Abstract
We evaluated effects of antiretroviral (ARV) therapy and lipid-based–nutrient-supplements (LNS) on iron, copper and zinc in milk of exclusively breastfeeding HIV-infected Malawian mothers, and their correlations with maternal and infant biomarkers. Human milk and blood at 2, 6, and 24wk postpartum and blood during pregnancy (≤30wk gestation) were collected from 535 mothers/infant-pairs in the Breastfeeding, Antiretrovirals, and Nutrition (BAN) study. The participants received ARV, LNS, ARV and LNS, or no intervention from 0–28wk postpartum. ARVs negatively affected copper and zinc milk concentrations, but only at 2wk, while LNS had no effect. Among all treatment groups, approximately 80–90% of copper and zinc, and <50% of iron concentrations met the current Adequate Intake for infants at 2wk and only 1–19% at 24wk. Pregnancy hemoglobin was negatively correlated with milk iron at 2 and 6wk (r=−0.18, p<0.02 for both). The associations of the milk minerals with each other were the strongest correlations observed (r=0.11–0.47, p<0.05 for all); none were found with infant biomarkers. At 2wk, moderately anemic women produced milk higher in iron when ferritin was higher or TfR lower. At 6wk, higher maternal AGP and CRP were associated with higher milk minerals in mildly anemic women. Infant TfR was lower when milk mineral concentrations were higher at 6wk and when mothers were moderately anemic during pregnancy. ARV affects copper and zinc milk concentrations in early lactation, and maternal hemoglobin during pregnancy and lactation could influence the association between milk minerals and maternal and infant iron status and biomarkers of inflammation.
Keywords: Iron, copper, zinc, human milk, HIV, hemoglobin status
INTRODUCTION
Human milk is thought to ensure a balanced and adequate supply of nutrients to infants and is recommended by the World Health Organization (WHO) as the sole food source for the first six months of life (Brown et al. 2009; World Health Organization 2010). Maternal iron, copper, and zinc intake and status are assumed to have no effect on human milk minerals (Vuori et al. 1980; Moser et al. 1988; Picciano 2001; Domellöf et al. 2004; Mello-Neto et al. 2014; Montalbetti et al. 2014); however, Krebs et al. (1985) reported that milk zinc concentrations are affected by maternal zinc intake within a physiological range and effects of low maternal intakes are most apparent with prolonged lactation. Even though the total concentration of iron, copper and zinc in human milk is low and decreases throughout lactation, their high bioavailability is assumed to ensure adequate supply during the first six months (Dorea 2000). Nevertheless, iron and zinc deficiencies in the perinatal period remain a public health concern, particularly in low-income countries, including Malawi (Gibson and Huddle 1998; Domellöf et al. 2004, National Statistical Office and ICF 2017), causing symptoms such as diarrhea, pneumonia, sub-optimal growth and development, normocytic hypochromic anemia, or even osteoporosis (Dauncey et al. 1977; Black et al. 2008).
In the context of maternal HIV-infection, breastfeeding is recommended for at least 12 months, with continued breastfeeding up to 24 months while maternal antiretroviral (ARV) therapy is provided to reduce the risk of mother-to-child HIV-transmission (World Health Organization 2016). However, higher energy and nutrient requirements due to breastfeeding and HIV-infection might increase the risk of nutrient deficiencies for mother and infant (de Pee & Semba 2010; Kayira et al. 2012). Our previous research has shown that ARVs negate the positive effects of maternal LNS-consumption during lactation on B-vitamin concentrations in maternal serum and human milk (Flax et al. 2015; Allen et al. 2016). Negative ARV effects have also been reported on vitamin D and B12 status (Paltiel et al. 1995; Woods et al. 2003; Childs et al. 2012). Thus, a potential impact of ARVs on iron, copper, and zinc concentrations in milk is possible and remains to be determined.
We analyzed samples from a randomized controlled trial, in which lactating women were assigned to either ARV or lipid-based nutrient supplementation (LNS), ARV and LNS, or no intervention, to: a) examine the effects of ARV and LNS on iron, copper, and zinc concentrations in milk; b) compare the concentration of each mineral analyzed to the values that were used to set the Adequate Intake (AI) for infants 0–6 months (Institute of Medicine 2001); c) assess correlations among the milk nutrients analyzed (iron, copper, zinc, fat); and d) examine relationships between milk minerals and maternal and infant characteristics, mineral and inflammation status using maternal and infant biomarkers.
METHODS AND MATERIALS
Participants and sample collection
The participants of the Breastfeeding, Antiretrovirals, and Nutrition (BAN) study included HIV-infected women recruited 2004–2009 from four antenatal clinics in Lilongwe, Malawi. Details of the recruitment and study design have been previously described (Ferguson et al. 2009; van der Horst et al. 2009; Chasela et al. 2010; Kayira et al. 2012). Informed consent was obtained from all mothers. Based on the WHO guidelines at the time of the study, participants were encouraged to exclusively breastfeed for 24 weeks (wk) followed by rapid weaning from 24–28wk.
At delivery, mothers and their infants were randomized to a 2-arm (LNS, no-LNS) by 3-arm (maternal ARV, infant ARV, or neither) factorial design, which was condensed to four maternal intervention groups (Supplemental Figure 1). Infant ARV treatments were not considered as this report focuses on breast milk minerals and infant treatment would not influence human milk status. Since the LNS purposely included provision of energy and macronutrients, and micronutrients, neither participants nor physicians could be blinded to the study arm. Outcome assessors and sample and data analysts were blinded to the treatment allocation. The screening and enrollment process was conducted by the study nurses; a data manager produced the random distribution. The study pharmacist assigned the participants to the intervention using sequentially numbered envelopes and handed out ARV and LNS during the regular study visits at 0, 1, 2, 4, 6, 8, 12, 18, 21, 24, and 28wk postpartum. The women were instructed to consume two sachets of the LNS per day produced by Nutriset, France, www.nutriset.fr (Supplemental Table 1). The LNS provided 0.3mg copper, 19mg zinc, and 15mg iron equivalent to 23, 158, and 168% of the U.S.-Canada Recommended Dietary Allowances for copper, zinc, and iron respectively (Institute of Medicine 2001). The maternal ARV regimen consisted of zidovudine (300mg) and lamivudine (150mg) (Combivir®, GlaxoSmithKline) plus either nevirapine (until January 2005), nelfinavir (January 2005-February 2006) or lopinavir (200mg) and ritonavir (50mg) (Kaletra; Abbott; February 2006 until study completion).
Reports of maternal LNS consumption were obtained at 1, 4, 8, 12, and 21wk. Maternal hemoglobin (Hb) was at assessed at ≤ 30wk gestation during the prenatal screening, and maternal and infant venous blood was collected at birth, 2, 6, 12, 18, and 24wk for further Hb measurements. Plasma for additional biomarker analysis was separated from red blood cells within 60min and stored at −70°C in 1mL aliquots. 10mL of human milk was collected during the regular study visits at 2 and 24wk (n=366), or 6 and 24wk (n=169) when a 2wk milk or infant plasma sample was insufficient for micronutrient analysis. The milk was manually expressed by the study participant yielding an opportunistic sample that was immediately frozen after collection. The number of participants with available milk, maternal, and infant plasma samples pre-determined the sample size (n=535). Participants were preferentially selected if they provided anthropometry and dietary intake data. If the infants became HIV-positive or were multiple births, they were excluded from the sub-set. Details of the primary study’s sample size calculations have been previously described (van der Horst et al. 2009).
Samples were initially shipped on dry ice to the Centers for Disease Control and Prevention (CDC) in Atlanta and stored at −80°C until distribution to the USDA, ARS Western Human Nutrition Research Center (WHNRC) in Davis, CA for analysis.
Biochemical Analyses
Iron, copper, and zinc were analyzed in 500µL of whole human milk. 150µL of the 1.00ppm calibration standard in nitric acid (HNO3, 3.2N, for trace analysis), 2.25mL HNO3 (3.2N) and 100µL peroxide (for trace analysis) were added to a final volume of 3.0mL. Samples were mixed and microwaved for 15min at 90°C (600 watts, 5min ramp from ambient temperature to 90°C, temperature controlled). After a 5min cooling step the samples were centrifuged for 10min at 2750 × g (4°C) after which they were transferred into the 8mL polypropylene tubes (13 × 100mm, Perfector Scientific, Fair Lawn, NJ, USA) for analysis or capped and stored at 4°C until analysis. The laboratory internal control (BLS) and the 0.2ppm standard, analyzed with each sample set, revealed an inter-assay variation of 1.5 – 7.0% and an intra-assay variation of 0.1–10.8% over a period of 6wk (n=25). The calibration curve for each mineral consisted of a blank and ten standard solutions in a linear range of 0.0125 – 2.000ppm prepared in 3.2N HNO3. Due to the difference in concentration of each analyte in human milk, the actual standard concentrations used for each mineral were as follows: Cu: 0.0125–1.000ppm, Fe: 0.025–1.000ppm, and Zn: 0.0125–2.000ppm. Mean recovery rates for copper, iron, and zinc were 92.6 ±5.7%, 89.4 ±7.2% and 94.7 ± 6.8% respectively. The analyses were conducted using a Varian VISTA AX CCD Simultaneous ICP-AES (Folsom, CA, USA) operated by ICPExpert software. Samples were digested using the CEM Microwave Accelerated Reaction System (MARS 5; Matthews, NC, USA). The milk fat was measured using the Creamatocrit Plus (Medela, McHenry, IL, USA) according to the manufacturer’s protocol. The tube reader’s accuracy was validated using the Medela control strip.
The inflammatory markers α-1-acid glycoprotein (AGP) and C-reactive protein (CRP), and soluble transferrin receptors (TfR) in maternal and infant plasma were analyzed by a COBAS® Integra 400 Plus multianalyte-analyzer (Roche Diagnostics, Mannheim, Germany). Ferritin concentrations were determined using IRMA Ferritin Coat-a-Count radioimmunoassay (Siemens Health Care Diagnostics, Tarrytown, NY, USA), and Hb was measured using the AcT or AcT 5-part Differential Analyzer (Beckman Coulter, Fullerton, CA, USA).
