Abstract
Posttraumatic stress disorder (PTSD) affects up to 30% of military veterans. Older veterans, many of whom have lived with PTSD symptoms for several decades, report a number of negative health outcomes. Despite the demonstrated benefits of regular exercise on physical and psychological health, no studies have explored the impact of exercise in older veterans with PTSD. This paper describes the development, design, and implementation of the Warrior Wellness exercise pilot study for older veterans with PTSD. Veterans aged ≥60 with a Diagnostic and Statistical Manual of Mental Disorders (DSM-V) diagnosis of PTSD will be recruited and randomized to (a) Warrior Wellness, a 12-week supervised, facility-based exercise intervention, or (b) usual care for 12 weeks. Warrior Wellness is a theory- and evidence-based behavioral intervention that involves 3 sessions per week of multi-component exercise training that targets strength, endurance, balance, and flexibility. Warrior Wellness focuses on satisfaction with outcomes, self-efficacy, self-monitoring, and autonomy. Factors associated with program adherence, defined as the number of sessions attended during the 12 weeks, will be explored. Primary outcomes include PTSD symptoms and cardiovascular endurance, assessed at baseline and 12 weeks. Compared to those in usual care, it is hypothesized that those in the Warrior Wellness condition will improve on these efficacy outcomes. The Warrior Wellness study will provide evidence on whether a short-term exercise intervention is feasible, acceptable, and effective among older veterans with PTSD, and explore factors associated with program adherence.
ClinicalTrials.gov Identifier: NCT02295995
Keywords: physical activity, posttraumatic stress disorder, lifestyle, clinical trial, mental health
1. Introduction
PTSD is estimated to afflict up to 30% of the older veteran cohort (1). The prevalence of persistent PTSD among older veterans is troubling in light of the negative, long-term, and often cascading, consequences of this condition. PTSD has been linked to a number of negative cardiometabolic health outcomes and psychological disorders (2–6). Behavioral factors, such as low physical activity and poor diet may exacerbate these associations (7–9). There is substantial evidence demonstrating that exercise is an effective intervention for improving both physical and psychological outcomes (10–12), making it an exciting and novel treatment option for individuals with PTSD (13–15). Exercise programs may also be more acceptable than traditional psychological treatments and drug therapies, particularly among older veterans, who are less likely to initiate mental health treatment (16) but have a history of being physically active during military service. While there is growing recognition of the potential role of exercise as a mediating factor between PTSD and health outcomes (9, 17, 18), the impact of regular exercise on both the physical health and psychological well-being of veterans with PTSD remains to be determined.
Previous research suggests that individuals with PTSD are less likely to engage in regular physical activity and spend more time in sedentary activities compared to individuals without PTSD (7, 19). Recent exercise intervention studies among individuals with PTSD provide some evidence of the acceptability and efficacy of these programs (14, 20–22). In two separate studies of in-patients receiving care for PTSD, Rosenbaum and Babson showed significant reductions in PTSD and depression symptoms and improvements in cardiometabolic risk factors. However, these studies have a number of limitations including a highly specific sample and recruitment setting (in-patient, residential PTSD treatment programs), lack of a control group and/or theoretical framework, and low rates of intervention adherence. Individuals with PTSD have demonstrated poor adherence to other lifestyle interventions (23), suggestive of tailored approaches to implementing an exercise program in persons with PTSD are likely needed and may improve program adherence.
We developed the Warrior Wellness pilot study to examine the feasibility, acceptability, efficacy, and effectiveness of a 12-week exercise program culturally tailored for older military veterans with PTSD. The impact of this exercise intervention on PTSD symptoms and cardiovascular endurance compared to usual care will be explored as will other secondary outcomes of interest. The Warrior Wellness study is ongoing, and the rationale, design, and protocol of this randomized controlled trial are discussed below.
2. Methods
2.1. Phase 1: Expert and Consumer Advisory Boards
We adopted an iterative approach to study development that included quality improvement work to inform study design and implementation. Two groups were convened: an expert advisory board and a consumer advisory board.
Expert Advisory Board: Design and Methods
We convened a multidisciplinary group of researchers and clinicians (N=9) including exercise physiologists, clinical psychologists, behavioral scientists, geriatricians, and biostatisticians. The collective expertise of the panel informed the study design and implementation considerations, recruitment procedures, outcome measures, and methods for evaluating the efficacy and acceptability of the intervention. These discussions resulted in: a) a theory-based randomized controlled exercise trial consisting of usual care vs. supervised exercise, b) repeated measures of physical and psychological well-being, c) objective measures of physical activity and sleep, d) an emphasis on feasibility and acceptability with a secondary emphasis on efficacy and effectiveness, e) identification of screening tools and recruitment sources, and f) specification of theory-based behavioral strategies to promote initiation and adherence.
Consumer Advisory Board: Design and Recruitment Strategies
Veteran consumers (N=5) matched to our target participant characteristics were contacted to provide their feedback on program design elements (e.g., marketing, recruitment strategies), implementation plans and incentives, study measures, and to advise the research team on issues of importance to veterans with PTSD and potential special considerations for the team to consider. Inclusion criteria included: a) military veteran, b) age ≥55 years, c) and a diagnosis of PTSD in the medical chart. A diverse representation by race and gender was sought. Participants were recruited using established relationships in the area developed by the principal investigator, including outreach at the study site and through word of mouth and direct communication with veterans who had participated in other behavioral research studies in the Durham Veterans Affairs Health Care System (VAHCS). Discussions were facilitated by the principal investigator and the study coordinator, both of whom have previous research experience with older adults. Participants were financially compensated for their participation. Five older veterans with PTSD (M age = 64.2 years; 60% male; 80% African American) participated in the consumer advisory panels. The veteran consumer advisory board emphasized four themes.
