Abstract
A recent report from the National Academies of Sciences, Engineering, and Medicine (NASEM) highlights rising rates of working-age mortality in the United States, portending troubling population health trends for this group as they age. The Health and Retirement Study (HRS) is an invaluable resource for researchers studying health and aging dynamics among Americans ages 50 and above and has strong potential to be used by researchers to provide insights about the drivers of rising U.S. mortality rates. This paper assesses the strengths and limitations of HRS data for identifying drivers of rising mortality rates in the U.S. and provides recommendations to enhance the utility of the HRS in this regard. Among our many recommendations, we encourage the HRS to prioritize the following: link cause of death information to respondents; reduce the age of eligibility for inclusion in the sample; increase the rural sample size; enhance the existing HRS Contextual Data Resource by incorporating longitudinal measures of structural determinants of health; develop additional data linkages to capture residential settings and characteristics across the life course; and add measures that capture drug use, gun ownership, and social media use.
1. Introduction
U.S. life expectancy is lowest among all high-income countries and has been declining in recent years (Ho and Hendi 2018; NASEM 2021; Woolf et al. 2021). This decline has been driven by working-age adults (ages 25-64), portending troubling population health trends for this age group. A recent report from the National Academies of Sciences, Engineering, and Medicine (NASEM) shows that mortality rates are increasing among working-age adults in all racial/ethnic groups, both males and females (with increases more pronounced among women), and in most places in the U.S. (with the largest increases in rural areas) (NASEM 2021). The report also concluded that while there have been increases in numerous causes of death, the increase in working-age mortality since 1990 has been due primarily to the following causes: drug overdoses and alcohol-induced diseases, suicide, and cardiometabolic diseases. These trends are unique to the United States. These findings highlight the urgency of identifying the underlying multidimensional and multilevel drivers of these mortality trends to inform policy action, a task for which Health and Retirement Study (HRS) data may be uniquely positioned.
For the past 30 years, the HRS has been instrumental in enabling researchers to examine how social, economic, and behavioral risk factors contribute to individual health and mortality trajectories and population-level mortality trends. In recent years, the addition of biomarker, psychosocial, and contextual data have further expanded the usefulness of the HRS in understanding the drivers of poor health and premature mortality. To guide the National Institute on Aging’s (NIA) 2021 midterm review of the HRS, we conducted an assessment to inform recommendations for enhancing the utility of the HRS for identifying factors that have contributed to rising mortality rates in the United States, with particular attention to the causes of death implicated in recent troubling mortality trends among the working-age population – individuals who are either already in the HRS sampling frame or will soon be entering.
Our approach to this assessment was multipronged. From the HRS website, we reviewed the 2018 core and exit survey codebooks, and the codebooks for the Psychosocial and Lifestyle Questionnaire (PLQ), which began in 2006, the Life History Mail Survey (LHMS), the COVID-19 questionnaire, several experimental modules, and the restricted data resources. We also sought clarifying information from HRS staff regarding the current content of the HRS. We also used the interactive bibliography on the HRS website in August 2021 to identify 206 articles related to mortality produced using HRS data from 2000 to 2021.1 Finally, we solicited input from 29 colleagues across multiple disciplines2 who have authored health and mortality-related papers using HRS data.3
2. Strengths of the HRS for Mortality Research
Our review highlighted numerous strengths of the HRS for conducting mortality-related research. In terms of study design, strengths include its nationally-representative, long-running, and longitudinal design that has provided nearly 30 years of continuous data on individuals and relational dynamics affecting health, aging, and mortality; its comparatively large sample size and strong response rates; its use of a frequent interview schedule (annually prior to 1996 and biannually thereafter); its relatively consistent interview structure that facilitates high-quality comparisons of responses on the same items over a long time period; the regular inclusion of experimental modules that collect detailed information on timely economic and health topics; the inclusion of the old age population that enables the observation of more deaths than in other surveys; and oversamples of African Americans and Hispanics, which facilitate analyses of health and mortality trends among these groups. An additional strength of the study design is the HRS’s use of refreshed cohorts every six years so that studies remain nationally-representative over time and so that researchers have adequate sample sizes to examine mortality patterns by age, period, and birth cohort. In addition, the availability of user-friendly harmonized RAND HRS Longitudinal Files facilitates the use of these data by a wide range of researchers (Rand Center for Study of Aging n.d.).
In terms of measures, the HRS collects a wide constellation of individual, household, and relational factors that are rarely simultaneously included in large cohort studies. The HRS leadership team and the primary funder (NIA) have demonstrated tremendous openness, inclusion, and willingness to implement new HRS modules and questions throughout the years (Smith 2011). This model of openness and adaptation has expanded the use, reach, and impact of the HRS beyond its historical strengths in economic and social drivers of health to add critical new insights on cognition, psychosocial risk factors, and biomarker-based measures of health. Specific strengths include excellent measures of physical health (including self-rated, chronic diseases, pain, physical performance, and functioning), psychosocial health (via the Psychosocial and Lifestyle Questionnaire [PLQ]), cognitive health (starting at age 50 rather than age 65 like in most surveys), and socioeconomic resources (including detailed measures of wealth). The recent inclusion of biomarkers and retrospective measures of early life socioeconomic status and other health-risk exposures, such as lifetime traumas and stressful life events, enables a life course approach to studying mortality trends. Given the wide-reaching and enduring impact of the COVID-19 pandemic, we encourage the HRS to add questions to the core survey on whether the respondent tested positive for coronavirus, whether they were hospitalized as a result, and measures that capture “long-haul” symptoms.
Another key strength of the HRS is the effective completeness of the mortality data; the HRS ascertains respondents’ mortality status via both active (“exit” interviews) and passive methods (administrative record linkages), a feature that is unique to social surveys that include mortality information. HRS users also highlighted the ability to link HRS data to other data sources (through restricted data agreements) as a particular strength for understanding drivers of mortality trends (HRS 2020). For example, the linkage of respondents to data from the Centers for Medicare and Medicaid Services, Veterans Affairs, and the Social Security Administration provides rich information about health conditions and economic resources that would not otherwise be available. Linkage to the HRS Contextual Data Resource Series provides a wealth of information on place-level measures of health care, physical environment, food access, crime, and most recently - state COVID-19 policies. Linkage to newly released 1940 Census records extends the utility of the HRS for understanding the role that early life conditions play on subsequent health and mortality because it can provide not only actual childhood income for the approximately 9,600 HRS respondents who were alive in 1940 and for whom high-quality matches were identified, but also multiple indicators of household composition and neighborhood conditions that may be drivers of later life health and premature mortality (Warren et al. 2020).
The existence of HRS “clone studies” in multiple countries provides a unique opportunity for researchers interested in situating the health and mortality experiences among older adults in the United States within a cross-national context. This is particularly relevant as the United States continues to lose ground on life expectancy compared to our high-income peer counties (Ho and Hendi 2018; NASEM 2021; Woolf et al. 2021). The harmonized global HRS-like studies available at the Gateway to Global Aging Data (USC Dornsife Center for Economic and Social Research 2015) facilitates access to these data for comparative investigations.
Finally, the HRS team has demonstrated its ability to move quickly to capture information relevant to understanding respondents’ experiences during unanticipated exogenous shocks, with important implications for understanding related mortality, including their rapid collection and public release of COVID-19 project data from a random 50% sample of the core respondents. The HRS team should be commended for their efforts to collect this critical, time-sensitive wealth of information that will be used by social science and public health researchers for years to come.
3. A Framework for Enhancing the HRS to Better Understand Rising Mortality Rates in the United States
In 2021, NASEM released a Consensus Study Report entitled ‘High and Rising Mortality Rates among Working-Age Adults’ (NASEM 2021). The report provides a framework for understanding the general set of factors that may have contributed to high and rising mortality rates among U.S. working-age adults (ages 25-64). This framework and the findings from the NASEM report are particularly relevant for identifying necessary enhancements to the HRS because the HRS sampling frame already includes the later range of the working-age cohort (50-64), and the younger end of the age range will soon be entering the HRS sampling frame.