Ethics
This research was approved by the Malawian National Health Science Research Committee, the Institutional Review Boards at the University of North Carolina at Chapel Hill, the U.S. Centers for Disease Control and Prevention, and the University of California, Davis (Clinical Trials.gov; NCT00164762). The trial was monitored for safety and efficacy by the National Institute of Allergy and Infectious Diseases Vaccine and Prevention Data and Safety Monitoring Board.
Statistical Methods
Since milk sample collection started 2 to 6wk after the LNS intervention, no true baseline concentrations were available for statistical analyses (Allen et al. 2016). A separate binary variable, hereafter referred to FTP (first time point), was used to control for whether the first time point of sample collection occurred at 2wk (FTP2) or 6wk (FTP6). The outcomes were concentrations of iron, copper, and zinc in human milk, within the 4 defined groups (ARV, LNS, ARV/LNS, and control). SAS® for Windows Release 9.4 (SAS Institute, Cary, NC, USA) was used for all statistical analyses. Square root transformations were performed on all outcome variables to normalize the distributions. The original hypothesis focused on the effect of LNS supplementation on outcomes. However, preliminary data revealed significant effects due to ARV for some of the minerals so the hypothesis was modified to include possible main effects and modifying effects of ARV. Mixed models repeated measures analysis of variance was used to fit a 4-factor model, which included LNS, ARV, and FTP as between-subject main effects, time as a within-subject main effect, all 2-, 3-, and 4-factor interactions, and a random effect of subject assuming an unstructured covariance matrix. When there was no significant interaction between treatment and FTP, treatment was assessed as a main effect only.
All analyses described in this paragraph were conducted using pooled milk values for each mineral from all treatment groups. Iron, copper and zinc milk concentrations were significantly lower at 6wk than at 2wk; thus, to estimate the correlations of the breast milk iron, copper, and zinc concentrations with maternal and infant biomarkers and characteristics, we analyzed the data separately by FTP (2 or 6wk) subgroup. Pearson correlations procedure was used. Concentrations of maternal ferritin, maternal CRP, maternal TfR, infant ferritin, infant CRP, infant AGP, and maternal age were log-transformed; infant TfR and birthweight were square-root transformed, and maternal AGP, body mass index (BMI), and infant Hb were inverted (1/x) to achieve normal distributions. Inverted variables were multiplied by −1 to preserve direction. Pregnancy Hb, maternal Hb and infant birth length were normally distributed and not transformed. Spearman correlations were used to explore relationships of breast milk iron, copper, and zinc concentrations with non-normalized maternal and infant characteristics including marital status, literacy, education, parity, famine season (August to March), and infant sex. Linear regression analysis was used to examine associations a) between maternal iron status (ferritin, TfR) and inflammation (AGP, CRP) biomarkers on human milk iron, copper, and zinc at 2, 6, and 24wk, stratified by anemia status during pregnancy (non-anemic: Hb ≥ 110g/L, mildly anemic: Hb 100–109g/L, moderately anemic: Hb 70–99g/L, severely anemic: Hb ≤ 70g/L) and lactation (non-anemic: Hb ≥ 120g/L, mildly anemic: Hb 110–119g/L, moderately anemic: Hb 80–109g/L, severely anemic: Hb ≤ 80g/L) (World Health Organization 2011) and b) between maternal iron status biomarkers (ferritin, TfR, Hb, pregnancy Hb) on human milk iron, copper, and zinc at 2, 6, and 24wk, stratified by inflammation status (AGP > 1g/L and CRP > 5mg/L).
For all procedures, p-values <0.05 were considered to be statistically significant. Significant differences in the distribution of categorical variables were examined using the chi-square test. Significant changes in milk adequacy (based on AI) over time (2, 6, 24wk) were tested using the GLIMMIX procedure.
The measured human milk iron, copper, and zinc concentrations at each time point (TP), FTP of milk collection and treatment group were also compared to milk values from well-nourished women used by the Institute of Medicine to set Adequate Intakes (AIs) for infants from 0–6mo of age (Institute of Medicine 2001).
RESULTS
Maternal characteristics at first time point
The characteristics of the participants were similar among treatment groups at the FTP of human milk collection (Table 1). Significant differences were only observed for the CD4 counts with higher counts for the groups that received ARV. The median BMI was within the normal range and the overall compliance with supplementation and ARV treatment was high. In the adherence reports collected over five follow-up visits the mothers self-reported that they took their prescribed ARV treatment 89% of the time and LNS supplement 92% of the time. The self-reported frequency of exclusive breastfeeding was 96% at 21wk postpartum (Chasela et al. 2010; Kayira et al. 2012).
Table 1.
Characteristics of mothers in the BAN Study at the first time point of collection (2/6 weeks)1.
| Treatment group | |||||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||
| Control | LNS | ARV | ARV + LNS | ||||||
|
|
|||||||||
| Characteristics | n | Median (IQR) | n | Median (IQR) | n | Median (IQR) | n | Median (IQR) | P-valueg |
| Age (y) | 176 | 25.5 (22.9–29.8) | 183 | 26.2 (22.2–29.9) | 85 | 27.0 (24.0–29.4) | 90 | 25.0 (22.9–30.0) | 0.58 |
| Literacy (%) | 172 | 78.5 | 179 | 75.4 | 81 | 76.5 | 85 | 77.6 | 0.92 |
| Postprimary education (%) | 177 | 36.7 | 185 | 37.8 | 85 | 35.3 | 90 | 32.2 | 0.75 |
| Married (%) | 177 | 90.4 | 185 | 90.3 | 85 | 89.4 | 90 | 92.2 | 0.39 |
| Primiparous (%) | 177 | 18.1 | 185 | 17.8 | 85 | 11.8 | 90 | 16.7 | 0.59 |
| Vaginal delivery (%) | 177 | 96.6 | 185 | 95.7 | 85 | 96.5 | 90 | 94.4 | 0.91 |
| Anthropometric measurements | |||||||||
| Height (cm) | 177 | 157 (154–160) | 185 | 155 (152–159) | 85 | 157 (154–160) | 90 | 157 (154–161) | 0.05 |
| Weight (kg) | 177 | 55.5 (50.0–60.3) | 185 | 54.4 (50.3–59.1) | 85 | 54.6 (50.5–60.2) | 90 | 54.5 (50.2–60.4) | 0.84 |
| BMI (kg/m2) | 177 | 22.4 (20.7–24.1) | 185 | 22.3 (20.9–24.2) | 85 | 22.3 (20.3–24.3) | 90 | 22.2 (20.8–23.7) | 0.55 |
| BMI < 18.5 (%)a | 177 | 0.0 | 185 | 3.2 | 85 | 4.7 | 90 | 5.6 | 0.031 |
| BMI 18.5–24.9 (%) | 177 | 83.1 | 185 | 77.3 | 85 | 75.3 | 90 | 78.9 | 0.43 |
| BMI 25–29.9 (%) | 177 | 15.3 | 185 | 16.2 | 85 | 15.3 | 90 | 15.6 | 0.99 |
| BMI ≥ 30 (%) | 177 | 1.7 | 185 | 3.2 | 85 | 4.7 | 90 | 0.0 | 0.17 |
| Laboratory measurements | |||||||||
| AGP (g/L) | 177 | 1.2 (0.9–1.5) | 185 | 1.2 (0.9–1.4) | 85 | 1.2 (1.0–1.6) | 90 | 1.2 (0.9–1.4) | 0.65 |
| AGP > 1g/L (%)b | 177 | 27.1 | 122 | 35.7 | 85 | 40.0 | 90 | 35.6 | 0.14 |
| CRP (mg/L) | 177 | 3.3 (1.3–9.1) | 185 | 3.2 (1.5–7.5) | 85 | 2.8 (1.5–10.0) | 90 | 2.7 (1.4–6.1) | 0.43 |
| CRP > 5mg/L (%)c | 177 | 3.4 | 185 | 3.8 | 85 | 1.2 | 90 | 3.3 | 0.71 |
| AGP > 1gL and CRP > 5mg/L (%) | 177 | 39.0 | 185 | 30.3 | 85 | 35.3 | 90 | 25.6 | 0.12 |
| Ferritin | 177 | 30.2 (15.8–56.0) | 185 | 25.5 (13.0–49.7) | 85 | 26.0 (16.0–55.1) | 90 | 26.2 (12.8–68.5) | 0.85 |
| TfR | 177 | 4.9 (3.7–6.4) | 185 | 5.2 (3.9–7.2) | 85 | 5.1 (3.8–6.6) | 90 | 5.2 (3.7–7.0) | 0.43 |
| Hemoglobin (g/L) | 177 | 122 (111–131) | 185 | 121 (111–131) | 85 | 121 (107–126) | 90 | 120 (111–131) | 0.28 |
| Iron deficiency (%)d | 177 | 5.1 | 185 | 7.6 | 85 | 10.6 | 90 | 13.3 | 0.10 |
| Iron deficiency anemia (%)e | 177 | 3.4 | 185 | 5.9 | 85 | 7.1 | 90 | 13.3 | 0.020 |
| Anemic during pregnancy (%)f | 177 | 53.7 | 185 | 56.2 | 85 | 51.8 | 90 | 47.8 | 0.58 |
| CD4 count (cells/µL) | 159 | 465 (319–665) | 170 | 500 (337–738) | 78 | 616 (439–780) | 85 | 607 (412–796) | <0.001 |
Characteristics are provided for the sub-sample (n=535). Anemic during pregnancy: hemoglobin < 110g/L; ARV, antiretroviral; AGP, α-1-acid glycoprotein; BAN, Breastfeeding, Antiretrovirals, and Nutrition; CRP, C-reactive protein; IQR, interquartile range; LNS, lipid-based nutrient supplement; TfR, soluble transferrin receptors.
BMI categories: <18.5, underweight; 18.5–24.9, normal; 25–29.9, overweight; >30, obese.
Elevated AGP as an indicator for chronic inflammation.
Elevated CRP as an indicator acute inflammation.
Iron deficiency defined as ferritin < 15µg/L and TfR > 8.5mg/L.
Iron deficiency anemia defined as Hb < 120g/L, ferritin < 15µg/L and TfR > 8.5mg/L.
Defined as Hb < 110g/L.
P-value: chi square test for categorical variables and generalized linear models for continuous variables.
