Abstract
Objective:
To investigate associations between maternal rotating night shift work history before pregnancy and number of night shifts worked as nurses during pregnancy and offspring early-life through adolescence weight outcomes.
Methods:
Over 4,000 children, enrolled in the Growing Up Today Study 2 between 2004 and 2013, and their mothers participating in the Nurses Health Study 2 were included in our analyses.
Results:
Children of women who worked rotating night shifts before pregnancy were similar in birth weight and body size at age 5 compared to children of women without any night shift work before pregnancy. However, they had a modestly elevated risk of having overweight or obesity (relative risk (RR)=1.11, 95% confidence interval (CI): 1.02, 1.21), which was stronger for persistently having overweight or obesity during adolescence and early adulthood. Longer duration of rotating night shift work was not associated with any of these weight outcomes. Weight outcomes of children of women with versus without night shift work during pregnancy were similar, regardless of frequency of night shifts worked during pregnancy (all Ptrend>0.09).
Conclusions:
Overall, nurses’ night shift work before or during pregnancy did not affect offspring weight outcomes. Future larger studies should explore these associations in more detail.
Keywords: Youth, Public Health, Perinatal Programming, Overweight, Occupational Medicine
Introduction
Childhood and adolescent overweight and obesity have become a major public health concern in the United States and globally (1). Apart from childhood obesity’s more immediate co-morbidities, such as hyperinsulinaemia, poor glucose tolerance, and increased risk of type 2 diabetes and hypertension, it can also lead to an increased risk of heart disease and certain cancers later in life (2). Although environmental and behavioral factors, such as parental socio-economic status and children’s sedentary behavior, have been established as major determinants of childhood obesity (3), growing evidence suggests that several childhood and even adulthood health outcomes are, at least in part, programmed during pregnancy (4). Specifically, the maternal environment during pregnancy could influence fetal development and programming through alterations in the intrauterine environment (5).
Night shift work and the resulting disruption of social and biological rhythms have been linked to higher risk of several chronic diseases (6–8) as well as epigenetics alterations (9); in addition, night shift work during pregnancy has been linked to an increased risk of spontaneous abortions (10) and preterm delivery (11). Emerging evidence from animal models suggests that maternal circadian disruption can also induce long-term metabolic changes in the offspring (12–14). For example, exposing pregnant rats to reversals of the photoperiod twice every week throughout gestation and for the first week after birth showed no effect on litter size or birth weight; however, the progeny had an increased risk of adiposity, hyperleptinaemia and altered glucose metabolisms in adulthood (13).
Despite the high prevalence of shift work among US women during pregnancy (15), little is known about the potential health implications of pre-conception shift work and night shift work during pregnancy on offspring later in life. We therefore aimed to provide insights regarding the association of pre-conception night shift work history and shift work during pregnancy with offspring weight outcomes during childhood and adolescence using existing data from mother-child pairs participating in the Nurses Health Study II (NHS II) and Growing Up Today Study 2 (GUTS2).
Methods
Study population
The present study included mothers who were enrolled in the Nurses’ Health Study II (NHS II) and their children who participated in the Growing Up Today Study 2 (GUTS2). NHS II is an ongoing prospective cohort study of US female nurses, which was established in 1989 when 116,430 female nurses aged 25–42 years responded to mailed questionnaires regarding their lifestyle, reproductive factors, and medical history. Follow-up questionnaires are mailed biennially to these nurses to update information on various risk factors and occurrence of major diseases. GUTS2 began in 2004 when NHS II participants who had previously reported to have children born between 1987 and 1995 were asked whether their children could participate in a follow-up study. After receiving maternal consent, invitation letters and questionnaires were sent to 17,280 children; 10,918 children returned their completed questionnaire. Follow-up questionnaires were sent to these children in 2006, 2008, 2011, and 2013 to update information on health, lifestyle factors, and growth indicators.
This study was approved by the Committee on the Use of Human Subject in Research at the Brigham and Women’s Hospital and the Harvard T.H. Chan School of Public Health (Boston, MA, USA). Returning the self-administered questionnaires was taken to imply informed consent in both cohorts.
Ascertainment of night shift work among mothers
Mother’s history of rotating night shift before pregnancy
The NHS II baseline questionnaire queried number of years having worked rotating night shifts (defined as “at least three nights per month in addition to working days or evenings in the respective month”). This information was updated in 1991 and 1993 to capture changes since the previous questionnaire, and again in 2001 to capture changes between 1993 and 1995 (the latest possible year of conception). Based on the return date of the respective NHS II questionnaire and birth date of the GUTS2 participant, we calculated the cumulative number of years a mother had worked rotating night shifts before conception for children born in 1989 or later.
Mother’s night shift work exposure during pregnancy:
On the 2001 NHS II questionnaire, participants were asked whether they had experienced at least one pregnancy since 1993, had worked as a nurse during the most recent pregnancy, and would be willing to answer a supplemental questionnaire focused on occupational activities and exposures during this pregnancy. A supplemental questionnaire that queried shift work information among other occupational exposures during the most recent pregnancy since 1993 was mailed to those participants who answered ‘yes’ to all 3 questions. Women were asked to report usual working schedules and average number of night shifts per month for each trimester of pregnancy, with the following response options: none, 1–2 nights/month, 3–4 nights/month, 2–3 nights/week, or 4+ nights/week.
Ascertainment of weight outcomes among offspring
Information on offspring birth weight was obtained from the 2009 GUTS2 mothers’ questionnaire. Recall of offspring birth weight has been found to have excellent validity (16). On the baseline questionnaire in 2004, GUTS2 participants (age range 9–15 years) were asked to recall their body size at age 5 by selecting one of eight pictograms (‘somatotypes’) that would most accurately represent their body shape at that age (ranging from 1=most lean to 8=most obese). Correlations between recalled somatotypes and BMI measured at approximately the same ages have ranged from 0.53 to 0.75 among studies of adults (17). We created a binary outcome splitting at the median value of the distribution, and defined larger than median body sizes as cases. Information on weight and height was self reported on each GUTS2 questionnaire. To classify the offspring as having normal weight, overweight, or obesity, we used age-and sex specific cutoffs from the International Obesity Task Force (18) for participant aged 18 years or younger. Beyond age 18, overweight and obesity were defined using standard World Health Organization (WHO) cutoffs (i.e., body mass index (BMI, kg/m2) 25.0–29.9 overweight, BMI >30 obese). We defined participants as cases if they were classified as having either overweight or obesity at any given time during follow-up. Additionally, we defined participants as persistently having overweight or obesity if they were classified as having overweight or obesity at three consecutive questionnaire cycles. Figure 1 displays a timeline of exposure and outcomes assessments.
Figure 1.
