Abstract
Recognizing that electrically stimulating the motor cortex could relieve chronic pain sparked development of non-invasive technologies. In transcranial magnetic stimulation (TMS), electromagnetic coils held against the scalp influence underlying cortical firing. Multi-day repetitive TMS (rTMS) can induce long-lasting, potentially therapeutic, brain plasticity. Nearby ferromagnetic or electronic implants are contraindications, and adverse effects are minimal, primarily headaches. Single provoked seizures are very rare. TMS devices are marketed for depression and migraine in the U.S. and for multiple indications elsewhere. Although multiple studies report that high-frequency rTMS of motor cortex reduces neuropathic pain, their quality has been insufficient to support FDA application. Harvard’s Radcliffe Institute therefore sponsored a workshop to solicit advice from experts in TMS, pain research, and clinical trials. They recommended that researchers standardize and document all TMS parameters, and improve strategies for sham and double-blinding. Subjects should have common, well-characterized pain conditions amenable to motor-cortex rTMS and samples should be adequately powered. They recommended standardized assessment tools (e.g., NIH’s PROMIS) plus validated condition-specific instruments and consensus-recommended metrics (e.g. IMMPACT). Outcomes should include pain intensity and qualities, patient and clinician impression of change, and proportions achieving 30% and 50% pain relief. Secondary outcomes could include function, mood, sleep, and/or quality of life. Minimum required elements include sample sources, sizes, and demographics, recruitment methods, inclusion/exclusion criteria, baseline and post-treatment means and standard deviations, adverse effects, safety concerns, discontinuations, and medication-usage records. Outcomes should be monitored for at least 3 months post-initiation with pre-specified statistical analyses. Multi-group collaborations or registry studies may be needed for pivotal trials.
Keywords: neuropathic pain, neuromodulation, treatment, human, device
1. Transcranial magnetic stimulation (TMS): Principles and applications
TMS is being explored as a noninvasive alternative to invasive neurostimulation techniques such as deep brain stimulation and epidural cortical stimulation for treating neurological disorders and exploring brain function. First demonstrated in 1985 [13], TMS uses electromagnetic induction to electrically influence nearby cells. Strong effects can depolarize neurons sufficiently to trigger action potentials. Low-intensity TMS appears to mostly stimulate low-threshold inhibitory interneurons, whereas higher intensities excite projection neurons [93]. TMS pulses can be applied singly, but for therapeutic use, multiple pulses are rapidly applied, (repetitive-TMS; rTMS).
1.1 Insights from studies of invasive brain stimulation for treating pain
TMS emerged from experience with invasive brain stimulation. Neurosurgical motor cortex stimulation (MCS) and deep brain stimulation (DBS) are proven effective for treating chronic pain (typically defined as more than 40% reduction of pain scores for at least 12 months post- implantation). Epidural MCS involves surgically opening the skull to attach an electrode array to dura directly above the motor cortex. Subdural electrodes, although still used, convey additional risk from breaching the dura.
A 2009 systematic review reported evidence from 14 studies that intracranial MCS is safe and effective for treating neuropathic pain (NP). Half of patients reported at least 40–50% pain reduction with best outcomes for central post-stroke pain and neuropathic facial pain [32]. Systematic review by the European Federation of Neurological Societies also found MCS efficacious for central post-stroke and facial pain [21]. In a series of 100 consecutive patients, 80% with post-stroke-pain and 56% with pain from spinal cord injury benefited [79]. In the four small randomized controlled trials (RCT) of MCS for central and peripheral NP with at least 12-month follow-up, about 60% were responders [61;63;67;117]. Not surprisingly, metanalysis found that intracranial motor cortex stimulation is more effective than extracranial stimulation, so patients with partial pain relief after rTMS should consider implanted MCS [71] especially since pain relief from high-frequency rTMS predicts success of later MCS [11;68].
DBS is a more-invasive technique in which electrodes are implanted through the skull, dura, and brain to stimulate deep targets. Stimulation sites for treating pain include the periventricular/periaqueductal grey matter (PVG/PAG), internal capsule, and sensory thalamus. Metanalysis indicated that long-term success is most common after DBS of the PVG/PAG (79%), or the PVG/PAG plus sensory thalamus/internal capsule (87%); stimulating the thalamus alone was less effective (58%) [15]. Two controlled non-randomized prospective studies [43;91], multiple uncontrolled retrospective studies, and a recent large retrospective study [102] together indicate that over 80% of patients with intractable low back pain (failed back surgery) and 58% of patients with post-stroke pain achieved long-lasting relief, with even higher rates for phantom limb pain and polyneuropathies [15].
MCS and DBS should be more effective than rTMS, as they directly contact target neurons and can be administered continually, but their use is limited in part by cost and complications, which include infections in 5–15% of cases [32;110] and technical failures (e.g., electrode migration, fractures, skin erosion) in 1/4 of cases [31;88]. DBS, which conveys risk of brain hemorrhage, causes permanent harm in less than 1% of patients [106]. Minor side effects (e.g., muscle contraction or tingling) are common and often ameliorated by changing stimulation parameters. Epidural hematomas are a rare concern, and other complications are minor and transient, including a seizure during programming trials in 12%, infections in 6%, and technical failures in 5% [31]. This combination of demonstrated efficacy but high cost and significant risk drove the development of non-invasive modalities such as rTMS.
1.2 Technical basis of TMS
To summarize how TMS works, capacitors in a pulse generator are rapidly charged and then discharged by a thyristor trigger switch to send brief currents through coils of conductive wire to produce brief, rapidly changing magnetic fields. These induce local electric fields that cause current to flow in any conducting structures within a few cm according to Faraday’s law (Figure 1A). The characteristic click of discharging TMS coils is caused by Lorenz forces that mutually repel adjacent windings. TMS coils thus must be tightly encapsulated to hold together, which imposes limits on design and use. Plus, coils heat the during prolonged repeated use, so they may need to be cooled or interchanged with a spare coil to prevent overheating. Other design considerations include focality and depth of penetration. The most common figure-of-8 coils (two adjacent circular coils with counter-rotatory currents (Figure 1)) provide more focal stimulation than single-circle coils [50], and newer configurations, such as the double-cone or H-coil reportedly deepen penetration [27].
Fig. 1.
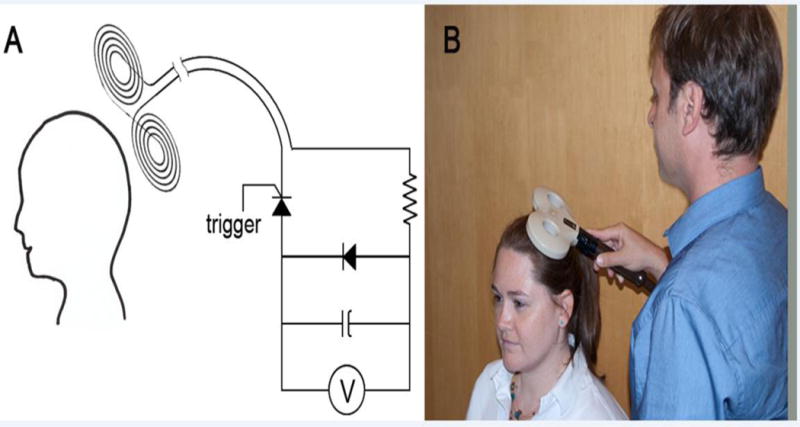
A) Schematic of the electrical circuits that underlie TMS: A capacitor or group of capacitors is charged by a high voltage power supply (V). They are then discharged by a thyristor trigger switch to send a rapidly changing current through the coil, which produces a transient magnetic field locally. This penetrates through the scalp, skull, meninges and cerebrospinal fluid to induce a current pulse that transiently changes the polarization across the cell membrane of underlying cells. Specific conditions can depolarize some neurons sufficiently to trigger an action potential, which propagates along that neuron’s pre-existing anatomical connections. B) Depiction of TMS administration using a figure-of-8 coil to stimulate the primary (M1) motor cortex.
1.3 Using repetitive TMS (rTMS) for medical therapy
The rationale for applying rTMS to treat neurological or psychiatric disorders is that it can change the brain to produce effects that last beyond the duration of stimulation. Such “plasticity” underlies normal brain functions such as learning, adaptation to changes, and recovery from brain injury. Different TMS application patterns have different effects. Generally, early changes involve altering synaptic strength whereas longer exposures trigger longer-lasting anatomical changes such as sprouting and alterations of dendritic spines. By analogy to basic synaptic physiology, strengthening synaptic strength is often referred to as long-term potentiation (LTP) and reducing synaptic strength is called long-term depression (LTD).
Depending on how it is applied, rTMS can induce either LTP or LTD [101], since high-frequency rTMS (5 Hz or faster) increases excitability, whereas slow rTMS at about 1 Hz decreases it. The mechanism of increased excitability after rapid rTMS may involve weakened intracortical inhibition [54]. “Theta burst TMS” is delivery of 5 Hz trains of clusters of 3 TMS stimuli at 50 ms intervals. Long trains of theta burst TMS lead to depression, whereas periodic short trains increase excitability [49]. Quadripulse TMS involves delivering clusters of 4 pulses at different intervals. Short intervals of about 5 ms in the cluster lead to facilitation, whereas longer intervals (e.g., 50–100 ms) cause depression.
Psychiatric applications of rTMS include obsessive compulsive disorder and suppressing hallucinations, but use for medication-resistant depression is currently most successful and approved for clinical marketing in multiple countries (see Section 4.3). A recent systematic review found level A evidence supporting this use [59]. The rationale comes from the success of electroconvulsive therapy and observations that depressed patients have hypometabolism of the left dorsolateral prefrontal cortex (DLPFC). This is ameliorated (along with the depression) by repeated rapid rTMS delivered to the left DLPFC, which affects a cortico-subcortical network involved in mood regulation [34].
Currently in the U.S., the only FDA-approved neurological indication for TMS is acute migraine with aura [34;72]. In Europe other devices, e.g., from Magstim Inc., MagVenture, Nexstim, and Neuronix have also obtained CE Mark and are applied clinically for multiple neurological disorders including pain, dementia, stroke recovery, epilepsy, and movement disorders. Parkinson’s disease research followed a similar logic to depression, namely since motor-cortex excitability is low, increasing it with rapid rTMS might improve movement, but so far, benefits have been too mild for clinical approval. Of note, motor-cortex rTMS augments dopamine release in the striatum [112]. While probably not its major mechanism, this illustrates that the mechanisms of TMS effects are still not fully understood. Since tinnitus involves overactivity of the auditory cortex, slow rTMS is used to suppress it [113] but clinical utility is uncertain. Epilepsy is also treated with suppressive TMS. Improving recovery from stroke is complex and may require increasing and decreasing different types of cortical excitability [59].
1.4 Parameters of TMS administration
Multiple technical parameters contribute to the effects of TMS and those described in Table 1 should be specified in publications. Pulse intensity influences safety and is usually tailored to individual subjects’ threshold for inducing a motor response (muscle twitch). Regarding pulse frequency, 10 Hz or 20 Hz have been most common in pain research. However, since prolonged high frequency stimulation increases risk (see below), rTMS is usually applied in “trains” of pulses interspersed with rest periods. Train length and inter-train interval thus also need to be specified. Most prior studies did not fully report these technical parameters, hindering reproducibility and metanalysis. Improving sham TMS [23] is another technical priority. Double-blinding researchers plus subjects, as expected for medication trials, is exceedingly difficult with devices. Parameters pertinent to blinding TMS subjects include: A) the auditory click of coil discharge, B) the visual stimulation including coil location and orientation, C) the touch of the coil tapping, D) the electrical sensation associated with activating scalp muscles, and E) avoiding brain stimulation. Hardly any prior studies addressed these fully. Future studies should consider reporting to what extent their sham meets each consideration. For instance, inert sham coils offer visual, tactile, and sometimes auditory stimuli, but the lack of electrical sensations unblinds experienced subjects. An active coil angled so only one wing touches the scalp [52], or nonconductive spacers between the coil and scalp, satisfy the A and partially satisfy the B,C, D requirements. Adding electrodes for electrical stimulation can satisfy D [17;48]. The E criterion is better met by a spacer of appropriate thickness than by coil angling, which is also hard to standardize. Another strategy for sham is to stimulate cortex expected to lack relevant effect, such as the vertex [23], which controls for A-D. However, pain processing is highly distributed throughout the brain. A small study recently demonstrated a trend towards reduction of acute pain after rTMS application to occipital cortex [105], and this approach was considered unacceptable in a recent systematic review [59]. Blinding TMS administrators is even more difficult and currently best addressed by coils that can be remotely programmed to deliver sham or true pulses, for instance by opposing current flow within the loops to cancel their magnetic fields [47] or with a commercially available sham-capable system such as a MagVenture MagPro.
