISTI, integrase strand transfer inhibitor; PI, protease inhibitor; NNRTI, non-nucleoside reverse transcriptase inhibitor
In participants with HIV, median (IQR) known duration of HIV was 13 (8–18) years. Those using heroin had shorter ART duration [4 (2–9) vs 9 (7–14) years, p=0.02] and lower current, but similar nadir CD4+ cell counts [562 (276–799) vs 767 (623–1,035) cells/mm3; p=0.02, and 201 (42–301) vs 212 (110–280) cells/mm3; p=0.82, respectively]. All but two participants were on ART, and all participants on ART had HIV-1 RNA < 400 copies/ml.
Gut Integrity and Microbial Translocation Markers
Figure 1 shows the adjusted least square means for each outcome by group. Concentrations of I-FABP were similar among groups (p=0.21), and neither heroin use or HIV were independently associated with I-FABP in unadjusted analyses. However, with adjustment there was some evidence that among participants without HIV, I-FABP concentration was higher in those who use heroin (HIV- heroin+ vs HIV- heroin-; p=0.06). HIV status, but not heroin use, was independently associated with zonulin (p=0.02), and there was some evidence that among heroin users, those with HIV had higher zonulin in adjusted models (HIV+ heroin+ vs HIV- heroin+; p=0.07). When adjusting for route of heroin use, among participants who use heroin, those with HIV had higher zonulin concentrations than participants without HIV (p=0.04). HIV status did not modify the effect of heroin on IFAB or zonulin.
Figure 1. Gut Integrity and Microbial Translocation Markers by Group.
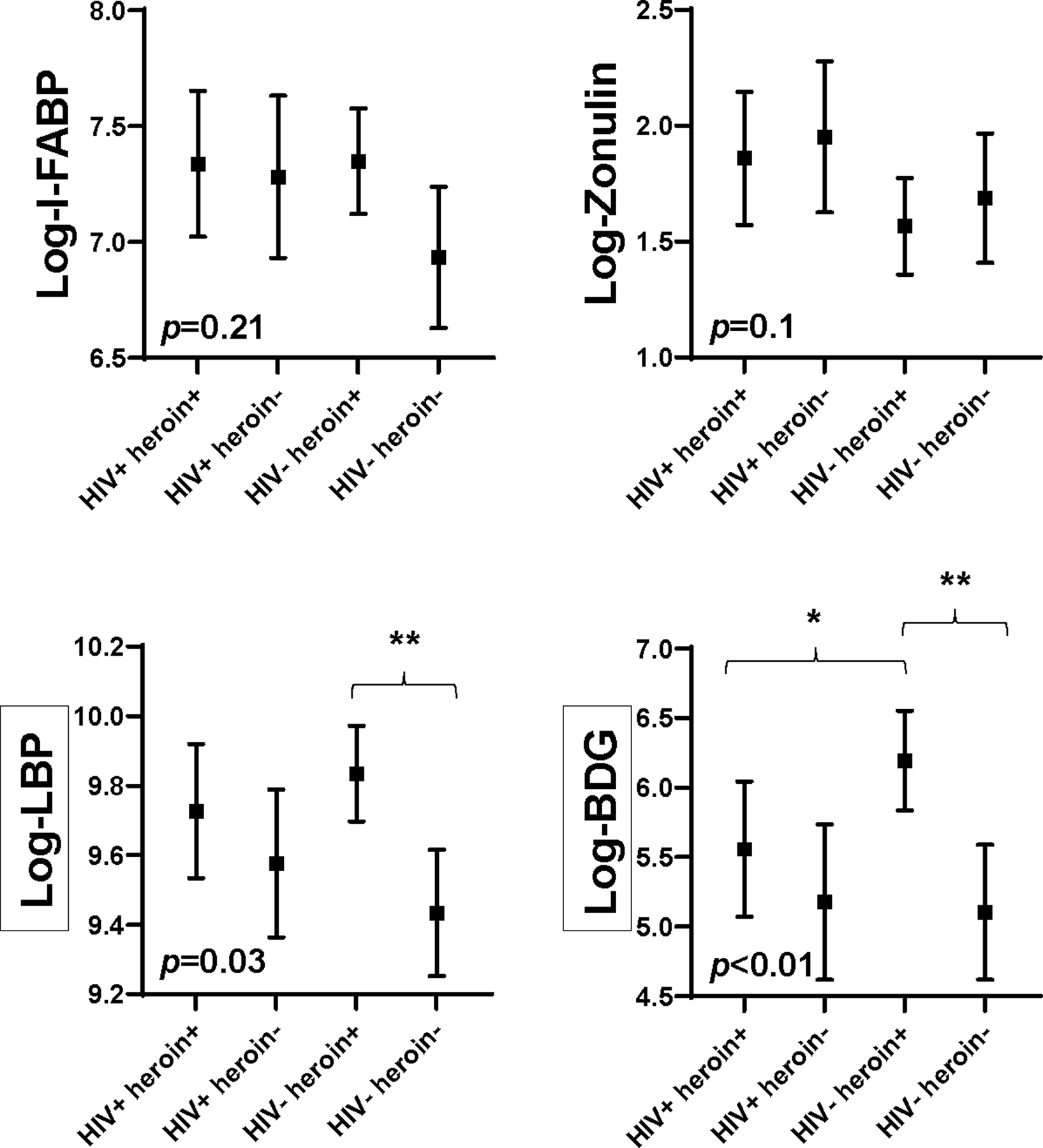
Symbols represent adjusted least squares means for each marker by group. Means are adjusted for age, sex, race, trunk fat, smoking, and hepatitis c status. Error bars show 95% confidence interval around means. p-value < 0.05 indicates there are differences between the means among groups. ** denotes p < 0.01 between groups; * denotes p < 0.05 between groups. Black boxes surrounding a y axis variable indicate there is effect modification by HIV status for this marker, i.e. p < 0.15 for heroin use-by-HIV status interaction term.