Treatment effects and time interactions
The mixed model analysis revealed that the concentrations of the three minerals changed over time (TP) and differed by FTP (p<0.02 for all). For iron, no interactions by treatment (ARV and LNS) or with treatment and TP and/or FTP were significant indicating that the effects of ARV and LNS at 2, 6, and 24 wk were not different from each other (Supplemental Table 2). Therefore, pooled data for all treatment groups and all time points combined were used for further statistical analyses involving iron. ARV by TP by FTP interactions were significant for copper (p=0.034), while ARV by FTP interactions were significant for zinc (p=0.031). Thus, to evaluate the main effects, samples from 2, 6, and 24wk were analyzed separately for copper and zinc.
The reduction in milk iron concentrations between 2, 6 and 24wk was independent of treatment. ARV by LNS interactions were not significant for any of the minerals analyzed nor were LNS and ARV main effects significant for iron (Table 2). The mixed model analysis for copper and zinc at 2, 6, and 24wk showed that ARV treatment significantly and negatively affected milk copper and zinc concentrations (p=0.044 and p=0.014) but only at the initial 2wk time point.
Table 2.
Median concentrations and interquartile ranges (IQR) of iron, copper, and zinc and main effects of ARV and LNS of iron, copper, and zinc at 2, 6, and 24 wk in breast milk of HIV-infected Malawian mothers assigned to one of the four treatment arms in the BAN study
| Treatment | Iron
|
Copper
|
Zinc
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| wk | 2 | 6 | 24 | 2 | 6 | 24 | 2 | 6 | 24 | |
| Control mg/L | n | 118 | 59 | 177 | 118 | 59 | 177 | 118 | 59 | 177 |
| Median | 0.342 | 0.250 | 0.190 | 0.387 | 0.223 | 0.143 | 3.57 | 2.49 | 1.16 | |
| IQR | 0.23–0.50 | 0.17–0.40 | 0.13–0.30 | 0.32–0.47 | 0.20–0.31 | 0.10–0.18 | 3.01–4.21 | 2.07–3.06 | 0.75–1.57 | |
| LNS mg/L | n | 140 | 45 | 185 | 140 | 45 | 185 | 140 | 45 | 185 |
| Median | 0.331 | 0.230 | 0.188 | 0.372 | 0.247 | 0.127 | 3.59 | 2.39 | 1.05 | |
| IQR | 0.25–0.49 | 0.14–0.37 | 0.11–0.27 | 0.32–0.45 | 0.21–0.30 | 0.09–0.17 | 2.92–4.31 | 1.89–3.10 | 0.70–1.56 | |
| ARV mg/L | n | 53 | 31 | 85 | 53 | 31 | 85 | 53 | 31 | 85 |
| Median | 0.337 | 0.297 | 0.157 | 0.379 | 0.273 | 0.151 | 3.16 | 2.46 | 1.05 | |
| IQR | 0.24–0.46 | 0.16–0.45 | 0.11–0.27 | 0.32–0.45 | 0.23–0.35 | 0.12–0.207 | 2.75–3.63 | 1.95–3.20 | 0.75–1.54 | |
| ARV/LNS mg/L | n | 55 | 34 | 90 | 55 | 34 | 90 | 55 | 34 | 90 |
| Median | 0.301 | 0.265 | 0.210 | 0.341 | 0.258 | 0.141 | 3.40 | 2.47 | 1.13 | |
| IQR | 0.21–0.43 | 0.13–0.36 | 0.13–0.27 | 0.29–0.40 | 0.21–0.33 | 0.10–0.18 | 2.88–3.85 | 1.95–2.94 | 0.72–1.57 | |
|
| ||||||||||
| Treatment effects1 | ||||||||||
| LNS | LS Mean | 0.516 | 0.615 | 0.504 | 0.362 | 1.87 | 1.53 | 1.04 | ||
| No LNS | LS Mean | 0.514 | 0.621 | 0.508 | 0.376 | 1.86 | 1.57 | 1.07 | ||
| P-value | 0.86 | 0.49 | 0.80 | 0.08 | 0.74 | 0.34 | 0.14 | |||
| ARV | LS Mean | 0.505 | 0.603 | 0.519 | 0.378 | 1.82 | 1.55 | 1.06 | ||
| No ARV | LS Mean | 0.520 | 0.624 | 0.498 | 0.364 | 1.89 | 1.55 | 1.06 | ||
| P-value | 0.23 | 0.044 | 0.16 | 0.11 | 0.014 | 0.95 | 0.95 | |||
Treatment effects (LNS – no LNS; ARV – no ARV) were tested by mixed model repeated measures ANOVA. ARV, antiretrovirals; BAN, Breastfeeding, Antiretrovirals, and Nutrition; LNS, lipid-based nutrient supplement; LS Mean, least-square mean.
Comparison of milk iron, copper, and zinc concentrations with values used to set the Adequate Intake (AI) for infants 0–6mo
At 2wk, 38–48% of all milk samples met the milk iron concentrations assumed from reported data used to estimate the AI for infants from 0–6mo (Table 3). Depending on treatment group approximately 89–94% and 78–88% of the samples had copper and zinc concentrations at 2wk that corresponded to AI values (Institute of Medicine 2001).
Table 3.
Percentage [%] of milk samples from the sub-sample of the BAN Study that meet the values used to set the Adequate Intake (AI) for each mineral, by collection time and treatment group
| Mineral [mg/L] |
AI [mg/L] |
Control | LNS | ARV | ARV/LNS | |||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||||
| [%] | (n) | [%] | (n) | [%] | (n) | [%] | (n) | P-valueb | ||
| Iron | ||||||||||
| 2 wk | 0.346 | 48 | (57/118) | 44 | (61/140) | 45 | (24/53) | 38 | (21/55) | 0.62 |
| 6 wk | 32 | (19/59) | 27 | (12/45) | 35 | (11/31) | 32 | (11/34) | 0.83 | |
| 24 wk | 18 | (31/177) | 16 | (30/185) | 11 | (9/85) | 19 | (15/80) | 0.54 | |
| p-valuea | < 0.024 | |||||||||
| Copper | ||||||||||
| 2 wk | 0.256 | 91 | (107/118) | 94 | (132/140) | 92 | (49/53) | 89 | (49/55) | 0.64 |
| 6 wk | 39 | (23/59) | 44 | (20/45) | 61 | (19/31) | 50 | (17/34) | 0.17 | |
| 24 wk | 9 | (15/177) | 6 | (11/185) | 9 | (8/85) | 5 | (4/80) | 0.48 | |
| p-value | < 0.001 | |||||||||
| Zinc | ||||||||||
| 2 wk | 2.564 | 88 | (104/118) | 88 | (123/140) | 81 | (43/53) | 78 | (43/55) | 0.21 |
| 6 wk | 44 | (26/59) | 40 | (18/45) | 45 | (14/31) | 47 | (16/31) | 0.92 | |
| 24 wk | 3 | (6/177) | 1 | (2/185) | 4 | (1/85) | 1 | (1/85) | 0.34 | |
| p-value | < 0.001 | |||||||||
ARV, antiretrovirals; BAN, Breastfeeding Antiretrovirals, and Nutrition; LNS, lipid based nutrient; number of samples given in parentheses (numerator: n of samples that met AI, denominator: total n).
P-values for comparison of proportions of samples with adequate milk iron, copper, zinc concentrations over time (2, 6, 24wk; proc glimmix).
P-value for comparison of proportions of samples with adequate milk iron, copper, and zinc concentrations based on treatment (LNS, ARV, ARV/LNS, and control; chi square test).
Lower breast milk iron, copper, and zinc concentrations were observed at 6wk: 27–35% of the milk samples met the AI for iron concentrations, 39–61% and 40–47% the AI for copper and zinc concentrations.
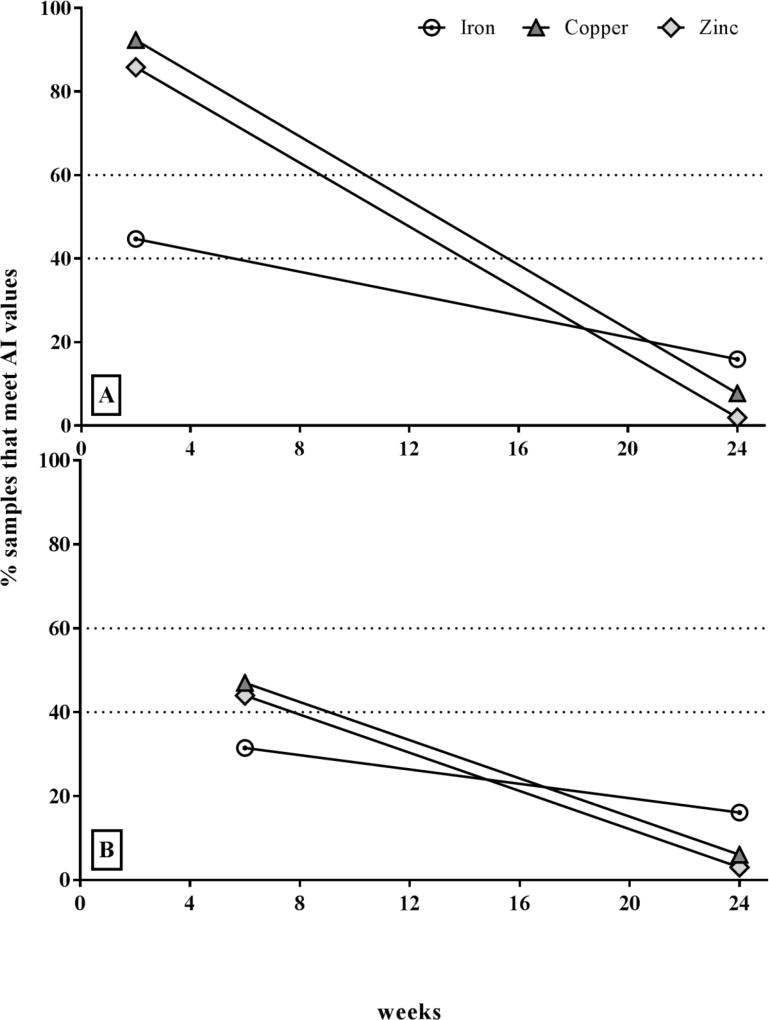
At 24wk only about 11–19% of all samples met the AI estimates for iron. Copper and zinc concentrations were even lower; only 5–9% (copper) and 1–4% (zinc) of the samples met the AI concentrations. Plotting the relative amount of samples that met the AI longitudinally by FTP subgroup (2–24 and 6–24wk), copper and zinc followed the same pattern of decrease, while the iron AI was met by considerably fewer samples compared to the copper and zinc already at 2wk, but then followed a slower rate of decrease (Figure 1).