Table 1.
Minimum technical parameters to describe a TMS study
| Category | Parameters |
|---|---|
| Coil design | Shape Size |
| Coil placement | Coil orientation Stimulation site Method for locating stimulation site |
| Stimulation parameters | Pulse intensity (as %RMT) Pulse frequency Train length Train duration Number of trains Inter-train interval |
| Session parameters | Total pulses per session Total number of sessions Between session intervals (e.g., weekday, every consecutive day) Maintenance session parameters |
| Sham conditions | Strategies for allocation concealment Extent of blinding of subjects and administrators Control of auditory, visual, tactile, electrical effects Were subjects asked to identify real vs. sham? Were subjects asked to rate sensory and/or auditory and visual sensations? |
1.5 Safe administration of rTMS
As for most trials of potential therapies, benefit to research subjects is assumed to be nil, thus even relative risks acceptable for some medical uses will usually disqualify subjects for research study. Single-pulse TMS has no long lasting effects but rTMS conveys a few risks that must be minimized by proper patient selection and technique. A 2009 international consensus meeting established safety precautions that are universally endorsed [104]. The most important potential adverse event (AE), heating, moving, or damaging ferromagnetic implants including electronic devices in or near the head, is managed by strictly excluding patients with such devices or ferromagnetic fragments. These restrictions are similar to those for magnetic resonance imaging (MRI). Patients with pain should be queried specifically about prior neurosurgical procedures, and the presence of neural stimulators or pumps.
For the vast majority of people without implants, the only known significant risk is inducing a single seizure during TMS. The risk is small, estimated at ≤ 1/10,000 [104] among all rTMS studies to-date. Only two seizures have been reported among more than 30 published studies of rTMS for pain [57;83;98] in which safety recommendations were followed [104]. The total number of pulses, pulse intensity and frequency must be carefully chosen, particularly for high frequency (> 10 Hz) rTMS. A single induced seizure does not increase the risk for epilepsy (recurrent seizures), and one seizure in a monitored medical setting is unlikely to cause serious harm, but all TMS facilities need explicit plans for providing rapid medical response in the event of an induced seizure. Since risk is higher in people with prior seizures or brain lesions, or use of medications that reduce the seizure threshold (see Section 4.2), these are considered relative contraindications to medical use of TMS (Table 2). The possibility of inducing cognitive changes is a valid concern that requires further study. The limited data so far show no cognitive changes after 3 months of motor cortex rTMS for treating pain [14].
Table 2.
Contraindications to medical use of TMS
| Absolute contraindications | Very strong contraindications | Relative contraindications | |
|---|---|---|---|
| Regarding ferromagnetic metal | Ferromagnetic metal in the head (e.g., plates or pins, bullets, shrapnel) | Ferromagnetic metal in the neck or chest | |
| Regarding microprocessors | Microprocessor implants in the head (e.g., cochlear implants) or life-sustaining microprocessor implants anywhere in the body (e.g. prosthetic cardiac valves) | Microprocessor implants in the neck (e.g. vagus nerve stimulator) | Microprocessor implants below the neck (e.g. spinal pumps, stimulators) |
| Regarding seizure risk | Epilepsy or prior induced seizures | Prior brain lesions, major head trauma, medications that lower seizure threshold, recent withdrawal from sedative medications that raise seizure risk (e.g., alcohol, barbiturate) | |
| Miscellaneous | Pregnancy | Hearing loss, tinnitus |
The most common AE of TMS is headache, reported in one study in up to 42% of participants having active rTMS and 33% having sham TMS [83]. These may be caused by pressing the coil against subjects’ heads for extended periods or by the muscle contractions induced. Most are mild and respond to over-the-counter treatments. Other reported AEs include pain at the stimulation site, neck pain, muscle aches, dizziness, nausea, tiredness and tinnitus [75]. Of note, metanalysis reveals that AE are no more common after real than after sham-TMS [83]. Lastly, as for MRI, patients should wear earplugs to minimize noise exposure from coil discharge and thus reduce the risk of transient threshold shifts or hearing loss.
2. What is already established about rTMS for treating pain?
TMS activates short intracortical interneurons and long axons connected with distant structures [61;63]. Passing axons–particularly those with bends–are more easily excited than cell bodies [80] and therefore, rTMS has remote effects. Motor-cortex rTMS oriented posteroanteriorly and parallel to the midsagittal plane preferentially activates horizontal cortical axons running parallel to the surface [11;66]. Early studies of dural MCS implicated antidromic activation of thalamocortical pathways [115], and recent studies show that integrity of the thalamocortical tracts is required to treat pain [89]. Imaging shows that MCS additionally affects structures involved in affective, cognitive, and emotional aspects of pain, such as the cingulate and orbitofrontal cortices [38], perhaps by influencing opioidergic or gamma-aminobutyric acid transmission [74].
For treatment, research has established that a figure-of-8 coil delivering biphasic pulses should be placed over the precentral gyrus (primary motor cortex) contralateral to the painful side with a posteroanterior orientation (Figure 1B). High frequency (10 or 20 Hz) should be used to activate projecting axons as well as local interneurons [11]. It should be applied below the threshold for motor activation to avoid triggering muscle contractions. Proof-of-principle studies demonstrate that repeated rTMS sessions can produce cumulative pain reductions for at least several weeks after 10 consecutive weekday sessions [52], but the optimal timing for long-term efficacy and safety are undefined. Many labs empirically use 10 consecutive weekday “induction” sessions followed by a “maintenance” phase comprising 3 sessions a week apart, 3 sessions a fortnight apart, then 3 sessions a month apart [78]. It is also largely unexplored whether rTMS should also be considered for acute pain, such as postoperatively and whether efficacy might be augmented by combining rTMS with medications or physical therapy [98]. Regarding where best to administer rTMS to relieve pain, it is still debated whether the cortical representation of the painful body region should be targeted or adjacent cortex in the precentral gyrus [65]. If precise targeting is important, it needs to be clarified whether or not image-guided navigation systems [5], which are expensive and require subjects to obtain MRI, improve efficacy. There may also be other potential cortical targets such as the posterior insula, the right secondary somatosensory cortex (SII) or the DLPFC, although one study finds DLPFC stimulation ineffective for post-stroke pain [25;108].
Two 2014 systematic reviews synthesize the results of published rTMS studies for chronic pain. Both find rTMS efficacious, but the evidence for neuropathic pain appears strongest. The Cochrane metanalysis of all pain indications stated that “the pooled estimate approaches the threshold of minimal clinical significance” [83]. However, a consortium of European experts found level A evidence of “definite efficacy” of high frequency rTMS of the primary motor cortex for neuropathic pain [59]. Both reviews emphasize the need to improve the quality of future trials.
3. Which conditions are most suitable for studies of repetitive TMS (rTMS) for treating pain?
Some pain syndromes are more appropriate for research than others. rTMS has not usually been considered for treating acute or nociceptive/inflammatory pain, presumably because the standard of care is to resolve its underlying cause. However, not all causes can be cured, and there is evidence of efficacy of rTMS for chronic visceral pain including cancer [111] and even for transient syndromes such as postoperative pain [16] and aborting migraine headache with aura [72]. Neuropathic pain syndromes are reported to benefit most from rTMS of the motor cortex [59], but some chronic-pain syndromes labeled as “non-neuropathic” [59] include conditions such as CRPS-I and fibromyalgia that have been associated with nerve injury [7;39;85–87]. Focal lesions with defined onset, for instance from shingles or trauma, have the advantage of known localization and time of onset, but early cases often improve spontaneously, which complicates outcome, so established cases, for instance of more than a year’s duration, are preferable.
3.1 Central pain (CP) from lesions of the brain or spinal cord
NP is common in multiple sclerosis (MS) affecting between 14–28% of patients [114]. A survey of over 10,000 MS patients reported some evidence of NP in 75%, rated by half as severe [42]. A long-term prospective study of 15,754 stroke patients identified CP in 2.7% [84]. There are few trials of any treatments for CP, so guidelines come from studies of peripheral neuropathic pain, despite uncertain relevance [12]. The highest quality study found pregabalin not superior to placebo for post-stroke pain [53]. The only adequately powered drug trial with positive results for CP found pregabalin efficacious for spinal-cord injury (SCI) [109]. The only trial for MS pain found uncertain benefit of cannabinoids [56].
In contrast, most among the small RCTs report efficacy of rTMS in CP [10;11], but stimulation location and frequency seem to matter. For SCI, which causes predominantly torso and leg pain, a sham-controlled trial in 111 patients showed benefits for overall and worst pain when the motor-cortex representation of the hand was targeted at 10 Hz [51], whereas a double-blinded, placebo-controlled study of 17 SCI patients stimulated at 10 Hz at the vertex (closer to the leg cortex) was negative [122], as was a study of 5 Hz vertex stimulation [26]. Ten sessions of 5 Hz rTMS applied to cortex innervating the painful area in 64 patients with predominantly central NP had intermediate results, namely transient reduction in mean pain [48]. For post-stroke CP, 5 sessions of MRI-guided 10 Hz rTMS applied to motor cortex innervating the painful area gave modest pain relief in 14 patients for up to 4 weeks [45]. Pain relief correlated with improved warmth perception in the painful area [45;63]. Single 10 Hz rTMS sessions applied to the hand site (regardless of the site of pain) gave short-term relief and suggested that pain caused by brainstem strokes responds less than pain from supratentorial strokes [64]. A well-designed, double-blind, placebo-controlled study found that 10 sessions of 10 Hz rTMS applied to the left DLPFC did not relieve post-stroke pain [25].
3.2. Facial neuropathic pain
There are effective pharmacological and surgical treatments for classic trigeminal neuralgia, but these are not universally efficacious, and there are few treatments for other types of facial NP. The overall prevalence of facial NP is unknown, but causes other than classical trigeminal neuralgia are common. Significant proportions of patients with idiopathic facial pain have evidence of neuropathic mechanisms [33]. Systematic reviews of case series report moderate-to-good outcomes from epidural MCS in facial NP, with 68% responding initially, and 50% of implanted patients benefiting at one year [21;31]. For rTMS, multiple studies suggest that facial NP responds better than other types of NP [64;69], making it a leading candidate for rTMS trials.
3.3 Postherpetic neuralgia
PHN is the 2nd most common neuropathic-pain condition for pain-medication trials because it is so common (1/3–1/2 lifetime prevalence [92]) and etiology, localization, and onset are evident. PHN is dermatomal-centered pain caused by damage to sensorineural cell-bodies within one trigeminal or spinal ganglia caused by shingles (zoster). Early PHN improves spontaneously, which complicates trials. PHN risk is age-dependent with patients over age 70 having more than a 50% risk of pain lasting at least a year [24]. It can affect any location but the torso and first trigeminal ganglion are most common. Many studies evaluating rTMS included PHN patients.
3.4 Fibromyalgia (FM) and painful small-fiber polyneuropathy (SFPN)
FM is a globally prevalent, well-studied, widespread-pain syndrome affecting 1–5% of the population. Recent consensus criteria for diagnosis and scoring are useful for trials [120]. Several well-designed studies, including one reporting long-term efficacy of maintenance rTMS, require external confirmation [14;78;94]. A 2013 systematic review found high-frequency rTMS to motor cortex efficacious for FM [77] but a small 2014 study did not find benefit for average daily pain [18]. Multiple new studies report evidence of small-fiber polyneuropathy (SFPN) among FM patients, e.g. [86][85;86], meaning this population may be heterogenous.