I-FABP, intestinal fatty acid binding protein; LBP, lipopolysaccharide binding protein; BDG, beta-D-glucan
Heroin use was independently associated with higher concentrations of LBP and BDG (p<0.01 and p=0.01 in the fully adjusted models, respectively); and, these effects were modified by HIV status (p=0.07 and p=0.10 for heroin use-by-HIV status interactions, respectively). Concentrations of LBP and BDG were higher in heroin users than non-users among those without HIV in adjusted models (HIV- heroin+ vs HIV- heroin-; p<0.01 for both), while concentrations were more similar between heroin users and non-users among those with HIV (HIV+ heroin+ vs HIV+ heroin-; p=0.36 and p=0.38, respectively). Interestingly, BDG was higher in heroin users without HIV than in heroin users with HIV (HIV+ heroin+ vs HIV- heroin+; p=0.02). The results described above were similar after excluding three participants on antibiotics (two HIV+ heroin+ participants on cephalexin and on doxycycline, respectively, and one HIV- heroin- participant on penicillin); there were no participants on antifungal medications. Further, adjusting for route of heroin use and intensity of use did not change the results.
Systemic and Vascular Inflammation Markers
Heroin use was independently associated with higher hsCRP (p=0.01), sTNF-RI (p<0.01), sTNF-RII (p<0.001), and D-dimer (p<0.01) in adjusted models. Associations between heroin use and IL6 and sVCAM-1 attenuated with adjustment (p=0.29 and 0.57, respectively). HIV status was not independently associated with inflammation marker concentrations. In fact, all inflammation markers were similar among those using heroin, regardless of HIV status (HIV+ heroin+ vs HIV- heroin-). HIV status did modify the effect between heroin use and hsCRP (p=0.09 for heroin use-by-HIV status interaction). Concentrations of hsCRP were higher in heroin users than non-users among those without HIV (HIV- heroin+ vs HIV- heroin-; p<0.01 in adjusted model), whereas differences among participants with HIV were smaller and did not meet statistical significance (HIV+ heroin+ vs HIV+ heroin-; p=0.34). See Figure 2.