In this framework (Figure 1), the factors involved are thought to operate throughout the life course at three main levels: macrostructural, meso and community level, and individual level. Each level contains multiple dimensions of influence. The macro level captures overarching institutions and structures, including policies, corporate influences, social and economic inequality, macroeconomic conditions and trends, technology, and culture. The meso level incorporates intermediary settings and relationships, including families, workplaces, social networks, the health care system, and built, social, and physical environments. The micro level includes individual-level and proximate factors, such as socioeconomic status, health behaviors, health care use, and biological function. The layers are interdependent and operate across the life course, from gestation to death. Although not explicitly portrayed in the model, these multilevel and multidimensional factors are also described as having potentially heterogenous effects among different demographic and social groups (e.g., race/ethnicity, gender, sexual identity) and across different geographic contexts.
Figure 1. A Life Course Multilevel Model of Factors Involved in High and Rising Mortality among Working-Age Adults.
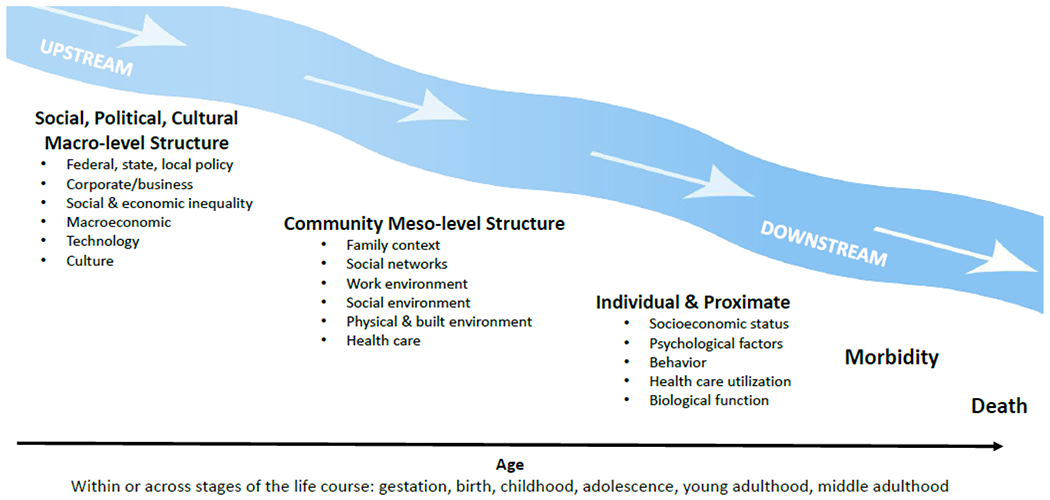
Credit: National Academies of Sciences, Engineering, and Medicine. 2021. High and Rising Mortality Rates Among Working-Age Adults. https://doi.org/10.17226/25976. Reproduced with permission from the National Academy of Sciences, Courtesy of the National Academies Press, Washington, D.C.
We use this framework to organize our assessment and recommendations for HRS data collection and potential design changes that would enable informed analysis and hypothesis-testing about rising mortality rates in the United States. Given the relative ease of capturing more proximate determinants of mortality, we begin there and work our way upstream.
3.1. Individual and Proximate Determinants
Individual (proximate) drivers of morbidity and mortality include biological function, socioeconomic status and resources, health behaviors, psychological factors, and health care use.
3.1.1. Biological Function
HRS began biomarker collection in 2006 during face-to-face interviews with half of the sample (selected randomly), with data from the other half collected in 2008. Beginning in 2016, venous blood samples were collected, and many assays were performed. These measures may prove useful as researchers attempt to identify how socio-environmental and biological risk factors combine to influence rising middle-age and older adult mortality risk through gene-environment interactions and epigenetic risk factors. We recommend continued collection of these data in future waves.
3.1.2. Socioeconomic and Housing Indicators
The wide range of socioeconomic indicators has been an historical strength of the HRS. The HRS core survey includes information on education, employment status and changes, income and income sources, pensions, homeownership, housing costs, foreclosures, assets and wealth, and retrospective childhood socioeconomic status (SES) (parents’ education and employment, financial situation, receipt of financial help, and residential move due to financial difficulties). The 2016 HRS experimental module on material hardship has additional details on housing quality and evictions. The Psychosocial and Lifestyle Questionnaire (PLQ) includes measures of lifetime homelessness, whether the respondent ever lived in homeless shelter, was ever incarcerated or in a juvenile detention center, and amount of time incarcerated. These questions capture important lifetime stressors that can influence later life health and mortality. The LHMS collects schooling histories, providing the potential to examine not only the role of educational attainment and type of education, but also some aspects of quality of schooling, which has been shown to predict health outcomes and mortality (Frisvold and Golberstein 2011). Through restricted data linkages, researchers can also connect HRS respondents to social security data.
Nonetheless, there are areas for improvement. Specifically, the way education is measured seems less well-suited for adults from more recent birth cohorts. While there are response options for no formal education, grades 1-11, high school, some college, college graduate, and post-college (including Masters/MBA), and higher (MD, Law, PhD), there is no way to determine whether a respondent earned an Associate’s degree or whether they attended community college. This despite the rise in Associate’s degrees over the past several years. The distinction between having an Associate’s degree versus other levels of education is important, considering recent findings from Zajacova and Lawrence (2021) that there are significant health returns to education for those with a Bachelor’s degree, but not for those with an Associate’s or trade degree. Given the increasing importance of education for patterning health outcomes and mortality (Sasson 2016; Montez et al. 2019), updating the education variable to reflect the experiences of more recent birth cohorts would extend its utility. Although the LHMS has detailed information on educational history, which captures far more detail than the core questionnaire, updating the education variable in the core survey for entering cohorts would provide added value and potentially greater use.
3.1.3. Health Behaviors
The HRS core questionnaire contains a wide range of questions on health behaviors that are useful for understanding rising rates of mortality from cardiometabolic and alcohol-related causes, including nutrition and diet (from the 2013 Health Care and Nutrition Study), types and frequency of exercise, sleep behaviors and quality, smoking, and alcohol use (including binge drinking, guilt about drinking, and morning drinking). Given the importance of obesity and cardiometabolic diseases to recent mortality trends, it would be useful to regularly repeat the Health Care and Nutrition Study, which includes detailed information on diet.
Given the prominent role of drug overdoses in driving recent midlife mortality trends (NASEM 2021), and increasing rates of illicit drug use and prescription drug misuse among older adults (Arndt et al. 2011; Kuerbis 2020), the absence of measures of drug misuse in the HRS is a glaring weakness for explaining mortality trends. The HRS includes a single question on use of any opioid pain medication in the past three months, but it does not distinguish between whether the respondents took the medication as prescribed or misused opioids. Use of other medications with high risk of misuse and overdose (e.g., sedatives and tranquilizers) and use of illicit drugs are missing entirely from the survey. Of course, accurately capturing problematic substance use poses challenges, including recall and social desirability bias. One possibility is to consider using biomarkers to capture alcohol and drug use (Stewart et al. 2010). Another is to include such questions in a mail survey or a leave behind questionnaire. Alternatively, these topics could be tested in an experimental module that would ideally also collect information on individuals’ and family members’ use of illicit and prescription drugs and the impact of such use on other family members (also see below). Ultimately, the inclusion of substance use measures should be considered a top priority.
Beyond drug use, the HRS data users we contacted expressed the desire for additional questions on social media consumption, trust in social and political institutions, and gun ownership. Research on the role of social media consumption on health, especially among older adults, is still in the nascent stage. Unlike earlier cohorts, social media has been a staple of modern life for cohorts aging into the HRS sample frame, and social media use may be just as relevant for health as some of the items captured in the current social participation-social engagement module of the PLQ (e.g., watching television). The current polarization on COVID-19 mitigation protocols and vaccinations, for example, highlights the role of social media as a key influencer of health-related behaviors. Given this role and the evidently increasing distrust in government and science, an improved understanding of the impact of social media on health behaviors seems a particularly relevant topic for further investigation. Firearm availability in turn has been consistently identified as a key risk factor for suicide, a trend-driving cause of death among working-age adults, including the younger age band included in the HRS sample (NASEM 2021). Yet the HRS does not include any measures of gun ownership. We recommend its inclusion in future survey waves.