SFPN is highly prevalent although most cases remain undiagnosed and complex tests are required to confirm diagnosis [8]. Diabetic polyneuropathy is overall the most-trialed neuropathic-pain condition. Advantages for trials include high and increasing prevalence, global relevance, and widespread availability of inexpensive blood tests for hyperglycemia. Cancer chemotherapy, another common cause of painful polyneuropathy, has unique advantages since it is pre-planned and temporal precise. Pretreatment data can be obtained. Research tools for diabetic polyneuropathy are well-developed, less so for other causes. A potential disadvantage is that the motor cortex representation of the feet is not easily accessible transcranially (Figure 2), although evidence from patients with central causes of foot pain (see above) supports off-site stimulation. The cooled, Hesed (H)-coil, that reportedly allows deeper penetration of TMS is reported as efficacious for painful diabetic polyneuropathy [90].
Fig. 2.
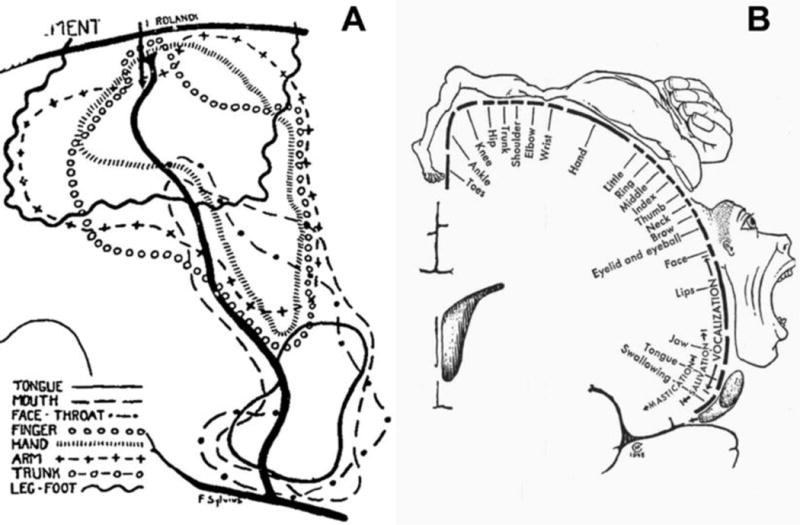
Pictorial representations of the anatomical targets of neurons within the primary motor cortex located in the precentral gyrus in the brain’s frontal lobe. The amount of cortex devoted to each body region is proportional to how richly innervated that region is, not to its actual size, which creates a distorted representation of the body called a “homunculus”. Neurosurgeon Wilder Graves Penfield (1891–1976), a trainee of Osler, Cushing, and Sherrington, mapped brain functions while developing neurosurgical treatments for epilepsy as the founding director of the Montreal Neurological Institute at McGill University. While operating, he used electrical stimulation to map “eloquent” portions of each patient’s exposed brain to minimize surgical damage [100].
(A) A map of the motor cortex published in 1937 by Penfield and Boldrey based on electrical exploration of the cortex of 163 awake, cooperative patients with craniotomies [96]. The lines enclose the areas within which electrical stimulation of exposed cortex triggered a movement in that part of the body.
(B) This anatomical homunculus based on the work of Penfield and colleagues was drawn for illustrative purposes by medical artist Hortense Cantile [97][94]. Although oversimplified and criticized, the motor and sensory homunculi continue to be widely reproduced to educate about brain function[97].
3.5 Less-studied conditions
Back and neck pain must be considered because of their prevalence, although there are no rTMS studies so far. Potential disadvantages include the fact that their causes are usually mixed, the torso has less cortical representation (Figure 2), and there are strong psychosocial influences [19]. Focal or regional pain disorders have the advantage of being common but the disadvantage of being heterogenous in location and cause. The most common cause of unilateral distal neuropathy is trauma–often medical or military–with occasional internal causes, for instance in carpal tunnel syndrome. Post-traumatic neuralgias with additional visible signs, termed “complex regional pain syndrome” have been studied in two small trials of motor-cortex rTMS totaling 32 patients [98;99]. Spinal radicular pain, usually from osteoarthritis, is very common and a likely future target. There is preliminary evidence of efficacy of motor cortex rTMS for brachial plexus lesions [62]. Phantom-limb pain is associated with cortical reorganization, making rTMS an attractive option that has not yet been studied.
4. Designing clinical trials of rTMS for pain
Many prior studies not only often fail to report all technical parameters (Section 1), but also lack the details needed to measure effect sizes, to permit calculating sample-sizes for future studies, and to perform metanalysis. Minimum required elements should include baseline plus post-treatment means and standard deviations for all primary outcomes. Exact sample sizes, full inclusion and exclusion criteria, methods of allocation concealment, subjects’ demographic and medical characteristics, plus the source of subjects (e.g., community vs. hospital), and recruitment methods should be specified. Studies should document ethical approval, monitor safety, and report all AEs and reasons for subject withdrawal or discontinuation. For chronic pain, it is important that benefits and risks be assessed for long enough, meaning that primary outcomes should usually be monitored for at least 3 months after treatment initiation. All statistical analyses should be pre-specified. The field is not yet mature enough to know the utility of biomarkers (e.g., gene sequences or imaging) as outcomes, but banking this information for future evaluation should be encouraged.
4.1 Outcome measures
The literature describing rTMS for pain indications resembles that for interventional pain therapies in that few patients are studied, often in uncontrolled case series, with non-uniform case definitions and outcomes, as summarized in Table 3. Research standards have progressed towards increased rigor and objectivity, and using recommended outcomes would strengthen the field. The usual primary outcome (endpoint) is treatment efficacy or effectiveness (which incorporates tolerability and ease of use as well as efficacy) for reducing pain. Pain intensity scales such as the numeric pain rating scales (NPRS) or visual analog scale (VAS) are validated and universally accepted. Mean change from baseline, and responder analyses (30% and 50%) may also be appropriate.
Table 3.
Outcome measures used in published studies of multi-day rTMS applied to primary motor cortex to treat chronic neuropathic pain
| Study (see references below) | A | B | C | D | E | F | G | H | I | J | K | L | M | N | O |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| General Pain | |||||||||||||||
|
| |||||||||||||||
| Numeric Pain Rating Scale (NPRS) | X | X | X | ||||||||||||
| Visual Analogue Scale (VAS) for pain | X | X | X | X | X | X | X | X | X | X | |||||
| Brief Pain Inventory (BPI) | X | X | X | ||||||||||||
| McGill Pain Questionnaire (MPQ) | X | X | X | X | |||||||||||
| Short form McGill Pain Questionnaire (SF-MPQ) | X | ||||||||||||||
| Brazilian Profile of Chronic Pain: Screen (B-PCP:S) | X | ||||||||||||||
| Pain Impact questionnaire (PIQ-6) | X | ||||||||||||||
|
| |||||||||||||||
| Neuropathic Pain | |||||||||||||||
| Douleur Neuropathique en 4 Questions (DN4) | X | X | |||||||||||||
| Neuropathic Pain Symptom Inventory (NPSI) | X | ||||||||||||||
| The Leeds Assessment of Neuropathic Symptoms and Signs (LANSS) | X | X | |||||||||||||
|
| |||||||||||||||
| Depression/Anxiety | |||||||||||||||
| Beck Depression Inventory (BDI) | X | X | X | X | X | X | X | X | |||||||
| Hamilton Depression Rating Scale (HDRS) | X | X | |||||||||||||
| Hospital Anxiety and Depression Scale (HAD) | X | X | X | ||||||||||||
| Hamilton Anxiety Rating Scale (HARS) | X | ||||||||||||||
| State-Trait Anxiety Inventory (STAI) | X | ||||||||||||||
| Pain Catastrophizing Scale (PCS) | X | X | |||||||||||||
|
| |||||||||||||||
| Disability | |||||||||||||||
| Disabilities of the Arm, Shoulder and Hand (DASH) | X | ||||||||||||||
| The 36-Item Short Form Health Survey (SF-36) | X | X | X | ||||||||||||
|
| |||||||||||||||
| General | |||||||||||||||
| Linkert Scale (satisfaction with treatment) | X | ||||||||||||||
| Patient Global Impression of Change (PGIC) | X | X | |||||||||||||
|
| |||||||||||||||
| Sleep | |||||||||||||||
| Pittsburgh Sleep Quality Index (PSQI) | X | ||||||||||||||
|
| |||||||||||||||
| Disease Specific | |||||||||||||||
| Fibromyalgia Impact Questionnaire (FIQ) | X | X | X | X | |||||||||||
A: Khedr et al., JNNP 2005 [52]. B: Passard et al., Brain 2007 [94]. C: Defrin et al., Arch Phys Med Rehabil 2007 [26]. D: Kang et al., Arch PM&R 2009 [51]. E: Picarelli et al., J of Pain 2010 [98]. F: Mhalla et al., PAIN 2011 [78] G: Lee et al., Am J PM&R 2012 [57]. H: Lefaucheur et al., EJP 2012 [60]. I: Hosomi et al., PAIN 2013 [48]. J: Onesti et al., PAIN 2013 [90]. K: Fricová et al., Physiol. Res. 2013 [37]. L: Hasan et al., Neuromodulation Journal 2014 [45]. M: Dall’Agnol et al., J of Pain 2014 [22]. N: Boyer et al., Neurology 2014 [18]. O: Yýlmaz et al., J of Spinal Cord Medicine 2014 [122].
Secondary outcomes are encouraged to provide added information, such as effects on activities of daily living, disability, quality of life, decreases in medication use, and subject satisfaction. Secondary outcomes now often include patient-reported health-related quality of life (HRQOL). Another patient-centered trend influencing outcome measures is shared medical decision making [118]. Effects of treatment on health-care utilization is an outcome of increasing relevance given the importance of reducing medical costs. Section 4.2 discusses monitoring concomitant medications. Every TMS study should document ethical approval, monitor safety, and report all AE and reasons for subject withdrawal or discontinuation [28], but metanalysis of 30 trials of rTMS for pain revealed that 17 did not report any information regarding AE [83]. We recommend active capture questionnaires for more sensitive and detailed monitoring than passive capture or general inquiry. These should include participant ratings of frequency, severity, importance, and associated distress.
The proceedings of the “Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials (IMMPACT)” meetings provide consensus guidelines about outcomes of pain-treatment trials. These identified six core domains to consider: Pain, physical functioning, emotional functioning, participant ratings of improvement and satisfaction with treatment, symptoms and AEs, and participant disposition [116], and proposed specific core outcome measures (Table 4) to consider in designing studies of chronic-pain treatments [28]. The balance between generic and focused instruments is important. Generic instruments facilitate comparison with data from other healthy or ill cohorts and facilitate collaboration (see Section 4.4), whereas condition-specific instruments may better capture disease-specific concerns [119]. For example, the 36-item Medical Outcomes Study Short-Form Questionnaire (SF-36) was designed to assess overall health of populations in which no one disease is excessively prevalent. Unless supplemented by questions targeting mental health, physical function and other domains important for assessing HRQOL, the SF-36 lacks the sensitivity necessary for decisions about whether a specific treatment is working at the N-of-1 level [103]. The voluminous array of generic and specific HRQOL assessment instruments is summarized in monographs and web-based repositories of open-access questionnaires and other instruments [103]. The IASP suggests that “for future NP trials, pain relief scales, patient and clinician global impression of change, the proportion of responders (50% and 30% pain relief), validated NP quality measures and assessment of sleep, mood, functional capacity and quality of life are recommended” [41]. A recent high-quality trial of motor-cortex rTMS included most of these outcomes and also measured depression [48]. This approach to outcome assessment can help demonstrate that any pain relief is not merely a non-specific correlate of treating depression.
Table 4.
The IMMPACT-II recommendations for core outcome measures to be considered in clinical trials of chronic pain treatment efficacy and effectiveness; reprinted with permission from [27].
| Pain |
|
| Physical functioning (either one of two measures) |
|
| Emotional functioning (at least one of two measures) |
|
| Participant ratings of global improvement and satisfaction with treatment |
|
| Symptoms and adverse events (AE) |
|
| Participant disposition |
|
Because TMS and other device trials study fewer subjects than drug trials, information provided by each enrollee should be maximized. Descriptions of enrollees’ demographics and TMS parameters must meet or surpass recent consensus recommendations [20]. Variables such as gender, age, and ethnicity should always be reported. As discussed above, studying homogenous groups of patients with at least moderate pain intensity can maximize signal-to-noise ratio [29] and training subjects at enrollment may reduce variability and reporting errors.