Figure 2. Systemic and Vascular Inflammation Markers by Group.
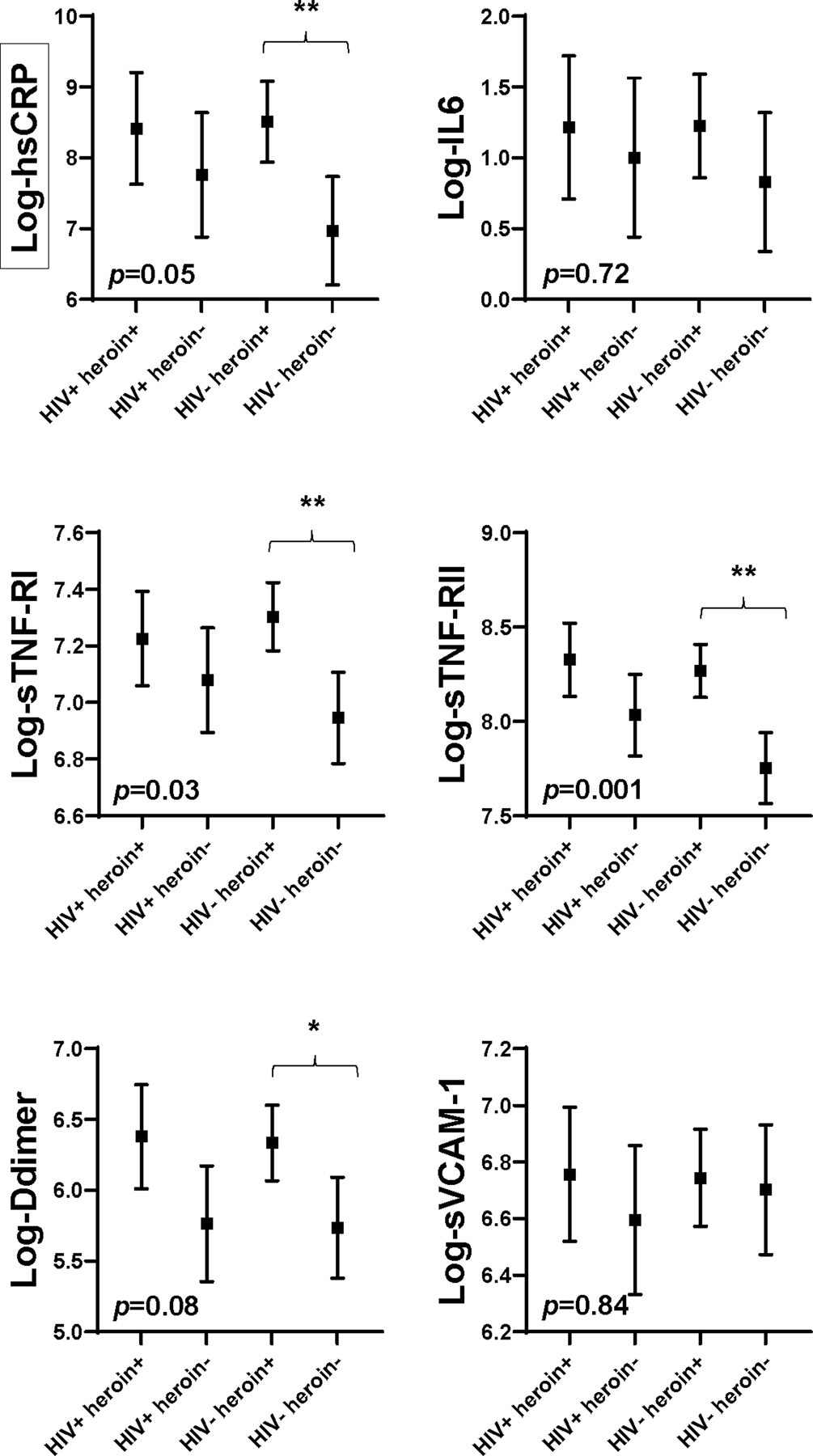
Symbols represent adjusted least squares means for each marker by group. Means are adjusted for age, sex, race, trunk fat, smoking, and hepatitis c status. Error bars show 95% confidence interval around means. p-value < 0.05 indicates there are differences between the means among groups. ** denotes p < 0.01 between groups; * denotes p < 0.05 between groups. Black boxes surrounding a y axis variable indicate there is effect modification by HIV status for this marker, i.e. p < 0.15 for heroin use-by-HIV status interaction term.
hsCRP, high sensitivity C-reactive protein; IL6, interleukin 6; sTNF-RI and –RII, soluble tumor necrosis factor α receptor-I and receptor-II; sVCAM-1, soluble vascular cell adhesion molecule-1
Monocyte and T Lymphocyte Activation
Heroin use was independently associated with higher sCD163 (p=0.04 in adjusted model) and there was some evidence of association with higher sCD14 (p=0.05). Additionally, heroin use was independently associated with higher proportion of inflammatory (CD14+CD16+) monocytes (p<0.05) and there was some evidence of association with lower proportion of patrolling (CD14+CD16dim) monocytes (p=0.09). HIV infection was only associated with higher sCD163 (p=0.02). HIV status modified the effect of heroin use on proportion of patrolling monocytes (p=0.13 for heroin use-by-HIV status interaction). Proportion of patrolling monocytes were lower in heroin users than in non-users among those with HIV (p<0.05 in adjusted model), whereas proportions were more similar among those without HIV (p=0.32). See Figure 3.
Figure 3. Soluble and Cellular Markers of Monocyte and T cell Activation by Group.