Culture and Study Branding
Individuals emphasized promoting a wellness model (as opposed to a disease model) that empowers veterans to make behavioral changes. They also noted that study branding through the use of “swag” and group “membership” (which adds an element of exclusivity) would likely impact individuals’ willingness to volunteer and enhance adherence over the course of the program. Finally, several participants noted that the fact that this study didn’t include psychotherapy should be made clear and emphasized up front in recruitment materials (“Many of us who have PTSD just don’t want to talk about it. I like this program because it’s not focusing on PTSD, but it can help with everything else.”).
Individual Tailoring
Some participants voiced interest in integrating wearable and mobile technologies to monitor exercise participation and promote adherence. There were several comments about the importance of individual tailoring of the exercise prescriptions, given the high rates of chronic disease, physical impairment, and low levels of physical activity in this population.
Barriers to Physical Activity
Several general barriers were mentioned-, and included psychological and behavioral characteristics of this population (“There are lots of barriers; depression, sleep deprivation, motivation…need to let them know that it’s ok to miss a day. The important thing is that the next day you get back on the horse.”). One woman noted the tendency for veterans with PTSD to isolate themselves and avoid many social situations as a barrier, “We’re talking about people who are isolated, who think nobody cares about them. This program is helping people get in shape—physically, emotionally, socially, and mentally. And they can encourage each other.” Participants also stressed that body image and dissatisfaction are also prevalent in older veterans and may be a barrier to participation. Cognitive-behavioral strategies for promoting adherence including goal setting, troubleshooting barriers, personalized feedback, and behavioral contracts were also discussed.
Education
All members of the consumer advisory board noted it was crucial to include some education for patients (and research staff) around physiologic activation and hyperarousal dimensions of PTSD symptoms and how these might be impacted by exercise and a public gym environment (“A noisy gym can be scary. They need to know that other Vets with PTSD are also exercising and doing just fine (in that environment). But be upfront about the challenges with PTSD symptoms). Participants also mentioned the need to consider PTSD symptom flare-ups outside of the gym environment. They suggested discussing triggers and management strategies with participants prior to initiation of the exercise program as a strategy to maximize adherence.
The input gathered from both the expert and consumer advisory boards helped us to understand issues of feasibility, retention, characteristics of the exercise prescription that may impact compliance, and efficacy of the Warrior Wellness Study. Members of both panels reported excitement for programming that addresses core health behaviors like physical activity in this population. The feedback provided by these panels also proved essential to developing a culturally tailored behavioral intervention for this unique population, which has not previously been targeted for physical activity promotion programs. We continue to engage these groups as needed for further input as the study continues.
2.2. Study Design
This study is a two-arm randomized controlled trial (RCT; Figure 1) design with participants randomized to the Warrior Wellness exercise condition or to a usual care control group (2:1 randomization scheme). We will examine the feasibility and efficacy of Warrior Wellness, a 12-week supervised, facility-based exercise program. Patients randomized into the usual care control group will have a 12 week waiting period prior to the start of the exercise intervention. All participants continue with other medical and PTSD-related care, including medications and physician visits, with the exception of trauma-focused therapies. Participants in both groups are asked to refrain from initiating trauma-focused therapies (e.g., Prolonged Exposure Therapy, Cognitive Processing Therapy) for the duration of the study. Participants are enrolled from the Durham VA Medical Center and community-based veterans service centers (e.g., Vet Centers, VA outpatient clinics). We propose to enroll approximately 45 participants (30 in intervention and 15 in the comparison). The study protocol was approved by the Durham VAHCS Institutional Review Board (IRB) and Research and Development committees.
Figure 1.
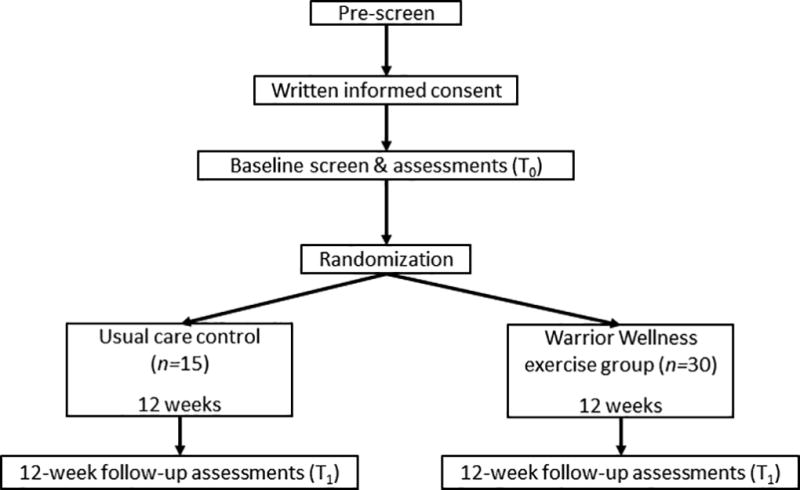
Study design
2.3. Screening and Recruitment
Eligible participants are military veterans aged 60 years or more, with a current diagnosis of PTSD as indicated by the Clinician Administered PTSD Scale (CAPS; 24). Potential participants are recruited via self-, patient-, and provider referrals in response to advertisements placed throughout the Durham VA Medical Center and associated outpatient clinics (e.g., PTSD clinic, Vet Centers). Research staff conduct further eligibility screening by telephone, and individuals meeting these criteria are scheduled for an in-person baseline appointment (see Table 1 for eligibility criteria). A data pull from the electronic medical record was also conducted to obtain a pool of potentially eligible veterans, and identified over 11,000 veterans meeting the initial age, geographic, and PTSD eligibility criteria. The electronic medical records of individuals identified through the data pull are reviewed to ensure that patients meet age, location, and select clinical eligibility criteria. Qualifying individuals from the data pull are sent an introductory letter in the mail describing the study and inviting them to contact the study office for information and further eligibility screening by telephone. We employ an opt-out recruitment strategy, contacting each individual who is sent a letter unless they contact us directly to indicate that they are not interested in the program. At the baseline appointment, written informed consent and HIPAA authorization are obtained, and then patients complete a psychological status screening that includes the CAPS and the Short Portable Mental Status Questionnaire (SPMSQ; 25) to determine final eligibility. If deemed eligible for the study, the research staff continues with a battery of health questionnaires and physical performance tests, detailed below. Participants also receive an ActiGraph activity monitor, which they are instructed to wear for 7 consecutive days (24 hours/day) and mail back to the lab.