4.2 Use of concomitant medications, therapies, and other environmental factors
Medication use is a common secondary outcome that must be monitored in trials of rTMS since medications (and other therapies and environmental conditions) can modify effectiveness and safety (Table 4) [28]. Plus, a goal of many non-pharmacological pain treatments is to enable patients to reduce or discontinue high doses of undesirable pain medications (viz opioids). Due to ethical considerations, studies of rTMS for pain have primarily been conducted in patients using other (insufficient or poorly tolerated) pain therapies, which often include multiple neuroactive medications. Patients with chronic pain often use multiple classes of pain medications, more than one medication in a class, and even multiple formulations of the same medication (e.g., long- and short-acting opioids), plus, medications are taken variably according to need, so accurate documentation is difficult.
One simple metric is to quantify use of approved “rescue” analgesics; another is to track proportions of subjects taking various classes of pain medications [30]. It is possible to quantitate overall opioid consumption using morphine equivalents, but conversion tables do not accommodate individual differences in pharmacokinetics and pharmacodynamics, and in any case are applicable only to opioids. Real-time using medication diaries may improve the depth and accuracy of data collection. The Medication Quantification Scale combines drug class, dose, and detriment (risk) to compute a single numeric medication profile value [44]. There are few metrics for other pain co-treatments including alternative, over-the-counter, herbal and folk remedies and physical-medicine treatments. At a minimum, rTMS studies should include detailed records of all medication use, including specific doses, and recording of non-medical pain therapies. Large registry studies may be needed to analyze these complex variables. Since co-treatments add “noise” to clinical trials that can obscure signals, consideration should be given to trials of “stand-alone” rTMS.
Monitoring recent as well as current consumption, and non-prescribed as well as prescribed medications is required to screen for study eligibility and ensure subject safety. Potentially problematic prescription medications used by some patients having pain include tricyclics (e.g., nortriptyline, amitriptyline), antiviral medications, and antipsychotic medications (chlorpromazine, clozapine), but there are no analyses measuring how each medication alters seizure risk and few TMS publications even fully describe subjects’ medications and doses. Consuming or discontinuing commonly abused substances can increase cortical excitability and risk of a TMS-induced seizure (Table 2) [104]. Withdrawal from sedatives (e.g., alcohol, barbiturates, benzodiazepines, meprobamate, and chloral hydrate) increases seizure risk so patients must be asked about recent as well as current use, and recent substance abuse should be an exclusion criterion. Other potentially problematic drugs of abuse include phencyclidine, amphetamines, ketamine, and gamma-hydroxybutyrate. Establishing a national or a global registry to report and fully document every case of TMS-induced seizures is recommended to better characterize specific risk factors since these are far too rare for individual centers to acquire enough cases to study.
There are yet additional parameters to consider recording for potential future use, including state of mind and health at the time of the study, and use of non-prescription neuroactive substances such as caffeine [20]. Sleep deficits alter cortical excitability, and given the efficacy of ketogenic diets in suppressing the cortical excitability that causes seizures [73], low-carbohydrate diets could conceivably influence the outcomes of rTMS. One study coupled rTMS with behavioral training to increase benefit for tinnitus [121]. However, rTMS studies have not been designed or powered to assess these added variables and there are currently no validated methods for data collection and analysis. Large collaborative studies or registries (Section 4.4) plus real-time data entry by subjects or passive capture by monitoring devices will be necessary. “Health connectivity” is an emerging trend in medicine and public health, so these parameters may soon become available.
4.3 Regulatory considerations
Authorization processes vary in different countries and influence the pace of clinical application of TMS. There are differences in risk classification, transparency, and rigor of assessment of safety and effectiveness. For medical devices, the U.S. FDA, the Canadian Therapeutic Products Directorate (TPD), and the Australian Therapeutic Goods Administration (TGA) require evidence of clinical efficacy, device quality and performance, as well as safety, whereas Europe has emphasized safety and performance over efficacy, thus European CE marking typically precedes U.S. clearance by 2–5 years [55]. For a device to be legally marketed in the European Union (E.U.), the requirements of the European Medical Device Directives must be met and a CE Mark obtained from the European Commission. Directive 93/42/EEC and its subsequent amendments regulate medical devices such as TMS.
The U.S. FDA’s Center for Devices and Radiological Health (CDRH) and the European Commission have approved TMS devices for several indications. The Japanese Pharmaceuticals and Medical Devices Agency (PMDA) requires compliance with the Pharmaceutical and Medical Device Law (PMDL), and in 2013, Brainsway announced plans to seek permission to market their Deep TMS system in Japan for major depression. The most widely approved TMS application is major depression, for which rTMS has been approved in Canada, Australia, New Zealand, the E.U., and Israel as well as the U.S.
In the U.S., the FDA’s CDRH has tiered risk-based requirements, with Class I defined as low to moderate risk, Class II as moderate to high risk and Class III as high risk. For Class I devices, adherence to general controls (e.g., good manufacturing processes, registration, medical device reporting, labeling) is considered sufficient to reasonably ensure safety and effectiveness. For Class II devices, adherence to general plus special controls (e.g., performance standards, postmarket surveillance, patient registries, special labeling requirements) is required. Class III devices must additionally undergo premarket approval (PMA). TMS devices have been classified as Class II as they are not implanted nor do they have long-lasting or potentially fatal AE, so the investigational device exemptions (IDE) process is not required. The 510(k) process, typical for Class II devices, requires demonstrating substantial equivalence (SE) in safety, efficacy, intended use, and technological characteristics to a legally marketed “predicate” device. The de novo pathway is used for low- to moderate-risk devices such as TMS devices without predicates. This establishes a new regulation and allows this device to serve as a predicate subsequently. For instance, in 2008, a first TMS device was authorized by the CDRH through the de novo classification process for treatment-resistant major depression (Neuronetics’ NeuroStar) [1], and in 2013 Brainsway’s H1 System was approved for marketing after demonstrating SE [2]. And, de novo classification was granted in 2013 to eNeura’s single-pulse CerenaTMS device for treating acute pain in migraine with aura, and then in 2014 their portable device, SpringTMS [3] was approved using 510(k) with CerenaTMS as the predicate. Both were CE-marked in the E.U. prior to FDA application.
For devices to treat pain, prospective, sham-controlled RCTs are preferred for the pivotal trials that establish device safety and effectiveness when seeking regulatory approval. This is because of the subjective nature of pain and significant placebo effects. Pivotal trials generally have pre-specified hypotheses, inclusion/exclusion criteria, and description of device-specific attributes, endpoints, and statistical analyses. In pain trials, suboptimal shams and blinding are problematic due to the subjective nature of pain assessment. A blinding assessment that requires forced choice of group assignment and the reason for the choice can help assess the integrity of blinding as discussed in the CDRH’s “Guidance for Industry and FDA Staff – Class II Special Controls Guidance Document: Repetitive Transcranial Magnetic Stimulation (rTMS) Systems” [4]. While randomized sham-controlled trials have historically been used to support TMS applications to the FDA, other study designs can be considered if they provide reasonable assurances of device safety and effectiveness for intended purpose, including randomized comparative trials (with previously cleared or approved treatments), comparison with usual treatment, cross-over designs, and prospective nonrandomized observational trials (propensity analyses).
The FDA often determines the indication for use of a device based upon the adequacy of trial design and the collected data. Considerations for designing pain trials include: Will the device be used to treat acute and/or chronic pain? What type and etiology of pain will be treated? Will it be used as an adjunct to medications or as monotherapy? Will it be used in adults and/or children? Will it be used to treat mild, moderate and/or severe pain?
4.4 Resources for multi-center networks and trials
Given the difficulty of assembling sufficient numbers of homogenous subjects to sufficiently power studies of rTMS, multicenter research consortia that provide infrastructure and standardized metrics are increasingly recognized to add efficiency and lower cost. Collaborative TMS studies face additional difficulties regarding acquisition of identical expensive TMS devices and standardization of TMS administration, but a recent multicenter, randomized, double-blind, sham-controlled, crossover study of rTMS for neuropathic pain was successfully conducted at 7 Japanese centers [48]. Global collaboration offers added difficulties pertaining to language, such as the need to validate study instruments in different languages, and variations in national medical and regulatory practices.
Some collaborations originate from within communities of researchers focusing on specific conditions, others are organized by governmental agencies. An example of a disease-based consortium is the U.S.’ Northeast amyotrophic lateral sclerosis (NEALS) consortium (http://www.alsconsortium.org/) created in 1995 to coordinate collaborative clinical research on amyotrophic lateral sclerosis. Membership grew to more than 100 centers comprising over 500 personnel with varying roles. Clinical data and biosamples are banked and shared, and clinical-research training is offered. An example of a government-funded organization is the NIH-funded consortium of Clinical and Translational Science Award Centers at more than 60 U.S. academic medical institutions (https://www.ctsacentral.org/). This offers resources to enhance general clinical research, some accessible to non-U.S. investigators. For instance, NIH supports a free, public domain resource called the Patient-Reported Outcomes Measurement System (PROMIS; www.nihpromis.org) that contains outcome assessments applicable to a wide variety of chronic diseases and conditions. It currently has 3 items pertaining to pain intensity, 39 items measuring pain behaviors, and 40 items pertaining to pain interference [9]. It is not yet clear whether these pain-related items are sufficiently comprehensive for clinical analgesic trials, and whether they can exclusively support regulatory applications for new drug approval.
The NIH National Institute for Neurological Disorders and Stroke funds an initiative specifically designed for neurological disorders, called “NeuroNEXT” (Network for Excellence in Neuroscience Clinical Trials; http://www.neuronext.org/). It was created to more efficiently ready promising neurological therapies for phase II testing. A Clinical Coordinating Center at the Massachusetts General Hospital manages the 27 participating research institutions using master research service sub-contracts and a central IRB, so that individual member institutions do not need to separately approve each study. A Data Coordinating Center at University of Iowa provides a centralized repository and resource for data-collection and statistical analysis. NeuroNEXT accepts applications and funds trials from industry and academic groups; to date, no TMS or pain studies have been conducted.
5. Technological advances that might improve efficacy of rTMS for treating pain
Technological improvements might also yield more-conclusive studies, so below we review emerging technologies that might potentially improve outcomes.
5.1 Using anatomical MRI to guide coil placement
For localized brain functions, the stimulation site determines the type and magnitude of the effect. To maximize therapeutic effects of rTMS for pain, one would ideally know where the neuronal representation regulating pain is located, select a cortical portion that is accessible to TMS, and target it as precisely and selectively as possible. However, pain is widely distributed, and individual differences in cortical anatomy, white-matter connectivity, and structure-to-function mappings make this challenging. A basic prerequisite for precise rTMS is being able to repeatedly place the coil over a patient-specific cortical target. This is improved by commercially available MRI-guided navigation systems that use infrared cameras to coordinate the relative 3-dimensional location of subjects’ heads and TMS coil, and user-selected landmarks from each subject’s head MRI [40]. MRI-guidance is required to accurately compare the effects of stimulating different cortical targets. There is some evidence that MRI-guided rTMS is more efficacious for pain [46;58], but this is not conclusive. Given the added cost and effort of obtaining MRIs for each subject, the value of MRI-navigation should be clarified before undertaking large clinical trials.
5.2 Mapping TMS electric fields on cortical surfaces
Current TMS navigators localize the TMS coil, but not its predicted cortical activations, yet this refinement is within reach. Each person’s individual cortical surface can be automatically extracted from their MRI, e.g., with FreeSurfer software [35]. This also permits parsing of possible cortex orientation-specific influences. Individual cortical surfaces can also be non-linearly morphed to other brain surfaces (e.g. group averages), to facilitate group-level studies and metanalyses, as recently published [6]. Estimating the primary electric fields induced in the brain by specific TMS parameters requires volume conductor models. Present-day commercial navigation devices either omit these or use simplified, less-accurate spherical models [82]. Realistically shaped models utilizing Finite Element Methods (FEMs) and Boundary Element Models (BEMs) have already been used in at least one group-level TMS study [6]. Employing them in practical TMS navigation systems seems feasible and might improve further targeting accuracy at modest computational and labor cost.