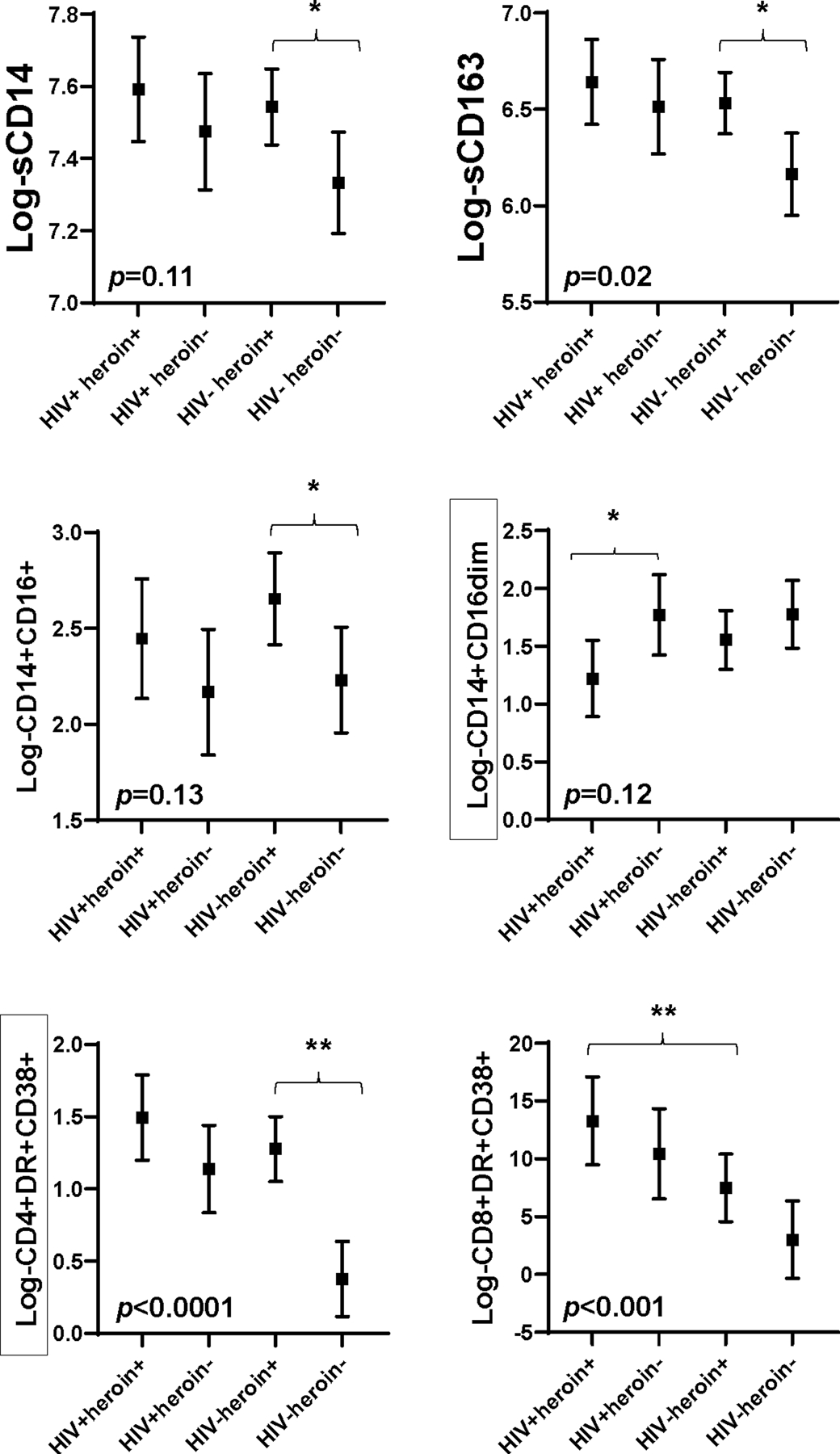
Symbols represent adjusted least squares means for each marker by group. Means are adjusted for age, sex, race, trunk fat, smoking, and hepatitis c status. Error bars show 95% confidence interval around means. p-value < 0.05 indicates there are differences between the means among groups. ** denotes p < 0.01 between groups; * denotes p < 0.05 between groups. Black boxes surrounding a y axis variable indicate there is effect modification by HIV status for this marker, i.e. p < 0.15 for heroin use-by-HIV status interaction term.
sCD14, soluble CD14; sCD163, soluble CD163
Both heroin use and HIV infection were independently associated with heightened CD4+ (p<0.001 for both) and CD8+ (p=0.09 and <0.0001, respectively) T cell activation. HIV status modified the effect of heroin use on CD4+ T cell activation (p=0.12 for heroin use-by-HIV status interaction). The difference in CD4+ T cell activation between heroin users and non-users was significant and much greater among those without HIV (HIV- heroin+ vs HIV- heroin-; p<0.0001 in adjusted model) than among those with HIV (HIV+ heroin+ vs HIV+ heroin-; p=0.14). CD8+ T cell activation was higher in participants with HIV than without HIV among heroin users (HIV+ heroin+ vs HIV- heroin+; p<0.01). For CD4+ and CD8+ T cell activation, adjusting for current CD4+ T cell count did not change the results among participants with HIV.
Discussion
In this study of 100 participants with and without HIV who use and do not use heroin, we have shown that heroin use is independently associated with higher microbial translocation (LBP and BDG), systemic inflammation (hsCRP, sTNF-RI, sTNF-RII and D-dimer), monocyte activation (sCD163 and proportion of inflammatory monocytes) and CD4+ T cell activation; HIV infection is independently associated with higher gut permeability (zonulin), monocyte activation (sCD163), CD4+ and CD8+ T cell activation; and, HIV status modifies the effect of heroin on concentrations of microbial translocation markers (LBP and BDG), hsCRP, proportion of patrolling monocytes and CD4+ T cell activation. Counter to our hypothesis that heroin use would worsen these markers to a greater degree in people with HIV, differences in these markers between heroin and non-heroin users were greatest in those without HIV for all markers except in proportion of patrolling monocytes (Figure 4).