3.1.4. Psychological Wellbeing
Psychological wellbeing has increasingly become recognized in recent years as an important driver of health and mortality. In 2006, the HRS added the self- (or proxy-) administered Psychosocial and Lifestyle Questionnaire (PLQ), which is completed by a rotating random 50% sample of the core panel participants who complete the enhanced face-to-face interview. This was a welcome addition to the core questionnaire wherein psychological health measures were limited to those capturing various components of depression. The PLQ covers six substantive areas of relevance for understanding how psychological well-being, social relationships, and work experience factors influence mortality:
subjective well-being (life satisfaction, domain satisfaction, depression, positive/negative affect, hedonic well-being, purpose in life, self-acceptance, personal growth, financial strain, and experienced well-being [in some waves]);
lifestyle and experience of stress (activities in life, social participation, neighborhood evaluation, religiosity, perceived everyday discrimination and major experiences of lifetime discrimination, lifetime traumas, early life experiences [in some waves], stressful life events, ongoing stress);
quality of social ties (spouse/child/kin/friends, positive support, negative support, closeness, division of household tasks, loneliness, early parental relationships [in some waves], friend contact, child contact);
personality traits (extraversion, neuroticism, openness, agreeableness, conscientiousness, cynical hostility, anxiety, anger, impulsivity);
work-related beliefs (work stress, work discrimination, work satisfaction, capacity to work, effort-reward balance, work support, work/family priorities, work/life balance, job lock); and
self-related beliefs (personal mastery, domain-specific control, perceived constraints, hopelessness, subjective age, perceptions of aging, subjective social status, optimism/pessimism, need for cognition).
Collectively, these measures are valuable for researchers trying to understand relationships between indicators of despair and rising rates of various types of cause-specific mortality (an area of inquiry that has seen substantial debate among researchers over the past several years (NASEM 2021). However, because the PLQ is administered to only half of the sample in each wave, small cell sizes sometimes create challenges for conducting robust analysis, and there are also challenges related to the timing and causal ordering with other relevant health exposures. We recommend that the PLQ be administered to all respondents.
Moreover, although the psychosocial content is more comprehensive than what is available in other social surveys, additional measures are warranted, including measures that capture decision making (some of which is available in the 2014 experimental module), measures that tap into prosocial factors (e.g., altruism, empathy, compassion, gratitude) that have been found to be associated with a range of mood-boosting and stress-reducing effects (Raposa et al. 2016), and measures that capture personal values related to self-direction, stimulation, hedonism, power, security, conformity, tradition, benevolence, and universalism (Schwartz 2012). Finally, given the U.S.’s increasing polarization on culturally dispositional factors (such as trust in government and science; attitudes about individual freedom versus collective responsibility) that may affect health behaviors, stress, and social relationships (Boxell et al. 2020; Heltzel and Laurin 2020; Weber et al. 2021), it would be valuable to incorporate measures of these factors (as well as political engagement) into the PLQ or the core questionnaire on a regular basis.
3.1.5. Health Care Access and Use
Finally, at the proximate level, the HRS includes several measures of health care access and use, including health insurance and dental coverage and source, out-of-pocket health care costs, usual source of care, satisfaction with care, ability to afford care, preventive health visits, vaccinations, surgeries, overnight hospital stays, dental visits, nursing home residence, and medication use for cholesterol, pain, breathing problems, stomach problems, help with sleep, and anxiety or depression. Linking to data from CMS and the VA through restricted data use agreements provides additional useful health care use information. However, there are no measures of substance use or mental health treatment use in the core survey – potentially important variables given the role of drugs and alcohol in driving recent working-age mortality trends. In addition, given the increasing importance of aging service organizations in helping older adults age-in-place, the HRS could benefit from the inclusion of questions on the use of formal aging services, such as senior centers, home-delivered meals, and home health aides, and the perceptions of the quality and accessibility of these services in their communities, perhaps modeled after the 2012 experimental module on utilization of home and community-based services.
In sum, we recommend the following changes and additions to the core survey or inclusion in more regularly offered experimental modules:
Change the educational attainment questions in the core questionnaire (or the education categories provided to researchers) to capture the completion of an Associate’s degree, in addition to the detail provided in the LHMS.
Add health behavior measures of illicit drug use, misuse of prescription drugs with high abuse potential (opioids, sedatives, and tranquilizers), social media use, and gun ownership.
Administer the PLQ to all respondents.
More frequently include psychosocial measures that capture decision making, and add measures that capture prosocial factors, personal values, culturally dispositional factors (e.g., trust in government and science, attitudes toward individual freedom versus collective responsibility), and political engagement.
Add health care use measures related to substance use and mental health treatment and the use of formal aging services.
3.2. Community- and Meso-Level Determinants
Meso-level factors potentially driving mortality trends include intermediary settings and relationships, such as family characteristics and relationships, workplaces, social networks, the health care system, and built, social, and physical environments. Some of these factors are already measured directly in the HRS, and others are captured in restricted data resources, including the HRS 1940 Census Data and the HRS Contextual Data Resource Series.
3.2.1. Family Context
The HRS provides rich detail on family structure over time and changes therein, due in large part to the multiple HRS file levels that capture household, respondent, sibling, household member, child, and helper measures, as well as transfers between respondents and children/grandchildren. In particular, the Family Structure Questionnaire provides information on family relationships, including but not limited to household structure, number of children, including stepchildren, grandchildren, and great grandchildren, frequency of contact, child care, and in kind and monetary intergenerational transfers. These data provide a wealth of information on family context.
There are, however, areas for improvement. One of the consequences of the contemporary drug overdose crisis, and more recently the COVID-19 pandemic, is the loss of family members, raising concerns about what happens to children of adults with substance use disorders or whose parents have died (Hillis et al. 2021; Verdery et al. 2020). Recent evidence suggests that grandparents are stepping into this void (Anderson 2019). The HRS has the potential to shed light on the resulting caregiver burden and potential health consequences for older adults. To capture this phenomenon, we recommend adding questions on the reasons a grandparent is taking care of grandchildren or great grandchildren and deaths of other family members besides parents and spouses, including their cause of death (e.g., COVID-19, gun violence, drug overdose, suicide).
In addition, the PLQ (discussed above) collects information on respondents’ childhood experiences, such as quality of relationships with parents early in life and a module on lifetime traumas before the age of 18 (e.g., having to repeat a year of school, ever in trouble with the police, parental drug or alcohol abuse, physical abuse by parent). However, there are not questions on other potentially important adverse childhood experiences (ACEs), such as parental incarceration. Given that the U.S. entered an era of mass incarceration starting in the 1980s, the large generation of children who lost parents to incarceration is nearing inclusion in the HRS sample. We recommend the HRS capture retrospective measures of parental incarceration and other ACEs that are included in prospective panel studies like the National Longitudinal Study of Adolescent to Adult Health (AddHealth) and Fragile Families.
3.2.2. Social Relationships, Networks, and Social Contexts
The PLQ includes numerous measures of social context (neighborhood social cohesion and violence), social relationships, including social participation and engagement (e.g., volunteering, participation in clubs), retrospective social participation at age 30, composition of and contact with social network, and perceived positive and negative social support, all of which facilitate analyses on relationships between changing trends in social conditions and trends in mortality.
Although the PLQ includes questions about the number of social ties and contact and quality of interactions with those social ties, other longitudinal surveys of older populations, such as the National Social Life, Health, and Aging Project (NSHAP), have incorporated more detailed social network data. The lack of such data in the HRS was noted by several HRS data users we contacted and was outlined by Pescosolido in her 2011 commissioned paper related to improving the utility of HRS data. Social networks can play important roles in health and wellbeing through multiple mechanisms and may have become increasingly important sources of health-related information (Zhang and Centola 2019). We recommend giving consideration to including a module to gather egocentric social networks that includes demographic and socioeconomic information on network members. Such a module would be even more beneficial if it included more information on the characteristics of people who live with the respondent. Such information may also help researchers understand the roles of end-of-life informal caregiving on risk of death.