Table 1.
Inclusion and exclusion criteria
| Inclusion criteria | Assessment method |
|
| |
| Live within 50 miles of Durham VAMC | 1,2 |
| Access to reliable transportation | 1,2 |
| Has a Durham VAMC provider | 1 |
| Independently mobile (assistive devices acceptable) | 1,2,3 |
| Meet DSM-V criteria for PTSD | 3 |
| Exercising less than 30 minutes/day on less than 5 days/week | 2,3 |
| Agrees to attend regular exercise sessions per study protocol | 2,3 |
| Willing to be randomized | 2,3 |
|
| |
| Exclusion criteria | Assessment method |
|
| |
| Age <60 years old | 1,2 |
| Dementia, psychiatric illness, or substance abuse that may interfere with adherence (e.g., illness that is currently unstable or resistant to first-line therapy; substance abuse in the past 6 months) | 1,2,3 |
| Clinical history of CVD occurring with the past 3 months (angina, ventricular tachycardia, COPD with 2 or more hospitalizations and/or on oxygen, stroke with moderate to severe aphasia) | 1,2 |
| Cognitive dysfunction (≥3 errors on the SPMSQ) | 3 |
| Uncontrolled hypertension (systolic BP >200 mmHg or diastolic BP > 110 mmHg on medications at rest) | 1,2,3 |
| Renal disease or currently receiving dialysis | 1,2 |
| Non-recommended for supervised exercise by healthcare provider | 1,2 |
| Proliferative retinopathy | 1 |
| Currently receiving trauma-focused therapy, those individuals excluded for current enrollment in trauma-focused therapy may be rescreened for eligibility | 1,2,3 |
Note: 1 = electronic medical record; 2 = telephone screen; 3 = in-person screening
2.4. Randomization
At the end of the baseline study visit, participants are randomly assigned to the Warrior Wellness program or the usual care control arm by drawing from a pool containing “PA” (physical activity) or “UC” (usual care) cards. The enrollment ratio is 2: 1 to the exercise intervention of usual care arm, respectively. Neither the participants nor the research staff are masked to treatment assignment.
2.5. Arm 1: Warrior Wellness supervised exercise arm
The Warrior Wellness exercise intervention is delivered over 12 weeks and includes an individualized exercise prescription based on the individual’s exercise history, current exercise capacity, personal preferences, and current health status. This is a multicomponent intervention that includes strength, balance, and flexibility training and aerobic exercise. The program aims to have participants engaging in moderate to vigorous exercise for at least 150 minutes/week, in line with current recommendations and American College of Sports Medicine (ACSM) guidelines (26). Supervised exercise sessions are held three days per week (Monday, Wednesday, Friday). The duration of each exercise session lasts 60 to 90 minutes, depending on the individual prescription and pace.
2.5.1. Exercise Prescription
The individual exercise prescriptions and progression plan are consistent with American College of Sports Medicine (ACSM) guidelines for older adults (26). Participants are provided a weekly exercise prescription card detailing exercise mode, duration, frequency, and intensity. During the first two weeks of the program an exercise physiologist works one-on-one with each participant to instruct proper use of the equipment, technique, and safety considerations. Once proper technique has been established, participants are encouraged to proceed through their exercise prescription independently, with minimal guidance from the exercise physiologist. Personalized programs are multicomponent, and include a selection of 8 to 12 strengthening, balance, and flexibility exercises targeting the major muscle groups (e.g., shoulders, arms, back, abdomen, legs) as well as primary joints (e.g., knees, hips, and shoulders). Exercises will be introduced in a staged manner to maximize adherence and proper technique acquisition. Participants are encouraged to complete 1–2 sets of 8–15 repetitions for each exercise, with a 30-second rest period in between sets. Table 2 details the overall exercise battery and progression of intensity for each exercise. Modalities include body weight, free weights, cables and exercise bands. Additionally, participants are instructed in endurance exercise, with preferred modes being walking (treadmill) and stationary cycle. Balance training and flexibility are also core components of the program, and are incorporated into both the strengthening exercises (i.e., toe raises, shoulder rotation) and through targeted exercises (e.g., heel-toe walk, standing hamstring stretch). This exercise program emphasizes ‘functional training,’ and uses movements and exercise modalities that mimic everyday activities. Our use of free weights and bands instead of weight machines is one example of this principle. Individual limitations such as musculoskeletal conditions and postural control are considered when prescribing individual exercises and modalities, and physical-activity related adverse events/injuries will be recorded over the course of the program.
Table 2.