Figure 4. Mean Difference Between Groups for Soluble Markers of Gut Integrity, Microbial Translocation, Systemic and Vascular Inflammation and Monocyte Activation.
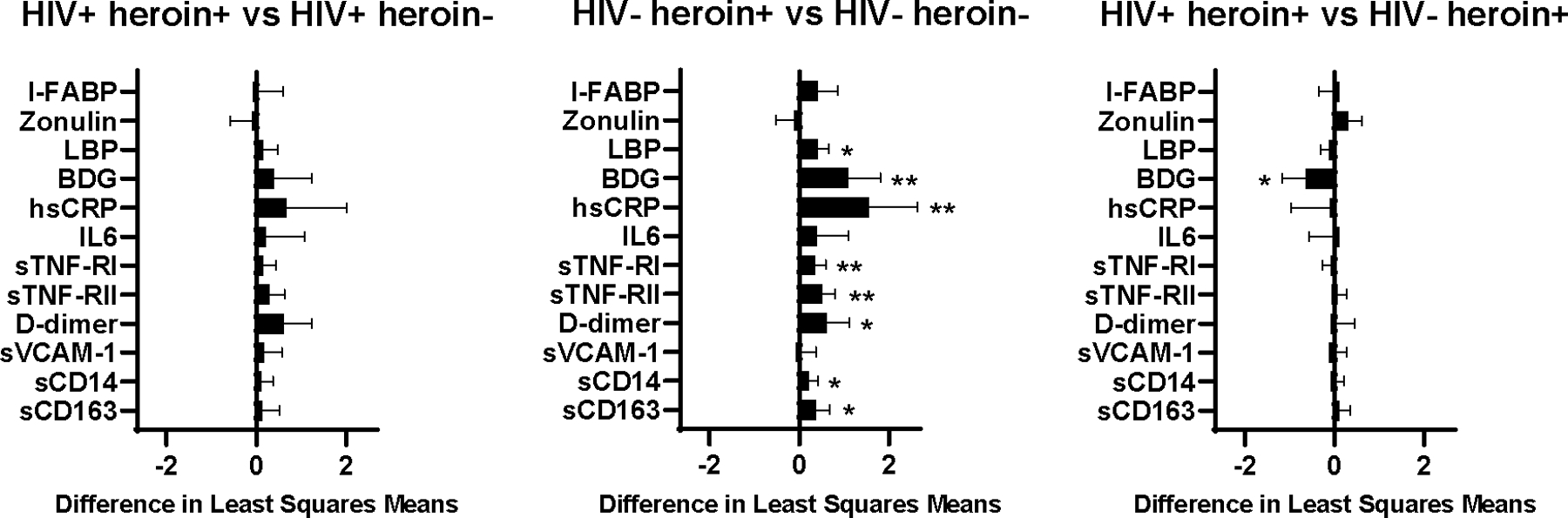
Bars represent difference in adjusted least square means between groups. Means are adjusted for age, sex, race, trunk fat, smoking, and hepatitis c status. Error bars show 95% confidence interval around difference in means. ** denotes p < 0.01; * denotes p < 0.05. As an example, in the first graph, values to the right of zero indicate marker values are higher in the HIV+ heroin+ group compared to the HIV+ heroin- group.
Importantly, heightened concentrations of both bacterial and fungal translocation markers were associated with heroin use in this study. In a cross-sectional study (N=119), circulating LPS was higher in PWH who use intravenous drugs compared to people who do not11. In that study, despite lower HIV-1 RNA levels and higher CD4+ cell counts, those who used intravenous heroin, but not intravenous cocaine, had higher plasma LPS compared to those without substance use. Our study extends these results as higher BDG was also associated with heroin use which has high significance given this fungal translocation marker has links to HIV-associated immune activation and downstream metabolic effects13–18. Interestingly, in this study, while there was some evidence that HIV infection was associated with higher zonulin, having HIV did not appear to substantially worsen either gut integrity or microbial translocation markers among participants using heroin. It is possible that greater differences were not apparent because the majority of participants with HIV in this study were on ART and virologically-suppressed. The chronic immune activation that characterizes HIV infection is driven in large part by the depletion of intestinal CD4+ T cells leading to altered gut integrity and microbial translocation. While not to pre-infection levels, ART initiation can improve gastrointestinal-associated lymphoid tissue function especially if ART is initiated early19,20. Also, we are unaware of the additives in the heroin preparations used by participants. Additives, such as cellulose, may have resulted in higher concentrations of BDG in plasma. While we did further adjust models for how heroin was used (injection vs intranasal) and results were unchanged, we cannot exclude this as a possible explanation for why BDG concentrations were higher in heroin users without HIV compared to those with HIV.