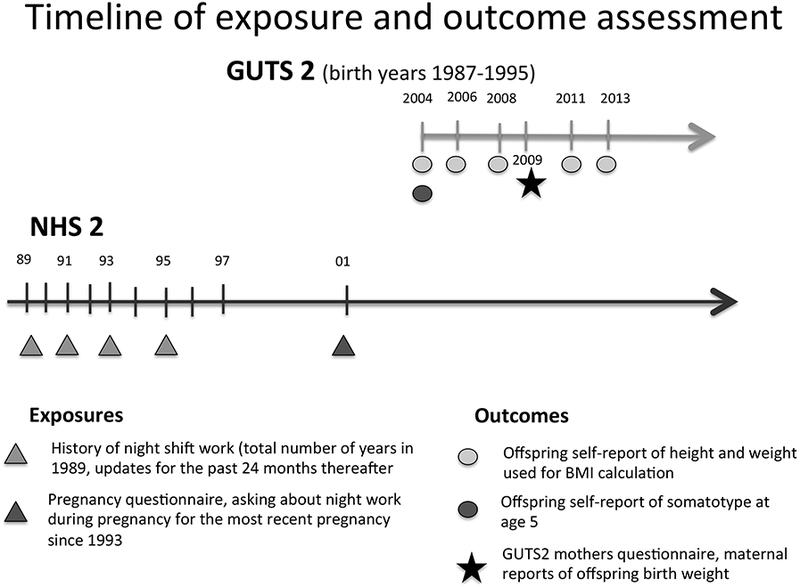
Timeline of exposure and outcomes assessments in NHS2 and GUTS2 cohorts.
Ascertainment of covariates
Maternal age at delivery was derived calculating the difference between a mother’s birth date and that of her child. We utilized maternal dietary information assessed by the well-validated Willett food frequency questionnaire FFQ (19) using information from the 1991 NHS II questionnaire to calculate the Alternative Healthy Eating Index (AHEI) (20). Physical activity was assessed in 1989 and derived as metabolic equivalent (MET)-hours per week (21). Smoking status and BMI were queried biannually, and we selected the most recent value prior to conception of the first included child. Maternal chronotype was assessed in 2009. As a proxy for socioeconomic status, we used husband’s education, which was assessed in 1999.
Information on number of previous pregnancies, mode of delivery, pregnancy-related hypertension, pre-eclampsia, gestational diabetes, gestational age at delivery, and pregnancy multiplicity was extracted from the lifetime pregnancy assessment in 2009. We approximated pregnancy-related weight gain by taking the difference of the first BMI reported after delivery and the last recorded BMI before conception.
From the occupational supplemental questionnaire, we had trimester-specific information on smoking behavior, alcohol consumption, coffee consumption, and frequency of activities involving lifting or moving a physical load of 25 pounds or more during pregnancy.
Offspring Tanner stage of pubertal development was determined in 2004 on the GUTS2 baseline questionnaire, using a validated scale of pubic hair illustrations (22). Tanner stage ranges from 1 to 5, with stage 1 indicating prepubescence and stage 5 indicating maturity. Offspring sedentary behavior was summarized by the sum of the hours per week spent watching television, using the computer, surfing on the internet, and reading/doing homework over the past year, as reported in 2004. Detailed cutoffs used in all analyses are presented in the footnotes of Tables 2 and 3.
Table 2.
Adjusted Mean Differences (MD) and Relative risks (RR) for Offspring Weight Outcomes Through Childhood and Adolescence According to Maternal Rotating Night Shiftwork History Before Pregnancy, Using Data From the Growing Up Today Study 2 From 2004 to 2013, Restricted to Singleton, Full-term Births.
| History of rotating night shift work | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Never worked rotating night shifts | <3 yrs | 3–5 yrs | ≥6 yrs | P trend | Ever worked rotating night shifts | |||||
| Mean differences in offspring birth weight (grams) | ||||||||||
| Participants | 1,458 | 1,305 | 964 | 416 | 2,685 | |||||
| MD | 95% CI | MD | 95% CI | MD | 95% CI | MD | 95% CI | |||
| Basic model a | 0 (reference) | 10.68 | −26.33, 47.69 | 0.98 | −39.06, 41.03 | −7.80 | −65.11, 49.51 | 0.79 | 4.41 | −27.48, 36.30 |
| MV model 1 b | 0 (reference) | 12.16 | −24.54, 48.87 | 4.73 | −34.55, 44.02 | −1.43 | −59.29, 56.43 | 0.99 | 7.51 | −23.89, 38.92 |
| MV model 2 c | 0 (reference) | 10.33 | −26.26, 49.91 | 2.39 | −36.85, 41.64 | −6.28 | −63.84, 51.27 | 0.85 | 5.06 | −26.32, 36.44 |
| Relative risk of offspring’s somatotype at age 5 being larger than the median | ||||||||||
| Cases/participants | 628/1,631 | 584/1,451 | 437/1,103 | 186/474 | 1,207/3,028 | |||||
| RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI | |||
| Basic model a | 1 (reference) | 1.04 | 0.95, 1.14 | 1.02 | 0.93, 1.13 | 1.01 | 0.89, 1.15 | 0.82 | 1.03 | 0.95; 1.11 |
| MV model 1 b | 1 (reference) | 1.03 | 0.94, 1.12 | 1.02 | 0.92, 1.12 | 1.01 | 0.88, 1.15 | 0.87 | 1.02 | 0.95; 1.10 |
| MV model 2 c | 1 (reference) | 1.02 | 0.94, 1.12 | 1.01 | 0.92, 1.12 | 1.00 | 0.88, 1.14 | 0.97 | 1.02 | 0.94; 1.10 |
| Relative risk of offspring having overweight or obesity at any time between 2004 and 2013 d | ||||||||||
| Cases/participants | 523/1,667 | 523/1,494 | 394/1,125 | 168/487 | 1,085/3,106 | |||||
| RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI | |||
| Basic model a | 1 (reference) | 1.10 1.00, 1.22 | 1.11 | 1.00, 1.24 | 1.08 | 0.94, 1.25 | 0.11 | 1.10 | 1.01, 1.20 | |
| MV model 1 b | 1 (reference) | 1.11 | 1.01, 1.23 | 1.12 | 1.01, 1.25 | 1.07 | 0.92, 1.23 | 0.14 | 1.11 | 1.02, 1.21 |
| MV model 2 c | 1 (reference) | 1.11 1.00, 1.22 | 1.10 | 0.99, 1.23 | 1.03 | 0.89, 1.18 | 0.31 | 1.09 | 1.00, 1.19 | |
| Relative risk of offspring persistently having overweight or obesity e | ||||||||||
| Cases/participants | 114/1,667 | 124/1,494 | 103/1,125 | 37/487 | 264/3,106 | |||||
| RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI | |||
| Basic modela | 1 (reference) | 1.19 | 0.92, 1.54 | 1.35 | 1.04, 1.76 | 1.07 | 0.74, 1.55 | 0.13 | 1.23 | 0.99, 1.53 |
| MV model 1b | 1 (reference) | 1.22 | 0.95, 1.58 | 1.39 | 1.06, 1.80 | 1.04 | 0.71, 1.52 | 0.17 | 1.25 | 1.00, 1.56 |
| MV model 2 c | 1 (reference) | 1.21 | 0.94, 1.55 | 1.33 | 1.02, 1.73 | 0.96 | 0.67, 1.40 | 0.31 | 1.21 | 0.97, 1.51 |