5.3 Measuring distant effects of TMS using MRI tractography
TMS activations spread to secondary areas via white matter tracts [95] including spread to deep subcortical targets [70] and these secondary activations correlate with therapeutic potency [34]. Thus, cortical TMS targets can be considered as windows to networks extending throughout the brain. Once these are characterized, it becomes possible to apply TMS using parameters designed to maximize network-level activations. Diffusion MRI tractography allows identifying individual-specific white-matter pathways. Once TMS-induced electric field distributions on each subject’s cortex is computed as above, the resulting binary mask can be used to seed tractography and estimate distant effects. These can be further refined by considering axonal orientation and bending relative to the electric field [50] and advances in diffusion MRI [107] bring this within reach [81].
5.4 Resting state functional connectivity MRI (rs-fcMRI)
Rs-fcMRI utilizes correlations in spontaneous fluctuations in blood oxygenation to reveal brain networks. This has helped identify network abnormalities correlated with chronic pain symptoms [76]. Recent work suggests that rs-fcMRI may predict the propagation of focal brain stimulation, facilitate visualization of TMS induced network changes, and lend insight into therapeutic mechanisms [35]. Rs-fcMRI is now sufficiently robust and reproducible to help identify patient-specific targets based on their connectivity [36]. For pain, it can test whether efficacy of rTMS application to specific motor cortex targets is due to connectivity with deeper regions implicated in pain perception (Figure 3) [34]. If confirmed, this might improve targeting and perhaps efficacy.
Fig. 3.
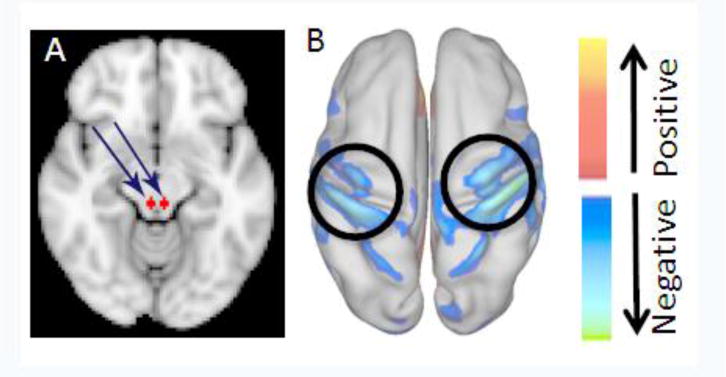
Magnetic resonance imaging (MRI) depicting deep and cortical sites most efficacious to stimulate for treating chronic pain. (A) Depicts the periaqueductal gray (PAG), the primary control center for descending pain modulation, and the most effective target for deep brain stimulation (DBS) for pain (arrows). (B) Depicts mean resting state functional MRI (rs-fcMRI) connectivity mapping of 1,000 normal subjects. Spontaneous modulations in the fMRI signal are extracted from the PAG. Fluctuations in the primary sensory and motor cortices (circles) are most correlated with those of the PAG. Modified with permission from [34].
Today, we recommend transition from the still-widespread practice of applying rTMS without imaging guidance, where resources permit it. Even basic navigators that record coil position relative to each subject’s MRI document the precise cortical areas activated needed to clarify which specific sites offer best efficacy, and off-line tools available today may augment their scientific utility.
6. Future considerations
Most research studies provide proof-of-concept that rTMS can improve some chronic-pain syndromes, but they have been insufficient to confirm specific indications and best methods [83]. Most published studies have been small and unblinded, with exceptions, e.g., [48]. Study designs, subjects, technical parameters, and outcomes have been inconsistent with full details only rarely fully reported, hindering confirmation or metanalysis. Several recent studies are higher quality, demonstrating a commitment to improvement. Funding agencies should support research designed to build towards clinical trials of sufficient quality to support regulatory approval of rTMS for clinical use in chronic pain. We suggest a round of studies to optimize design and methods for clinical trials for pain indications. TMS administration parameters, subject populations, and outcome measures should be standardized and optimized. Other important goals include identifying the best location for motor-cortex stimulation relative to subjects’ painful body area, and clarifying whether MRI-guided localization is cost effective. Guidelines for accreditation and expertise need improvement.
Given the difficulties inherent in recruiting large numbers of well-characterized subjects with homogenous pain syndromes, multi-site collaborations between teams using identical equipment, parameters, and methods should be established and supported, along with bioinformatic resources for securely collecting and analyzing complex data. These could provide foundations for the post-marketing surveillance probably necessary to power analysis of very rare side effects and potential complex consequences for memory, learning, or personality. Global registries, passive electronic collection of TMS administration parameters, patient-reported outcomes, and information technology applications would permit data accrual with less effort required from TMS administrators.
We suggest that the suffering and disability associated with uncontrolled chronic pain, the common and serious adverse effects associated with pain medications, and the preliminary evidence of efficacy and safety of TMS for treating some types of pain, mandate greater investment in developing this therapy.
Supplementary Material
Acknowledgments
Supported in part by the Radcliffe Institute for Advanced Study and the Samuels Family Foundation, the Public Health Service (K24NS059892, K23NS083741, NS38493, R01HD069776, R01NS073601, R21 MH099196, R21 NS082870, R21 NS085491, R21 HD07616, U01NS077179) and NINDS intramural support to MH, the UK National Institute of Health Research (PB-PG-0110-20321 to TN), the Hopkins Neurosurgery Pain Research Institute, the American Academy of Neurology/American Brain Foundation, the Sidney R. Baer Foundation, the Harvard Catalyst|Clinical and Translational Science Center (UL1 RR025758). The content is solely the responsibility of the authors and does not necessarily represent the official views of Harvard Catalyst, Harvard University and its affiliated academic health care centers, the National Institutes of Health or the Sidney R. Baer Jr. Foundation.
Footnotes
Conflict of interest statement
The authors have only the following conflicts of interest:
Dr. Pascual-Leone serves on the scientific advisory boards for Nexstim, Neuronix, Starlab, Neuroelectrics, Axilum Robotics, Magstim, and Neosync; and is listed as an inventor on several issued and pending patents on the real-time integration of TMS with EEG and MRI. None of these patents is currently licensed or generating any license fees. Dr. Hallett may accrue revenue on U.S. Patent #7,407,478 (Issued: August 5, 2008): Coil for Magnetic Stimulation and methods for using the same (H-coil) and he has received license fee payments from the NIH (from Brainsway) for licensing of this patent. Dr. Fox is listed as inventor in issued patents or patent applications on functional connectivity and guidance of TMS.
Reference List
- 1.http://www.fda.gov/MedicalDevices/DeviceRegulationandGuidance/GuidanceDocuments/ucm265269.htm 2015
- 2.http://www.accessdata.fda.gov/cdrh_docs/pdf12/K122288.pdf 2015
- 3.http://www.fda.gov/AboutFDA/CentersOffices/OfficeofMedicalProductsandTobacco/CDRH/CDRHTransparency/ucm232269.htm 2015
- 4.Guidance for Industry and FDA Staff – Class II Special Controls Guidance Document: Repetitive Transcranial Magnetic Stimulation (rTMS) Systems. http://www.fda.gov/downloads/MedicalDevices/DeviceRegulationandGuidance/GuidanceDocuments/UCM311176.pdf.
- 5.Ahdab R, Ayache SS, Brugieres P, Goujon C, Lefaucheur JP. Comparison of “standard” and “navigated” procedures of TMS coil positioning over motor, premotor and prefrontal targets in patients with chronic pain and depression. Neurophysiol Clin. 2010;40:27–36. doi: 10.1016/j.neucli.2010.01.001. [DOI] [PubMed] [Google Scholar]
- 6.Ahveninen J, Huang S, Nummenmaa A, Belliveau JW, Hung AY, Jaaskelainen IP, Rauschecker JP, Rossi S, Tiitinen H, Raij T. Evidence for distinct human auditory cortex regions for sound location versus identity processing. Nat Commun. 2013;4:2585. doi: 10.1038/ncomms3585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Albrecht PJ, Hines S, Eisenberg E, Pud D, Finlay DR, Connolly MK, Pare M, Davar G, Rice FL. Pathologic alterations of cutaneous innervation and vasculature in affected limbs from patients with complex regional pain syndrome. Pain. 2006;120:244–266. doi: 10.1016/j.pain.2005.10.035. [DOI] [PubMed] [Google Scholar]
- 8.Amato AA, Oaklander AL. Case records of the Massachusetts General Hospital. Weekly clinicopathological exercises. Case 16-2004. A 76-year-old woman with numbness and pain in the feet and legs. N Engl J Med. 2004;350:2181–2189. doi: 10.1056/NEJMcpc049005. [DOI] [PubMed] [Google Scholar]
- 9.Amtmann D, Cook KF, Jensen MP, Chen WH, Choi S, Revicki D, Cella D, Rothrock N, Keefe F, Callahan L, Lai JS. Development of a PROMIS item bank to measure pain interference. Pain. 2010;150:173–182. doi: 10.1016/j.pain.2010.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.André-Obadia N, Mertens P, Gueguen A, Peyron R, Garcia-Larrea L. Pain relief by rTMS: Differential effect of current flow but no specific action on pain subtypes. Neurology. 2008;71:833–840. doi: 10.1212/01.wnl.0000325481.61471.f0. [DOI] [PubMed] [Google Scholar]
- 11.André-Obadia N, Peyron R, Mertens P, Mauguière F, Laurent B, Garcia-Larrea L. Transcranial magnetic stimulation for pain control. Double-blind study of different frequencies against placebo, and correlation with motor cortex stimulation efficacy. Clinical Neurophysiology. 2006;117:1536–1544. doi: 10.1016/j.clinph.2006.03.025. [DOI] [PubMed] [Google Scholar]
- 12.Attal N, Cruccu G, Baron R, Haanpää M, Hansson P, Jensen TS, Nurmikko T. EFNS guidelines on the pharmacological treatment of neuropathic pain: 2010 revision. Eur J Neurol. 2010;17:1113–1123. doi: 10.1111/j.1468-1331.2010.02999.x. [DOI] [PubMed] [Google Scholar]
- 13.Barker AT, Jalinous R, Freeston IL. Non-invasive magnetic stimulation of human motor cortex. Lancet. 1985;1:1106–1107. doi: 10.1016/s0140-6736(85)92413-4. [DOI] [PubMed] [Google Scholar]
- 14.Baudic S, Attal N, Mhalla A, Ciampi de AD, Perrot S, Bouhassira D. Unilateral repetitive transcranial magnetic stimulation of the motor cortex does not affect cognition in patients with fibromyalgia. J Psychiatr Res. 2013;47:72–77. doi: 10.1016/j.jpsychires.2012.09.003. [DOI] [PubMed] [Google Scholar]