Figure 1.
Relative median decrease [%] in human milk iron, copper, and zinc over time compared to AI (values pooled from all treatment groups at each time point of sample collection: A – FTP2 subgroup (2–24wk; n = 366); B – FTP6 subgroup (6–24wk; n = 169).
Correlations of maternal and infant biomarkers and characteristics with breast milk minerals
Iron, 2 and 6wk
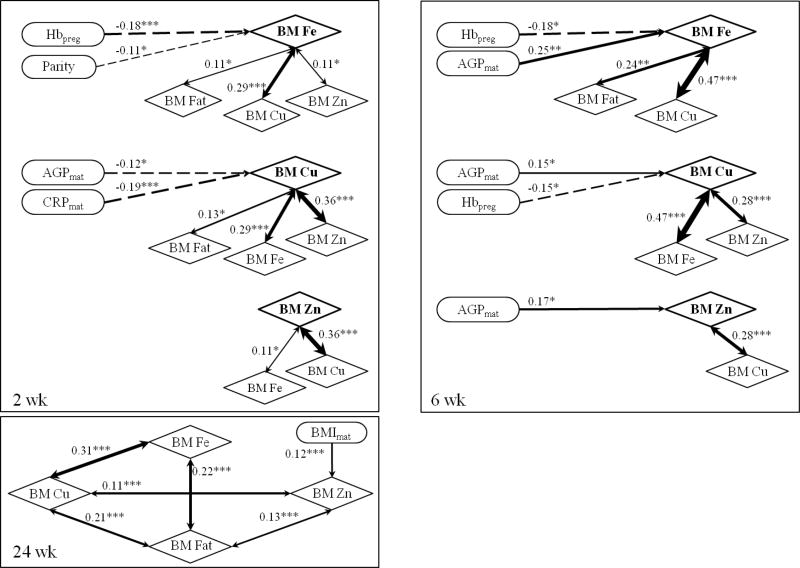
At 2wk, human milk iron concentrations were significantly correlated with pregnancy Hb (r = −0.18, p<0.001) and parity (r = −0.11, p=0.031) as well as with breast milk copper (r = 0.29, p<0.001), zinc (r = 0.11, p=0.028), and fat (r = 0.11, p=0.044; Figure 2). At 6wk, breast milk iron was correlated with pregnancy Hb (r = −0.18, p=0.019), maternal AGP (r = −0.25, p=0.001), and breast milk copper (r = 0.47, p<0.001) and fat (r = 0.24, p=0.002).
Figure 2.
Significant correlations between milk minerals and maternal biomarkers at 2, 6, and 24 wk. Pearson’s correlation coefficients (Spearman correlations coefficient for the characteristics) are shown and level of significance as: * p < 0.05; ** p < 0.01; *** p < 0.001 (Preg.- pregnancy (during screening), Hb – hemoglobin, BM - breast milk, Fe - iron, Cu – copper, Zn – zinc, Mat. – maternal, AGP - α-1-acid glycoprotein, CRP - C-reactive protein, BMI - body mass index).
Copper, 2 and 6wk
At 2wk, human milk copper concentrations were correlated with maternal AGP (r = 0.12, p=0.021) and CRP (r = −0.19, p<0.001), and milk iron, zinc (r = 0.36, p<0.001), and fat (r = 0.13, p=0.01) (Figure 2). At 6wk, milk copper was also correlated with pregnancy Hb (r = −0.15, p=0.047), maternal AGP (r = −0.15, p=0.049) and breast milk iron and zinc (r = 0.28, p<0.001).
Zinc, 2 and 6wk
At 2wk, milk zinc concentrations were significantly correlated only with milk iron and copper. At 6wk, human milk zinc was correlated with maternal AGP (r = −0.17, p=0.03) and breast milk copper.
Iron, copper, and zinc, 24wk
At 24wk, neither iron nor copper concentrations were correlated with any of the maternal or infant biomarkers (Figure 2). Only zinc showed a correlation with maternal BMI (r = 0.12, p=0.006). Significant correlations remained between the analyzed human milk minerals and fat: iron was correlated with copper (r = 0.31, p<0.001) and fat (r = 0.22, p<0.001), and copper with zinc (r = 0.11, p < 0.001) and fat (r = 0.21, p<0.001), additionally, zinc was correlated with fat (r = 0.13, p=0.003).
None of the infant biomarkers or characteristics were significantly associated with human milk iron, copper, or zinc concentrations at any time point.
Associations of human milk iron, copper and zinc with maternal and infant biomarkers, stratified by maternal Hb (anemia status) during pregnancy and lactation
Maternal Biomarkers
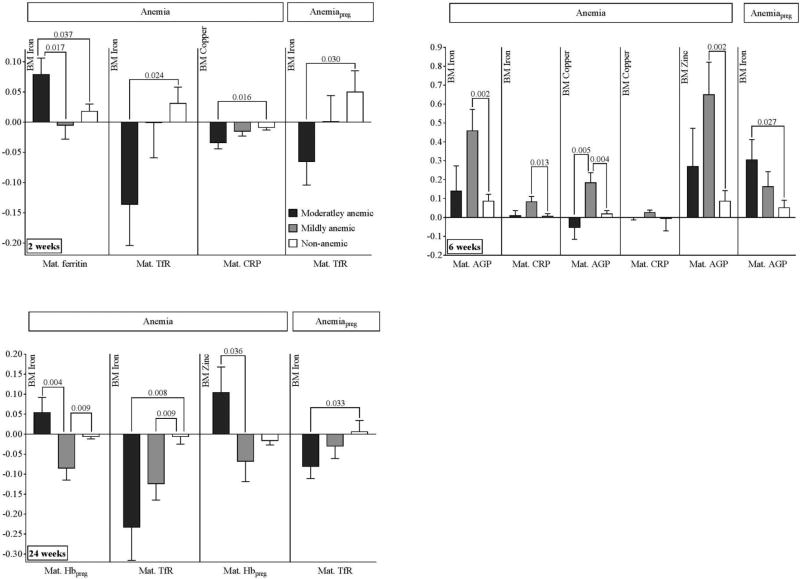
2wk
When women were moderately anemic postpartum, higher ferritin during lactation was associated with higher human milk iron concentrations when compared to mildly anemic (p=0.017) and non-anemic (p=0.037, Figure 3) pregnant women, while higher TfR in lactation was associated with lower milk iron compared to the non-anemic group (p=0.024). Additionally, higher maternal CRP during lactation was associated with lower milk copper compared to that of non-anemic women (p=0.016). The degree of anemia in pregnancy did not affect the relationship of the maternal biomarkers to milk zinc concentrations (data not shown). When women were moderately anemic during pregnancy, higher TfR concentrations postpartum were associated with lower milk iron concentrations compared to those of non-anemic women (p=0.030).
Figure 3.
Associations of human milk iron, copper, and zinc with maternal biomarkers stratified by maternal hemoglobin status during pregnancy and lactation on (Coefficients and SEs obtained from regression procedure displayed as bar graphs with error bars. P-values for comparisons of moderately or mildly anemic to non-anemic group, and comparison of moderately to mildly anemic group, using linear regression analysis. Anemia, state of anemia - moderately, mildly, or non-anemic - based on maternal hemoglobin status at indicated week postpartum (World Health Organization 2003). AnemiaPreg, state of anemia during pregnancy (moderately, mildly, or non-anemic based on maternal Hb during pregnancy, World Health Organization, 2003). BM – breast milk, CRP - C-reactive protein, AGP - α-1-acid glycoprotein, TfR - soluble transferrin receptors; n - number of samples (moderatly anemic/mildly anemic/non-anemic): 2wk anemia: 41/49/276; 2wk anemiaPreg: 91/106/169; 6wk anemia: 13/25/131; 6wk anemiaPreg: 35/53/81; 24wk anemia: 16/45/476; 24wk anemiaPreg: 126/160/251; Separate models were used for each time point and FTP and anemia status).
6wk
In women who were mildly anemic during lactation, higher CRP postpartum was associated with higher milk iron (p=0.013) and copper (p=0.036) compared to non-anemic women, while higher AGP was associated with higher milk iron (p=0.002), and zinc (p=0.002) concentrations. Higher AGP was associated with lower copper concentrations when comparing moderately anemic postpartum women to mildly-anemic women (p=0.004), yet higher AGP was associated with higher copper when comparing mildly anemic to non-anemic postpartum women (p=0.005). When women were moderately anemic during pregnancy, higher postpartum AGP concentrations at 6wk were associated with higher milk iron concentrations compared to concentrations in non-anemic women (p=0.027).
24wk
Higher maternal TfR concentrations at 24wk were associated with lower milk iron values in moderately (p=0.008) and mildly (p=0.009) anemic women compared to non-anemic participants at 24wk.
Infant biomarkers
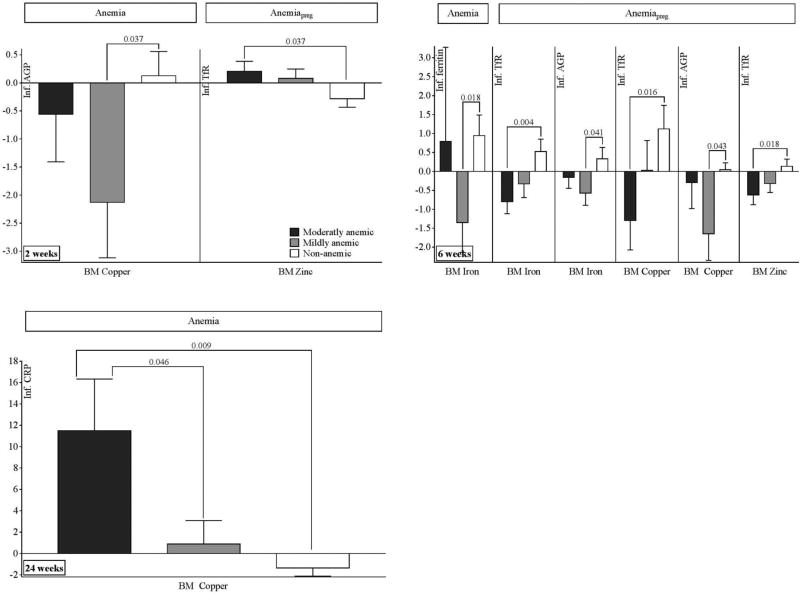
2wk
Higher milk copper was associated with lower AGP at 2wk among infants of mothers who were mildly anemic during lactation, compared to infants of mothers who were not anemic, (p=0.037) (Figure 4). For those infants whose mothers were moderately anemic during pregnancy, higher milk zinc was associated with higher infant TfR concentrations compared to infants born to women who were not anemic during pregnancy (p=0.037).