Another form of social engagement is religious service participation. Measures that capture religiosity and faith (psychosocial measures) have been found in numerous studies to be associated with mortality (Hummer et al. 1999; Nisbet et al. 2000; Idler 2020; see Chida et al. 2009 for systematic review). But religion also involves a social component. Studies of religious involvement using the HRS have also shown aspects of religious service participation to be associated with both higher and lower mortality and better health outcomes (e.g., Idler et al. 2017; Ofstedal et al. 2019; Suh et al. 2019). The HRS included questions on religious involvement in the core questionnaire beginning in 2004, as well as a more detailed battery of questions in the 2016 Religious Life Histories Experimental module. Given declines in formal religious participation in recent decades (Lipka 2015; Jones 2021), we recommend that questions on religious participation be regularly incorporated in the core survey or repeated more frequently in experimental modules to capture the potential role of religion as a social institution that may buffer against unexpected life events and external shocks.
3.2.3. Work Environment
The PLQ includes several questions on work environment, including employment satisfaction, stressors, demands, and perceived control; workplace discrimination; and coworker and supervisor support. The 2018 Section V Module also includes numerous questions about work conditions and experiences. In addition, the 2017 LHMS includes information on lifetime occupational and work history and some job characteristics, which can facilitate research on some aspects of the changing nature of work on mortality trends.
What is currently lacking is information on work quality (e.g., predictability, stability) and work arrangements, such as gig work that can take many forms that have potential serious consequences for health and well-being, including independent contract work, online platform work, on-call workers, and temporary workers (Freni-Sterrantino and Salerno 2021). For example, a recent study found that although low wages were associated with psychosocial stress, habitual instability in work schedules had stronger associations with such distress as well as with poor sleep quality and unhappiness (Schneider and Harknett 2019). Both younger cohorts entering the labor force and older cohorts who are not in long-term steady jobs have been exposed to increasingly precarious and unpredictable employment in recent years. This is particularly the case for those without a 4-year college degree – a group who is driving working-age mortality trends (Case and Deaton 2020).
3.2.4. Built, Physical, and Health Care Environments
Short of questions on neighborhood physical disorder in the PLQ, the individual questionnaires contain few measures of built, physical, and health care environments. However, valuable contextual information can be gained by linking to some of the restricted data resources. By accessing the HRS Contextual Data Resource, researchers can gain access to data on land use, air quality, street connectivity, food access, and the Dartmouth Atlas of Health Care (HRS 2020). These data can be linked to HRS respondents based on their place of residence. The 1940 Census Linkage provides information on childhood place of residence, and the 2015 and 2017 LHMS collects residential history. Relatively few data sources make it possible to trace individual residential histories over time. Residential mobility, particularly during childhood, has been identified as a risk factor for poor later-life health outcomes (Bures 2003; Jelleyman and Spencer 2008; Oishi and Schimmack 2010). Moreover, one-time measures of residential context are unlikely to capture the full extent of exposures to various community contexts. Thus, the 1940 Census Linkage and the LHMS data are potentially valuable sources of information that can be used to examine frequency of residential moves and characteristics of places of residence over the respondent’s life course. However, repetition of the LMHS will be necessary to capture more recent and incoming HRS cohorts. We elaborate on this further in the final section of this paper.
As noted previously, the HRS has moved quickly to survey respondents to obtain information about experiences during unanticipated shocks. We encourage HRS to continue to administer such surveys to respondents in geographic areas that have experienced recent exogenous shocks (e.g., climate events, police shootings) to shed light on the impacts of rapid-onset changes to physical and social environments on psychological and physical health. For example, there has been an increasing focus on how climate change and its associated weather events can impact human health and mortality in multiple ways (Hajat et al. 2014; CDC 2021). Other recent events that have drawn national attention are police shootings and their impact on the mental health of Black Americans (Bor et al. 2018).
In sum, we recommend the following changes and additions to the core survey or inclusion in more regularly offered experimental modules:
Add questions on reasons a grandparent is taking care of a grandchild and on causes of death for family members besides parents and spouses.
Add additional adverse childhood experience measures similar to those in AddHealth and Fragile Families.
Add a module to collect egocentric social network data that includes demographic and socioeconomic information on network members.
More frequently include questions on religious participation.
Include measures of work quality, such as predictability and stability.
Develop rapid-response surveys targeted to respondents in specific geographic areas to capture the impacts of recent exogenous environmental and social shocks.
3.3. Social, Political, Cultural, and Macro-Level Structures
For decades now, life expectancy in the U.S. has become increasingly unequal between regions, states, counties, and across the rural-urban continuum (Murray et al. 2006; Fenelon 2013; Vierboom et al. 2019; Cosby et al. 2019; Elo et al. 2019; Montez et al. 2019; Monnat 2020; Montez et al. 2020; NASEM 2021; Graetz and Elo 2021). Indeed, rising geographic disparities in mortality rates among working-age adults were a key finding of the NIA-funded NASEM report on High and Rising Mortality Rates among Working-Age Adults (2021). That this increasing divergence does not appear to be fully (or even mostly) explained by differential demographic and socioeconomic composition (James et al. 2018; Graetz and Elo 2021) suggests that upstream contextual and structural causes are contributing to this trend.
There are growing calls among social scientists that to adequately understand these trends and to address disparities in U.S. population health, researchers need to incorporate measures of structural determinants of health, including political, economic, commercial, and legal determinants (Bambra 2016; Bambra et al. 2019; Montez et al. 2021), as well as structural racism (Bailey et al. 2017; O’Brien et al. 2020) and structural sexism (Homan 2019; Homan et al. 2021). Many of these structural factors affect U.S. population health in the aggregate (e.g., technological change, structural racism). However, numerous factors can be operationalized at various geographic levels, such as states and counties. The HRS and its linked data resources currently capture few such measures. For example, although the PLQ includes a handful of measures on perceived interpersonal discrimination, it does not capture structural aspects that manifest at the level of state or county policies and institutions. Although the HRS Contextual Data Resource includes information on air quality and place-level socioeconomic indicators, it does not include information on the policies or institutions that drive these downstream contextual determinants (except for the recent inclusion of the COVID-19 US State Policy Database). It also does not include measures that capture macro-economic change, such as deindustrialization and other changes in the structure of job opportunities and quality, which have varied in their impacts across places and may be driving diverging mortality across geographic areas and sociodemographic groups (NASEM 2021).
“Scaling up” or “refocusing upstream” (McKinlay 1975; Bambra 2016) not only enables researchers to identify the beginning point in the causal sequence portrayed in Figure 1 (the cause of the cause of the cause) but also facilitates multilevel analysis to consider the ways that factors at multiple levels intersect to influence mortality trends; also one of the key recommendations of the NASAM Report on High and Rising Mortality Rates among Working-Age Adults (NASAM 2021).
Just as the HRS has adapted over time to add measures that have emerged in the literature as important to health and mortality (e.g., psychosocial and biomarker measures), we encourage continued adaptation and growth via the inclusion of structural determinants of health, including measures that capture change in these conditions over time. Like individuals, places have life courses. Accordingly, data should be longitudinal to enable examination of how changes in structural conditions over time affect morbidity and mortality among HRS respondents. The ability to examine the impact of changing social, economic, and political conditions on mortality represents a unique opportunity in the HRS.
To capitalize on this opportunity, the existing HRS Contextual Data Resource should be expanded to incorporate state- and county-level structural determinants. We view this as a top priority and “low-hanging” fruit for NIA and the HRS because it would not increase the length of the survey and would require no additional investment of respondents’ time. One recommendation is to add new derived measures computed from multiple variables already included in the HRS Contextual Data Resource, such as the share of livable wage jobs or Black-White and Hispanic-White ratios in place-level household income, employment, home ownership, and housing values. Another recommendation is to merge in existing sources of contextual data, such as the Opportunity Insights database on economic mobility (Opportunity Insights n.d.) or state policies across a variety of domains relevant to health, such as those available in the LawAtlas Project (Temple University n.d.) and Preemption Watch (Grassroots Change n.d.). It is our understanding that the NIA-funded R24 Network on Life Course Health Dynamics and Disparities (NLCHDD) (https://gero.usc.edu/nlchdd/) is already engaged in work to compile a state-level policy database such as the type we are recommending. Once completed, linking that database to the HRS could accelerate research on the contribution of state policies to mortality trends.