- 15.Bittar RG, Kar-Purkayastha I, Owen SL, Bear RE, Green A, Wang S, Aziz TZ. Deep brain stimulation for pain relief: a meta-analysis. J Clin Neurosci. 2005;12:515–519. doi: 10.1016/j.jocn.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 16.Borckardt JJ, Reeves ST, Weinstein M, Smith AR, Shelley N, Kozel FA, Nahas Z, Byrne KT, Morgan K, George MS. Significant analgesic effects of one session of postoperative left prefrontal cortex repetitive transcranial magnetic stimulation: a replication study. Brain Stimul. 2008;1:122–127. doi: 10.1016/j.brs.2008.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Borckardt JJ, Walker J, Branham RK, Rydin-Gray S, Hunter C, Beeson H, Reeves ST, Madan A, Sackeim H, George MS. Development and evaluation of a portable sham transcranial magnetic stimulation system. Brain Stimul. 2008;1:52–59. doi: 10.1016/j.brs.2007.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Boyer L, Dousset A, Roussel P, Dossetto N, Cammilleri S, Piano V, Khalfa S, Mundler O, Donnet A, Guedj E. rTMS in fibromyalgia: A randomized trial evaluating QoL and its brain metabolic substrate. Neurology. 2014;82:1231–1238. doi: 10.1212/WNL.0000000000000280. [DOI] [PubMed] [Google Scholar]
- 19.Cassidy JD, Carroll LJ, Cote P, Lemstra M, Berglund A, Nygren A. Effect of eliminating compensation for pain and suffering on the outcome of insurance claims for whiplash injury. N Engl J Med. 2000;342:1179–1186. doi: 10.1056/NEJM200004203421606. [DOI] [PubMed] [Google Scholar]
- 20.Chipchase L, Schabrun S, Cohen L, Hodges P, Ridding M, Rothwell J, Taylor J, Ziemann U. A checklist for assessing the methodological quality of studies using transcranial magnetic stimulation to study the motor system: an international consensus study. Clin Neurophysiol. 2012;123:1698–1704. doi: 10.1016/j.clinph.2012.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cruccu G, Aziz TZ, Garcia-Larrea L, Hansson P, Jensen TS, Lefaucheur JP, Simpson BA, Taylor RS. EFNS guidelines on neurostimulation therapy for neuropathic pain. Eur J Neurol. 2007;14:952–970. doi: 10.1111/j.1468-1331.2007.01916.x. [DOI] [PubMed] [Google Scholar]
- 22.Dall’Agnol L, Medeiros LF, Torres IL, Deitos A, Brietzke A, Laste G, de SA, Vieira JL, Fregni F, Caumo W. Repetitive transcranial magnetic stimulation increases the corticospinal inhibition and the brain-derived neurotrophic factor in chronic myofascial pain syndrome: an explanatory double-blinded, randomized, sham-controlled trial. J Pain. 2014;15:845–855. doi: 10.1016/j.jpain.2014.05.001. [DOI] [PubMed] [Google Scholar]
- 23.Davis NJ, Gold E, Pascual-Leone A, Bracewell RM. Challenges of proper placebo control for non-invasive brain stimulation in clinical and experimental applications. Eur J Neurosci. 2013;38:2973–2977. doi: 10.1111/ejn.12307. [DOI] [PubMed] [Google Scholar]
- 24.de Moragas JM, Kierland RR. The outcome of patients with herpes zoster. Arch Dermatol. 1957;75:193–196. doi: 10.1001/archderm.1957.01550140037006. [DOI] [PubMed] [Google Scholar]
- 25.de Oliveira RA, de Andrade DC, Mendonca M, Barros R, Luvisoto T, Myczkowski ML, Marcolin MA, Teixeira MJ. Repetitive transcranial magnetic stimulation of the left premotor/dorsolateral prefrontal cortex does not have analgesic effect on central poststroke pain. J Pain. 2014;15:1271–1281. doi: 10.1016/j.jpain.2014.09.009. [DOI] [PubMed] [Google Scholar]
- 26.Defrin R, Grunhaus L, Zamir D, Zeilig G. The effect of a series of repetitive transcranial magnetic stimulations of the motor cortex on central pain after spinal cord injury. Arch Phys Med Rehabil. 2007;88:1574–1580. doi: 10.1016/j.apmr.2007.07.025. [DOI] [PubMed] [Google Scholar]
- 27.Deng ZD, Lisanby SH, Peterchev AV. Electric field depth-focality tradeoff in transcranial magnetic stimulation: Simulation comparison of 50 coil designs. Brain Stimul. 2012;6:1–13. doi: 10.1016/j.brs.2012.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dworkin RH, Turk DC, Farrar JT, Haythornthwaite JA, Jensen MP, Katz NP, Kerns RD, Stucki G, Allen RR, Bellamy N, Carr DB, Chandler J, Cowan P, Dionne R, Galer BS, Hertz S, Jadad AR, Kramer LD, Manning DC, Martin S, McCormick CG, McDermott MP, McGrath P, Quessy S, Rappaport BA, Robbins W, Robinson JP, Rothman M, Royal MA, Simon L, Stauffer JW, Stein W, Tollett J, Wernicke J, Witter J. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain. 2005;113:9–19. doi: 10.1016/j.pain.2004.09.012. [DOI] [PubMed] [Google Scholar]
- 29.Dworkin RH, Turk DC, Peirce-Sandner S, He H, McDermott MP, Farrar JT, Katz NP, Lin AH, Rappaport BA, Rowbotham MC. Assay sensitivity and study features in neuropathic pain trials: an ACTTION meta-analysis. Neurology. 2013;81:67–75. doi: 10.1212/WNL.0b013e318297ee69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Eisenberg E, Lurie Y, Braker C, Daoud D, Ishay A. Lamotrigine reduces painful diabetic neuropathy: a randomized, controlled study. Neurology. 2001;57:505–509. doi: 10.1212/wnl.57.3.505. [DOI] [PubMed] [Google Scholar]
- 31.Fontaine D, Hamani C, Lozano A. Efficacy and safety of motor cortex stimulation for chronic neuropathic pain: critical review of the literature. J Neurosurg. 2008 doi: 10.3171/2008.6.17602. [DOI] [PubMed] [Google Scholar]
- 32.Fontaine D, Hamani C, Lozano A. Efficacy and safety of motor cortex stimulation for chronic neuropathic pain: critical review of the literature. J Neurosurg. 2009;110:251–256. doi: 10.3171/2008.6.17602. [DOI] [PubMed] [Google Scholar]
- 33.Forssell H, Tenovuo O, Silvoniemi P, Jaaskelainen SK. Differences and similarities between atypical facial pain and trigeminal neuropathic pain. Neurology. 2007;69:1451–1459. doi: 10.1212/01.wnl.0000277274.83301.c0. [DOI] [PubMed] [Google Scholar]
- 34.Fox MD, Buckner RL, Liu H, Chakravarty MM, Lozano AM, Pascual-Leone A. Resting-state networks link invasive and noninvasive brain stimulation across diverse psychiatric and neurological diseases. Proc Natl Acad Sci U S A. 2014;111:E4367–E4375. doi: 10.1073/pnas.1405003111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fox MD, Buckner RL, White MP, Greicius MD, Pascual-Leone A. Efficacy of transcranial magnetic stimulation targets for depression is related to intrinsic functional connectivity with the subgenual cingulate. Biol Psychiatry. 2012;72:595–603. doi: 10.1016/j.biopsych.2012.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fox MD, Liu H, Pascual-Leone A. Identification of reproducible individualized targets for treatment of depression with TMS based on intrinsic connectivity. Neuroimage. 2012;66C:151–160. doi: 10.1016/j.neuroimage.2012.10.082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fricová J, Klirová M, Masopust V, Novák T, Vérebová K, Rokyta R. Repetitive transcranial magnetic stimulation in the treatment of chronic orofacial pain. Physiol Res. 2013;62(Suppl 1):S125–S134. doi: 10.33549/physiolres.932575. [DOI] [PubMed] [Google Scholar]
- 38.Garcia-Larrea L, Peyron R. Motor cortex stimulation for neuropathic pain: From phenomenology to mechanisms. Neuroimage. 2007;37(Suppl 1):S71–S79. doi: 10.1016/j.neuroimage.2007.05.062. [DOI] [PubMed] [Google Scholar]
- 39.Geertzen JH, Bodde MI, van den Dungen JJ, Dijkstra PU, den Dunnen WF. Peripheral nerve pathology in patients with severely affected complex regional pain syndrome type I. Int J Rehabil Res. 2014 doi: 10.1097/MRR.0000000000000096. [DOI] [PubMed] [Google Scholar]
- 40.Gugino LD, Romero JR, Aglio L, Titone D, Ramirez M, Pascual-Leone A, Grimson E, Weisenfeld N, Kikinis R, Shenton ME. Transcranial magnetic stimulation coregistered with MRI: a comparison of a guided versus blind stimulation technique and its effect on evoked compound muscle action potentials. Clin Neurophysiol. 2001;112:1781–1792. doi: 10.1016/s1388-2457(01)00633-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Haanpää ML, Attal N, Backonja M, Baron R, Bennett M, Bouhassira D, Cruccu G, Hansson P, Haythornthwaite JA, Iannetti GD, Jensen TS, Kauppila T, Nurmikko TJ, Rice AS, Rowbotham M, Serra J, Sommer C, Smith BH, Treede RD. NeuPSIG guidelines on neuropathic pain assessment. Pain. 2011;152:14–27. doi: 10.1016/j.pain.2010.07.031. [DOI] [PubMed] [Google Scholar]
- 42.Hadjimichael O, Kerns RD, Rizzo MA, Cutter G, Vollmer T. Persistent pain and uncomfortable sensations in persons with multiple sclerosis. Pain. 2007;127:35–41. doi: 10.1016/j.pain.2006.07.015. [DOI] [PubMed] [Google Scholar]
- 43.Hamani C, Schwalb JM, Rezai AR, Dostrovsky JO, Davis KD, Lozano AM. Deep brain stimulation for chronic neuropathic pain: long-term outcome and the incidence of insertional effect. Pain. 2006;125:188–196. doi: 10.1016/j.pain.2006.05.019. [DOI] [PubMed] [Google Scholar]
- 44.Harden RN, Weinland SR, Remble TA, Houle TT, Colio S, Steedman S, Kee WG. Medication Quantification Scale Version III: update in medication classes and revised detriment weights by survey of American Pain Society Physicians. J Pain. 2005;6:364–371. doi: 10.1016/j.jpain.2005.01.350. [DOI] [PubMed] [Google Scholar]
- 45.Hasan M, Whiteley J, Bresnahan R, MacIver K, Sacco P, Das K, Nurmikko T. Somatosensory change and pain relief induced by repetitive transcranial magnetic stimulation in patients with central poststroke pain. Neuromodulation. 2014 doi: 10.1111/ner.12198. [DOI] [PubMed] [Google Scholar]
- 46.Hirayama A, Saitoh Y, Kishima H, Shimokawa T, Oshino S, Hirata M, Kato A, Yoshimine T. Reduction of intractable deafferentation pain by navigation-guided repetitive transcranial magnetic stimulation of the primary motor cortex. Pain. 2006;122:22–27. doi: 10.1016/j.pain.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 47.Hoeft F, Wu DA, Hernandez A, Glover GH, Shimojo S. Electronically switchable sham transcranial magnetic stimulation (TMS) system. PLoS ONE. 2008;3:e1923. doi: 10.1371/journal.pone.0001923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hosomi K, Shimokawa T, Ikoma K, Nakamura Y, Sugiyama K, Ugawa Y, Uozumi T, Yamamoto T, Saitoh Y. Daily repetitive transcranial magnetic stimulation of primary motor cortex for neuropathic pain: A randomized, multicenter, double-blind, crossover, sham-controlled trial. Pain. 2013;10 doi: 10.1016/j.pain.2013.03.016. [DOI] [PubMed] [Google Scholar]
- 49.Huang YZ, Edwards MJ, Rounis E, Bhatia KP, Rothwell JC. Theta burst stimulation of the human motor cortex. Neuron. 2005;45:201–206. doi: 10.1016/j.neuron.2004.12.033. [DOI] [PubMed] [Google Scholar]
- 50.Ilmoniemi RJ, Ruohonen J, Karhu J. Transcranial magnetic stimulation–a new tool for functional imaging of the brain. Crit Rev Biomed Eng. 1999;27:241–284. [PubMed] [Google Scholar]