Figure 4.
Associations of human milk iron, copper, and zinc with infant biomarkers stratified by maternal hemoglobin status during pregnancy and lactation (Coefficients and SEs obtained from regression procedure displayed as bar graphs with error bars). P-values for comparisons of moderately or mildly anemic to non-anemic group, and comparison of moderately to mildly anemic group, using linear regression analysis. Anemia, state of anemia - moderately, mildly, or non-anemic - based on maternal hemoglobin status at indicated week postpartum (World Health Organization 2003). AnemiaPreg, state of anemia during pregnancy (moderately, mildly, or non-anemic based on maternal Hb during pregnancy, World Health Organization, 2003). BM – breast milk, CRP - C-reactive protein, AGP - α-1-acid glycoprotein, TfR - soluble transferrin receptors, n - number of samples (moderatly anemic/mildly anemic/non-anemic): 2wk anemia: 41/49/276; 2wk anemiaPreg: 91/106/169; 6wk anemia: 13/25/131; 6wk anemiaPreg: 35/53/81; 24wk anemia: 16/45/476; 24wk anemiaPreg: 126/160/251; Separate models were used for each time point and FTP and anemia status).
6wk
When the women had been mildly anemic during lactation, higher milk iron concentrations were associated with lower infant ferritin (p=0.018) compared to infants born to non-anemic women. When mothers were moderately anemic during pregnancy, higher milk iron, copper, and zinc concentrations were associated with lower infant TfR compared to women whom were not anemic (piron=0.004, pcopper=0.016, pzinc=0.018). When women were mildly anemic during pregnancy, higher milk iron and copper were associated with lower infant AGP at 6wk compared to non-anemic women during pregnancy (piron=0.041, pcopper=0.043).
24wk
When mothers were moderately anemic, increasing copper in milk was associated with increasing infant CRP when compared to mildly (p=0.046) and non-anemic (p=0.009) women.
Human milk iron, copper and zinc concentrations and inflammation
In the pooled samples set (n = 1074), iron, copper, and zinc concentrations in the milk of HIV-infected Malawian mothers were significantly higher (p<0.001 for all; Table 4) in women with evidence of inflammation (AGP > 1g/L, CRP > 5mg/L). Moreover, women with inflammation revealed higher milk iron concentrations at 2wk when their pregnancy Hb status was lower (p = 0.015; no inflammation (coeff. (std error): −0.012 (0.010), inflammation: −0.050 (0.013)), and showed higher milk zinc concentrations at 6wk when their pregnancy Hb status was higher (p = 0.020; no inflammation (coeff. (std error): −0.032 (0.022), inflammation: 0.091 (0.047)).
Table 4.
Median concentrations and interquartile ranges (IQR) of the pooled samples (all TP and FTP) of iron, copper, and zinc in breast milk of HIV-infected Malawian mothers in the BAN Study based on inflammation status1
| Mineral | No inflammation | Inflammation |
|---|---|---|
| n | 835 | 239 |
| Iron | ||
| Median, mg/L | 0.224 | 0.325 |
| IQR, mg/L | 0.140–0.342 | 0.212–0.456 |
| p-valuea | < 0.001 | |
|
| ||
| Copper | ||
| Median, mg/L | 0.196 | 0.291 |
| IQR, mg/L | 0.129–0.319 | 0.192–0.375 |
| p-value | < 0.001 | |
|
| ||
| Zinc | ||
| Median, mg/L | 1.75 | 2.90 |
| IQR, mg/L | 0.988–2.93 | 1.69–3.74 |
| p-value | < 0.001 | |
Inflammation defined as AGP > 1g/L and CRP > 5mg/L.
P-values obtained from general linear models.
DISCUSSION
The recommendation to exclusively breast feed for the first 6mo of life demands an understanding of how maternal micronutrient supplementation and drugs, such as ARVs, affect human milk nutrient concentrations. LNS are commonly used to treat severe acute malnutrition in children; their effectiveness in improving birth and health outcomes in infants and children with moderate malnutrition and their effectiveness in prevention of stunting has also been under evaluation (Phuka et al. 2010; Thakwalakwa et al. 2010; Adu-Afarwuah et al. 2015, Prado et al., 2016). In the BAN study, maternal LNS mitigated maternal weight-loss even when ARVs were given (Kayira et al. 2012) and increased human milk B-vitamin concentrations, while ARVs negatively affected some B-vitamins. When ARV and LNS were given, ARV diminished the positive LNS effect (Allen et al. 2016). However, beneficial effects of maternal supplemetation or fortification on human milk B-vitamins have been also observed in other studies (Duggan et al. 2014; Shahab-Ferdows et al. 2015; Siddiqua et al. 2015; Whitfield et al. 2016).
Treatment effects
Human milk iron, copper, and zinc concentrations are thought to be unaffected by maternal supplementation (Vuori et al. 1980; Moser et al. 1988; Picciano 2001; Domellöf et al. 2004; Montalbetti et al. 2014), which is consistent with our results. Maternal ARV treatment, however, negatively affected milk copper and zinc concentrations at 2wk, resulting in a 5–8% reduction of the median copper and zinc concentration available to the infant. These reduced amounts might not be significant to a healthy infant but could impact infants exposed to nutritional deficiencies as they do not possess extensive zinc or copper stores. Moreover, maternal ARV treatment in this study was reflected in the milk and lamivudine was found in infant plasma (Shapiro et al. 2005; Corbett et al. 2014), observations particularly important in light of the 2016 WHO guidelines that recommend ARV provision to HIV-infected mothers of HIV-exposed infants. Certain ARVs provided to the mother are transmissible through human milk, which could impact the infants’ ability to fight a possible HIV infection (Zeh et al. 2011). Thus, maternal ARVs are not only transferring to the infant through human milk but also, in our study, affect the transfer of zinc and copper during early lactation, and possibly other nutrients, into milk and subsequently to the infant.
The milk mineral concentrations from these HIV-infected mothers were comparable to other reported values from healthy women in the USA, Iran, and Brazil (Picciano & Guthrie 1976; Mahdavi et al. 2010; Mello-Neto et al. 2013). Thus, maternal HIV status might not or only marginally affect milk mineral concentrations. However, another study conducted in the USA revealed considerably higher mineral concentrations in milk from apparently healthy mothers (Feeley et al. 1983), while women in Vietnam produced milk with higher iron and copper but lower zinc concentrations at 6mo postpartum (Nakamori et al. 2009).
Comparison of milk iron, copper, and zinc concentrations with values used to set the Adequate Intake (AI) for infants 0–6mo
Despite the negative ARV effect on breast milk copper and zinc concentrations, 89–94% and 78–81% respectively of the milk samples obtained at 2wk met the concentrations used to set the AI for infants. When no ARVs were provided, 88% of the samples reached adequate zinc concentrations at 2wk versus 78–81% when ARV were taken, reiterating the already noted negative influence of ARV on zinc levels in breast milk at early stages of lactation. Only 38–48% of the iron concentrations at 2wk met AI values. However, the naturally occurring decrease in concentrations during lactation (Lönnerdal et al. 1981a; Silvestre et al. 2001; Brown et al. 2009) was lower for iron than for copper and zinc, suggesting mineral-specific kinetic rates of transport and secretion into milk. Iron, copper, and zinc concentrations in milk are at their peak during the first few days postpartum and decrease as lactation progresses. However, the concentrations of these trace minerals are remarkably stable at all lactation stages as they are tightly regulated and maintained by the mammary epithelial cells (Montalbetti et al. 2014).
Infants possess extensive iron stores in the liver that offset the low milk levels and ensure adequate supply. Due to the extreme changes in concentrations of minerals in milk within the first 6mo postpartum, a range of AI values would be more accurate for estimating adequate intake than the current single value approach; the natural decrease in concentration will result in theoretically insufficient concentrations of these minerals in breast milk, even though the infant may actually be adequately supplied. Moreover, the AI values for these trace minerals are based on limited data (9–15 studies with low numbers of participants) (Institute of Medicine 2001). Thus, the concentrations of iron, copper, and zinc measured in our study cannot be interpreted as insufficient based solely on the current AI-estimates. Longitudinal data from big data sets such as the BAN study provide important additional information for the assessment of milk mineral content.
Correlations of maternal and infant biomarkers and characteristics with human milk minerals
In the BAN study, changes in maternal TfR and Hb were associated with those observed in infant TfR and Hb (Widen et al. 2014). However, neither of these maternal or infant iron status biomarkers showed a significant correlation with milk iron, copper, or zinc, indicating that the breast milk minerals are not the determining factor for infant iron (TfR, ferritin, Hb) status during lactation. In fact, Mahdavi et al. (2010) showed that milk iron, copper, and zinc concentrations and the infant’s weight for age and height for age Z-score are not significantly associated, and Murray et al. (1978) reported no significant differences between milk iron and infant iron status measures, showing the independence of infant outcomes from human milk mineral concentrations.