| Mean differences in offspring BMI (kg/m2) using n=15,008 repeated measurements from 2004–2013 | ||||||||||
| Observations | 5,309 | 4,674 | 3,528 | 1,487 | 9,689 | |||||
| MD | 95% CI | MD | 95% CI | MD | 95% CI | MD | 95% CI | |||
| Basic model a, f | 0 (reference) | 0.04 | −0.20, 0.29 | 0.22 | −0.04, 0.49 | 0.53 | 0.17, 0.89 | <0.01 | 0.18 | −0.03, 0.39 |
| MV model 1 b | 0 (reference) | 0.07 | −0.18, 0.31 | 0.26 | −0.01, 0.52 | 0.49 | 0.13, 0.85 | <0.01 | 0.20 | −0.01, 0.41 |
| MV model 2 c | 0 (reference) | 0.03 | −0.21, 0.26 | 0.20 | −0.06, 0.45 | 0.33 | −0.02, 0.67 | 0.03 | 0.13 | −0.01, 0.41 |
Abbreviations: CI, confidence interval; MD, mean difference; MV, multivariable model; RR, relative risk
Adjusted for offspring gender (boy/girl) and gestational age ≥42 wks (yes/no)
Additionally adjusted for maternal age at pregnancy, smoking status before pregnancy (never, current, past), alternative healthy eating score (quintiles), physical activity (METs hours/week; quintiles), husband’s education (less than 2yr college, 4yr college, grad school), parity (nulliparity, 1, 2, 3+ previous pregnancies)
Additionally adjusted for BMI before pregnancy (<25, 25–29, ≥30 kg/m2)
Overweight and obesity status defined according to the age-and sex specific cutoffs from the International Obesity Task Force.
Persistently overweight or obese was defined as falling into that category in 3 consecutive follow-up cycles.
All models are additionally adjusted for age at BMI measurement.
Table 3.
Adjusted Mean Differences (MD) and Relative Risks (RR) for Offspring Weight Outcomes Through Childhood and Adolescence by Categories of Average Number of Night Shifts Worked per Month During Pregnancy, Using Data From the Growing Up Today Study 2 from 2004 to 2013, Restricted to Singleton, Full Term Nirths (n=545).
| Average number of night shifts/ month | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| None | <3 nights/month | 3–9 nights/month | ≥10 nights/month | P trend | Any no. nights/month | |||||
| Mean differences in offspring birth weight (grams) | ||||||||||
| Participants | 352 | 39 | 17 | 35 | 91 | |||||
| MD | 95% CI | MD | 95% CI | MD | 95% CI | MD | 95% CI | |||
| Basic model a | 0 (reference) | −54.19 | −209.96, 101.58 | −203.53 | −432.97, 25.92 | −46.27 | −210.25, 117.70 | 0.23 | −79.04 | −187.53, 29.45 |
| MV model 1 b | 0 (reference) | −54.48 | −215.12, 106.17 | −231.85 | −463.36, −0.33 | 18.94 | −146.85, 184.73 | 0.58 | −57.76 | −170.10, 54.58 |
| MV model 2 c | 0 (reference) | −64.28 | −225.75, 97.19 | −223.23 | −456.26, 9.80 | 19.51 | −146.50, 185.51 | 0.60 | −59.64 | −172.11, 52.82 |
| Relative risk of offspring’s somatotype at age 5 being larger than the median | ||||||||||
| Cases/participants | 159/417 | 16/43 | 8/21 | 10/45 | 34/109 | |||||
| RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI | |||
| Basic model a | 1 (reference) | 0.95 | 0.64, 1.42 | 1.01 | 0.57, 1.78 | 0.59 | 0.34, 1.04 | 0.08 | 0.82 | 0.60, 1.11 |
| MV model 1 b | 1 (reference) | 0.96 | 0.62, 1.47 | 1.03 | 0.60, 1.78 | 0.59 | 0.33, 1.04 | 0.09 | 0.82 | 0.60, 1.12 |
| MV model 2 c | 1 (reference) | 0.96 | 0.63, 1.48 | 1.06 | 0.61, 1.84 | 0.59 | 0.33, 1.05 | 0.10 | 0.82 | 0.60, 1.13 |
| Relative risk of offspring having overweight or obesity at any time between 2004 and 2013 d | ||||||||||
| Cases/participants | 156/431 | 12/43 | 4/21 | 13/45 | 29/109 | |||||
| RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI | |||
| Basic model a | 1 (reference) | 0.75 | 0.46, 1.21 | 0.54 | 0.22, 1.33 | 0.82 | 0.51, 1.31 | 0.19 | 0.74 | 0.53, 1.03 |
| MV model 1 b | 1 (reference) | 0.76 | 0.45, 1.29 | 0.51 | 0.20, 1.27 | 0.80 | 0.49, 1.29 | 0.16 | 0.73 | 0.51, 1.03 |
| MV model 2 c | 1 (reference) | 0.80 | 0.48, 1.35 | 0.53 | 0.21, 1.37 | 0.78 | 0.48, 1.25 | 0.14 | 0.74 | 0.52, 1.05 |
| Mean differences in offspring BMI (kg/m2) using n=1,632 repeated measurements from 2004–2013 | ||||||||||
| Observations | 1,306 | 120 | 64 | 142 | 326 | |||||
| MD | 95% CI | MD | 95% CI | MD | 95% CI | MD | 95% CI | |||
| Basic model a, f | 0 (reference) | 0.24 | −0.85, 1.32 | −0.27 | −1.78, 1.23 | −0.02 | −1.07, 1.03 | 0.88 | 0.03 | −0.69, 0.75 |
| MV model 1 b | 0 (reference) | 0.21 | −0.91, 1.34 | −0.54 | −2.08, 1.00 | −0.21 | −1.29, 0.87 | 0.56 | −0.11 | −0.86, 0.64 |
| MV model 2 c | 0 (reference) | 0.45 | −0.64, 1.54 | −0.26 | −1.75, 1.24 | −0.31 | −1.35, 0.73 | 0.53 | −0.01 | −0.74, 0.72 |
Abbreviations: CI, confidence interval; MD, mean difference; MV, multivariable model; RR, relative risk
Adjusted for offspring gender (boy/girl) and gestational age ≥42 wks (yes/no)
Additionally adjusted for maternal age at pregnancy, smoking status before pregnancy (never, current, past), alternative healthy eating score (quintiles), physical activity (METs hours/week; quintiles), husband’s education (less than 2yr college, 4yr college, grad school), parity (nulliparity, 1, 2, 3+ previous pregnancies), history of rotating night shift work (never, <3 yrs, 3–5 yrs, ≥ 6 yrs).