Examples of structural measures that could be captured at the state and/or county levels include:
Political economy: economic, social, health, environmental, and regulatory policies; preemption laws; political campaign contributions; governing body partisan balance; government revenue and expenditures by type; social welfare generosity; unionization rates; share of livable wage jobs
Corporate/commercial determinants: market concentration; corporate taxes, subsidies, and incentives; marketing expenditures; concentration of extractive industries (e.g., mining, oil extraction; fracking); per capita sales of disease and injury inducing products (e.g., ultra-processed foods, tobacco, alcohol, firearms, prescription drugs with high abuse potential, pesticides and fertilizers)
Structural sexism: ratio of men’s to women’s weekly earnings for full-time workers, labor force participation, and poverty rates; percentage of legislative seats occupied by men; percentage of population composed of religious conservatives; percentage of women who live in a place without an abortion provider, gun laws (Homan 2019; Rapp et al. 2021; Graetz et al. 2020).
Structural racism: Agenor et al. (2021) identified 843 state laws linked to structural racism, including domains of voting rights, stand-your-ground, racial profiling, mandatory minimum sentencing, immigrant protections, fair-housing, predatory lending, punishment in schools, and stop-and-identify laws. Homan et al. (2021) used the ratio of Black-to-White and Hispanic-to-White incarceration; percentage of the population unable to vote due to a felony conviction; Black-to-White and Hispanic-to-White ratios of percentage with a Bachelor’s degree, unemployment rate, poverty rate, and home ownership rate; Black-to-White and Hispanic-to-White voting ratios; level of Black and Hispanics under representation in legislatures; and measures of residential segregation. Additional potential measures may include the presence of hate groups, historical racism (lynching, land theft, redlining), and use of policy force.
Although researchers are currently able to work with HRS to merge in contextual resources themselves, providing a ready-to-use structural determinant database as part of the existing HRS Contextual Data Resource would facilitate multilevel and multidimensional research in this area and signal to the research community that NIA and HRS view a focus on structural determinants as a critical direction for understanding health, aging, and mortality trends. We encourage NIA to fund studies that could identify the structural factors contributing most to recent U.S. mortality trends (such as the recent RFA on Understanding and Addressing the Impact of Structural Racism and Discrimination on Minority Health and Health Disparities) and then prioritize the addition of measures that capture those factors in the HRS Contextual Data Resource.
Beyond adding structural determinants, the HRS might also consider collecting information via the experimental questionnaires on respondents’ attitudes toward big social problems of the time, such as income inequality, climate change, mental health, race relations, social unrest, political polarization, and corporate influences on politics, so that researchers can better understand the role of these structural stressors on health. The addition of in-depth qualitative interviews with a sample of HRS respondents in different geographic areas would also help researchers understand the processes through which upstream structural factors and changes therein affect poor health and mortality (NASAM 2021).
In sum, we recommend the following additions to better identify and understand macro-level and structural determinants of mortality trends:
Incorporate longitudinal measures of structural determinants of health (political, macro-economic, commercial, legal), structural sexism, and structural racism into the HRS Contextual Data Resource.
Use experimental modules to collect information on respondents’ attitudes and concerns about pressing or emerging social problems.
Add qualitative interviews with a geographically diverse sample of HRS respondents.
3.4. Overarching Constraints and Recommendations
In this section, we summarize overarching limitations and recommendations that intersect with the sections above. They are related to providing cause of death data, capturing more of the working-age population, oversampling rural residents to facilitate analyses of rural-urban and within-rural differences, capturing more measures of residential contexts throughout the life course, expanding certain sub-group samples, and providing additional administrative data linkages.
3.4.1. Provide Cause of Death Information
One key piece of information missing for analyses of mortality trends is the respondent’s cause of death, which had been available via the linked National Death Index (NDI) until 2018. Cause-of death data are critical for assessing the life course determinants of the rise in mortality from the causes that have been driving recent trends. We thus strongly recommend that the HRS resume the linkage to the NDI or find an alternative linkage strategy to make cause-of-death data available for all deceased respondents. Such data will also provide a check on date of death currently provided by a proxy informant. Such data linkage should be given high priority.
3.4.2. Capture More of the Working-Age Population
To better understand the drivers of rising mortality rates in the United States, a major limitation of the HRS is the age of eligibility, which is currently set at age 50. Large inequalities in health and mortality begin to emerge before age 50 when U.S. death rates are already substantially higher than in other high-income countries (Ho 2013). The NASEM report documented rising mortality rates starting at age 25. The HRS misses entirely the experience of these younger cohorts and captures a select sample of these cohorts only when they enter the HRS sampling frame (a time at which many at the highest risk of premature mortality have already perished). We recommend that the HRS reduce the age of eligibility. Such an extension has become increasingly important given the continuing drug overdose epidemic that is killing young and middle-age adults at exceedingly high rates, and the anticipated lingering effects of the COVID-19 pandemic on families and survivors, as well as individuals with long-haul symptoms.
3.4.3. Oversample Rural Residents
In recent decades, the United States has witnessed widening geographic inequalities in mortality. In general, while coastal regions in the East and the West have experienced mortality declines, the Midwest and the South have fared less well. Geographic inequalities also vary by metropolitan status with death rates increasing in many rural areas but declining in large central metropolitan areas and their suburbs in many parts of the country, at least until the mid-2010s (Cosby et al. 2019; Elo et al. 2019; Graetz and Elo 2021; Monnat 2020; NASAM 2021). Furthermore, the drug overdose epidemic has had an unequal impact on mortality across the U.S. (Monnat 2018; Monnat 2019; Monnat et al. 2019; Peters et al. 2020). For example, in the past three decades, fatal drug overdose rates have risen much more in Appalachia, the Industrial Midwest, and New England than in other regions of the U.S. (Monnat 2020; NASEM 2021). Widening geographic divergence in numerous other causes of death, including suicide, cardiometabolic diseases, and respiratory diseases highlight the critical need for geocoded health data that can facilitate research to understand these troubling trends.
Why the U.S. has experienced increasing geographic mortality divergence is not that well understood (NASEM 2021). Several of the factors discussed above in the macro-level and structural determinants section are likely to have played a role in this divergence, including state policy polarization (Montez et al. 2019; Montez et al. 2020) and the impacts of industrial restructuring which affected some places more than others (NASEM 2021). HRS data are currently poorly suited to examine increasing geographic inequalities in mortality trends, including increasing disparities within rural areas (Jensen et al. 2020; Monnat 2020), due the relatively small rural sample size. We endorse the recommendation of the NASAM report that urges NIH to “support the oversampling of rural populations in national health and aging surveys,” including the HRS.
3.4.4. Develop Additional Data Linkages to Characterize Residential Setting across the Life Course
The HRS should be commended for the efforts already undertaken (and those that are ongoing) to create contextual data sets that can be used to characterize the residential environments of respondents. However, it has long been recognized that experiences and exposures throughout the life course contribute to health and mortality in mid-life and at older ages (Ben-Shlomo and Kuh 2002; Kuh and Ben-Shlomo 2004; Felitti et al. 1998; Harris et al. 2006; Hayward and Gorman 2004; Hertzman and Boyce 2010). Such exposures include not only individual experiences and family circumstances, but also characteristics of the places of residence and local and state-level policy contexts. Therefore, it is critical to capture more measures of the residential characteristics of respondents throughout their life course. The LHMS, which collects information on residential histories, provides a unique opportunity to link individuals to their residential settings. We recommend that the HRS develop additional data linkages to characterize the residential settings of respondents across their life course.
3.4.5. Consider Increasing Sample Sizes for Certain Subgroups
Among the most common limitations identified by the HRS users we contacted was small sample sizes that prohibit examination of health and mortality trends among certain subgroups. In terms of race/ethnicity, sub-group analysis is not possible for any groups other than Whites and Blacks. Although Hispanics are oversampled, the sample size remains too small for country-of-origin analysis. Mexicans are the only national-origin group that can be reliably disaggregated from other Hispanics. Separating the Hispanic and Asian samples into U.S. versus foreign born also produces samples sizes too small for robust analysis. Although the size of the older foreign-born population in the U.S. has increased considerably in the last two decades, the HRS has not increased its sample of foreign-born older adults to allow an investigation of health and mortality trends for immigrants by national origin. This data gap means that older age outcomes can only be viewed at the aggregate level, preventing an understanding of the heterogeneity of mortality, particularly based on race and nativity. It also limits our ability to compare mortality rates of U.S. based immigrants and non-immigrants by country of origin using HRS sister data sets. Sexual minority sample sizes are also small, and there is currently no way to assess gender minority status. Given the increasing size of the gender minority population and their higher risk of poor health and premature mortality (Institute of Medicine 2011), it is critical to monitor mortality trends in this group. The number of respondents who are willing to identify as gender minorities will likely increase in forthcoming cohorts, so the HRS should be mindful about including response options that accurately classify gender minorities.