Often aligned with heightened microbial translocation, markers of monocyte activation, sCD14 and sCD163 and the proportion of inflammatory monocytes, were also associated with heroin use in adjusted analyses. In a matched, cross-sectional study (N=50) of viremic PWH and people without HIV who inject drugs and viremic PWH and people without HIV who never injected drugs, sCD14 concentrations were highest in PWH regardless of injection drug use21. In our study, differences in soluble measures of monocyte activation were not significantly different among people who use heroin with and without HIV possibly because the majority of PWH were virologically-suppressed on ART. Our results extend the literature by showing a heightened proportion of inflammatory monocytes similar among people who use heroin regardless of HIV status, but lower proportion of patrolling monocytes that were lowest in PWH who use heroin. This is of particular relevance to PWH who are at heightened risk of cardiovascular disease22 as patrolling monocytes function to remove damaged cells and debris from vasculature promoting resolution of inflammation23. In the above study by Mehandru et al, CD4+ T cells were depleted in peripheral blood and colonic tissue and CD8+ T cells were increased in peripheral blood and colonic tissue without regard for injection drug use in viremic PWH21. Both CD4+ and CD8+ activation were significantly increased in people who inject drugs regardless of HIV status although the magnitude of increase in T-cell activation was greater in PWH who inject drugs. In our study, CD8+ T cell activation was highest in the heroin users with HIV. However, heightened CD4+ T cell activation in heroin users was independent of HIV status.
Last, heroin use was associated with heightened systemic inflammation independent of HIV infection. It is clear that injection drug use leads to an increase in systemic inflammation24,25 possibly through direct injection-related injury or infection26,27, type of heroin injected28,29, filler agents, injection practices such as reusing cotton filters30,31, other high risk behaviors32,33, or environmental factors such as low individual and community socioeconomic status34. From the Study to Assess Hepatitis C Risk (N=541), nearly half of people who inject drugs reported ever having an abscess35. Importantly, participants had greater number of injection partners, were more likely to inject daily, and to share cookers, and less likely to use new syringes with each injection. In another survey of people who inject heroin (N=145), two-thirds reported having at least one abscess ever and 20% reported having >2 abscesses per year36. In this study, 39% waited at least two weeks to seek care. It follows that injection drug use likely contributes to at least intermittent increases in systemic inflammation chronically. In our study, participants in the heroin use groups did not have active abscesses despite having higher levels of systemic inflammation, although we cannot rule out that prior or intermittent skin and soft tissue infections could have contributed to the heightened inflammatory response seen in these groups.
As with any cross sectional evaluation, causality cannot be determined. Longitudinal follow-up for the ACTIVATE study is currently underway. Additionally, while LBP and BDG are established markers of microbial translocation, it is possible that concentrations of these markers were elevated in this study population due to injection practices rather than altered gut integrity. Future study utilizing colonic tissue is needed. Further limitations of this study include inadequate power to detect all possible interactions or to dissect the effect of different opioids on the markers assessed. Further, it is possible that differences among the groups with HIV (HIV+heroin+ and HIV+heroin-) may not have met significance due to small sample size.
Conclusions
Heroin use is associated with heightened microbial translocation, systemic inflammation, monocyte and T cell activation and this is independent of HIV status. Participants with HIV who did not use heroin demonstrated heightened measures of nearly all markers tested when compared to those without HIV demonstrating that HIV infection results in disruption of gut integrity, microbial translocation, systemic inflammation and immune activation. This likely explains why differences in markers assessed among heroin users and non-users with HIV were smaller than differences between heroin users and non-users without HIV. Indeed, HIV infection did not appear to substantially worsen the multiple effects that heroin has on microbial translocation, systemic inflammation and immune activation. Future studies should assess the effects of heroin in the context of HIV infection over time and potential reversal of these effects with cessation of heroin with and without medication assisted treatment for opioid use disorder.
Acknowledgements
Source of funding. This study is funded by the National Institutes of Drug Abuse R01DA044576 to COH and GAM and the Clinical and Translational Science Collaborative of Cleveland (UL1TR002548) from the National Center for Advancing Translational Sciences component of the NIH and NIH roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Footnotes
Disclaimer: Preliminary results were presented at the Conference on Retroviruses and Opportunistic Infections, held virtually from Boston, MA, March 7–10, 2020.
Potential conflicts of interest. COH has served as consultant for Theratechnologies and Gilead and has received research grant support from Gilead. NF has served as consultant for Gilead. GAM has served as consultant for Gilead, Merck, Theratechnologies, Jannsen, GSK/ViiV, and has received research grants from Roche, Genentech, Vanda, Astellas, Tetraphase, Gilead, Merck, and ViiV. All other authors have no conflicts.
Contributor Information
Corrilynn O. Hileman, Department of Medicine, Division of Infectious Disease, MetroHealth Medical Center and Case Western Reserve University School of Medicine, Cleveland, Ohio, USA.
Emily R. Bowman, School of Health and Rehabilitation Sciences, Division of Medical Laboratory Science, The Ohio State University, Columbus, Ohio, USA.
Janelle Gabriel, School of Health and Rehabilitation Sciences, Division of Medical Laboratory Science, The Ohio State University, Columbus, Ohio, USA.