Additionally adjusted for BMI before pregnancy (<25, 25–29, ≥30 kg/m2)
Overweight and obesity status defined according to the age-and sex specific cutoffs from the International Obesity Task Force.
All models are additionally adjusted for age at BMI measurement.
Statistical analysis
Mother’s history of rotating night shift exposure before conception
As pre-conception history of rotating night shift work could be assessed only after 1989, we excluded from the original cohort of 10,918 children the 4,721 children conceived before 1989. Among the remainder born after 1989, we further excluded twins and triplets (195 children, 87 mothers), children who were not born full term (less than 37 weeks) (1,182 children, 1,001 mothers), and mother-child pairs with missing exposure information (7 children, 6 mothers), leaving 4,813 children bom to 4,044 mothers that comprised our analytic sample. Out of these 91% had a least 2 measurements of BMI at different time points.
We used generalized estimating equations (GEE) regression models specifying an exchangeable correlation structure with appropriate link functions (to account for within-sibling correlation in outcomes) to estimate mean differences (MD) and 95% confidence intervals (CIs) in offspring birth weight comparing none vs. any number of years of rotating night shiftwork, as well as across four data-driven categories of cumulative years of rotating night shift work before conception (none, <3 years, 3–5 years, and ≥6 years). We calculated relative risks (RR) and 95% CIs of offspring overweight/obesity and larger than median somatotype at age 5. We considered women without a history of rotating night shift work as the reference group. If the log-binomial model did not converge, we approximated RRs using Poisson models with robust variance estimators (23).
To utilize all available repeated measurements of offspring BMI, we applied linear mixed effects models with random intercepts and an unstructured covariance structure, which permit description of individual BMI trajectories across age and provide explicit tests for changes in BMI with age (24). In these analyses, we included terms for the exposure, covariates, offspring age, and the interaction of BMI and offspring age to evaluate differences in change in BMI over time across exposure groups.
In basic models, we adjusted for offspring sex, gestational age, and offspring age at baseline where appropriate (Basic model). We then considered the inclusion of several sets of potential confounding variables. First, we added maternal lifestyle characteristics (multivariate (MV) model 1), including smoking status before pregnancy, alternative healthy eating score (AHEI), physical activity, husband’s education, and parity. The addition of pregnancy-related factors including pre-eclampsia, gestational hypertension or diabetes, type of delivery, or change in maternal BMI before and after pregnancy did not markedly change effect estimates for shiftwork; therefore, these variables were not retained in the model. Lastly, we additionally adjusted for maternal BMI before pregnancy (MV model 2).
Mother’s night shift work exposure during pregnancy
For analyses assessing associations between night shift work during pregnancy and weight outcomes in the offspring, we identified all GUTS2 participants whose mothers had completed the supplemental pregnancy questionnaire between 2001 and 2003, resulting in 621 mother-child pairs with available information on pregnancy behaviors coupled with outcome information on the matching GUTS2 child. Of these, only full-term pregnancies were considered eligible (n=549). After further removal of mother-child pairs with missing exposure information, 545 matching pairs were left for these analyses, whereof 89% had at least 2 repeated BMI measurements.
Using trimester-specific information on shift work frequency from the supplemental questionnaire, we calculated average number of night shifts per month throughout the entire pregnancy and created four categories (none, ≤2, 3–9, and ≥10 night shifts per month); we also created the category of any number of night shifts per month.
We used standard generalized linear models with appropriate link functions (linear or log-binomial/Poisson), and added covariates following a similar approach as described above; we added history of night shift work to MV model 1. We also considered maternal pregnancy-related lifestyle factors (smoking behavior, alcohol consumption, coffee consumption, heavy lifting during first trimester), but did not retain these variables in our main models because they did not alter our estimates (data not shown).
Since previous studies found maternal BMI before pregnancy (25) to be one of the strongest predictors of offspring obesity during adolescence, in addition to adjustment for maternal BMI, we assessed effect modification for offspring weight outcomes by maternal BMI before pregnancy. Maternal chronotype was also found to potentially interact with work schedules in determining a person’s disease risk (26–28), hence we examined whether associations were different in children born to mothers with reportedly different chronotypes. In all analyses, missing indicators were created for missing covariate values. P values for interactions were obtained by testing the significance of multiplicative interaction terms in multivariable regression models. All statistical tests were two sided and were considered statistically significant at p<0.05. All analyses were conducted using SAS version 9.4 (SAS Institute, Cary, NC).
Results
Mother’s history of rotating night shift work before pregnancy
The 4,044 mothers were on average 33.4 (SD=3.6) years old when they gave birth to the children included in this analysis, and 65% of them reported ever having worked night shifts. At enrollment in GUTS2 in 2004, children were on average 11.7 (SD=1.2) years old. Overall, there were only modest differences in terms of maternal and offspring characteristics according to history of night shift work before pregnancy (Table 1a). Mothers who had worked night shifts for six years or more prior to conception of the first considered child were older, more likely to be past or current smokers, more adherent to a healthy diet (AHEI), and more physically active compared to women with no history of working night shifts. Also, offspring born to mothers with longer shift work history were more likely to be delivered by Cesarean section compared to those born to mothers without a history of shift work.
Table 1a.
Maternal and Offspring Characteristics by Rotating Night Shift Work History Before pregnancy, for 4,044 Mothers of a Total of 4,813 Children, Born Between 1989 and 1995, Enrolled in the Growing Up Today Study 2.