- 51.Kang BS, Shin HI, Bang MS. Effect of repetitive transcranial magnetic stimulation over the hand motor cortical area on central pain after spinal cord injury. Arch Phys Med Rehabil. 2009;90:1766–1771. doi: 10.1016/j.apmr.2009.04.008. [DOI] [PubMed] [Google Scholar]
- 52.Khedr EM, Kotb H, Kamel NF, Ahmed MA, Sadek R, Rothwell JC. Longlasting antalgic effects of daily sessions of repetitive transcranial magnetic stimulation in central and peripheral neuropathic pain. Journal of Neurology, Neurosurgery & Psychiatry. 2005;76:833–838. doi: 10.1136/jnnp.2004.055806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kim JS, Bashford G, Murphy TK, Martin A, Dror V, Cheung R. Safety and efficacy of pregabalin in patients with central post-stroke pain. Pain. 2011;152:1018–1023. doi: 10.1016/j.pain.2010.12.023. [DOI] [PubMed] [Google Scholar]
- 54.Kozyrev V, Eysel UT, Jancke D. Voltage-sensitive dye imaging of transcranial magnetic stimulation-induced intracortical dynamics. Proc Natl Acad Sci U S A. 2014;111:13553–13558. doi: 10.1073/pnas.1405508111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Krüger LJ, Wild C. Evidence requirements for the authorization and reimbursement of high-risk medical devices in the USA, Europe, Australia and Canada: An analysis of seven high-risk medical devices. Wien: Ludwig Boltzmann Institut für Health Technology Assessment; 2013. [Google Scholar]
- 56.Langford RM, Mares J, Novotna A, Vachova M, Novakova I, Notcutt W, Ratcliffe S. A double-blind, randomized, placebo-controlled, parallel-group study of THC/CBD oromucosal spray in combination with the existing treatment regimen, in the relief of central neuropathic pain in patients with multiple sclerosis. J Neurol. 2013;260:984–997. doi: 10.1007/s00415-012-6739-4. [DOI] [PubMed] [Google Scholar]
- 57.Lee SJ, Kim DY, Chun MH, Kim YG. The effect of repetitive transcranial magnetic stimulation on fibromyalgia: a randomized sham-controlled trial with 1-mo follow-up. Am J Phys Med Rehabil. 2012;91:1077–1085. doi: 10.1097/PHM.0b013e3182745a04. [DOI] [PubMed] [Google Scholar]
- 58.Lefaucheur JP. Why image-guided navigation becomes essential in the practice of transcranial magnetic stimulation. Neurophysiol Clin. 2010;40:1–5. doi: 10.1016/j.neucli.2009.10.004. [DOI] [PubMed] [Google Scholar]
- 59.Lefaucheur JP, André-Obadia N, Antal A, Ayache SS, Baeken C, Benninger DH, Cantello RM, Cincotta M, de CM, De RD, Devanne H, Di LV, Filipovic SR, Hummel FC, Jaaskelainen SK, Kimiskidis VK, Koch G, Langguth B, Nyffeler T, Oliviero A, Padberg F, Poulet E, Rossi S, Rossini PM, Rothwell JC, Schonfeldt-Lecuona C, Siebner HR, Slotema CW, Stagg CJ, Valls-Sole J, Ziemann U, Paulus W, Garcia-Larrea L. Evidence-based guidelines on the therapeutic use of repetitive transcranial magnetic stimulation (rTMS) Clin Neurophysiol. 2014 doi: 10.1016/j.clinph.2014.05.021. [DOI] [PubMed] [Google Scholar]
- 60.Lefaucheur JP, Ayache SS, Sorel M, Farhat WH, Zouari HG, Ciampi de Andrade D, Ahdab R, Menard-Lefaucheur I, Brugieres P, Goujon C. Analgesic effects of repetitive transcranial magnetic stimulation of the motor cortex in neuropathic pain: Influence of theta burst stimulation priming. Eur J Pain. 2012;16:1403–1413. doi: 10.1002/j.1532-2149.2012.00150.x. [DOI] [PubMed] [Google Scholar]
- 61.Lefaucheur JP, Drouot X, Cunin P, Bruckert R, Lepetit H, Créange A, Wolkenstein P, Maison P, Keravel Y, Nguyen JP, en JP. Motor cortex stimulation for the treatment of refractory peripheral neuropathic pain. Brain. 2009;132:1463–1471. doi: 10.1093/brain/awp035. [DOI] [PubMed] [Google Scholar]
- 62.Lefaucheur JP, Drouot X, Keravel Y, Nguyen JP. Pain relief induced by repetitive transcranial magnetic stimulation of precentral cortex. Neuroreport. 2001;12:2963–2965. doi: 10.1097/00001756-200109170-00041. [DOI] [PubMed] [Google Scholar]
- 63.Lefaucheur JP, Drouot X, Menard-Lefaucheur I, Keravel Y, Nguyen JP. Motor cortex rTMS in chronic neuropathic pain: pain relief is associated with thermal sensory perception improvement. J Neurol Neurosurg Psychiatry. 2008;79:1044–1049. doi: 10.1136/jnnp.2007.135327. [DOI] [PubMed] [Google Scholar]
- 64.Lefaucheur JP, Drouot X, Menard-Lefaucheur I, Zerah F, Bendib B, Cesaro P, Keravel Y, Nguyen JP. Neurogenic pain relief by repetitive transcranial magnetic cortical stimulation depends on the origin and the site of pain. Journal of Neurology, Neurosurgery & Psychiatry. 2004;75:612–616. doi: 10.1136/jnnp.2003.022236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lefaucheur JP, Hatem S, Nineb A, M+¬nard-Lefaucheur I, Wendling S, Keravel Y, Nguyen JP. Somatotopic organization of the analgesic effects of motor cortex rTMS in neuropathic pain. Neurology. 2006;67:1998–2004. doi: 10.1212/01.wnl.0000247138.85330.88. [DOI] [PubMed] [Google Scholar]
- 66.Lefaucheur JP, Holsheimer J, Goujon C, Keravel Y, Nguyen JP. Descending volleys generated by efficacious epidural motor cortex stimulation in patients with chronic neuropathic pain. Exp Neurol. 2010;223:609–614. doi: 10.1016/j.expneurol.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 67.Lefaucheur JP, Keravel Y, Nguyen JP. Treatment of poststroke pain by epidural motor cortex stimulation with a new octopolar lead. Neurosurg. 2011;68:180–187. doi: 10.1227/NEU.0b013e318207f896. [DOI] [PubMed] [Google Scholar]
- 68.Lefaucheur JP, Menard-Lefaucheur I, Goujon C, Keravel Y, Nguyen JP. Predictive value of rTMS in the identification of responders to epidural motor cortex stimulation therapy for pain. J Pain. 2011;12:1102–1111. doi: 10.1016/j.jpain.2011.05.004. [DOI] [PubMed] [Google Scholar]
- 69.Leung A, Donohue M, Xu R, Lee R, Lefaucheur JP, Khedr EM, Saitoh Y, André-Obadia N, Rollnik J, Wallace M, Chen R. rTMS for suppressing neuropathic pain: a meta-analysis. J Pain. 2009;10:1205–1216. doi: 10.1016/j.jpain.2009.03.010. [DOI] [PubMed] [Google Scholar]
- 70.Li X, Nahas Z, Kozel FA, Anderson B, Bohning DE, George MS. Acute left prefrontal transcranial magnetic stimulation in depressed patients is associated with immediately increased activity in prefrontal cortical as well as subcortical regions. Biol Psychiatry. 2004;55:882–890. doi: 10.1016/j.biopsych.2004.01.017. [DOI] [PubMed] [Google Scholar]
- 71.Lima MC, Fregni F. Motor cortex stimulation for chronic pain: systematic review and meta-analysis of the literature. Neurology. 2008;70:2329–2337. doi: 10.1212/01.wnl.0000314649.38527.93. [DOI] [PubMed] [Google Scholar]
- 72.Lipton RB, Dodick DW, Silberstein SD, Saper JR, Aurora SK, Pearlman SH, Fischell RE, Ruppel PL, Goadsby PJ. Single-pulse transcranial magnetic stimulation for acute treatment of migraine with aura: a randomised, double-blind, parallel-group, sham-controlled trial. The Lancet Neurology. 2010;9:373–380. doi: 10.1016/S1474-4422(10)70054-5. [DOI] [PubMed] [Google Scholar]
- 73.Maalouf M, Rho JM, Mattson MP. The neuroprotective properties of calorie restriction, the ketogenic diet, and ketone bodies. Brain Res Rev. 2009;59:293–315. doi: 10.1016/j.brainresrev.2008.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Maarrawi J, Peyron R, Mertens P, Costes N, Magnin M, Sindou M, Laurent B, Garcia-Larrea L. Motor cortex stimulation for pain control induces changes in the endogenous opioid system. Neurology. 2007;69:827–834. doi: 10.1212/01.wnl.0000269783.86997.37. [DOI] [PubMed] [Google Scholar]
- 75.Maizey L, Allen CP, Dervinis M, Verbruggen F, Varnava A, Kozlov M, Adams RC, Stokes M, Klemen J, Bungert A, Hounsell CA, Chambers CD. Comparative incidence rates of mild adverse effects to transcranial magnetic stimulation. Clin Neurophysiol. 2013;124:536–544. doi: 10.1016/j.clinph.2012.07.024. [DOI] [PubMed] [Google Scholar]
- 76.Makin TR, Scholz J, Filippini N, Henderson SD, Tracey I, Johansen-Berg H. Phantom pain is associated with preserved structure and function in the former hand area. Nat Commun. 2013;4:1570. doi: 10.1038/ncomms2571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Marlow NM, Bonilha HS, Short EB. Efficacy of transcranial direct current stimulation and repetitive transcranial magnetic stimulation for treating fibromyalgia syndrome: a systematic review. Pain Pract. 2013;13:131–145. doi: 10.1111/j.1533-2500.2012.00562.x. [DOI] [PubMed] [Google Scholar]
- 78.Mhalla A, Baudic S, de Andrade DC, Gautron M, Perrot S, Teixeira MJ, Attal N, Bouhassira D. Long-term maintenance of the analgesic effects of transcranial magnetic stimulation in fibromyalgia. Pain. 2011;152:1478–1485. doi: 10.1016/j.pain.2011.01.034. [DOI] [PubMed] [Google Scholar]
- 79.Nguyen JP, Nizard J, Keravel Y, Lefaucheur JP. Invasive brain stimulation for the treatment of neuropathic pain. Nat Rev Neurol. 2011;7:699–709. doi: 10.1038/nrneurol.2011.138. [DOI] [PubMed] [Google Scholar]
- 80.Nowak LG, Bullier J. Axons, but not cell bodies, are activated by electrical stimulation in cortical gray matter. I. Evidence from chronaxie measurements. Exp Brain Res. 1998;118:477–488. doi: 10.1007/s002210050304. [DOI] [PubMed] [Google Scholar]
- 81.Nummenmaa A, McNab JA, Savadjiev P, Okada Y, Hamalainen MS, Wang R, Wald LL, Pascual-Leone A, Wedeen VJ, Raij T. Targeting of white matter tracts with transcranial magnetic stimulation. Brain Stimul. 2014;7:80–84. doi: 10.1016/j.brs.2013.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Nummenmaa A, Stenroos M, Ilmoniemi RJ, Okada YC, Hamalainen MS, Raij T. Comparison of spherical and realistically shaped boundary element head models for transcranial magnetic stimulation navigation. Clin Neurophysiol. 2013;124:1995–2007. doi: 10.1016/j.clinph.2013.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.O’Connell NE, Wand BM, Marston L, Spencer S, DeSouza LH. Non-invasive brain stimulation techniques for chronic pain. Cochrane Database Syst Rev. 2014;4:CD008208. doi: 10.1002/14651858.CD008208.pub3. [DOI] [PubMed] [Google Scholar]
- 84.O’Donnell MJ, Diener H-C, Sacco RL, Panju AA, Vinisko R, Yusuf S. Chronic pain syndromes after ischemic stroke: PRoFESS trial. Stroke. 2013;44:1238–1243. doi: 10.1161/STROKEAHA.111.671008. [DOI] [PubMed] [Google Scholar]
- 85.Oaklander AL, Fields HL. Is reflex sympathetic dystrophy/complex regional pain syndrome type I a small-fiber neuropathy? Ann Neurol. 2009;65:629–638. doi: 10.1002/ana.21692. [DOI] [PubMed] [Google Scholar]