Interestingly, we found that women with lower Hb during pregnancy (≤30wk gestation) produced milk with higher iron concentrations at both 2 and 6wk, while none of the postpartum maternal iron status biomarkers (Hb, ferritin, TfR) were associated with milk minerals at these time points, suggesting that maternal iron status during pregnancy may affect milk iron concentrations during early stages of lactation. Using BeWo cell layers as a model for placental iron transfer in rats fed decreasing iron levels Gambling et al. (2001) found increased mRNA and protein expression of TfR and of the divalent metal transporter-1 (DMT-1). Recently, Jobarteh et al. (2017) confirmed an up-regulation of mRNA of placental TfR1 in Gambian women with low iron status; this increase might represent a mechanism to ensure fetal requirements are met. Such alterations in iron metabolism could also occur in the mammary epithelial cells that regulate mineral secretion into milk, which also involves TfR- and DMT1-regulated processes (Montalbetti et al. 2014). Given that this relationship was observed in two independent groups and time of pregnancy during screening did not affect Hb status (data not shown), this consistent significant and negative association between pregnancy Hb and human milk iron deserves further investigation. Parity and maternal BMI were the only characteristics associated with breast milk minerals; while parity and iron concentrations were correlated at 2 wk, maternal BMI and zinc concentrations were correlated at 24wk. These findings indicate that higher parity could adversely affect iron, while higher BMI might positively influence breast milk zinc concentration during later stages of lactation.
The strongest correlations (all positive) were found among the human milk minerals. All of them were also associated with the milk fat, an observation previously described by Finley et al. (1985). Given that all three minerals are partly present in the lipid fraction of the milk (Fransson & Lönnerdal 1980, 1982, 1984; Lönnerdal et al. 1982; Donangelo et al. 1989; Hiari et al. 1990; Wooten et al. 1996; Linder et al. 1998), the correlation with milk fat is not unexpected. Copper and zinc are both bound to serum albumin, casein, and citrate in milk (Lönnerdal et al. 1982); their positive association suggests that the two minerals are not competing for the same binding site but rather for the availability of additional binding capacity (Finley et al. 1985; Lönnerdal et al. 1981b). Positive correlations between milk iron and copper have also been reported by Feely et al. (1983), concluding that milk from mothers with high amounts of iron may also be more likely to contain high concentrations of copper. Given the intertwined relationships of mineral metabolism (Institute of Medicine 2001), the close association of their concentrations in milk is not surprising.
Associations of human milk iron, copper and zinc with maternal and infant biomarkers, stratified by maternal Hb (anemia status) during pregnancy and postpartum
Limited research has focused on the relationship of maternal and infant iron status biomarkers with breast milk mineral content. Kumar et al. (2008) showed that severe maternal anemia adversely affected cord blood and human milk iron concentrations. In our study, moderately anemic women with higher ferritin also had a higher concentration of iron in their milk compared to non-anemic or only mildly anemic women at 2wk, while lower TfR was associated with higher milk iron content in moderately anemic compared to non-anemic women at 2 and 24wk. Although iron secretion is tightly regulated and maintained by the mammary epithelial cells, little is known about the molecular and cellular mechanisms regulating mineral concentrations in the milk (Montalbetti et al. 2014). Thus, while milk iron concentrations are assumed to be independent from maternal intake, our observations indicate the possibility of a less understood yet complex relationship on the molecular and cellular level between maternal iron status during pregnancy and the amounts of iron in milk during early lactation.
At 6wk, mildly anemic women with higher concentrations of the inflammation biomarkers AGP and CRP also had higher concentrations of iron, copper and zinc in their milk than women with normal Hb. Based on the categories of inflammation proposed by Thurnham et al. (2008), about 23% of the mildly anemic women at 6wk showed early stages of infection or convalescence. After adjusting for inflammation the described relationships persisted, suggesting that the association of maternal AGP/CRP and milk minerals in mildly anemic women is not directly caused by inflammation (Supplemental Table 5).
The degree of maternal anemia during pregnancy or lactation may also affect the relationship between breast milk minerals and infant biomarkers. We found that infants from mildly anemic mothers at 2wk, who secrete more copper into milk, have lower AGP concentrations, an effect also found for breast milk iron and copper at 6wk for women who were mildly anemic during pregnancy. Infant TfR also seemed to be affected by maternal Hb status and was lower when breast milk iron, copper and zinc were higher, but only when comparing moderately-anemic to non-anemic mothers. To our knowledge, no previous reports have investigated these associations.
These relationships between milk minerals and infant status may be linked to maternal anemia status. Alterations in maternal mineral metabolism related to maternal iron status have been recently described (Jobarteh et al. 2017); however, more research is necessary to understand any influence of this effect on infant status.
Human milk iron, copper and zinc concentrations and inflammation
Information is sparse regarding the impact of inflammation on breast milk minerals. However, effects of inflammation on maternal status may indirectly affect breast milk mineral concentrations. Inflammation has been associated with reduced iron incorporation into heme, and increased blood copper, and decreased zinc concentrations (Aggett & Harries 1979; Beshgetoor & Hambidge 1998; van den Broek & Letsky 2000). The leucocyte endogenous mediator (LEM) is thought to be involved by enhancing the hepatic uptake of zinc and iron, and by synthesis of acute phase proteins such as ceruloplasmin, a multi-copper ferrioxidase (Gambling et al. 2008). Recent findings describe an up-regulation of placental iron and zinc transporters in Gambian women with low iron and zinc status (Jobarteh et al. 2017), proteins also located in the mammary gland (McCormick et al. 2014; Montalbetti et al. 2014). These alterations in mineral metabolism could extend into milk secretion, e.g. due to a signaling cascade. Our findings of higher milk iron, copper, and zinc concentrations in women with inflammation indicate higher influx of these minerals into milk when inflammation occurs. Moreover, the inflammation-related higher milk iron concentrations at 2wk when the woman’s pregnancy Hb status was lower, and higher milk zinc concentrations at 6wk when their pregnancy Hb status was higher, support a potential up-regulated iron and zinc secretion into milk when women were subjected to health challenges such as low status and inflammation. Interestingly, no such relationships were found with Hb status during lactation, indicating that pregnancy Hb status might have a stronger impact than Hb status during lactation. However, Broek and Letsky (2000) also found an independent effect of HIV-infection on Hb concentrations that was not associated with concurrent infection or dietary deficiencies. Thus, the extent of the interrelationships of inflammation, pregnancy Hb and milk mineral concentrations has yet to be determined.
Limitations and Conclusions
Despite the extensive number of milk samples analyzed in the BAN study, the samples collected are opportunistic and may not reflect a 24h milk sample. Moreover, our initial samples were collected 2 and 6wk into the intervention, thus not reflecting a true baseline. The low dose of copper in the LNS (only 23% of the RDA) may also be insufficient to detect a difference in milk copper concentrations. Exploring the data for associations based on maternal Hb status resulted in a few sub-groups with small sample sizes (e.g., n=13 or 16, Figures 3 and 4; Supplemental Tables 3 and 4) which may not be generalizable to the larger population. However, unique characteristics of the study include longitudinal collection of breast milk in a relatively large sample of women, high adherence to recommendations to exclusively breastfeed, and the randomized control design, which enabled analysis of the effects of LNS and ARV, and their interactions, on milk micronutrients. ARV affected milk copper and zinc concentrations and was not offset by maternal supplementation during lactation. Even though this negative effect appears to be limited and only at early lactation, the extent of the impact on the infant has yet to be determined as well as possible remedies. Although we found significant correlations between maternal biomarkers and characteristics with milk minerals, those correlations were weak and further studies are required to gain better insight into the complex relationships between maternal and infant biomarkers and breast milk mineral concentrations.
Supplementary Material
KEY MESSAGE.
Maternal supplementation with lipid-based nutrient supplements during lactation had no effect on iron, copper, and zinc concentration in human milk.
Maternal antiretroviral therapy negatively affected copper and zinc concentration in human milk in early lactation.
Milk mineral concentrations quickly decreased during lactation with less than 50% of samples with adequate iron concentrations at 2wk.
The strongest correlations throughout lactation were found among the milk minerals, and milk fat.
Maternal Hb during pregnancy or lactation could influence the relationship between milk minerals and maternal and infant biomarkers for inflammation and iron stores.
Acknowledgments
We thank Janet M. Peerson for guidance on the statistical analysis. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. We thank all the members of the BAN Study Team at the University of North Carolina at Chapel Hill, the CDC, Atlanta, and the University of North Carolina Project in Lilongwe. We are grateful to all the women and infants who agreed to participate in the study. USDA is an equal opportunity employer and provider.
Source of funding:
The Breastfeeding, Antiretrovirals, and Nutrition Study was supported by grants from the Prevention Research Centers Special Interest Project of the Centers for Disease Control and Prevention (SIP 13-01 U48-CCU409660-09, SIP 26-04 U48-DP000059-01, and SIP 22-09 U48-DP001944-01), Bill & Melinda Gates Foundation (OPP53107 and OPP1061055), the National Institute of Allergy and Infectious Diseases, the University of North Carolina Center for AIDS Research (P30-AI50410), the Carolina Population Center (P2C HD050924), the NIH Fogarty AIDS International Training and Research Program (DHHS/NIH/FIC 2-D43 Tw01039-06 and R24 Tw00798; the American Recovery and Reinvestment Act), and intramural USDA-ARS Project (5306-51000-003-00D). The antiretrovirals used in the BAN study were donated by Abbott Laboratories, GlaxoSmithKline, Boehringer Ingelheim, Roche Pharmaceuticals, and Bristol-Myers Squibb. The Call to Action PMTCT program was supported by the Elizabeth Glaser Pediatric AIDS Foundation, the United Nations Children’s Fund, the World Food Program, the Malawi Ministry of Health and Population, Johnson & Johnson, and the U.S. Agency for International Development.
Footnotes
Conflict of interest:
D.H., S.S.-F., E.G., V.L.F., L.S.A., M.E.B., D.J.J., G.T., C.S.C., D.K., and L.H.A.: no conflicts of interest. C.M. van der Horst received grant support from Abbott Laboratories and GlaxoSmithKline.
Contributor statement:
The author’s responsibilities were as follows: DH conducted the laboratory, data, and statistical analyses, wrote the paper, and is responsible for the final content; SSF contributed to sample, data, and statistical analysis; VLF contributed to data analysis and statistics; LSA and MEB contributed to the trial design and obtained funding for the study; LHA is responsible for the laboratory analyses conducted at the WHNRC, and for the final version of the manuscript. . All authors reviewed manuscript revisions and contributed to the intellectual content of the manuscript.