| Characteristic | History of rotating night shift work | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Never worked rotating night shifts (n=1,424) |
<3 yrs (n=1,254) |
3–5 yrs (n=946) |
≥6 yrs (n=420) |
Ever worked rotating night shfits (n=2,620) |
||||||
| Mean (SD) | %a | Mean (SD) | % | Mean (SD) | % | Mean (SD) | % | Mean (SD) | % | |
| Maternal age at delivery b | 33.1 (3.5) | 33.2 (3.6) | 33.4 (3.5) | 35.0 (3.2) | 33.6 (3.5) | |||||
| BMI before pregnancy | 22.7 (3.9) | 22.7 (3.8) | 23.0 (3.9) | 23.3 (4.2) | 22.9 (3.9) | |||||
| AHEI c | 42.6 (10.4) | 43.5 (9.9) | 43.7 (10.2) | 44.3 (10.2) | 43.7 (10.0) | |||||
| Physical activity, METS /wk d | 18.9 (21.4) | 23.2 (31.4) | 22.4 (28.7) | 22.6 (31.1) | 22.8 (30.4) | |||||
| Smoking history before pregnancy b | ||||||||||
| Never | 75.3 | 74.0 | 73.1 | 63.2 | 71.9 | |||||
| Past | 18.2 | 19.6 | 20.2 | 26.3 | 20.9 | |||||
| Current | 6.5 | 6.4 | 6.7 | 10.5 | 7.2 | |||||
| Husbands holding a graduate degree | 31.9 | 36.5 | 37.1 | 31.1 | 35.9 | |||||
| Mom’s chronotype | ||||||||||
| Definite morning type | 31.9 | 36.0 | 34.4 | 37.4 | 35.6 | |||||
| Intermediate type | 56.9 | 55.0 | 55.6 | 52.1 | 54.8 | |||||
| Definite evening type | 11.2 | 9.0 | 10.0 | 10.5 | 9.6 | |||||
| Parity before first included pregnancy | ||||||||||
| Nulliparity | 20.3 | 21.8 | 22.0 | 20.5 | 21.6 | |||||
| One previous pregnancy | 32.4 | 29.0 | 30.0 | 30.7 | 29.7 | |||||
| Two previous pregnancies | 24.0 | 25.8 | 26.0 | 25.2 | 25.8 | |||||
| Three previous pregnancies | 23.3 | 23.4 | 22.0 | 23.6 | 22.9 | |||||
| Number of pregnancies, n | 1,683 | 1,507 | 1,132 | 491 | 3,130 | |||||
| Gestational diabetes | 4.9 | 5.9 | 5.1 | 6.5 | 5.7 | |||||
| Pre-eclampsia | 2.3 | 2.4 | 3.3 | 2.7 | 2.8 | |||||
| Gestational hypertension | 4.1 | 3.7 | 5.0 | 5.3 | 4.4 | |||||
| Cesarean delivery | 21.6 | 21.6 | 23.7 | 27.1 | 23.2 | |||||
| Gestational age ≥42 wks | 4.7 | 4.8 | 4.3 | 4.9 | 4.7 | |||||
| Maternal change in BMI, from before to after current pregnancy | 1.0 (1.7) | 1.0 (1.6) | 1.1 (1.7) | 1.0 (1.8) | 1.1 (1.7) | |||||
| Offspring gender | ||||||||||
| Male | 46.0 | 45.0 | 48.2 | 49.3 | 46.8 | |||||
| Female | 54.0 | 55.0 | 51.8 | 50.7 | 53.2 | |||||
| Offspring age at GUTS2 baseline 2004 | 11.8 (1.2) | 11.6 (1.2) | 11.6 (1.2) | 11.6 (1.3) | 11.6 (1.2) | |||||
| Offspring Tanner stage e | 2.8 (1.3) | 2.6 (1.3) | 2.6 (1.3) | 2.7 (1.3) | 2.6 (1.3) | |||||
| Offspring weekly hrs sedentary behavior e | 4.0 (2.8) | 3.9 (2.7) | 3.9 (2.5) | 4.1 (2.4) | 3.9 (2.6) | |||||
Abbreviations: AHEI, Alternative Healthy Eating Index; METS, metabolic-equivalent hours; SD, standard deviation;
Percentages are of non-missing values.
Recorded on the most recent questionnaire prior to conception of first included offspring
Recorded in 1991
One metabolic-equivalent-hour is proportional to the amount of energy spent sitting quietly for one hour.
At GUTS2 baseline (2004)
Overall, when we evaluated the associations between night shift work history before pregnancy with different weight outcomes across childhood and adolescence, we observed few differences in offspring weight comparing women with and without night shift work history (Table 2). Because differences between basic and multivariable models were small, we describe results of fully-adjusted models only (i.e., MV models 1 including the most important confounding variables).
There were no associations of history of shiftwork with birth weight or somatotype at age 5 (Table 2). We did find a significantly higher risk of the offspring having overweight or obesity at any time during follow-up between 2004 and 2013 for mothers with any history of night shift work before pregnancy (MV RRany 1.11, 95% CI, 1.02–1.21) when compared to mothers who never worked any night shifts (Table 2). The association was slightly more pronounced for the risk of persistently having overweight or obesity (MV RRany 1.25, 95% CI, 1.00–1.56). However, there was no evidence of a dose-response association with increasing number of years of night shift work history (overweight/obese MV RRextreme 1.07, 95%CI, 0.92–1.23; Ptrend =0.14; persistently overweight/obese MV RRextreme 1.04, 95%CI, 0.71–1.52; Ptrend =0.17). Longer duration of night shift work was not associated with changes in BMI with age (Ptrend>0.34), but was associated with greater differences in mean BMI (Ptrend<0.01) at baseline age (Table 2).
Since maternal diet was first assessed in 1991, we conducted a sensitivity analysis, including only children who were born after 1991, and results remained largely unchanged. In addition to adjustment for maternal BMI, we examined whether associations were different in children born to normal weight versus overweight or obese mothers. Formal tests for interactions revealed no significant effect modification (Pinteraction for all outcomes >0.43). When examining whether associations were different in children born to mothers with reportedly different chronotypes (evening versus morning chronotypes), tests for interaction were not significant (all Pinteraction > 0.44).
Maternal night shift work exposure during pregnancy
Mothers included in the analyses exploring associations between night shift work during pregnancy and weight outcomes in their offspring were on average 34.7 (SD=3.3) years old when they gave birth to the children considered in this analysis, while these children were on average 10.0 (SD=0.6) years old at enrollment in GUTS2 (Table 1b). Of 545 women total, 110 women (20.2%) had worked night shifts during their pregnancy; they worked a mean of 6.0 (SD=4.8) night shifts per month (range 0.5 and 16 night shifts per month). Mothers reporting a higher number of night shifts were more likely to be either current or past smokers and more likely to describe themselves as definite evening chronotypes compared to women who did not work night shifts during pregnancy. They also exercised less and adhered to a less healthy diet than mothers with no night shift work during pregnancy.
Table 1b.