3.4.6. Develop Additional Administrative Data Linkages
Record linkage is an increasingly common and relative low-cost way to enhance existing surveys. As noted above, the HRS has made commendable efforts to link the HRS data to other data sources, including Medicare records, Social Security Administration data, contextual-level data to characterize the participants’ residential context, 1940 Census records to link data on childhood characteristics, and previously to the National Death Index (which ended in 2018). We strongly recommend that these record linkage efforts continue, including updating the linkage to Medicaid records and the identification of potential additional administrative data sources, such as data from the U.S. Department of Housing and Urban Development.
4. Conclusions
The Health and Retirement Study has proven to be an invaluable resource for studying aging, health, and mortality in the United States for the past 30 years. Its many strengths for understanding drivers of mortality trends include its nationally-representative longitudinal design and its rich data on social, psychological, economic, and behavioral health risk factors. The HRS team has also demonstrated a willingness to integrate emerging health factors, such as biomarker data collection, and to take advantage of administrative record linkages to enrich the survey data. The many experimental modules have allowed investigations of specific topics in greater depth and to test the feasibility of integrating new items to the core survey. Furthermore, the use of leave behind and mail surveys (e.g., the Life History Mail Survey) provides information on schooling, residential, and work histories that fill in missing detail before age 50. Over time the HRS has also moved away from focusing only on individual-level predictors of health and mortality to include data on contextual influences through data linkages. The HRS has also provided the platform to move quickly to examine the impact of unanticipated shocks, such as the COVID-19 pandemic, on the 50+ U.S. population.
Our assessment led to several recommendations related to the inclusion of new variables, modules, or linked data resources at the macrostructural, meso- and community-, and individual levels, as well as several overarching recommendations. Our recommendations are numerous, but we view the following six as the most critical for enhancing the utility of HRS data for understanding contempSorary U.S. mortality trends:
Provide cause of death (COD) information by either resuming linkage to the National Death Index or developing some other COD linkage.
Capture more of the population that is driving contemporary mortality trends by expanding the HRS inclusion criteria to younger adults.
Increase the rural sample size to enable analysis of rural-urban and within-rural differences and trends.
Enhance the HRS Contextual Data Resource by incorporating longitudinal measures of structural determinants of health (e.g., political, macro-economic, commercial, legal), structural sexism, and structural racism at the state- and county-levels.
Develop additional data linkages to capture resident settings and characteristics across the life course.
Add health behavior measures of drug use, social media use, and gun ownership.
Given our many recommendations to add new measures and expand the sample, it will likely be necessary for the HRS to eliminate some questions and/or modules that are not commonly used by researchers. We recommend that the NIA commission a study to determine the least frequently used HRS items in research to inform items that could be removed or moved from the core survey to less frequently administered questionnaires.
Acknowledgements
The authors acknowledge grant funding from the National Institute on Aging (R01AG060115) and National Institute on Drug Abuse (U01DA055972), and support from two NIA-funded research networks (R24AG065159 and R24AG045061), the NIA-funded Center for Aging and Policy Studies at Syracuse University (P30AG066583), the NICHD-funded Population Studies Center (P2CHD044964) and NIA-funded Population Aging Research Center (P30AG012836) at University of Pennsylvania, the NICHD-funded Population Research Institute at Penn State (P2CHD041025) and the USDA Agricultural Experiment Station Multistate Research Project: W4001, Social, Economic and Environmental Causes and Consequences of Demographic Change in Rural America.
Footnotes
Conflict of Interest: The authors state no conflict of interest
Many thanks to Yue Sun (Syracuse University) for providing assistance with the literature review and searching for specific items across the multiple HRS surveys.
We are grateful for feedback provided by numerous colleagues who have used the HRS for mortality-related research: Theresa Andrasfay (University of Southern California), Courtney Boen (University of Pennsylvania), Dustin Brown (Mississippi State University), Rebecca Brown (University of Pennsylvania), Chi-Tsun Chiu (Institute of European and American Studies), Emily Choi (Texas Tech University), Norma Coe (University of Pennsylvania), Rachel Donnelly (Vanderbilt University), Michal Engelman (University of Wisconsin), Wen Fan (Boston College), Mara Getz Sheftel (University of Western Ontario), Maria Glymour (University of California San Francisco), Noreen Goldman (Princeton University), Robert Hummer (University of North Carolina), Ellen Idler (Emory University), Heide Jackson (University of Maryland), Jennifer Karas Montez (Syracuse University), Eric Kim (University of British Columbia), Rachel Margolis (University of Western Ontario), Neil Mehta (University of Texas Medical Branch), Sung Park (Princeton University), Sarah Patterson (University of Michigan), Claire Pendergrast (Syracuse University), Borianna Pratt (Princeton University), Nicholas Schiltz (Case Western Reserve University), Connor Sheehan (Arizona State University), Douglas Wolf (Syracuse University), Mengyi Xu (Purdue University), and Anna Zajacova (University of Western Ontario).
Given that this paper does not report findings based on human subjects research, it does not require IRB review.
The Veterans Affairs Health Care Information linkage includes measures of substance use and mental health treatment services, include clinic visits, inpatient stays, and average cost data. Medicare and Medicaid linkage provide such information if mental health services were covered. However, the linkage to Medicaid data is available only through 2012.
Contributor Information
Shannon M. Monnat, Lerner Chair for Public Health Promotion and Lerner Center Director, Associate Professor of Sociology, Maxwell School of Citizenship and Public Affairs, Syracuse University, 426 Eggers Hall, Syracuse, NY 13244
Irma T. Elo, Professor and Chair of Sociology, Chair, Graduate Group in Demography, 229 McNeil Building, University of Pennsylvania
References
- Agenor Madina, Perkins Carly, Stamoulis Catherine, Hall Rahsaan D., Samnaliev Mihail, Berland Stephanie, and Austin S. Bryn. 2021. “Developing a Database of Structural Racism-Related State Laws for Health Equity Research and Practice in the United States.” Public Health Reports 136(4):428–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson Lydia. 2019. “The Opioid Prescribing Rate and Grandparents Raising Grandchildren: State and County Level Analysis.” United States Census Bureau Working Paper SEHSD-WP2019-04. [Google Scholar]
- Arndt Stephan, Clayton Rebecca, and Schultz Susan K.. 2011. “Trends in Substance Abuse Treatment 1998–2008: Increasing Older Adult First-Time Admissions for Illicit Drugs.” The American Journal of Geriatric Psychiatry 19(8):704–711. [DOI] [PubMed] [Google Scholar]
- Bailey Zinzi D., Krieger Nancy, Agenor Madina, Graves Jasmine, Linos Natalia, and Bassett Mary T.. 2017. “Structural Racism and Health Inequities in the USA: Evidence and Interventions.” The Lancet 389(10077):1453–63. [DOI] [PubMed] [Google Scholar]
- Bambra Clare. 2016. Health Divides: Where You Live Can Kill You. Bristol, UK: Policy Press. [Google Scholar]
- Bambra Clare, Smith Katherine E., and Pearce Jamie. 2019. “Scaling Up: The Politics of Health and Place.” Social Science & Medicine 232:36–42. [DOI] [PubMed] [Google Scholar]