Exercise Battery and Progression of Intensity for Each Exercise in the Warrior Wellness Program
| Exercise | Level 1 | Level 2 | Level 3 | Level 4 | Level 5 |
|---|---|---|---|---|---|
| STRENGTHENING EXERCISES | |||||
| Squat | Sit-to-stand in chair | Squat w/ rail | Squat w/o rail | Squat w/ weights | Increase volume/load |
| Bent-over or seated row | Seated w/ Thera-tube | Bench w/ weight OR Seated row w/ cable | Increase volume/load | ||
| Chest press | Thera-tube pull | Bench w/ weights | Increase volume/load | ||
| Step- ups | 12” step box w/ rail | 12” step box no rail | 12” step box w/ weights | 12” step box w/ balance, floating leg | Increase volume/load |
| Lat/overhead pull-down | Thera-tube pull | Seated w/ cable | Increase volume/load | ||
| Triceps extension | Bench w/ weight OR Standing cable w/ weight | Increase volume/load | |||
| Hip abduction | Seated, no resistance | Seated w/ thera-tube | Standing w/rail | Standing w/o rail | Standing w/ thera-tube |
| Shoulder rotation (internal & external) | Thera-tube ‘light’ single/double | Thera-tube ‘medium’ single/double | Thera-tube ‘heavy’ single/double | Thera-tube ‘very heavy’ single/double | |
| Push-up | Wall push-ups | Wall push-ups w/ thera-tube | Modified push-ups on knees | Regular push-up | Increase volume/duration |
| Calf raises | Double w/rail | Double w/o rail | Double w/weight | Increase volume/load | |
| Core | Standing core engagement | Plank on knees/forearms | Increase volume/duration | Plank on toes/forearms | Increase volume/duration |
| Core | Bird-dog: arms only | Bird-dog: opposite arm + leg lift | Bird-dog: opposite arm + leg w/ crunch | Increase volume/duration | |
| BALANCE EXERCISES | |||||
| Heel-toe walk | Single-leg stand | Clock | Tree | Increase volume/duration | |
| FLEXIBILITY EXERCISES | |||||
| S1-Standing hamstring& calf stretch | S1+ overhead side bend stretch (S2) | S1+S2+ cat/cow stretch (S3) | S1+S2+S3+ child’s pose | S1+S2+S3+ bridge pose | |
ACSM guidelines for older adults recommend that activity intensity be defined within the context of perceived physical exertion (RPE), measured using the Borg RPE (0–10) scale. RPE scale is a valid measure of exercise intensity in older adults, and is particularly valuable when heart rate measures of exercise intensity are inaccurate or dampened, such as in patients on beta blocker medication (which we expect to be a high percentage of our participants). During early stages, the level of intensity targets an RPE of 2 or 3 (“light” and “moderate”), as we expect much of this group to be sedentary. During the latter stages, the level of intensity targets an RPE of 3 to 7 (“moderate,” “somewhat hard,” and “hard”). Progression plans are made for each participant based on physiologic responses and RPE ratings during/after exercise. In accordance with ACSM guidelines, progression in resistance exercises will be obtained by modifying the volume and/or load of individual exercises. For example, if a participant is able to perform 1 set of 12 repetitions at 5 pounds of the chest press with an RPE below 3/10 (indicating light exertion) for 3 consecutive training days, then a second set will be added. Similarly, if a participant is able to perform 2 sets of 15 repetitions at 5 pounds of the chest press with an RPE below 3/10 (indicating light exertion) for 3 consecutive training days, then the load will be increased by 5–10% and the volume dropped to 2 sets of 8–10 repetitions, depending on RPE. Cardiovascular exercise is also programmed progressively, with increases from baseline of 5 minutes/week until the goal of 30 continuous minutes is reached. Once the veteran has maintained this 30 minute goal for a sustained period, the physiologist may opt to increase incline and/or speed to ensure the veteran’s RPE stays between 4 and 7.
The Warrior Wellness program is designed as an individual program, and does not include any group instruction. Although independent work is expected throughout the 12-week exercise prescription, interaction with other participants and the exercise physiologist is always encouraged. The exercise physiologist checks on each participant frequently to ensure proper technique, gauge their preference and tolerance for the prescription, track their progress, and make any adjustments to the exercise prescription for the coming week.
2.5.2. Strategies to facilitate exercise adherence
The primary aim of this pilot intervention is to explore the feasibility and acceptability of a 12-week supervised exercise program among older veterans with PTSD. Thus, the study design involves numerous strategies to motivate and encourage ongoing participation in the program, with an eye to improving recruitment and retention. The core components of the Warrior Wellness intervention are derived from Social Cognitive Theory (SCT; 27) and our previous research for maximizing compliance to prescribed exercise in older adults. Consistent with this theoretical orientation, within-person factors and factors in the social and physical environments are targeted using cognitive and behavioral strategies to enhance self-efficacy, ultimately influencing behavior. The intervention builds on the following 5 SCT domains: 1) self-monitoring and mastery experience, 2) anticipated positive and negative outcomes of the behavior change, 3) behavior planning and associated self-efficacy, and 4) modeling and social support (Table 3).
Table 3.
Theoretical Constructs and Behavioral Strategies for Promoting Adherence and Compliance
| SCT Domain | Warrior Wellness intervention component |
|---|---|
| Favorable expectations about future outcomes associated with increased activity | Review perceived benefits, modify and reinforce realistic expectations |
| Intervention duration (12 weeks): It takes ~60 days for a new behavior to become a habit, and 12 weeks is the minimum duration associated with functional improvements | |
|
| |
| Self-efficacy to initiate changes in physical activity | Discuss gym environment, review and troubleshoot perceived barriers (physical, psychological, social, logistical) |
|
| |
| Monitoring by exercise physiologist and self | Personalized exercise prescription, weekly exercise logs, biometric data, frequent “check-ins” |
|
| |
| Goal setting/action planning | Set S.M.A.R.T. goals, PA contract, attendance goals |
|
| |
| Social support | Derived from exercise physiologist or similar others (other study participants) in addition to social network |
|
| |
| Positive reinforcement | Iterative incentives (water bottle, towel, silicone bracelet), attendance award, end-of-study feedback forms for participants |
The first day with the participant at the exercise location serves as an orientation to the gym environment, facilities, and exercise equipment. Research staff speak with the participant about expectations, attendance, barriers, and physical limitations the individual may have. Previous research has shown that there are many barriers to exercise participation among individuals with psychological conditions (28, 29). Discussing potential barriers with participants at the beginning of the program provides an opportunity to address strategies for dealing with these barriers and to address unrealistic expectations, particularly among individuals who state no anticipated barriers. The research staff provides suggestions for dealing with specific barriers, but we also encourage participants to suggest strategies they have used to deal with any barriers being discussed (for example, lack of motivation, lapse in attendance, or acute onset of depressive symptoms). To facilitate adherence, participants are asked to complete a behavioral contract which includes two self-selected goals using S.M.A.R.T. (Specific, Measurable, Agreed upon, Realistic, Time-based) principles. We specify that one of these goals must address program attendance. The goal is to attend 36 sessions over the 12 week period. However, we inform participants that we understand that there are unavoidable reasons for missing sessions, and the goal is to have them resume participation as soon as they are able after missing a session or two, and to not catastrophize and discontinue participation after a setback. Both the participant and the staff member signs the contract and the participant is instructed to take it home and keep it somewhere visible in their home to remind them of their commitment and goals.