Maternal and Offspring Characteristics by Categories of Average Number of Night Shifts per Month During Pregnancy, for 545 Mothers and the 545 Children, born between 1993 and 1995, Enrolled in GUTS2 with Whom They Were Pregnant During Reported Night Work.
| Characteristics | Average number of night shifts/month during pregnancy | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| None (n=435) |
<3 nights/mo (n=44) |
3–9 nights/mo (n=21) |
≥10 nights/mo (n=45) |
Any no. nights/mo (n=110) |
||||||
| Mean (SD) | %a | Mean (SD) | % | Mean (SD) | % | Mean (SD) | % | Mean (SD) | % | |
| Maternal age at delivery b | 34.9 (3.4) | 33.8 (2.5) | 34.4 (2.8) | 34.0 (3.1) | 34.0 (2.8) | |||||
| BMI before pregnancy, | 23.9 (4.5) | 23.1 (3.6) | 22.8 (3.4) | 24.1 (4.1) | 23.5 (3.8) | |||||
| AHEI c | 42.7 (9.9) | 44.4 (11.6) | 40.3 (8.9) | 38.4 (9.4) | 41.0 (10.5) | |||||
| Physical activity, METS/wk d | 23.2 (34.0) | 23.9 (27.2) | 13.3 (13.1) | 17.7 (19.6) | 19.3 (22.2) | |||||
| Smoking before pregnancy b | ||||||||||
| Never | 76.0 | 72.7 | 76.2 | 71.1 | 72.7 | |||||
| Past | 18.7 | 25.0 | 14.3 | 22.2 | 21.8 | |||||
| Current | 5.3 | 2.3 | 9.5 | 6.7 | 5.5 | |||||
| Husband holding a graduate degree | 29.4 | 22.7 | 33.3 | 24.4 | 25.5 | |||||
| Mom’s chronotype, | ||||||||||
| Definite morning type | 29.6 | 43.6 | 10.0 | 20.5 | 27.6 | |||||
| Intermediate type | 60.6 | 41.0 | 70.0 | 51.3 | 51.0 | |||||
| Definite evening type | 9.8 | 15.4 | 20.0 | 28.2 | 21.4 | |||||
| Parity | ||||||||||
| Nulliparity | 6.0 | 5.4 | 0 | 15.4 | 8.5 | |||||
| One previous pregnancy | 28.3 | 29.7 | 33.3 | 28.2 | 29.8 | |||||
| Two previous pregnancies | 32.7 | 37.9 | 33.3 | 23.1 | 30.8 | |||||
| Three previous pregnancies | 33.0 | 27.0 | 33.3 | 33.3 | 30.9 | |||||
| History of rotating night shift work, | ||||||||||
| None | 34.7 | 6.8 | 14.3 | 35.6 | 20.0 | |||||
| <3 years | 36.6 | 40.9 | 33.3 | 24.4 | 32.7 | |||||
| 3–5 years | 21.6 | 31.8 | 38.1 | 24.4 | 30.0 | |||||
| ≥6 years | 7.1 | 20.5 | 14.3 | 15.6 | 17.3 | |||||
| Number of pregnancies, n | 435 | 44 | 21 | 45 | 110 | |||||
| Gestational Diabetes | 6.4 | 2.3 | 4.8 | 4.4 | 3.6 | |||||
| Pre-eclampsia | 0.9 | 0.0 | 0.0 | 2.2 | 0.9 | |||||
| Gestational hypertension | 3.0 | 2.3 | 0.0 | 6.7 | 3.6 | |||||
| Cesarean delivery | 22.3 | 18.2 | 14.3 | 20.0 | 18.2 | |||||
| Gestational age ≥42 wks | 5.8 | 9.1 | 0.0 | 2.2 | 4.6 | |||||
| Maternal change in BMI, from before to after the current pregnancy | 0.8 (1.7) | 0.6 (1.9) | 0.8 (1.7) | 1.2 (2.0) | 0.9 (1.9) | |||||
| Offspring gender | ||||||||||
| Male | 45.3 | 52.3 | 47.6 | 42.2 | 47.3 | |||||
| Female | 54.7 | 47.7 | 52.4 | 57.8 | 52.7 | |||||
| Offspring age at baseline 2004 | 10.0 (0.6) | 9.9 (0.6) | 10.0 (0.6) | 10.0 (0.6) | 10.0 (0.6) | |||||
| Offspring Tanner stage e | 1.5 (0.7) | 1.6 (0.8) | 1.5 (0.8) | 1.5 (0.8) | 1.5 (0.8) | |||||
| Offspring weekly hrs sedentary behavior e | 3.5 (2.3) | 3.1 (1.5) | 3.9 (2.5) | 4.1 (2.4) | 3.7 (2.1) | |||||
Abbreviations: AHEI, Alternative Healthy Eating Index; METS, metabolic-equivalent hours; SD, standard deviation;
Percentages are of non-missing values.
Recorded on the most recent questionnaire prior to conception of first included offspring
Recorded in 1991
One metabolic-equivalent-hour is proportional to the amount of energy spent sitting quietly for one hour.
At GUTS2 baseline (2004)
Because estimates comparing results from base and multivariable-adjusted models were similar, we report results from the fully-adjusted models (MV model 1) only. We found no associations of night shiftwork during pregnancy with offspring birth weight, offspring somatotype at age 5, or relative risk of having overweight or obesity (Table 3); we were unable to examine the risk for persistently having overweight/obesity due to small numbers. We observed no differences in change in BMI at baseline age or over time across exposure groups.
When investigating potential effect modification by maternal BMI before pregnancy and mother’s chronotype using collapsed exposure categories (no night shifts, 1–5 nights/month and ≥6 nights per month), we did not find evidence for effect modification by maternal BMI (Pinteraction for all outcomes >0.13) or mother’s chronotype (all Pinteraction >0.28).
Discussion
In this study conducted among NHS II participants and their children enrolled in GUTS2, we found little evidence to support the hypothesis that history of night shift work before pregnancy or higher frequency of night shiftwork during pregnancy increases the risk of adverse weight outcomes in offspring during childhood and adolescence. Although we observed a modest association between a history of night shift work before pregnancy and offspring’s risk of having overweight or obesity, there was no dose-response association with longer duration of night shiftwork before pregnancy, and other weight outcomes were not related to mother’s shift work history before or during pregnancy.
Animal studies have suggested that perturbations at critical windows of development can cause life-long alterations in adiposity (29). More particularly, studies in rats have demonstrated that disruptions of the maternal photoperiod (i.e. exposing pregnant rats to chronic phase shifts, thereby mimicking shift work) negatively influences several metabolic parameters in the subsequent adult offspring, such as increased adiposity, hyperleptinaemia, hyperinsulinaemia, and reduced glucose tolerance and insulin sensitivity (12, 13, 30). A recent study modeling the impact of circadian disruption through mice with knockout clock genes did not find any of these associations. However, the authors suggested that previous findings might be explained by mediation through other pathways activated by circadian disruption that may not have been activated in the knockout gene experiment (14).
Previous meta-analyses consistently suggested no association between shift work exposure during pregnancy and pre-term birth (11, 31, 32) or low birth weight (31, 32), which is in line with our findings. We too did not observe any associations between shift work during pregnancy and birth weight even after adjusting for maternal pre-pregnancy night shift work history.