References
- Adu-Afarwuah S, Lartey A, Okronipa H, Ashorn P, Zeilani M, Peerson JM, Arimond M, Vosti S, Dewey KG. Lipid-based nutrient supplement increases the birth size of infants of primiparous women in Ghana. American Journal of Clinical Nutrition. 2015;101:835–846. doi: 10.3945/ajcn.114.091546. [DOI] [PubMed] [Google Scholar]
- Aggett PJ, Harries JT. Current status of zinc in health and disease states. Archives of Disease in Childhood. 1979;54:909–917. doi: 10.1136/adc.54.12.909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen LH, Hampel D, Shahab-Ferdows S, York ER, Adair LS, Flax VL, Tegha G, Chasela CS, Kamwendo D, Jamieson DJ, Benltey ME. Antiretroviral therapy provided to HIV-infected Malawian women in a randomized trial diminishes the positive effects of lipid-based nutrient supplements on breast-milk B vitamins. American Journal of Clinical Nutrition. 2015;102:1468–1476. doi: 10.3945/ajcn.114.105106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beshgetoor D, Hambidge M. Clinical conditions altering copper metabolism in humans. American Journal of Clinical Nutrition. 1998;67(suppl):1017S–1021S. doi: 10.1093/ajcn/67.5.1017S. [DOI] [PubMed] [Google Scholar]
- Black RE, Allen LH, Bhutta ZA, Caufield LE, de Onis M, Ezzati M, Mathers C, Rivera J. Maternal and child unternutrition: global and regional exposures and health consequences. The Lancet. 2008;371:243–260. doi: 10.1016/S0140-6736(07)61690-0. [DOI] [PubMed] [Google Scholar]
- Brown KH, Engle-Stone R, Krebs NF, Peerson JM. Dietary intervention strategies to enhance zinc nutrition: Promotion and support of breastfeeding for infants and young children. Food and Nutrition Bulletin. 2009;30:S144–S171. doi: 10.1177/15648265090301S108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chasela CS, Hudgens MG, Jamieson DJ, Kayira D, Hosseinipour MC, Kourtis AP, Martinson F, Tegha G, Knight RJ, Ahmed YI. Maternal or infant antiretroviral drugs to reduce HIV-1 transmission. New England Journal of Medicine. 2010;362:2271–2281. doi: 10.1056/NEJMoa0911486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Childs K, Welz T, Samarawickrama A, Post FA. Effects of vitamin D deficiency and combination antiretroviral therapy on bone in HIV-positive patients. AIDS. 2012;26:253–262. doi: 10.1097/QAD.0b013e32834f324b. [DOI] [PubMed] [Google Scholar]
- Corbett AH, Kayira D, White NR, Davis NL, Kourtis AP, Chasela C, Martinson F, Phiri G, Musisi B, Kamwendo D. Antiretroviral pharmacokinetics in mothers and breastfeeding infants from 6 to 24 weeks post partum: results of the BAN Study. Antiviral Therapy. 2014;19:587–595. doi: 10.3851/IMP2739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dauncy MJ, Shaw JCL, Urman J. The absorption and retention of magnesium, zinc, and copper by low birth weight infants fed pasteurized human breast milk. Pediatric Research. 1977;11:991–997. doi: 10.1203/00006450-197710000-00001. [DOI] [PubMed] [Google Scholar]
- de Pee S, Semba RD. Role of nutrition in HIV infection: Review of evidence for more effective programming in resource-limited settings. Food and Nutrition Bulletin. 2010;31:313S–344S. [PubMed] [Google Scholar]
- Domellöf M, Lönnerdal B, Dewey KG, Cohen RJ, Hernell O. Iron, zinc, and copper concentrations in breast milk are independent of maternal mineral status. American Journal of Clinical Nutrition. 2004;79:111–115. doi: 10.1093/ajcn/79.1.111. [DOI] [PubMed] [Google Scholar]
- Donangelo C, Trugo N, Koury J, Barreto SMI, Freitas L, Feldheim W, Barth C. Iron, zinc, folate and vitamin B12 nutritional status and milk composition of low-income Brazilian mothers. European Journal of Clinical Nutrtition. 1989;43:253–266. [PubMed] [Google Scholar]
- Dorea JG. Iron and copper in human milk. Nutrition. 2000;16:209–220. doi: 10.1016/s0899-9007(99)00287-7. [DOI] [PubMed] [Google Scholar]
- Duggan C, Srinivasan K, Thomas T, Samuel T, Rajendran R, Muthayya S, Finkelstein JL, Lukose A, Fawzi W, Allen LH. Vitamin B-12 supplementation during pregnancy and early lactation increases maternal, breast milk, and infant measures of vitamin B-12 status. Journal of Nutrition. 2014;144:758–64. doi: 10.3945/jn.113.187278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feeley RM, Eitenmiller R, Jones J, Barnhart H. Copper, iron, and zinc contents of human milk at early stages of lactation. American Journal of Clinical Nutrition. 1983;37:443–448. doi: 10.1093/ajcn/37.3.443. [DOI] [PubMed] [Google Scholar]
- Ferguson YO, Eng E, Bentley M, Sandelowski M, Steckler A, Randall-David E, Piwoz EG, Zulu C, Chasela C, Soko A. Evaluating nurses’ implementation of an infant-feeding counseling protocol for HIV-infected mothers: The BAN study in Lilongwe, Malawi. AIDS Education and Prevention. 2009;21:141–155. doi: 10.1521/aeap.2009.21.2.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finley DA, Lönnerdal B, Dewey KG, Grivetti LE. Inorganic constituents of breast milk from vegetarian and nonvegetarian women: Relationships with each other and with organic constituents. Journal of Nutrition. 1985;115:772–781. doi: 10.1093/jn/115.6.772. [DOI] [PubMed] [Google Scholar]
- Flax VL, Adair LS, Allen LH, Shahab-Ferdows S, Hampel D, Chasela CS, Tegha G, Daza EJ, Corbett A, Davis NL. Plasma micronutrient concentrations are altered by antiretroviral therapy and lipid-based nutrient supplements in lactating HIV-infected Malawian women. Journal of Nutrition. 2015;145:1950–1957. doi: 10.3945/jn.115.212290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fransson GB, Lönnerdal B. Iron in human milk. Journal of Paediatrics. 1980;96:380–384. doi: 10.1016/s0022-3476(80)80676-7. [DOI] [PubMed] [Google Scholar]
- Fransson GB, Lönnerdal B. Zinc, copper, calcium, and magnesium in human milk. Journal of Paediatrics. 1982;101:504–508. doi: 10.1016/s0022-3476(82)80690-2. [DOI] [PubMed] [Google Scholar]
- Fransson GB, Lönnerdal B. Iron, copper, zinc, calcium, and magnesium in human milk fat. American Journal of Clinical Nutrition. 1984;39:185–189. doi: 10.1093/ajcn/39.2.185. [DOI] [PubMed] [Google Scholar]
- Gambling L, Danzeisen R, Gair S, Lea RG, Charania Z, Solanky N, Joory KD, Srai SKS, McArdle HJ. Effect of iron deficiency on placental transfer of iron and expression of iron transport proteins in vivo and in vitro. Biochemical Journal. 2001;356:883–889. doi: 10.1042/0264-6021:3560883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gambling L, Andersen HS, McArdle HJ. Iron and copper, and their interactions during development. Biochemical Society Transactions. 2008;36:1258–1261. doi: 10.1042/BST0361258. [DOI] [PubMed] [Google Scholar]
- Gibson RS, Huddle JM. Suboptimal zinc status in pregnant Malawian women: its association with low intakes of poorly available zinc, frequent reproductive cycling, and malaria. American Journal of Clinical Nutrition. 1998;67:702–709. doi: 10.1093/ajcn/67.4.702. [DOI] [PubMed] [Google Scholar]
- Hirai Y, Kawakata N, Satoh K, Ikeda Y, Hisayasu S, Orimo H, Yoshino Y. Concentrations of lactoferrin and iron in human milk at different stages of lactation. Journal of Nutritional Science Vitaminology. 1990;36:531–544. doi: 10.3177/jnsv.36.531. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc. National Academies Press; Washington DC: 2001. Free on-line book. [PubMed] [Google Scholar]
- Jobarteh ML, McArdle HJ, Holtrop G, Sise EA, Prentice AM, Moore SE. mRNA levels of placental iron and zinc transporter genes are upregulated in Gambian women with low iron and zinc status. Journal of Nutrition. 2017 doi: 10.3945/jn.116.244780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kayira D, Bentley ME, Wiener J, Mkhomawanthu C, King CC, Chitsulo P, Chigwenembe M, Ellington S, Hosseinipour MC, Kourtis AP. A lipid-based nutrient supplement mitigates weight loss among HIV-infected women in a factorial randomized trial to prevent mother-to-child transmission during exclusive breastfeeding. American Journal of Clinical Nutrition. 2012;95:759–765. doi: 10.3945/ajcn.111.018812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krebs NF, Hambidge K, Jacobs M, Rasbach JO. The effects of a dietary zinc supplement during lactation on longitudinal changes in maternal zinc status and milk zinc concentrations. American Journal of Clinical Nutrition. 1985;41:560–570. doi: 10.1093/ajcn/41.3.560. [DOI] [PubMed] [Google Scholar]
- Kumar A, Rai AK, Basu S, Dash D, Singh JS. Cord blood and breast milk iron status in maternal anemia. Pediatrics. 2008;121:e673–e677. doi: 10.1542/peds.2007-1986. [DOI] [PubMed] [Google Scholar]
- Linder MC, Wooten L, Cerveza P, Cotton S, Shulze R, Lomeli N. Copper transport. American Journal of Clinical Nutrition. 1998;67:965S–971S. doi: 10.1093/ajcn/67.5.965S. [DOI] [PubMed] [Google Scholar]
- Lönnerdal B, Keen CL, Hurley LS. Iron, copper, zinc, and manganese in milk. Annual Review of Nutrition. 1981a;1:149–174. doi: 10.1146/annurev.nu.01.070181.001053. [DOI] [PubMed] [Google Scholar]