During this orientation session, the research staff also makes sure to discuss aspects of the fitness center environment that may impact the individual’s PTSD symptoms (i.e., loud noises, startling, insecurity). We also educate participants about the expected physiologic responses to exercise (e.g., increased heart rate, respiration rate, sweating), which could be misinterpreted as anxiety symptoms or signs of a panic attack. Educating patients about what to expect during their exercise sessions is done in an effort to minimize avoidance behaviors and early attrition. It is important to note that the decision to deliver this program in a community-based fitness facility was intentional. First, when developing this program we recognized that the gym environment could operate as an In Vivo exposure of sorts for these veterans with PTSD, many of whom endorse an avoidance of crowds, social situations, and a fear of loud noises/uncontrolled environments. The progressive approach to exercise prescription adopted in this study afforded us an opportunity to offer graduated exposure to the gym environment as well, which we hoped would reduce the fear associated with these identified triggers and facilitate social re-integration. Second, we recognized that a common limitation of supervised exercise interventions is that exercise participation rates may not be maintained for long after the intervention concludes, and the supports are removed. In an effort to help the veterans maintain their new exercise habits, we decided to offer the intervention in a non-clinical setting that more closely emulates the type of facility individuals go to for exercise in the community. By doing so, we hope to effectively address a barrier to exercise maintenance and encourage community engagement in this population that is characterized by avoidance behaviors.
The Warrior Wellness program includes study incentives to enhance adherence and retention. For example, our previous intervention work with older adults has shown that Fridays are traditionally a low attendance day. To combat this, we have implemented weekly blood pressure checks at the start of the Friday sessions. Because of the high incidence of hypertension in this population, veterans typically have a vested interest in checking blood pressure. These sessions offer a “hands-on” moment between the exercise physiologist and study participants, provide patients with clinical feedback that they value, and give our staff a chance to check in and inquire about any adverse responses to exercise training. The weekly exercise prescription card was created as an adherence and retention strategy based upon feedback from the consumer advisory board that many older veterans (regardless of PTSD status) lack a “mission.” It was our hope that providing an explicit directive each week would be an effective, culturally tailored practice that encouraged ongoing engagement among these veterans.
Another consideration was the role of social support. Little is known about environmental predictors of exercise participation among veterans. Male veterans typically report exercising alone, though they endorse a desire to perform physical activities with fellow veterans (30, 31). Mindful of the avoidance behaviors characteristic of PTSD, we thought that a facility-based program would provide important opportunities for socialization and integration among program participants, but that group-based exercise classes would likely not be as well received. Instead, we sought to offer a compromise in the gym environment; providing each participant with their own exercise prescription that they completed independently but encouraging interaction with other veteran participants.
Marketing research and the feedback we received from our own consumer advisory board both emphasize the importance of branding for patient recruitment and retention. We also recognize the added value of developing culturally tailored study materials for veteran recruitment and retention (32, 33). With this in mind, a memorable name, the Warrior Wellness project, was selected and printed on all study materials including research staff uniforms, silicone wristbands, water bottles, and exercise towels (Figure 2). The study-branded “swag” items were distributed to providers for making referrals and to participants for study identity and branding. Incentives are given out over the course of the study to encourage adherence by celebrating attendance milestones in the exercise group. Silicone bracelets are given to UC participants at the baseline appointment to encourage a sense of belonging to the study even though they are not receiving the intervention. Perfect attendance certificates are also given out to PA participants at the 6- and 12-week marks. It is important to note that the duration of the program, 12 weeks, was also deliberate. Twelve weeks is the duration of military boot camp, which all of these service members have completed.. Twelve weeks is also the approximate duration of a typical course of trauma-focused psychotherapy, the gold standard treatment for PTSD.
Figure 2.
Warrior Wellness Branding Materials
Finally, another incentive tool that we have developed is the individual feedback form. In addition to the intrinsic benefits of exercise participation, we also emphasize the quantitative data that individuals will receive through their participation in this program. Each veteran is provided an individual feedback form which details the participant’s pre/post performance on physical performance assessments and progression from baseline to the final week of the exercise program in terms of duration and intensity of exercises. These changes are interpreted for the veteran relative to age- and gender-matched population norms. This form is mailed to participants upon completion of their final follow-up appointment, along with the NIH physical activity workbook for older adults, and two Theraband resistance tubes. Providing participants with this detailed report is done as an enrollment incentive and to motivate participants to continue in their active lifestyle after they complete the program by providing them with feedback, exercise equipment, and education.
2.5.3. Arm 2: Usual care control arm
Participants randomized to the UC control group receive the regular standard of care as provided in their usual VA primary, women’s health, mental health, or geriatric clinic for 12 weeks. Several resources are available as part of usual care at the Durham VAHCS. First, patients may be referred by their providers to MOVE! or TeleMove!, a group-based education program that covers nutrition, weight management, and physical activity. Also available is Gerofit, an outpatient supervised exercise program for veterans ≥65 years old, that requires physician referral. Finally, patients with type 2 diabetes may attend a one-time diabetes education class that addresses physical activity and nutrition among other topics. After 12 weeks, each veteran randomized to the UC group comes into the lab to complete 12-week assessments.