- 86.Oaklander AL, Herzog ZD, Downs HM, Klein MM. Objective evidence that small-fiber polyneuropathy underlies some illnesses currently labeled as fibromyalgia. Pain. 2013;154:2310–2316. doi: 10.1016/j.pain.2013.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Oaklander AL, Rissmiller JG, Gelman LB, Zheng L, Chang Y, Gott R. Evidence of focal small-fiber axonal degeneration in complex regional pain syndrome-I (reflex sympathetic dystrophy) Pain. 2006;120:235–243. doi: 10.1016/j.pain.2005.09.036. [DOI] [PubMed] [Google Scholar]
- 88.Oh MY, Abosch A, Kim SH, Lang AE, Lozano AM. Long-term hardware-related complications of deep brain stimulation. Neurosurg. 2002;50:1268–1274. doi: 10.1097/00006123-200206000-00017. [DOI] [PubMed] [Google Scholar]
- 89.Ohn SH, Chang WH, Park CH, Kim ST, Lee JI, Pascual-Leone A, Kim YH. Neural correlates of the antinociceptive effects of repetitive transcranial magnetic stimulation on central pain after stroke. Neurorehabil Neural Repair. 2012;26:344–352. doi: 10.1177/1545968311423110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Onesti E, Gabriele M, Cambieri C, Ceccanti M, Raccah R, Di SG, Biasiotta A, Truini A, Zangen A, Inghilleri M. H-coil repetitive transcranial magnetic stimulation for pain relief in patients with diabetic neuropathy. Eur J Pain. 2013:10–2149. doi: 10.1002/j.1532-2149.2013.00320.x. [DOI] [PubMed] [Google Scholar]
- 91.Owen SL, Green AL, Nandi D, Bittar RG, Wang S, Aziz TZ. Deep brain stimulation for neuropathic pain. Neuromodulation. 2006;9:100–106. doi: 10.1111/j.1525-1403.2006.00049.x. [DOI] [PubMed] [Google Scholar]
- 92.Oxman MN, Levin MJ, Johnson GR, Schmader KE, Straus SE, Gelb LD, Arbeit RD, Simberkoff MS, Gershon AA, Davis LE, Weinberg A, Boardman KD, Williams HM, Zhang JH, Peduzzi PN, Beisel CE, Morrison VA, Guatelli JC, Brooks PA, Kauffman CA, Pachucki CT, Neuzil KM, Betts RF, Wright PF, Griffin MR, Brunell P, Soto NE, Marques AR, Keay SK, Goodman RP, Cotton DJ, Gnann JW, Jr, Loutit J, Holodniy M, Keitel WA, Crawford GE, Yeh SS, Lobo Z, Toney JF, Greenberg RN, Keller PM, Harbecke R, Hayward AR, Irwin MR, Kyriakides TC, Chan CY, Chan IS, Wang WW, Annunziato PW, Silber JL. A vaccine to prevent herpes zoster and postherpetic neuralgia in older adults. N Engl J Med. 2005;352:2271–2284. doi: 10.1056/NEJMoa051016. [DOI] [PubMed] [Google Scholar]
- 93.Pashut T, Wolfus S, Friedman A, Lavidor M, Bar-Gad I, Yeshurun Y, Korngreen A. Mechanisms of magnetic stimulation of central nervous system neurons. PLoS Comput Biol. 2011;7:e1002022. doi: 10.1371/journal.pcbi.1002022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Passard A, Attal N, Benadhira R, Brasseur L, Saba G, Sichere P, Perrot S, Januel D, Bouhassira D. Effects of unilateral repetitive transcranial magnetic stimulation of the motor cortex on chronic widespread pain in fibromyalgia. Brain. 2007;130:2661–2670. doi: 10.1093/brain/awm189. [DOI] [PubMed] [Google Scholar]
- 95.Paus T, Jech R, Thompson CJ, Comeau R, Peters T, Evans AC. Transcranial magnetic stimulation during positron emission tomography: a new method for studying connectivity of the human cerebral cortex. J Neurosci. 1997;17:3178–3184. doi: 10.1523/JNEUROSCI.17-09-03178.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Penfield W, Boldrey E. Somatic motor and sensory representation in the cerebral cortex of man studied by electrical stimulation. Brain. 1937;60:389–443. [Google Scholar]
- 97.Penfield W, Rasmussen T. The Cerebral Cortex of Man: A Clinical Study of Localization of Function. Hafner Publishing Company; 1950. [Google Scholar]
- 98.Picarelli H, Teixeira MJ, de Andrade DC, Myczkowski ML, Luvisotto TB, Yeng LT, Fonoff ET, Pridmore S, Marcolin MA. Repetitive transcranial magnetic stimulation is efficacious as an add-on to pharmacological therapy in complex regional pain syndrome (CRPS) type I. J Pain. 2010;11:1203–1210. doi: 10.1016/j.jpain.2010.02.006. [DOI] [PubMed] [Google Scholar]
- 99.Pleger B, Janssen F, Schwenkreis P, V+¦lker B, Maier C, Tegenthoff M. Repetitive transcranial magnetic stimulation of the motor cortex attenuates pain perception in complex regional pain syndrome type I. Neuroscience Letters. 2004;356:87–90. doi: 10.1016/j.neulet.2003.11.037. [DOI] [PubMed] [Google Scholar]
- 100.Pogliano C. Penfield’s homunculus and other grotesque creatures from the Land of If. Nuncius. 2012;27:141–162. doi: 10.1163/182539112x637192. [DOI] [PubMed] [Google Scholar]
- 101.Quartarone A, Siebner HR, Rothwell JC. Task-specific hand dystonia: can too much plasticity be bad for you? Trends Neurosci. 2006;29:192–199. doi: 10.1016/j.tins.2006.02.007. [DOI] [PubMed] [Google Scholar]
- 102.Rasche D, Rinaldi PC, Young RF, Tronnier VM. Deep brain stimulation for the treatment of various chronic pain syndromes. Neurosurg Focus. 2006;21:E8. doi: 10.3171/foc.2006.21.6.10. [DOI] [PubMed] [Google Scholar]
- 103.Rogers WH, Wittink H, Wagner A, Cynn D, Carr DB. Assessing individual outcomes during outpatient multidisciplinary chronic pain treatment by means of an augmented SF-36. Pain Med. 2000;1:44–54. doi: 10.1046/j.1526-4637.2000.99102.x. [DOI] [PubMed] [Google Scholar]
- 104.Rossi S, Hallett M, Rossini PM, Pascual-Leone A. Safety, ethical considerations, and application guidelines for the use of transcranial magnetic stimulation in clinical practice and research. Clin Neurophysiol. 2009;120:2008–2039. doi: 10.1016/j.clinph.2009.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Sacco P, Prior M, Poole H, Nurmikko T. Repetitive transcranial magnetic stimulation over primary motor vs non-motor cortical targets; effects on experimental hyperalgesia in healthy subjects. BMC Neurol. 2014;14:166. doi: 10.1186/s12883-014-0166-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Sansur CA, Frysinger RC, Pouratian N, Fu KM, Bittl M, Oskouian RJ, Laws ER, Elias WJ. Incidence of symptomatic hemorrhage after stereotactic electrode placement. J Neurosurg. 2007;107:998–1003. doi: 10.3171/JNS-07/11/0998. [DOI] [PubMed] [Google Scholar]
- 107.Setsompop K, Cohen-Adad J, Gagoski BA, Raij T, Yendiki A, Keil B, Wedeen VJ, Wald LL. Improving diffusion MRI using simultaneous multi-slice echo planar imaging. Neuroimage. 2012;63:569–580. doi: 10.1016/j.neuroimage.2012.06.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Short EB, Borckardt JJ, Anderson BS, Frohman H, Beam W, Reeves ST, George MS. Ten sessions of adjunctive left prefrontal rTMS significantly reduces fibromyalgia pain: a randomized, controlled pilot study. Pain. 2011;152:2477–2484. doi: 10.1016/j.pain.2011.05.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Siddall PJ, Cousins MJ, Otte A, Griesing T, Chambers R, Murphy TK. Pregabalin in central neuropathic pain associated with spinal cord injury: a placebo-controlled trial. Neurology. 2006;67:1792–1800. doi: 10.1212/01.wnl.0000244422.45278.ff. [DOI] [PubMed] [Google Scholar]
- 110.Sillay KA, Larson PS, Starr PA. Deep brain stimulator hardware-related infections: incidence and management in a large series. Neurosurg. 2008;62:360–366. doi: 10.1227/01.neu.0000316002.03765.33. [DOI] [PubMed] [Google Scholar]
- 111.Silva G, Miksad R, Freedman SD, Pascual-Leone A, Jain S, Gomes DL, Amancio EJ, Boggio PS, Correa CF, Fregni F. Treatment of cancer pain with noninvasive brain stimulation. J Pain Symptom Manage. 2007;34:342–345. doi: 10.1016/j.jpainsymman.2007.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Strafella AP, Paus T, Fraraccio M, Dagher A. Striatal dopamine release induced by repetitive transcranial magnetic stimulation of the human motor cortex. Brain. 2003;126:2609–2615. doi: 10.1093/brain/awg268. [DOI] [PubMed] [Google Scholar]
- 113.Theodoroff SM, Folmer RL. Repetitive transcranial magnetic stimulation as a treatment for chronic tinnitus: a critical review. Otol Neurotol. 2013;34:199–208. doi: 10.1097/mao.0b013e31827b4d46. [DOI] [PubMed] [Google Scholar]
- 114.Truini A, Galeotti F, La Cesa S, Di Rezze S, Biasiotta A, Di Stefano G, Tinelli E, Millefiorini E, Gatti A, Cruccu G. Mechanisms of pain in multiple sclerosis: A combined clinical and neurophysiological study. Pain. 2012;153:2048–2054. doi: 10.1016/j.pain.2012.05.024. [DOI] [PubMed] [Google Scholar]
- 115.Tsubokawa T, Katayama Y, Yamamoto T, Hirayama T, Koyama S. Treatment of thalamic pain by chronic motor cortex stimulation. Pacing Clin Electrophysiol. 1991;14:131–134. doi: 10.1111/j.1540-8159.1991.tb04058.x. [DOI] [PubMed] [Google Scholar]
- 116.Turk DC, Dworkin RH, Allen RR, Bellamy N, Brandenburg N, Carr DB, Cleeland C, Dionne R, Farrar JT, Galer BS, Hewitt DJ, Jadad AR, Katz NP, Kramer LD, Manning DC, McCormick CG, McDermott MP, McGrath P, Quessy S, Rappaport BA, Robinson JP, Royal MA, Simon L, Stauffer JW, Stein W, Tollett J, Witter J. Core outcome domains for chronic pain clinical trials: IMMPACT recommendations. Pain. 2003;106:337–345. doi: 10.1016/j.pain.2003.08.001. [DOI] [PubMed] [Google Scholar]
- 117.Velasco F, Argüelles C, Carrillo-Ruiz JD, Castro G, Velasco AL, Jiménez F, Velasco M. Efficacy of motor cortex stimulation in the treatment of neuropathic pain: a randomized double-blind trial. Journal of Neurosurgery. 2008;108:698–706. doi: 10.3171/JNS/2008/108/4/0698. [DOI] [PubMed] [Google Scholar]
- 118.Wittink H, Carr DB. Pain Management: Evidence, Outcomes and Quality of Life. St. Louis, MO: Elsevier; 2008. [Google Scholar]
- 119.Wittink H, Turk DC, Carr DB, Sukiennik A, Rogers W. Comparison of the redundancy, reliability, and responsiveness to change among SF-36, Oswestry Disability Index, and Multidimensional Pain Inventory. Clin J Pain. 2004;20:133–142. doi: 10.1097/00002508-200405000-00002. [DOI] [PubMed] [Google Scholar]
- 120.Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Katz RS, Mease P, Russell AS, Russell IJ, Winfield JB, Yunus MB. The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res (Hoboken) 2010;62:600–610. doi: 10.1002/acr.20140. [DOI] [PubMed] [Google Scholar]
- 121.Yang YR, Tseng CY, Chiou SY, Liao KK, Cheng SJ, Lai KL, Wang RY. Combination of rTMS and treadmill training modulates corticomotor inhibition and improves walking in Parkinson disease: a randomized trial. Neurorehabil Neural Repair. 2013;27:79–86. doi: 10.1177/1545968312451915. [DOI] [PubMed] [Google Scholar]
- 122.Yilmaz B, Kesikburun S, Yas AE, Tan AK. The effect of repetitive transcranial magnetic stimulation on refractory neuropathic pain in spinal cord injury. J Spinal Cord Med. 2014;37:397–400. doi: 10.1179/2045772313Y.0000000172. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