Aaren Kettelhut, School of Health and Rehabilitation Sciences, Division of Medical Laboratory Science, The Ohio State University, Columbus, Ohio, USA.
Danielle Labbato, Department of Medicine and Pediatrics, Division of Infectious Disease, University Hospitals Cleveland Medical Center, Cleveland, Ohio, USA.
Cheryl Smith, Department of Medicine, Division of Infectious Disease, MetroHealth Medical Center, Cleveland, Ohio, USA.
Ann Avery, Department of Medicine, Division of Infectious Disease, MetroHealth Medical Center, Cleveland, Ohio, USA.
Theodore Parran, Case Western Reserve University School of Medicine, Cleveland, Ohio, USA.
Nicholas Funderburg, School of Health and Rehabilitation Sciences, Division of Medical Laboratory Science, The Ohio State University, Columbus, Ohio, USA.
Grace A. McComsey, Department of Medicine and Pediatrics, Division of Infectious Disease, University Hospitals Cleveland Medical Center and Case Western Reserve University School of Medicine, Cleveland, Ohio, USA.
References
- 1.An Q, Song R, Hernandez A, Hall HI. Trends and Differences Among Three New Indicators of HIV Infection Progression. Public Health Rep 2015;130(5):468–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ingle SM, May MT, Gill MJ, et al. Impact of risk factors for specific causes of death in the first and subsequent years of antiretroviral therapy among HIV-infected patients. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America 2014;59(2):287–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moore RD, Keruly JC, Chaisson RE. Differences in HIV disease progression by injecting drug use in HIV-infected persons in care. J Acquir Immune Defic Syndr 2004;35(1):46–51. [DOI] [PubMed] [Google Scholar]
- 4.Trickey A, May MT, Vehreschild J, et al. Cause-Specific Mortality in HIV-Positive Patients Who Survived Ten Years after Starting Antiretroviral Therapy. PloS one 2016;11(8):e0160460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Piggott DA, Varadhan R, Mehta SH, et al. Frailty, Inflammation, and Mortality Among Persons Aging With HIV Infection and Injection Drug Use. The journals of gerontology Series A, Biological sciences and medical sciences 2015;70(12):1542–1547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Peterson PK, Sharp BM, Gekker G, Jackson B, Balfour HH Jr. Opiates, human peripheral blood mononuclear cells, and HIV. Advances in experimental medicine and biology 1991;288:171–178. [DOI] [PubMed] [Google Scholar]
- 7.Zhu JW, Liu FL, Mu D, Deng DY, Zheng YT. Heroin use is associated with lower levels of restriction factors and type I interferon expression and facilitates HIV-1 replication. Microbes Infect 2017;19(4–5):288–294. [DOI] [PubMed] [Google Scholar]
- 8.Guo CJ, Li Y, Tian S, Wang X, Douglas SD, Ho WZ. Morphine enhances HIV infection of human blood mononuclear phagocytes through modulation of beta-chemokines and CCR5 receptor. Journal of investigative medicine : the official publication of the American Federation for Clinical Research 2002;50(6):435–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brenchley JM, Price DA, Schacker TW, et al. Microbial translocation is a cause of systemic immune activation in chronic HIV infection. Nat Med 2006;12(12):1365–1371. [DOI] [PubMed] [Google Scholar]
- 10.Marchetti G, Tincati C, Silvestri G. Microbial translocation in the pathogenesis of HIV infection and AIDS. Clin Microbiol Rev 2013;26(1):2–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ancuta P, Kamat A, Kunstman KJ, et al. Microbial translocation is associated with increased monocyte activation and dementia in AIDS patients. PLoS One 2008;3(6):e2516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Funderburg NT, Jiang Y, Debanne SM, et al. Rosuvastatin treatment reduces markers of monocyte activation in HIV-infected subjects on antiretroviral therapy. Clin Infect Dis 2014;58(4):588–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ramendra R, Isnard S, Mehraj V, et al. Circulating LPS and (1-->3)-beta-D-Glucan: A Folie a Deux Contributing to HIV-Associated Immune Activation. Front Immunol 2019;10:465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dirajlal-Fargo S, Moser C, Rodriguez K, et al. Changes in the Fungal Marker beta-D-Glucan After Antiretroviral Therapy and Association With Adiposity. Open Forum Infect Dis 2019;6(11):ofz434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gianella S, Letendre SL, Iudicello J, et al. Plasma (1 --> 3)-beta-D-glucan and suPAR levels correlate with neurocognitive performance in people living with HIV on antiretroviral therapy: a CHARTER analysis. J Neurovirol 2019;25(6):837–843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mehraj V, Ramendra R, Isnard S, et al. Circulating (1-->3)-beta-D-glucan Is Associated With Immune Activation During Human Immunodeficiency Virus Infection. Clin Infect Dis 