2.6. Measures
All study measures are collected by trained study staff. Participants who wish to discontinue their participation in the study are asked to return for assessment visits. All participants receive $50 for baseline assessments, and $75 at week 12. This monetary compensation is meant to help offset transportation costs and the increased payment schedule is intended to incent participants further so as to reduce missing data for the primary outcome. Table 4 describes study measures and the time points at which they are assessed.
Table 4.
Outcomes schedule
| Procedure or measure | Screening/Baseline | Week 12 |
|---|---|---|
| Primary outcomes | ||
| Current PTSD symptoms (PCL-5) | X | X |
| Cardiovascular endurance (6-minute walk test) | X | X |
| Process/adherence measures | ||
| Medical history | X | |
| Clinical measurements | X | X |
| Cognition (SPMSQ) | X | X |
| Current PTSD diagnosis (CAPS-5) | X | |
| Number of exercise sessions attended | X | |
| Warrior Wellness program evaluation | X-Intervention arm only | |
| Secondary outcomes | ||
| Physical performance (4 tests) | X | X |
| Physical activity: self-report & accelerometer | X | X |
| Health-related quality of life | X | X |
| Depressive symptoms | X | X |
| Sleep: self-report and accelerometer | X | X |
| Dietary intake | X | X |
| Exercise barriers self-efficacy | X | X |
2.6.1. Process/adherence measures
The primary aim of this pilot study is to determine the feasibility, fidelity, and acceptability of a 12 week supervised exercise program among older veterans with PTSD. We are tracking the number of patients contacted, screened, eligible, and enrolled, to determine acceptability rates. Source (clinics, electronic data pull, advertisements, participant referral) of patients screened will be tracked so that we can examine which method is more effective for enrolling and whether one method results in variations in the sample. Reasons for refusal will also be collected. Feasibility proportions for screening and recruitment will be calculated at the end of the study.
The number of sessions attended over the course of the 12-week intervention period will be used as a measure of treatment fidelity. Participants who attend ≥85% of the offered exercise sessions over 12 weeks will be classified as “adherent.” Proportion retention will be computed by dividing the number of retained participants at the end of the study by the total number randomized into the study. Based upon our previous studies with older veterans, we project an attrition rate of 20%.
Upon completion of the exercise program participants are asked to complete a program evaluation form to assess feasibility and acceptability of the intervention. This form includes targeted and open-ended questions about their experience with the program and suggestions for how it might be improved. Example items include, “I felt comfortable in the exercise setting (1 (strongly disagree) – 5 (strongly agree)),” and “How can we improve the exercise routine (for example, how the exercise session was conducted, muscle groups targeted, or suggestions for designing the exercise card)?”.
2.6.2. Primary outcomes
Change in PTSD symptom severity over time is the primary outcome of this study. The PTSD Checklist (PCL-5; 34), a 20-item self-report measure reflecting the DSM-V symptoms of PTSD will be used to assess PTSD symptom severity. A total PTSD symptom severity score (20–100) can be obtained by summing the scores from each of the 20 items. All items are rated on a Likert scale of 1 (Not at all) to 5 (Extremely). The PCL-5 can also be used to calculate PTSD symptom severity scores by symptom cluster: re-experiencing (5 items), avoidance (2 items), negative alterations in cognitions and mood (7 items), and hyperarousal (6 items). The reliability and validity of the PCL-5 has been confirmed (35).
Because cardiovascular conditions are prevalent among individuals with PTSD, particularly older veterans, we also objectively assess aerobic capacity using a six-minute walk test (6MWT). This is a self-paced test during which participants are encouraged to walk as far as they can in 6 minutes, taking breaks as necessary. The course is set in a hallway at the Durham VA Medical Center. The total distance walked in 6 minutes is noted for scoring purposes. Greater distance covered indicates better aerobic endurance. This assessment has excellent reliability and validity in older adults when compared to maximal oxygen uptake tests (36).
2.6.3. Participant demographic and clinical characteristics
These characteristics will be used to describe the study sample, as well as to conduct exploratory analyses of effect modification. Demographic characteristics include age, gender, race/ethnicity, education, socioeconomic status, and military service era and branch. Clinical and health-related variables include DSM-V clinical criteria for current PTSD symptoms, self-reported PTSD symptom severity, body mass index (calculated based on measured height and weight), blood pressure, waist circumference, general self-rated health, mood, comorbid medical conditions, sleep, and smoking.
2.6.4. Additional measures
We also collect additional, secondary measures, shown in Table 3, that add important information about the efficacy and effectiveness of the Warrior Wellness intervention. Finally, we will assess both intervention-related and participant costs to create a picture of the costs incurred for intervention delivery. Participant-reported measures of health-related quality of life will also be used to explore cost-effectiveness of this intervention compared to usual care.
2.7. Statistical analysis
The data analysis will be performed using PASW Statistics 18.0 (Chicago, IL) and SAS (9.3). The data will initially be examined for normality violations, outliers, errors, and pattern of missing variables. Baseline differences between the two groups will be examined using analysis of variance for continuously measured variables and χ2 statistics for noncontinuous variables. The efficacy of exercise training compared with usual care in reducing PTSD symptoms and improving cardiovascular endurance will be examined using condition by time multivariate analysis of variance (MANOVA). Condition will be a between-subjects factor and time will be a within-subjects factor. Next, analysis of covariance (ANCOVA) will be conducted on these outcomes, using baseline values as covariates.
To inform subsequent full-scale trials, F tests and effect sizes will be reported. Effect sizes associated with univariate F-statistics will be expressed as eta-squared (ƞ2). Effect sizes based on a difference in mean scores will be expressed as Cohen’s d. The percentage of participants who show clinically significant improvement on primary and secondary outcomes based on criteria in the literature will also be calculated.