- Lönnerdal B, Keen C, Hurley L. Trace elements in milk from various species. In: Howel McC TT, Gawthorne JM, White CL, editors. Trace Element Metabolism in Man and Animals (TEMA-4) Australian Academy of Science; Canberra: 1981b. pp. 249–252. [Google Scholar]
- Lönnerdal B, Hoffman B, Hurley L. Zinc and copper binding proteins in human milk. American Journal of Clinical Nutrition. 1982;36:1170–1176. doi: 10.1093/ajcn/36.6.1170. [DOI] [PubMed] [Google Scholar]
- Mahdavi R, Nikniaz L, Gayemmagami SJ. Association between zinc, copper, and iron concentrations in breast milk and growth of healthy infants in tabriz, Iran. Biological Trace Element Research. 2010;135:174–181. doi: 10.1007/s12011-009-8510-y. [DOI] [PubMed] [Google Scholar]
- McCormick NH, Hennigar SR, Kiselyov K, Kelleher SL. The biology of zinc transport in mammary epithelial cells: implications for mammary gland development, lactation, and involution. Journal of Mammary Gland Biology and Neoplasia. 2014;19:59–71. doi: 10.1007/s10911-013-9314-4. [DOI] [PubMed] [Google Scholar]
- Mello-Neto J, Rondó PHC, Oshiiwa M, Morgano MA, Zacari CZ, dos Santos ML. Iron supplementation in pregnancy and breastfeeding and iron, copper and zinc status of lactating women from a human milk bank. Journal of Tropical Pediatrics. 2013;59:140–144. doi: 10.1093/tropej/fms055. [DOI] [PubMed] [Google Scholar]
- Montalbetti N, Dalghi MG, Albrecht C, Hediger MA. Nutrient transport in the mammary gland: calcium, trace minerals and water soluble vitamins. Journal of Mammary Gland Biology and Neoplasia. 2014;19:73–90. doi: 10.1007/s10911-014-9317-9. [DOI] [PubMed] [Google Scholar]
- Moser PB, Reynolds RD, Acharya S, Howard MP, Andon M, Lewis S. Copper, iron, zinc, and selenium dietary intake and status of Nepalese lactating women and their breast-fed infants. American Journal of Clinical Nutrition. 1988;47:729–734. doi: 10.1093/ajcn/47.4.729. [DOI] [PubMed] [Google Scholar]
- Murray M, Murray AB, Murray N, Murray MB. The effect of iron status of Nigerien mothers on that of their infants at birth and 6 months, and on the concentration of Fe in breast milk. British Journal of Nutrition. 1978;39:627–630. doi: 10.1079/bjn19780077. [DOI] [PubMed] [Google Scholar]
- Nakamori M, Ninh NX, Isomura H, Yodshiike N, Hien VTT, Nhug BT, Nhien NV, Nakano T, Khan NC, Yamamoto S. Nutritional status of lactating mothers and their breast milk concentration of iron, zinc and copper in rural Vietnam. Journal of Nutritional Science and Vitaminology. 2009;55:338–345. doi: 10.3177/jnsv.55.338. [DOI] [PubMed] [Google Scholar]
- National Statistical Office (NSO) [Malawi] and ICF. Malawi demographic and health survey 2015–16. Zomba; Malawi, and Rockville, MD, USA: 2017. [Google Scholar]
- Prado EL, Phuka J, Maleta K, Ashorn P, Ashorn U, Vosti SA, Dewey KG. Provision of lipid-based nutrient supplements from age 6 to 18 months does not affect infant development scores in a randomized trial in Malawi. Maternal and Child Health Journal. 2016 doi: 10.1007/s10995-016-2061-6. [DOI] [PubMed] [Google Scholar]
- Paltiel O, Falutz J, Veilleux M, Rosenblatt DS, Gordon K. Clinical correlates of subnormal vitamin B12 levels in patients infected with the human immunodeficiency virus. American Journal of Hematology. 1995;49:318–322. doi: 10.1002/ajh.2830490410. [DOI] [PubMed] [Google Scholar]
- Picciano MF, Guthrie HA. Copper, iron, and zinc contents of mature human milk. American Journal of Clinical Nutrition. 1976;29:242–254. doi: 10.1093/ajcn/29.3.242. [DOI] [PubMed] [Google Scholar]
- Picciano MF. Nutrient composition of human milk. Pediatric Clinics of North America. 2001;48:53–67. doi: 10.1016/s0031-3955(05)70285-6. [DOI] [PubMed] [Google Scholar]
- Shahab-Ferdows S, Engle-Stone R, Hampel D, Ndjebayi AO, Nankap M, Brown KH, Allen LH. Regional, socioeconomic, and dietary risk factors for vitamin B-12 deficiency differ from those for folate deficiency in Cameroonian women and children. Journal of Nutrition. 2015;145:2587–2595. doi: 10.3945/jn.115.210195. [DOI] [PubMed] [Google Scholar]
- Shapiro RL, Holland DT, Capparelli E, Lockman S, Thior I, Wester C, Stevens L, Peter T, Essex M, Connor JD. Antiretroviral concentrations in breast-feeding infants of women in Botswana receiving antiretroviral treatment. Journal of Infectious Diseases. 2005;192:720–727. doi: 10.1086/432483. [DOI] [PubMed] [Google Scholar]
- Siddiqua TJ, Ahmad SM, Ahsan KB, Rashid M, Roy A, Rahman SM, Shahab-Ferdows S, Hampel D, Ahmed T, Allen LH. Vitamin B12 supplementation during pregnancy and postpartum improves B12 status of both mothers and infants but vaccine response in mothers only: a randomized clinical trial in Bangladesh. European Journal of Nutrition. 2016;55:281–293. doi: 10.1007/s00394-015-0845-x. [DOI] [PubMed] [Google Scholar]
- Silvestre D, Martìnez-Costa C, Lagarda MJ, Brines J, Farré R, Clemente G. Copper, iron, and zinc contents in human milk during the first three months of lactation. Biological Trace Element Research. 2001;80:1–11. doi: 10.1385/BTER:80:1:01. [DOI] [PubMed] [Google Scholar]
- Thakwalakwa C, Ashorn P, Phuka J, Cheung YB, Briend A, Puumalainen T, Maleta K. A lipid-based nutrient supplement but not corn-soy blend modestly increases weight gain among 6-to 18-month-old moderately underweight children in rural Malawi. Journal of Nutrition. 2010;140:2008–2013. doi: 10.3945/jn.110.122499. [DOI] [PubMed] [Google Scholar]
- Thurnham DI, Mburu AS, Mwaniki DL, Muniu EM, Alumasa F, de Wagt A. Using plasma acute-phase protein concentrations to interpret nutritional biomarkers in apparently healthy HIV-1-seropositive Kenyan adults. British Journal of Nutrition. 2008;100:174–182. doi: 10.1017/S0007114507883012. [DOI] [PubMed] [Google Scholar]
- Van den Broek NR, Letsky EA. Etiology of anemia in pregnancy in south Malawi. American Journal of Clinical Nutrition. 2000;72(suppl):247S–256S. doi: 10.1093/ajcn/72.1.247S. [DOI] [PubMed] [Google Scholar]
- van der Horst C, Chasela C, Ahmed Y, Hoffman I, Hosseinipour M, Knight R, Fiscus S, Hudgens M, Kazembe P, Bentley M. Modifications of a large HIV prevention clinical trial to fit changing realities: a case study of the Breastfeeding, Antiretroviral, and Nutrition (BAN) protocol in Lilongwe, Malawi. Contemporary Clinical Trials. 2009;30:24–33. doi: 10.1016/j.cct.2008.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vuori E, Mäkinen S, Kara R, Kuitunen P. The effects of the dietary intakes of copper, iron, manganese, and zinc on the trace element content of human milk. American Journal of Clinical Nutrition. 1980;33:227–231. doi: 10.1093/ajcn/33.2.227. [DOI] [PubMed] [Google Scholar]
- Widen EM, Bentley ME, Kayira D, Chasela CS, Daza EJ, Kacheche ZK, Tegha G, Jamieson DJ, Kourtis AP, van der Horst CM. Changes in soluble transferrin receptor and hemoglobin concentrations in Malawian mothers are associated with those values in their exclusively breastfed, HIV-exposed infants. Journal of Nutrition. 2014;144:367–373. doi: 10.3945/jn.113.177915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitfield KC, Karakochuk CD>, Kroeun H, Hampel D, Sokhoing L, Chan BB, Borath M, Sophonneary P, McLean J, Talukder A, Lynd LD, Li-Chian ECY, Kitts DD, Allen LH, Green TJ. Perinatal consumption of thiamine-fortified fish sauce in rural Cambodia. JAMA Pediatrics. 2016;170:e162065. doi: 10.1001/jamapediatrics.2016.2065. [DOI] [PubMed] [Google Scholar]
- Woods MN, Tang AM, Forrester J, Jones C, Hendricks K, Ding B, Knox TA. Effect of dietary intake and protease inhibitors on serum vitamin B12 levels in a cohort of human immunodeficiency virus—positive patients. Clinical Infectious Diseases. 2003;37:S124–S131. doi: 10.1086/375893. [DOI] [PubMed] [Google Scholar]
- Wooten L, Shulze RA, Lancey RW, Lietzow M, Linder MC. Ceruloplasmin is found in milk and amniotic fluid and may have a nutritional role. Journal of Nutritional Biochemistry. 7:632–639. [Google Scholar]
- World Health Organization. HIV and infant feeding: guidelines for decision-makers. World Health Organization; Geneva: 2003. [Google Scholar]
- World Health Organization. Guidelines on HIV and Infant Feeding 2010: Principles and Recommendations for Infant Feeding in the Context of HIV and a Summary of Evidence. WHO; Geneva: 2010. [PubMed] [Google Scholar]
- World Health Organization. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. World Health Organization; Geneva: 2011. [Google Scholar]
- World Health Organization. Guidline updates on HIV and infant feeding: the duration of breastfeeding and support from health services to improve feeding practices among mothers living with HIV. WHO; Geneva: 2016. [PubMed] [Google Scholar]
- Zeh C, Weidle PJ, Nafisa L, Lwamba HM, Okonji J, Anyango E, Bondo P, Masaba R, Fowler MG, Nkengasong JN. HIV-1 drug resistance emergence among breastfeeding infants born to HIV-infected mothers during a single-arm trial of triple-antiretroviral prophylaxis for prevention of mother-to-child transmission: a secondary analysis. PLoS Medicine. 2011;8:e1000430. doi: 10.1371/journal.pmed.1000430. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.