- Ben-Shlomo Yoav, and Kuh Diana. 2002. “A Life Course Approach to Chronic Disease Epidemiology: Conceptual Models, Empirical Challenges and Interdisciplinary Perspectives.” International Journal of Epidemiology 31(2):285–93. [PubMed] [Google Scholar]
- Bor Jacob, Venkataramani Atheendar S., Williams David R., and Tsai Alexander C.. 2018. “Police Killings and their Spillover Effects on the Mental Health of Black Americans: A Population-Based, Quasi-Experimental Study.” The Lancet 392(10144):302–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boxell Levi, Gentzkow Matthew, and Shapiro Jesse M.. 2020. “Cross-Country Trends in Affective Polarization.” National Bureau of Economic Research Working Paper 26669. [Google Scholar]
- Bures Regina. 2003. “Childhood Residential Stability and Health at Midlife.” American Journal of Public Health 93(7):1144–1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Case Anne, and Deaton Angus. 2020. Deaths of Despair and the Future of Capitalism. Princeton, NJ: Princeton University Press. [Google Scholar]
- Chida Yoichi, Steptoe Andrew, and Powell Lynda H.. 2009. ”Religiosity/Spirituality and Mortality: A Systematic Quantitative Review. Psychotherapy and Psychosomatics 78(2):81–90. [DOI] [PubMed] [Google Scholar]
- Cosby Arthur, Maya McDoom-Echebiri Wesley James, Khandekar Hasna, Brown Willie, and Hanna Heather L.. 2019. “Growth and Persistence of Place-Based Mortality in the United States: The Rural Mortality Penalty.” American Journal of Public Health 109(1):155–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elo Irma, Hendi Arun S., Ho Jessica Y., Vierboom Yana C., and Preston Samuel L.. 2019. “Trends in Non-Hispanic White Mortality in the United States by Metropolitan-Nonmetropolitan Status and Region, 1990-2016.” Population and Development Review 45(3):549–583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felitti Vincent J., Anda Robert F., Nordenberg Dale, Williamson David F., Spitz Alison M., Edwards Valerie, Koss Mary P., and Marks James S.. 1998. “Relationship of Childhood Abuse and Household Dysfunction to Many of the Leading Causes of Death in Adults: The Adverse Childhood Experiences (ACE) Study.” American Journal of Preventive Medicine 14(4):245–258. [DOI] [PubMed] [Google Scholar]
- Fenelon Andrew. 2013. “Geographic Divergence in Mortality in the United States.” Population and Development Review 39(4):611–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freni-Sterrantino Anna, and Salerno Vincenzo. 2021. “A Plea for the Need to Investigate the Health Effects of Gig-Economy.” Frontiers in Public Health 9:638767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frisvold David, and Golberstein Ezra. 2011. “School quality and the education-health relationship: Evidence from Blacks in segregated schools.” Journal of Health Economics 30(6):1232–1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graetz Nick, and Elo Irma. 2021. “Decomposing County-Level Working-Age Mortality Trends in the United States Between 1999-2011 and 2015-2017.” Spatial Demography. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graetz Nick, Preston Samuel H., Peele Morgan, and Elo Irma T.. 2020. “Ecological Factors Associated with Suicide Mortality among non-Hispanic Whites.” BMC Public Health 20:1339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grassroots Change. n.d. “Preemption Watch Database.” Grassroots Change. Retrieved October 2021 (https://grassrootschange.net/preemption-watch/).
- Hajat Shakoor, Vardoulakis Sotiris, Heaviside Clare, and Eggen Bernd. 2014. “Climate Change Effects on Human Health: Projections of Temperature-Related Mortality for the UK during the 2020s, 2050s and 2080s.” Journal of Epidemiology and Community Health 68:641–648. [DOI] [PubMed] [Google Scholar]
- Harris Kathleen Mullan, Gordon-Larsen Penny, Chantala Kim, and Udry J. Richard. 2006. “Longitudinal Trends in Race/Ethnic Disparities in Leading Health Indicators from Adolescence to Young Adulthood.” Archives of Pediatrics & Adolescent Medicine 160(1):74–81. [DOI] [PubMed] [Google Scholar]
- Hayward Mark D., and Gorman Bridget K.. 2004. “The Long Arm of Childhood: The Influence of Early-Life Social Conditions on Men’s Mortality.” Demography 41(1):87–107. [DOI] [PubMed] [Google Scholar]
- Health and Retirement Study. 2020. “Available Restricted Data Products.” Health and Retirement Study. Retrieved October 2021 (https://hrs.isr.umich.edu/data-products/restricted-data/available-products).
- Heltzel Gordon, and Laurin Kristin. 2020. “Polarization in America: Two Possible Futures.” Current Opinion in Behavioral Sciences 34:179–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hertzman Clyde, and Boyce Tom. 2010. “How Experience Gets Under the Skin to Create Gradients in Developmental Health.” Annual Review of Public Health 31:329–347. [DOI] [PubMed] [Google Scholar]
- Hillis Susan D., Blenkinsop Alexandra, Villaveces Andrés, Annor Francis B., Liburd Leandris, Massetti Greta M., Demissie Zewditu, Mercy James A., Nelson Charles A., Cluver Lucie, Flaxman Seth, Sherr Lorraine, Donnelly Christl A., Ratmann Oliver, and Unwin H. Juliette T.. 2021. “COVID-19-Associated Orphanhood and Caregiver Death in the United States.” Pediatrics e2021053760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho Jessica Y. 2013. “Mortality under age 50 accounts for much of the fact that US life expectancy lags that of other high-income countries.” Health Affairs 32(3):459–467. [DOI] [PubMed] [Google Scholar]
- Ho Jessica Y., and Hendi Arun S.. 2018. “Recent Trends in Life Expectancy Across High Income Countries: Retrospective Observational Study.” BMJ 362:k2562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Homan Patricia. 2019. “Structural Sexism and Health in the United States: A New Perspective on Health Inequality and the Gender System.” American Sociological Review 84(3):486–516. [Google Scholar]
- Homan Patricia, Brown Tyson H., and King Brittany. 2021. “Structural Intersectionality as a New Direction for Health Disparities Research.” Journal of Health and Social Behavior 62(3):350–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hummer Robert A., Rogers Richard G., Charles B Nam, and Ellison Christopher G.. 1999. “Religious Involvement and U.S. Adult Mortality.” Demography 36(2):273–285. [PubMed] [Google Scholar]
- Idler Ellen. 2020. “Equal Protection? Differential Effects of Religious Attendance on Black-White Older Adult Mortality.” Innovation in Aging 4(S1):395. [Google Scholar]
- Idler Ellen, Blevins John, Kiser Mimi, and Hogue Carol. 2017. “Religion, a Social Determinant of Mortality? A 10-Year Follow-Up of the Health and Retirement Study.” PloS One 12(12):e0189134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. 2011. The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding. Washington, DC. The National Academies Press. Retrieved October 21, 2021. ( 10.17226/13128). [DOI] [PubMed] [Google Scholar]
- James Wesley, Cossman Jeralynn, and Wolf Julia Kay. 2018. “Persistence of Death in the United States: The Remarkably Different Mortality Patterns between America’s Heartland and Dixieland.” Demographic Research 39(33):897–910. [Google Scholar]
- Jelleyman Tim, and Spencer Nicole. 2008. “Residential Mobility in Childhood and Health Outcomes: A Systematic Review. Journal of Epidemiology and Community Health 62(7):584–592. [DOI] [PubMed] [Google Scholar]
- Jensen Leif, Monnat Shannon M., Green John J., Hunter Lori, and Sliwinski Martin J.. 2020. “Rural Population Health and Aging: Toward a Multilevel and Multidimensional Research Agenda for the 2020s.” American Journal of Public Health 110(9):1328–1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones Jeffrey M. 2021. “U.S. Church Membership Falls Below Majority for First Time.” Gallup. Retrieved October 21, 2021. (https://news.gallup.com/poll/341963/church-membership-falls-below-majority-first-time.aspx). [Google Scholar]
- Kuerbis Alexis. 2020. “Substance Use among Older Adults: An Update on Prevalence, Etiology, Assessment, and Intervention.” Gerontology 66(3):249–258. [DOI] [PubMed] [Google Scholar]
- Kuh Diana, and Ben-Shlomo Yoav. 2004. A Life Course Approach to Chronic Diseases Epidemiology. 2nd Ed. New York, NY: Oxford University Press. [Google Scholar]