There are virtually no data regarding the potential long-term impacts of night shift work on weight outcomes after birth on children born to night shift workers. In our study, we observed no association between night shift work before or during pregnancy and offspring childhood somatotype. While a recent study has shown associations between nighttime feeding post partum and risk of overweight in early childhood (33), our study is the first to examine the relationship between circadian disruption before and during pregnancy and offspring early life weight outcomes. We did find a modestly increased risk for the offspring having overweight or obesity among offspring born to mothers who worked night shifts at any time before pregnancy, but the risk did not increase with longer duration of shiftwork. Night work during pregnancy did not further alter this association.
To the best of our knowledge, there is no inter-generational study thus far relating pre-conception shift work exposure and shift work during pregnancy to offspring outcomes during childhood and adolescence. Strengths of the current study include the longitudinal follow up of mothers and children, and detailed information on multiple potential confounders including shift work information during pregnancy. However, our study also has several limitations. We only had limited information on paternal factors. Nevertheless, in all our multivariable models we adjusted for husband’s education, a proxy for socioeconomic status and important confounding variable possibly affecting both maternal shift work exposure and offspring weight outcomes. Most mothers gave birth to respective child included in our study relatively late, i.e. in their early to mid 30ies. Hence, our results might not be generalizable to women giving birth at a younger age. Further, power was limited for some secondary analyses, including for mothers who continued to work night shifts throughout their pregnancies and in analyses differentiating having overweight or obesity. Other limitations include the retrospective assessment of body size at age 5 and the self-reported nature of maternal and offspring weight measures. Previous validation studies within the Harvard cohorts (34–38) have shown reasonable accuracy of self-reported maternal physical characteristics. Studies comparing measured vs. self-reported weight and height in US-adolescents (39–41) concluded that on average self-reports are a useful proxy. Self-reported history of rotating night shift work may have been misclassified, though likely randomly, hence biasing our results only towards the null. Further, this exposure has previously been linked to several chronic disease outcomes (e.g. 42).
Conclusion
In conclusion, while women’s night shiftwork before pregnancy was associated with a modestly increased risk of having overweight or obesity in their offspring through adolescence and young adulthood, there was no overall evidence that duration of night shift work before pregnancy or night shift work during pregnancy was associated with offspring adiposity in this study. Further studies with larger sample sizes and more detailed information on shift work exposure and outcomes into adulthood as well as more specific markers of metabolic alterations during adulthood are needed.
What is already known about this subject?
Several childhood and/or adulthood health outcomes are probably in part programmed during pregnancy
Night shift work and the resulting disruption of social and biological rhythms is a risk factor for several chronic diseases and epigenetics alterations
Animal models suggest that maternal circadian disruption can induce long-term metabolic changes in the offspring
What does the study add?
First inter-generational study in humans relating pre-conception shift work exposure and shift work during pregnancy to offspring outcomes during childhood and adolescence.
Children of women who worked rotating night shifts before pregnancy had a modestly elevated risk of having overweight in our study
Longer duration of rotating night shift work before pregnancy or night shift work during pregnancy were not associated with any of these weight outcomes
Acknowledgements
We thank the thousands of participants in the Growing Up Today Study 2, as well as their mothers.
Funding/Support: This study was supported by Center for Disease Control and Prevention/The National Institute for Occupational Safety and Health grant 5R01OH009803 (PI: Schernhammer E), as well as grants UM1 CA176726 from the National Institute of Health.
Role of the Funder/Sponsor: The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Conflict of Interest Disclosures: None reported
References
- 1.Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384(9945):766–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lobstein T, Baur L, Uauy R, TaskForce IIO. Obesity in children and young people: a crisis in public health. Obes Rev. 2004;5 Suppl 1:4–104. [DOI] [PubMed] [Google Scholar]
- 3.Vos MB, Welsh J. Childhood obesity: update on predisposing factors and prevention strategies. Curr Gastroenterol Rep. 2010;12(4):280–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Burton GJ, Fowden AL, Thornburg KL. Placental Origins of Chronic Disease. Physiol Rev. 2016;96(4):1509–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gaillard R Maternal obesity during pregnancy and cardiovascular development and disease in the offspring. Eur J Epidemiol. 2015;30(11):1141–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vyas MV, Garg AX, Iansavichus AV, Costella J, Donner A, Laugsand LE, et al. Shift work and vascular events: systematic review and meta-analysis. Bmj. 2012;345:e4800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Straif K, Baan R, Grosse Y, Secretan B, El Ghissassi F, Bouvard V, et al. Carcinogenicity of shift-work, painting, and fire-fighting. The Lancet Oncology. 2007;8(12):1065–6. [DOI] [PubMed] [Google Scholar]
- 8.Knutsson A, Kempe A. Shift work and diabetes--a systematic review. Chronobiol Int. 2014;31(10):1146–51. [DOI] [PubMed] [Google Scholar]
- 9.Zhu Y S R, Hoffman AE, Tjonneland A, Vogel UB, Zheng T, Hansen J. Epigenetic impact of long-term shiftwork: pilot evidence from circadian genes and whole-genome methylation analysis. Chronobiology international. 2011;28(11):852–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bonde JP, Jorgensen KT, Bonzini M, Palmer KT. Miscarriage and occupational activity: a systematic review and meta-analysis regarding shift work, working hours, lifting, standing, and physical workload. Scand J Work Environ Health. 2013;39(4):325–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.van Melick MJ, van Beukering MD, Mol BW, Frings-Dresen MH, Hulshof CT. Shift work, long working hours and preterm birth: a systematic review and meta-analysis. International archives of occupational and environmental health. 2014;87(8):835–49. [DOI] [PubMed] [Google Scholar]
- 12.Mendez N, Halabi D, Spichiger C, Salazar ER, Vergara K, Alonso-Vasquez P, et al. Gestational Chronodisruption Impairs Circadian Physiology in Rat Male Offspring, Increasing the Risk of Chronic Disease. Endocrinology. 2016;157(12):4654–68. [DOI] [PubMed] [Google Scholar]