2020;70(2):232–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Weiner LD, Retuerto M, Hager CL, et al. Fungal Translocation Is Associated with Immune Activation and Systemic Inflammation in Treated HIV. AIDS Res Hum Retroviruses 2019;35(5):461–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.El Kamari V, Moser C, Hileman CO, et al. Lower Pretreatment Gut Integrity Is Independently Associated With Fat Gain on Antiretroviral Therapy. Clin Infect Dis 2019;68(8):1394–1401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Allers K, Puyskens A, Epple HJ, et al. The effect of timing of antiretroviral therapy on CD4+ T-cell reconstitution in the intestine of HIV-infected patients. Mucosal Immunol 2016;9(1):265–274. [DOI] [PubMed] [Google Scholar]
- 20.Costiniuk CT, Angel JB. Human immunodeficiency virus and the gastrointestinal immune system: does highly active antiretroviral therapy restore gut immunity? Mucosal Immunol 2012;5(6):596–604. [DOI] [PubMed] [Google Scholar]
- 21.Mehandru S, Deren S, Kang SY, et al. Behavioural, Mucosal and Systemic Immune Parameters in HIV-infected and Uninfected Injection Drug Users. J Addict Res Ther 2015;6(4):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shah ASV, Stelzle D, Lee KK, et al. Global Burden of Atherosclerotic Cardiovascular Disease in People Living With HIV: Systematic Review and Meta-Analysis. Circulation 2018;138(11):1100–1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thomas G, Tacke R, Hedrick CC, Hanna RN. Nonclassical patrolling monocyte function in the vasculature. Arterioscler Thromb Vasc Biol 2015;35(6):1306–1316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Salter ML, Lau B, Mehta SH, Go VF, Leng S, Kirk GD. Correlates of elevated interleukin-6 and C-reactive protein in persons with or at high risk for HCV and HIV infections. J Acquir Immune Defic Syndr 2013;64(5):488–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Strickler HD, Blanchard JF, Vlahov D, et al. Elevated serum levels of neopterin but not beta 2-microglobulin in HIV-1-seronegative injecting drug users. AIDS 1993;7(3):361–367. [DOI] [PubMed] [Google Scholar]
- 26.Phillips KT, Stein MD. Risk practices associated with bacterial infections among injection drug users in Denver, Colorado. The American journal of drug and alcohol abuse 2010;36(2):92–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Smith ME, Robinowitz N, Chaulk P, Johnson KE. High rates of abscesses and chronic wounds in community-recruited injection drug users and associated risk factors. Journal of addiction medicine 2015;9(2):87–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mars SG, Bourgois P, Karandinos G, Montero F, Ciccarone D. The Textures of Heroin: User Perspectives on “Black Tar” and Powder Heroin in Two U.S. Cities. J Psychoactive Drugs 2016;48(4):270–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Summers PJ, Struve IA, Wilkes MS, Rees VW. Injection-site vein loss and soft tissue abscesses associated with black tar heroin injection: A cross-sectional study of two distinct populations in USA. Int J Drug Policy 2017;39:21–27. [DOI] [PubMed] [Google Scholar]
- 30.Torka P, Gill S. Cotton fever: an evanescent process mimicking sepsis in an intravenous drug abuser. The Journal of emergency medicine 2013;44(6):e385–387. [DOI] [PubMed] [Google Scholar]
- 31.Dwyer R, Topp L, Maher L, et al. Prevalences and correlates of non-viral injecting-related injuries and diseases in a convenience sample of Australian injecting drug users. Drug and alcohol dependence 2009;100(1–2):9–16. [DOI] [PubMed] [Google Scholar]
- 32.Siegel AJ, Mendelson JH, Sholar MB, et al. Effect of cocaine usage on C-reactive protein, von Willebrand factor, and fibrinogen. The American journal of cardiology 2002;89(9):1133–1135. [DOI] [PubMed] [Google Scholar]
- 33.Kidd SE, Grey JA, Torrone EA, Weinstock HS. Increased Methamphetamine, Injection Drug, and Heroin Use Among Women and Heterosexual Men with Primary and Secondary Syphilis - United States, 2013–2017. MMWR Morb Mortal Wkly Rep 2019;68(6):144–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Petersen KL, Marsland AL, Flory J, Votruba-Drzal E, Muldoon MF, Manuck SB. Community socioeconomic status is associated with circulating interleukin-6 and C-reactive protein. Psychosomatic medicine 2008;70(6):646–652. [DOI] [PubMed] [Google Scholar]
- 35.Asher AK, Zhong Y, Garfein RS, Cuevas-Mota J, Teshale E. Association of Self-Reported Abscess With High-Risk Injection-Related Behaviors Among Young Persons Who Inject Drugs. J Assoc Nurses AIDS Care 2019;30(2):142–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Summers PJ, Hellman JL, MacLean MR, Rees VW, Wilkes MS. Negative experiences of pain and withdrawal create barriers to abscess care for people who inject heroin. A mixed methods analysis. Drug Alcohol Depend 2018;190:200–208. [DOI] [PubMed] [Google Scholar]