- Lipka Michael. 2015. “5 Key Findings about Religiosity in the U.S. – and How It’s Changing.” Pew Research Center. Retrieved October 21, 2021. (https://www.pewresearch.org/fact-tank/2015/11/03/5-key-findings-about-religiosity-in-the-u-s-and-how-its-changing/). [Google Scholar]
- McKinlay John B. 1975. “A Case for Refocusing Upstream: The Political Economy of Illness.” Applying Behavioral Science to Cardiovascular Risk. [Google Scholar]
- Monnat Shannon M. 2018. “Factors Associated with County-Level Differences in U.S. Drug-Related Mortality Rates.” American Journal of Preventive Medicine 54(5):611–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monnat Shannon M. 2019. “The Contribution of Socioeconomic and Opioid Supply Factors to U.S. Drug Mortality Rates: Urban-Rural and Within-Rural Differences.” Journal of Rural Studies 68:319–335. [Google Scholar]
- Monnat Shannon M. 2020. “Trends in U.S. Working-Age non-Hispanic White Mortality: Rural-Urban and Within-Rural Differences.” Population Research and Policy Review 39:805–834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monnat Shannon M., Peters David J., Berg Mark, and Hochstetler Andrew. 2019. “Using Census Data to Understand County-Level Differences in Overall Drug Mortality and Opioid-Related Mortality by Opioid Type.” American Journal of Public Health 109:1084–1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montez Jennifer Karas, Beckfield Jason, Julene Kemp Cooney Jacob M. Grumbach, Hayward Mark D., Huseyin Zeyd Koytak Steven H. Woolf, and Zajacova Anna. 2020. “U.S. State Policies, Politics, and Life Expectancy.” The Milbank Quarterly 98(3):688–699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montez Jennifer Karas, Hayward Mark D., and Zajacova Anna. 2021. “Trends in U.S. Population Health: The Central Role of Policies, Politics, and Profits.” Journal of Health and Social Behavior 62(3):286–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montez Jennifer Karas, Zajacova Anna, Hayward Mark. D., Woolf Steven H., Chapman Derek, and Beckfield Jason. 2019. “Educational Disparities in Adult Mortality across U.S. States: How do they Differ, and Have they Changed Since the Mid-1980s?” Demography 56(2):621–644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray Christopher J. L., Kulkarni Sandeep C., Michaud Catherine, Tomijima Niels, Bulzacchelli Maria T., Iandiorio Terrell J., and Ezzati Majid. 2006. “Eight Americas: Investigating Mortality Disparities across Races, Counties, and Race-Counties in the United States.” PLoS Medicine 3(9):e260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine. 2021. High and Rising Mortality Rates Among Working-Age Adults. Washington, DC: The National Academies Press. [PubMed] [Google Scholar]
- Nisbet Paul A., Duberstein Paul R., Conwell Yeates, and Seidlitz Larry. 2000. “The Effect of Participation in Religious Activities on Suicide Versus Natural Death in Adults 50 and Older.” The Journal of Nervous and Mental Disease 188(8):543–546. [DOI] [PubMed] [Google Scholar]
- O’Brien Rourke, Neman Tiffany, Seltzer Nathan, Evans Linnea, and Venkataramani Atheendar. 2020. “Structural Racism, Economic Opportunity and Racial Health Disparities: Evidence from U.S. Counties.” SSM - Population Health 11:100564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oishi Shigehiro, and Schimmack Ulrich. 2010. “Residential Mobility, Well-Being, and Mortality.” Journal of Personality and Social Psychology 98(6):980–994. [DOI] [PubMed] [Google Scholar]
- Ofstedal Mary Beth, Chiu Chi-Tsun, Jagger Carol, Saito Yasuhiko, and Zimmer Zachary. 2019. “Religion, Life Expectancy, and Disability-Free Life Expectancy Among Older Women and Men in the United States.” The Journals of Gerontology: Series B 74(8):e107–e118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Opportunity Insights. Nd. Retrieved October 21, 2021 (https://opportunityinsights.org/).
- Peters David J., Monnat Shannon M., Hochstetler Andrew, and Berg Mark. 2020. “The Opioid Hydra: Understanding Overdose Mortality Epidemics and Syndemics Across the Rural-Urban Continuum.” Rural Sociology 85(3):589–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rand Center for Study of Aging. n.d. “RAND HRS Data Products.” RAND. Retrieved October 2021 (https://www.rand.org/well-being/social-and-behavioral-policy/centers/aging/dataprod.html). [Google Scholar]
- Raposa Elizabeth B., Laws Holly B., and Ansell Emily B.. 2016. “Prosocial Behavior Mitigates the Negative Effects of Stress in Everyday Life.” Clinical Psychological Science 4(4):691–698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rapp Kristen Schopp, Volpe Vanessa V., and Neukrug Hannah. 2021. “State-Level Sexism and Women’s Health Care Access in the United States: Differences by Race/Ethnicity, 2014-2019.” American Journal of Public Health 111(10):1796–1805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sasson Isaac. 2016. “Trends in life expectancy and lifespan variation by educational attainment: United States, 1990-2010.” Demography 53:269–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider Daniel, and Harknett Kristen. 2019. “Consequences of Routine Work-Schedule Instability for Worker Health and Well-being.” American Sociological Review 84(1):82–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz Shalom H. 2012. “An Overview of the Schwartz Theory of Basic Values.” Online Readings in Psychology and Culture 2(1). [Google Scholar]
- Smith James P. 2011. “Introduction to the Health and Retirement Study: An Evaluation and Scientific Ideas for the Future.” Forum for Health Economics & Policy 14(3):Article1. [Google Scholar]
- Stewart Scott H., Goldmann Anton, Neumann Tim, and Spies Claudia. 2010. “Biomarkers of Alcohol and other Drug Use.” Chapter 10 in Addiction Research Methods, edited by Miller PG, Strang J, and Miller PM. Hoboken, NJ: Wiley-Blackwell. [Google Scholar]
- Suh Hyungjun, Hill Terrence D., and Koenig Harold G.. 2019. “Religious Attendance and Biological Risk: A National Longitudinal Study of Older Adults.” Journal of Religion and Health 58(4): 1188–1202. [DOI] [PubMed] [Google Scholar]
- Temple University. n.d. “LawAtlas Project.” The Policy Surveillance Program. Retrieved October 2021 (https://lawatlas.org/). [Google Scholar]
- University of Southern California Dornsife Center for Economic and Social Research. 2015. “Gateway to Global Aging Data.” Gateway to Global Aging Data. Retrieved October 2021 (https://g2aging.org/#).
- U.S. Centers for Disease Control and Prevention (CDC). 2021. Climate Effects on Health. Retrieved October 21, 2021 (https://www.cdc.gov/climateandhealth/effects/default.htm).
- Verdery Ashton M., Smith-Greenaway Emily, Margolis Rachel, and Daw Jonathan. 2020. “Tracking the Reach of COVID-19 Kin Loss with a Bereavement Multiplier Applied to the United States.” Proceedings of the National Academy of Sciences 117(30):17695–17701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vierboom Yana C., Preston Samuel H., and Hendi Arun S.. 2019. “Rising Geographic Inequality in Mortality in the United States.” SSM-Population Health 9:100478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warren Robert J., Pfeffer Fabian, Helgertz Jonas, and Xu Dafeng. 2020. “Linking the U.S. Census Data to the Health and Retirement Survey: Technical Documentation.” HRS Documentation Report. Retrieved October 21, 2021 (https://hrs.isr.umich.edu/data-products/restricted-data/available-products/11132). [Google Scholar]
- Weber TJ, Hydock Chris, Ding William, Gardner Meryl, Jacob Pradeep, Mandel Naomi, Sprott David E., and Van Steenburg Eric. 2021. “Political Polarization: Challenges, Opportunities, and Hope for Consumer Welfare, Marketers, and Public Policy.” Journal of Public Policy & Marketing 40(2):184–205 [Google Scholar]
- Woolf Steven H., Masters Ryan K., and Aron Laudan Y.. 2021. “Effect of the Covid-19 Pandemic in 2020 on Life Expectancy Across Populations in the USA and Other High Income Countries: Simulations of Provisional Mortality Data.” BMJ 373:n1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zajacova Anna, and Lawrence Elizabeth. 2021. “Postsecondary Educational Attainment and Health among Younger U.S. Adults in the “College-for-All” Era. Socius. 10.1177/23780231211021197 [DOI] [Google Scholar]
- Zhang Jingwen, and Centola Damon. 2019. “Social Networks and Health: New Developments in Diffusion, Online and Offline.” Annual Review of Sociology 45:91–109. [Google Scholar]