- 13.Varcoe TJ, Wight N, Voultsios A, Salkeld MD, Kennaway DJ. Chronic phase shifts of the photoperiod throughout pregnancy programs glucose intolerance and insulin resistance in the rat. PloS one. 2011;6(4):e18504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Varcoe TJ, Voultsios A, Gatford KL, Kennaway DJ. The impact of prenatal circadian rhythm disruption on pregnancy outcomes and long-term metabolic health of mice progeny. Chronobiology international. 2016;33(9):1171–81. [DOI] [PubMed] [Google Scholar]
- 15.Whelan EA, Lawson CC, Grajewski B, Hibert EN, Spiegelman D, Rich-Edwards JW. Work schedule during pregnancy and spontaneous abortion. Epidemiology (Cambridge, Mass). 2007;18(3):350–5. [DOI] [PubMed] [Google Scholar]
- 16.Tomeo CA, Rich-Edwards JW, Michels KB, Berkey CS, Hunter DJ, Frazier AL, et al. Reproducibility and validity of maternal recall of pregnancy-related events. Epidemiology. 1999;10(6):774–7. [PubMed] [Google Scholar]
- 17.Must A, Willett WC, Dietz WH. Remote recall of childhood height, weight, and body build by elderly subjects. Am J Epidemiol. 1993;138(1):56–64. [DOI] [PubMed] [Google Scholar]
- 18.Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. Bmj. 2000;320(7244):1240–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Willett WC, Sampson L, Stampfer MJ, Rosner B, Bain C, Witschi J, et al. Reproducibility and validity of a semiquantitative food frequency questionnaire. American journal of epidemiology. 1985;122(1):51–65. [DOI] [PubMed] [Google Scholar]
- 20.McCullough ML, Feskanich D, Stampfer MJ, Giovannucci EL, Rimm EB, Hu FB, et al. Diet quality and major chronic disease risk in men and women: moving toward improved dietary guidance. Am J Clin Nutr. 2002;76(6):1261–71. [DOI] [PubMed] [Google Scholar]
- 21.Ainsworth BE, Haskell WL, Leon AS, Jacobs DR Jr., Montoye HJ, Sallis JF, et al. Compendium of physical activities: classification of energy costs of human physical activities. Medicine and science in sports and exercise. 1993;25(1):71–80. [DOI] [PubMed] [Google Scholar]
- 22.Morris NM, Udry JR. Validation of a self-administered instrument to assess stage of adolescent development. J Youth Adolesc. 1980;9(3):271–80. [DOI] [PubMed] [Google Scholar]
- 23.Spiegelman D, Hertzmark E. Easy SAS calculations for risk or prevalence ratios and differences. American journal of epidemiology. 2005;162(3):199–200. [DOI] [PubMed] [Google Scholar]
- 24.Berkey CS, Colditz GA. Adiposity in adolescents: change in actual BMI works better than change in BMI z score for longitudinal studies. Annals of epidemiology. 2007;17(1):44–50. [DOI] [PubMed] [Google Scholar]
- 25.Dhana K, Zong G, Yuan C, Schernhammer ES, Zhang C, Wang X, et al. Lifestyle of women before pregnancy and the risk of offspring obesity during early childhood through early adulthood.. International journal of Obesity. 2018;doi: 10.1038/s41366-018-0052-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vetter C, Devore EE, Ramin CA, Speizer FE, Willett WC, Schernhammer ES. Mismatch of Sleep and Work Timing and Risk of Type 2 Diabetes. Diabetes care. 2015;38(9):1707–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hansen J, Lassen CF. Nested case-control study of night shift work and breast cancer risk among women in the Danish military. Occup Environ Med. 2012;69(8):551–6. [DOI] [PubMed] [Google Scholar]
- 28.Papantoniou K, Castano-Vinyals G, Espinosa A, Aragones N, Perez-Gomez B, Burgos J, et al. Night shift work, chronotype and prostate cancer risk in the MCC-Spain case-control study. Int J Cancer. 2015;137(5):1147–57. [DOI] [PubMed] [Google Scholar]
- 29.Tibu F, Hill J, Sharp H, Marshall K, Glover V, Pickles A. Evidence for sex differences in fetal programming of physiological stress reactivity in infancy. Dev Psychopathol. 2014;26(4 Pt 1):879–88. [DOI] [PubMed] [Google Scholar]
- 30.Varcoe TJ, Boden MJ, Voultsios A, Salkeld MD, Rattanatray L, Kennaway DJ. Characterisation of the maternal response to chronic phase shifts during gestation in the rat: implications for fetal metabolic programming. PloS one. 2013;8(1):e53800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bonzini M, Palmer KT, Coggon D, Carugno M, Cromi A, Ferrario MM. Shift work and pregnancy outcomes: a systematic review with meta-analysis of currently available epidemiological studies. BJOG: an international journal of obstetrics and gynaecology. 2011;118(12):1429–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Palmer KT, Bonzini M, Harris EC, Linaker C, Bonde JP. Work activities and risk of prematurity, low birth weight and pre-eclampsia: an updated review with meta-analysis. Occup Environ Med. 2013;70(4):213–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cheng TS L S, Toh JY, Cheung YB, Chan JK, Godfrey KM, Gluckman PD, Saw SM, Chong YS, Lee YS, Lek N, Chong MF, Yap F. Predominantly nighttime feeding and weight outcomes in infants. Am J Clin Nutr. 2016;104(2):380–8. [DOI] [PubMed] [Google Scholar]
- 34.Colditz GA M P, Stampfer MJ, Willett WC, Sampson L, Rosner B, Hennekens CH, Speizer FE. Validation of questionnaire information on risk factors and disease outcomes in a prospective cohort study of women. American journal of epidemiology. 1986;123(5):894–900. [DOI] [PubMed] [Google Scholar]
- 35.Colditz GA S M, Willett WC, Stason WB, Rosner B, Hennekens CH, Speizer FE. Reproducibility and validity of self-reported menopausal status in a prospective cohort study. American journal of epidemiology. 1987;126(2):319–25. [DOI] [PubMed] [Google Scholar]
- 36.Rich-Edwards JW G M, Willett WC,Hunter DJ, Stampfer MJ, Colditz GA, Manson JE. Adolescent body mass index and infertility caused by ovulatory disorder. Am J Obstet Gynecol 1994;171(1):171–7. [DOI] [PubMed] [Google Scholar]
- 37.Rimm EB S M, Colditz GA, Chute CG, Litin LB, Willett WC. Validity of self-reported waist and hip circumferences in men and women. Epidemiology. 1990;1(6):466–73. [DOI] [PubMed] [Google Scholar]
- 38.Troy LM H D, Manson JE, Colditz GA, Stampfer MJ, Willett WC. The validity of recalled weight among younger women. International journal of obesity and related metabolic disorders: journal of the International Association for the Study of Obesity. 1995;19(8):570–2. [PubMed] [Google Scholar]
- 39.Field AE A P, Rosner B. The validity of self-reported weight change among adolescents and young adults. Obesity Reviews. 2007;15(9):2357–64. [DOI] [PubMed] [Google Scholar]
- 40.Straus R Comparision of measured and self-reported weight and height in a cross-sectional sample of young adolescents. International Journal of Obesity 1999;23:904–8. [DOI] [PubMed] [Google Scholar]
- 41.Himes J, Faricy A. Validity and reliability on self-reported stature and weight of US adolescents. American Journal of Human Biology 2001;13(2):255–60. [DOI] [PubMed] [Google Scholar]
- 42.Vetter C, Devore EE, Wegrzyn LR, Massa J, Speizer FE, Kawachi I, et al. Association Between Rotating Night Shift Work and Risk of Coronary Heart Disease Among Women. Jama. 2016;315(16):1726–34. [DOI] [PMC free article] [PubMed] [Google Scholar]