Retention will be calculated as the number of participants who complete 12 week assessments from the initial number randomized to the trial. For the Warrior Wellness group, adherence to the prescribed protocol (3 times per week), will be calculated using program attendance logs.
3. Discussion
This study is one of the first clinical trials to evaluate the feasibility, acceptability, efficacy, and effectiveness of a supervised exercise program culturally tailored for older veterans with PTSD. The Warrior Wellness Study was designed and implemented following principles of physical activity and exercise prescription established by the American College of Sports Medicine (26). Many previous studies of physical activity and mental illness appear to have been conducted without consideration for similar established guidelines, making this a notable strength of our study design. The assessment tools in this study, particularly the CAPS (24) and objective assessments of physical activity, sleep, and physical function, are the gold standard measurements. Finally, our recruitment of individuals with PTSD outside of the inpatient setting is a notable difference from previous studies that have relied exclusively on inpatient samples, and enhances the generalizability of our program and results. It is our hope that the detailed and comprehensive reporting of the exercise intervention, following the Consensus on Exercise Reporting Template (CERT; 37), provides information for clinicians and researchers interested in delivering this program in practice or in replicating this work in other samples.
Results of this pilot trial will provide evidence of the acceptability of a supervised exercise intervention among older adults with PTSD and the effectiveness of regular exercise training on important clinical endpoints. Physical activity is associated with improved physical and psychological well-being, but it is unknown if individuals with PTSD will adhere to an exercise program, and whether exercise training alters PTSD symptoms and other clinical health indicators in this complex patient group. If effective, this study will contribute to the development and application of exercise therapeutic approaches to reduce the disease burden and impact morbidity in persons with PTSD, as a stand-alone therapy, or as an evidence-based adjunct to psychotherapeutic treatments.
Acknowledgments
This research is supported by a Career Development grant from the Department of Veterans Affairs Rehabilitation Research and Development (RR&D) service to Dr. Hall (2RX001316). Drs. Hall and Morey are supported by the Duke Pepper Center (NIA P30AG028716). We express our deepest gratitude to Lisa Brown for her assistance with the implementation of the program.
Footnotes
Conflict of Interest
The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs and do not constitute endorsement by ACSM. None of the authors have any conflicts of interest to report.
References
- 1.Marmar CR, Schlenger W, Henn-Haase C, Qian M, Purchia E, Li M, et al. Course of posttraumatic stress disorder 40 years after the Vietnam War: Findings from the National Vietnam Veterans Longitudinal Study. JAMA Psychiatry. 2015;72(9):875–81. doi: 10.1001/jamapsychiatry.2015.0803. [DOI] [PubMed] [Google Scholar]
- 2.Dedert EA, Calhoun PS, Watkins LL, Sherwood A, Beckham JC. Posttraumatic stress disorder, cardiovascular, and metabolic disease: a review of the evidence. Ann Behav Med. 2010;39(1):61–78. doi: 10.1007/s12160-010-9165-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hall KS, Beckham JC, Bosworth HB, Sloane R, Pieper CF, Morey MC. PTSD is negatively associated with physical performance and physical function in older overweight military Veterans. J Rehabil Res Dev. 2014;51(2):285–95. doi: 10.1682/JRRD.2013.04.0091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Levine AB, Levine LM, Levine TB. Posttraumatic stress disorder and cardiometabolic disease. Cardiology. 2014;127(1):1–19. doi: 10.1159/000354910. [DOI] [PubMed] [Google Scholar]
- 5.Pietrzak RH, Goldstein RB, Southwick SM, Grant BF. Physical health conditions associated with posttraumatic stress disorder in U.S. older adults: results from wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. J Am Geriatr Soc. 2012;60(2):296–303. doi: 10.1111/j.1532-5415.2011.03788.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rosenbaum S, Stubbs B, Ward PB, Steel Z, Lederman O, Vancampfort D. The prevalence and risk of metabolic syndrome and its components among people with posttraumatic stress disorder: a systematic review and meta-analysis. Metabolism. 2015;64(8):926–33. doi: 10.1016/j.metabol.2015.04.009. [DOI] [PubMed] [Google Scholar]
- 7.Hall KS, Hoerster KD, Yancy WS., Jr Post-traumatic stress disorder, physical activity, and eating behaviors. Epidemiol Rev. 2015;37:103–15. doi: 10.1093/epirev/mxu011. [DOI] [PubMed] [Google Scholar]
- 8.Vancampfort D, Stubbs B, Richards J, Ward PB, Firth J, Schuch FB, et al. Physical fitness in people with posttraumatic stress disorder: a systematic review. Disabil Rehabil. 2016:1–7. doi: 10.1080/09638288.2016.1226412. [DOI] [PubMed] [Google Scholar]
- 9.Whitworth JW, Ciccolo JT. Exercise and post-traumatic stress disorder in military veterans: A systematic review. Mil Med. 2016;181(9):953–60. doi: 10.7205/MILMED-D-15-00488. [DOI] [PubMed] [Google Scholar]
- 10.Geneen LJ, Moore RA, Clarke C, Martin D, Colvin LA, Smith BH. Physical activity and exercise for chronic pain in adults: an overview of Cochrane Reviews. Cochrane Database Syst Rev. 2017;4 doi: 10.1002/14651858.CD011279.pub3. CD011279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Penedo FJ, Dahn JR. Exercise and well-being: a review of mental and physical health benefits associated with physical activity. Curr Opin Psychiatry. 2005;18(2):189–93. doi: 10.1097/00001504-200503000-00013. [DOI] [PubMed] [Google Scholar]
- 12.Stonerock GL, Hoffman BM, Smith PJ, Blumenthal JA. Exercise as Treatment for Anxiety: Systematic Review and Analysis. Ann Behav Med. 2015;49(4):542–56. doi: 10.1007/s12160-014-9685-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Busch AM, Ciccolo JT, Puspitasari AJ, Nosrat S, Whitworth JW, Stults-Kolehmainen M. Preferences for exercise as a treatment for depression. Ment Health Phys Act. 2016;10:68–72. doi: 10.1016/j.mhpa.2015.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hall KS, Gregg J, Bosworth HB, Beckham JC, Hoerster KD, Sloane R, et al. Physical activity counseling promotes physical and psychological resilience in older veterans with posttraumatic stress disorder. Ment Health Phys Act. 2016;11:53–9. doi: 10.1016/j.mhpa.2016.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rosenbaum S, Tiedemann A, Ward PB, Curtis J, Sherrington C. Physical activity interventions: an essential component in recovery from mental illness. Br J Sports Med. 2014 doi: 10.1136/bjsports-2014-094314. [DOI] [PubMed] [Google Scholar]
- 16.Lu MW, Carlson KF, Duckart JP, Dobscha SK. The effects of age on initiation of mental health treatment after positive PTSD screens among Veterans Affairs primary care patients. Gen Hosp Psychiatry. 2012;34(6):654–9. doi: 10.1016/j.genhosppsych.2012.07.002. [DOI] [PubMed] [Google Scholar]
- 17.Rosenbaum S, Tiedemann A, Berle D, Ward PB, Zachary S. Exercise as a novel treatment option to address cardiometabolic dysfunction associated with PTSD. Metabolism. 2015;64(5):e5–6. doi: 10.1016/j.metabol.2015.01.016. [DOI] [PubMed] [Google Scholar]
- 18.Wolf EJ, Schnurr PP. PTSD-related cardiovascular disease and accelerated cellular aging. Psychiatr Ann. 2016;46:527–32. doi: 10.3928/00485713-20160729-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zen AL, Whooley MA, Zhao S, Cohen BE. Post-traumatic stress disorder is associated with poor health behaviors: Findings from the Heart and Soul Study. Health Psychol. 2012;31(2):194–201. doi: 10.1037/a0025989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Babson KA, Heinz A, Ramirez G, Puckett M, Irons JG, Bonn-Miller MO, et al. The interactive role of exercise and sleep on veteran recovery from symptoms of PTSD. Ment Health Phys Act. 2015;8:15–20. [Google Scholar]
- 21.Manger TA, Motta RW. The impact of an exercise program on posttraumatic stress disorder, anxiety, and depression. Int J Emerg Ment Health. 2005;7(1):49–57. [PubMed] [Google Scholar]
- 22.Rosenbaum S, Sherrington C, Tiedemann A. Exercise augmentation compared with usual care for post-traumatic stress disorder: a randomized controlled trial. Acta Psychiatr Scand. 2015;131(5):350–9. doi: 10.1111/acps.12371. [DOI] [PubMed] [Google Scholar]
- 23.Maguen S, Hoerster KD, Littman AJ, Klingaman EA, Evans-Hudnall G, Holleman R, et al. Iraq and Afghanistan veterans with PTSD participate less in VA's weight loss program than those without PTSD. J Affect Disord. 2016;193:289–94. doi: 10.1016/j.jad.2015.12.078. [DOI] [PubMed] [Google Scholar]
- 24.Weathers FW, Blake DD, Schnurr PP, Kaloupek DG, Marx BP, Keane TM. Clinician-Administered PTSD Scale for DSM-5 (CAPS-5) Boston, MA: National Center for PTSD; 2013. [Google Scholar]
- 25.Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975;23(10):433–41. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- 26.U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Physical Activity Guidelines for Americans. Washington, D.C.: 2008. [Google Scholar]
- 27.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice Hall; 1986. [Google Scholar]
- 28.Firth J, Rosenbaum S, Stubbs B, Gorczynski P, Yung AR, Vancampfort D. Motivating factors and barriers towards exercise in severe mental illness: a systematic review and meta-analysis. Psychol Med. 2016;46(14):2869–81. doi: 10.1017/S0033291716001732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Seime RJ, Vickers AJ. The challenges of treating depression with exercise: from evidence to practice. Clin Psychol. 2006;13(2):194–7. [Google Scholar]
- 30.Buis LR, Kotagal LV, Porcari CE, Rauch SA, Krein SL, Richardson CR. Physical activity in postdeployment Operation Iraqi Freedom/Operation Enduring Freedom veterans using Department of Veterans Affairs services. J Rehabil Res Dev. 2011;48(8):901–11. doi: 10.1682/jrrd.2010.08.0144. [DOI] [PubMed] [Google Scholar]
- 31.Jay M, Mateo KF, Squires AP, Kalet AL, Sherman SE. Military service and other socioecological factors influencing weight and health behavior change in overweight and obese Veterans: a qualitative study to inform intervention development within primary care at the United States Veterans Health Administration. BMC Obesity. 2016;3:5. doi: 10.1186/s40608-016-0087-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Goodrich DE, Hall KS. Physical Activity among Military Veterans. In: Bopp M, editor. Physical Activity in Diverse Populations: Evidence and Practice. London, England: Routledge; 2017. [Google Scholar]
- 33.Michalek AK, Kan D, Prochaska J. Engaging veterans with substance abuse disorders into a research trial: success with study branding, networking, and presence. Transl Behav Med. 2015;5(2):167–76. doi: 10.1007/s13142-014-0302-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, Schnurr PP. The PTSD Checklist for DSM-5 (PCL-5) Boston, MA: National Center for PTSD; 2013. [Google Scholar]
- 35.Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, et al. Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition (PCL-5) in veterans. Psychol Assess. 2016;28(11):1379–91. doi: 10.1037/pas0000254. [DOI] [PubMed] [Google Scholar]
- 36.Rikli RE, Jones CJ. The reliability and validity of a 6-minute walk test as a measure of physical endurance in older adults. J Aging Phys Act. 1998;6:363–75. [Google Scholar]



